When the
laser is slowly withdrawn, heat is applied to the
vein walls, causing the
vein to permanently close and disappear.
In patients with Parkinson's
disease, for example, researchers have shown that electrical “
deep brain stimulation” of cells can help patients, but they don't know precisely why.
That could lead to making the electrical treatment, which has some unwanted side effects, more targeted.
The laser systems currently used for
biostimulation do not allow performing photobiomodulation in a region deep within thick tissue without a surgical invasion.
It is further well recognized that another problem associated with the existing methods of photobiomodulation is in differentiation of normal cells from target cells.
The preferential accumulation of PDT
drug molecules in
cancer cells combined with the localized delivery of light to the tumor, results in the selective destruction of the cancerous
lesion.
It is not clear that direct damage to
DNA is a major effect; therefore, this may indicate that photoactivation of
DNA crosslinking is not stimulated efficiently.
Furthermore, when
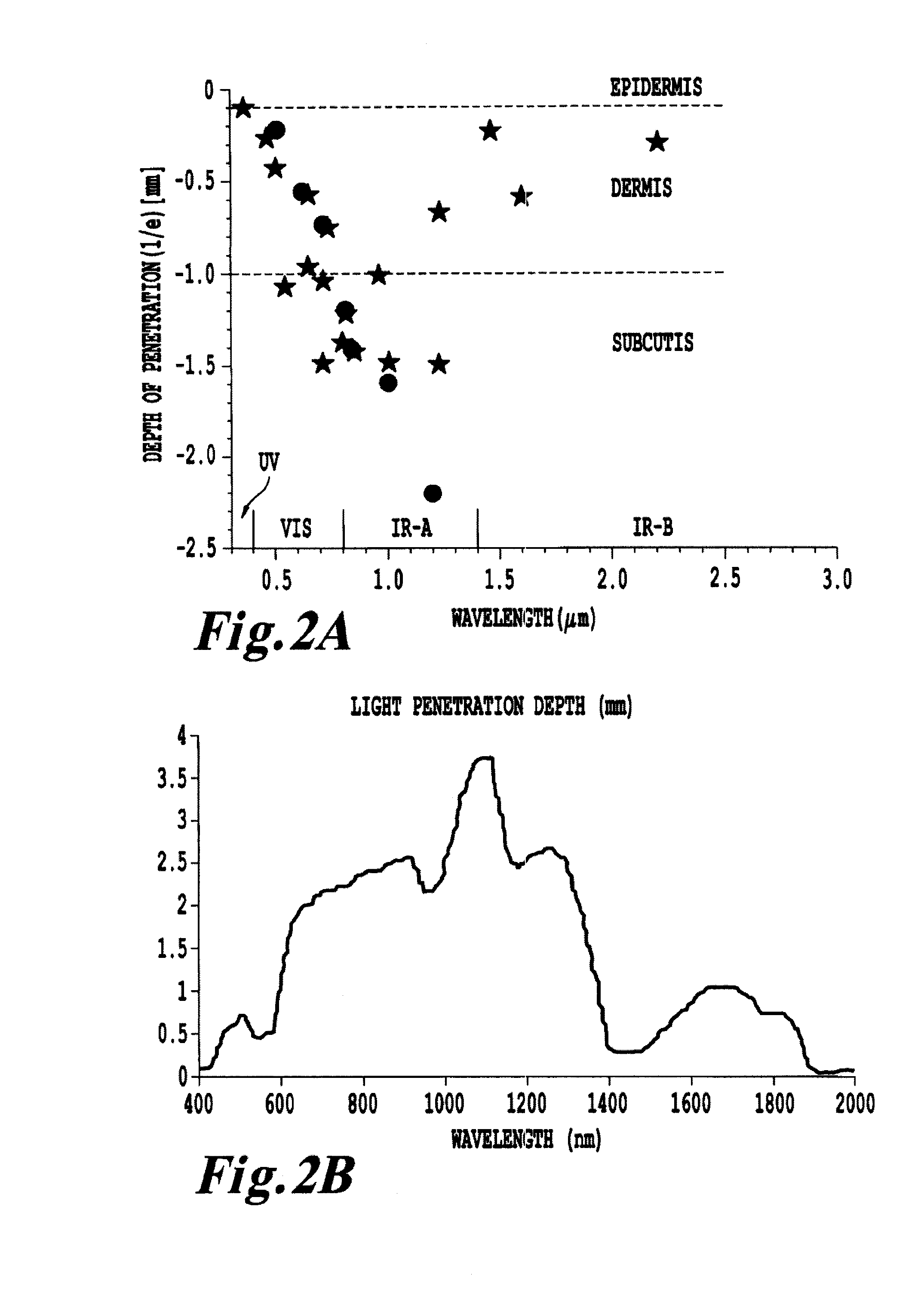
laser light is administered via external illumination of tissue surfaces, the
treatment effect of PDT is confined to a few millimeters (i.e. superficial).
The reason for this superficial limitation is mainly the limited penetration of the visible light used to activate the
photosensitizer.
However, even these treatments require significantly invasive techniques to treat the surface of the affected organs.
It is possible that the
laser light and small amount of remaining microscopic and minimal gross
disease results in too little or highly damaged structures.
It is not clear that direct damage to
DNA is a major effect; therefore, this may indicate that photoactivation of DNA crosslinking is not stimulated efficiently.
However, the percentage of patients eligible for this treatment is limited.
However, given that only a small percentage of the body's lymphocytes; are treated, this seems unlikely to be the only
mechanism of action.
However, there are still many limitations to ECP.
Further, it requires removing typically several hundred milliliters of
whole blood from the patient, hence, the treatment is limited to patients who has sufficiently large initial volume of blood to be withdrawn.
A survey of known treatment methods reveals that these methods tend to face a primary difficulty of differentiating between normal cells and target cells when delivering treatment, often due to the production of
singlet oxygen which is known to be non-selective in its
attack of cells, as well as the need to perform the processes
ex vivo, or through highly invasive procedures, such as
surgical procedures in order to reach tissues more than a few centimeters deep within the subject.
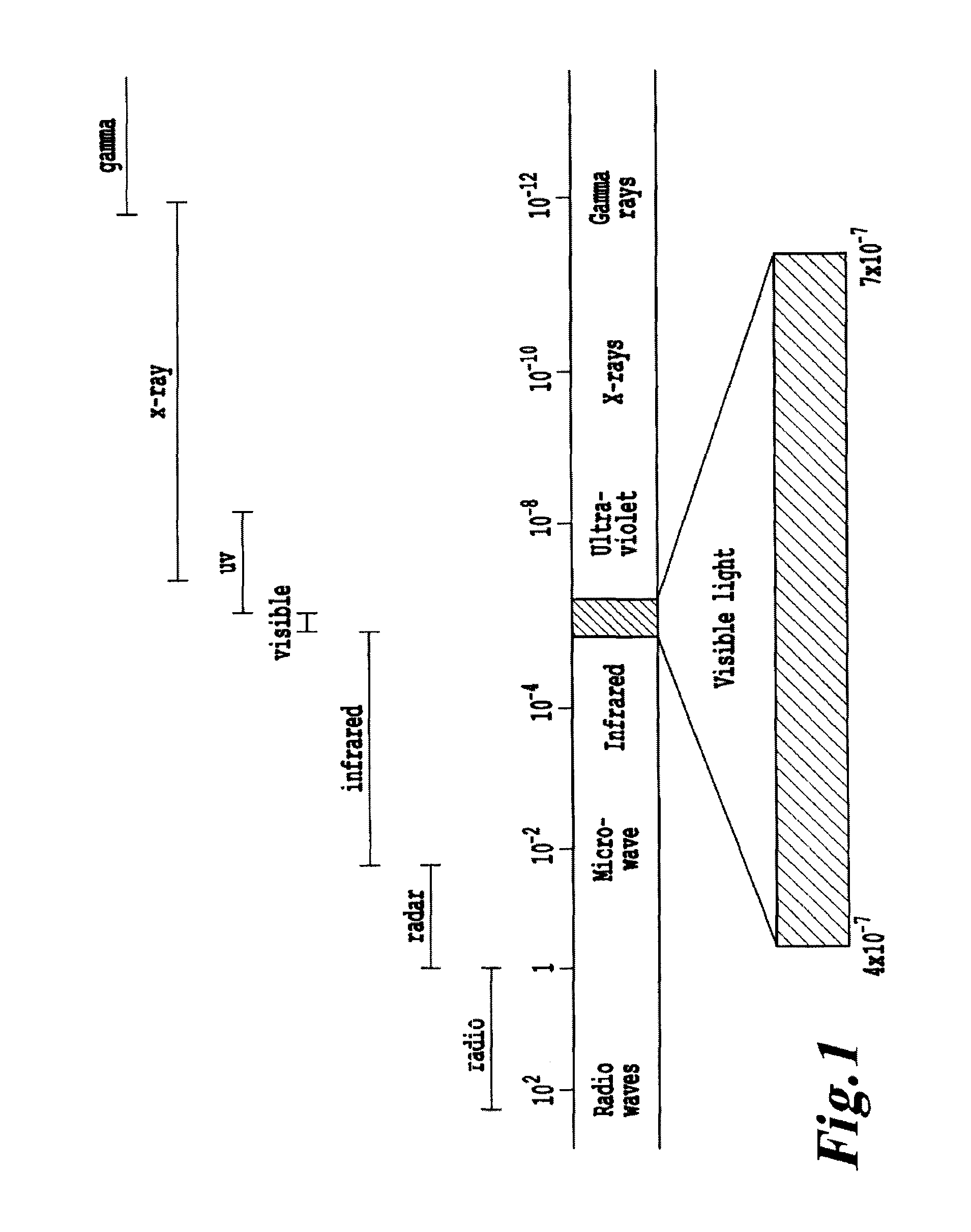
However, the use of NRI or UV
radiation is known to penetrate tissue to only a depth of a few centimeters.
Also, this patent does not describe
initiation energy sources emitting energy other than UV, visible, and near
infrared energy; energy upgrading other than within the range corresponding to UV and IR light, and downgrading from high to low energy.
However, each suffers from the drawback that the treatment is dependent on the production of
singlet oxygen to produce the desired effect on the tissue being treated, and is thus largely indiscriminate in affecting both healthy cells and the diseased tissue desired to be treated.
However, the method is not suitable for treating a patient and does not teach any mechanisms for stimulating the photosensitizers, indirectly.
However, the reference fails to disclose any mechanism of photoactivation using
energy modulation agent that converts the initiation energy to an energy that activates the activatable pharmaceutical agent and also use of other energy wavebands, e.g., X-rays, gamma-rays,
electron beam, microwaves or radio
waves.
However, the reference fails to address any specific molecules for use in treating lymphomas or any other
cancer.
Fluorescing photosensitizers are said to be preferred, but the reference does not teach how to select a
system of fluorescent stimulation or photoactivation using fluorescent photosensitizers.
In addition, the reference teaches that 8-MOP is unsuitable for use as an antiviral, because it damages both cells and viruses.
It is well known that UV activation creates such
reactive oxygen species, which are capable of seriously damaging otherwise healthy cells.
The use of
psoralen and
coumarin photosensitizers can give rise to alternative chemical pathways for dissipation of the
excited state that are either not beneficial to the goal of
viral inactivation, or that are actually detrimental to the process.
Both may lead to inactivating damage of
tumor cells, viruses and healthy cells.
However, neither, alone or combined, lead to an auto vaccine effect.
While the complexity of the immune response and cytotoxic effects is fully appreciated by researchers, a therapy that harnesses the
system to successfully stimulate an auto vaccine effect against a targeted, malignant
cell has been elusive, except for
extracorporeal photopheresis for treating
lymphoma.
U.S. Pat. No. 6,235,508 teaches that 8-MOP and AMT are unacceptable photo sensitizers, because each indiscriminately damages both cells and viruses.
It is well recognized that a major problem associated with the existing methods of diagnosis and treatment of
cell proliferation disorders is in differentiation of normal cells from target cells.
These
high energy beams ionize the atoms which make up
a DNA chain, which in turn leads to cell death.
However, the
high doses of
radiation needed for such therapies damages healthy cells just as effectively as it does diseased cells.
There is no intrinsic means for a
radiation beam to differentiate between a healthy cell from a diseased cell either.
Another problem encountered in PDT therapy is the inability to treat target areas that are more than a few centimeters beneath the surface of the
skin without significant invasive techniques.
 Login to View More
Login to View More  Login to View More
Login to View More