Scarring due to chemical burns,
missile damage, genetic disorders, radial keratomy, or failed LCAP are leading causes of corneal eye damage.
In particular, failed LCAP is the most
common source of vision loss due to corneal damage.
Refractive complications can include too much or too little correction, or an imbalance in correction between the eyes.
In some cases, patients who experience improper LCAP may be left near or farsighted or with
astigmatism, necessitating spectacles or
contact lens wear, or in severe cases, may be faced with
blindness.
However, all ophthalmologists readily admit, in their FDA-mandated informed consent that not everyone sees well enough after a LCAP procedure to truly eliminate their use of glasses and contact lenses.
In fact, studies have shown that over 2 percent of LCAP patients experience degradation in
visual acuity that was uncorrectable through refractive means.
This is particularly troublesome since, unlike
cataract surgery, which restores vision in defective eyes, LCAP is an elective process practiced on healthy eyes.
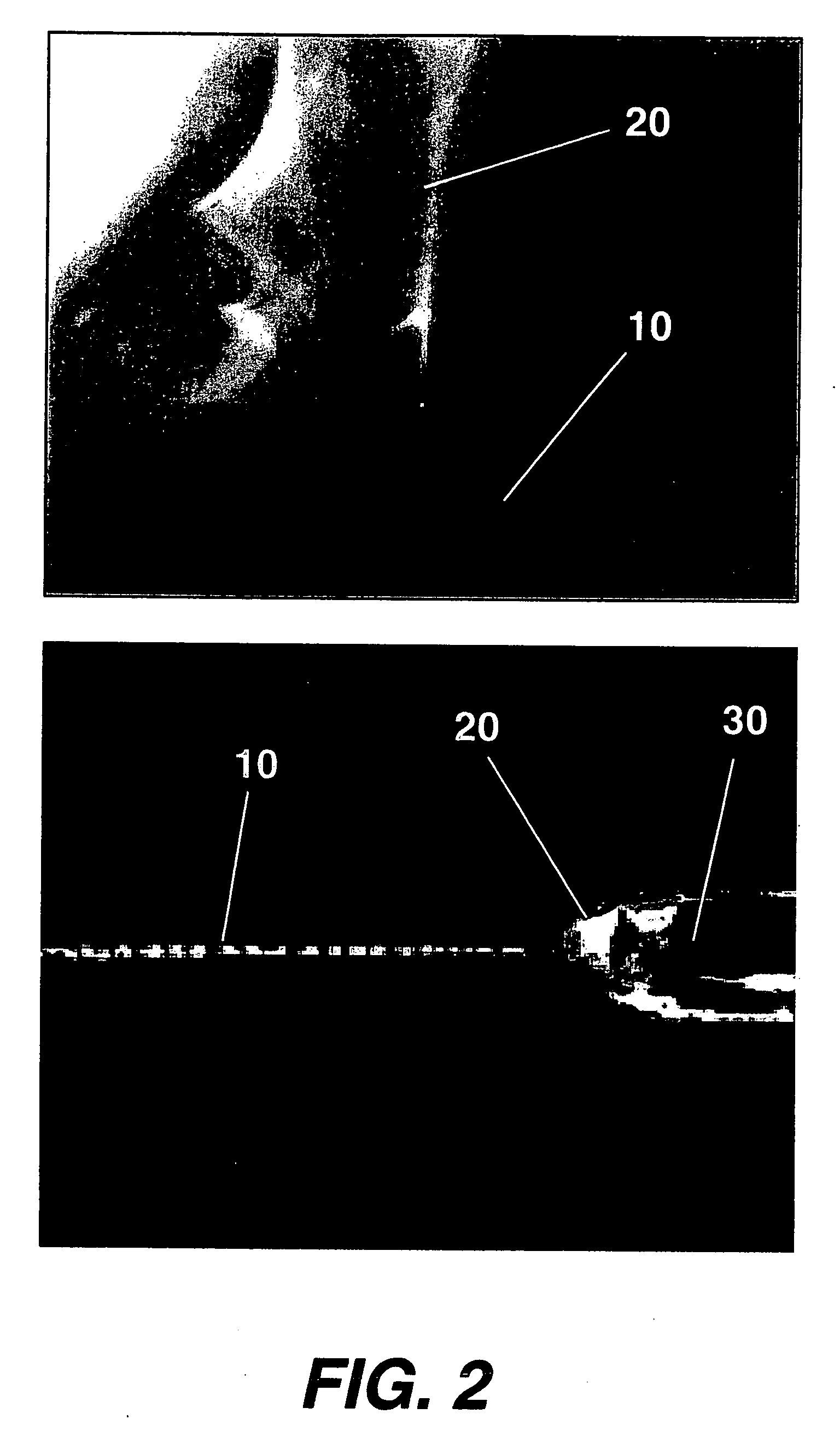
Further, intraoperative complications include decentered ablations and flap complications, such as a partial or lost flap.
Previous attempts to correct the corneal structure to alleviate the aforementioned conditions have been hampered by the fact that only a fixed quantity of tissue is available for ablative modification.
Replacement tissue is not available due to the fact that no other part of the body has the specialized
collagen fibril structure inherent in the
cornea.
However, problems of tissue rejection, of immunosuppressive medication, gross refractive errors, and limited supplies of suitable
donor tissue hamper transplants.
While numerous experiments have been conducted in an effort to create laboratory-grown corneal tissue
in vitro, the drawback of most of these methods is that they attempt to generate only one type of
corneal cell structure, such as the epithelial or endothelial
layers.
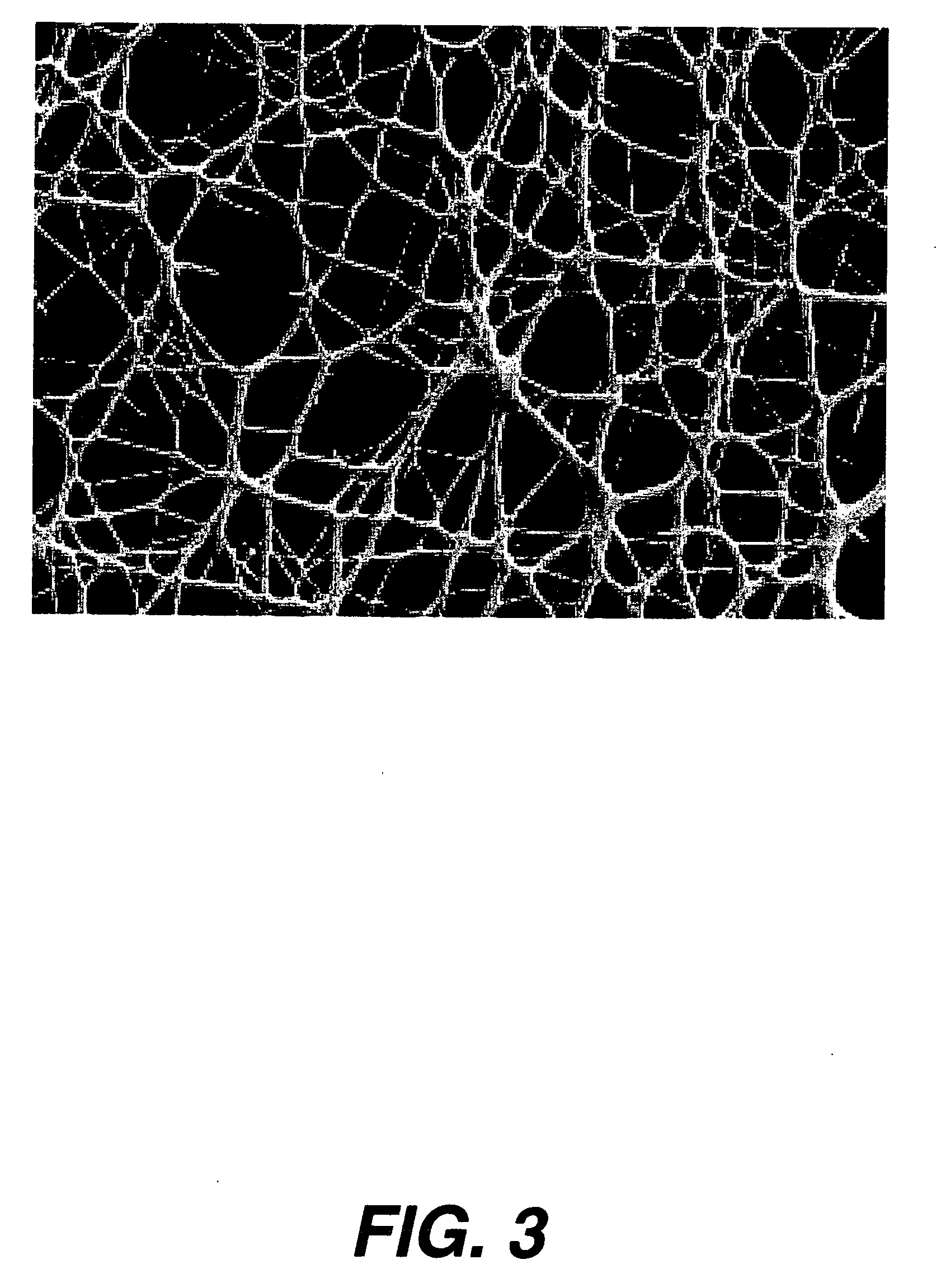
Stromal creation in the laboratory has in the past been met with limited success since no means have been found that successfully form the delicate collagen fibrils with micron sized diameters and
fibril spacing necessary for corneal transparency and diffusive permeability.
Many prior art techniques rely on implanting a
polymer of material (other than collagen or collagen that is devoid of fibrils), thus lacking in permeability as well as transparency inherent in
native tissue.
This concept suffers from the fact that the lack of a controlled
fibril diameter and fibril organizational structure significantly hinders the osmotic pumping of proteins and aqueous media through the fabricated collagen region.
As a result, transparency will be impaired.
Subtle changes in the intraocular pumping mechanism can cause significant loss in
visual acuity.
While providing improvements over simple collagen or other
polymer implants, this suffers from the fact that the polymerized collagenous core does not contain fibrils at all as
native tissue.
As such, the permeability of the
implant is low, thus affecting corneal hydration and overall nutritional levels.
Further, since the collagen source employed can be derived from nonhuman sources, there is a susceptibility to immunologic effects.
While this
coating does improve epithelial adhesion, the problems of lack of diffusibility, optical
clarity, and
foreign body rejection are still present.
This product suffers from the fact that as essentially a simple buffered isotonic
saline solution, it is incapable of rendering any of the structural changes in the
cornea required to correct high
astigmatism,
keratoconus, ectasia, burns, or corneal
thinning.
Further, the solution of Ohuchi and Kato is capable only of yielding temporary
corneal surface relief due to minor, transient optical modifications.
This process repeats itself, leading an uncontrolled ability to deposit material at a precise target and pattern.
Further, the splaying about of the fibers results in tensile forces which varies the
fiber diameter considerably.
However,
cell and vessel in growth are detrimental to a successful corneal
collagen fibril structure and if allowed to transpire, would result in
blindness.
And the lack of such exact fibril specification, uniform diameter, and
matrix pattern would result in reduced
optical transparency of the material and insufficient permeability for ocular use.
 Login to View More
Login to View More