Pressure Sensing Catheter
a technology catheter, which is applied in the field of pressure sensing catheter, can solve the problems of inconvenient intra-arterial placement, inconvenient catheter placement, and significant differences between cvcs and piccs in placement techniques and potential complications, so as to facilitate catheter placement, minimize catheter insertion-related complications, and eliminate inherent shortcomings
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
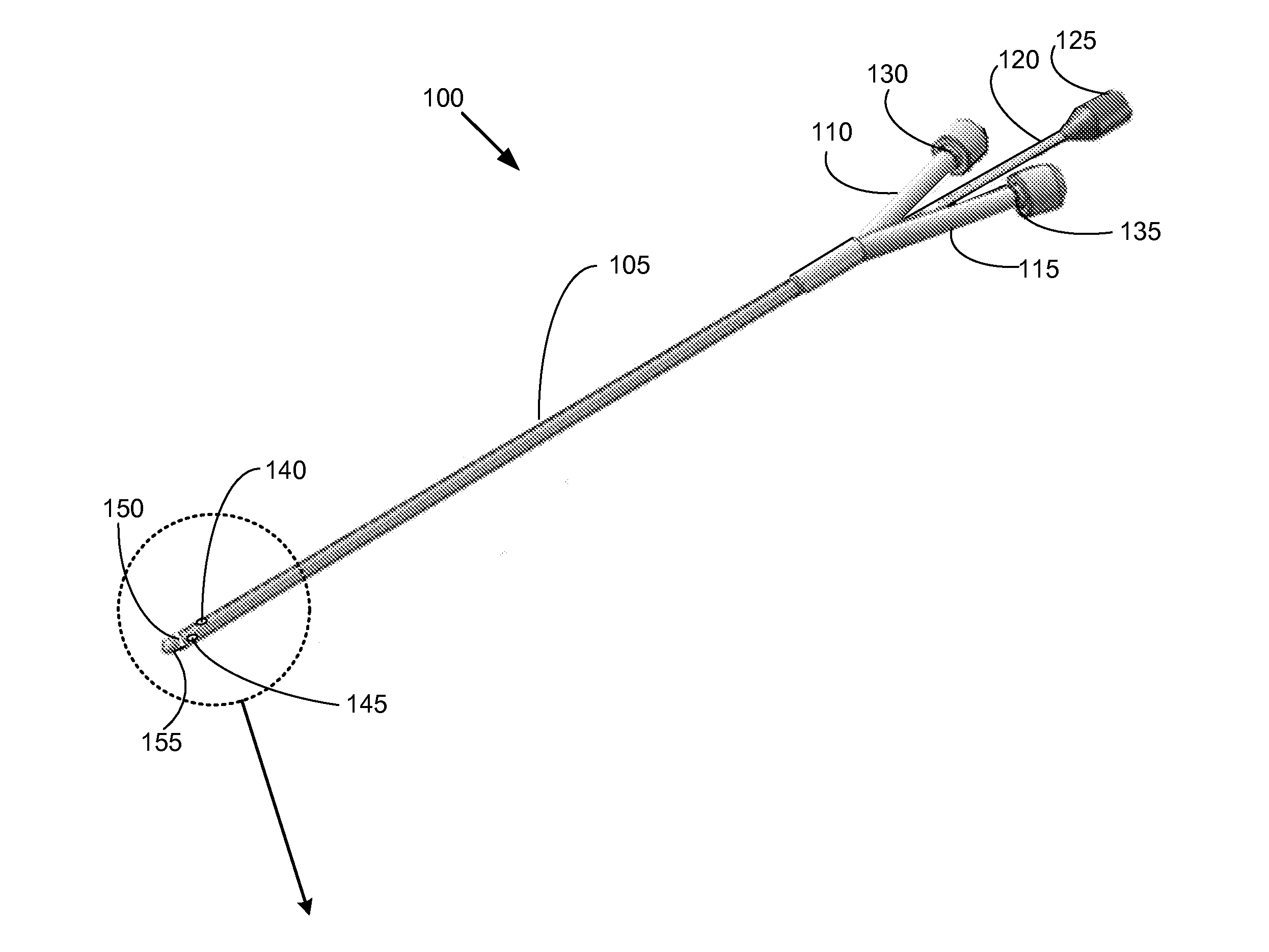
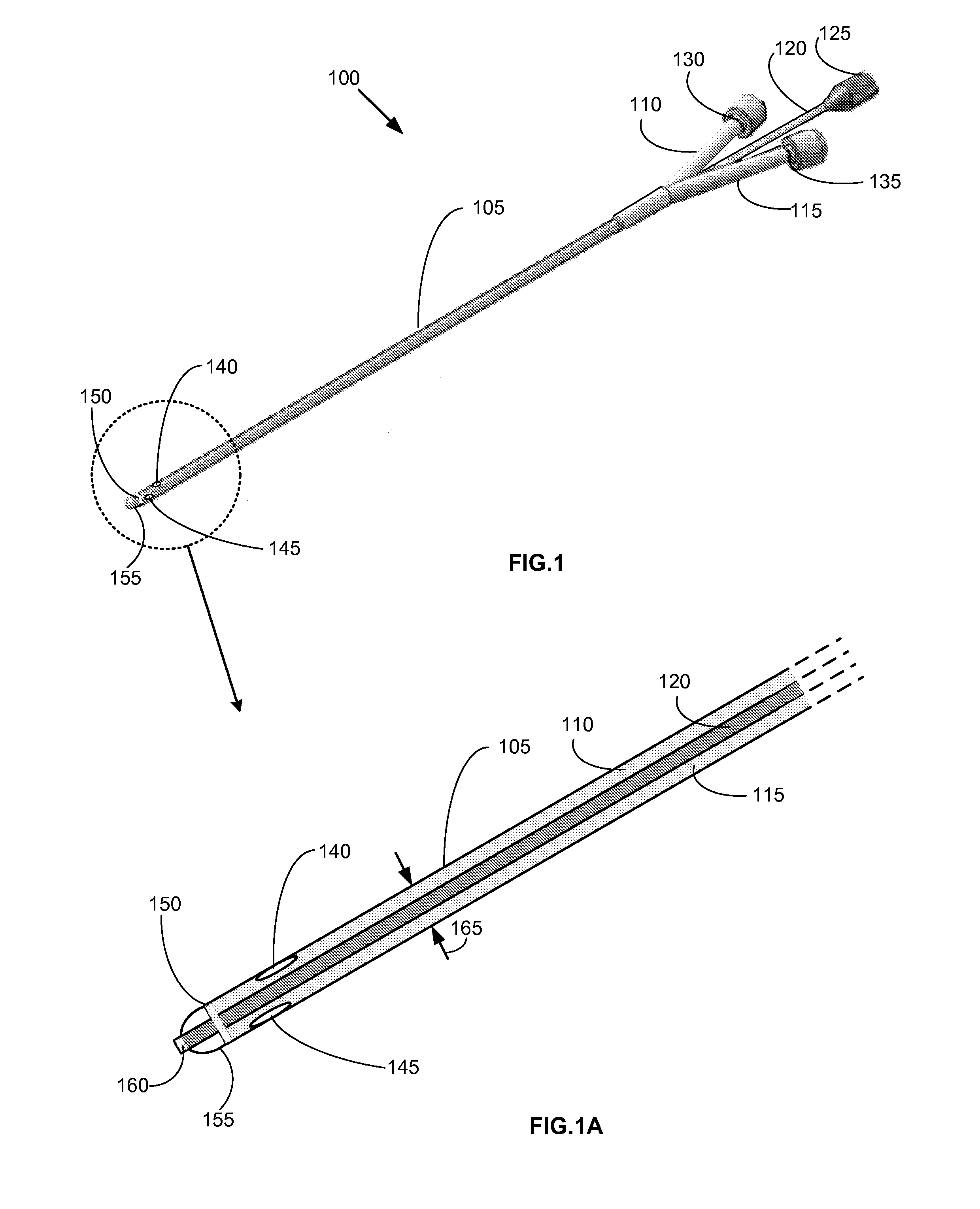
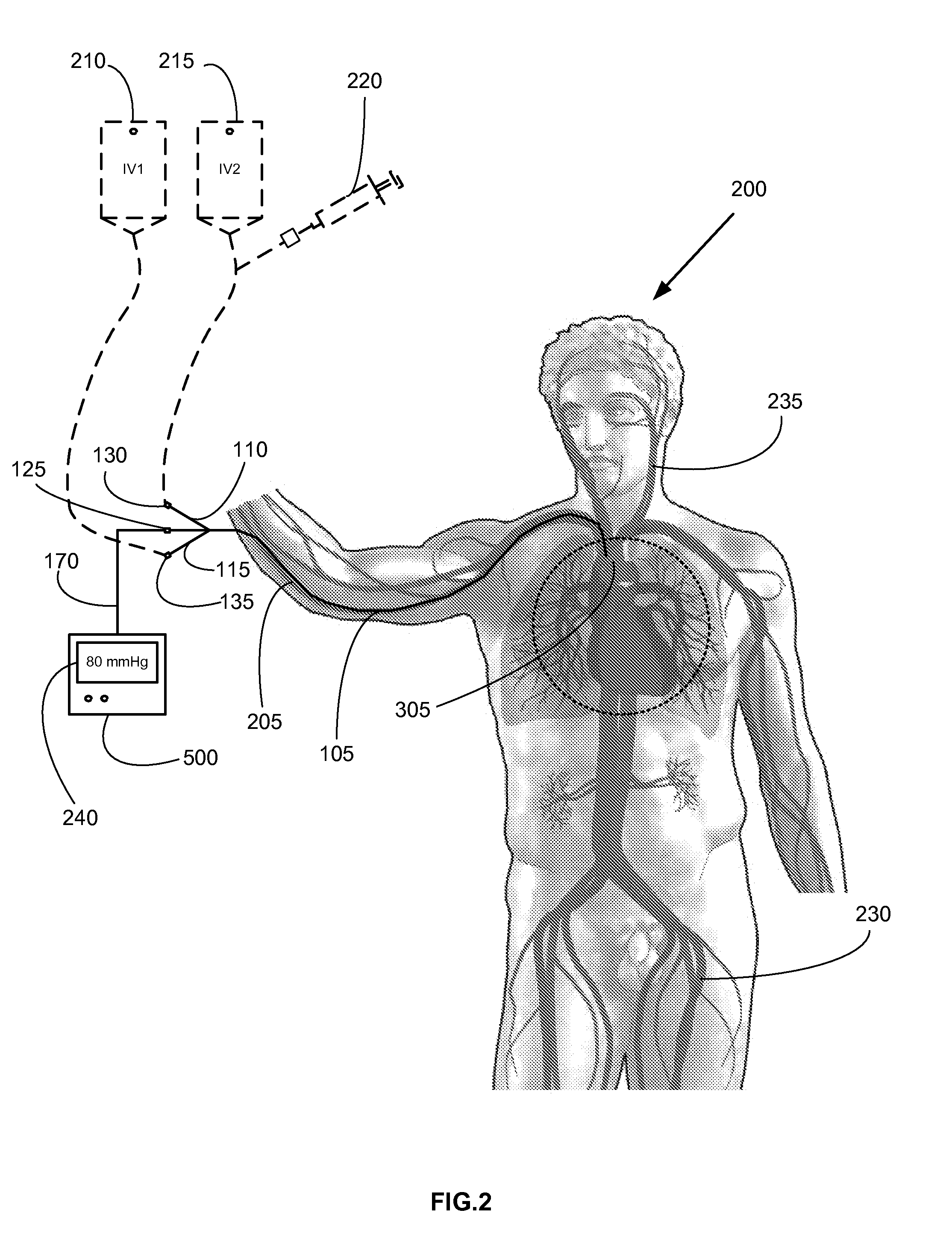
FIGS. 1, 1A provide an exemplary embodiment of a pressure sensing catheter. In an embodiment, pressure sensing catheter 100 is comprised of a flexible conduit section 105 having dual lumens 110, 115 (FIG. 1A). Each lumen 110, 115 is contiguously connected at a proximal end to a leur connector 130, 135 (FIG. 1A; shown with leur caps installed). Leur connectors 130, 135 allow for the contemporaneous infusion of fluids and / or withdrawal of fluid samples from a patient when pressure sensing catheter 100 is disposed in situ. One skilled in the art will appreciate that other types of connectors known in the relevant art may be used in lieu of the leur connectors 130, 135.
A separate signal lead connector 125 is provided at the proximal end of pressure sensing catheter 100 which facilitates coupling of a signal lead 120 with an electronic monitor 500 (FIG. 5). Signal lead 120 longitudinally extends from signal lead connector 125 to a pressure transducer 160 disposed at about a distal end of...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com