Assembled Cartilage Repair Graft
a cartilage repair and graft technology, applied in the field of assembled cartilage repair grafts, can solve the problems of reducing affecting the overall quality of life of individuals, and each have limitations ranging from the quality of cartilage repair to the cost and complexity of surgical procedures, and the procedures themselves create defects (i.e. oats). , to achieve the effect of adding extra cost and complications
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
[0203]This example demonstrates a method of making an embodiment of an assembled implant.
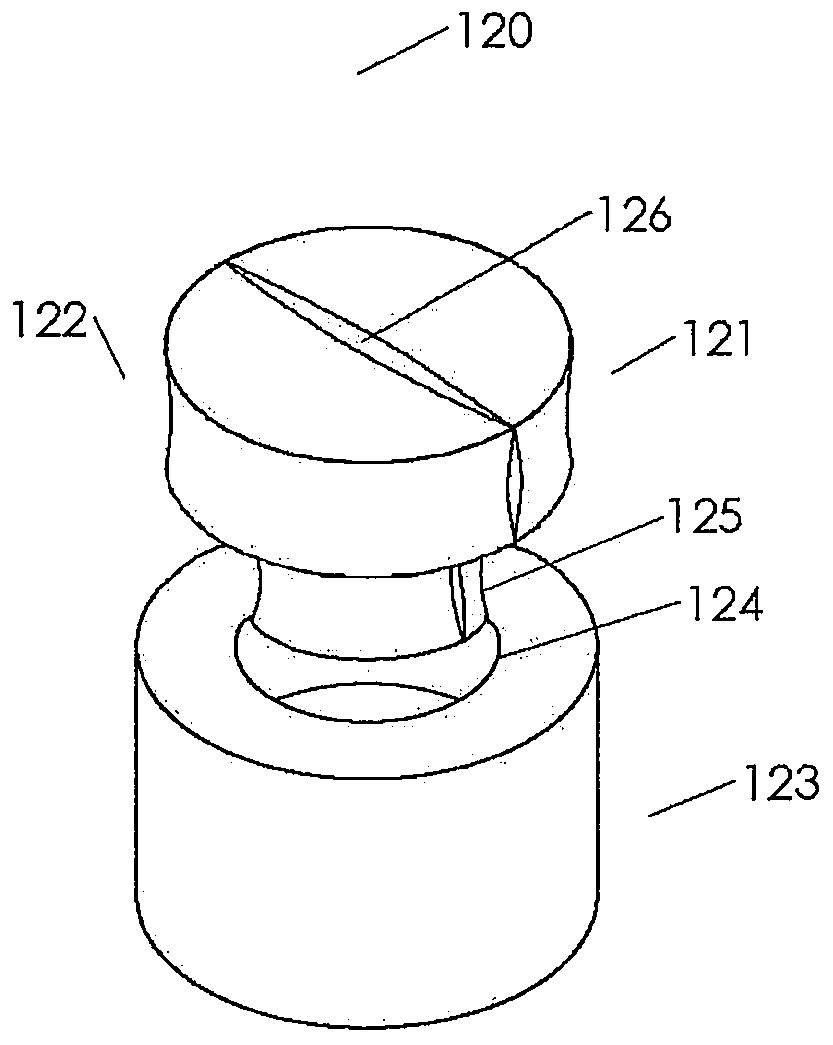
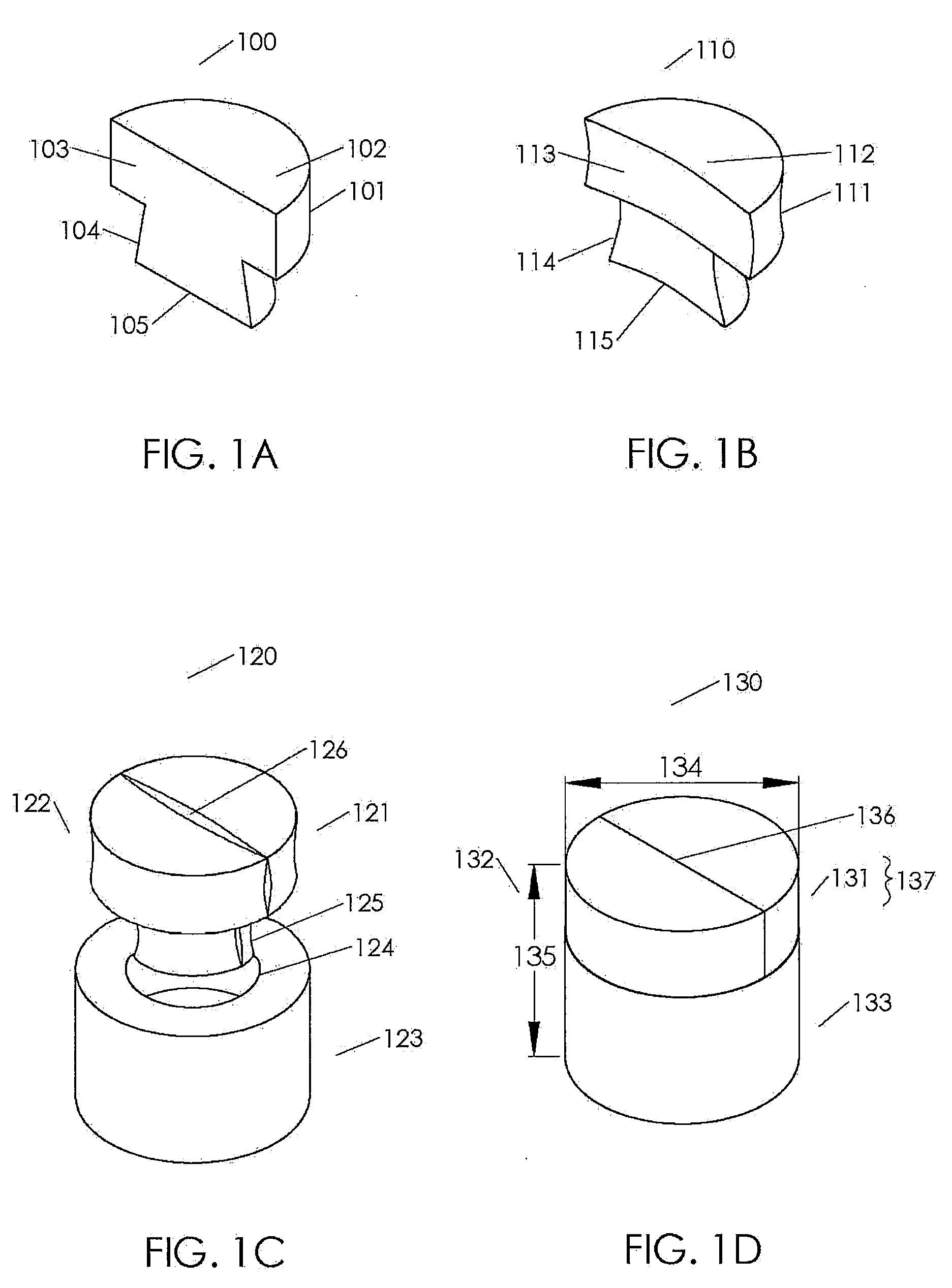
[0204]Cancellous bone was obtained from the condyles of long bones, or optionally from the Talus or heel bone. The bone was cut into blanks with diameters ranging from roughly 6-13 mm and heights from 8-10 mm using a band saw and coring tools. The inner geometry of the cancellous bone was then machined using a dovetail cutter. A 1.5 mm hole was machined in the bottom center of the 8 mm and 10 mm cancellous bone portions. The cancellous bone portions are measured, inspected for quality, packaged, and stored frozen until processing for sterilization. The cancellous bone portions were sterilized, defatted and deantigenized, and soluble protein was removed by subjecting the cancellous tissue to cyclically alternating cycles of pressure and vacuum in the sequential presence of mild sterilizing chemical solutions. Following sterilization, the cancellous bone portions were packaged and stored until ass...
example 2
[0208]This example documents an animal study completed to confirm the chondroinductivity of an implant.
[0209]Prototype implants were implanted into an ectopic site in an athymic nude rat model, resulting in histologic evidence of chondroinduction without any signs of an inflammatory response.
[0210]Specifically, a 4 mm diameter by 2 mm tall disc taken from the demineralized cortical bone portion of Example 1 was implanted in abdominal muscle pouches of athymic nude rats using a modified Urist model, Urist, M. R., “Bone: Formation by Autoinduction,” Science 160:893-894 (1965). The explants were retrieved two weeks later, processed, and evaluated histologically for evidence of new cartilage formation. The control implants made from chemically inactivated demineralized cortical bone material formed only fibrous material within the Haversian canals with minimal evidence of inflammation. More significantly, the implants made from active demineralized cortical bone demonstrated signs of ch...
example 3
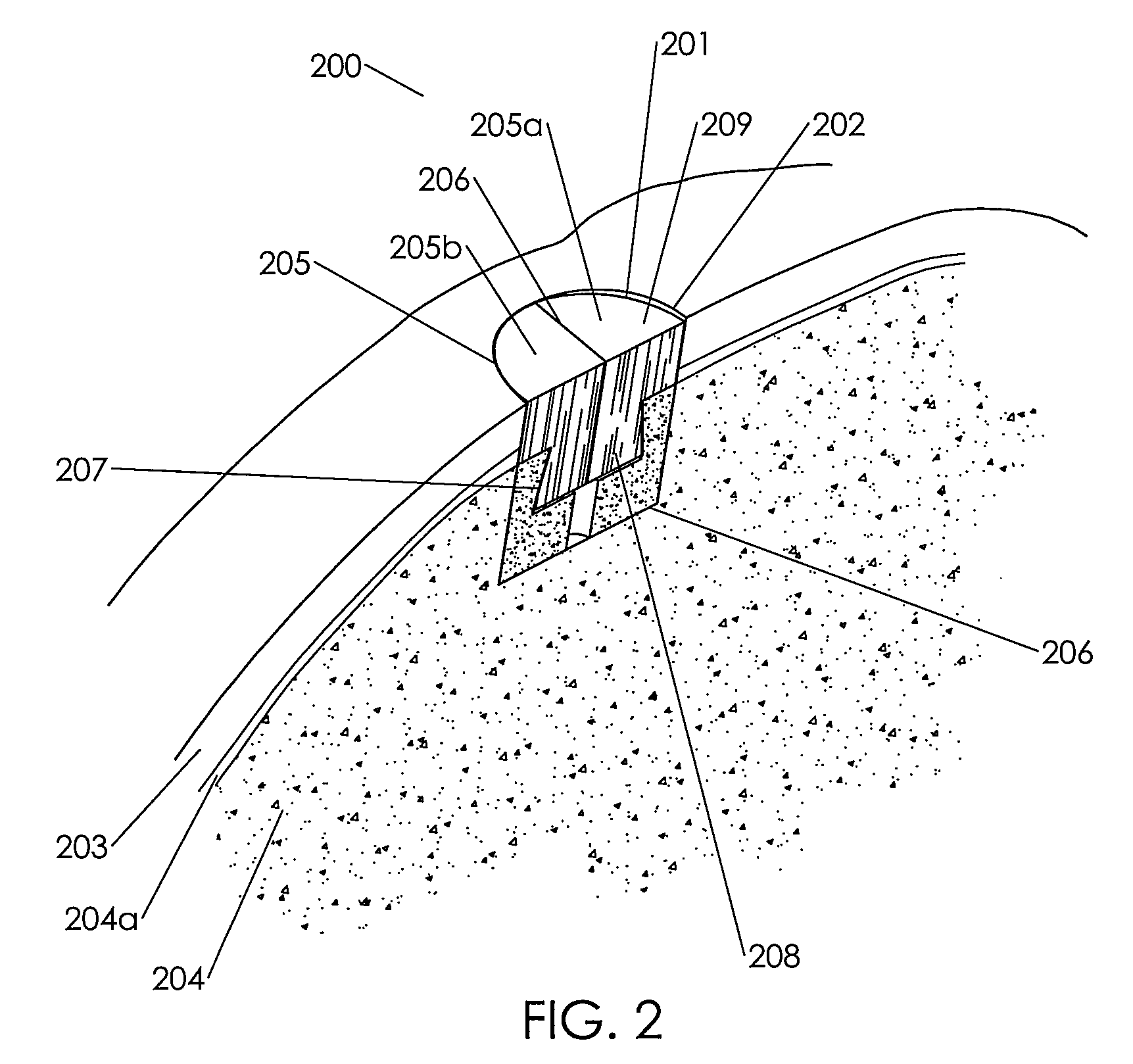
[0211]This example documents a cadaver study completed by a practicing surgeon experienced in cartilage repair at an orthopedic clinic to confirm the proper function and methods of use for the present implants.
[0212]Several primary-site implants were made to production specifications using an assembled biological implant comprising a two piece chondroinductive demineralized cortical bone cap assembled via a hydration controlled interference fit to a mineralized cancellous bone osteoconductive portion. The assembled implants were implanted into a cadaver knee using an open approach. The implants were left out at room temperature for several minutes and were then placed in room temperature saline for a minimum of ten minutes to ensure consistent final levels of hydration prior to implantation. The surgeon prepared the implantation site by coring out an 8 mm diameter plug from the primary site using an OATS single-use kit. He measured the depth of the defect using the depth gauge and v...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com