A 3D printed artificial periosteum, artificial bone, artificial bone and preparation method thereof
A 3D printing, artificial bone technology, applied in the field of medical materials, can solve problems such as increased infection risk, application limitation, peripheral fibrosis, etc., to improve mechanical strength and biocompatibility, good histocompatibility and degradability , the effect of promoting degradation and bone remodeling
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment 1
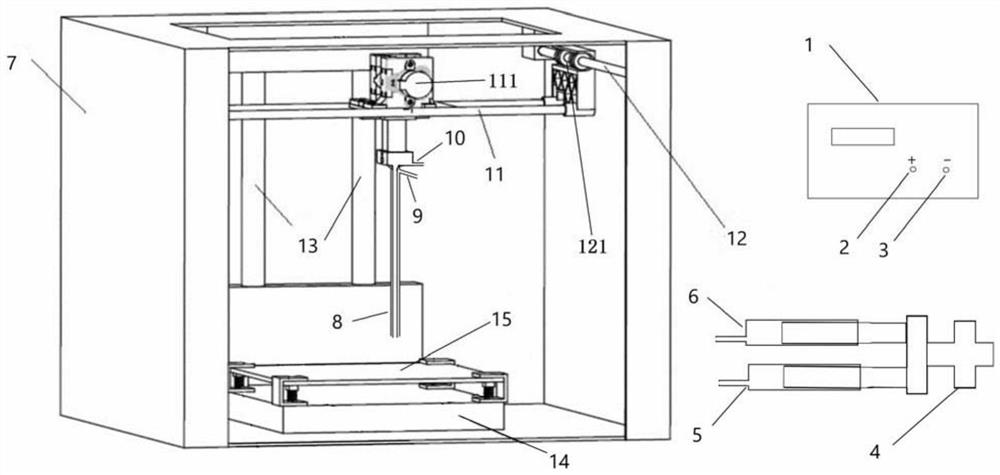
[0070] 1. Preparation of 3D printed artificial bone
[0071] 2g of nanoscale porcine cross-linked collagen fibers, 4g of nanoscale hydroxyapatite and 94g of PLA (Sigma, USA) were used for ultrasonic dispersion respectively, and 120mL of chloroform was added and mixed by mechanical stirring. After mixing uniformly, vacuum freezing Dryer for drying. Then it is crushed by a crusher to form small particles with a particle size of ≤2mm. Finally, a single / twin screw extruder is used to set the temperature of the three zones to be controlled at 160°C, 190°C, and 160°C respectively (extrusion die) for wire production. Manufactured and extruded into a uniform 3D printable linear material with a diameter of 2mm. The performance of the produced wire rod was tested, and the tensile strength was 29.7MPa, the elongation at break was 6.7%, and the tensile modulus was 984MPa.
[0072] When performing bone repair surgery, according to the actual size and shape of the patient's bone defect, t...
Embodiment 2
[0081] 1. Preparation of 3D printed artificial bone
[0082] 3 g of nano-scale porcine cross-linked collagen fibers, 7 g of nano-scale hydroxyapatite and 90 g of PLA (Sigma, USA) were used for ultrasonic dispersion respectively, and 110 mL of chloroform was added and mixed by mechanical stirring. After mixing uniformly, vacuum freezing Dryer for drying. Then it is crushed by a crusher to form small particles with a particle size of ≤2mm. Finally, a single / twin screw extruder is used to set the temperature of the three zones to be controlled at 150°C, 200°C, and 160°C respectively (extrusion die) for wire production. Manufactured and extruded into a uniform linear material with a diameter of 2.0mm for 3D printing. For the produced wire rod, the performance test of the produced wire rod shows that the tensile strength is 35.2MPa, the elongation at break is 6.9%, and the tensile modulus is 1228MPa.
[0083] When performing bone repair surgery, according to the actual size and s...
Embodiment 3
[0091] 1. Preparation of 3D printed artificial bone
[0092] 1 g of nano-scale porcine cross-linked collagen fibers, 2 g of nano-scale hydroxyapatite and 95 g of PLA (Sigma, USA) were used for ultrasonic dispersion respectively, 110 mL of chloroform was added, and mixed by mechanical stirring. After mixing uniformly, vacuum freezing Dryer for drying. Then it is crushed by a crusher to form small particles with a particle size of ≤2mm. Finally, a single / twin screw extruder is used to set the temperature of the three zones to be controlled at 150°C, 180°C, and 150°C (extrusion die) for wire rod production. Manufactured and extruded into a uniform 3D printable linear material with a diameter of 2mm. The performance of the produced wire rod was tested, and the tensile strength was 26.3MPa, the elongation at break was 6.6%, and the tensile modulus was 870MPa.
[0093] When performing bone repair surgery, according to the actual size and shape of the patient's bone defect, the art...
PUM
| Property | Measurement | Unit |
|---|---|---|
| diameter | aaaaa | aaaaa |
| thickness | aaaaa | aaaaa |
| thickness | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com