Anti-blood coagulation surface modifying method of artificial implant
A surface modification and implant technology, applied in the field of anticoagulant materials, can solve the problems of reducing the flexibility of artificial blood vessels, insufficient anticoagulant performance, and poor stability, so as to improve anticoagulant performance and overcome insufficient stability of performance , the effect of avoiding damage
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
specific Embodiment approach 1
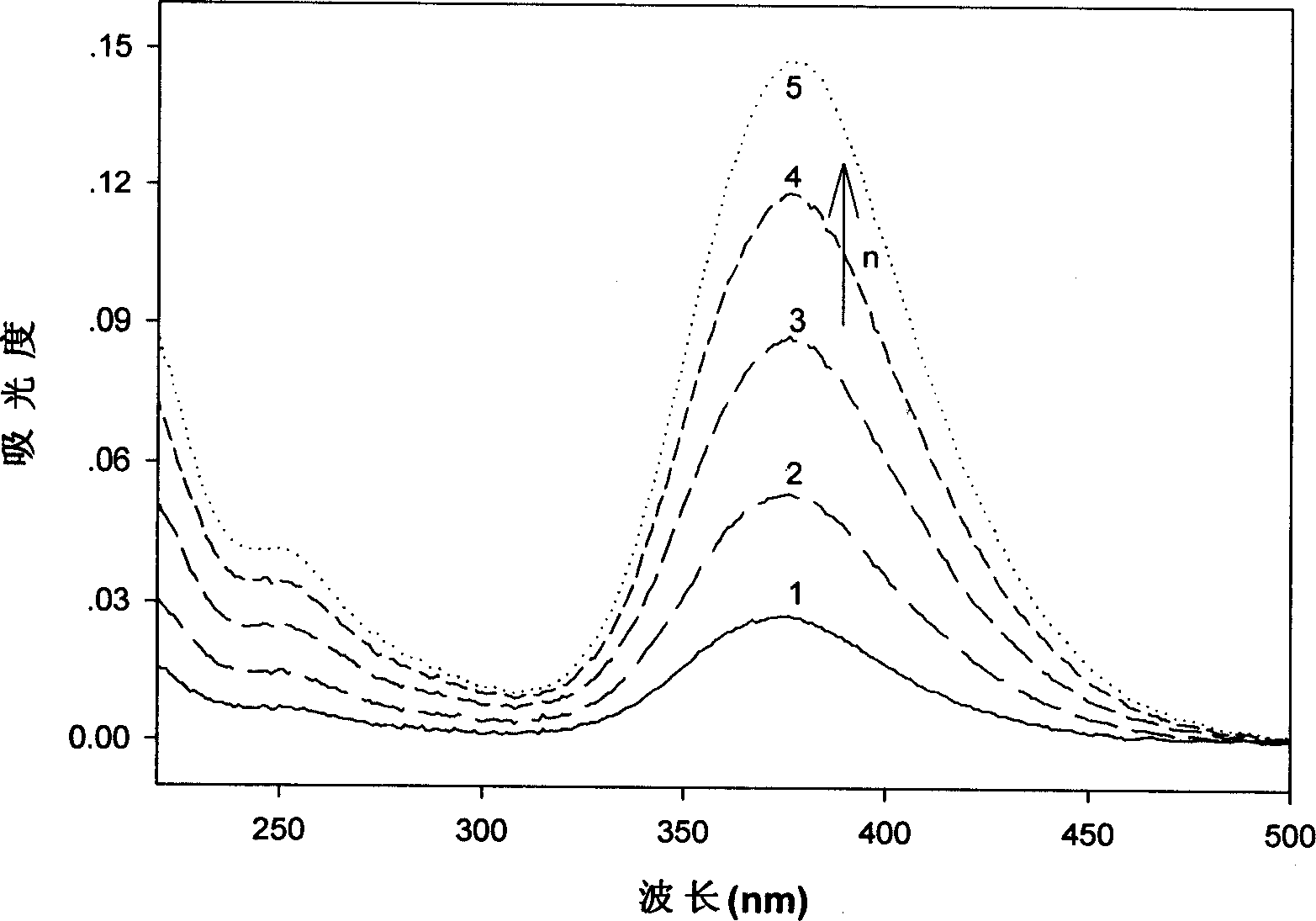
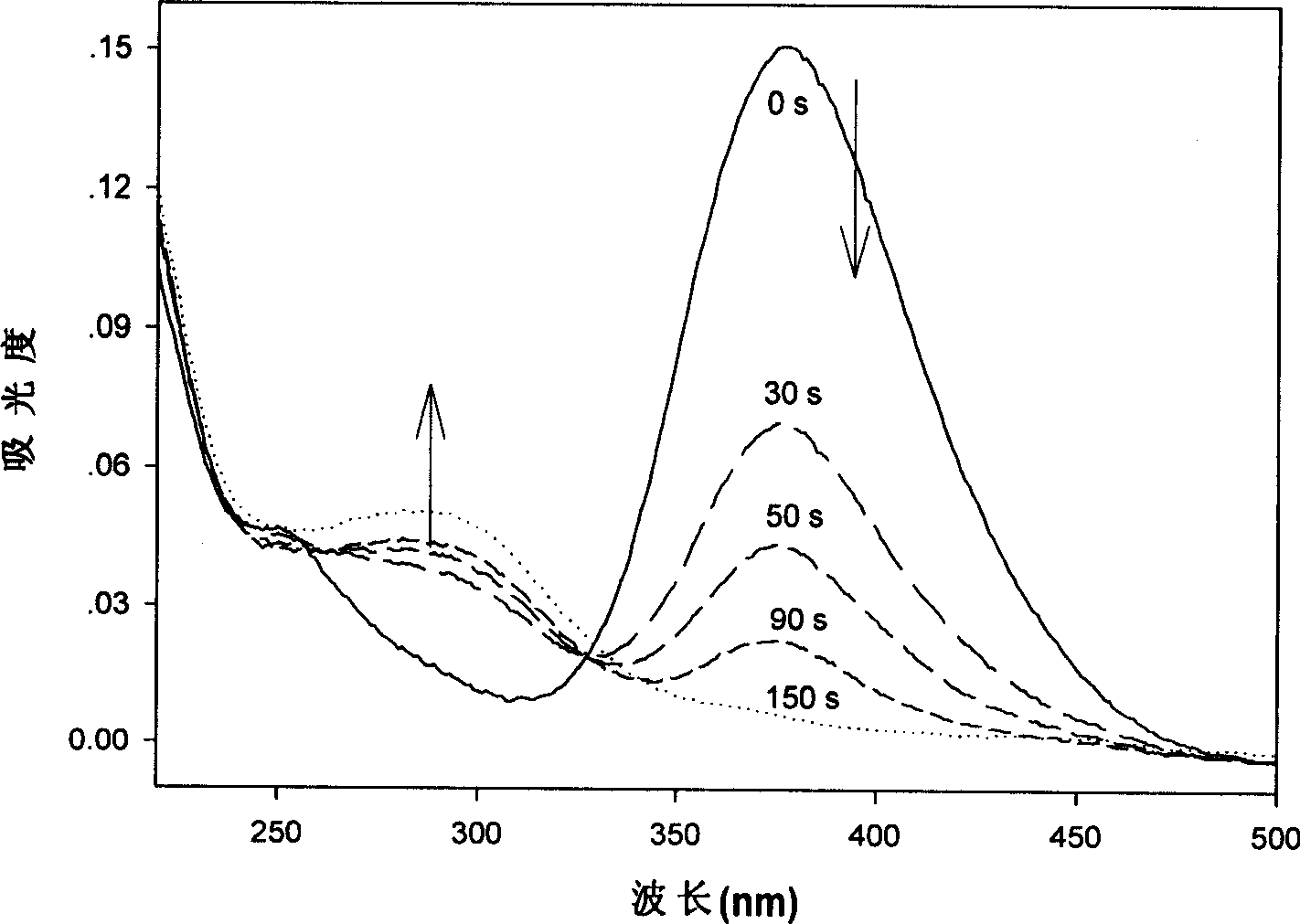
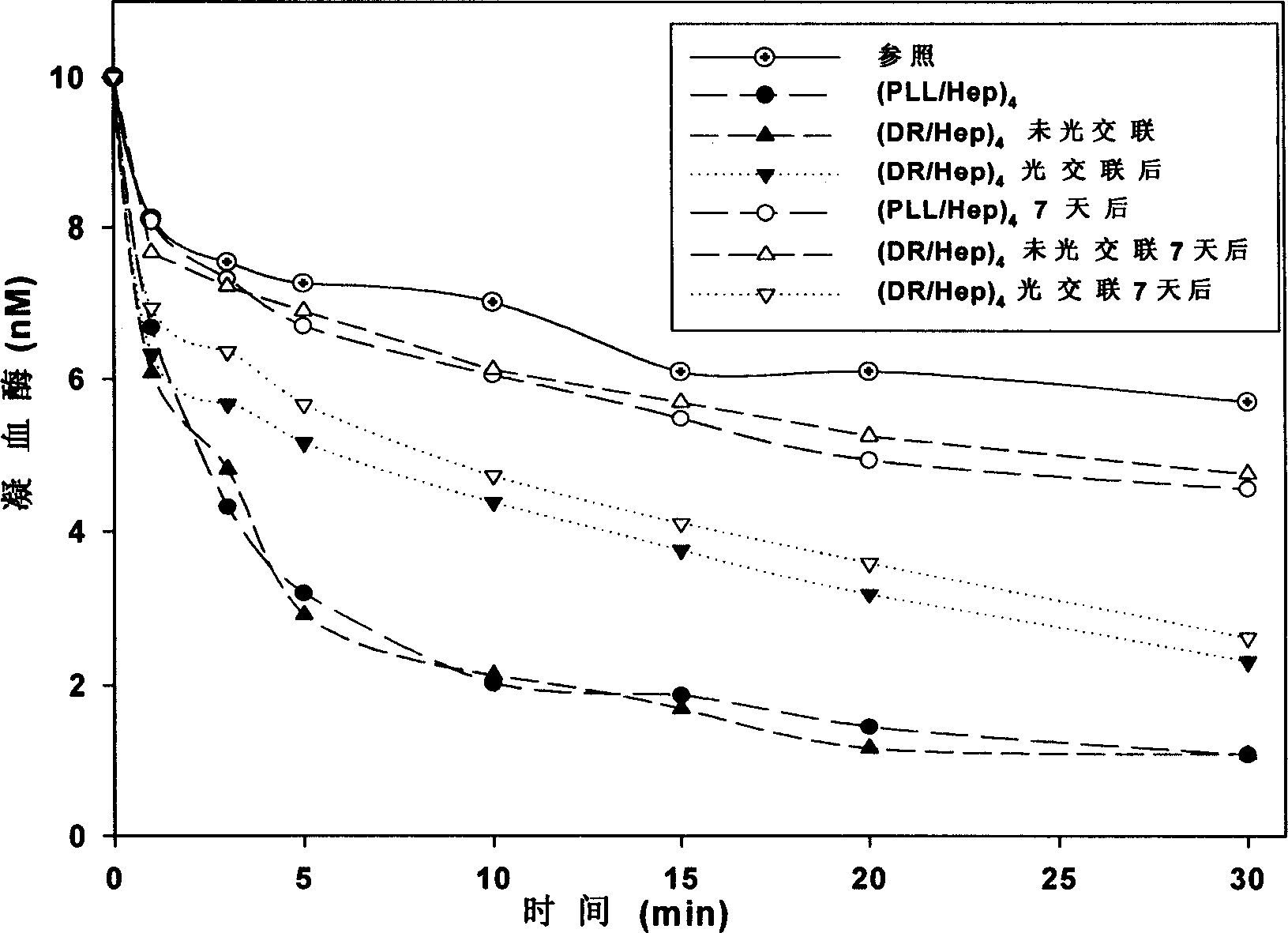
[0017] Specific Embodiment 1: This embodiment is achieved in the following way: a. Soak the artificial implant in an organic solvent, ultrasonically clean it for 30 to 120 minutes, and then dry it at 30 to 90°C for 0.5 to 2 hours; b. Medical silicone rubber is used as a room temperature curing adhesive, which is dissolved in an organic solvent to prepare a silicone rubber solution; c. Coating medical silicone rubber on the inner surface of the artificial implant as a soft support; d. Coating the silicone rubber coated with perfluorosulfonic acid on the surface; e, positively charged polycations and negatively charged polyanions are alternately deposited on the surface of perfluorosulfonic acid coating through electrostatic attraction; f, artificially irradiated with ultraviolet light Implanted into the inner wall of the body, the ionic bonds between the inner layers of the membrane are converted into covalent bonds through photochemical reactions, and an anticoagulant surface u...
specific Embodiment approach 2
[0023] Specific implementation mode two: this implementation mode is realized in this way:
[0024] 1) Cleaning the artificial blood vessel: Soak the expanded polytetrafluoroethylene artificial blood vessel in an organic solvent, sonicate for 30-120 minutes, and then dry it at 30-90° C. for 0.5-2 hours.
[0025] 2) Dissolving the silicone rubber: dissolving the medical silicone rubber as a room temperature curing adhesive in an organic solvent to prepare a silicone rubber solution with a volume concentration of 0.1-100v / v%.
[0026] 3) Silicone rubber coating: connect the artificial blood vessel to the syringe, erect it, and then use the syringe to inject the silicone rubber solution into the lumen of the artificial blood vessel from the end until the lumen is filled. Then remove the silicone rubber solution from the end of the artificial blood vessel with a syringe, and dry it in the air at room temperature for 2 to 100 hours.
[0027] 4) Soak the silicone rubber coating: seal...
specific Embodiment approach 3
[0040] Specific implementation mode three: this implementation mode is realized in this way:
[0041] a. Soak the expanded polytetrafluoroethylene artificial blood vessel in absolute ethanol, sonicate for 30 minutes, and then dry at 60° C. for 1 hour.
[0042] b. Using medical silicone rubber as a room temperature curing adhesive, dissolve it in an organic solvent to prepare a 50v / v% silicone rubber solution;
[0043] c. Connect the artificial blood vessel to the syringe, stand it upright, and then use the syringe to inject 50v / v% silicone rubber solution into the lumen of the artificial blood vessel from the end until the lumen of the artificial blood vessel is filled. The silicone rubber solution was removed and dried in air at room temperature for 24 hours. Clamp the end of the artificial blood vessel with clips, fill the lumen with absolute ethanol, and let it stand for 2 hours.
[0044] d. Remove the ethanol, and inject 5wt% Nafion solution from the end of the artificia...
PUM
| Property | Measurement | Unit |
|---|---|---|
| thickness | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com