Unfortunately, the TRAM flap is a major surgical procedure that carries a substantial amount of morbidity, inflicts multiple incisions and has a significant failure and
complication rate.
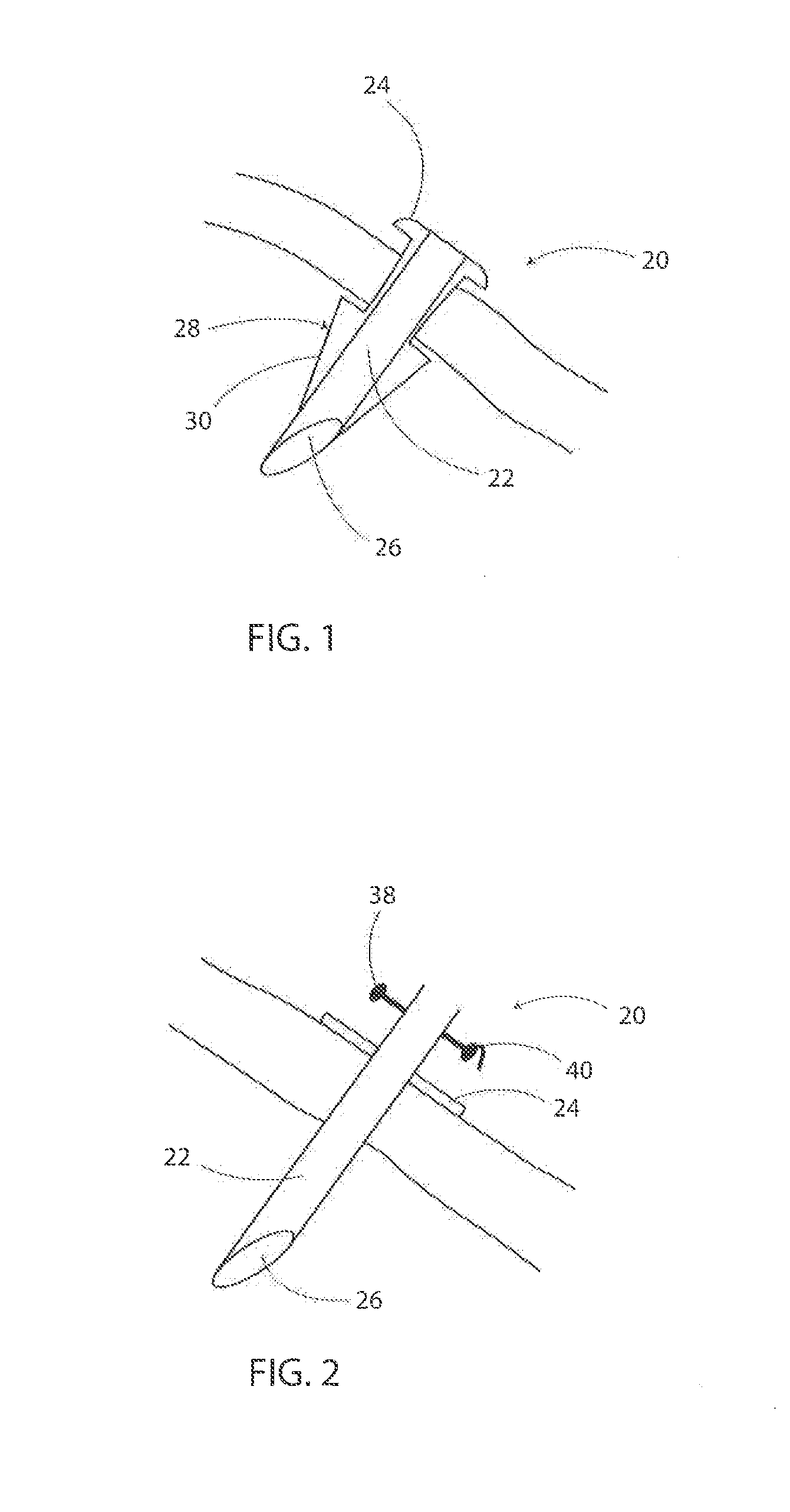
With this process, as dictated by the typical prior art needle, it is difficult to penetrate the
skin again back through the exact same exit pin hole, and even if it does, it is even more difficult to follow the exact same path along the subdermal fibers.
As a result, the thread that follows will inevitably grab some
skin or some subdermal fibers along its in and out looping path, and when tightened, the stitch will almost invariably create some dimpling of the skin at each entry /
exit site.
Otherwise, instead of resulting in an even line fold, the purse-string tightening may result in unsightly curtain like dimples, bulges and folds.
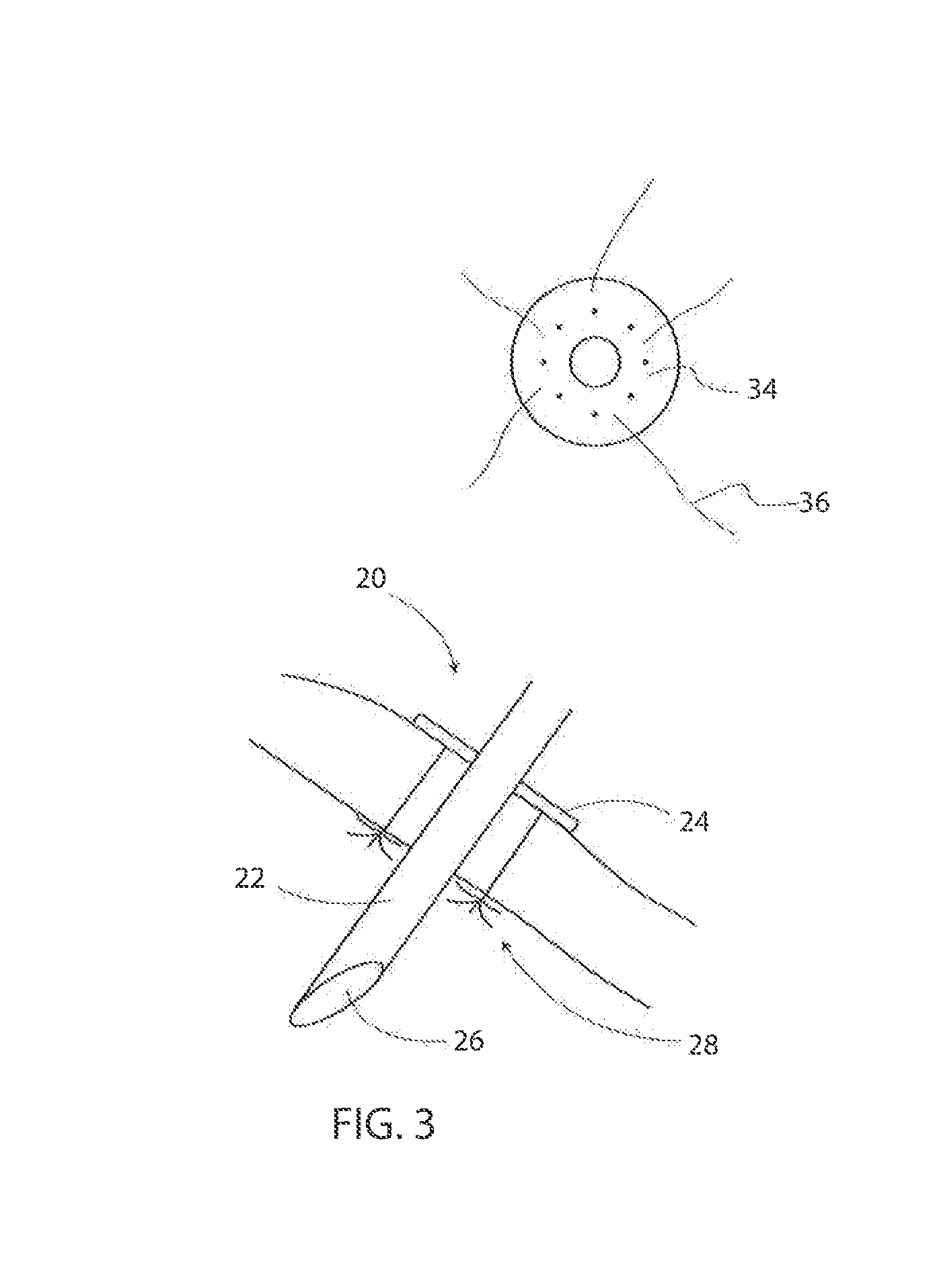
This mechanically weakens the needle at its very center where the torque is strongest while it is driven through the patient, making it prone to breaking with a broken piece deeply lodged and causing complications.
This is delicate and trickier than it may seem, as inadvertent minimal exiting of the second needle tip will inevitably catch dermal fibers during re-entry, annul the
advantage of the double pointed needle and lead to failure of that entire needle path.
The problem becomes even more delicate when the desired depth / level of tissue suturing is more superficial or needs to be precisely set.
However, this may be found to be cumbersome and not ideal.
Adjusting the tightness of the suspension and of the purse string by tying a knot is not precise and the secured knot leaves behind an undesirable
mass of palpable bulky tissue.
For the breast
surgery procedures described infra, pulling up the abdominal tissue to the chest is limited by the
resultant tightness of the advanced tissues.
First, the large gap created when the released tissue is advanced leaves behind a void or a cavity that needs to be filled in order to properly heal. This void is usually filled with a flap of tissue; a step that often requires another major surgical intervention whereby vascularized tissue taken from another location on the patient's body is transferred to fill that gap.
Second, the
surgical incision itself to release the tissue leaves new permanent
scars. The same is true for the site where the flap is excised. This amounts to treating a scar with a scar inducing procedure.
Third, this alternative does not address the stiff fibrous scar; it only incises it and divides it in half so that the bulk of the
scar tissue remains in its present state.
Fourth, the degree of advancement that can be achieved with a
single incision is limited.
Fifth, by also dividing the endogenous blood vessels, the incision impairs the circulation and limits the amount of advancement.
Attempts at excising the scar are also often futile.
Simply excising the block wall in itself induces
tissue trauma that often heals by leaving behind a new scar and often re-erects a new wall and does nothing to address the
scar tissue deficiency problem.
If we forcefully tighten one of the strings and keep the other loose, a needle nick to this construct will cause the tight one to snap but will leave the loose one relatively unaffected.
There is a natural limit to how much tissue can normally be advanced in order to close a wound defect, release a tight
contracture or create a breast mound.
Trying to advance the skin beyond the natural laxity limit of this subcutaneous
aponeurosis places these structures under tension rendering them much more susceptible to being nicked by a needle tip and thus separated than the surrounding tissues.
Too aggressive a meshing will destroy the circulation, leading to
ischemia and
necrosis.
It can also tear the deeper tissues and result in the creation of excessively large cavities instead of those of a delicate fibrovascular recipient
scaffold.
Excessive meshing destroys the integrity of the
scaffold and leads to excessive numbers or sizes of cavities.
The current practical limitation of
tissue engineering is not the cells, as these are readily available from simple
liposuction or from tissue cultures, but the three dimensional supporting
scaffold with functional blood capillaries connected to the circulation of the recipient.
It is the inability in the prior art to build a fibrovascular scaffold (fibrous scaffold with capillary circulation) in the laboratory and connect it to the recipient
blood circulation that limits the ability to build three dimensional
solid organs or blocks of tissue.
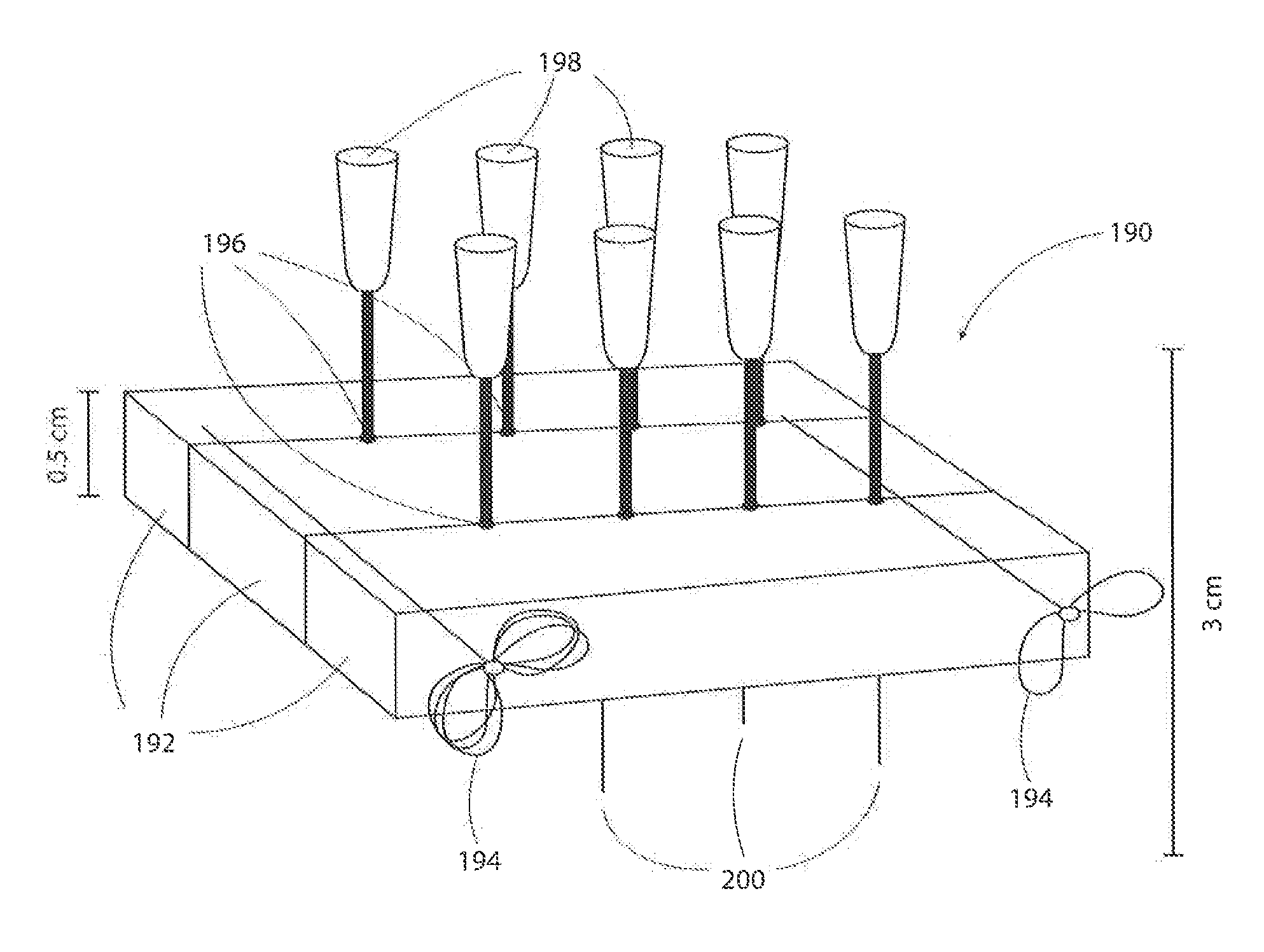
The inventor contemplates that thinner rods will not have enough mechanical
torsional strength to do most jobs and thicker ones will leave more noticeable
scars at the entrance points.
Unfortunately, these devices have limited effectiveness; proof is that despite years on the market, they have not replaced the surgical facelift operation.
The effectiveness of these devices is limited by their inability to safely deliver the amount of injury to the deep
dermis and
subcutaneous tissue that will result in the required scar retraction while completely sparing the more superficial delicate tissues from the injurious agent.
Since the distance between these two tissue
layers is of the order of millimeters and fractions of millimeters, even a limited scatter of the most precisely focused agent is bound to cause collateral damage.
This tailoring operation requires multiple incisions to remove (or plicate) the excess skin and therefore leaves behind unsightly
scars.
The main problem in breast ptosis is the excess skin and laxity of the internal suspensory
ligament (also called
ligament of Cooper).
If the brassiere is not adherent or not stiff, some threads might be tightened more than others to cause unsightly dimples.
 Login to View More
Login to View More  Login to View More
Login to View More