Patents
Literature
71 results about "Respiratory effort" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
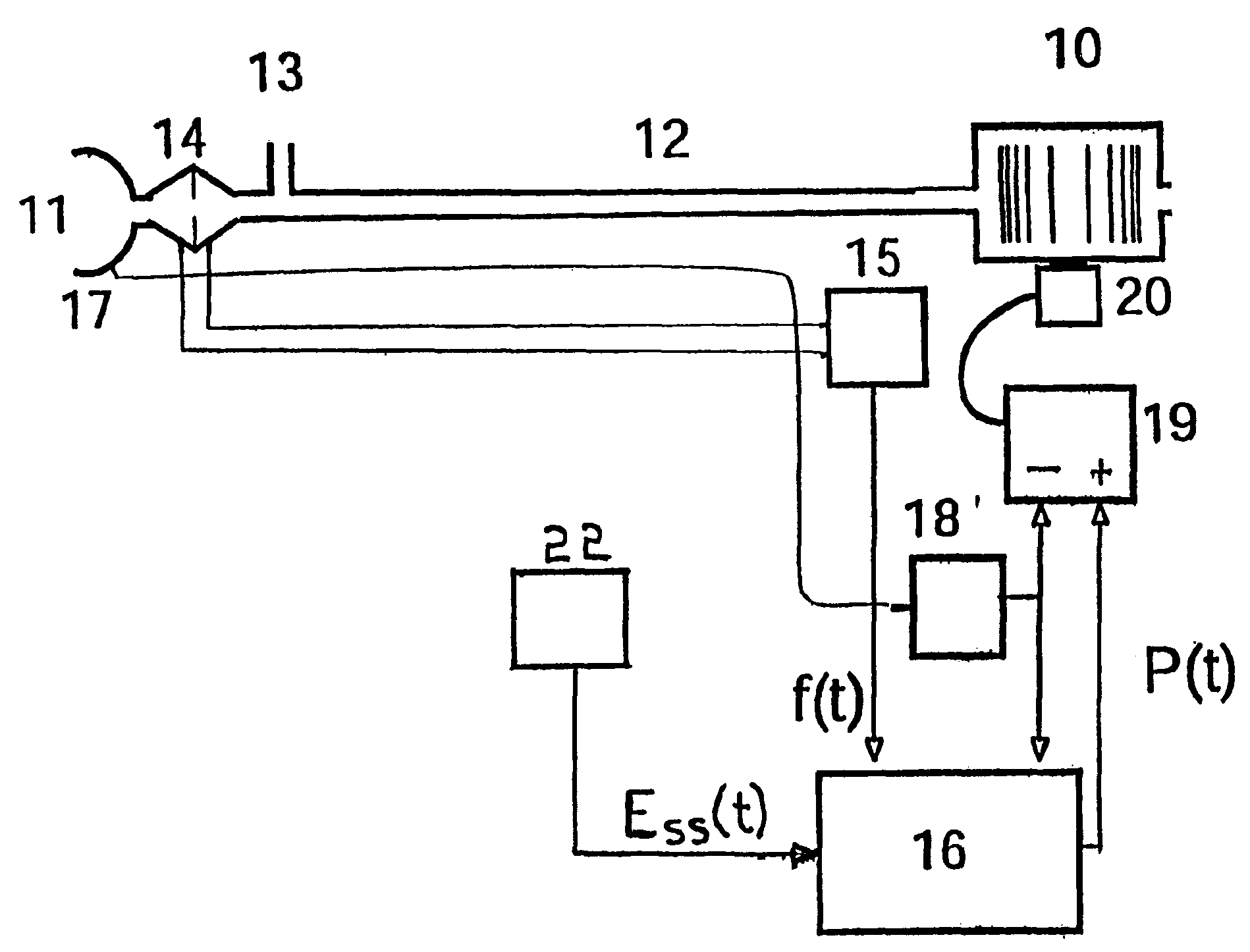
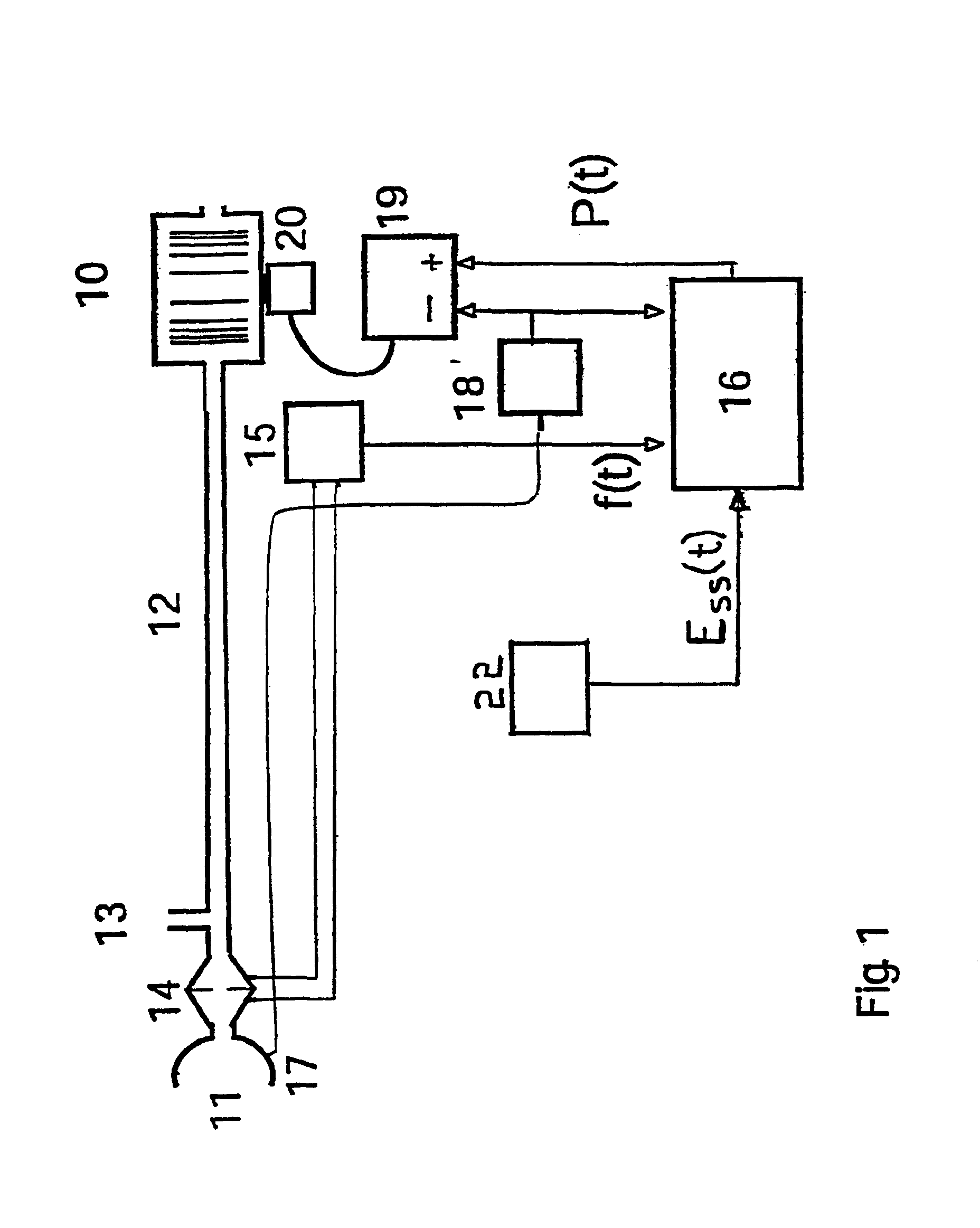
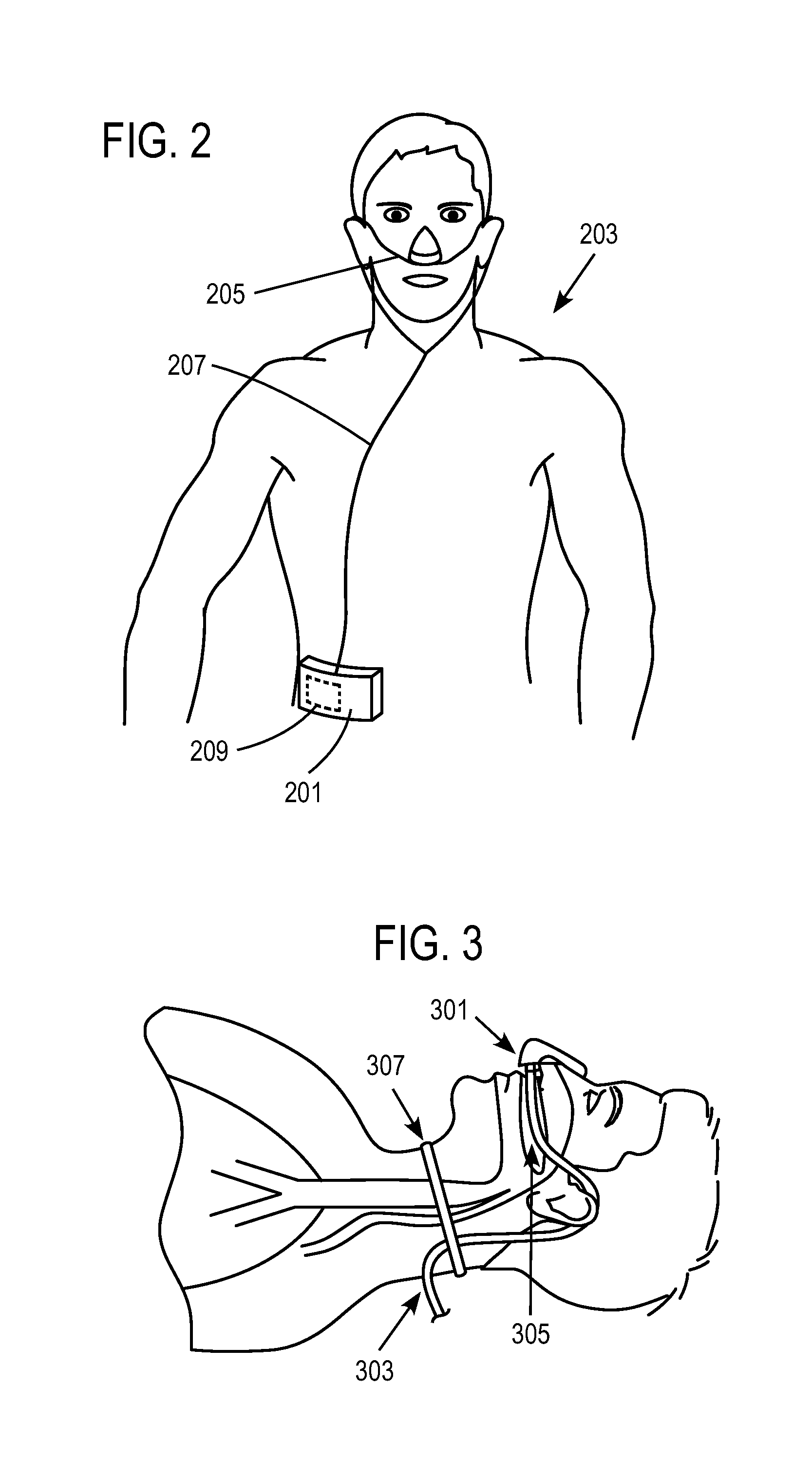
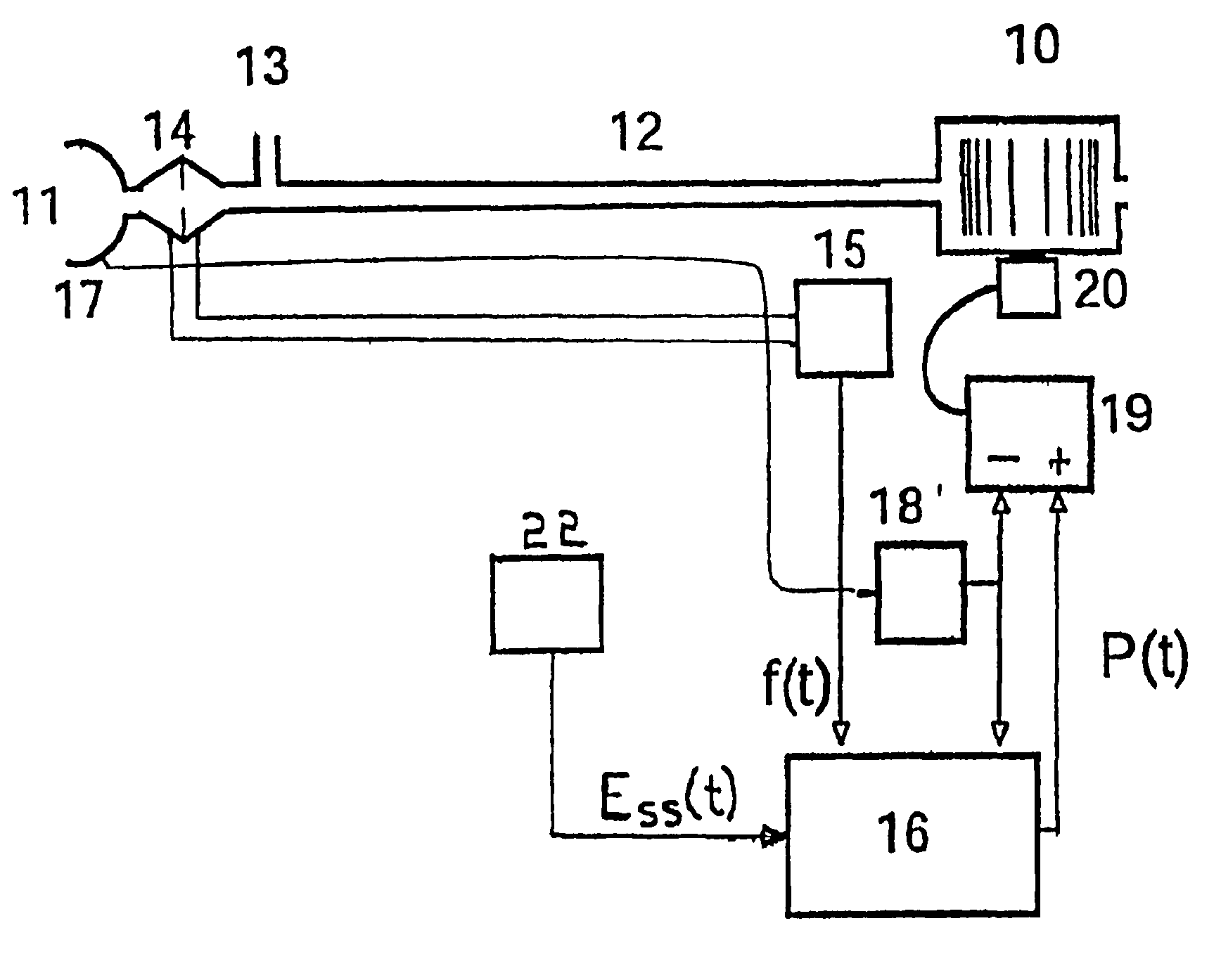
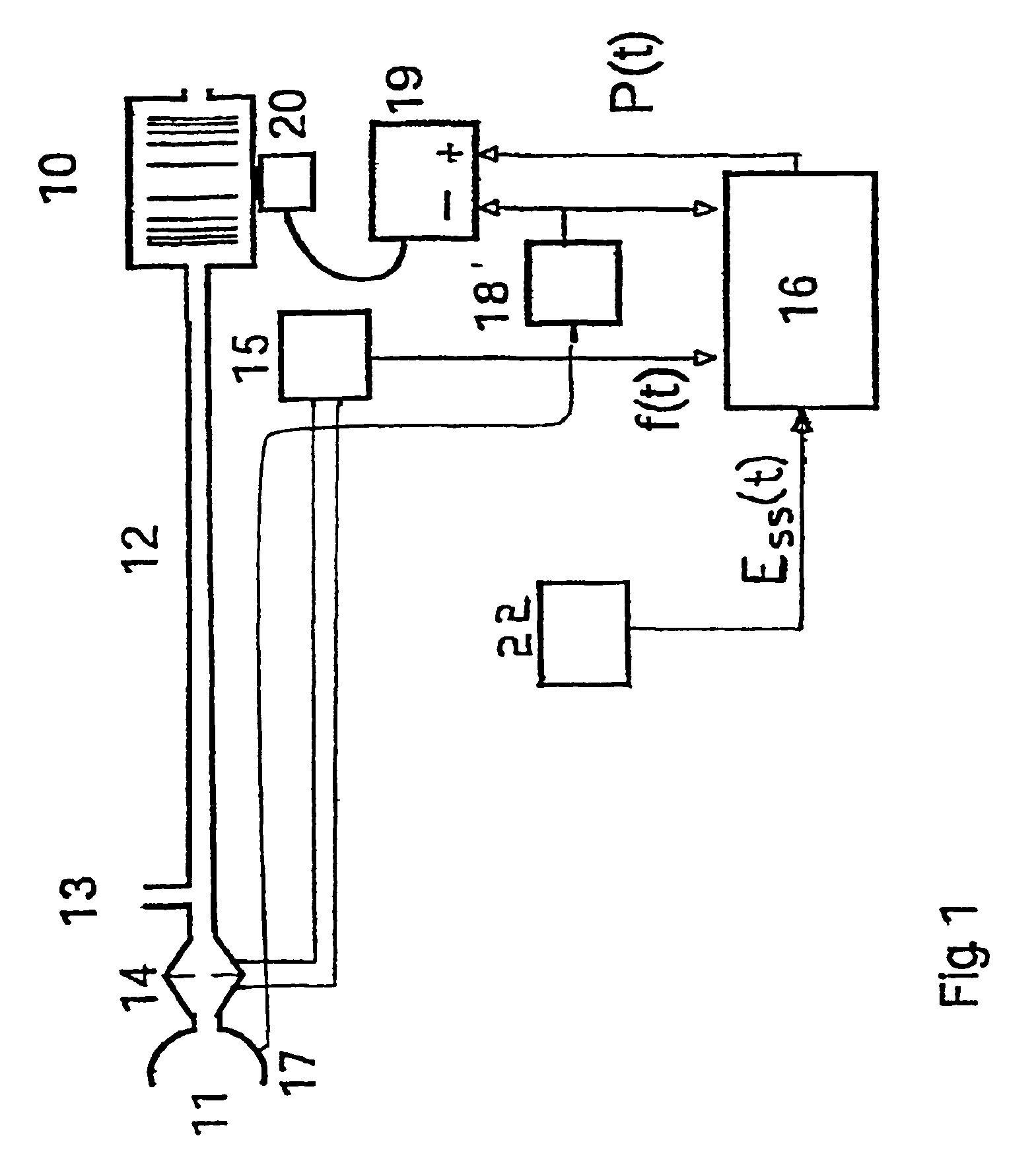
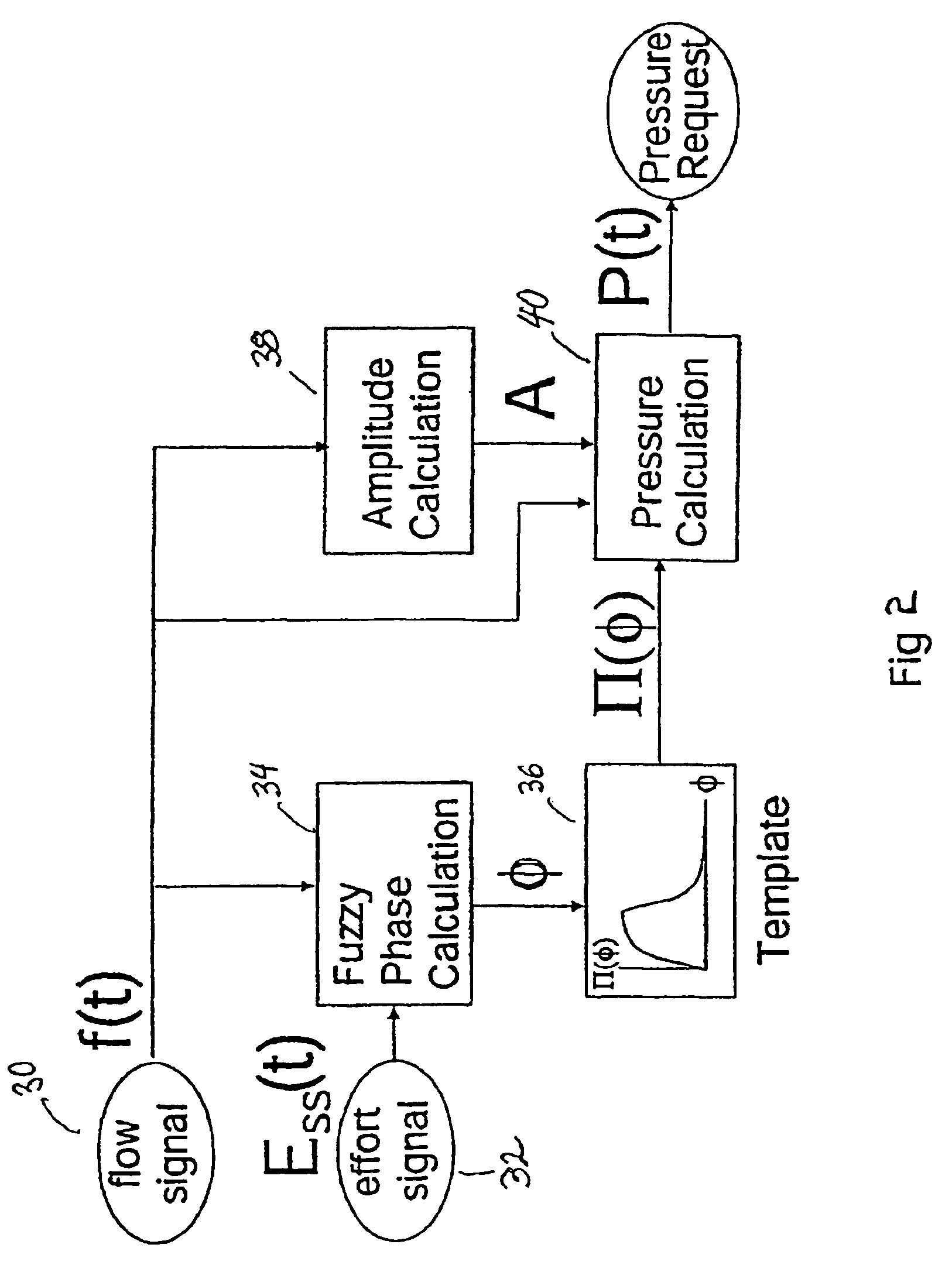
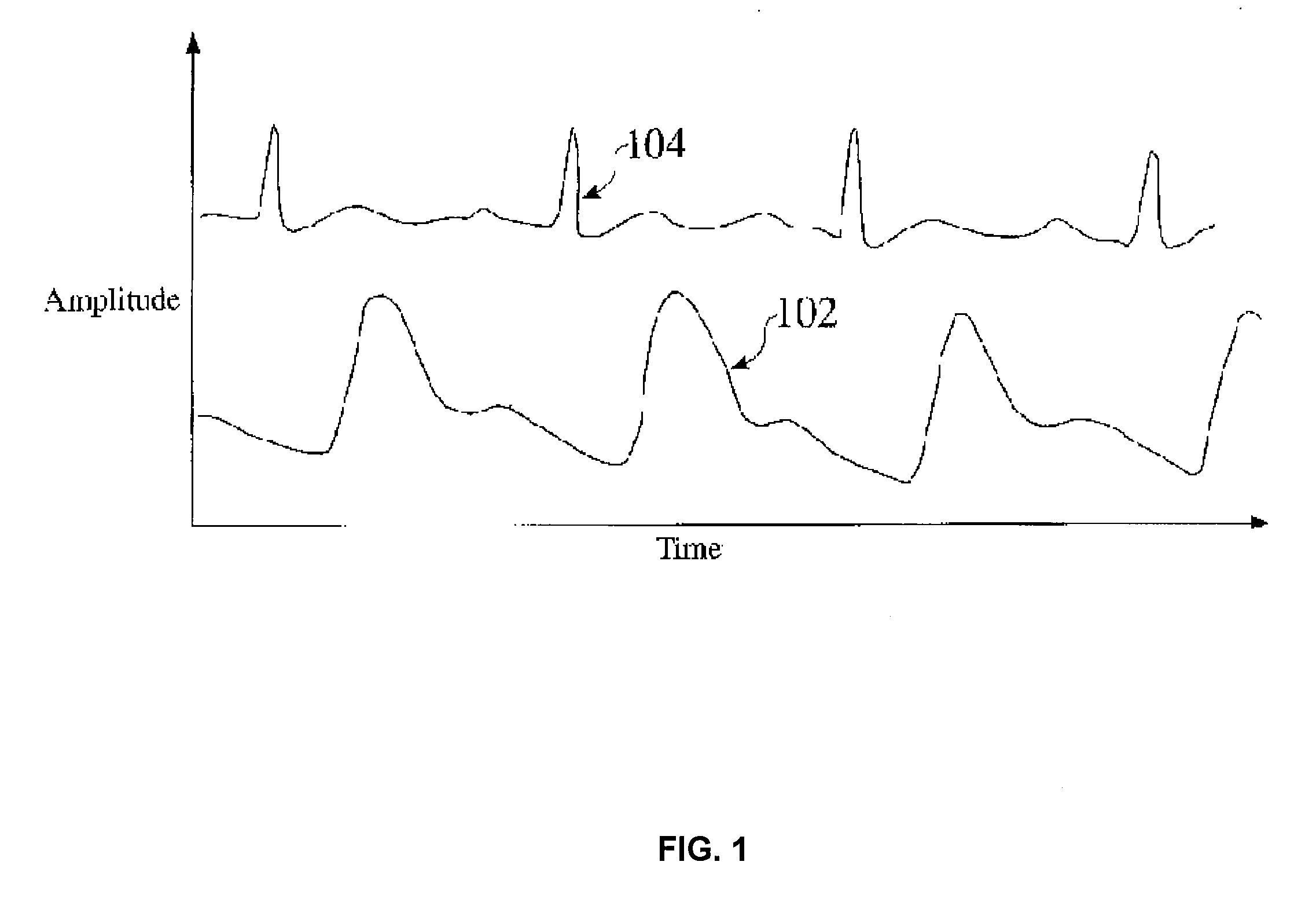
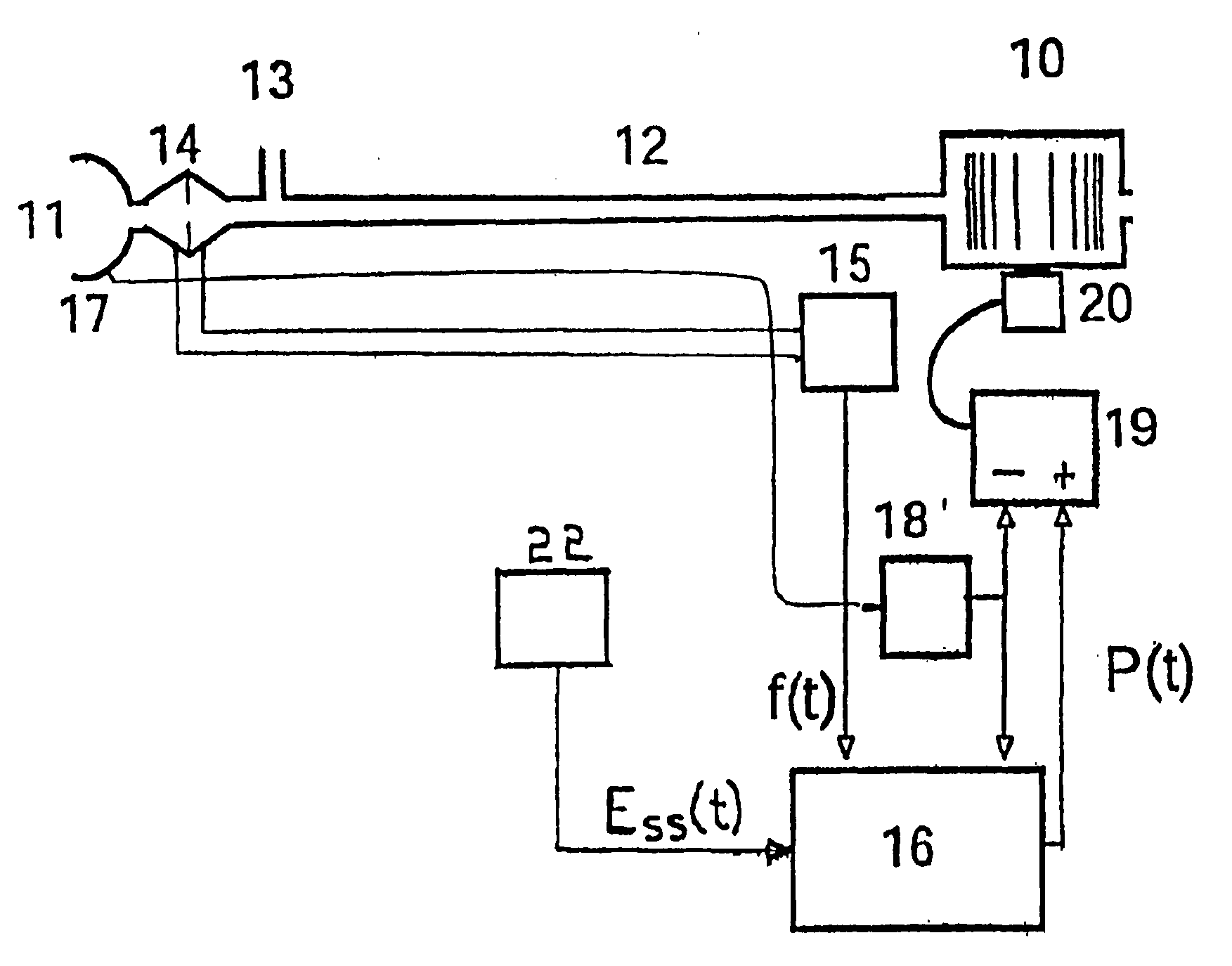
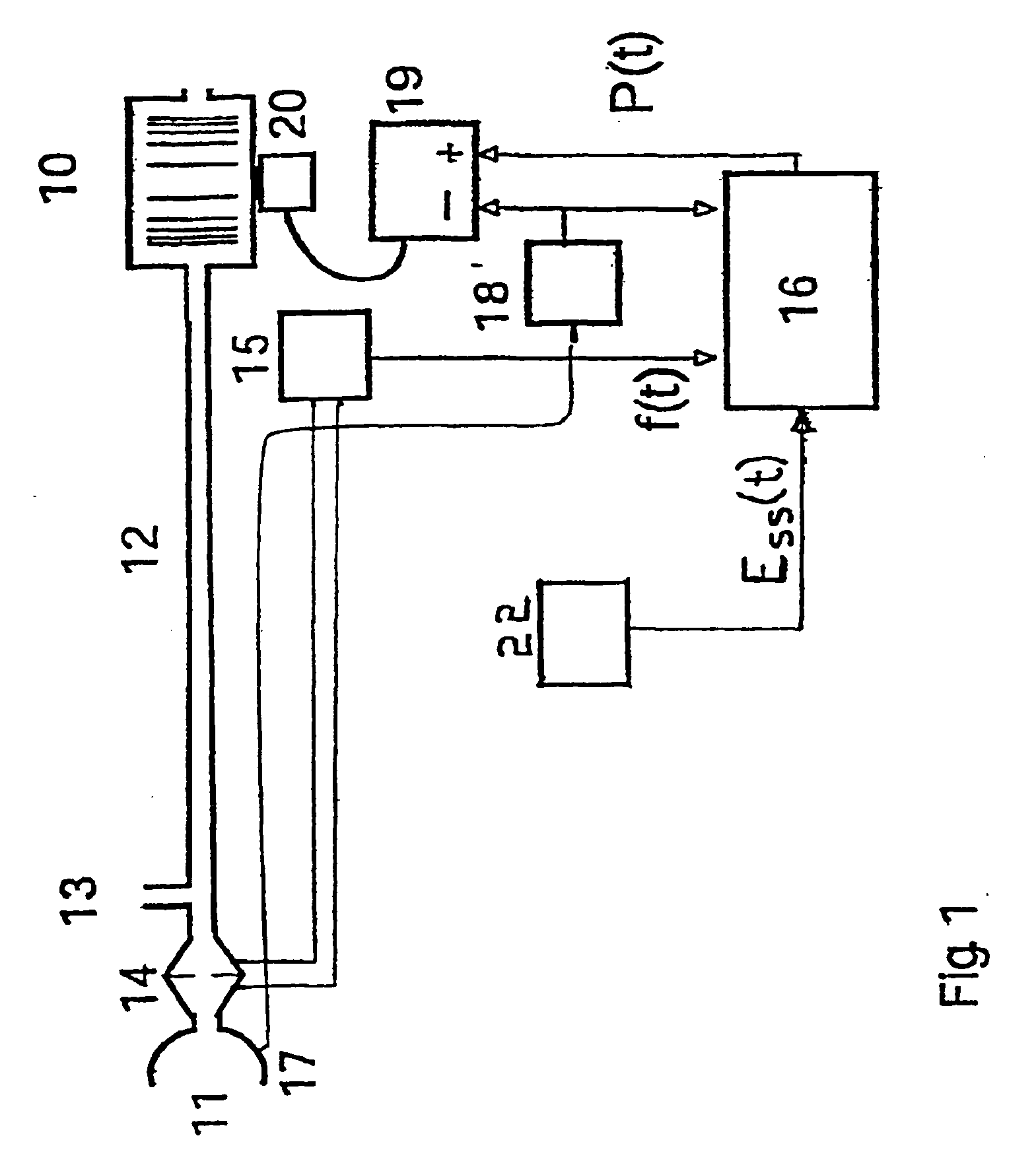
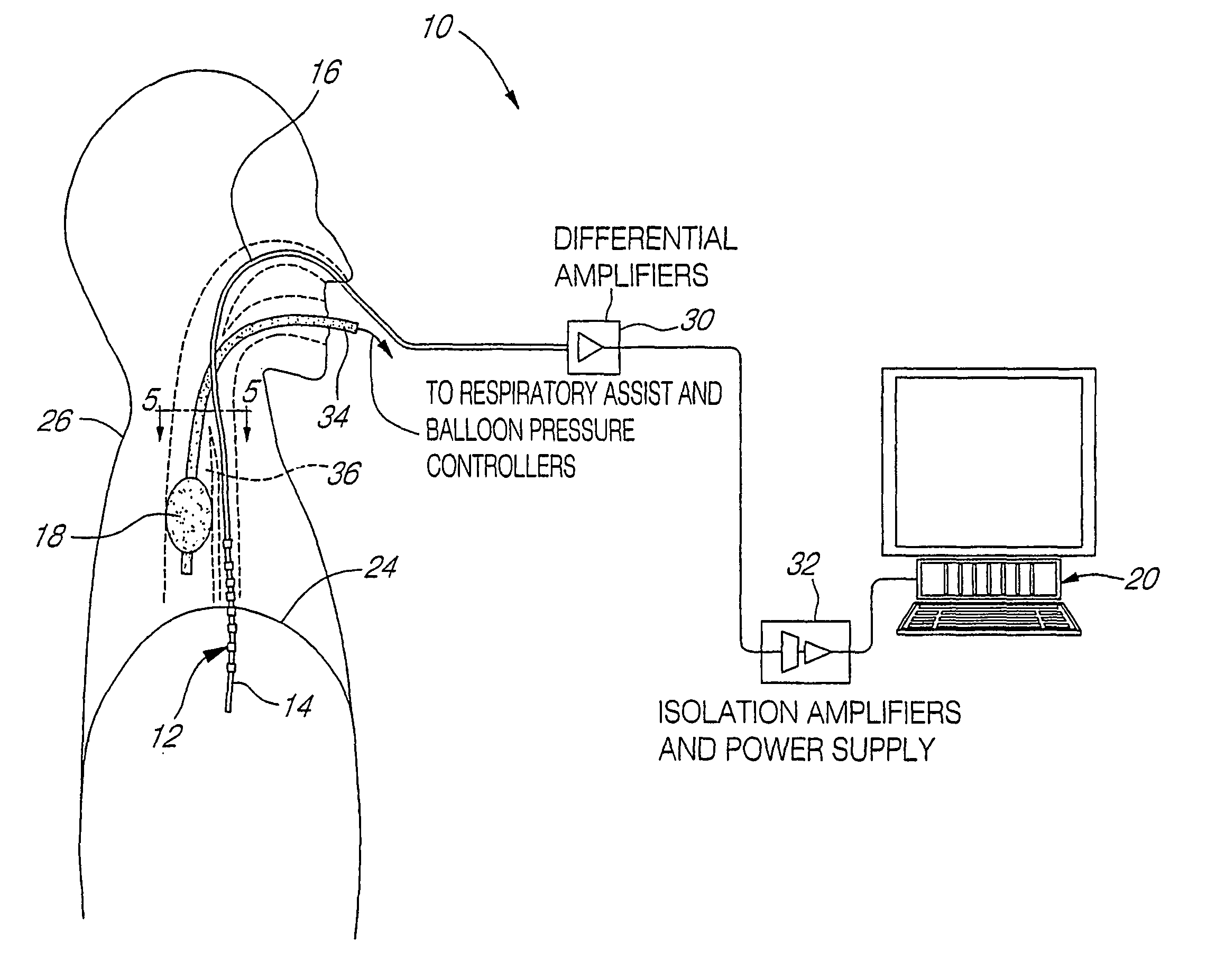
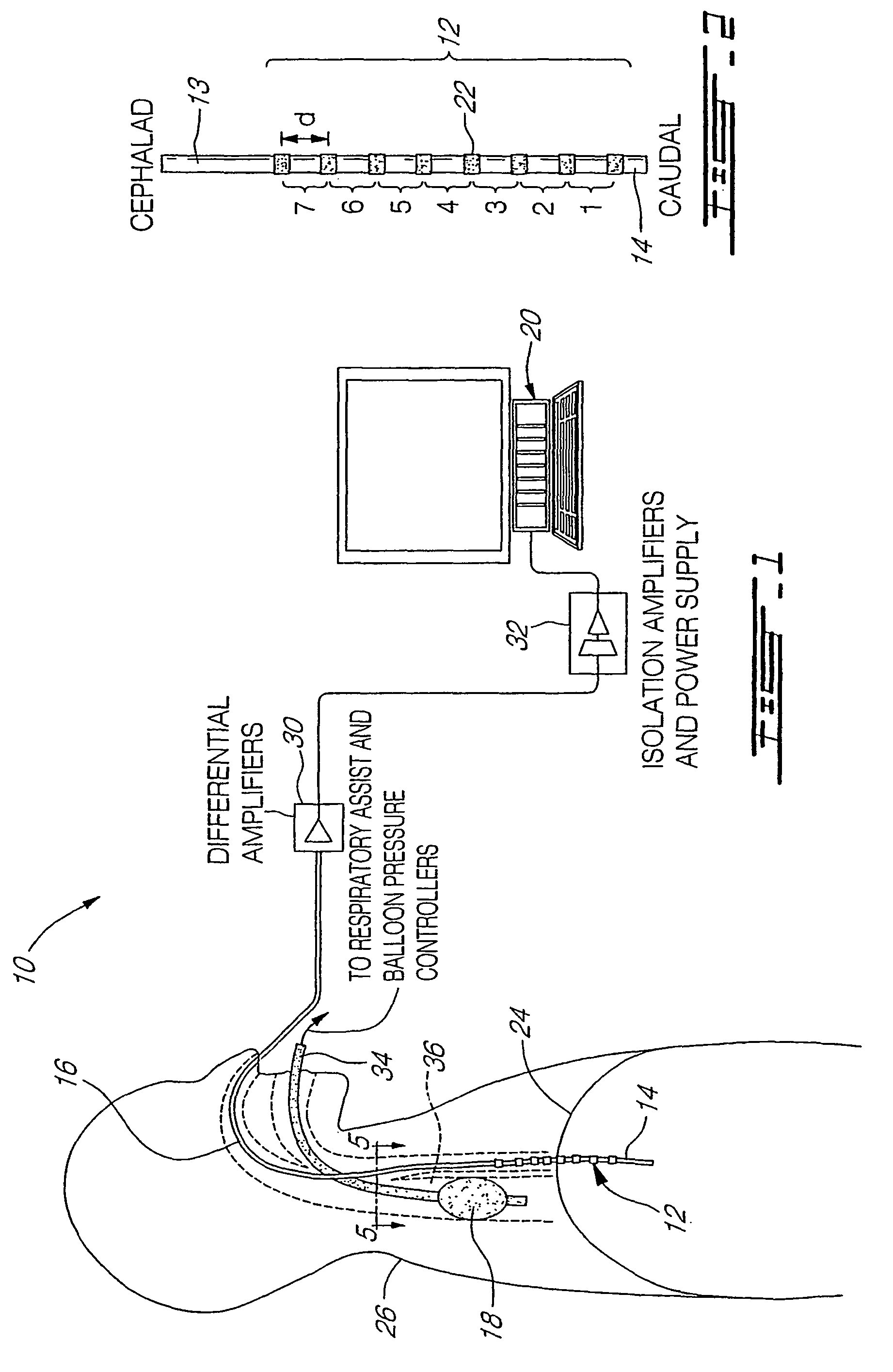
Patient-ventilator synchronization using dual phase sensors
InactiveUS6910480B1Minimum ventilationImprove determinationRespiratorsOperating means/releasing devices for valvesRespiratory phasePressure amplitude
An improved ventilator which delivers ventilatory support that is synchronized with the phase of the patient's respiratory efforts and guarantees a targeted minimum ventilation. Improved synchronization is achieved through an instantaneous respiratory phase determination process based upon measured respiratory airflow as well as measured respiratory effort using an effort sensor accessory, preferably a suprasternal notch sensor. The ventilator processes a respiratory airflow signal, a respiratory effort signal and their respective rates of change to determine a phase using standard fuzzy logic methods. A calculated pressure amplitude is adjusted based upon the calculated phase and a smooth pressure waveform template to deliver synchronized ventilation.
Owner:RESMED LTD
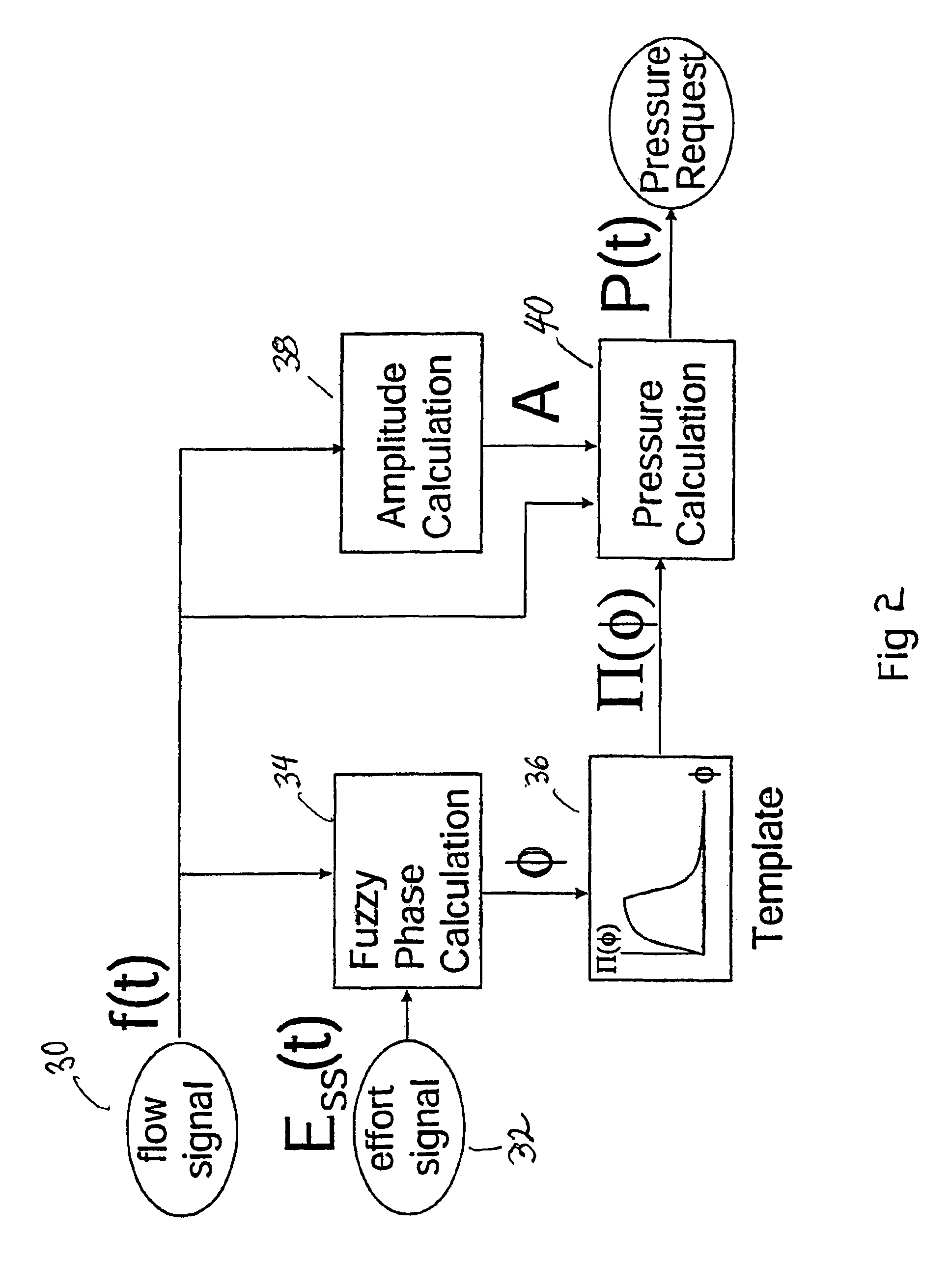
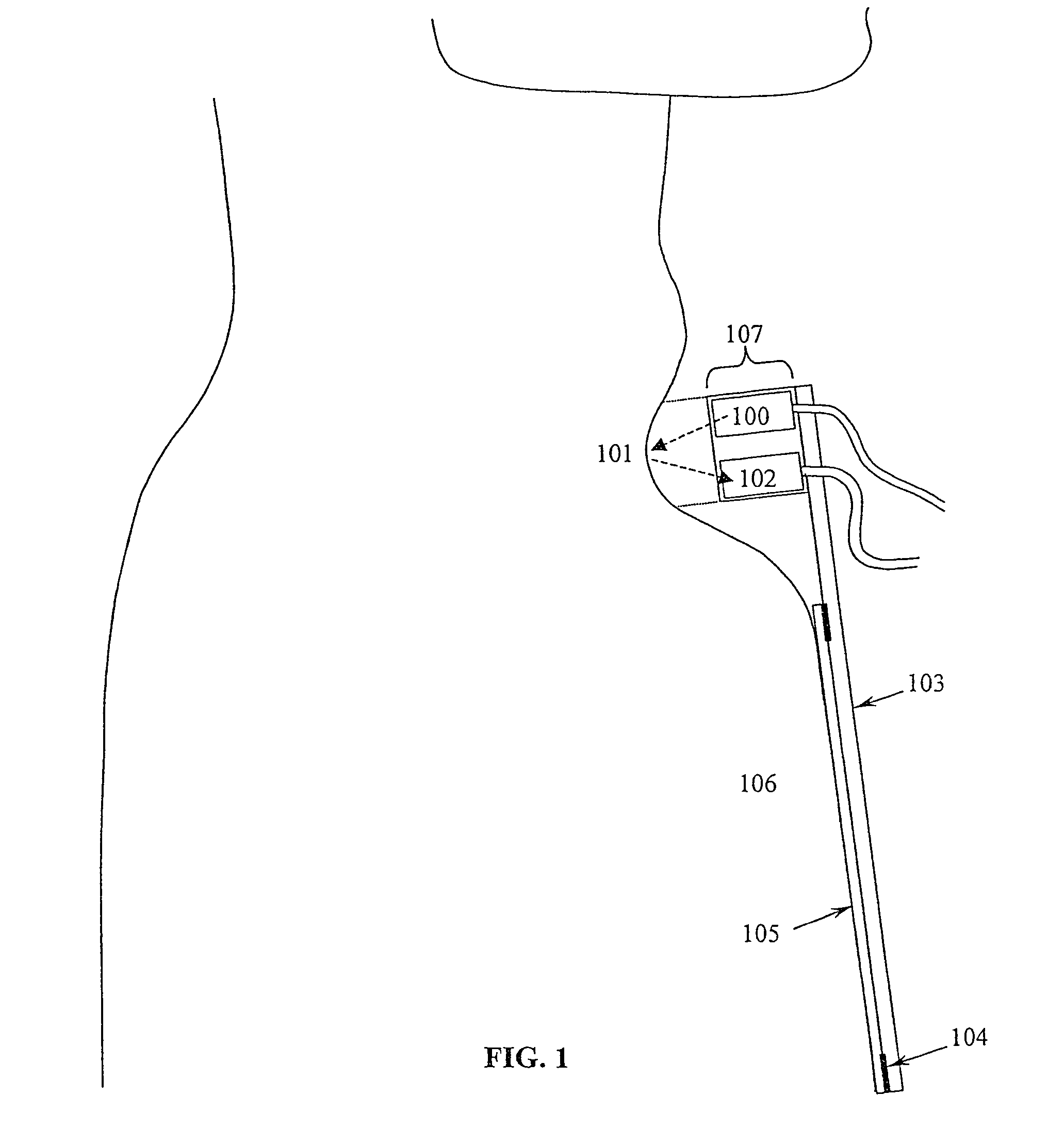
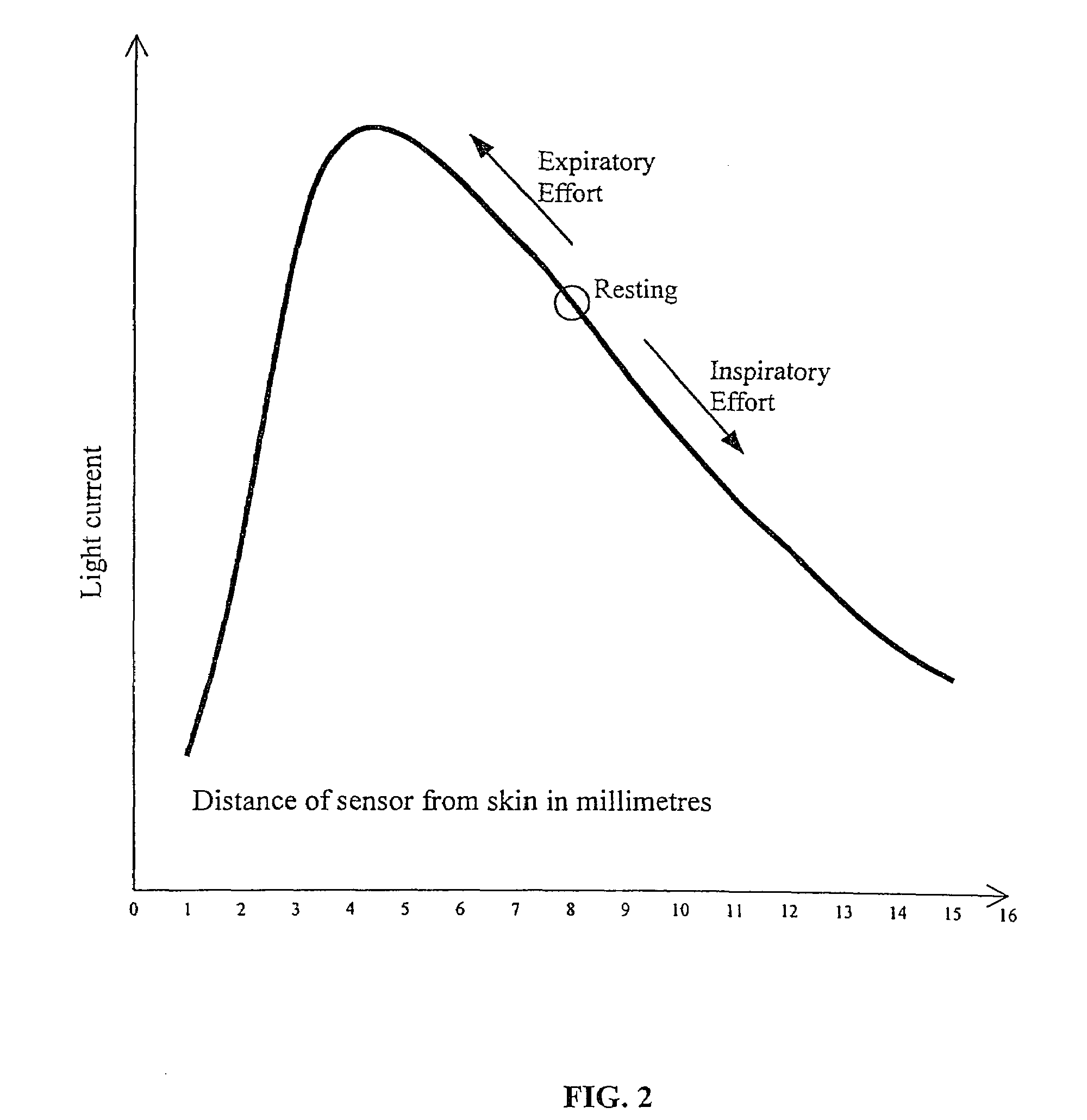
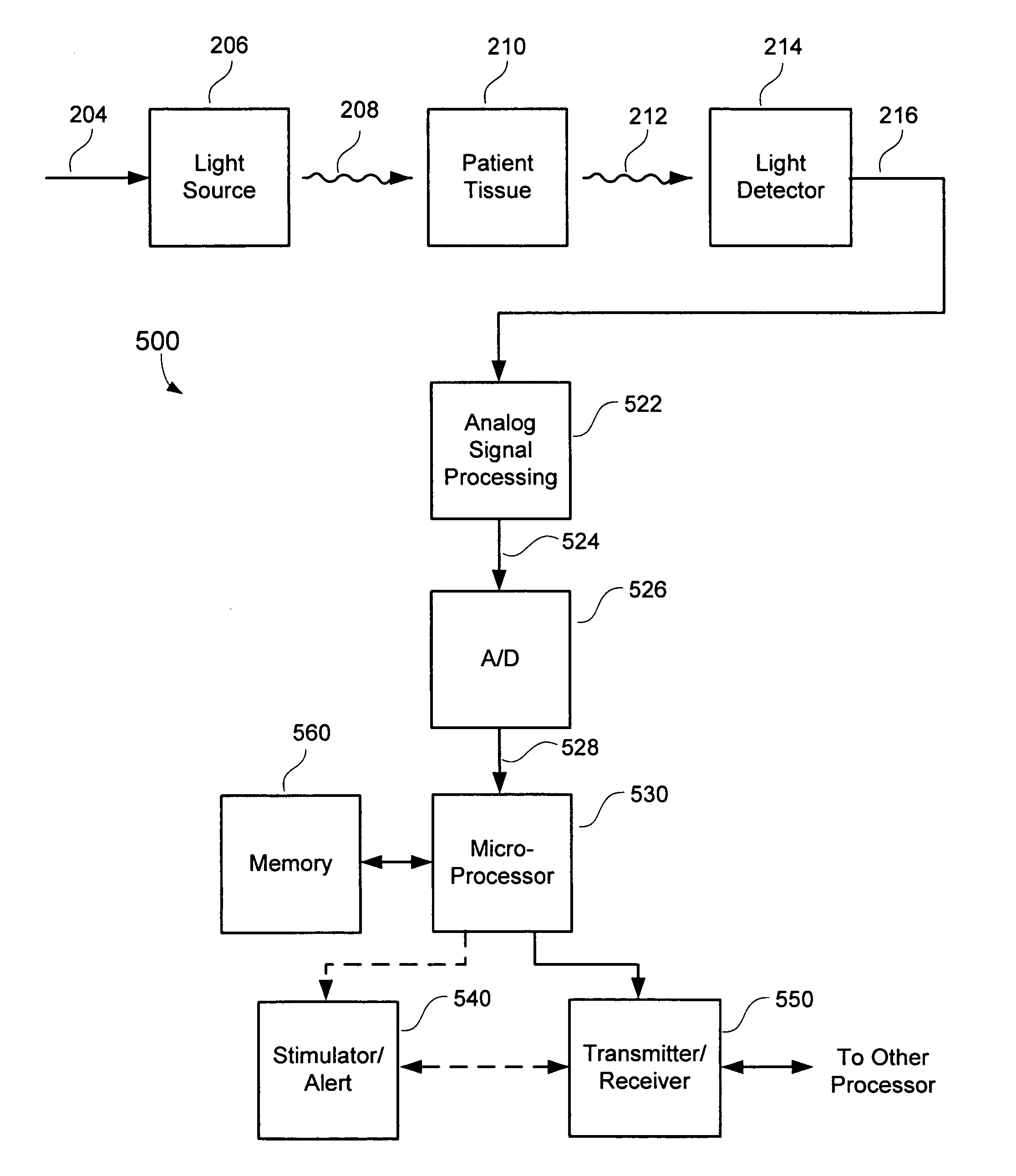
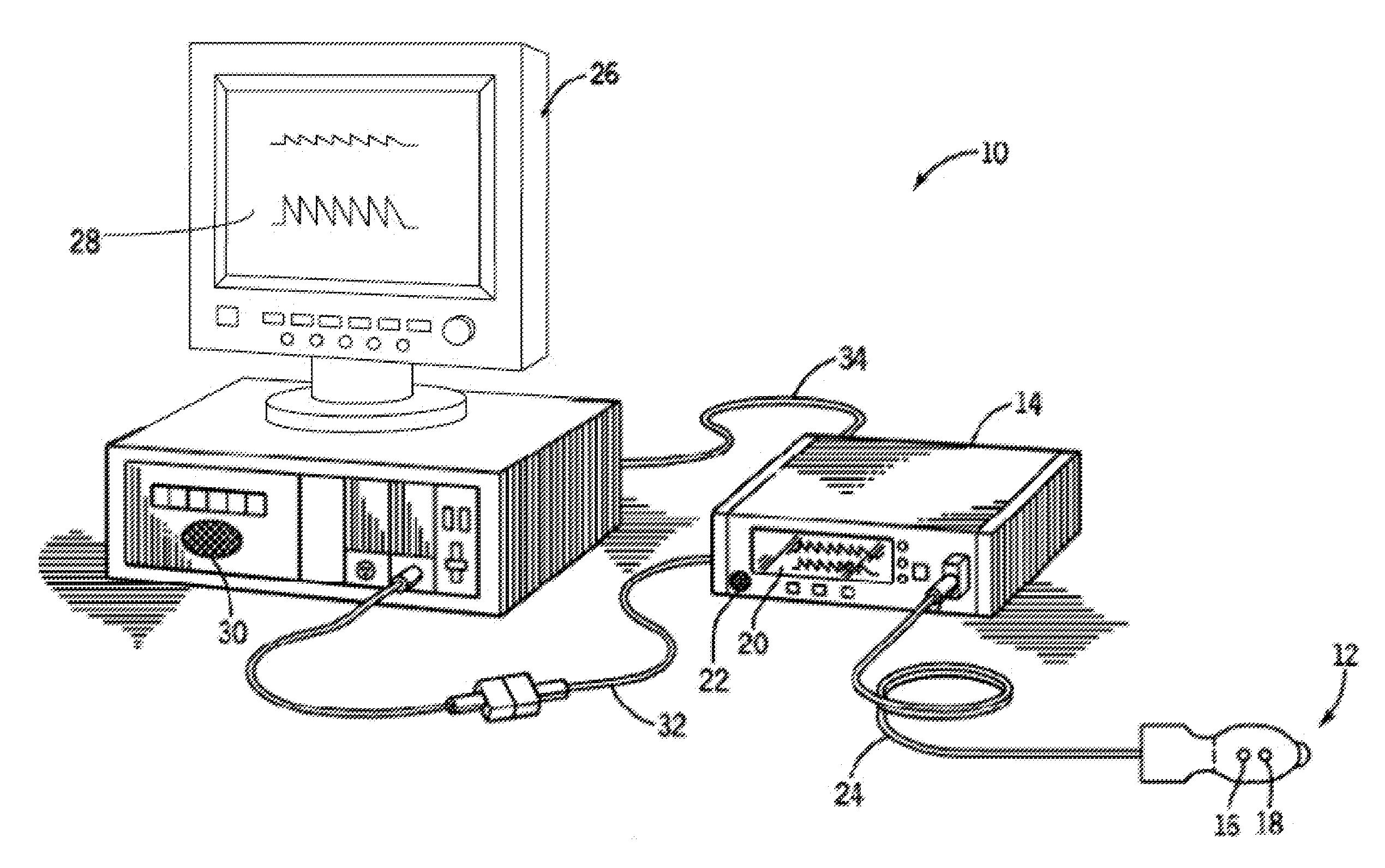
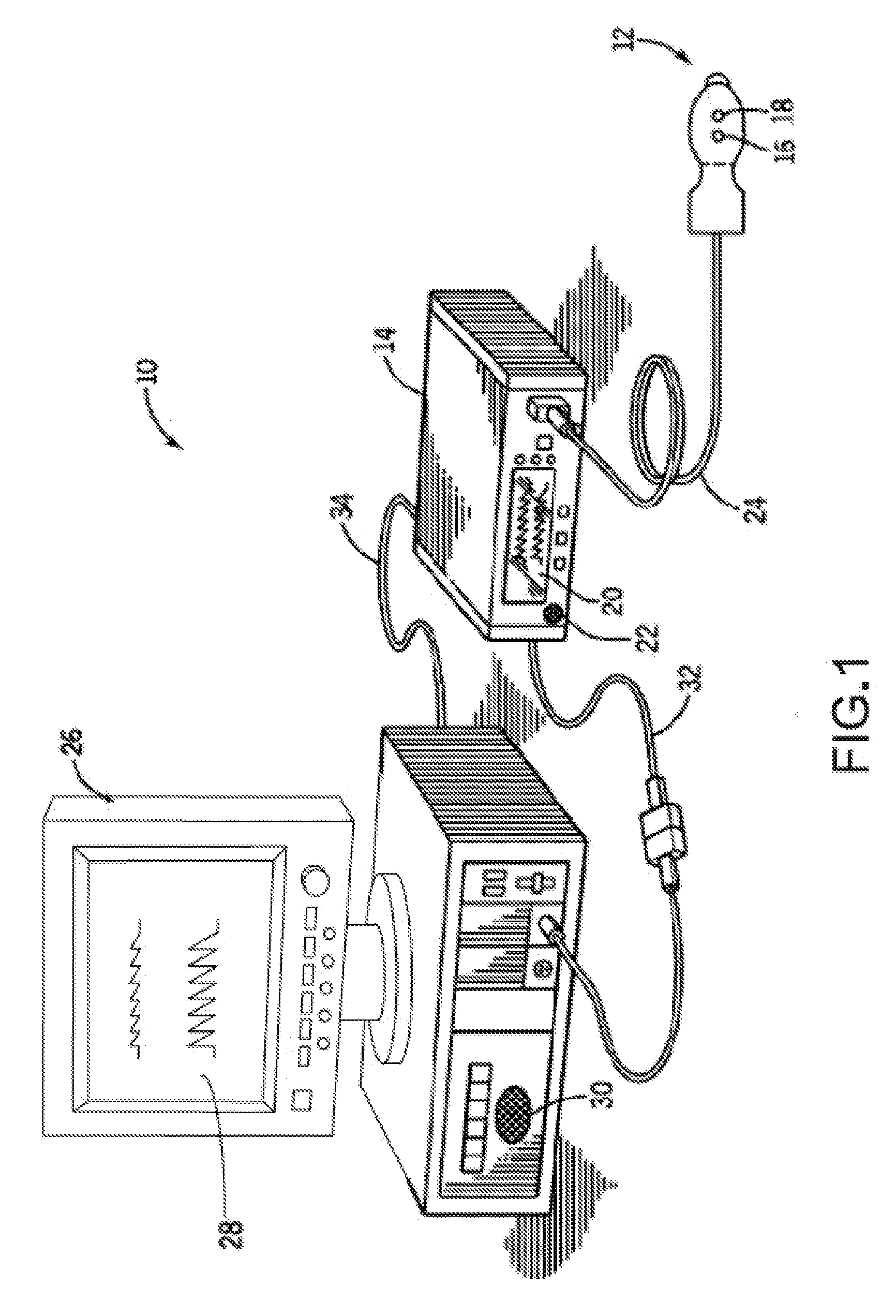
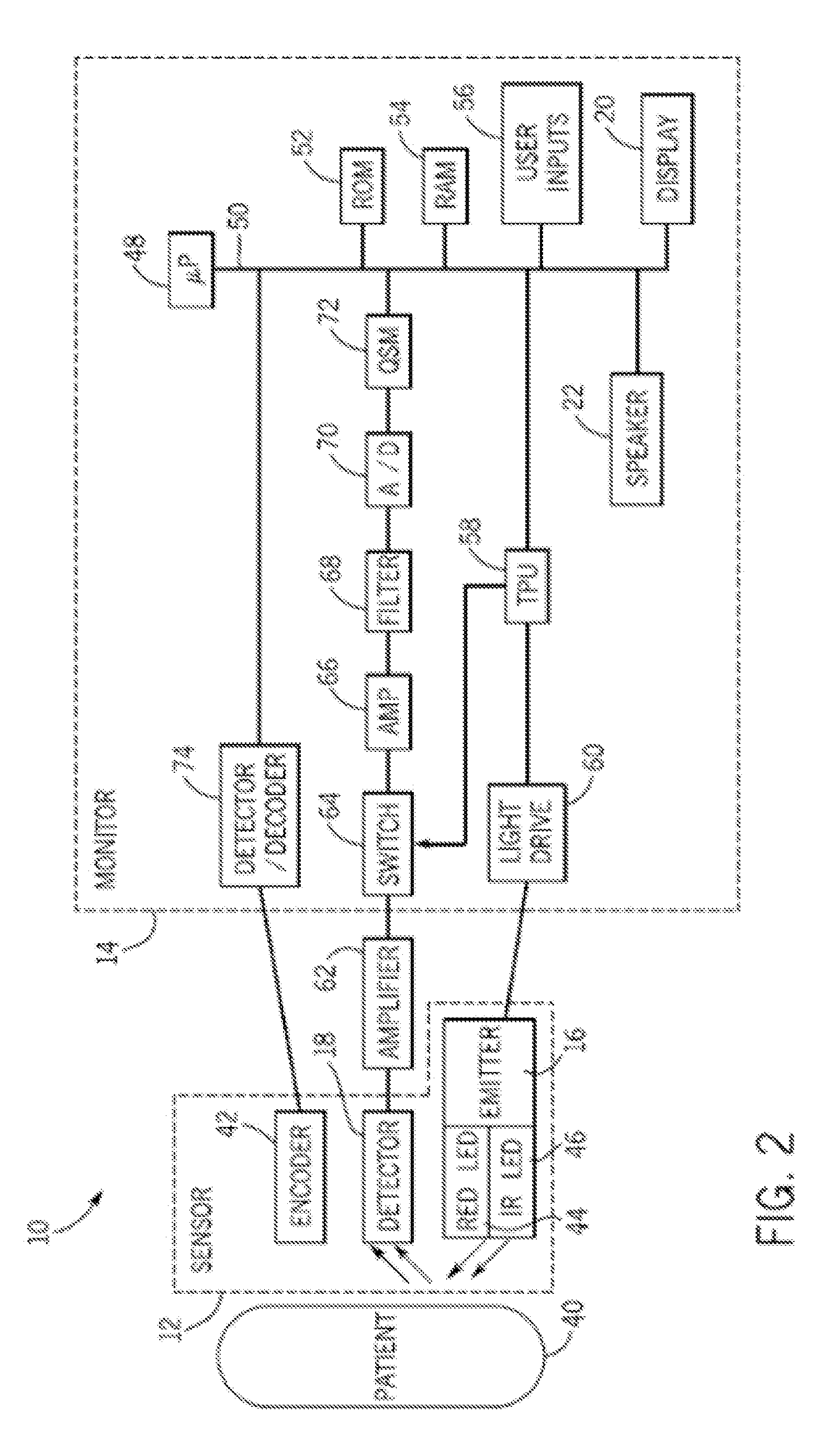
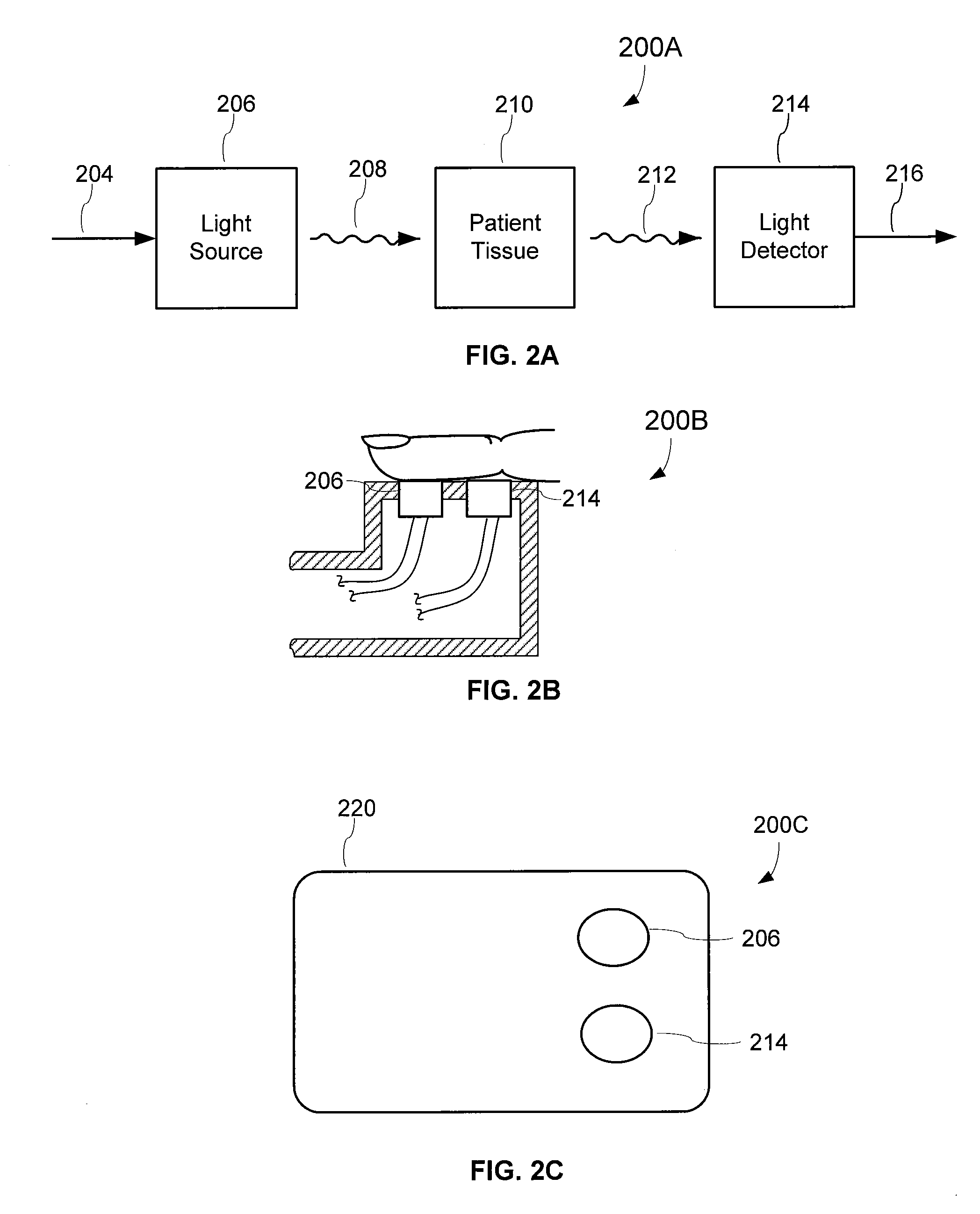
Method for measuring central venous pressure or respiratory effort
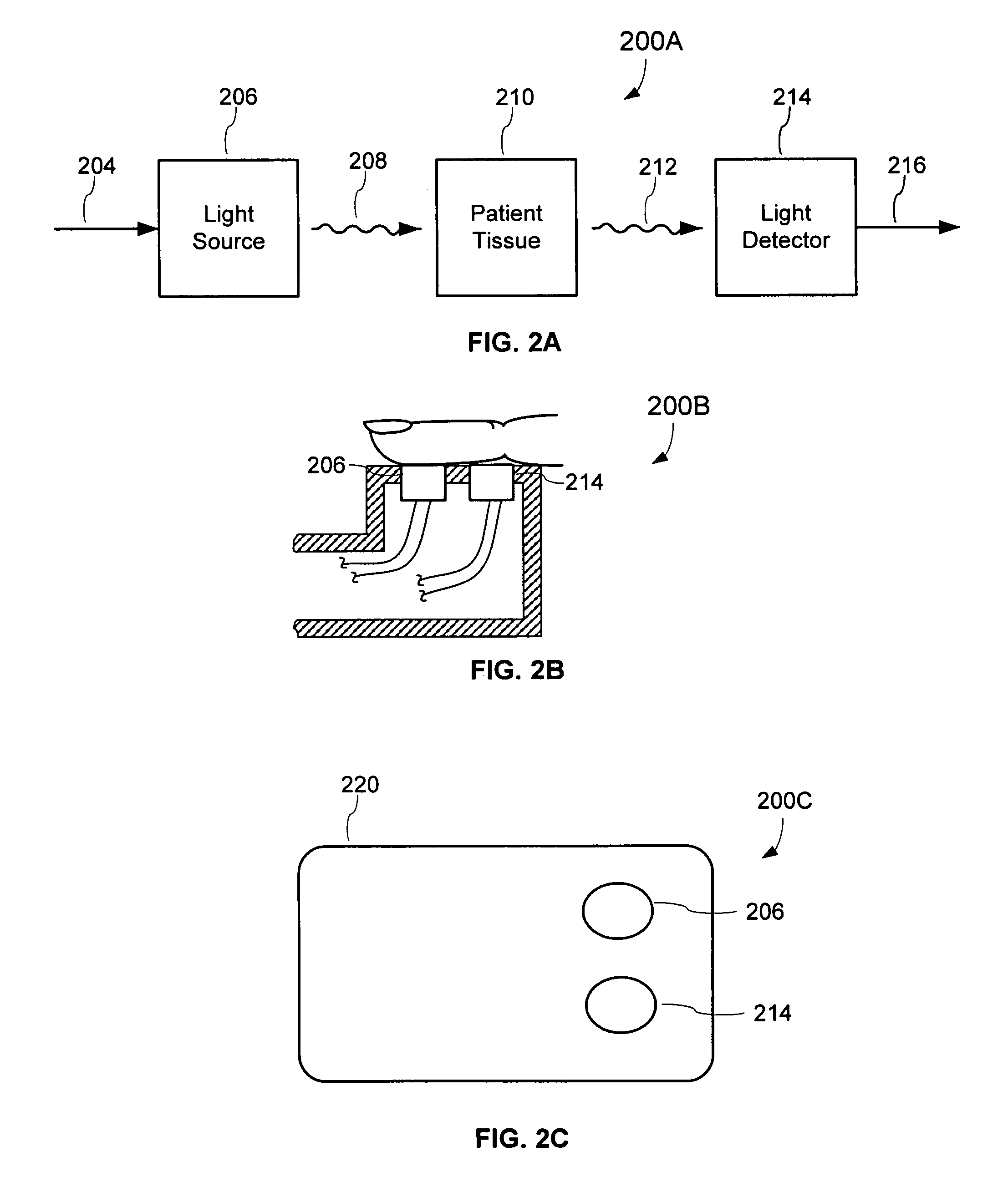
Photoplethysmography (PPG) is obtained using one red (e.g., 660 nm) and one infrared (e.g., 880 to 940 nm) light emitting diode with a single photo diode in combination with a pressure transducer thereby allowing both CVP and SpO2 to be measured simultaneously. The system also includes sensors capable of measuring position, angle and / or movement of the sensor or patient. Once the PPG signal is acquired, high pass adaptive and / or notch filtering can be used with one element of the filter from the red and infrared signals used to measure the arterial changes needed to compute SpO2 and the other element of the signal can be used to measure CVP changes.
Owner:WATERMARK MEDICAL
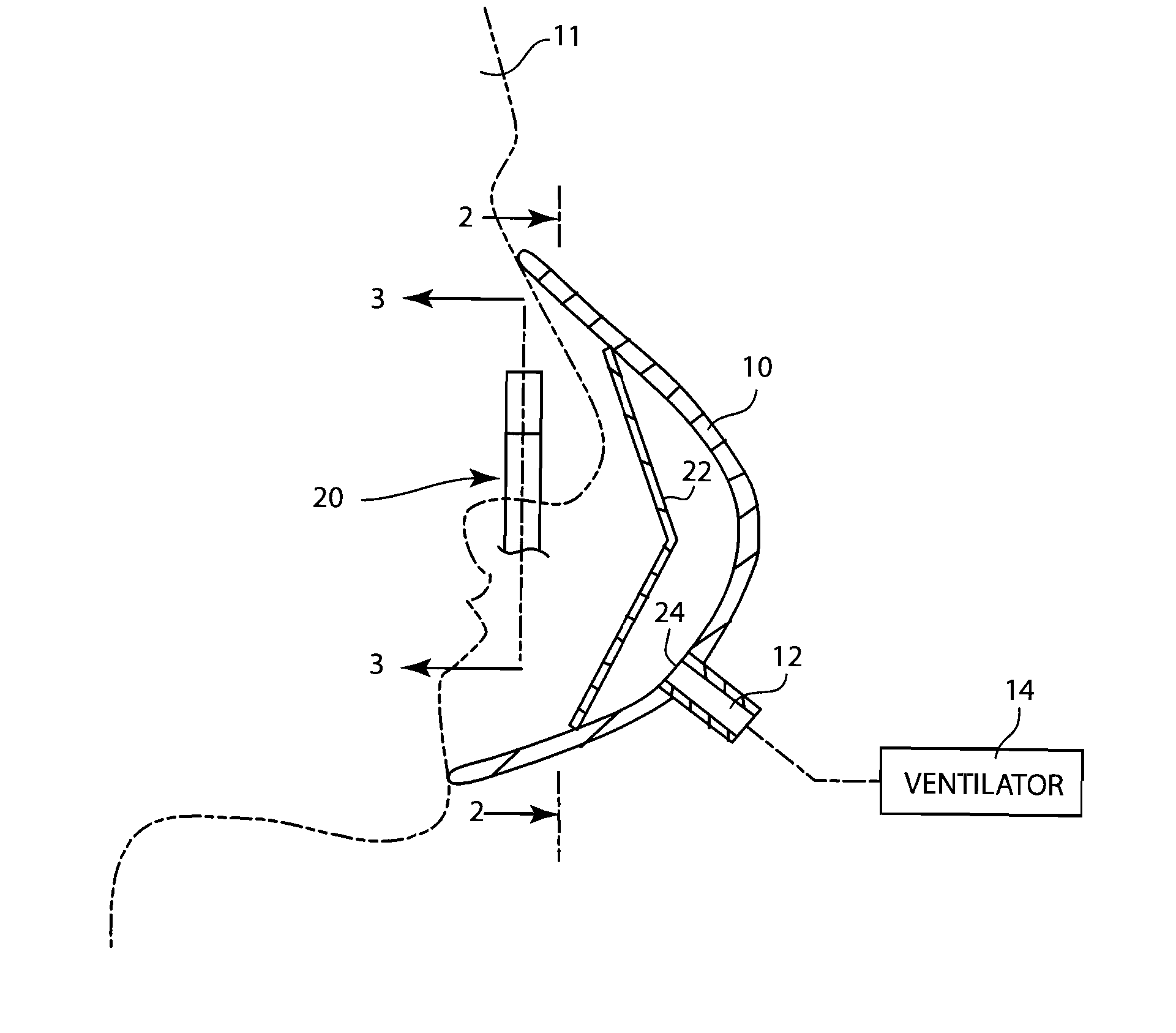
Methods, systems and devices for non-invasive open ventilation for treating airway obstructions
ActiveUS20100252042A1Work lessIncrease airway pressureRespiratorsOperating means/releasing devices for valvesAutonomous breathingControl cell
A system for reducing airway obstructions of a patient may include a ventilator, a control unit, a gas delivery circuit with a proximal end in fluid communication with the ventilator and a distal end in fluid communication with a nasal interface, and a nasal interface. The nasal interface may include at least one jet nozzle, and at least one spontaneous respiration sensor in communication with the control unit for detecting a respiration effort pattern and a need for supporting airway patency. The system may be open to ambient. The control unit may determine more than one gas output velocities. The more than one gas output velocities may be synchronized with different parts of a spontaneous breath effort cycle, and a gas output velocity may be determined by a need for supporting airway patency.
Owner:BREATHE TECHNOLOGIES INC
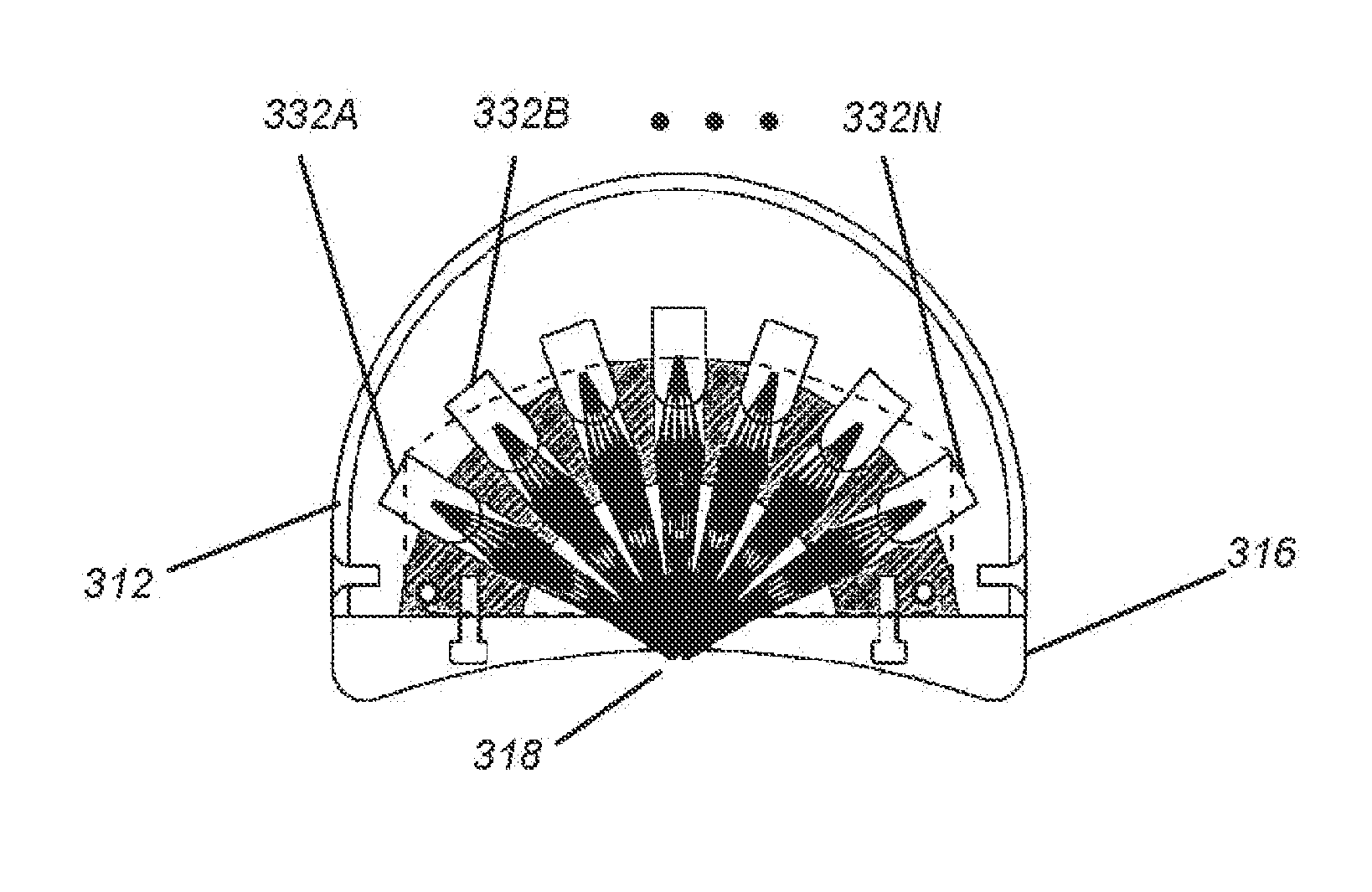
Ventilatory assistance using an external effort sensor
InactiveUS7100609B2SynchronizationRobustness and ease of useRespiratorsOperating means/releasing devices for valvesSuprasternal notchProportional Assist Ventilation
Owner:RESMED LTD
Method for measuring central venous pressure or respiratory effort
Photoplethysmography (PPG) is obtained using one red (e.g., 660 nm) and one infrared (e.g., 880 to 940 nm) light emitting diode with a single photo diode in combination with a pressure transducer thereby allowing both CVP and SpO2 to be measured simultaneously. The system also includes sensors capable of measuring position, angle and / or movement of the sensor or patient. Once the PPG signal is acquired, high pass adaptive and / or notch filtering can be used with one element of the filter from the red and infrared signals used to measure the arterial changes needed to compute SpO2 and the other element of the signal can be used to measure CVP changes.
Owner:WATERMARK MEDICAL
Patient-ventilator synchronization using dual phase sensors
InactiveUS7934499B2Minimum ventilationImprove determinationRespiratorsRespiratory device testingRespiratory phasePressure amplitude
An improved ventilator which delivers ventilatory support that is synchronized with the phase of the patients respiratory efforts and guarantees a targeted minimum ventilation. Improved synchronization is achieved through an instantaneous respiratory phase determination process based upon measured respiratory airflow as well as measured respiratory effort using an effort sensor accessory, preferably a suprasternal notch sensor. The ventilator processes a respiratory airflow signal, a respiratory effort signal and their respective rates of change to determine a phase using standard fuzzy logic methods. A calculated pressure amplitude is adjusted based upon the calculated phase and a smooth pressure waveform template to deliver synchronized ventilation.
Owner:RESMED LTD
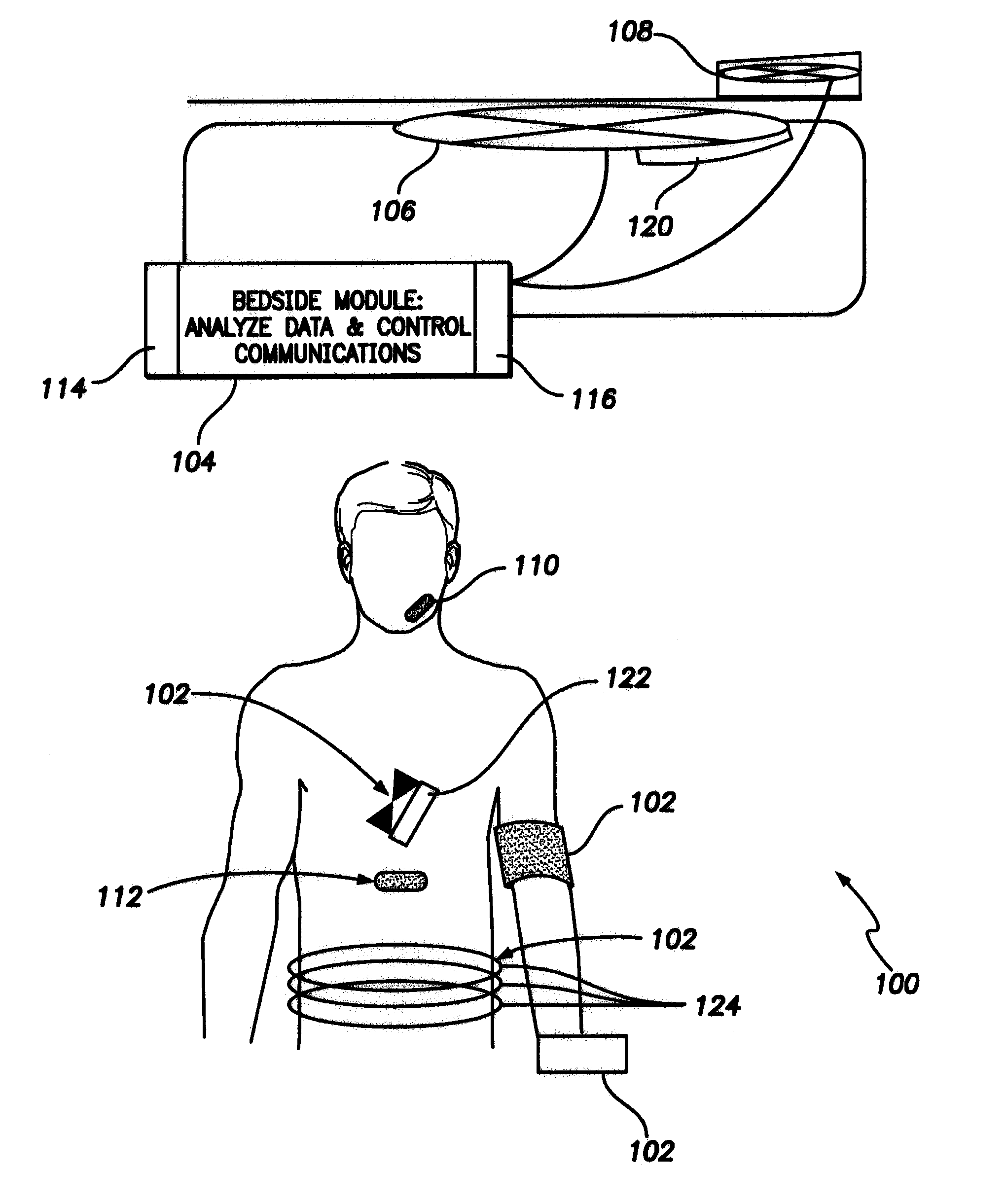
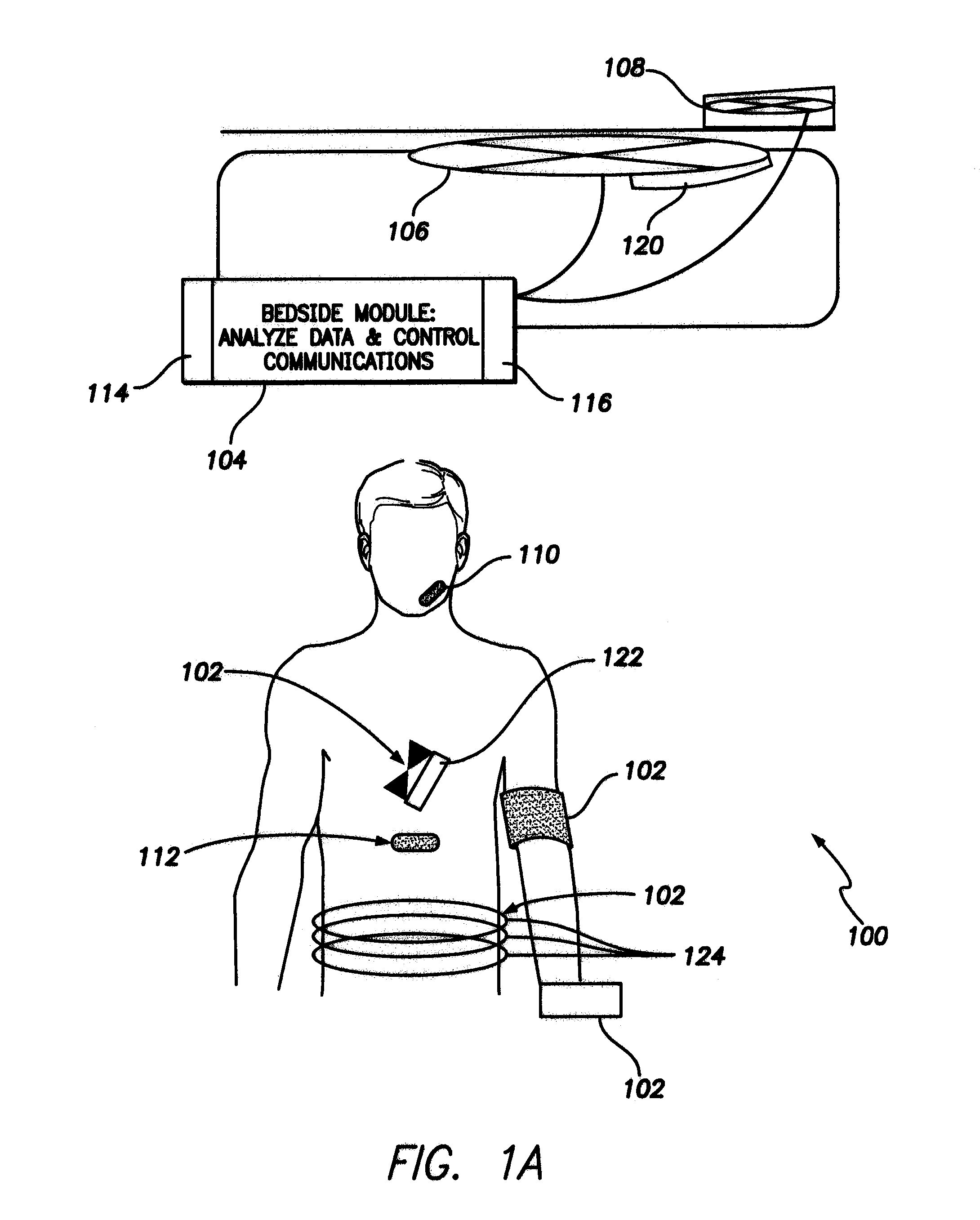
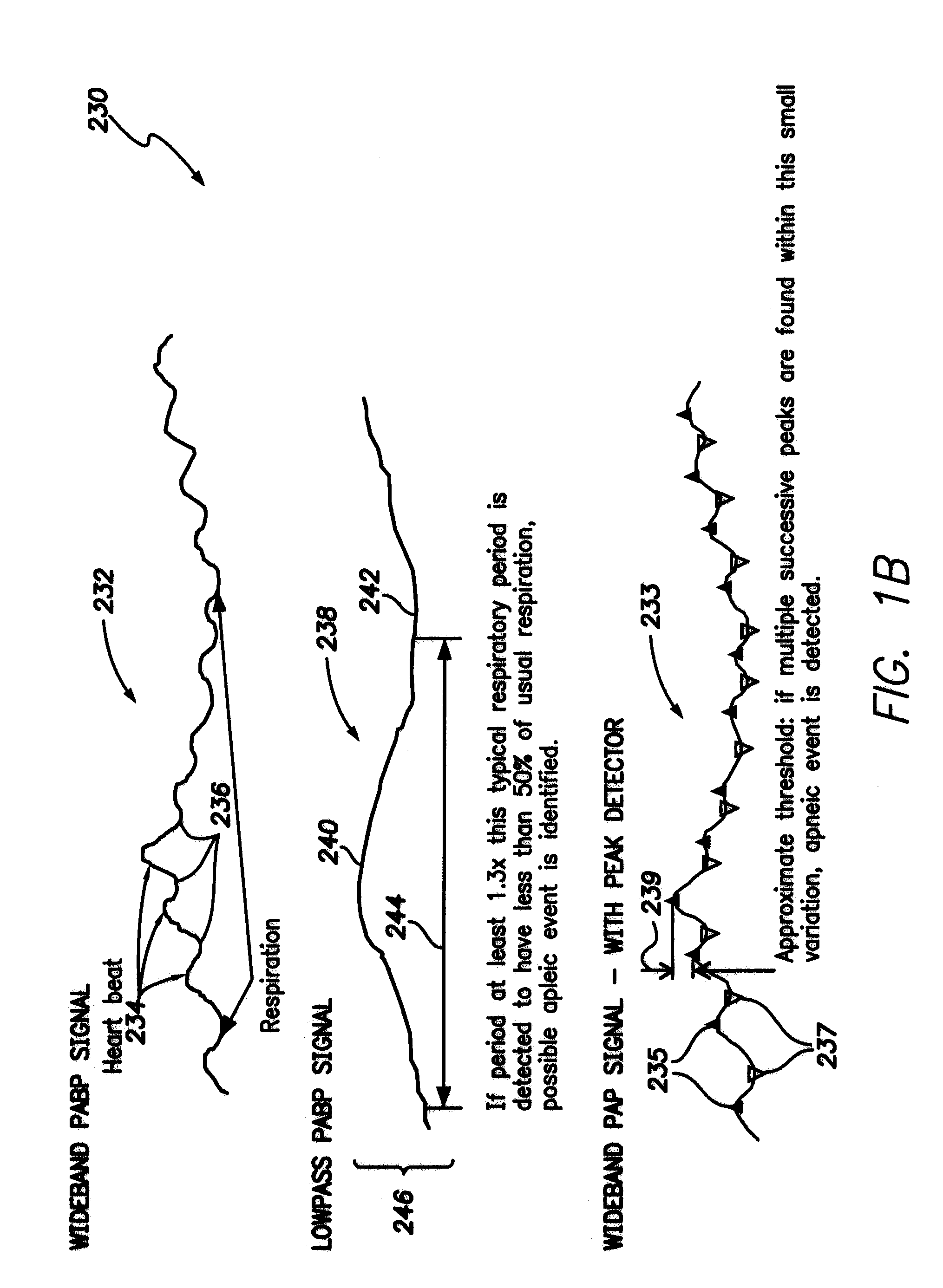
Methods, systems and devices for monitoring respiratory disorders
InactiveUS7690378B1Ultrasonic/sonic/infrasonic diagnosticsChemical protectionRespiratory effortAnesthesia
Methods, systems and devices are provided for monitoring respiratory disorders based on monitored factors of a photoplethysmography (PPG) signal that is representative of peripheral blood volume. The monitored factors can be respiratory effort as well as respiratory rate and / or blood oxygen saturation level. The systems and devices may or may not be implanted in a patient.
Owner:PACESETTER INC
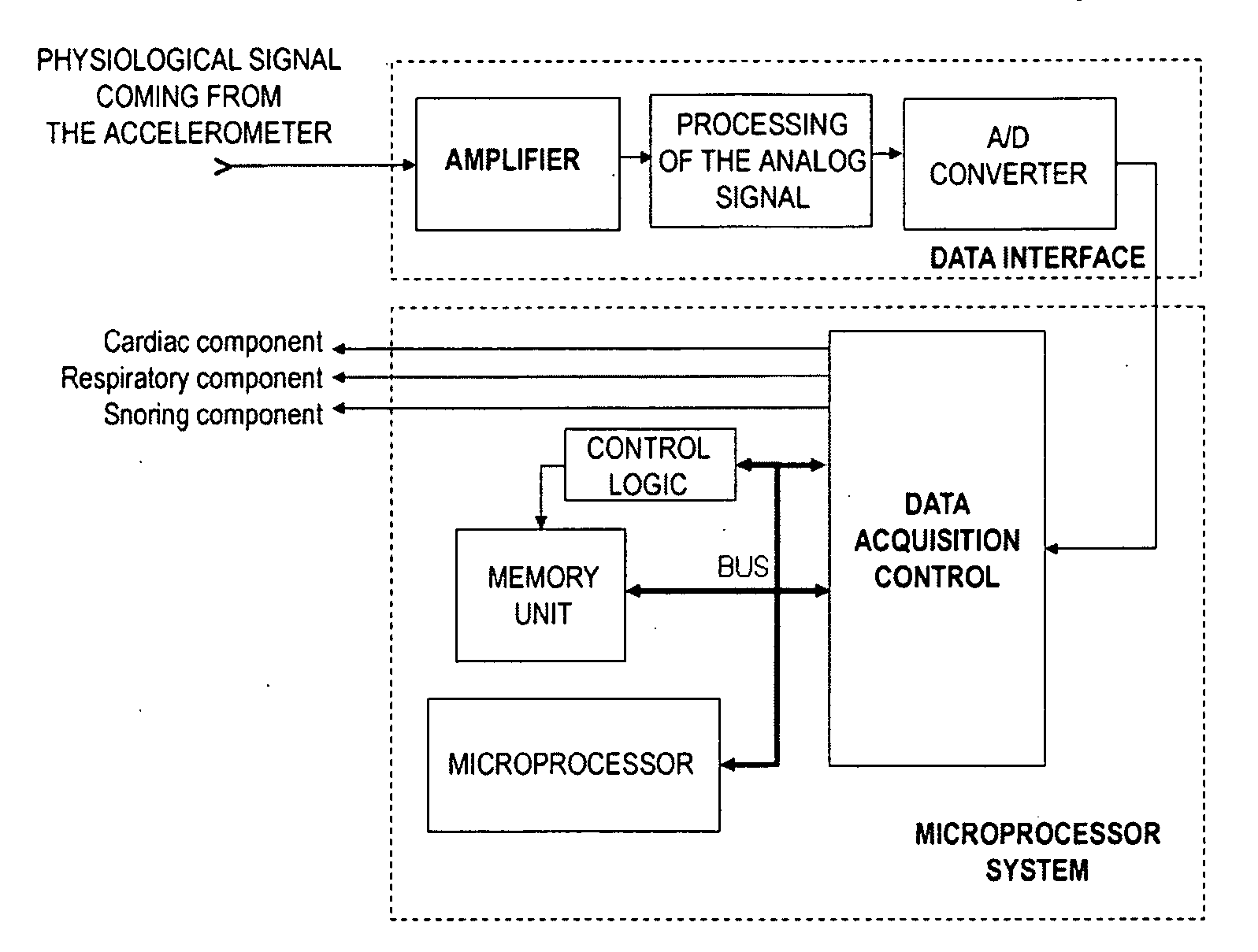
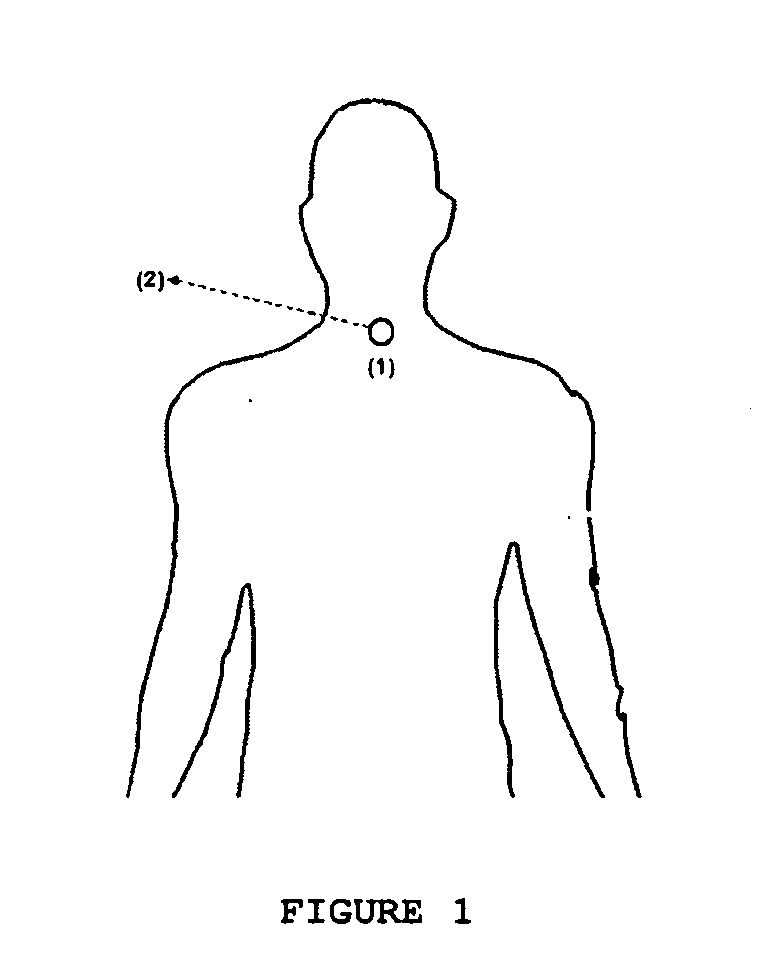
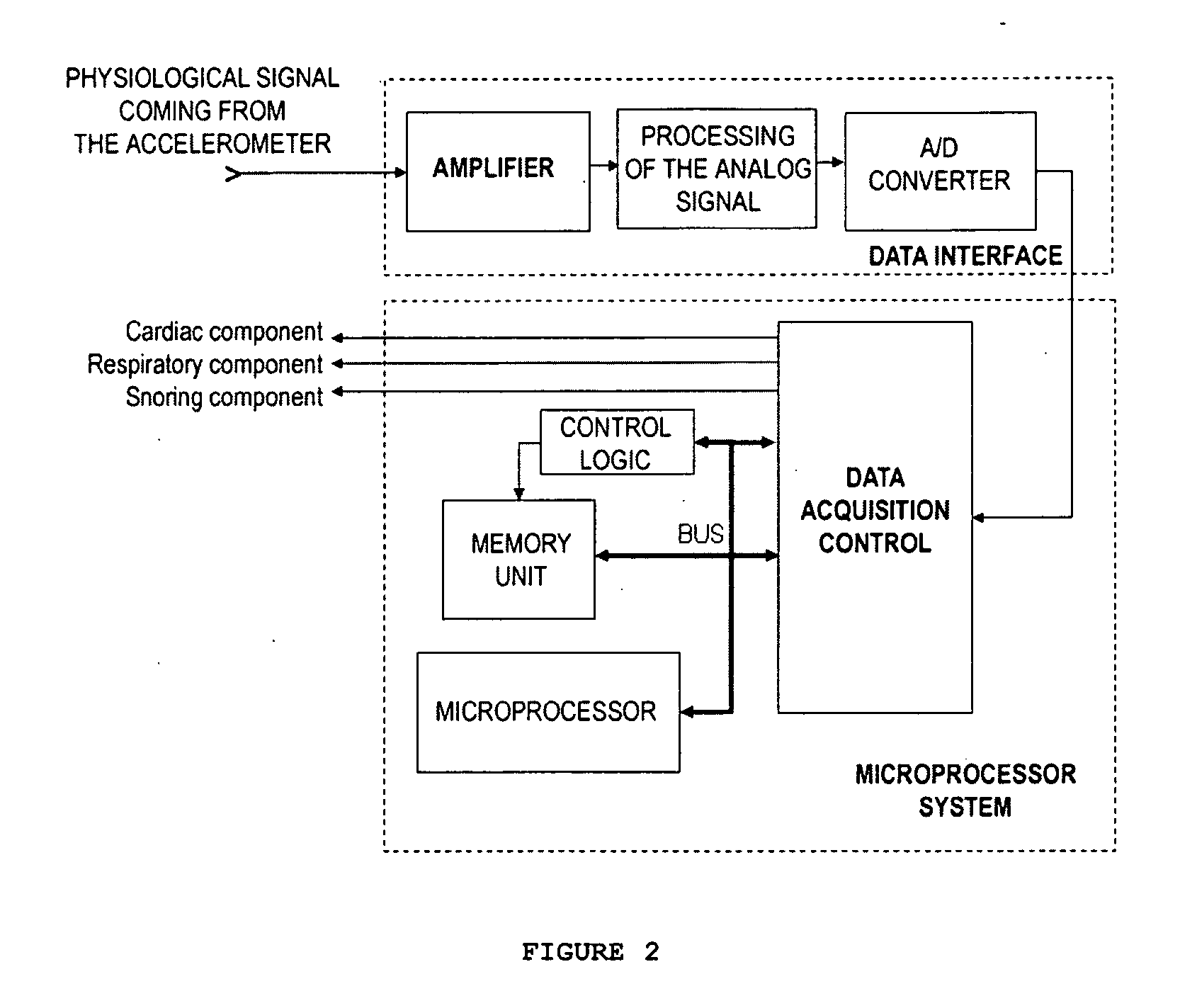
System for monitoring and analysing cardiorespiratory signals and snoring
Extraction of components of the a signal captured by an accelerometer, obtaining information about physiological data such as cardiac, respiratory and snoring activity. The extracted signal components are useful for the diagnosis of different types of abnormal respiratory phenomena during sleep (apneas, hypopneas and respiratory efforts associated to micro-arousals).
Owner:UNIV DE CADIZ
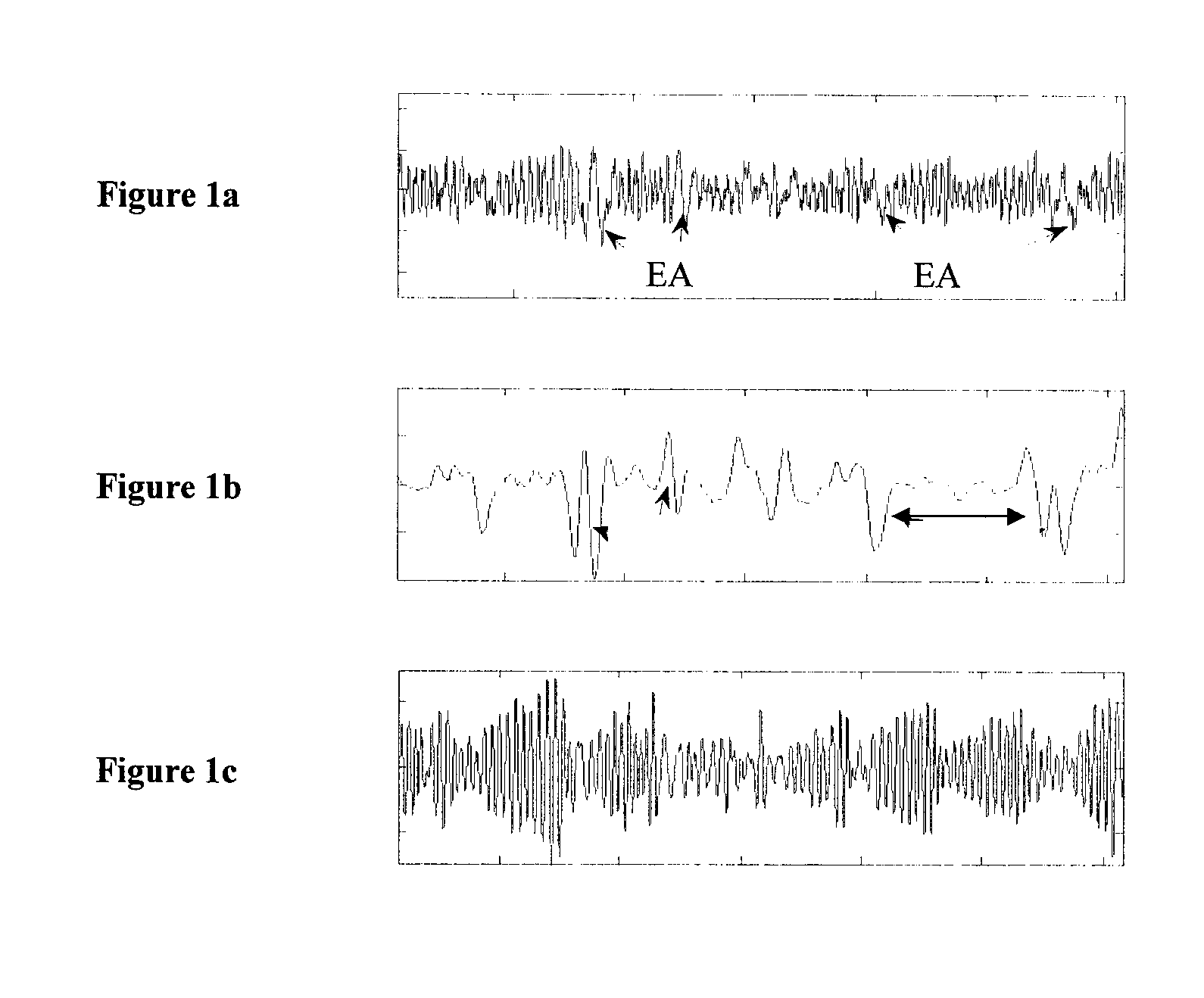
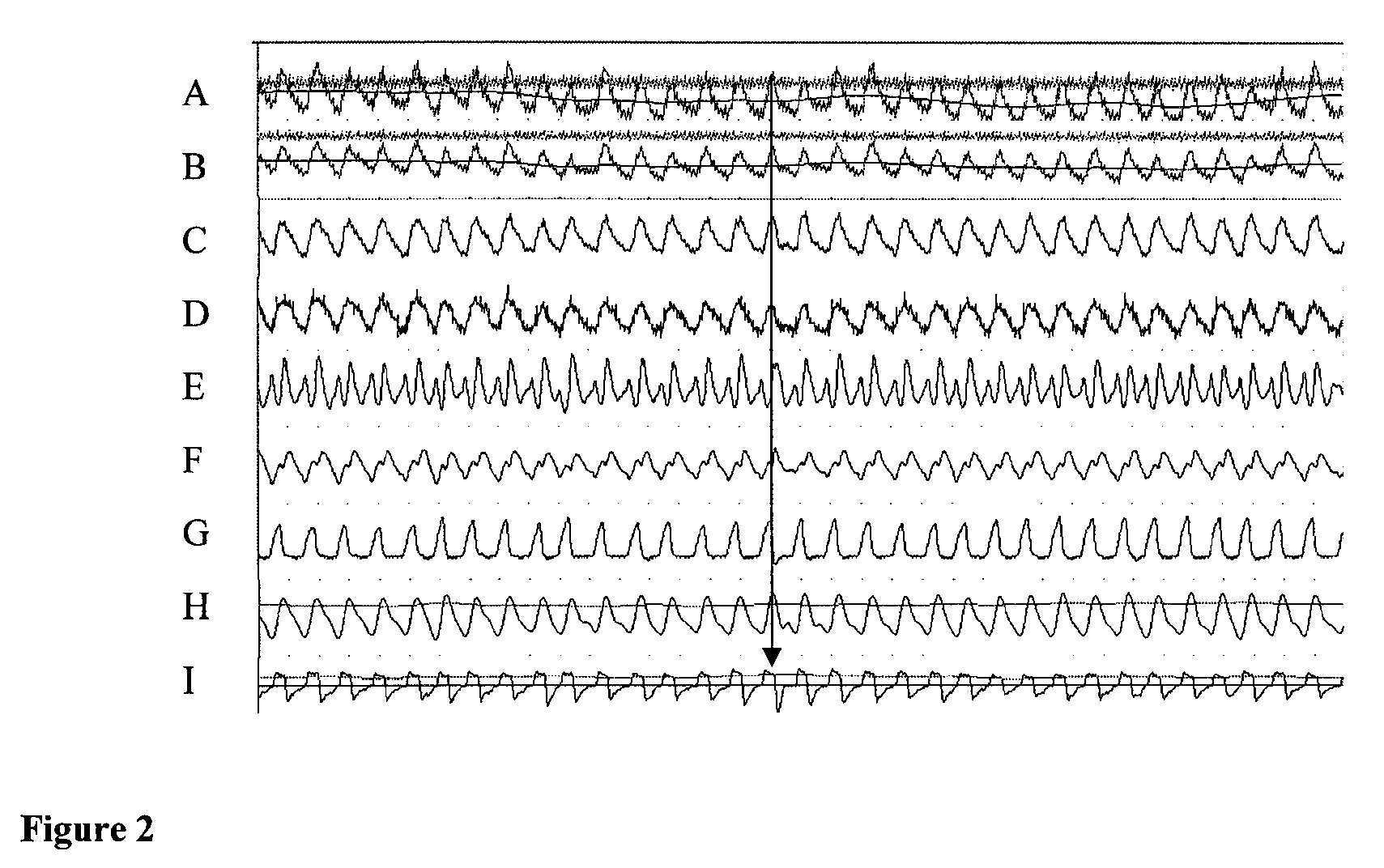
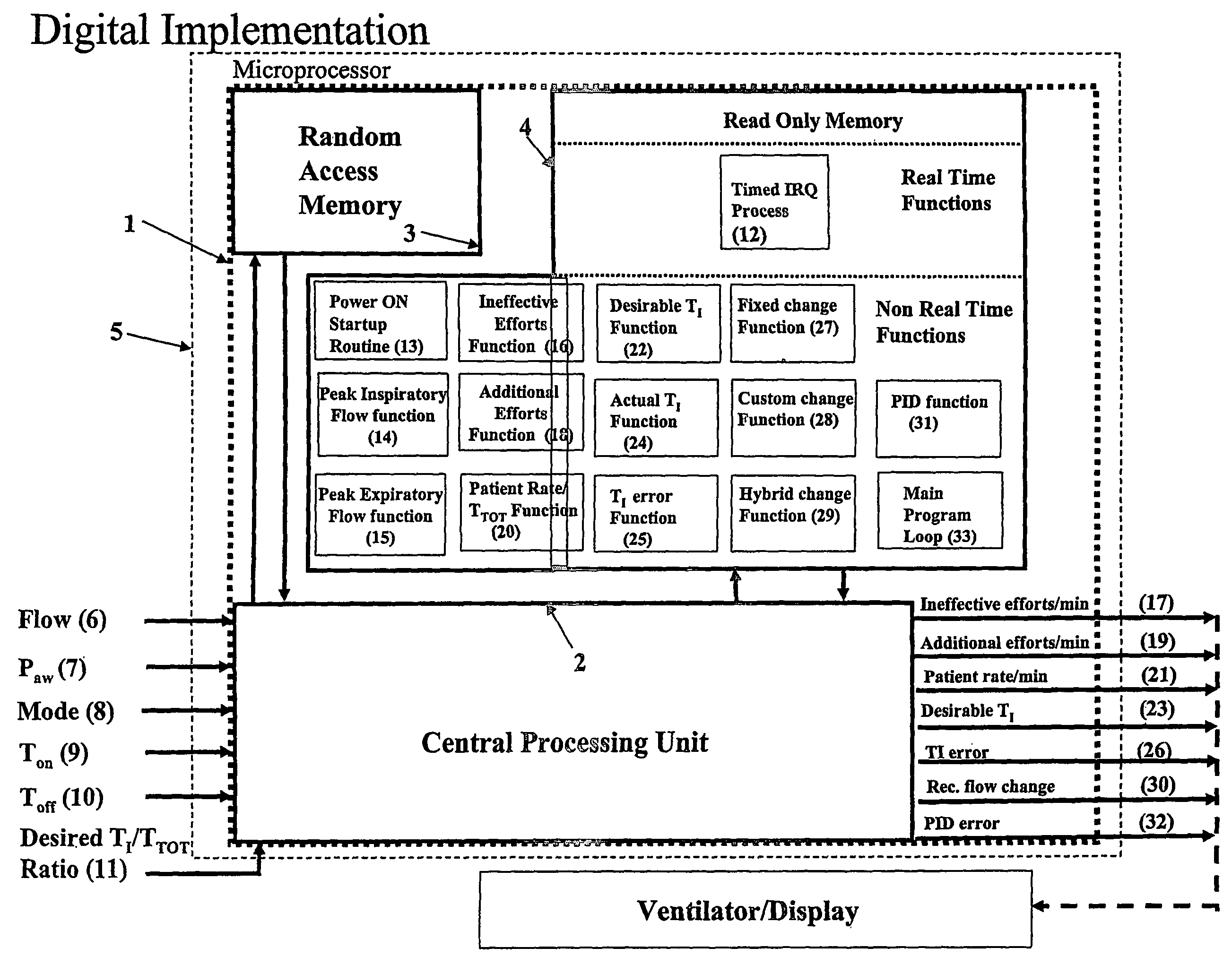
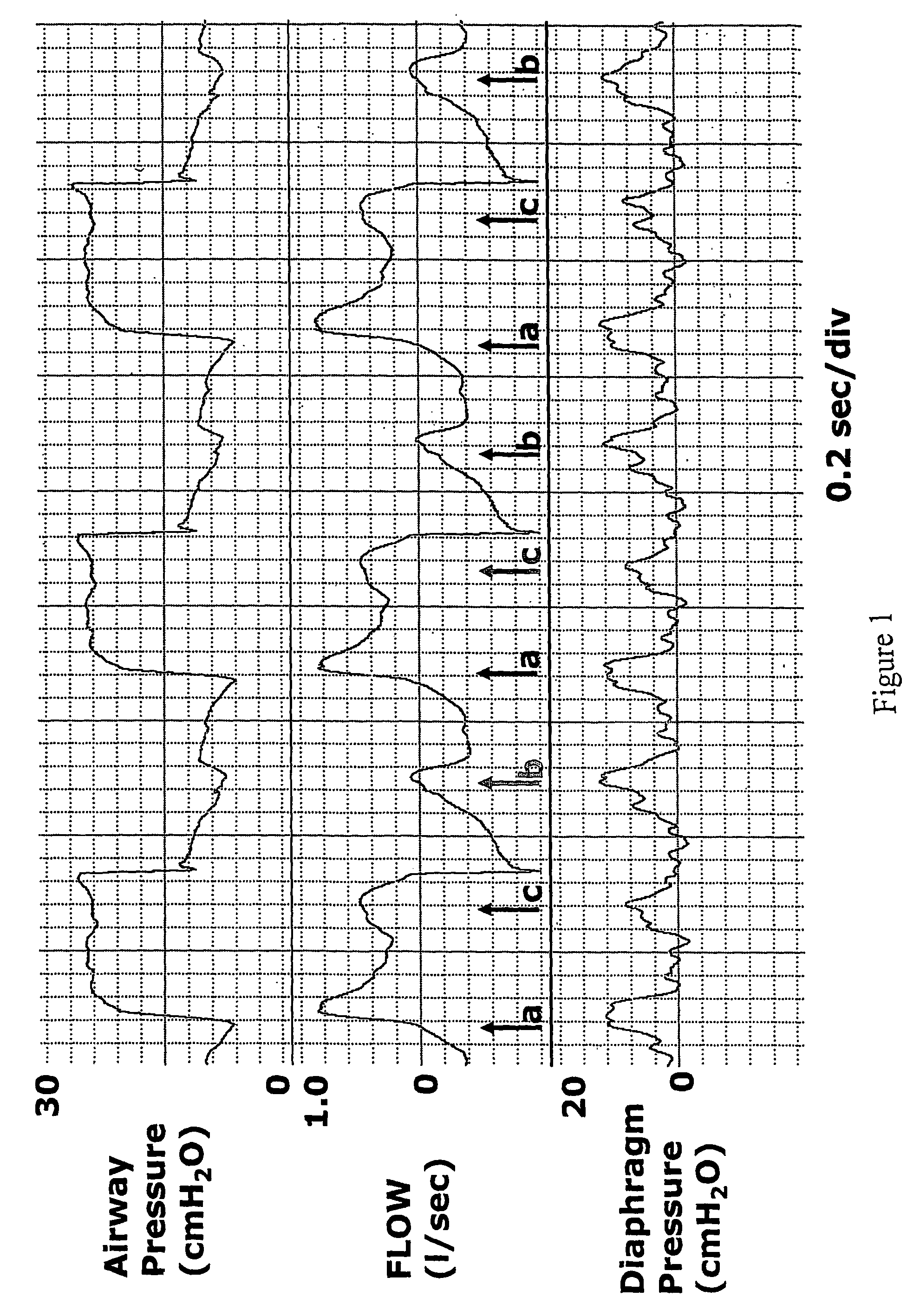
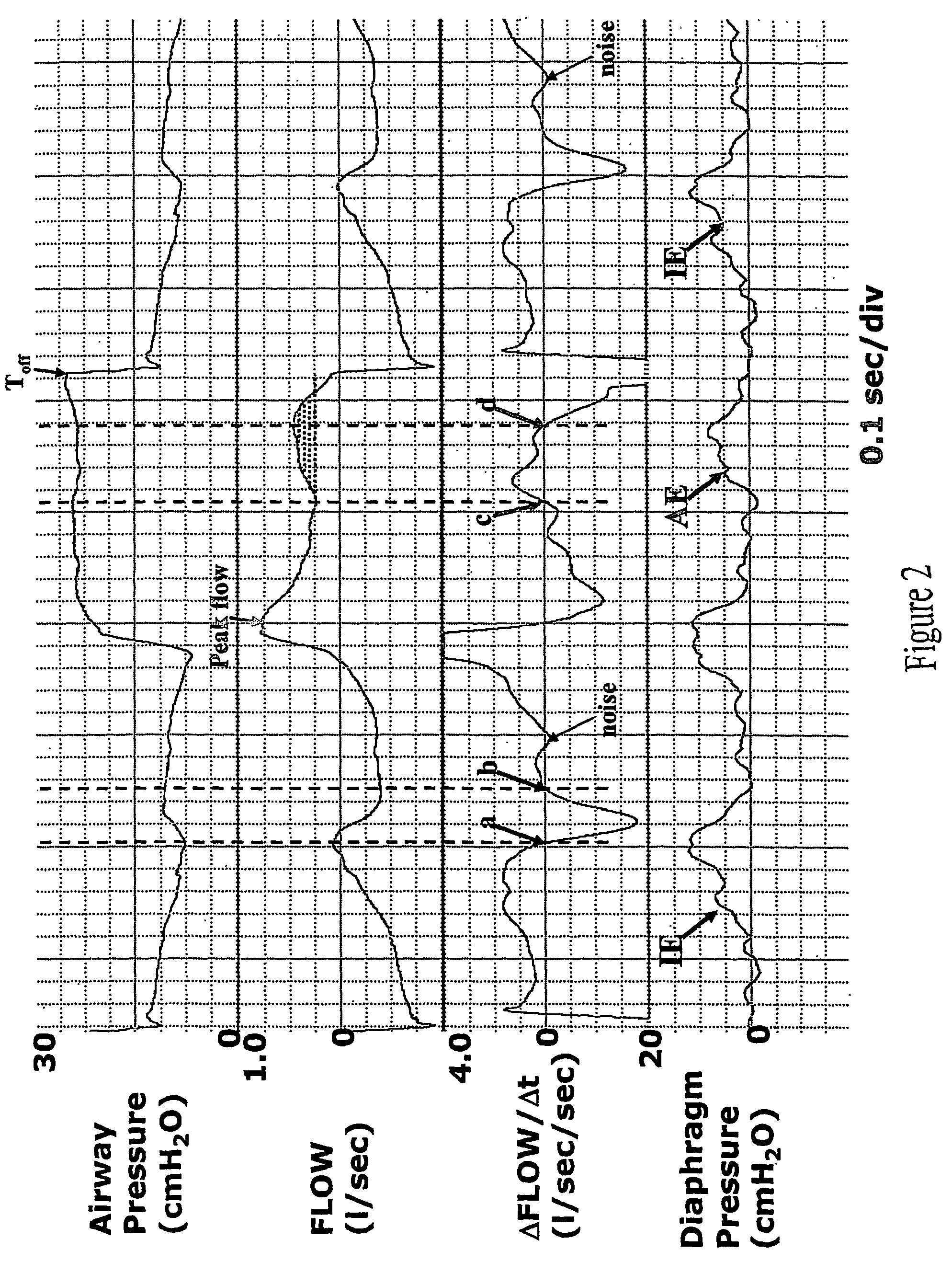
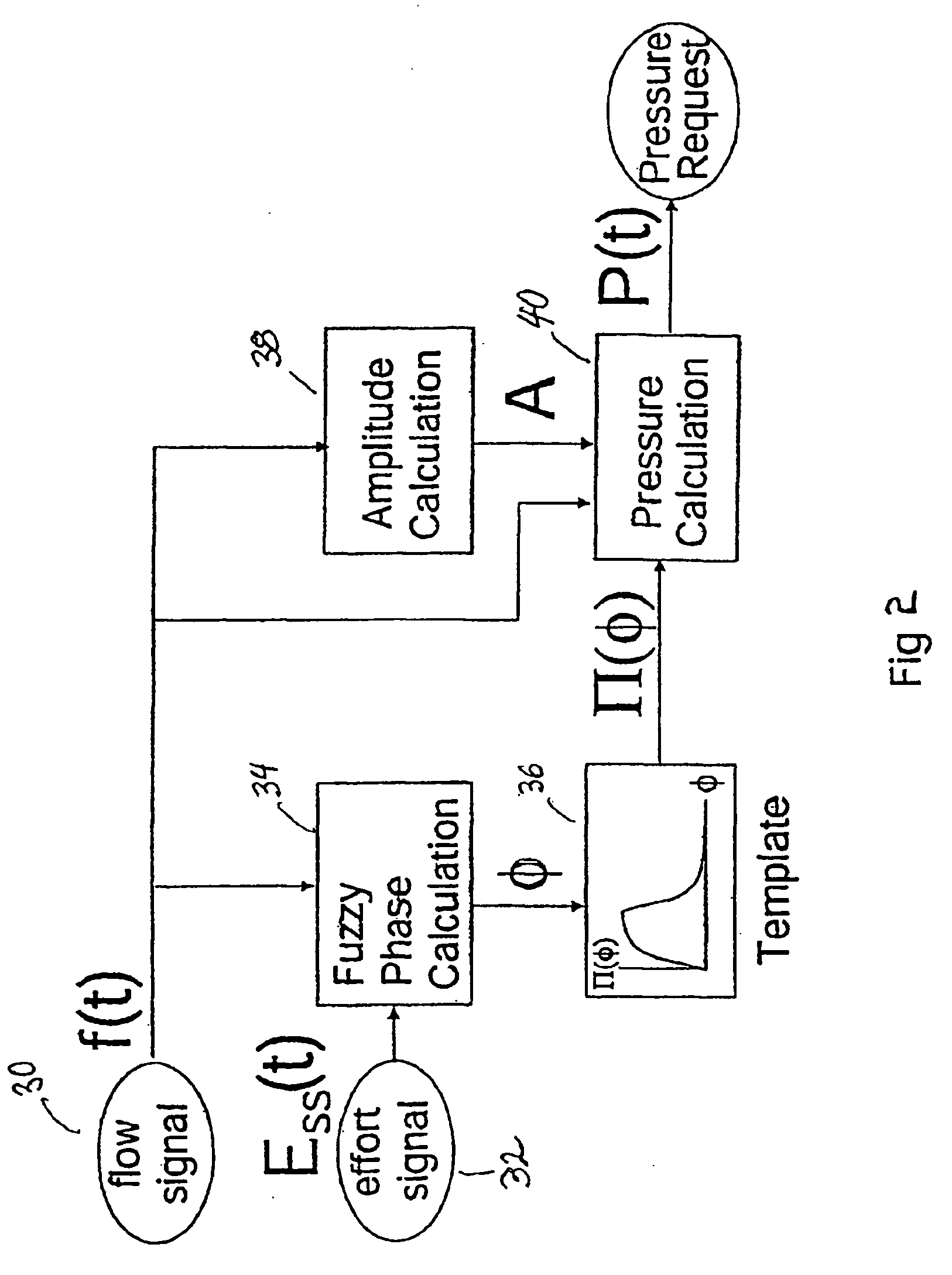
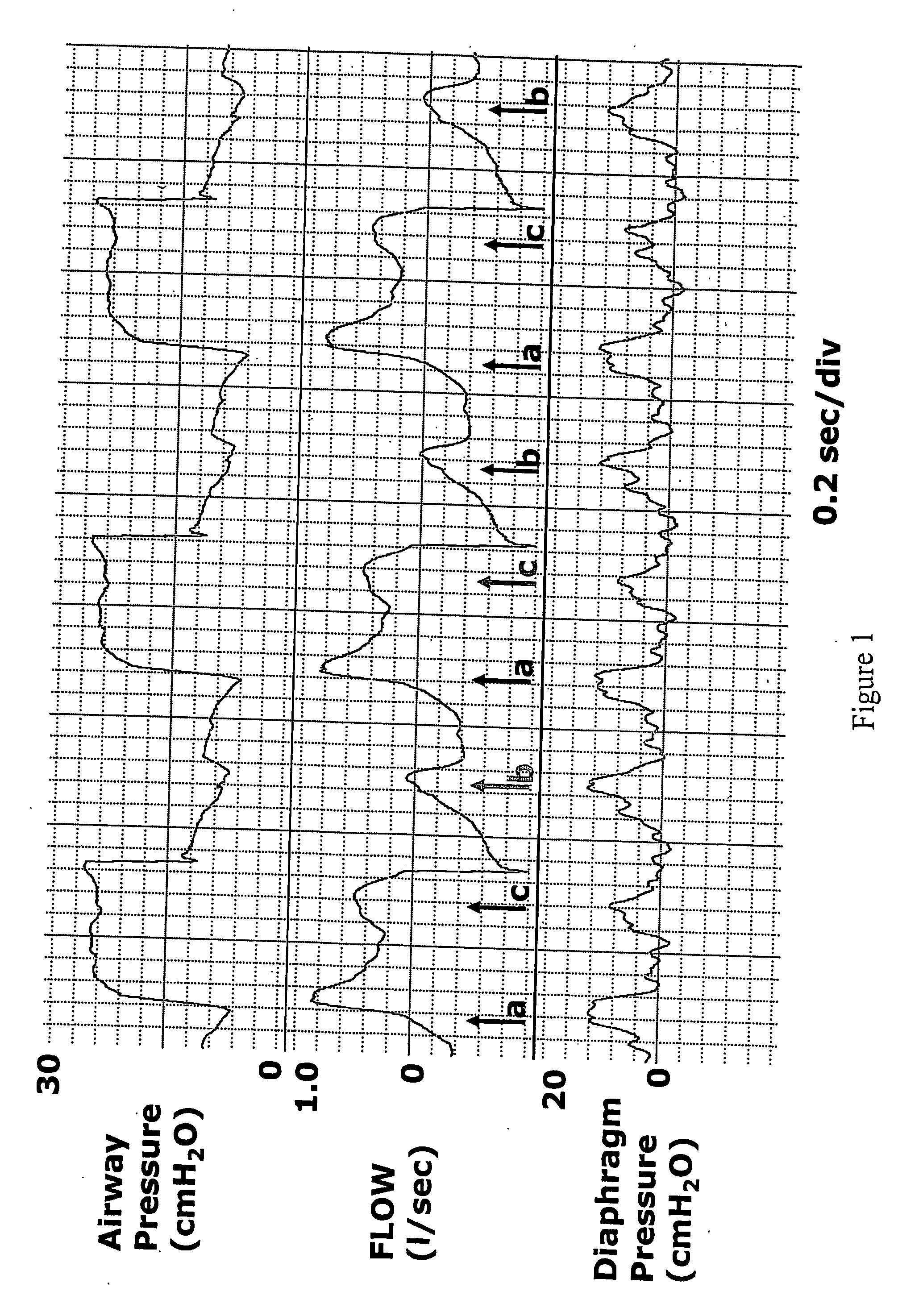
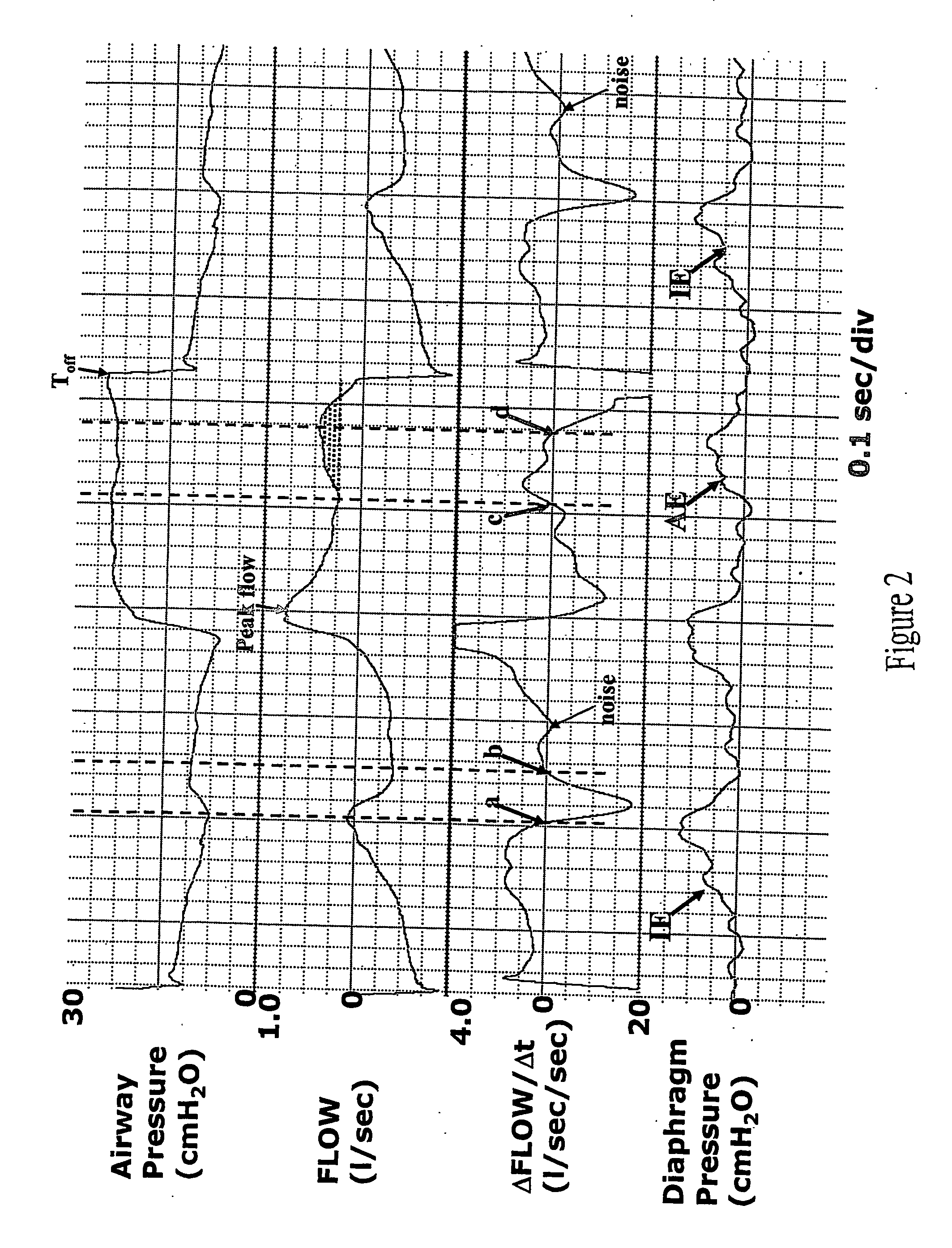
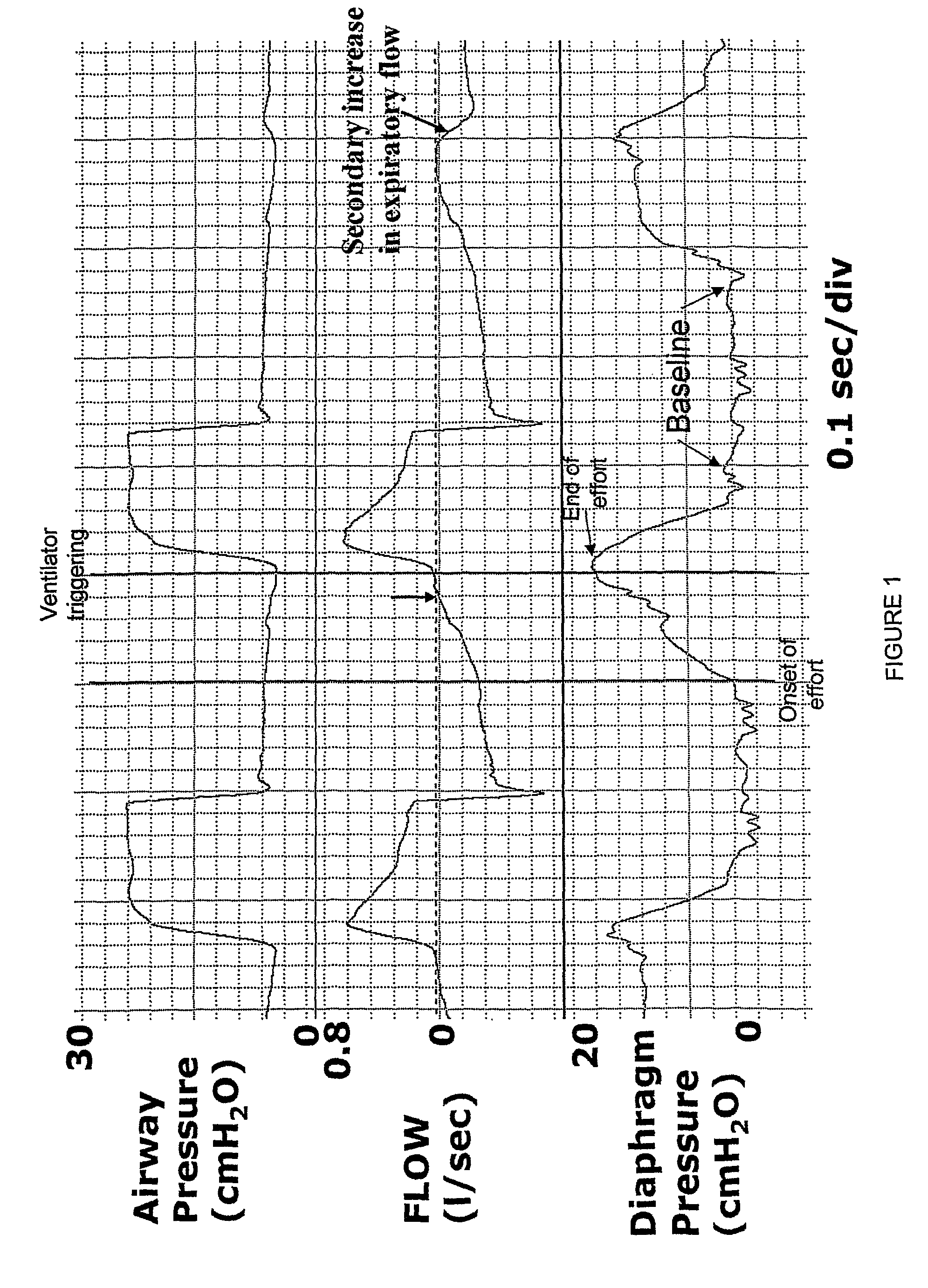
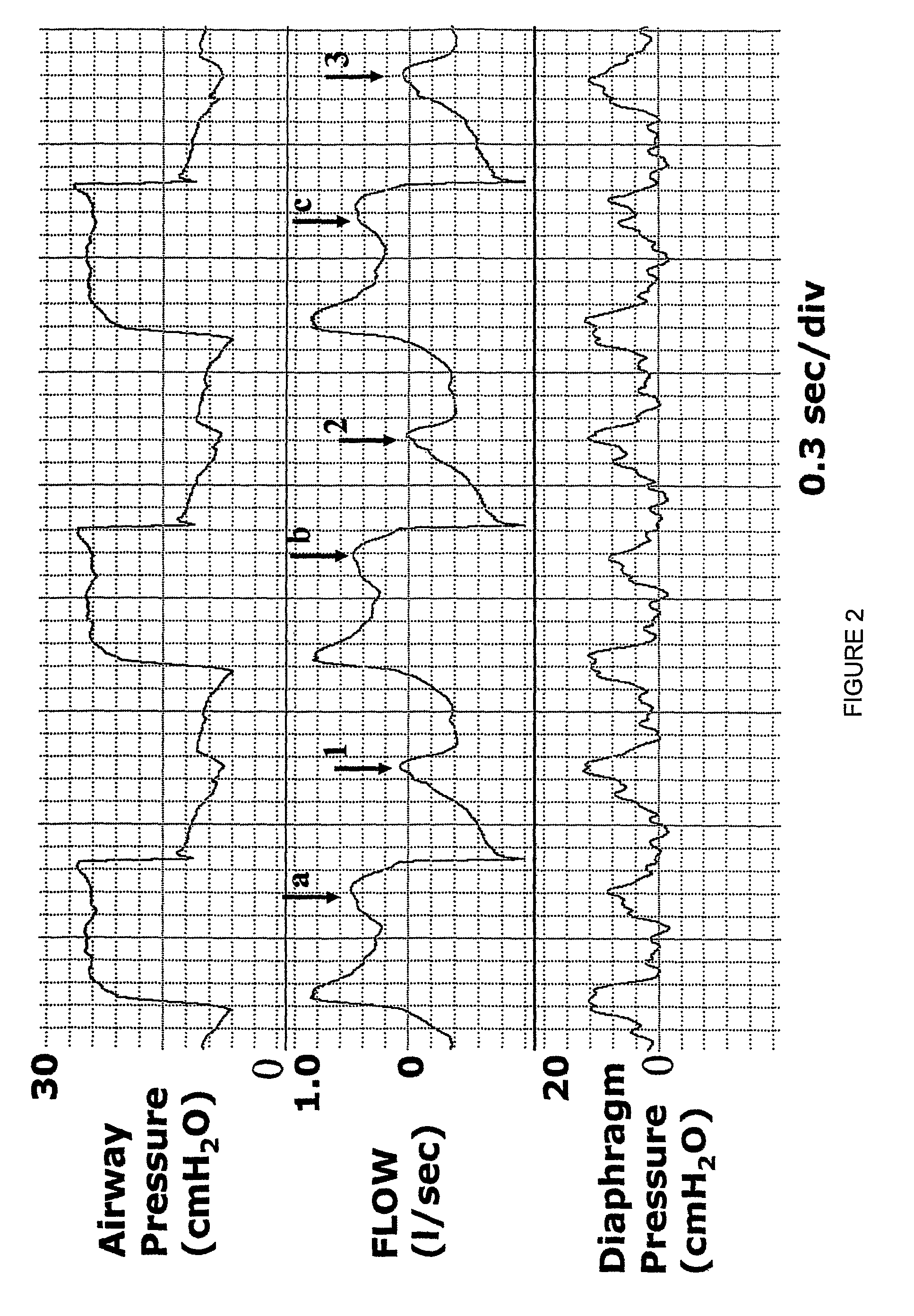
Synchrony between end of ventilator cycles and end of patient efforts during assisted ventilation
InactiveUS7819815B2RespiratorsOperating means/releasing devices for valvesAssisted ventilationInhalation
Automatic ongoing adjustment of the cycling-off time of ventilator inflation phase during assisted ventilation in accordance with true respiratory rate of a patient. Electrical signals are generated corresponding to the gas flow exchanged between patient and ventilator (flow) and / or to airway pressure (Paw) and the true respiratory rate of the patient (patient RR) is determined on an ongoing basis from the flow and / or Paw. The current average cycle duration of patient respiratory efforts (current patient TTOT) is estimated from patient RR. A current desirable duration of the inhalation phase (desirable TI) is calculated from the product of current patient TTOT a TI / TTOT ratio chosen to be in the physiological range, usually 0.25 to 0.50. The ventilator phase is caused to terminate in accordance with the desirable TI.
Owner:YRT
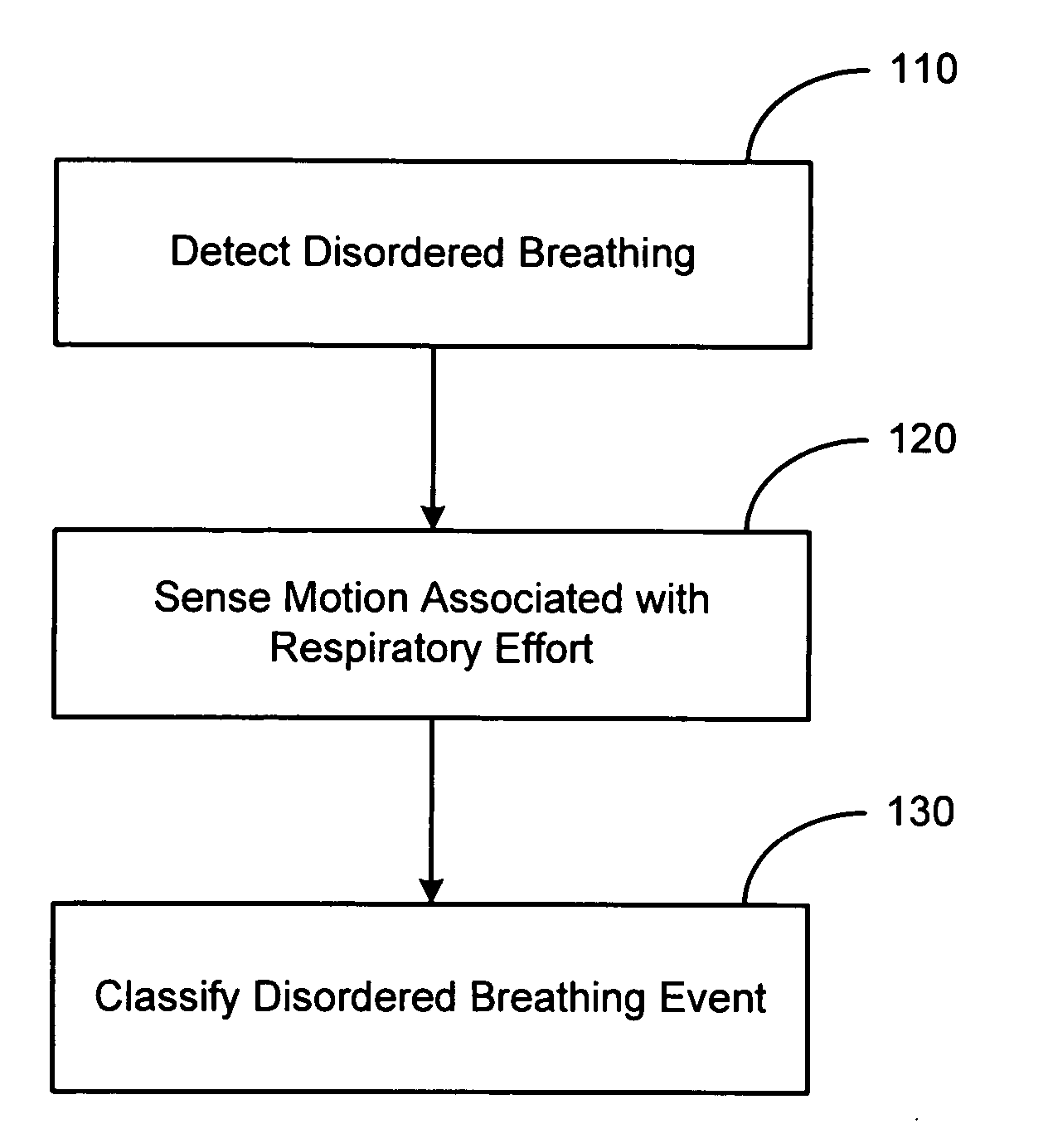
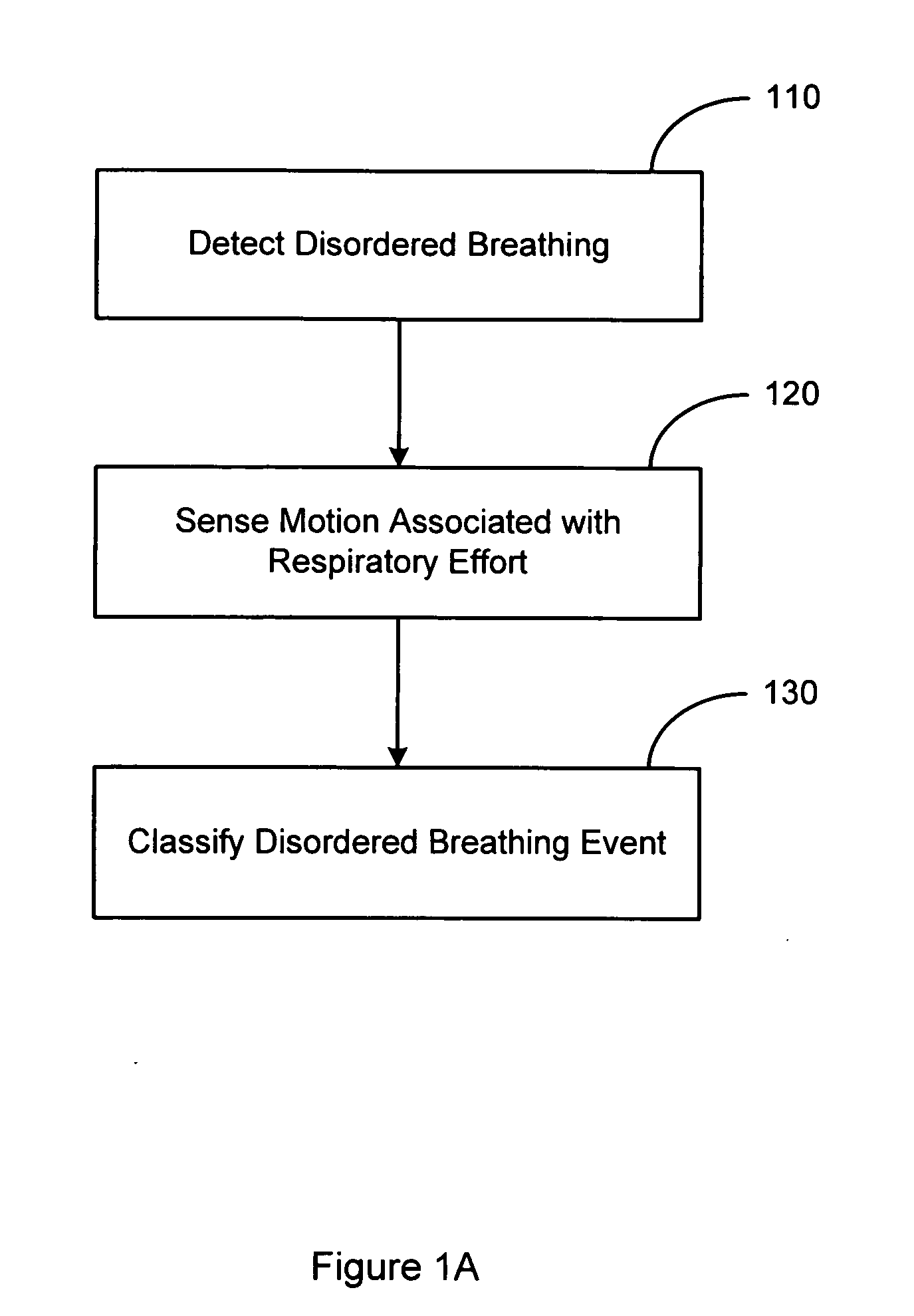
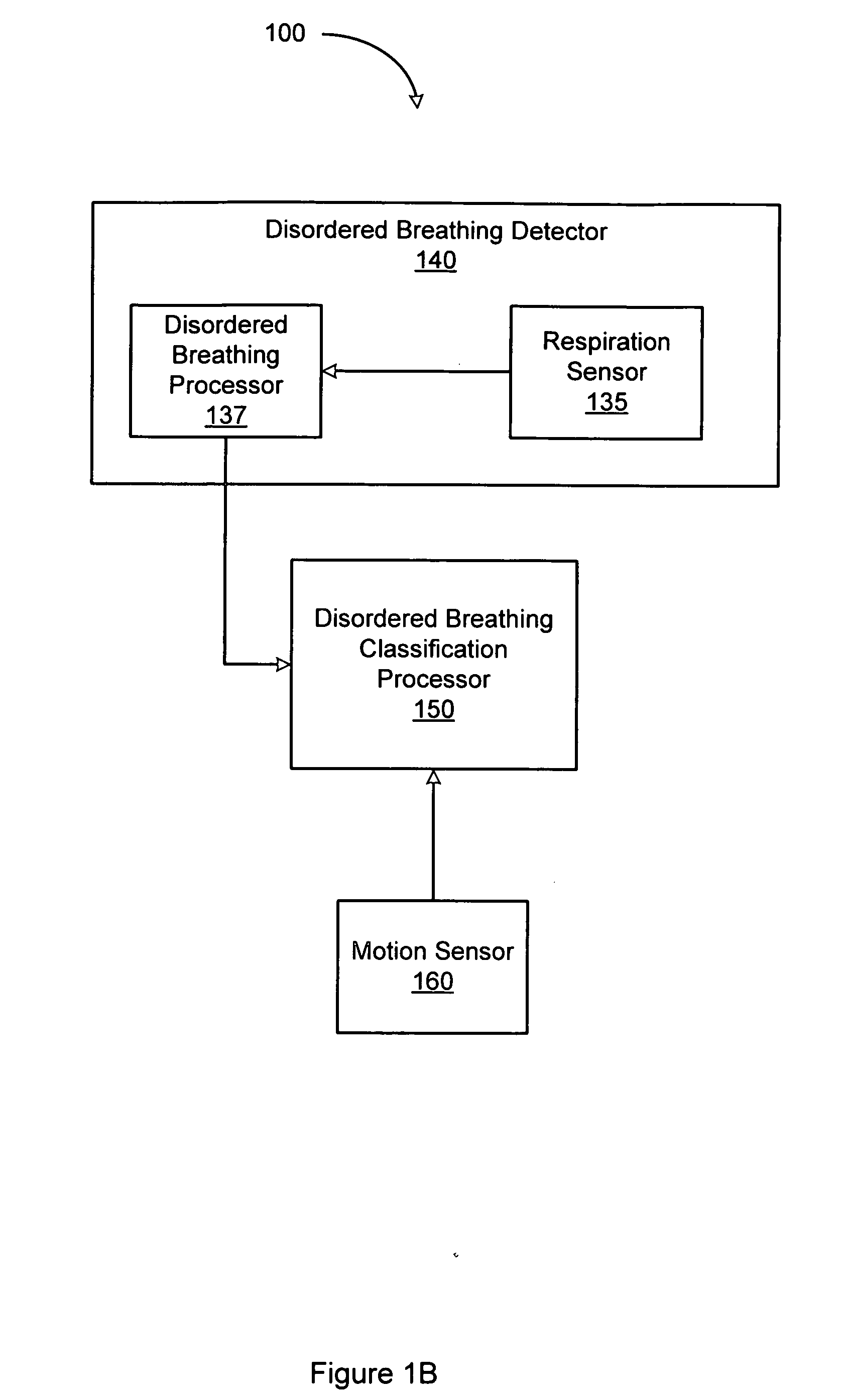
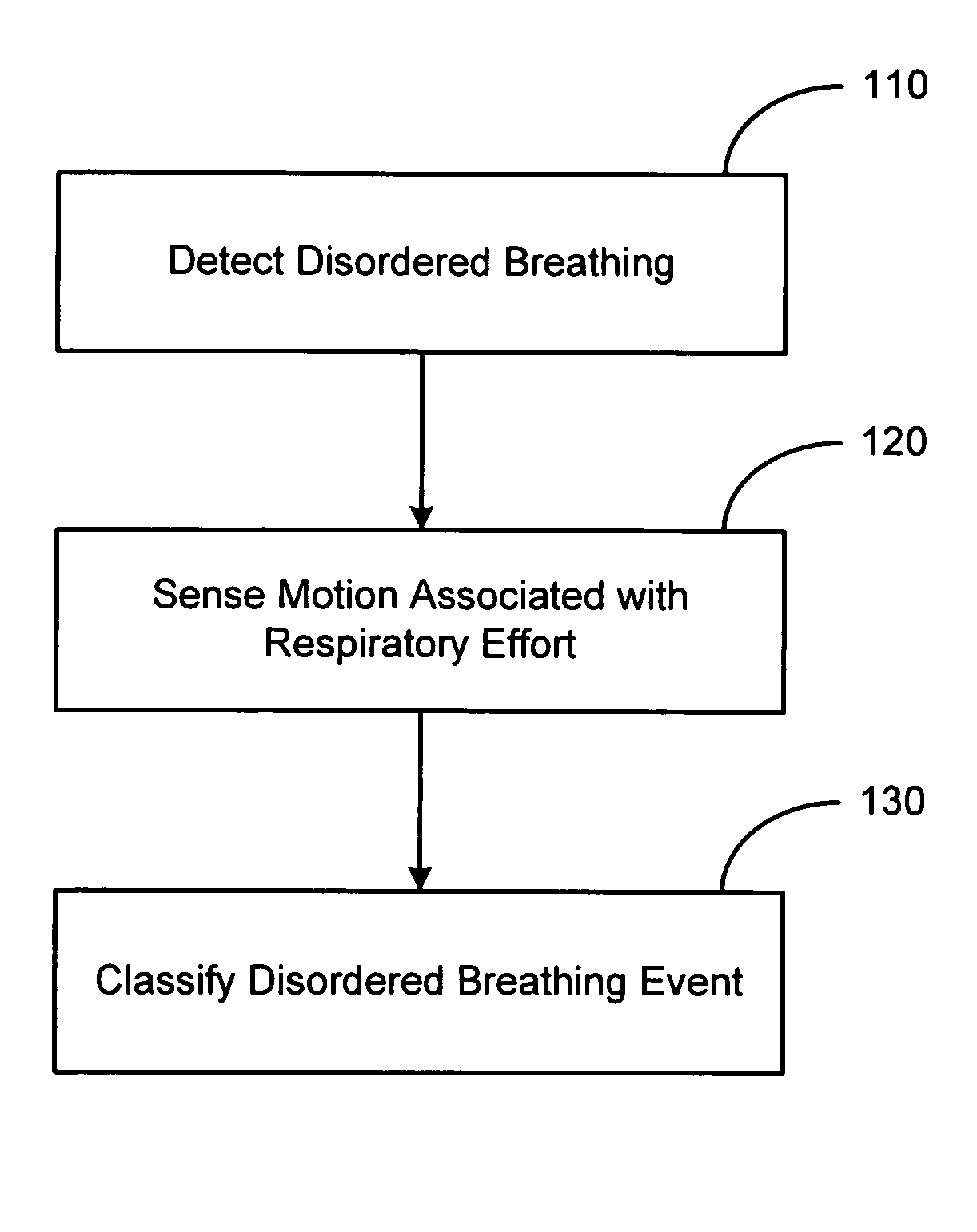
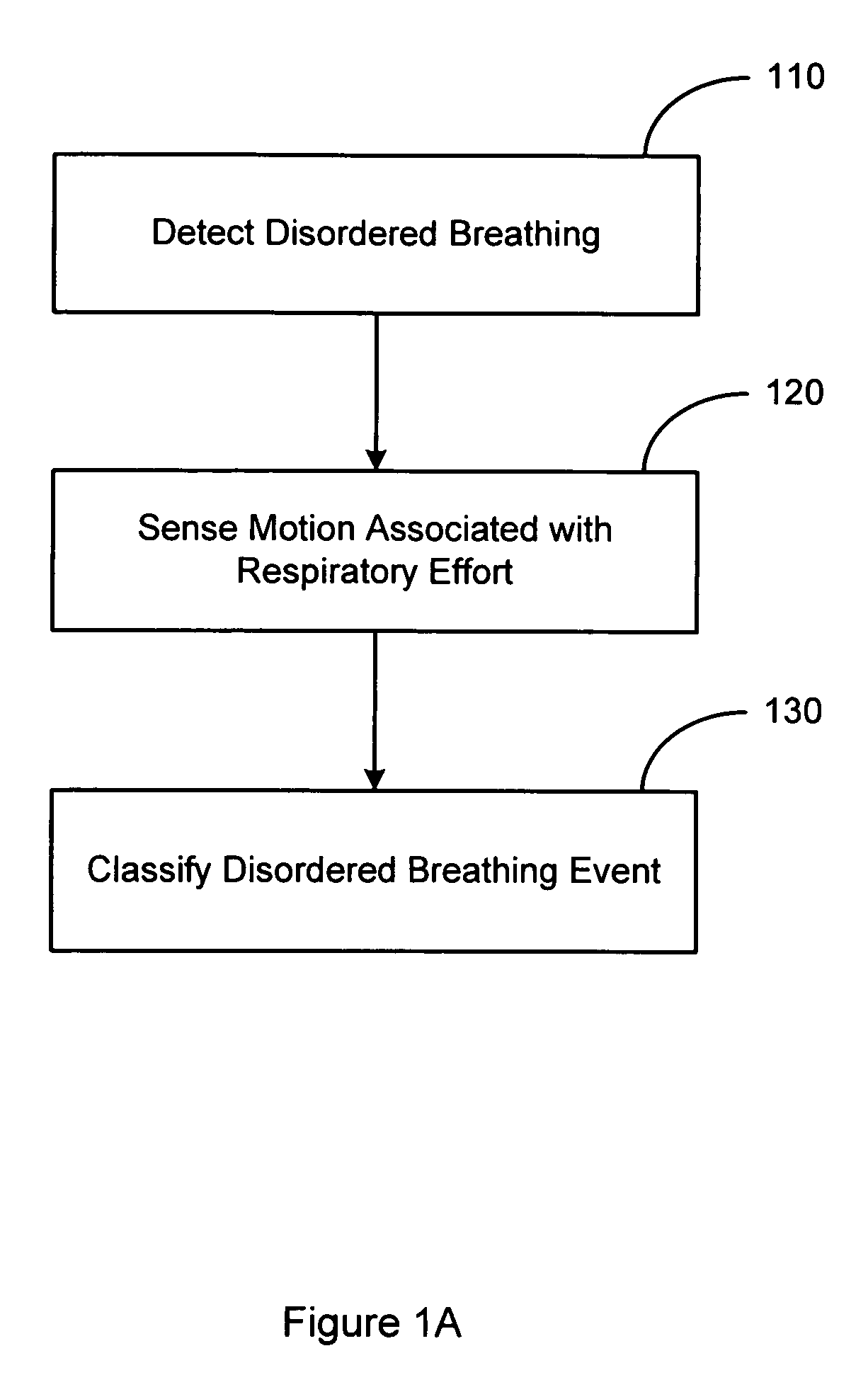
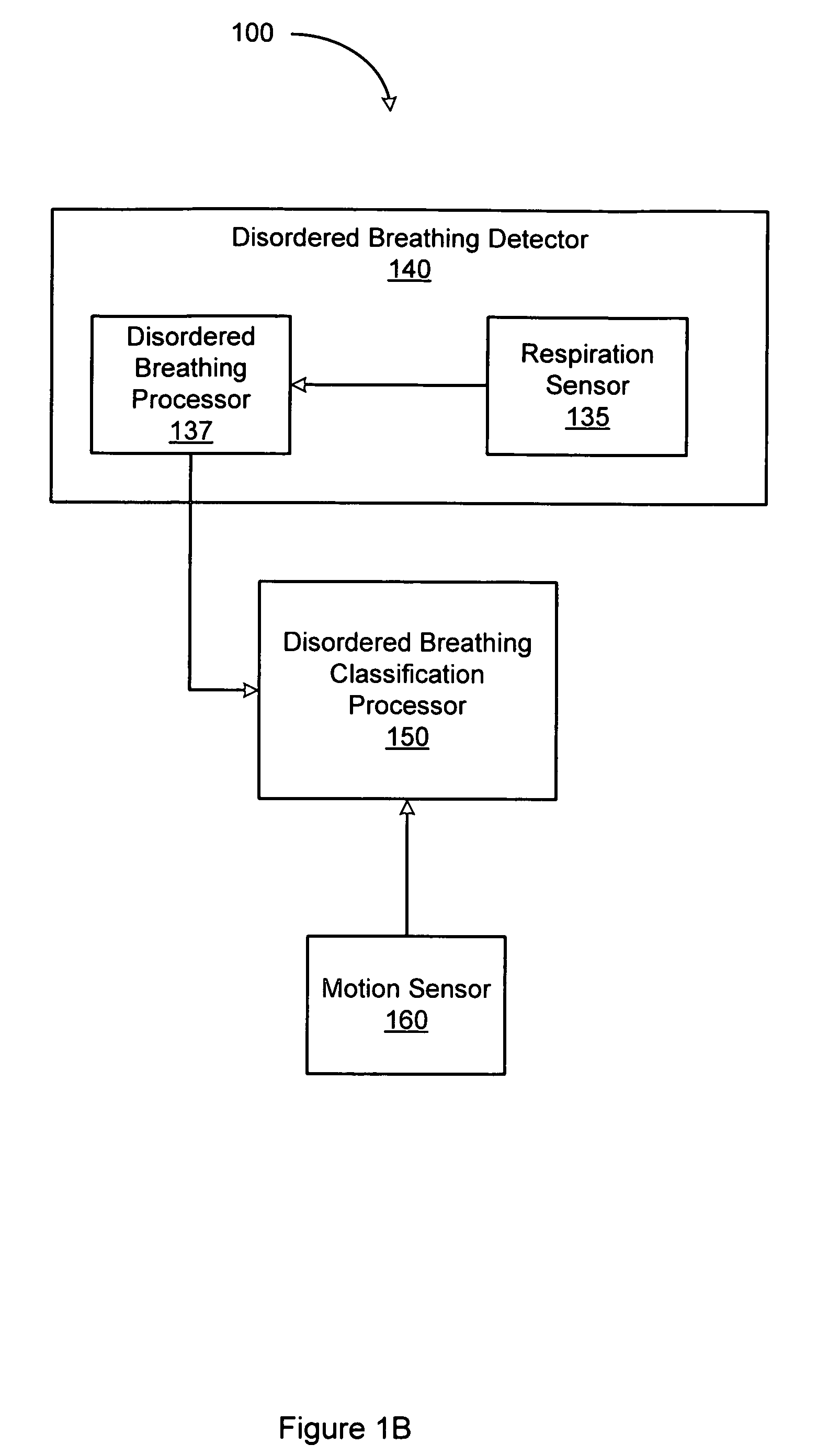
System and method for discrimination of central and obstructive disordered breathing events
Disordered breathing events may be classified as central, obstructive or a combination of central an obstructive in origin based on patient motion associated with respiratory effort. Central disordered breathing is associated with disrupted respiration with reduced respiratory effort. Obstructive disordered breathing is associated with disrupted respiration accompanied by respiratory effort. A disordered breathing classification system includes a disordered breathing detector and a respiratory effort motion sensor. Components of the disordered breathing classification system may be fully or partially implantable.
Owner:CARDIAC PACEMAKERS INC
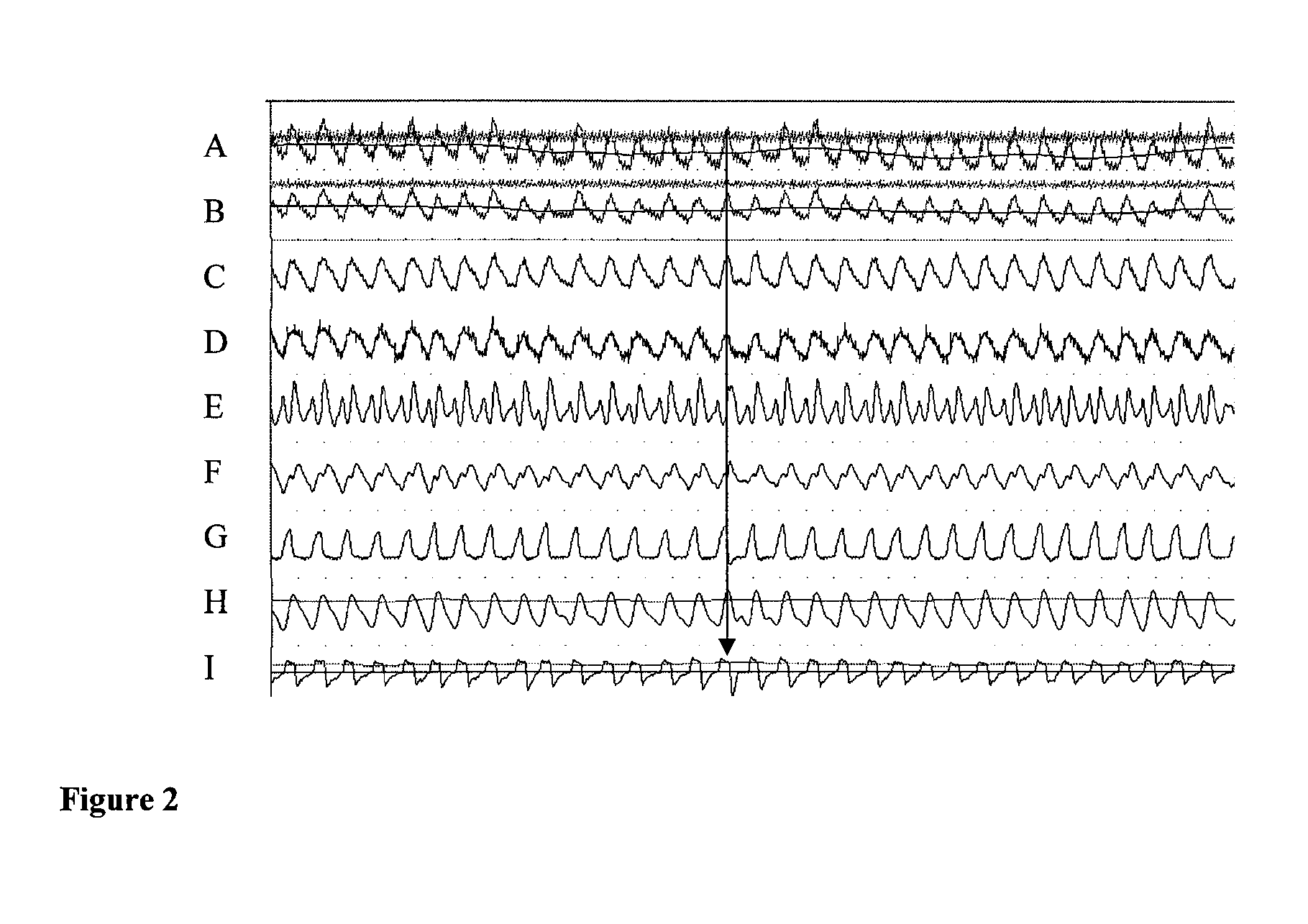
Method of automatically controlling a respiration system and a corresponding respirator
ActiveUS20090159082A1Convenient for patientAccurate operationRespiratorsOperating means/releasing devices for valvesAutomatic controlProportional Assist Ventilation
A method of automatically controlling a respiration system for proportional assist ventilation with a control device and with a ventilator. An electrical signal is recorded by electromyography with electrodes on the chest in order to obtain a signal uemg(t) representing the breathing activity. The respiratory muscle pressure pmus(t) is determined by calculating it in the control unit from measured values for the airway pressure and the volume flow Flow(t) as well as the patient's lung mechanical parameters. The breathing activity signal uemg(t) is transformed by means of a preset transformation rule into a pressure signal pemg(uemg)(t)) such that the mean deviation of the resulting transformed pressure signal pemg(t) from the respiratory muscle pressure pmus(t) is minimized. The respiratory effort pressure ppat(t) is determined as a weighted mean according to ppat(t)=a·pmus(t)+(1−a)·pemg(t), where a is a parameter selected under the boundary condition 0≦a≦1. The airway pressure paw(t) to be delivered is calculated as a function of preselected degrees of assist VA (Volume Assist) and FA (Flow Assist) by sliding adaptation aspaw(ti)=k0+∑j=1nkj·paw(ti-j)+∑j=0nhj·ppat(ti-j)wherein ti is a current point in time and ti−j, wherein j=1, . . . , n, are previous points in time of a periodical time-discrete sampling, and kj and hj, wherein j=1, . . . , n are parameters dependent on resistance (R), elastance (E), positive end-expiratory pressure (PEEP), intrinsic PEEP (iPEEP), Volume Assist (VA) and Flow Assist (FA) and the sampling time Δt, and the ventilator is set by the control unit so as to provide this airway pressure paw(ti)
Owner:DRAGERWERK AG
System and method for discrimination of central and obstructive disordered breathing events
InactiveUS7510531B2ElectroencephalographyElectro-oculographyRespiratory effortIntensive care medicine
Disordered breathing events may be classified as central, obstructive or a combination of central an obstructive in origin based on patient motion associated with respiratory effort. Central disordered breathing is associated with disrupted respiration with reduced respiratory effort. Obstructive disordered breathing is associated with disrupted respiration accompanied by respiratory effort. A disordered breathing classification system includes a disordered breathing detector and a respiratory effort motion sensor. Components of the disordered breathing classification system may be fully or partially implantable.
Owner:CARDIAC PACEMAKERS INC
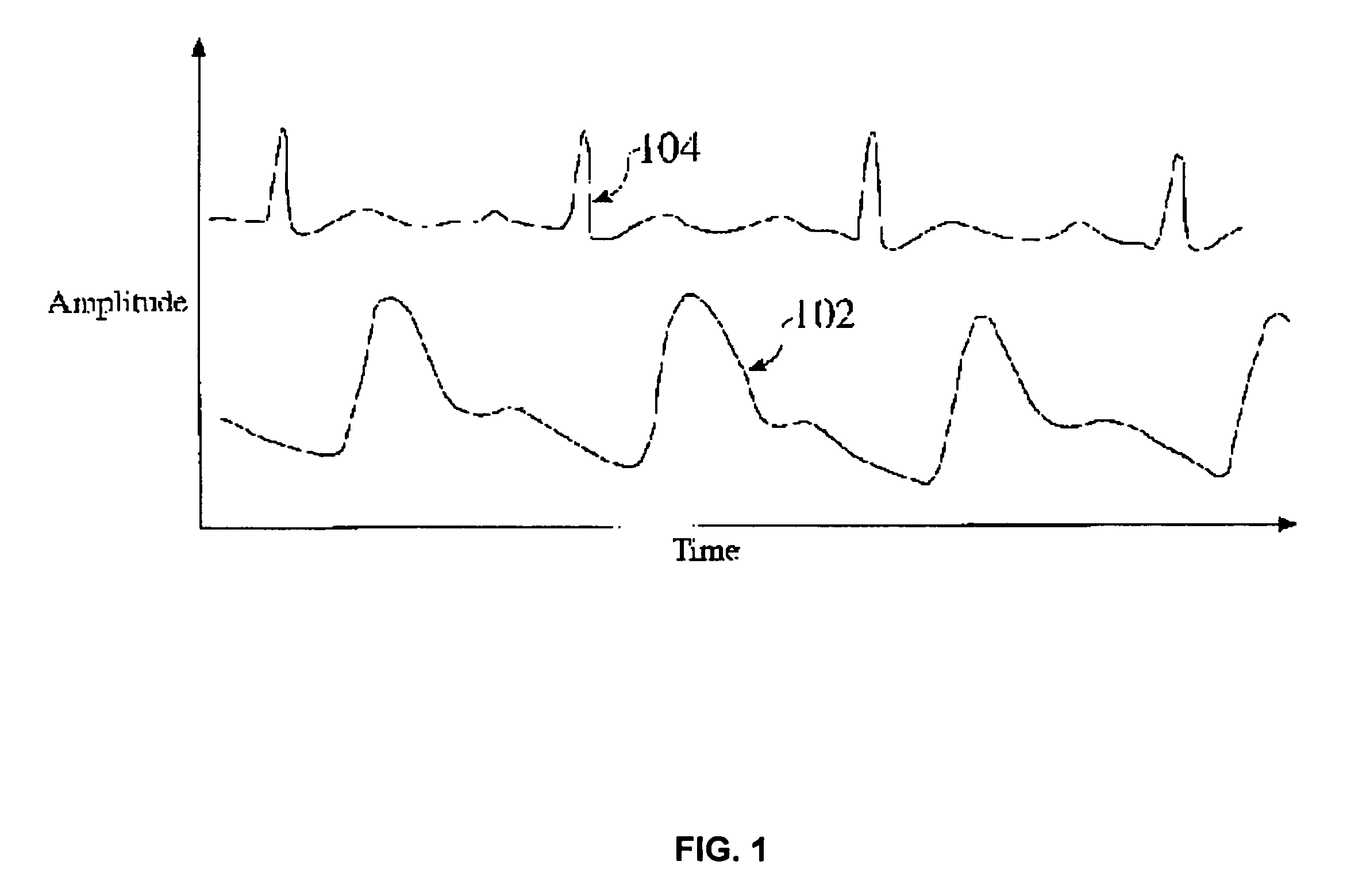
Systems and methods for detecting effort events
InactiveUS20100331715A1Reduce sensitivityAbility to detectRespiratory organ evaluationSensorsContinuous wavelet transformRespiratory effort
A method and system for detecting effort events is disclosed. Effort may be determined through feature analysis of the signal as transformed by a continuous wavelet transform, which may be compared against a reference effort measure to trigger an effort event flag that signals the onset and / or severity of an effort event. For example, a respiratory effort measure may be determined based at least in part on a wavelet transform of a photoplethysmograph (PP G) signal and features of the transformed signal. A respiratory reference effort measure may be based at least in part on past values of the respiratory effort measure, and a threshold test may be used to trigger an effort event flag, which may indicate a marked change in respiratory effort exerted by a patient.
Owner:NELLCOR PURITAN BENNETT IRELAND
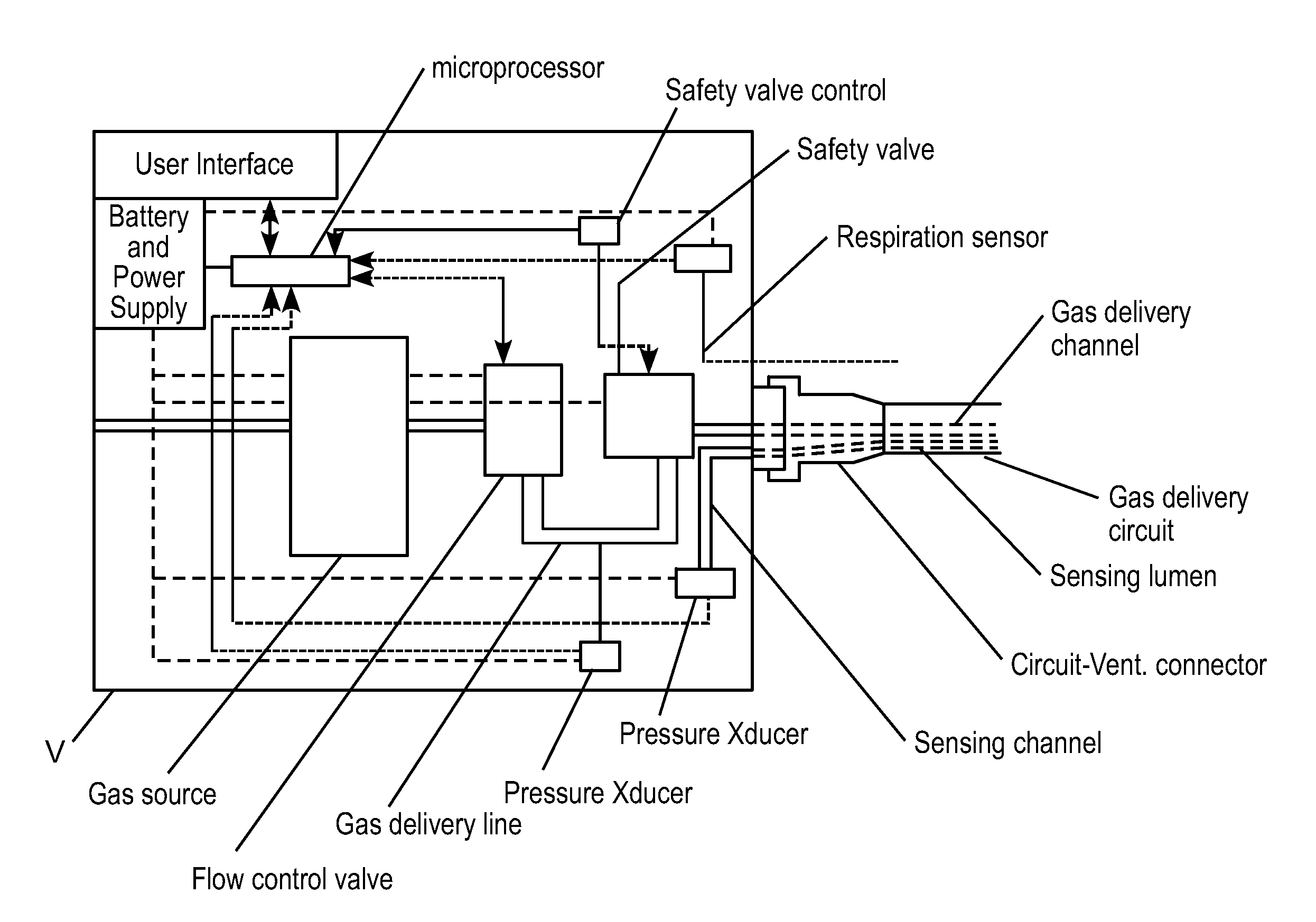
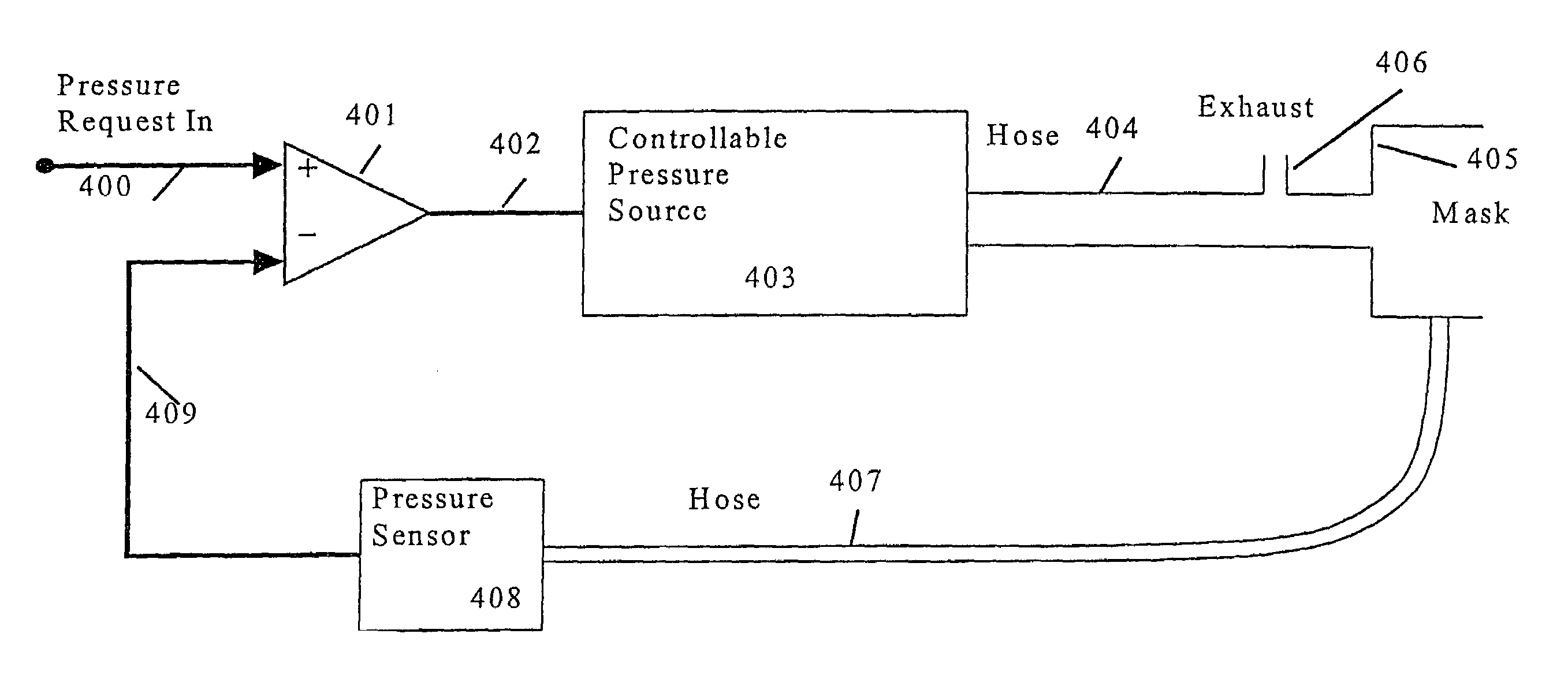
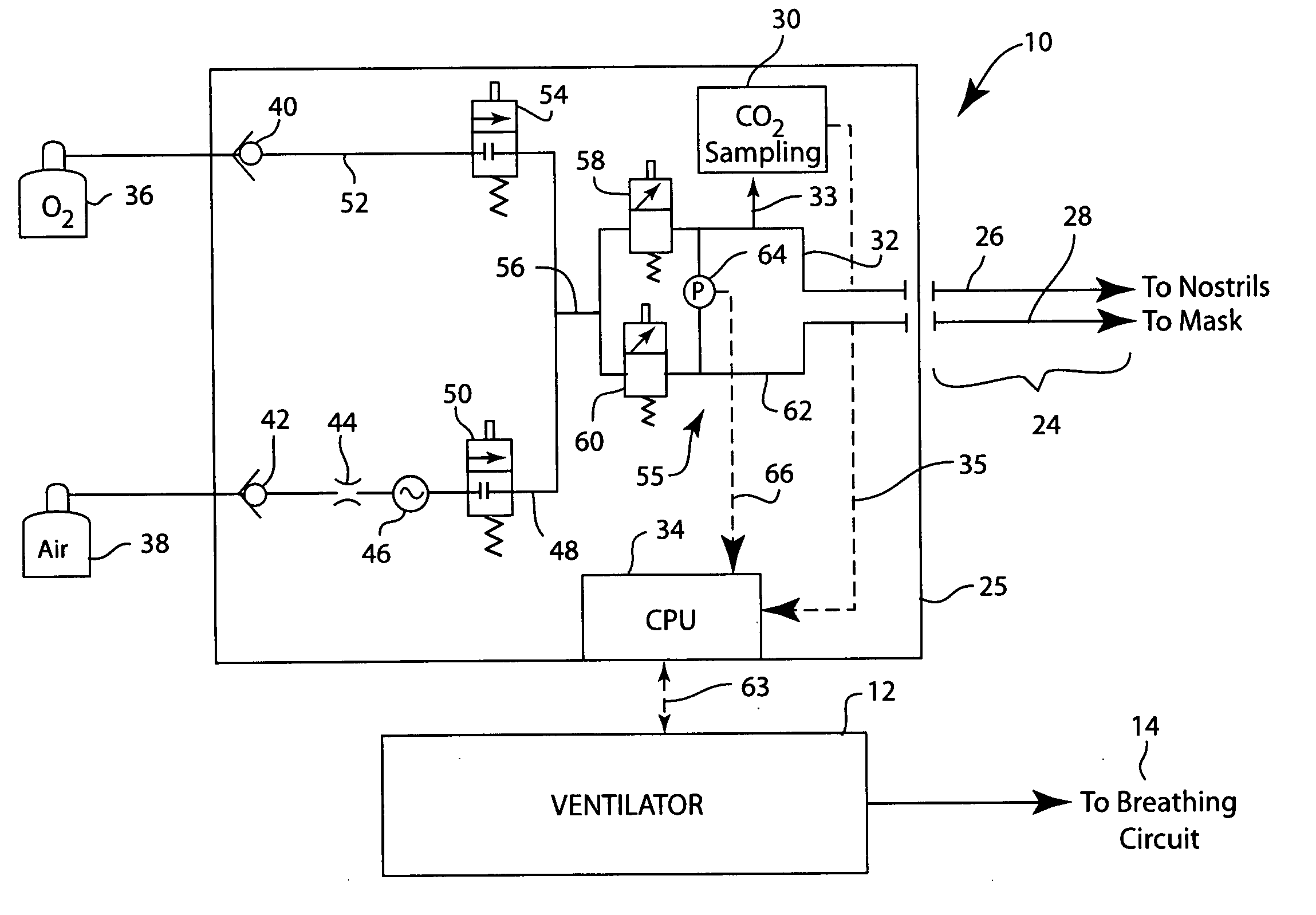
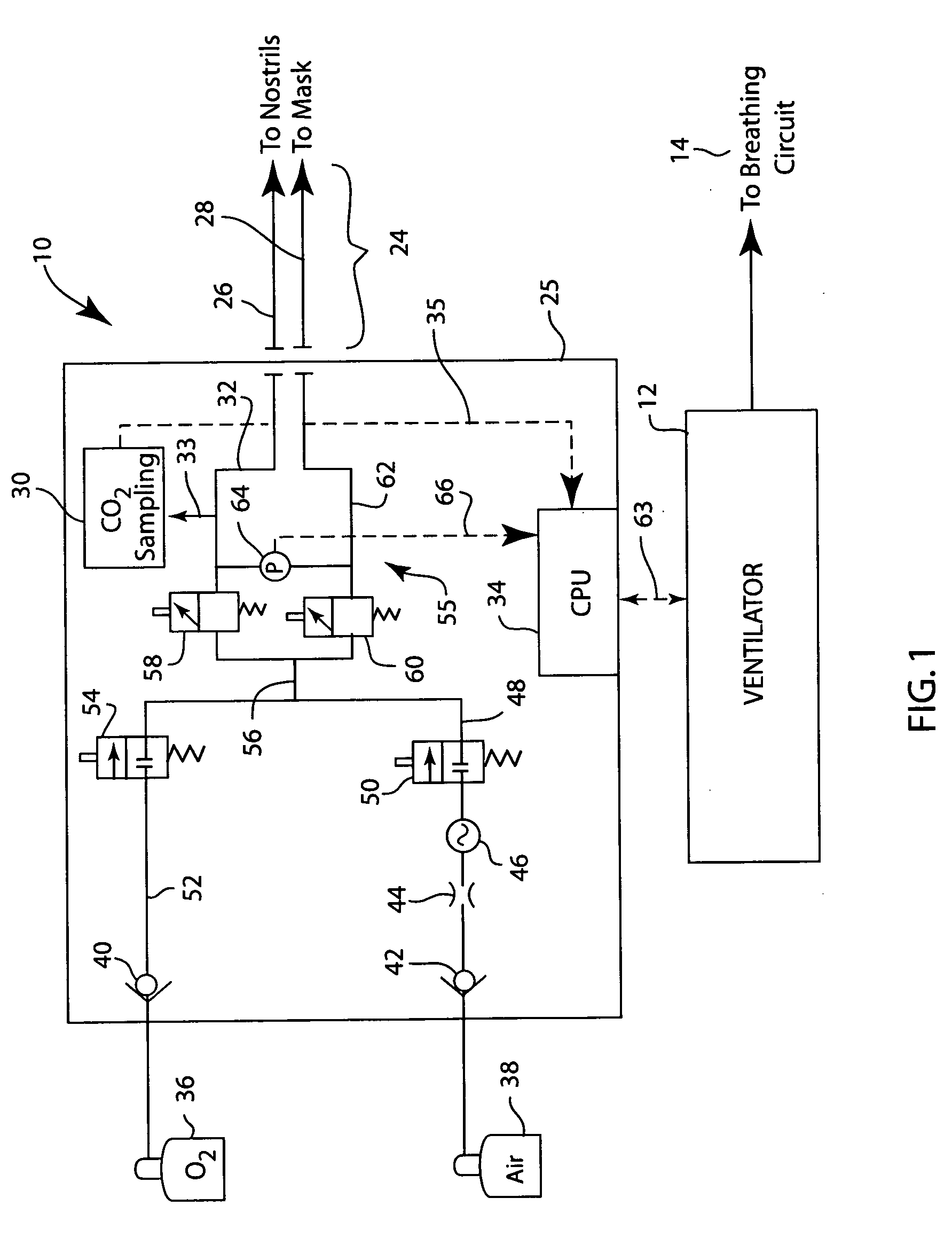
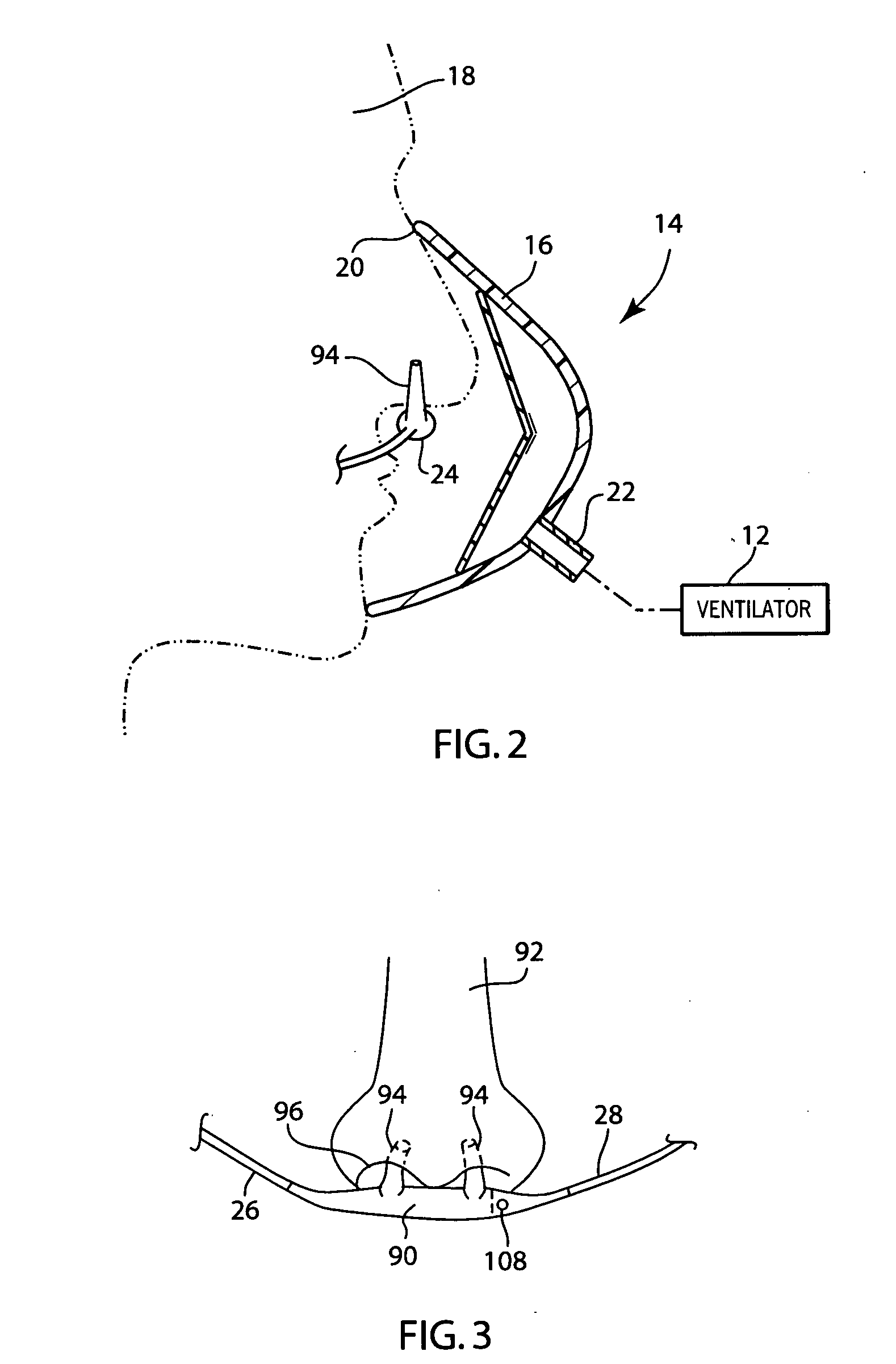
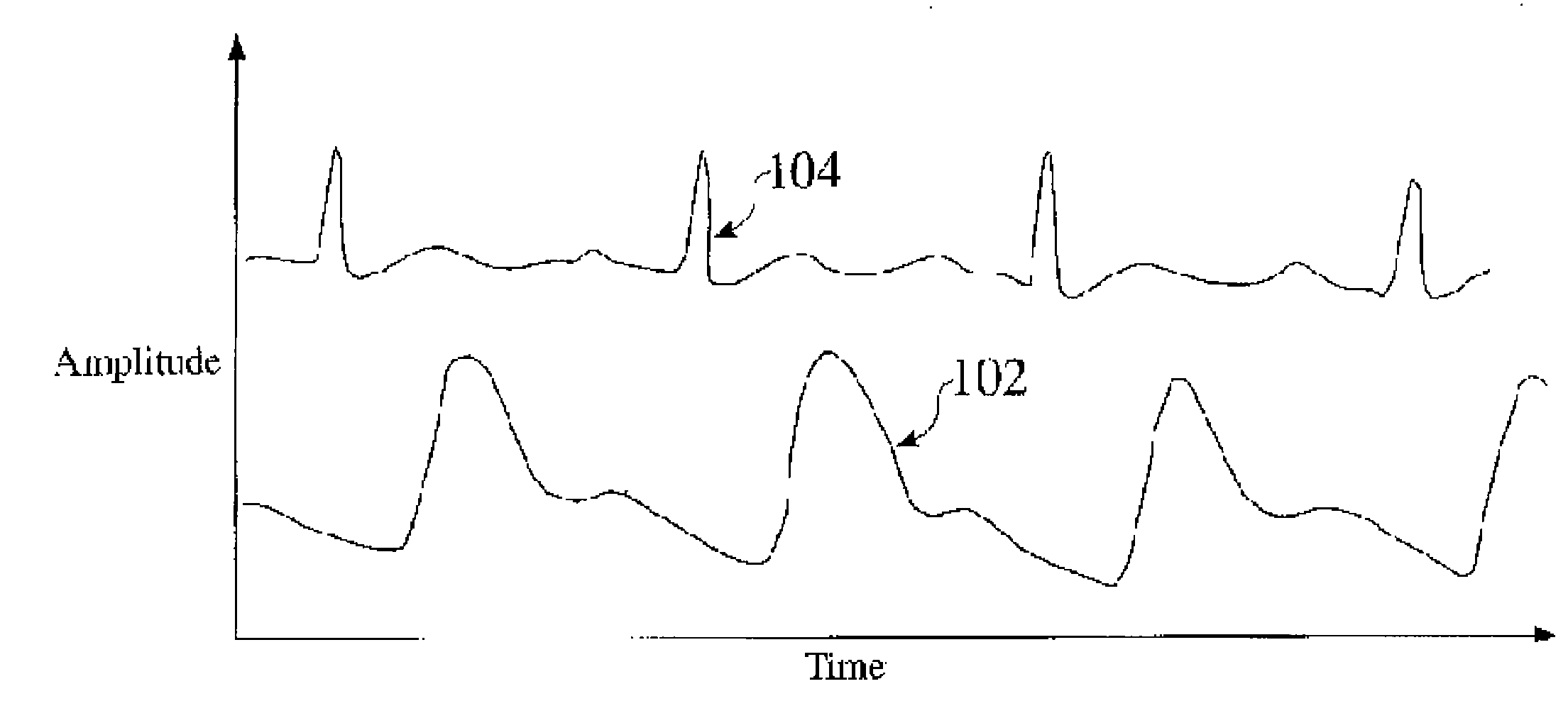
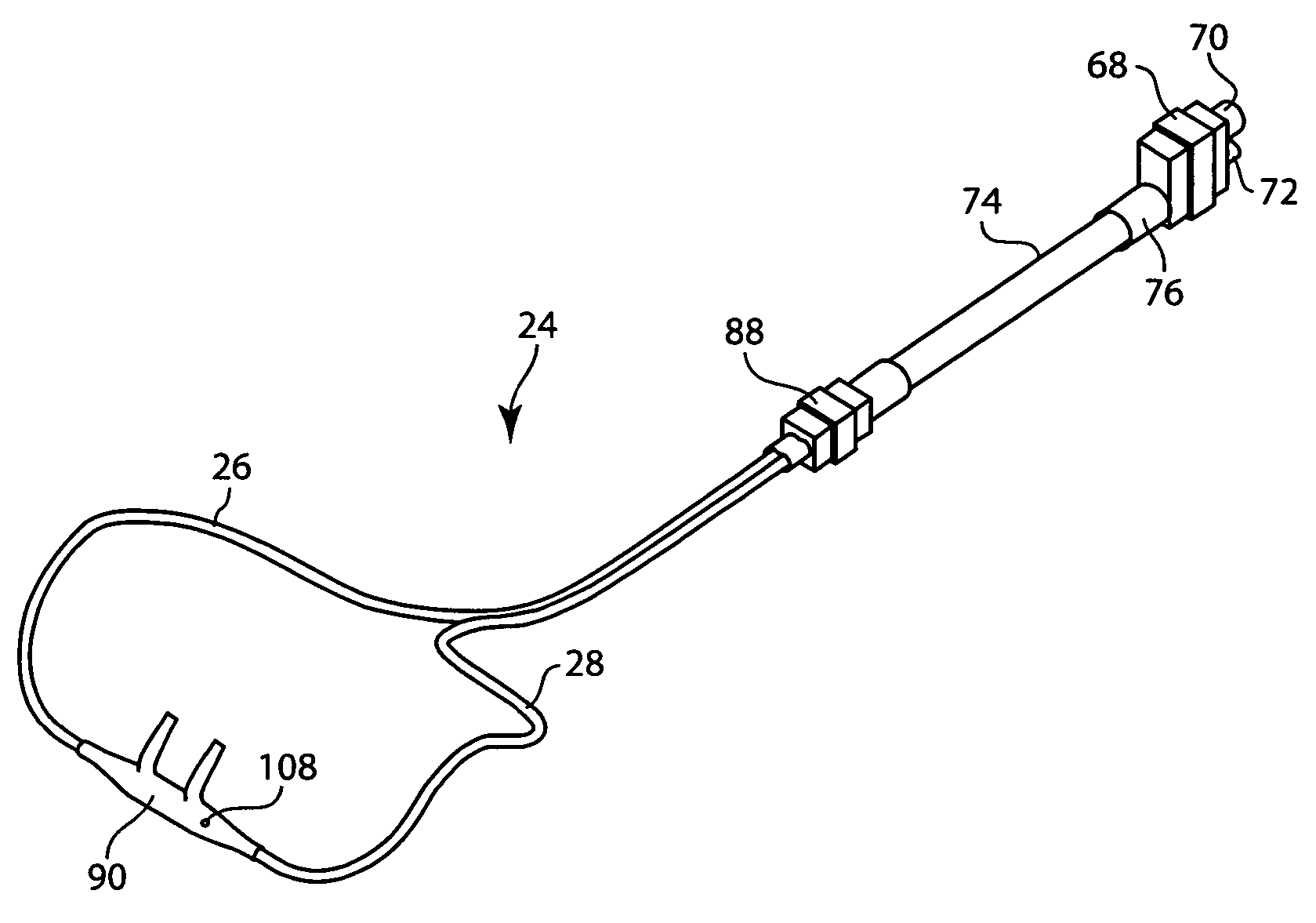
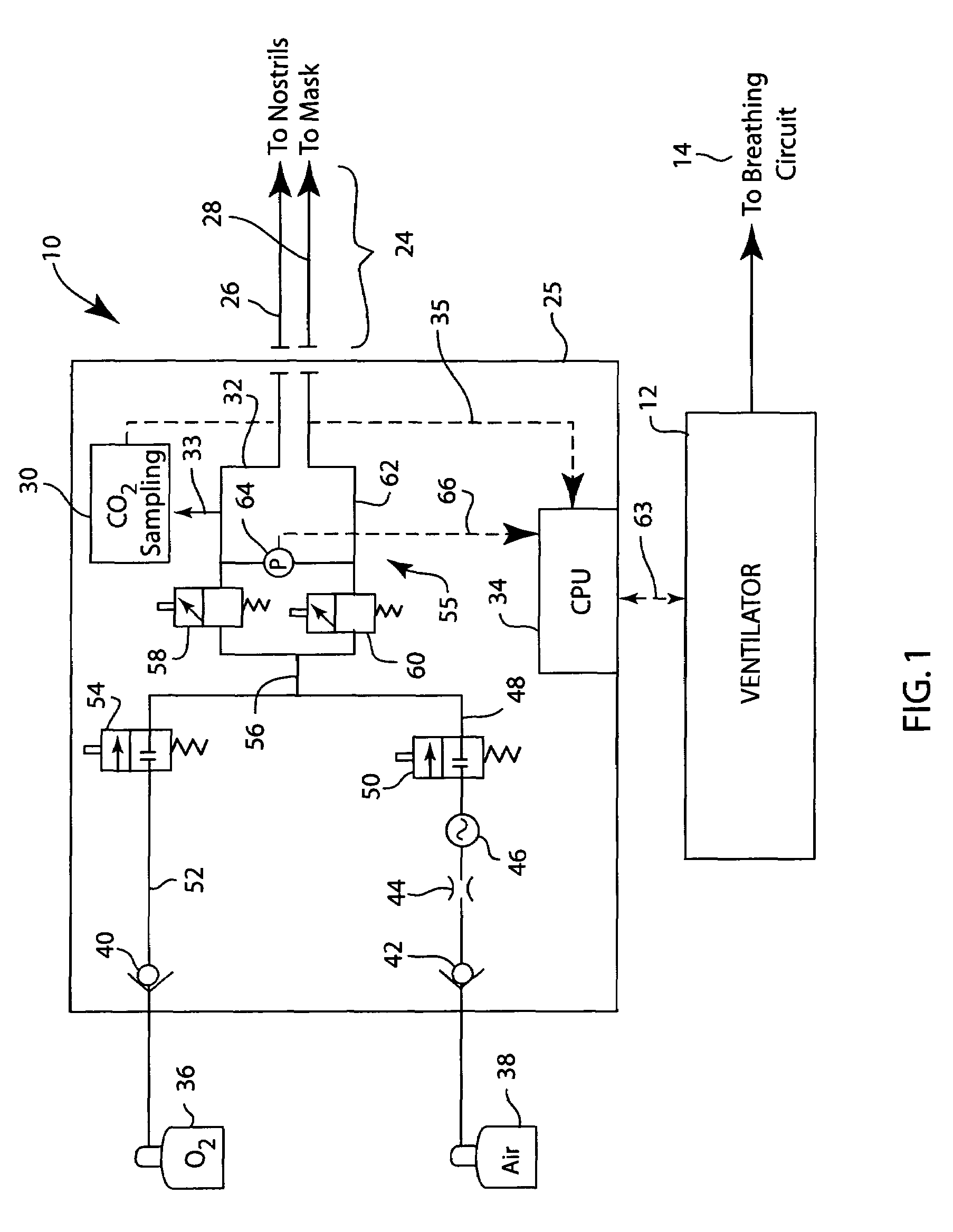
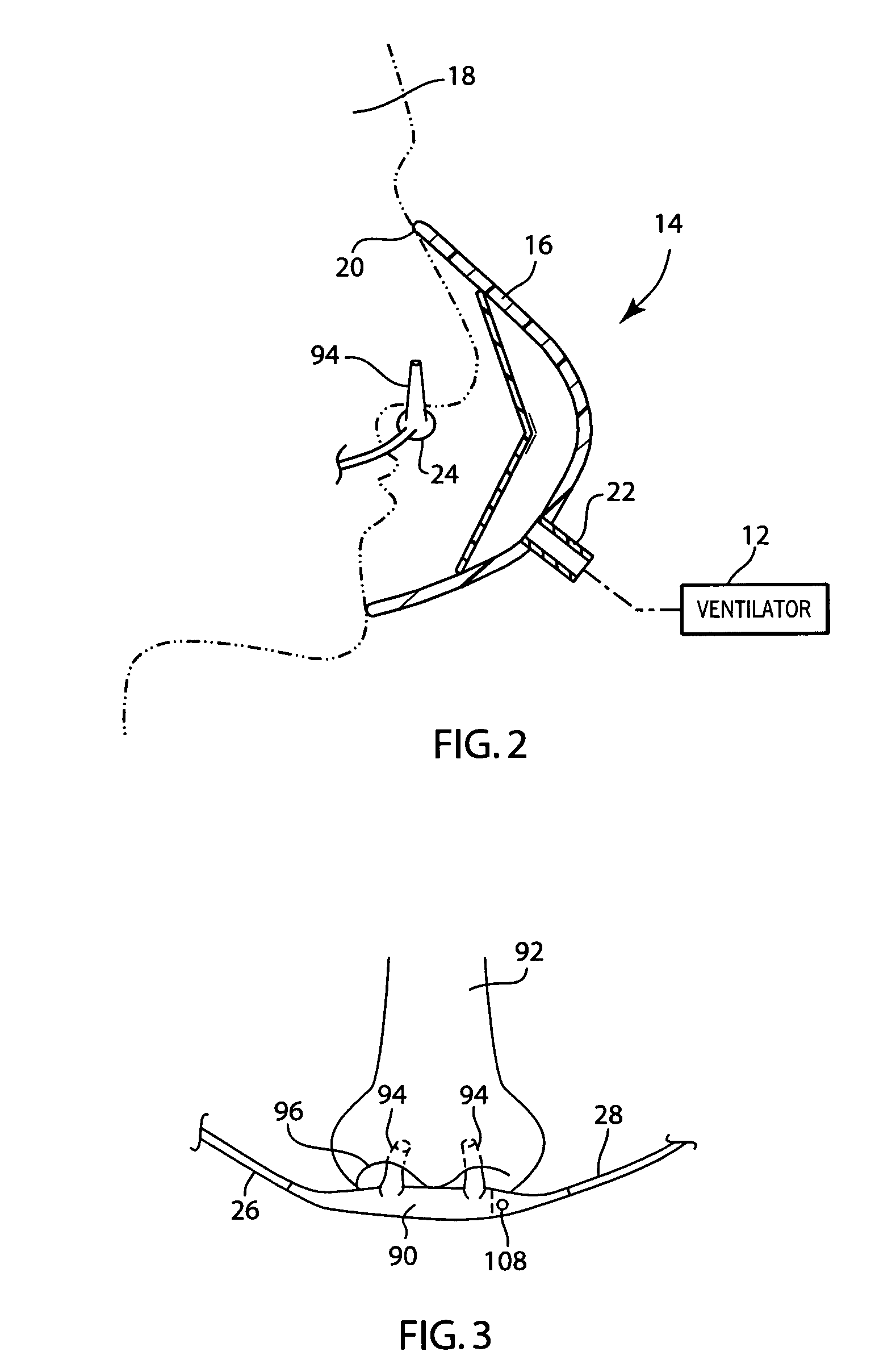
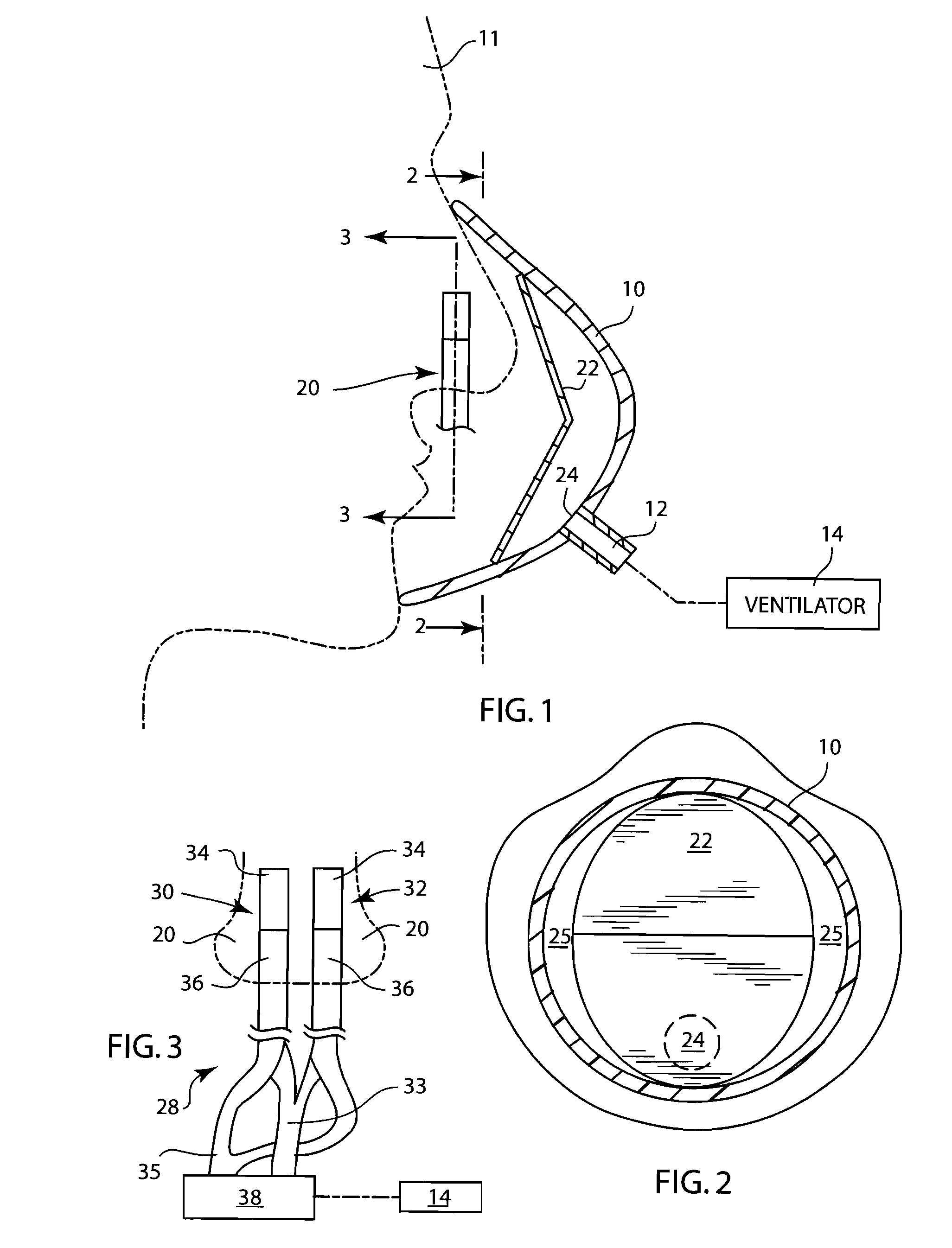
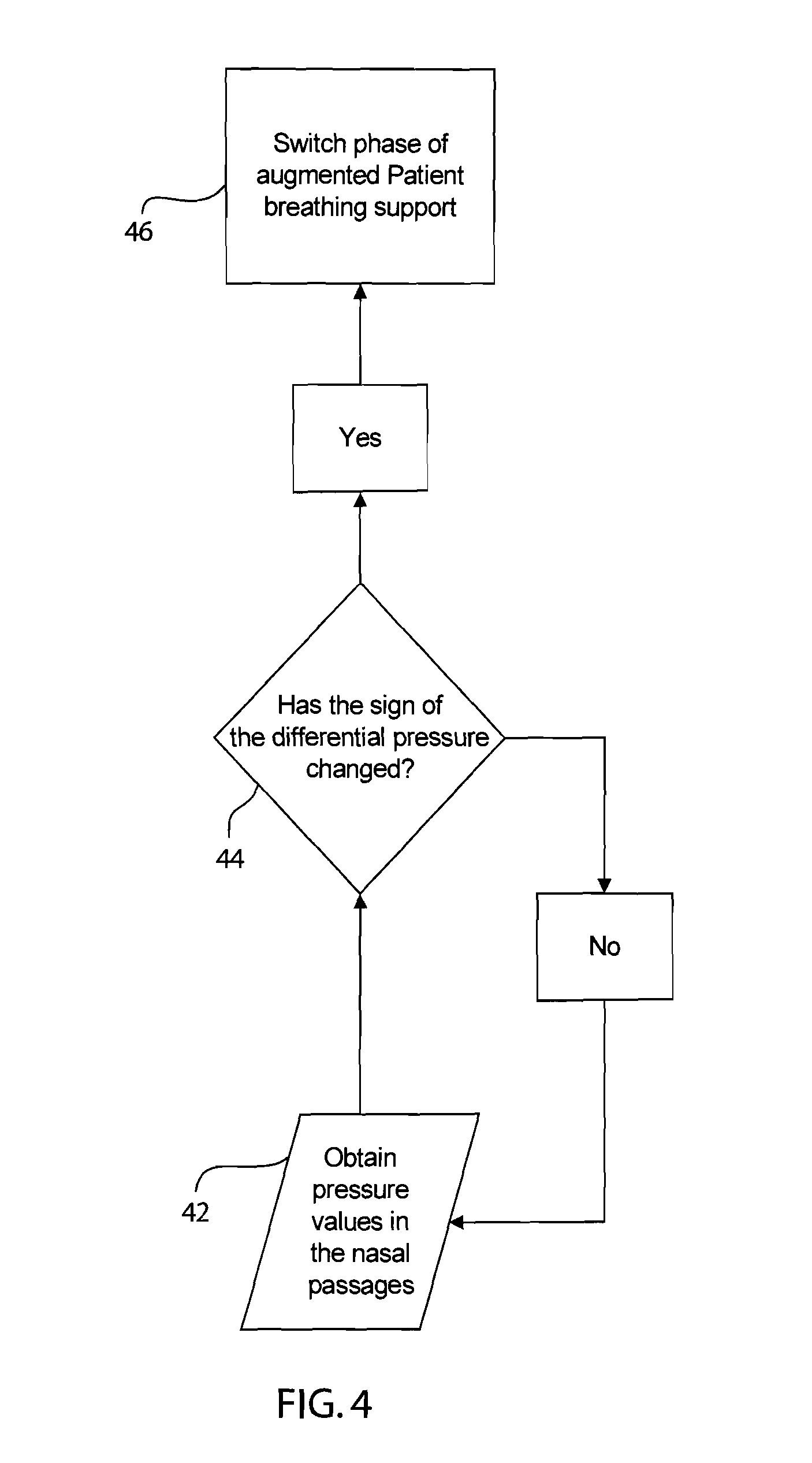
Integrated ventilator nasal trigger and gas monitoring system
ActiveUS20070144518A1Efficient combinationOperating means/releasing devices for valvesRespiratory masksNostrilDifferential pressure
An arrangement and method for detecting spontaneous respiratory effort of a patient receiving ventilatory support by a breathing circuit. The nasal cannula control system includes a nasal cannula assembly having two distinct lumens. A different pressure sensor is positioned to detect the pressure difference between each of the two lumens, thereby determining the differential pressure from within the patient's nostrils and within a breathing mask. The nasal cannula control system includes a gas sampling system such that the amount of a monitored gas discharged or exhaled by the patient can be monitored using the same nasal cannula assembly used to generate the differential pressure signal.
Owner:GENERAL ELECTRIC CO
Methods, systems and devices for monitoring respiratory disorders
Methods, systems and devices are provided for monitoring respiratory disorders based on monitored factors of a photoplethysmography (PPG) signal that is representative of peripheral blood volume. The monitored factors can be respiratory effort as well as respiratory rate and / or blood oxygen saturation level. The systems and devices may or may not be implanted in a patient.
Owner:PACESETTER INC
Integrated ventilator nasal trigger and gas monitoring system
ActiveUS7305988B2Efficient combinationOperating means/releasing devices for valvesRespiratory masksNostrilDifferential pressure
An arrangement and method for detecting spontaneous respiratory effort of a patient receiving ventilatory support by a breathing circuit. The nasal cannula control system includes a nasal cannula assembly having two distinct lumens. A different pressure sensor is positioned to detect the pressure difference between each of the two lumens, thereby determining the differential pressure from within the patient's nostrils and within a breathing mask. The nasal cannula control system includes a gas sampling system such that the amount of a monitored gas discharged or exhaled by the patient can be monitored using the same nasal cannula assembly used to generate the differential pressure signal.
Owner:GENERAL ELECTRIC CO
Patient-ventilator synchronization using dual phase sensors
InactiveUS20060102180A1Improve determinationMinimum ventilationRespiratorsOperating means/releasing devices for valvesRespiratory phasePressure amplitude
An improved ventilator which delivers ventilatory support that is synchronized with the phase of the patients respiratory efforts and guarantees a targeted minimum ventilation. Improved synchronization is achieved through an instantaneous respiratory phase determination process based upon measured respiratory airflow as well as measured respiratory effort using an effort sensor accessory, preferably a suprasternal notch sensor. The ventilator processes a respiratory airflow signal, a respiratory effort signal and their respective rates of change to determine a phase using standard fuzzy logic methods. A calculated pressure amplitude is adjusted based upon the calculated phase and a smooth pressure waveform template to deliver synchronized ventilation.
Owner:RESMED LTD
Synchrony between end of ventilator cycles and end of a patient efforts during assisted ventilation
InactiveUS20060278223A1RespiratorsOperating means/releasing devices for valvesAssisted ventilationInhalation
Automatic ongoing adjustment of the cycling-off time of ventilator inflation phase during assisted ventilation in accordance with true respiratory rate of a patient. Electrical signals are generated corresponding to the gas flow exchanged between patient and ventilator (flow) and / or to airway pressure (Paw) and the true respiratory rate of the patient (patient RR) is determined on an ongoing basis from the flow and / or Paw. The current average cycle duration of patient respiratory efforts (current patient TTOT) is estimated from patient RR. A current desirable duration of the inhalation phase (desirable TI) is calculated from the product of current patient TTOT a TI / TTOT ratio chosen to be in the physiological range, usually 0.25 to 0.50. The ventilator phase is caused to terminate in accordance with the desirable TI.
Owner:YRT
Myoelectrically activated respiratory leak sealing
InactiveUS7963283B2Reduce decreaseAdequate flowTracheal tubesOperating means/releasing devices for valvesRespiratory flowRespiratory pressure
Owner:MONTREAL UNIV DE
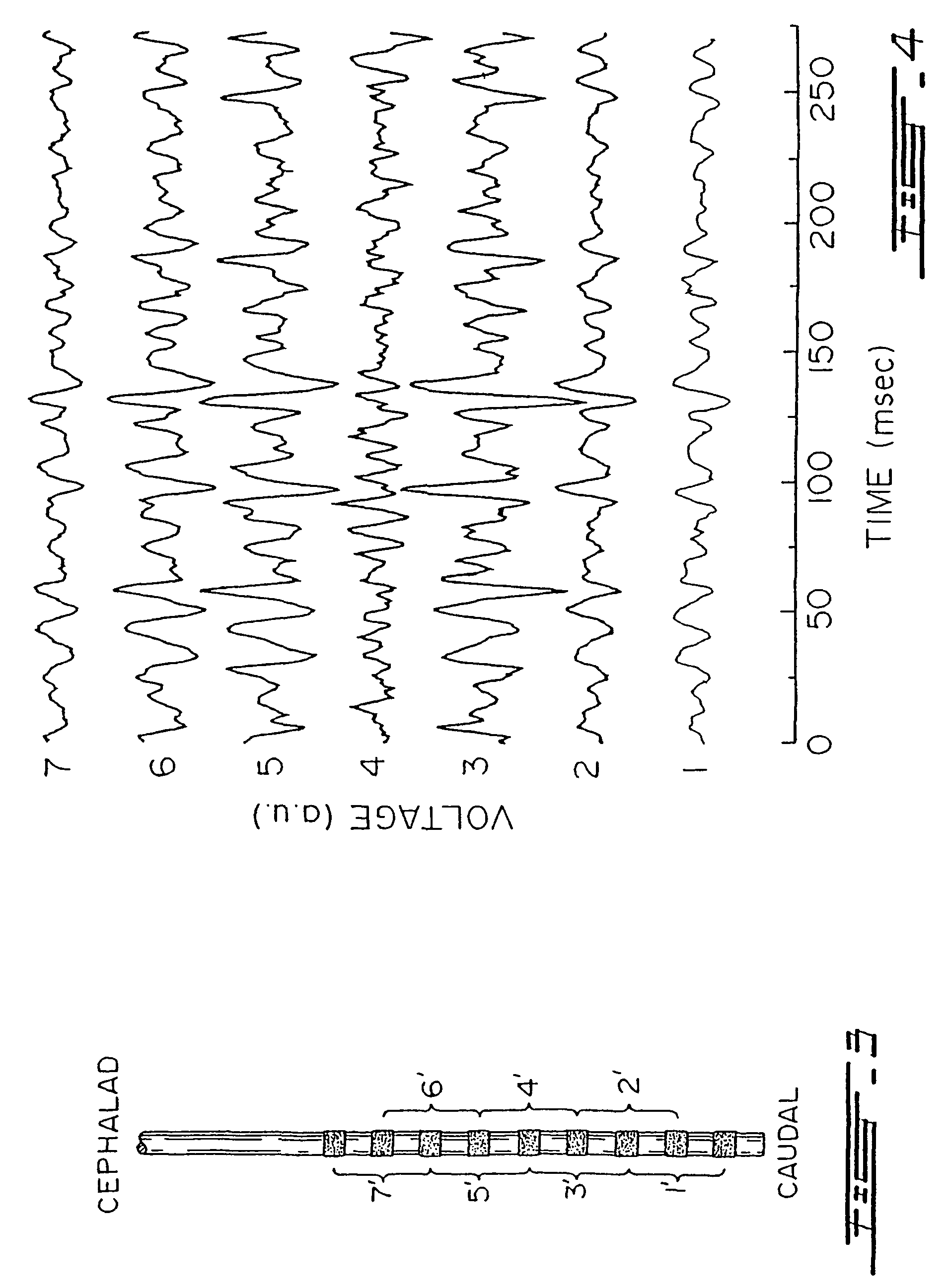
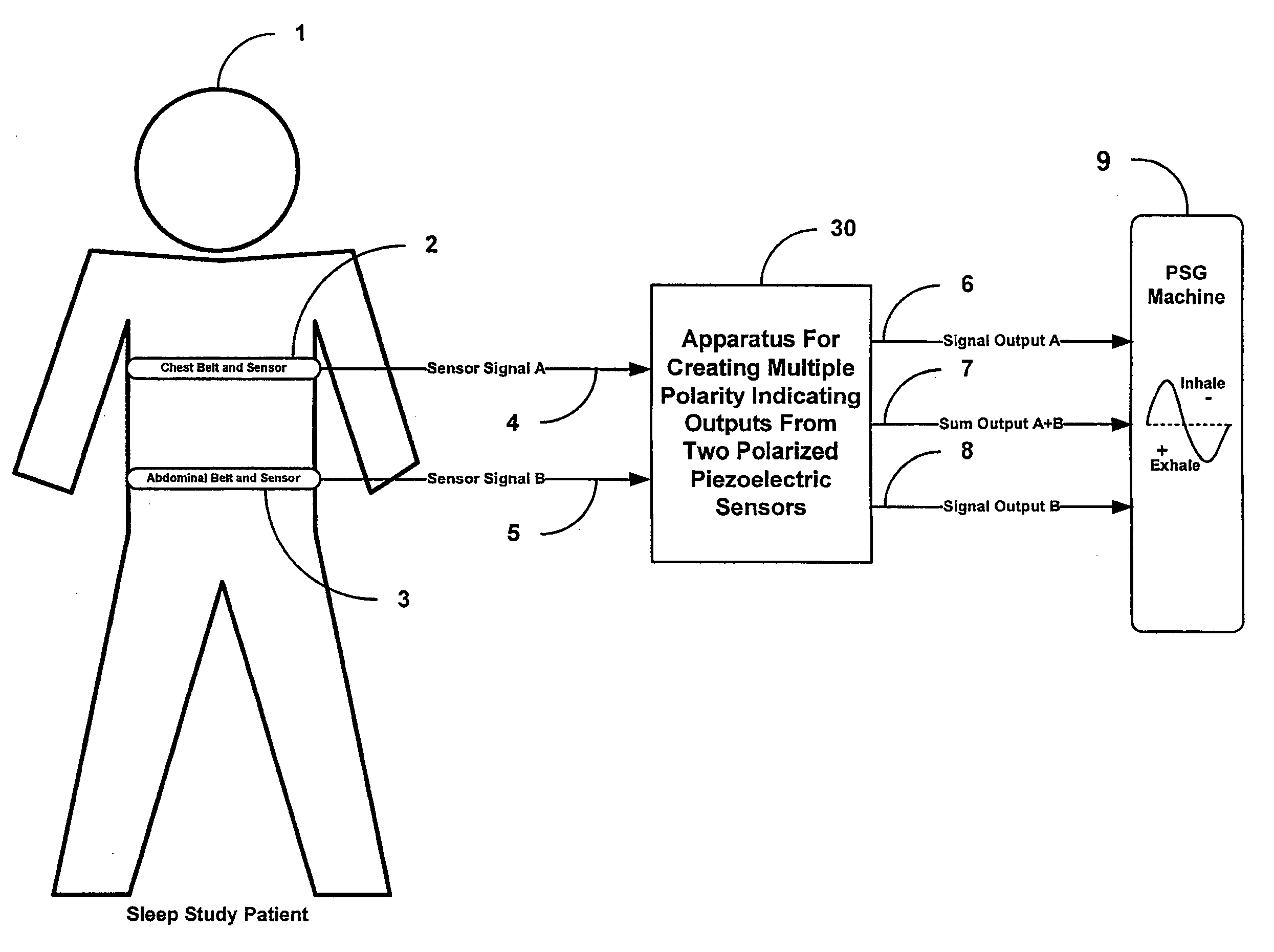
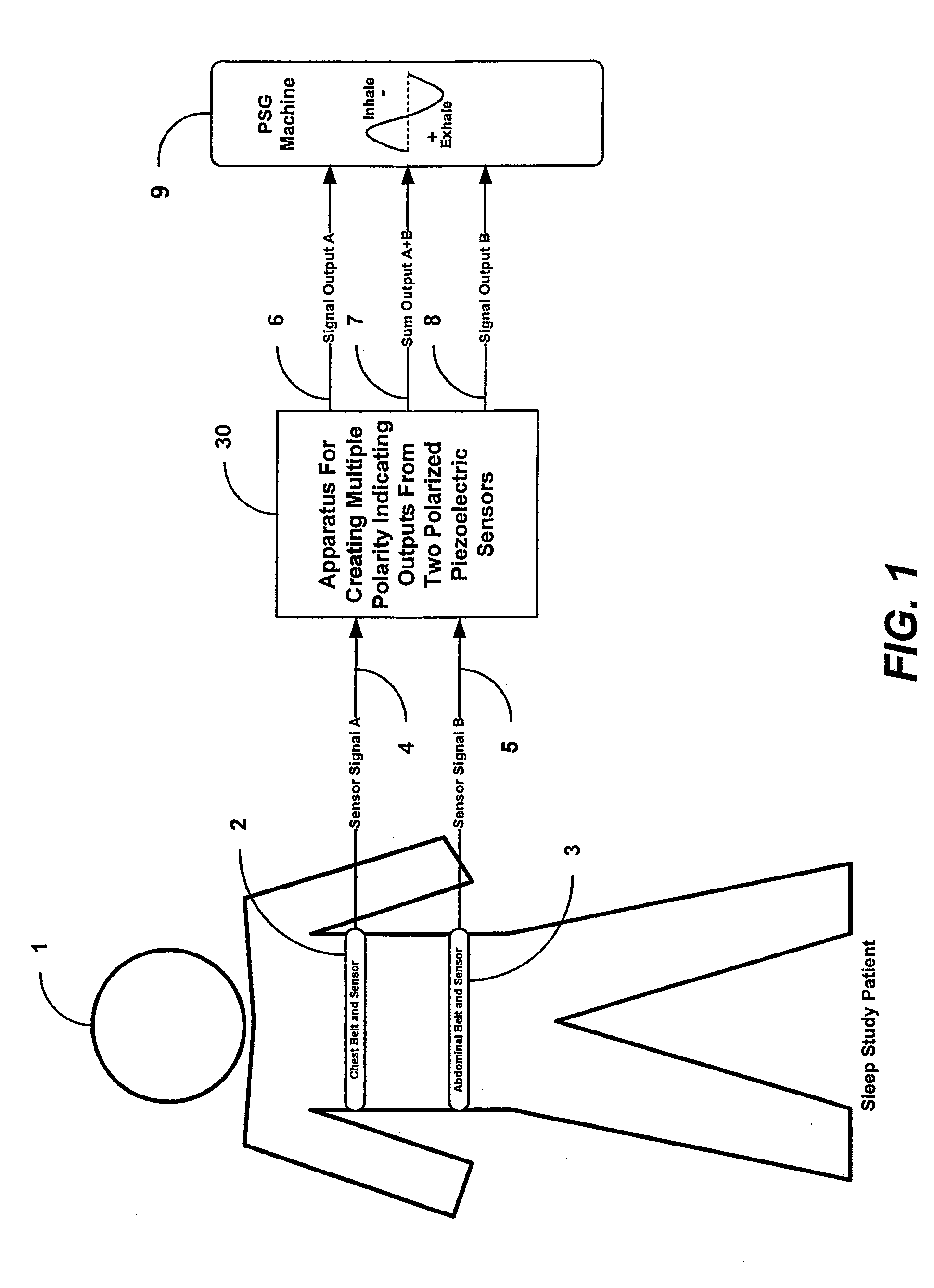
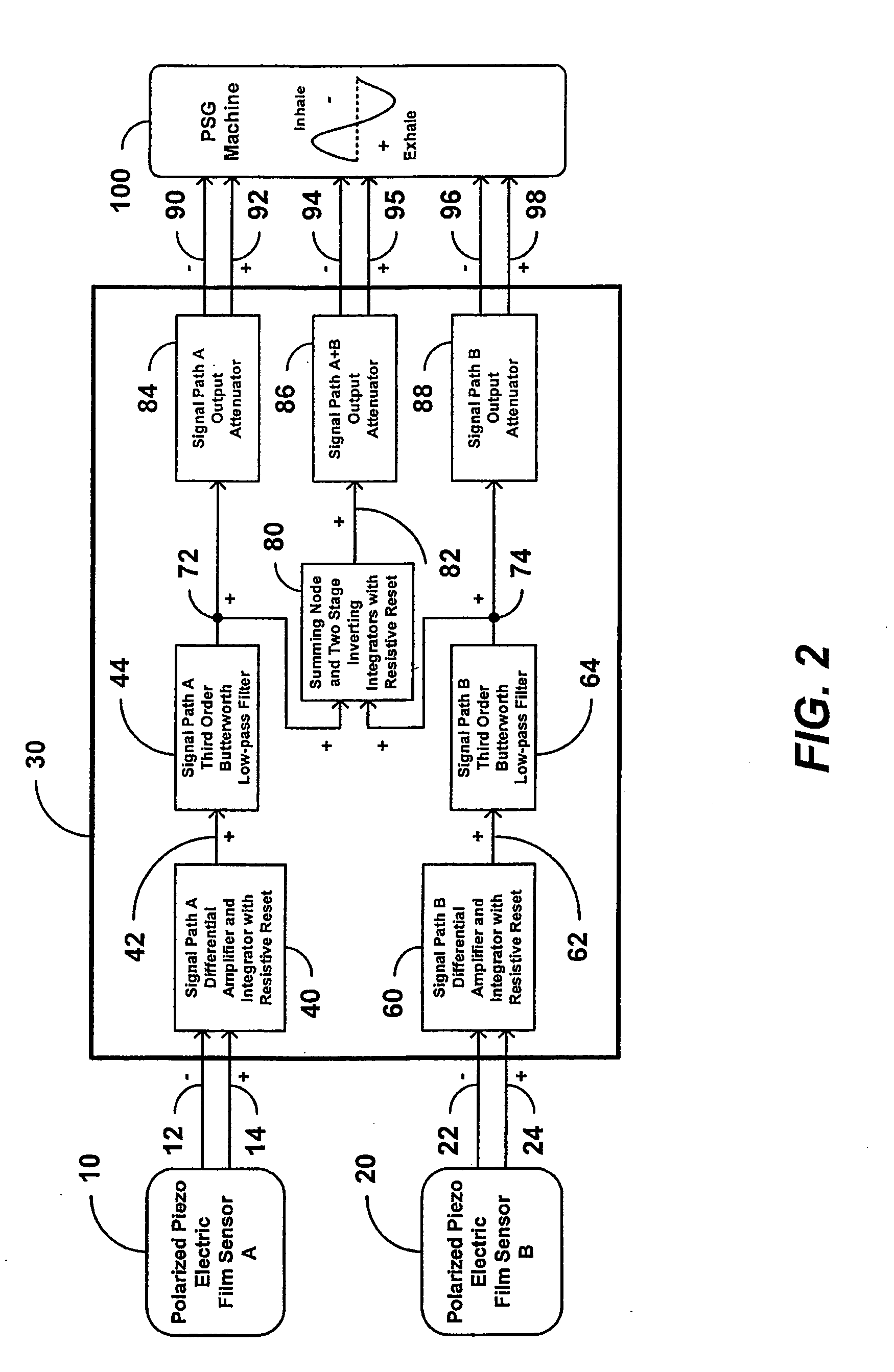
Apparatus and method for creating multiple polarity indicating outputs from two polarized piezoelectric film sensors
InactiveUS20090259135A1Reduce unwanted differential noiseReduce common mode noiseRespiratory organ evaluationSensorsElectrical resistance and conductanceElectricity
An apparatus or method can be configured to receive first information indicative of respiratory effort of a subject from a first piezoelectric film sensor and second information indicative of respiratory effort of the subject from a second piezoelectric film sensor, and to process the received first and second information to produce an electronic signal output indicative of respiratory effort of the subject, the processing including averaging the received first information using a first differential amplifier and signal integrator with resistive reset to reduce differential noise and to attenuate common-mode noise, and averaging the received second information using a second differential amplifier and signal integrator with resistive reset to reduce differential noise and to attenuate common-mode noise.
Owner:DYMEDIX
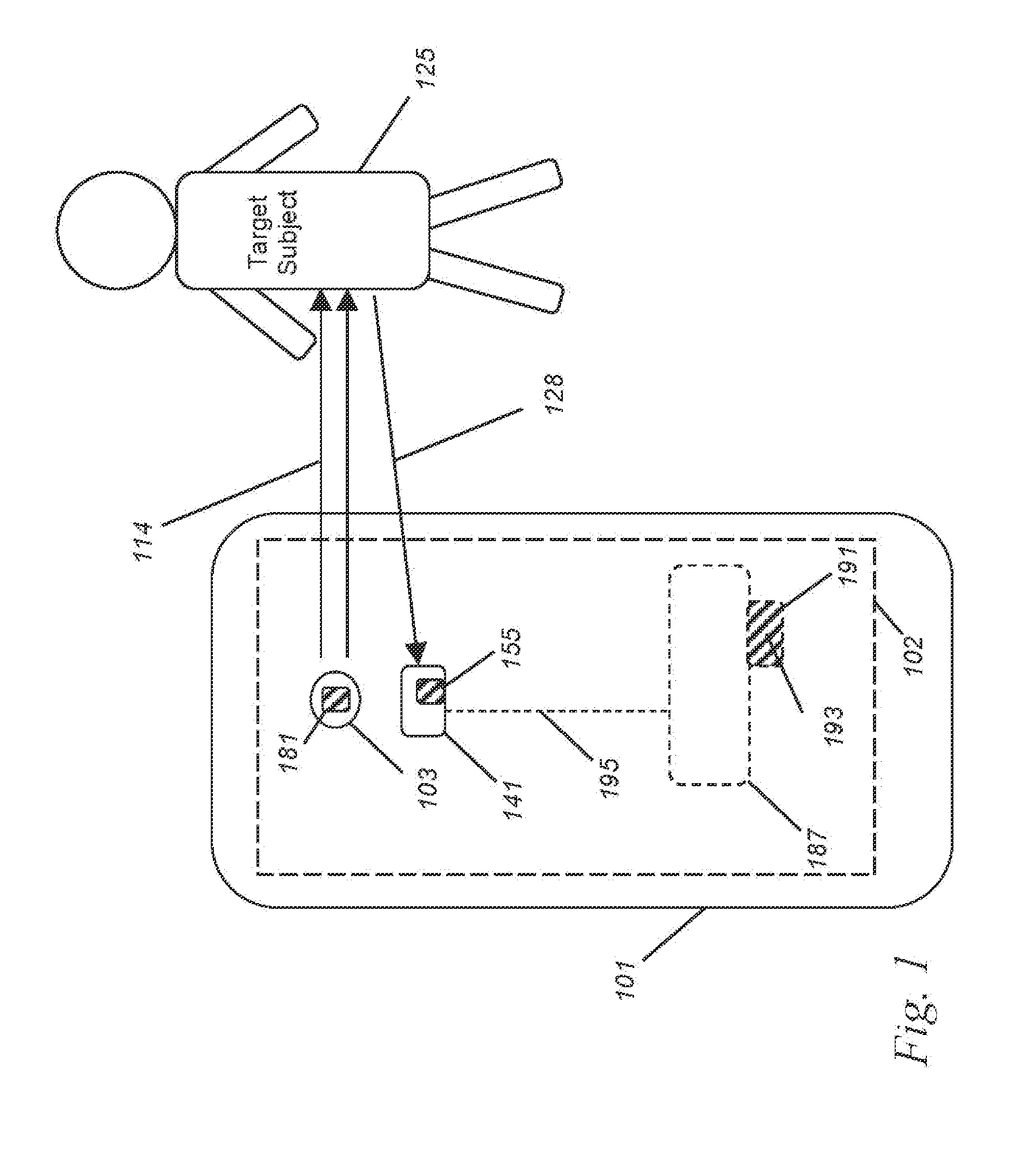
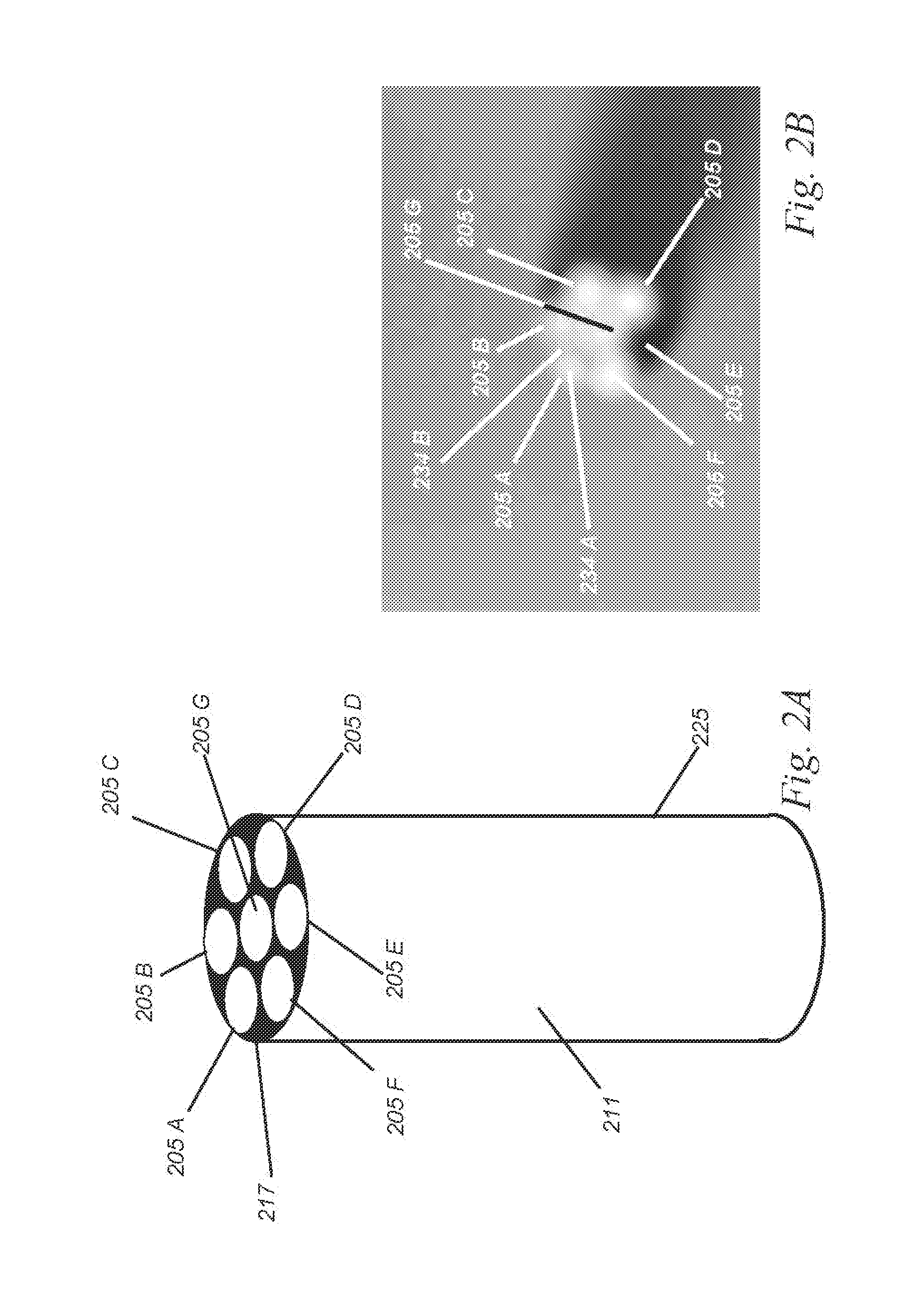
Calorie Monitoring Sensor And Method For Cell Phones, Smart Watches, Occupancy Sensors, And Wearables
InactiveUS20150148632A1Implementation more simply and inexpensivelyDiagnostics using lightDiagnostics using spectroscopyFluorescenceLarge Calorie
An improved sensor (102) for calorie monitoring in mobile devices, wearables, security, illumination, photography, and other devices and systems uses an optional phosphor-coated broadband white LED (103) to produce broadband light (114), which is then transmitted along with any ambient light to target (125) such as the ear, face, or wrist of a living subject. Some of the scattered light returning from the target to detector (141) is passed through narrowband spectral filter set (155) to produce multiple detector regions, each sensitive to a different narrowband wavelength range, and the detected light is spectrally analyzed to determine a measure of calories, such as calories expended, calories ingested, calorie balance, or rate of calories expended, in part based on a noninvasive measure of respiration, such as respiratory rate, respiratory effort, respiratory depth, or respiratory variability. In one example, variations in concentration in components of the bloodstream over time, such as hemoglobin and water in the arteries, are determined based on the detected light, and the measure of respiration is then determined based on the variations in concentration over time. In the absence of the LED light, ambient light may be sufficient illumination for analysis. The same sensor can provide identifying features of type or status of a tissue target, such as heart rate or heart rate variability, hydration status, sleep state, or even occupancy counting. Calorie monitoring systems incorporating the sensor as well as methods are also disclosed.
Owner:J FITNESS LLC
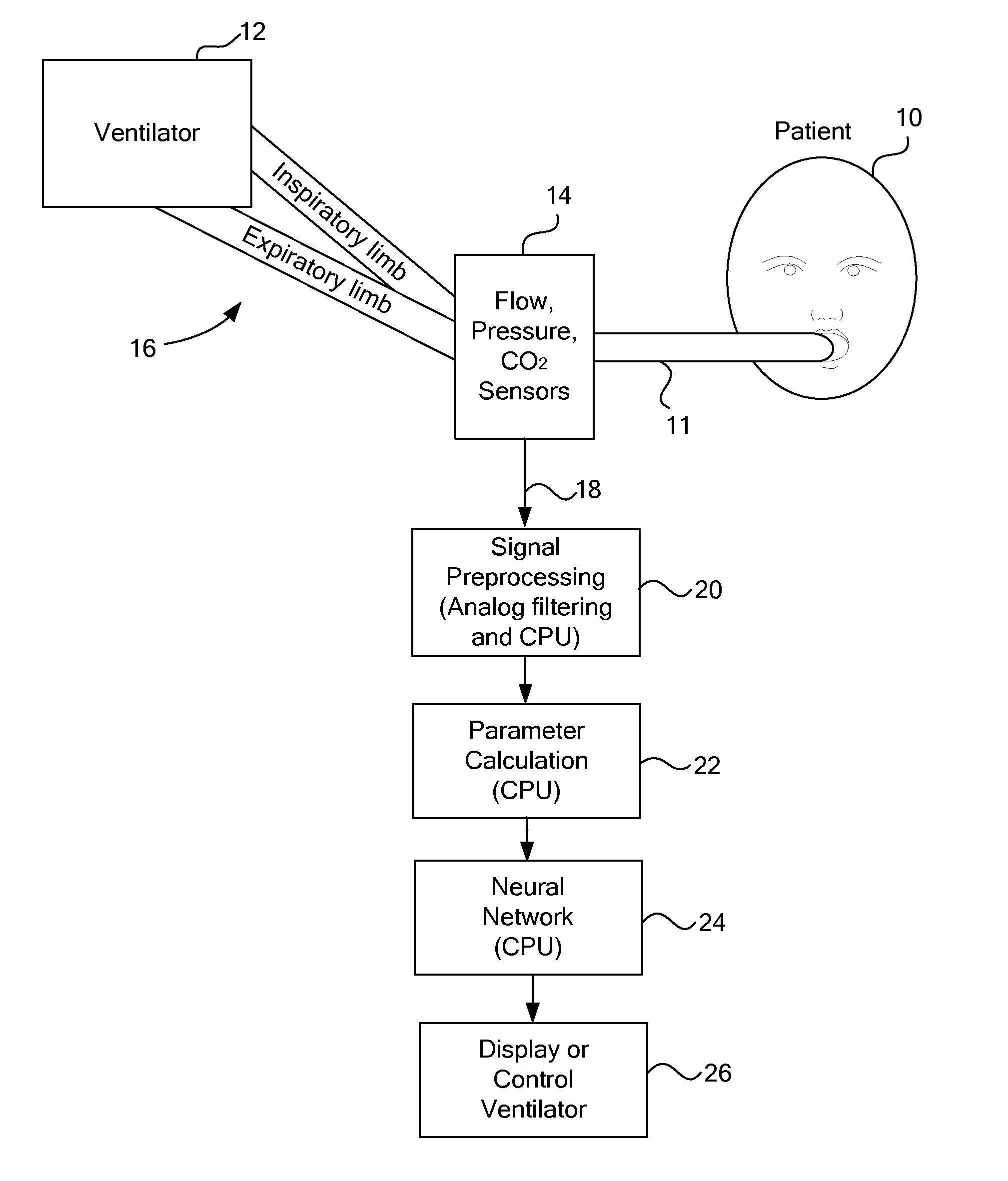
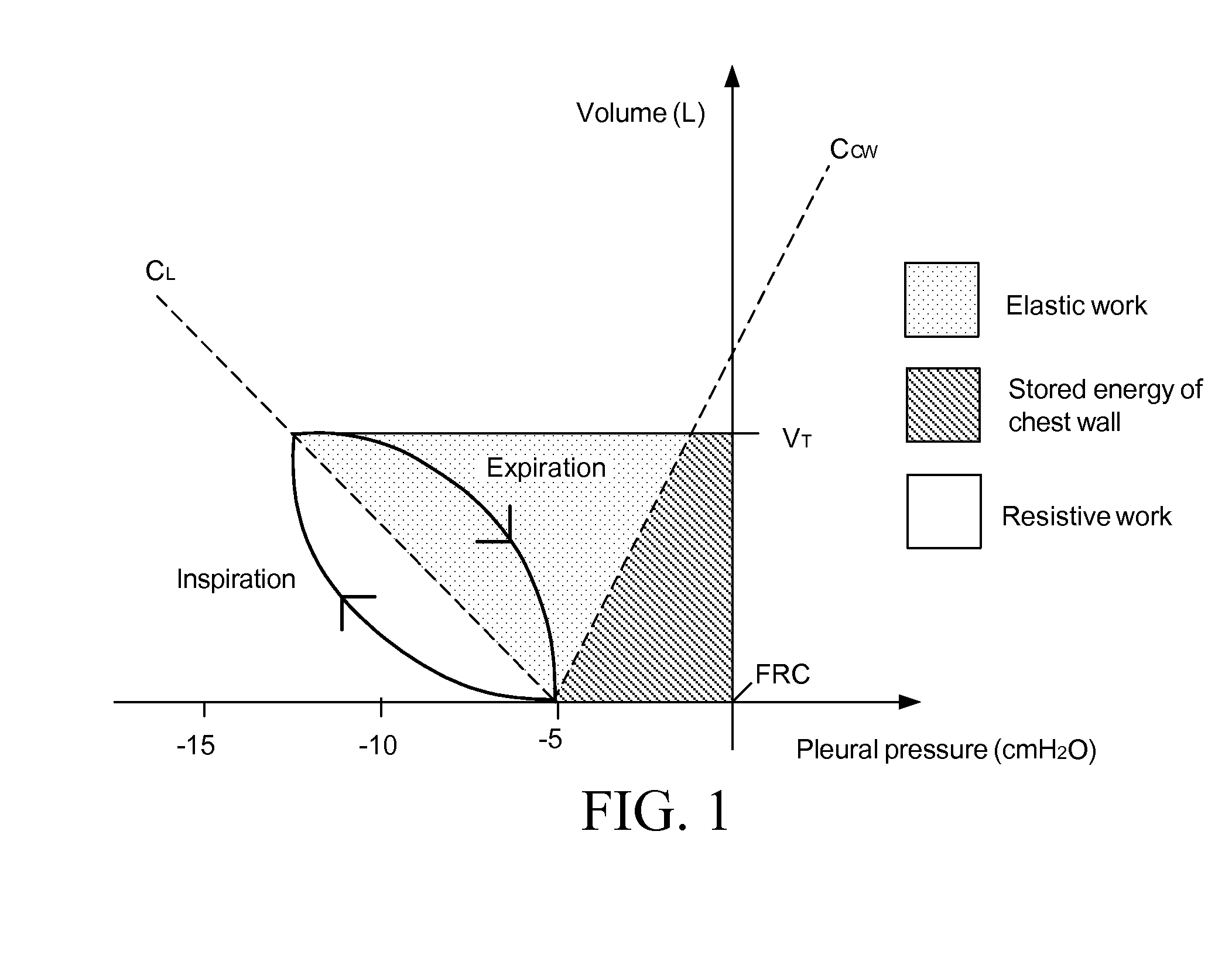
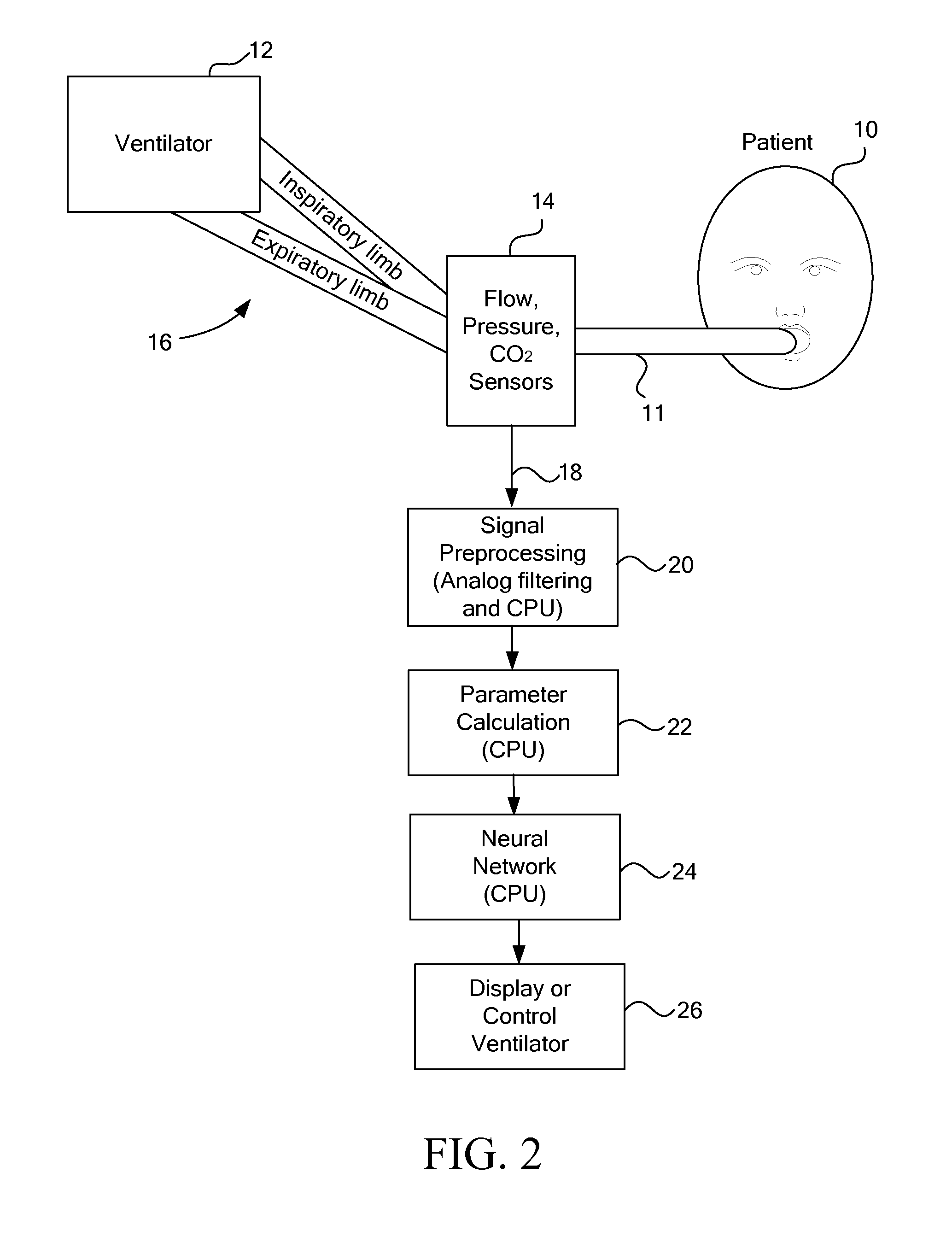
Method and Apparatus for Predicting Work of Breathing
ActiveUS20120215081A1Avoids respiratory muscle fatigue respiratory muscleAvoids respiratory muscle respiratory muscle deconditioningRespiratorsMedical devicesPhysical medicine and rehabilitationMathematical model
A method of creating a noninvasive predictor of both physiologic and imposed patient effort of breathing from airway pressure and flow sensors attached to the patient using an adaptive mathematical model. The patient effort is commonly measured via work of breathing, power of breathing, or pressure-time product of esophageal pressure and is important for properly adjusting ventilatory support for spontaneously breathing patients. The method of calculating this noninvasive predictor is based on linear or non-linear calculations using multiple parameters derived from the above-mentioned sensors.
Owner:UNIV OF FLORIDA RES FOUNDATION INC
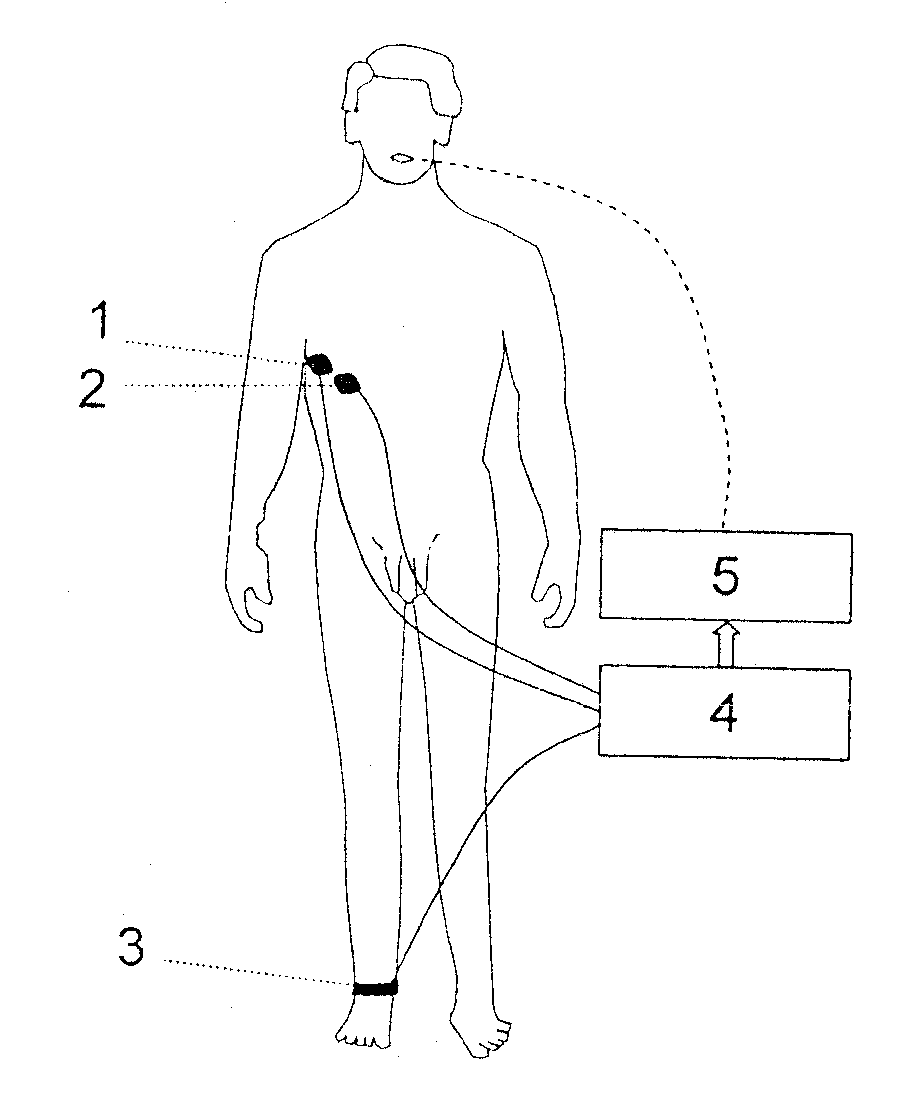
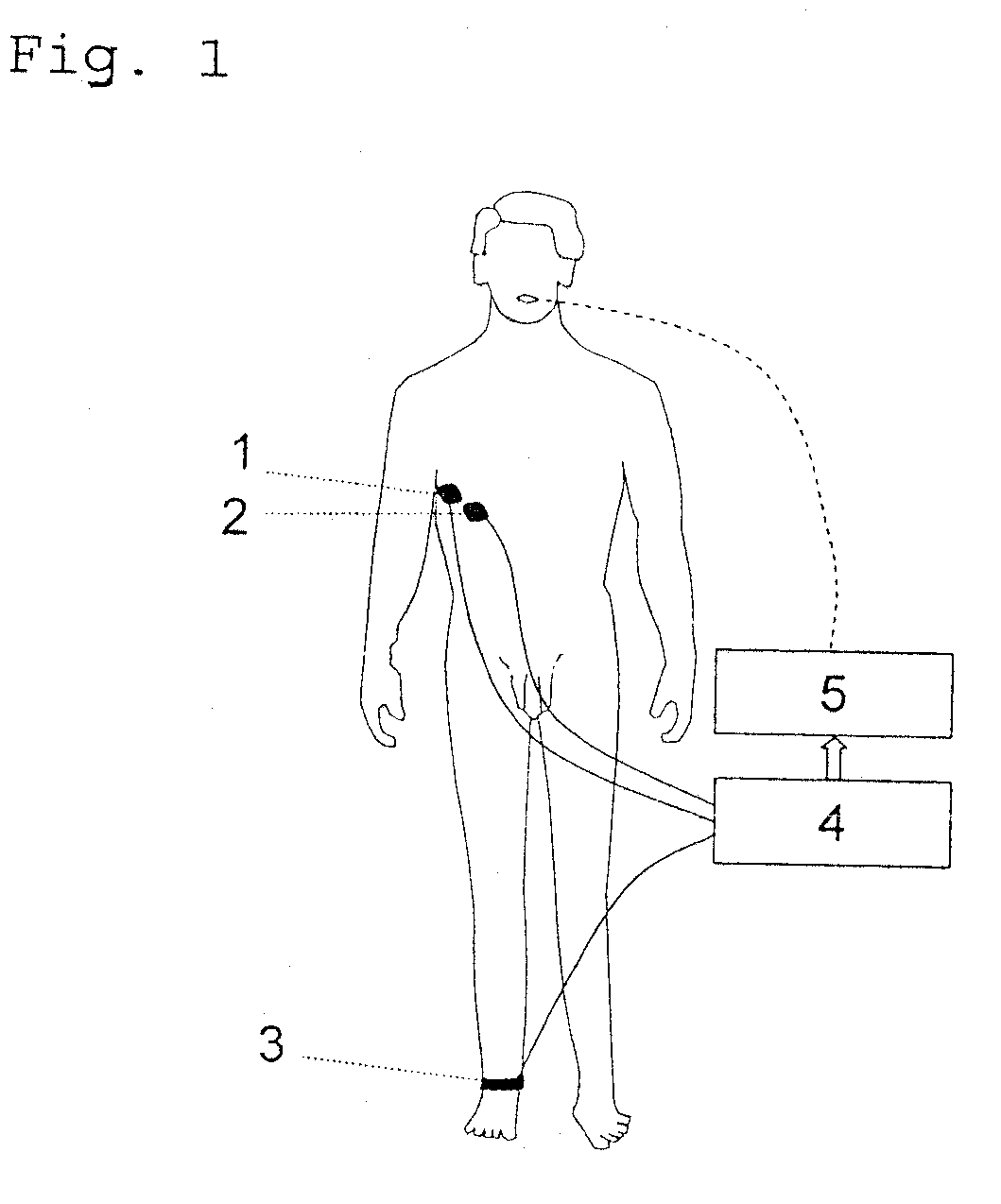
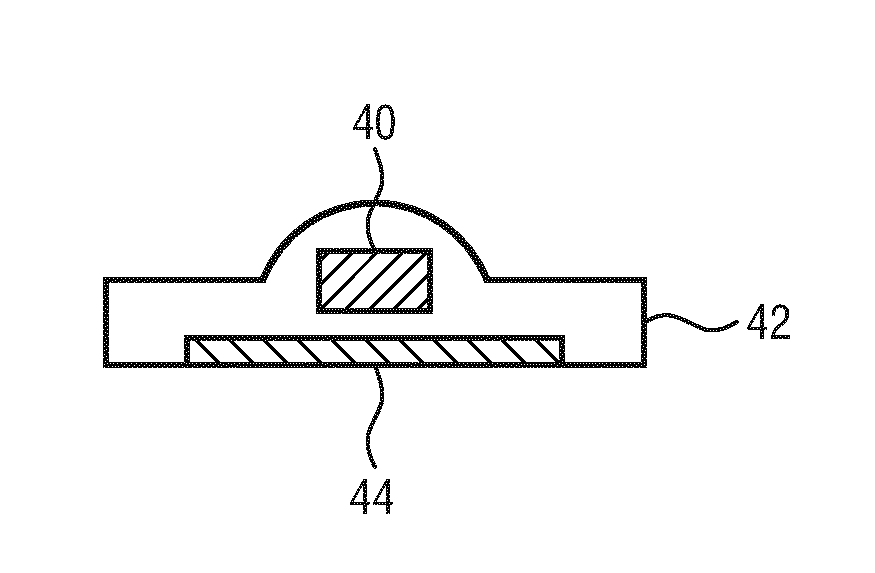
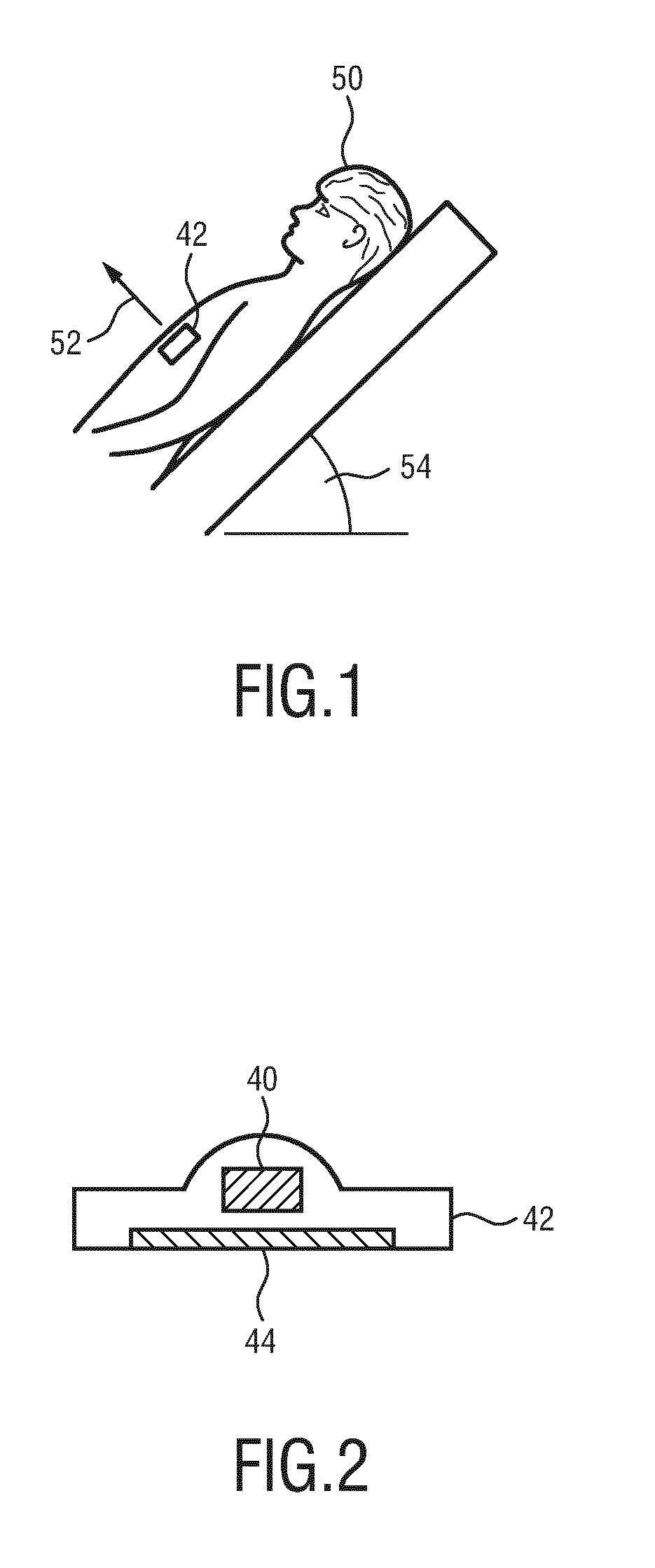
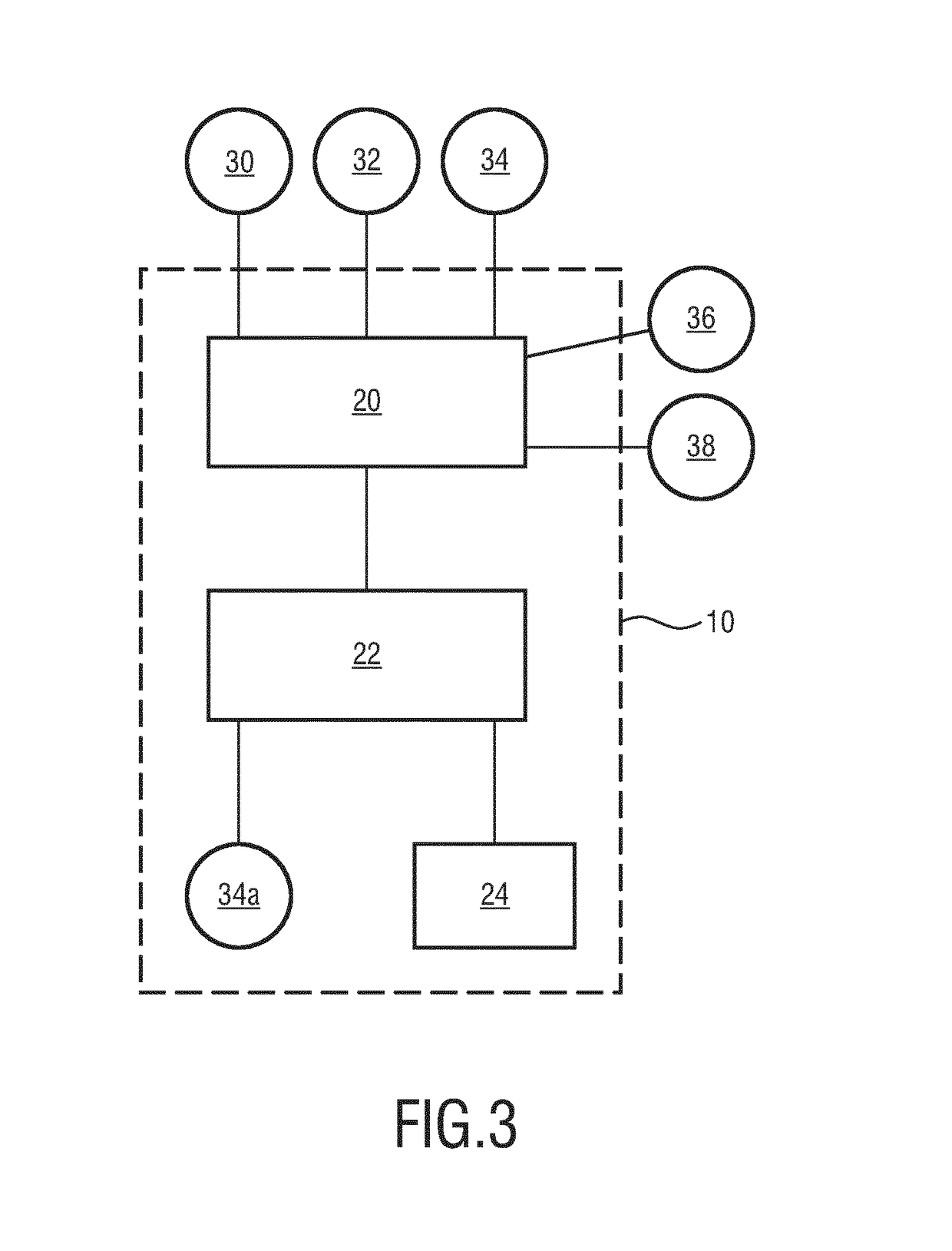
Device and method for determining and/or monitoring the respiratory effort of a subject
PendingUS20170360329A1Precise positioningEasy to operateElectromyographyInertial sensorsRespiratory effortPostural orientation
A device and method for determining and / or monitoring the respiratory effort of a subject are presented. The device comprises a receiving unit for receiving a posture signal of the subject, a breathing signal of the subject, and an electromyography signal of the subject; and a processing unit for determining an electromyography signal based on the posture signal and the breathing signal and for deriving the respiratory effort based on the determined electromyography signal.
Owner:KONINKLJIJKE PHILIPS NV
Wireless closed-loop and system to detect and treat sleep apnea
ActiveUS20150196766A1ElectrotherapyEvaluation of blood vesselsCentral sleep apneaClosed loop feedback
A wireless implantable system is provided that is externally powered and comprises of a closed-loop feedback for treating both patients with obstructive and central sleep apnea. A method is provided for treating sleep apnea using an implantable device. The method comprises sensing an inspiration (IN) signal representative of inspiration experienced by a patient from a respiratory surrogate signal and sensing a respiratory effort (RE) signal representative of an amount of effort exerted by the patient during respiration. The method also comprises analyzing the inspiration signal relative to an IN baseline, that corresponds to normal respiratory behavior, to identify an IN indicator, analyzing the RE signal relative to an RE baseline, that corresponds to a normal amount of respiratory exerted by the patient, to identify an RE indicator, declaring a central sleep apnea (CSA) state or an obstructive sleep apnea (OSA) state based on the IN and RE indicators, and delivering at least one of a CSA therapy when the CSA state is declared or an OSA therapy when the OSA state is declared.
Owner:PACESETTER INC
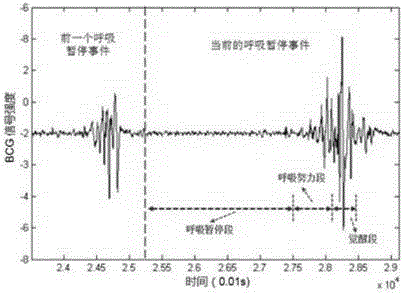
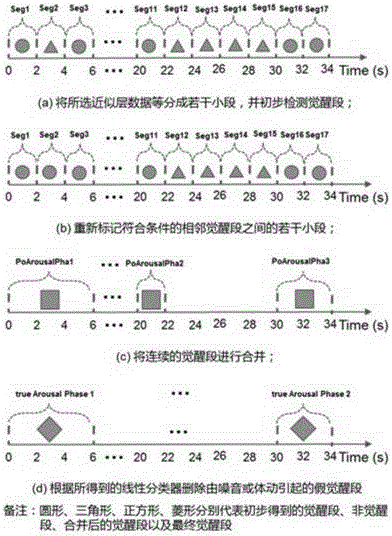
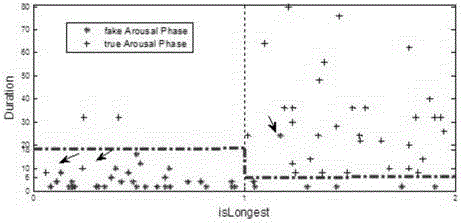
Method and system for apnea event detection based on BCG signal
InactiveCN106037671APrecise positioningEasy to describeDiagnostic signal processingSensorsSimulationThree-phase
The invention discloses a method and system for detecting apnea events based on BCG signals, which are used to accurately detect apnea events during sleep. This method locates the potential occurrence interval of respiratory events by identifying the arousal segment, and then divides the event potential occurrence interval into apnea segment, respiratory effort segment, and arousal segment, and then extracts fine-grained features that can describe the breathing pattern from the three segments. , and finally with the help of machine learning methods, it is judged whether the potential occurrence stage of the event contains an apnea event. The system mainly includes: a signal acquisition module, a data processing module, and a detection result output module. The method and system can automatically and accurately locate the potential occurrence interval of apnea events and automatically divide the interval into three different stages, which facilitates the description of breathing patterns from multiple aspects and in a fine-grained manner, and greatly improves the detection accuracy of apnea events Rate.
Owner:NORTHWESTERN POLYTECHNICAL UNIV
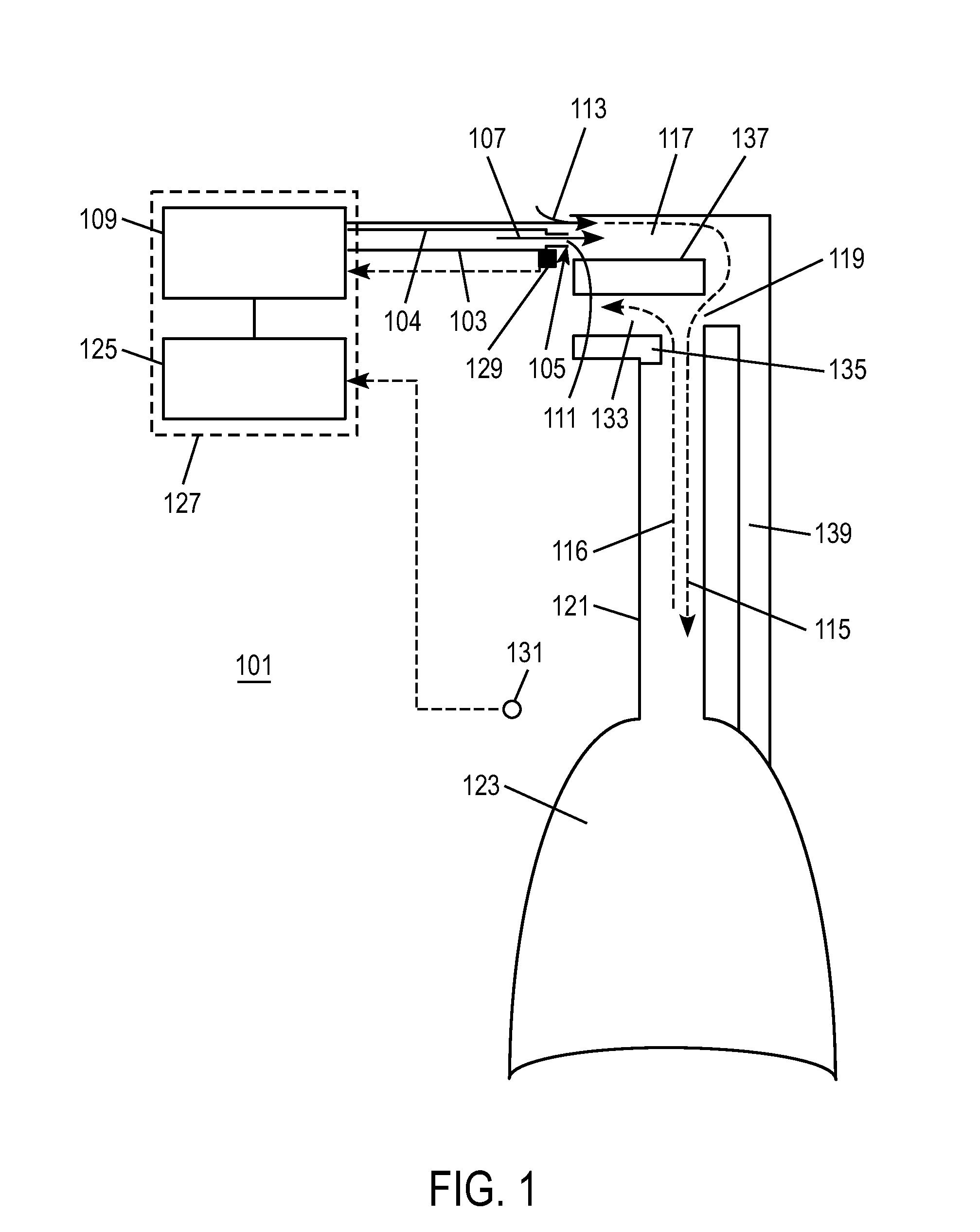
Arrangement and method for detecting respiratory effort of a patient
InactiveUS20070113851A1Accurate measurementPrecise deliveryOperating means/releasing devices for valvesRespiratory masksRespiratory effortAirway pressures
An arrangement and method for detecting spontaneous respiratory effort of a patient receiving ventilatory support via a breathing circuit. A patient / breathing circuit interface is adapted to provide a closed connection between a breathing passage of the patient and the breathing circuit. A sensor is disposed at least partially in the breathing passage of the patient and arranged to sense flow of gas through the breathing passage. The arrangement and method individually or in addition to the airway pressure measurement promotes reliable and rapid detection of breathing efforts of a non-intubated patient to promote efficient augmentation of patient breathing.
Owner:GENERAL ELECTRIC CO
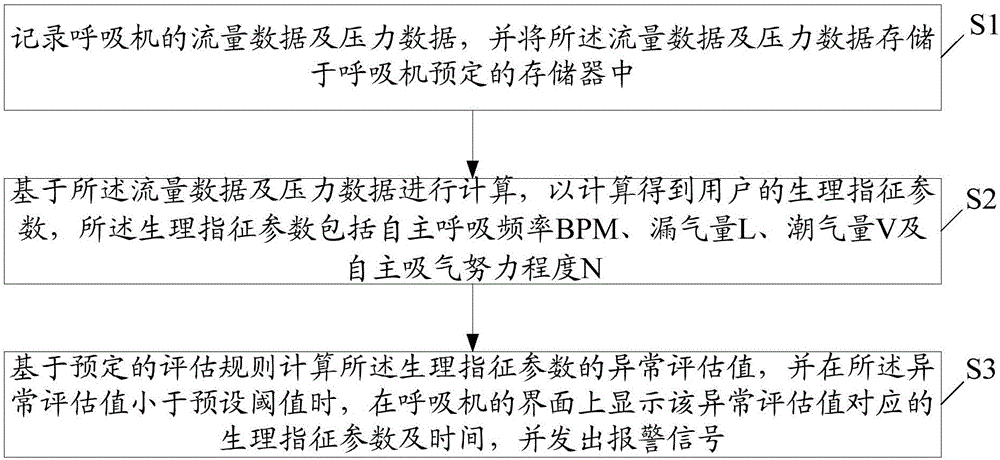
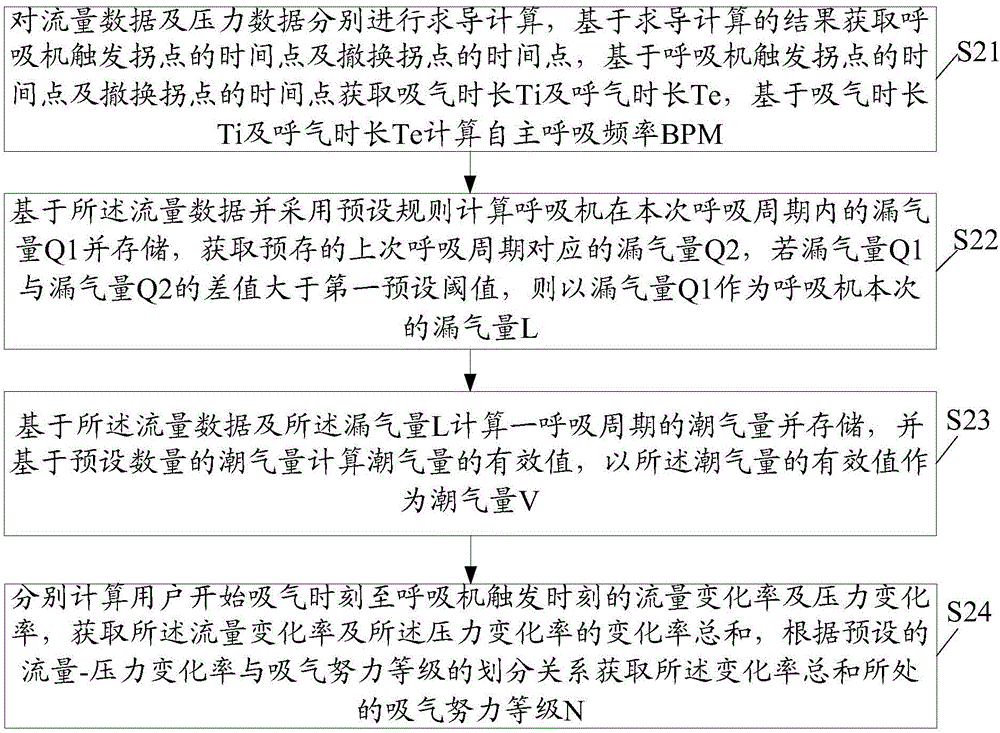
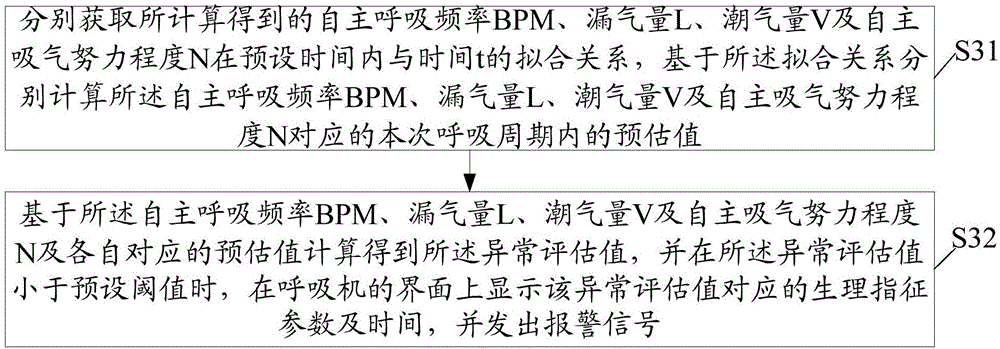
Ventilator warning method and ventilator
ActiveCN106730209AIntegrity guaranteedImprove accuracyRespiratorsMedical devicesAir volumeRespiratory effort
The invention relates to a ventilator warning method and a ventilator; the ventilator warning method comprises: recording flow data and pressure data of the ventilator, and storing the flow data and pressure in a predetermined storage of the ventilator; calculating based on the flow data and pressure data to obtain a user's physiological indicator parameters including Spontaneous respiratory rate BPM, air leakage L, moist air volume V and spontaneous respiratory effort level N; calculating abnormal assessment values of the physiological indicator parameters based on predetermined assessment rules, displaying the physiological indicator parameters and time corresponding to the abnormal assessment values on an interface of the ventilator if the abnormal assessment values are less than a preset threshold, and sending out a warning signal. The ventilator warning method and the ventilator can send out a warning signal when a user is in abnormal condition, monitoring data integrity is guaranteed, and subsequent treatment accuracy can be improved.
Owner:HUNAN MICOME ZHONGJIN MEDICAL SCI & TECH DEV CO LTD
Methods and apparatus for detection of disordered breathing
PendingUS20220007965A1Improve comfortIncrease costHealth-index calculationAcoustic sensorsPhysical medicine and rehabilitationSleeping disorders
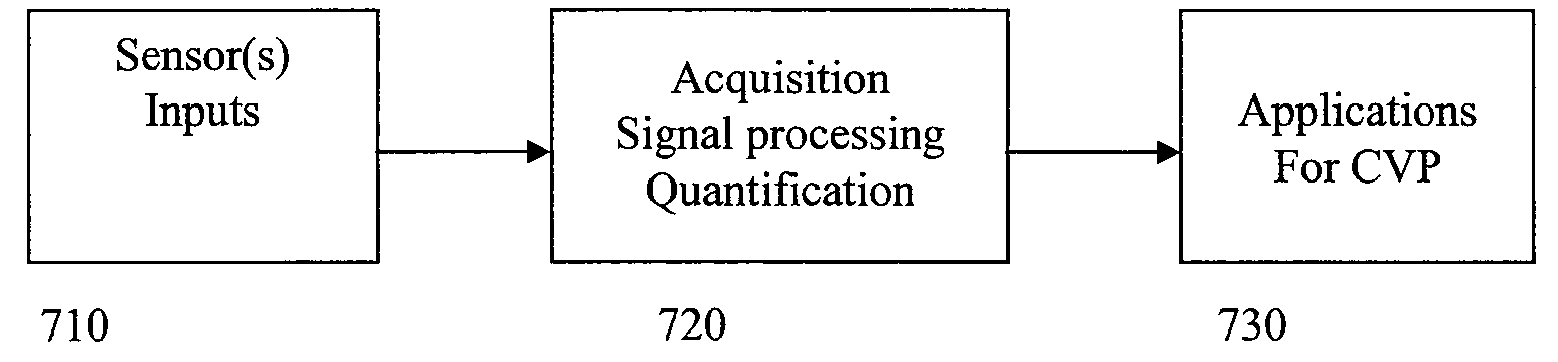
Methods and apparatus provide monitoring of a sleep disordered breathing state of a person such as for screening. One or more sensors may be configured for non-contact active and / or passive sensing. The processor(s) (7304, 7006) may extract respiratory effort signal(s) from one or more motion signals generated by active non-contact sensing with the sensor(s). The processor(s) may extract one or more energy band signals from an acoustic audio signal generated by passive non-contact sensing with the sensor(s). The processor(s) may assess the energy band signal(s) and / or the respiratory efforts signal(s) to generate intensity signal(s) representing sleep disorder breathing modulation. The processor(s) may classify feature(s) derived from the one or more intensity signals to generate measure(s) of sleep disordered breathing. The processor may generate a sleep disordered breathing indicator based on the measure(s) of sleep disordered breathing. Some versions may evaluate sensing signal(s) to generate indication(s) of cough event(s) and / or cough type.
Owner:RESMED SENSOR TECH
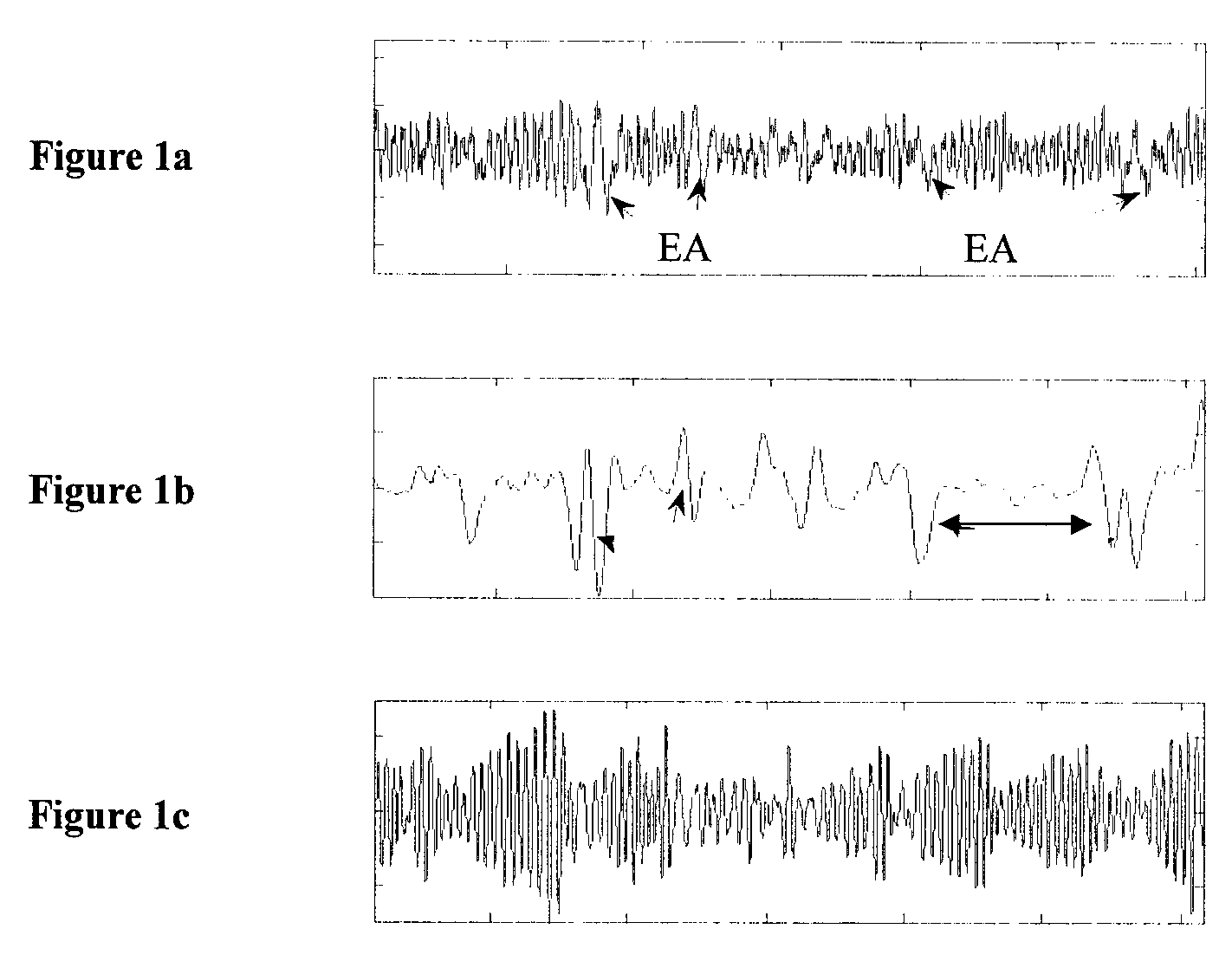
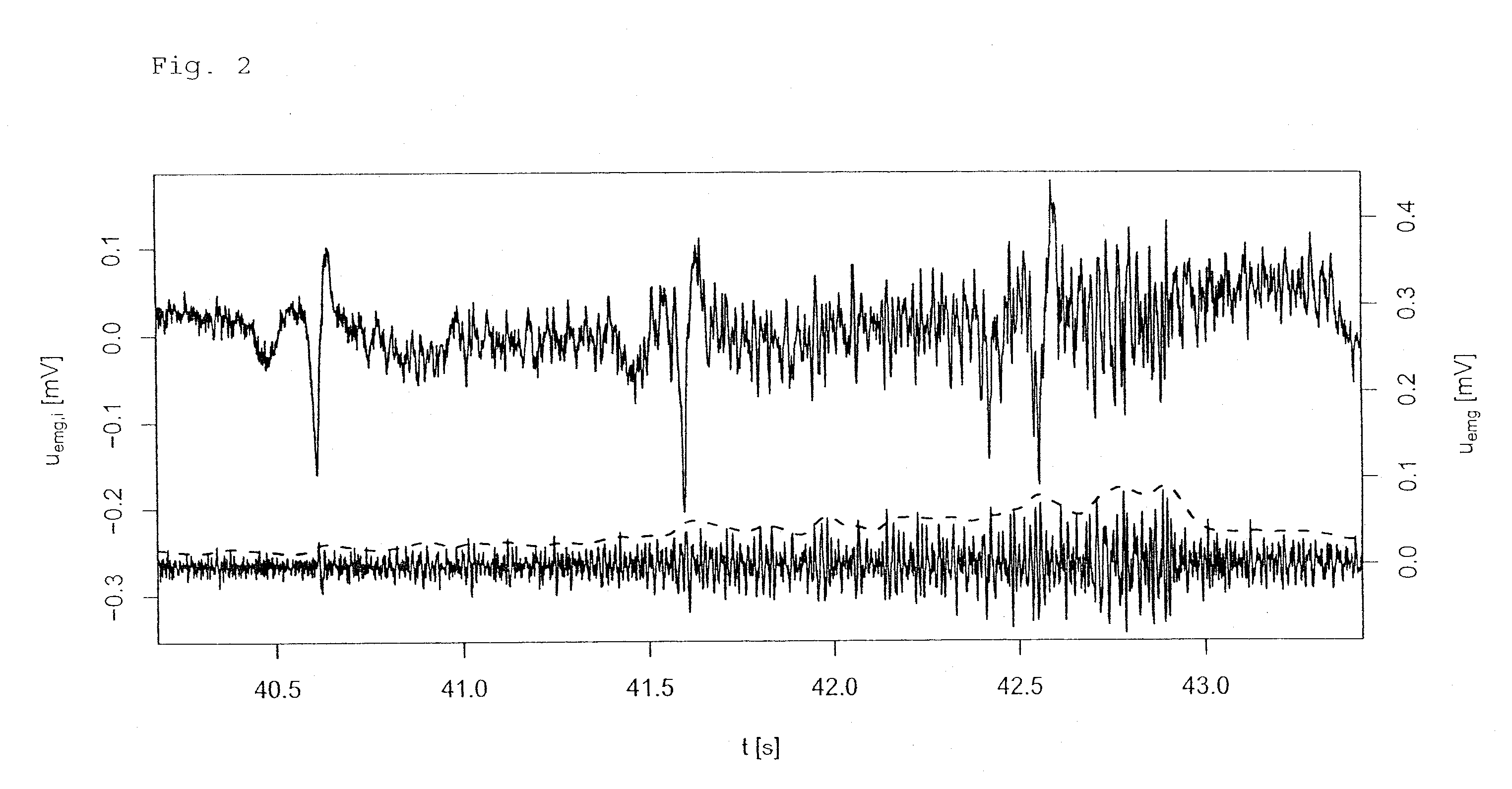
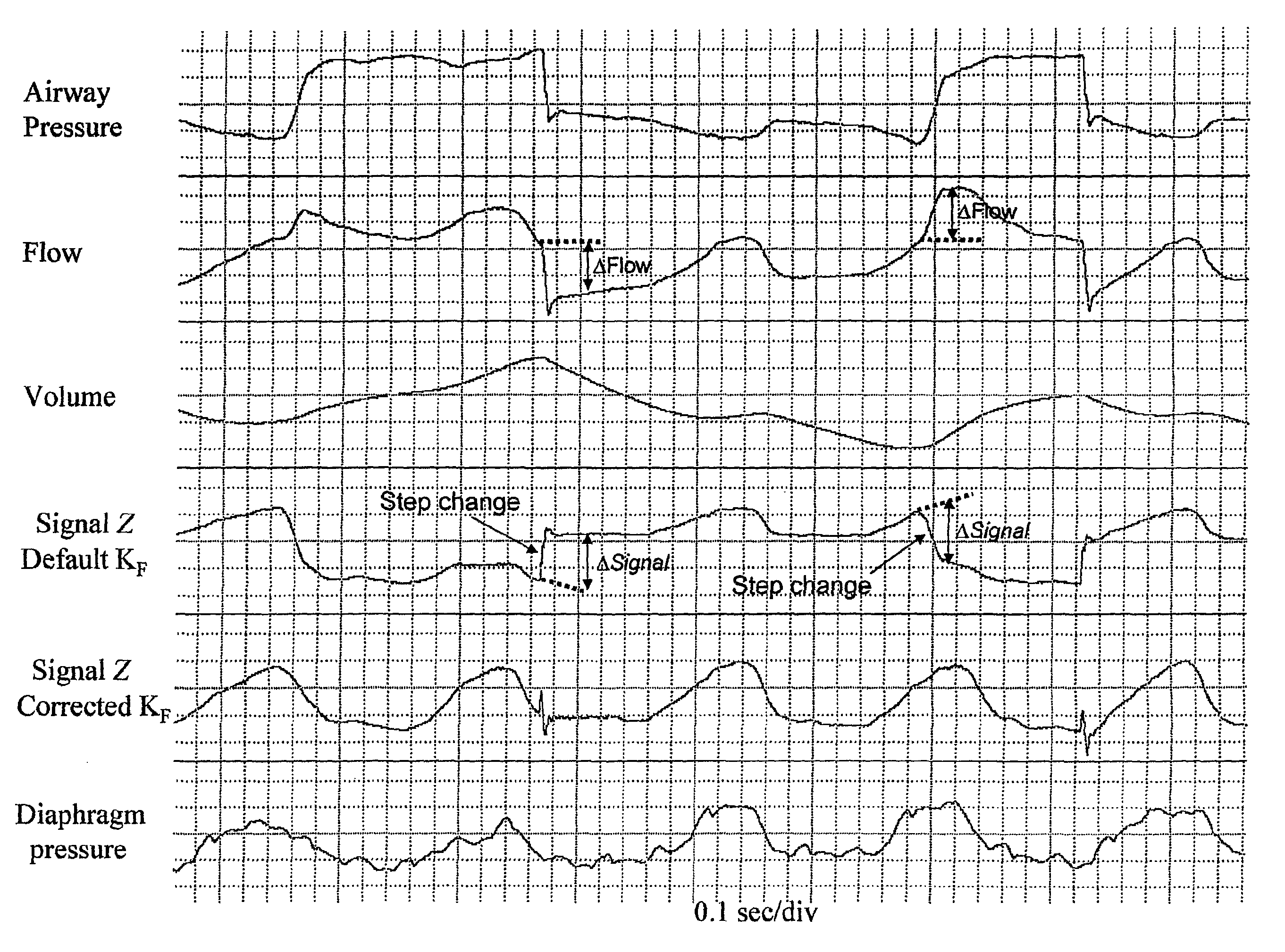
Method and device for generating of a signal that reflects respiratory efforts in patients on ventilatory support
A method and device for generating a signal that mirrors changes in the level of effort exerted by respiratory muscles of patients on mechanical ventilatory support comprising: monitoring and storing airway pressure (Paw), rate of gas flow (F), and volume of gas flow (V), and generating a composite pressure signal using resistive pressure units (KF) determined from elapsed data and selected to minimize step changes in the calculated signal and elastic pressure units (Kv) determined from elapsed data by steps comprising: —scanning stored F or Paw during exhalation and identifying where their trajectory transiently reverses direction to detect transients; —selecting points within the exhalation that are at preselected distances away from the transients; —calculating the value of Kv required to force the values of the calculated signal at said selected points in elapsed breaths to be substantially equal when the selected value of KF is used as the flow coefficient.
Owner:YRT
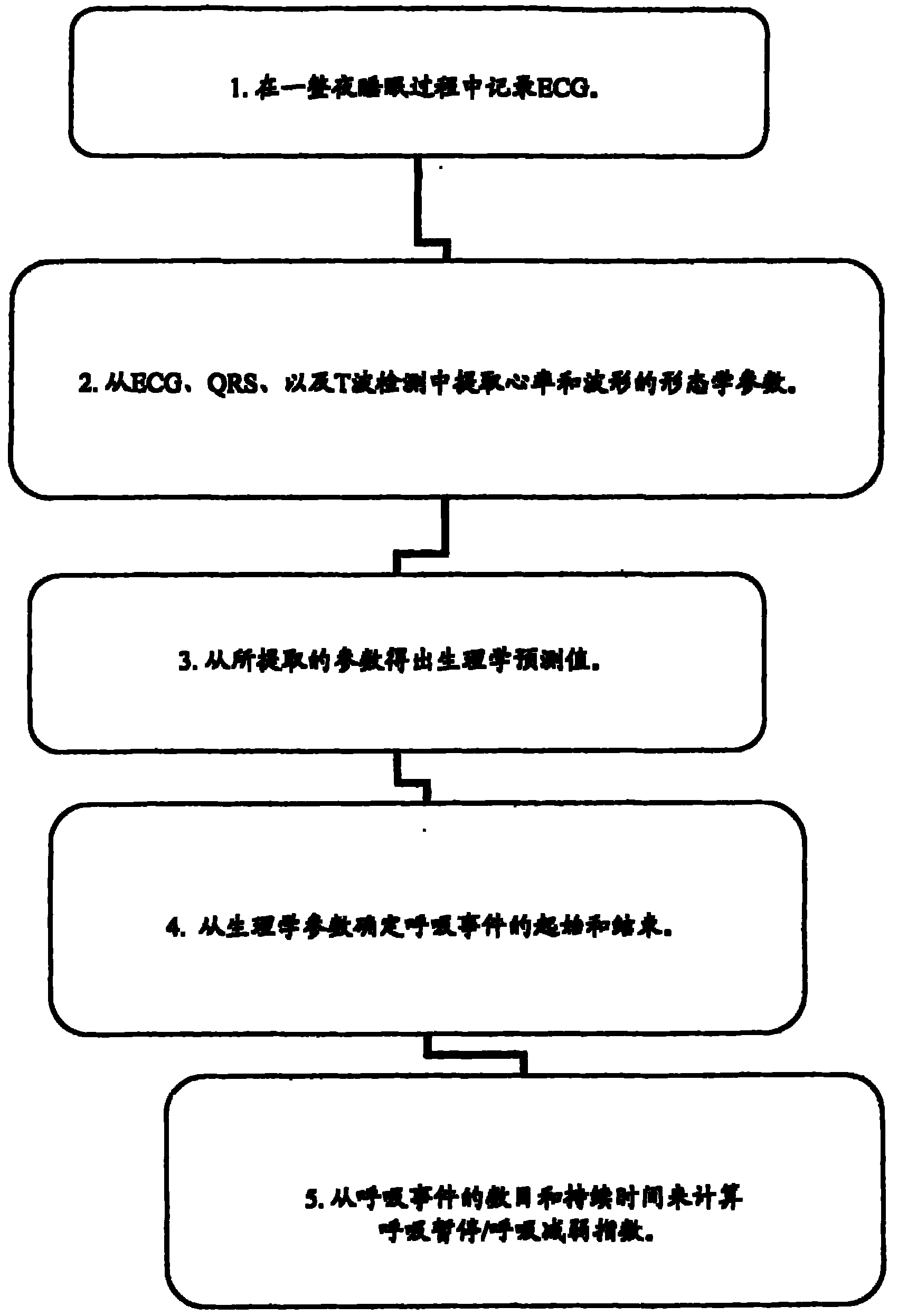
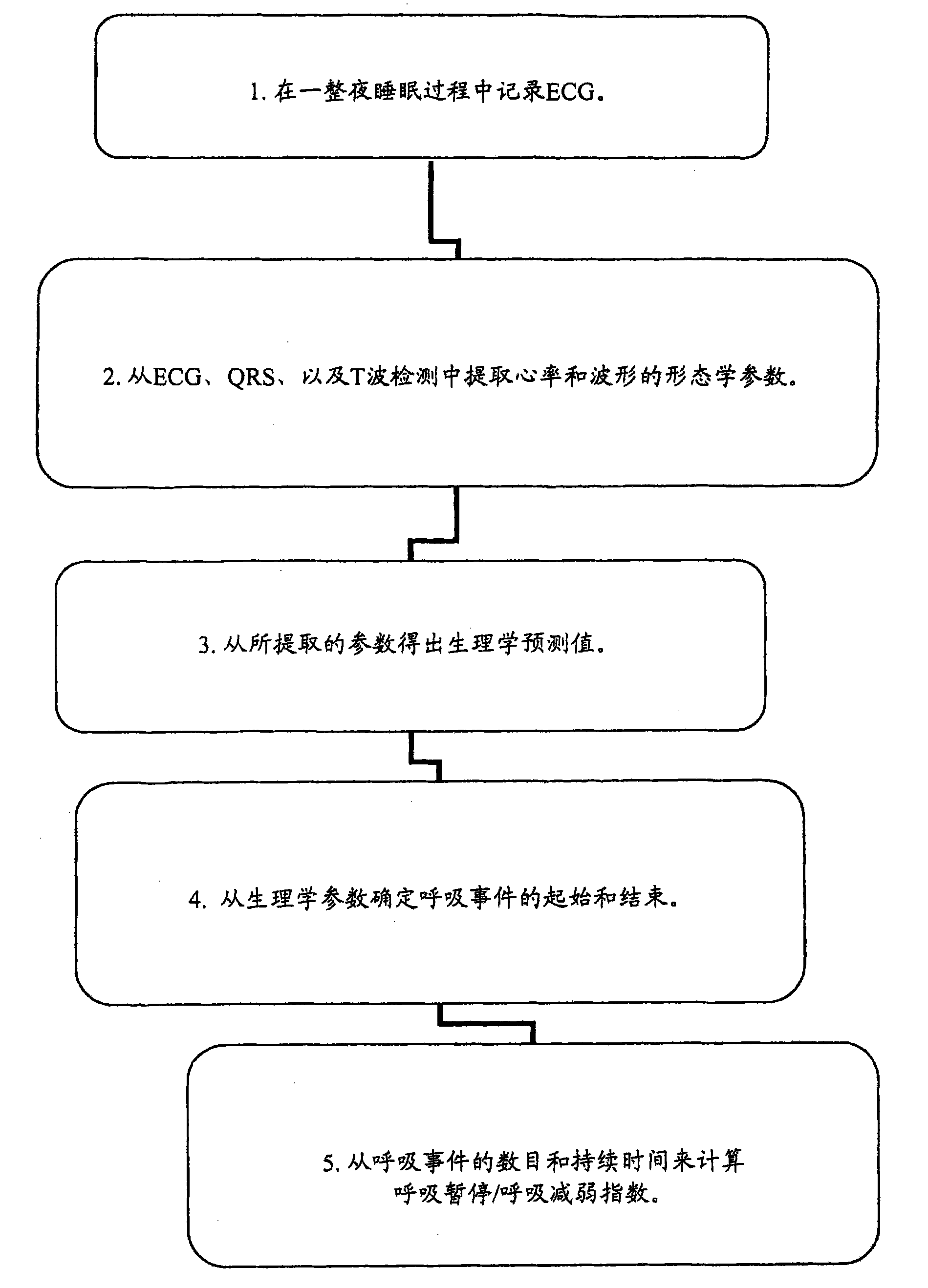
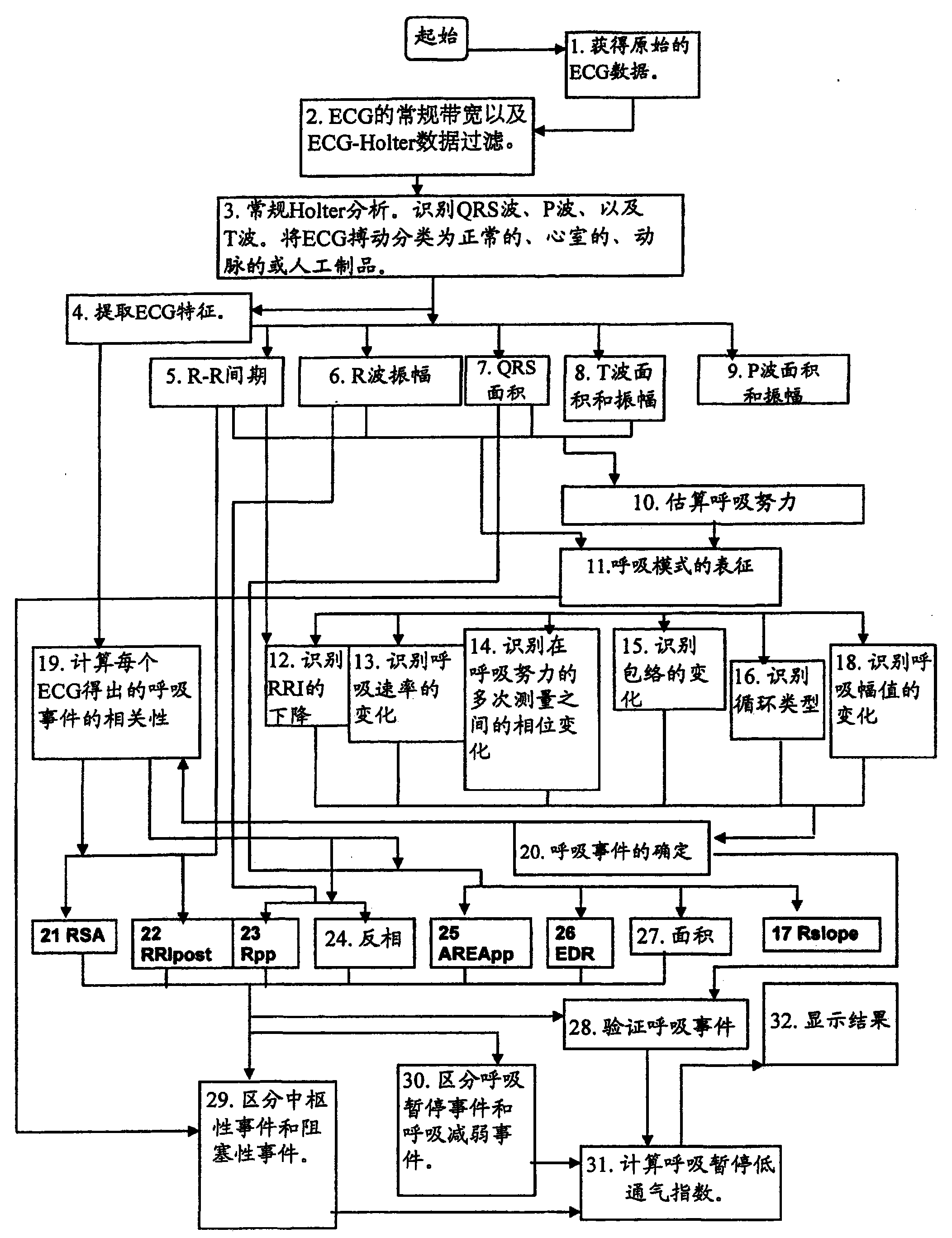
Electrocardiogram derived apnoea/hypopnea index
The present invention provides a method and apparatus for determining the occurrence of apnoeas or hypopneas from ECG signal data alone. The method is carried out by apparatus configured to acquire ECG signals from a sleeping subject, transform the signals to data, and extract ECG features relevant to estimate breathing effort for the determination of respiratory events characteristic of apnoeas and hypopneas. The extracted ECG features are correlates of breathing efforts and are used as surrogate measures of breathing or respiratory events. The method may include calculating an AHI or apnoea / hypopnea index. The method may classify apnoeas into obstructive or central apnoeas.
Owner:COMPUMEDICS MEDICAL INNOVATION
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com