Administration of “standard acceptable dosages” to patients with potentially unstable
physiology can produce an insidious and deadly occurrence of relative
drug excess, which will not be prevented by simple computer matching of
patient name and
drug.
Further, the present nventors recognized that failure to timely interrupt infusion upon the occurrence of physiologic
instability represented a major
cause of death.
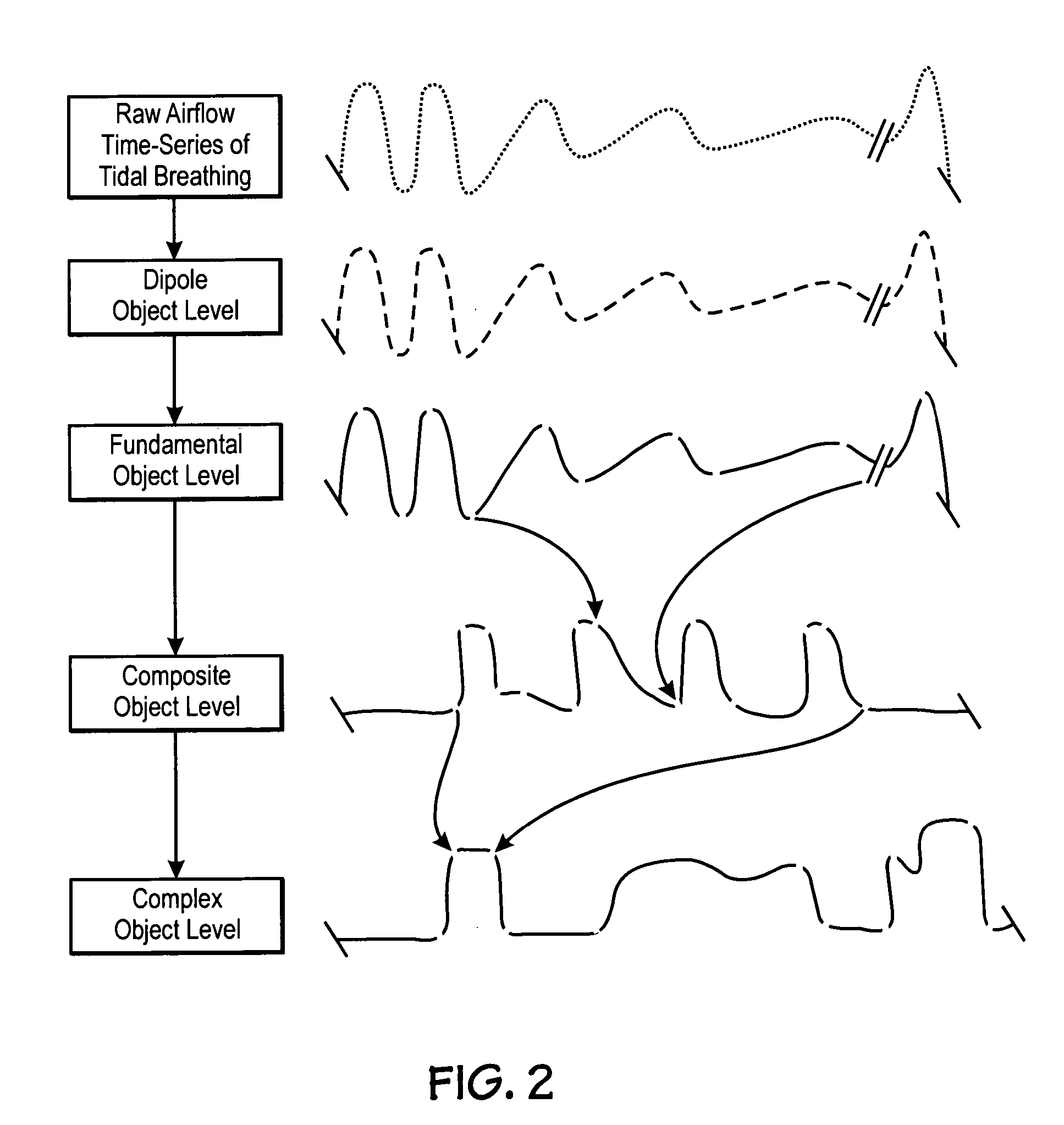
In hospitals, throughout the United States monitored patients are experiencing profound physiologic
instability before and during
medication infusion producing patterns as shown in FIG. 2 and yet still are being subjected to
continuous infusion of further destabilizing and potentially deadly narcotics and
sedation simply because the hospital monitors do not recognize the patterns nor are they programmed to warn the hospital worker or to lock out the infusion based on such recognition.
Subgroups of patients in the hospital are at considerable risk from this type of instability.
In addition patients with otherwise relatively stable airways may have instability induced by sedation or narcotics.
For these reasons thousands of patients each day enter and leave hospital-monitored units with unrecognized
sleep apnea and ventilation and airway instability.
This failure of conventional
hospital based patient monitors to timely and / or automatically detect cluster patterns indicative of airway instability can be seen as a major health care deficiency indicative of a long unsatisfied need.
Because
obstructive sleep apnea, a condition derived from airway instability, is so common, the consequence of the failure of conventional hospital monitors to routinely recognize upper airway instability clusters means that many of patients with this disorder will never be diagnosed in their lifetime.
A second group of patients will have a complication in the hospital due to the failure to timely recognize airway instability.
Without recognition of the inherent instability, a patient may be extubated too early after
surgery or given too much
narcotic (the right
drug, the right patient, the ordered
dose but unknowingly a “relative drug excess”).
Such a patient may be at particular risk for increased airway instability in association with
narcotic therapy in the through 3rd post-operative day due to
sleep deprivation, airway
edema, and sedation.
Furthermore, in the second and third postoperative day monitoring the vigilance of hospital personnel may diminish due to perceived stability, and rebound rapid
eye movement (REM) sleep which can increase upper airway instability may occur due to antecedent
sleep deprivation.
Indeed, many of these patients have significant
sleep apnea prior to admission to the hospital which is unknown to the surgeon or the anesthesiologist due to the subtly of symptoms.
Such patients, even with severe
sleep apnea, are relatively safe at home because of an intact
arousal response; however, in the hospital, narcotics and sedatives often remove this “
safety net.
The administration of post-operative narcotics can shift the
arousal curve to the right and this can significantly increase the danger of airway instability and, therefore, place the patient at substantial risk.
In addition, simple oximetry evaluation is also a poor method to identify airway instability.
Even when the clustered desaturations occur they are often thought to represent false alarms because they are brief.
When desaturations are recognized as potentially real this often results in the simple and often misguided addition of nasal
oxygen.
However, nasal
oxygen may prolong the apneas and potentially increase functional airway instability.
From a monitoring perspective, the addition of
oxygen therapy can be seen to potentially hide the presence of significant airway instability by attenuation of the level of desaturation and reduction in the effectiveness of the oximeter as a
monitoring tool in the diagnosis of this disorder.
Oxygen and sedatives can be seen as a deadly combination in patients with severely unstable airways since the sedatives increase the apneas and the oxygen hides them from the oximeter.
A fall in
afferent output from the brain controller to the airway dilators results in upper airway collapse.
Alternatively, a fall in
afferent output to the pump muscles causes hypoventilation.
The first and most traditionally considered
potential effect of narcotics or sedation is the suppression by the narcotic or
sedative of the brains
afferent output to pump
muscle such as the diaphragm and chest wall, resulting in inadequate
tidal volume and associated fall in minute ventilation and a progressive rise in
carbon dioxide levels.
However, in the presence of oxygen administration, oximetry is a poor indicator of ventilation.
In addition, patients may have a combined cause of ventilation failure induce by the presence of both upper airway instability and decreased diaphragm output as will be discussed, this complicates the output patterns of CO2 monitors making recognition of evolving
respiratory failure due to hypoventilation more difficult for conventional threshold alarm based systems.
This reduction in airway tone results in dynamic airway instability and precipitates monomorphic cluster cycles of airway collapse and
recovery associated with the arousal response as the patient engages in a recurrent and
cyclic process of arousal based rescue from each airway collapse.
If, despite the development of significant cluster of airway collapse, the narcotic administration or sedation is continued, this can lead to further
prolongation of the apneas, progression to dangerous polymorphic desaturation, and eventual
respiratory arrest.
There is, therefore, a dynamic interaction between suppression of respiratory drive, which results in hypoventilation and suppression of respiratory drive, which results in upper airway instability.
At any given time, a patient may have a greater degree of upper airway instability or a greater degree of hypoventilation.
Unfortunately, this has been one of the major limitations of
carbon dioxide monitoring.
Although breath by breath monitoring may show evidence of
apnea, conversion from nasal to
oral breathing can reduce the ability of the CO2 monitor to identify even severe hypoventilation in association with upper airway obstruction, especially if the
signal is averaged or sampled at a low rate.
For this reason, conventional tidal CO2 monitoring when applied with conventional monitors without out cluster
pattern recognition may be least effective when applied to patients at greatest risk, that is, those patients with combined upper airway instability and hypoventilation.
In addition, the present inventors recognized that the complexity and
time course variability of these patterns commonly overwhelms hospital workers so that timely intervention is often not applied, resulting in unnecessary death or patient injury.
 Login to View More
Login to View More  Login to View More
Login to View More