Osseointegrative surgical implant
a surgical implant and osseointegration technology, applied in the field of osseointegration surgical implants, can solve the problems of limited flexibility in the placement of implants, limiting or precluding the use of conventional single-stage implants, and the abutment of the anchorage of the retaining screw or other mechanical fastening device can eventually loosen or break, so as to promote healing and osseointegration, improve primary stability, and reduce friction
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
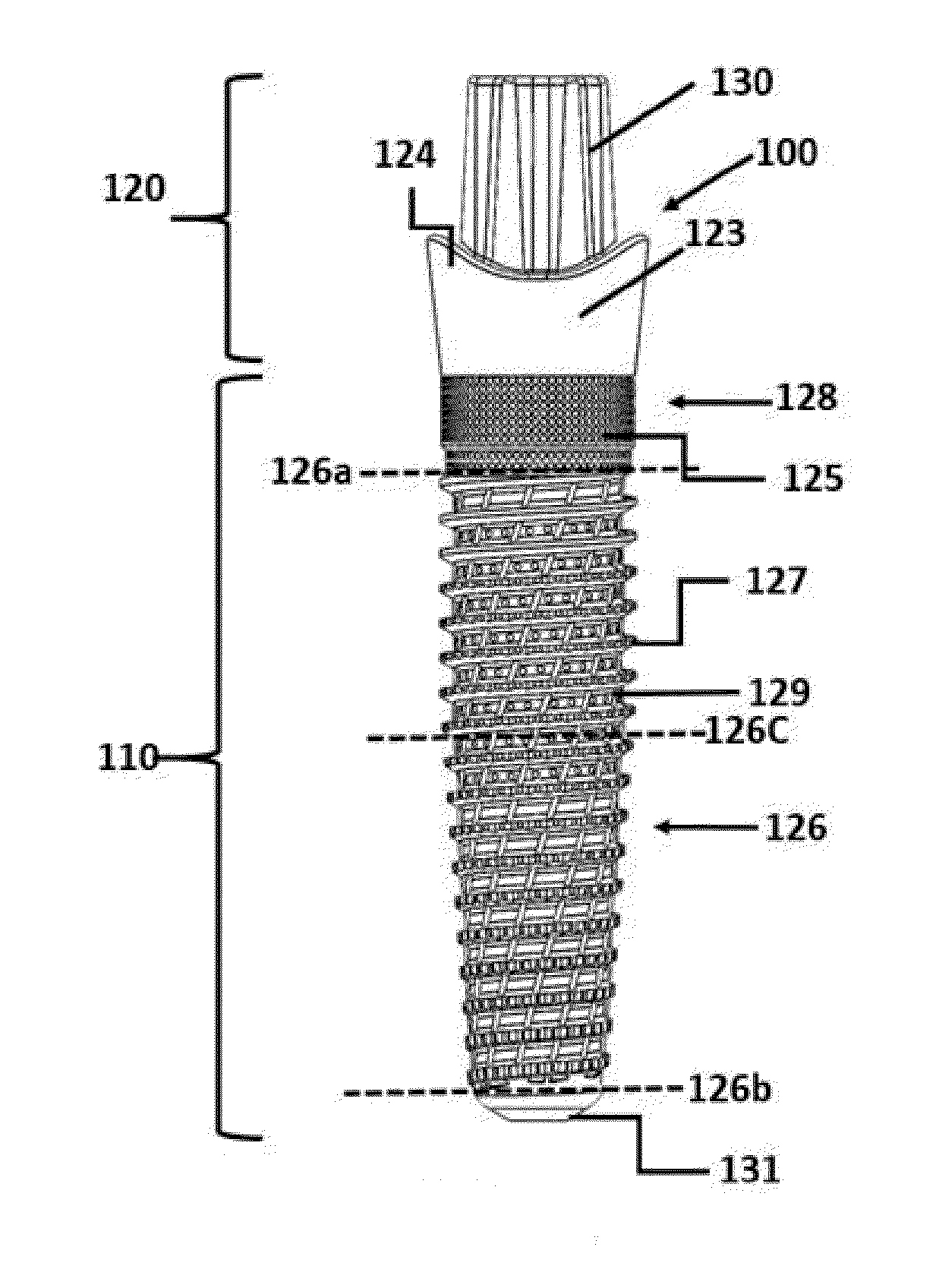
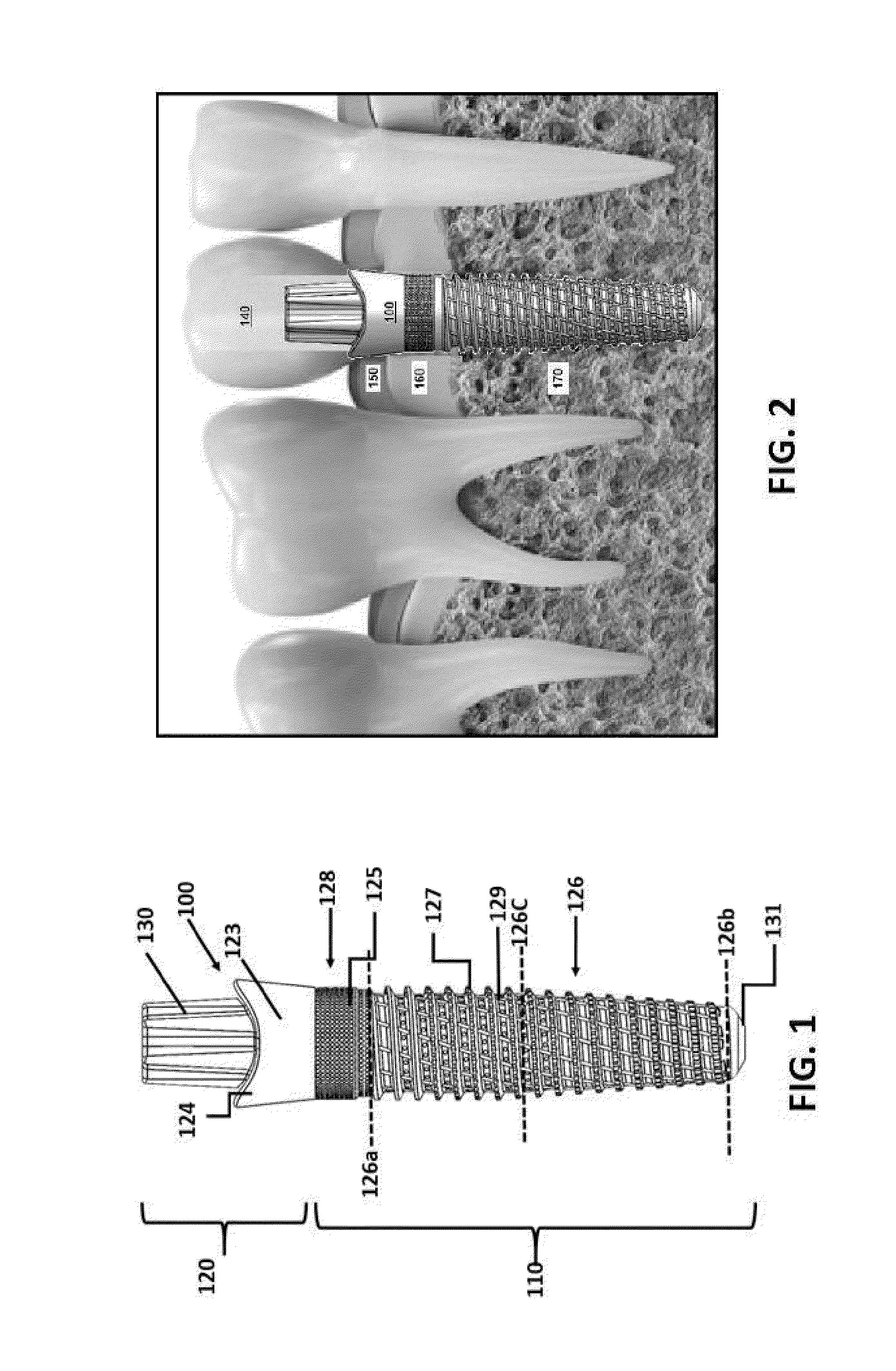
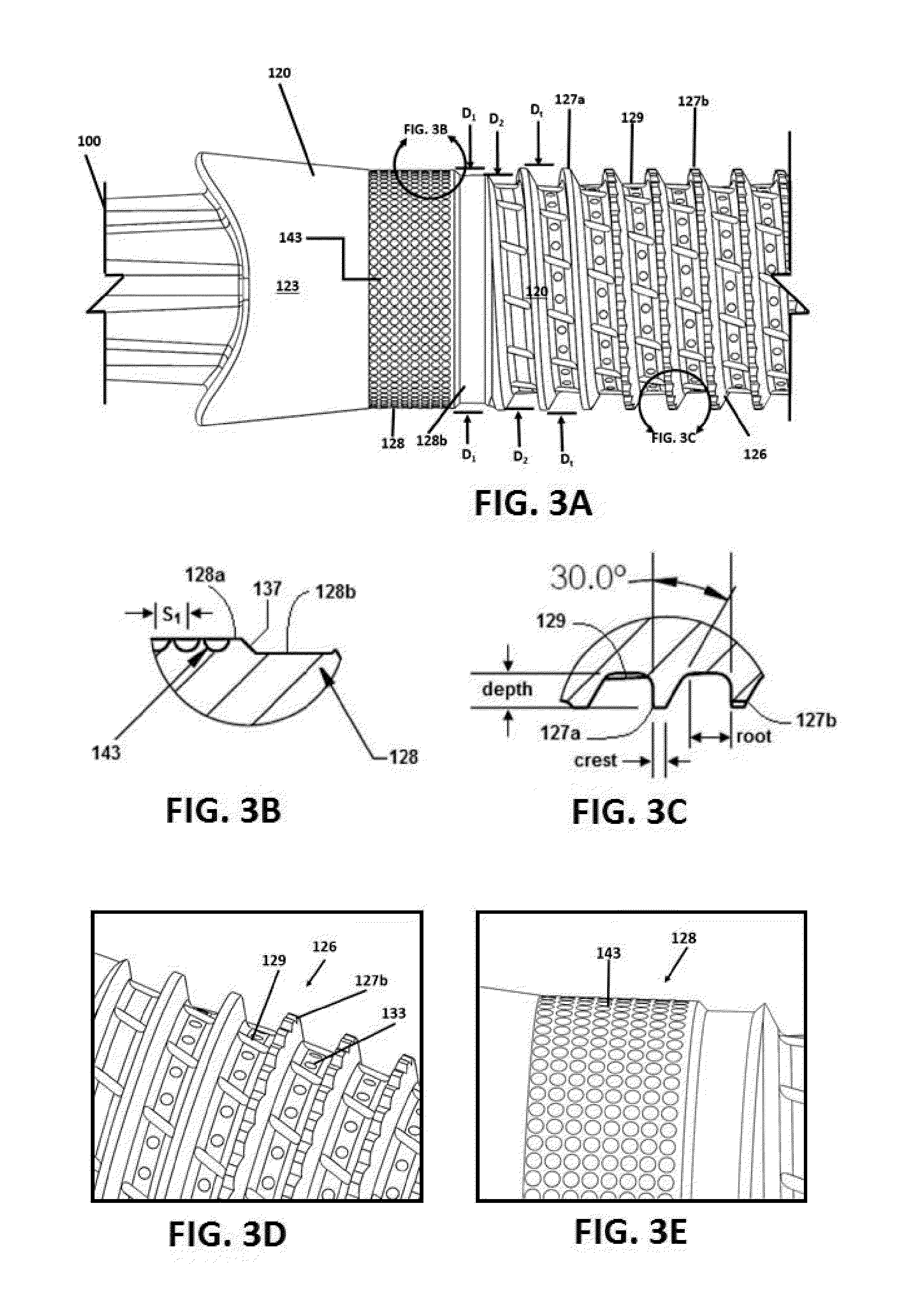
example 1
[0251]A single-stage threaded implant is formed having one or more of the features and geometries as illustrated and described above in connection with FIGS. 1-8. The implant is formed by conventional machining and / or grinding of a solid cylinder of pure titanium or titanium alloy material.
example 2
[0252]A single-stage press-fit implant is formed having one or more of the features and geometries as illustrated and described above in connection with FIGS. 11A-C. The implant is formed by conventional machining and / or grinding of a solid cylinder of pure titanium or titanium alloy material.
example 3
[0253]A two-stage threaded ceramic implant is formed having one or more of the features and geometries as illustrated and described above in connection with FIGS. 9-10. At least one portion of the implant is formed by conventional machining and / or grinding of a solid cylinder of pure titanium, titanium alloy or stainless steel material. At least the outer bone-engaging portion of the implant is formed by densely sintering a ceramic green body formed by slip casting, powder compacting or injection molding a ceramic feedstock comprising 3 mol % yttria-stabilized powdered zirconia having an average particle size of about 0.16 μm.
PUM
| Property | Measurement | Unit |
|---|---|---|
| particle size | aaaaa | aaaaa |
| particle size | aaaaa | aaaaa |
| temperature | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com