Percutaneous valve prosthesis and system and method for implanting same
a technology of heart valve and prosthesis, which is applied in the field of heart valve prosthesis, can solve the problems of thromboembolic complications, catastrophic valve failure, and high risk of valve replacement surgery, and achieve the effect of minimizing the gradient across the valv
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
[0058]In describing preferred embodiments of the present invention illustrated in the drawings, specific terminology is employed for the sake of clarity. However, the invention is not intended to be limited to the specific terminology so selected, and it is to be understood that each specific element includes all technical equivalents that operate in a similar manner to accomplish a similar purpose.
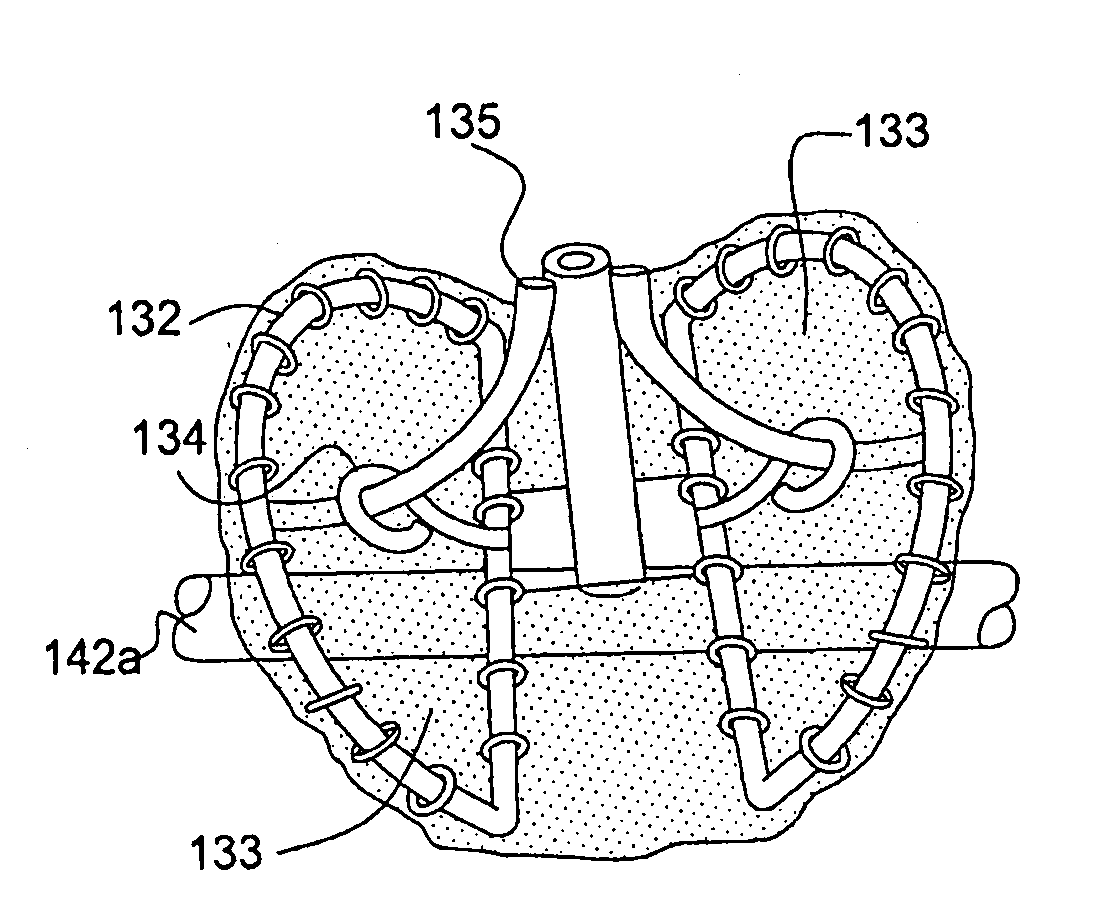
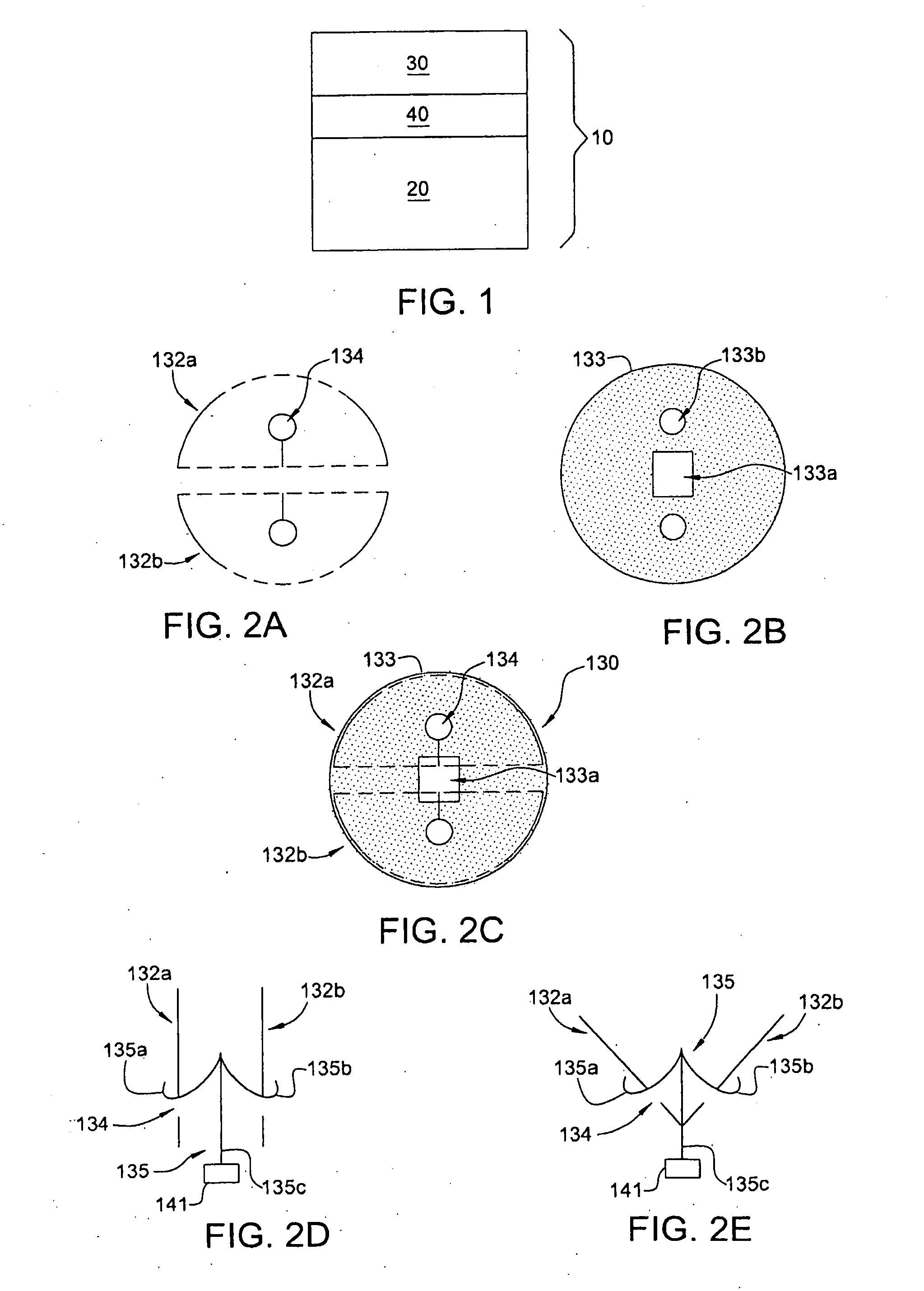
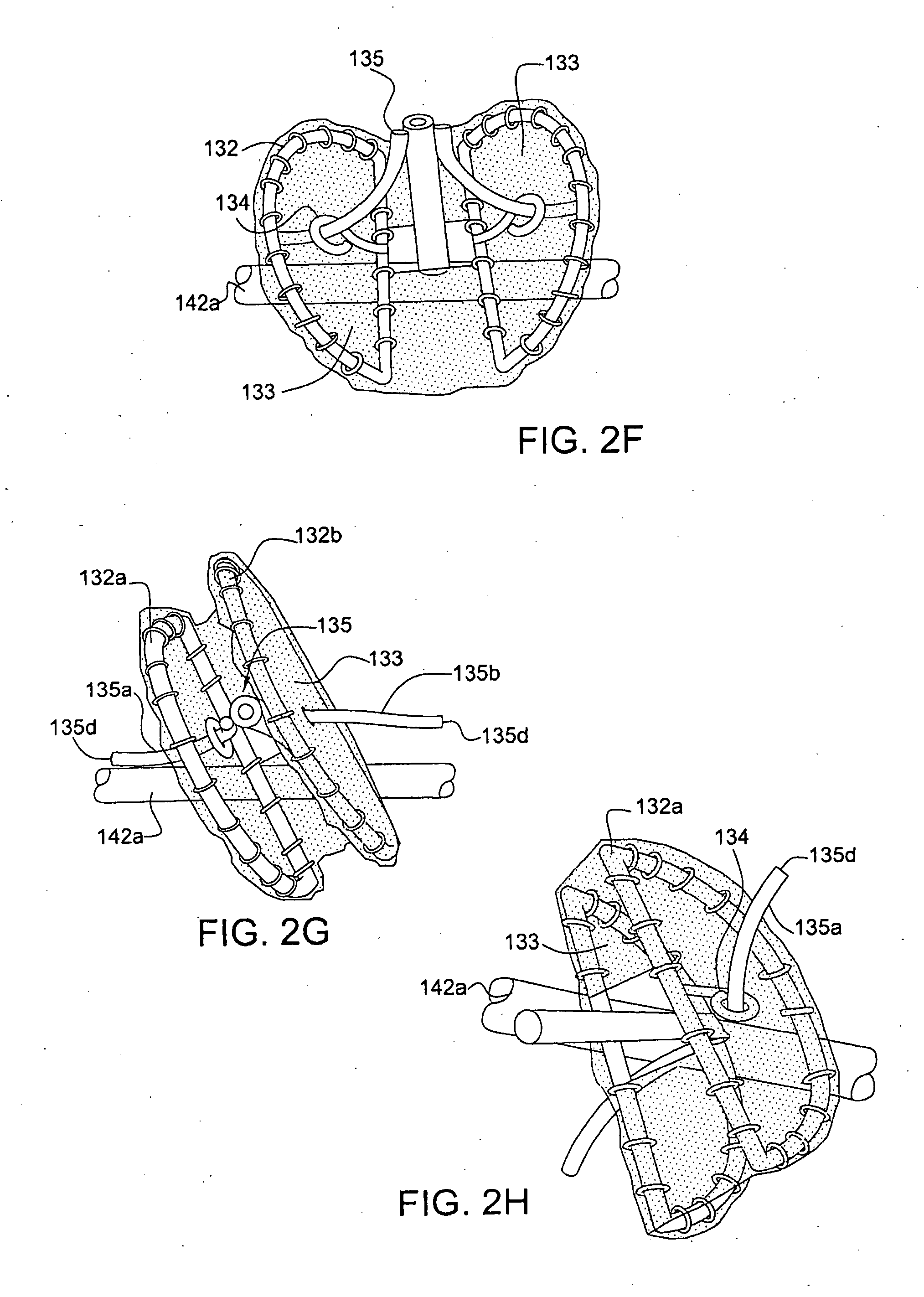
[0059]The present invention relates to heart valve prostheses that can be implanted percutaneously by means of a catheter from a remote location without opening the chest cavity. As shown in FIG. 1, the valve prosthesis 10 comprises two parts, (1) a valve cage stent 20 constructed to be implanted in the planar axis of the native valve annulus, (2) an elastic and compressible valve 30, and (3) an attachment mechanism for attaching the valve 30 to the superior rim of the above mentioned valve cage stent 20. In accordance with the present invention, two types 110 and 210 of heart valve prost...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com