Implant for soft tissue reconstruction
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
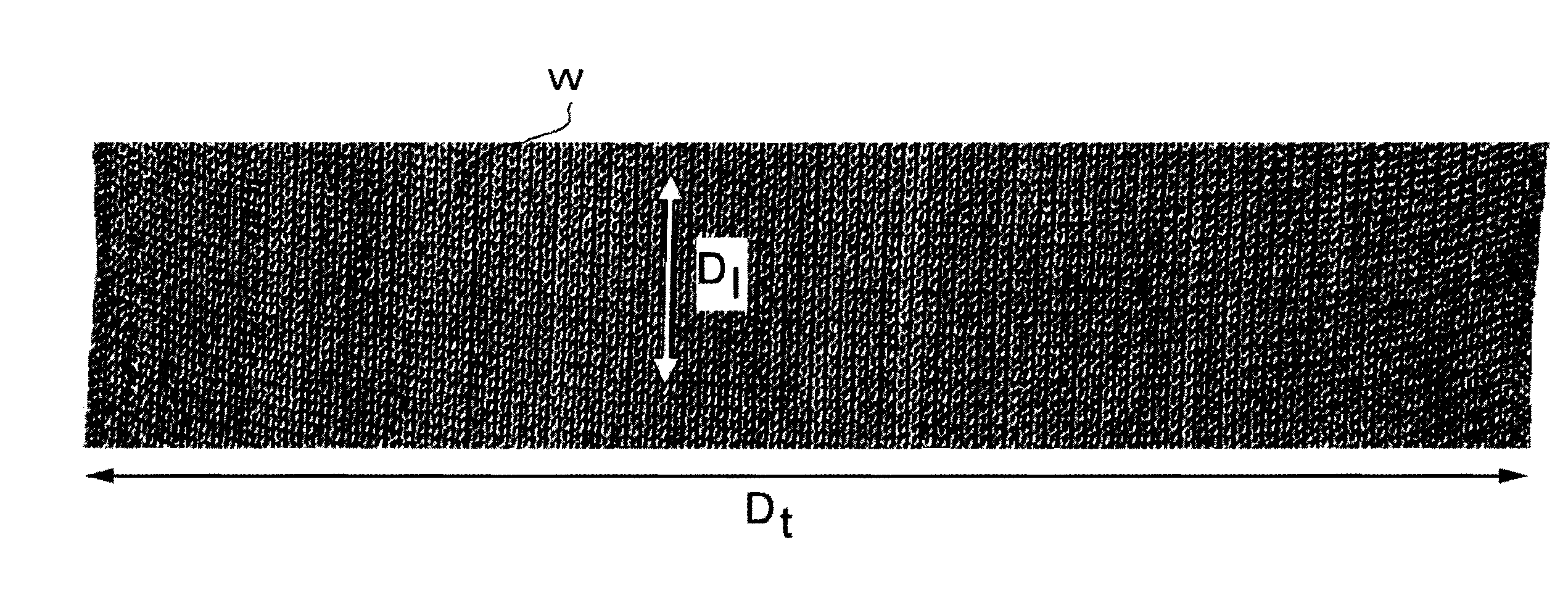
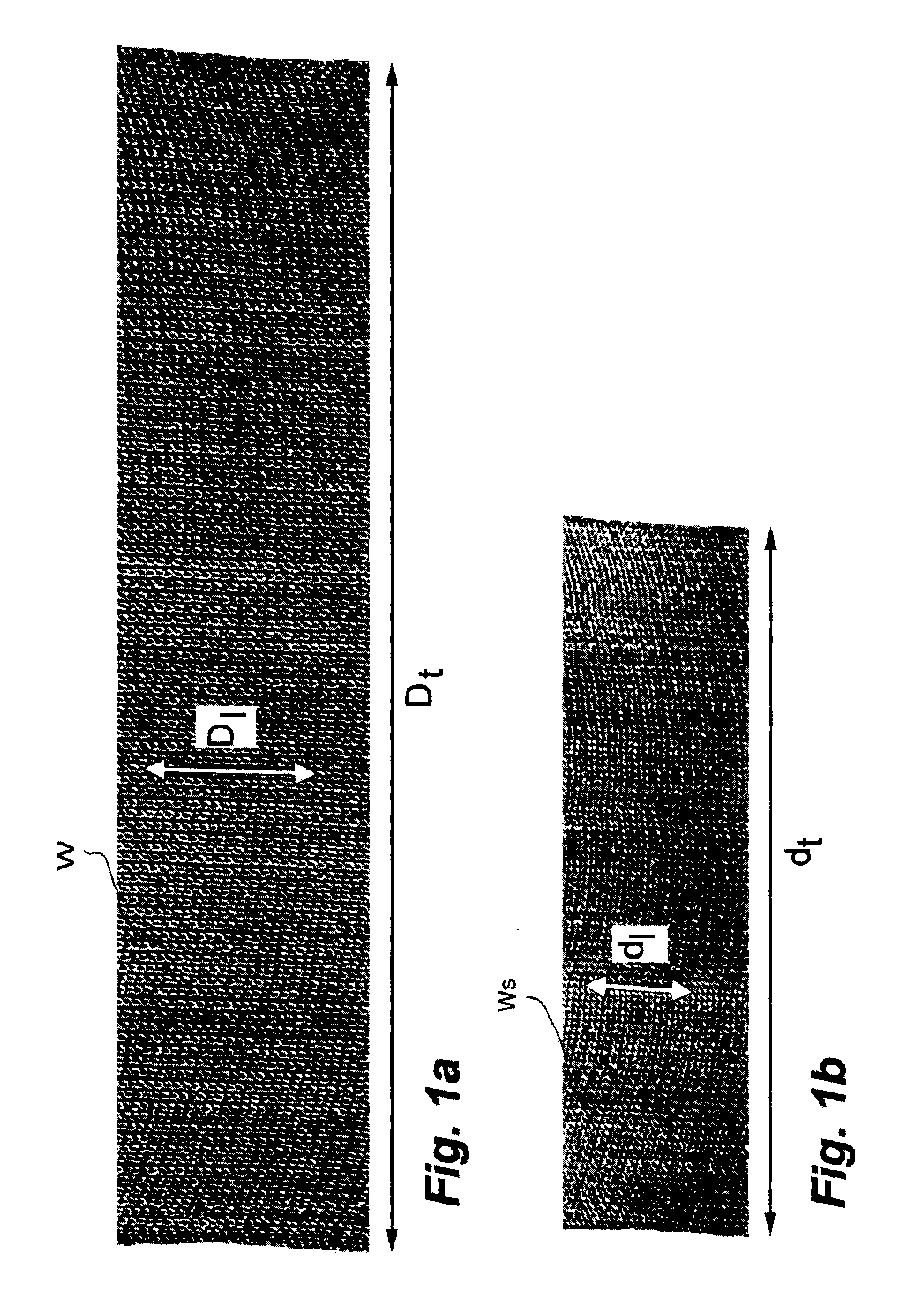
[0028]Shrunk knitted poly(urethane urea) ribbon. Yarn: 13 Tex poly(urethane urea) (Artelon®, Artimplant AB, Goteborg, Sweden). Equipment: Comez DNB / EL-800 (Comez s.p.A., Cilavegna, Italy) double needle bed crochet machine, for the production of technical and medical articles. Machine specifications: 15 gauge, 6 weft bars, double needle bed, latch needles. Heat set unit: Comez HSD / 800 comprising 2 heat-set cylinders. A plain ribbon W of 14 cm width was knit in the machine (FIG. 1). The ribbon W was shrunk in the heat set unit at 130° C. to produce a shrunk ribbon Ws at a thickness of 0.8 mm (FIG. 1).
[0029]Process parameters: Knitting speed: 26 cm / min; heat set unit speed: 14 cm / min; shrinkage along warp: about 45% (cf D1, width of ribbon W and d1, width of ribbon Ws); shrinkage across warp: about 45% (cf Dt, 20 loops, and dt, 20 loops). Warp thickness is slightly increased by shrinking. The warp knitting pattern is shown in Table 1. It is a sequence of four steps with 12 loops / cm.
TAB...
example 2
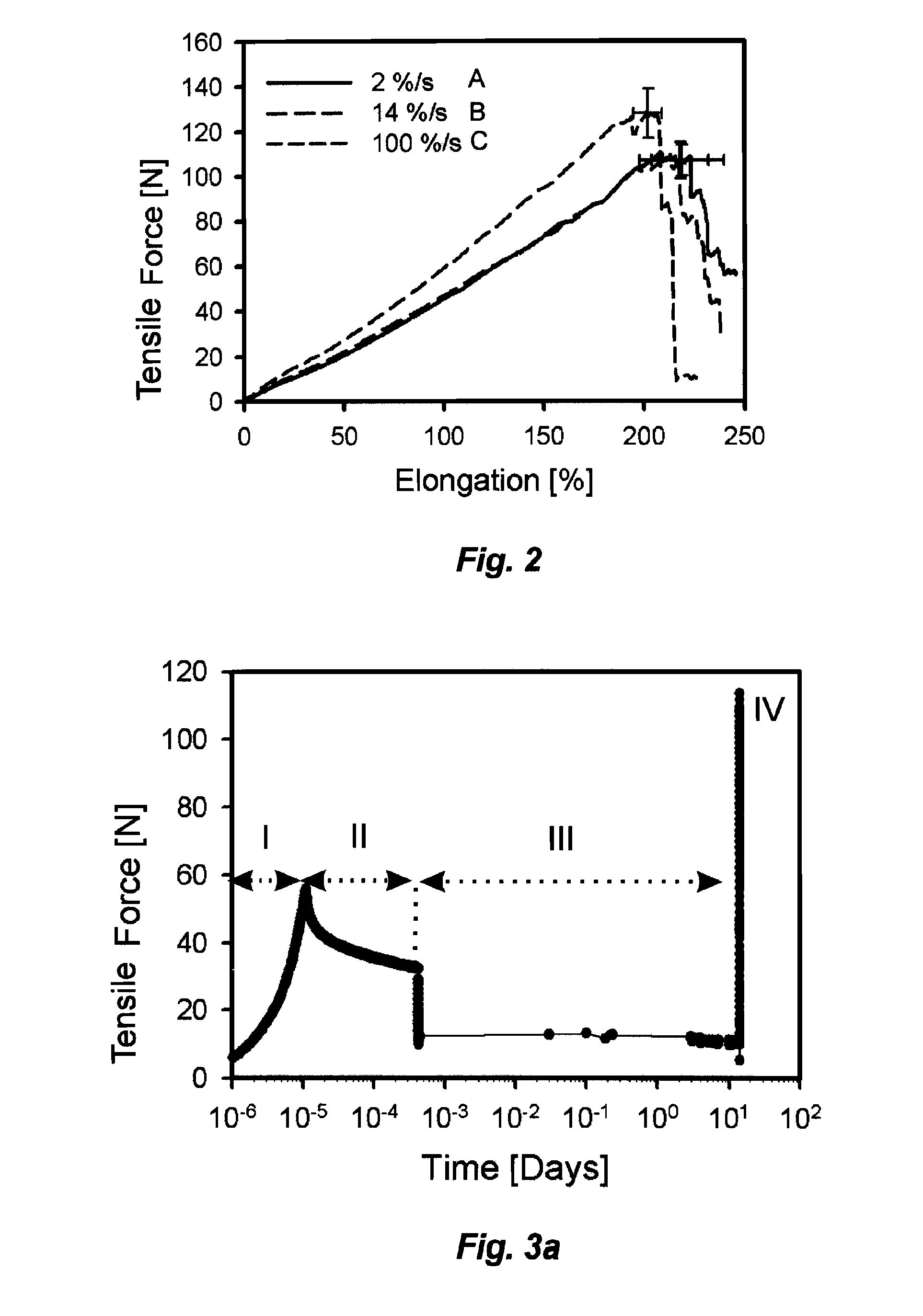
[0030]Tensile force v. elongation of strip samples of the fabric of Example 1. Ten millimeter wide strip samples were cut from the crimped knitted fabric As of Example 1. The elongation of three samples A, B, C at physiological elongation rates of 2% / s (A), 14% / s (B), and 100% / s (C) , gauge length of 20 mm, and physiological conditions, was recorded . Physiological conditions imply pH-buffered saline at 37° C. The curves for samples A and B were practically identical up 200% elongation. The samples burst at an elongation of about 220% and 230%, respectively. In contrast, sample C required an about 20% higher force for a given elongation and burst already at an elongation of about 210%.
example 3
[0031]Tensile force v. time of a sample of the fabric of Example 1. A 10 mm wide cut-out strip sample of the crimped knitted fabric As of Example 1, gauge length 20 mm, was stretched in a first step I to an elongation of 95% at about 55 N, elongation rate of 100% / s (FIG. 3a). Within a minute the force needed to keep the sample at that elongation dropped to about 35 N, step II. In a following step III the pre-stretched sample was kept at a reduced elongation of 70% for two weeks, during which period the free sample length remained constant. A bursting test at an elongation rate of 100% / s, step IV, concluded the experiment. The elongation of the sample during the stretching procedure is shown in FIG. 3b.
PUM
| Property | Measurement | Unit |
|---|---|---|
| Fraction | aaaaa | aaaaa |
| Fraction | aaaaa | aaaaa |
| Time | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com