Today, active pumping APD devices are expensive, with significant costs associated with the pump, valves, pressure sensors, and / or pneumatic manifolds, along with significant costs associated with the disposable tubing sets with cassettes to interface with said APD devices.
Additionally, excessive delivery and / or suction pressures causes inflow or outflow pain during filling or draining phases for many patients.
Today, active pumping APD devices' disposable tubing sets with cassettes are expensive.
Some cassettes may require expensive
ultrasonic welding or other technology to bond a rigid plastic cassette with a flexible thin plastic sheeting membrane, with costly high
scrap rates associated with failed sheeting bonds.
A common, serious complication of APD therapy is
peritonitis.
However, there are no shrouded female Luer fittings which mate to the dialysate bags' shrouded male Luer fittings.
An APD device's disposable tubing set without a cassette poses a potential problem with the user loading the tubing into the hardware
enclosure in the reverse orientation.
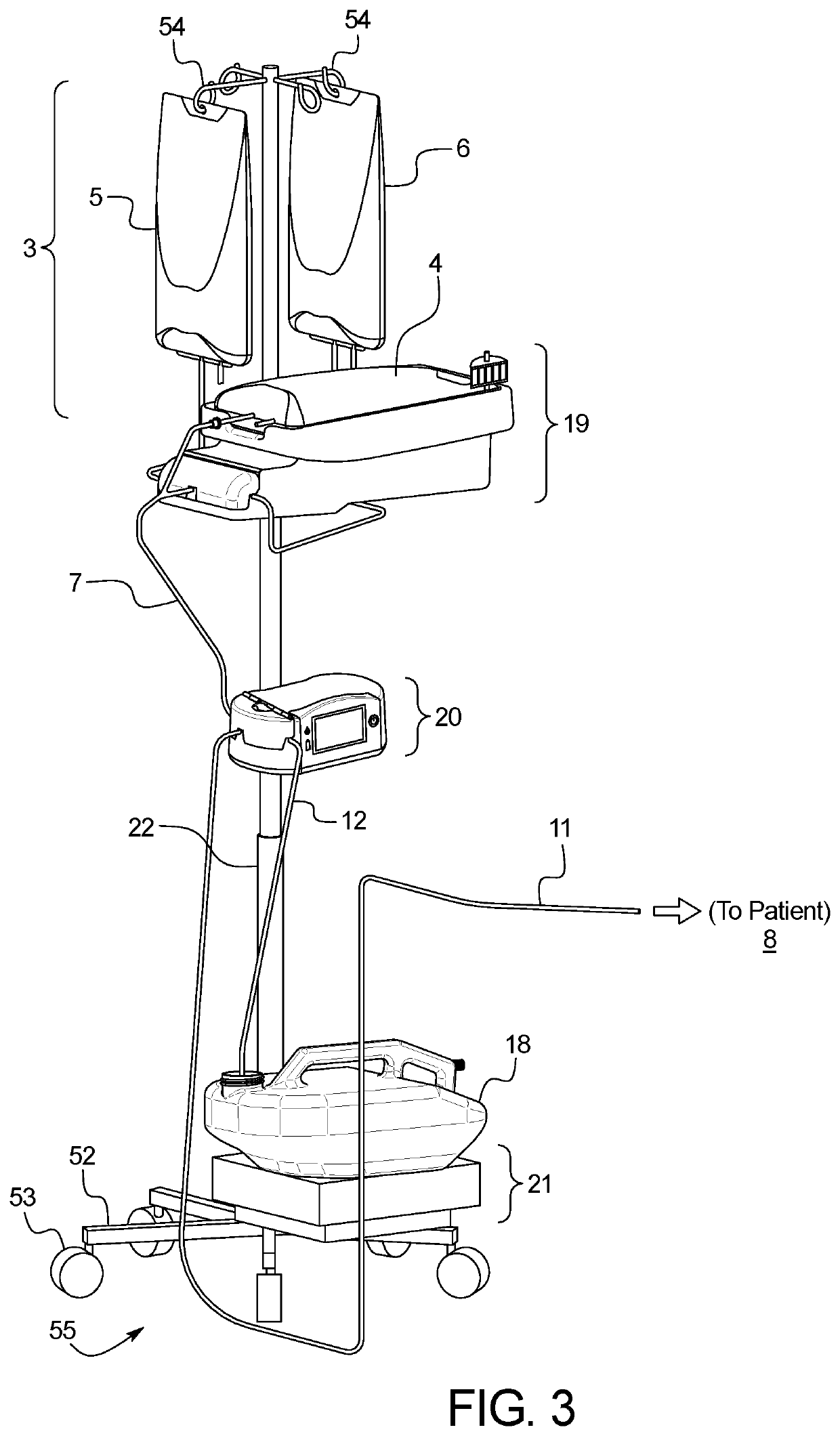
For gravity-based devices, portability poses a problem since the machines tend to be rather tall in their therapy operational position.
Free flow of fluid from an APD device resulting in unintended Increased Intraperitoneal Volume (IIPV) can be fatal to patients.
Conventionally, APD devices are often audibly noisy during operation.
They are also prone to fluid ingress.
Conventionally dialysate bags are often difficult to lift up to place them in the proper position required for therapy.
Lifting heavy dialysate bags may cause shoulder or back problems, may lead to the user losing balance and / or falling over.
These same difficulties may be experienced by caregivers who may perform setup rather than the patients themselves.
Additionally, patients and caregivers in certain regions in the globe and / or female patients may have smaller statures and may not have as much strength as others.
Additionally, many PD patients also suffer from other comorbidities or illnesses such as
diabetes mellitus, which may further reduce the patient's ability to lift heavy objects.
Existing APD devices do not provide any sort of
mechanical advantage nor any other active or passive features to assist patients or caregivers in lifting heavy bags to the proper height required to perform APD therapy.
As such, some physicians may be hesitant to prescribe APD therapy to a patient they believe may not possess the strength to lift the bags into place.
Those patients may be forced to perform
hemodialysis instead, which may not be the preferred
dialysis modality for those patients.
However, several smaller bags are more expensive to manufacture than fewer larger bags.
APD patients and / or their caregivers may be illiterate or have low literacy.
They may not be able to read text-based prompts to properly set up, monitor, tear down, or troubleshoot their APD therapy.
This will either result in a longer therapy duration or less effective therapeutic outcomes.
If it takes longer to fill due to suboptimal dialysate bag head height, then there may be less time available for dwelling.
Therefore, therapy is less effective if low flow rates result in less dwell time, for a given (e.g. 8 hour) total therapy time.
Alternatively, low flow rates could lead to longer total therapy duration, which is not desirable since patients' lives are disrupted with therapy durations that exceed the patient's normal nocturnal
sleep duration.
In some locations,
AC power outages are a frequent occurrence, each potentially lasting several hours.
Other locations may have frequent,
short duration AC power outages and / or brownouts, each lasting a few seconds or several minutes.
Additionally, if patients want to start therapy in one room within their home while performing some activity (e.g. watching TV, cooking, studying, etc), followed by movement to their
bedroom to complete therapy, there may not be AC plugs readily available in all of the locations within the home that patients may find themselves wanting to perform some or all of their APD therapy.
To date, no commercially available APD device is able to continue delivering therapy during an
AC power outage.
Currently, none of the widely available, inexpensive pinch valves are capable of opening the pincher jaws if a tube is not already installed in the valve, using the manufacturer's recommended
voltage.
Additionally, APD users may have difficulty draining the relatively large fluid volumes that may be stored in one or more reusable or disposable drain containers if the drain containers do not contain features to facilitate easy drainage.
Users may not know which method they need to use, which could result in selecting the wrong
programming method, attempting to enter their prescribed parameters, only to later realize the
user interface doesn't have the programmable option(s) they need, thus resulting in the user backing out from the
programming menu and trying to program the prescription again using the alternate
programming method.
 Login to View More
Login to View More  Login to View More
Login to View More