Device and method for forming a lesion
a technology of ablating devices and lesions, applied in the field of ablating devices and lesion formation methods, can solve the problems of difficult manipulation of elongated and flexible endovascular ablation devices into complex geometries, significant difficulties of endocardial ablation devices, and insufficient visualization of endocardial anatomy and endovascular devices, etc., to achieve the effect of eliminating air gaps
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
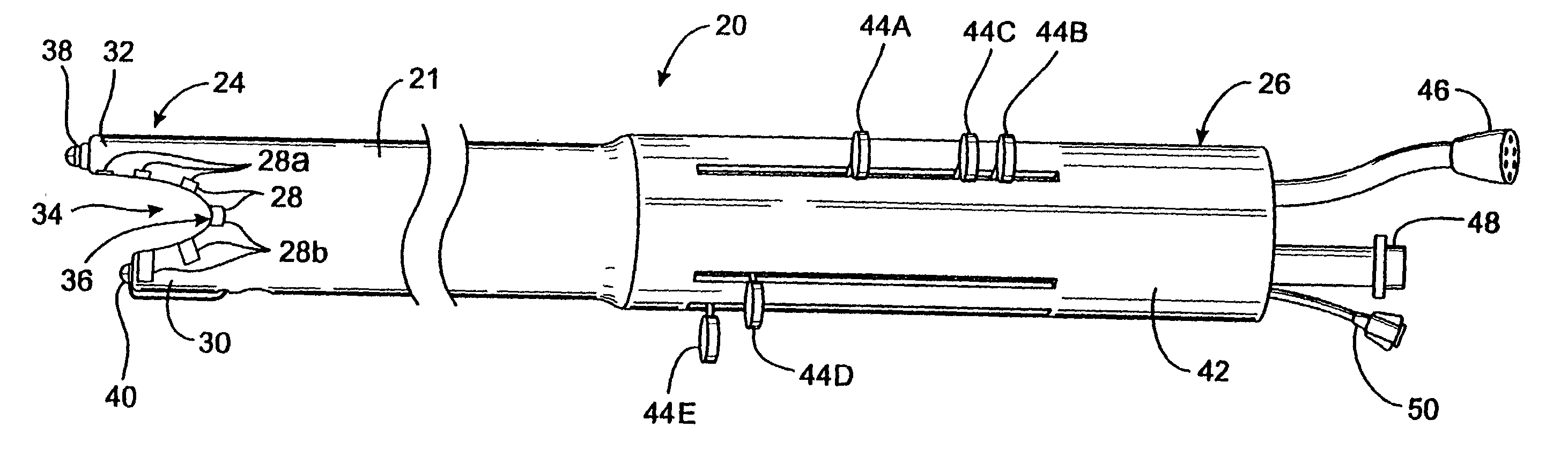
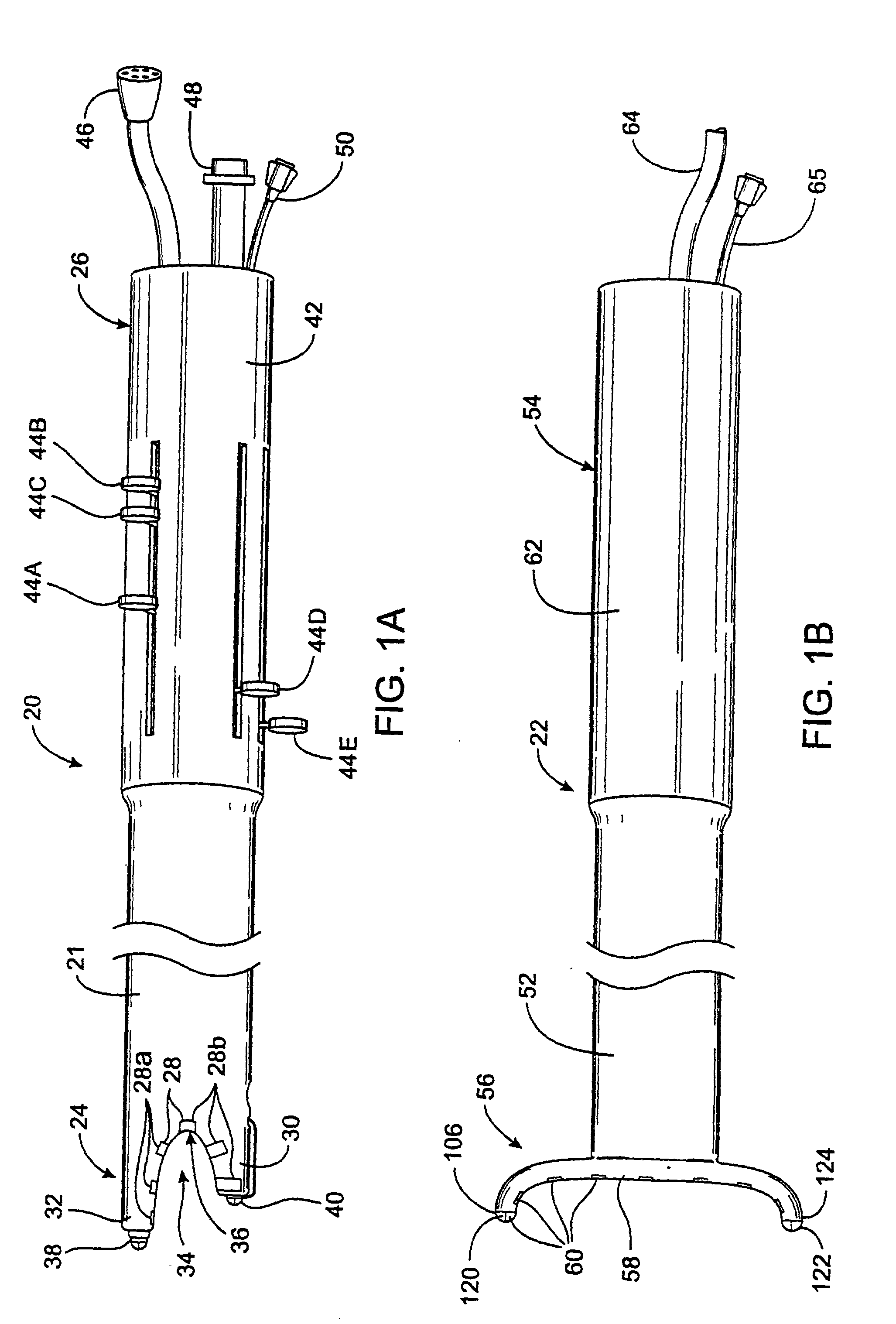
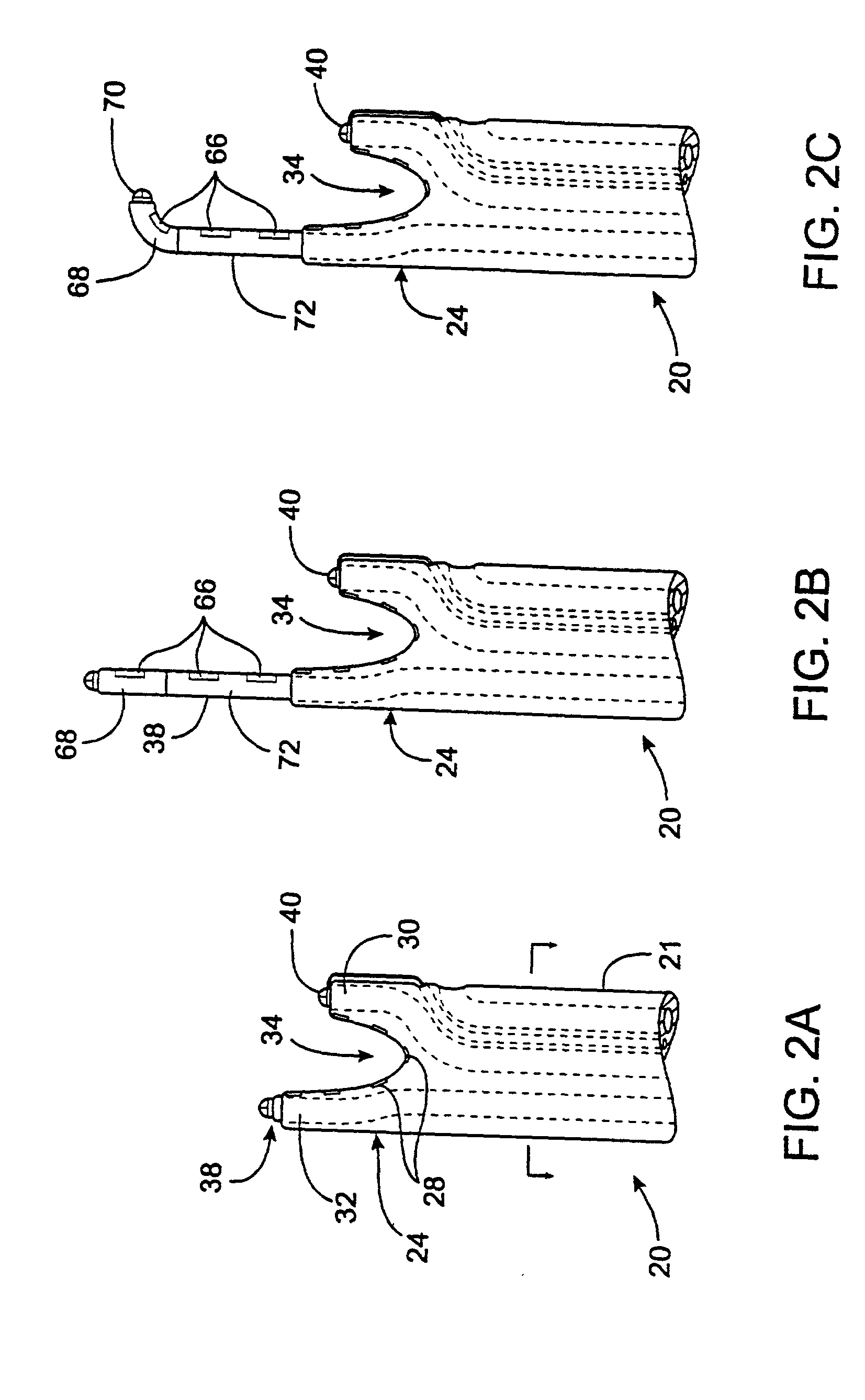
[0114] FIGS. 1A-1B illustrate a first embodiment of the apparatus of the invention. In this embodiment, the apparatus comprises a left ablation probe 20, shown in FIG. 1A, and a right ablation probe 22, shown in FIG. 1B, which work in tandem to form a transmural lesion isolating the pulmonary veins from the surrounding myocardium. Left ablation probe 20 has a flexible shaft 21 extending to a working end 24 configured for insertion into the chest cavity through a small incision, puncture or access port. Opposite working end 24, shaft 21 is attached to a control end 26 used for manipulating the working end 24 from outside the chest. Shaft 21 is dimensioned to allow introduction through a small incision in the chest, preferably in a subxiphoid location, and advanced to the pulmonary veins on the posterior side of the heart. Preferably, shaft 21 is configured to be flexible about a first transverse axis to allow anterior-posterior bending and torsional flexibility, but relatively stiff ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com