[0027] In some embodiments, genetically modified cells are used to over-express a therapeutic
gene. In preferred embodiments, genetically modified
smooth muscle cells (SMC) are used. This is because a large number of major human diseases, including
coronary artery disease, hypertension, and
asthma are associated with abnormal function of SMCs. In addition, SMC dysfunction also contributes to numerous other
human health problems including vascular aneurysms, and reproductive, bladder and gastrointestinal disorders. Therefore, a
therapeutic effect can be achieved by delivering SMCs which have been genetically modified to over express a therapeutic agent, thereby reducing or eliminating the physiological consequences caused by SMC dysfunction.
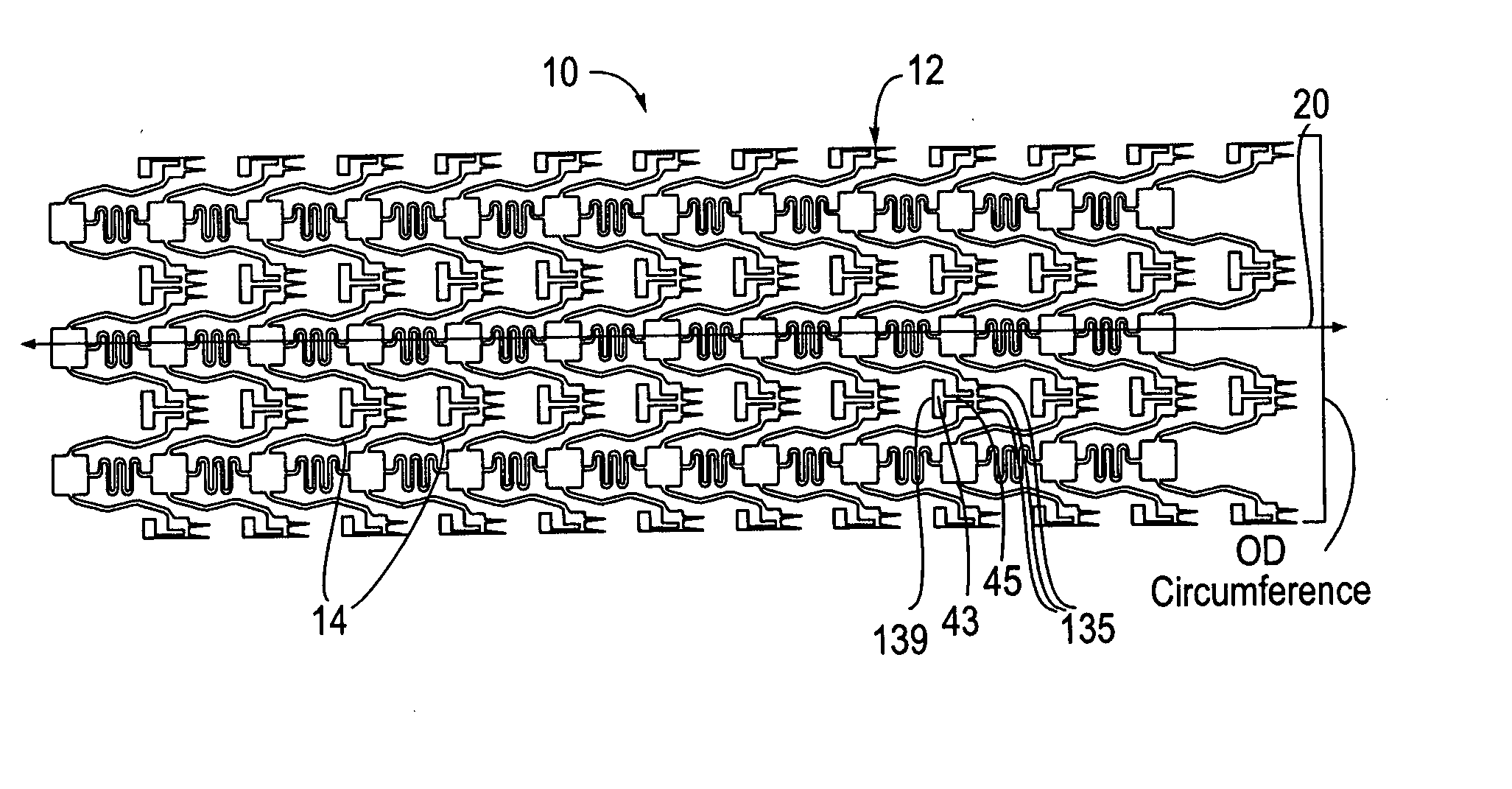
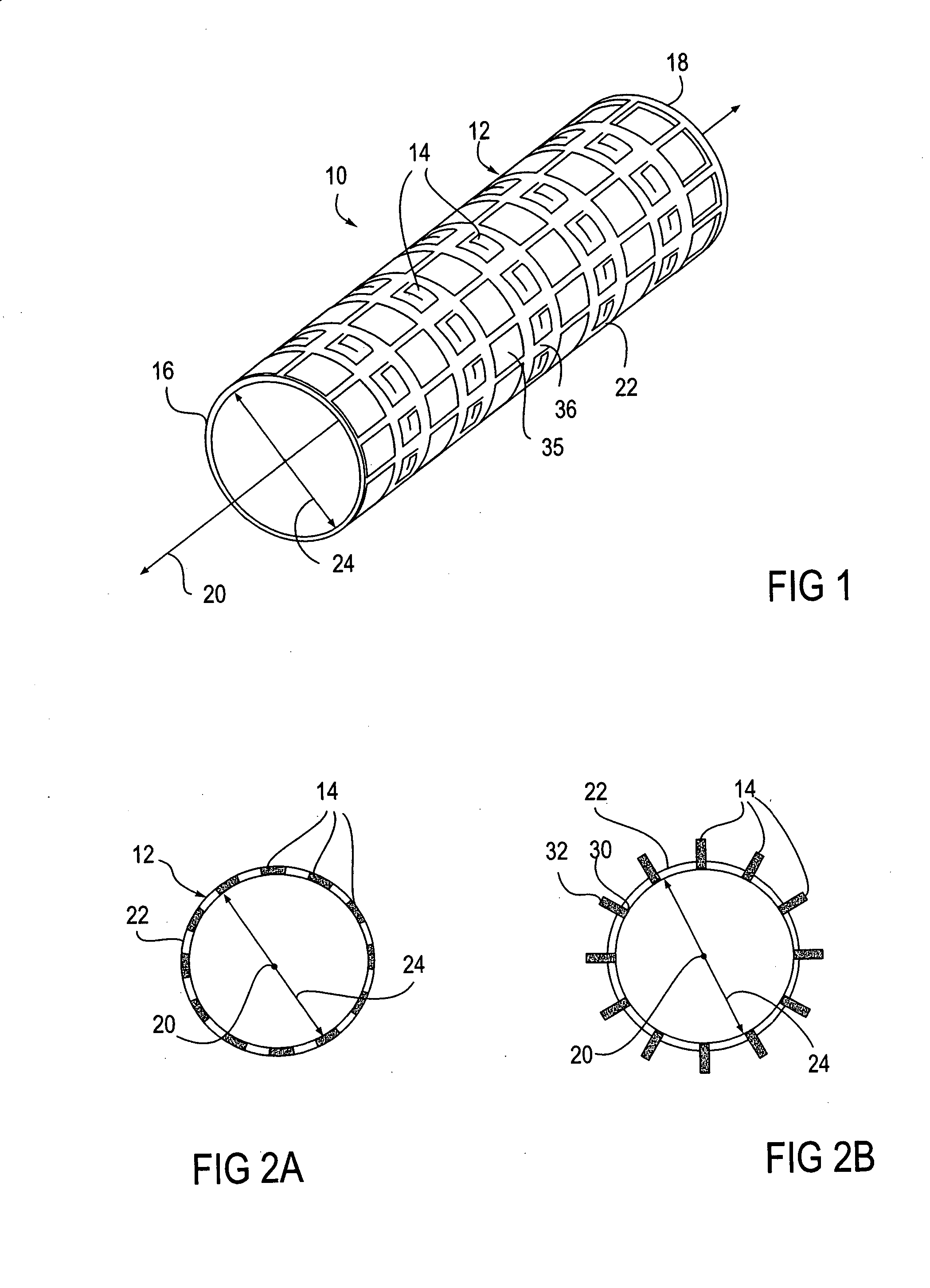
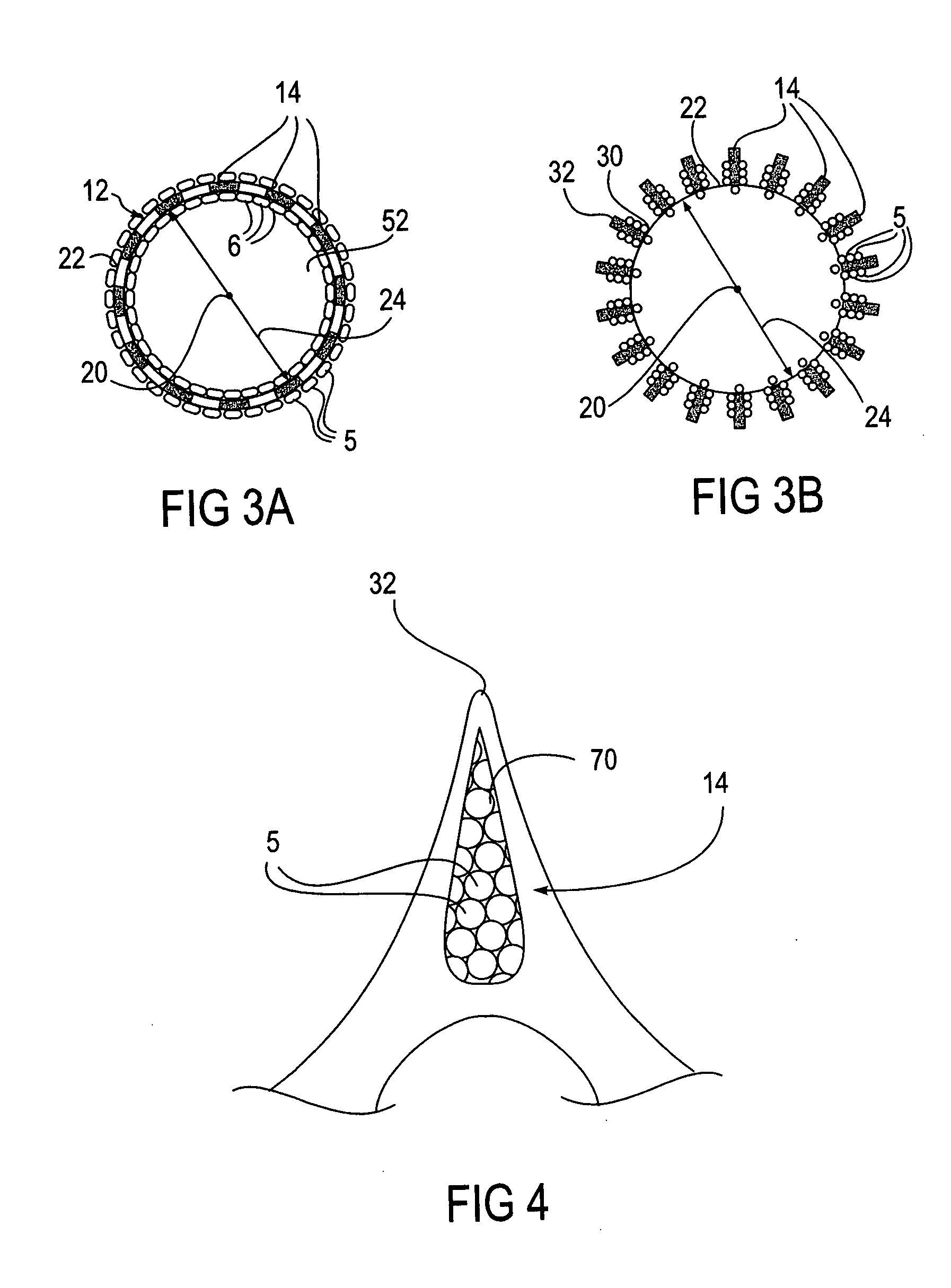
[0030] A major limitation in using these
stem cell derived
smooth muscle progenitor cells with conventional
delivery methods is that the conventional
delivery methods do not provide effective engraftment of the cells into the desired tissue site while at the same time reducing or eliminating the risks of delivery to non-target sites. As mentioned, the engraftment potential is highest for undifferentiated cells, however undifferentiated cells
pose the greatest risk for tumorigenesis or other undesired side effects. Therefore, a balance between these risks and benefits is desired. Such a balance may be achieved by the use of expandable bodies having micromechanical probes, such as provided by Reed et al. (U.S. Pat. No. 6,197,013), or expandable bodies having deployable microstructures as described above. In this preferred embodiment, the cells are seeded onto the expandable body and delivered directly to specific locations, particularly within the wall of a body lumen. The cells are mechanically embedded into and / or held against the wall of the body lumen which improves engraftment of the cells into the
target tissue. This process may be further aided by use of the
porous coating to deliver agents that promote engraftment as well as other desired properties of the cells.
[0032] Alternative genes that might be expressed to confer a therapeutic benefit include TGFβ1, which has anti-inflammatory properties and which also has been shown to inhibit SMC growth, promote differentiation, and enhance production of
extracellular matrix components. Other possibilities include cytokines IL-4, IL-10 or IL-13 whose anti-inflammatory properties may promote wound repair or regeneration and / or reduced
restenosis.
[0034] In other embodiments, cells which have not been genetically modified to over-express a possible therapeutic
gene, referred to herein as “unmodified cells”, are used. Such cells may be used to augment
tissue repair and regeneration. For example, when unmodified autologous SMC,
stem cell derived SMC or SMC progenitor cells are used, proliferation of the SMCs and / or associated production of
extracellular matrix components including collagen and
elastin can rebuild blood vessels. The blood vessels may have been damaged due to
traumatic injury, such as by an accident, major
reconstructive surgery, or repair of a congenital vascular defect. The SMCs can also be used to rebuild blood vessels which suffer from aneurysms, a progressive
vascular abnormality associated with degeneration and
dissection of the
blood vessel wall and SMC hypocellularity. They may be caused by many factors including extensive
atherosclerotic disease, a congenital vascular defect, or mutations in genes important for determining the tensile strength of blood vessels, such as in the case of Marfan'
s Syndrome which is the result of mutations in the fibrillin
gene. In addition, a porous surface on the expandable body may be employed to deliver agents that enhance the desired properties of the unmodified cells. For example, TGFβ1 may be used since it is known to dramatically enhance
matrix production, and / or PDGF BB may be used to promote proliferation of progenitor cells provided on the device as well as recruitment of resident cells that could aid in the repair process.
[0035] When the cell-seeded expandable bodies of the present invention are used to treat an
aneurysm, the expandable bodies anchor a tube or graft to the vessel walls surrounding an
aneurysm. SMCs may be delivered to the vessel walls to increase anchorage of the tube and reduce migration of the tube along the
blood vessel. Such migration could lead to leakage,
exposure of the
aneurysm and damage to the
blood vessel, to name a few. In addition, the improved anchorage may also prevent apparent migration of the apparatus which occurs when the aneurysmal sac grows in size and as such encroaches upon the ends of the apparatus. This results in a reduction of the distance between the terminus of the apparatus and the aneurysm which is the same effect as migration. Thus, the SMCs help maintain intimate contact between the apparatus and the vessel wall and prevent aneurysmal sac growth. The SMCs can also be delivered to the blood vessel lumen, the
blood vessel walls and / or the outer surface of the blood vessel to encourage tissue regrowth or extra-cellular matrix formation. The SMCs may also be delivered to the aneurysmal sac. This may allow for tissue regrowth within the sac, strengthening the tissue within the aneurysmal walls. In addition, as noted above, a porous surface on the device may be employed to deliver agents to enhance the repair or
regenerative process.
 Login to View More
Login to View More