Patents
Literature
92results about "Instrument probes" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
Intralumenal contact sensor
InactiveUS6942657B2Eliminate aberrant wave conductionReduce lossDiagnosticsCatheterLight treatmentLaser light
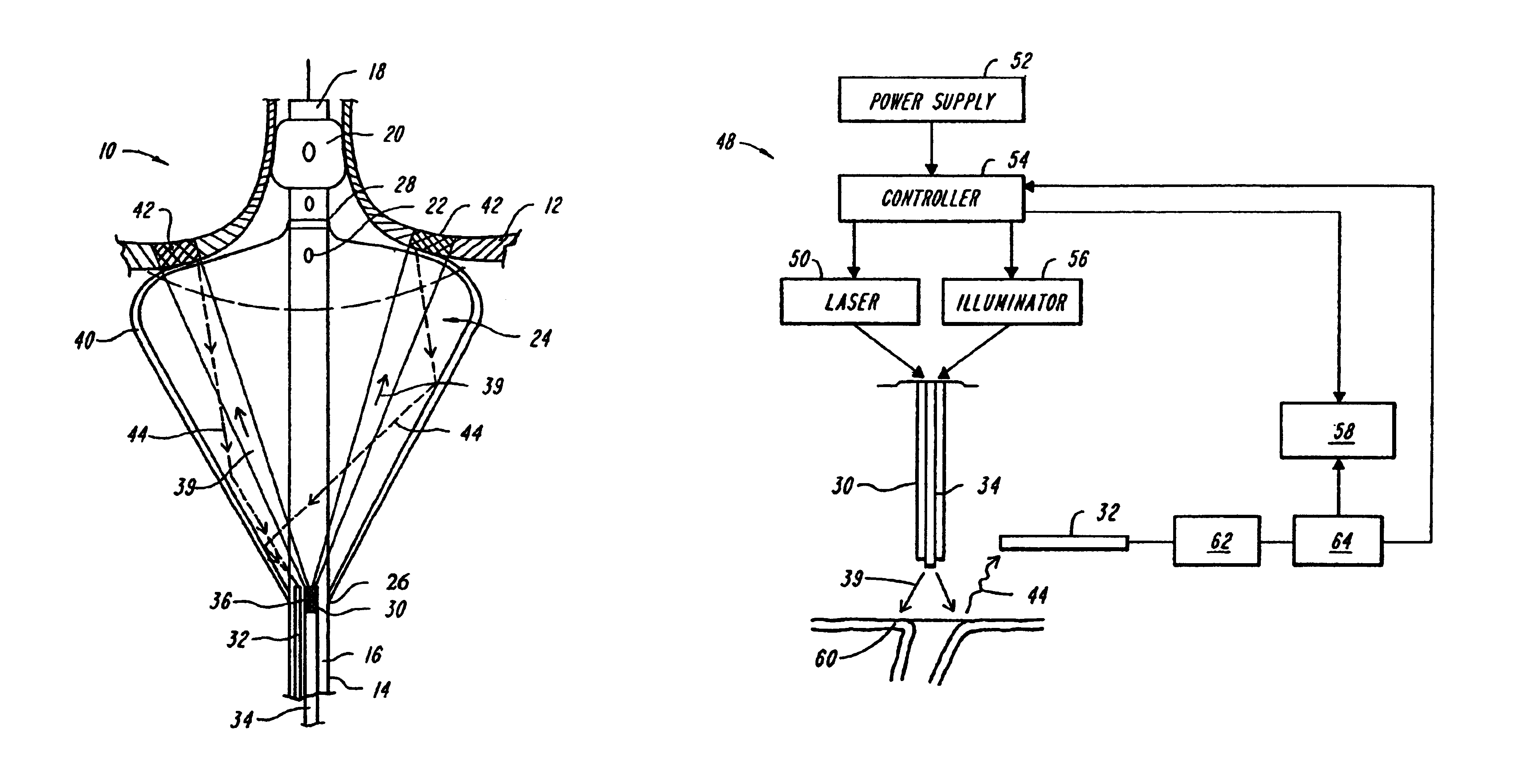
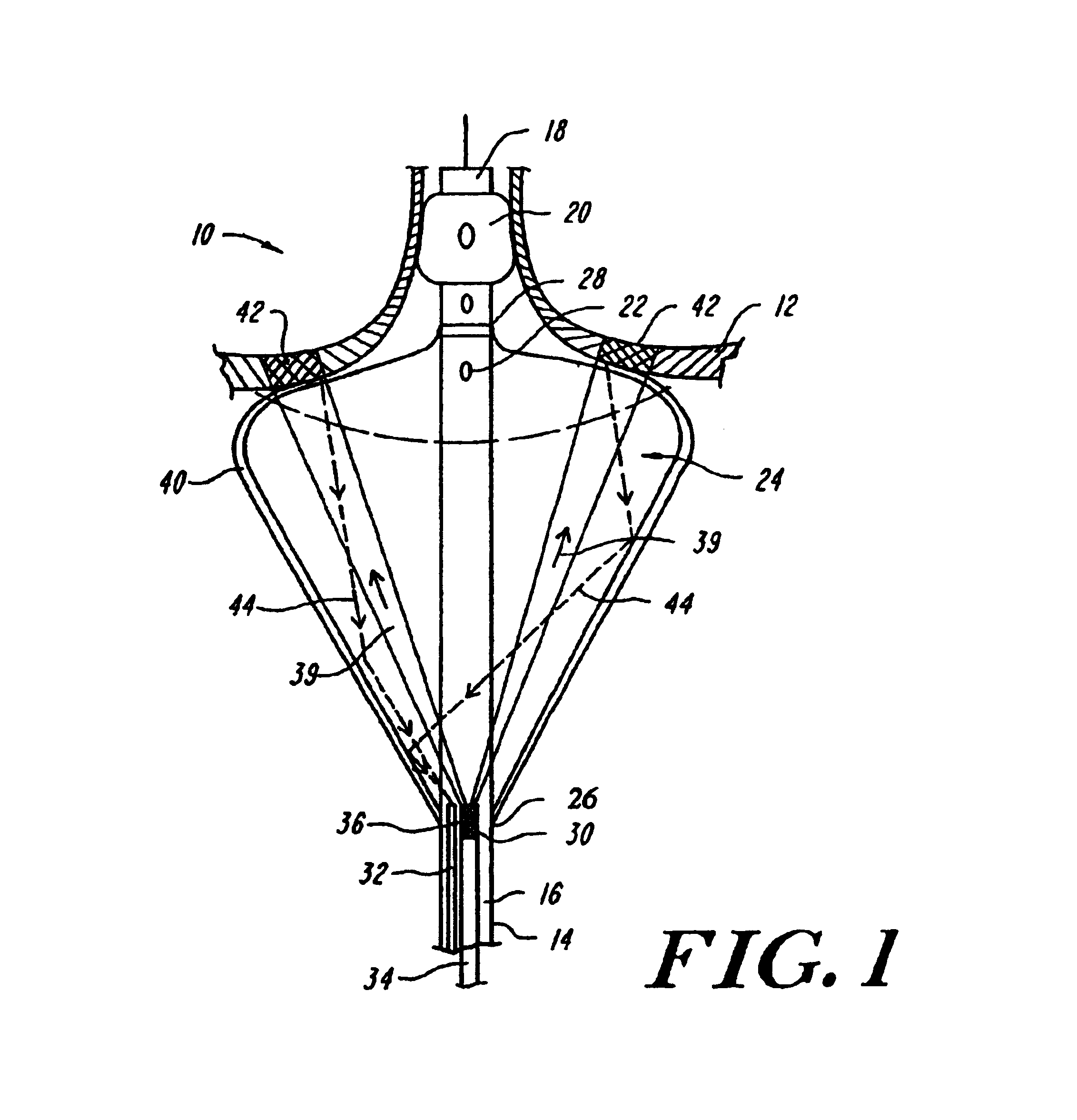
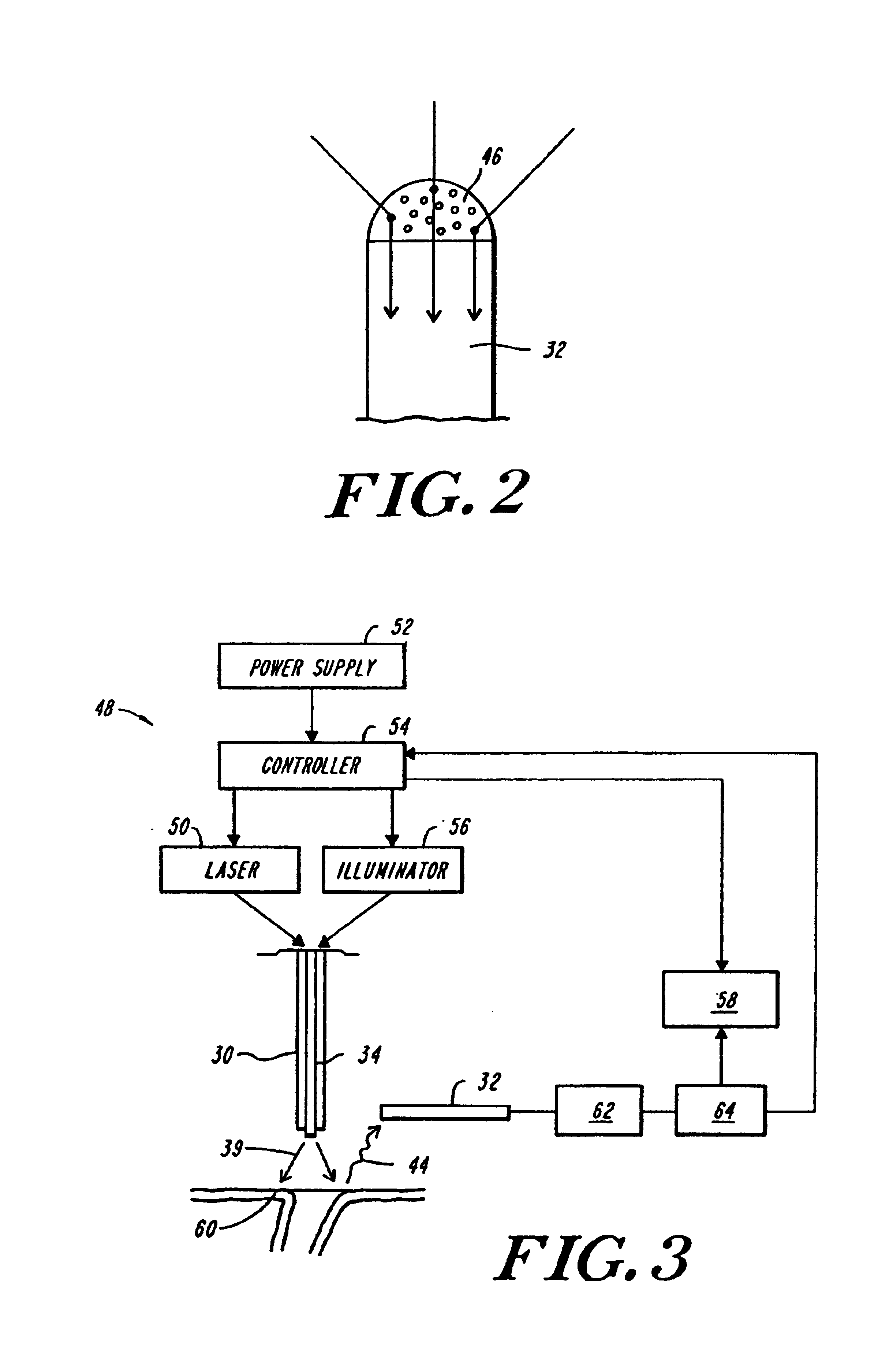
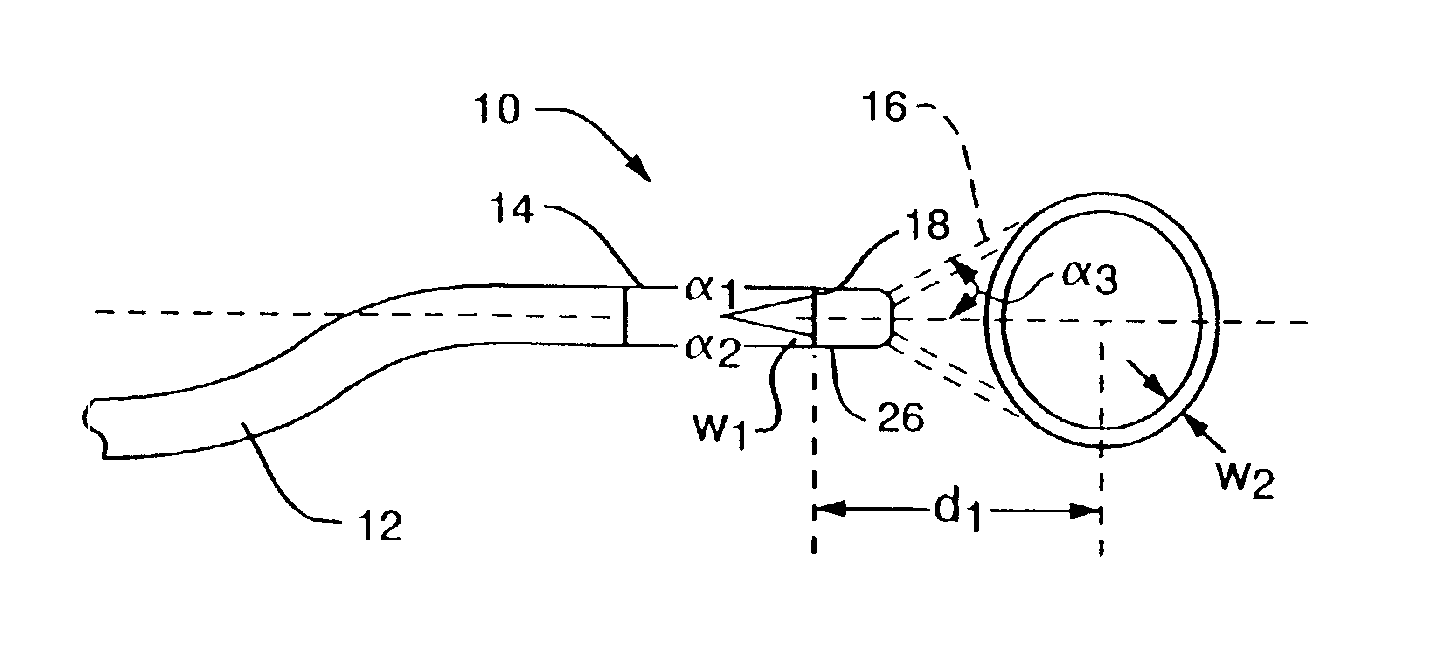
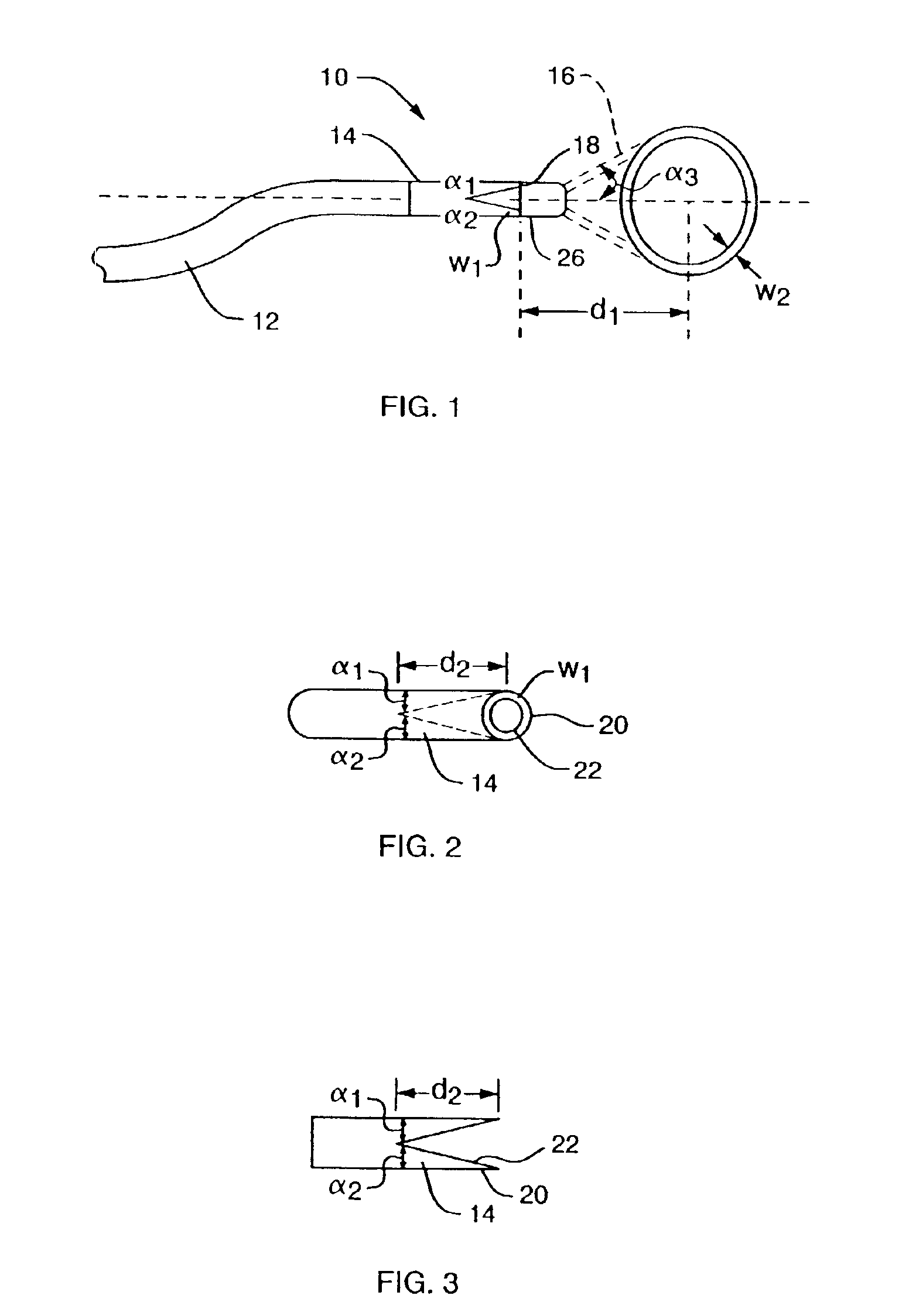
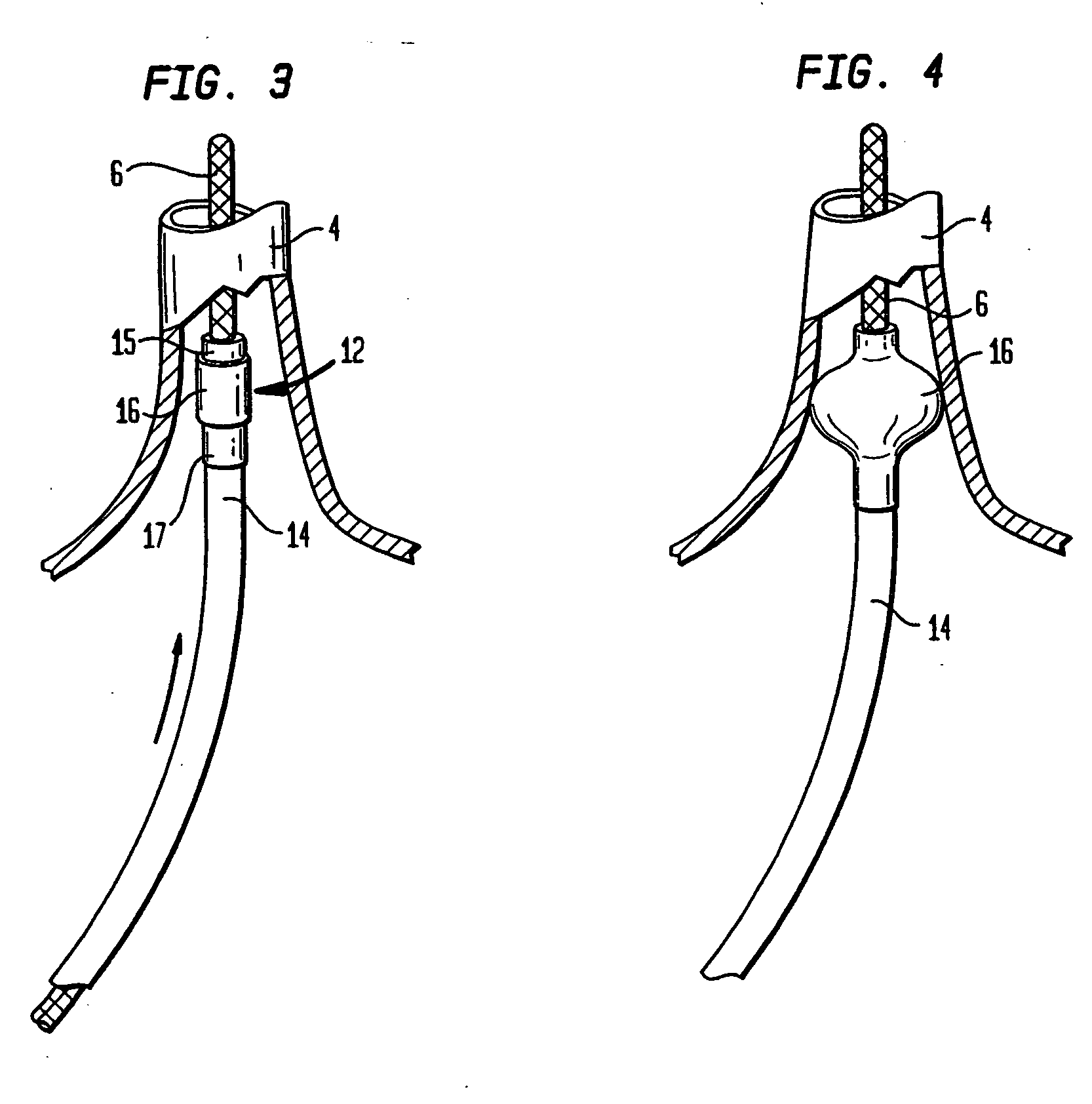
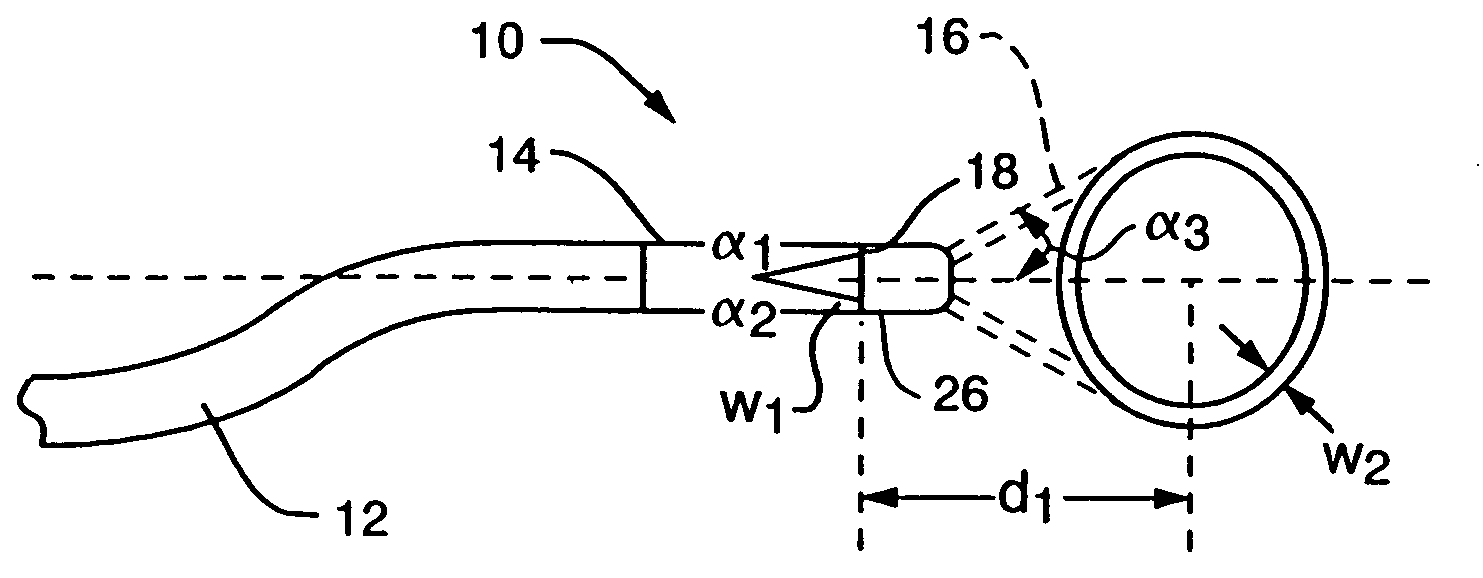
An apparatus and method for phototherapy are described in which laser light or other radiation is projected from within a catheter, through a balloon member, and toward the surface of tissue. The light reflected from body fluids or the tissue surface is captured by a collecting device located within the catheter, e.g., within the balloon member, and the intensity of the reflected light is ascertained. The apparatus and method provides for accurately positioning the apparatus against the tissue treatment site.
Owner:CARDIOFOCUS INC
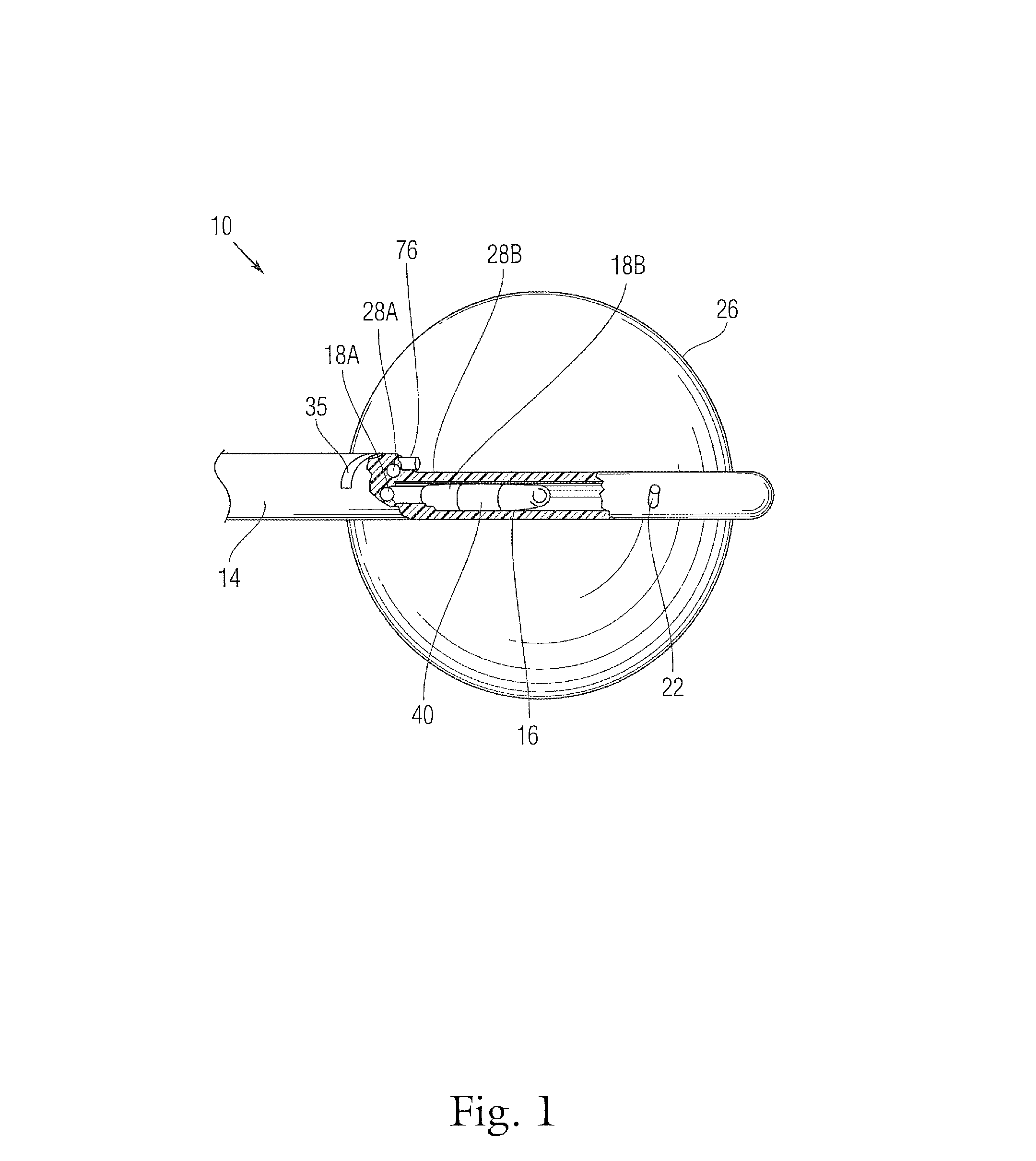
Coaxial catheter instruments for ablation with radiant energy
InactiveUS20050038419A9Rapid and effective photoablationLess timeStentsUltrasound therapyCoaxial catheterTarget tissue
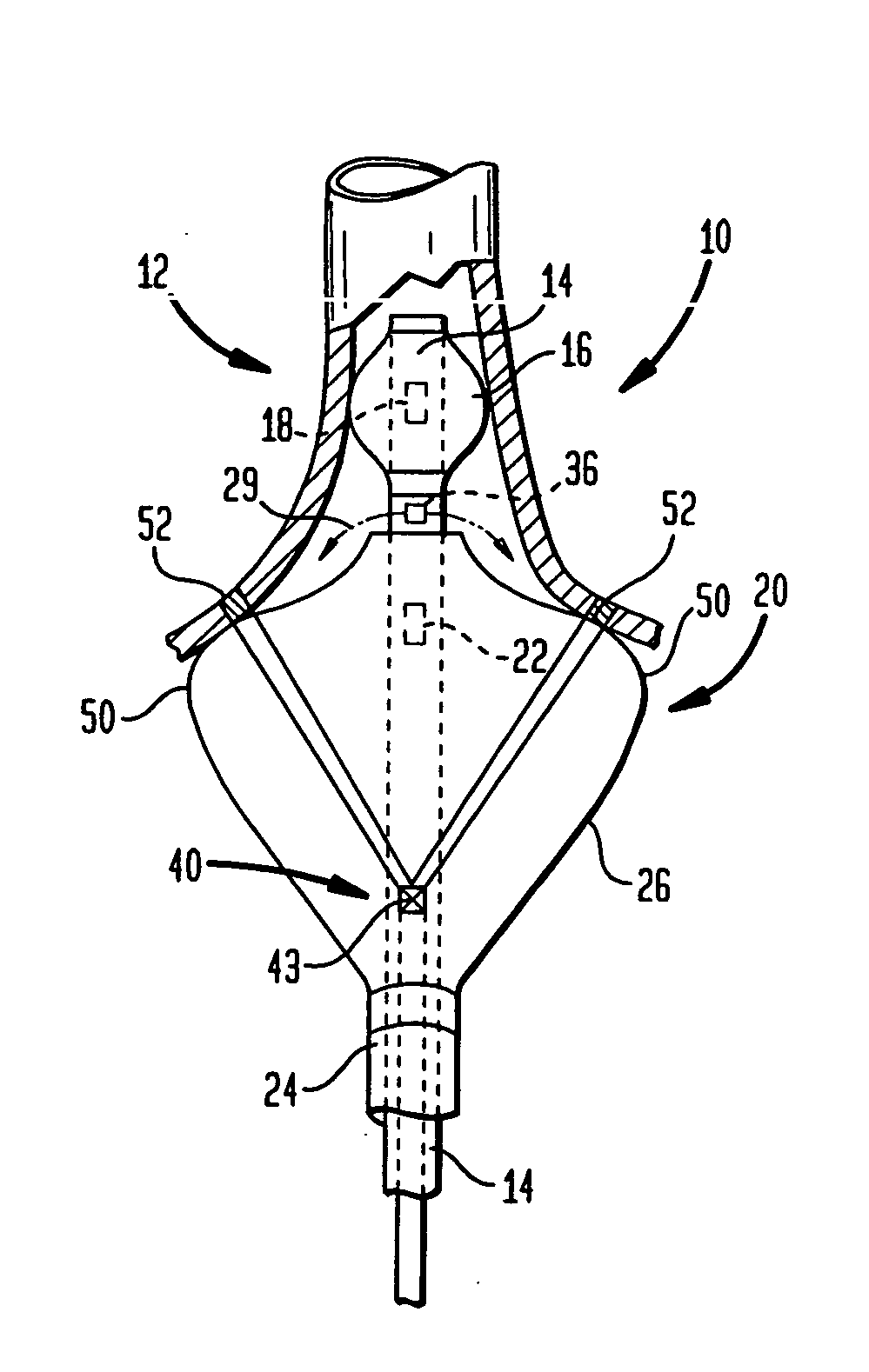
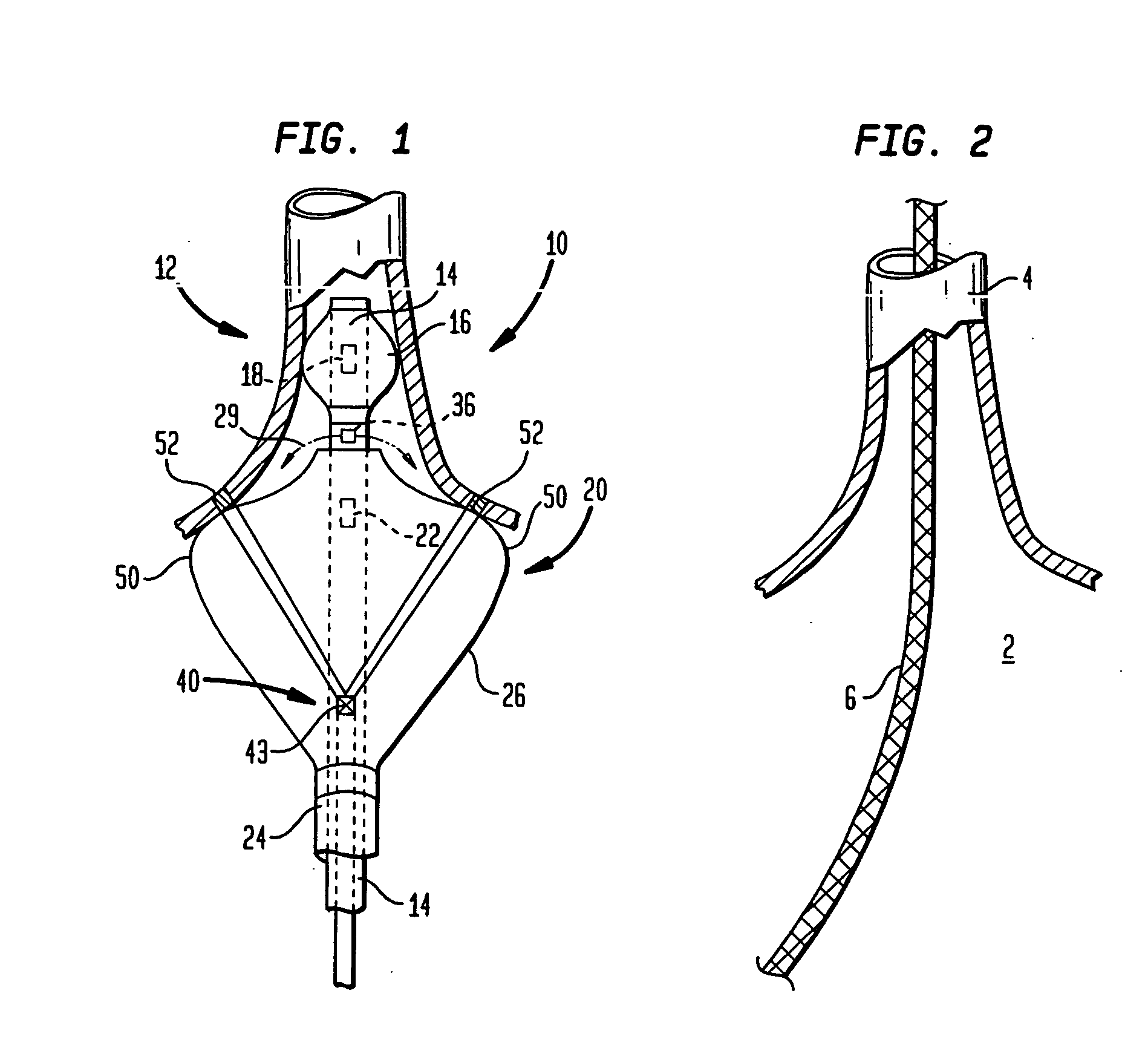
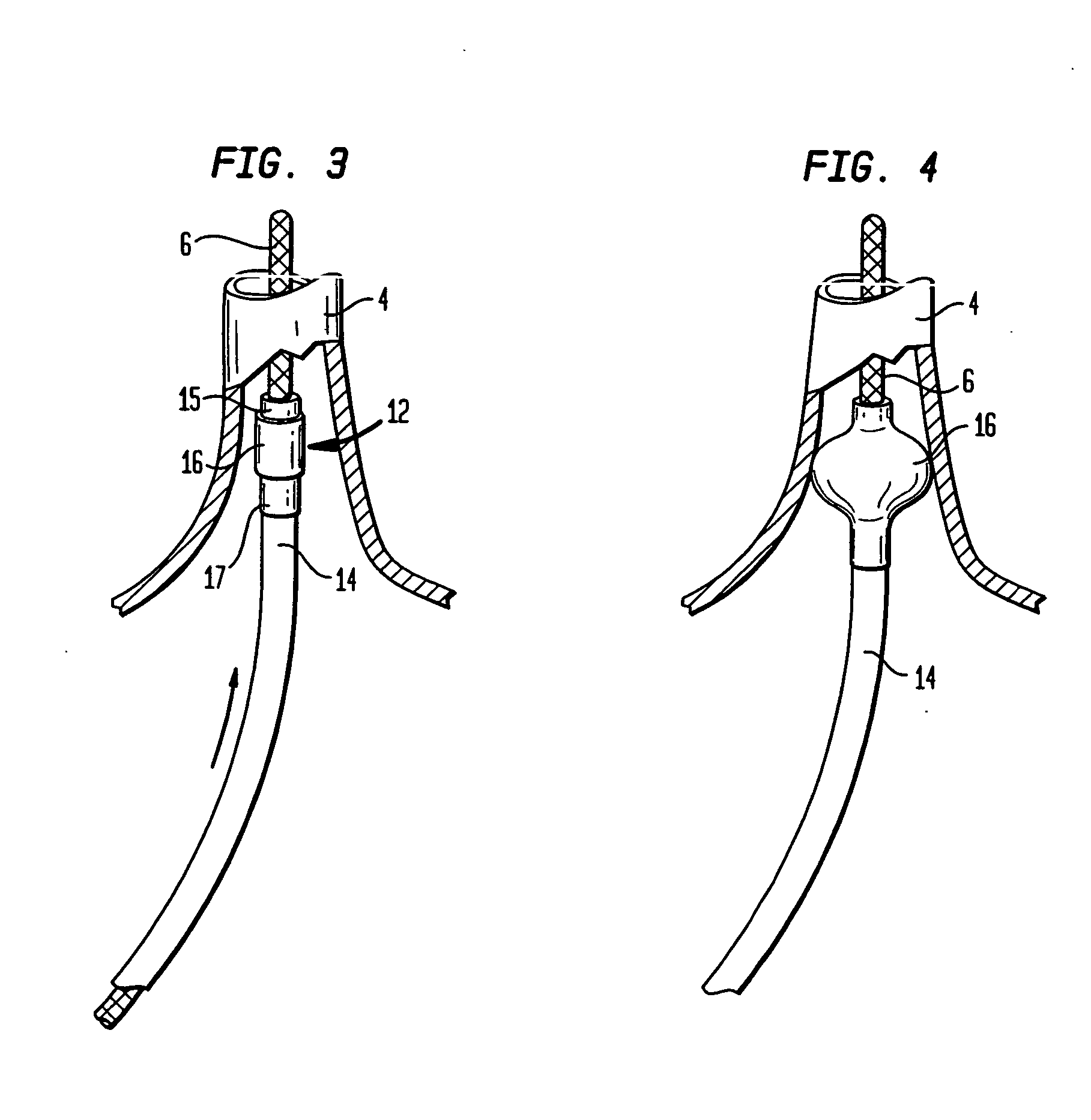
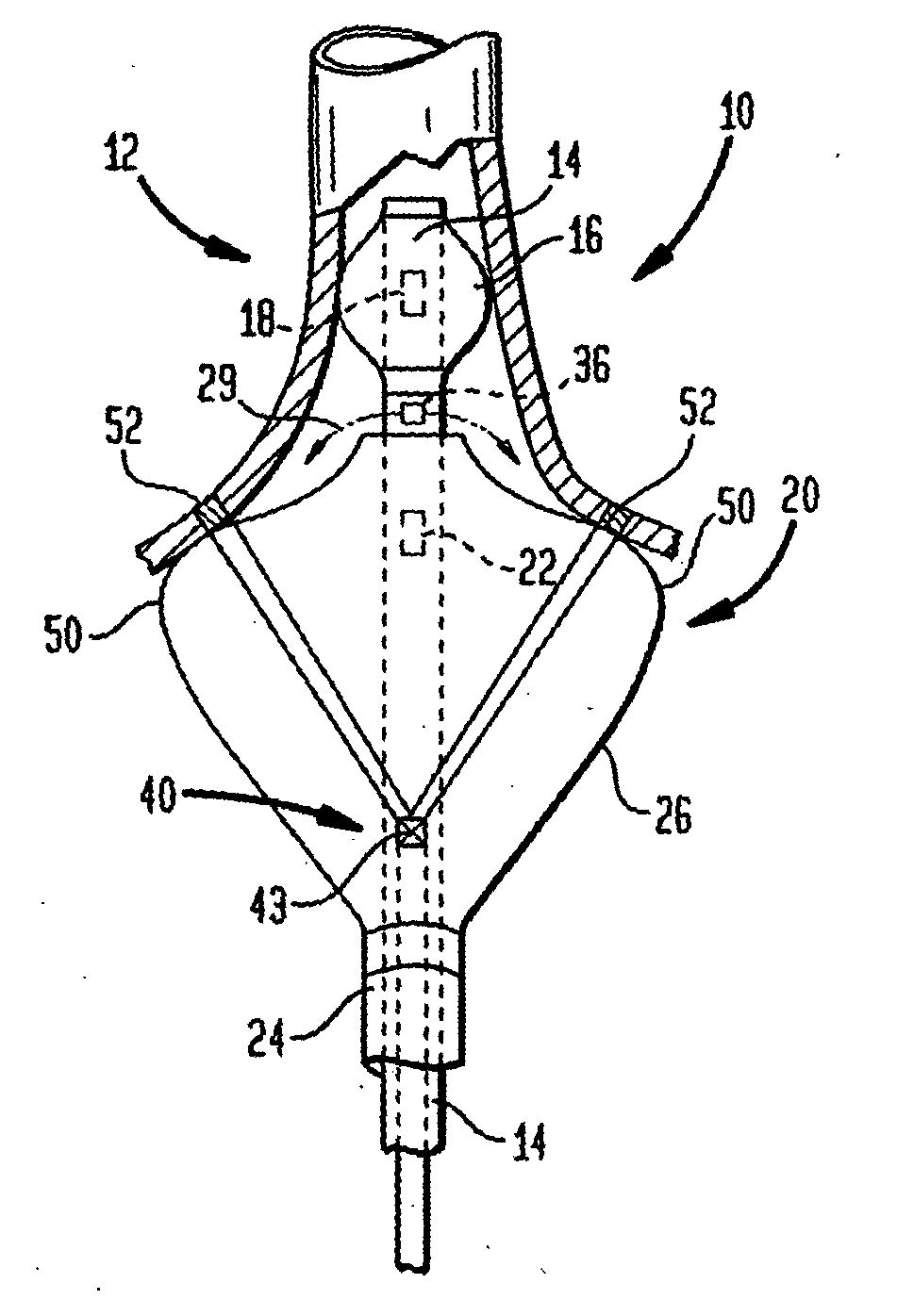
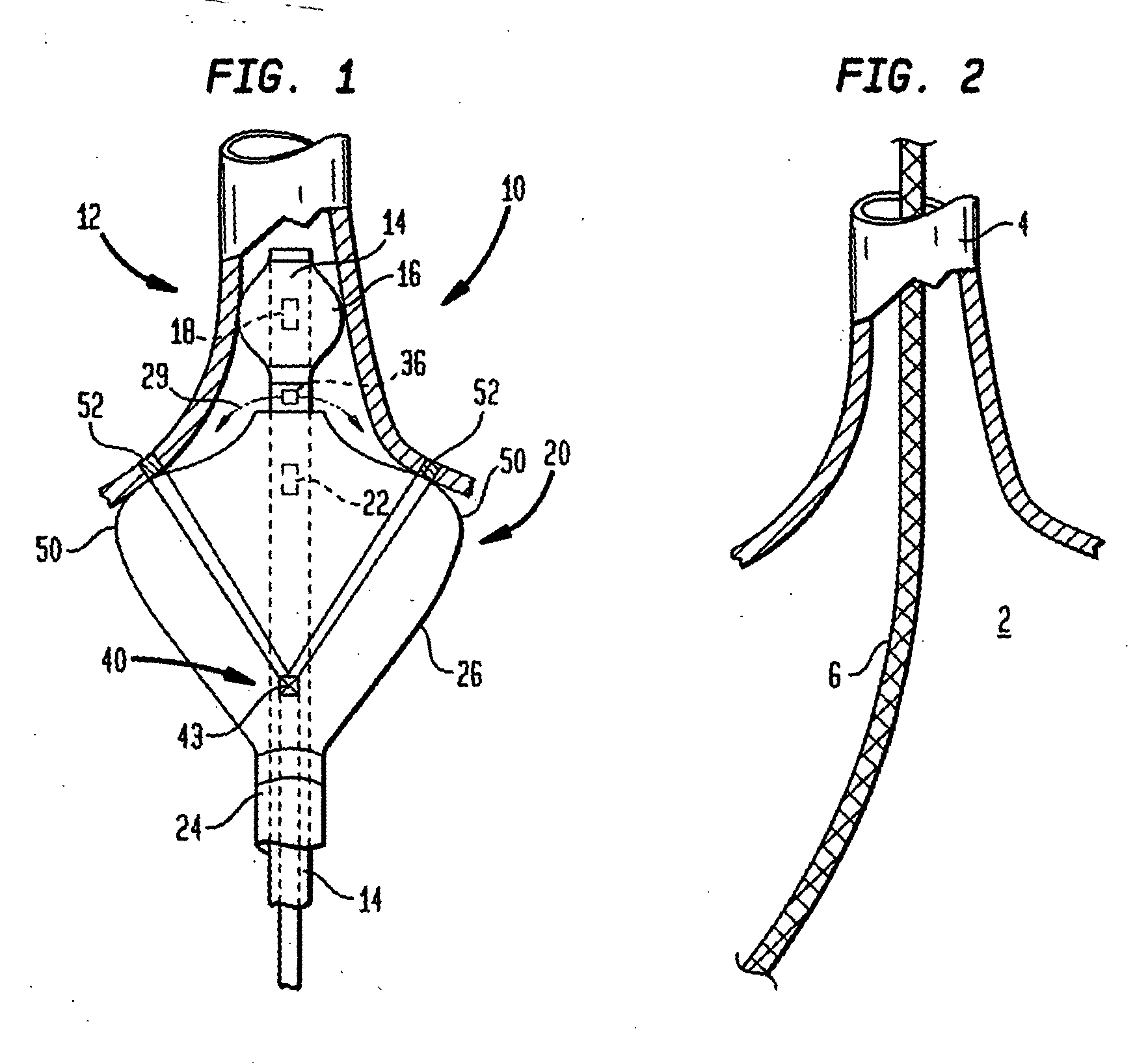
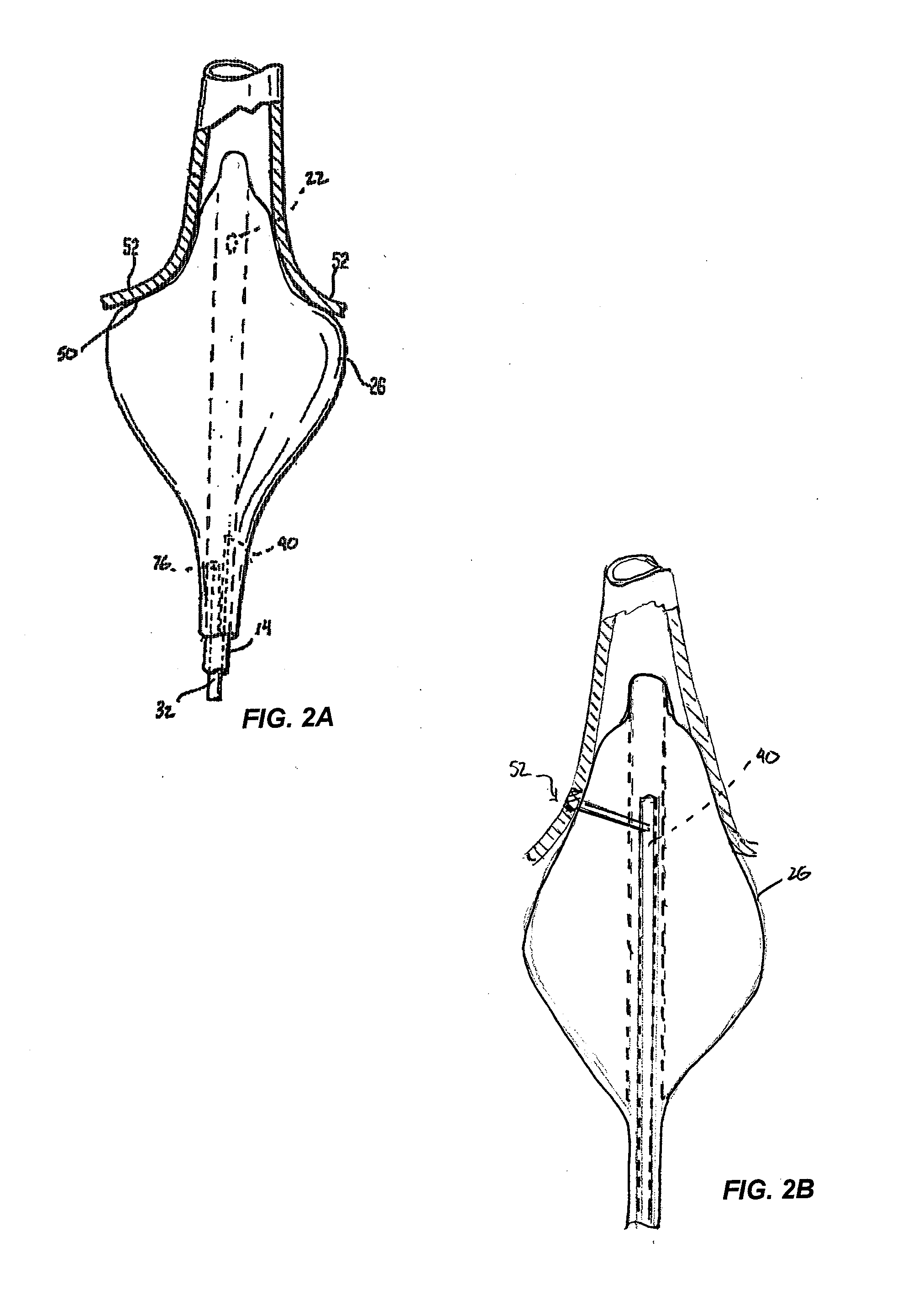
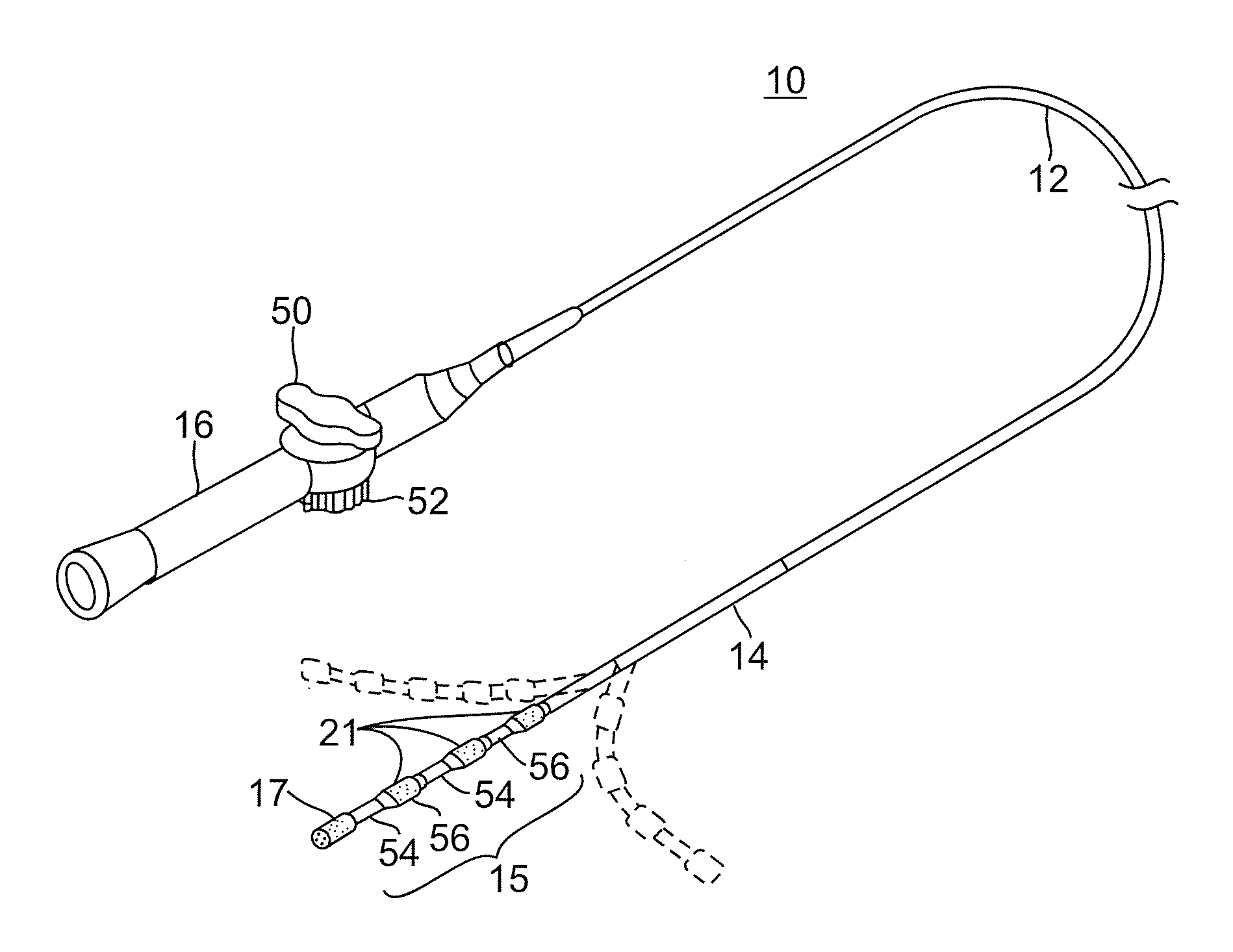
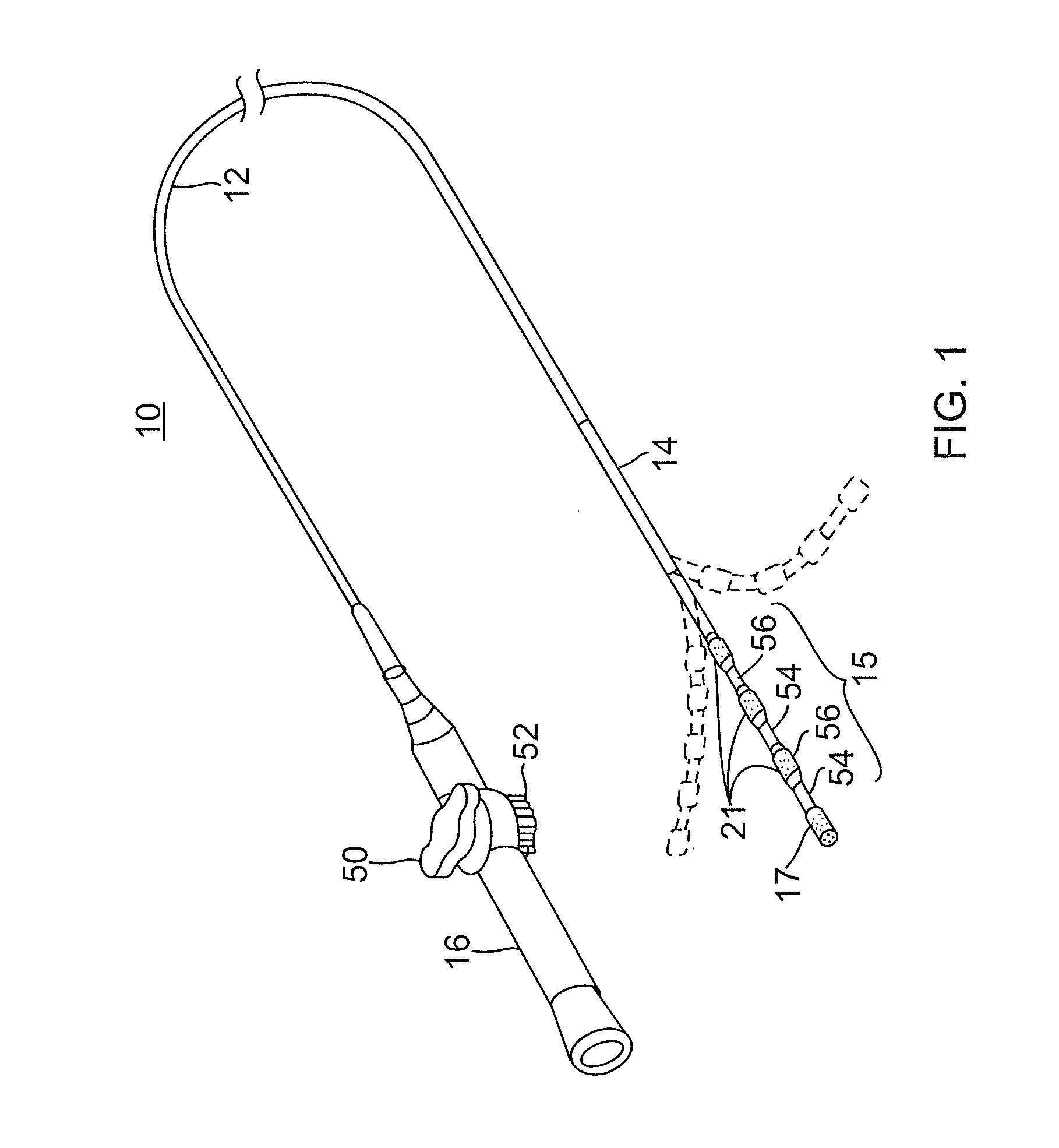
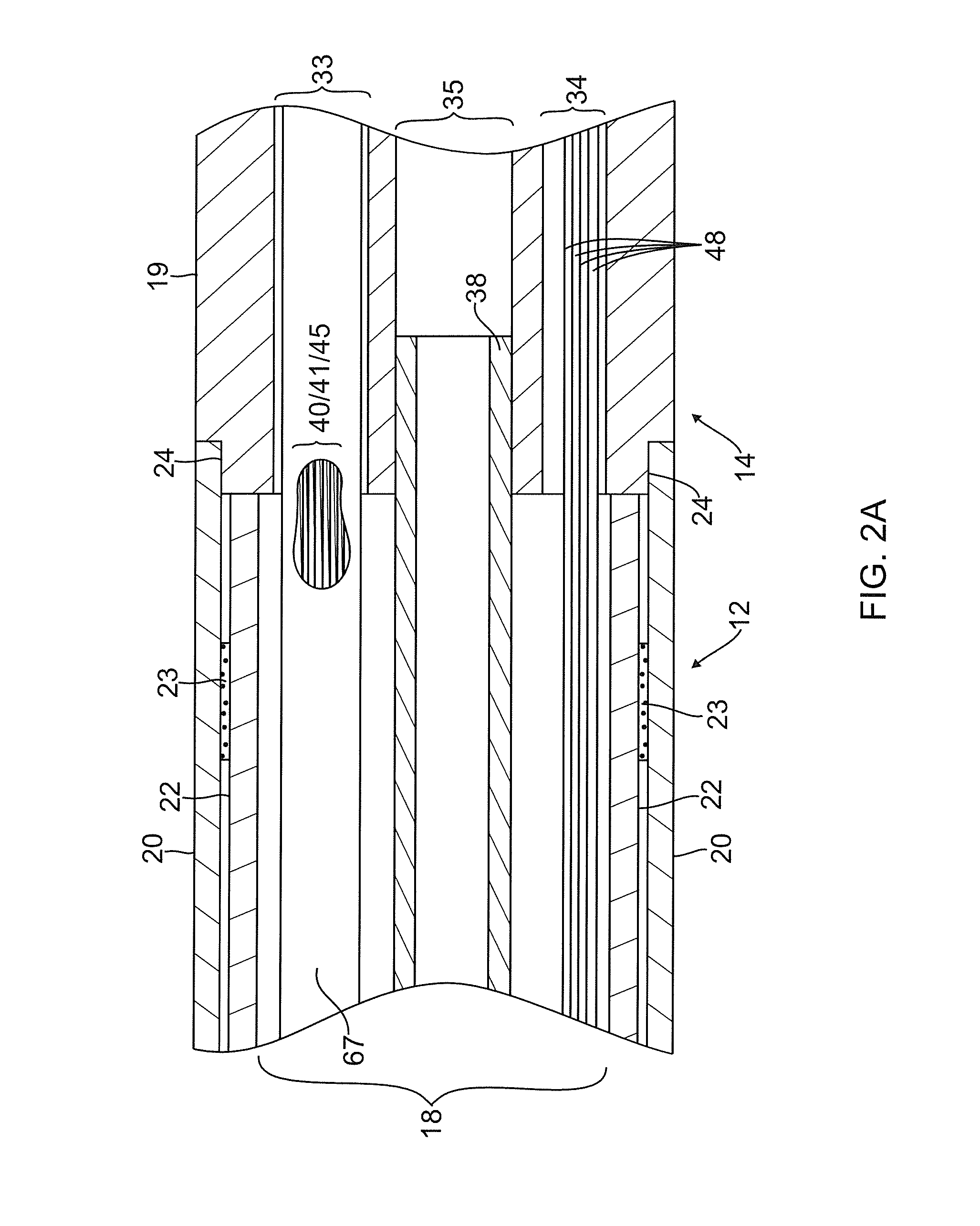
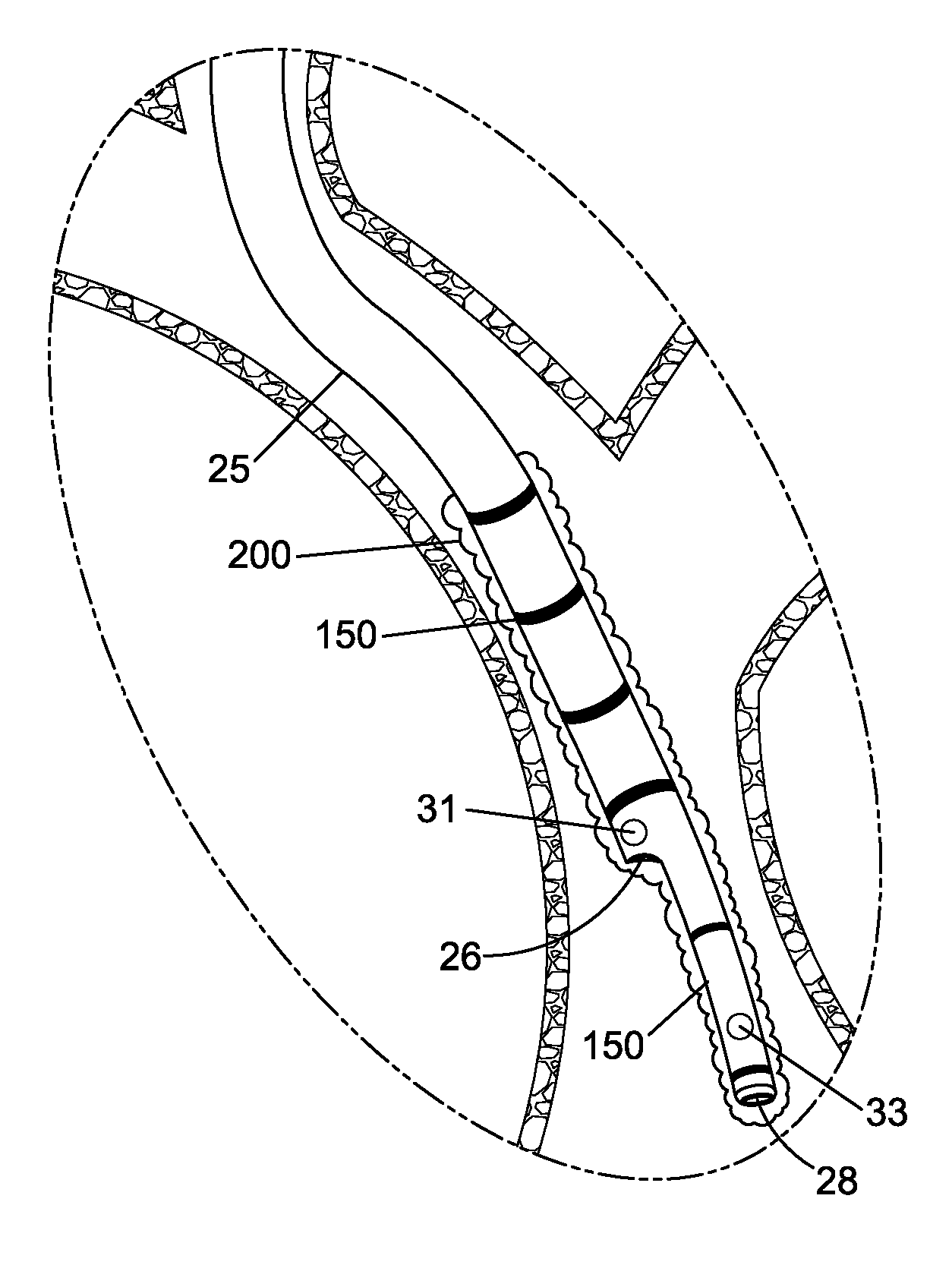
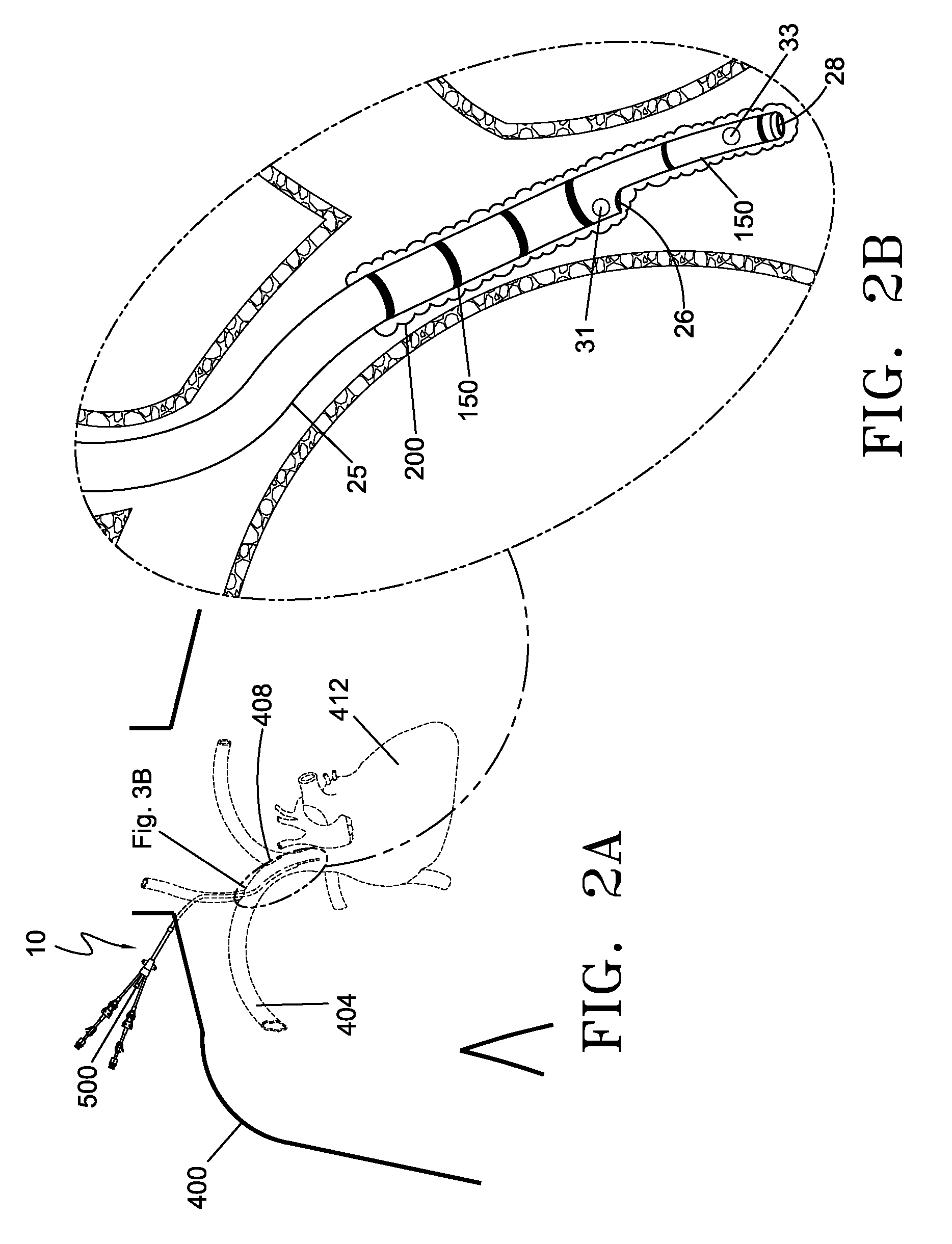
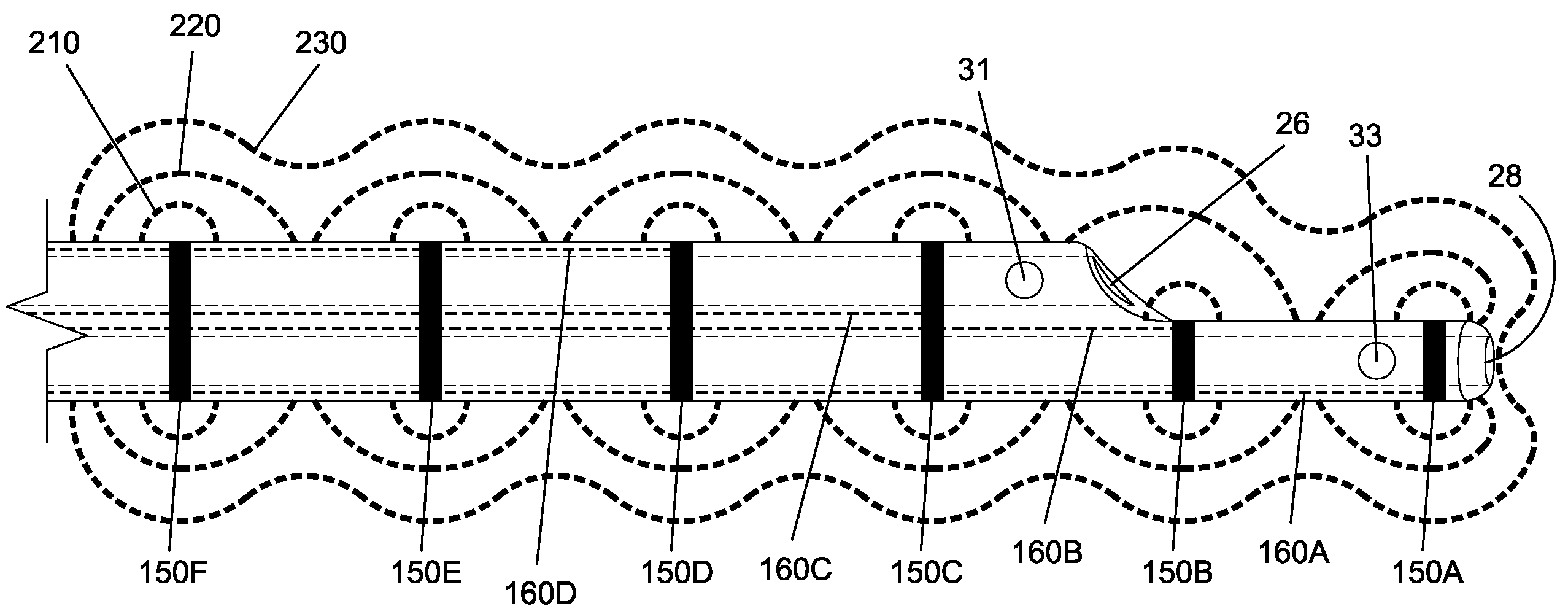
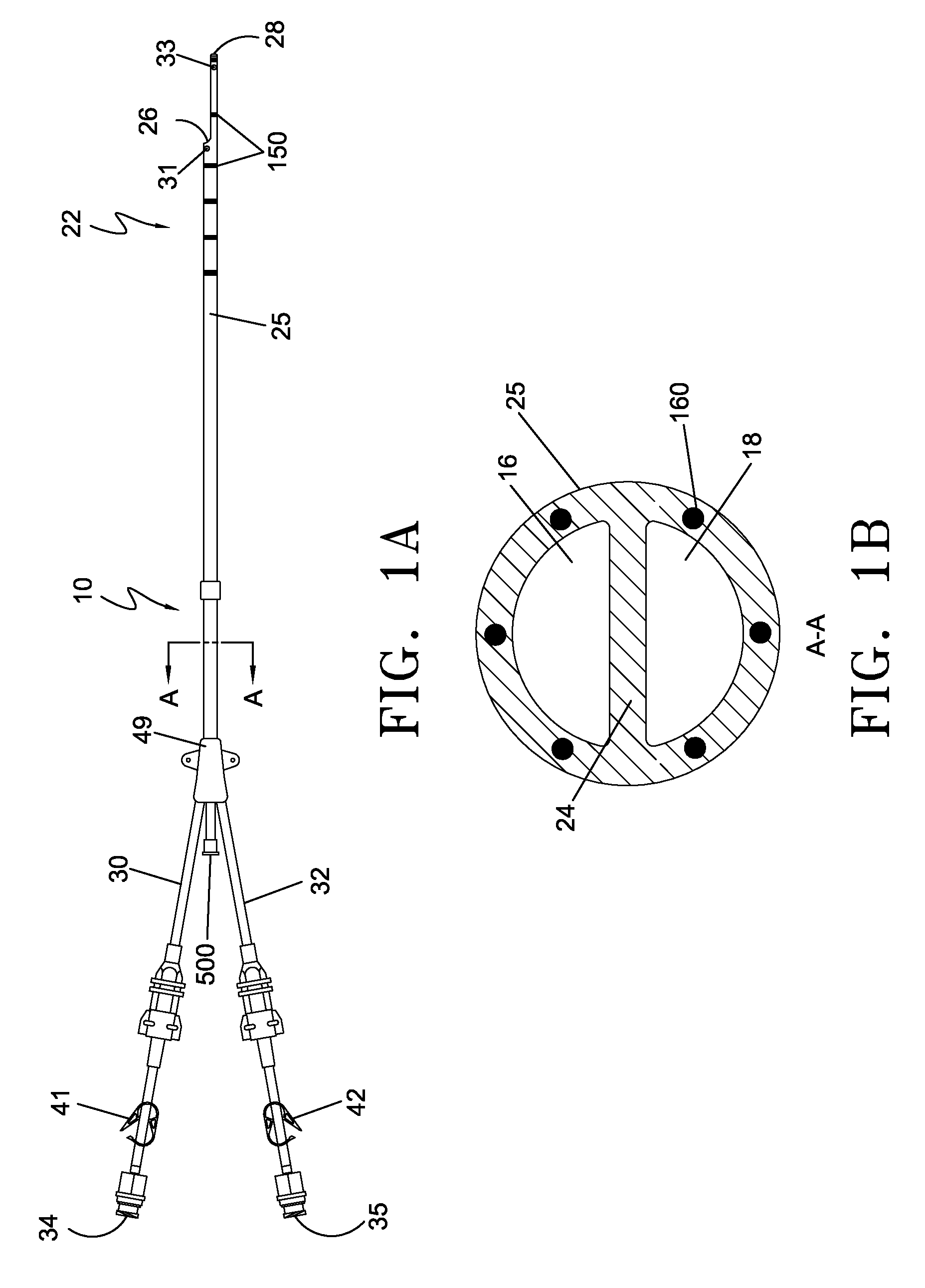
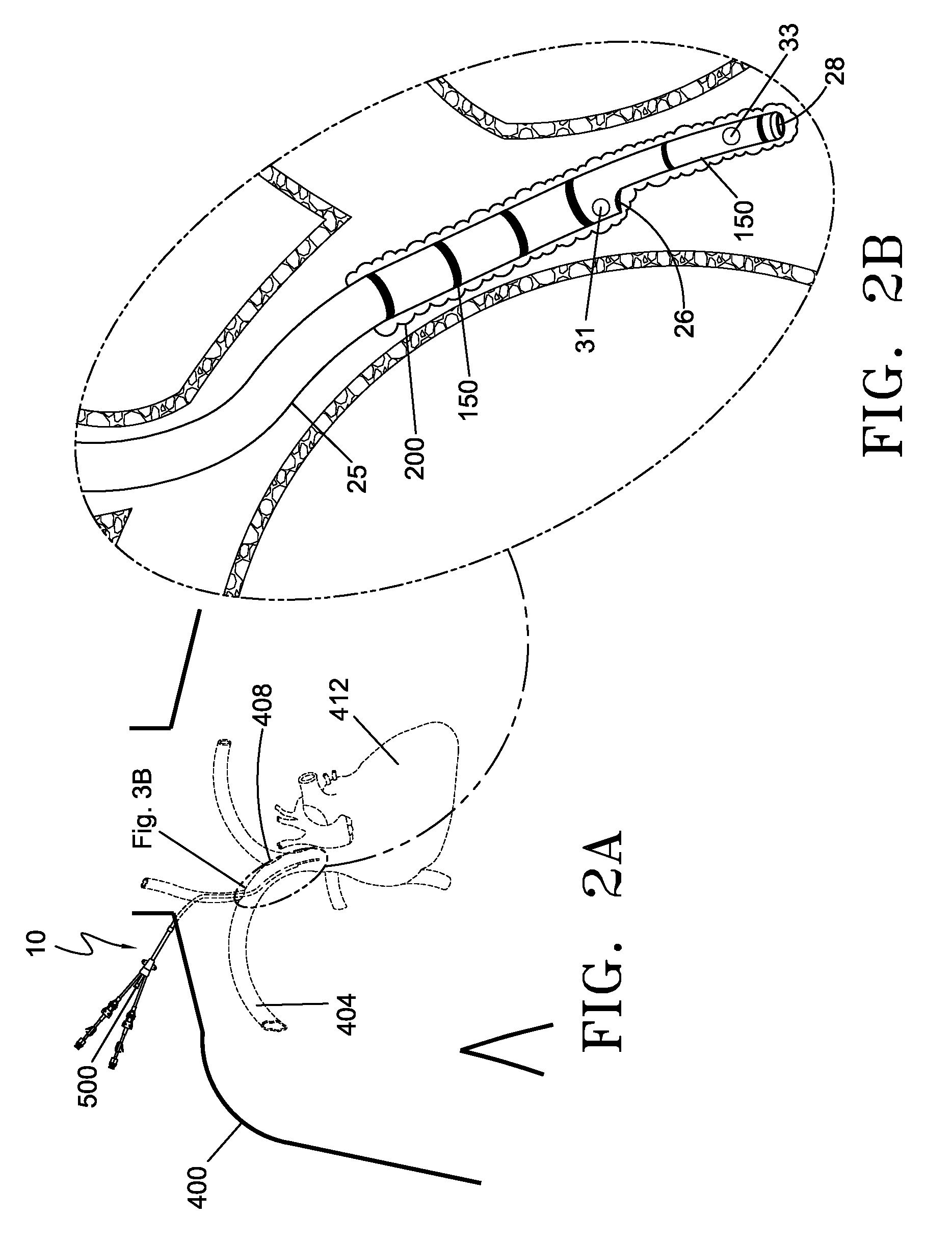
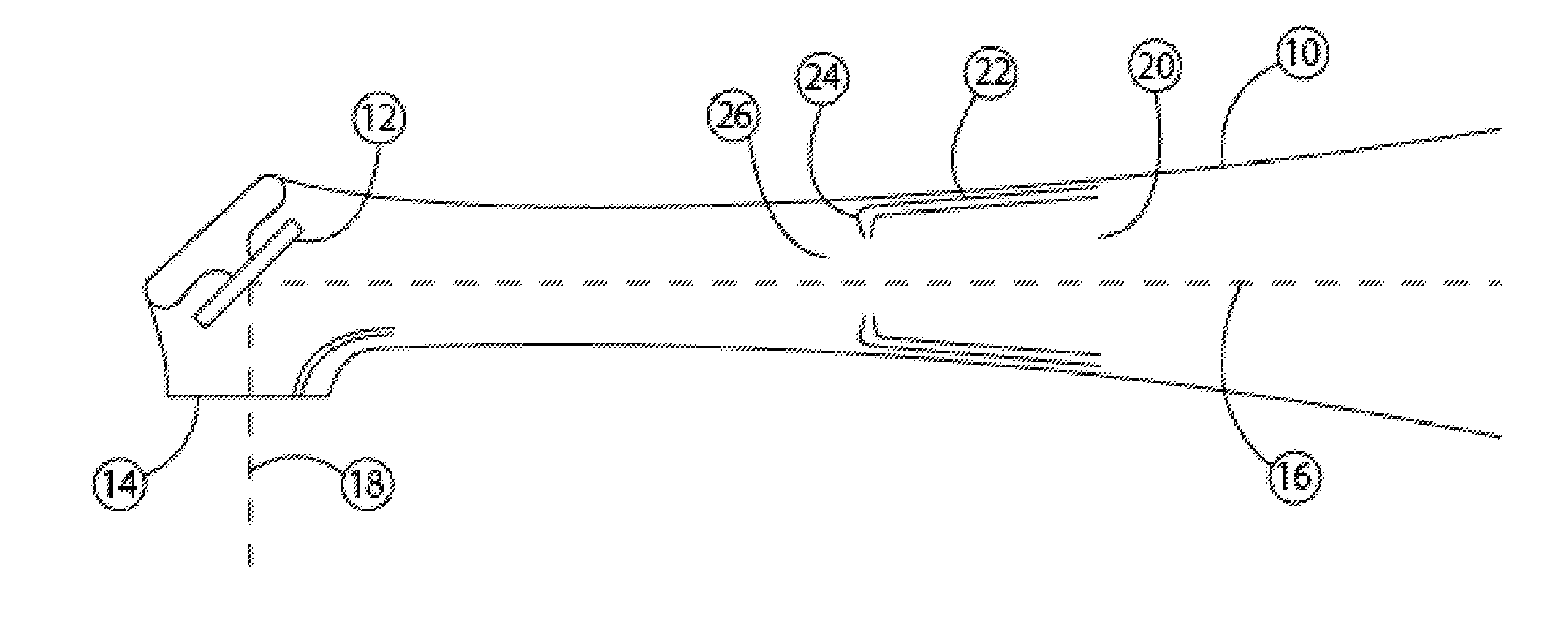
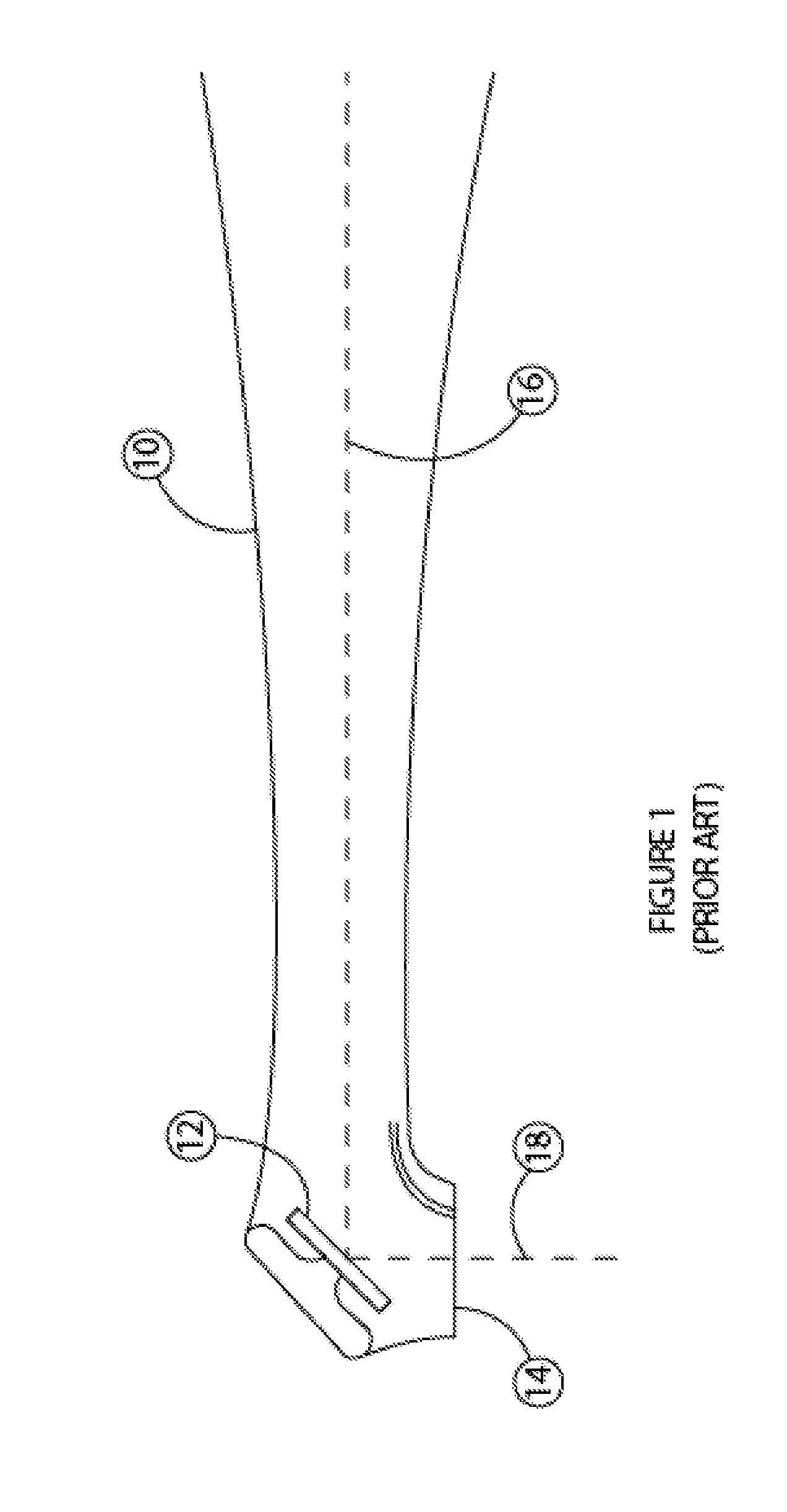
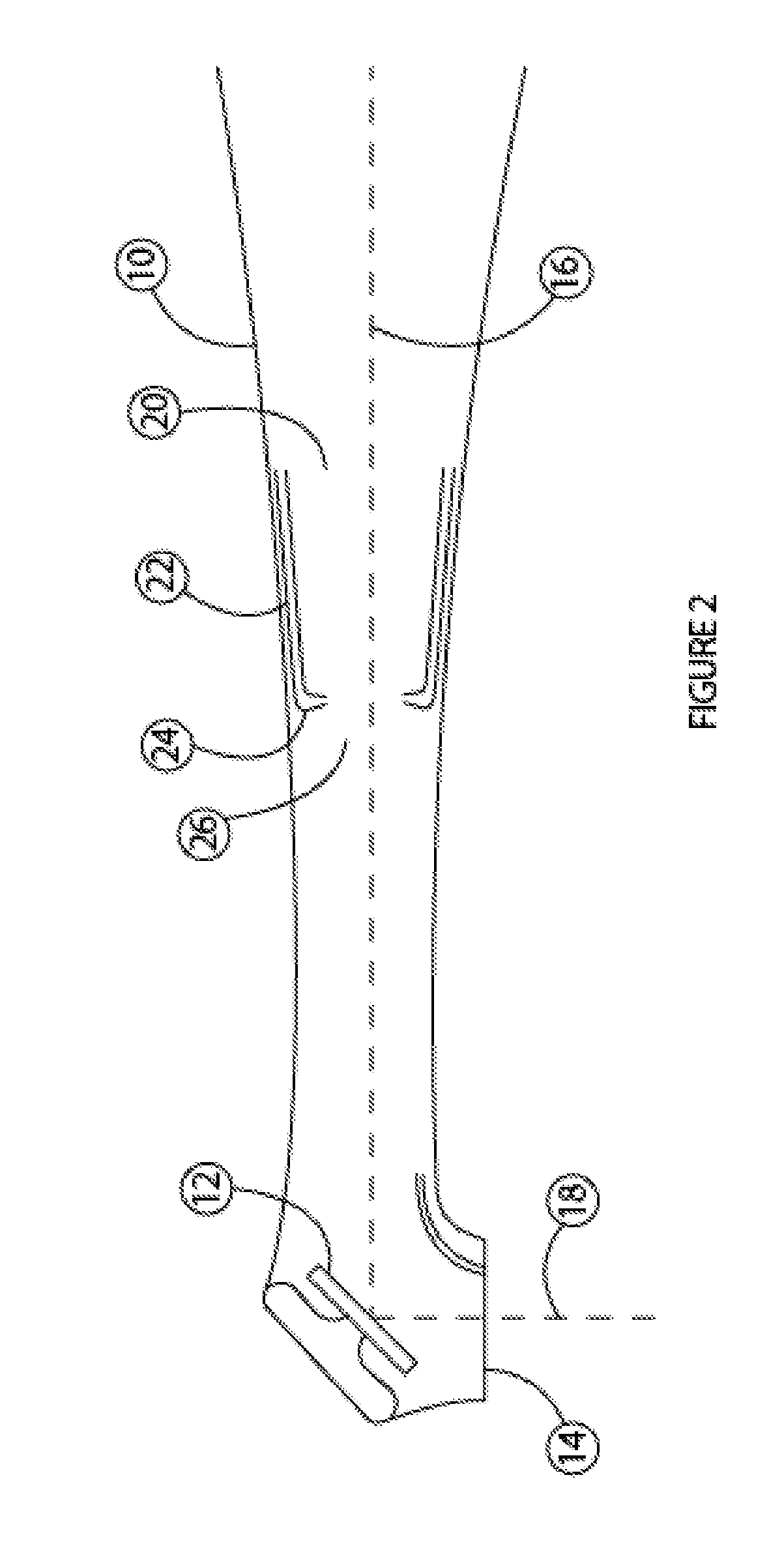
Ablation methods and instruments are disclosed for creating lesions in tissue, especially cardiac tissue for treatment of arrhythmias and the like. Percutaneous ablation instruments in the form of coaxial catheter bodies are disclosed having at least one central lumen therein and having one or more balloon structures at the distal end region of the instrument. The instruments include an energy emitting element which is independently positionable within the lumen of the instrument and adapted to project radiant energy through a transmissive region of a projection balloon to a target tissue site. The instrument can optionally include at least one expandable anchor balloon disposed about, or incorporated into an inner catheter body designed to be slid over a guidewire. This anchor balloon can serve to position the device within a lumen, such as a pulmonary vein. A projection balloon structure is also disclosed that can be slid over the first (anchor balloon) catheter body and inflated within the heart, to define a staging from which to project radiant energy. An ablative fluid can also be employed outside of the instrument (e.g., between the balloon and the target region) to ensure efficient transmission of the radiant energy when the instrument is deployed. In another aspect of the invention, generally applicable to a wide range of cardiac ablation instruments, mechanisms are disclosed for determining whether the instrument has been properly seated within the heart, e.g., whether the device is in contact with a pulmonary vein and / or the atrial surface, in order to form a lesion by heating, cooling or projecting energy. This contact-sensing feature can be implemented by an illumination source situated within the instrument and an optical detector that monitors the level of reflected light. Measurements of the reflected light (or wavelengths of the reflected light) can thus be used to determine whether contact has been achieved and whether such contact is continuous over a desired ablation path.
Owner:CARDIOFOCUS INC
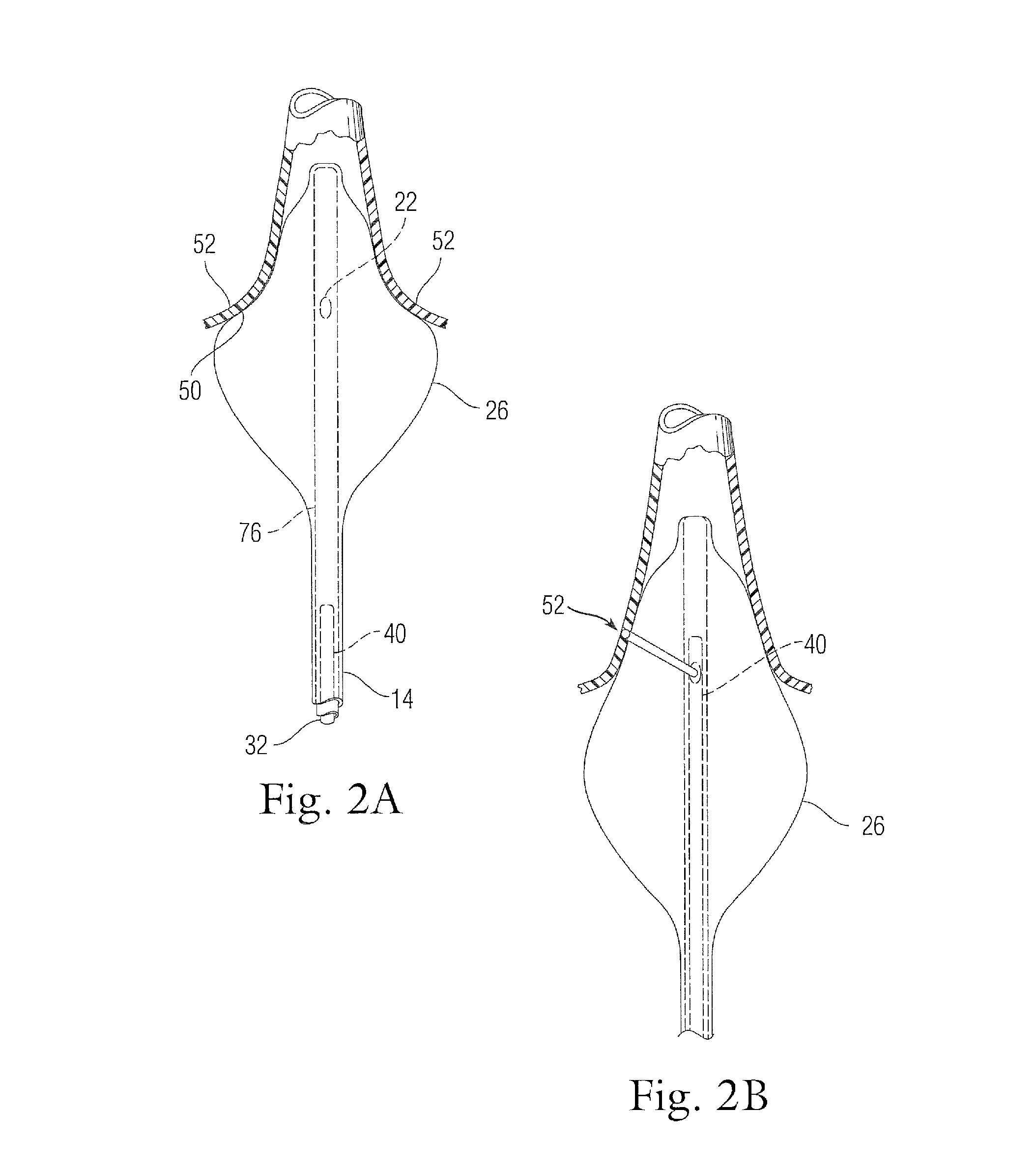
Phototherapeutic wave guide apparatus
InactiveUS6953457B2Minimize and eliminate such damageEliminating aberrant wave conductionDiagnosticsCatheterAnnular LesionProximate
Owner:CARDIOFOCUS INC
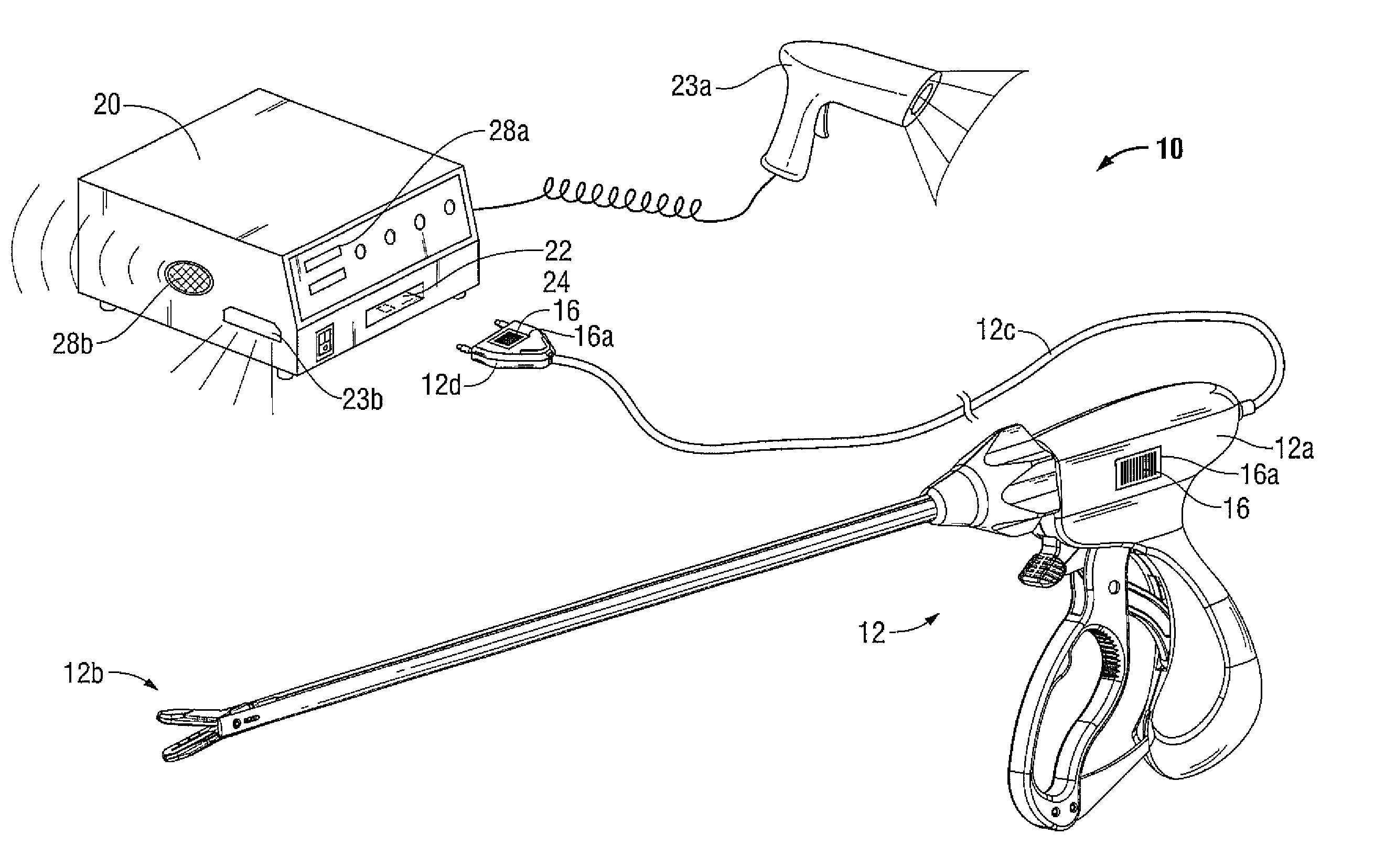
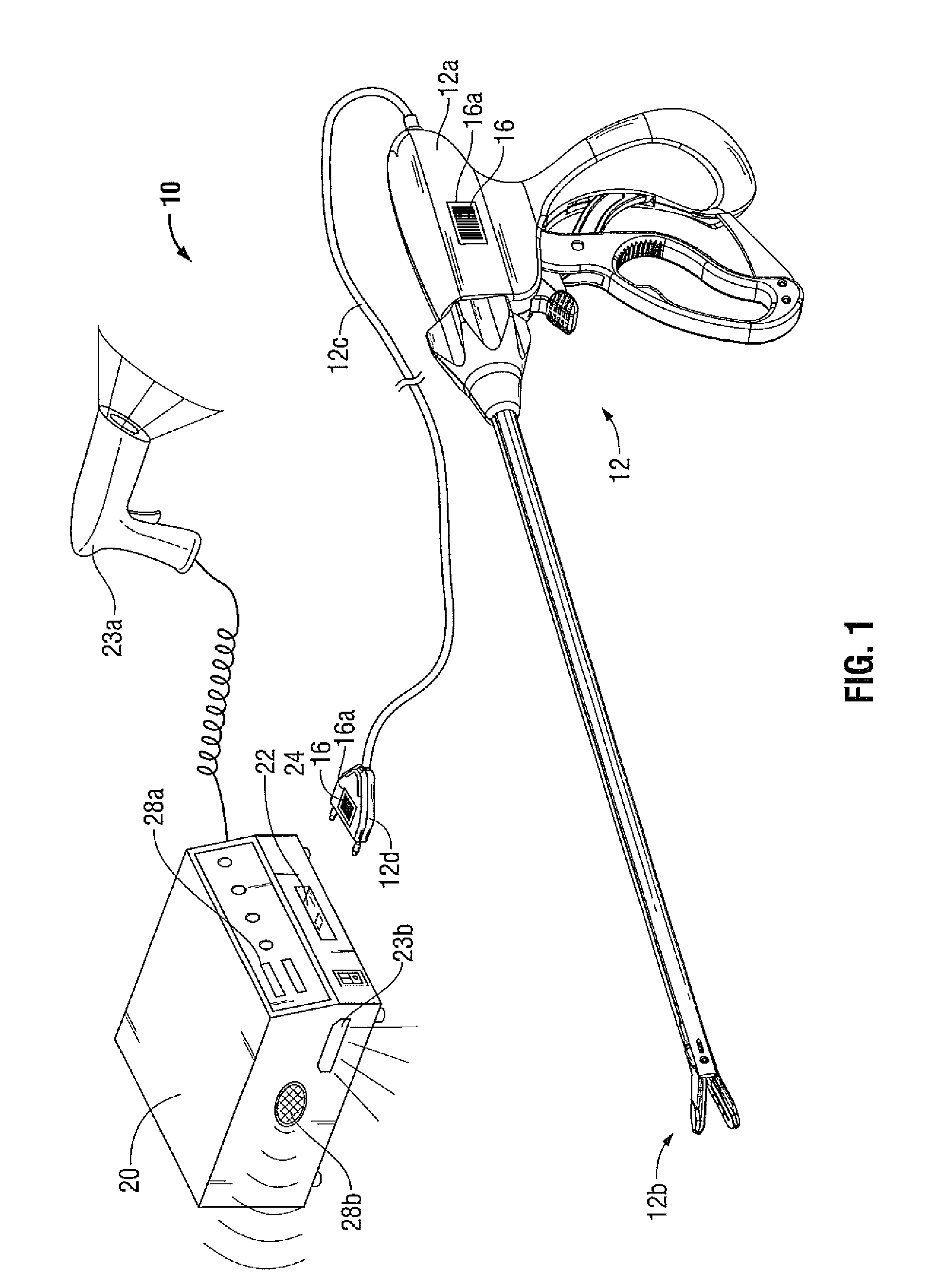
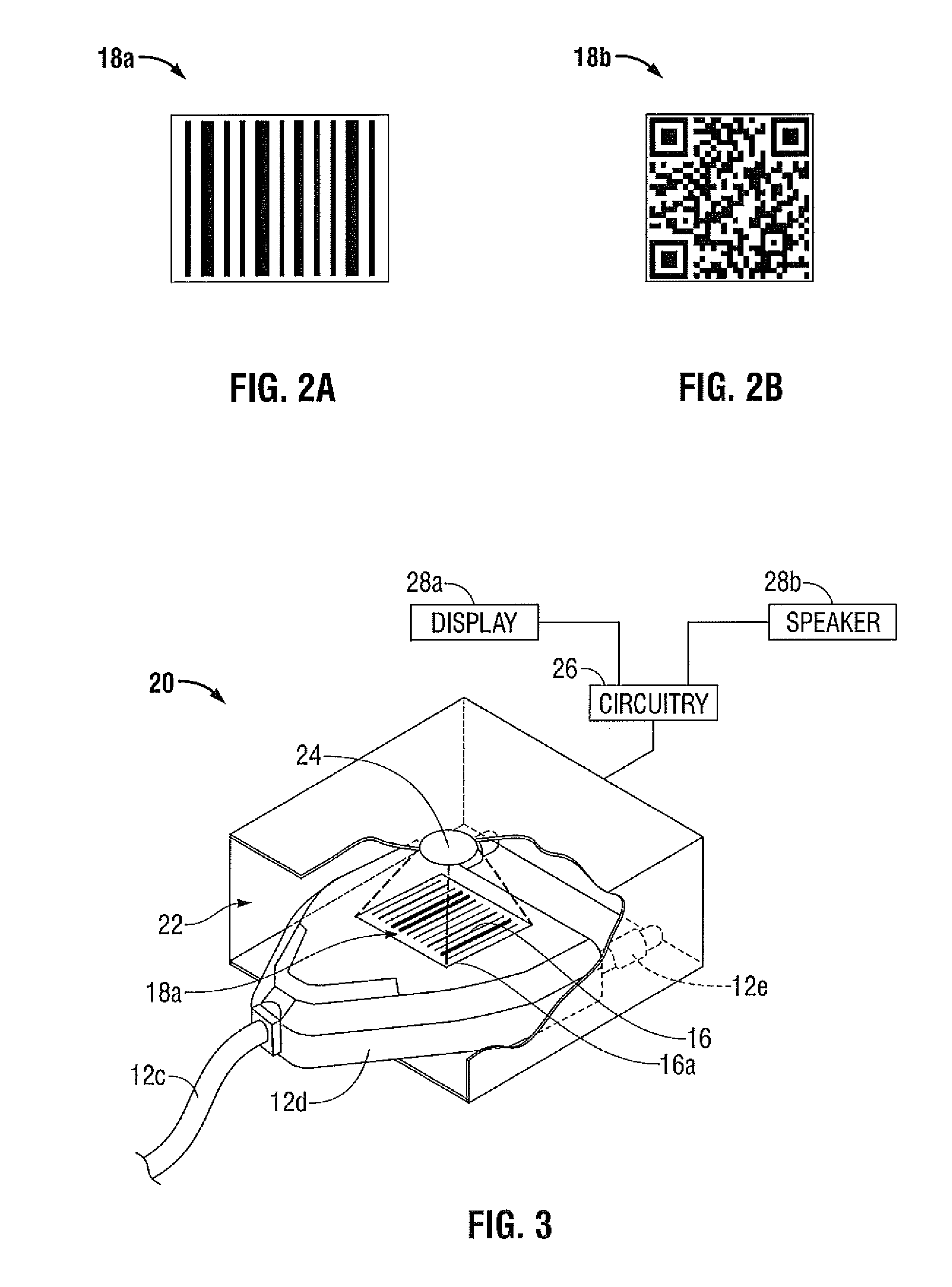
Removable ink for surgical instrument
The present disclosure relates to an apparatus and method for preventing reuse of a surgical instrument. The single-use surgical instrument includes a housing, an electrical connector and a treatment component. Indicia may be printed on the housing, the electrical connector and / or the treatment component. A removable ink is applied to any portion of the surgical instrument in the form of indicia that is readable by a scanning device. The removable ink includes a protein-based composition that is reactivateable with a sterilization solution having an enzyme-based composition such that upon sterilization, the removable ink reacts with the sterilizing solution and becomes unreadable by the scanning device.
Owner:TYCO HEALTHCARE GRP LP
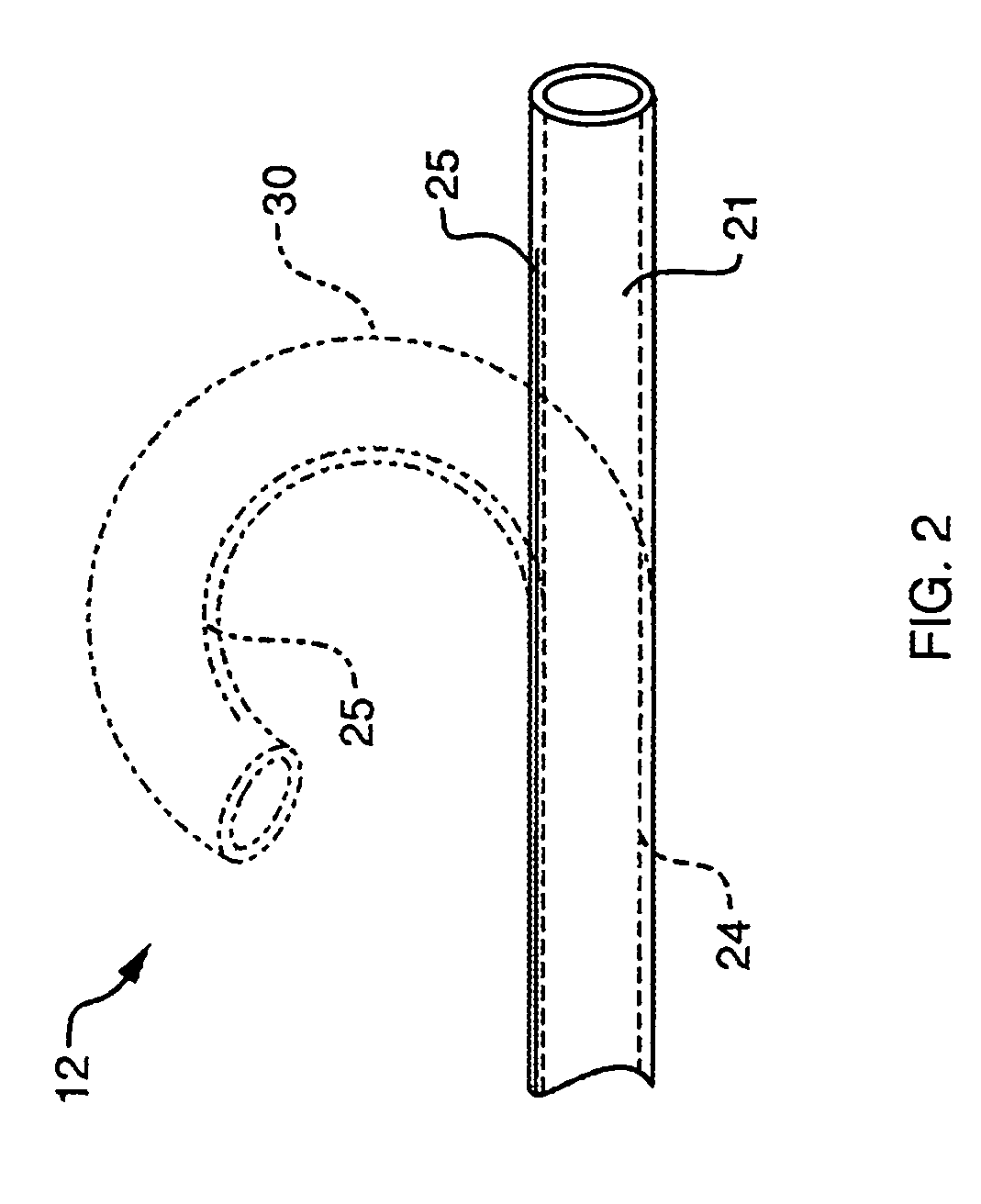
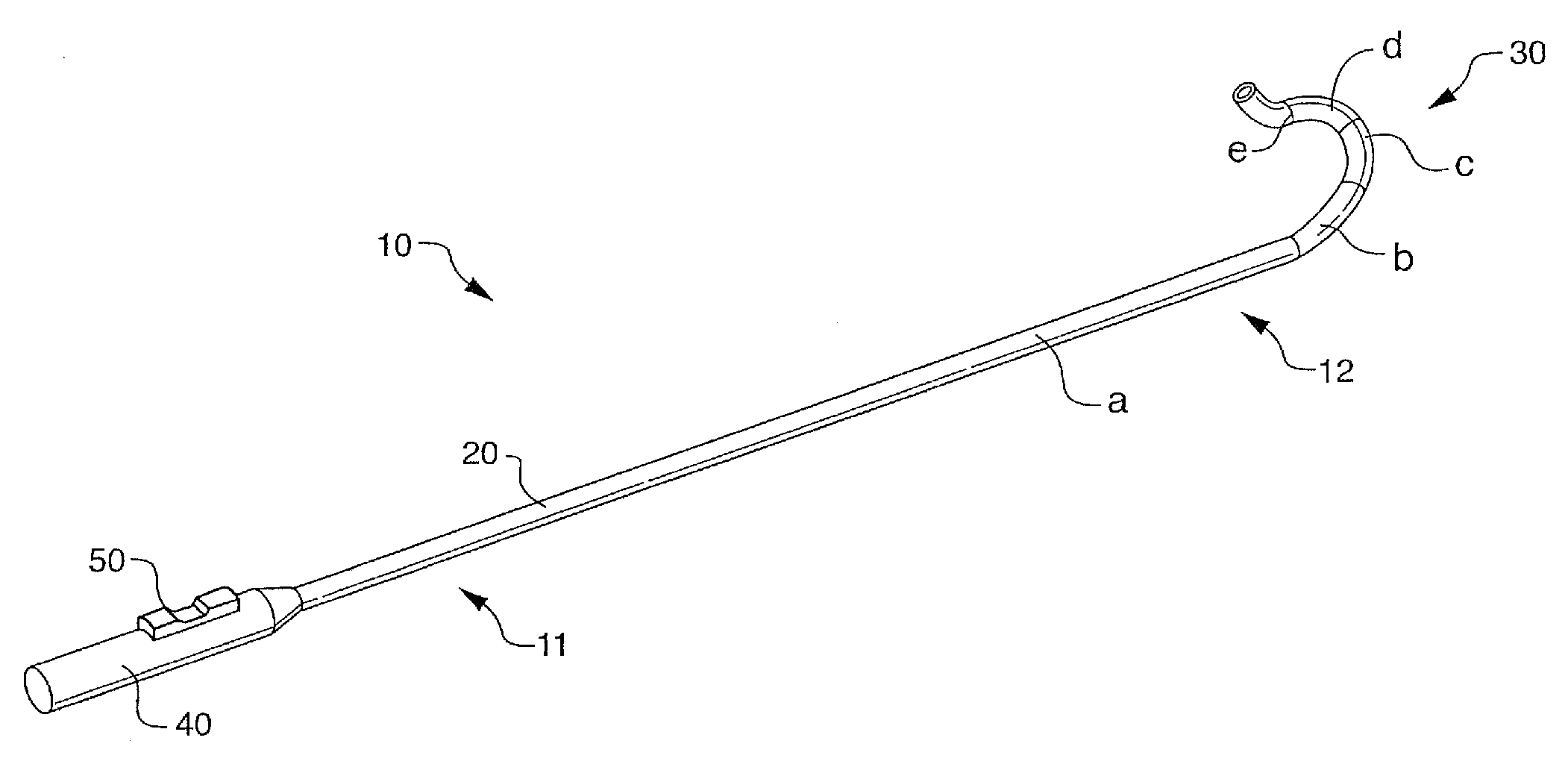
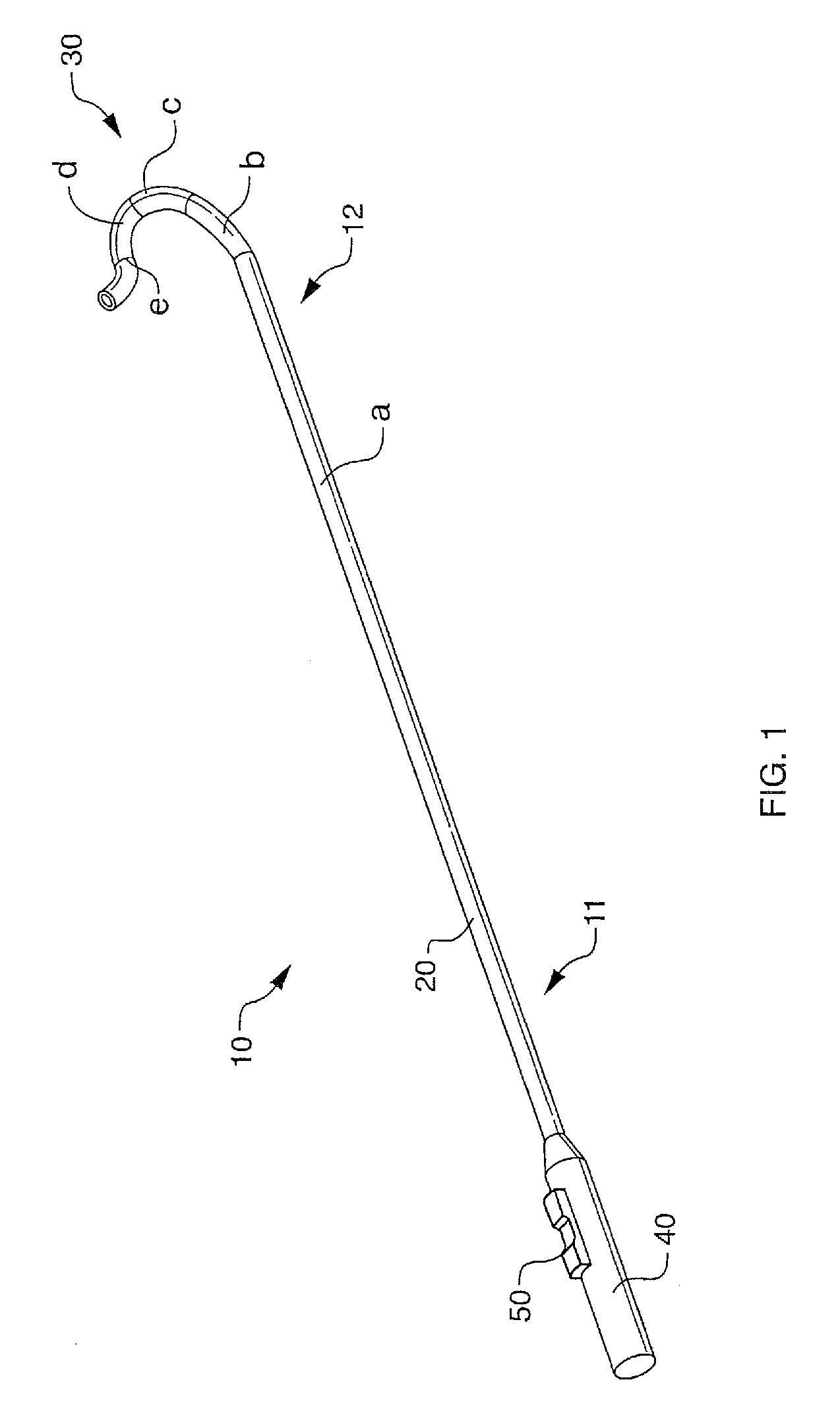
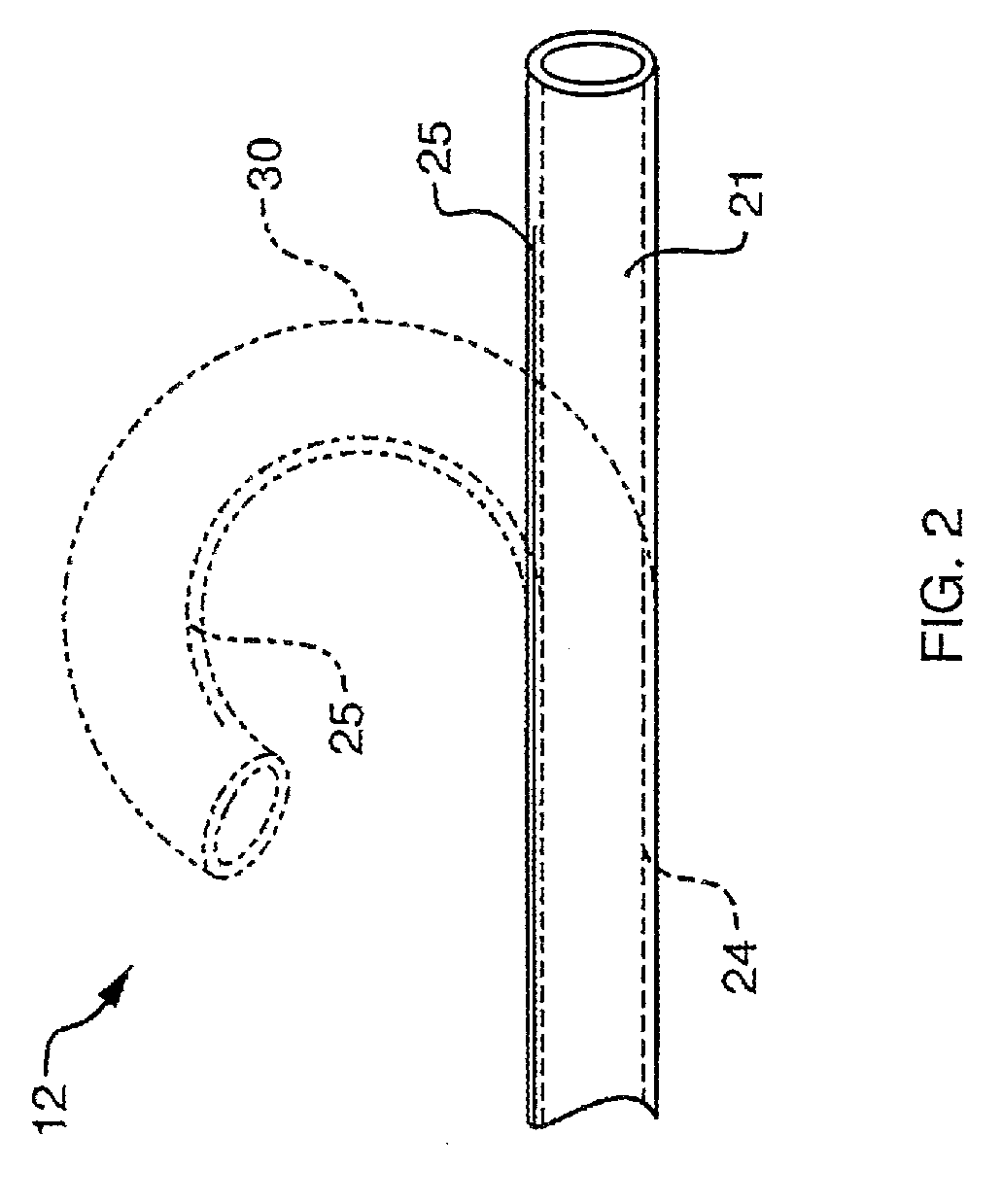
Deflectable sheath catheters
The present invention provides devices and methods for the treatment of atrial fibrillation. In one embodiment a deflectable sheath catheter includes an elongate catheter body having proximal and distal ends, the distal end having a distal tip region that includes a plurality of flexible segments with varying degrees of stiffness. A handle portion can be located at the proximal end of the catheter body to provide a steering mechanism that causes the distal tip region to deflect according to a compound curve.
Owner:CARDIOFOCUS INC
Methods for ablation with radiant energy
InactiveUS20060253113A1Rapid and efficient creationRapid and effective photoablationStentsUltrasound therapyCoaxial catheterTarget tissue
Ablation methods and instruments are disclosed for creating lesions in tissue, especially cardiac tissue for treatment of arrhythmias and the like. Percutaneous ablation instruments in the form of coaxial catheter bodies are disclosed having at least one central lumen therein and having one or more balloon structures at the distal end region of the instrument. The instruments include an energy emitting element which is independently positionable within the lumen of the instrument and adapted to project radiant energy through a transmissive region of a projection balloon to a target tissue site. The instrument can optionally include at least one expandable anchor balloon disposed about, or incorporated into an inner catheter body designed to be slid over a guidewire. This anchor balloon can serve to position the device within a lumen, such as a pulmonary vein. A projection balloon structure is also disclosed that can be slid over the first (anchor balloon) catheter body and inflated within the heart, to define a staging from which to project radiant energy. An ablative fluid can also be employed outside of the instrument (e.g., between the balloon and the target region) to ensure efficient transmission of the radiant energy when the instrument is deployed. In another aspect of the invention, generally applicable to a wide range of cardiac ablation instruments, mechanisms are disclosed for determining whether the instrument has been properly seated within the heart, e.g., whether the device is in contact with a pulmonary vein and / or the atrial surface, in order to form a lesion by heating, cooling or projecting energy. This contact-sensing feature can be implemented by an illumination source situated within the instrument and an optical detector that monitors the level of reflected light. Measurements of the reflected light (or wavelengths of the reflected light) can thus be used to determine whether contact has been achieved and whether such contact is continuous over a desired ablation path.
Owner:CARDIOFOCUS INC
Cardiac ablation catheters for forming overlapping lesions
InactiveUS20090299354A1Improve energy transferEnhance the imageUltrasound therapyDiagnosticsCardiac AblationTarget tissue
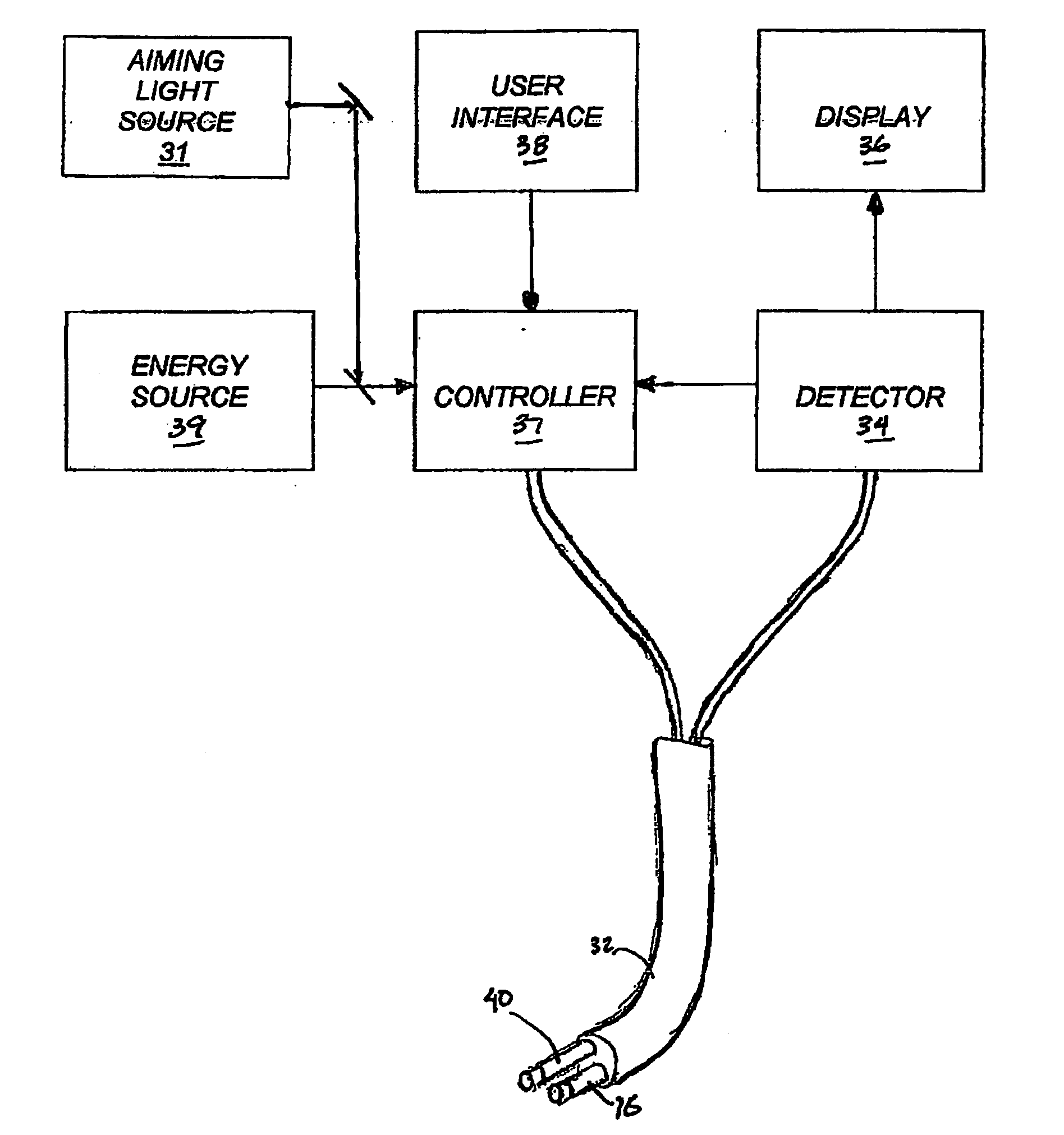
Methods and instruments are disclosed for creating lesions in tissue, especially cardiac tissue, for treatment of arrhythmias and the like, by employing an elastic balloon and an energy emitter, which is independently positionable within the lumen of the instrument and adapted to project a series of spots of ablative energy through a transmissive region of the balloon to a target tissue site. The energy emitter preferably is configured such the spots of energy result in a series of lesions formed in the target tissue region when the emitter is activated, the lesions having an average area ranging from about 5 mm2 to about 100 mm2. In one aspect of the invention, percutaneous ablation instruments are disclosed in the form of catheter bodies having one or more balloon structures at the distal end region of the instrument and an energy emitting element, which is independently positionable and rotatable within a lumen of the instrument and adapted to project ablative energy through a transmissive region of the balloon to a target tissue site in contact with, or proximal to, the balloon surface.
Owner:CARDIOFOCUS INC
Phototherapeutic wave guide apparatus
InactiveUS20050267452A1Minimize and eliminate such damageEliminating aberrant wave conductionDiagnosticsCatheterAnnular LesionProximate
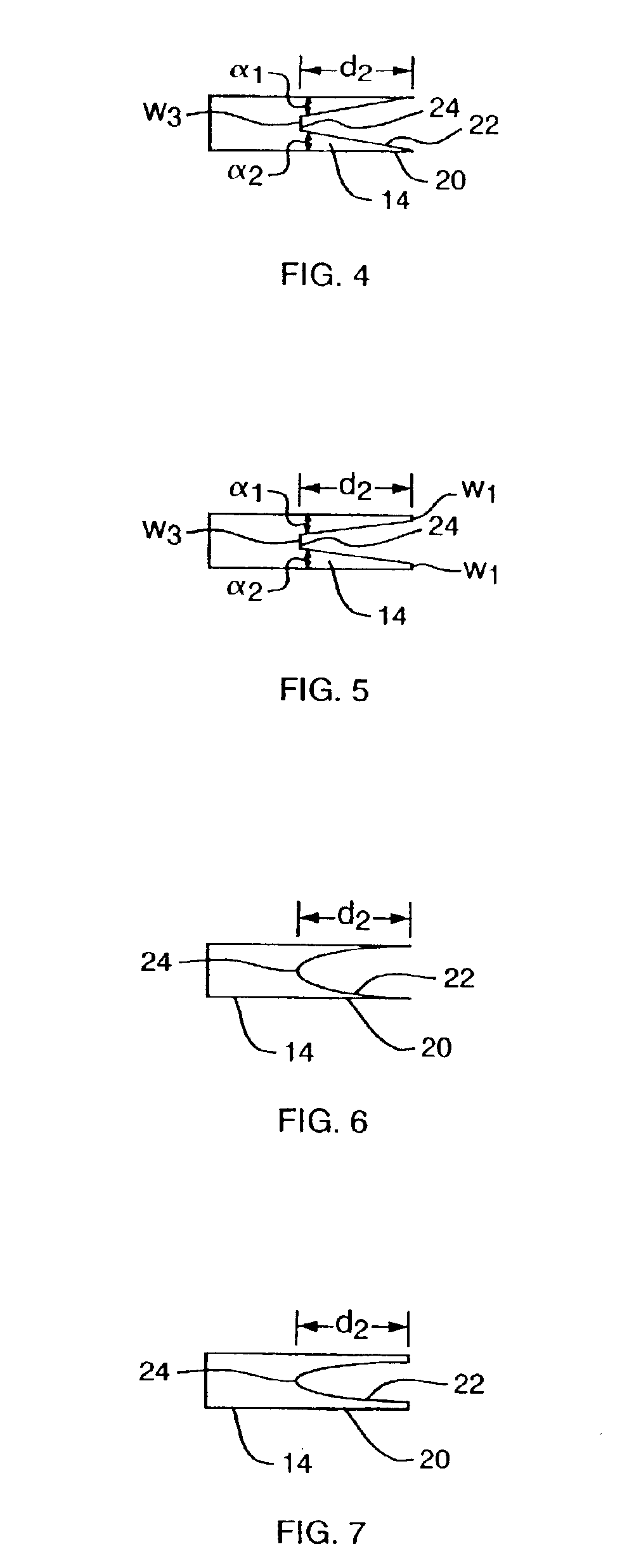
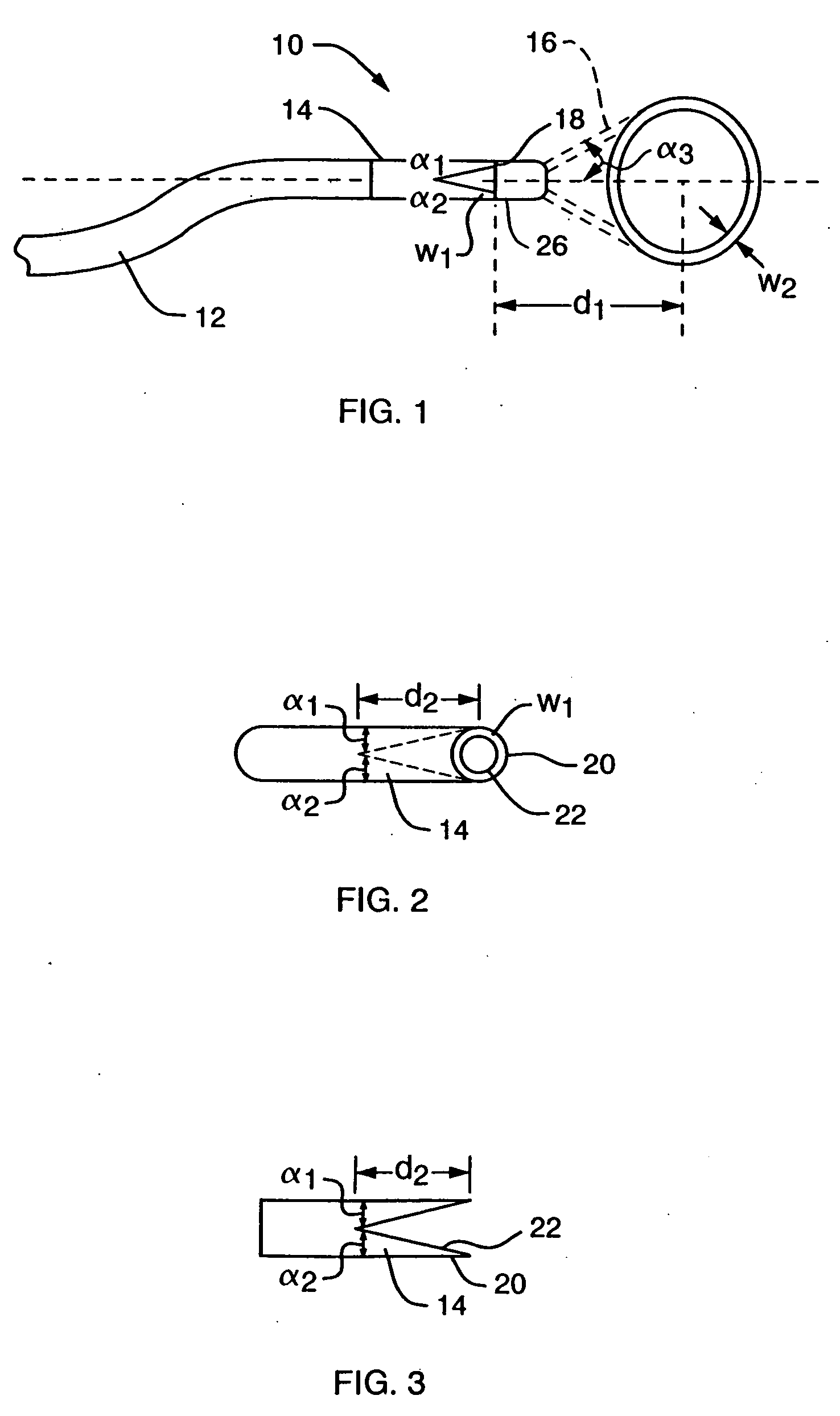
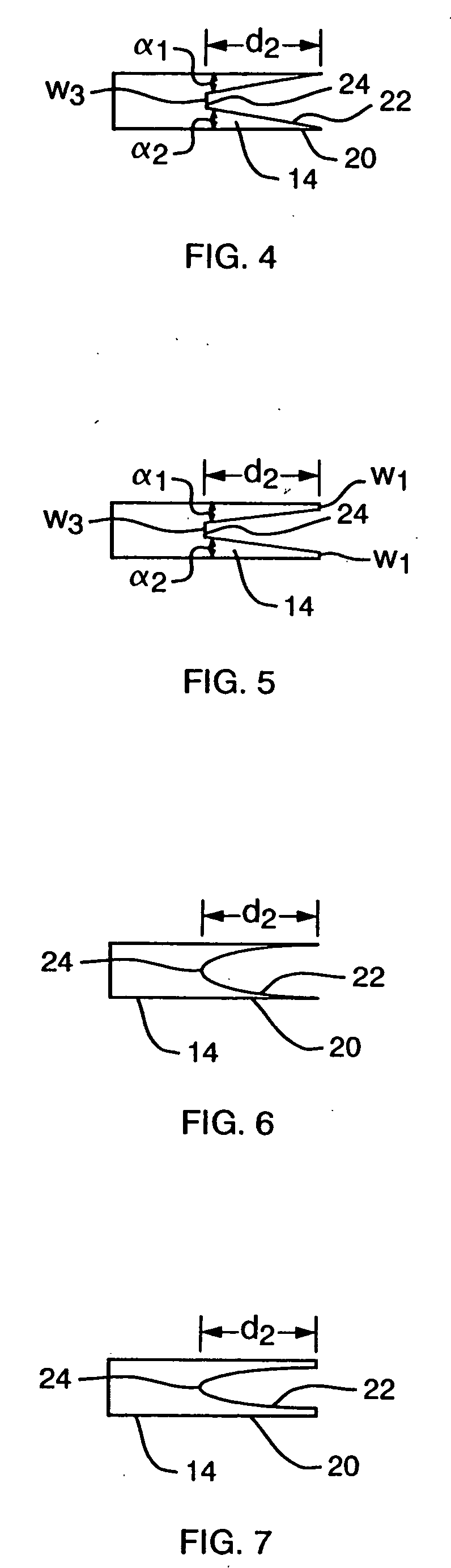
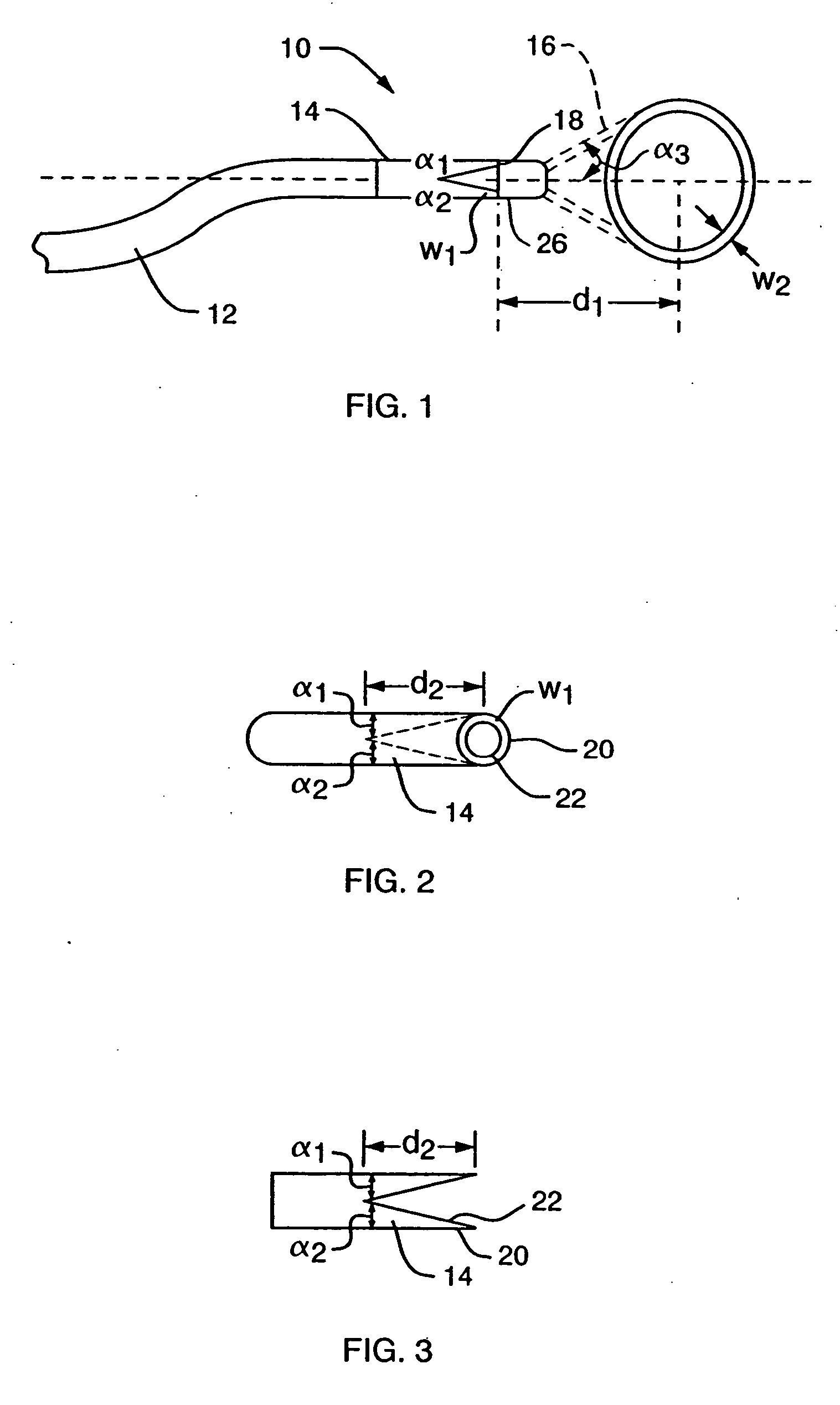
Methods and apparatus are disclosed for forming annular lesions in tissue. The methods include introduction of an optical apparatus proximate to a tissue site, via, for example, a catheter. The optical apparatus includes a pattern-forming optical wave guide in communication with a light transmitting optical fiber. Energy is transmitted through the optical fiber, such that radiation is propagated through the optical fiber and the wave guide projects an annular light pattern, e.g., a circle or a halo.
Owner:CARDIOFOCUS INC
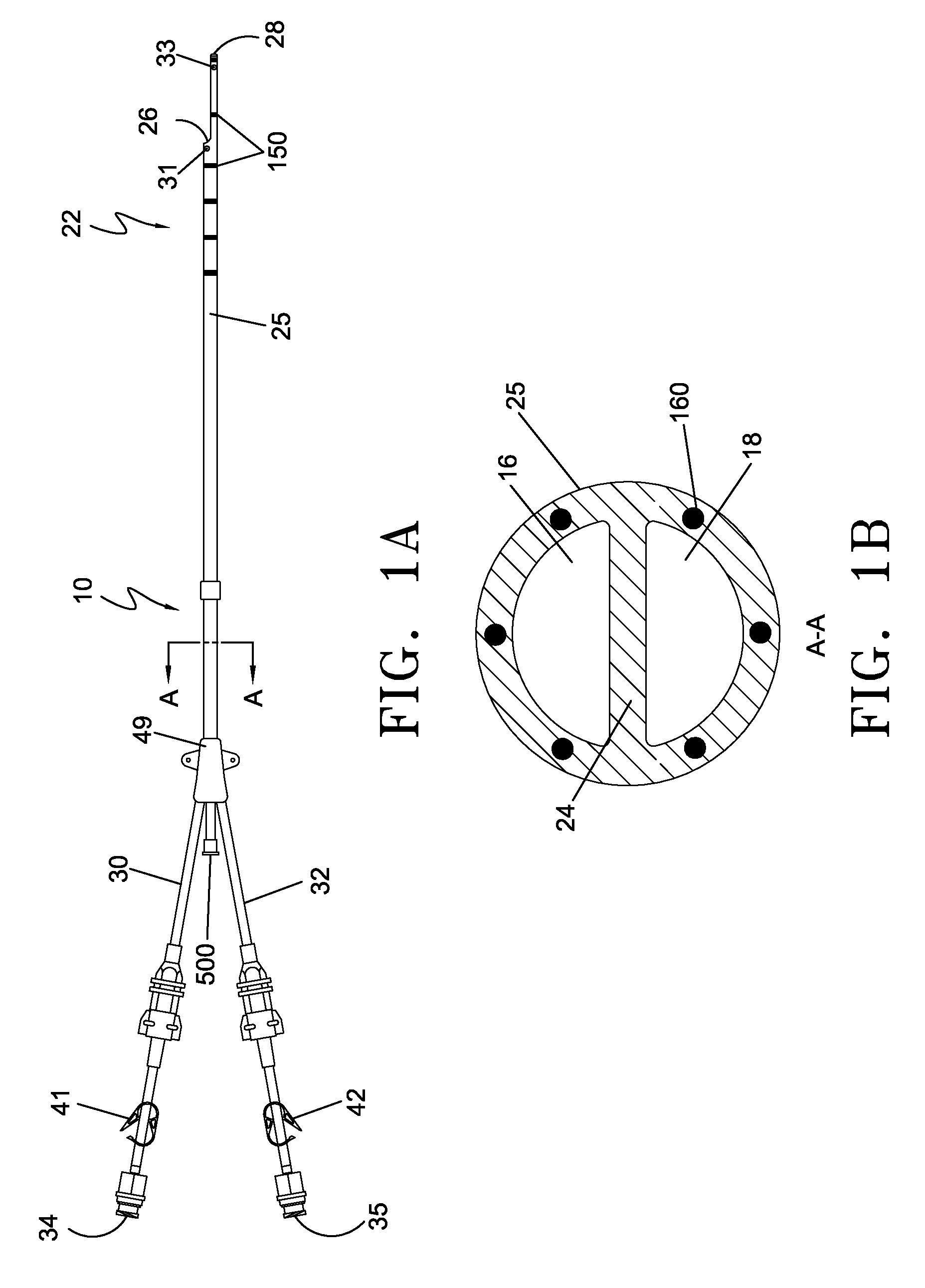
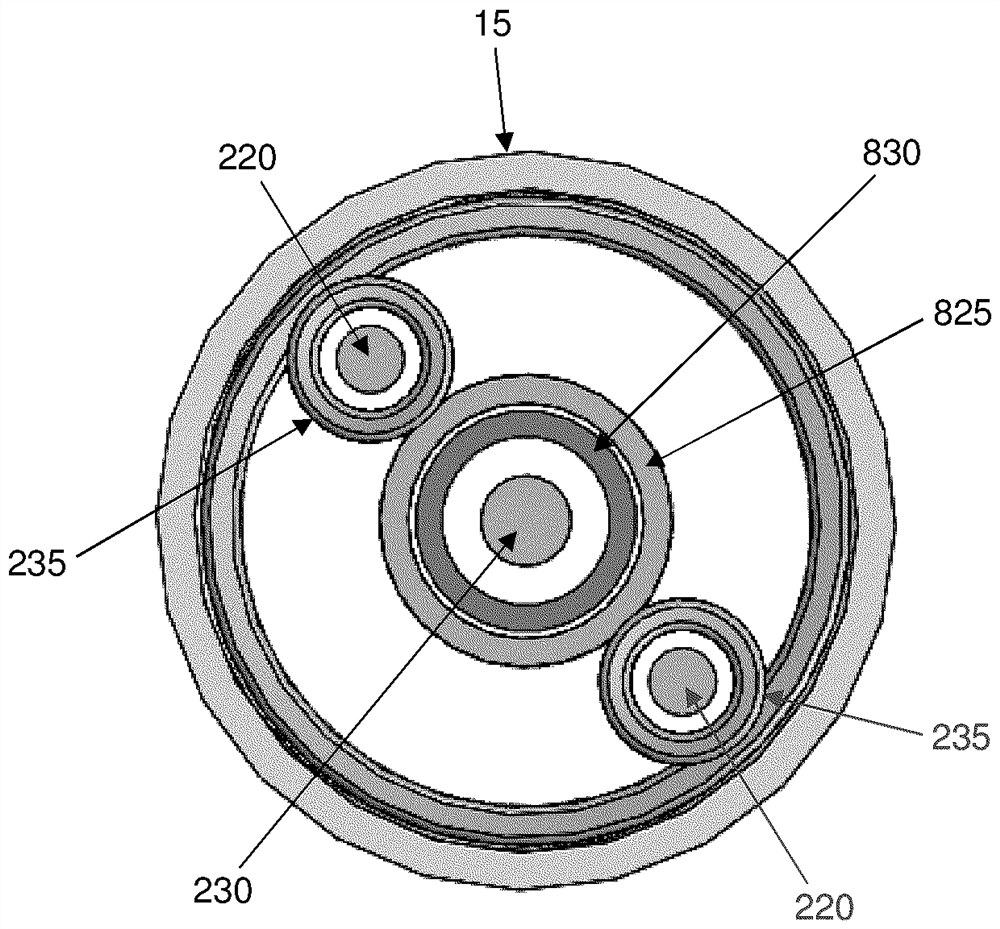
Catheter with composite construction
ActiveUS20130253505A1Increase catheter sizeLess spaceDiagnosticsSurgical navigation systemsComposite constructionEngineering
A catheter has a composite and segmented construction in a distal section that includes deflectable members and support member arranged in alternating sequence, with each support member carrying a ring electrode and the deflectable members being flexible to allow deflection of the distal section as a whole. Carried on an outer surface of the support member is a coil location sensor. The distal section is configured with a distal irrigation fluid path extending axially through the deflectable members and the support members to deliver irrigation fluid to the ring electrode and the tip electrode. A method of constructing a catheter includes building a section of the catheter from the inside out by mounting the support members on a tubing at predetermined locations and filling gaps in between with a more flexible material to form the deflectable members by extrusion segments or injection molding over assembled components internal to the catheter.
Owner:BIOSENSE WEBSTER (ISRAEL) LTD
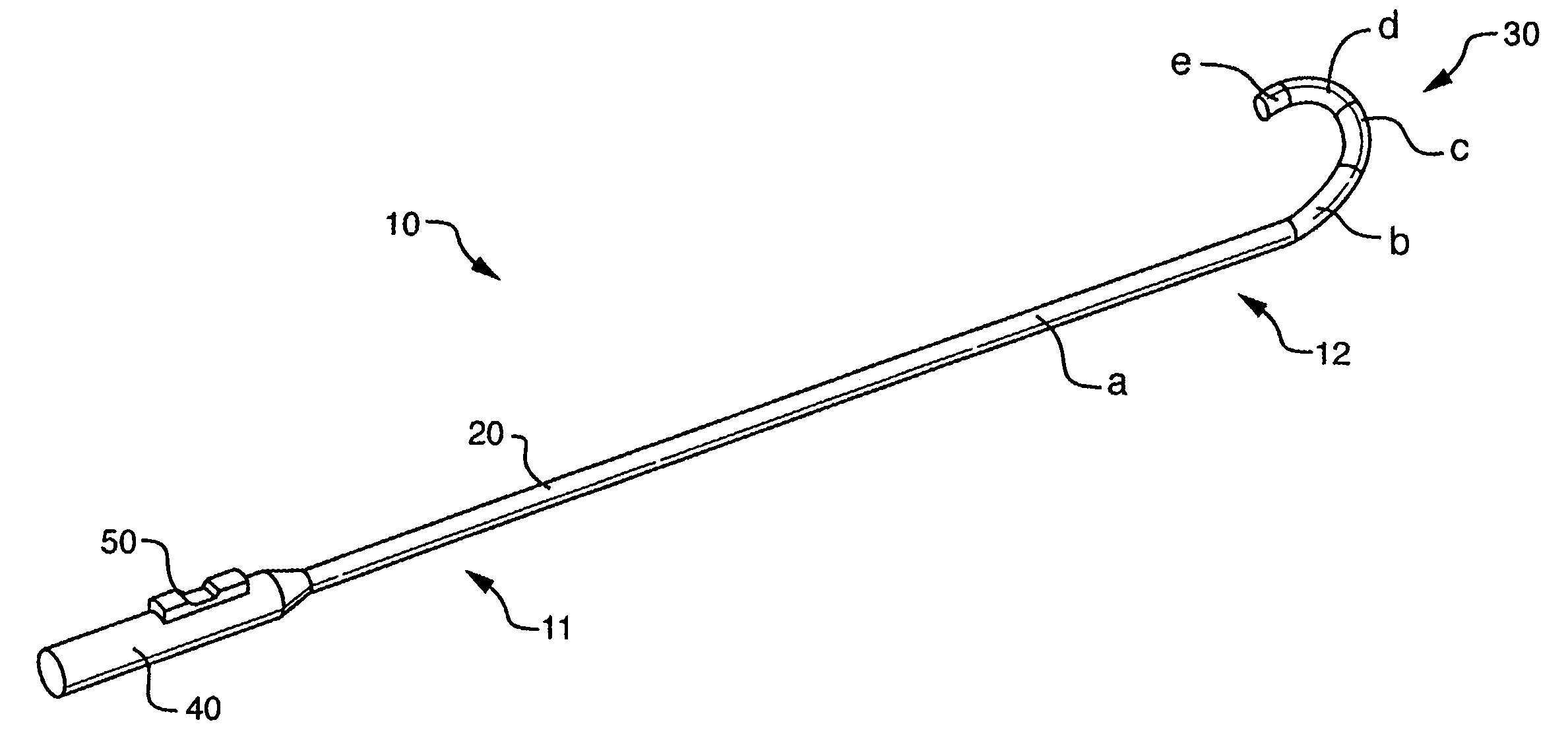
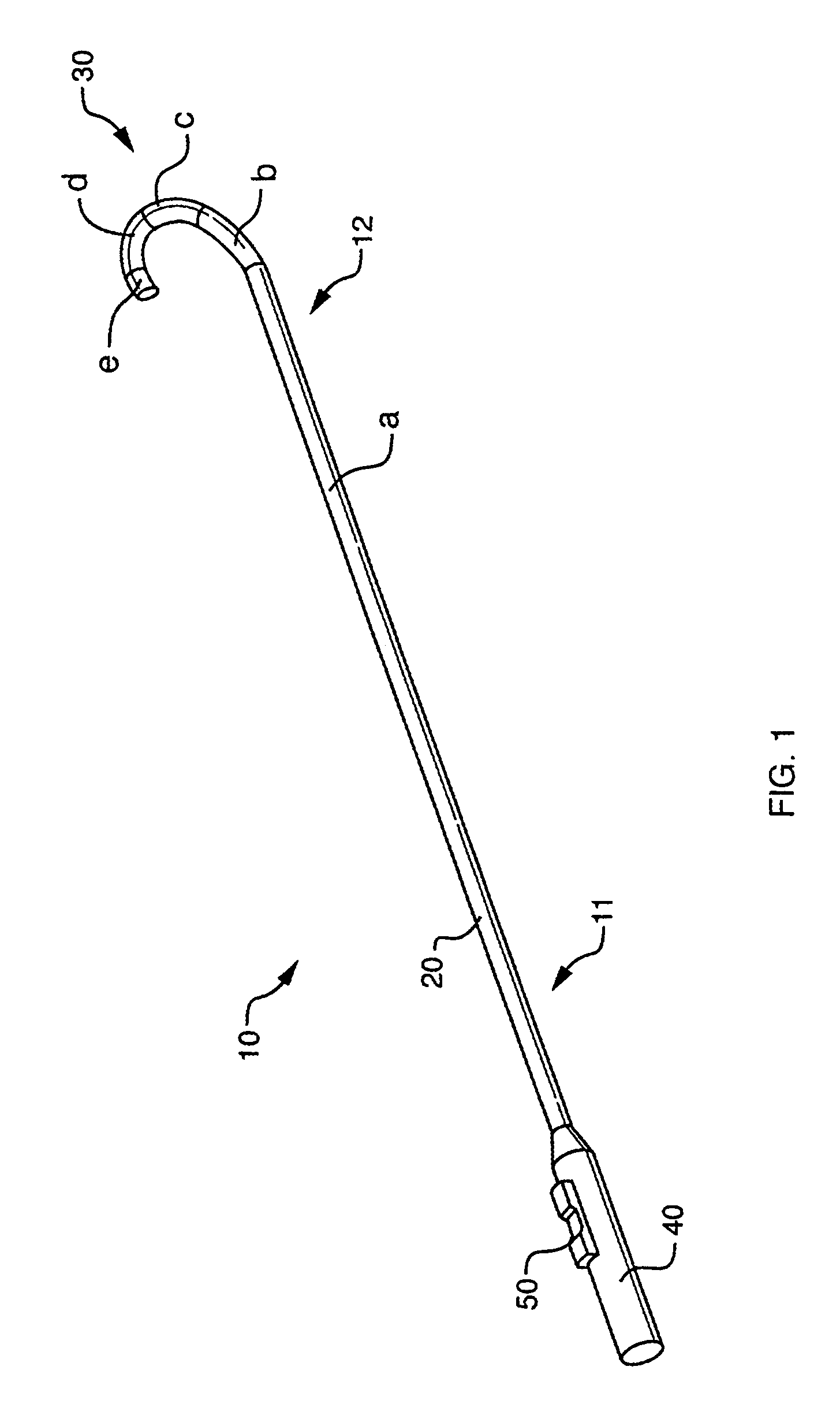
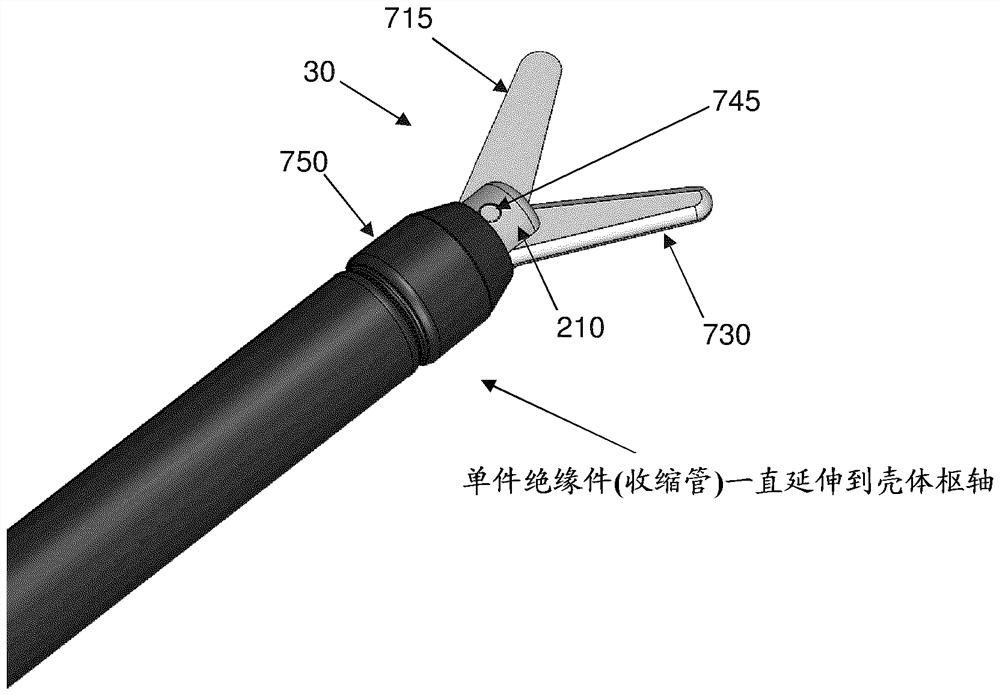
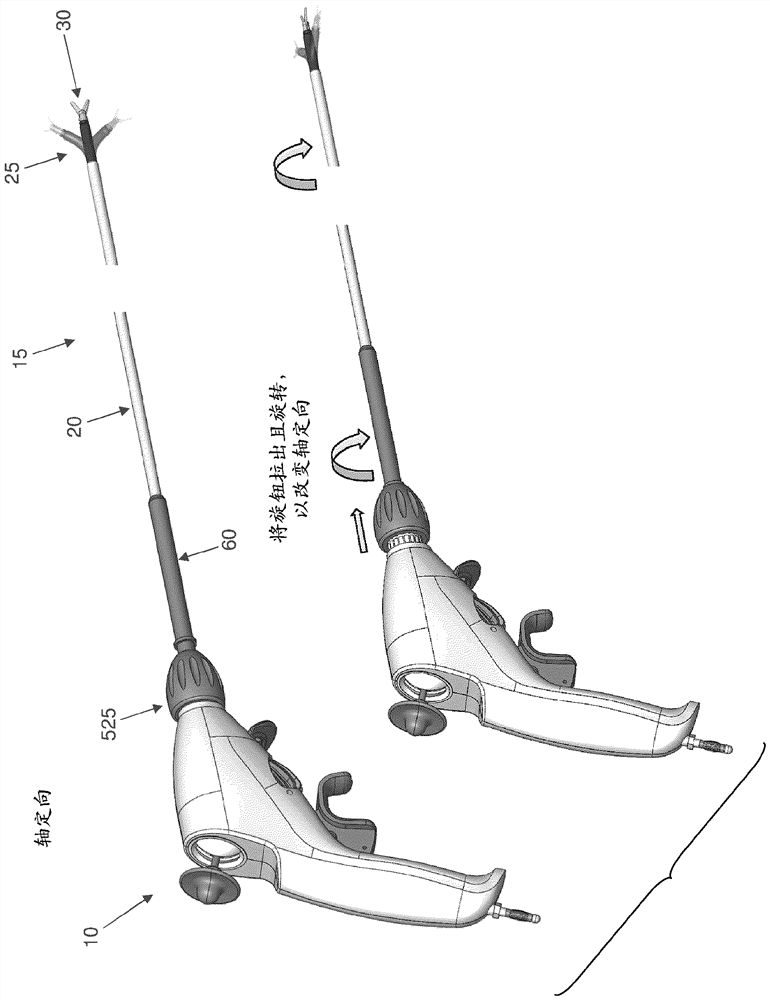
Ablation instrument having deflectable sheath catheters with out-of plane bent tip
The present invention provides devices and methods for the treatment of atrial fibrillation. In one embodiment, a deflectable sheath catheter includes an elongate catheter body having proximal and distal ends, a deflectable end section at the distal end of the catheter body, which upon deflection causes the distal end segment to bend into various curved positions within a plane of deflection, and a bent tip oriented in a direction that is out of the plane of deflection.
Owner:CARDIOFOCUS INC
Device and method for the ablation of fibrin sheath formation on a venous catheter
An indwelling venous catheter and method capable of destroying undesirable cellular growth is provided. The catheter includes a shaft having at least one lumen and adapted to be placed inside a vein for long term use. A plurality of electrodes are positioned near a distal section of the shaft and are adapted to receive from a voltage generator a plurality of electrical pulses in an amount sufficient to cause destruction of cells in the undesirable cellular growth that have grown around the shaft. In one aspect of the invention, a probe is configured to be removably insertable into the at least one lumen and the electrodes are positioned near the distal section of the probe.
Owner:ANGIODYNAMICS INC
Device and Method for the Ablation of Fibrin Sheath Formation on a Venous Catheter
An indwelling venous catheter and method capable of destroying undesirable cellular growth is provided. The catheter includes a shaft having at least one lumen and adapted to be placed inside a vein for long term use. A plurality of electrodes are positioned near a distal section of the shaft and are adapted to receive from a voltage generator a plurality of electrical pulses in an amount sufficient to cause destruction of cells in the undesirable cellular growth that have grown around the shaft. In one aspect of the invention, a probe is configured to be removably insertable into the at least one lumen and the electrodes are positioned near the distal section of the probe.
Owner:ANGIODYNAMICS INC
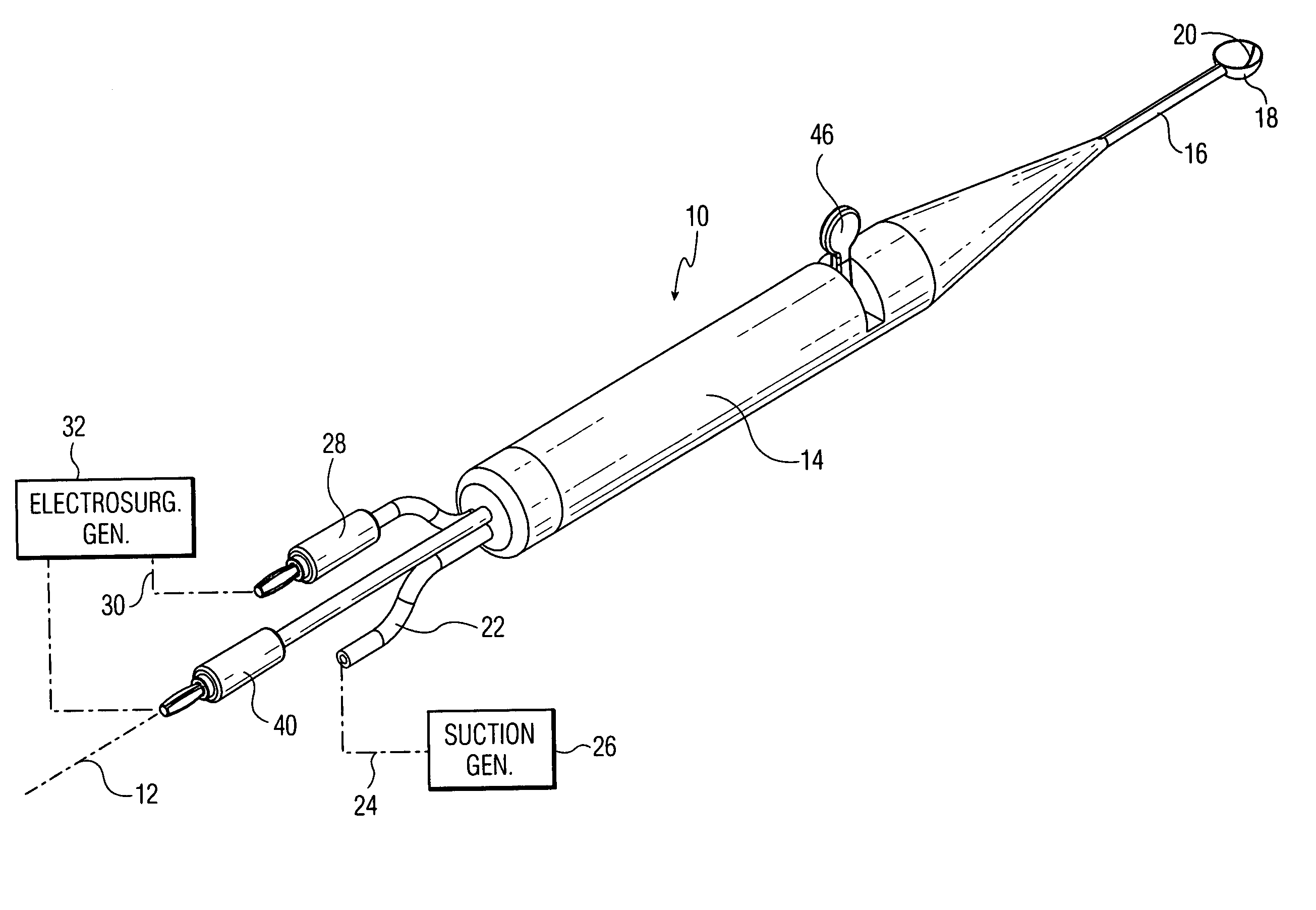
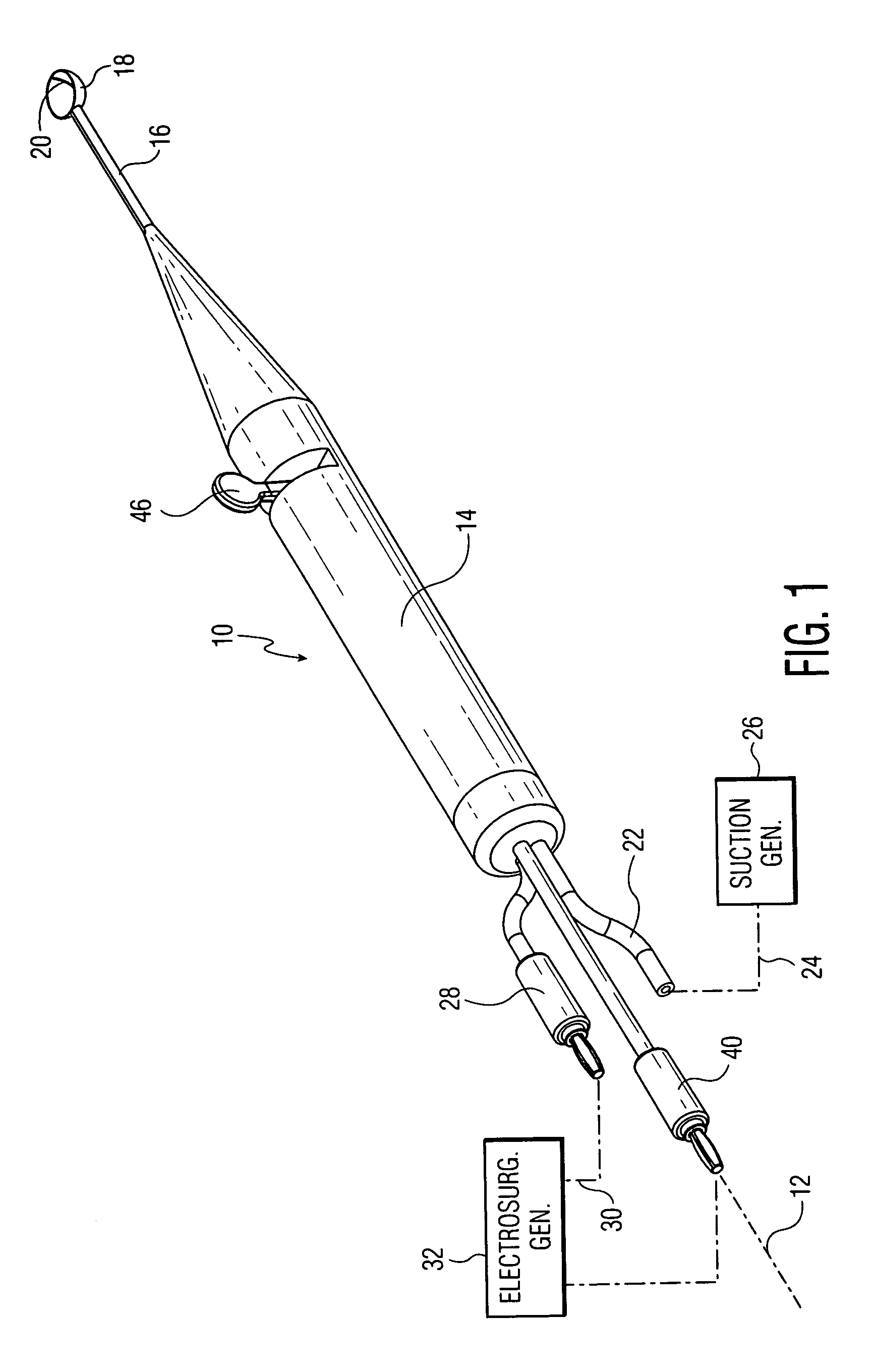
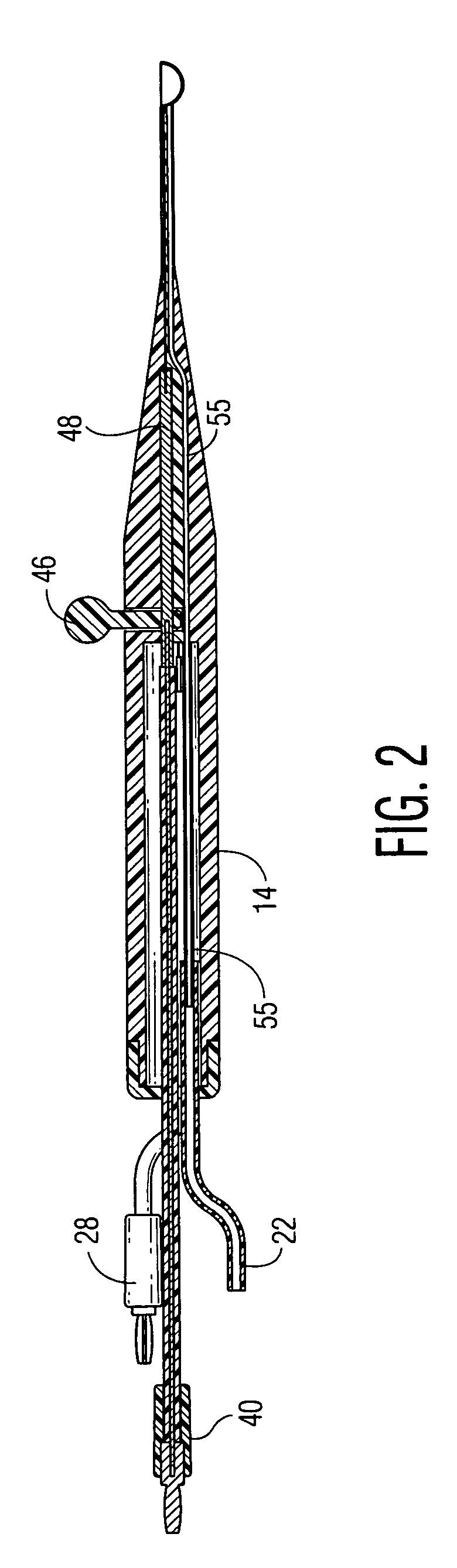
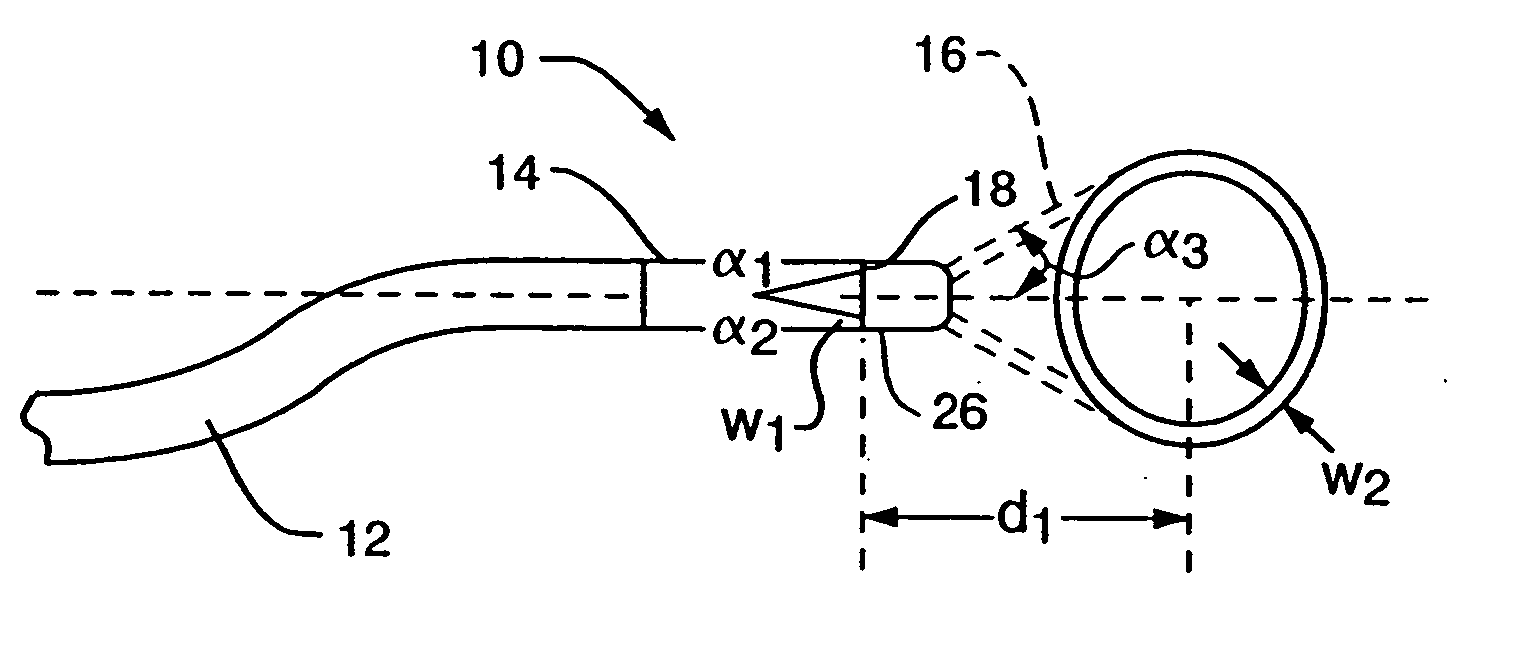
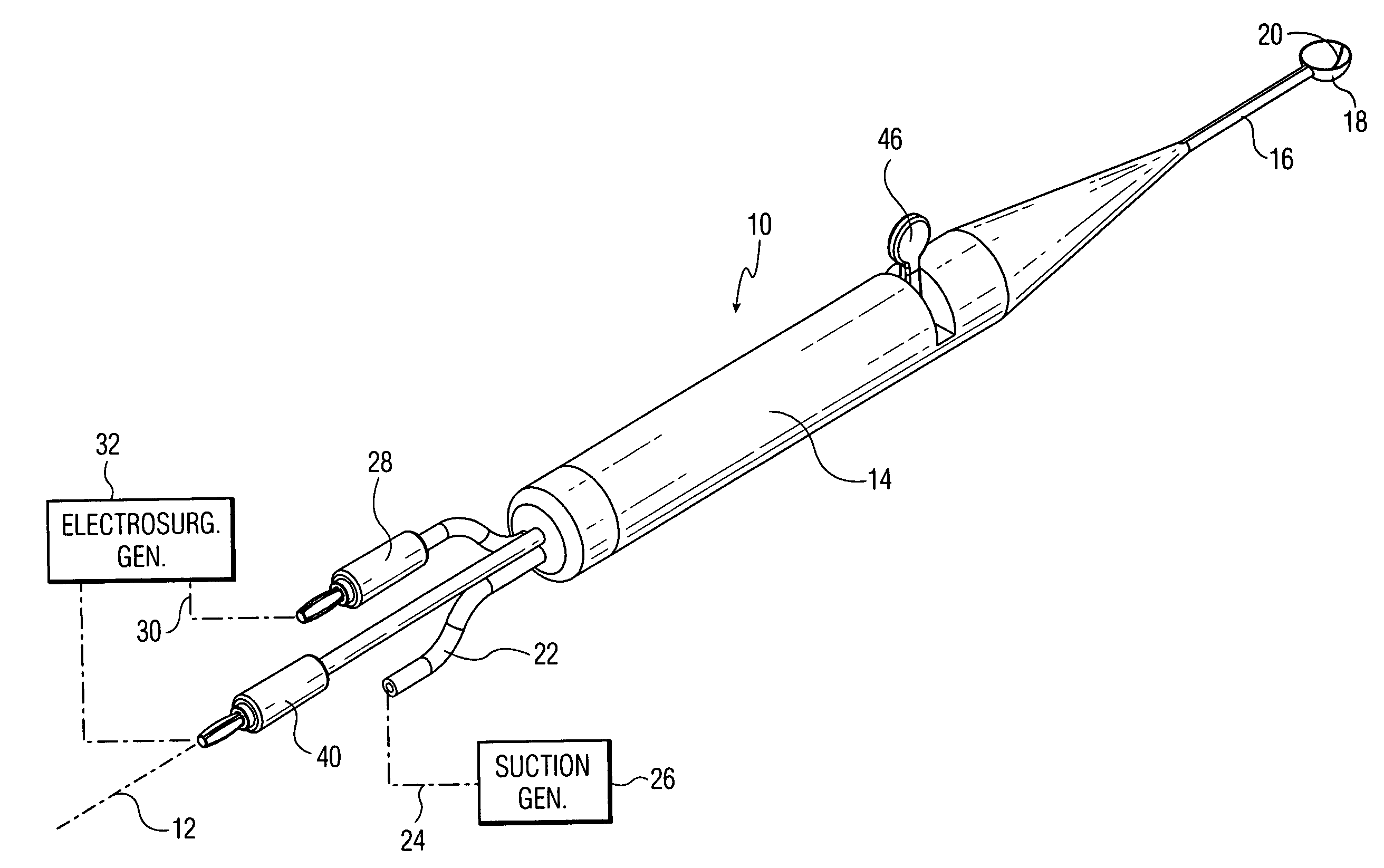
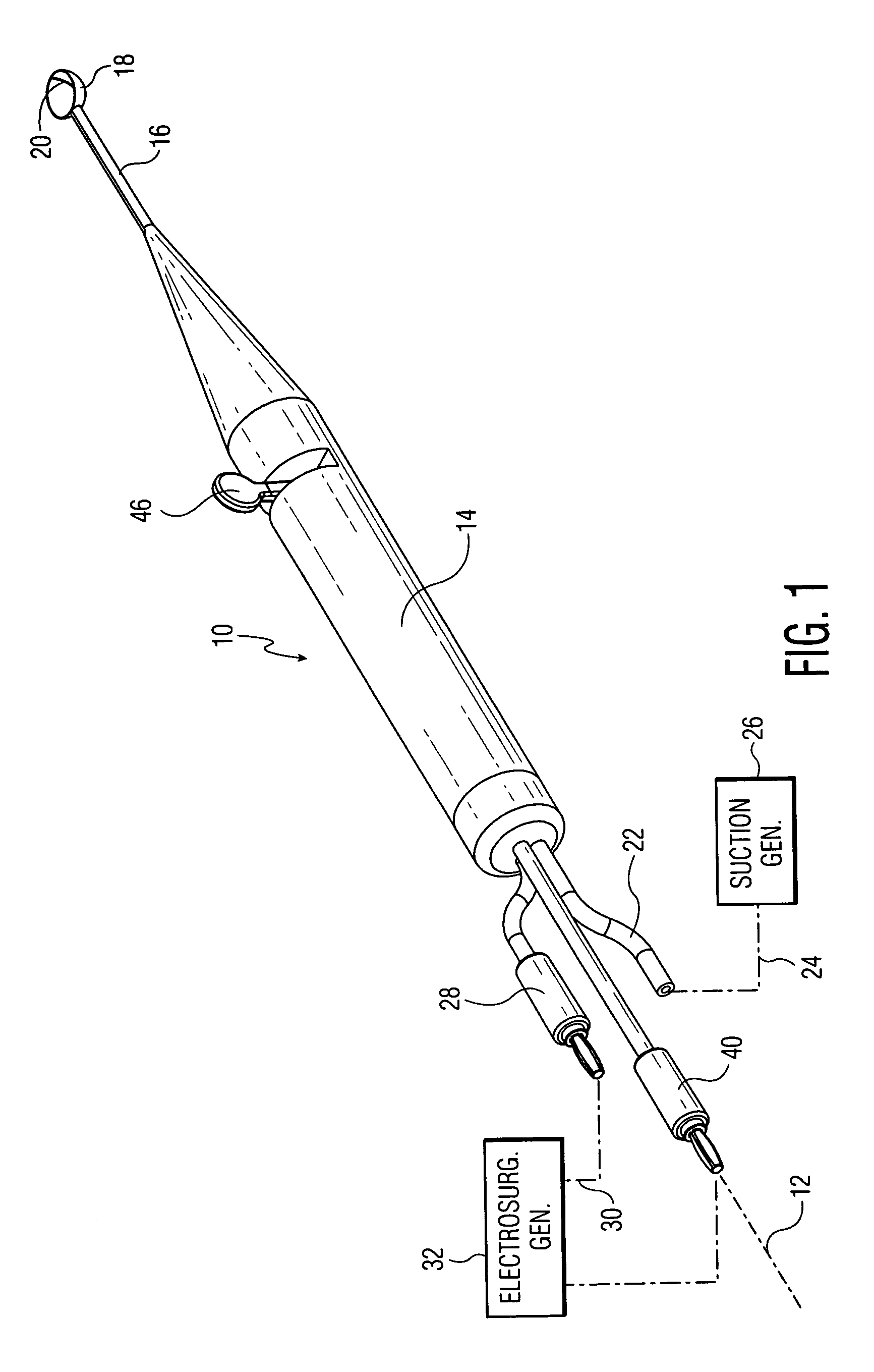
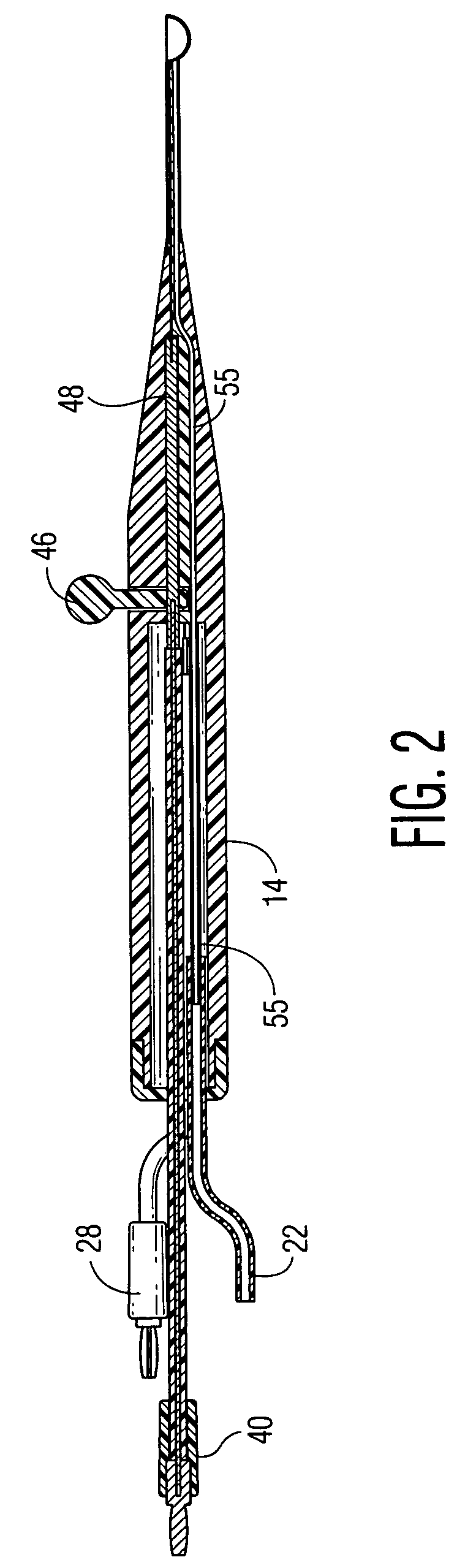
RF intervertebral electrosurgical probe
ActiveUS20060095034A1Small lateral heat spreadAvoid damageSurgical instruments for heatingSurgical pincettesLeading edgeTissue clearing
An electrosurgical instrument for spinal procedures comprises a generally scoop-shaped cup whose periphery is electrically active and is capable of applying RF electrosurgical currents to spinal tissue. The active electrode may comprise an exposed bare wire at the leading edge of the cup. A conduit in a handle section can convey suction to the cup. A tissue clearing member is pivotably mounted on or inside the cup and can be manipulated via a lever on the handle to help dislodge tissue. The tissue clearing member may be a radially-extending vane for rotation in the plane of the cup edge. The tissue clearing member may also be made electrically active thus selectively providing unipolar or bipolar operation.
Owner:ELLIQUENCE
Phototherapeutic wave guide apparatus
InactiveUS20050171520A1Eliminating aberrant wave conductionMinimize and eliminate such damageDiagnosticsCatheterAnnular LesionProximate
Methods and apparatus are disclosed for forming annular lesions in tissue. The methods include introduction of an optical apparatus proximate to a tissue site, via, for example, a catheter. The optical apparatus includes a pattern-forming optical wave guide in communication with a light transmitting optical fiber. Energy is transmitted through the optical fiber, such that radiation is propagated through the optical fiber and the wave guide projects an annular light pattern, e.g., a circle or a halo.
Owner:CARDIOFOCUS INC
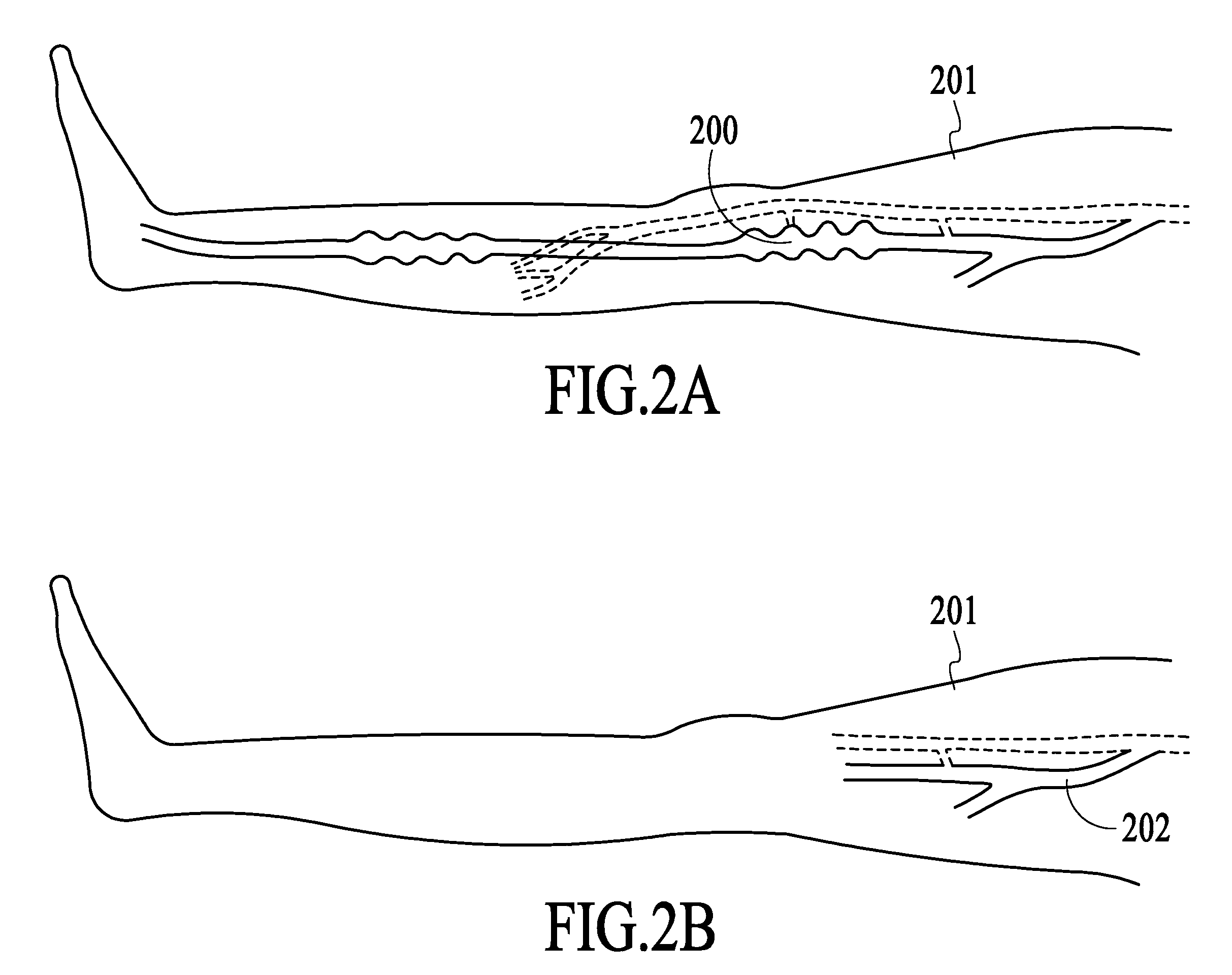
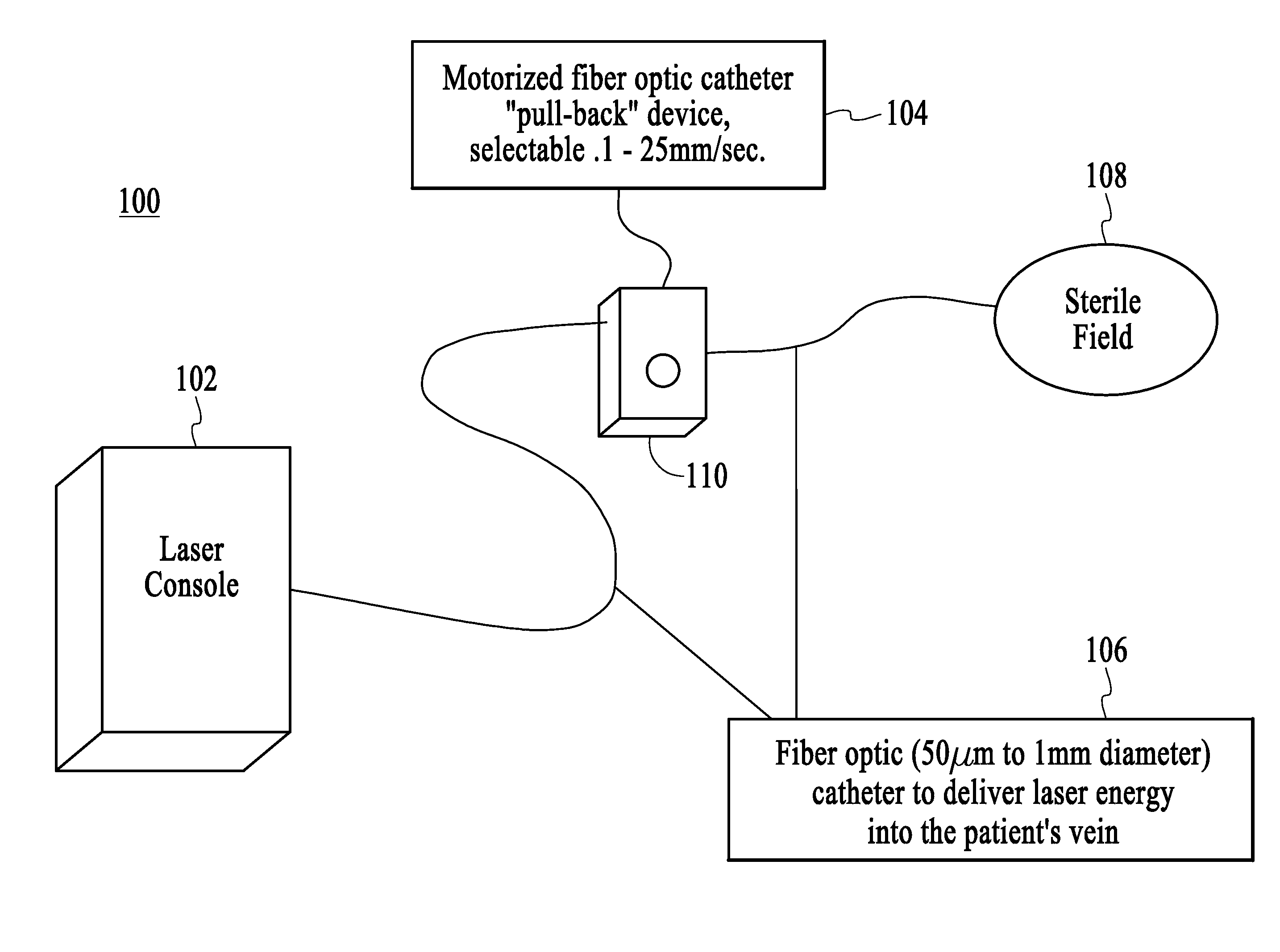
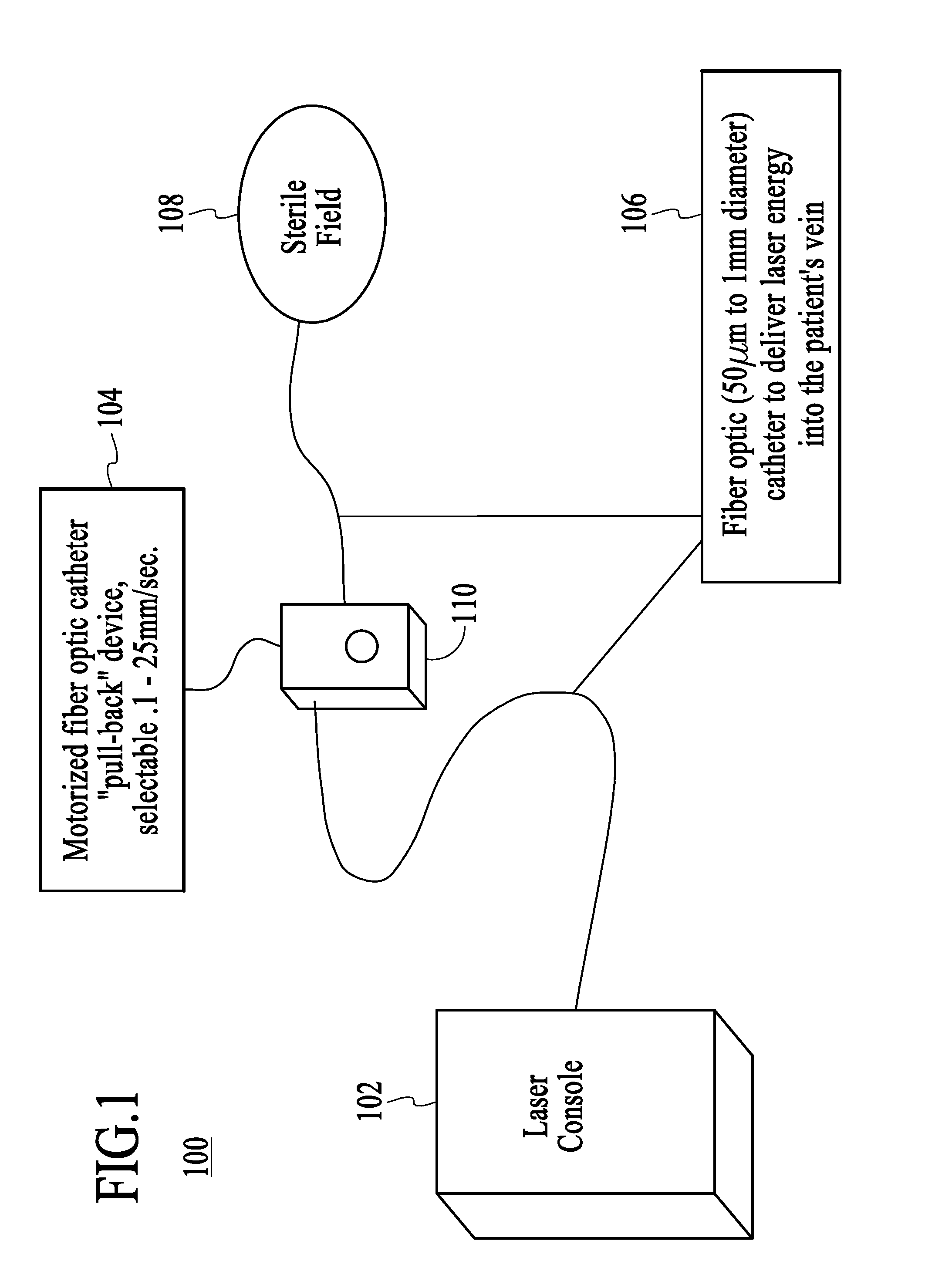
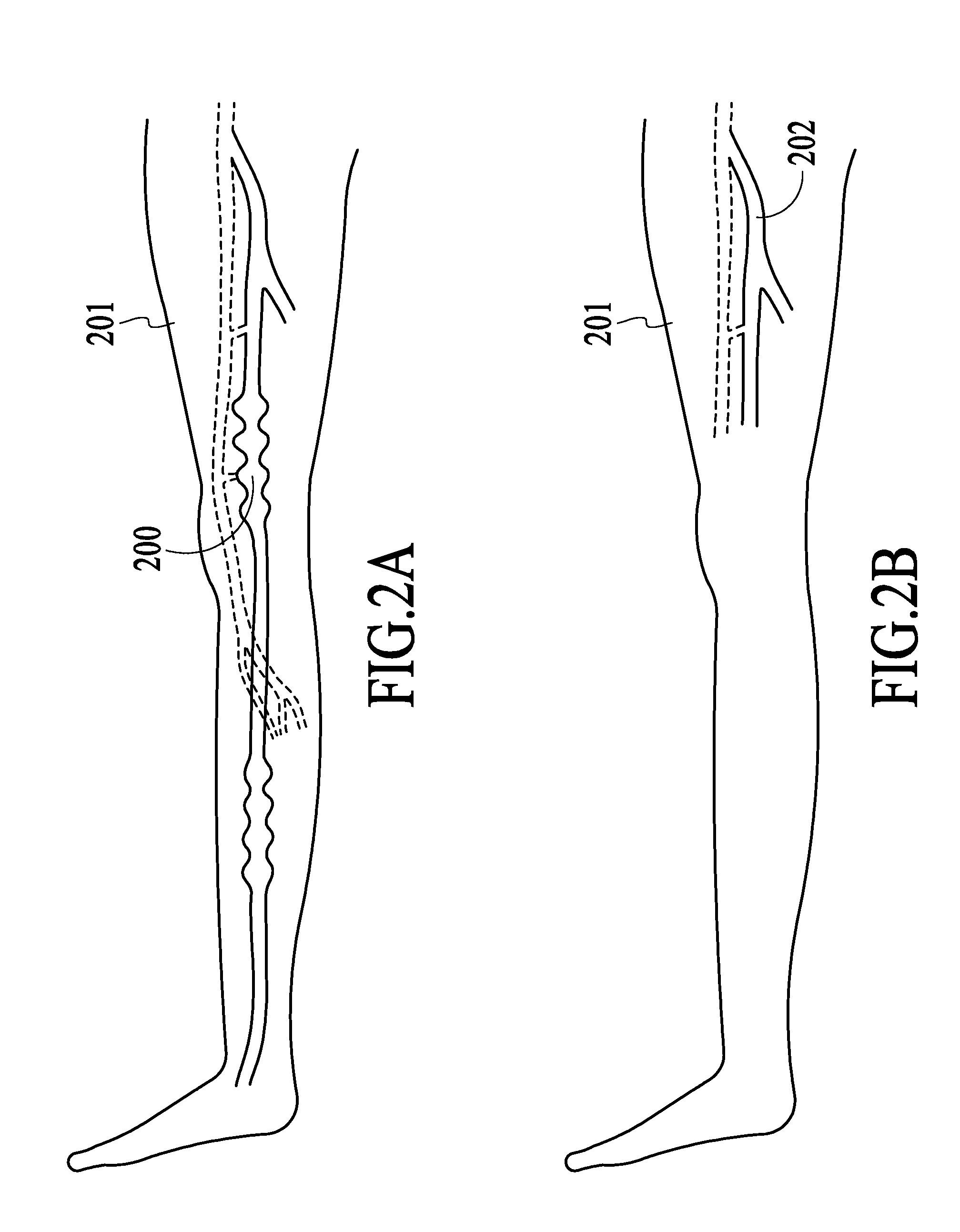
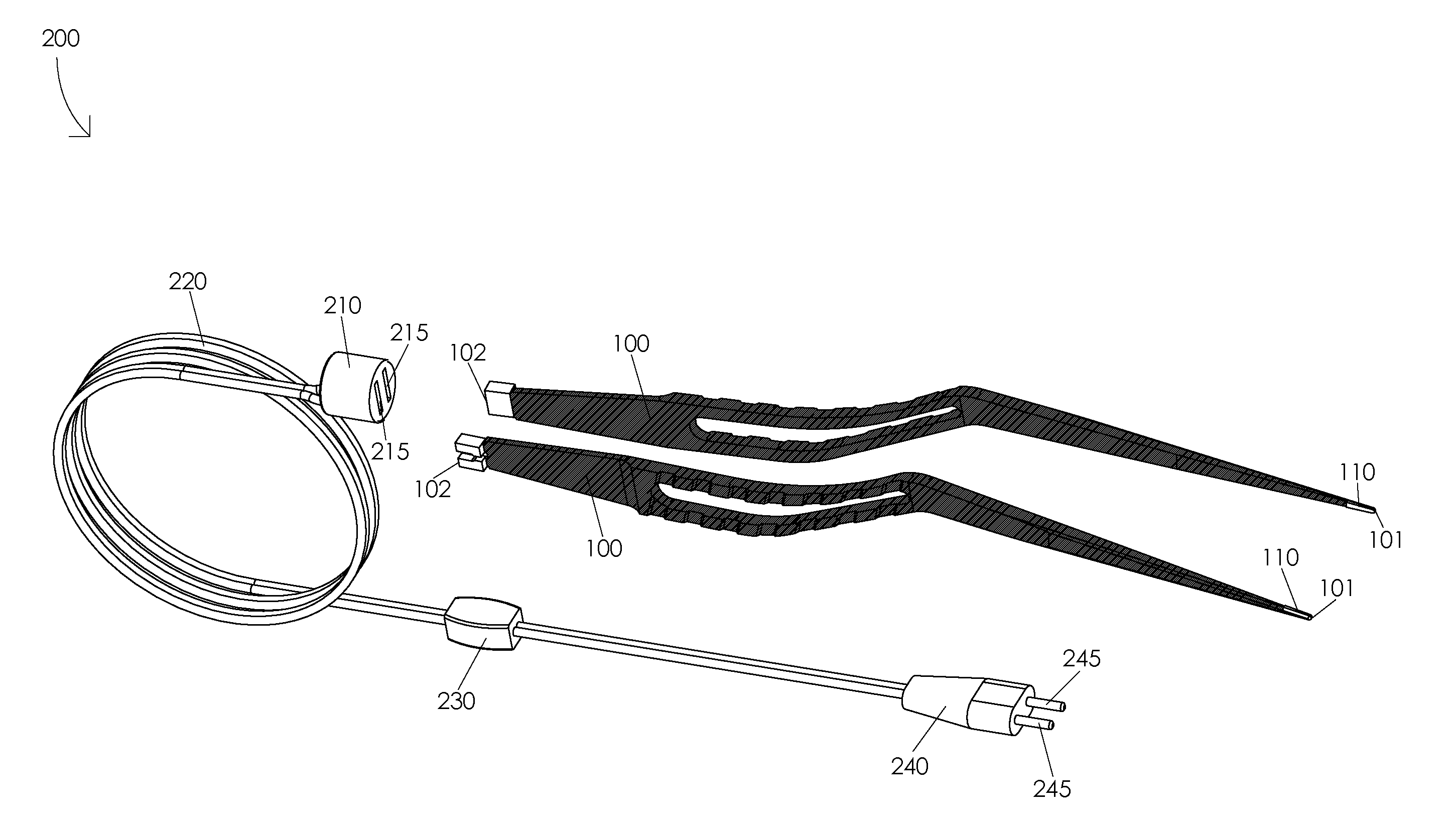
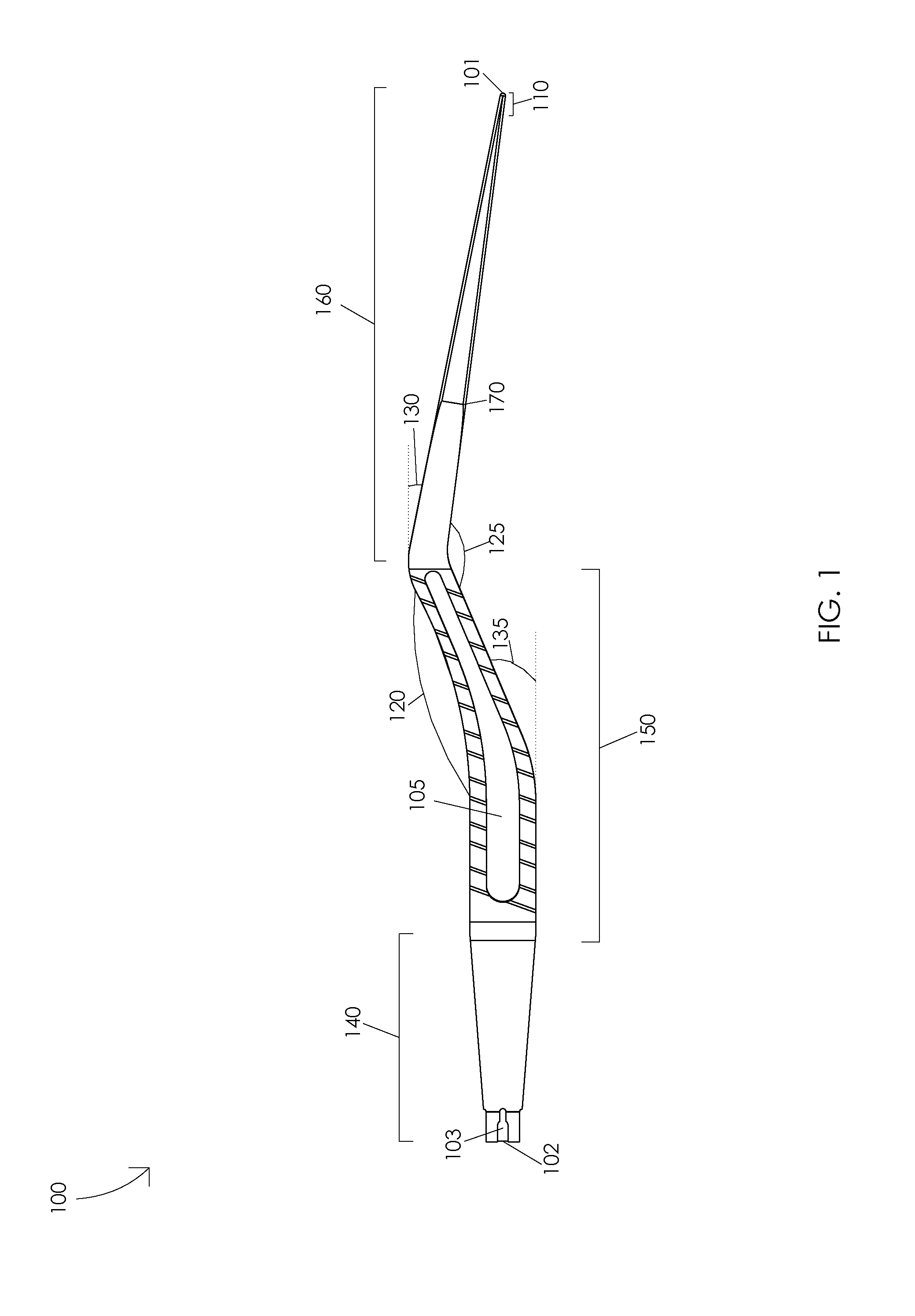
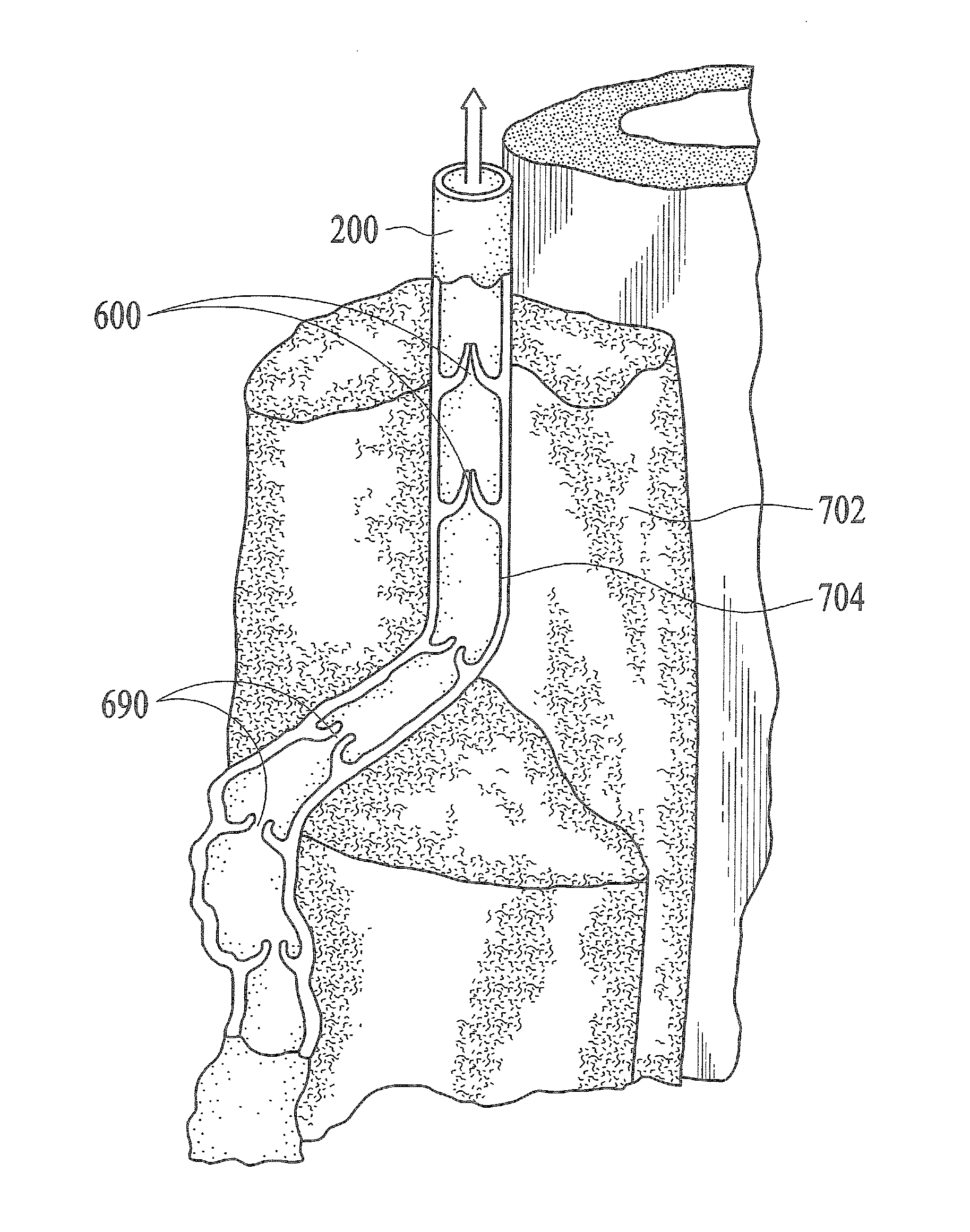
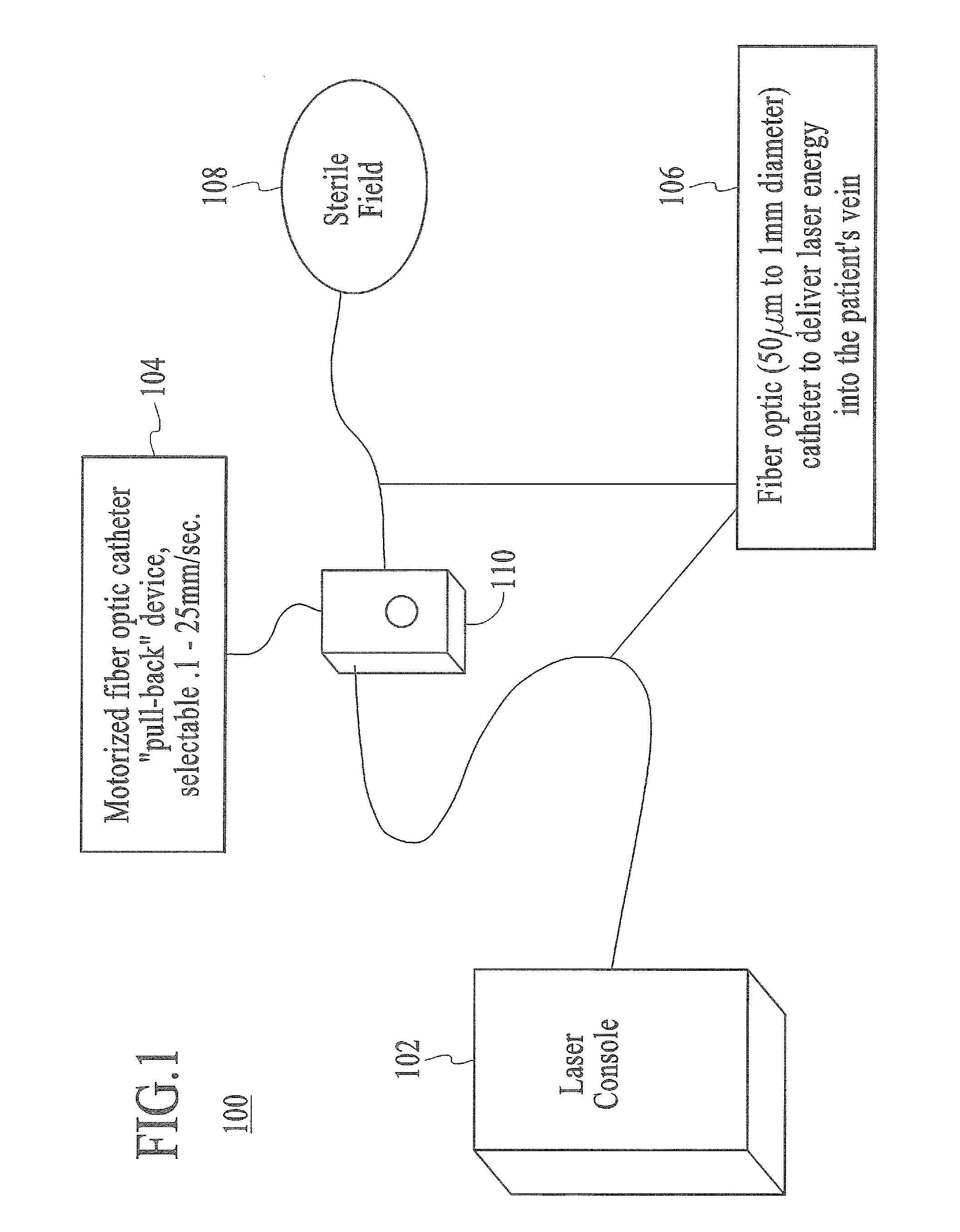
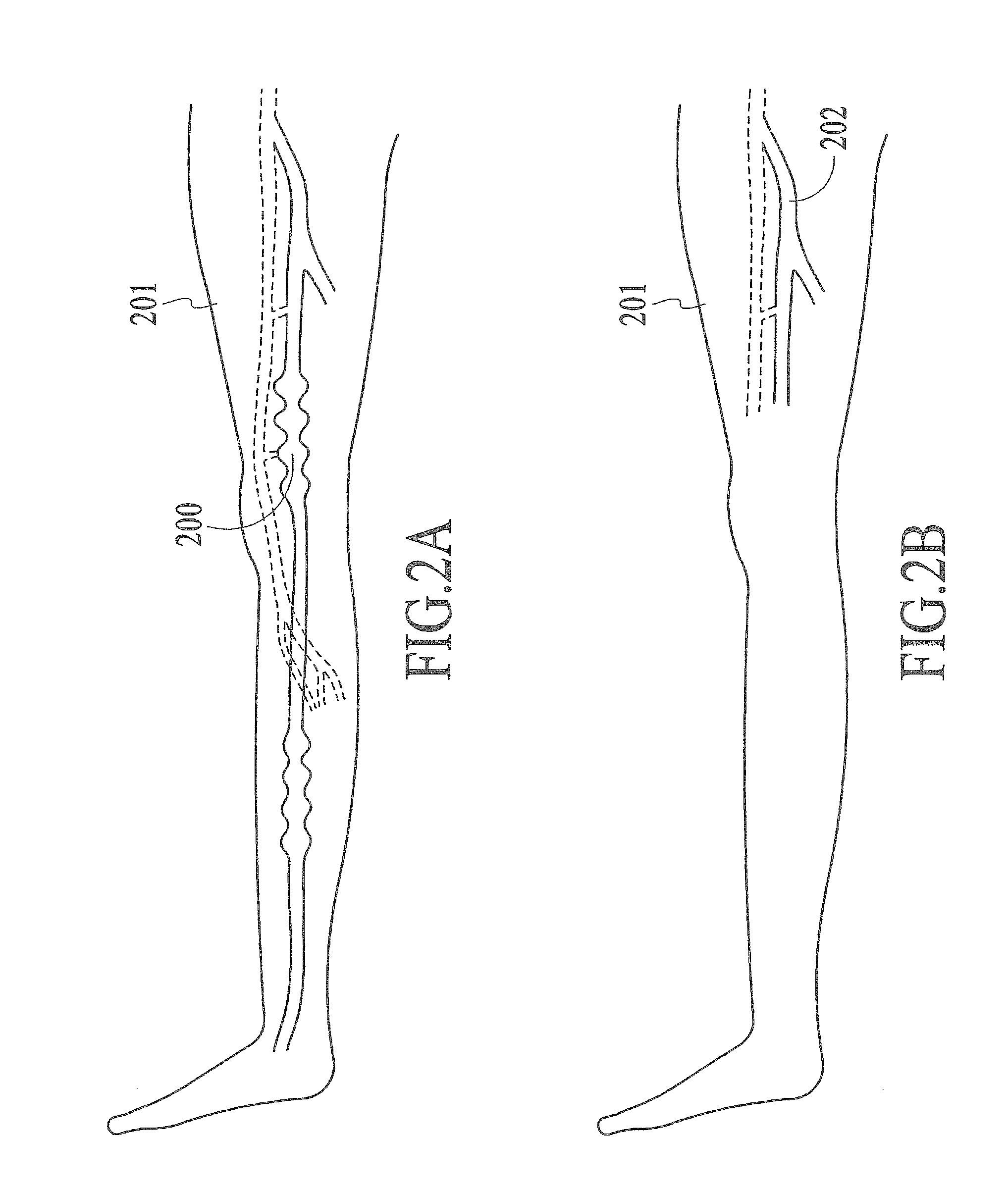
Endovenous laser treatment generating reduced blood coagulation
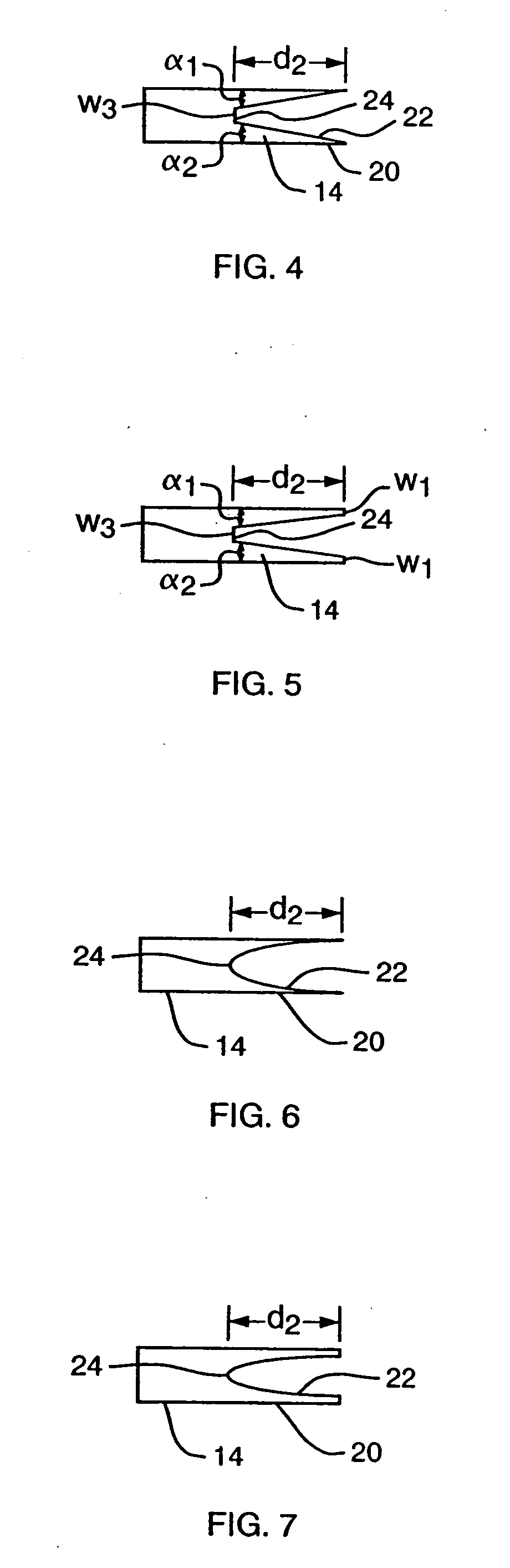
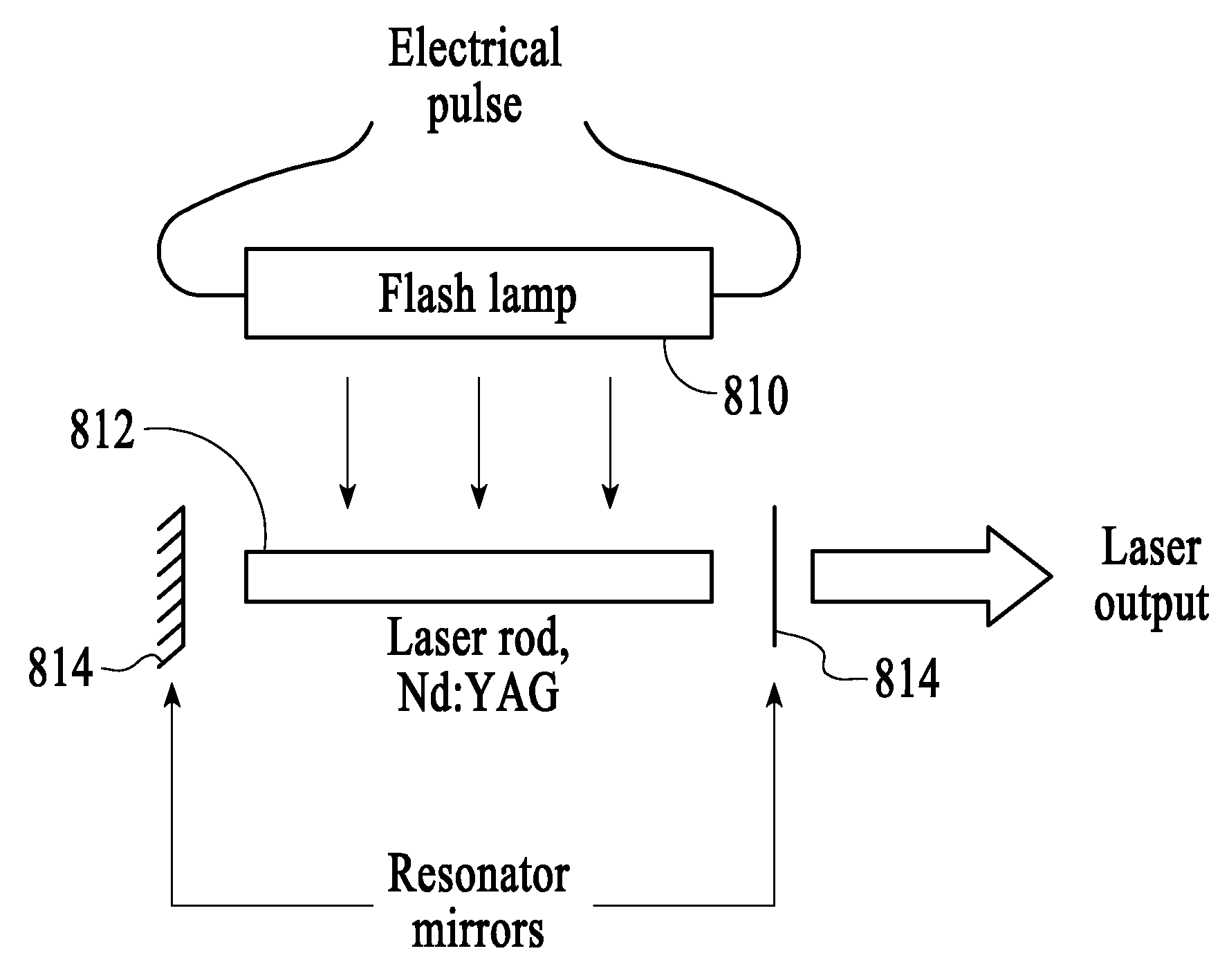
InactiveUS20080021527A1Improve efficacyImprove securityCatheterLight therapyMedicineEndovenous laser treatment
This invention is an improved method and device for treating varicose veins 200 or the greater saphenous vein 202. The method comprises the use of infrared laser radiation in the region of 1.2 to 2.2 um in a manner from inside the vessel 200 or 202 such that the endothelial cells of the vessel wall 704 are damaged and collagen fibers in the vessel wall 704 are heated to the point where they permanently contract, the vessel 200 or 202 is occluded and ultimately resorbed. The device includes a laser 102 delivering laser energy via a fiber optic catheter 300. A motorized pull back device 104 may be used. The laser is preferably operated under laser energy delivery conditions that substantially prevent the formation of coagulum on the energy emitting tip of the fiber.
Owner:COOLTOUCH
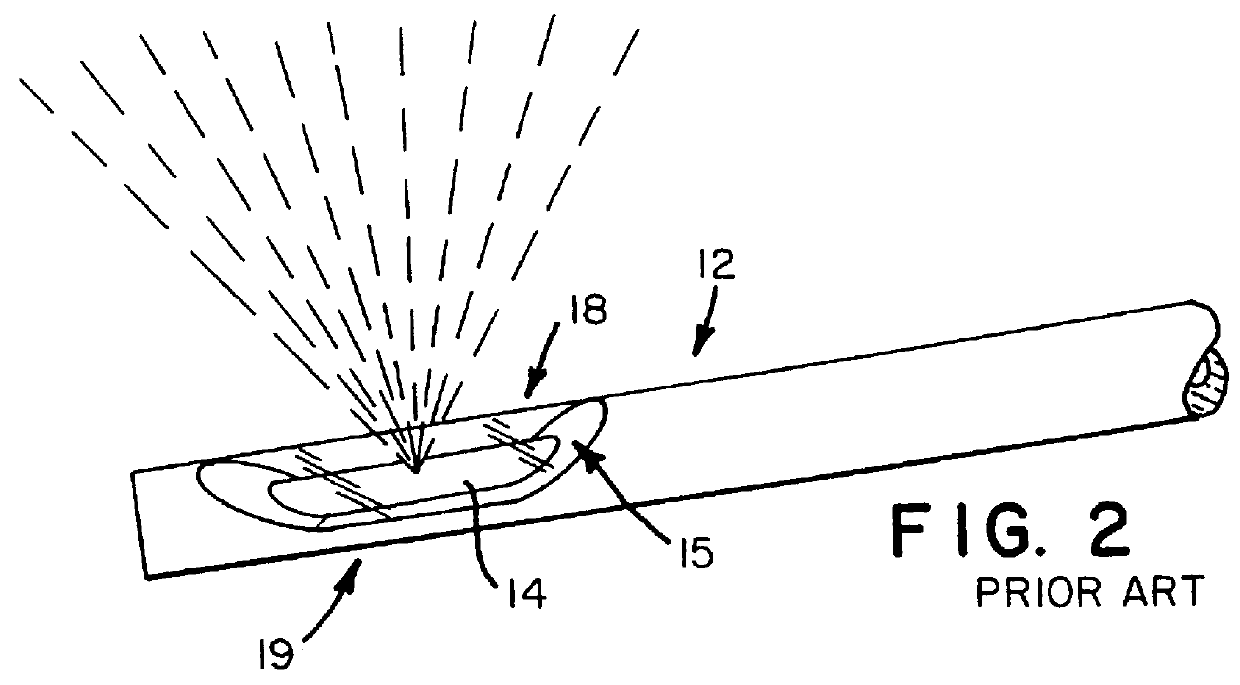
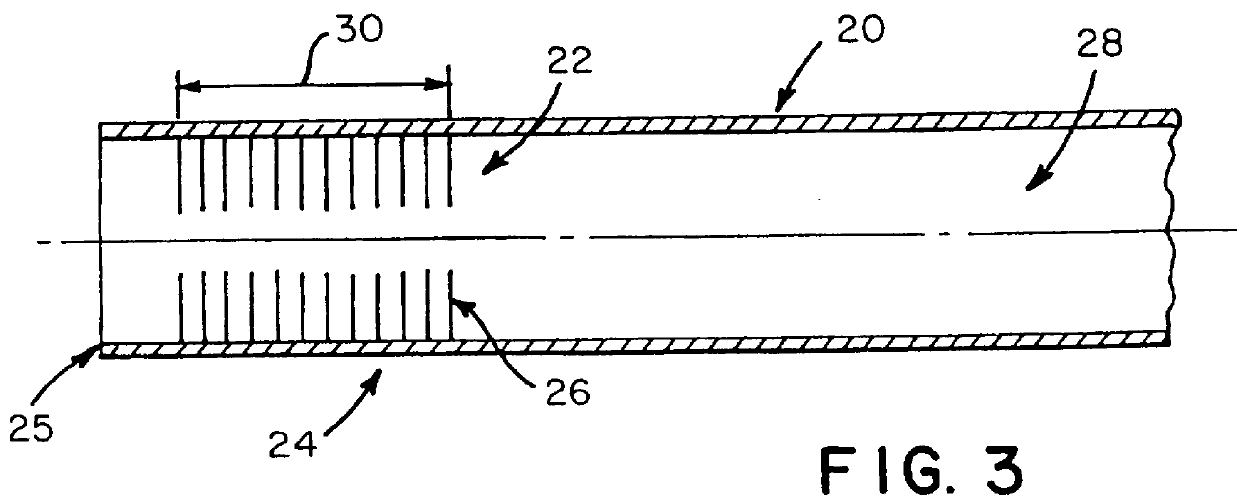
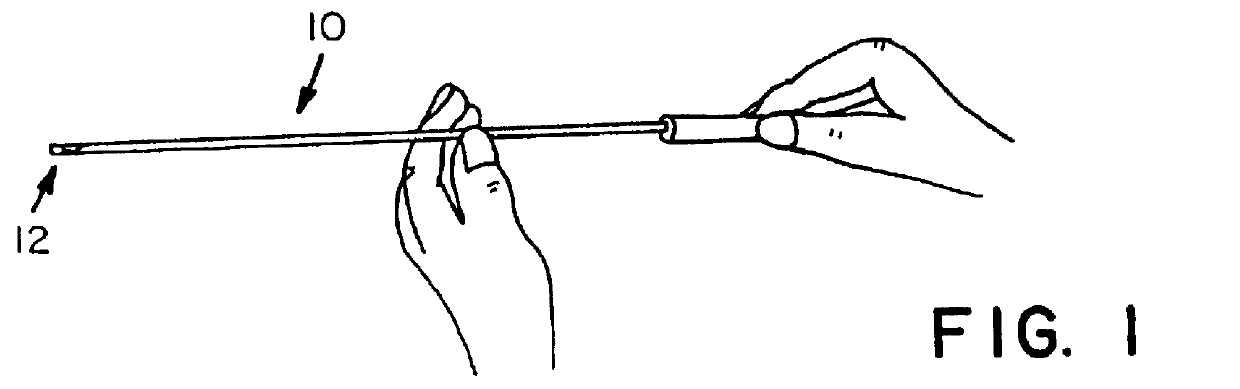
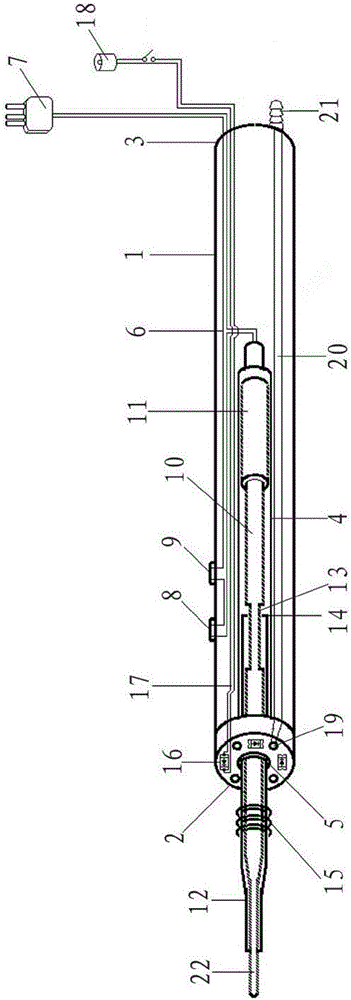
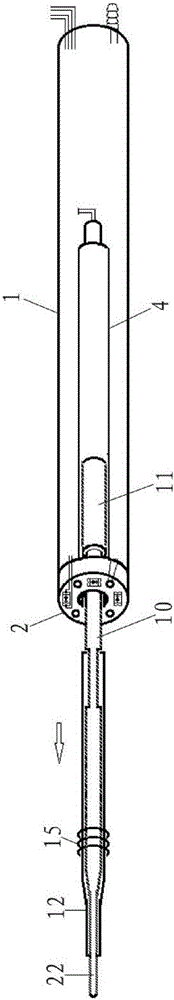
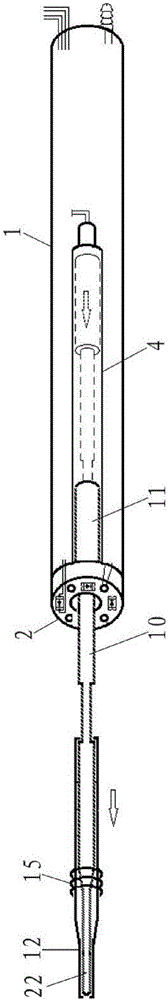
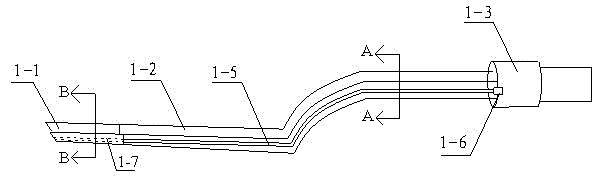
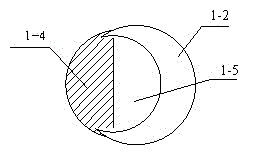
Laser therapy system and method of cutting and vaporizing a tissue body
InactiveUS6126653AEfficient and effective techniqueShorten operation timeDiagnosticsCatheterFiberVaporization
A laser therapy system and method of cutting and vaporizing a tissue body which includes a fiber optic which is inserted into the lumen of a catheter and operable between an extended position wherein a distal end portion of the fiber optic is positioned to cut and vaporize a tissue body and a retracted position wherein the fiber optic is received within the lumen of the catheter. The catheter incorporates at a distal end portion a means for removing attached tissue fragments and the like from the distal end portion of the fiber optic such that tissue fragments stuck to the distal end portion of the fiber optic can be removed while the catheter and fiber remain at the treatment site. This improved system eliminates the need to completely remove the fiber optic during the cutting and vaporization procedure in order to remove the fragments and debris.
Owner:HAJJAR JOHN H
Cardiac ablation catheters for forming overlapping lesions
InactiveUS9033961B2Improve energy transferEnhance the imageUltrasound therapyCatheterCardiac AblationCatheter
Methods and instruments are disclosed for creating lesions in tissue, especially cardiac tissue, for treatment of arrhythmias and the like, by employing an elastic balloon and an energy emitter, which is independently positionable within the lumen of the instrument and adapted to project a series of spots of ablative energy through a transmissive region of the balloon to a target tissue site. The energy emitter preferably is configured such the spots of energy result in a series of lesions formed in the target tissue region when the emitter is activated, the lesions having an average area ranging from about 5 mm2 to about 100 mm2. In one aspect of the invention, percutaneous ablation instruments are disclosed in the form of catheter bodies having one or more balloon structures at the distal end region of the instrument and an energy emitting element, which is independently positionable and rotatable within a lumen of the instrument and adapted to project ablative energy through a transmissive region of the balloon to a target tissue site in contact with, or proximal to, the balloon surface.
Owner:CARDIOFOCUS INC
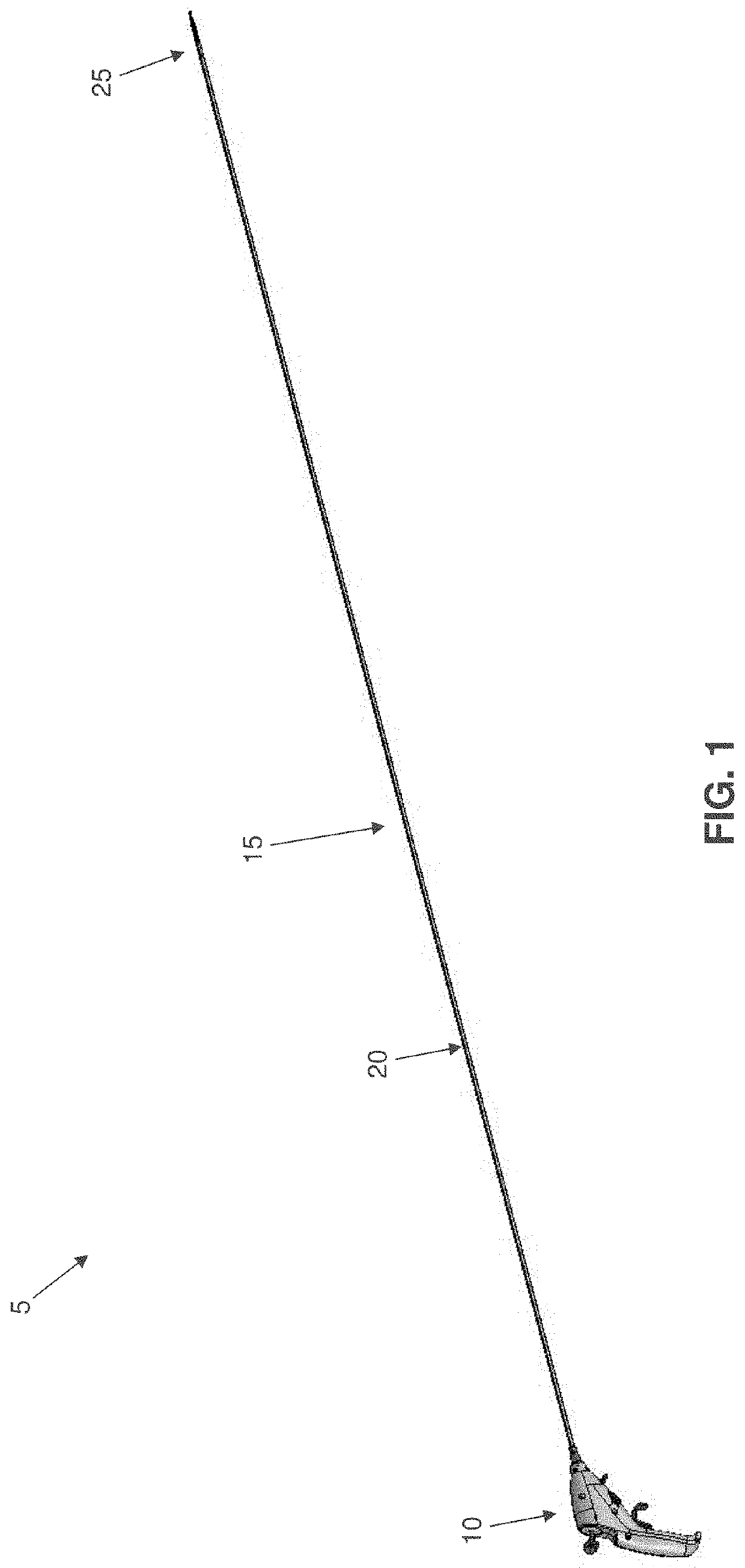
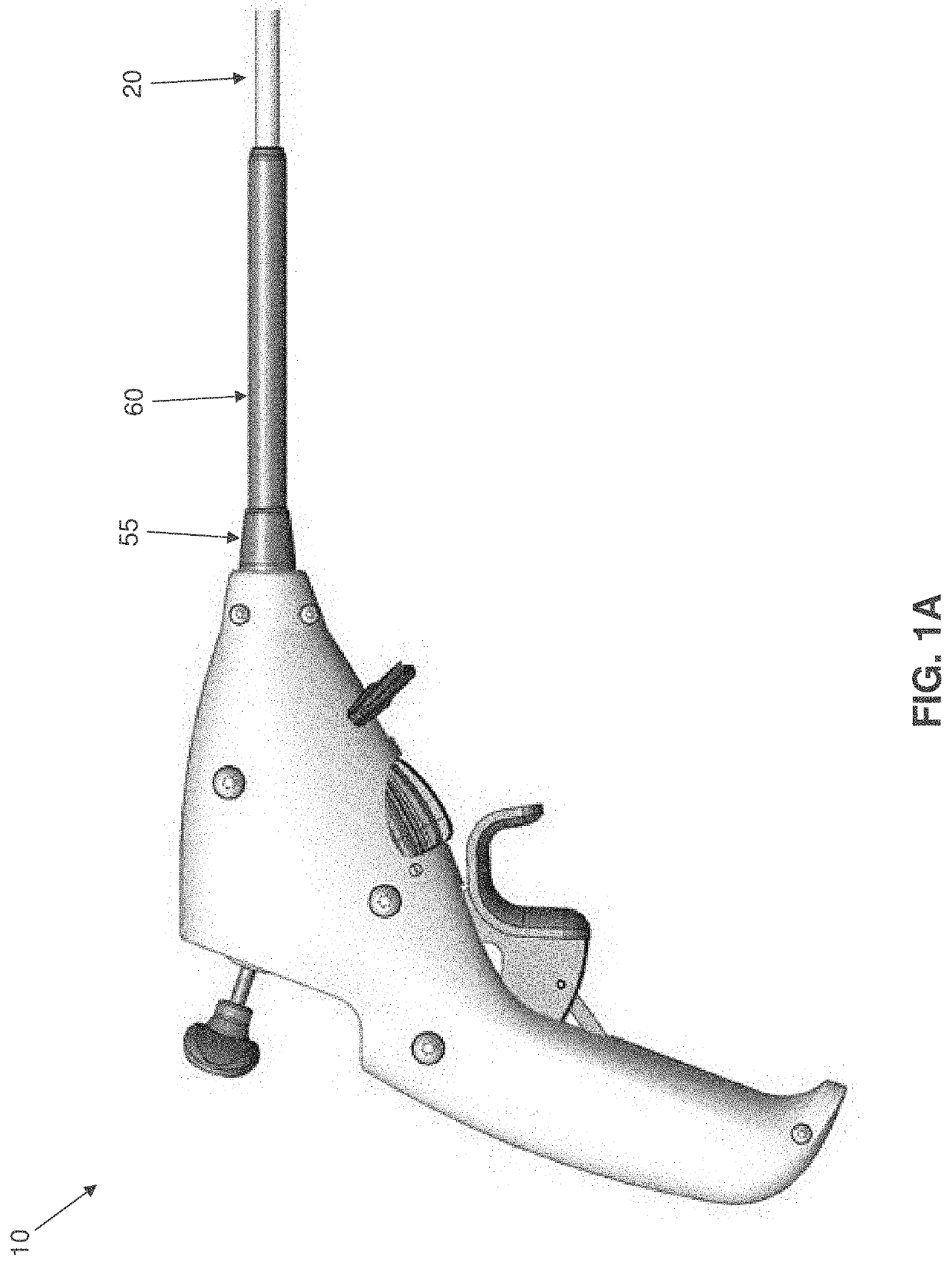
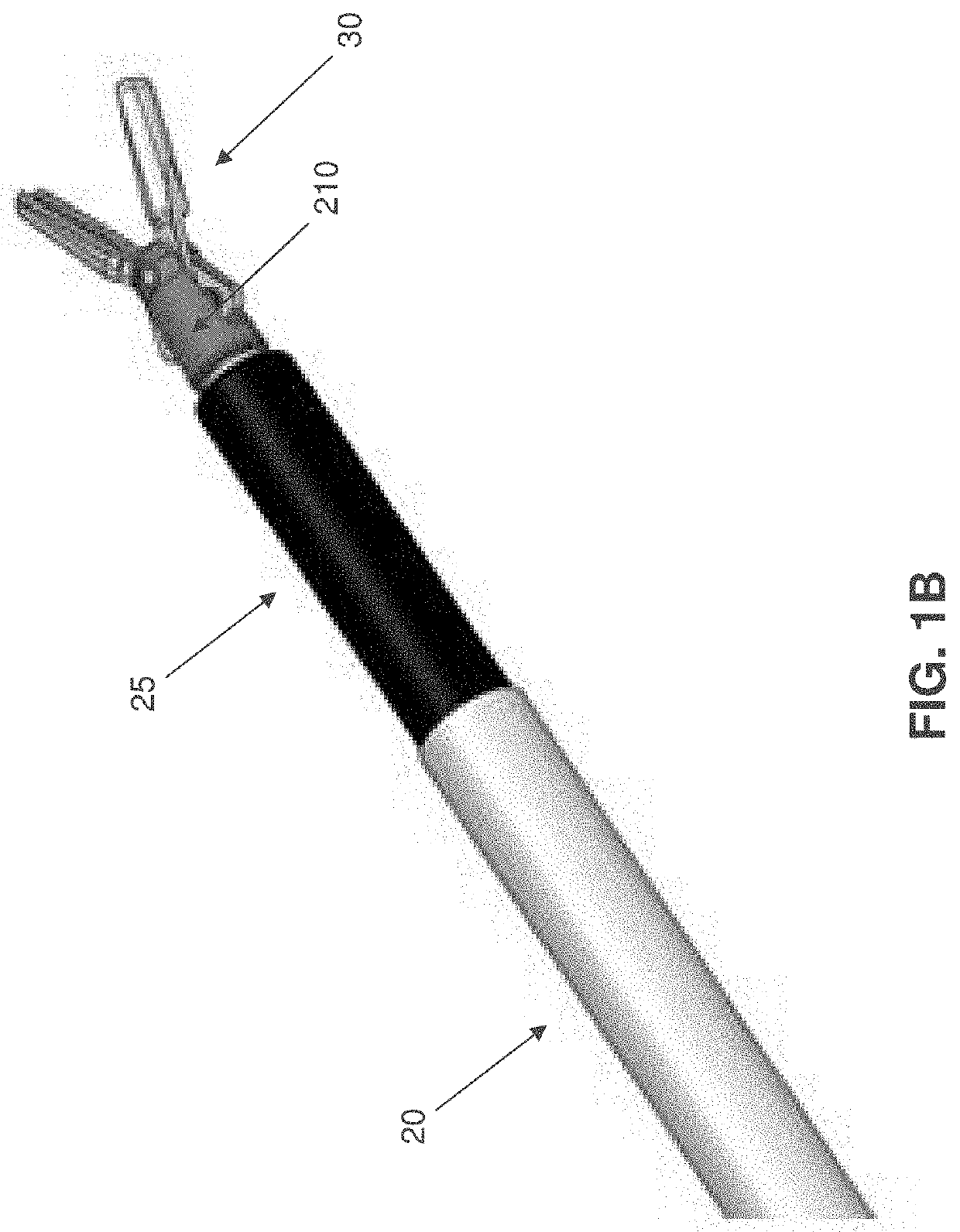
Medical instruments for performing minimally-invasive procedures
Apparatus for performing a minimally-invasive procedure, the apparatus comprising: a shaft having a distal end and a proximal end; a monopolar knife assembly attached to the distal end of the shaft, the monopolar knife assembly comprising a knife; a handle attached to the proximal end of the shaft; wherein the shaft comprises a flexible portion and an articulating portion, wherein the flexible portion extends distally from the handle and the articulating portion extends distally from the flexible portion; wherein at least one articulation cable extends from the handle to the articulating portion, such that when tension is applied to the at least one articulation cable, the articulating portion deflects; wherein an actuation element extends through the shaft from the handle to the knife, such that when the actuation element is moved, the knife is moved; and wherein the actuation element transmits electrical power from the handle to the knife.
Owner:LUMENDI LTD
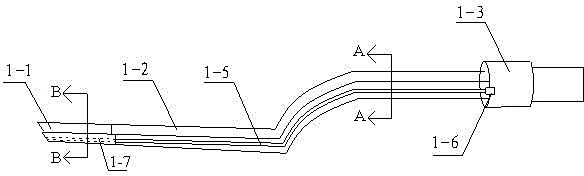
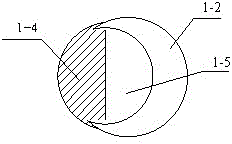
Electric coagulation forcep system convenient to clean
InactiveCN104013462ASimple structureReduce volumeCleaning using toolsSurgical instruments for heatingSemi openEngineering
The invention discloses an electric coagulation forcep system convenient to clean. The electric coagulation forcep system comprises a forcep body and a base. The forcep body comprises forcep tips and forcep rods, and the electric coagulation forcep system is characterized in that semi-opened suction grooves are formed in the forcep rods, the front ends of the suction grooves are connected with suction channels in the forcep tips, and inserting openings are formed in outlets of the rear ends of the suction grooves; the system further comprises sealing devices matched with the suction grooves, and the sections of the suction grooves are semicircular. The semi-opened suction grooves are formed in the forcep body, and when the system is used, the sealing devices are tightly pressed on the suction grooves, and the suction grooves form a sealed space. When hematocele needs to be removed, the system can work only by connecting the inserting openings and a suction machine in an operating room. After the system is used, the sealing devices can be taken down, and then the suction grooves are cleaned. The system is simple in principle, the hemostasis and suction work can be executed at the same time, and cleaning is convenient.
Owner:WENZHOU ZHICHUANG TECH
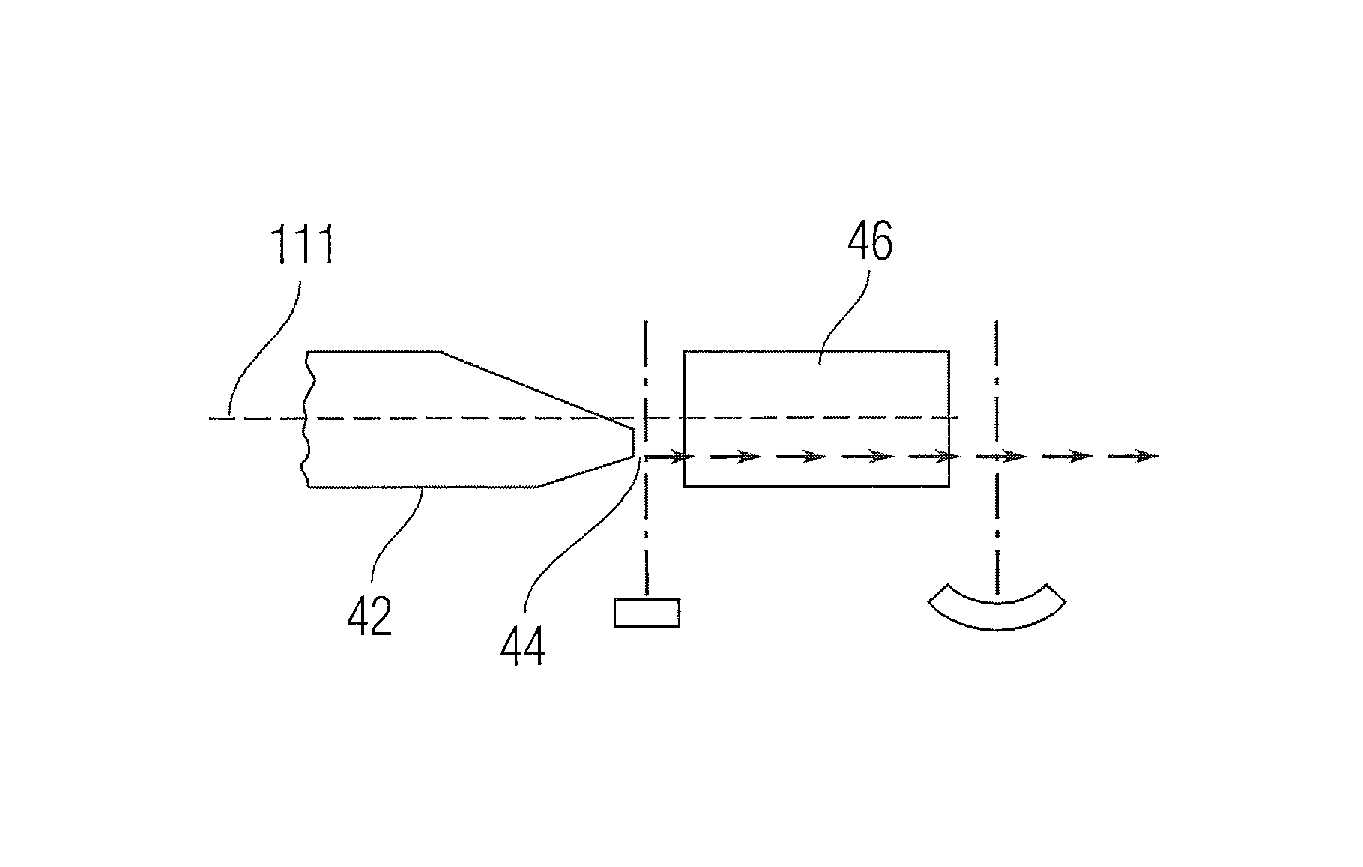
Systems and method for protection of optical system of laser-based apparatus
InactiveUS20150150649A1Reduce pollutionAvoid problemsInstrument probesBoring toolsOptic systemLaser beams
In an apparatus for directing a laser beam to a dental treatment area, where the apparatus includes a hand piece having an optical subsystem including a turning mirror for directing a laser beam to a treatment area via an orifice of the hand piece, a fluid supply subsystem creates a fluid flow within the hand piece proximate the turning mirror so as to mitigate contamination thereof.
Owner:CONVERGENT DENTAL INC
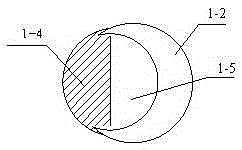
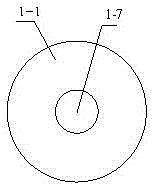
Multifunctional high-frequency electrosurgical pencil
PendingCN106691581ASimple structureReasonable designSurgical instruments for heatingInstrument probesElectricitySurgical operation
The invention provides a multifunctional high-frequency electrosurgical pencil. The multifunctional high-frequency electrosurgical pencil is characterized in that a head end and a tail end are arranged at two ends of a shell; a conductive slide is arranged in the shell, one end of the conductive slide is connected with the head end, and an electrode through hole is formed in the head end and in the position where the head end is connected with the conductive slide; an electrode is arranged in the conductive slide, and a knife head and a conductive limit portion are arranged at two ends of the electrode; one end of the electrode with the knife head extends out of the electrode through hole, and the conductive limit portion is conductively contacted with the conductive slide; the electrode and the knife head are sleeved with an insulating cleaning blade, one end of the knife head extends out of the cleaning blade, and a limit section is arranged on the electrode; LED lamps and blow holes are arranged in the head end, and the blow holes are connected with an air inlet connector via an air duct. The cleaning blade is used for cleaning the knife head; the LED lamps are used for lighting the surgical field; the electrode is telescopic and is suitable for different situations, and frequent exchanging of the knife head is not needed; the air blowing function is arranged, and air blowing can be performed during surgical operation to remove smoke, bleeding, drainage and the like of the surgical field.
Owner:DALIAN CORVIVO MEDICAL CO LTD
Endovenous Laser Treatment Generating Reduced Blood Coagulation
Inducing thrombolysis of thermally induced thrombus occurring during endovenous ablation of varicose veins by introducing an optical fiber laser deliver device with optical fiber portion and with an energy emitting tip at its distal end into the varicosed vein to be treated, emitting pulsed, laser energy with sufficient energy to close and destroy varicose veins to the emitting tip of the optical fiber laser delivery device, thereby inducing laser thrombolysis of coagulated blood which accumulates at the energy emitting tip of the fiber when the fiber is caused to emit energy in the presence of uncoagulated blood and minimizing adverse effects associated with thermally induced thrombus within a varicose vein.
Owner:NEW STAR LASERS
Electric coagulation forceps system with open-type suction groove
InactiveCN104013463ASimple structureThe principle is simpleCleaning using toolsSurgical instruments for heatingHematoceleForceps
The invention discloses an electric coagulation forceps system with an open-type suction groove. The electric coagulation forceps system comprises a forceps body and a base. The forceps body comprises a forceps tip and a forceps rod and is characterized in that the half-opened type suction groove is formed in the forceps rod, the front end of the suction groove is connected with an suction channel inside the forceps tip, an outlet in the rear end of the suction groove is provided with a socket, the system further comprises a sealing device matched with the suction groove, and the section of the suction groove is semicircular. The half-opened suction groove is formed in the forceps body; when the electric coagulation forceps system is used, the sealing device is tightly pressed on the suction groove so that the suction groove can form a closed pace; when hematocele needs to be eliminated, the system can work as long as the socket is connected with a suction machine in an operating room; after the system is used, the sealing device can be taken down, and a user only needs to wash the suction groove. The electric coagulation forceps system is simple in principle, can simultaneously execute hemostasis work and suction work, and is convenient to clean.
Owner:WENZHOU ZHICHUANG TECH
RF intervertebral electrosurgical probe
ActiveUS7137982B2Accurate interactionMinimizes and avoids damageSurgical instruments for heatingSurgical pincettesLeading edgePower flow
An electrosurgical instrument for spinal procedures comprises a generally scoop-shaped cup whose periphery is electrically active and is capable of applying RF electrosurgical currents to spinal tissue. The active electrode may comprise an exposed bare wire at the leading edge of the cup. A conduit in a handle section can convey suction to the cup. A tissue clearing member is pivotably mounted on or inside the cup and can be manipulated via a lever on the handle to help dislodge tissue. The tissue clearing member may be a radially-extending vane for rotation in the plane of the cup edge. The tissue clearing member may also be made electrically active thus selectively providing unipolar or bipolar operation.
Owner:ELLIQUENCE
Medical instruments for performing minimally-invasive procedures
The present invention provides an apparatus for performing a minimally-invasive procedure. The apparatus comprising: a shaft having a distal end and a proximal end; a monopolar knife assembly attachedto the distal end of the shaft, the monopolar knife assembly comprising a knife; a handle attached to the proximal end of the shaft; wherein the shaft comprises a flexible portion and an articulatingportion, wherein the flexible portion extends distally from the handle and the articulating portion extends distally from the flexible portion; at least one articulation cable extends from the handleto the articulating portion, such that when tension is applied to the at least one articulation cable, the articulating portion deflects; an actuation element extends through the shaft from the handle to the knife, such that when the actuation element is moved, the knife is moved; and the actuation element transmits electrical power from the handle to the knife.
Owner:LUMENDI LTD
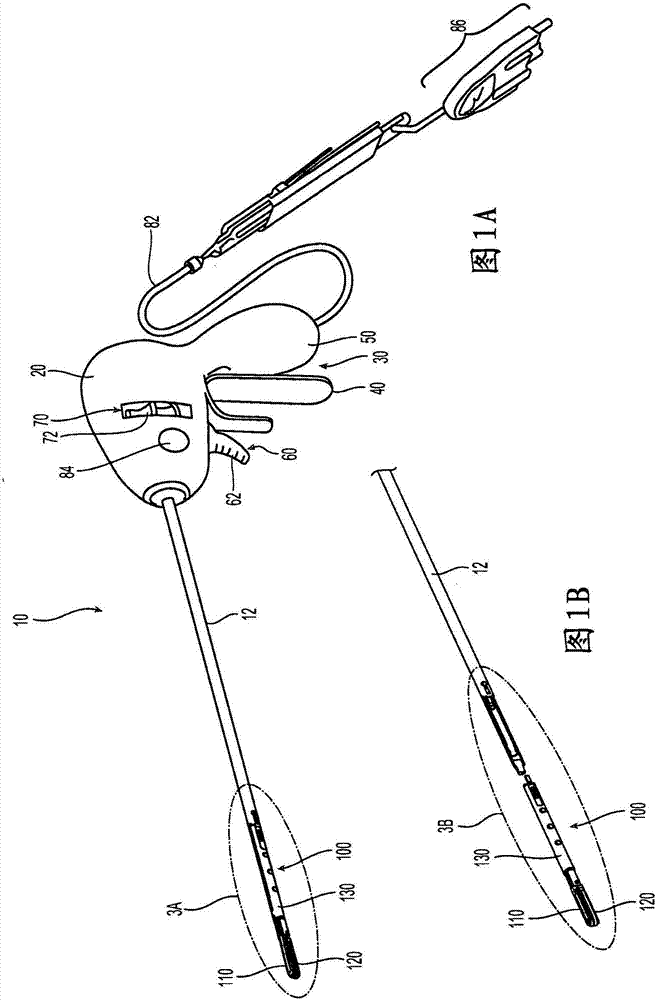
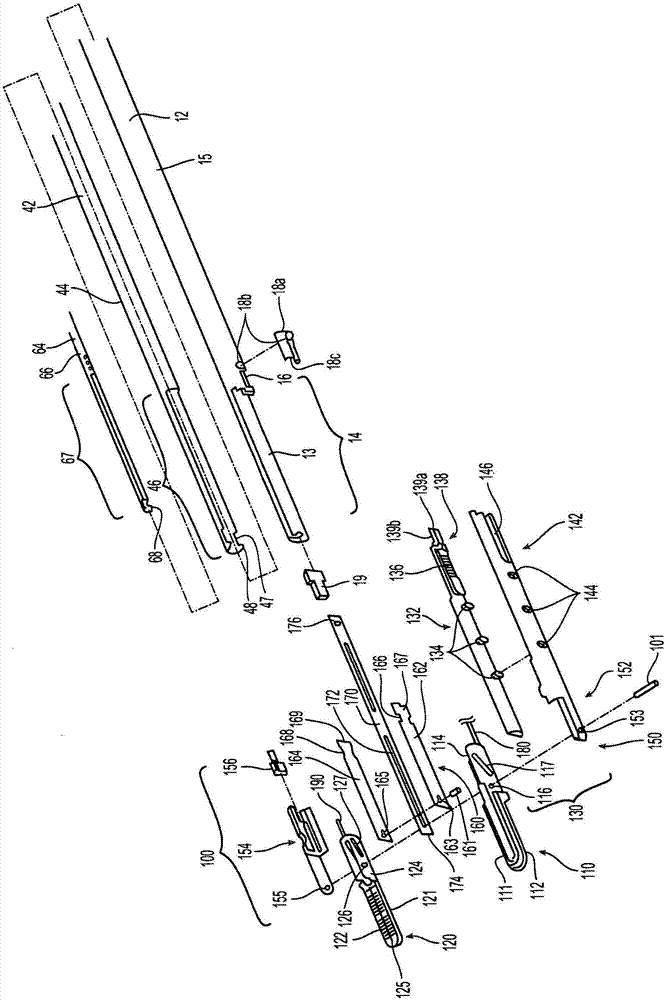
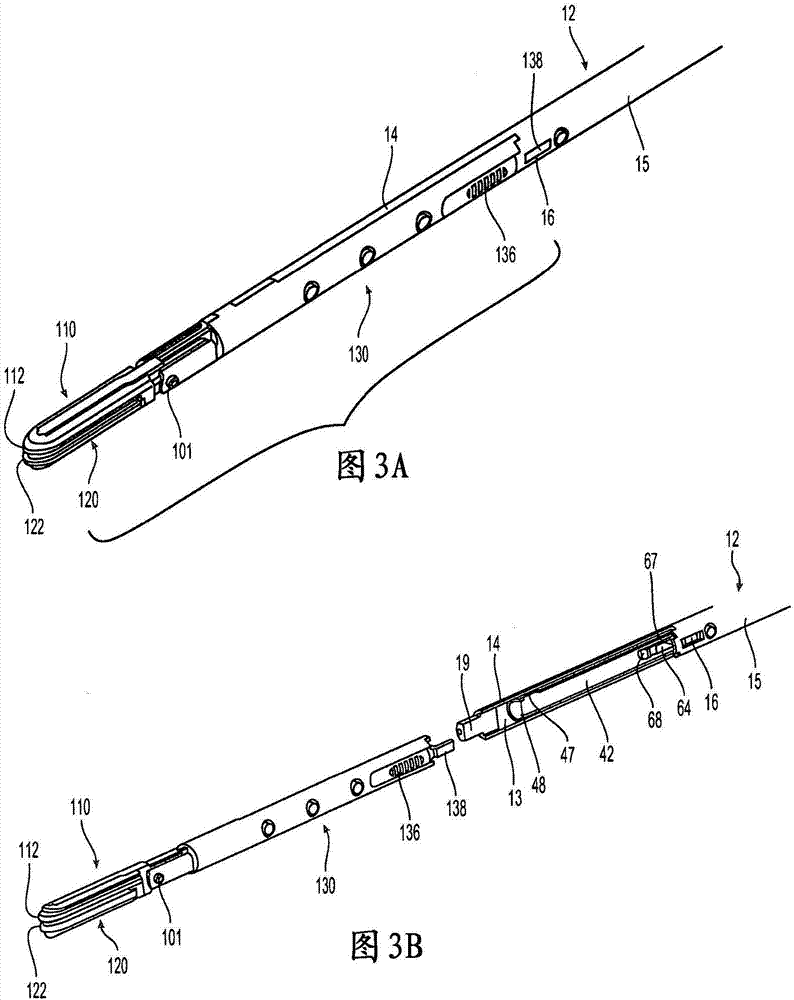
Surgical instruments facilitating replacement of disposable components and/or sterilization of reusable components
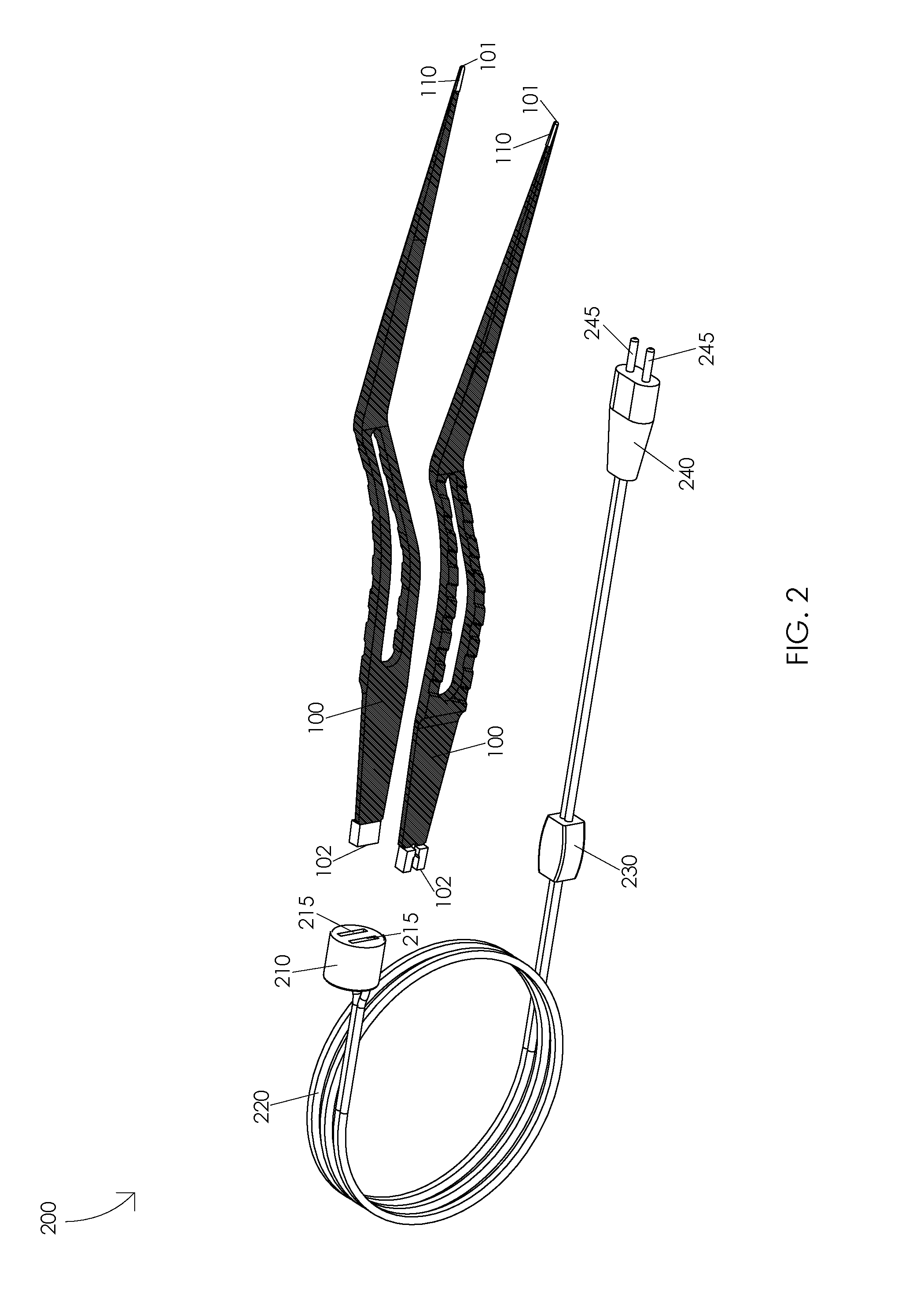
A surgical end effector assembly (100) includes a pair of jaw members (110, 120), a knife (170) defining a longitudinal slot (172), a pivot pin (101) coupling the jaw members (110, 120) to one another, and a drive member (160) including a drive pin (161) that is engaged to the jaw members (110, 120). The pivot pin (101) and / or the drive pin (161) extends through the longitudinal slot (172) of the knife (170) to couple the knife (170) to the jaw members (110, 120) and / or the drive member (160). The surgical end effector assembly (100) is transitionable between a use position, wherein the knife (170) and drive member (160) are generally aligned with one another to facilitate releasable engagement of the surgical end effector assembly (100) with a surgical instrument, and a cleaning position, wherein the jaw members (110, 120), knife (170), and drive member (160) are fanned apart from one another to facilitate cleaning of the surgical end effector assembly (100). Methods of disengaging and sterilizing end effector assemblies for reuse are also provided.
Owner:COVIDIEN LP
Bipolar forceps
InactiveUS20160008052A1Surgical instruments for heatingInstrument probesElectrical conductorEngineering
A bipolar forceps may include a first forceps arm having a first forceps arm conductor tip; a second forceps arm having a second forceps arm conductor tip; and an input conductor isolation mechanism having a first forceps arm housing and a second forceps arm housing. The first forceps arm may be disposed in the first forceps arm housing and the second forceps arm may be disposed in the second forceps arm housing. The first forceps arm conductor tip may include a chrome conversion coating configured to prevent tissue from sticking to the first forceps arm conductor tip during a surgical procedure. The second forceps arm conductor tip may include a chrome conversion coating configured to prevent tissue from sticking to the second forceps arm conductor tip during a surgical procedure.
Owner:KOGENT SURGICAL
Endovenous laser treatment generating reduced blood coagulation
Inducing thrombolysis of thermally induced thrombus occurring during endovenous ablation of varicose veins by introducing an optical fiber laser deliver device with optical fiber portion and with an energy emitting tip at its distal end into the varicosed vein to be treated, emitting pulsed, laser energy with sufficient energy to close and destroy varicose veins to the emitting tip of the optical fiber laser delivery device, thereby inducing laser thrombolysis of coagulated blood which accumulates at the energy emitting tip of the fiber when the fiber is caused to emit energy in the presence of uncoagulated blood and minimizing adverse effects associated with thermally induced thrombus within a varicose vein.
Owner:NEW STAR LASERS
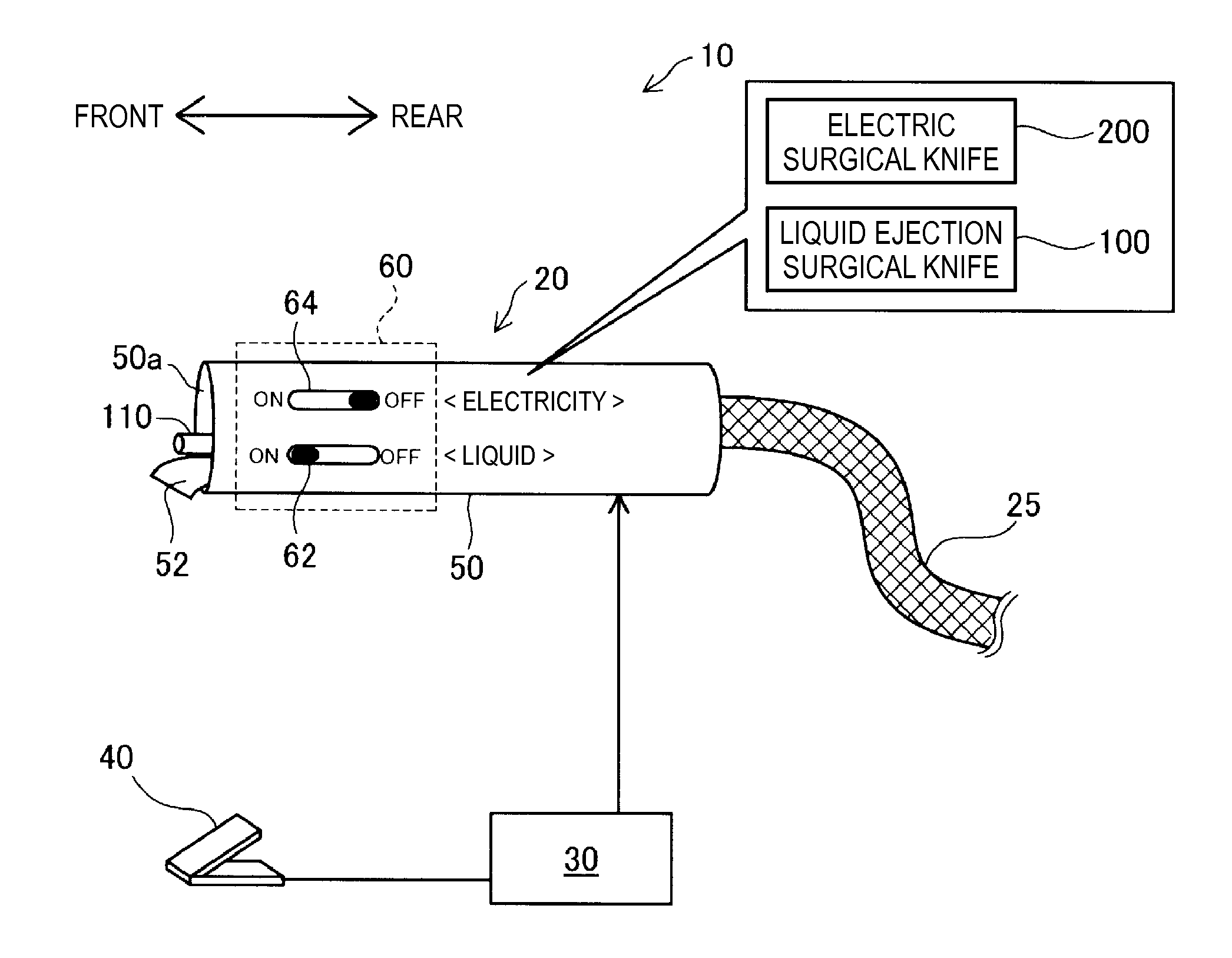
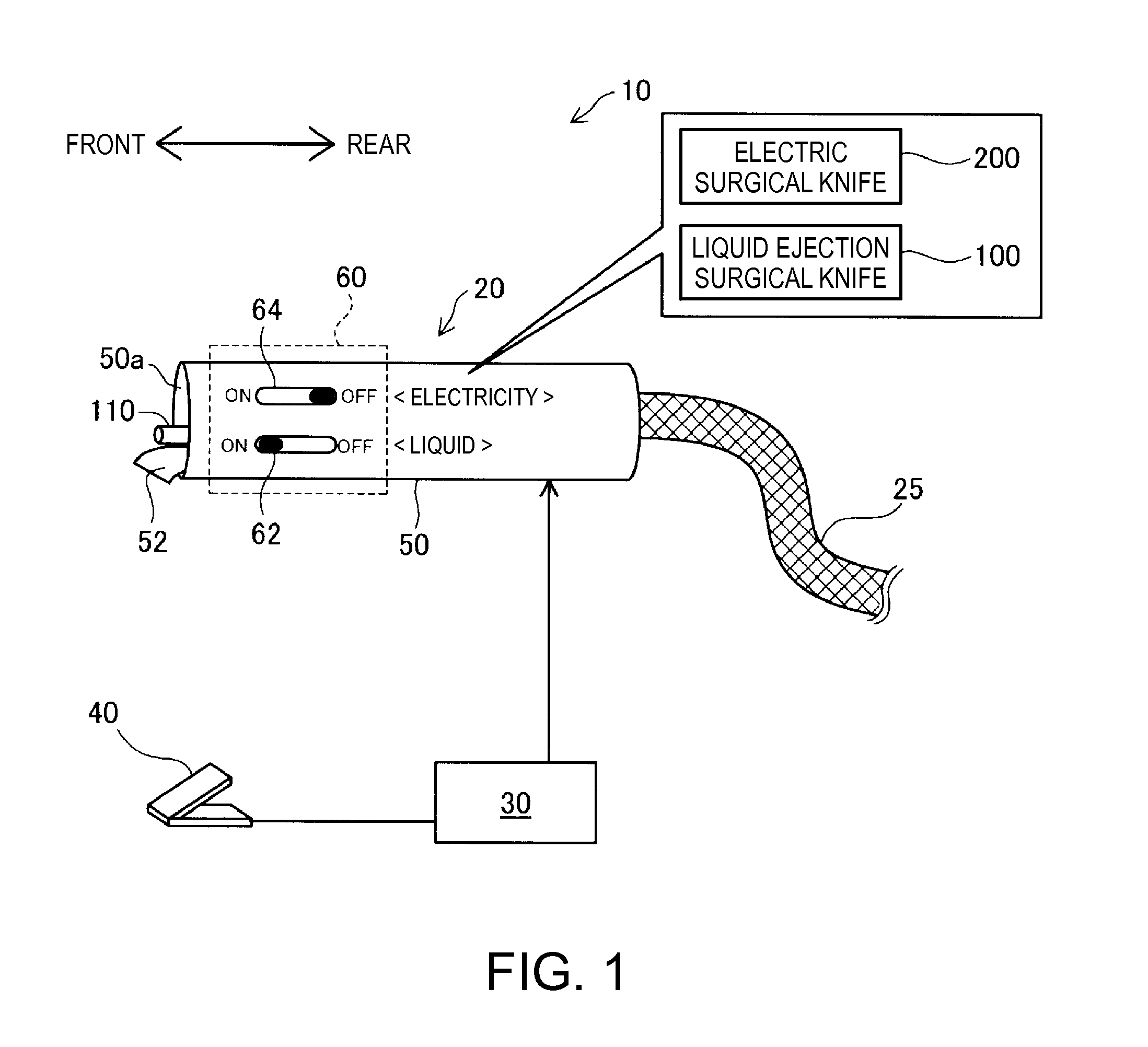
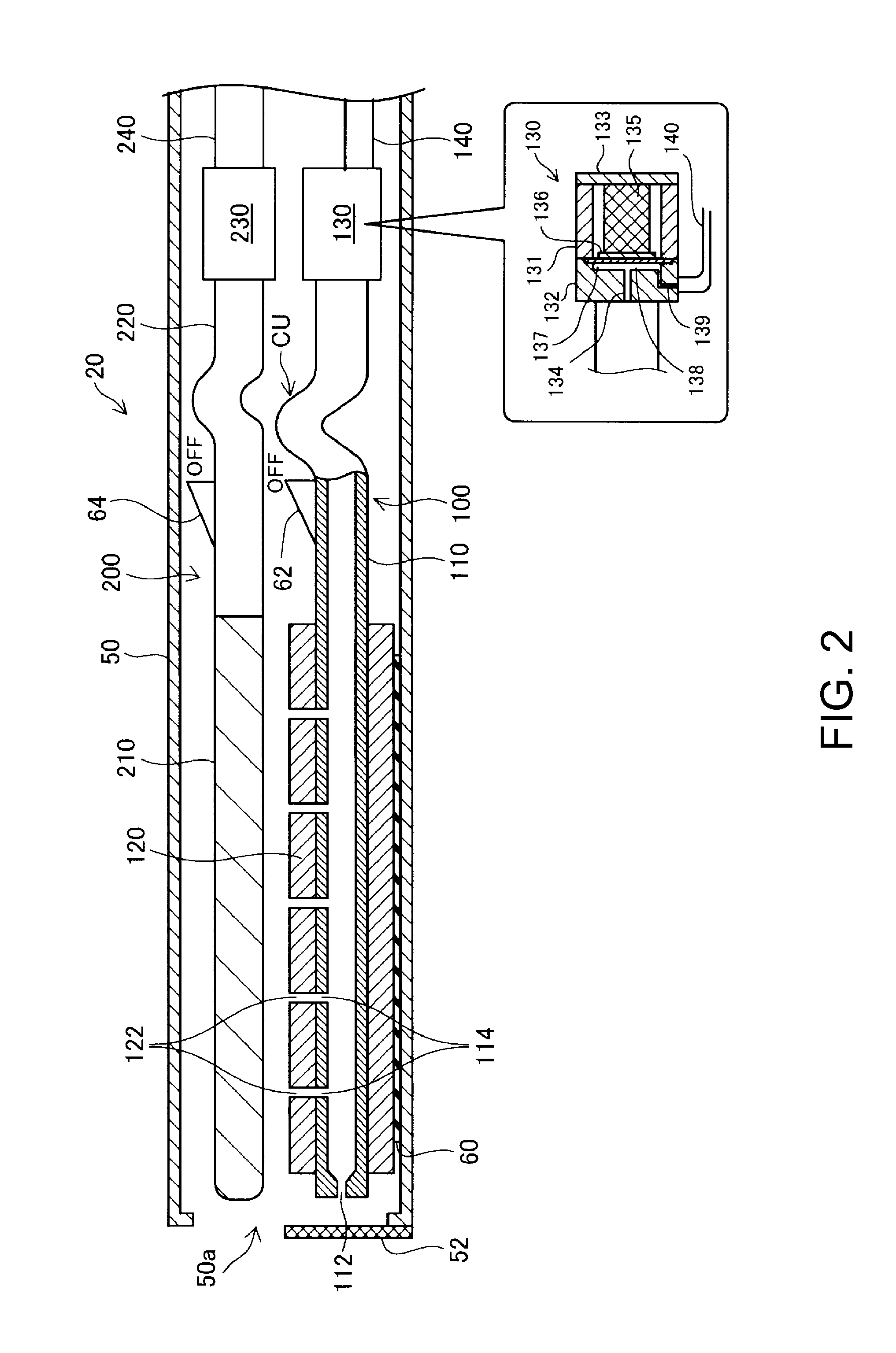
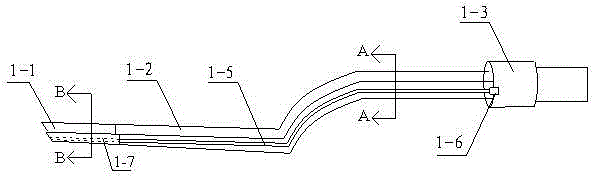
Operation instrument
InactiveUS20150238217A1Reduce laborEasy to operateIncision instrumentsFluid jet surgical cuttersEngineeringSurgical device
An operation instrument includes an electric surgical knife, a liquid ejection surgical knife capable of ejecting liquid; and an outer case configured to accommodate the electric surgical knife and the liquid ejection surgical knife, and including an opening which allows an electrode portion of the electric surgical knife to project therefrom. The liquid ejection surgical knife is operated so as to be switched between a therapy mode in which liquid is ejected to the outside of the outer case, and a cleaning mode configured to eject the liquid toward a high-frequency treatment electrode of the electric surgical knife in a state of being accommodated in the outer case.
Owner:SEIKO EPSON CORP
Electrocoagulation forcep system convenient to clean
InactiveCN105411674ASimple structureReduce volumeDiagnosticsCleaning using toolsElectrocoagulationMedicine
Owner:CHONGQING RUNZE PHARM CO LTD
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com