Catheter based balloon for therapy modification and positioning of tissue
a catheter and balloon technology, applied in the field of catheters, can solve the problems of cell death and tissue necrosis, etc., and achieve the effect of blocking the exposure of sensitive surrounding tissues
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
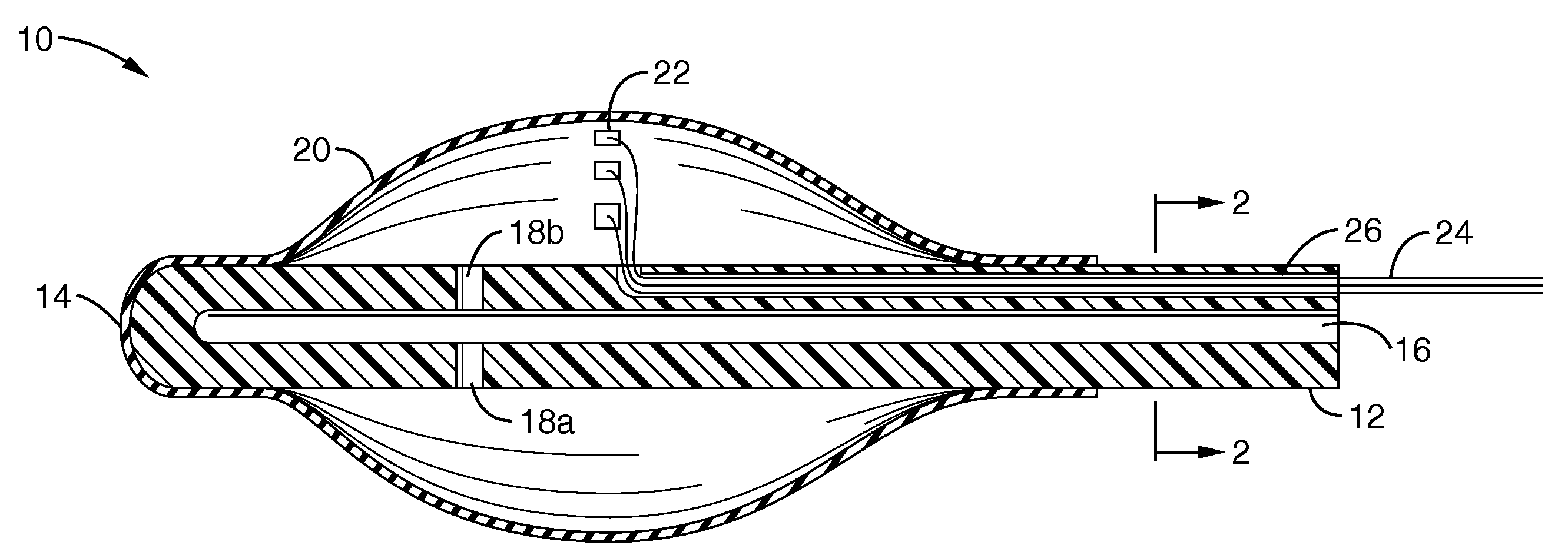
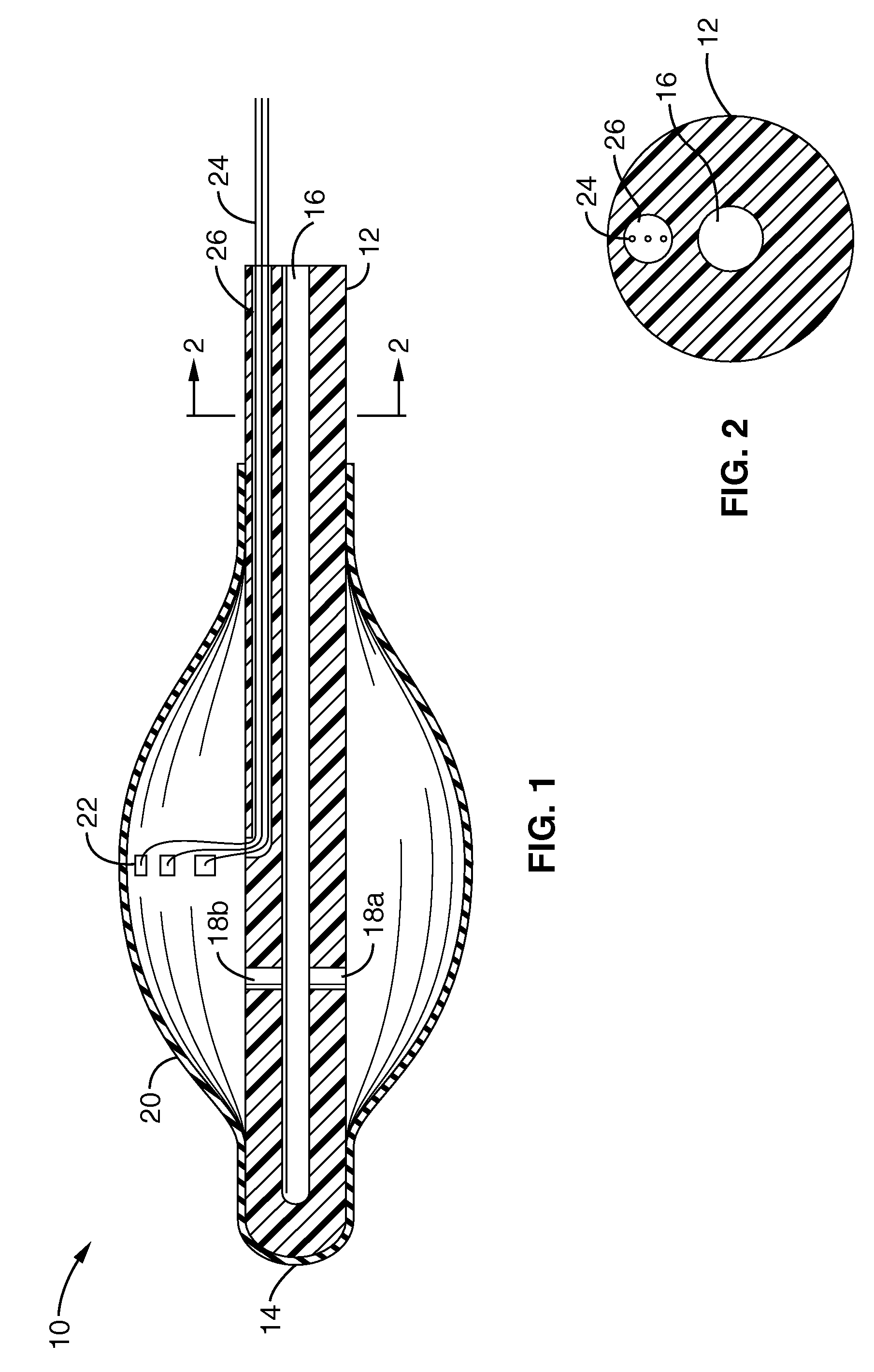
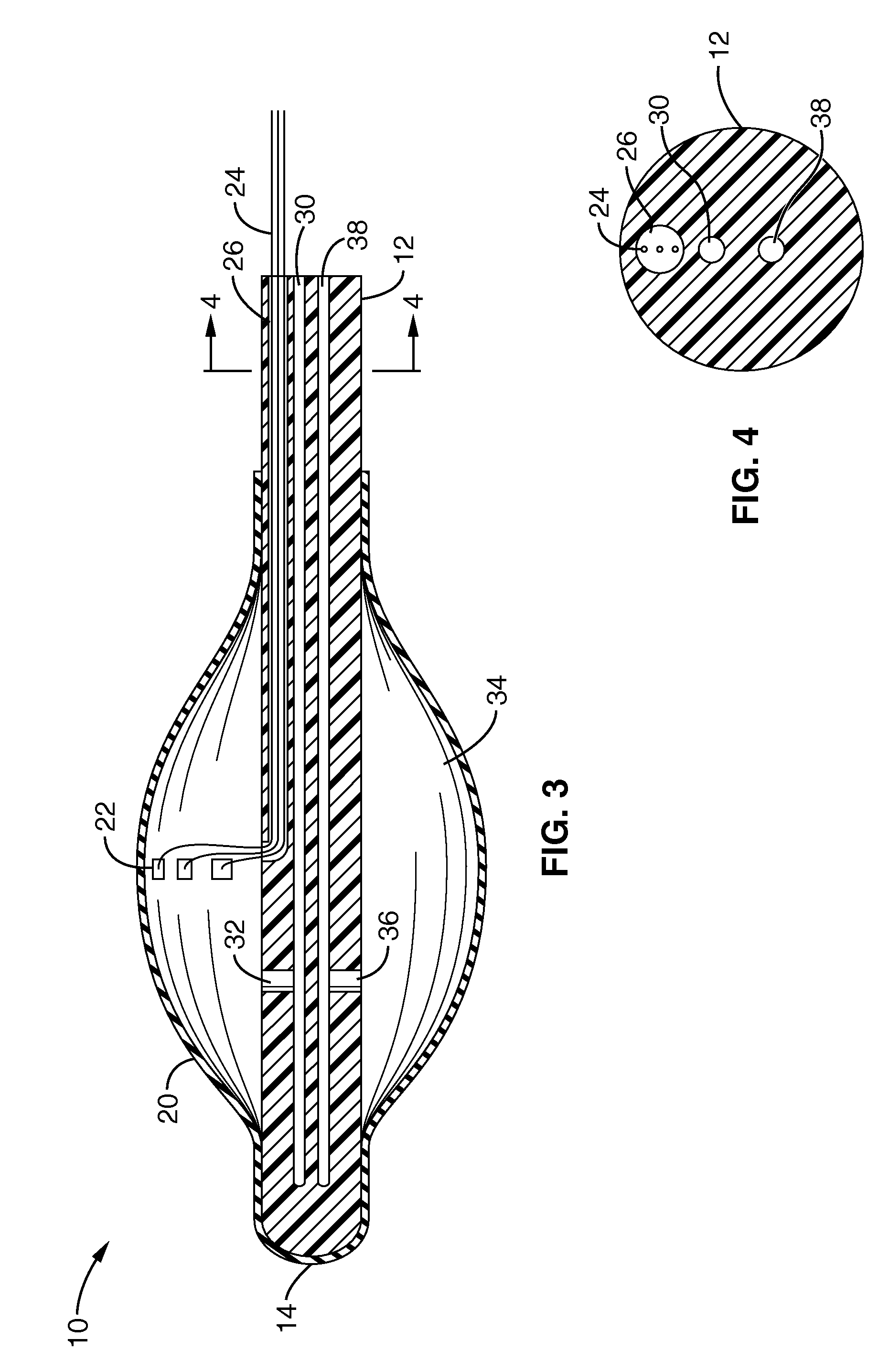
[0053]Referring more specifically to the drawings, for illustrative purposes the present invention is embodied in the apparatus and methods generally shown in FIG. 1 through FIG. 10. It will be appreciated that the apparatus may vary as to configuration and as to details of the parts, and that the methods may vary as to the specific steps and sequence, without departing from the basic concepts as disclosed herein.
[0054]Referring first to FIG. 1 and FIG. 2, the invention comprises a positioning catheter 10 with a catheter shaft 12 and tip 14 constructed for insertion into the body of a patient. The catheter shaft 12 and tip 14 may alternatively be configured to be inserted into tissue using a separate needle introduction catheter that is removed after insertion and provides protection to the components of the device during insertion. The apparatus may be used interstitially as well as laproscopically or endoscopically during procedures in the joints, abdomen, esophagus or uterus / cerv...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com