If
blood flow decreases sufficiently,
kidney function becomes impaired and results in fluid retention, abnormal
hormone secretions and increased
constriction of blood vessels.
This reduced capacity further reduces
blood flow to the kidney, which in turn further reduces the capacity of the blood.
Moreover, the fluid overload and associated clinical symptoms resulting from these physiologic changes are predominant causes for excessive hospital admissions, terrible
quality of life and overwhelming costs to the health care
system due to CHF.
Over years, chronic congestive
heart failure leads to cardiac insufficiency.
Chronic CHF patients may experience an abrupt, severe deterioration in heart function, termed Acute Congestive
Heart Failure, resulting in the inability of the heart to maintain sufficient
blood flow and pressure to keep vital organs of the body alive.
These acute CHF deteriorations can occur when extra stress (such as an infection or excessive fluid overload) significantly increases the
workload on the heart in a stable chronic CHF patient.
In case of renal
disease, some normal and important physiological functions become detrimental to the patient's health.
In the case of
Chronic Renal Failure (CRF) patients overcompensation often manifests in hypertension (pathologically high
blood pressure) that is damaging to heart and blood vessels and can result in a
stroke or death.
Without properly functioning kidneys, a patient will suffer
water retention, reduced
urine flow and an accumulation of wastes toxins in the blood and body.
Since measurement of GFR is very cumbersome and expensive, clinically, the
serum creatinine level or
creatinine clearance are used as surrogates to measure kidney function.
Without properly functioning kidneys, a patient will suffer
water retention, reduced
urine flow and an accumulation of wastes toxins in the blood and body.
These conditions resulting from reduced
renal function or renal failure (kidney failure) are believed to increase the
workload of the heart.
In a CHF patient, renal failure will cause the heart to further deteriorate as the water build-up and blood toxins accumulate due to the poorly functioning kidneys and in turn, cause the heart further harm.
In chronic heart failure, these same responses that initially aided survival in acute heart failure can become deleterious.
Without sufficient
urine output, the body retains fluids and the resulting fluid overload causes
peripheral edema (swelling of the legs), shortness of breath (from fluid in the lungs), and fluid in the
abdomen, among other undesirable conditions in the patient.
Heart failure and the resulting reduction in blood pressure reduces the blood flow and
perfusion pressure through organs in the body, other than the kidneys.
Disturbances in the heart's pumping function results in decreased
cardiac output and diminished blood flow.
This leads to fluid retention by the kidneys and formation of
edema causing fluid overload and
increased stress on the heart.
While in the short term, these commands can be beneficial, if these commands continue over hours and days they can jeopardize the persons life or make the person dependent on
artificial kidney for life by causing the kidneys to cease functioning.
When the kidneys do not fully filter the blood, a huge amount of fluid is retained in the body resulting in
bloating (fluid in tissues), and increases the workload of the heart.
The brain and heart cannot sustain low
perfusion for any substantial period of time.
A
stroke or a cardiac arrest will result if the blood pressure to these organs is reduced to unacceptable levels.
The
disease is progressive, and as of now, not curable.
The limitations of
drug therapy and its inability to reverse or even arrest the deterioration of CHF patients are clear.
Surgical therapies are effective in some cases, but limited to the end-stage
patient population because of the associated risk and cost.
Widespread use of implantable electric pacemakers resulted in prolonged productive life for millions of cardiac patients.
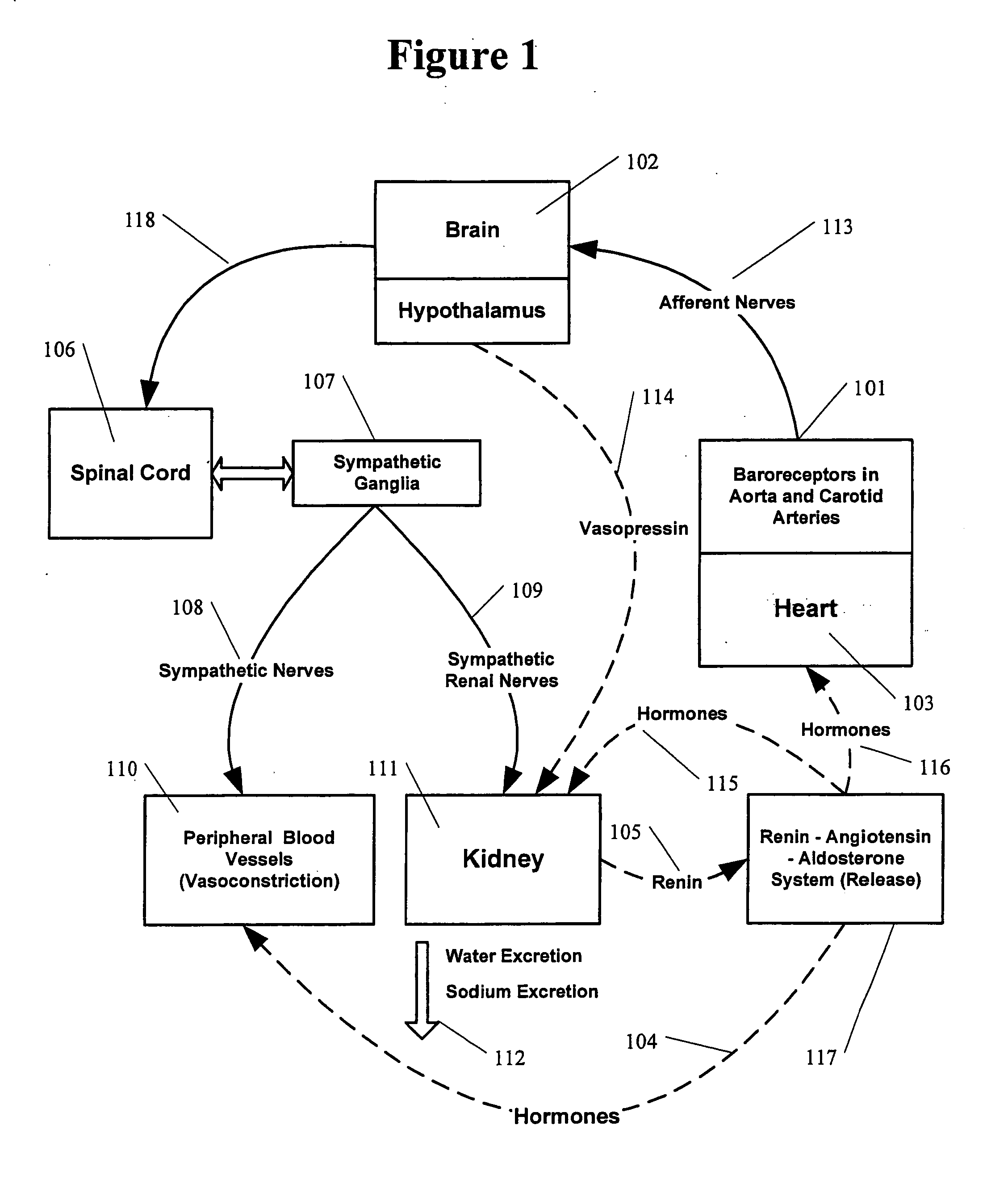
It was established in animal models that the heart failure condition results in the abnormally high sympathetic stimulation of the kidney.
Nevertheless the normal
baroreflex alone, cannot be responsible for the elevated
renal nerve activity in chronic CHF patients.
Therefore, in chronic CHF patients the components of the
autonomic nervous system responsible for the control of blood pressure and the
neural control of the kidney function become abnormal.
The exact mechanisms that cause this
abnormality are not fully understood but, its effects on the overall condition of the CHF patients are profoundly negative.
The primary cause of these problems is the slow relentless progression of
Chronic Renal Failure (CRF) to ESRD.
While some progress has been made in combating the progression to and complications of ESRD in last two decades, the clinical benefits of existing interventions remain limited with no new
drug or device therapies on the
horizon.
Eventually, however, the increasing numbers of nephrons “overworked” and damaged by hyperfiltration are lost.
At some point, a sufficient number of nephrons are lost so that normal GFR can no longer be maintained.
These
pathologic changes of CRF produce worsening systemic hypertension, thus high glomerular pressure and increased hyperfiltration.
This
protein is directly toxic to the tubules and leads to further loss of nephrons, increasing the rate of progression of CRF.
This vicious cycle of CRF continues as the GFR drops, with loss of additional nephrons leading to further hyperfiltration and eventually to ESRD requiring
dialysis.
Over time damage to the kidney leads to further increase of
afferent sympathetic signals from the kidney to the brain.
 Login to View More
Login to View More  Login to View More
Login to View More