Patents
Literature
39 results about "Prior authorization" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
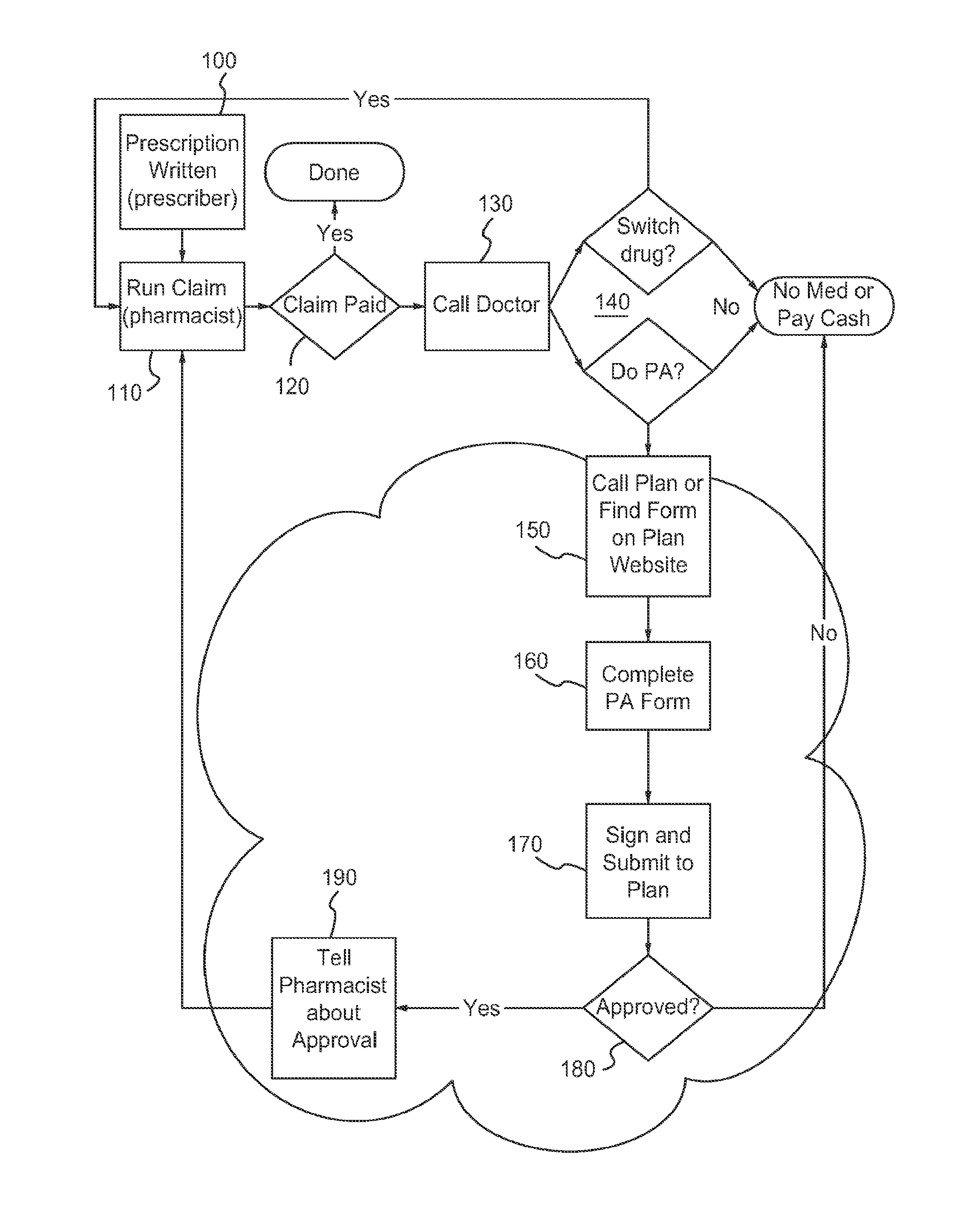
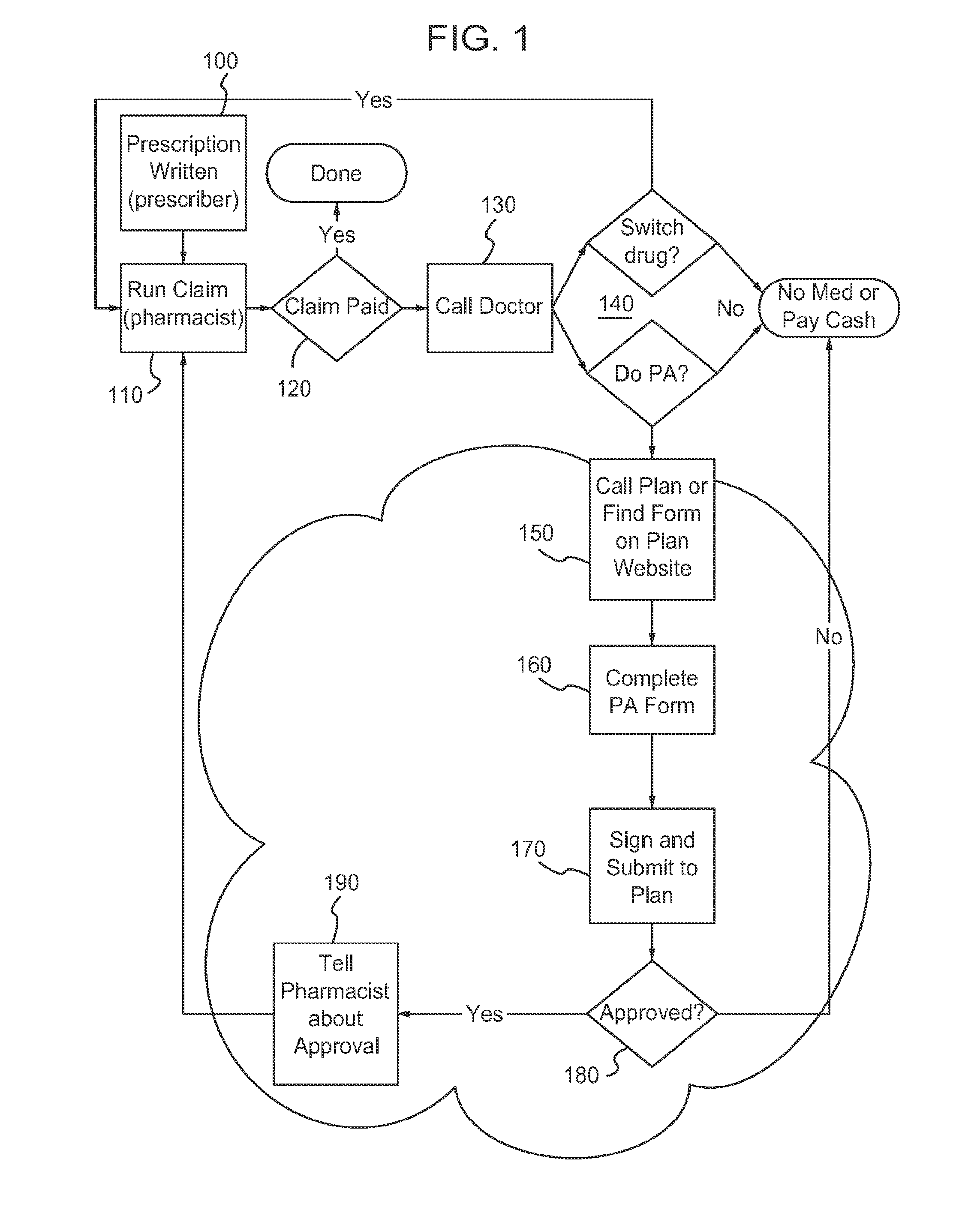
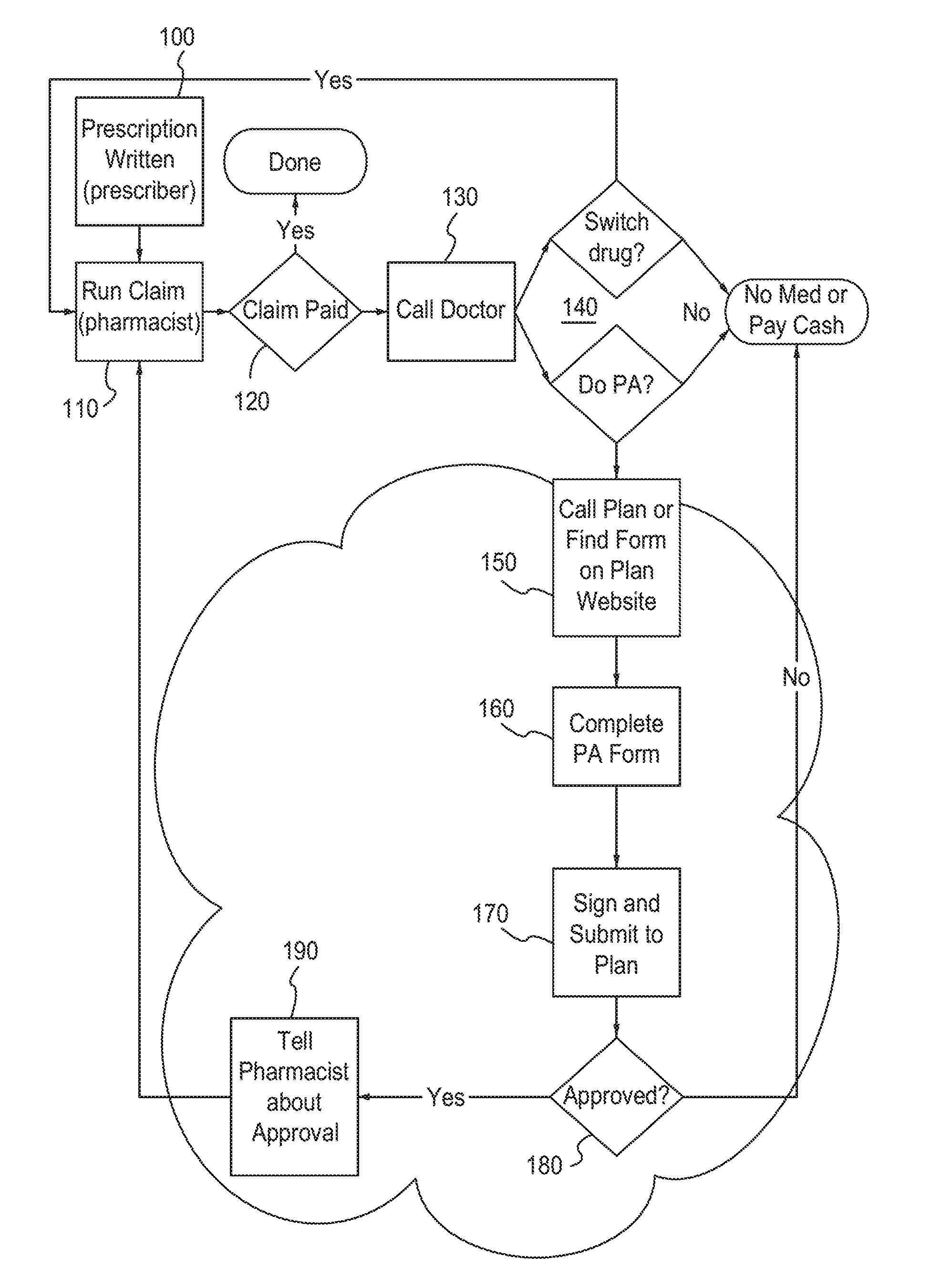
Prior authorization is a utilization management process used by some health insurance companies in the United States to determine if they will cover a prescribed procedure, service, or medication. The process is intended to act as a safety and cost-saving measure although it has received criticism from physicians for being costly and time-consuming.
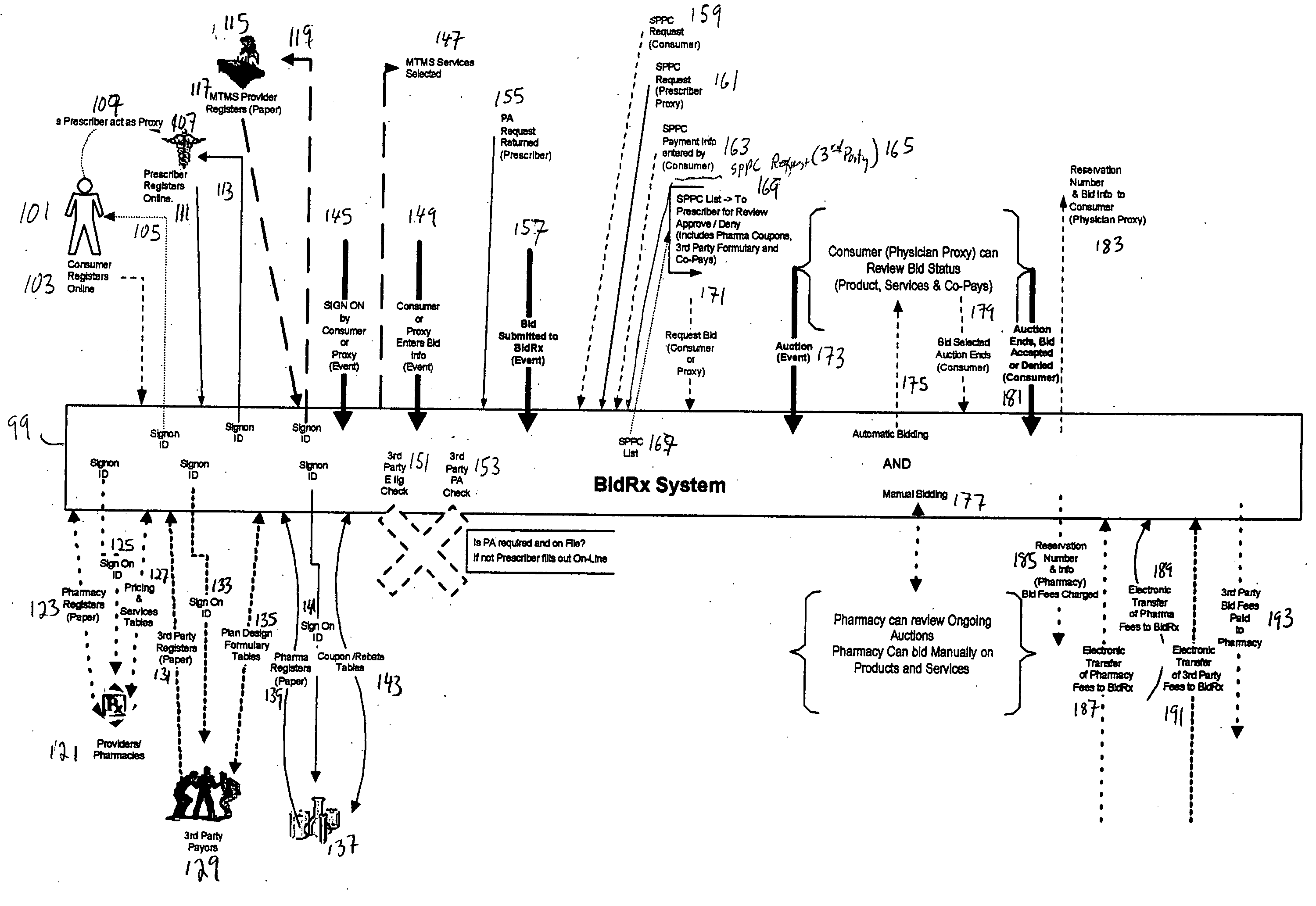
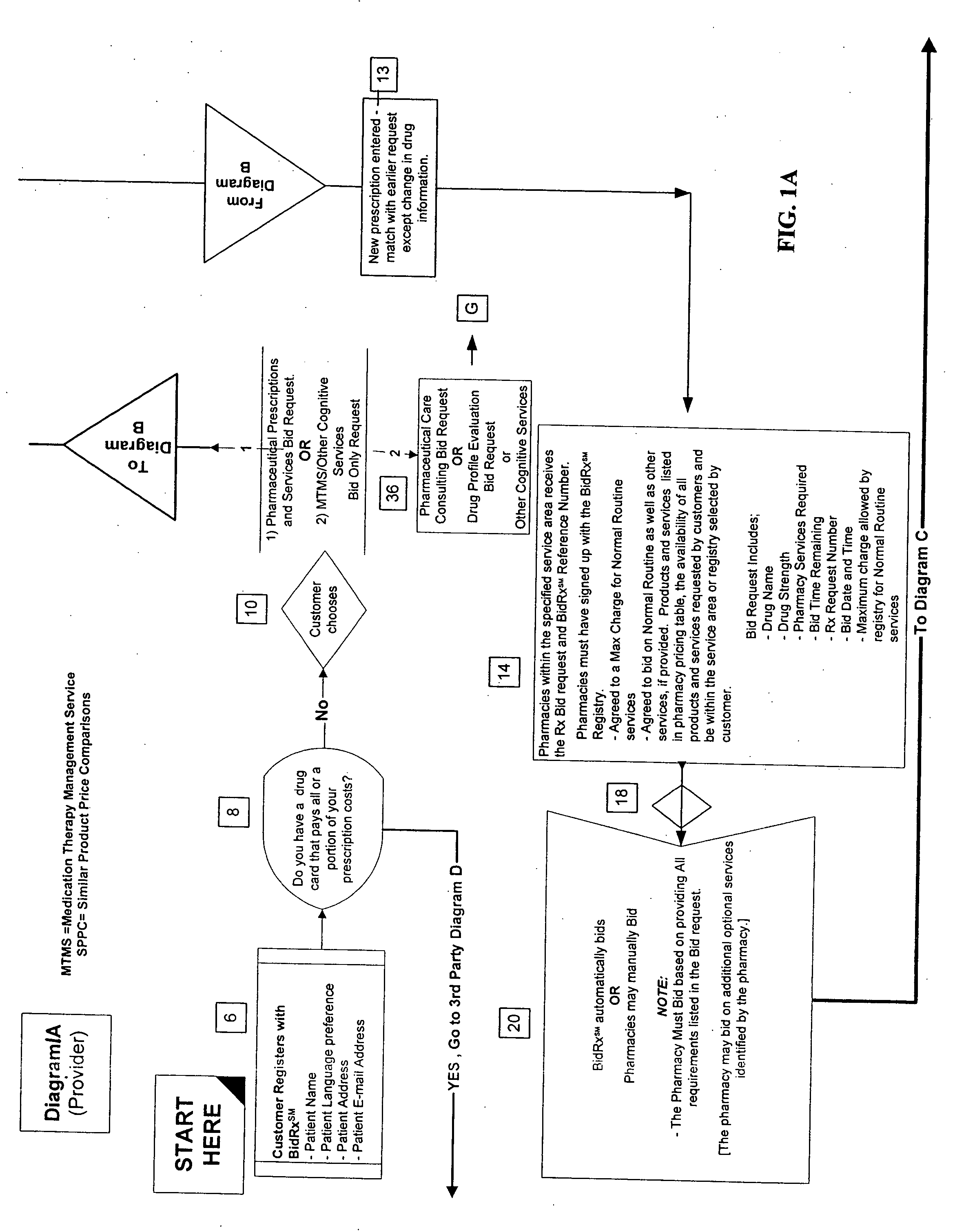
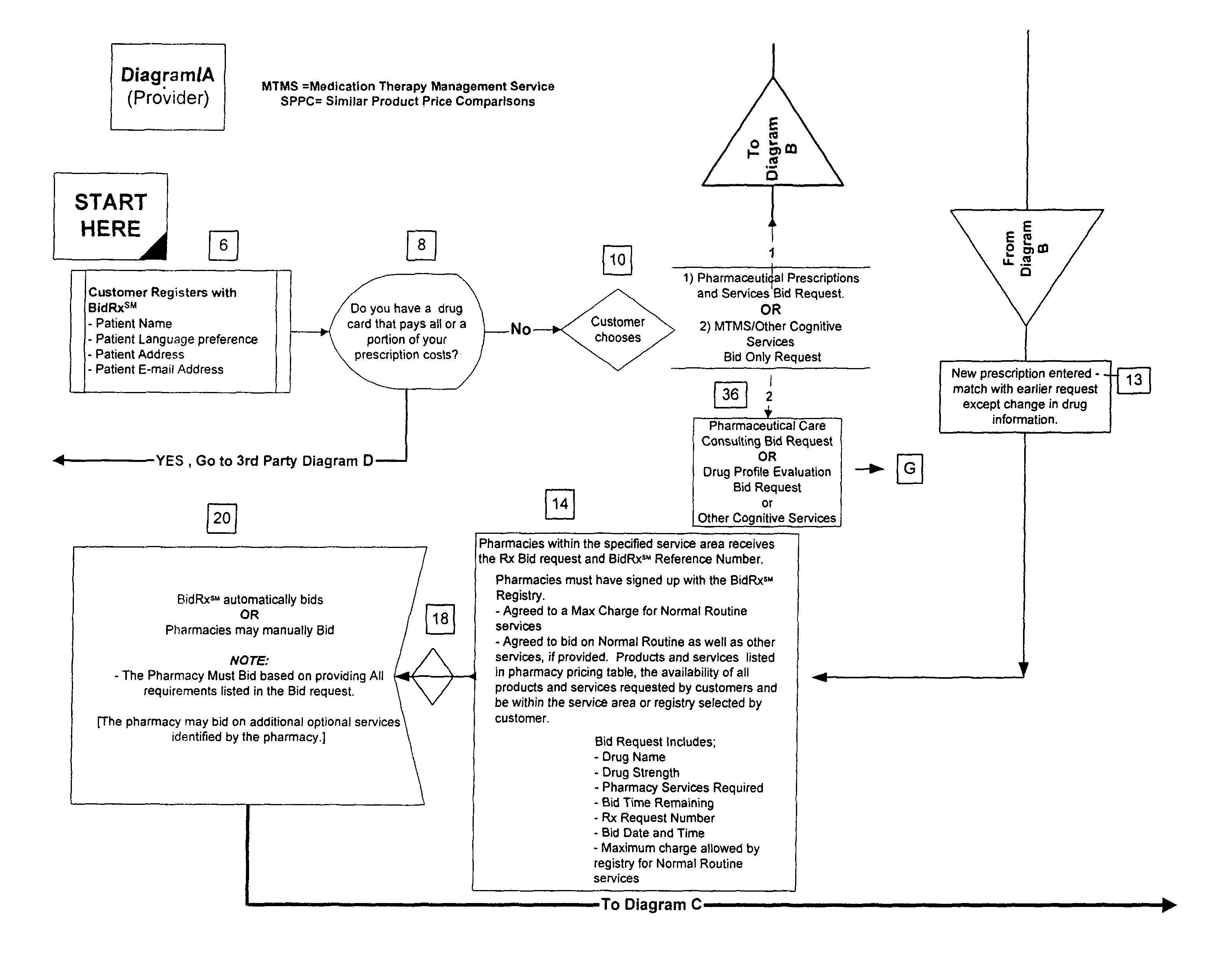
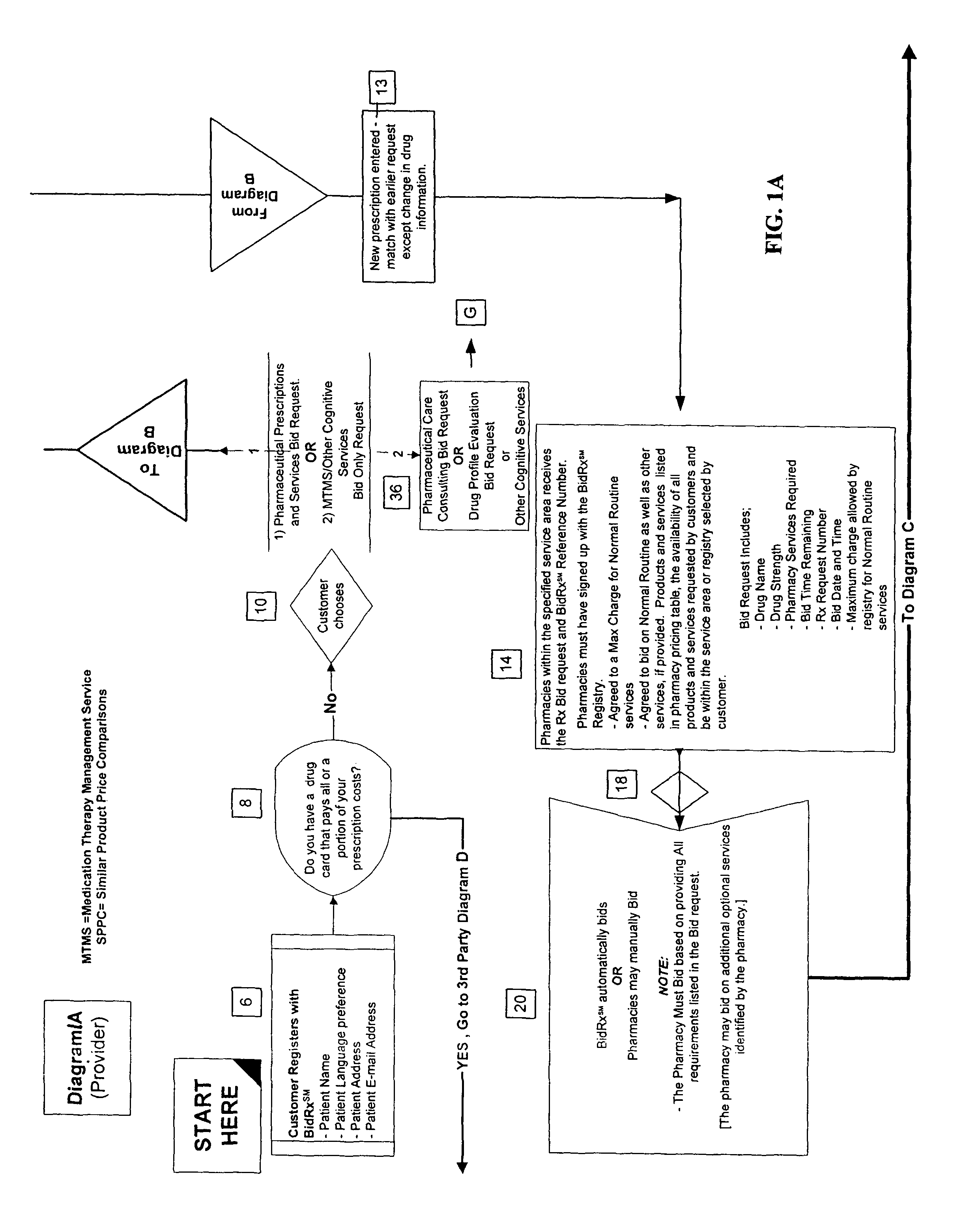
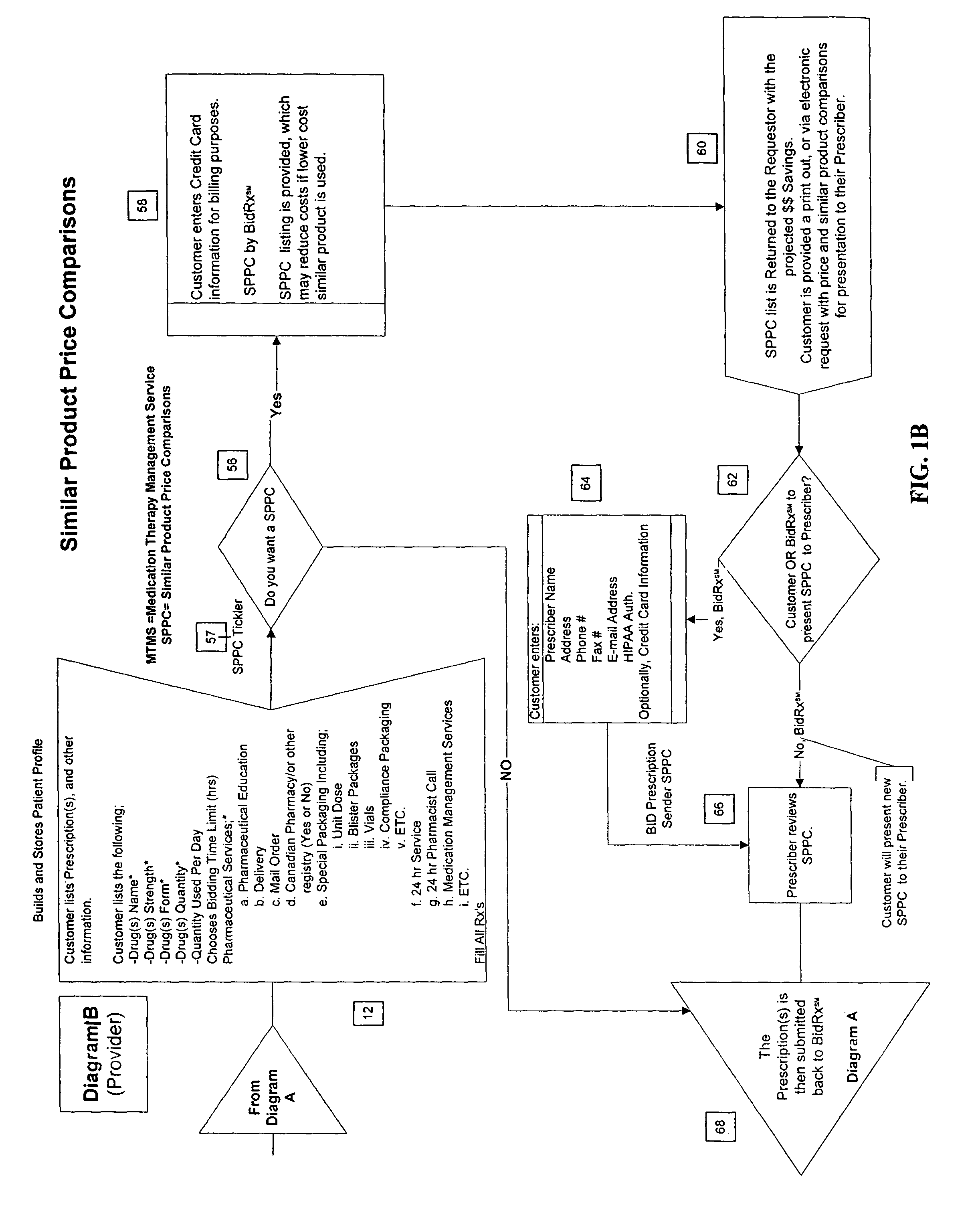
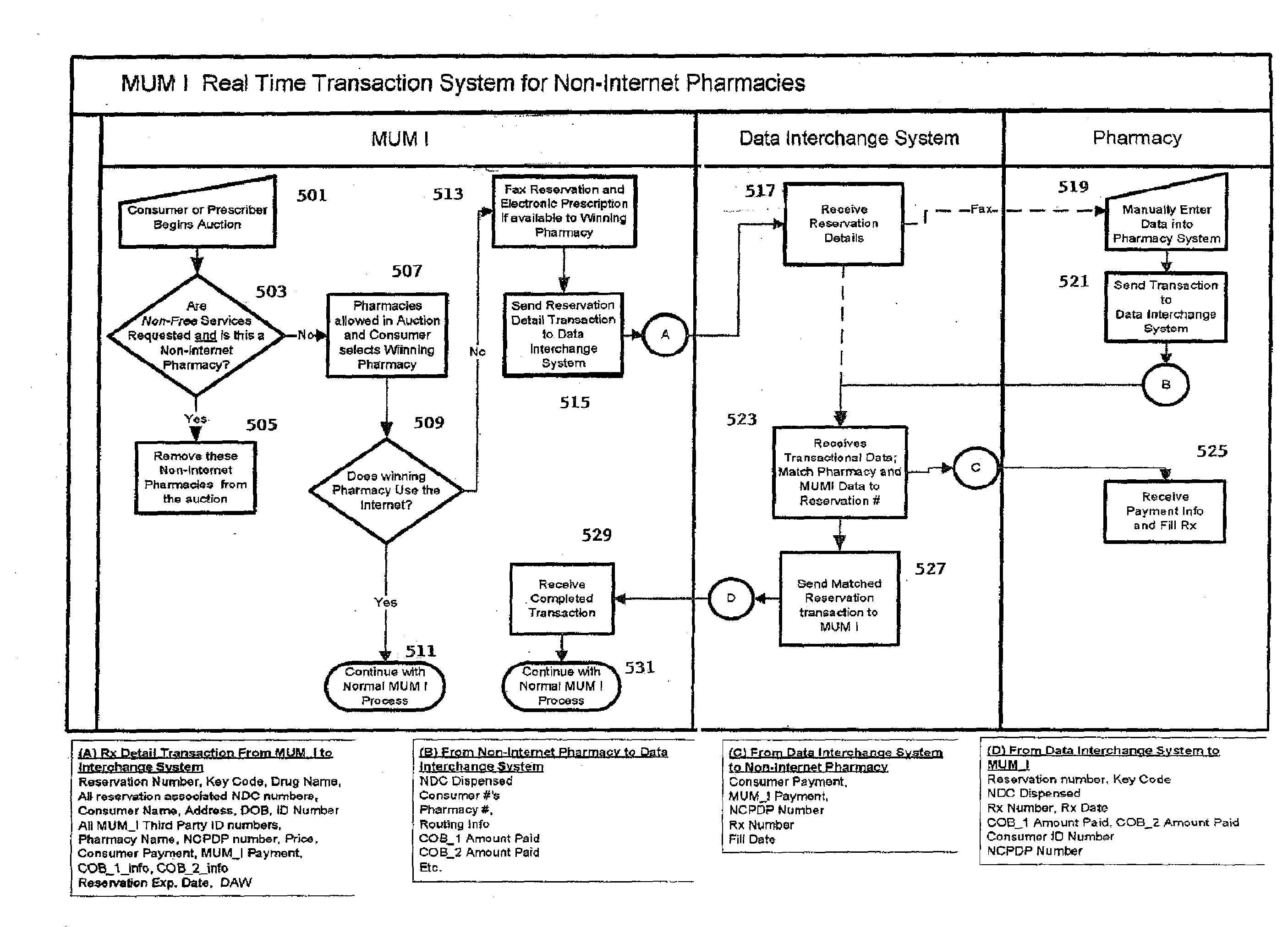
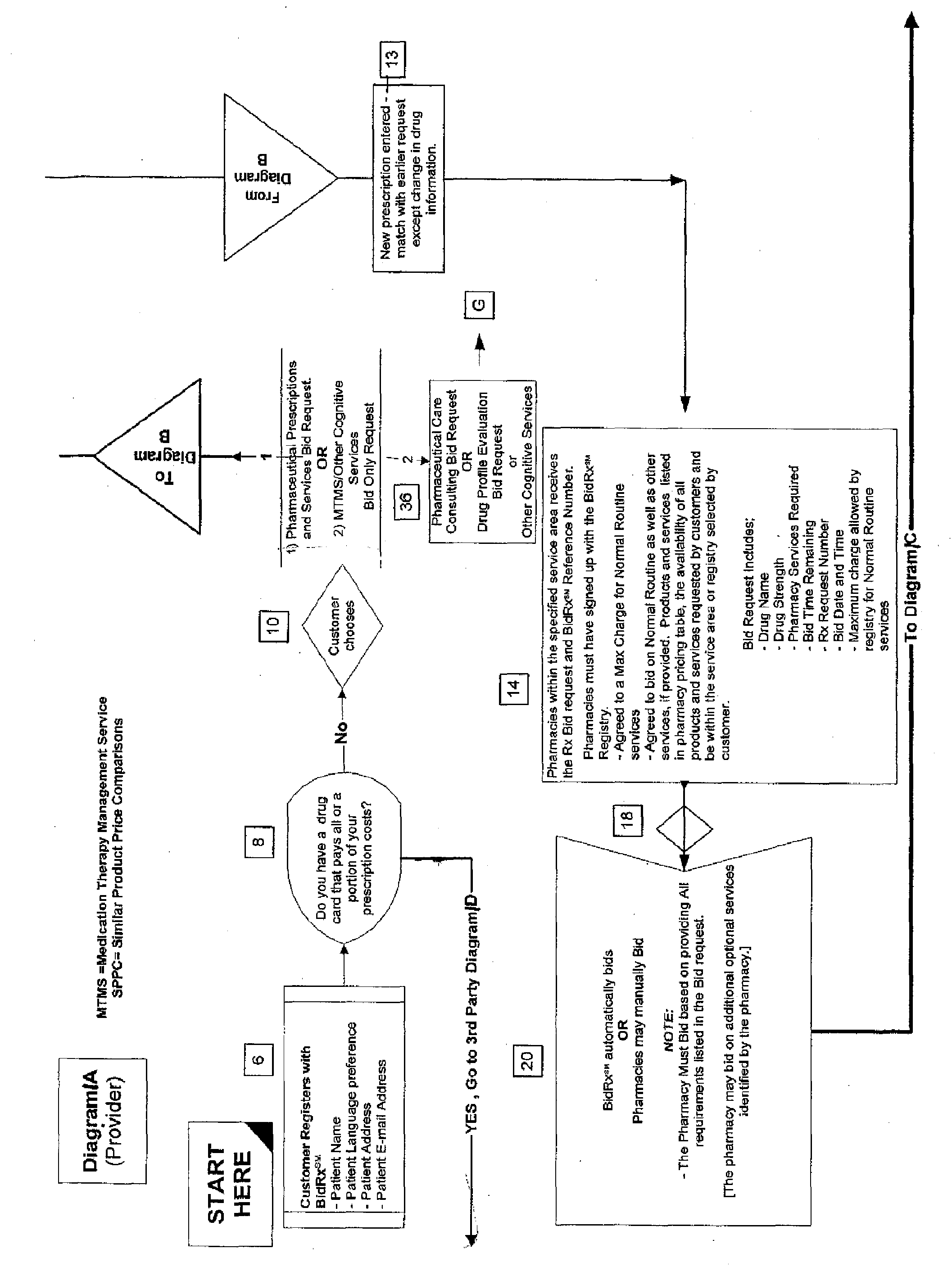
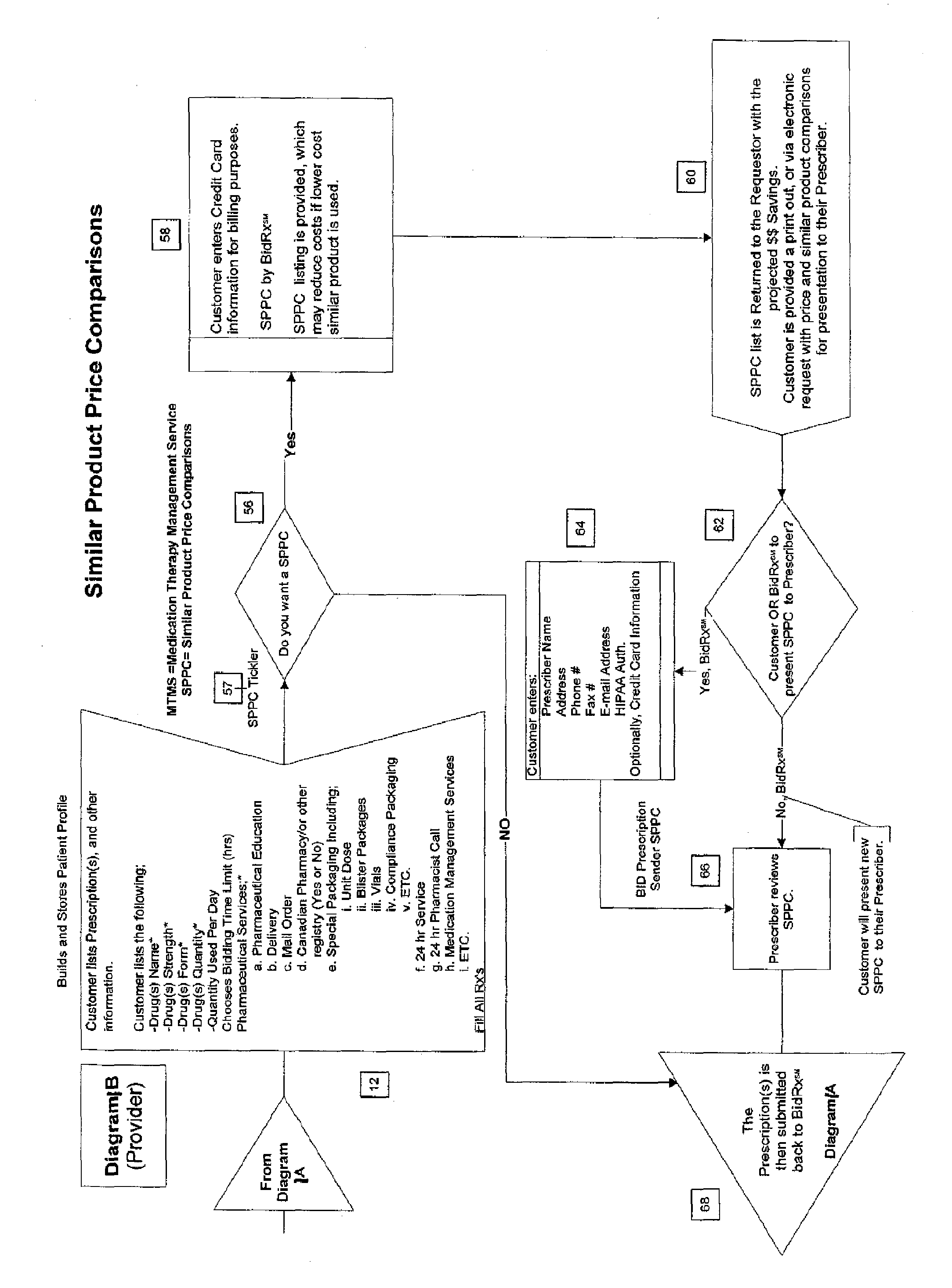
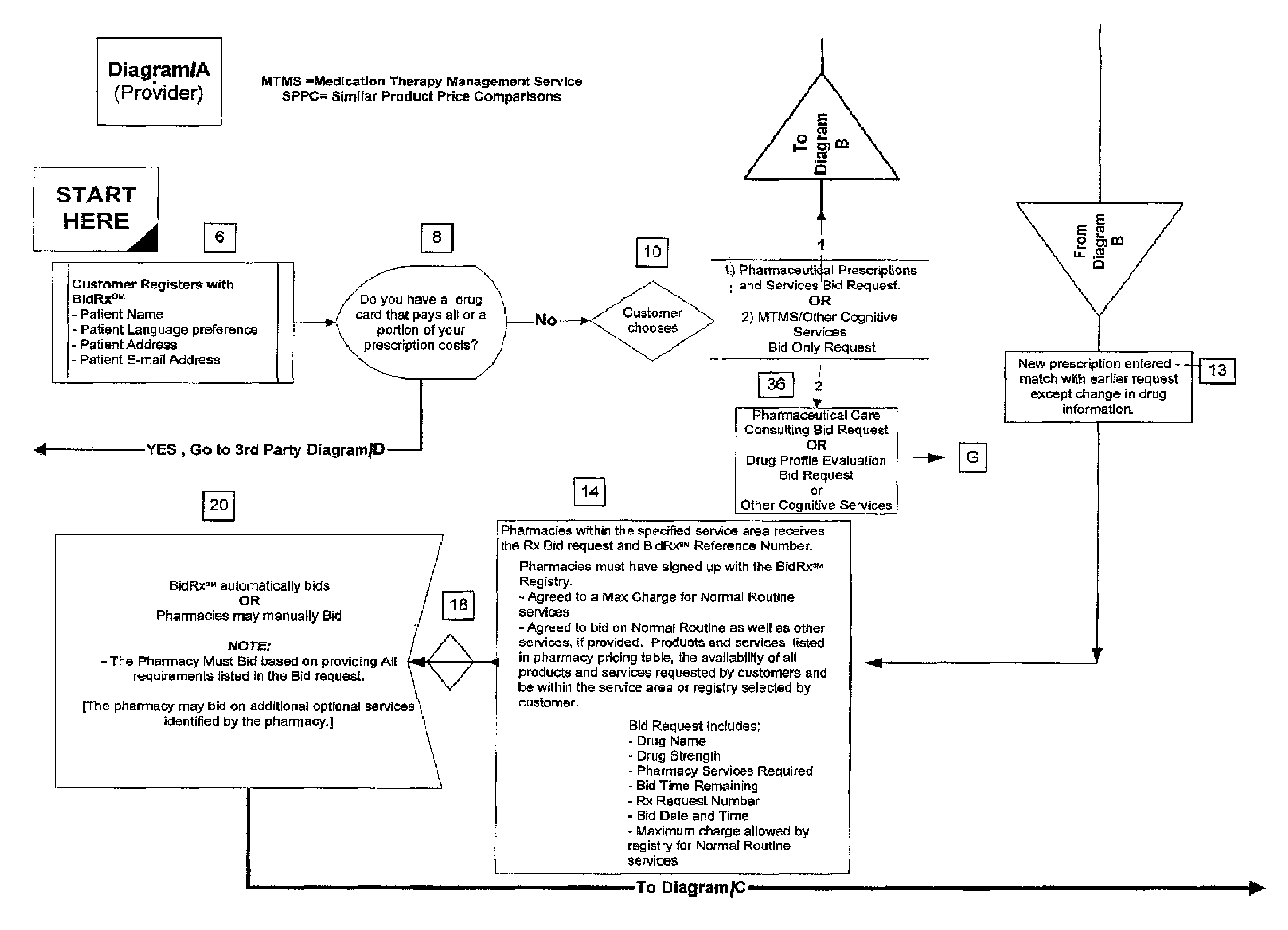
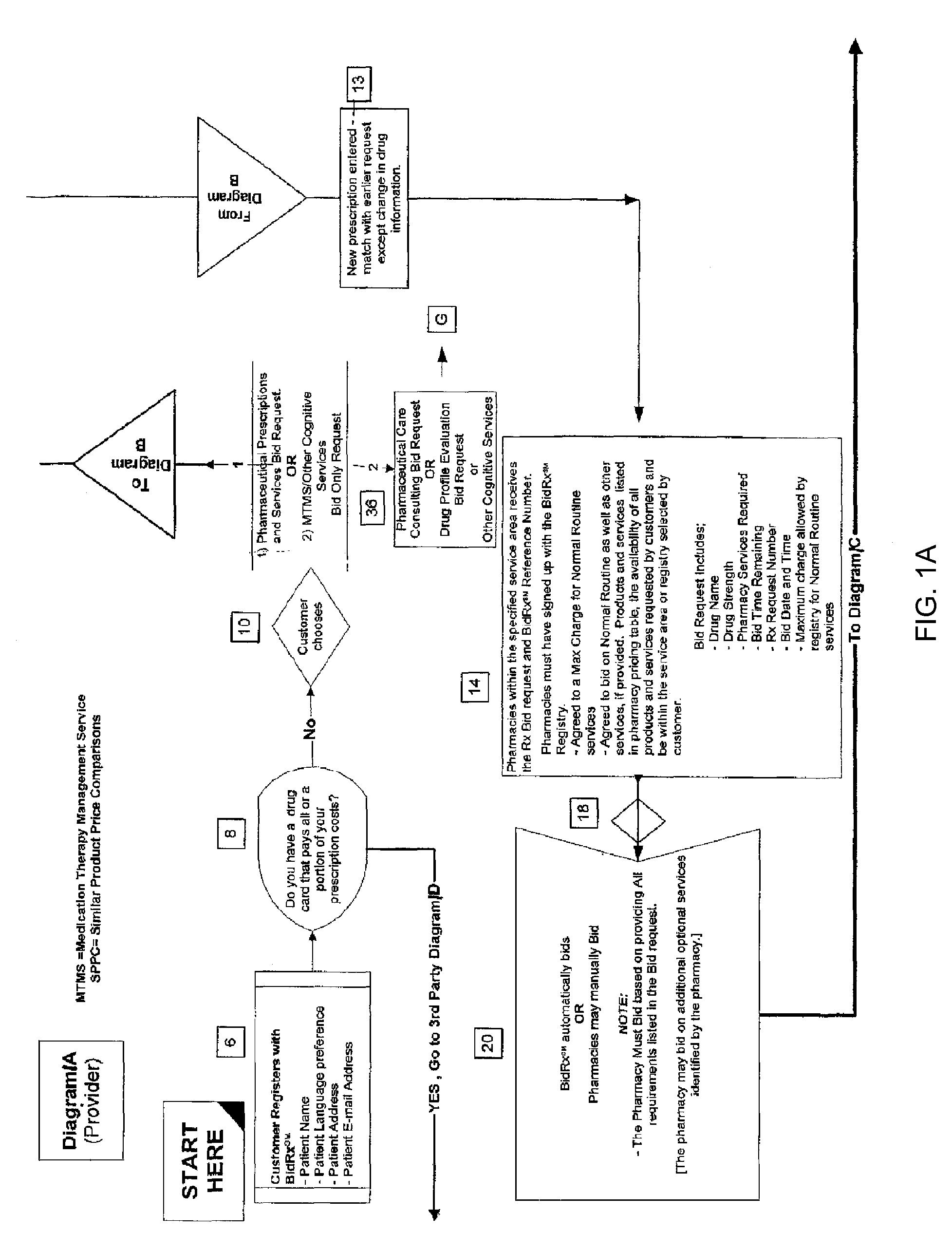
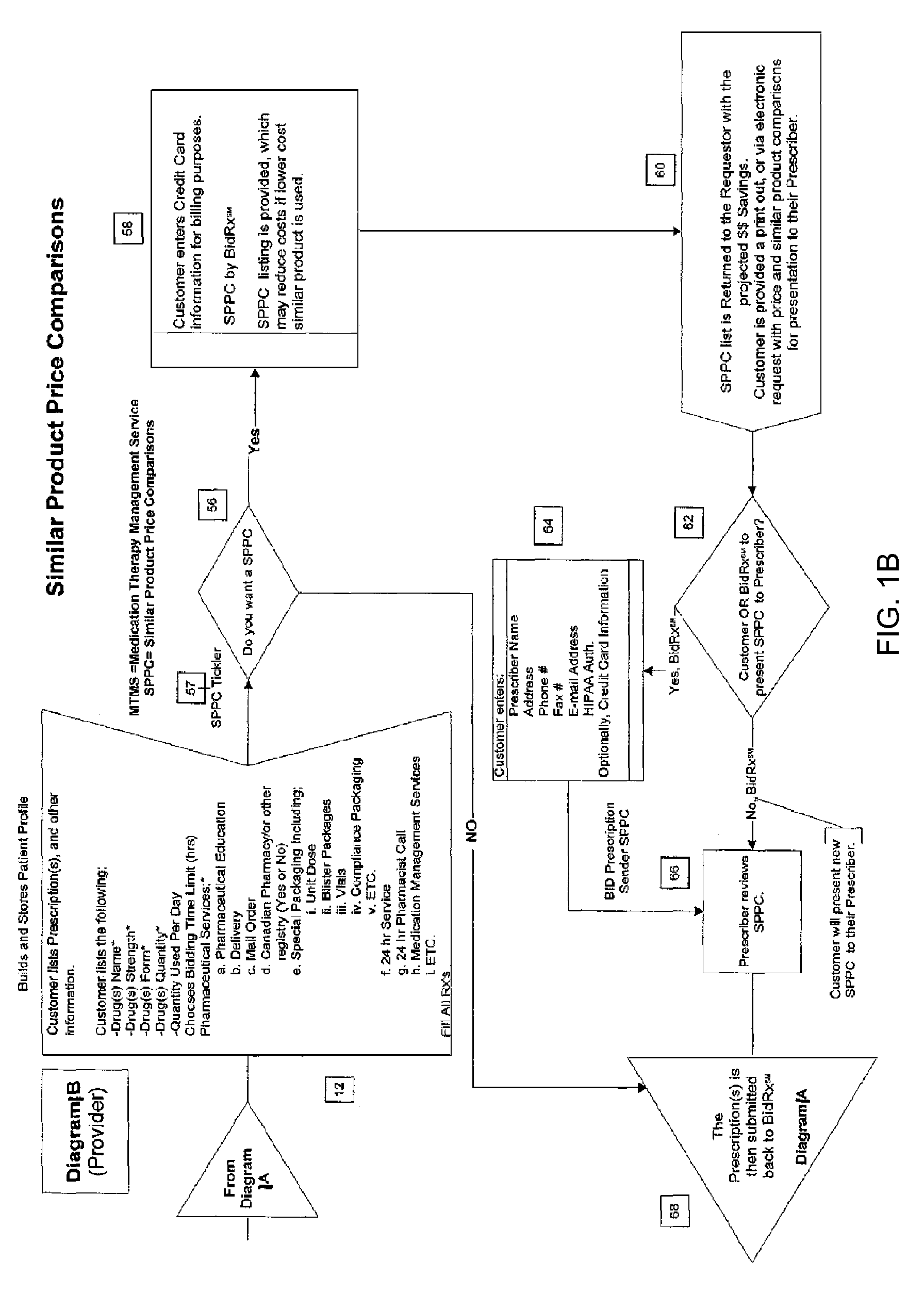
Method for competitive prescription drug and/or bidding service provider selection
Unfilled prescriptions are submitted to a registry comprising pre-qualified pharmacies for a “reverse auction” in which the pharmacies bid for the opportunity to fill the prescription. The pharmacies are allowed to bid based on price and / or offering ancillary services. The auction may also be used to bid on supplying specified pharmaceutical cognitive services. The method may also include obtaining cost comparisons with generic substitutes or similar alternative pharmaceutical products. The system may further comprise automatically requesting a review by the prescriber for a list of similar substitutes or prior-authorization for third-party payers. The winner of the reverse auction is selected by the customer.
Owner:TAG LLC (US)
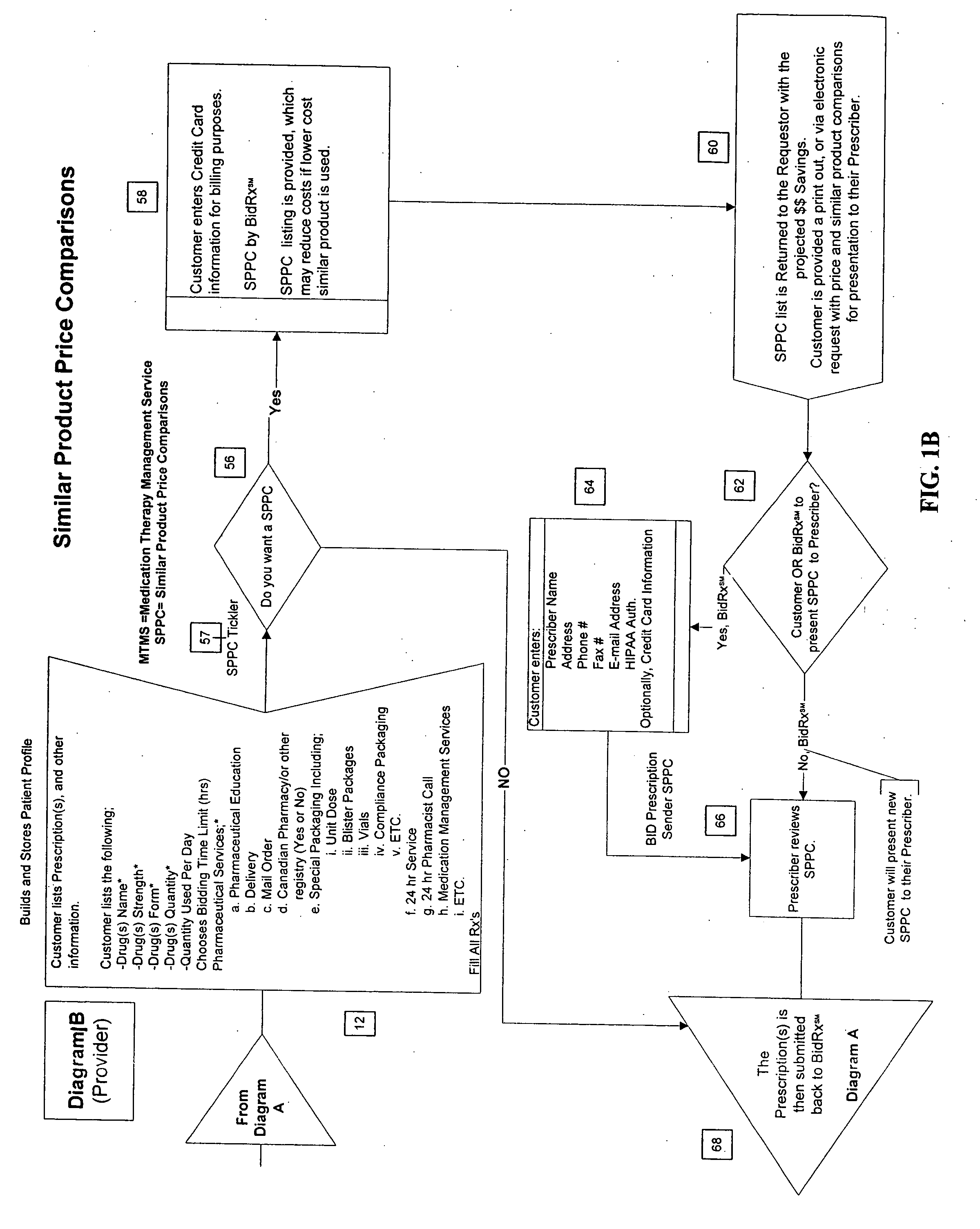
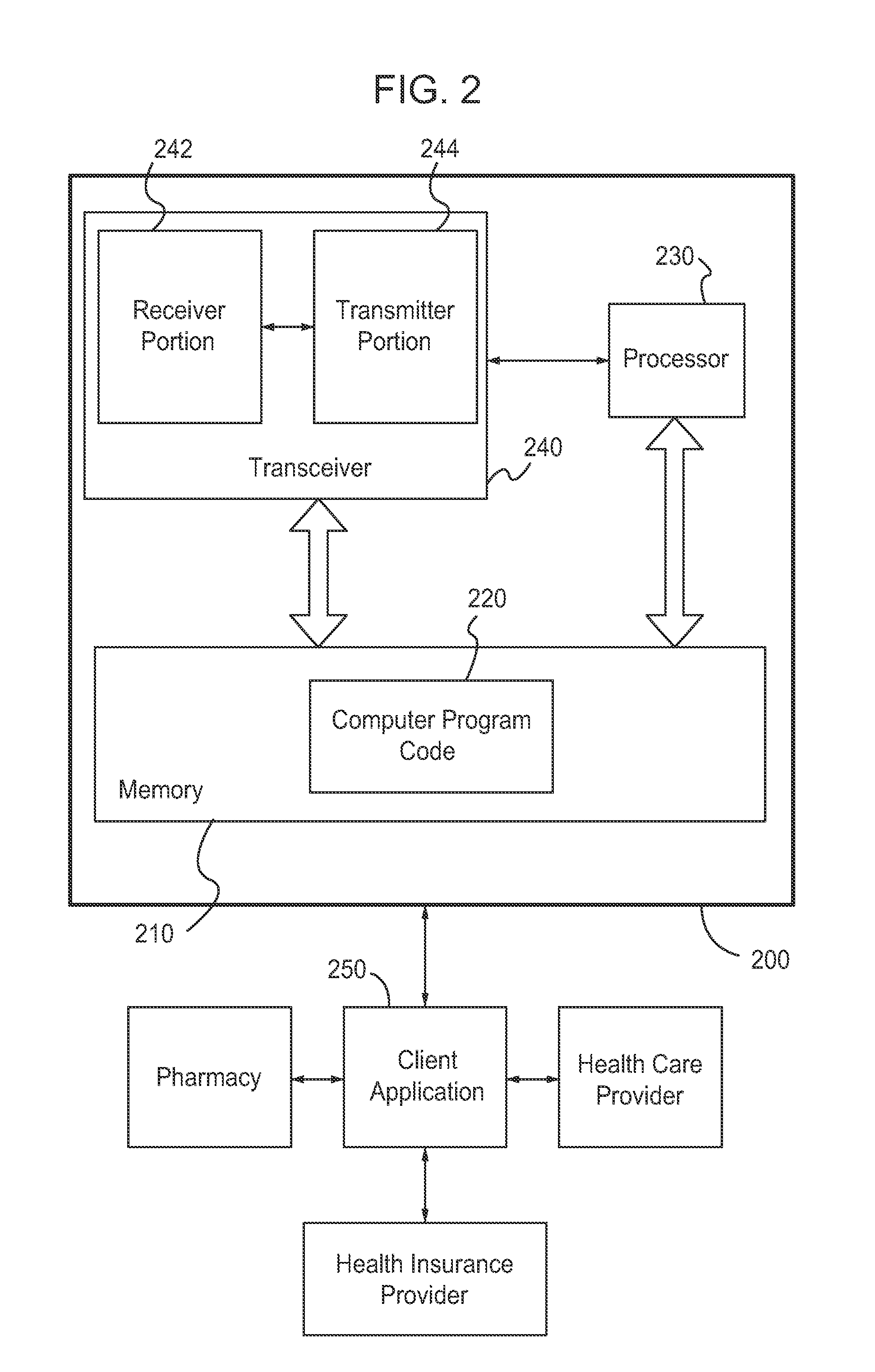
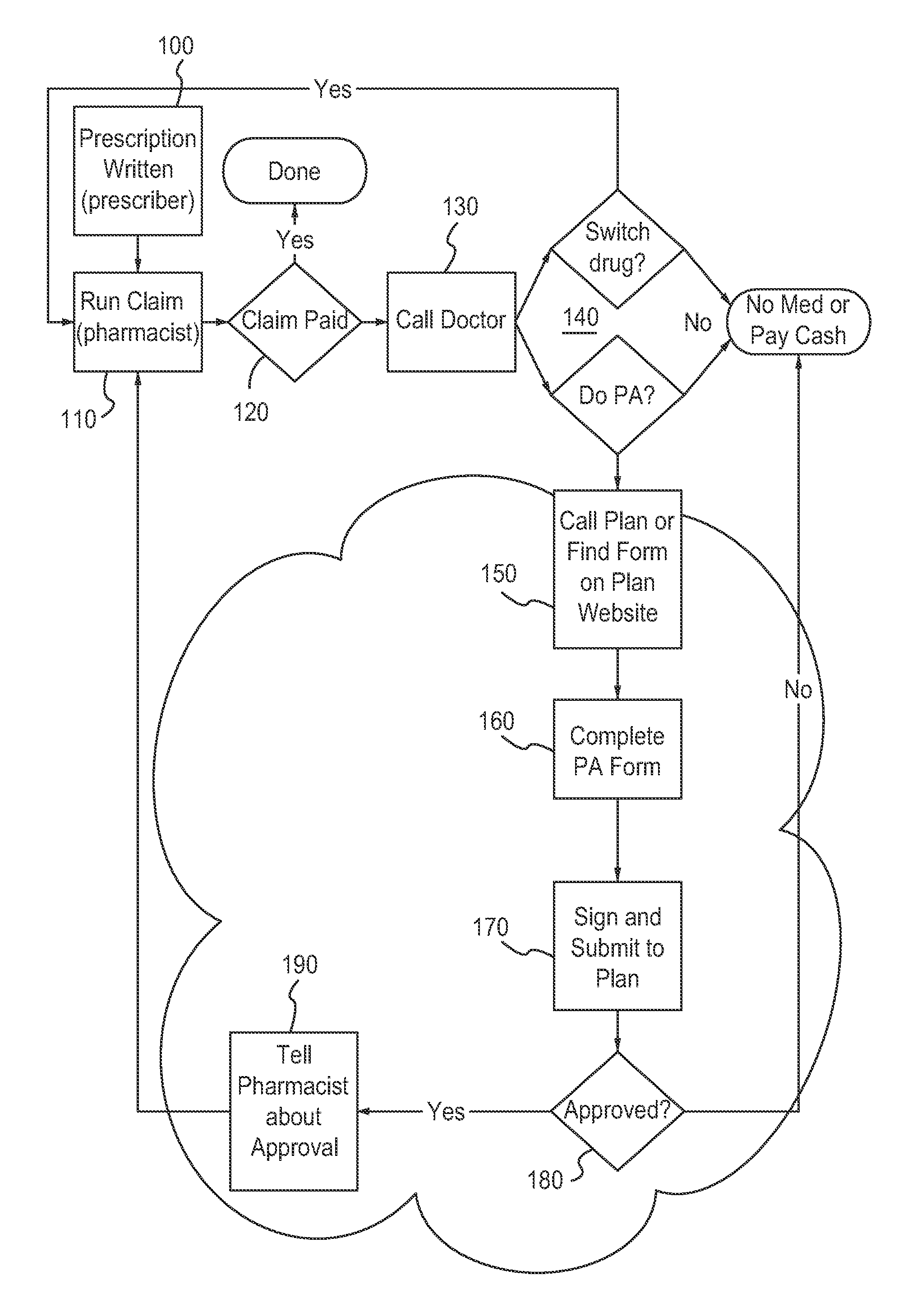
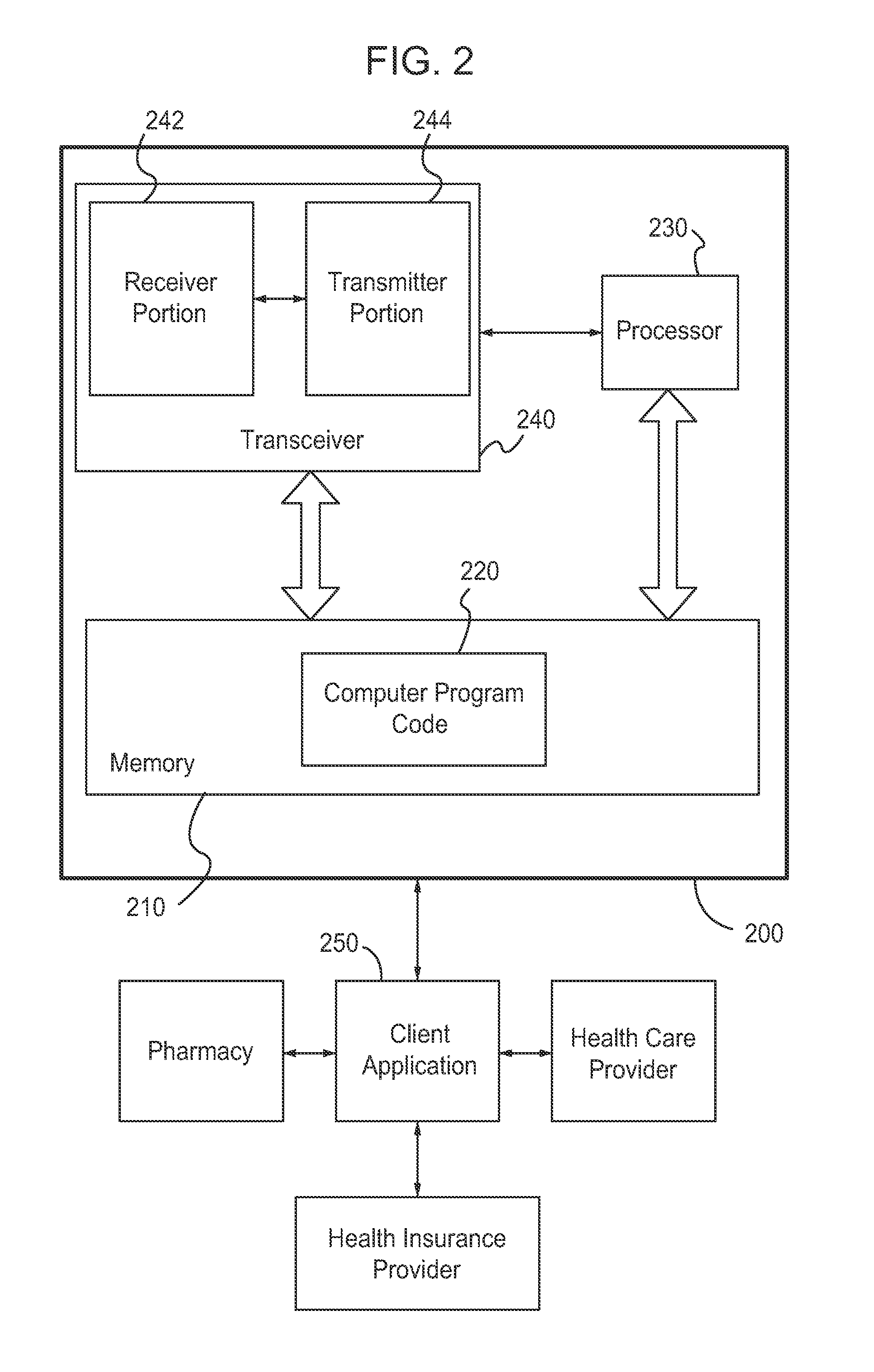
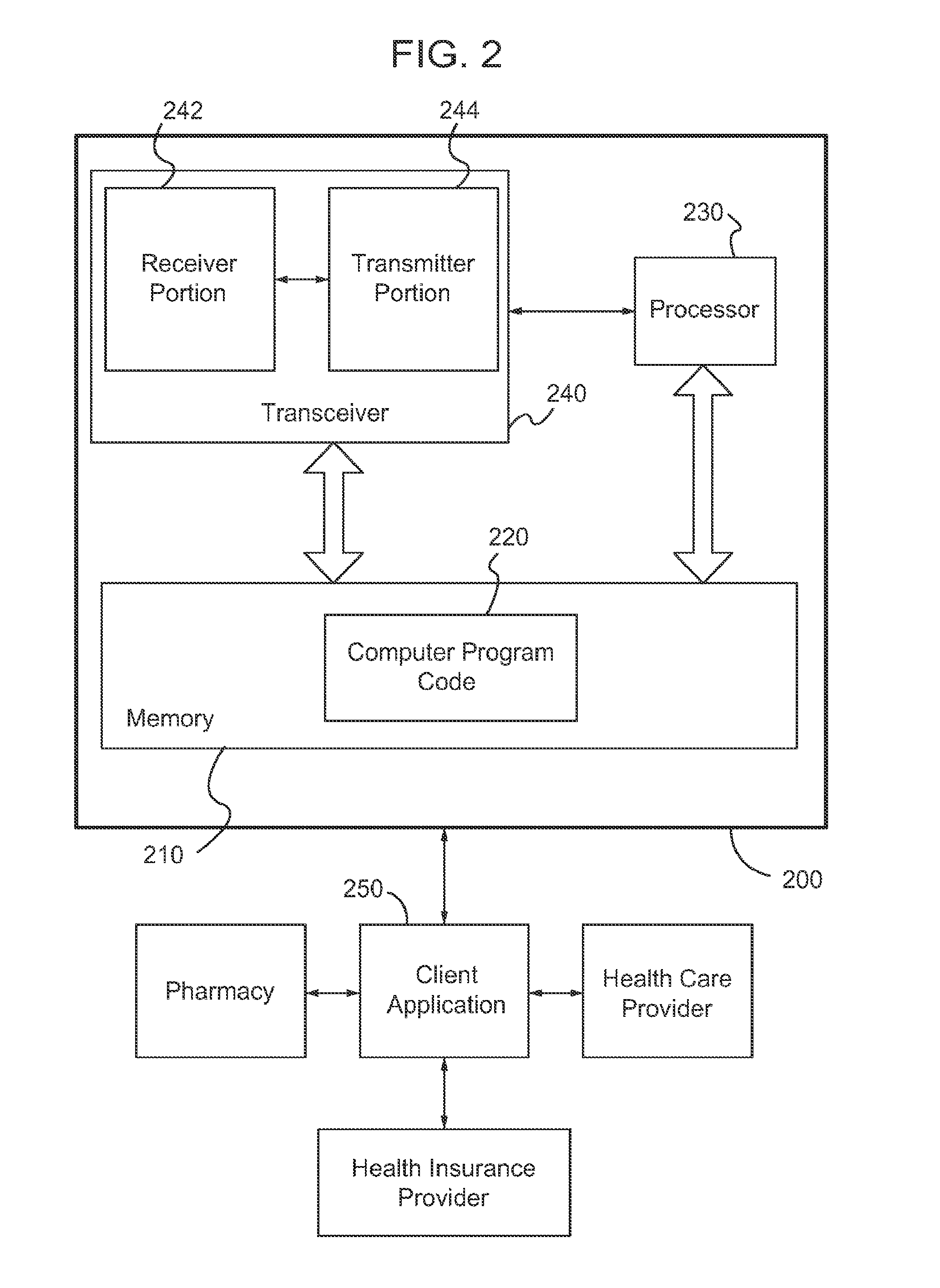
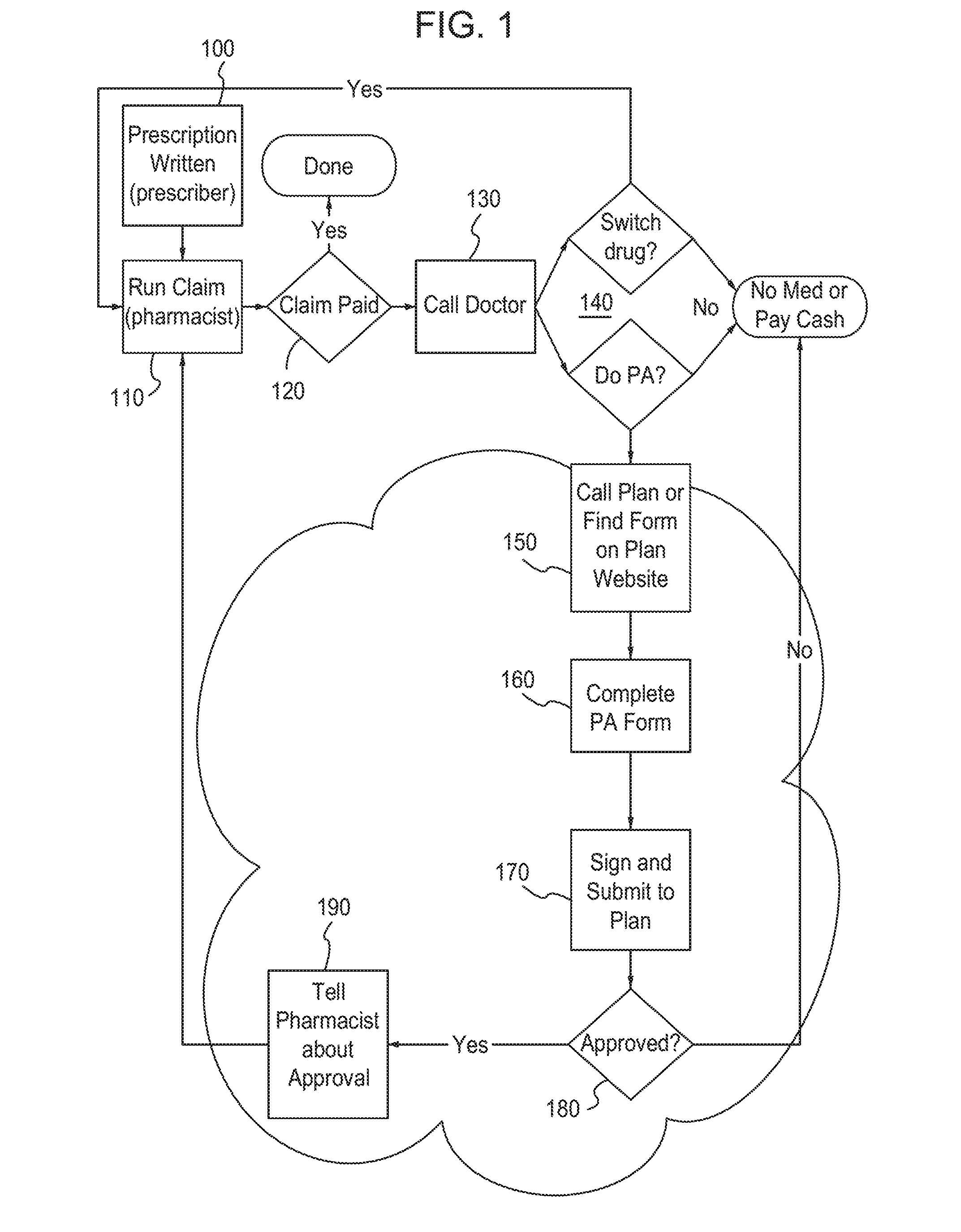
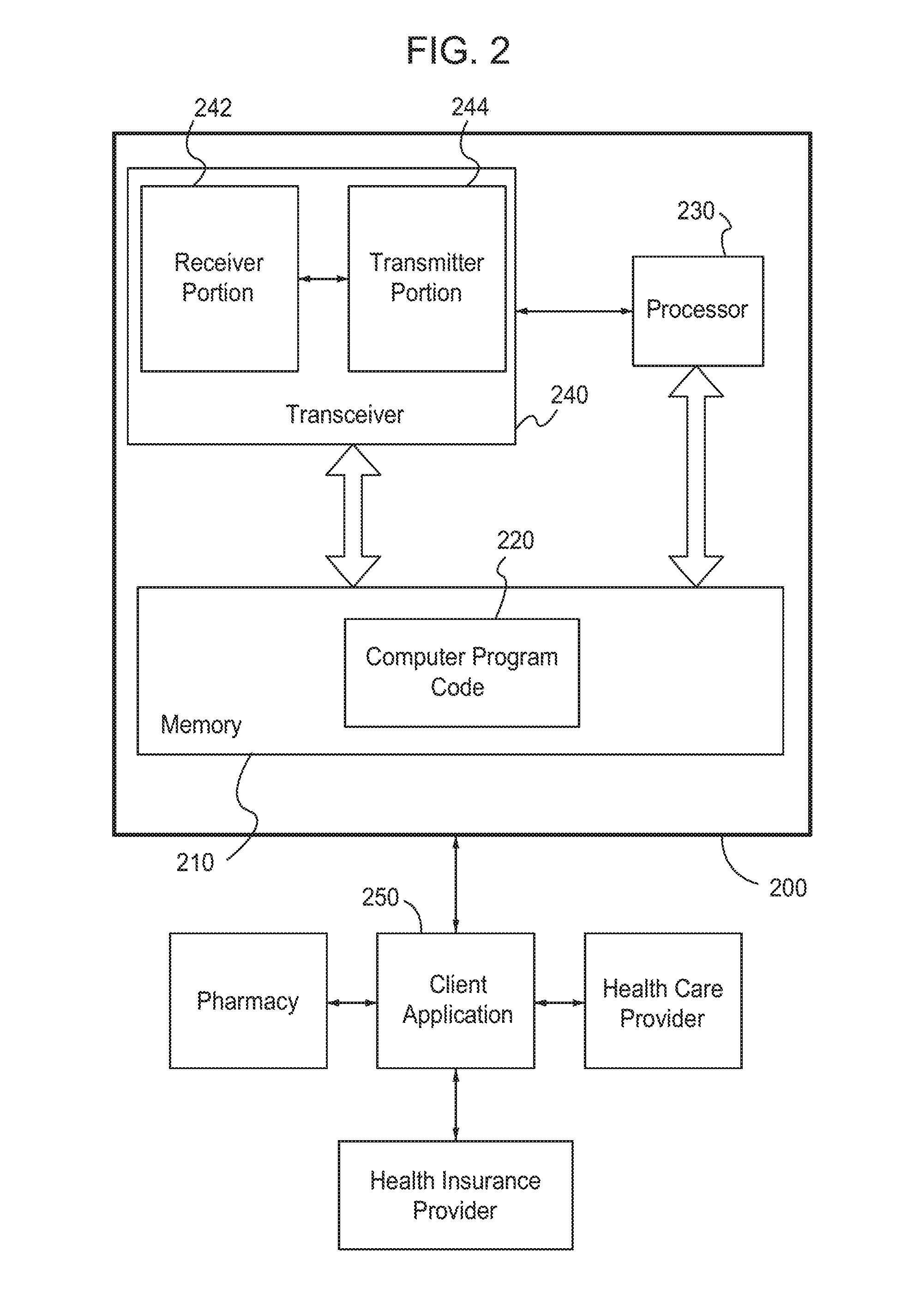
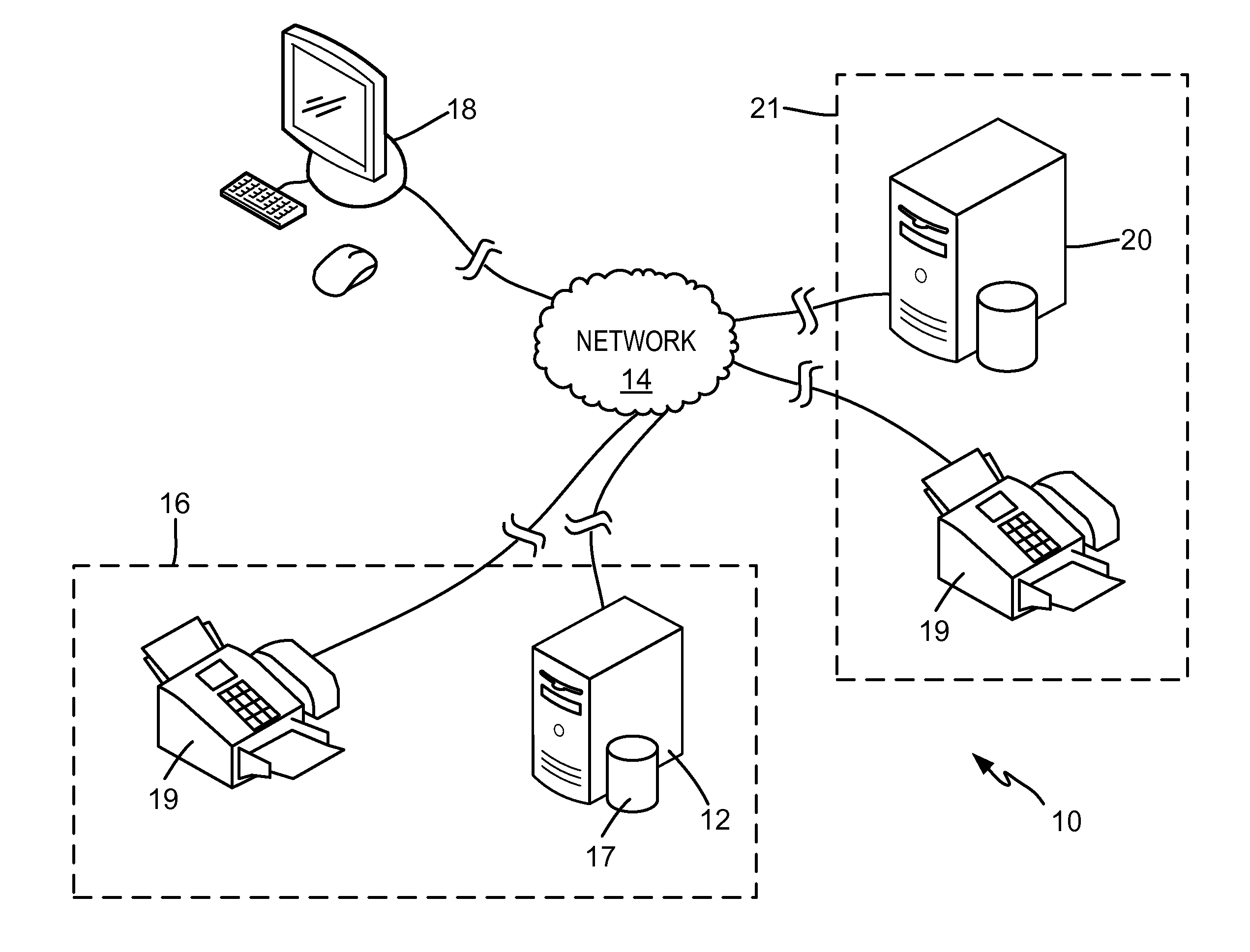
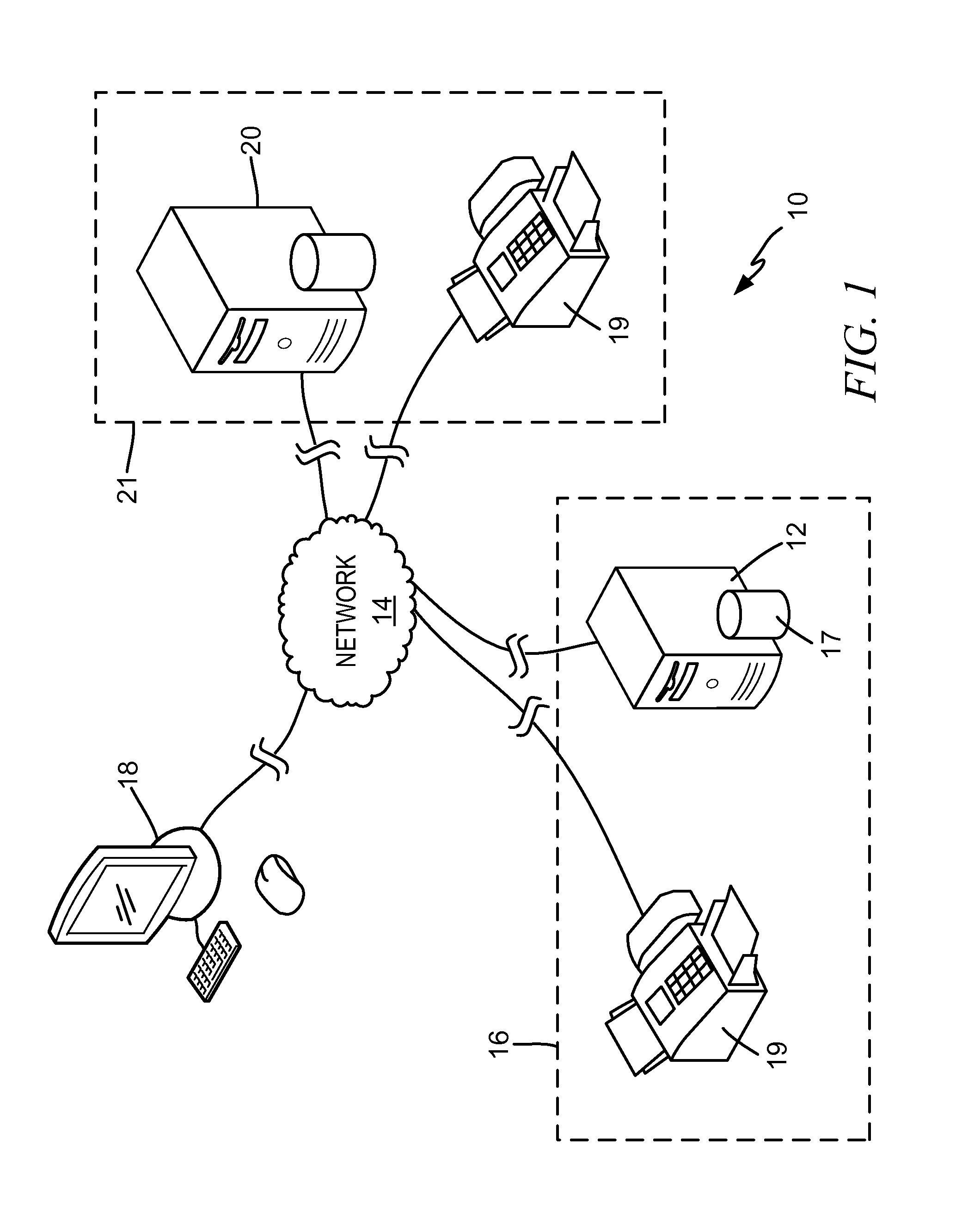
Apparatus and method for processing prior authorizations for prescription drugs
An apparatus, a method, and a computer program product are provided. The apparatus includes at least one memory including computer program code, and at least one processor. The at least one memory and the computer program code are configured to, with the at least one processor, cause the apparatus at least to receive a request to generate a prior authorization form for a prescription drug, and select the prior authorization form from a plurality of prior authorization forms based on the request. The prior authorization form is selected based on at least one of a user search result and a standardized transaction. The at least one memory and the computer program code are further configured to, with the at least one processor, cause the apparatus at least to transmit the selected prior authorization form to a user so that the user can complete and submit the prior authorization form to the health plan and receive a determination on the request.
Owner:COVERMYMEDS
Method for competitive prescription drug and/or bidding service provider selection
Unfilled prescriptions are submitted to a registry comprising pre-qualified pharmacies for a “reverse auction” in which the pharmacies bid for the opportunity to fill the prescription. The pharmacies are allowed to bid based on price and / or offering ancillary services. The auction may also be used to bid on supplying specified pharmaceutical cognitive services. The method may also include obtaining cost comparisons with generic substitutes or similar alternative pharmaceutical products. The system may further comprise automatically requesting a review by the prescriber for a list of similar substitutes or prior-authorization for third-party payers. The winner of the reverse auction is selected by the customer.
Owner:TAG LLC (US)
Method for Competitive Prescription Drug and/or Bidding Service Provider Selection
Unfilled prescriptions are submitted to a registry comprising pre-qualified pharmacies for a “reverse auction” in which the pharmacies bid for the opportunity to fill the prescription. The pharmacies are allowed to bid based on price and / or offering ancillary services. The auction may also be used to bid on supplying specified pharmaceutical cognitive services. The method may also include obtaining cost comparisons with generic substitutes or similar alternative pharmaceutical products. The system may further comprise automatically requesting a review by the prescriber for a list of similar substitutes or prior-authorization for third party payers. The winner of the reverse auction is selected by the customer.
Owner:TAG LLC (US)
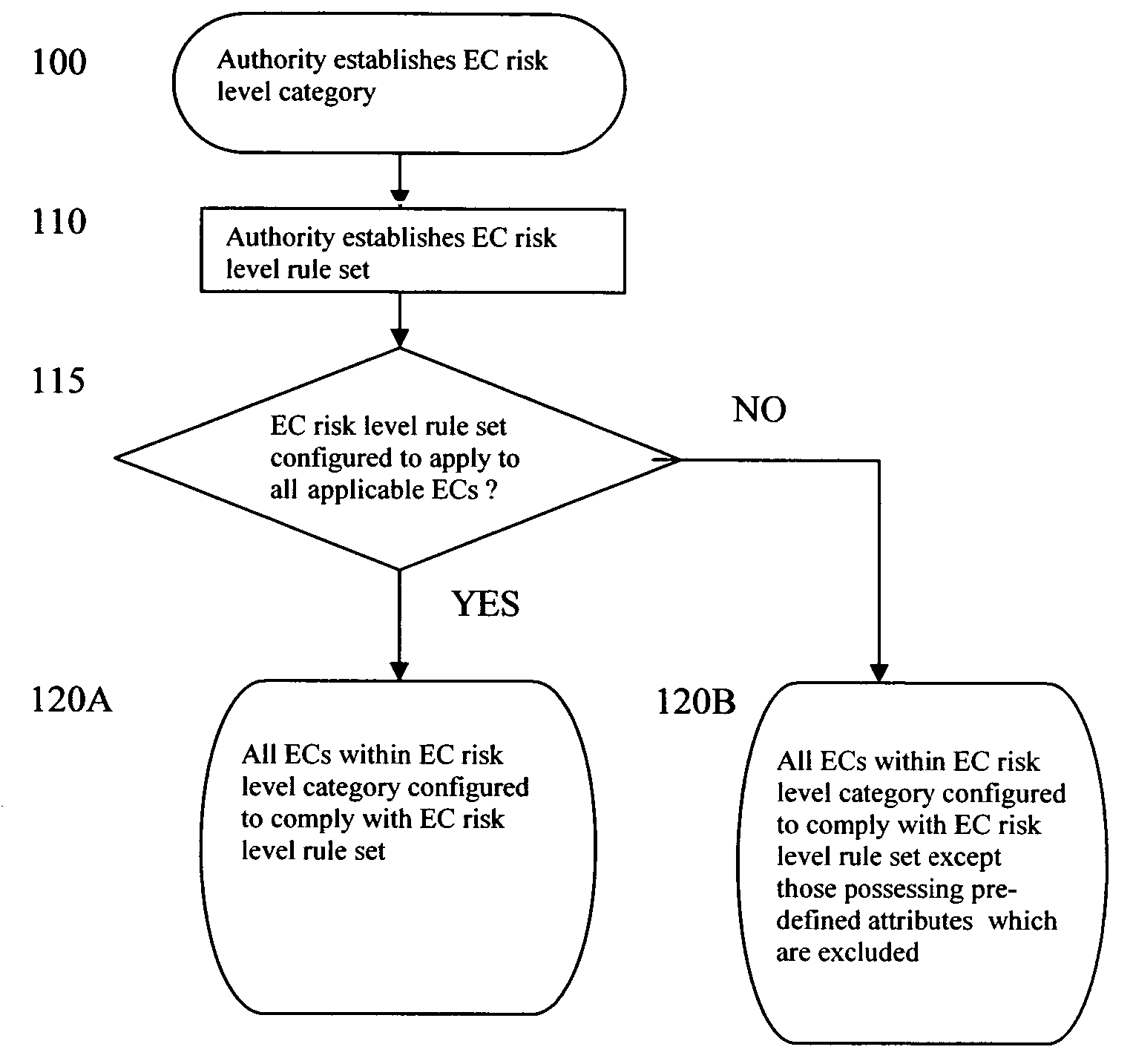
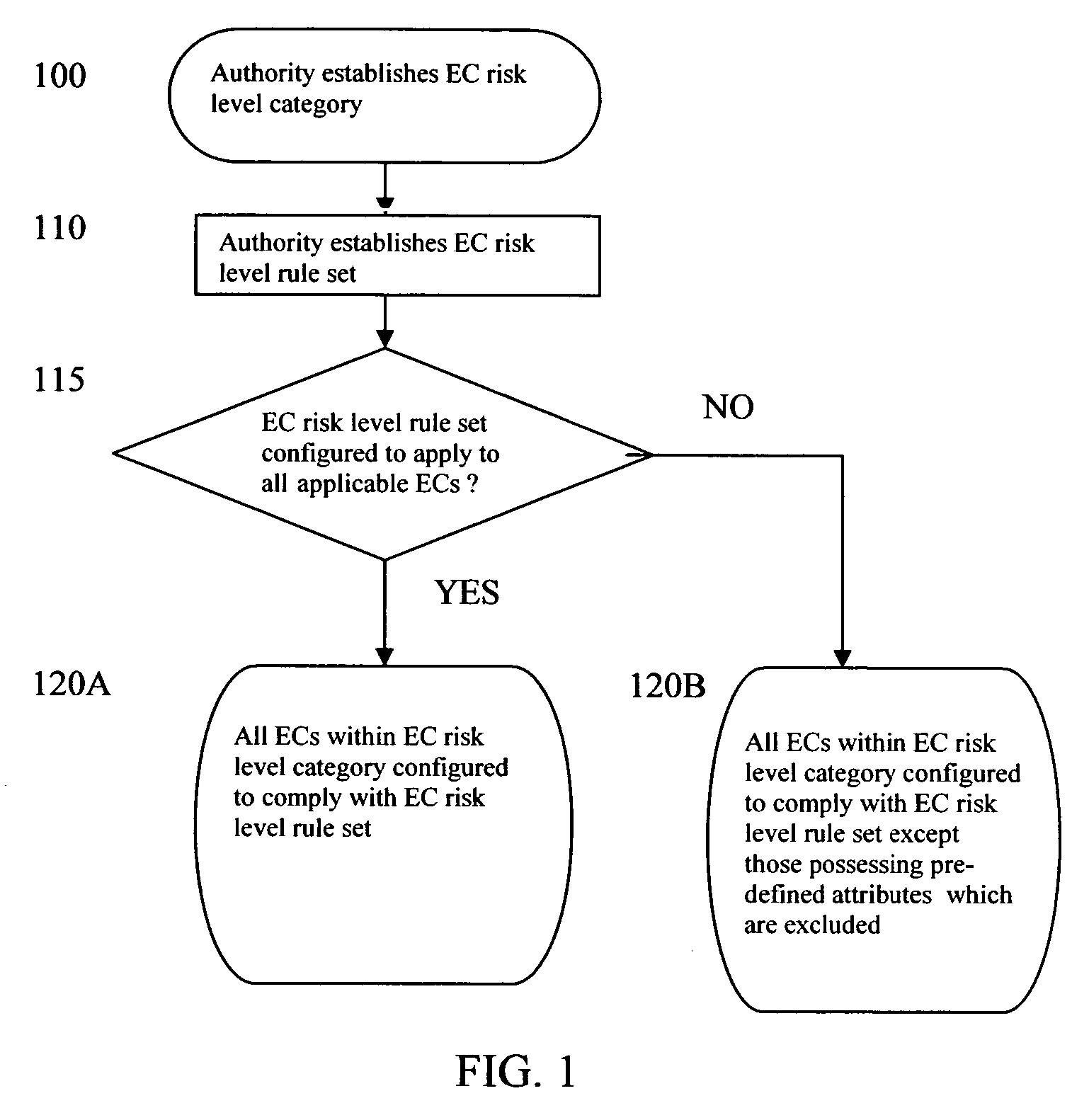
Method and system for electronic communication risk management
InactiveUS20060174111A1Reduce riskData switching networksSecuring communicationRisk levelPrior authorization
A method and system for electronic communication risk management through implementation of rule sets that impose electronic communication limitation options on electronic communications that meet the criteria for inclusion in an electronic communication risk level category. One such electronic communication limitation option gives an electronic communication a temporal life span after which it is automatically deleted from memory locations in which a copy of it is electronically stored. A second limitation option precludes an intended recipient from forwarding, copying, and / or printing the received EC. A third limitation option blocks electronic communications from being sent to certain recipients until prior authorization is obtained. The invention reduces the risks associated with electronic communication proliferation and inadequately managed electronic communications.
Owner:BURNS PAUL EDWARD
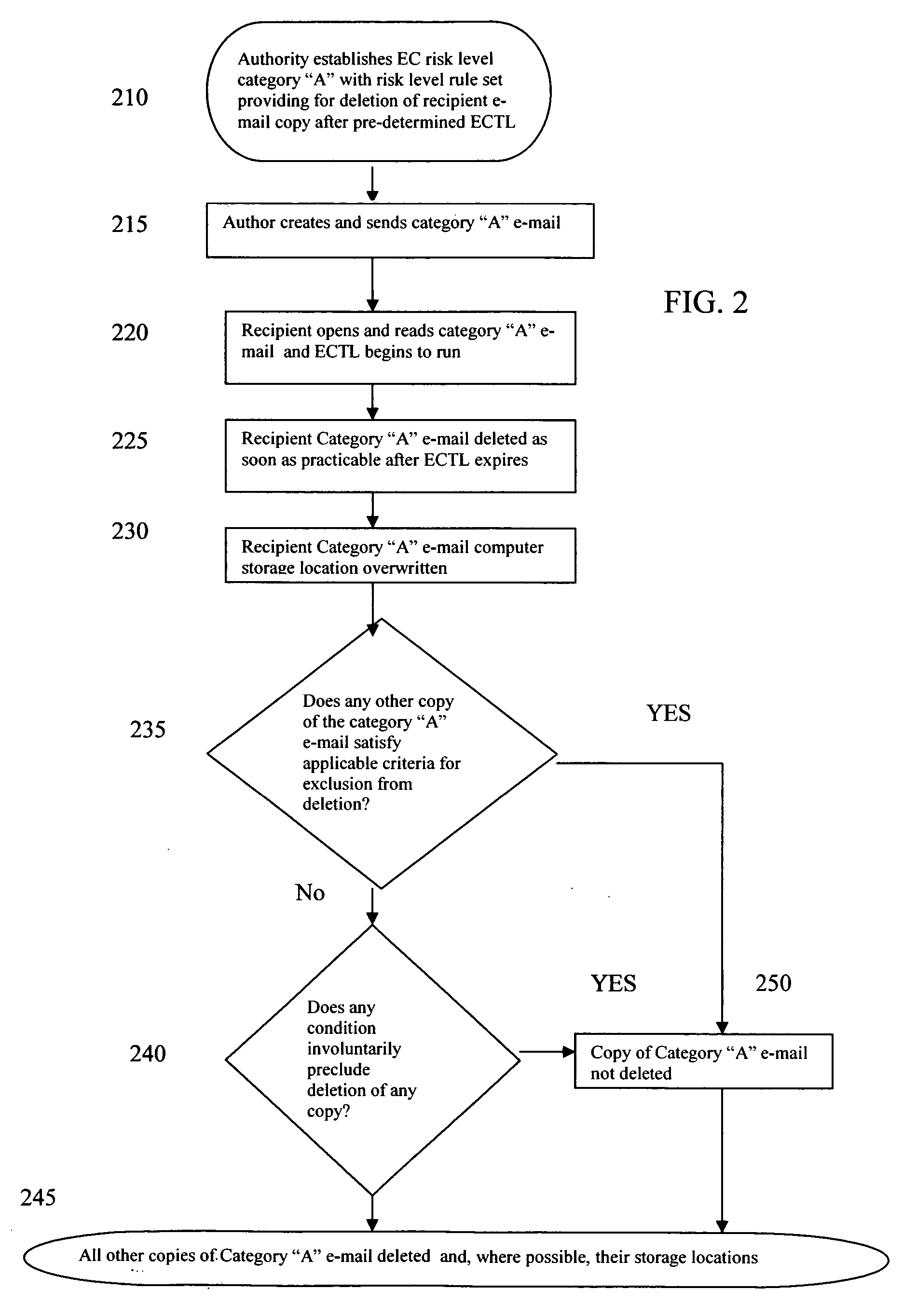
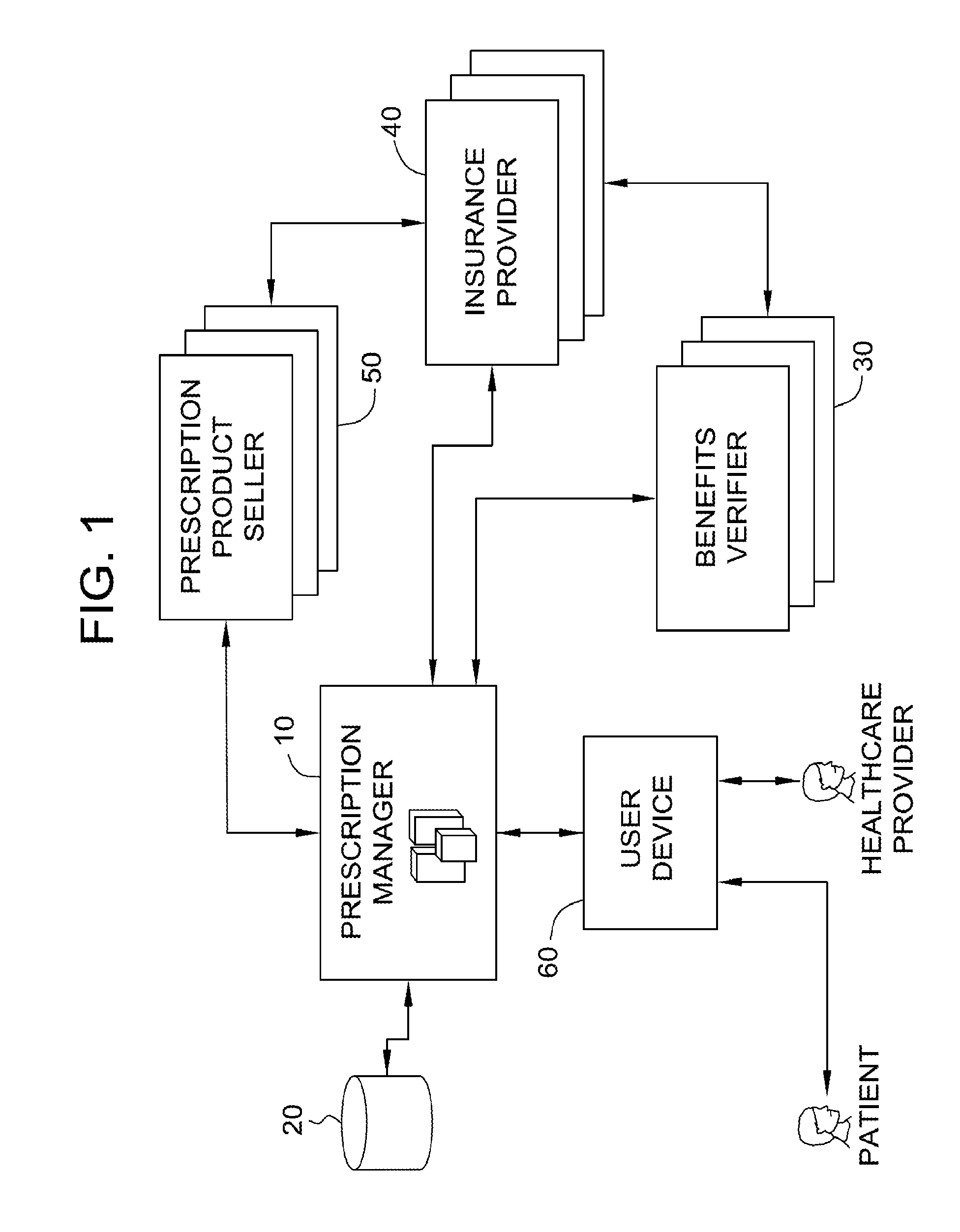
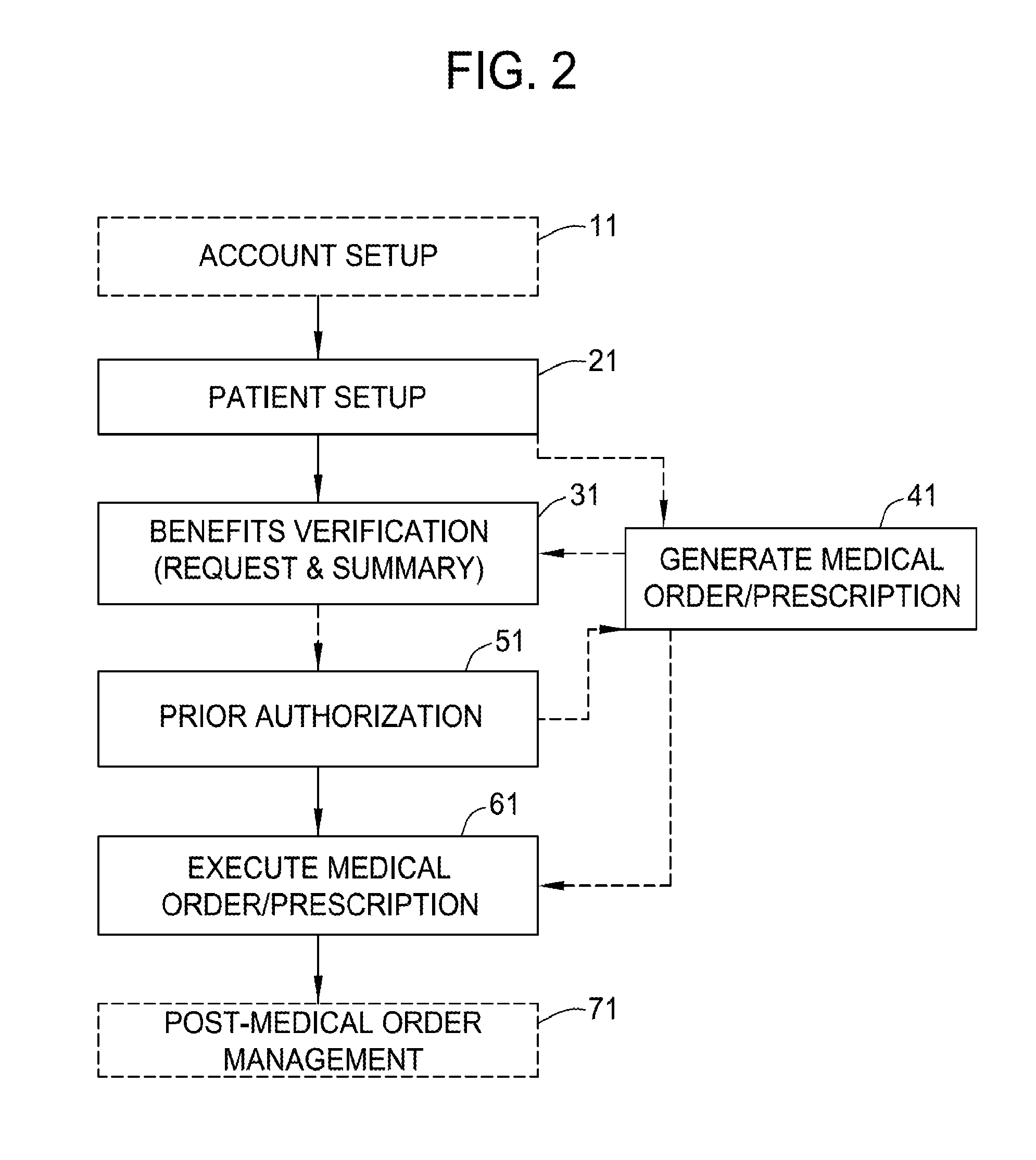
Managing healthcare services
InactiveUS20160342752A1Local control/monitoringDrug and medicationsFamily medicinePrior authorization
A computer system for processing a prescription for a prescription product prescribed by a healthcare provider (HCP) to a patient includes a memory device and a processor. The processor is programmed to receive patient data and insurance data from an HCP computing device, the patient data including a completed prescription form for the prescription product, and the insurance data identifying an insurance provider, wherein the prescription product is an antiviral product, store the patient data and the insurance data, determine a current electronic prior authorization request form, transmit the determined current electronic prior authorization request form to the HCP computing device, and prompt an HCP user to complete the determined current electronic prior authorization request form by enabling the HCP user to automatically populate at least one data field included within the determined current electronic prior authorization request form.
Owner:ABBVIE BIOTECHNOLOGY LTD
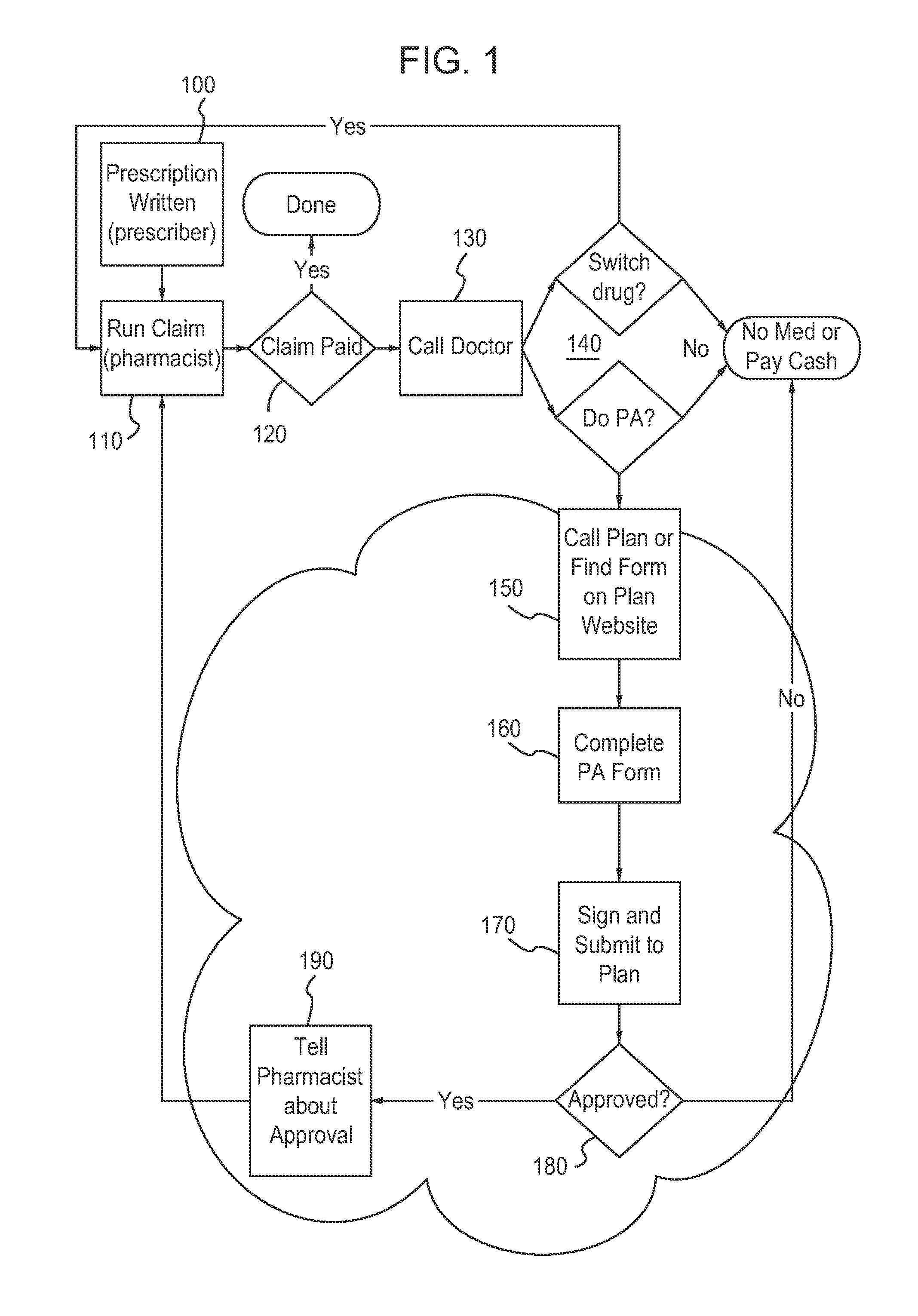
Prescription drug prior authorization system and method
ActiveUS20090198518A1Easy to useFacilitates submissionFinanceDrug and medicationsWeb sitePrior authorization
An online application for approving prior authorization requests for prescription drugs. The application is used by pharmacy benefits providers, physicians, and pharmacies to request prior authorizations for drugs and to receive approvals automatically if a requested drug meets authorization criteria. The online application is accessible through a group pharmacy benefits provider portal on a web site. Requests are processed through a pharmacy benefits manager computer that determines whether prior authorization is required and through a pharmacy benefits provider computer when the pharmacy benefits manager computer determines that prior authorization is required. Requests that meet certain authorization criteria are approved automatically. Requests that cannot be approved automatically are submitted for review by a clinical pharmacy review division that access requests through a drug request transaction computer.
Owner:HUMANA INC
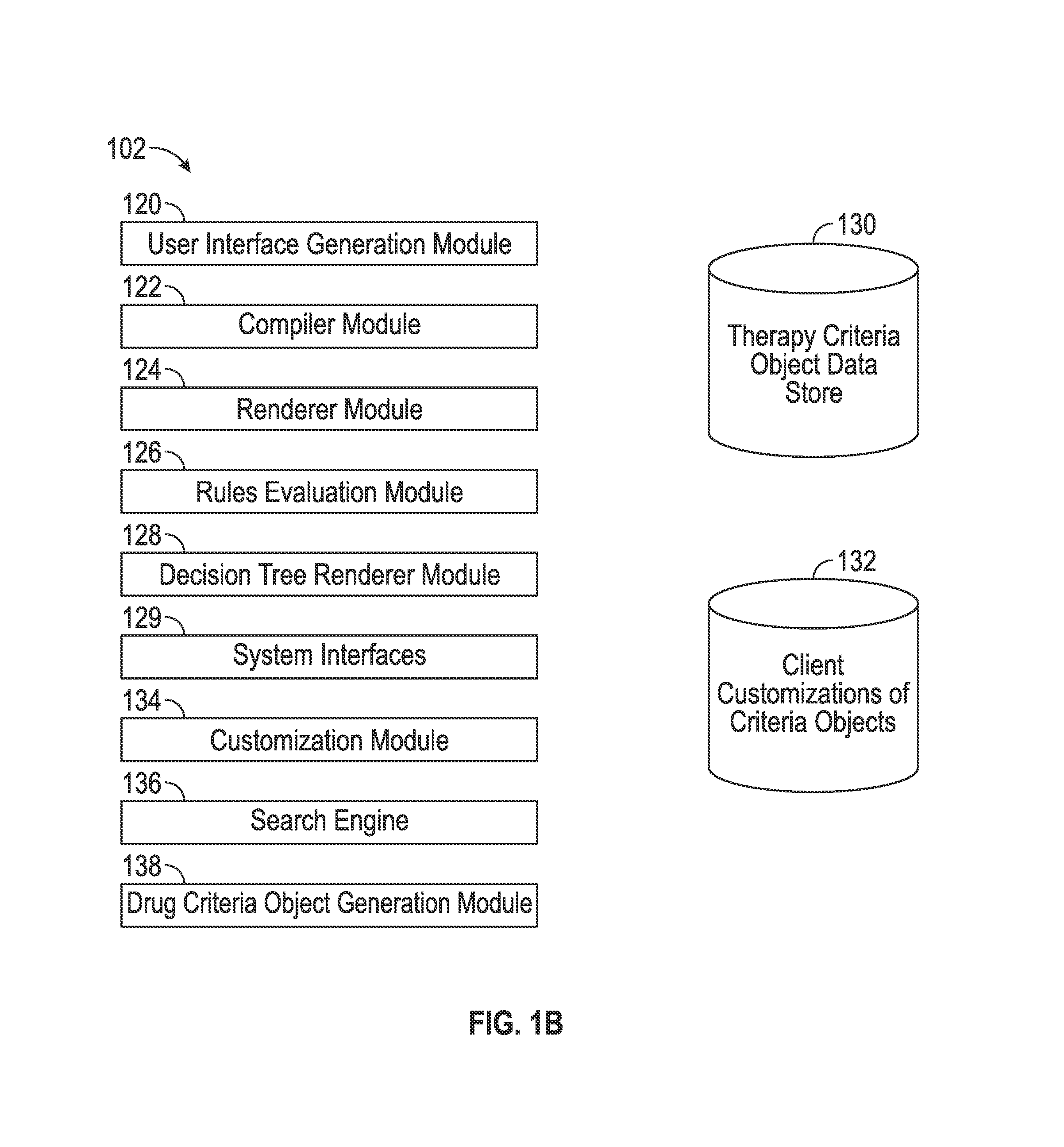
Methods and systems for pharmaceutical prescription authorization rules generation
InactiveUS20150324547A1Data processing applicationsDrug and medicationsStep therapyPrior authorization
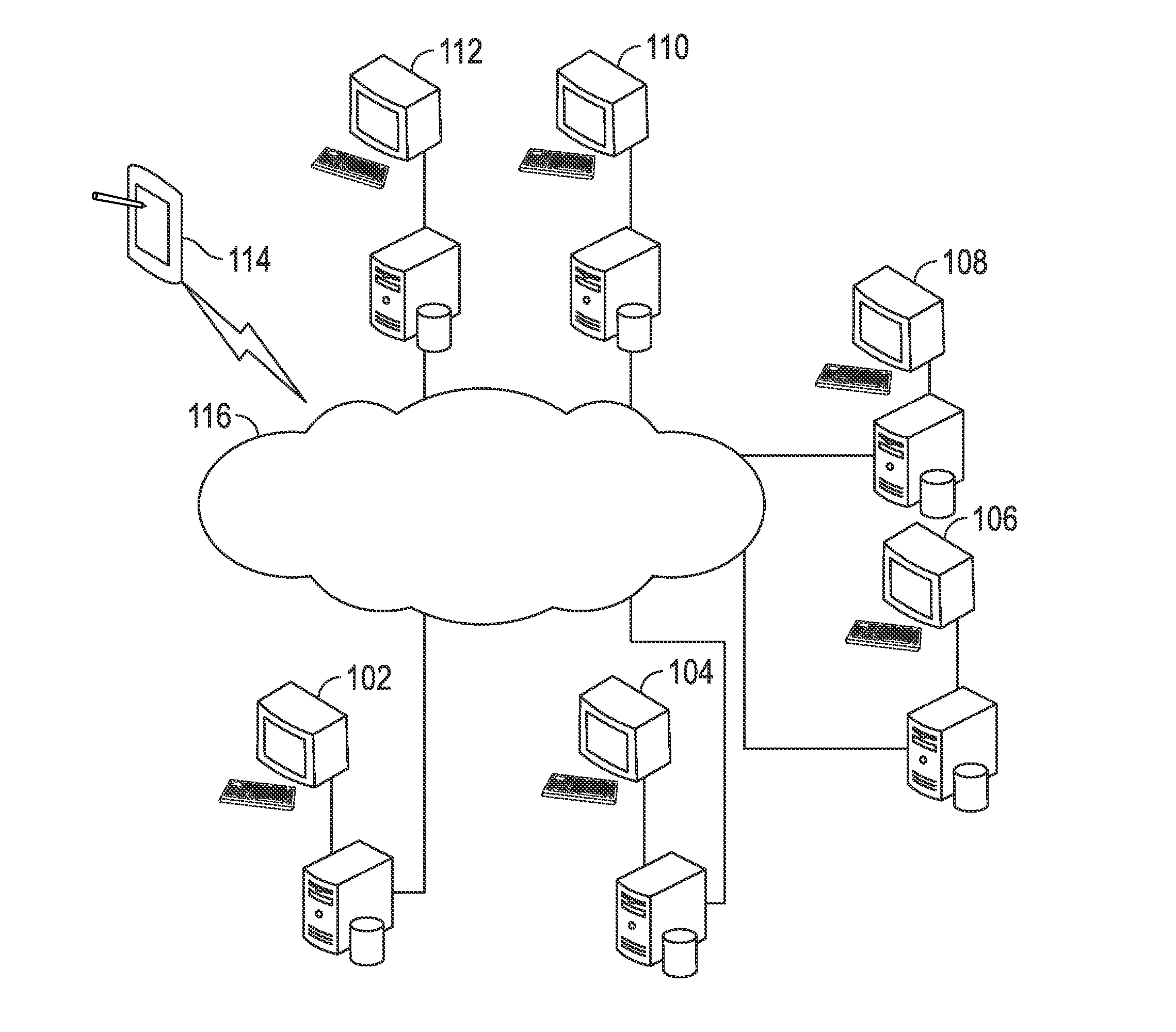
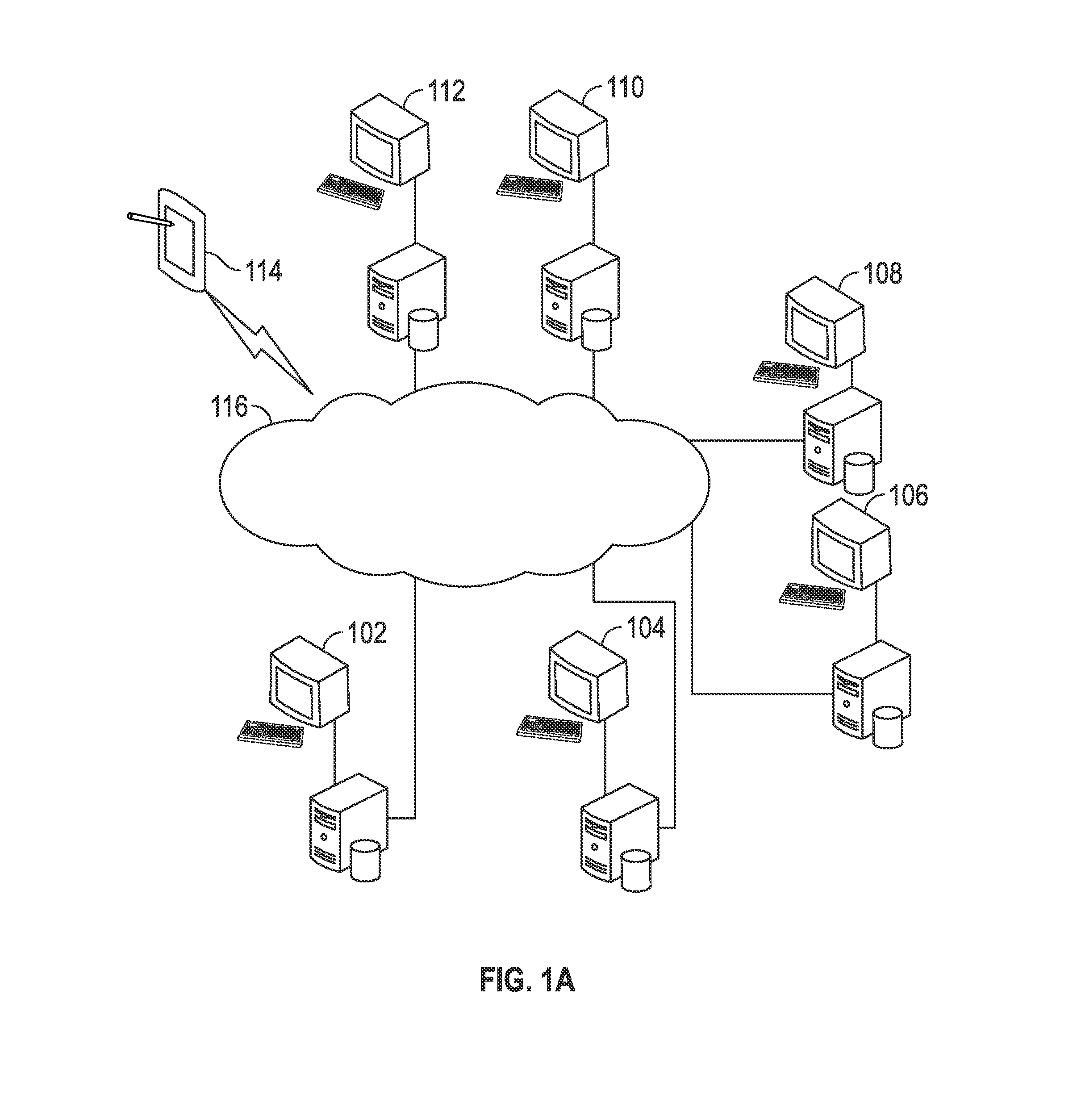
A system generates executable prior authorization drug request rules using a compiler. A data repository stores drug criteria. The system is configured to generate a criteria specification user interface that enables a user to specify exclusion criteria, inclusion criteria, preferred or step therapy criteria, concurrent therapy criteria, assessment criteria, quantity limits, and / or refill instructions. A prescription prior authorization rules compiler module is configured to access a criteria specification for the drug from the repository and to automatically compile the criteria specification into executable prescription prior authorization rules. A drug criteria object generation module is configured to generate a drug criteria object for the drug, including drug criteria object identification information, the executable prescription prior authorization rules, a data dictionary, and / or canonical data. A rules engine may be provided with access to the drug criteria object for execution of the prescription prior authorization rules.
Owner:HEARST COMM
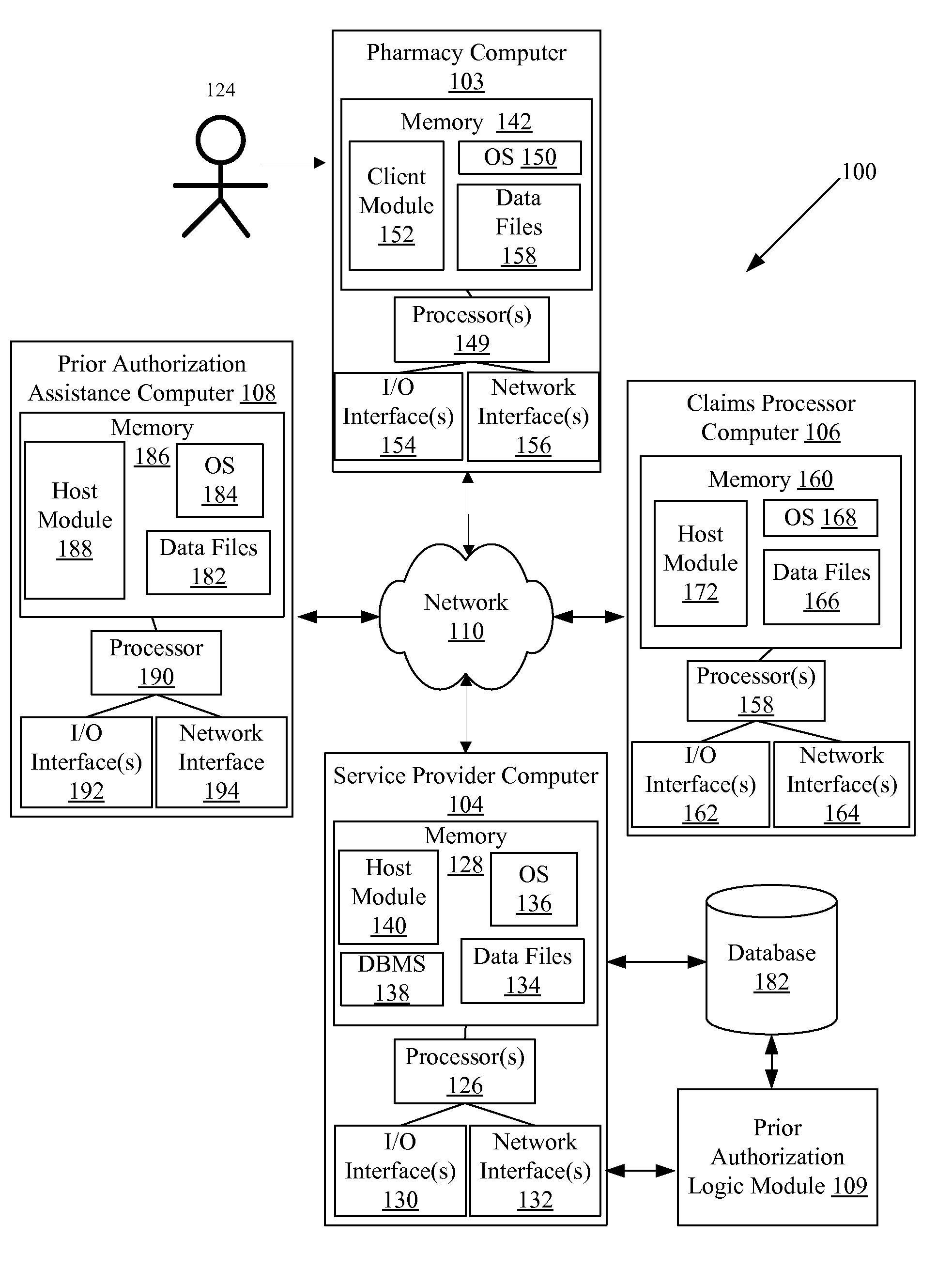
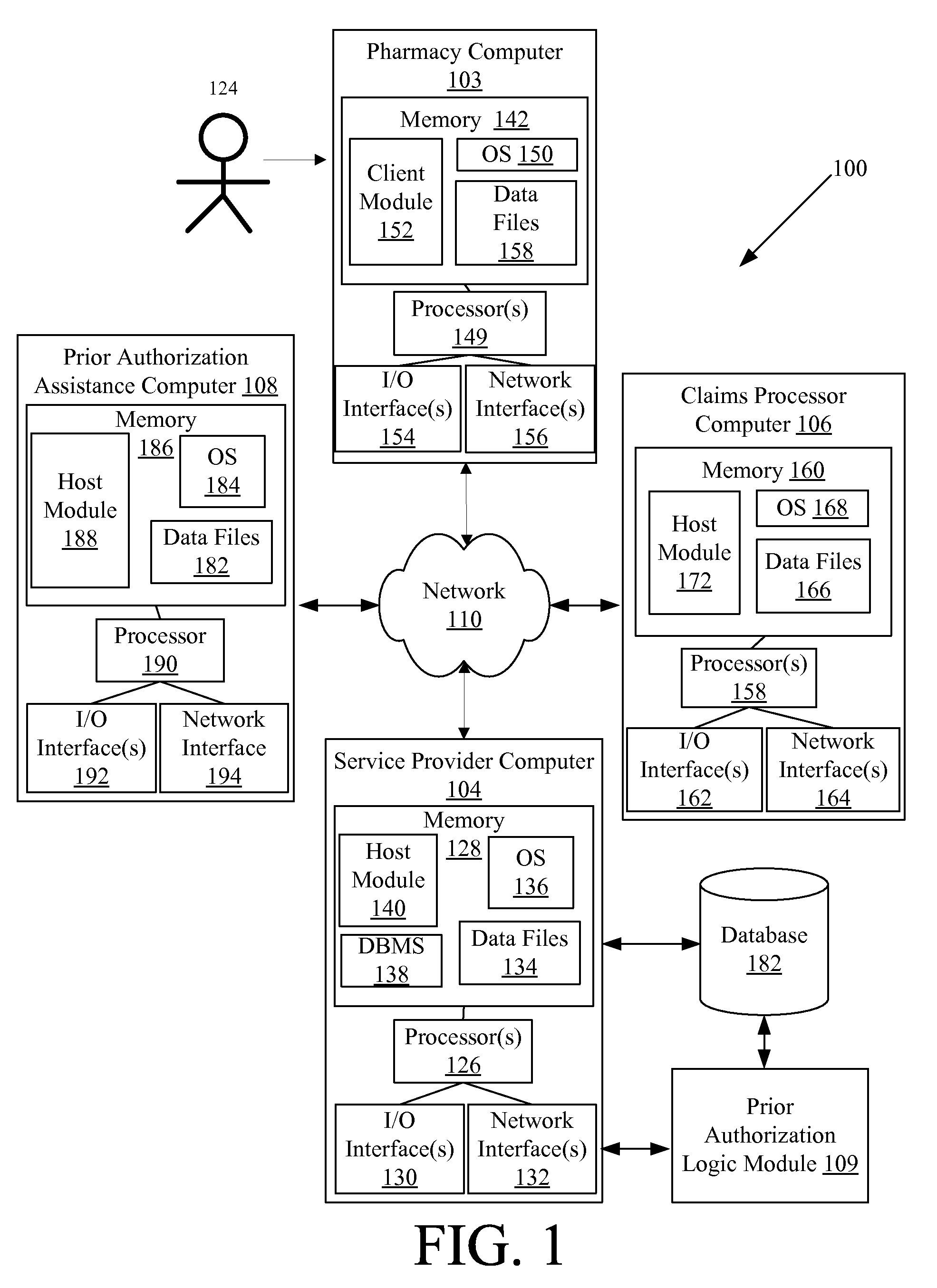
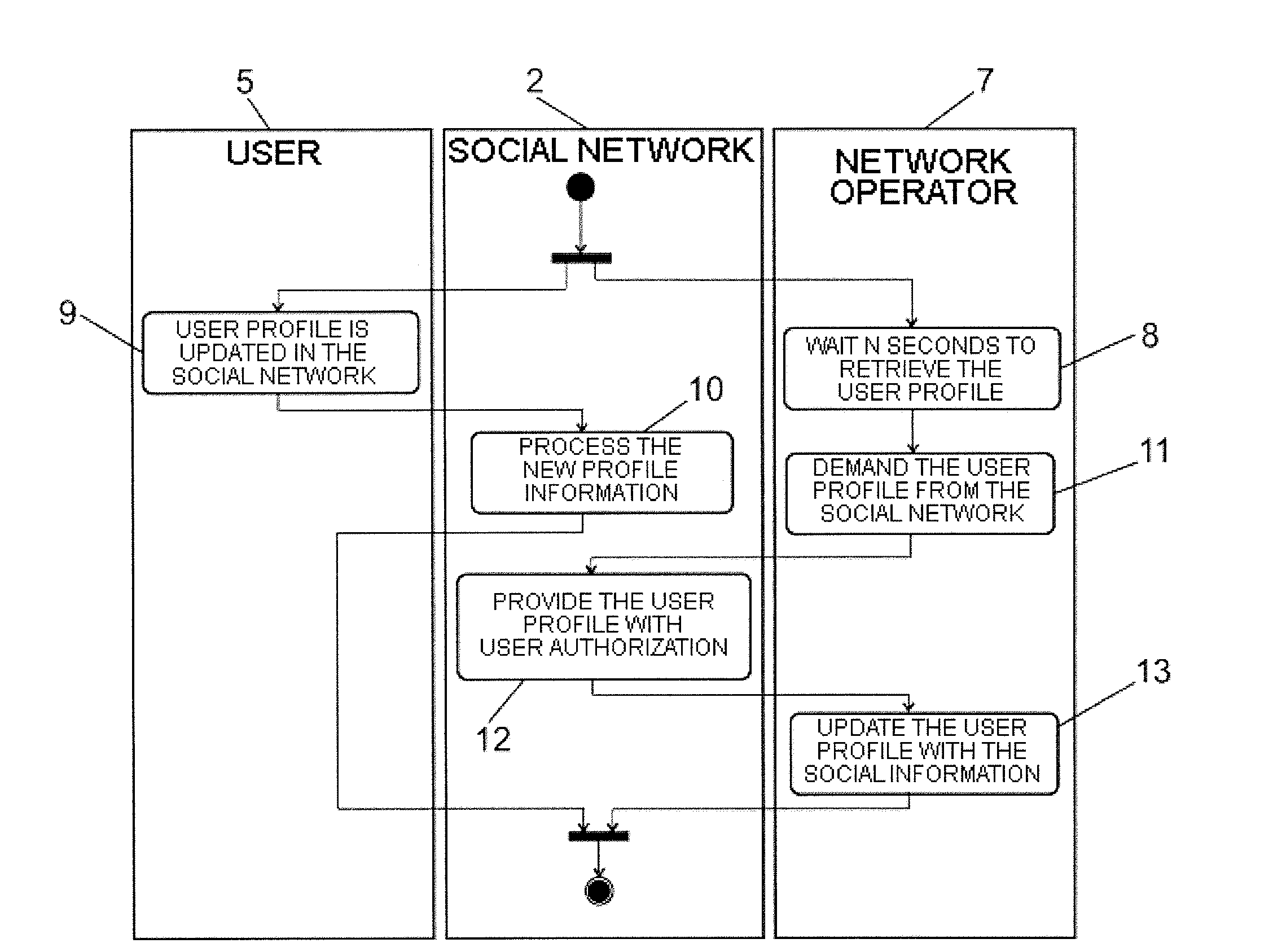
Systems and methods for facilitating claim rejection resolution by providing prior authorization assistance
Systems and methods are provided for providing prior authorization support. The systems and methods may include receiving a first request for prior authorization assistance from a pharmacy computer, wherein the request for assistance includes claim identification information for a prior healthcare claim transaction; identifying a stored transaction history record for the prior healthcare claim transaction, where the stored transaction record is identified based at least in part on the claim identification information, where the stored transaction history record indicates a denial of coverage by a payor of a drug or product for a patient; delivering, to a prior authorization assistance computer, a second request for prior authorization assistance, where the information included in the second request enables the prior authorization assistance computer to initiate a process for completing a prior authorization form and for delivering the completed form to the payor; and delivering, to the pharmacy computer, a response indicating acceptance of the first request for assistance.
Owner:MCKESSON CORPORATION
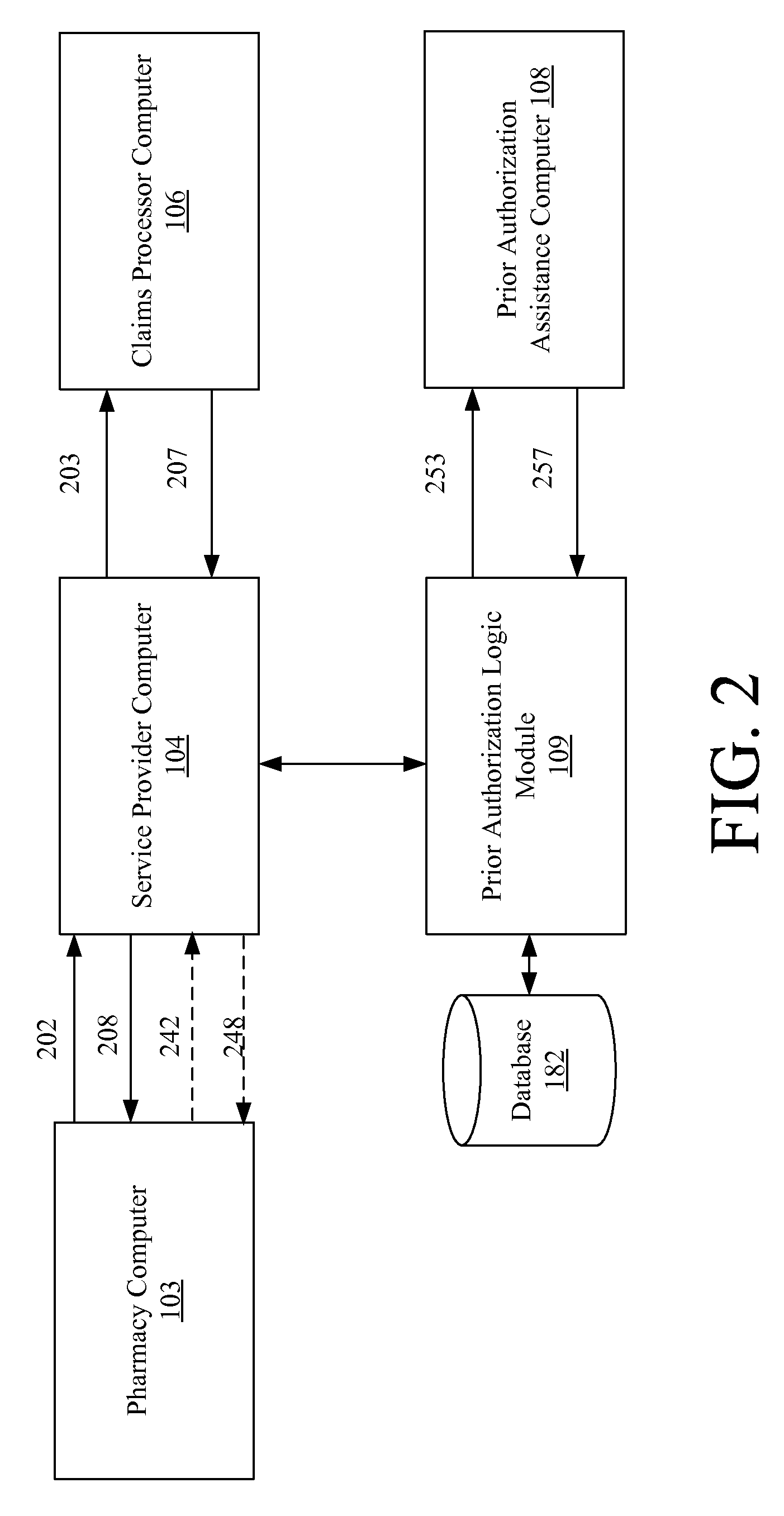
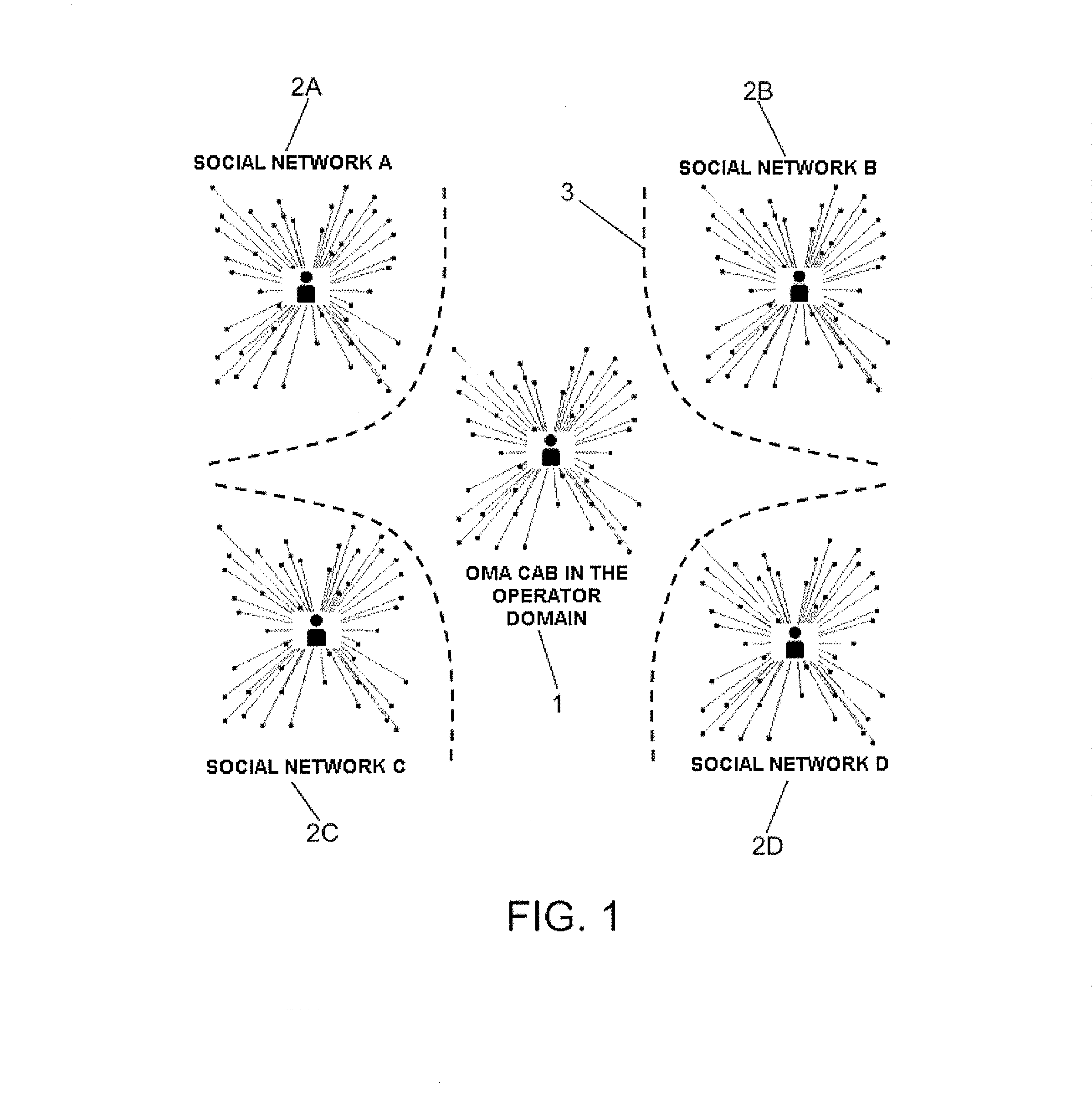
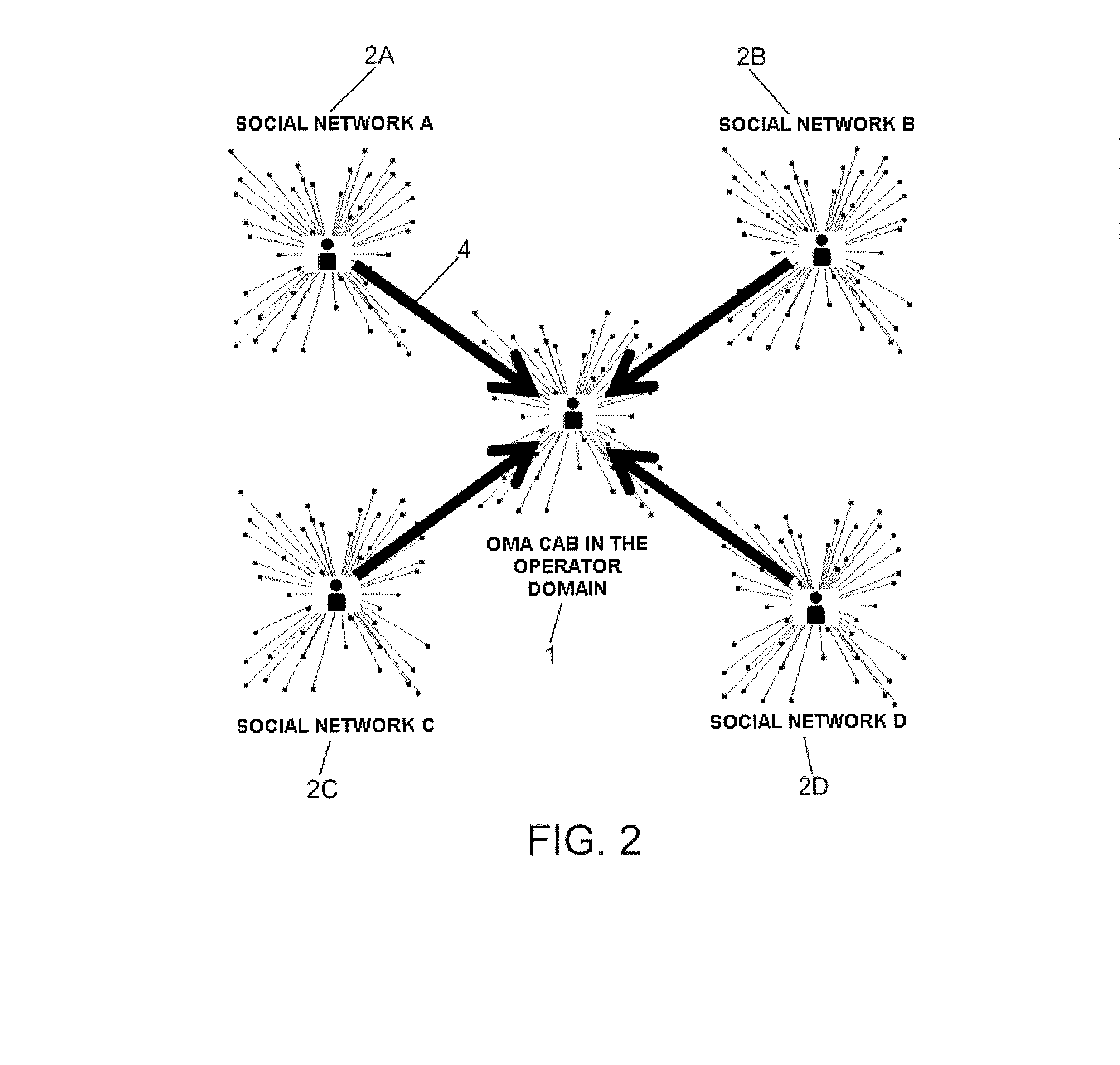
System and method for synchronizing the profile of a user in social networks and the user's personal contact card (PCC)
InactiveUS20130110776A1Service provisioningDigital data processing detailsAddress bookPrior authorization
The method and system for synchronizing social networks and Personal Contact Cards (PCC) update the profile of a user published in an Open Mobile Alliance Converged Address Book (OMA CAB) system with the information published and updated on one or more social networks to which the user subscribes, by means of synchronization by polling or synchronization by subscription / notification. To do so, the user sends prior authorization to access the user profile published in the social network to a telecommunication services provider operating the OMA CAB system.
Owner:TELEFONICA SA
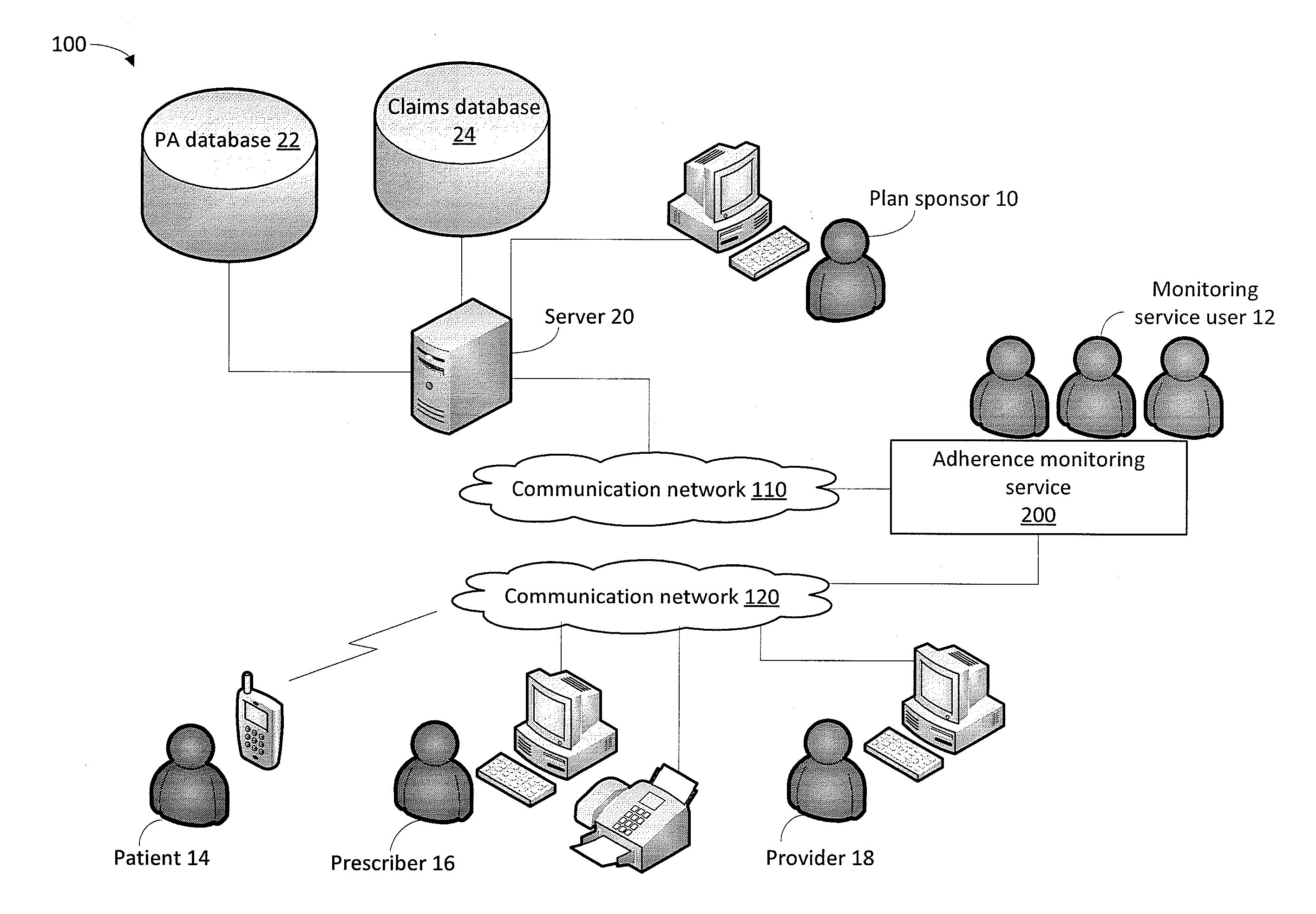
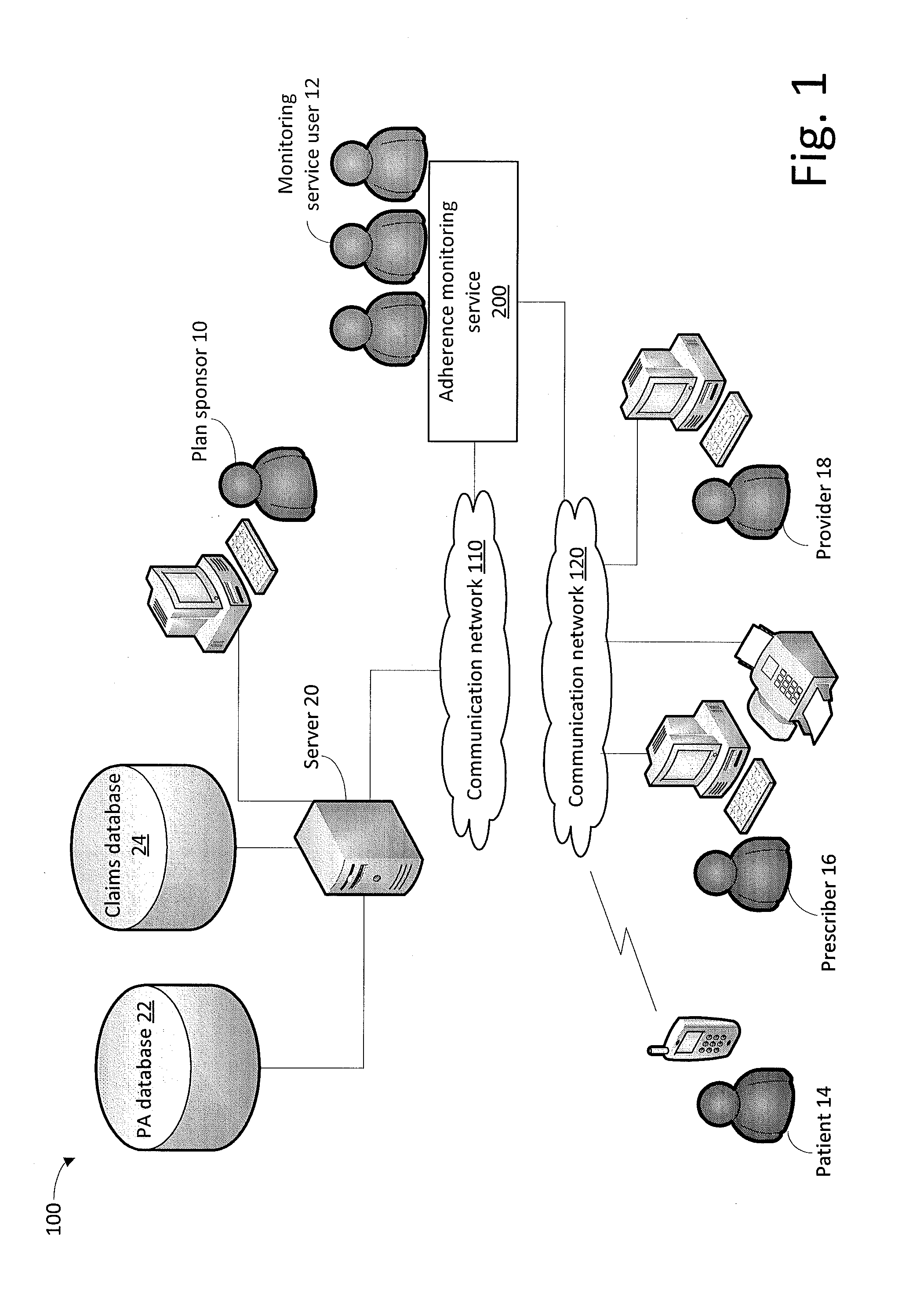
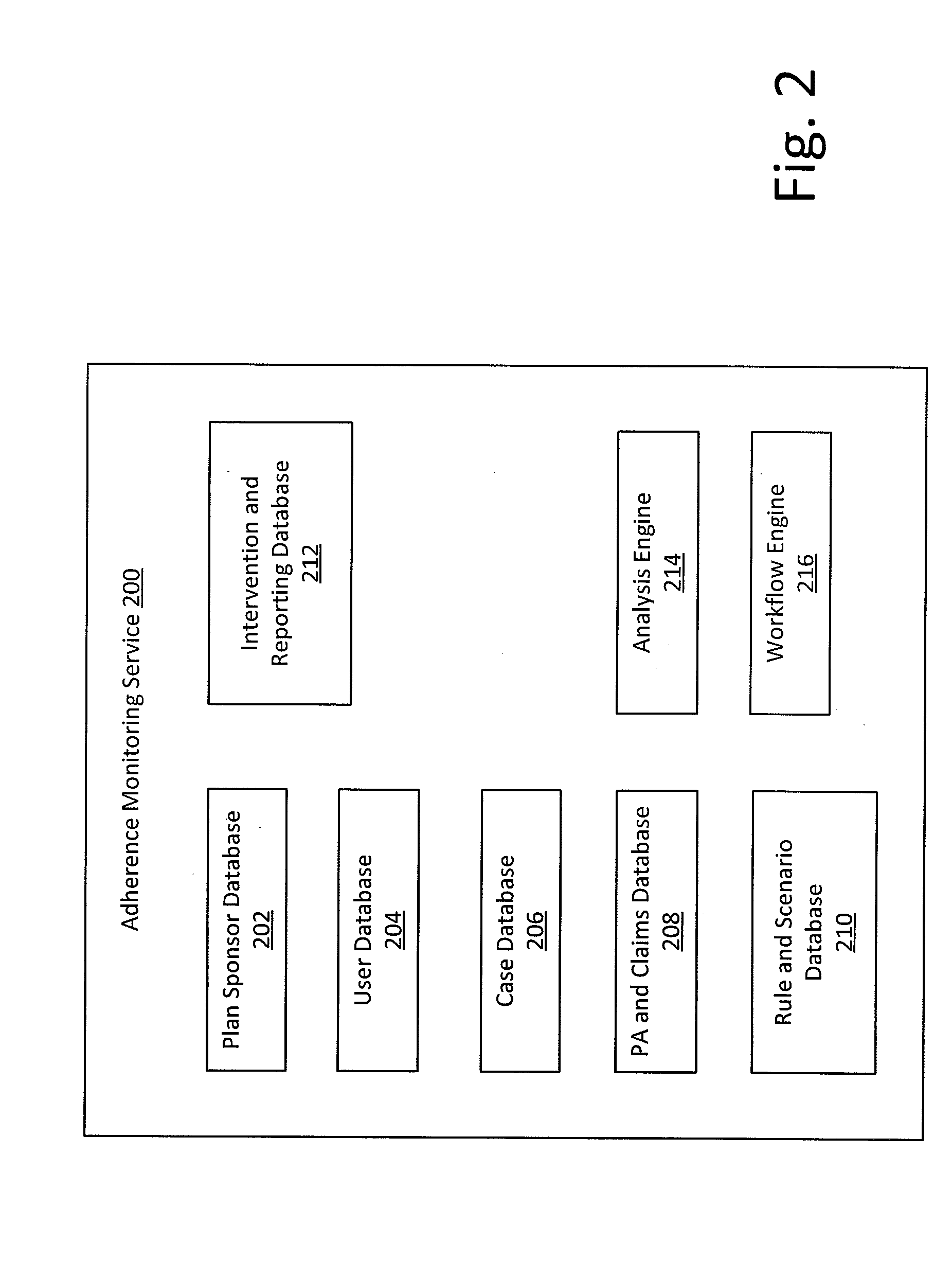
Method and system for monitoring medication adherence
InactiveUS20150248540A1Effective guidanceFinanceDrug and medicationsMedication adherencePrior authorization
A system and method for monitoring patient adherence to prescribed medications include a processor that analyzes prior authorization data and insurance claims data based on adherence rules, which are user configurable. The system assigns non-adherence cases for user review by creating work queues. Queues may be associated with respective user roles. In response to a non-adherence case, the system generates automated notifications using a notification template. Placeholder variables are insertable into the templates to describe a parameter applicable to a specific instance of non-adherence. The placeholder is replaced by an actual value of the parameter when a notification document is subsequently generated.
Owner:AGADIA SYST
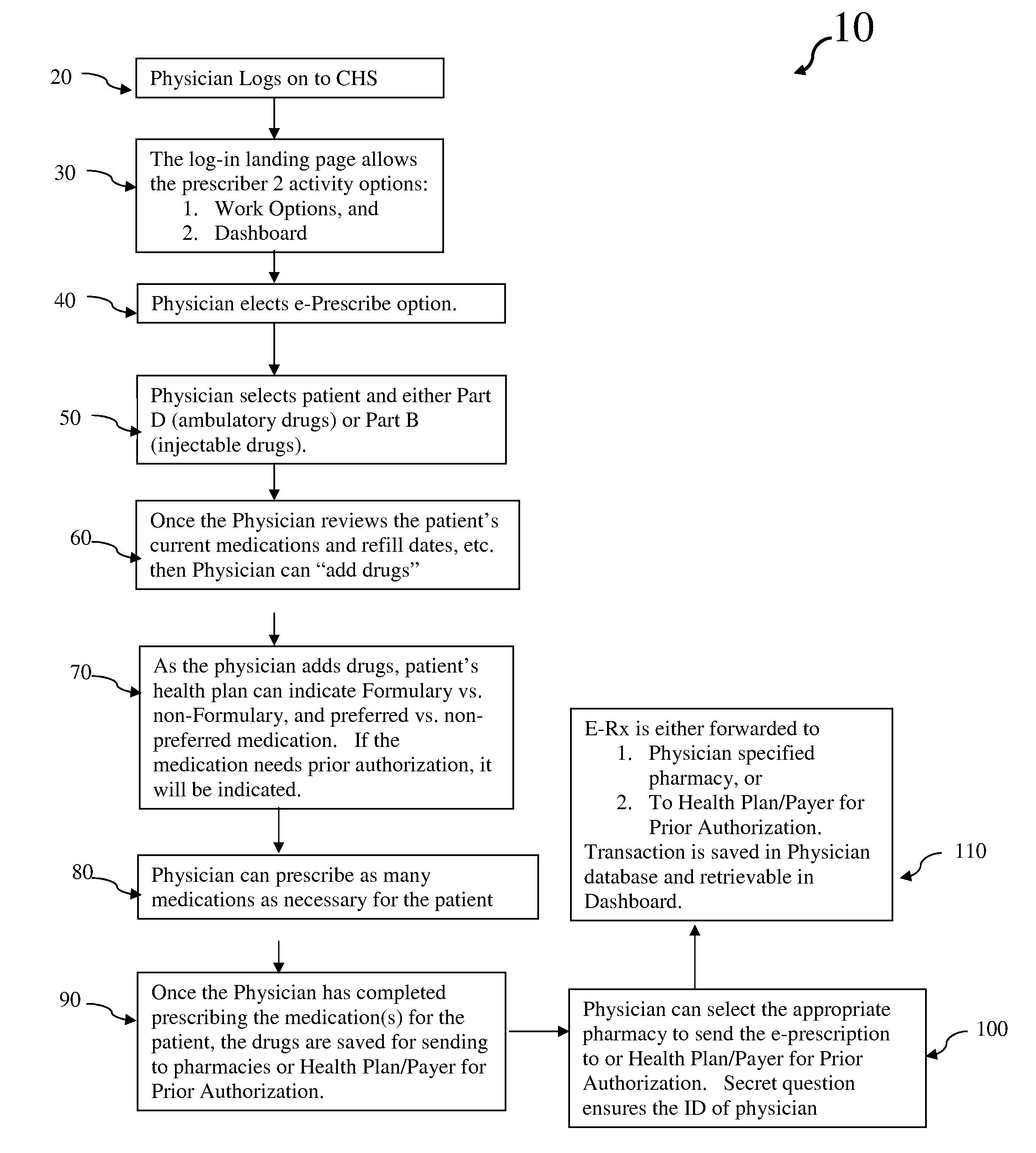
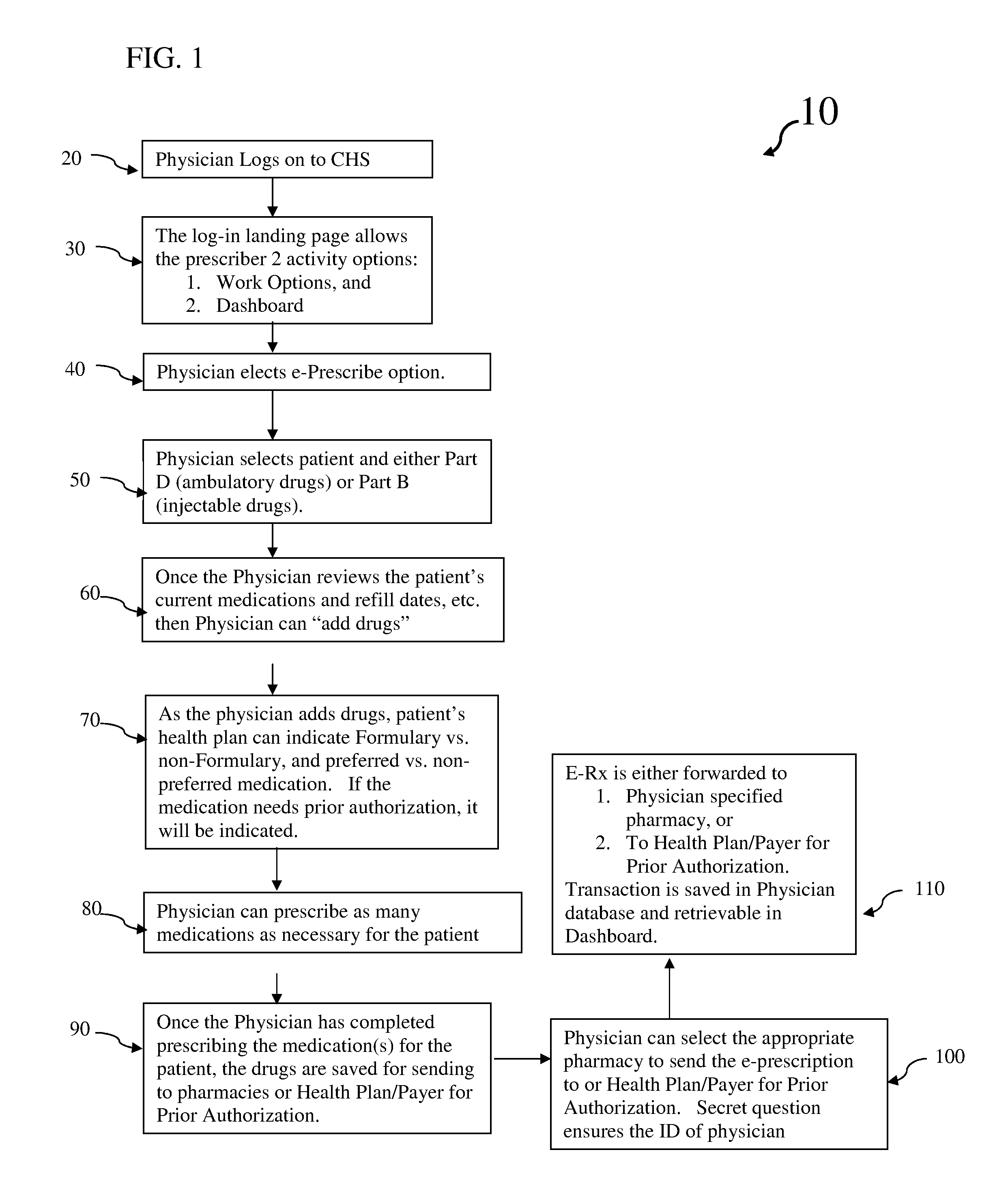
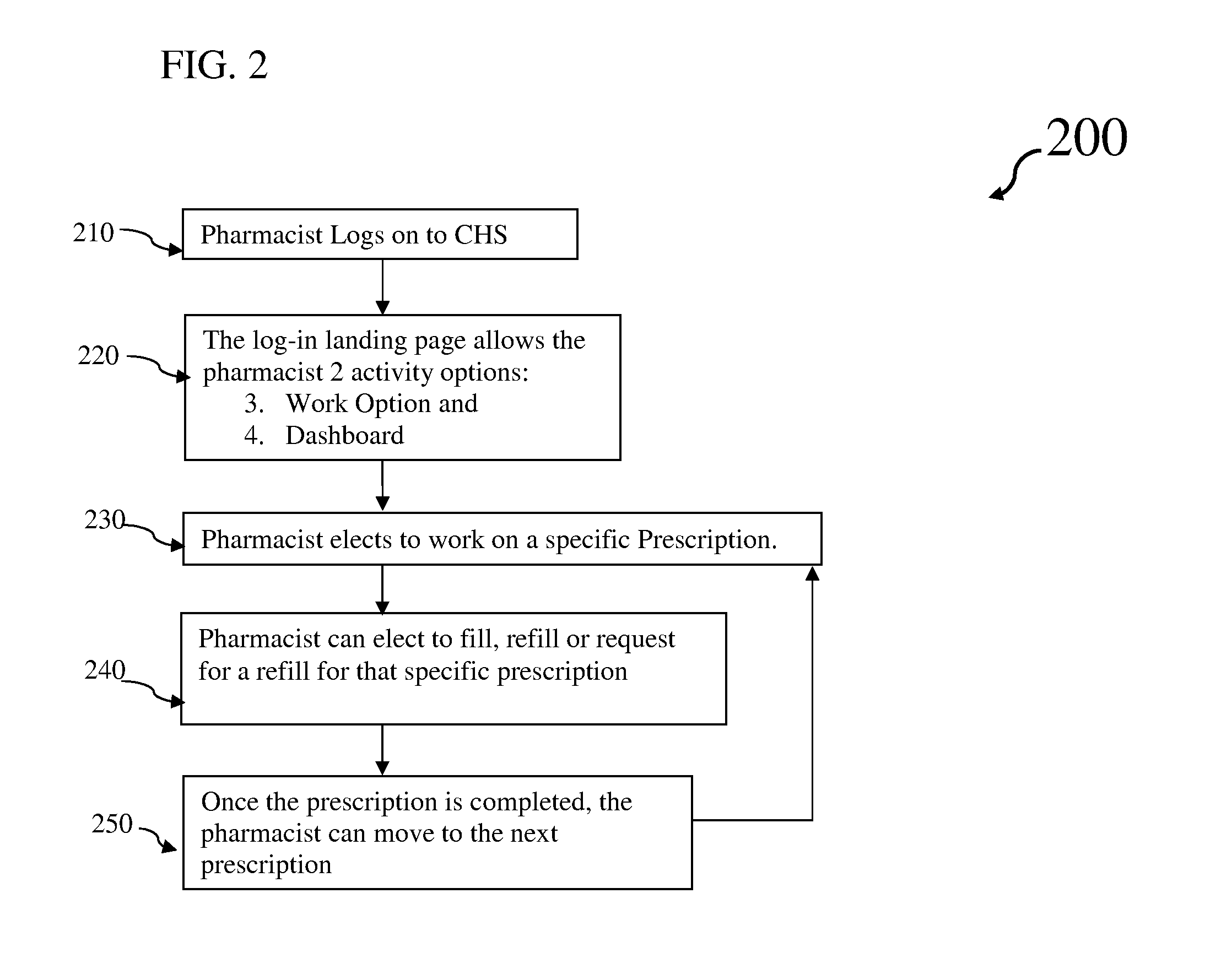
Interactive web-based prescription system and method
InactiveUS20130060575A1Eliminate inefficienciesEliminate cost over-runsFinanceDrug and medicationsFormularyDispensary
Systems and methods for facilitating electronic prescriptions and the dispensation of medications subject to prior authorization and / or adherence to a pre-established formulary. A web-based interactive system is established whereby all entities responsible for the prescription event, namely, the prescribing physician, pharmacist / pharmacy and payer / authorizing entity are kept in direct communication with one another via a conventional, secure communications link. All pertinent information regarding the prescription, as well as the patient, is made available to all entities and further, all information associated with a particular formulary is uploaded and made available to the prescribing physician and pharmacist for quick reference as the whether or not a given medication is preapproved. The systems and methods of the present invention are exceptionally effective and efficient, and can be readily utilized with all medications designated as either Part B or Part D per the United States' Medicare healthcare administration system.
Owner:NEE CHRISTOPHER
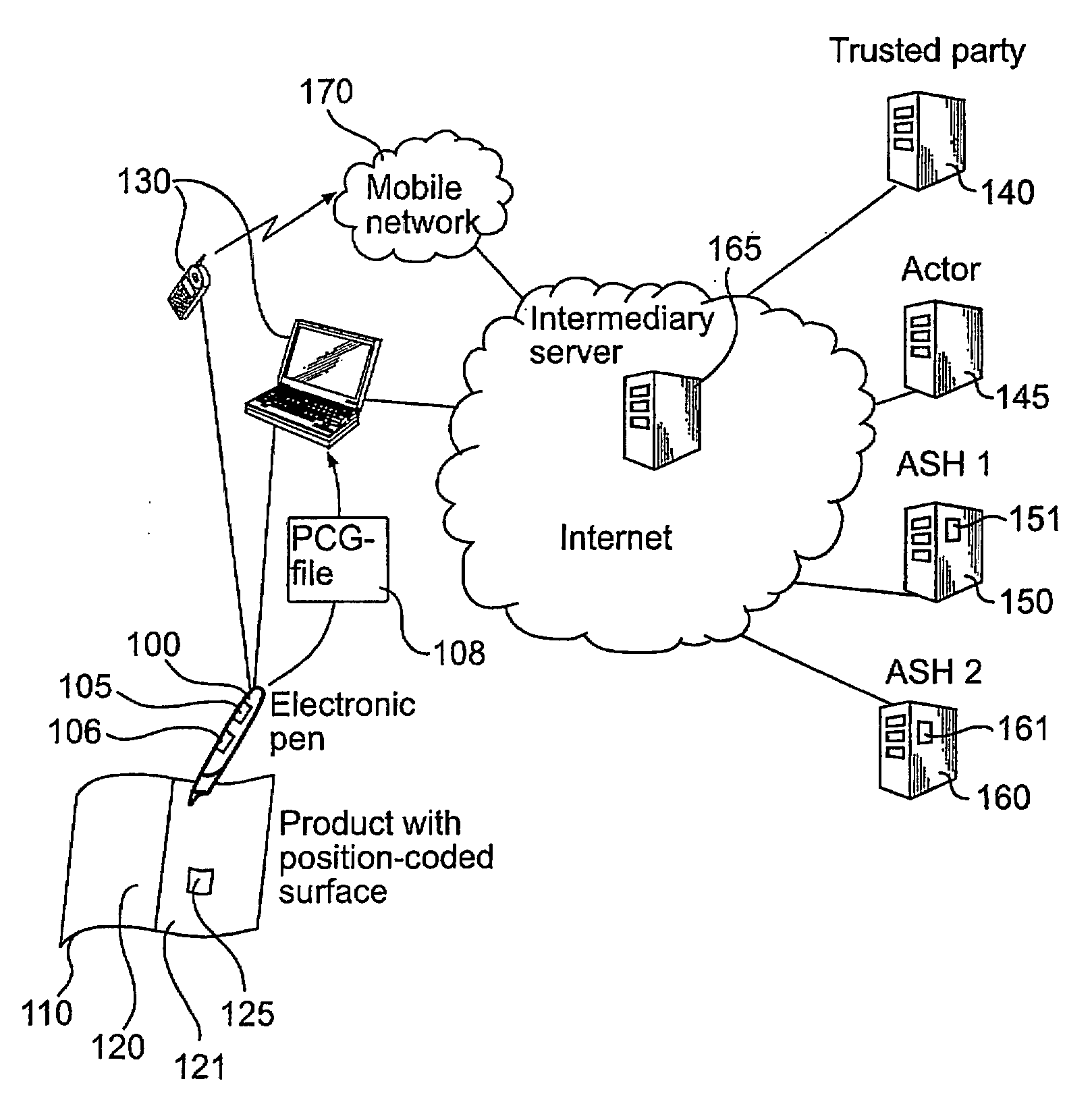
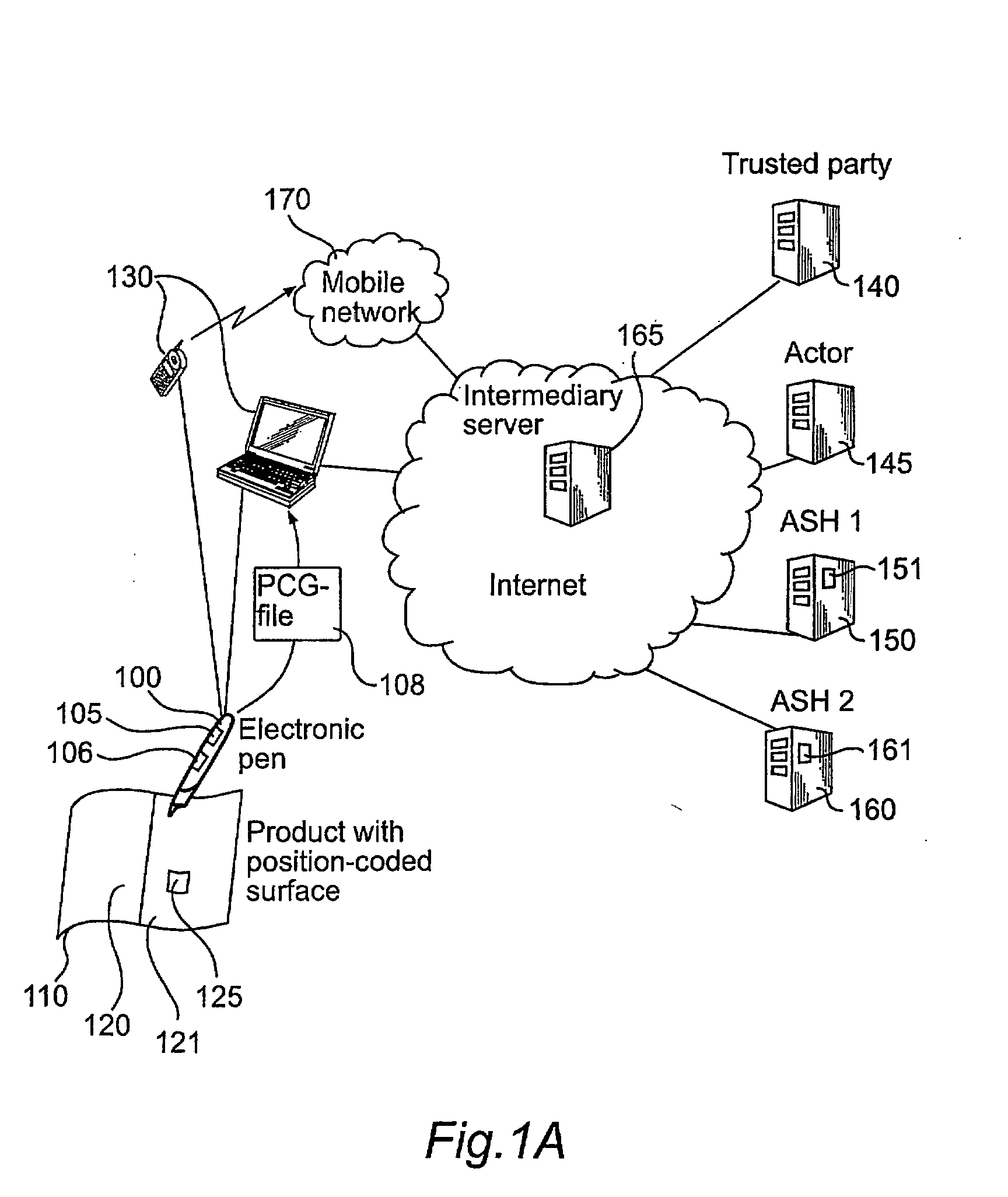
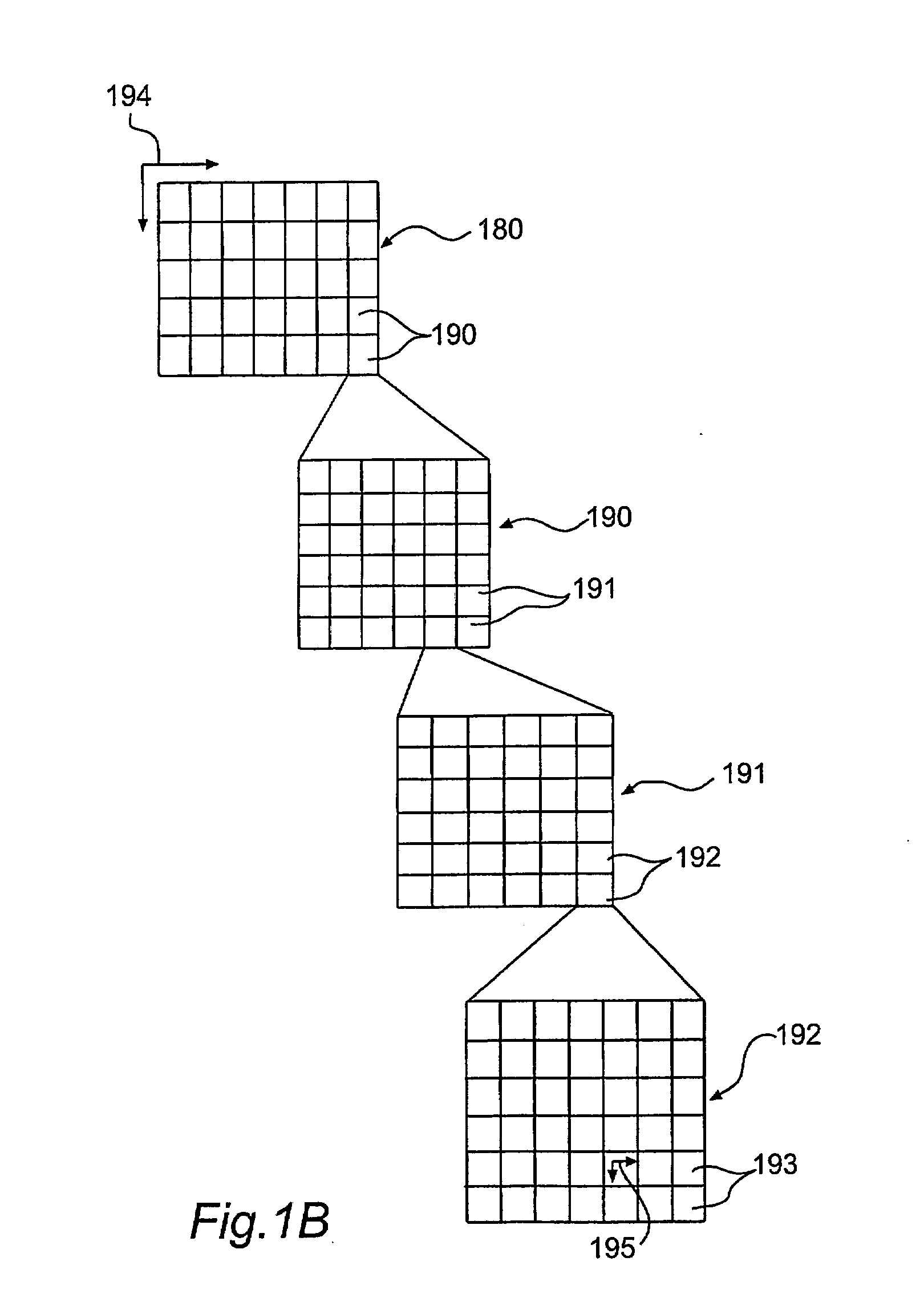
Secure management of information
InactiveUS20090019292A1Provide securityEncryption apparatus with shift registers/memoriesUnauthorized memory use protectionPrior authorizationDigital signature
Methods and system are devised to provide security with regard to position data recorded by an electronic pen. The position data originates from a specific area of a position-coding pattern and is destined for a specific Application Service Handler, ASH, which is allocated the specific area of the pattern. The pen stores one or more Pen Application Licenses, PALs, which each includes license data in association with an encryption key, the license data identifying an area of the pattern. The encryption key of a given PAL corresponds to an encryption key of a given ASH. Thus, the PALs enable the pen to encrypt recorded position data, originating from the specific area of the pattern, with the encryption key that is related to the encryption key of the receiving ASH. The license data may further define a group of pens and a validity period, allowing a party generating a PAL to control its use. Generating a PAL may in turn need prior authorization, given by PAL validation data derived from an authorizer. The PAL validation data, which is to be included in the PAL, may set boundaries for the license data that can be included in a PAL, and may also be digitally signed by the authorizer. The pen may be prohibited to install the PAL unless its license data can be properly validated against the PAL validation data.
Owner:ANOTO AB
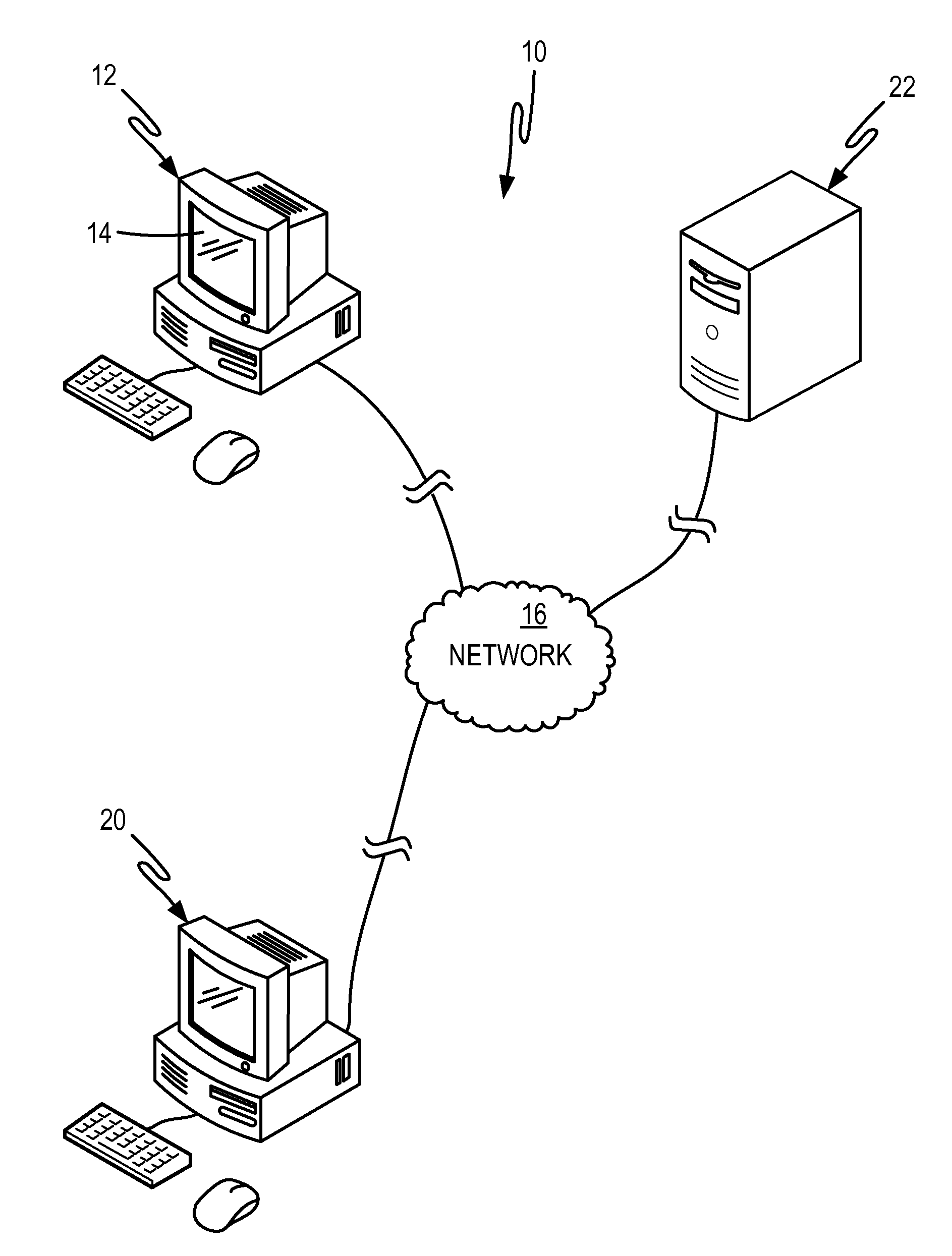
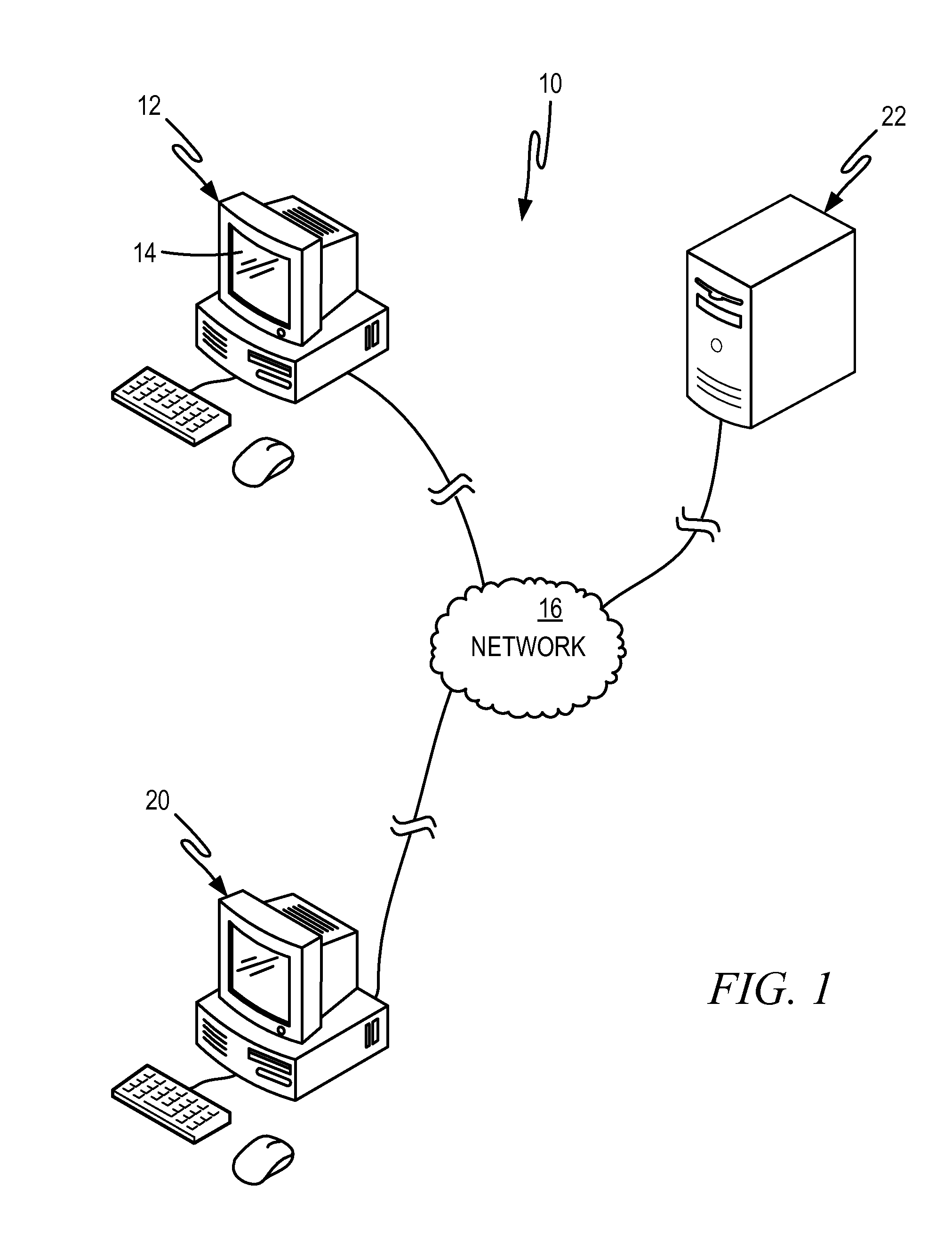
Apparatus and method for processing prior authorizations for prescription drugs
An apparatus, a method, and a computer program product are provided. The apparatus includes at least one memory including computer program code, and at least one processor. The at least one memory and the computer program code are configured to, with the at least one processor, cause the apparatus at least to receive a request to generate a prior authorization form for a prescription drug, select the prior authorization form from a plurality of prior authorization forms based on the request, and transmit the selected prior authorization form to a user so that the user can complete and submit the prior authorization form to the health plan and receive a determination on the request. The prior authorization form is selected based on at least one of a user search result and a standardized transaction.
Owner:COVERMYMEDS
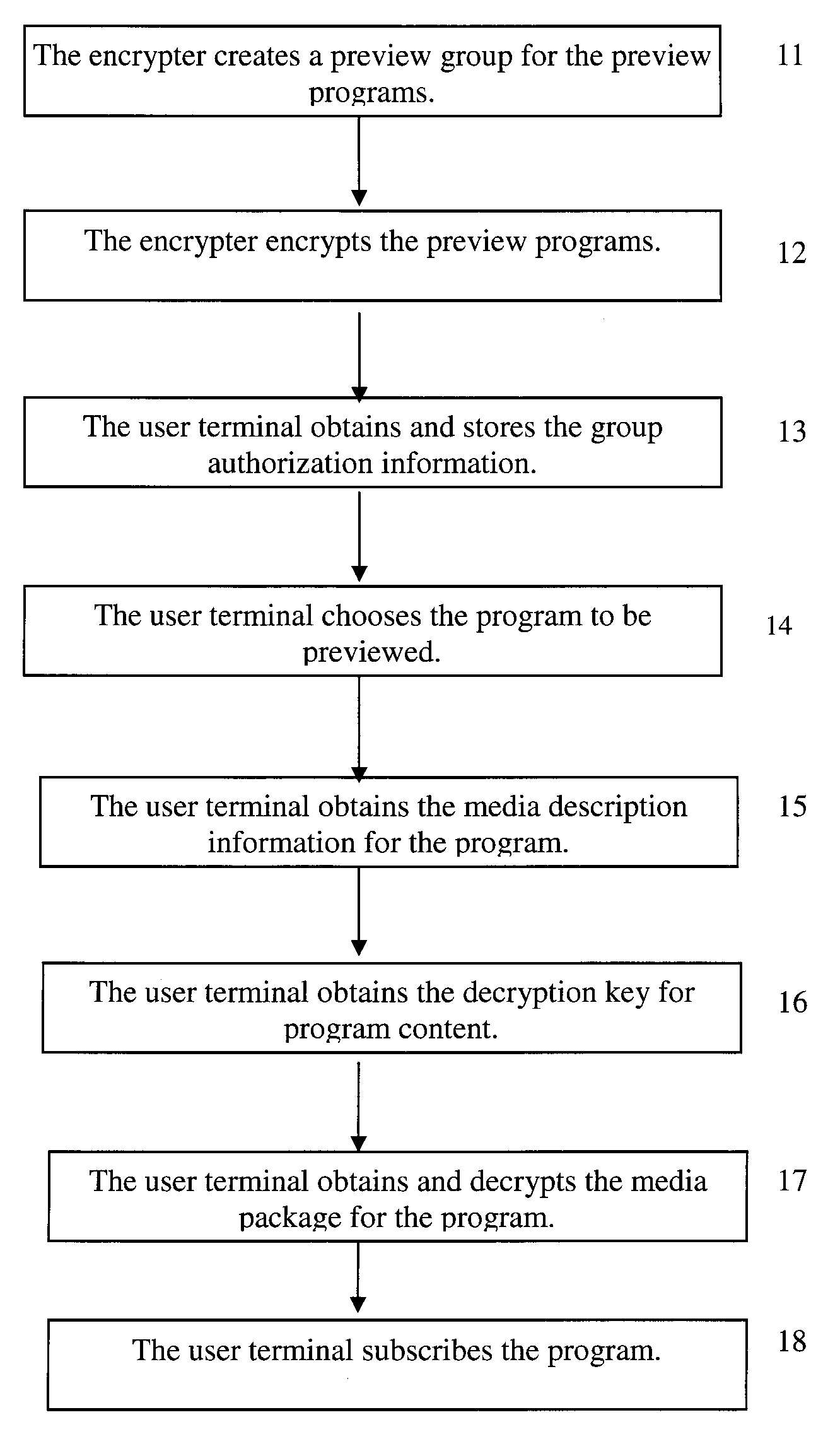
Method for realizing preview of IPTV programs, an encryption apparatus, a right center system and a user terminal
InactiveUS20080123844A1Reduces concurrent trafficImprove system reliabilityPulse modulation television signal transmissionTwo-way working systemsPrior authorizationSoftware engineering
A method for implementing preview of IPTV programs, an encryption apparatus, a right center system and a user terminal are provided. The preview groups are set up in the Digital Right Management DRM system; DRM system generates the group authorization information for the terminal according to the preview groups, and sends it to the terminal; the terminal obtains the Content Encrypt Key CEK or the seeds which generation the CEK, of the selected preview program in the corresponding preview group according to the received group authorization information, and decrypts the selected program, so as to preview the program. The prior authorization of program group can be realized using the method according to the invention; as a result, not only the concurrent access numbers to the right center can be reduced to improve the reliability of the system but also the users' waiting time can be reduced to improve the users' experience; further, the preview rules which can be arranged provide flexible business running method for providers, i.e. several programs with the same preview rule can be packed to be distributed.
Owner:HUAWEI TECH CO LTD
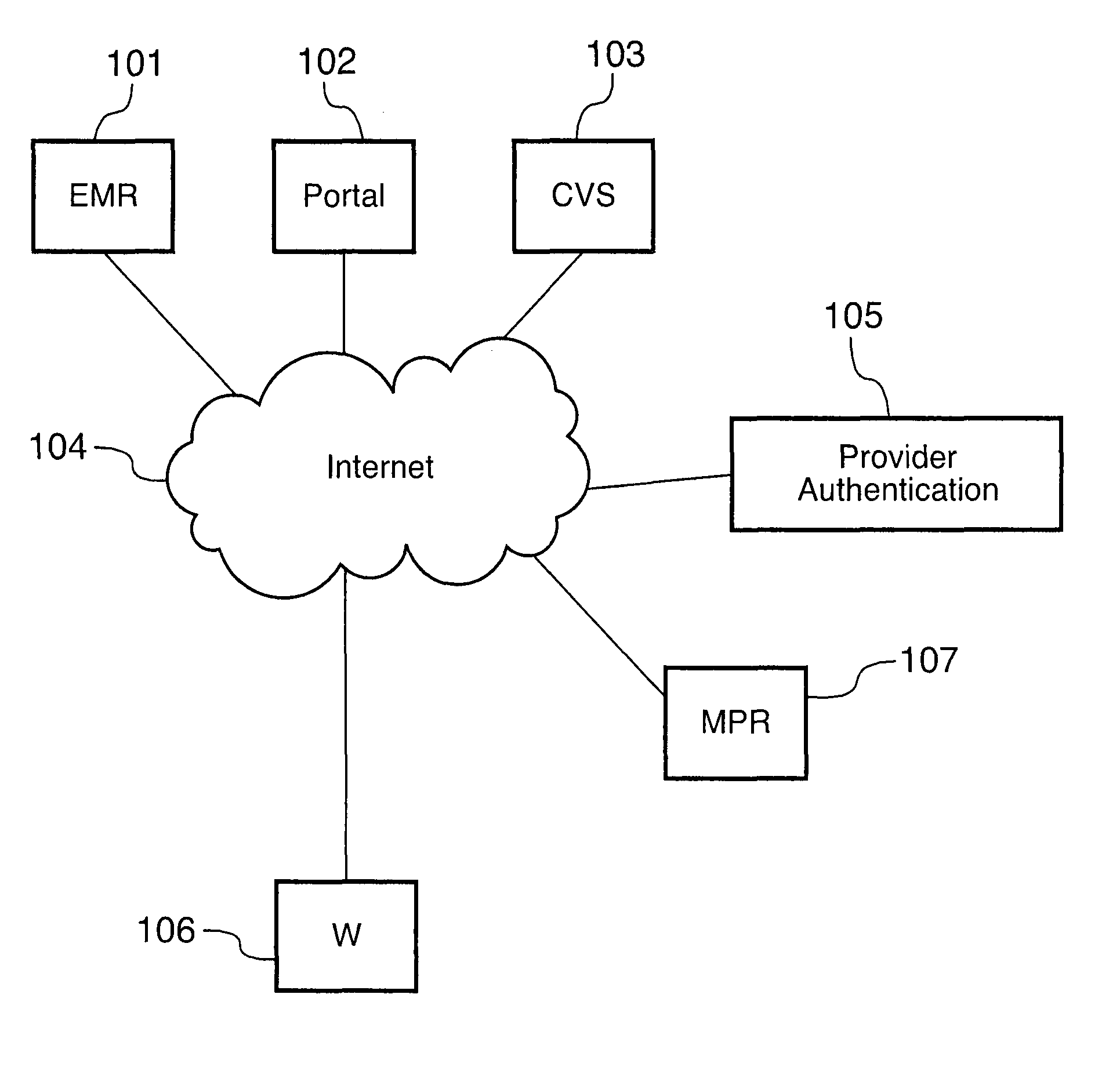
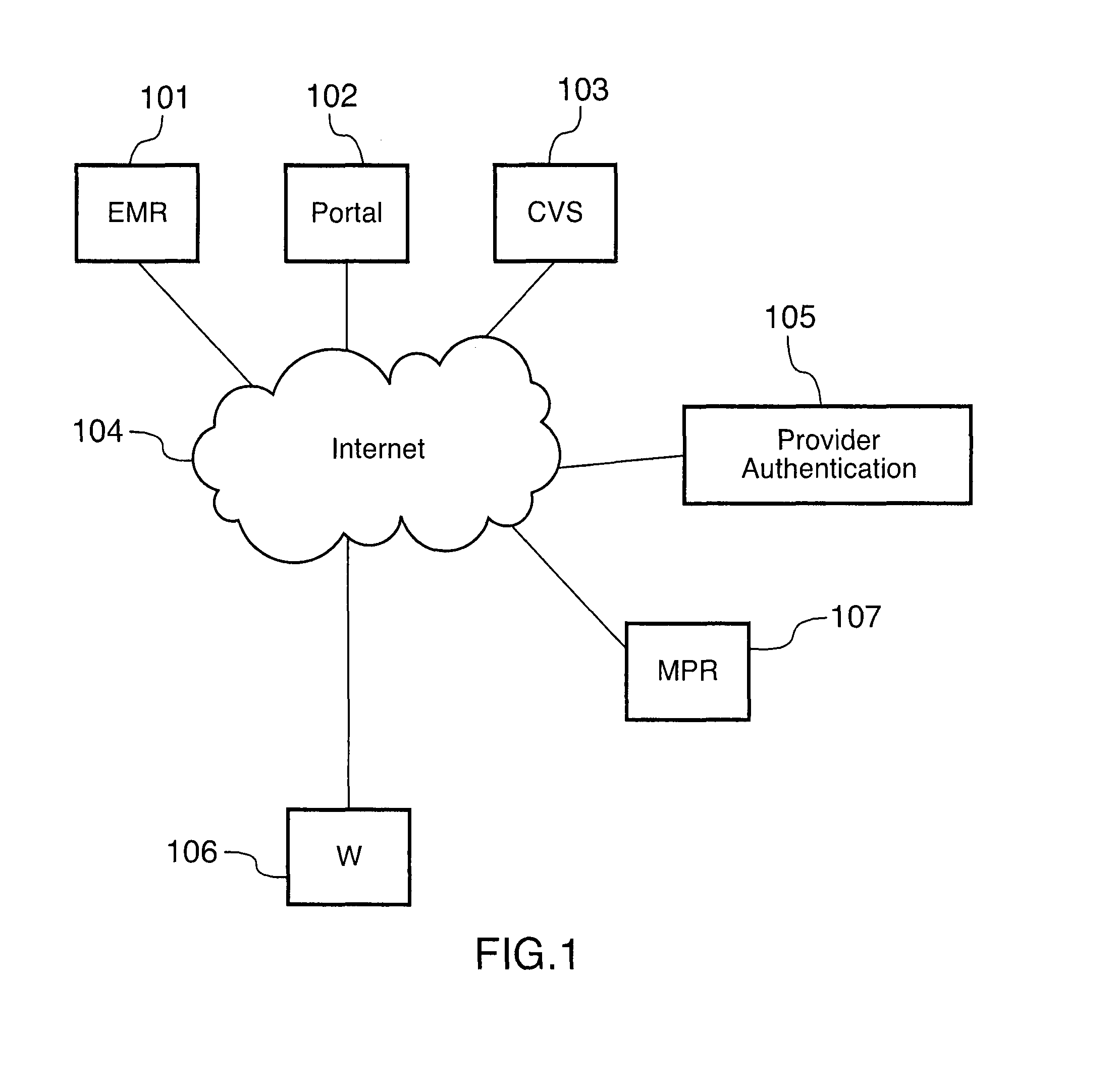
Methods for remotely accessing electronic medical records without having prior authorization
InactiveUS20150161328A1Data processing applicationsPatient personal data managementMedical recordPrior authorization
Methods are provided for allowing patients, health care practitioners and other service providers to have remote access to electronic medical records of a patient stored on a first computer network by the remote user requesting access to the electronic medical record from a second computer network and providing a first and second piece of patient derived information to the second computer network; the second computer network transferring the first and second piece of patient derived information to a third computer network; the third computer network authorizing the remote user through the first and second piece of patient derived information and dependent on a patient specific authorization protocol; the third computer network confirming a patient specific consent protocol; and the third computer network disclosing the electronic medical record to the remote user dependent upon an authorization and a confirmation received from the third computer network.
Owner:HIPAAT
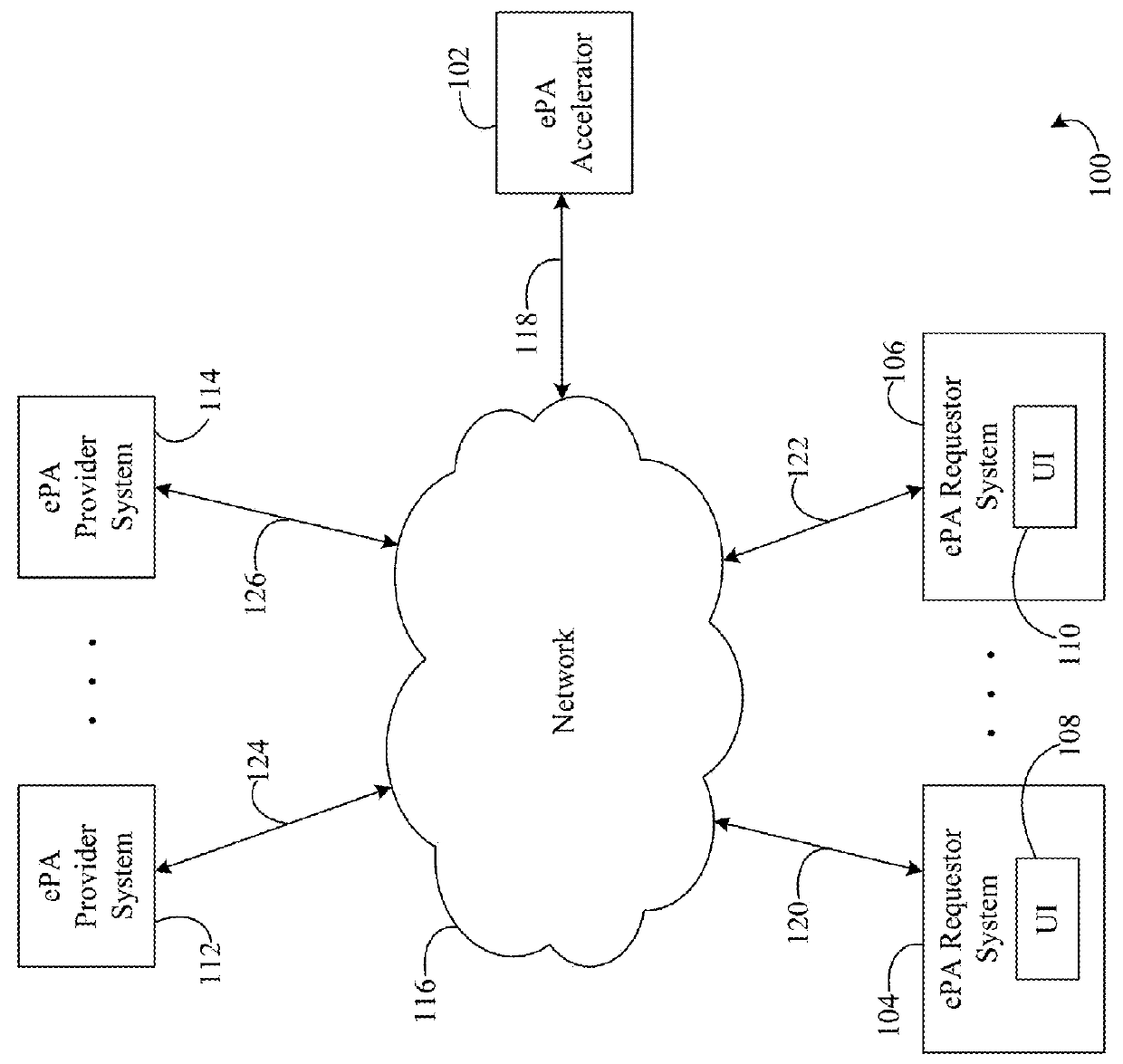
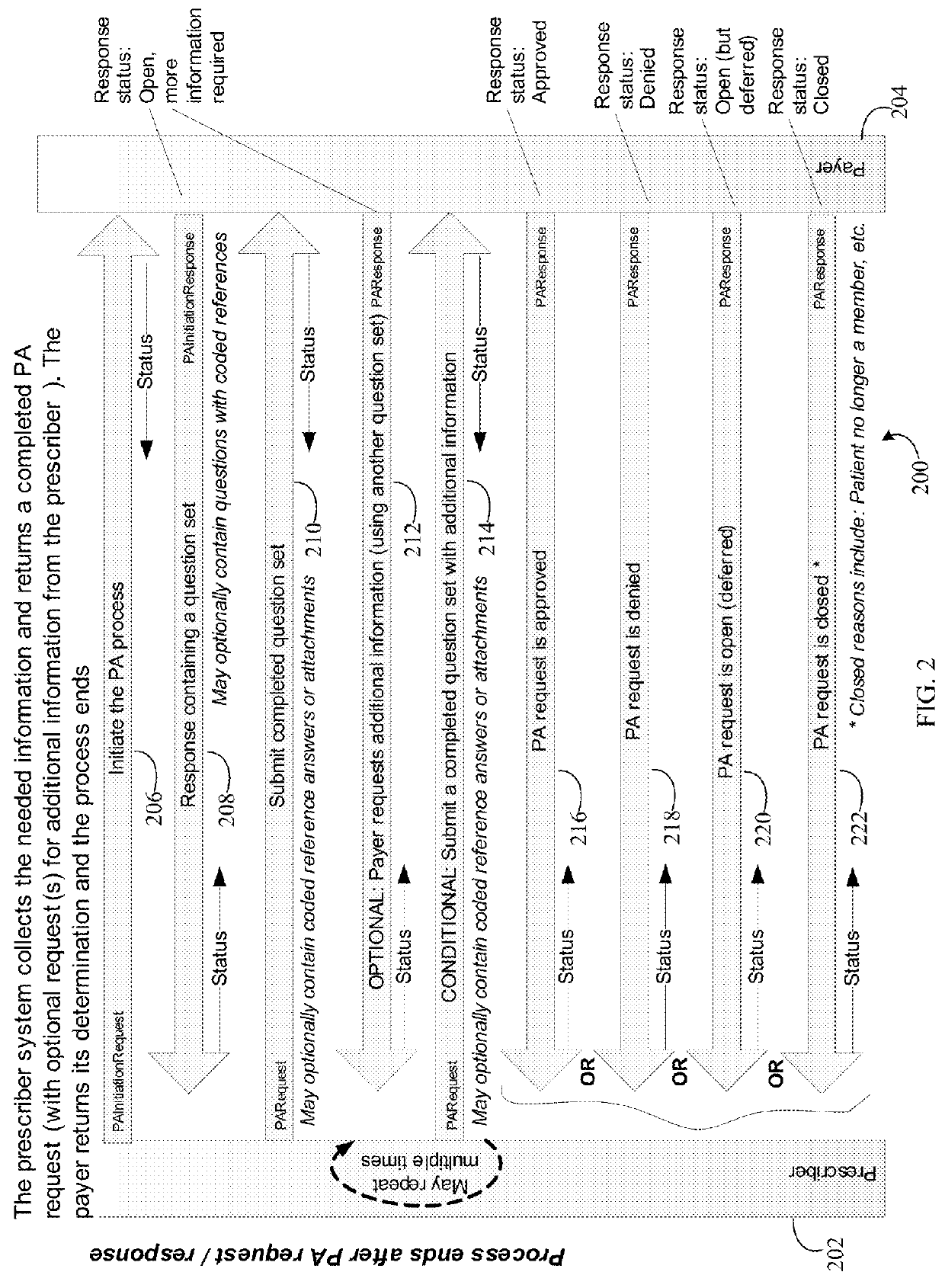
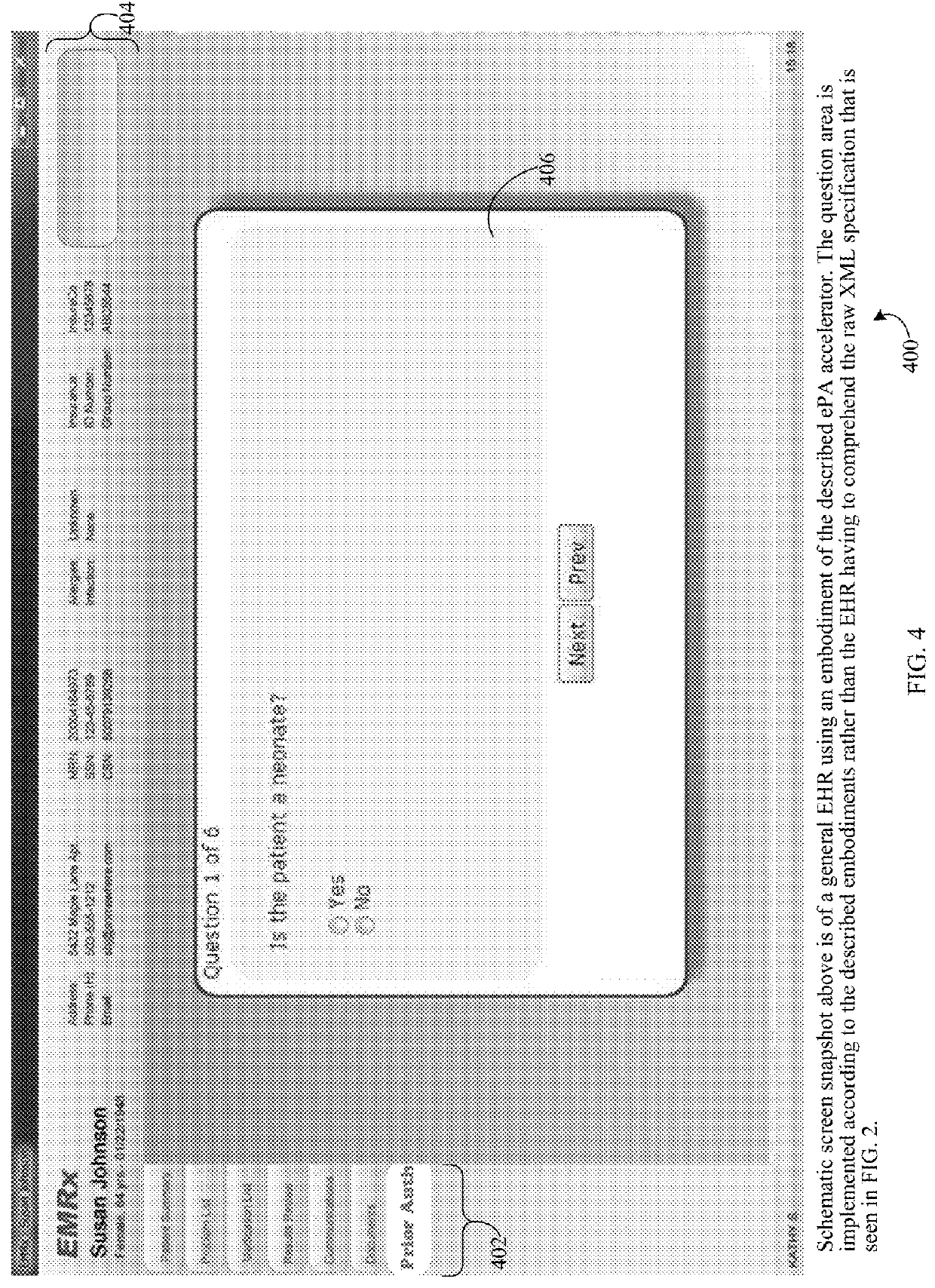
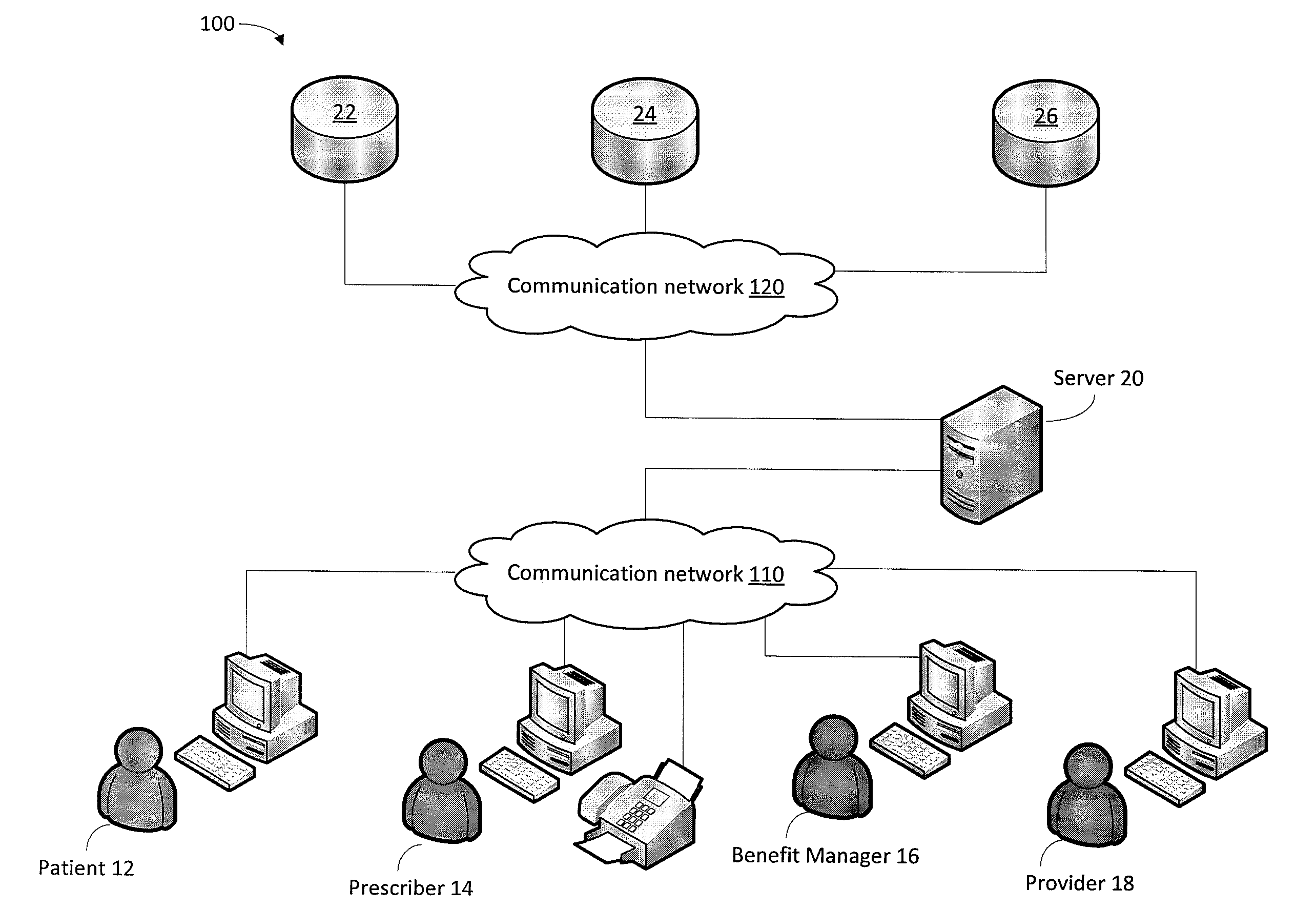
Method, system, and apparatus for electronic prior authorization accelerator
Methods, systems, and apparatuses are described for facilitating the delivery of an electronic prior authorization (ePA). Unique systems for facilitating the delivery of an ePA by an ePA provider system to an ePA requestor system and for modeling the state of an ePA request / response process are provided. A user interface (UI) generation component for dynamically generating a UI for presentation to a user is also provided. Methods corresponding to the functions performed by the systems and apparatuses are also provided.
Owner:SURESCRIPTS
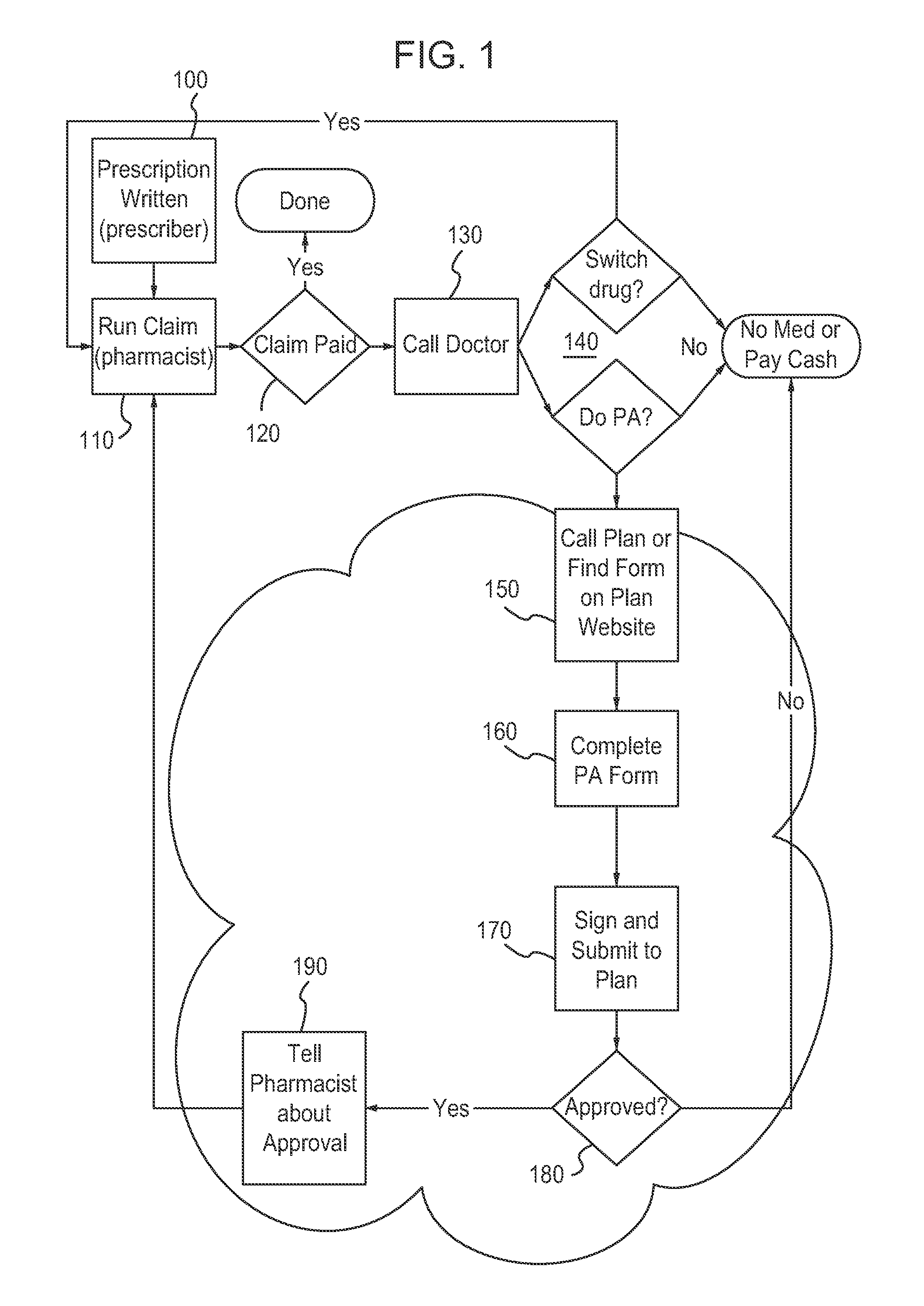
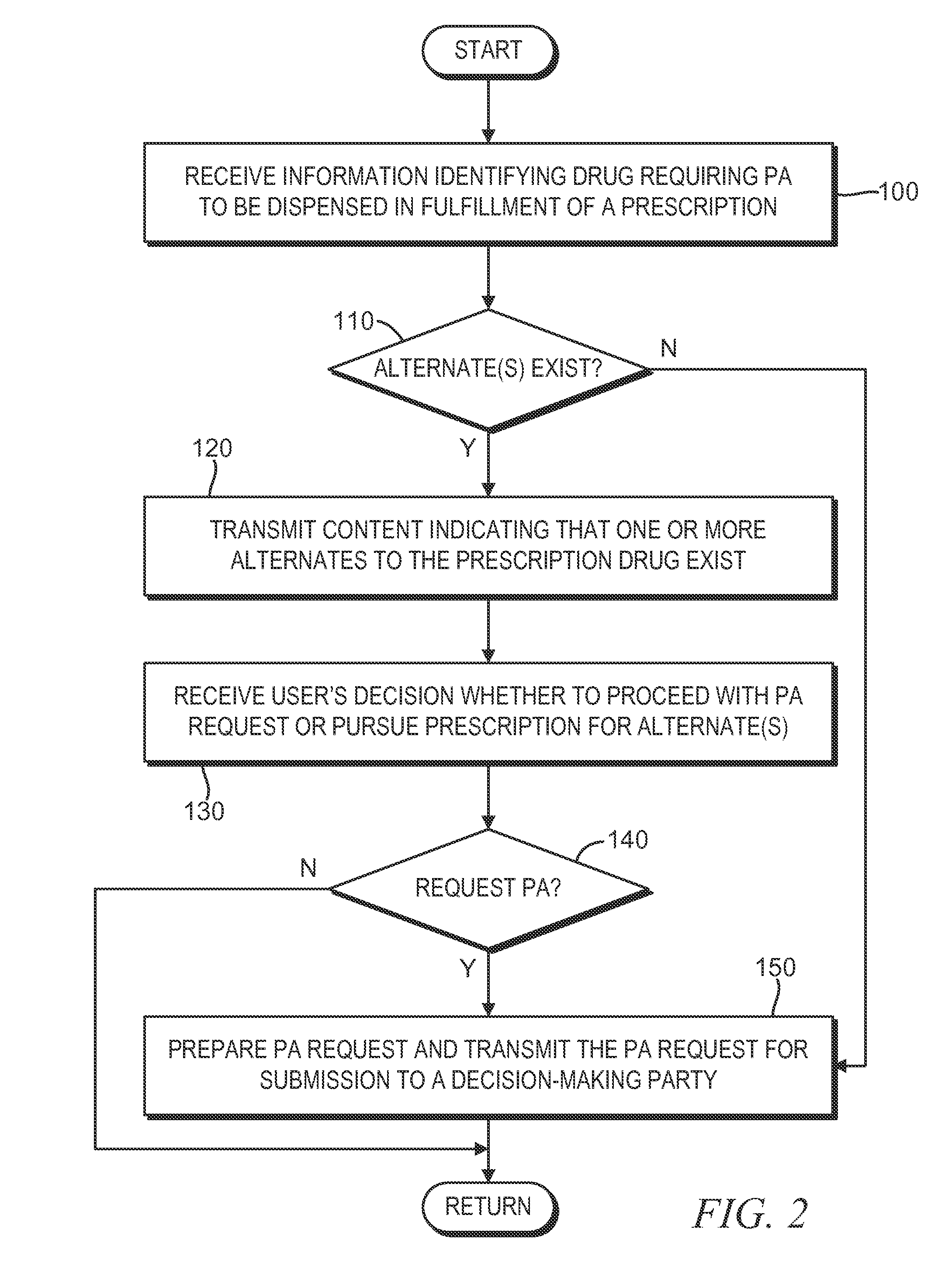
Method and apparatus for recommending an alternative to a prescription drug requiring prior authorization
Provided is a method of processing a request pertaining to a prescription drug. The method includes receiving, with a computer system after a claim requesting at least partial insurance coverage of a cost associated with the prescription drug has been submitted to an insurance benefits manager, a notification that prior authorization has been required. Before the request for prior authorization is submitted, it is determined that an alternate drug is a possible substitute for the prescription drug, and the alternate drug is believed to not require prior authorization under the insurance policy. The determination is made based on data contained in a database that is generally accepted in a pharmacy industry and is not unique to an insurer affiliated with the insurance policy.
Owner:COVERMYMEDS
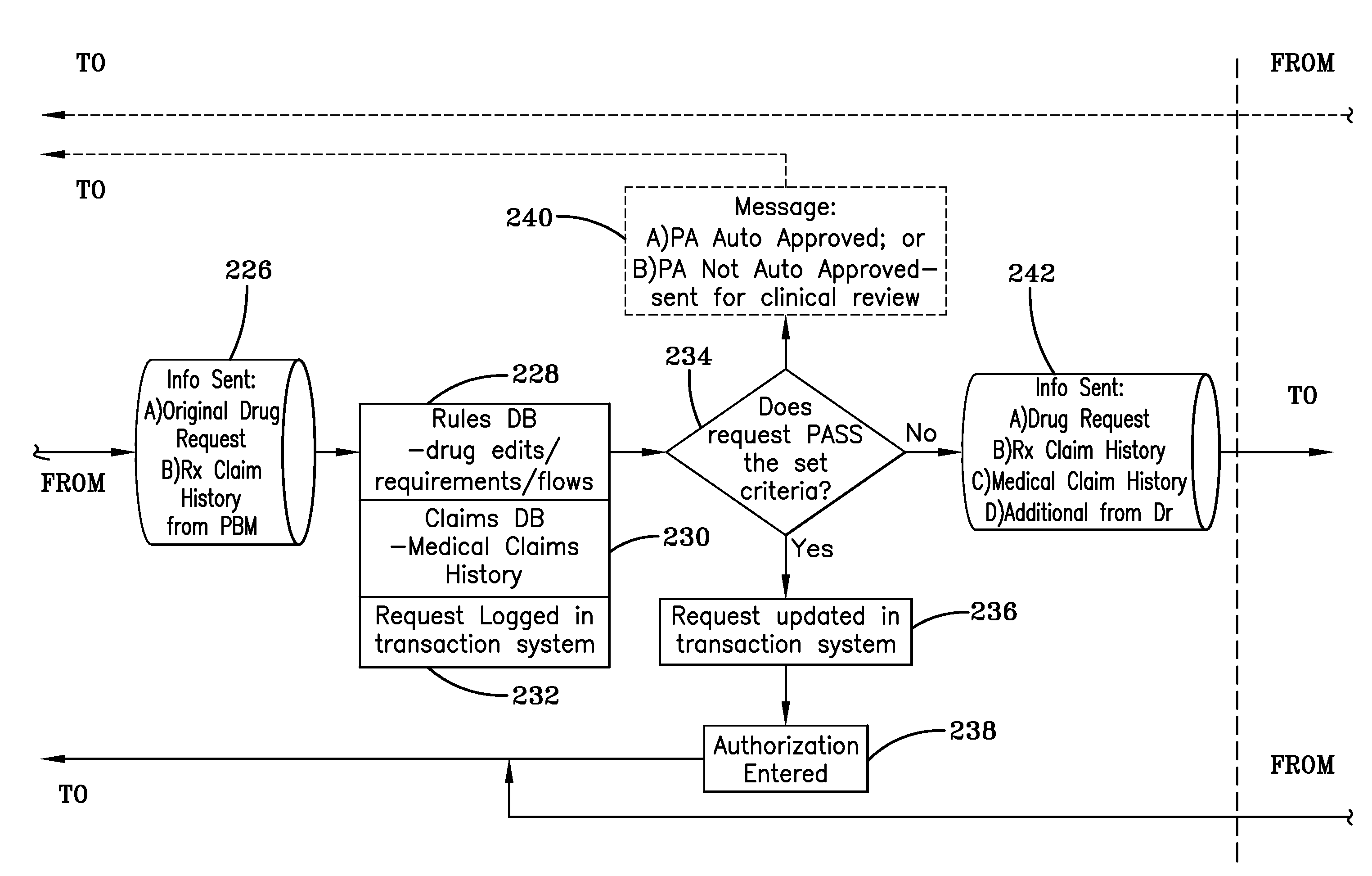
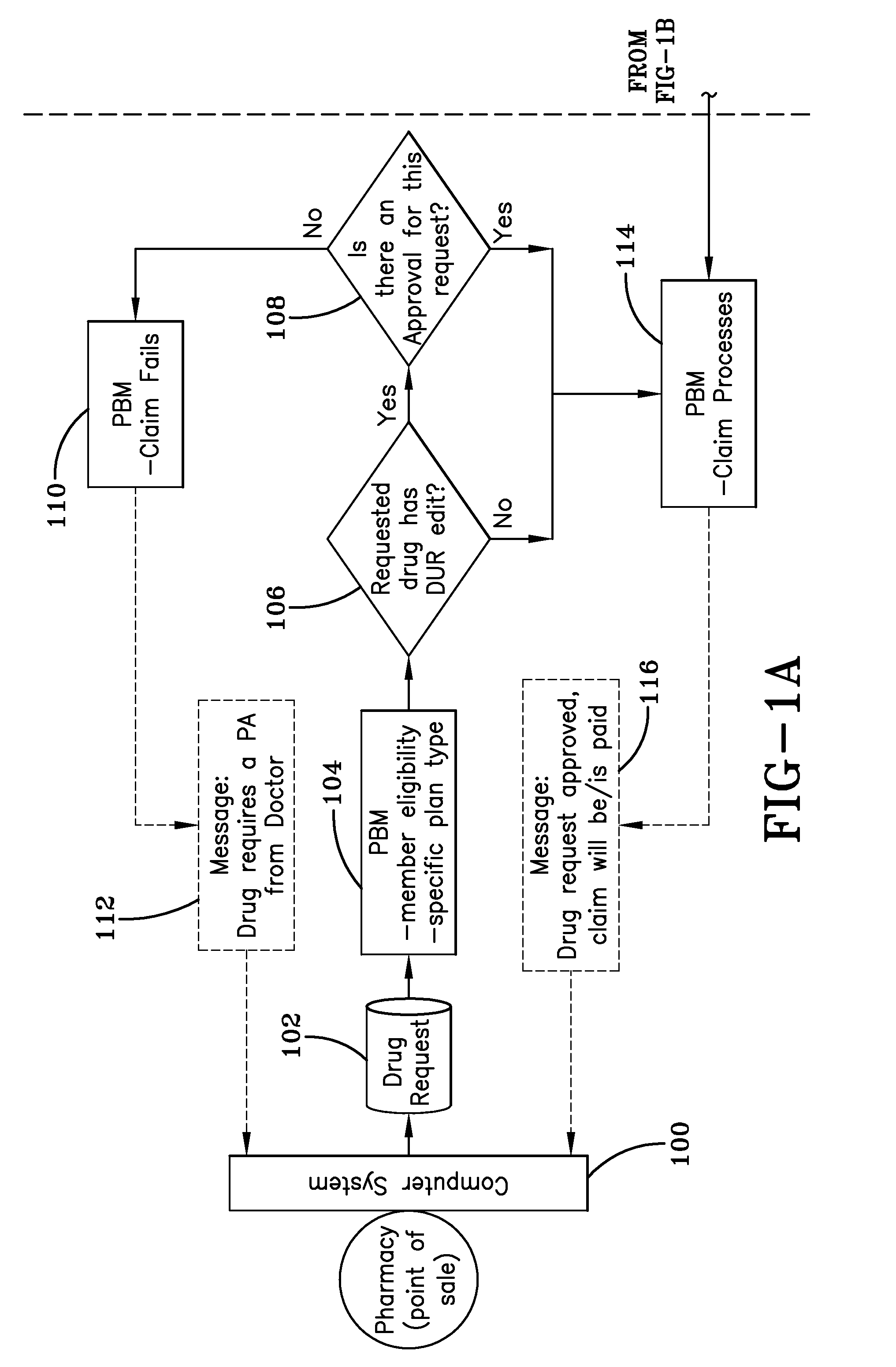
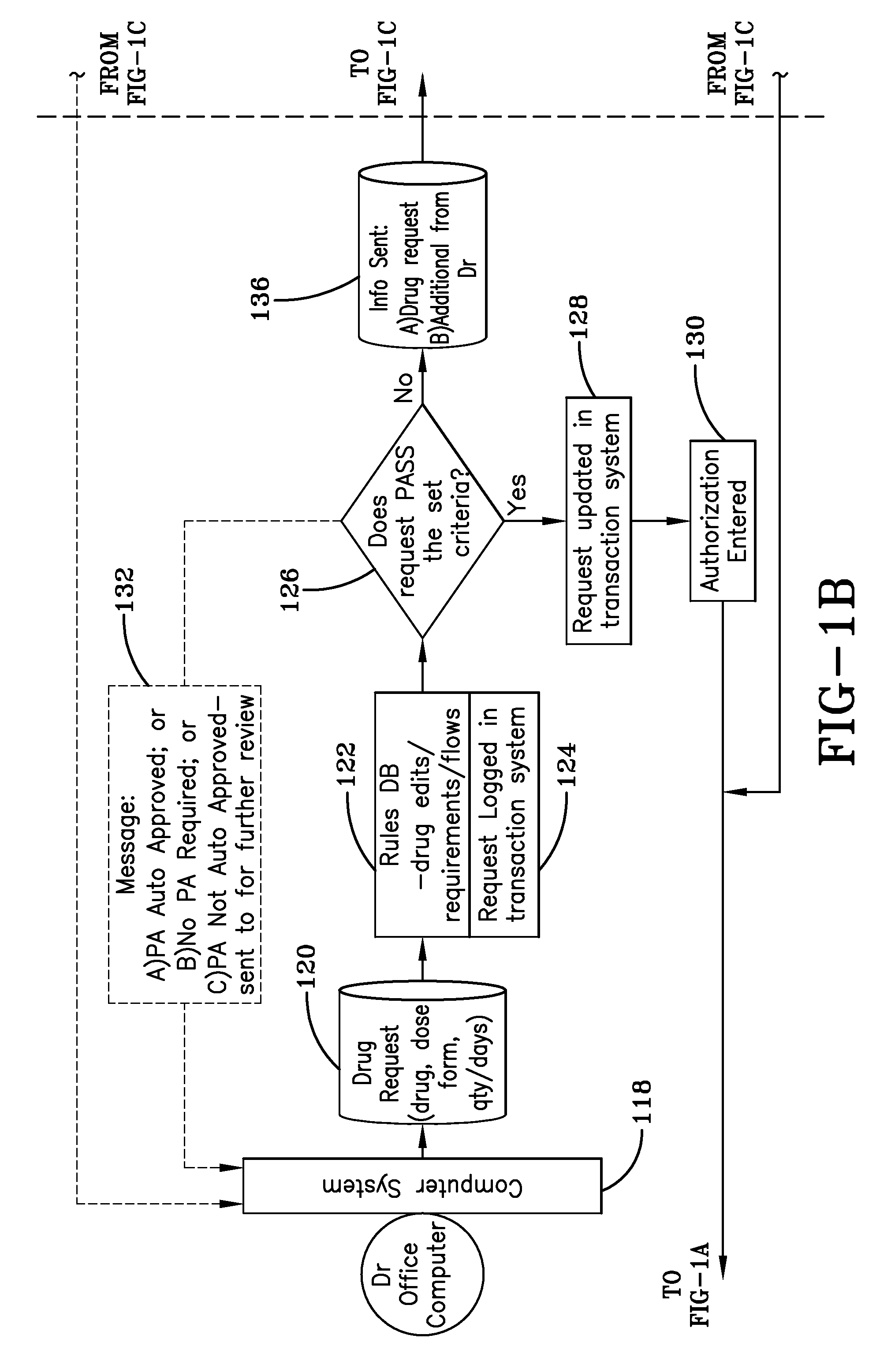
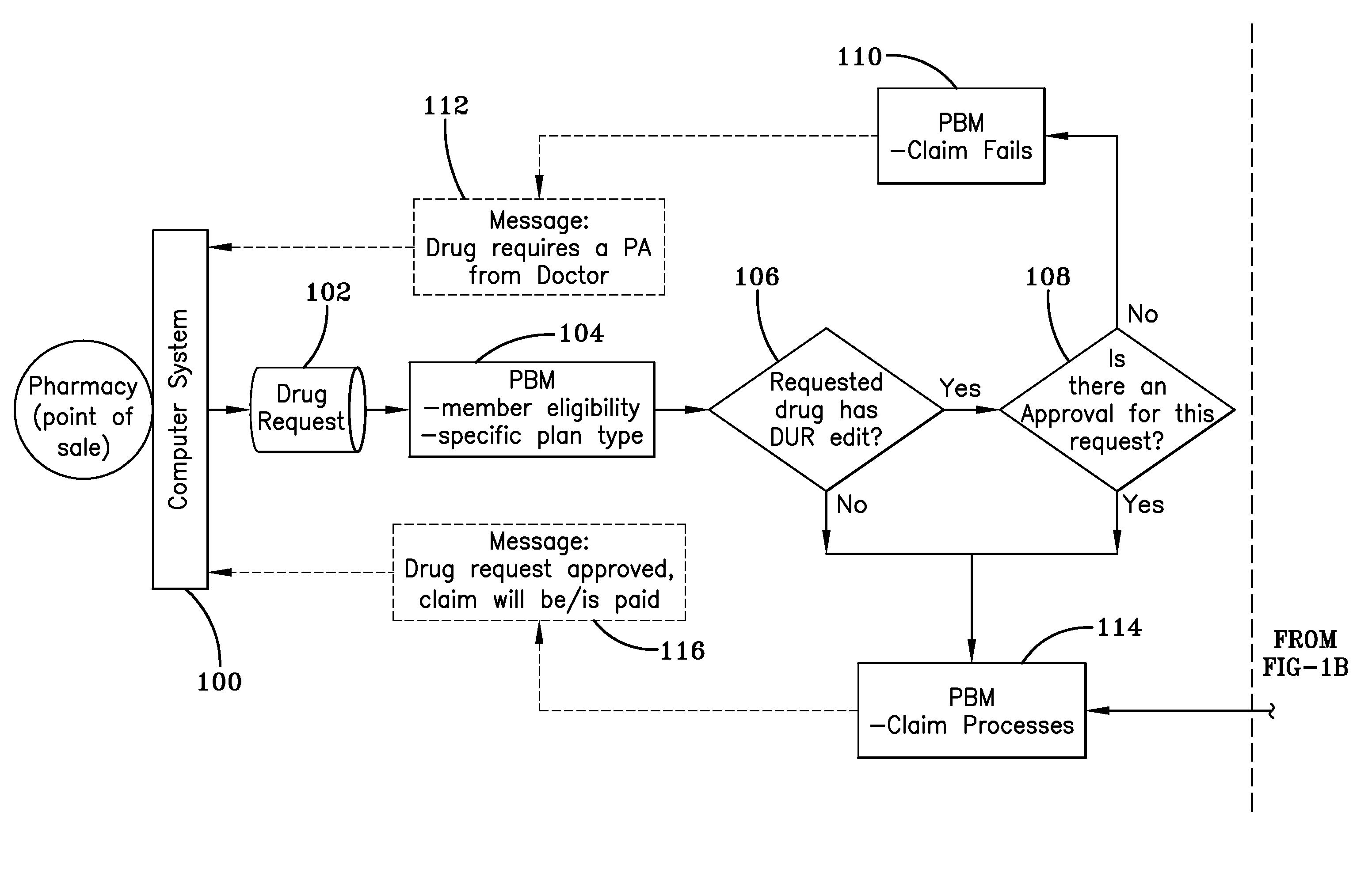
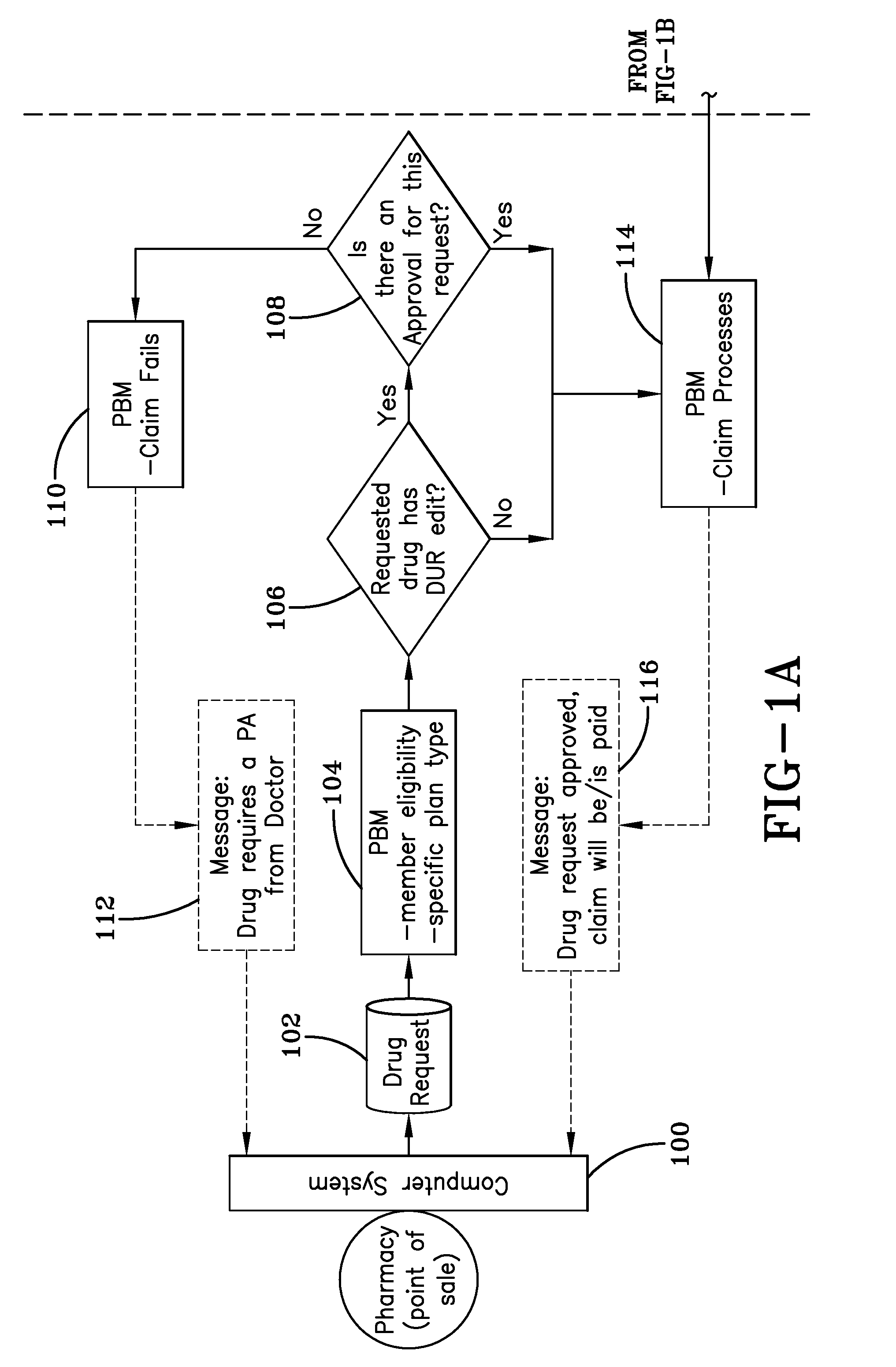
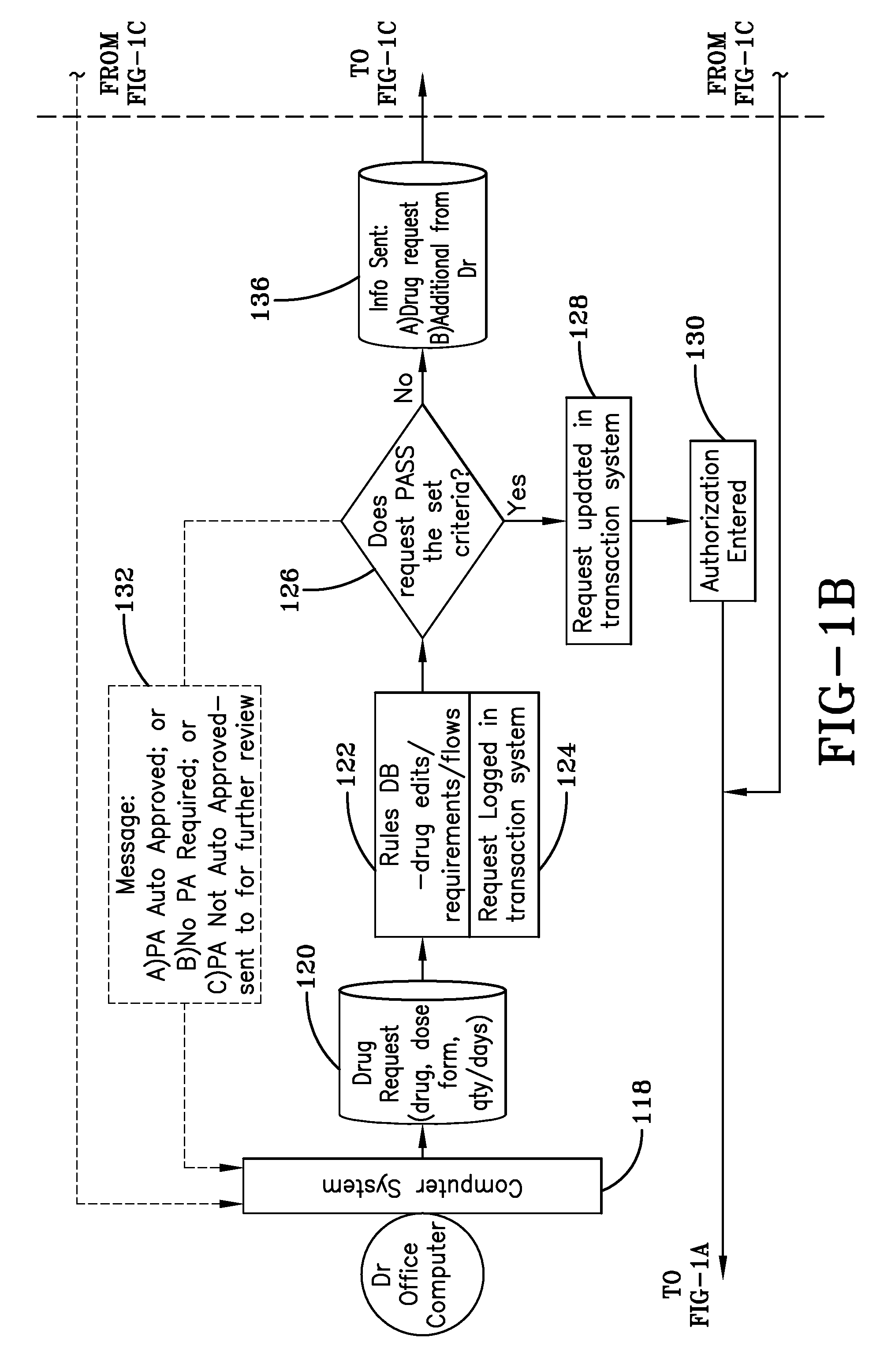
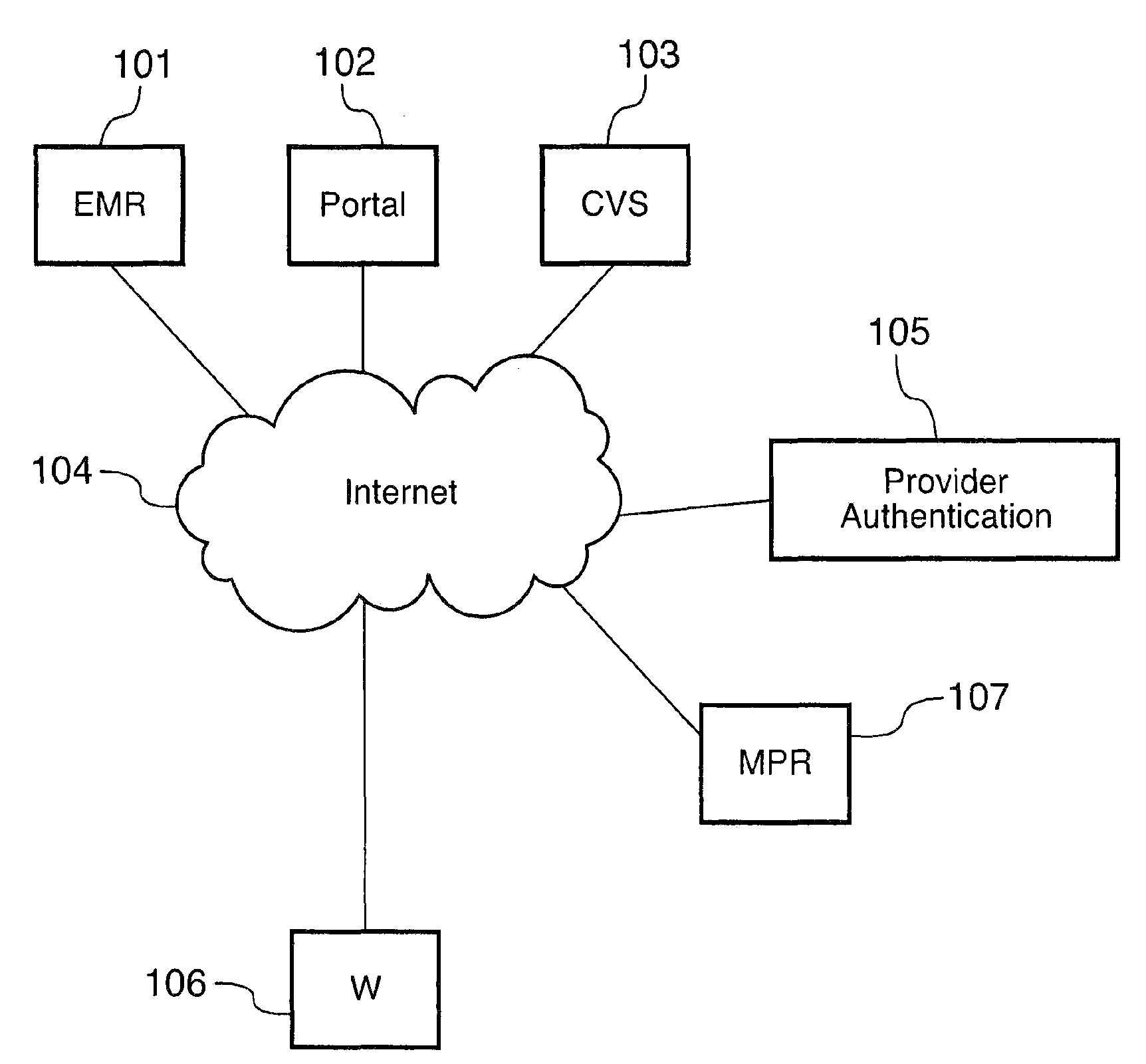
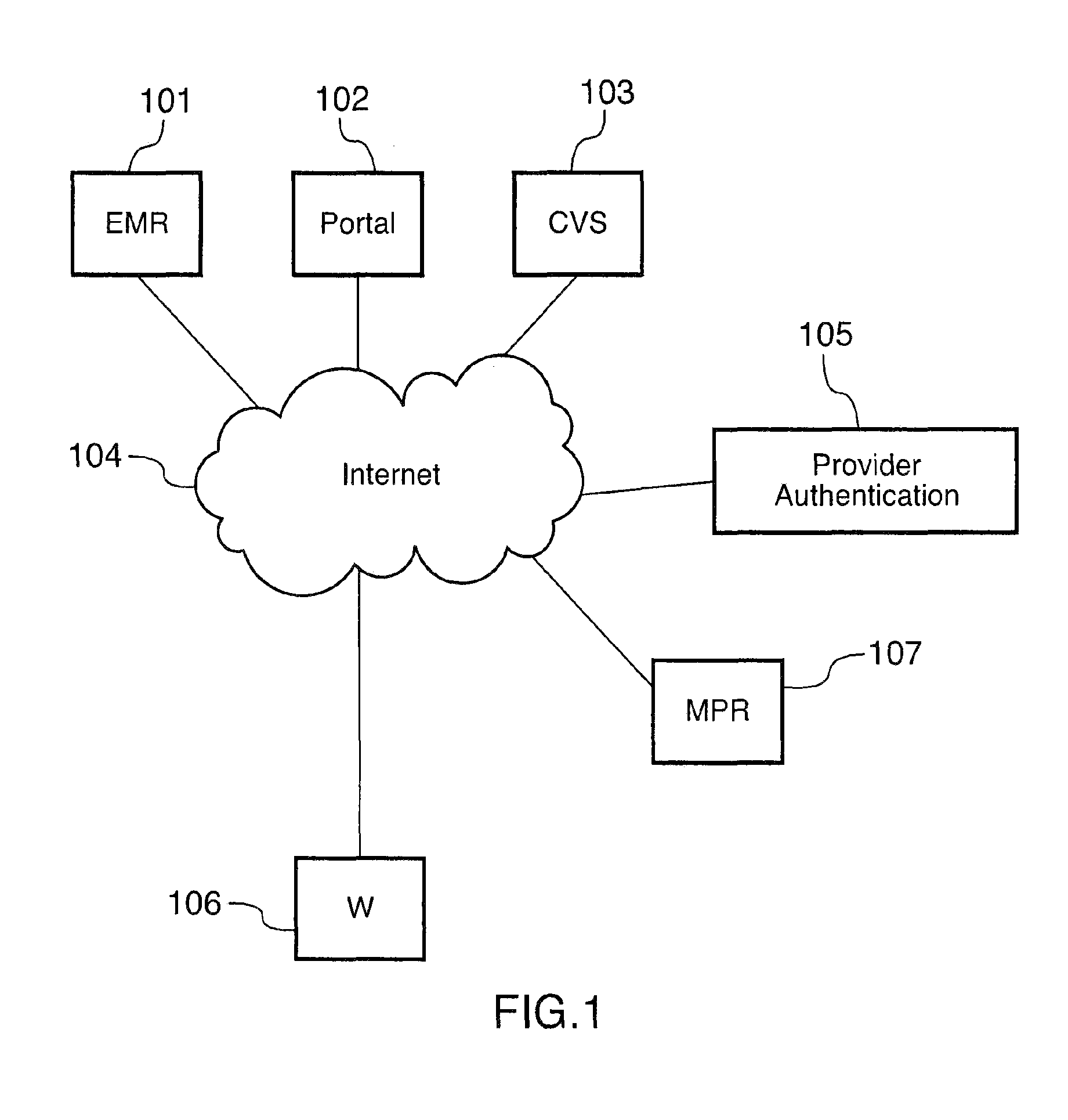
Prescription drug prior authorization system and method
ActiveUS8265959B2Easy to useFacilitates submissionFinanceDrug and medicationsPrior authorizationDrugs prescriptions
An online application for approving prior authorization requests for prescription drugs. The application is used by pharmacy benefits providers, physicians, and pharmacies to request prior authorizations for drugs and to receive approvals automatically if a requested drug meets authorization criteria. The online application is accessible through a group pharmacy benefits provider portal on a web site. Requests are processed through a pharmacy benefits manager computer that determines whether prior authorization is required and through a pharmacy benefits provider computer when the pharmacy benefits manager computer determines that prior authorization is required. Requests that meet certain authorization criteria are approved automatically. Requests that cannot be approved automatically are submitted for review by a clinical pharmacy review division that access requests through a drug request transaction computer.
Owner:HUMANA INC
Machine learning systems for predictive modeling and related methods
A machine learning system for training a data model to predict data states in medical orders is described. The machine learning system is configured to train a data model to predict whether a medical order requires prior authorization (“PA”) for medical orders within a medical order data set so that related systems may process incoming medical orders with PA determinations predicted by the data model. The machine learning system includes a first data warehouse system. The first prescription processing system generates a data model of historical orders and payer responses, apply a predictive machine learning model to the data model to generate a trained predictor of whether a medical order requires PA, associated with order data, apply the trained predictor to a plurality of production orders to determine PA for each of the plurality of production orders, and process the plurality of production orders with each associated PA determination.
Owner:EXPRESS SCRIPTS STRATEGIC DEV INC
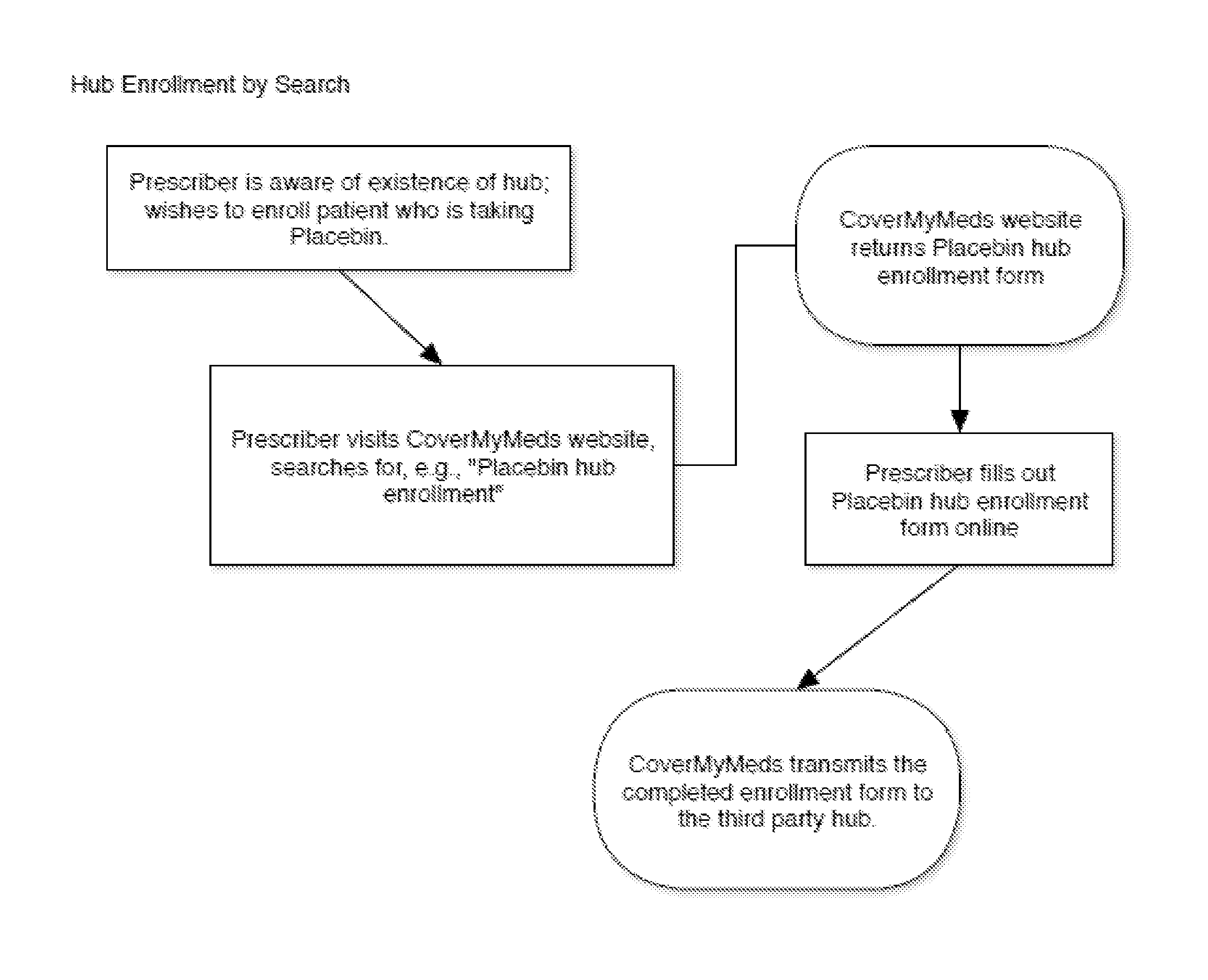
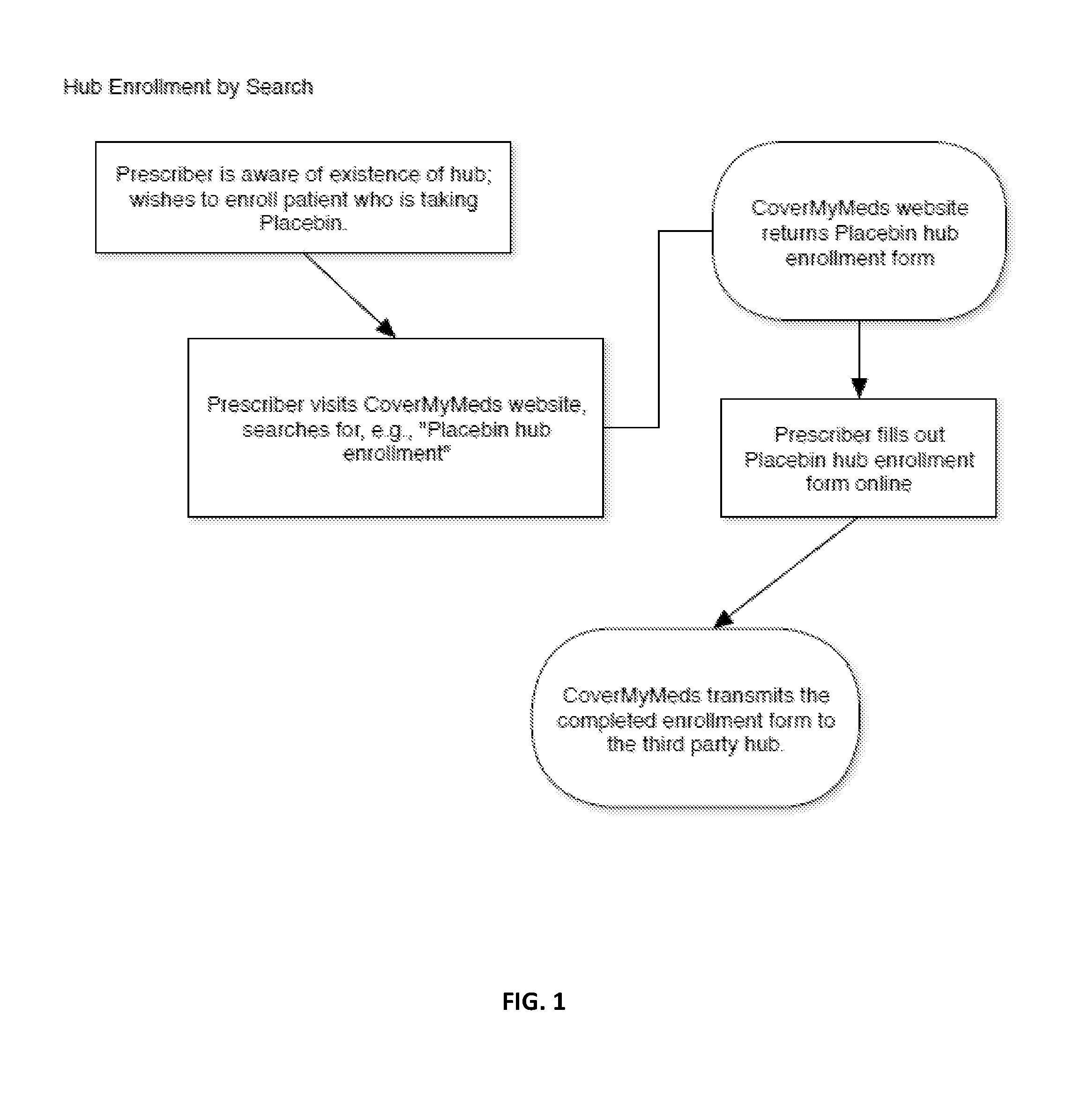
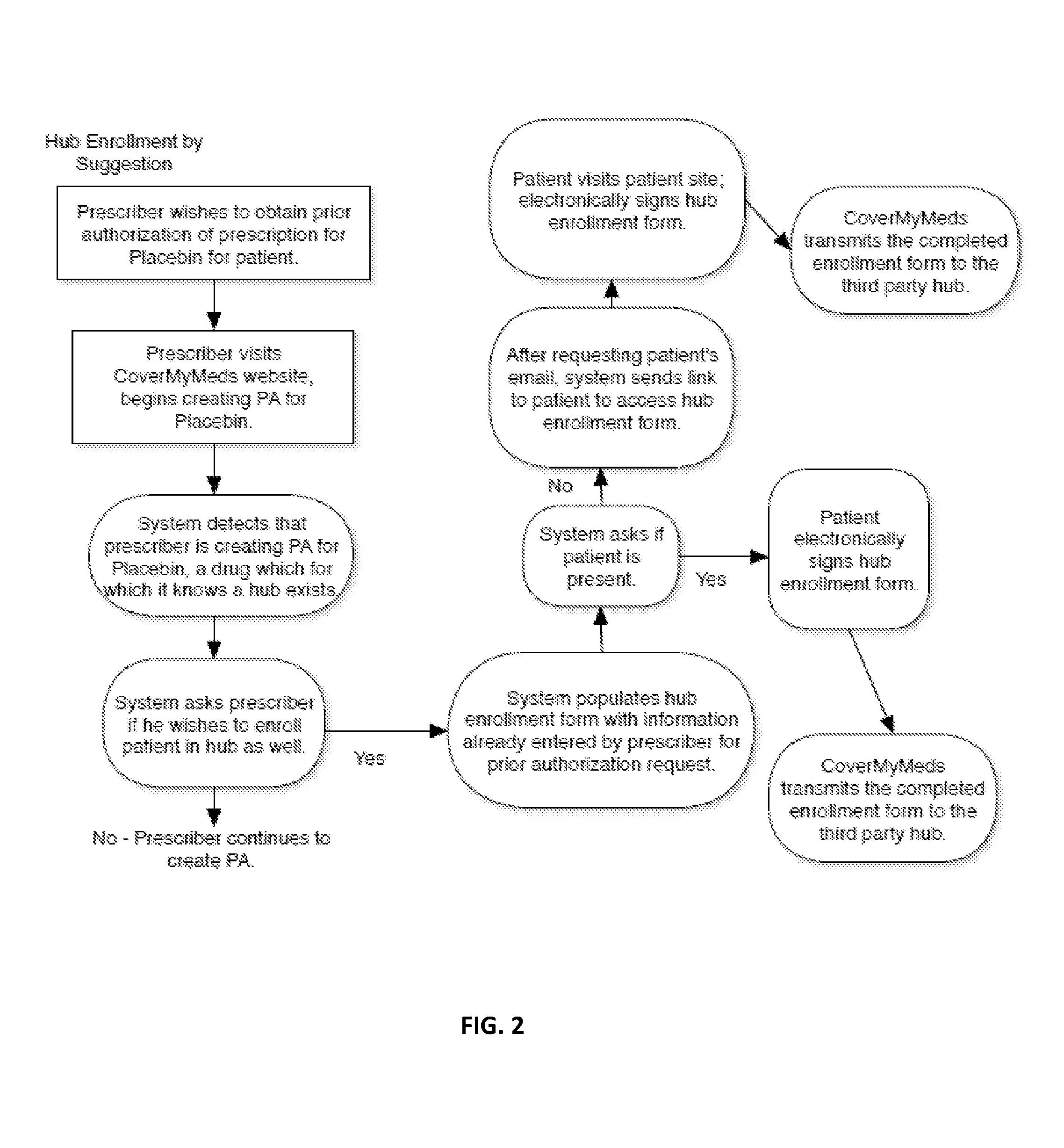
Processing enrollment into patient support centers for prescription medications
Systems and methods for facilitating enrollment into a patient support center for a medication are provided. The systems and methods can be configured to receive information from a prescriber regarding a prescription medication for a patient; determine whether the prescription medication is associated with a patient support center; communicate to the prescriber an inquiry regarding whether to enroll the patient in the patient support center; receive a request from the prescriber to begin an enrollment of the patient into the patient support center; communicate to the prescriber an interface by which the prescriber can input information regarding enrollment of the patient into the patient support center; receive an indicia of patient agreement to the enrollment into the patient support center; and communicate the patient enrollment information to the patient support center. The systems and methods may also facilitate electronic submission of a request for prior authorization for the medication.
Owner:COVERMYMEDS
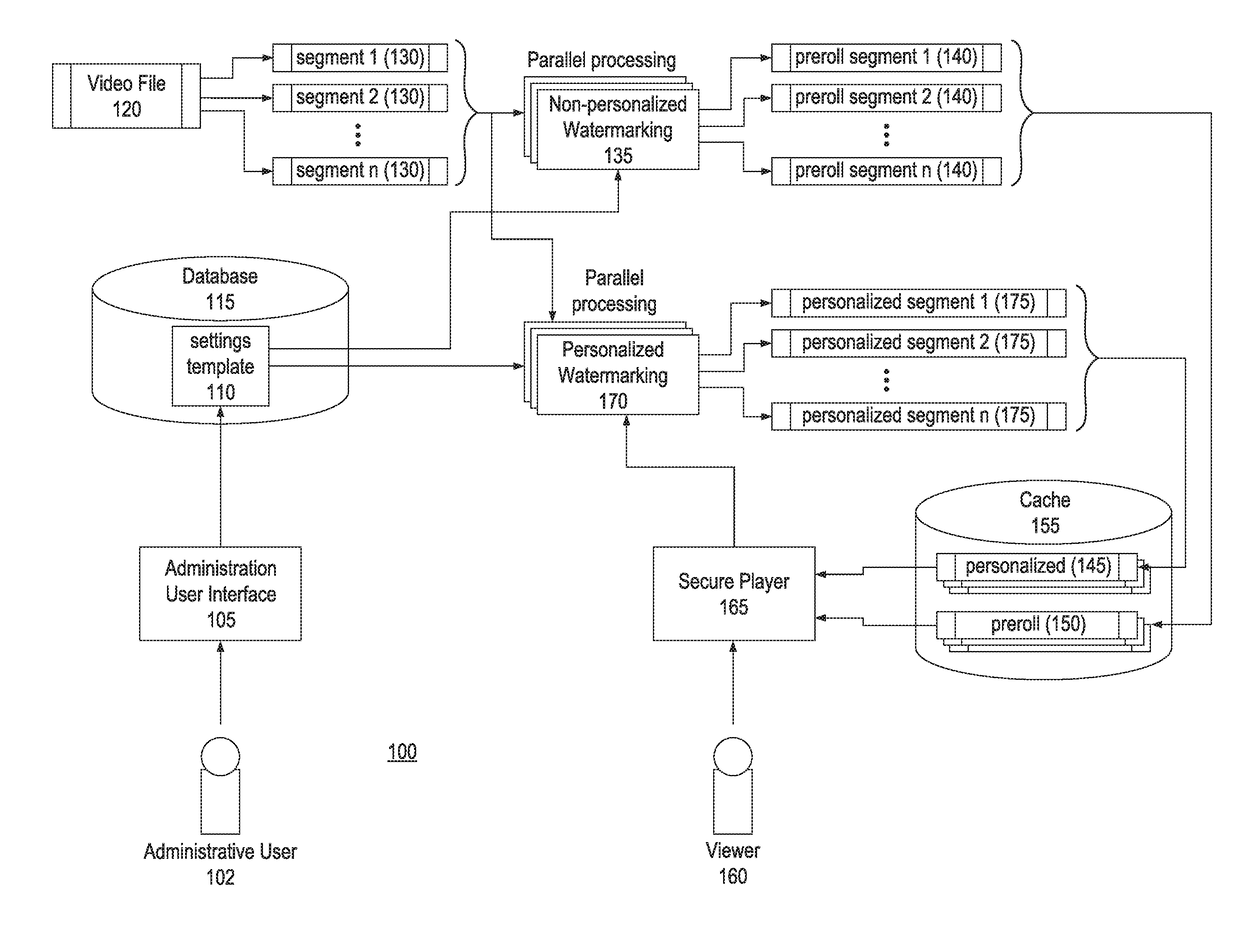
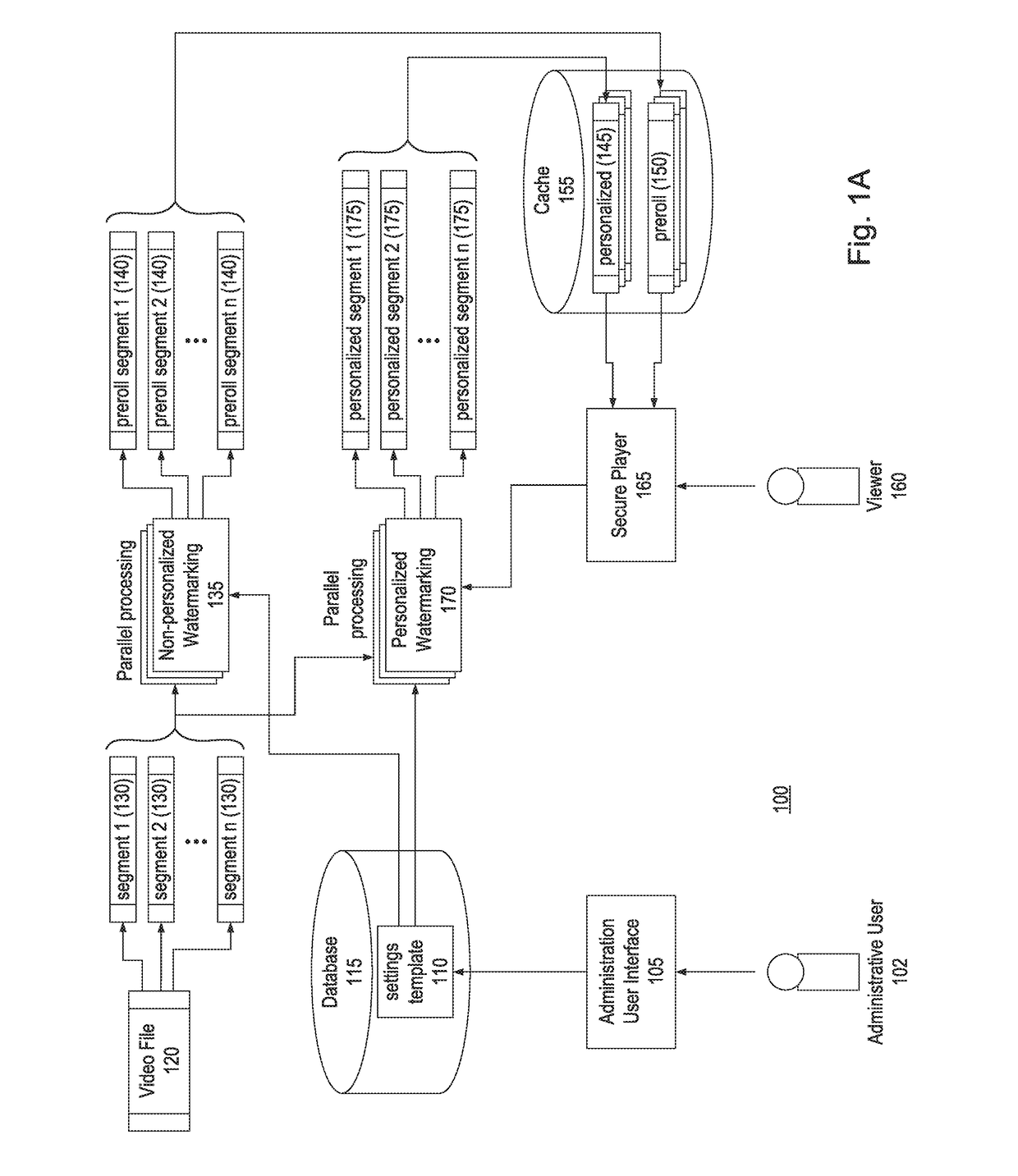
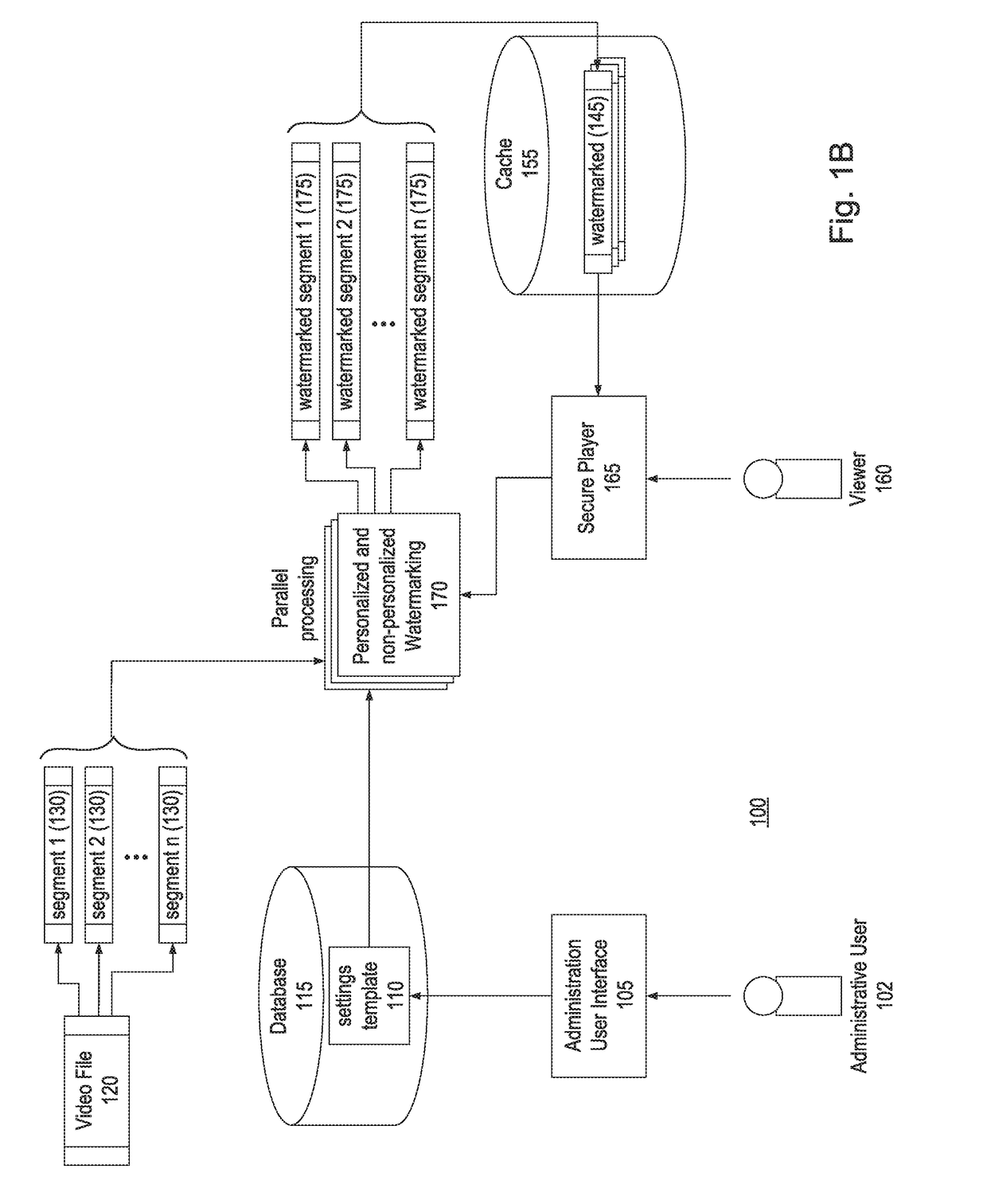
Real-Time Watermarking of Video Content
InactiveUS20170180822A1Lack of protection of contentAvoid attackSelective content distributionPrior authorizationTurnkey
Currently, there is no single turnkey solution for protecting video content online. Instead, the industry norm is to rely on a combination of techniques that aim to restrict access of video streams to only the audience with prior authorization to view the content. Embodiments of the present invention provide real-time methods and systems for watermarking video content by determining personal attribute information of a recipient of the subject video content and, in connection with streaming the subject video content to the recipient, executing a plurality of massively parallel servers to generate a watermark from the personal attribute information and embed the watermark into the subject video content in real-time during streaming of the video content by causing burn-in of the generated watermark into a layout of the subject video content and / or embedding the watermark as a code in the subject video content.
Owner:MEDIASILO INC
Apparatus and method for processing prior authorization for prescription drugs
An apparatus, a method, and a computer program product are provided. The apparatus includes at least one memory including computer program code, and at least one processor. The at least one memory and the computer program code are configured to, with the at least one processor, cause the apparatus at least to receive a request to generate a prior authorization form for a prescription drug, and select the prior authorization form from a plurality of prior authorization forms based on the request. The prior authorization form is selected based on at least one of a user search result and a standardized transaction. The at least one memory and the computer program code are further configured to, with the at least one processor, cause the apparatus at least to transmit the selected prior authorization form to a user so that the user can complete and submit the prior authorization form to the health plan and receive a determination on the request.
Owner:COVERMYMEDS
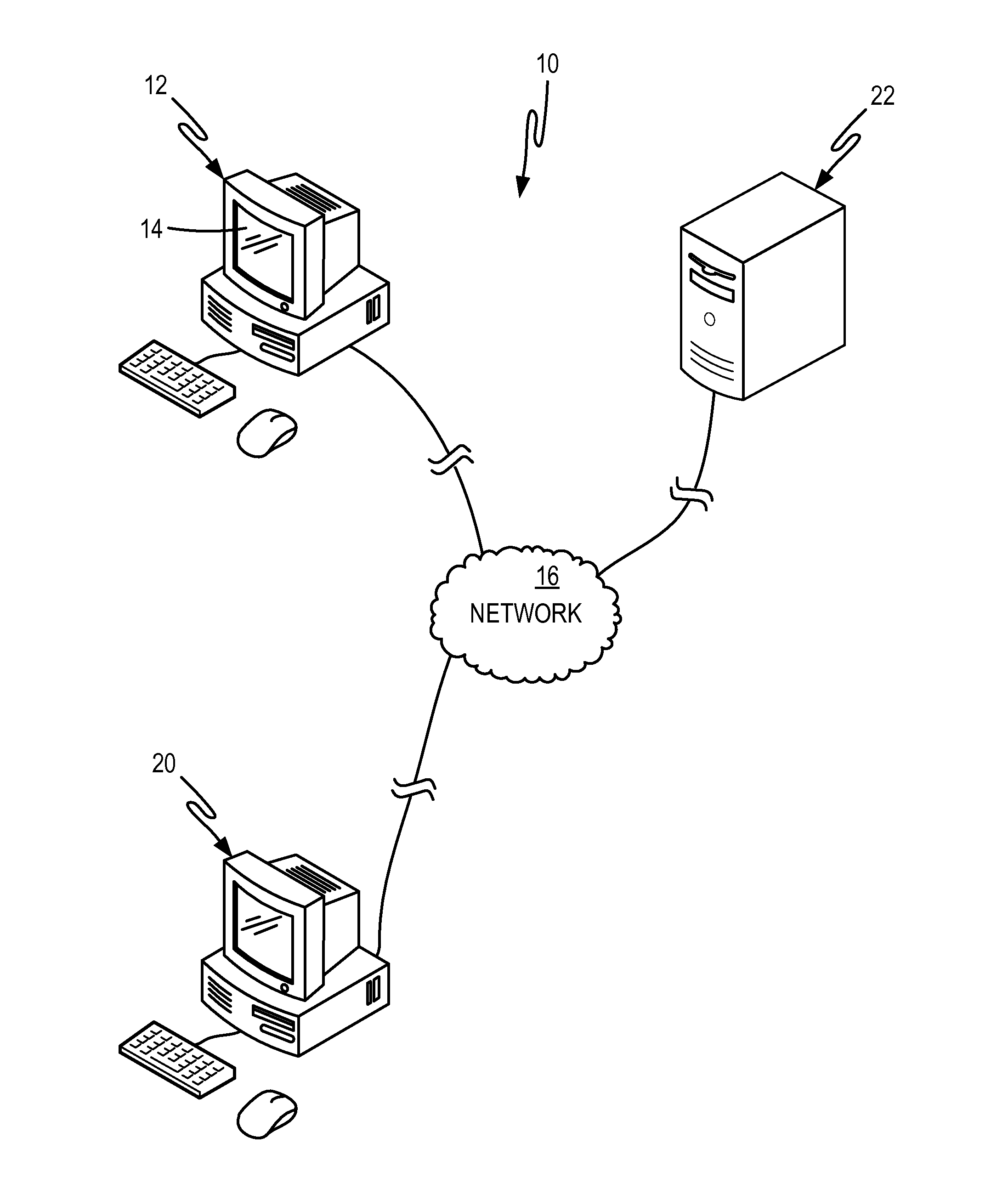
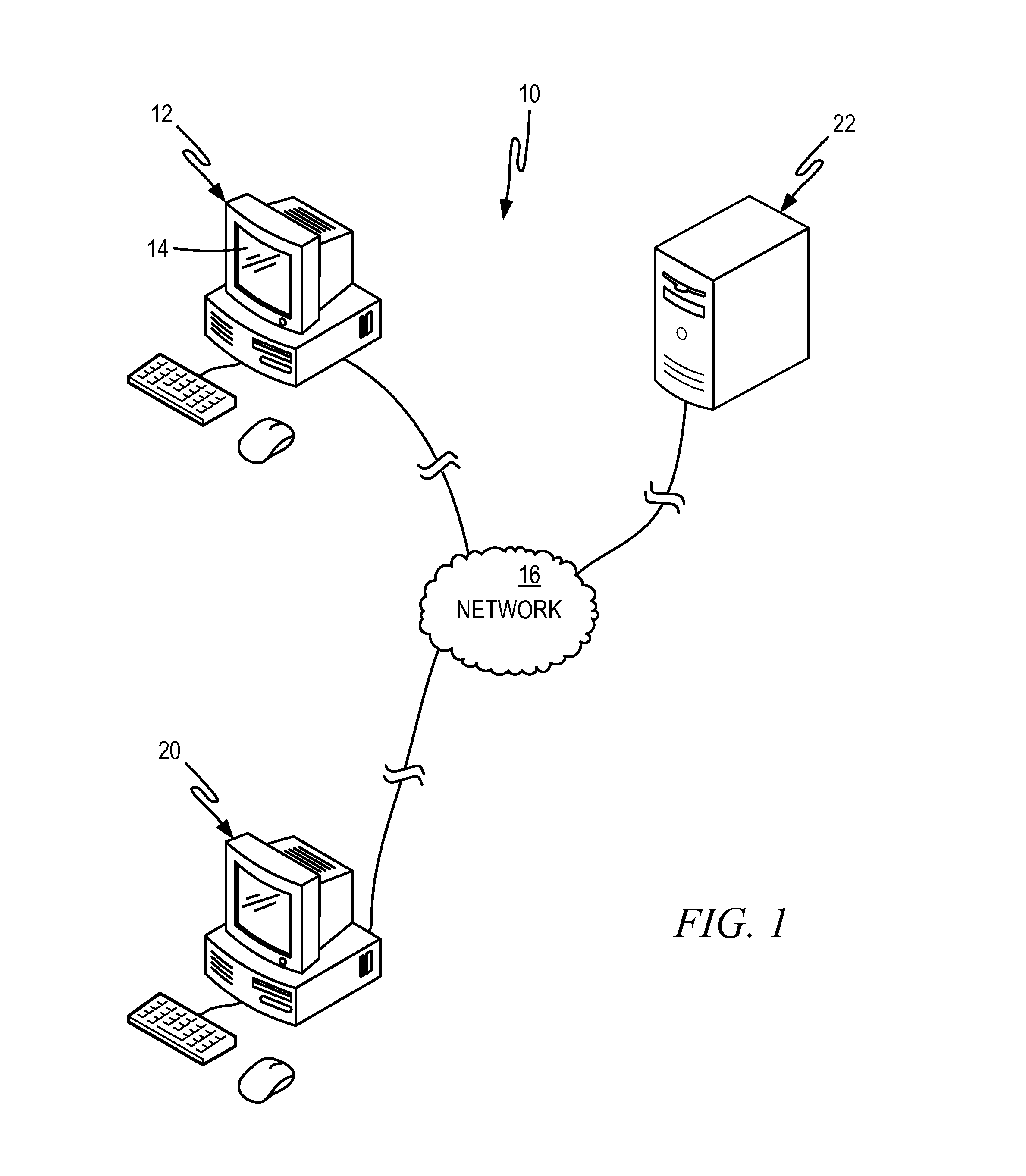
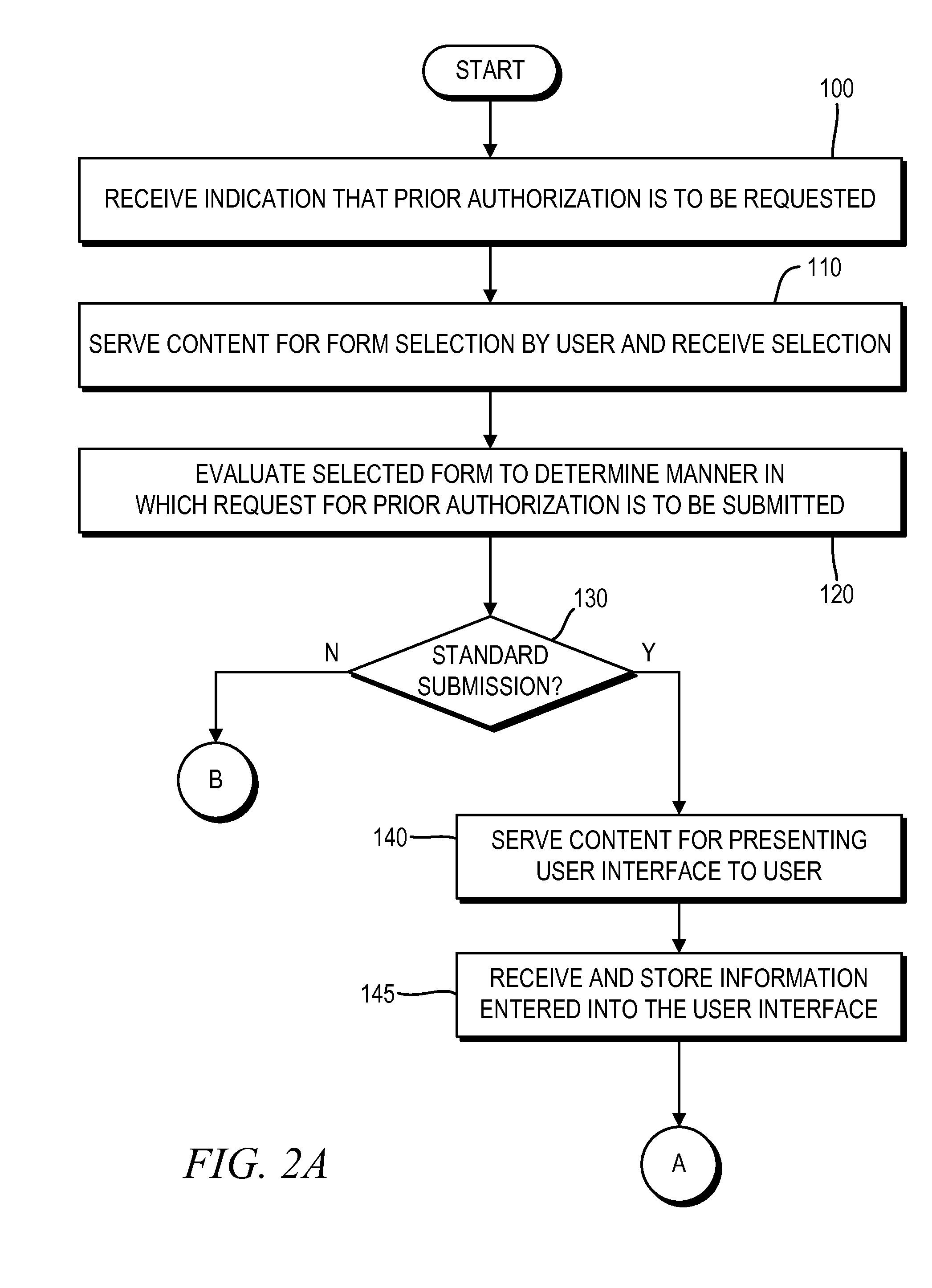
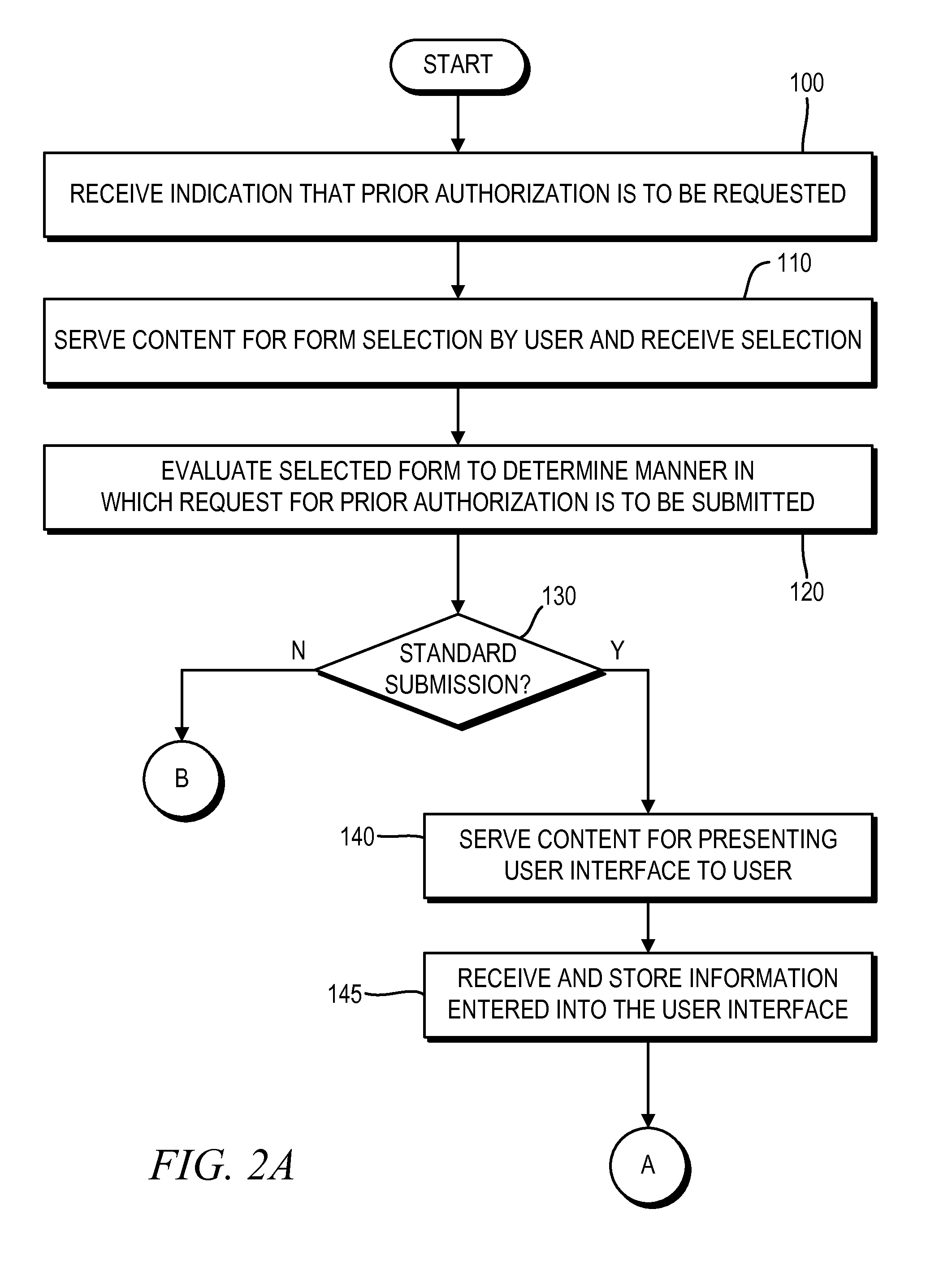
Diverse methods of facilitating a request for prior authorization with a common user experience
Provided are a method and computer system for facilitating a request for prior authorization of insurance coverage for a prescribed drug. An appropriate submission protocol is identified from among a plurality of different submission protocols available based on user input received over a communication network. Content is served to be utilized by a user computer for generating a user interface comprising a plurality of data-entry fields in which a user is to enter the patient-related information that is to be submitted as part of the request for prior authorization. The content transmitted is to be used for generating the user interface to include common fields regardless of which of the plurality of different submission protocols is to be utilized, thereby providing users with a transparent, familiar experience to submit a request for prior authorization according to different submission protocols.
Owner:COVERMYMEDS
Apparatus and method for processing prior authorizations for prescription drugs
Provided is a method and apparatus for preparing a request for prior authorization of coverage for a prescription drug. After a previous claim requesting at least partial coverage of a cost associated with the prescription drug has been submitted, a notification that prior authorization of the at least partial coverage has been required by the benefits manager is received. After receiving this notification, the method involves automatically conducting a query of a computer-accessible database to retrieve information included in a previously-submitted request for prior authorization. The information retrieved is presented to be confirmed as suitable for submission in the request for prior authorization as part of a current transaction and, in response to receiving confirmation that the information presented is suitable for submission as part of the request for prior authorization during the current transaction, transmitted to at least one of a prescriber for approval and the benefits manager.
Owner:COVERMYMEDS
Method for competitive prescription drug and/or bidding service provider selection
Owner:TAG LLC (US)
Diverse methods of facilitating a request for prior authorization with a common user experience
Provided are a method and computer system for facilitating a request for prior authorization of insurance coverage for a prescribed drug. An appropriate submission protocol is identified from among a plurality of different submission protocols available based on user input received over a communication network. Content is served to be utilized by a user computer for generating a user interface comprising a plurality of data-entry fields in which a user is to enter the patient-related information that is to be submitted as part of the request for prior authorization. The content transmitted is to be used for generating the user interface to include common fields regardless of which of the plurality of different submission protocols is to be utilized, thereby providing users with a transparent, familiar experience to submit a request for prior authorization according to different submission protocols.
Owner:COVERMYMEDS
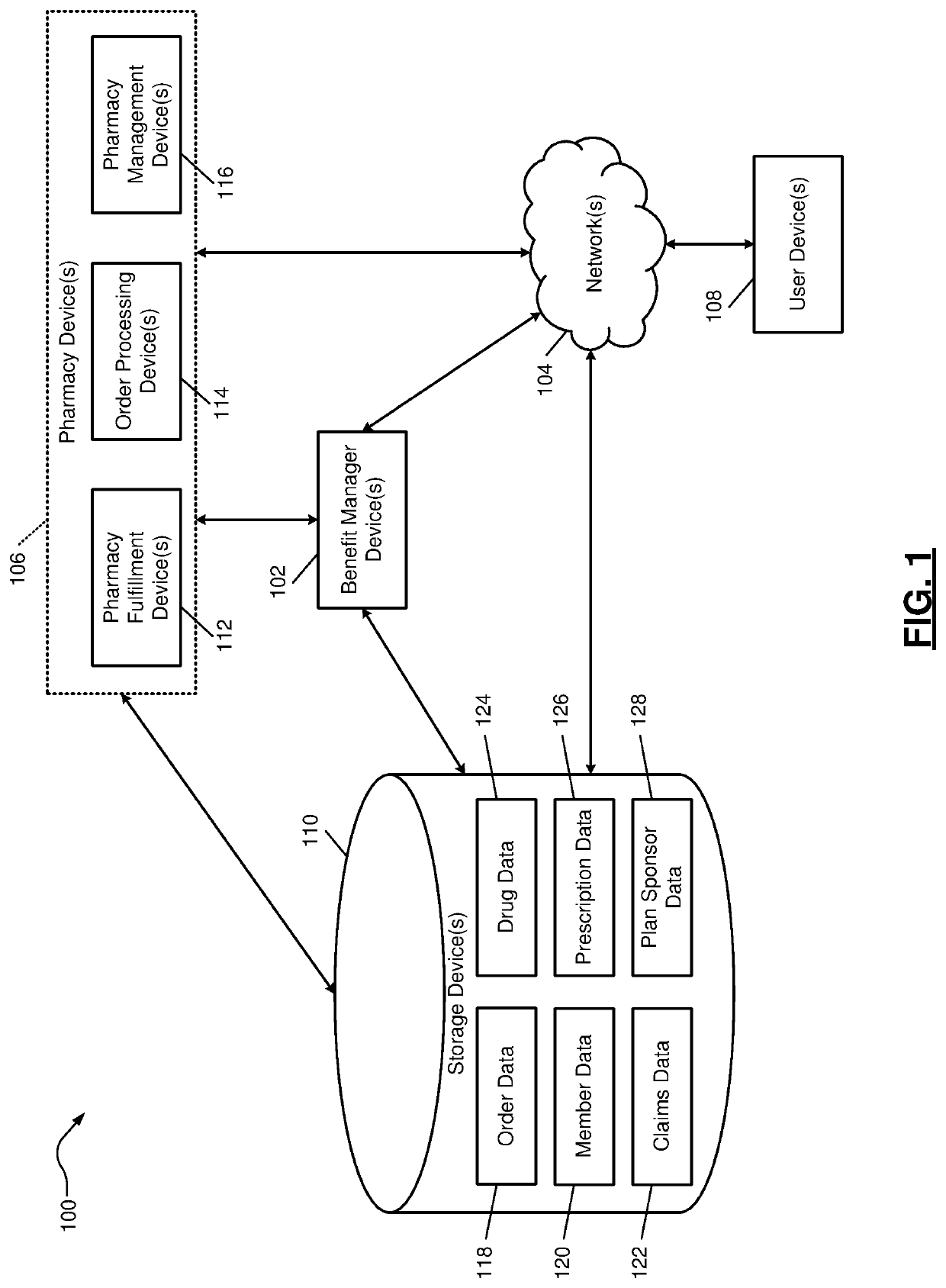
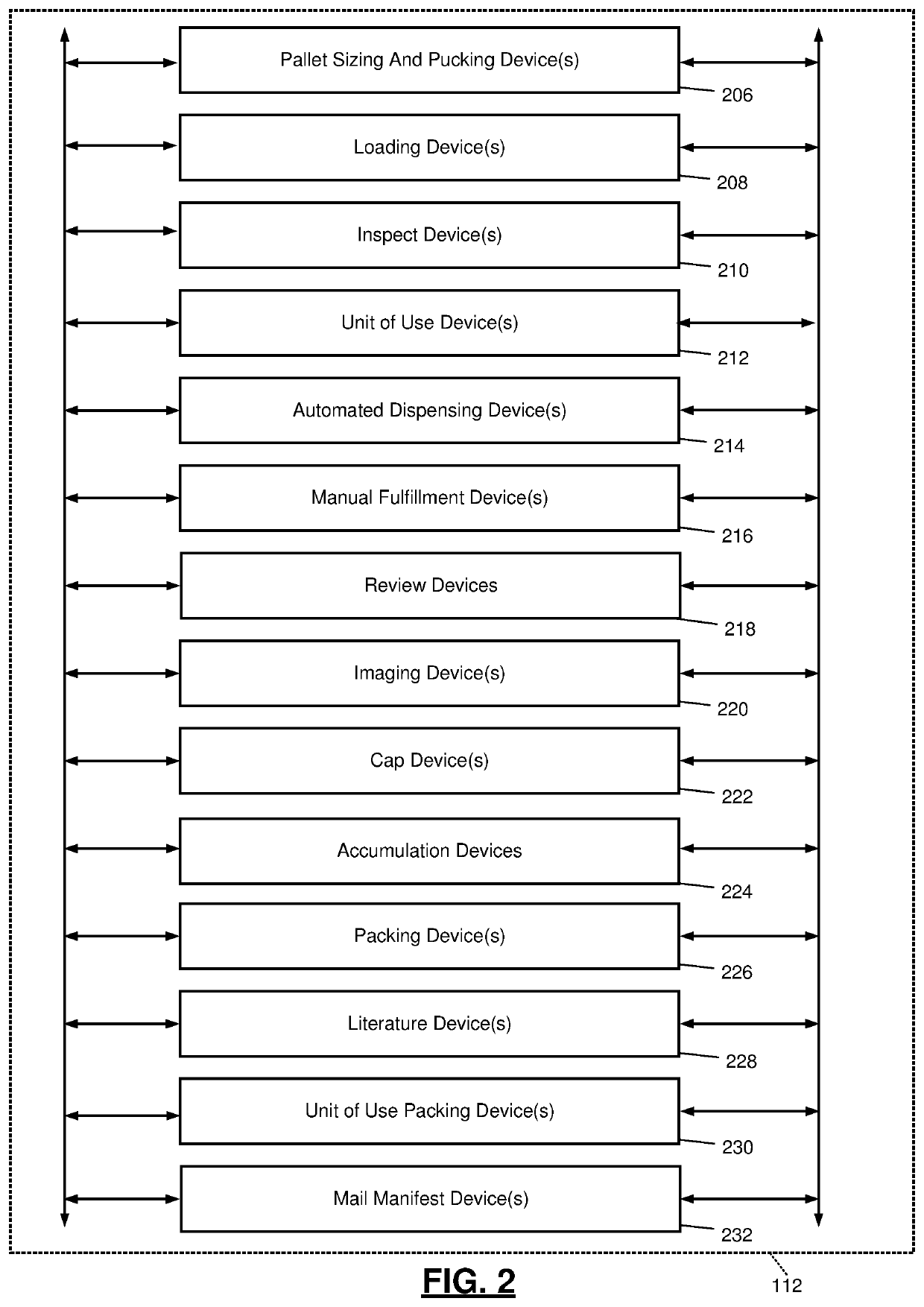
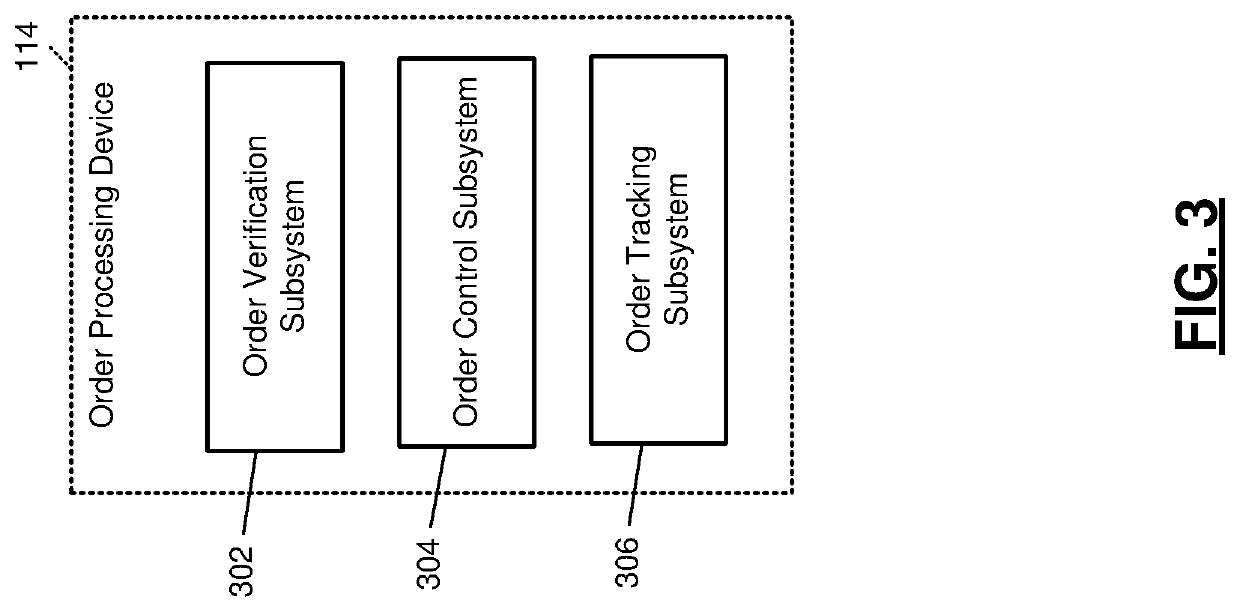
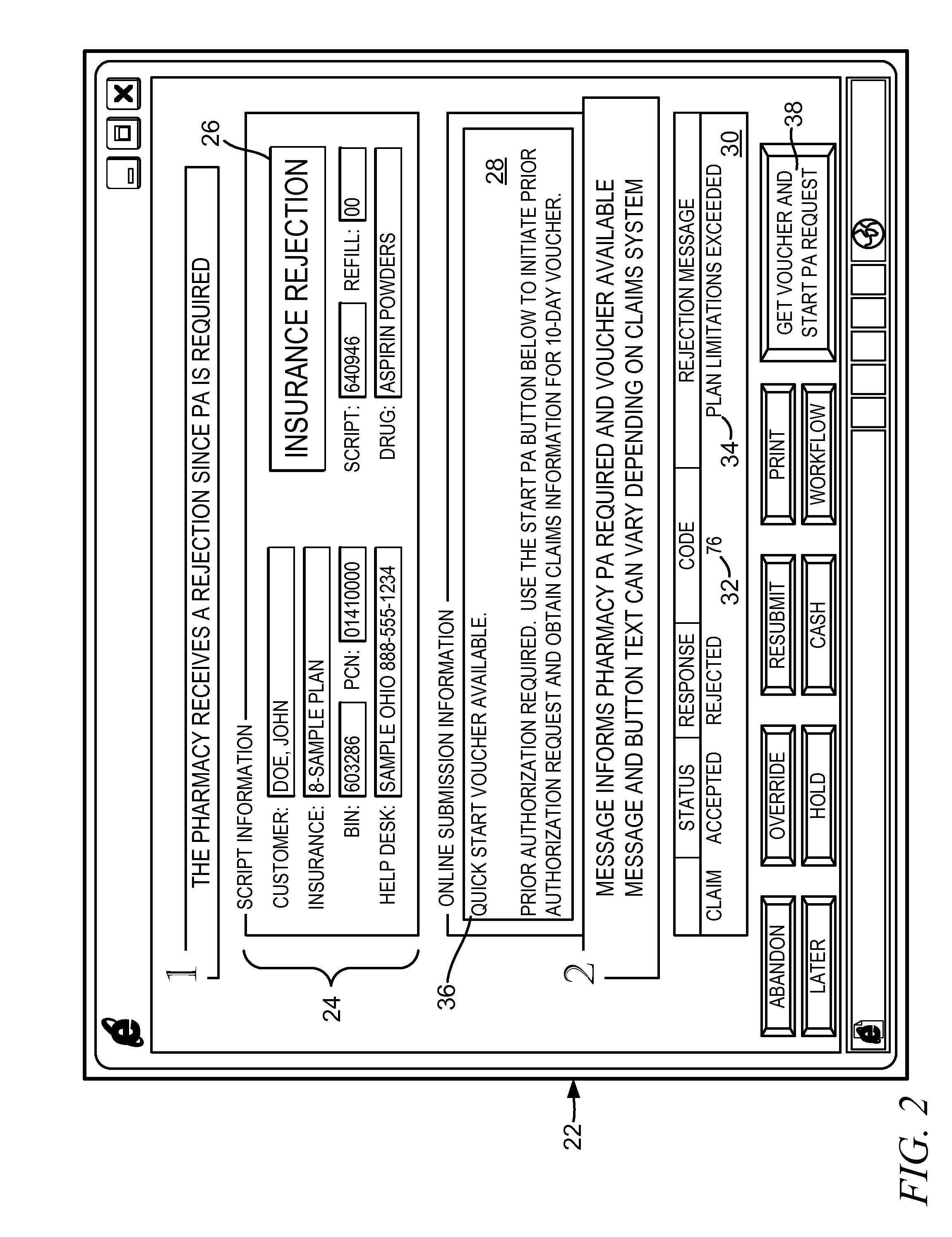
System and method of assisting prescription treatment fulfillment
Provided is a method and system for facilitating limited fulfillment of a prescription for a drug. An indication that an authorizing party has rejected an insurance claim submitted by a pharmacy for insurance coverage of at least a portion of a purchase price of a prescription drug on behalf of a patient is received over a network, in addition to an indication that prior authorization is required. Before a decision whether to grant the prior authorization is issued by the authorizing party, initiating transmission of an offer to allow redemption of a quick start voucher to the pharmacy over the communication network that allows the limited fulfillment of the prescription for the prescription drug, but less than the complete fulfillment.
Owner:COVERMYMEDS
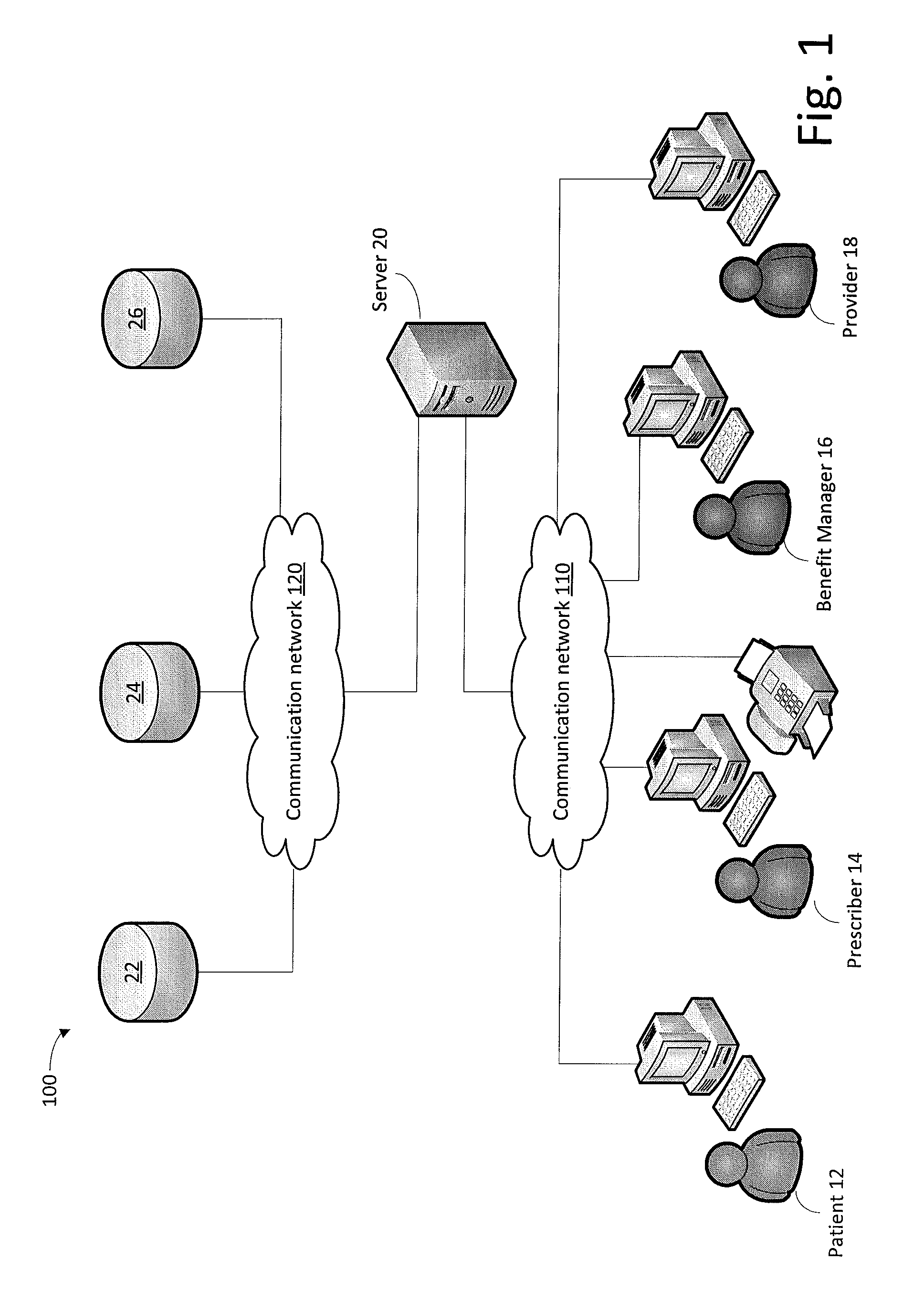
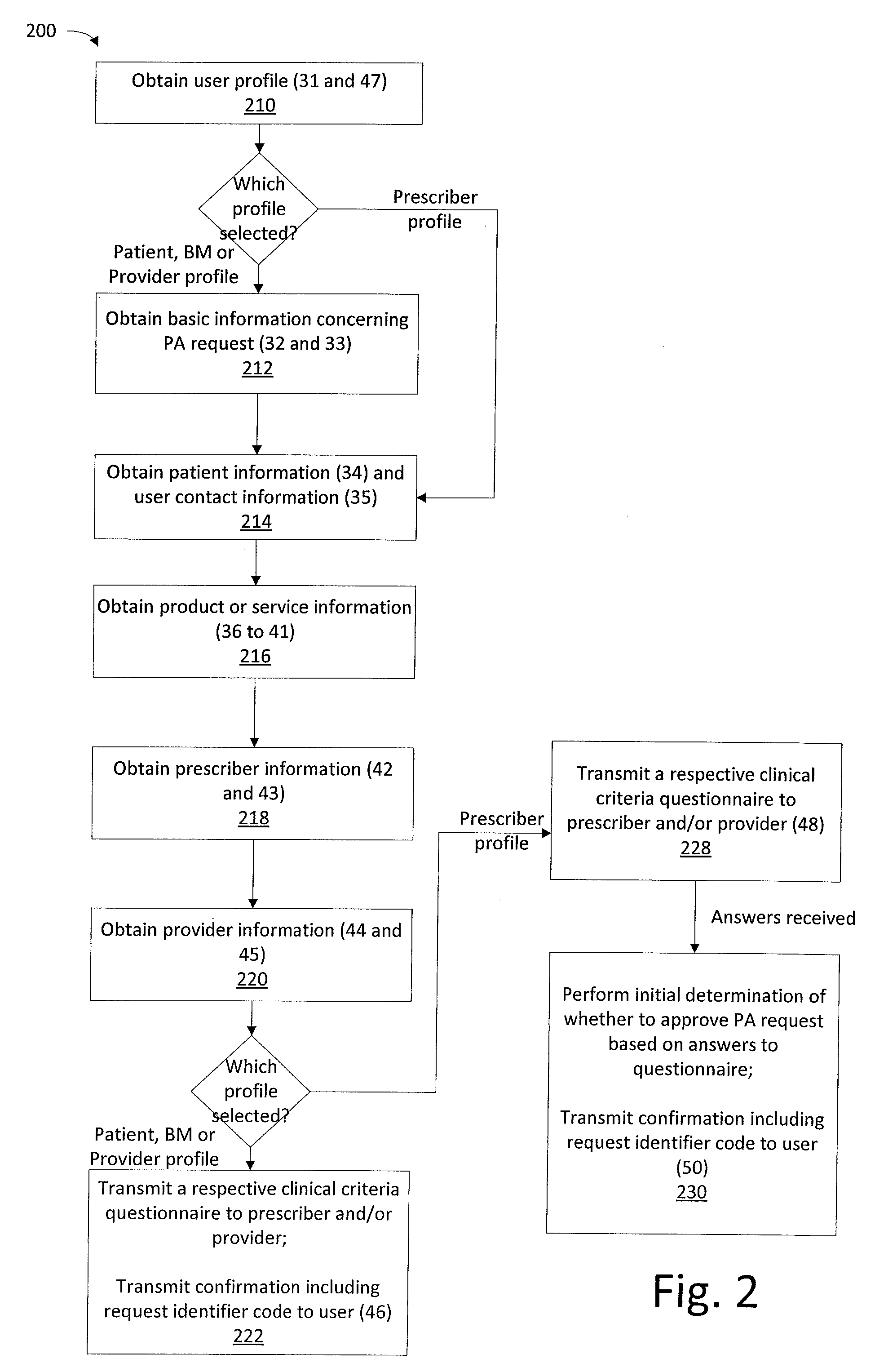
Method and system for requesting prior authorization for medical products and services
InactiveUS20150046173A1Facilitate initiationReduce the amount of communicationFinanceDrug and medicationsPrior authorizationProgram planning
A system and method for requesting prior authorization for a medical product and / or service includes a processor providing a user interface accessible over a network and via which to receive user input of information concerning the product and / or service, the intended recipient thereof, and the prescriber thereof. The user interface is accessible using each of a plurality of user profiles, including two or more of the prescriber, user, and provider. Login information is not required for the request generation, a recipient health plan identification being used instead. Different sequences are provided by the processor depending on the user profile used for generating the request. Request status is provided based on input of a code generated for the request and without requiring login information. The system is configured to generate and transmit to the prescriber a communication regarding the request where the request is initiated using a recipient profile.
Owner:AGADIA SYST
Methods for remotely accessing electronic medical records without having prior authorization
ActiveUS20140379380A1Data processing applicationsPatient personal data managementMedical recordPrior authorization
Methods are provided for allowing patients, health care practitioners and other service providers to have remote access to electronic medical records of a patient stored on a first computer network by the remote user requesting access to the electronic medical record from a second computer network and providing a first and second piece of patient derived information to the second computer network; the second computer network transferring the first and second piece of patient derived information to a third computer network; the third computer network authorizing the remote user through the first and second piece of patient derived information and dependent on a patient specific authorization protocol; the third computer network confirming a patient specific consent protocol; and the third computer network disclosing the electronic medical record to the remote user dependent upon an authorization and a confirmation received from the third computer network.
Owner:HIPAAT
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com