Patents
Literature
181 results about "Commissure" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
A commissure (/ˈkɒməʃər/) is the location at which two objects abut or are joined. The term is used especially in the fields of anatomy and biology. In biology, the meeting of the two valves of a brachiopod or clam is a commissure; in botany, the term is used to denote the place where a fern's laterally expanded vein endings come together in a continuous marginal sorus.
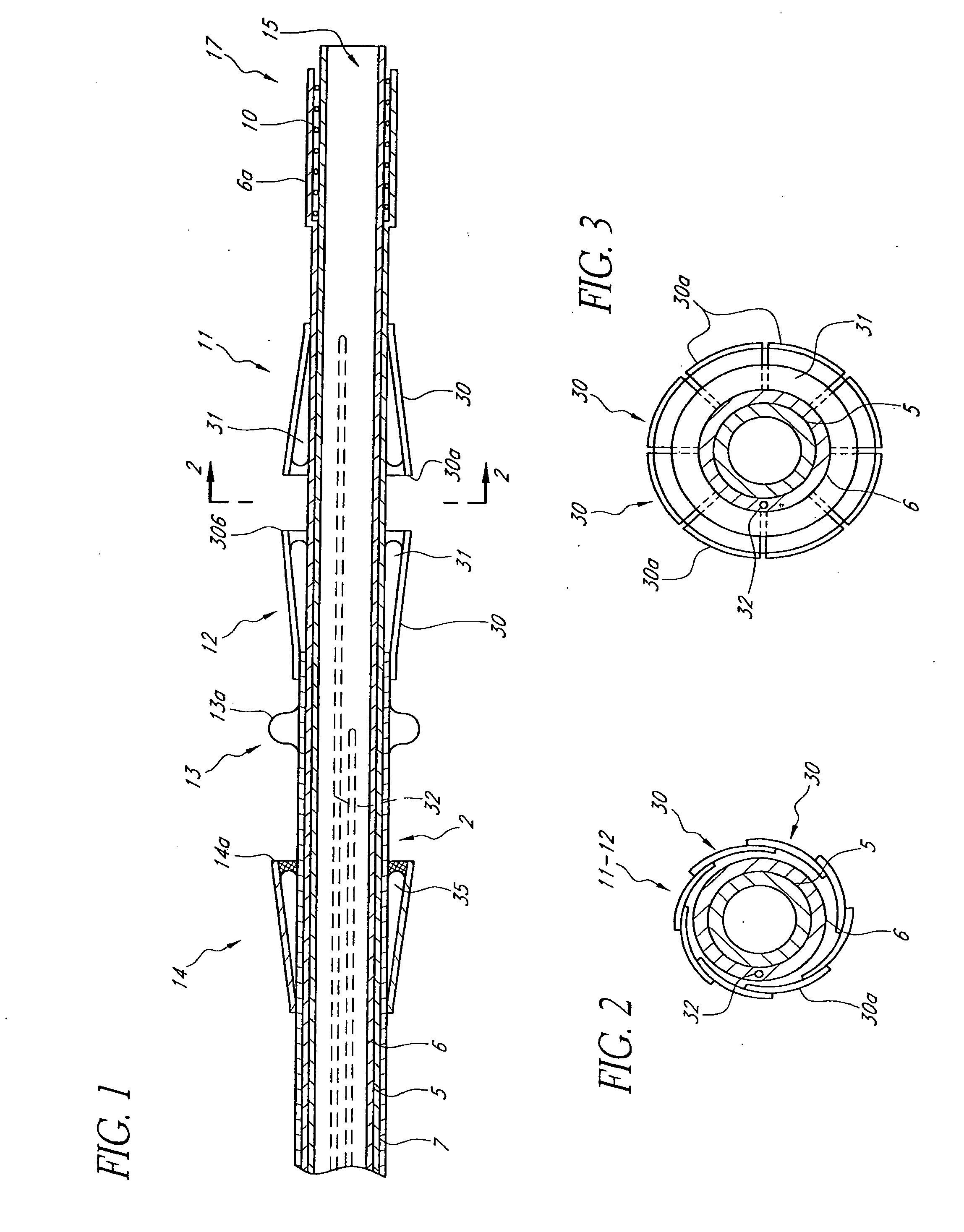
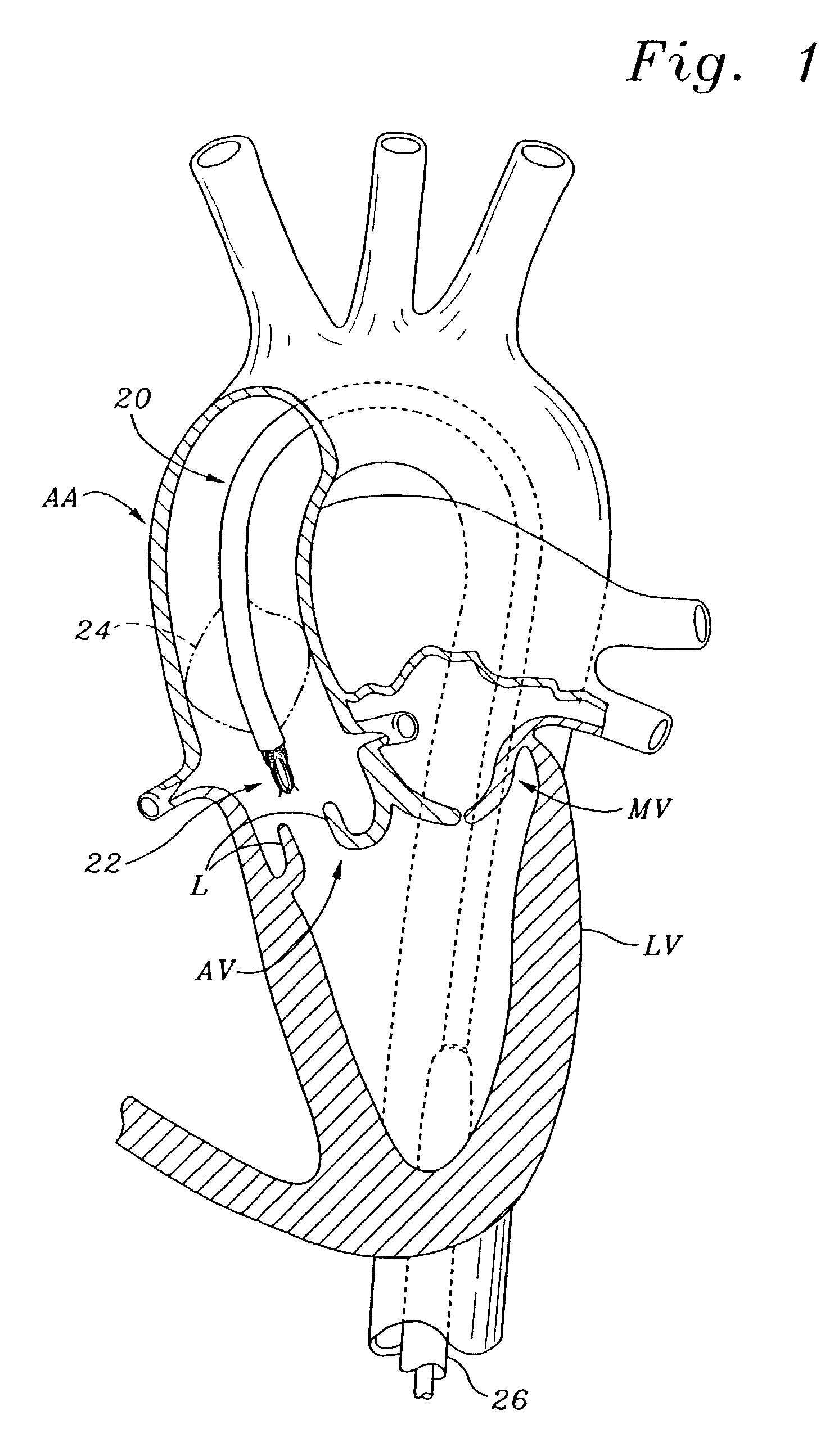
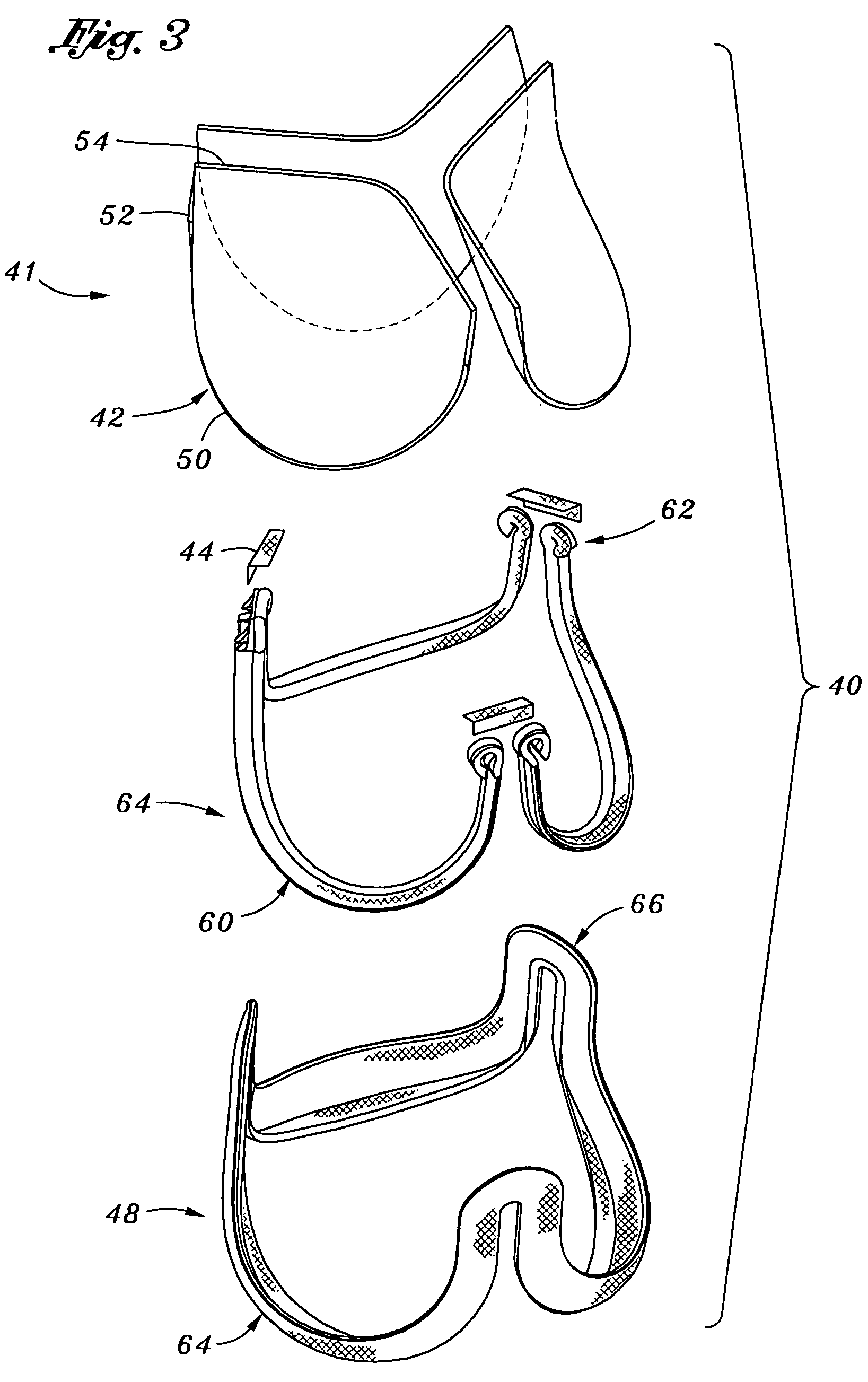
Prosthetic valve for transluminal delivery
InactiveUS7018406B2Preventing substantial migrationEliminate the problemBalloon catheterHeart valvesProsthesisCommissure
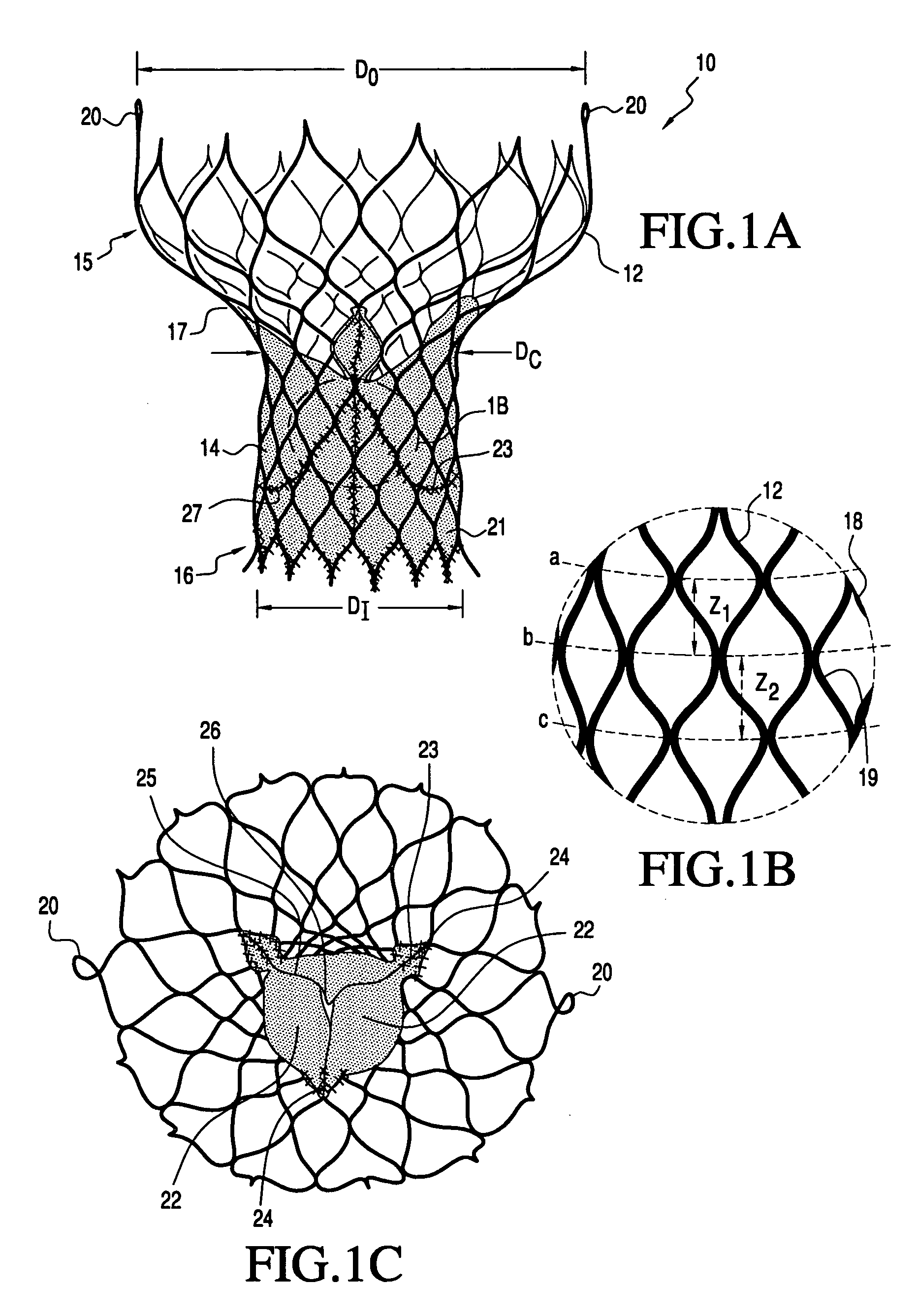
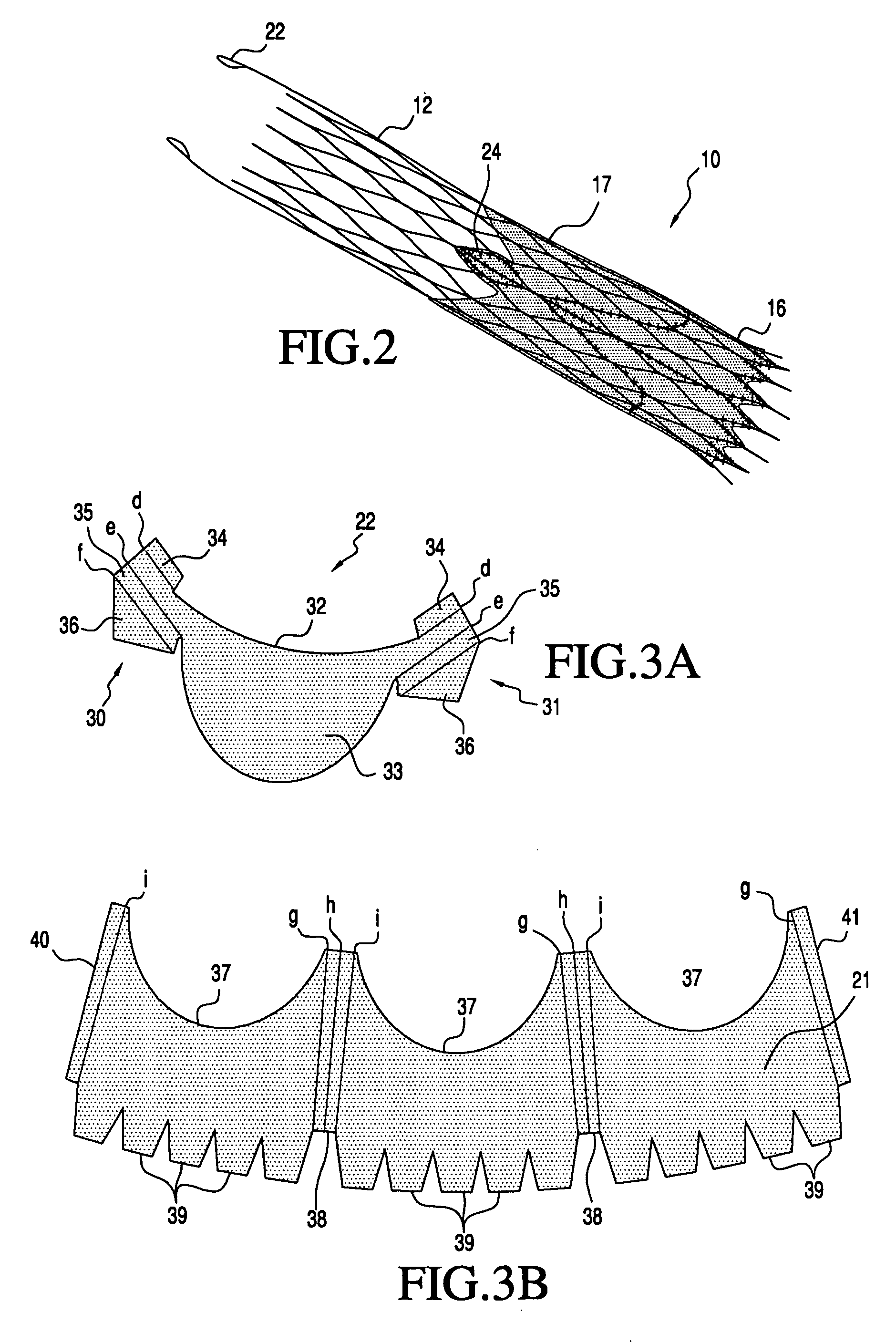
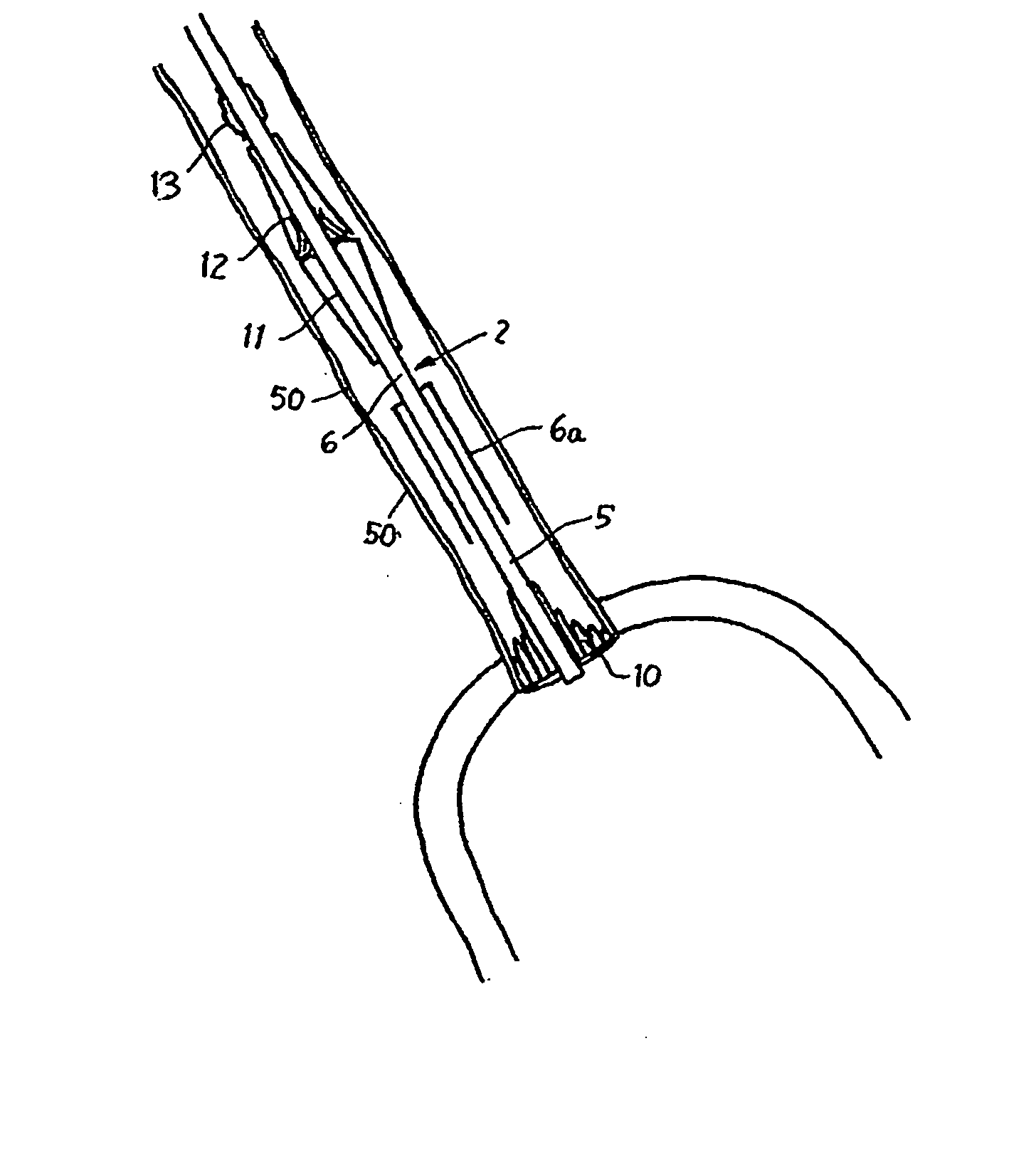
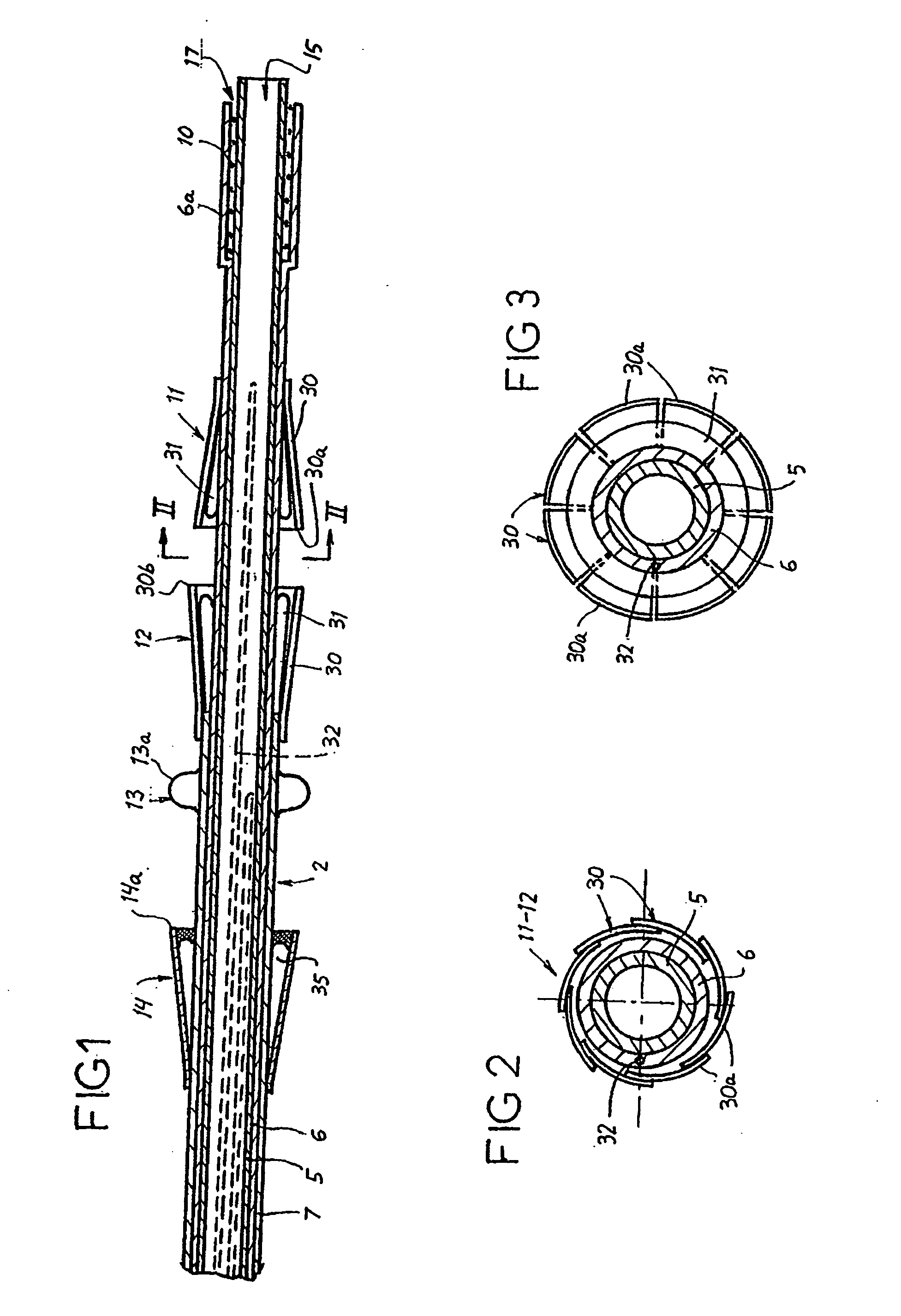
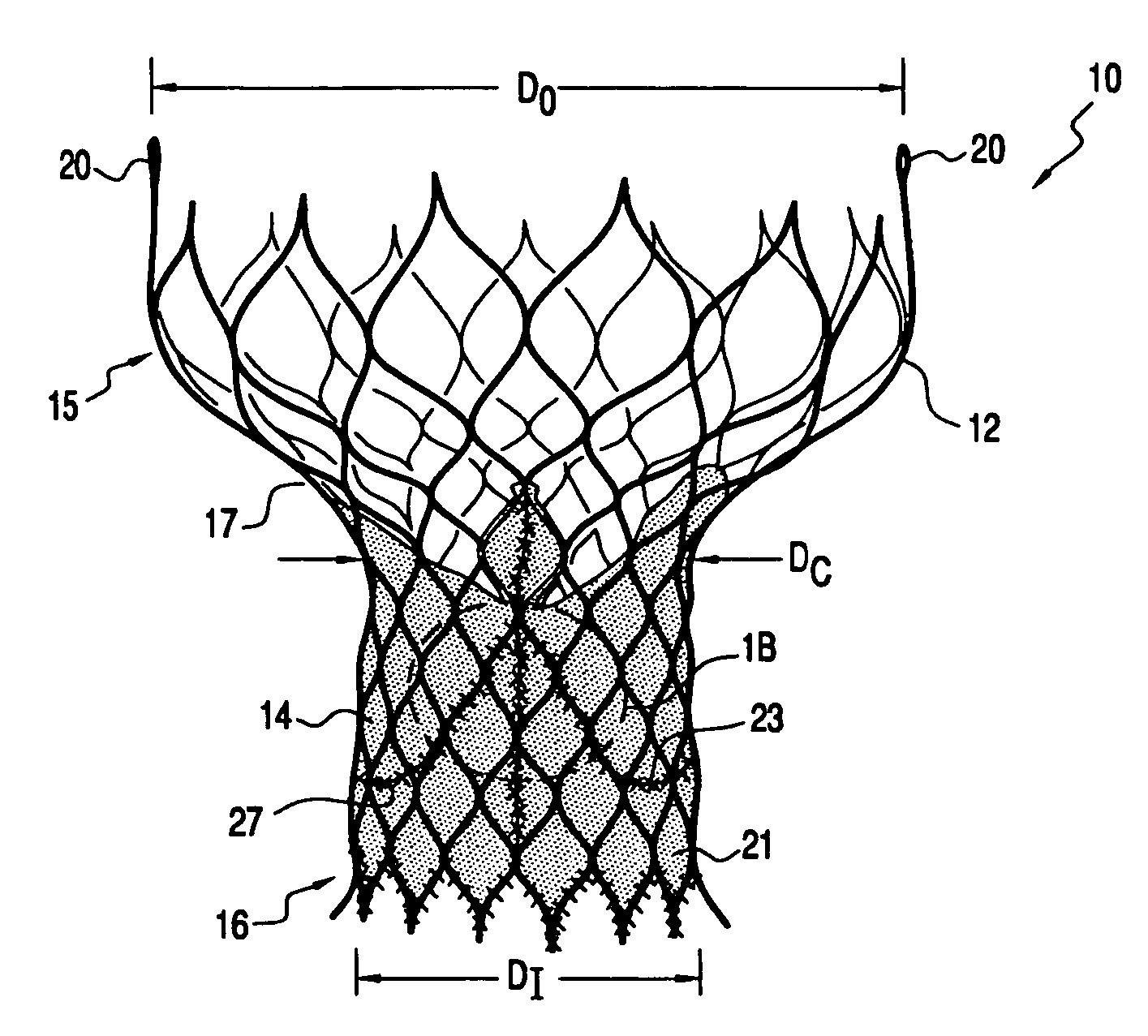
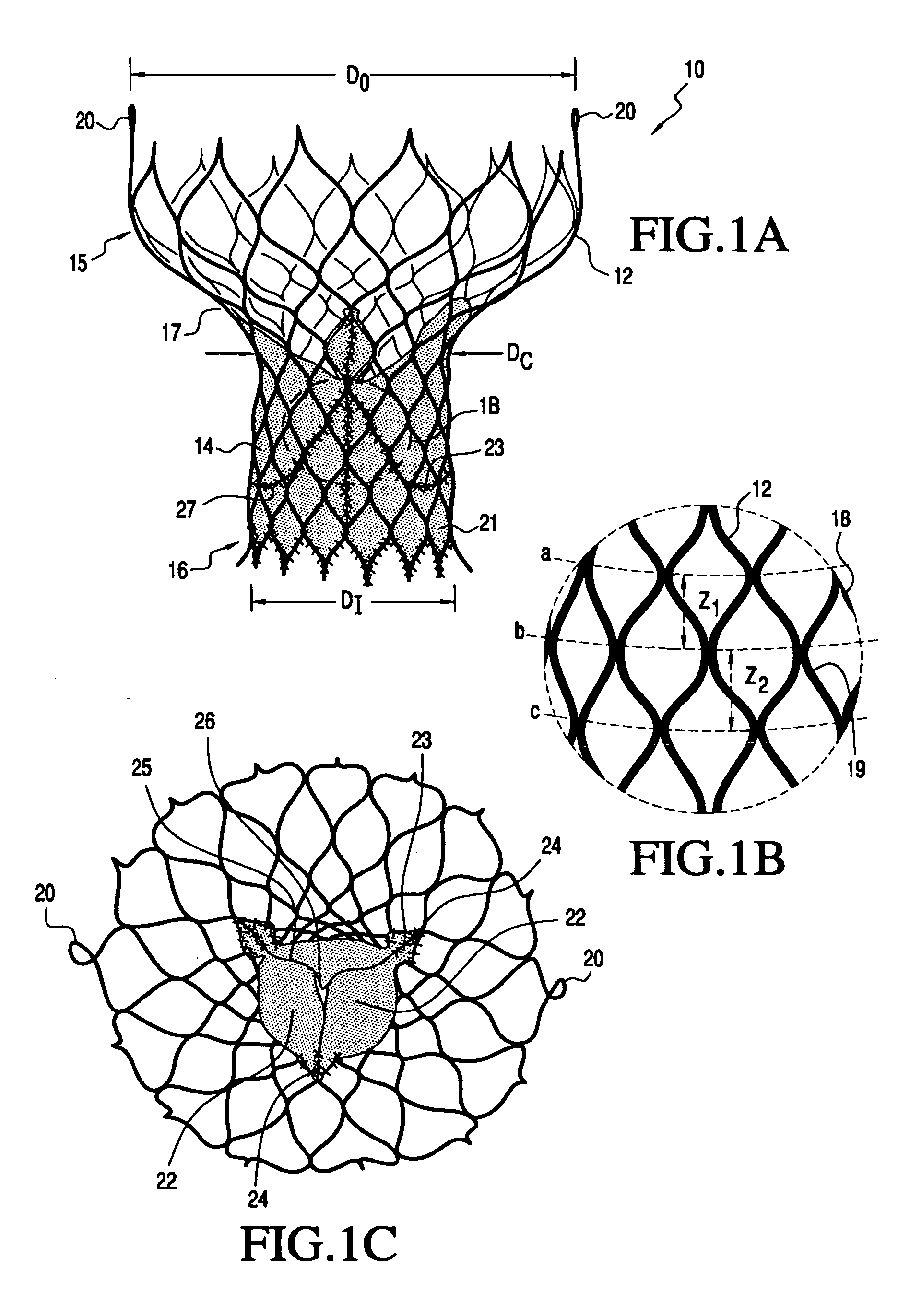
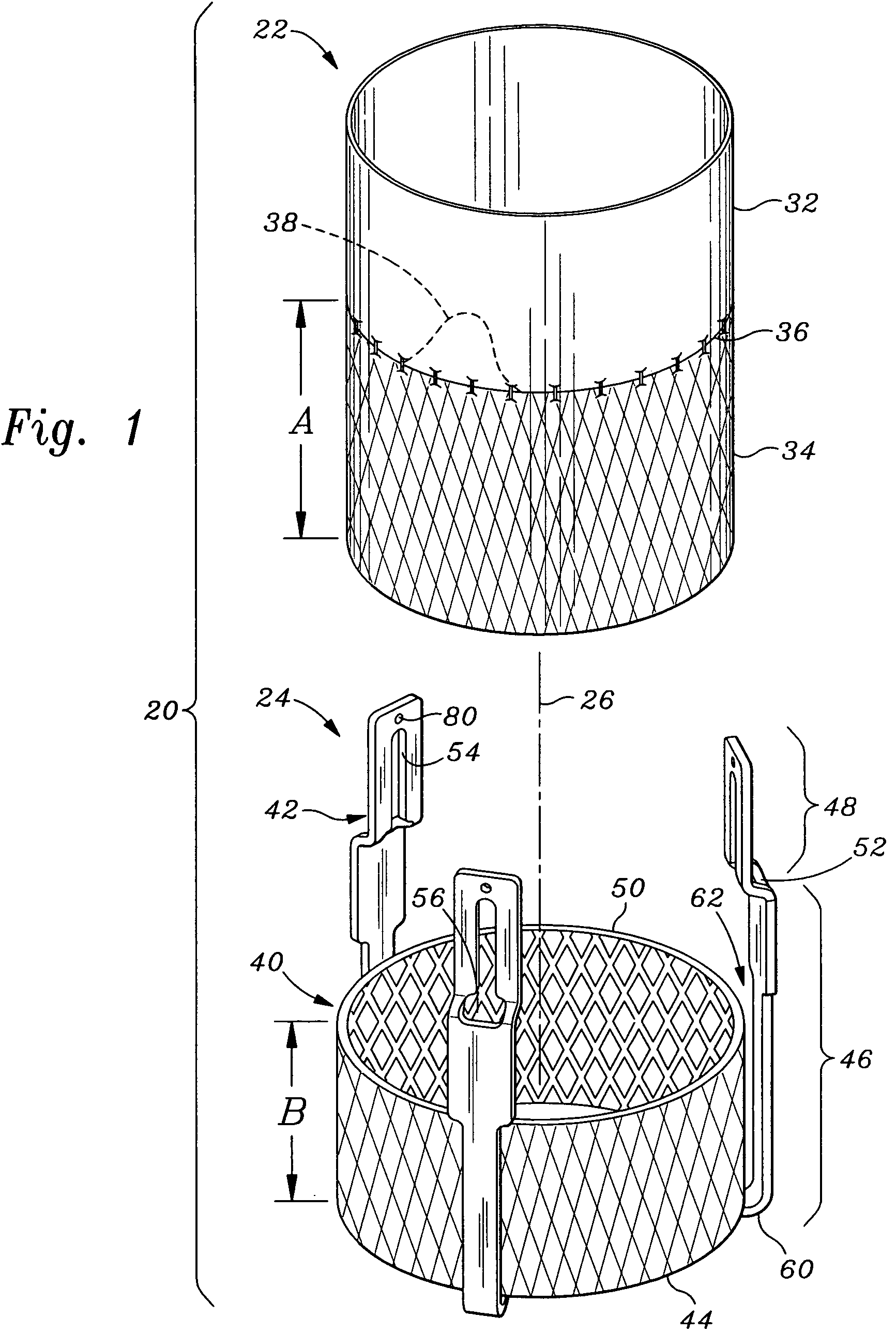
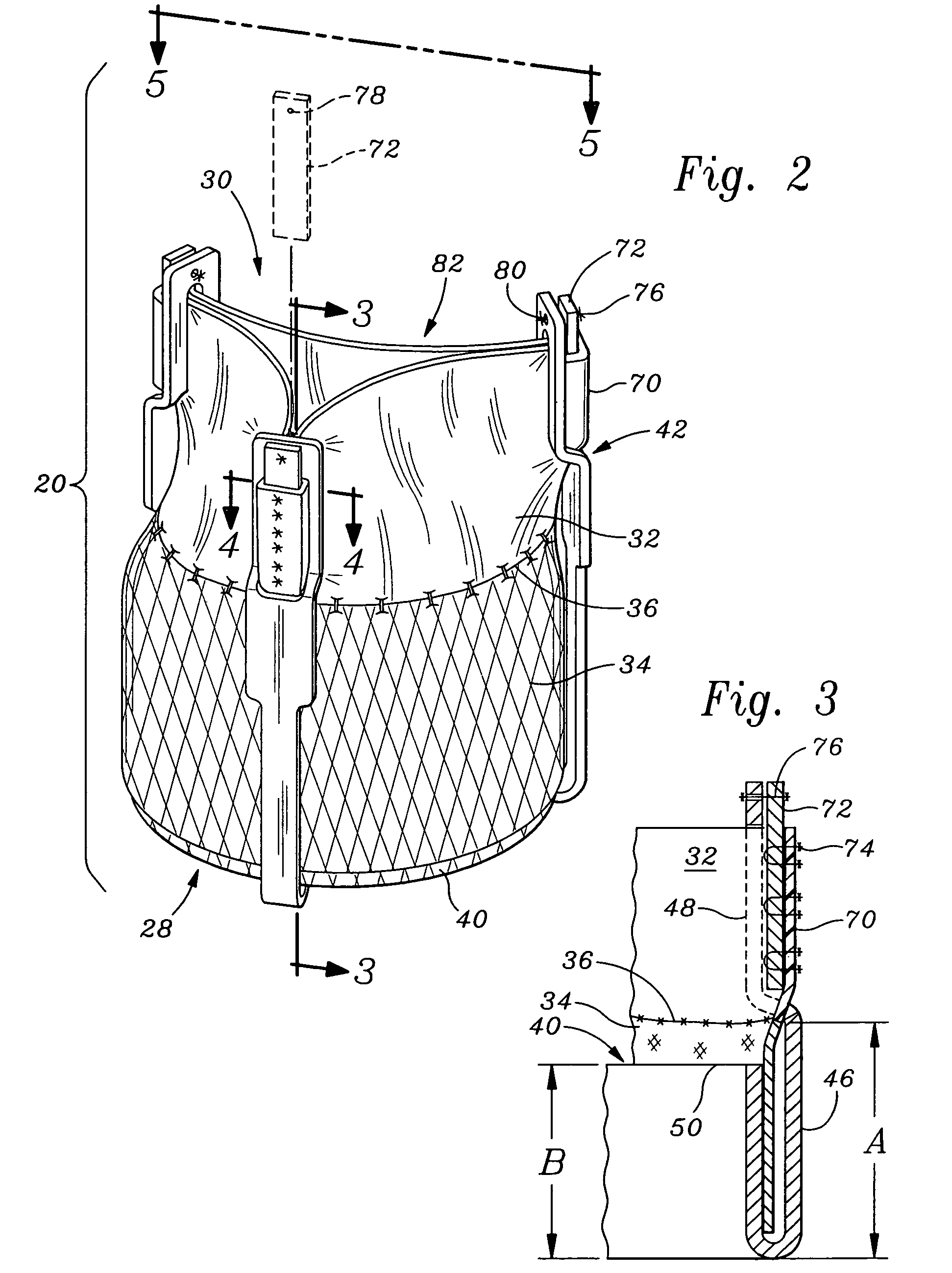
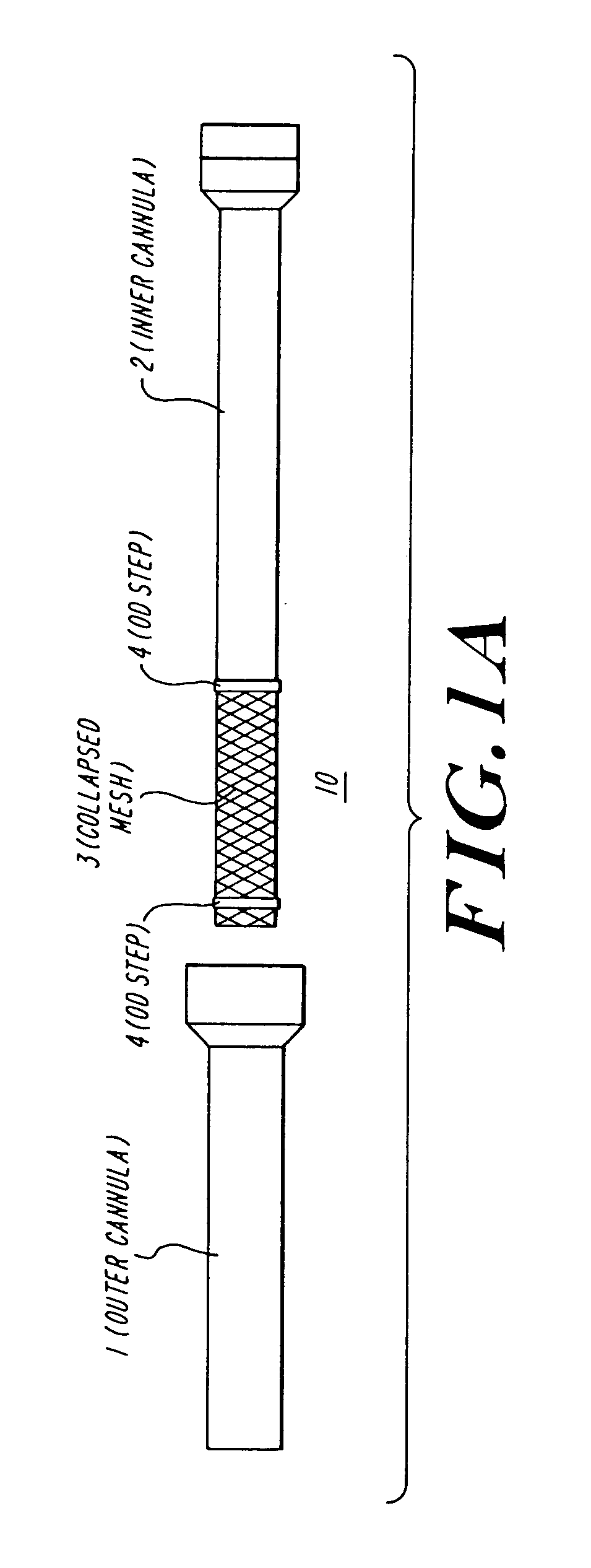
A prosthetic valve assembly for use in replacing a deficient native valve comprises a replacement valve supported on an expandable valve support. If desired, one or more anchor may be used. The valve support, which entirely supports the valve annulus, valve leaflets, and valve commissure points, is configured to be collapsible for transluminal delivery and expandable to contact the anatomical annulus of the native valve when the assembly is properly positioned. The anchor engages the lumen wall when expanded and prevents substantial migration of the valve assembly when positioned in place. The prosthetic valve assembly is compressible about a catheter, and restrained from expanding by an outer sheath. The catheter may be inserted inside a lumen within the body, such as the femoral artery, and delivered to a desired location, such as the heart. When the outer sheath is retracted, the prosthetic valve assembly expands to an expanded position such that the valve and valve support expand within the deficient native valve, and the anchor engages the lumen wall.
Owner:MEDTRONIC COREVALVE
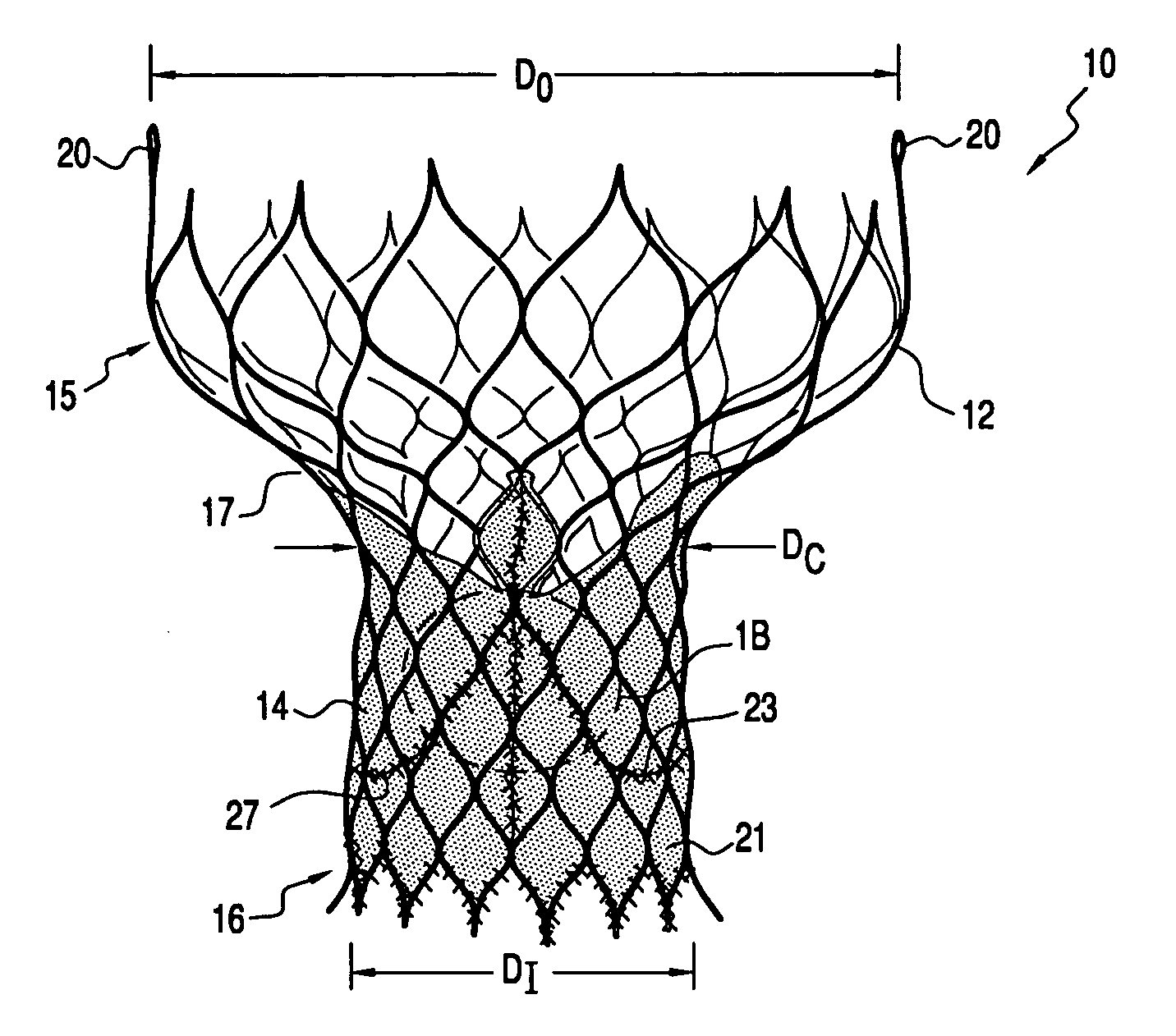
Heart valve prosthesis and methods of manufacture and use
ActiveUS20060259136A1Overcomes drawbackReduce riskHeart valvesBlood vesselsHorizontal forceHourglass
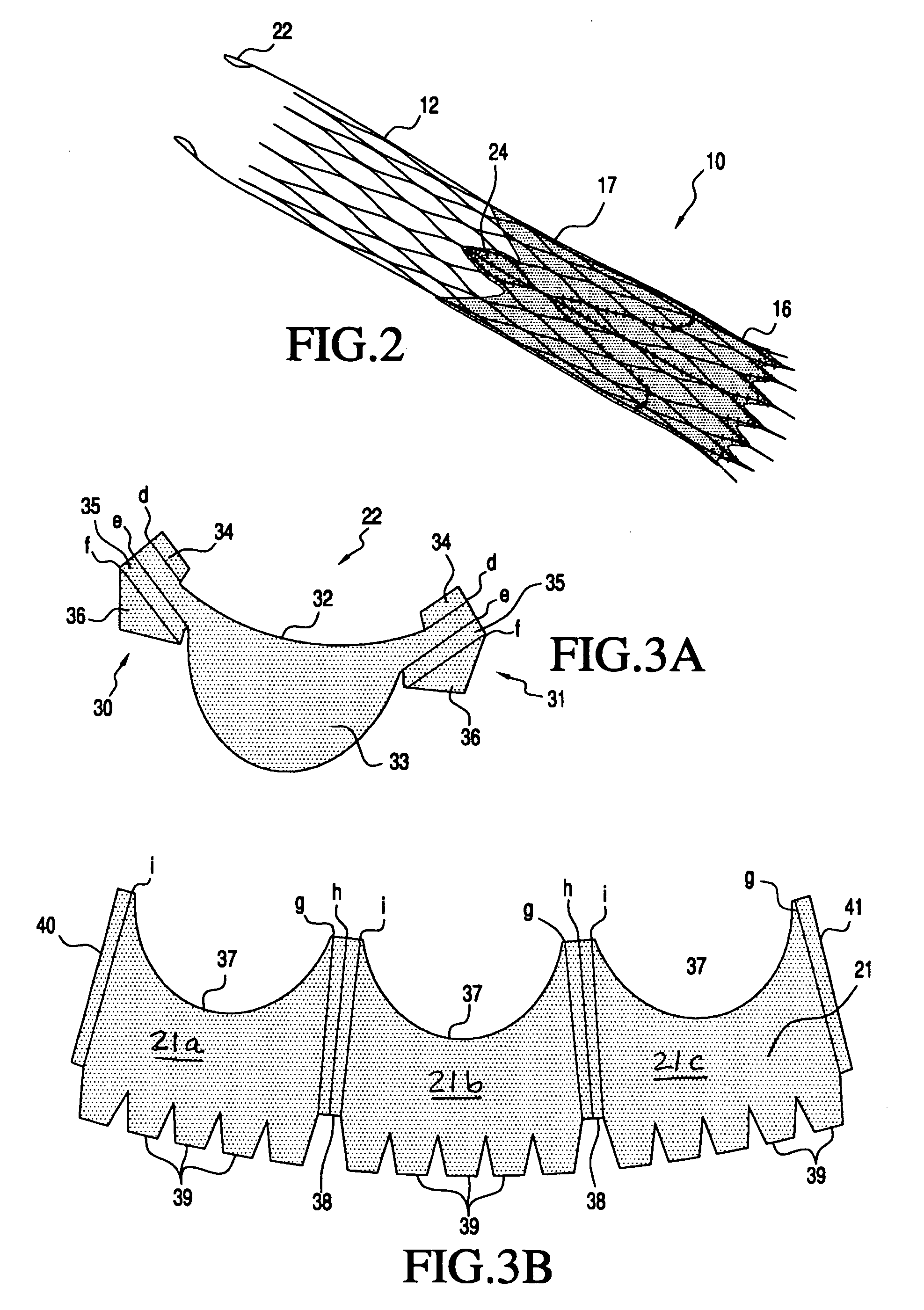
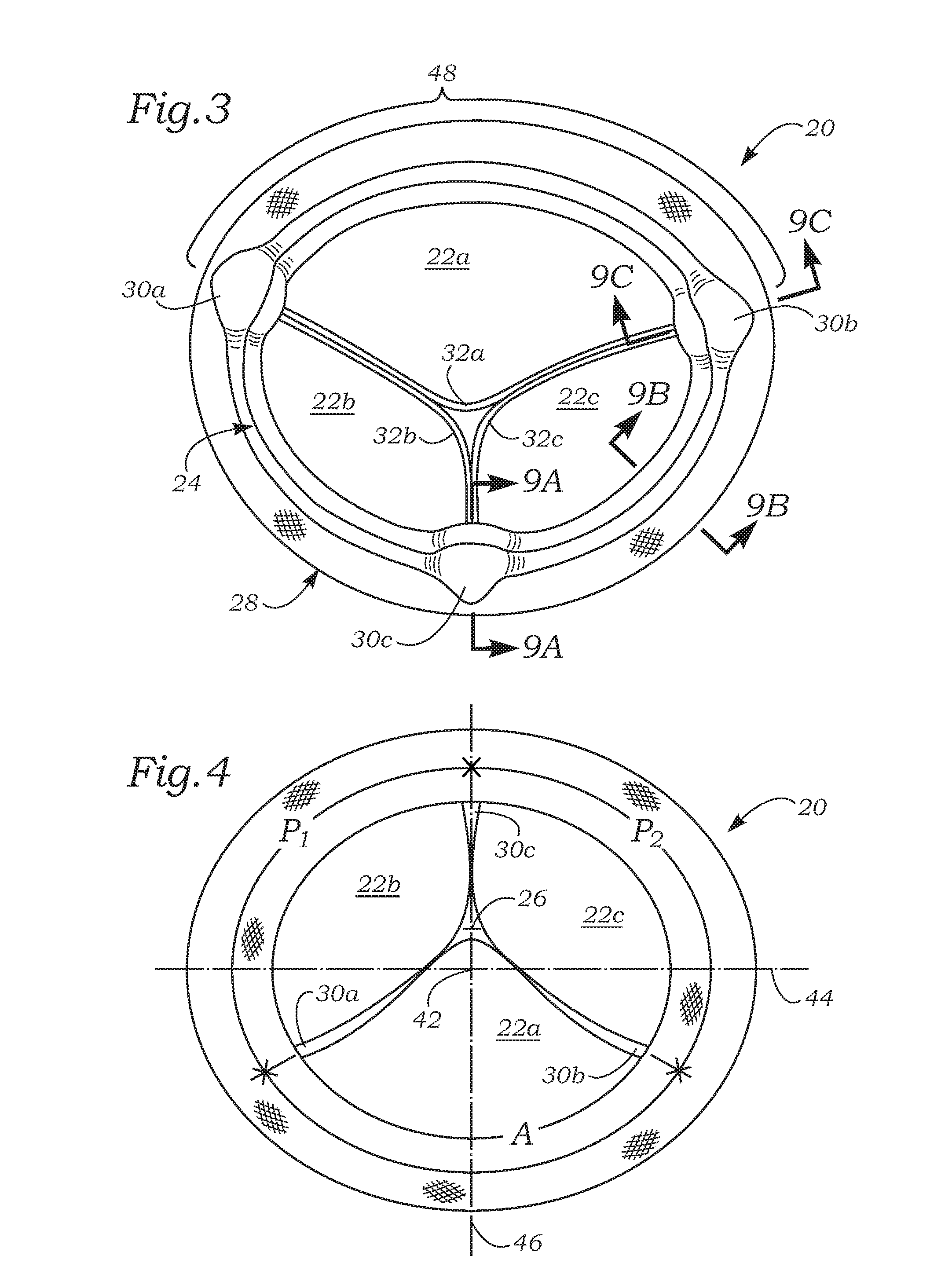
A heart valve prosthesis is provided having a self-expanding multi-level frame that supports a valve body comprising a skirt and plurality of coapting leaflets. The frame transitions between a contracted delivery configuration that enables percutaneous transluminal delivery, and an expanded deployed configuration having an asymmetric hourglass shape. The valve body skirt and leaflets are constructed so that the center of coaptation may be selected to reduce horizontal forces applied to the commissures of the valve, and to efficiently distribute and transmit forces along the leaflets and to the frame. Alternatively, the valve body may be used as a surgically implantable replacement valve prosthesis.
Owner:MEDTRONIC ARDIAN LUXEMBOURG SARL
Non-cylindrical prosthetic valve system for transluminal delivery
InactiveUS20070043435A1Preventing substantial migrationEliminate the problemBalloon catheterHeart valvesCoronary arteriesProsthesis
A prosthetic valve assembly for use in replacing a deficient native valve comprises a replacement valve supported on an expandable prosthesis frame. If desired, one or more expandable anchors may be used. The prosthesis frame, which entirely supports the valve annulus, valve leaflets, and valve commissure points, is configured to be collapsible for transluminal delivery and expandable to contact the anatomical annulus of the native valve when the assembly is properly positioned. Portions of the prosthesis frame may expand to a preset diameter to maintain coaptivity of the replacement valve and to prevent occlusion of the coronary ostia. The prosthesis frame is compressible about a catheter, and restrained from expanding by an outer sheath. The catheter may be inserted inside a lumen within the body, such as the femoral artery, and delivered to a desired location, such as the heart. When the outer sheath is retracted, the prosthesis frame expands to an expanded position such that the valve and prosthesis frame expand at the implantation site and the anchor engages the lumen wall. The prosthesis frame has a non-cylindrical configuration with a preset maximum expansion diameter region about the valve opening to maintain the preferred valve geometry. The prosthesis frame may also have other regions having a preset maximum expansion diameter to avoid blockage of adjacent structures such as the coronary ostia.
Owner:MEDTRONIC COREVALVE
Heart valve prosthesis and methods of manufacture and use
ActiveUS20060265056A1Reduce risk of damageEfficient configurationHeart valvesHorizontal forceHourglass
A heart valve prosthesis is provided having a self-expanding multi-level frame that supports a valve body comprising a skirt and plurality of coapting leaflets. The frame transitions between a contracted delivery configuration that enables percutaneous transluminal delivery, and an expanded deployed configuration having an asymmetric hourglass shape. The valve body skirt and leaflets are constructed so that the center of coaptation may be selected to reduce horizontal forces applied to the commissures of the valve, and to efficiently distribute and transmit forces along the leaflets and to the frame. Alternatively, the valve body may be used as a surgically implantable replacement valve prosthesis.
Owner:MEDTRONIC ARDIAN LUXEMBOURG SARL
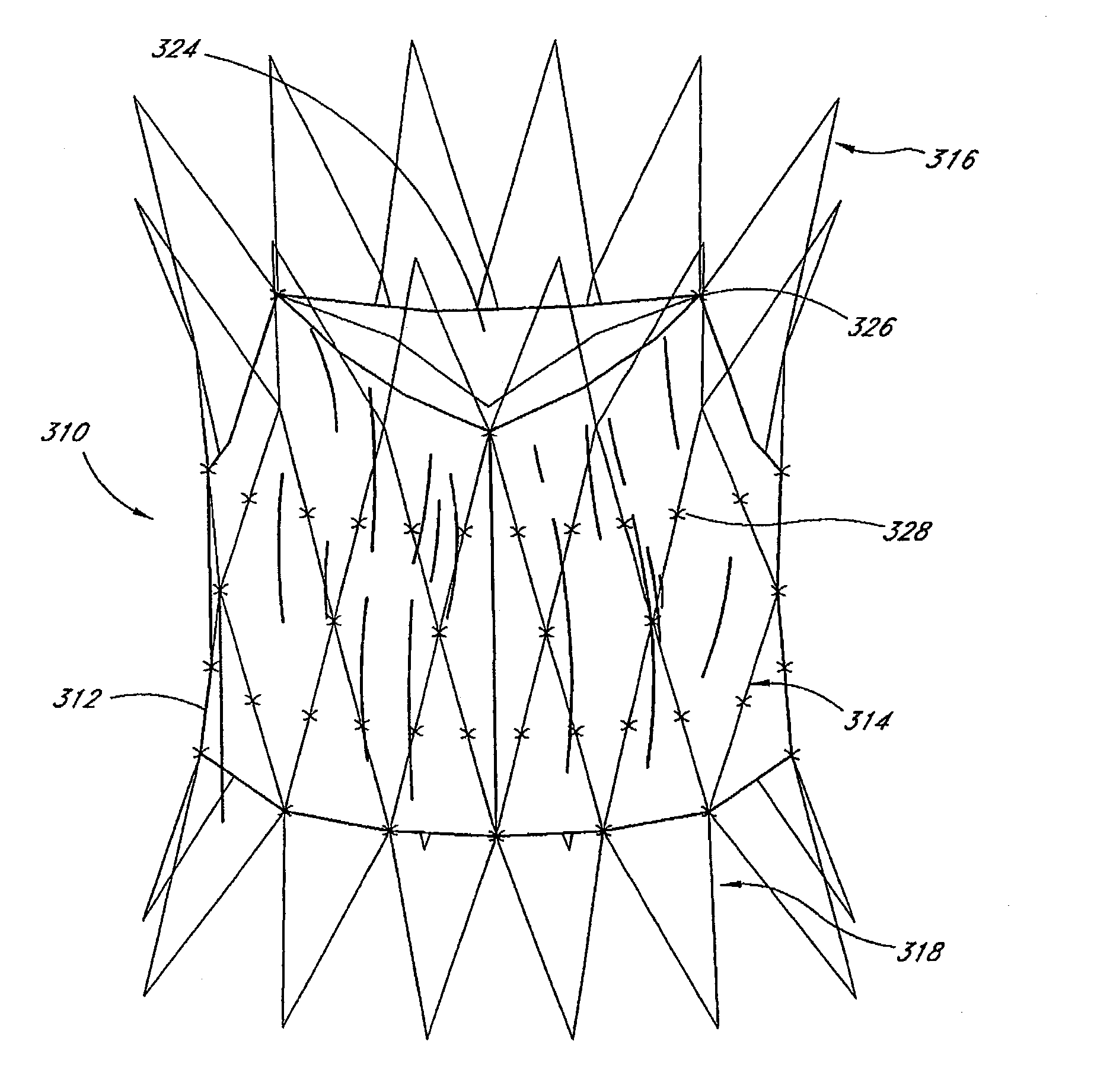
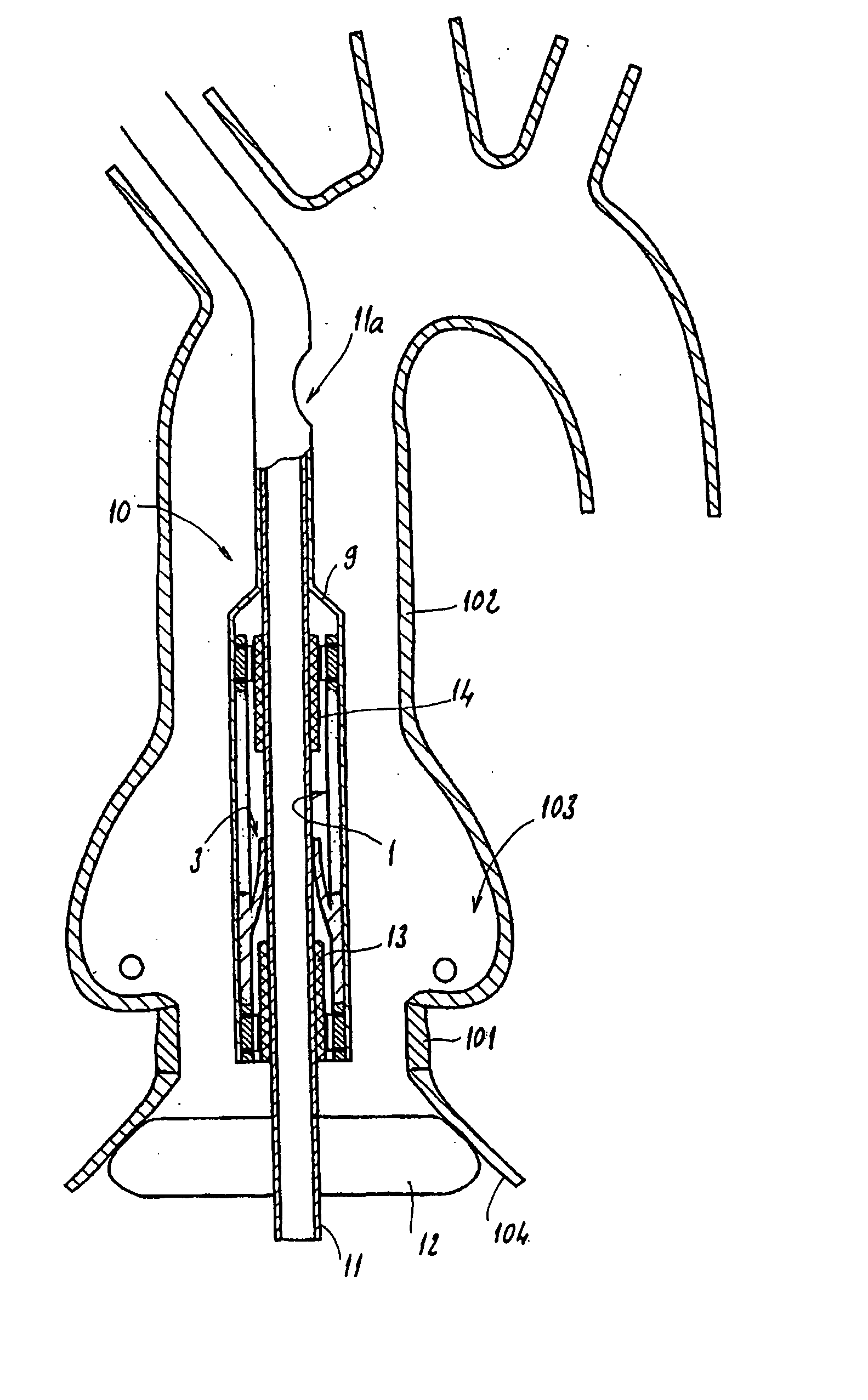
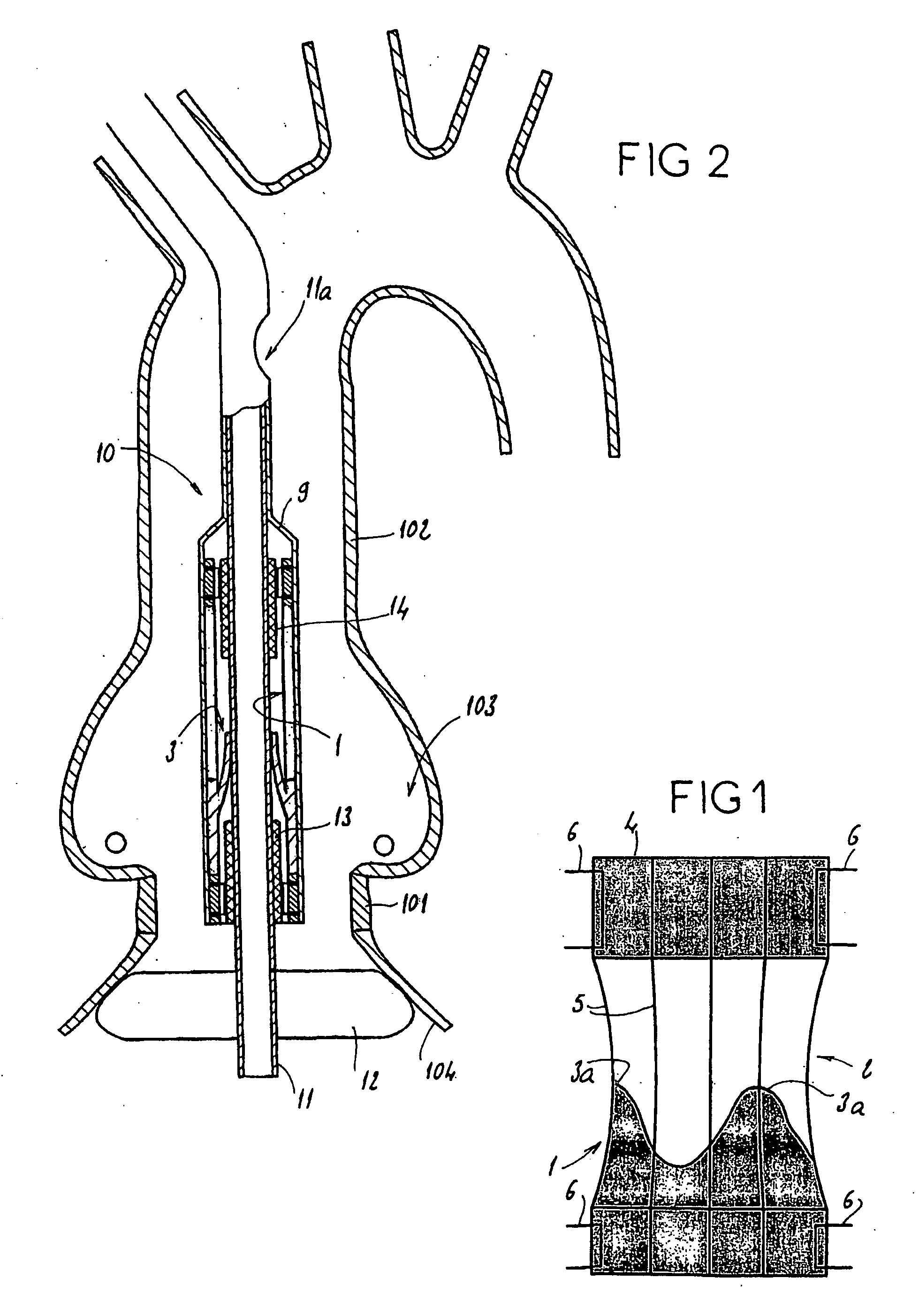
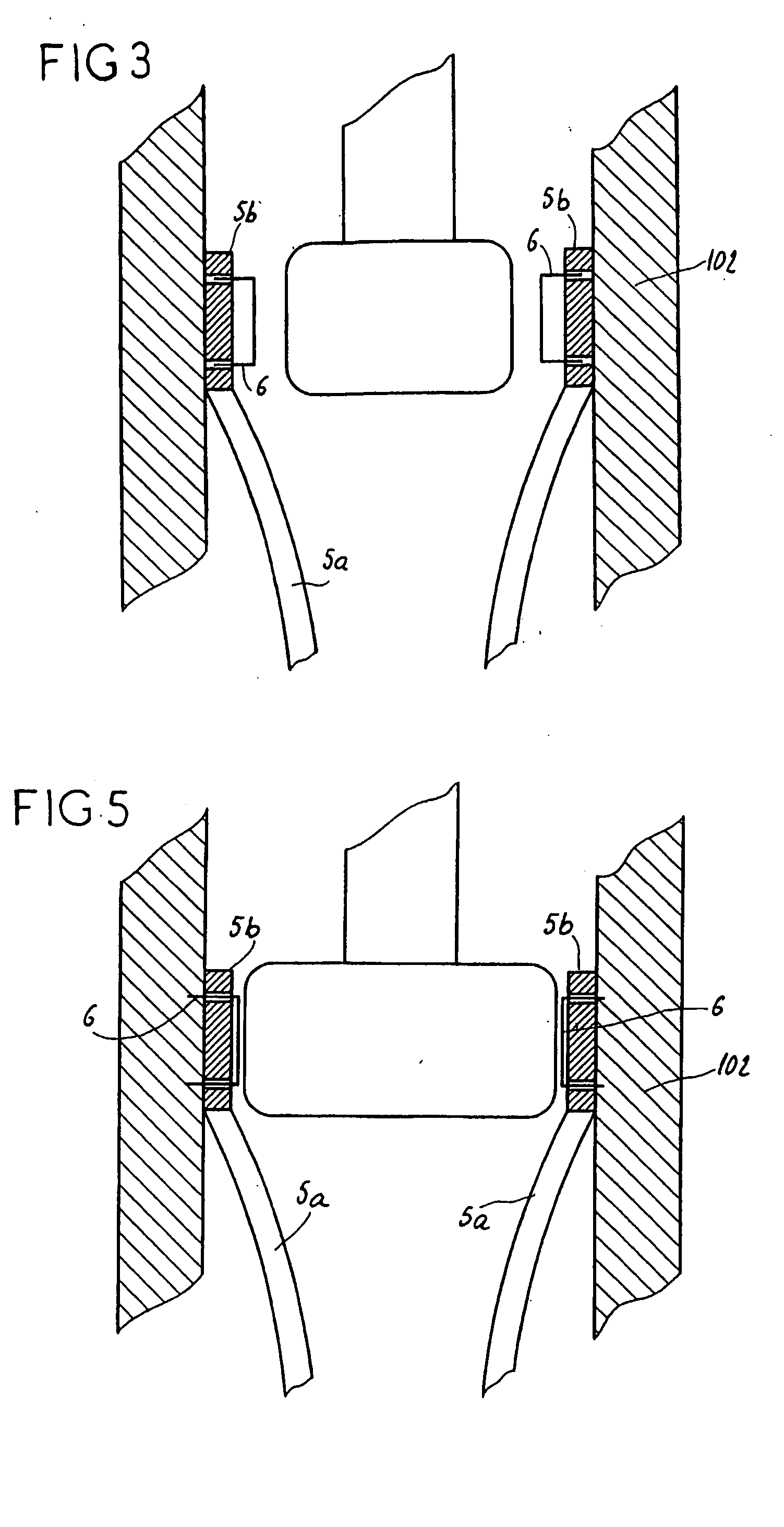
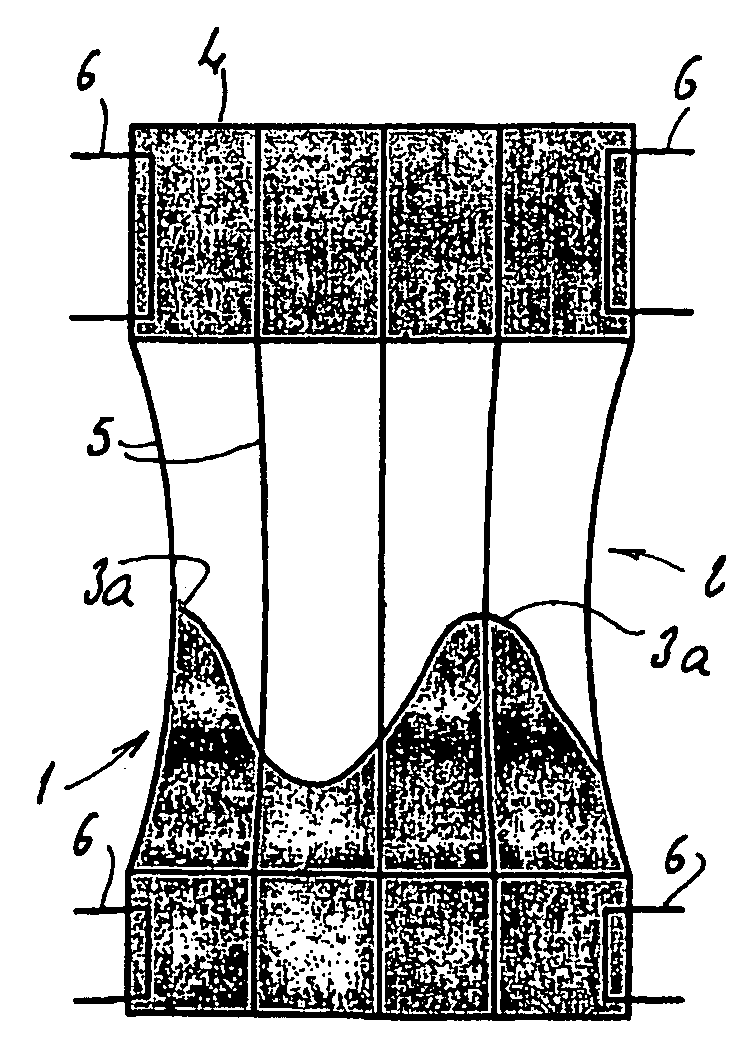
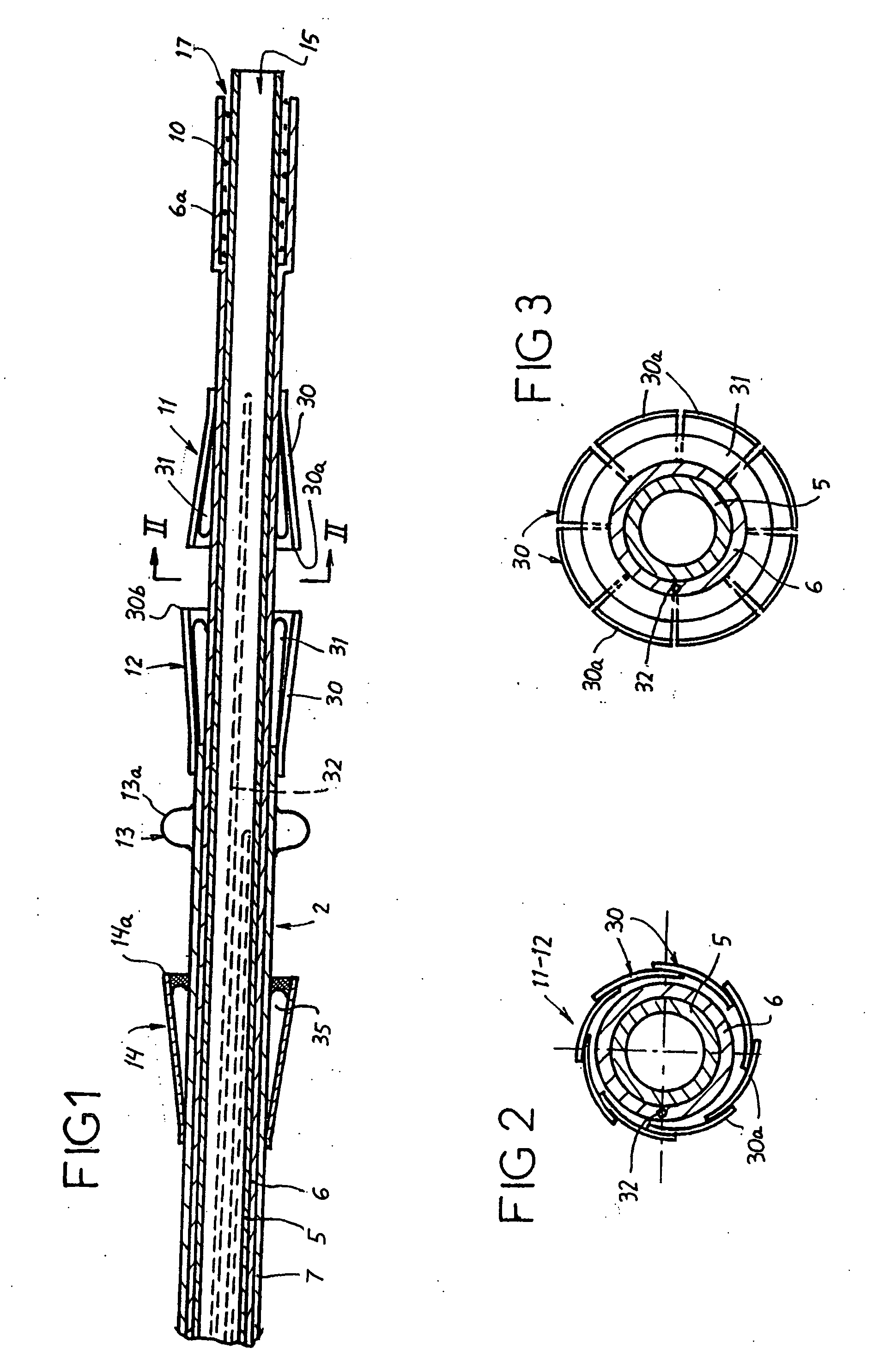
Assembly for setting a valve prosthesis in a corporeal duct
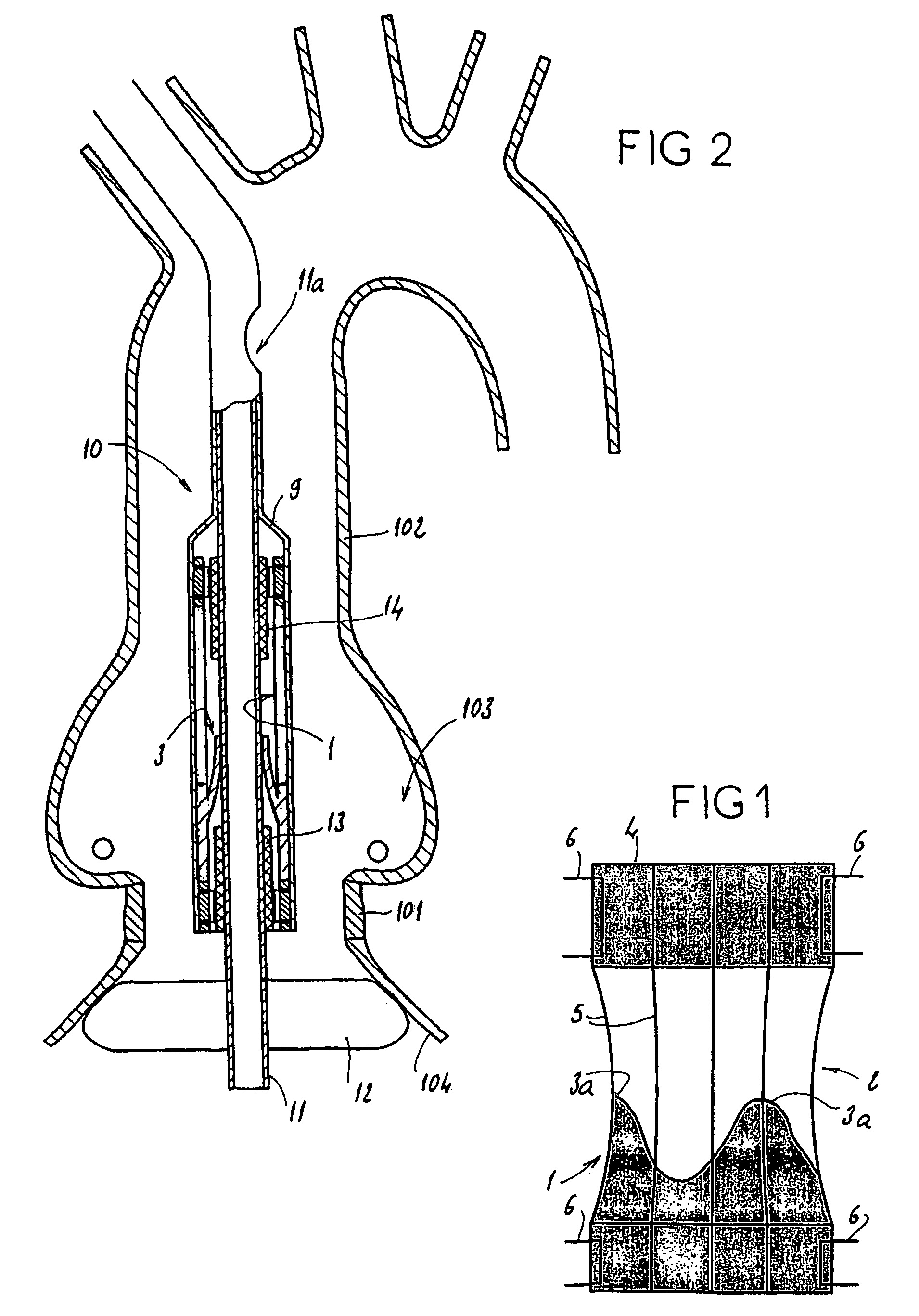
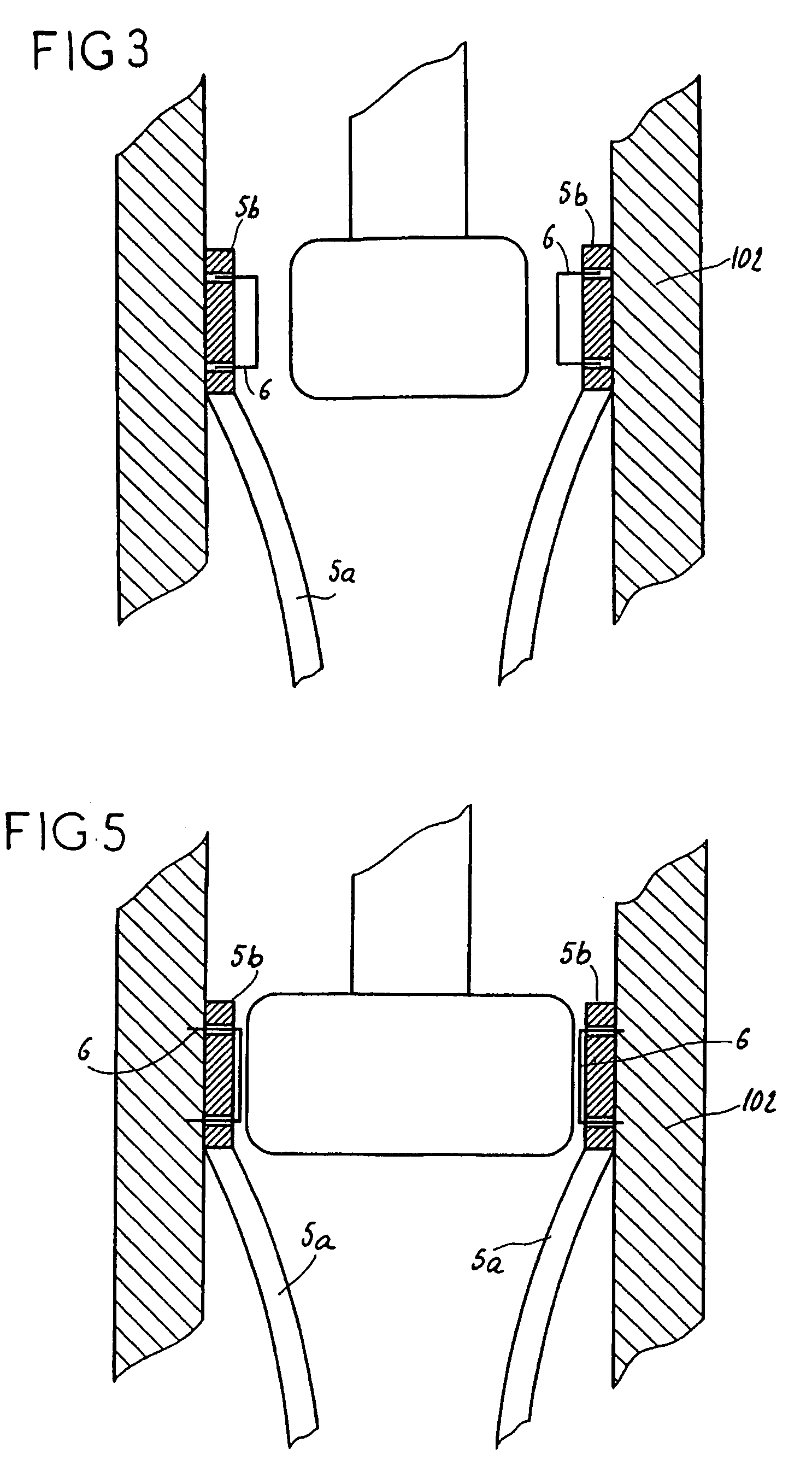
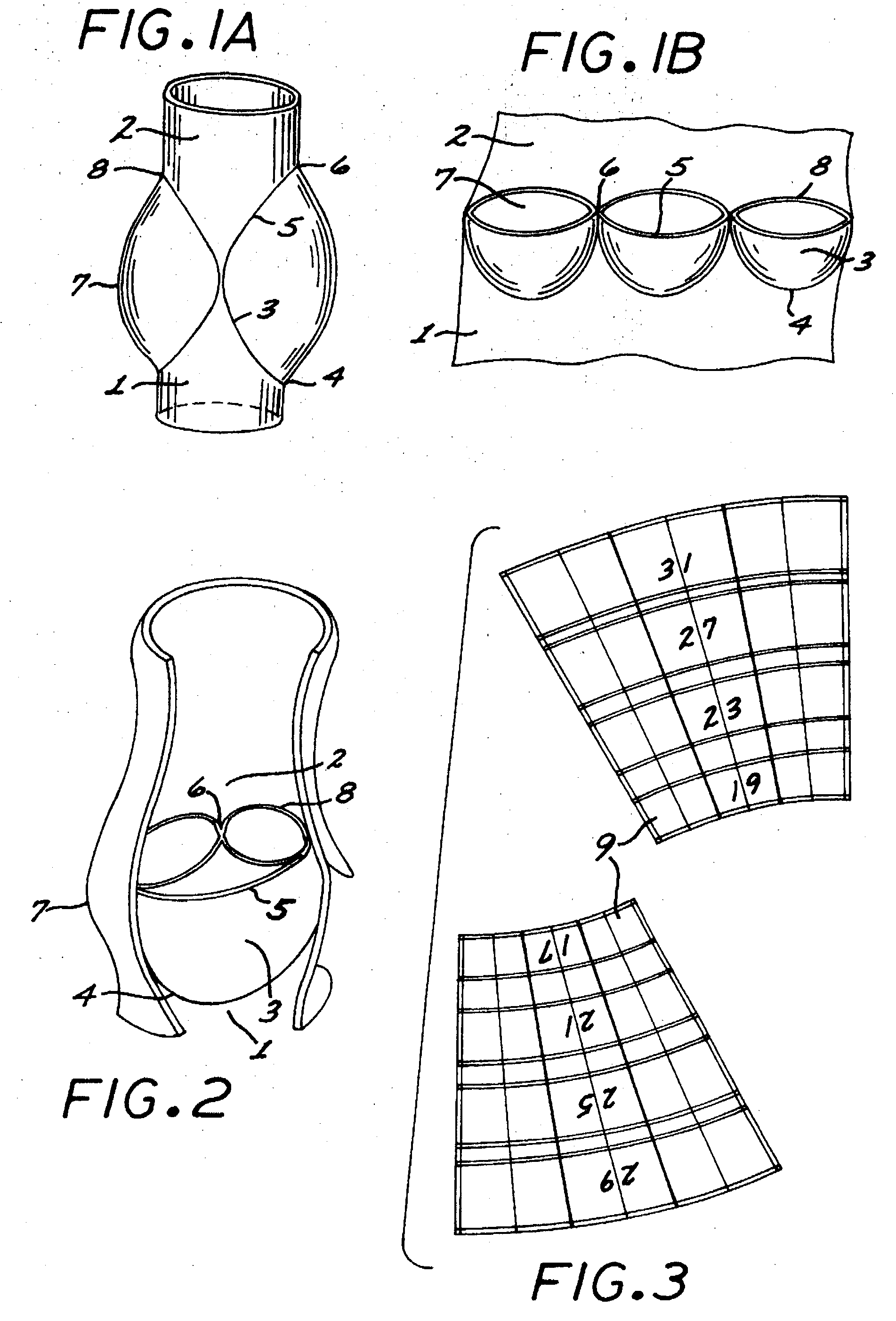
The invention concerns an assembly comprising a valve prosthesis to be implanted and a support receiving said valve. The support comprises: at least a tubular portion made of a pliable material slightly stretchable in the circumferential direction; means for fixing said tubular portion to the wall of the corporeal duct; and a plurality of elongated reinforcing elements, arranged on the circumference of said tubular portion and linked to said tubular portion independently of one another; the valve is linked at least partly to said elongated reinforcing elements, in particular at the commissures of its leaflets, and said elongated reinforcing elements jointly form, in extended position, a structure having a predetermined diameter that ensures sufficient extension of said valve.
Owner:MEDTRONIC COREVALVE
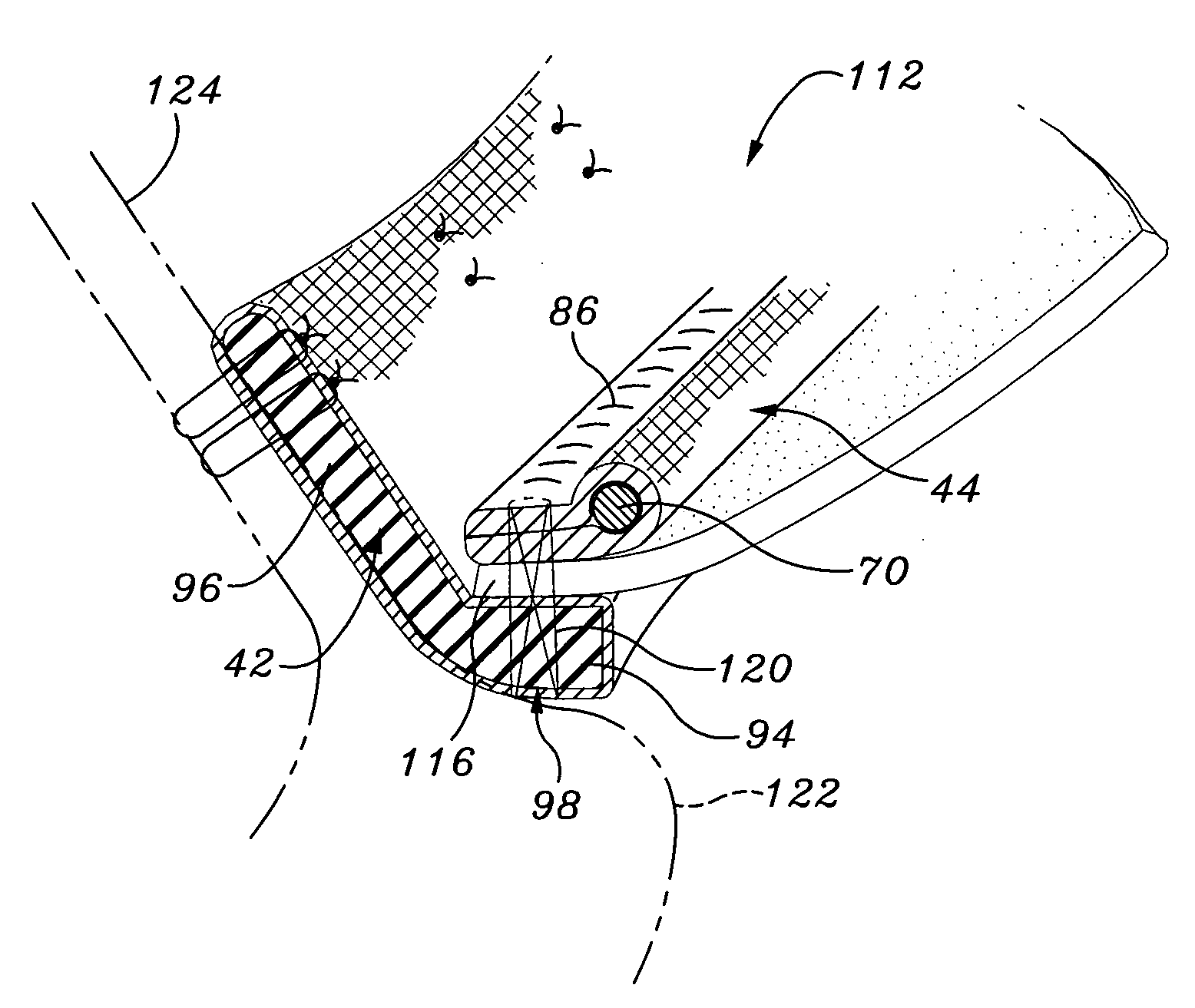
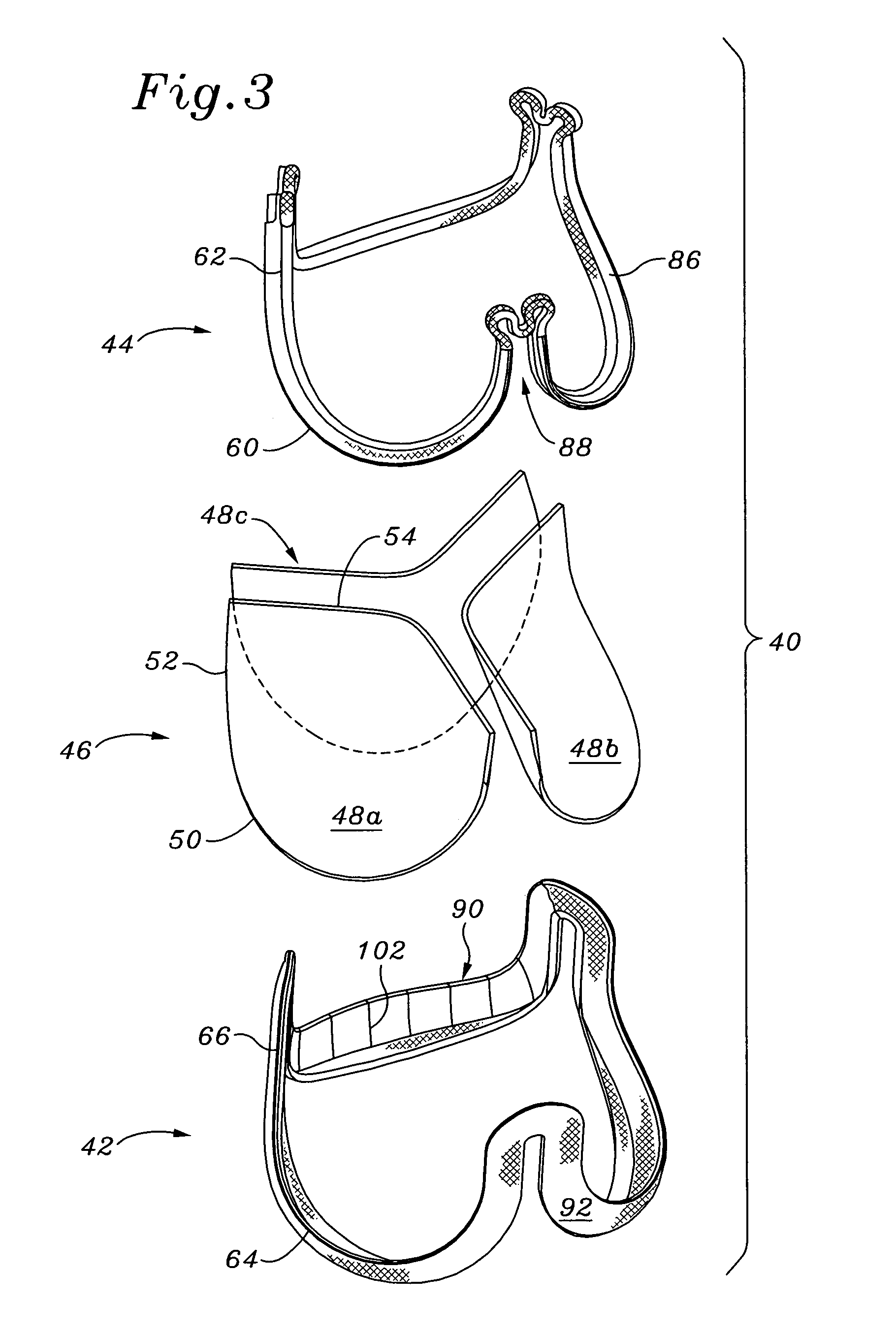
System and method for implanting a two-part prosthetic heart valve
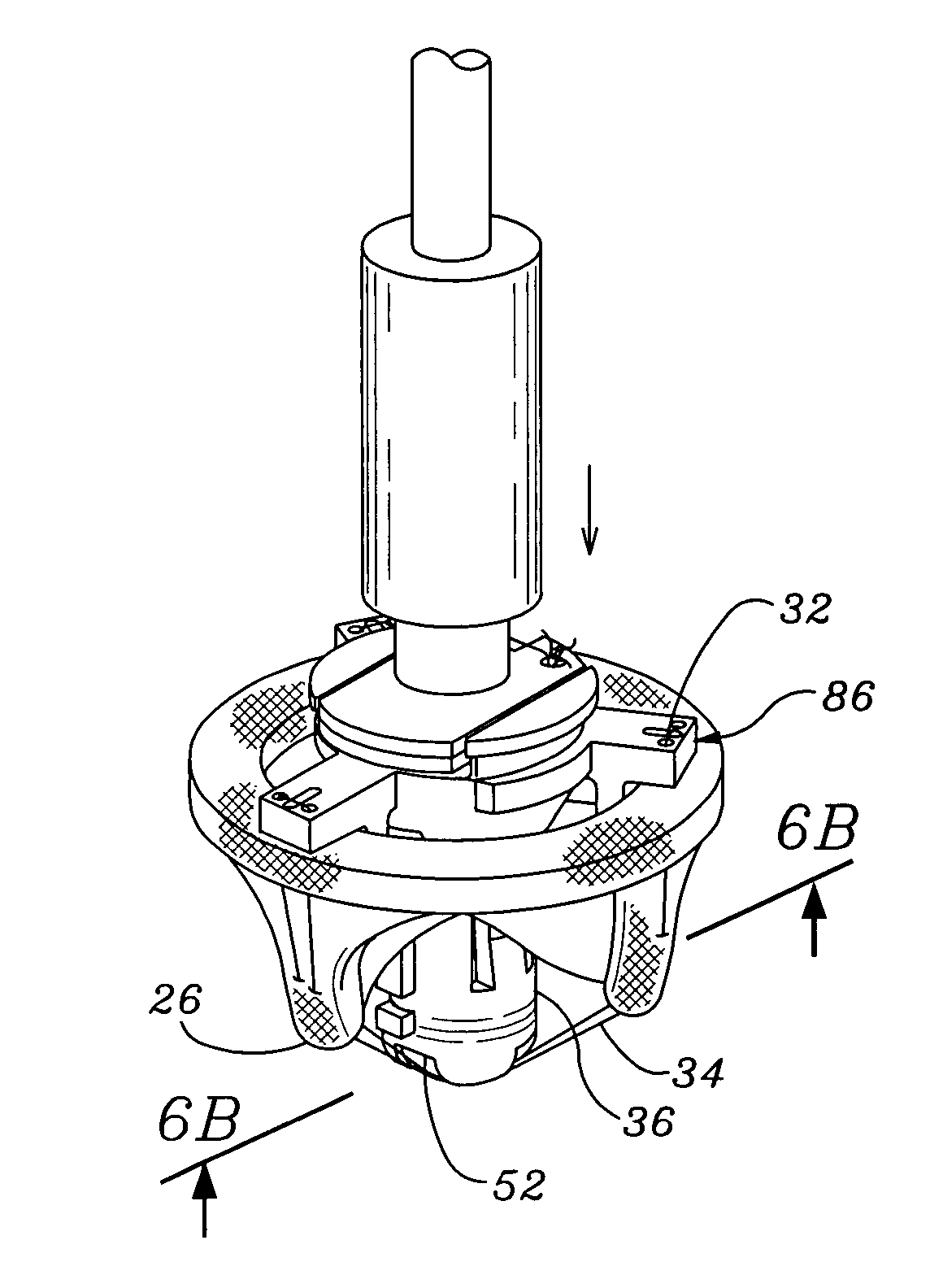
Expandable heart valves for minimally invasive valve replacement surgeries are disclosed. In a first embodiment, an expandable pre-assembled heart valve includes a plastically-expandable annular base having plurality of upstanding commissure posts. A tubular flexible member including a prosthetic section and a fabric section is provided, with the prosthetic section being connected to the commissure posts and defining leaflets therebetween, and the fabric section being attached to the annular base. In a second embodiment, an expandable heart valve includes an annular tissue-engaging base and a subassembly having an elastic wireform and a plurality of leaflets connected thereto. The annular base and subassembly are separately stored and connected just prior to delivery to the host annulus. Preferably, the leaflet subassembly is stored in its relaxed configuration to avoid deformation of the leaflets. The expandable heart valves maybe implanted using a balloon catheter. Preferably, the leaflets of the heart valves are secured to the commissure regions of the expandable stents using a clamping arrangement to reduce stress.
Owner:EDWARDS LIFESCIENCES CORP
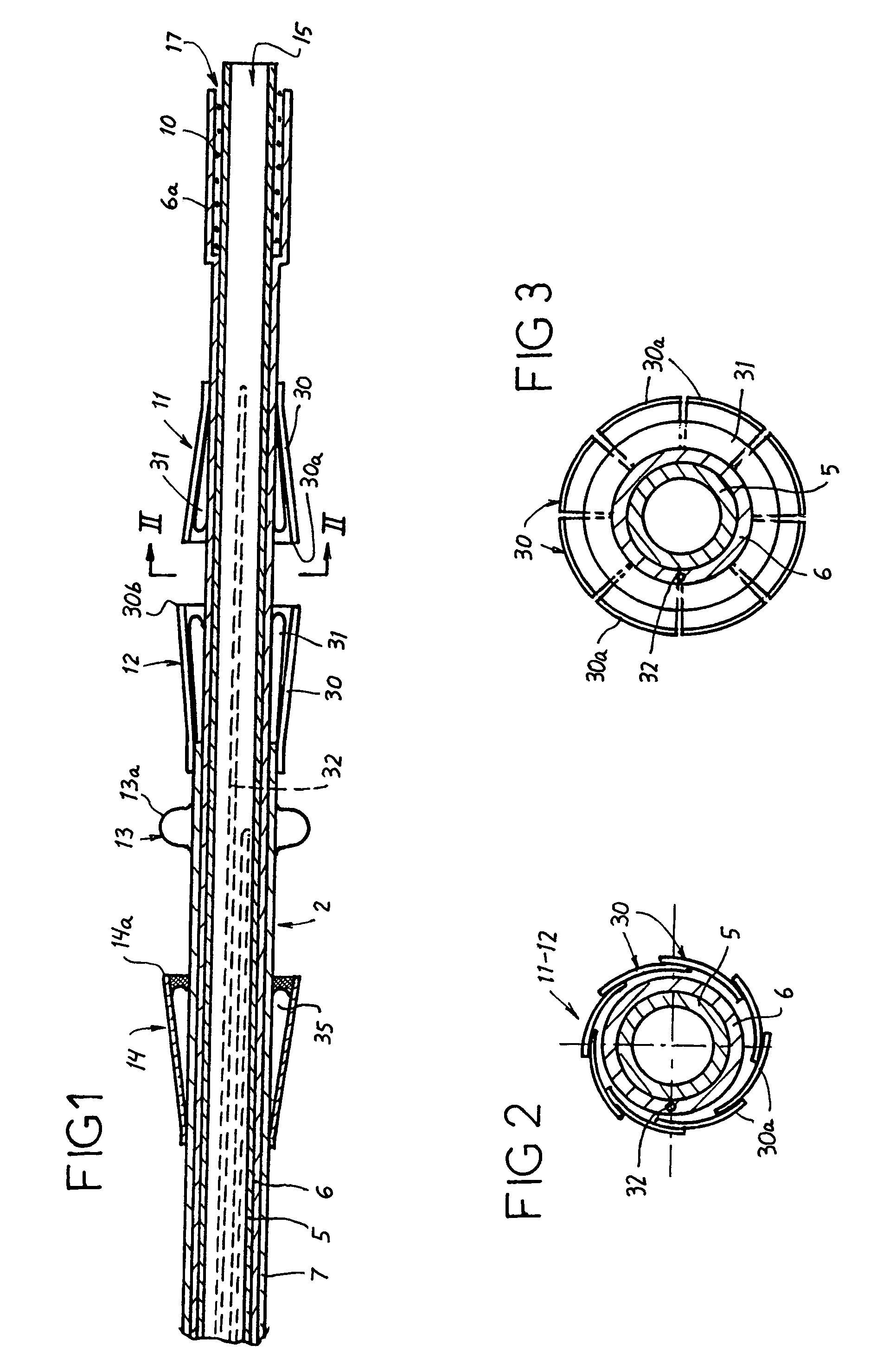
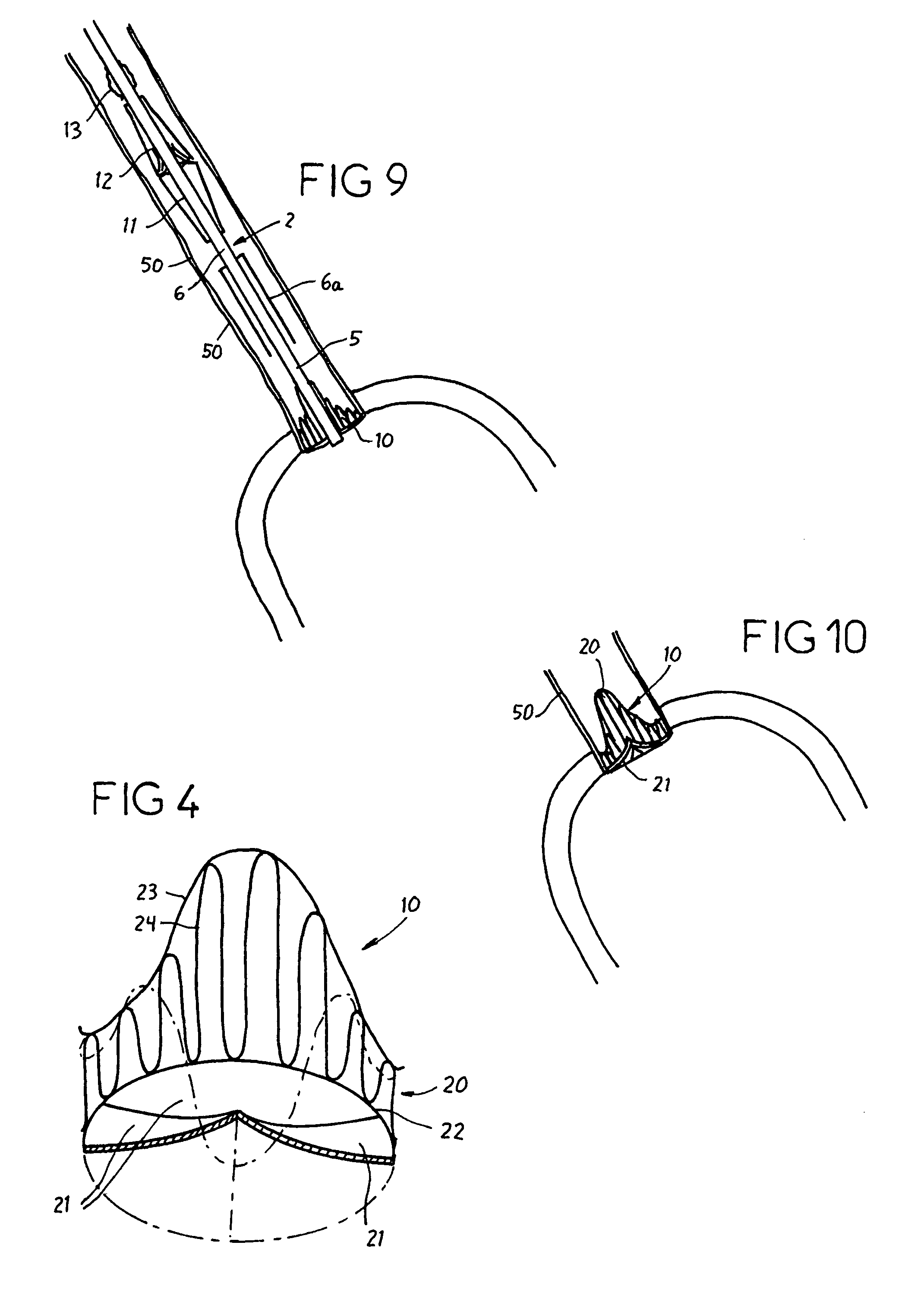
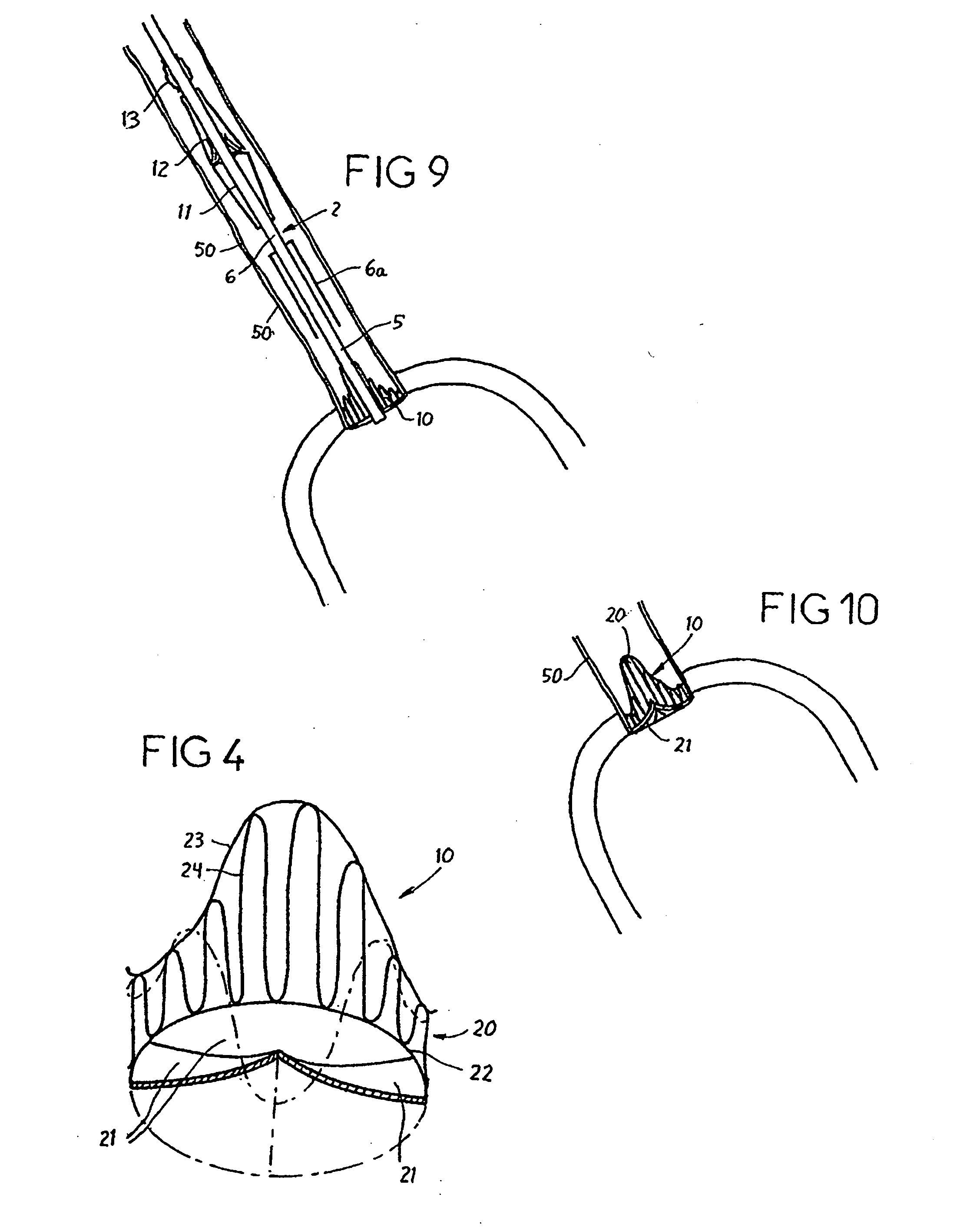
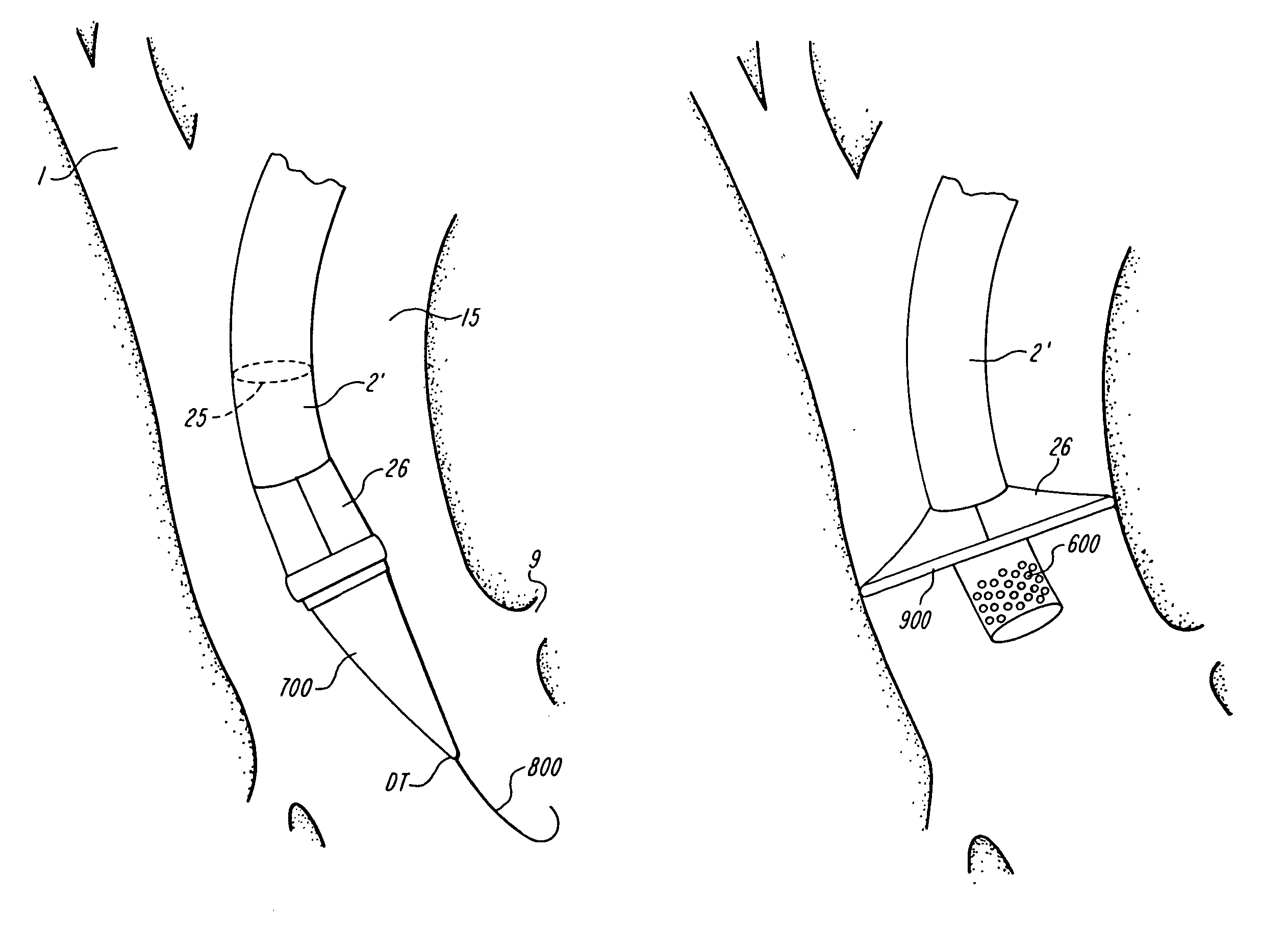
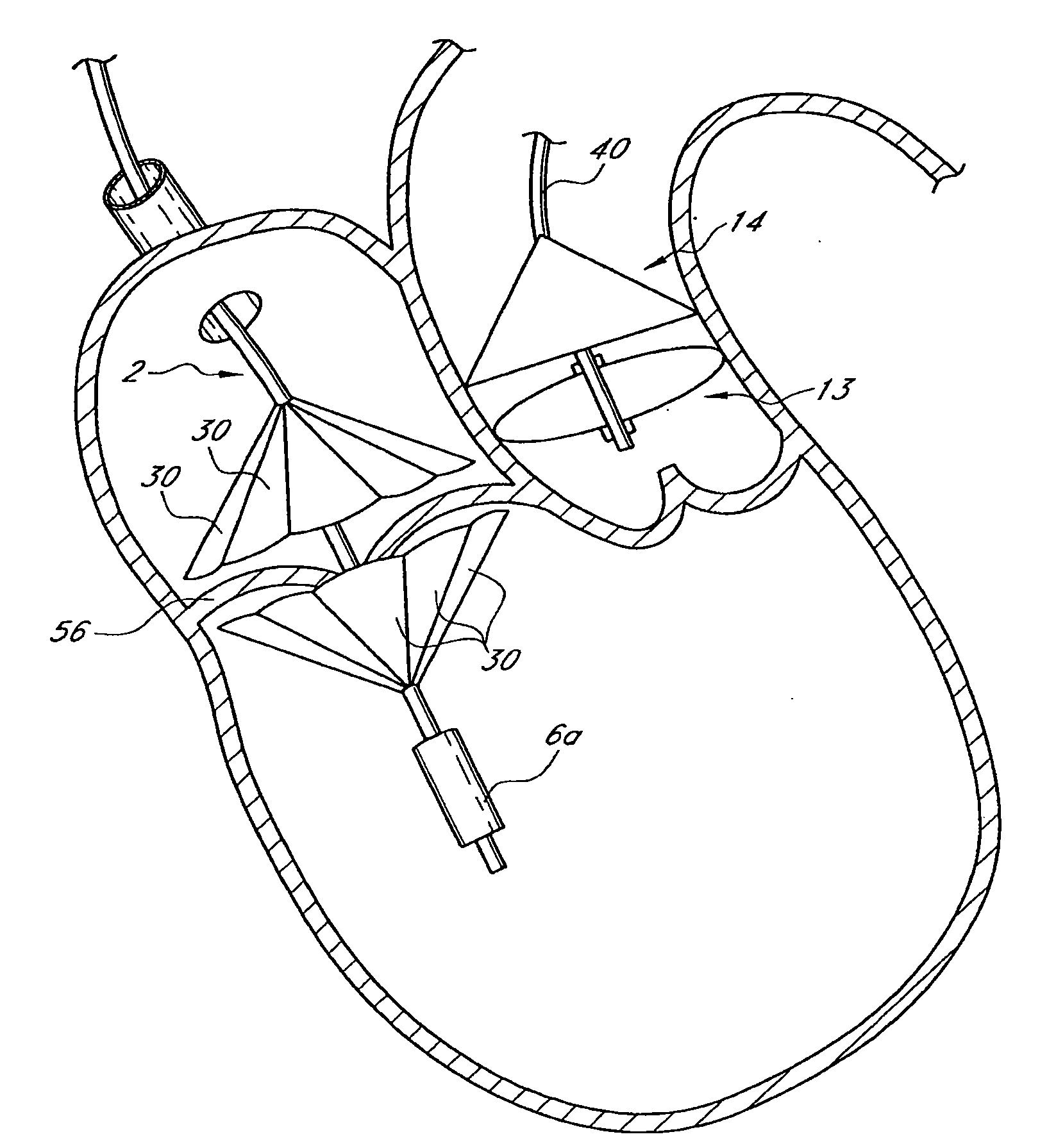
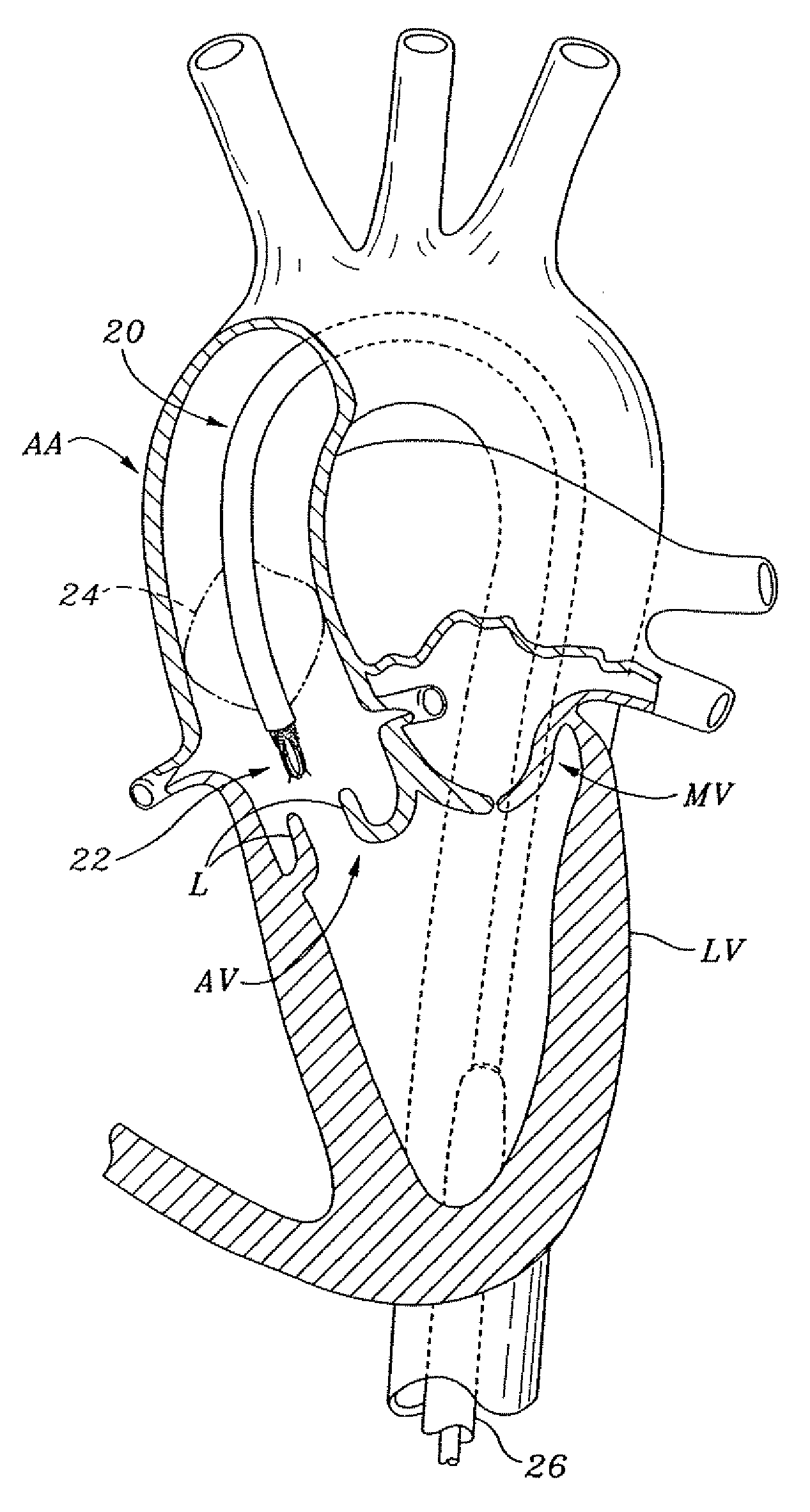
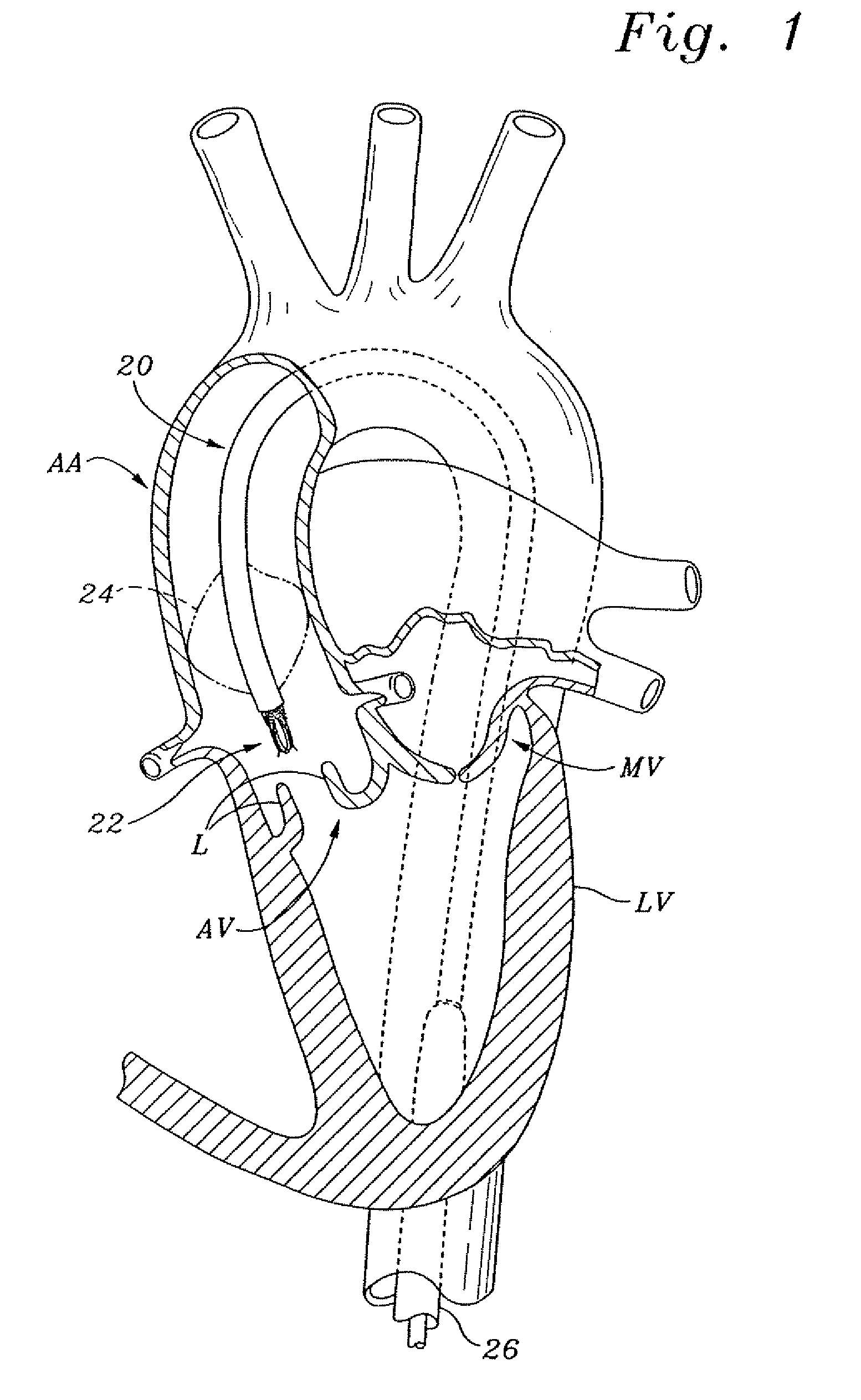
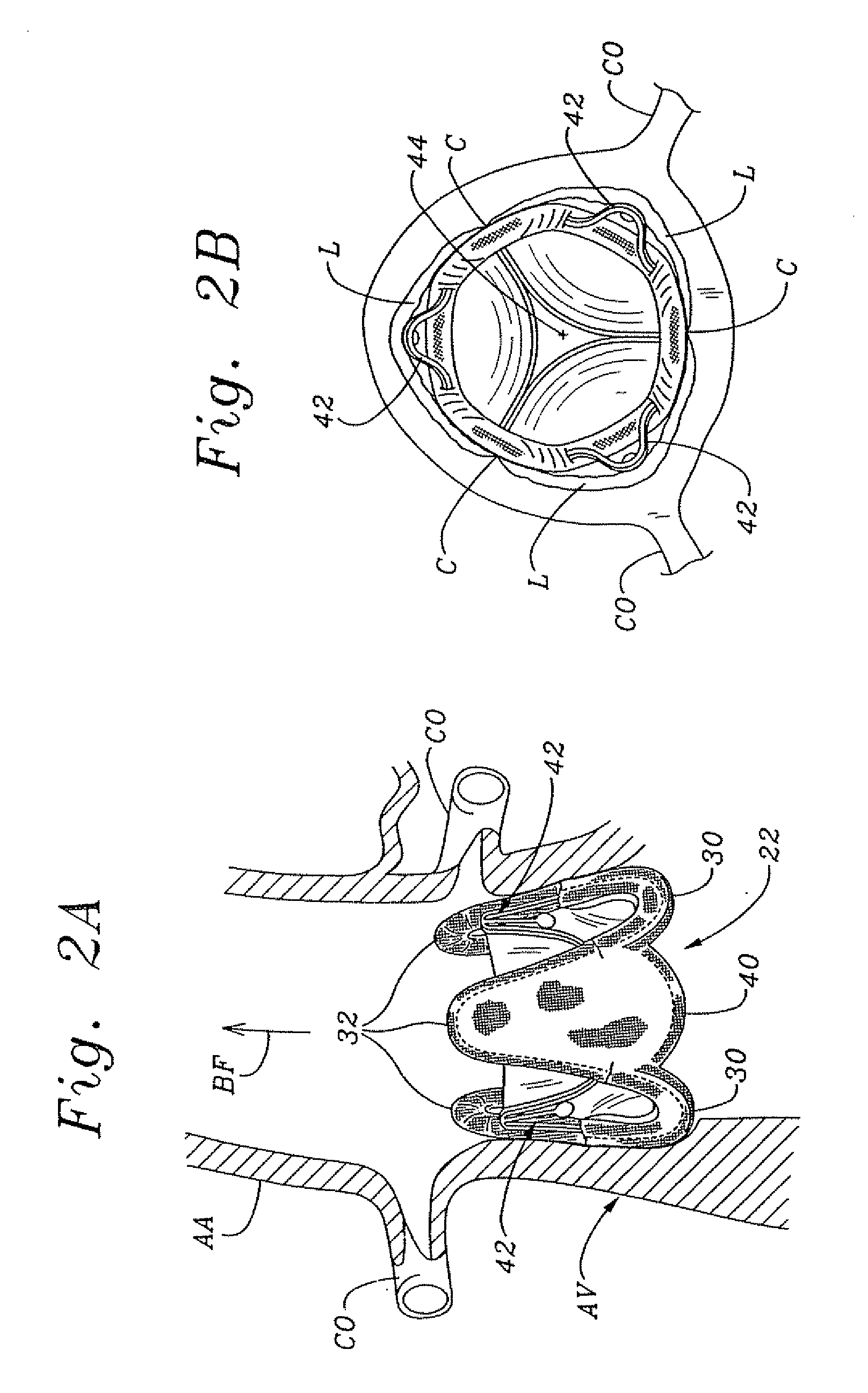
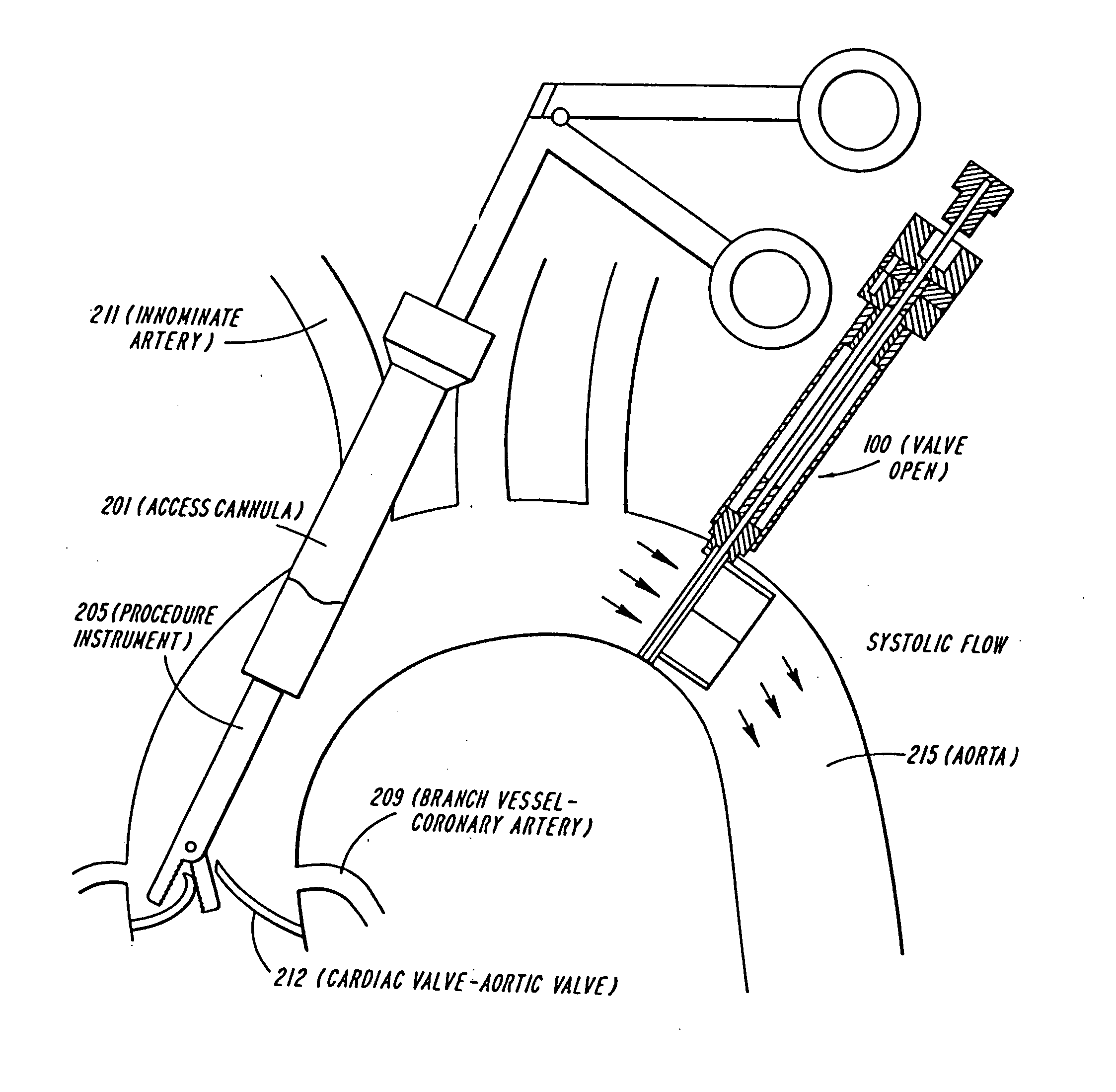
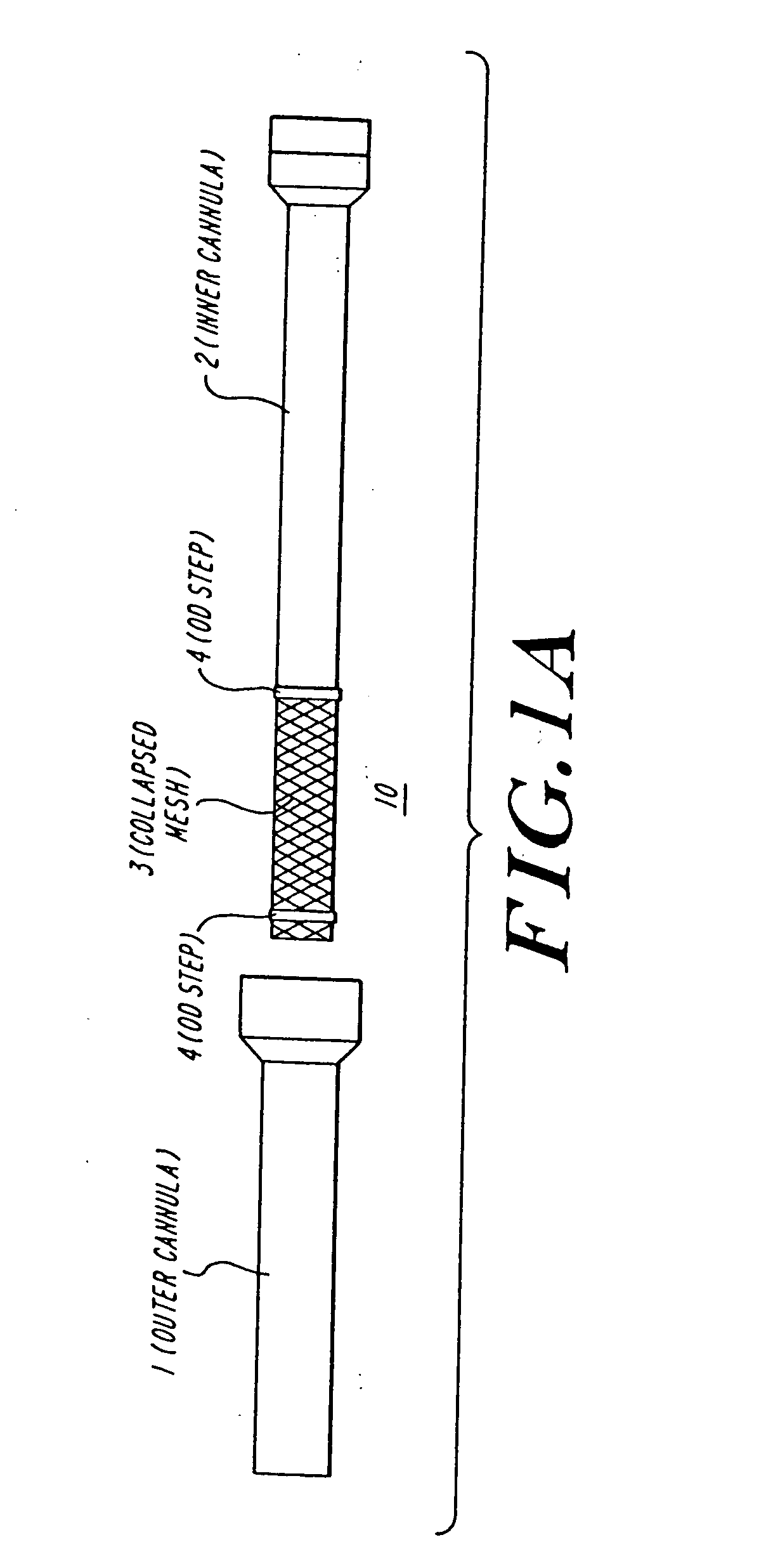
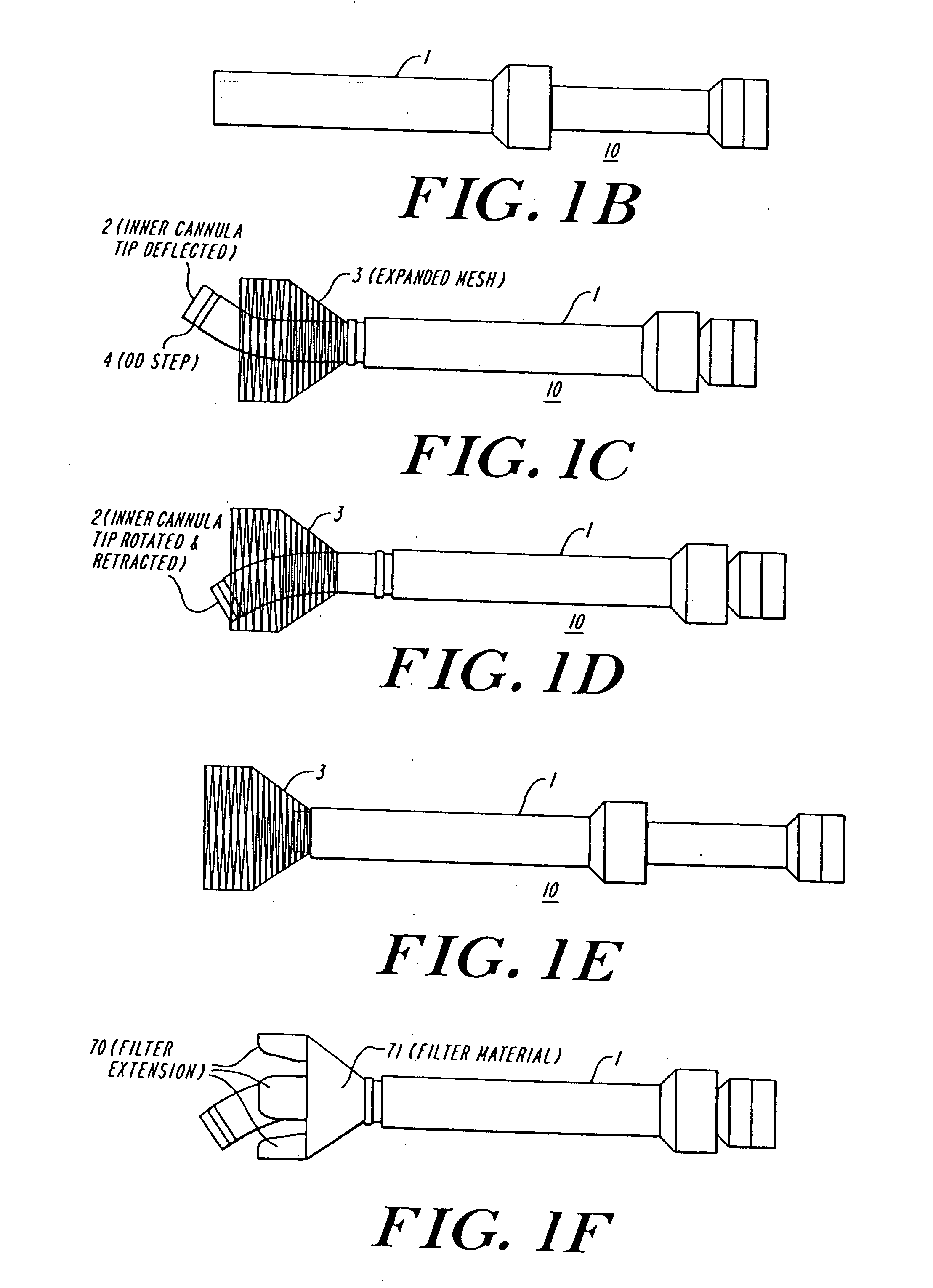
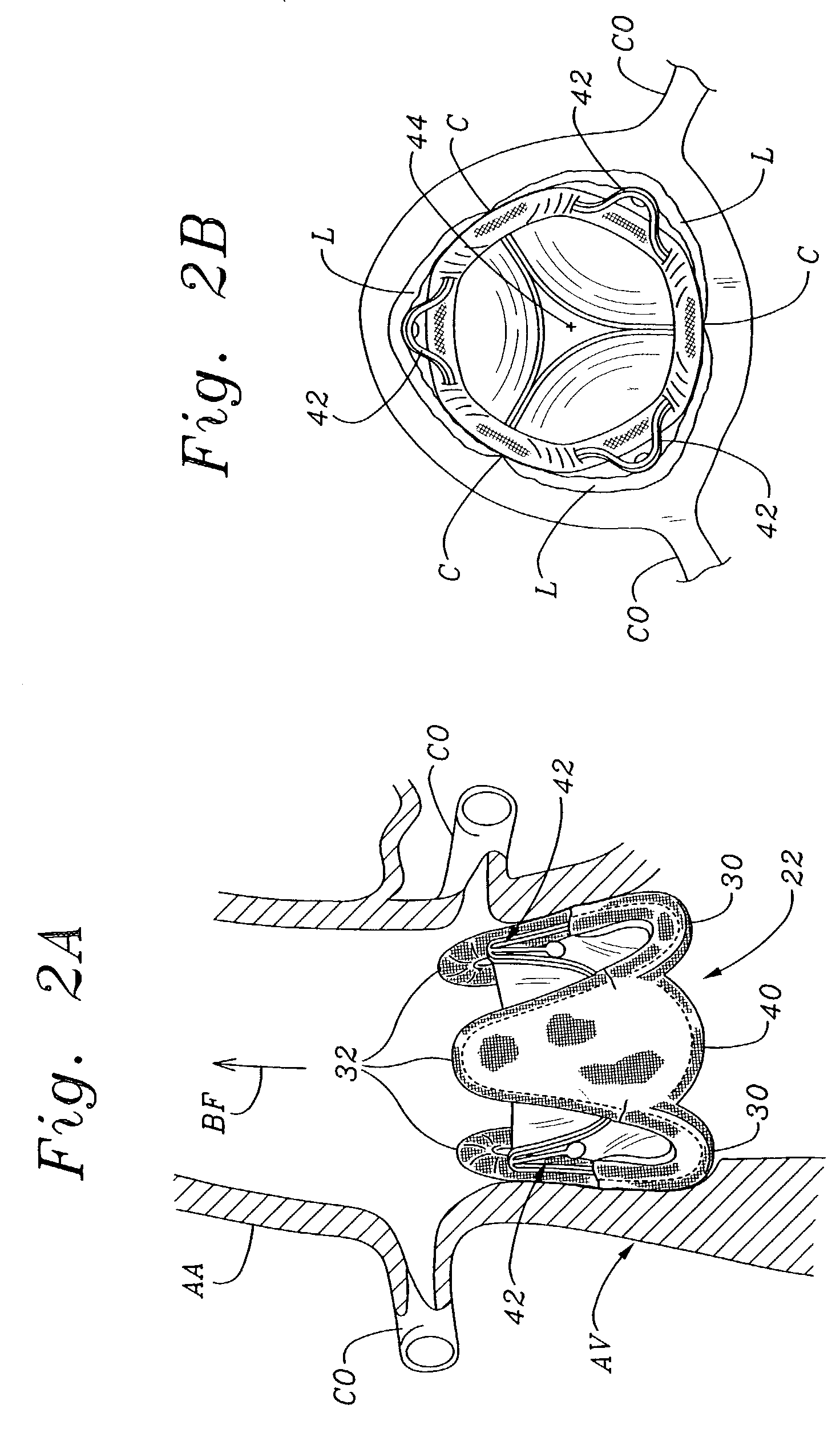
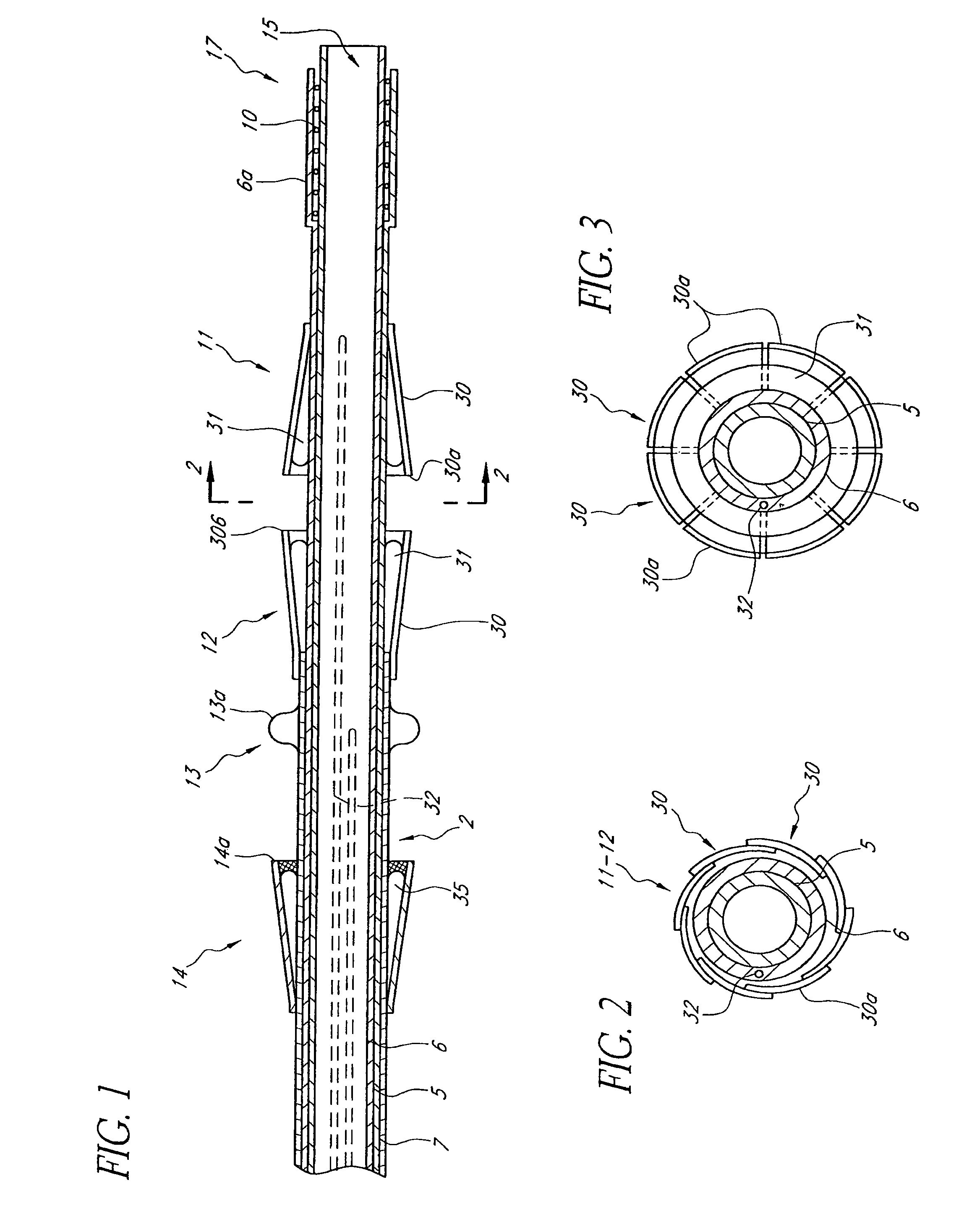
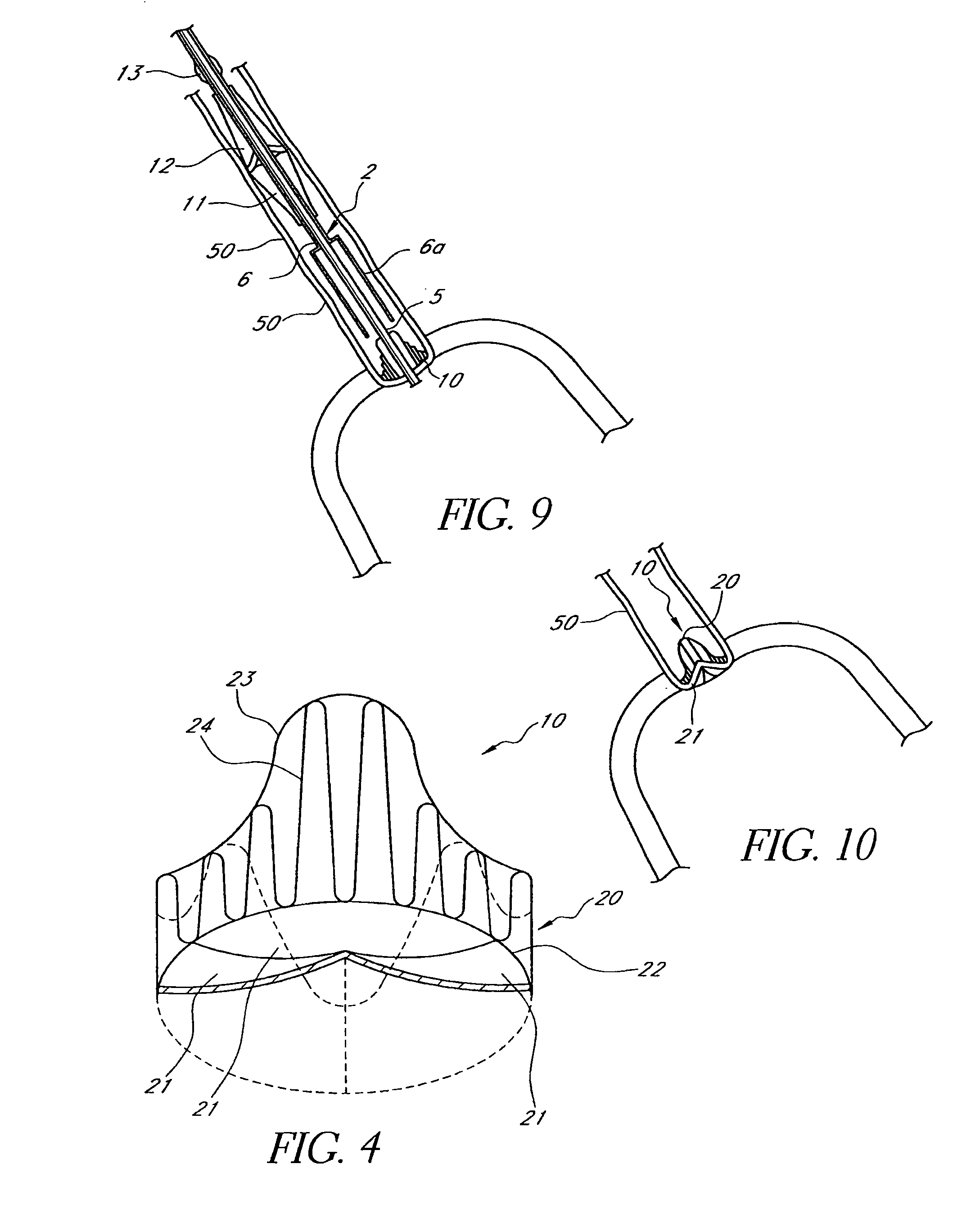
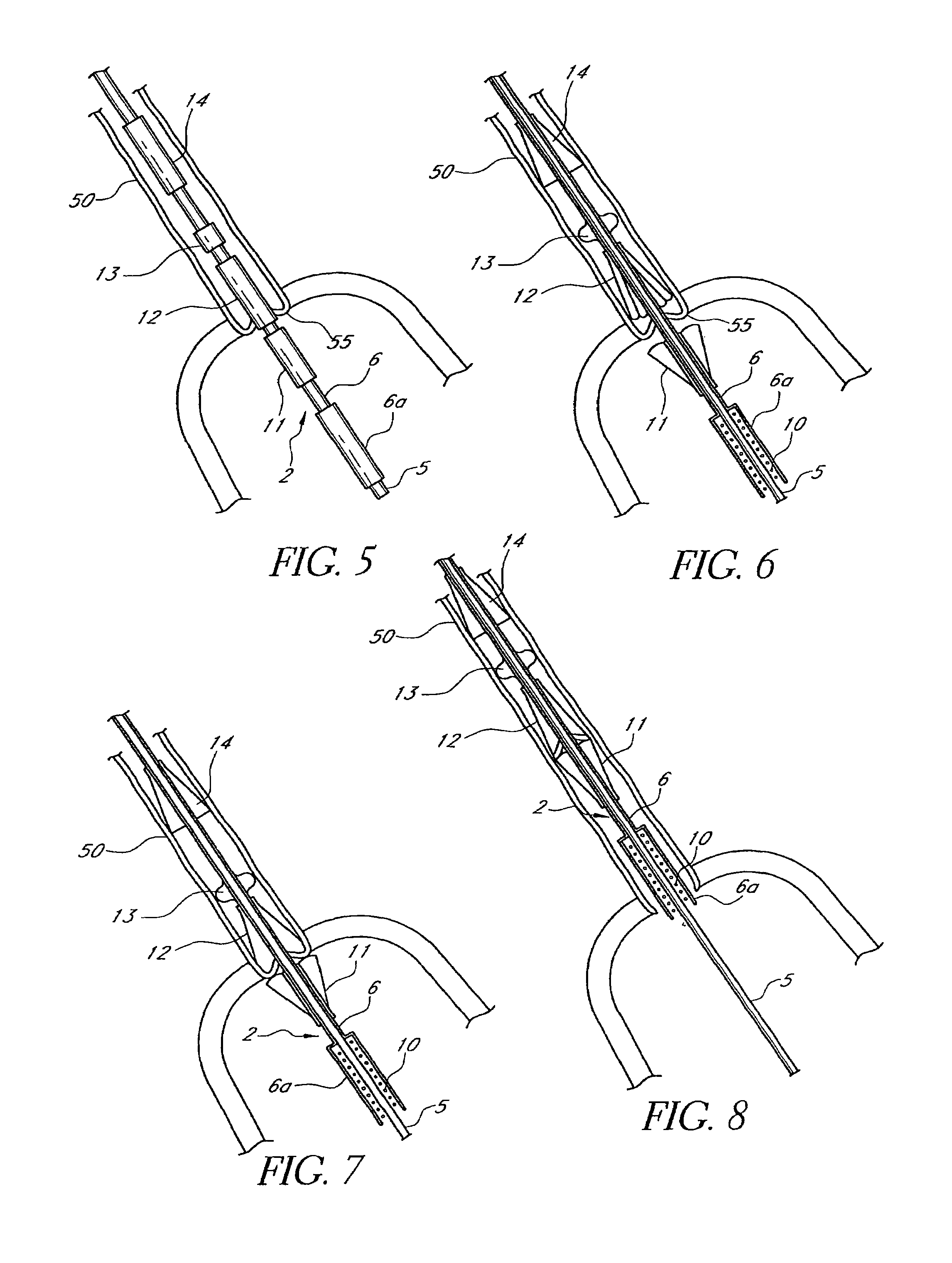
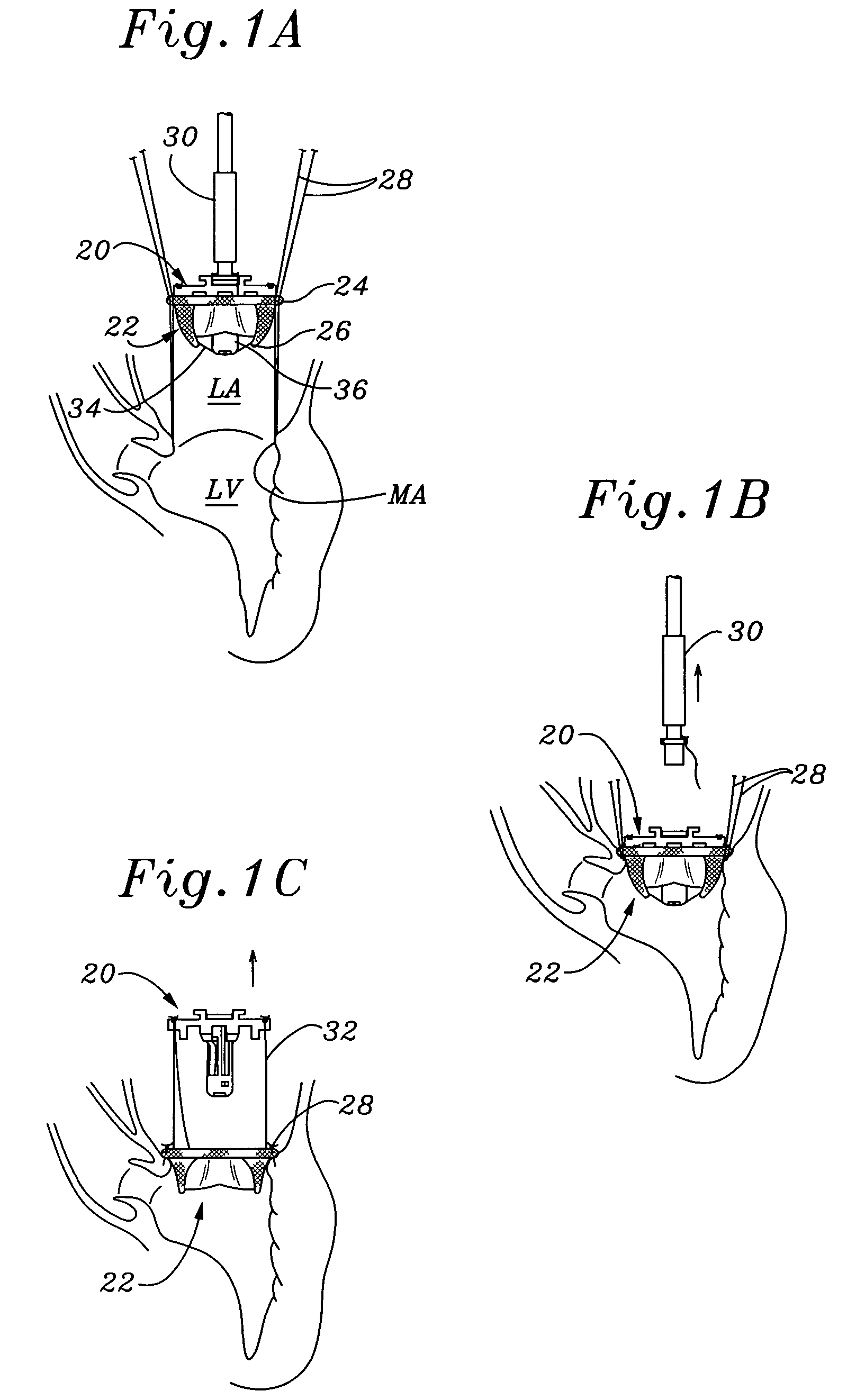
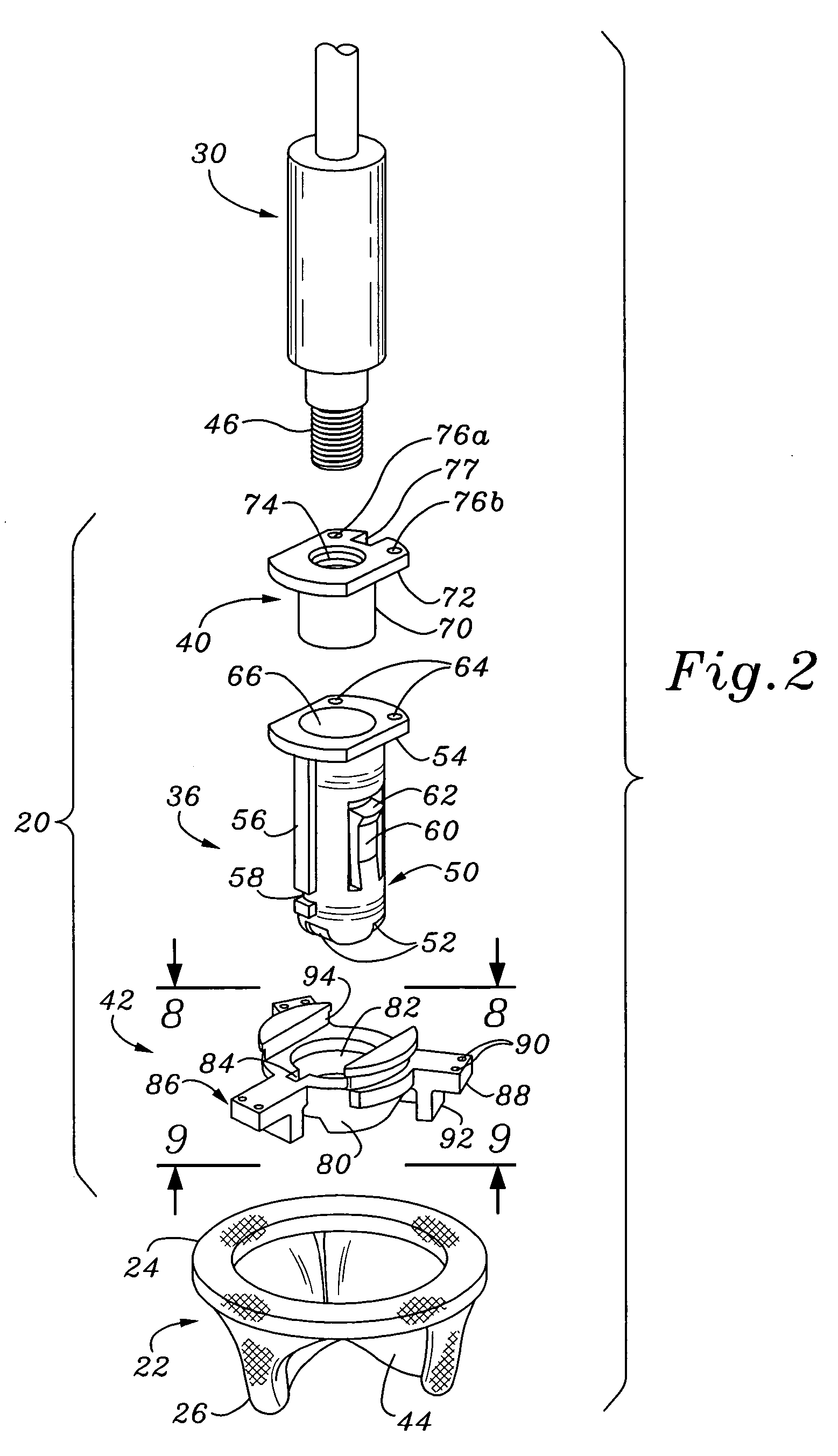
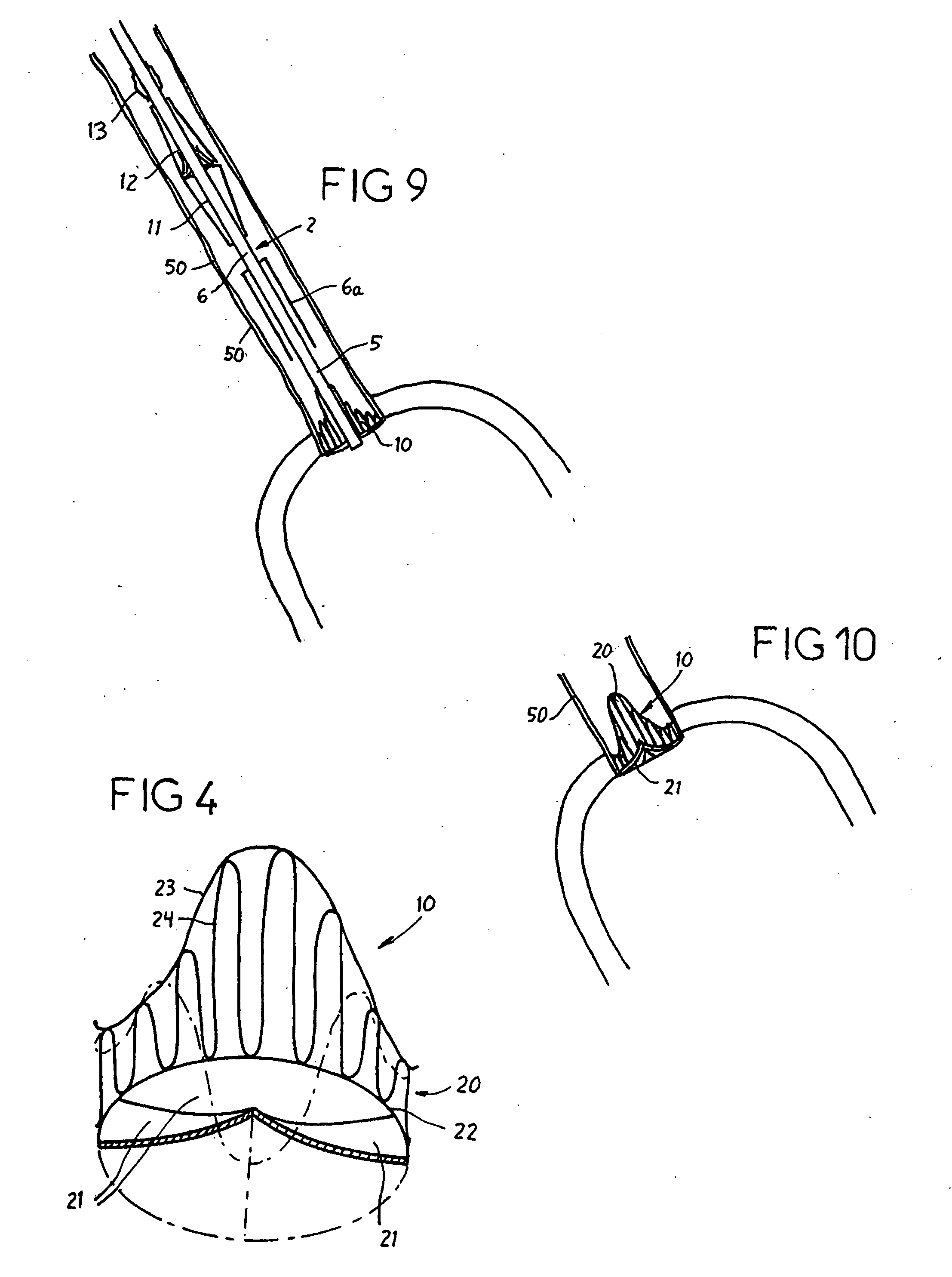
Cardiac valve procedure methods and devices
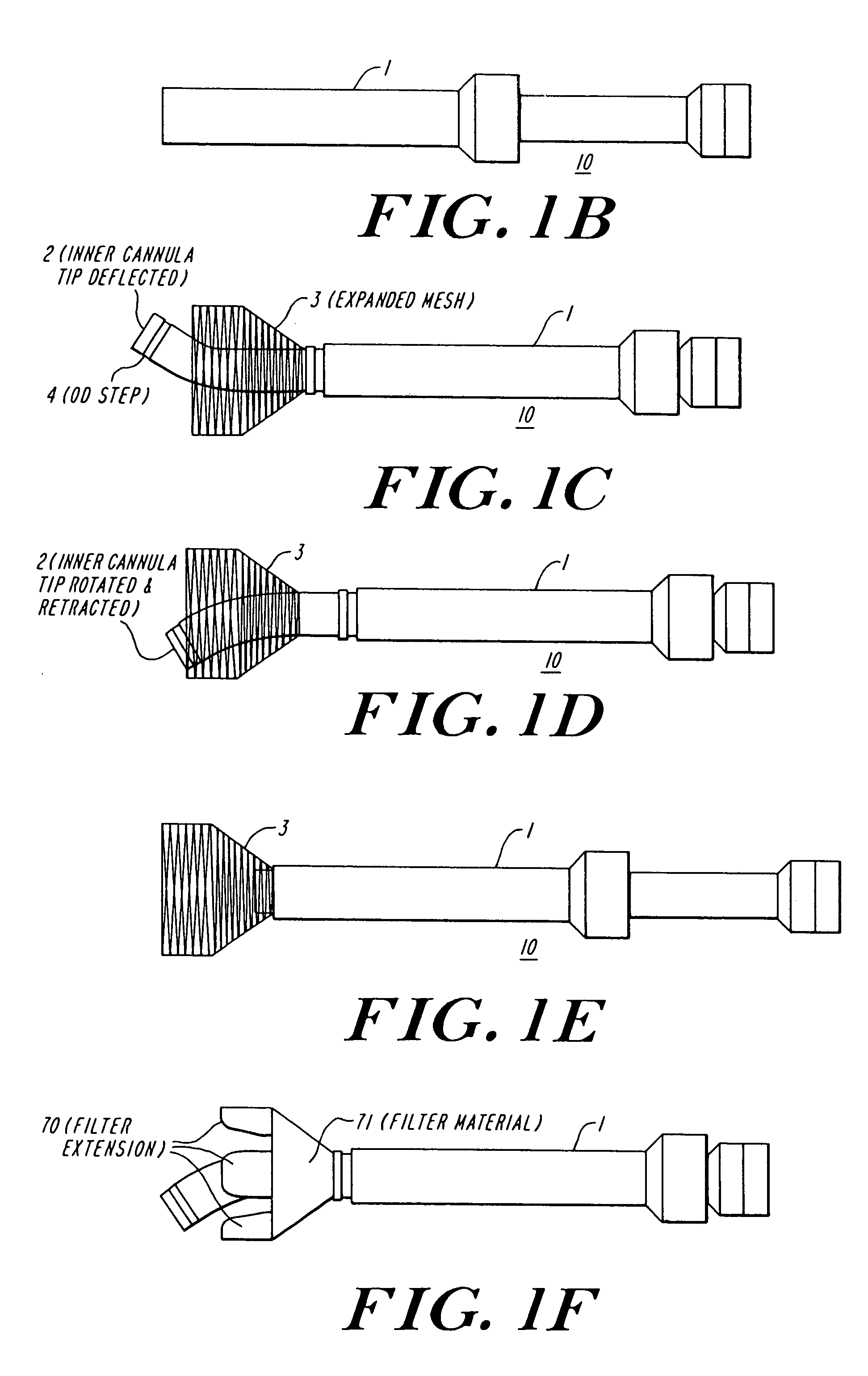
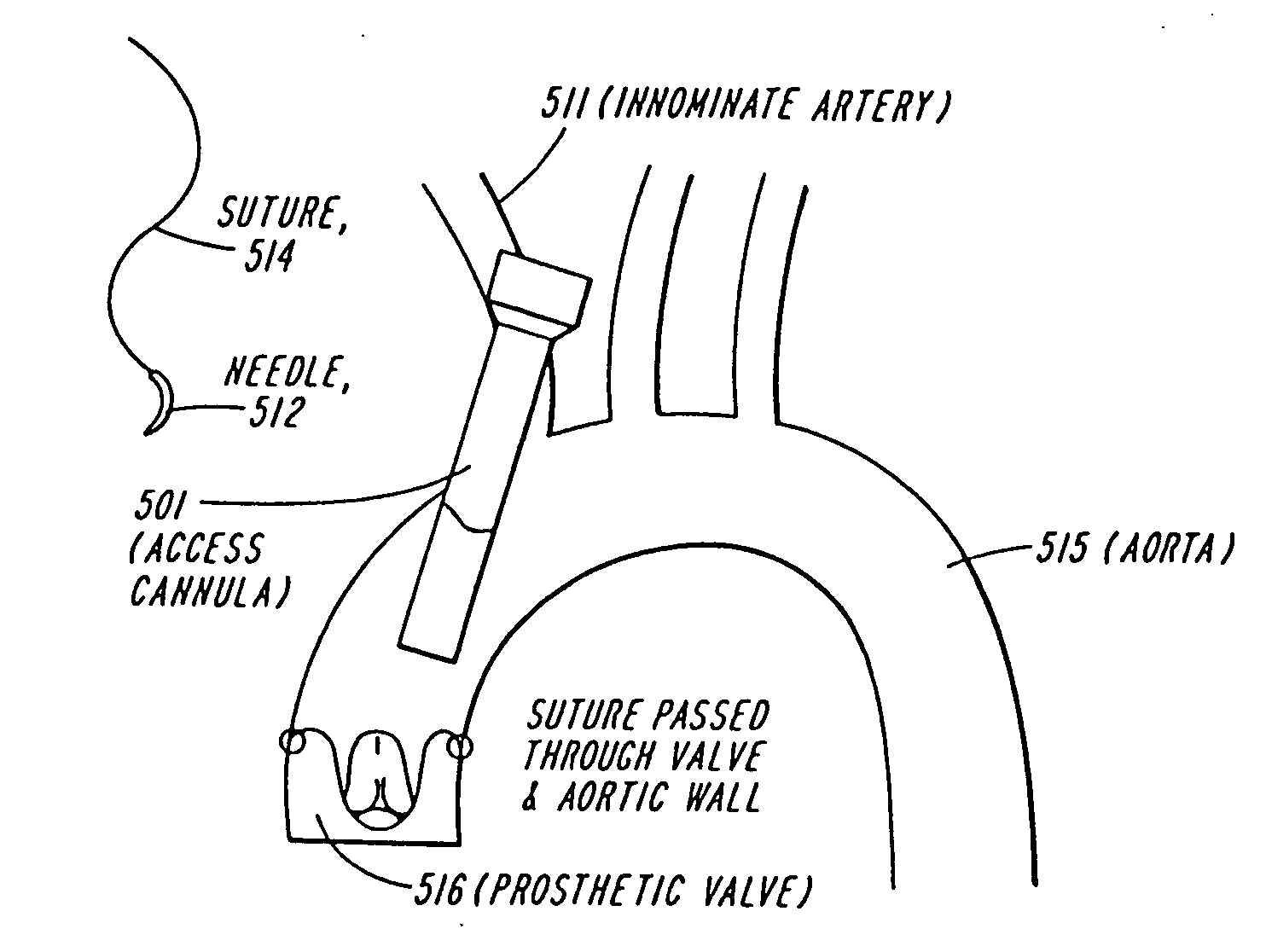
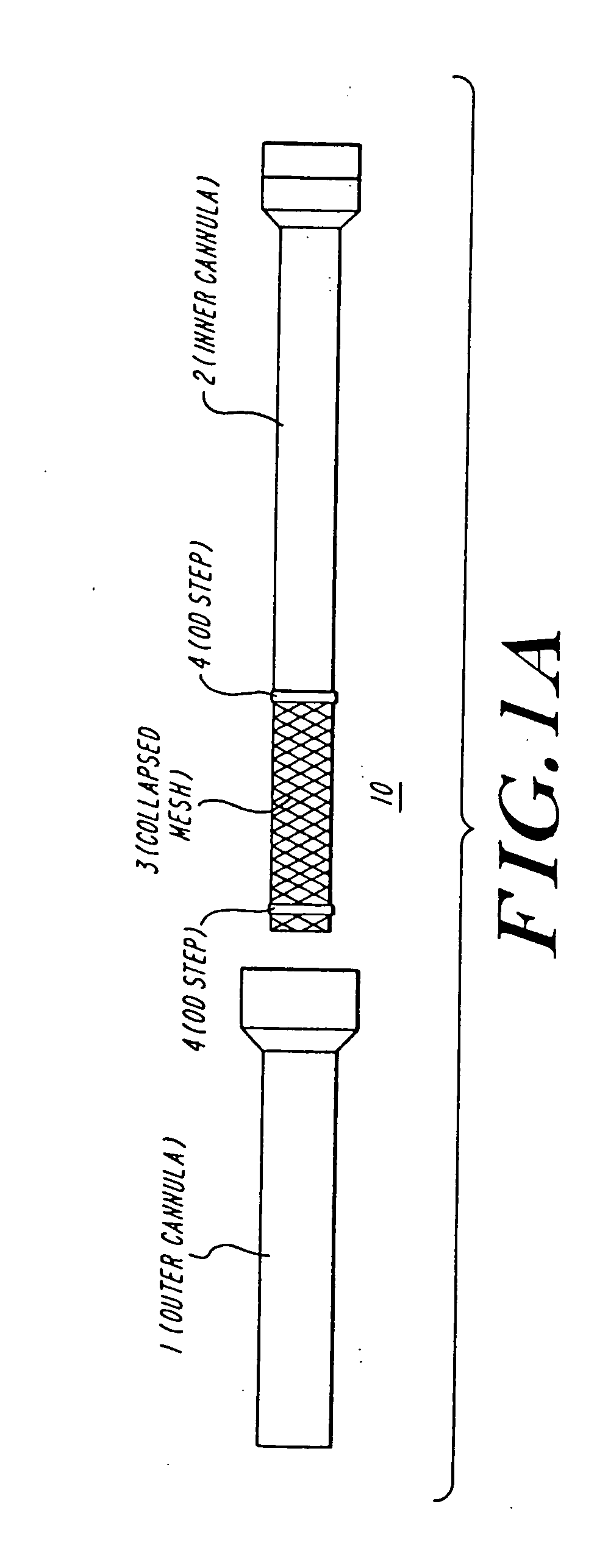
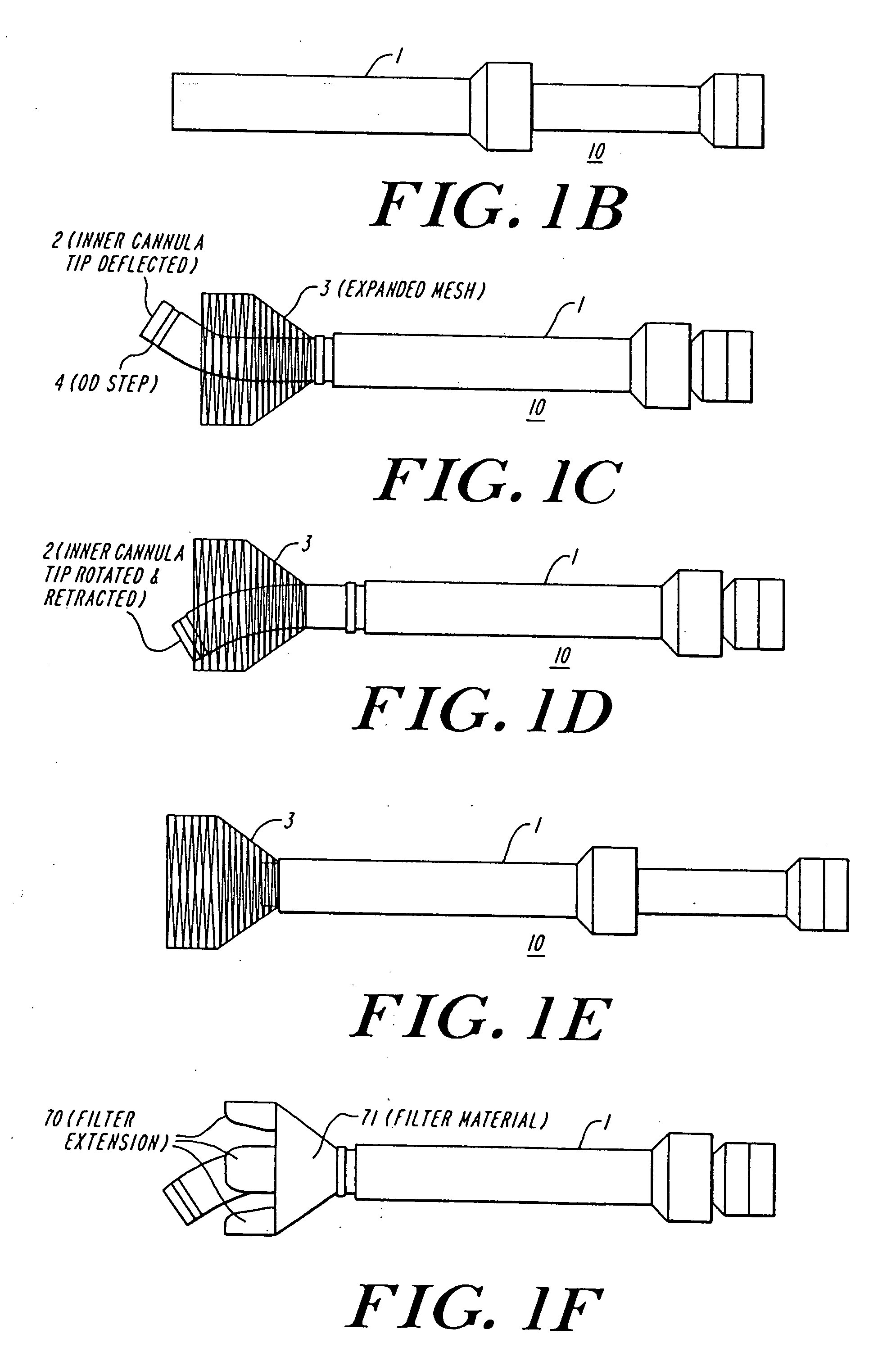
The present invention discloses devices and methods for performing intravascular procedures with out cardiac bypass. The devices include various embodiments of temporary filter devices, temporary valves, and prosthetic valves.The temporary filter devices have one or more cannulae which provide access for surgical tools for effecting repair of the cardiac valves. A cannula may have filters of various configurations encircling the distal region of the cannula, which prevent embolitic material from entering the coronary arteries and aorta.The temporary valve devices may also have one or more cannulae which guide the insertion of the valve into the aorta. The valve devices expand in the aorta to occupy the entire flow path of the vessel. In one embodiment, the temporary valve is a disc of flexible, porous, material that acts to filter blood passing therethrough. A set of valve leaflets extend peripherally from the disc. These leaflets can alternately collapse to prevent blood flow through the valve and extend to permit flow.The prosthetic valves include valve fixation devices which secure the prosthetic valve to the wall of the vessel. In one embodiment, the prosthetic valves have at least one substantially rigid strut, at least two expandable fixation rings located about the circumference of the base of the apex of the valve, and one or more commissures and leaflets. The prosthetic valves are introduced into the vascular system a compressed state, advanced to the site of implantation, expanded and secured to the vessel wall.
Owner:MEDTRONIC INC
Cardiac valve procedure methods and devices
The present invention discloses devices and methods for performing intravascular procedures with out: cardiac bypass. The devices include various embodiments of temporary filter devices, temporary valves, and prosthetic valves. The temporary filter devices have one or more cannulae which provide access for surgical tools for effecting repair of the cardiac valves. A cannula may have filters of various configurations encircling the distal region of the cannula, which prevent embolitic material from entering the coronary arteries and aorta. The temporary valve devices may also have one or more cannulae which guide the insertion of the valve into the aorta. The valve devices expand in the aorta to occupy the entire flow path of the vessel. In one embodiment, the temporary valve is a disc of flexible, porous, material that acts to filter blood passing therethrough. A set of valve leaflets extend peripherally from the disc. These leaflets can alternately collapse to prevent blood flow through the valve and extend to permit flow. The prosthetic valves include valve fixation devices which secure the prosthetic valve to the wall of the vessel. In one embodiment, the prosthetic valves have at least one substantially rigid strut, at least two expandable fixation rings located about the circumference of the base of the apex of the valve, and one or more commissures and leaflets. The prosthetic valves are introduced into the vascular system a compressed state, advanced to the site of implantation, expanded and secured to the vessel wall.
Owner:MEDTRONIC INC
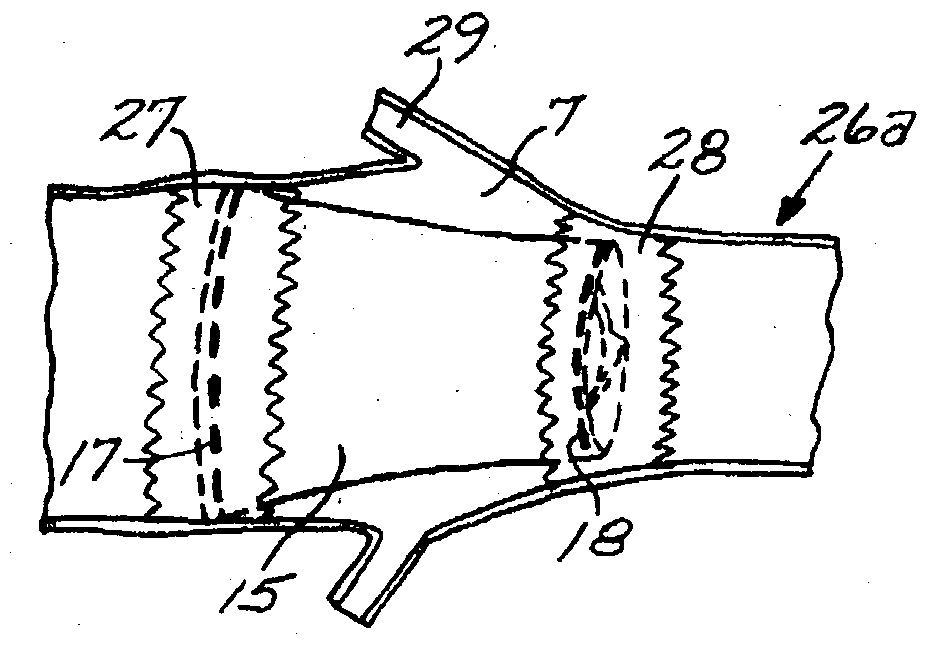
Prosthetic Valve for Transluminal Delivery
InactiveUS20100004740A1Preventing substantial migrationEliminate the problemBalloon catheterHeart valvesVenous accessImplantation Site
A prosthetic valve assembly for use in replacing a deficient native valve comprises a replacement valve supported on an expandable valve support. If desired, one or more anchors may be used. The valve support, which entirely supports the valve annulus, valve leaflets, and valve commissure points, is configured to be collapsible for transluminal delivery and expandable to contact the anatomical annulus of the native valve when the assembly is properly positioned. Portions of the valve support may expand to a preset diameter to maintain coaptivity of the replacement valve and to prevent occlusion of the coronary ostia. A radial restraint, comprising a wire, thread or cuff, may be used to ensure expansion does not exceed the preset diameter. The valve support may optionally comprise a drug elution component. The anchor engages the lumen wall when expanded and prevents substantial migration of the valve assembly when positioned in place. The prosthetic valve assembly is compressible about a catheter, and restrained from expanding by an outer sheath. The catheter may be inserted inside a lumen within the body, such as the femoral artery, and delivered to a desired location, such as the heart. A blood pump may be inserted into the catheter to ensure continued blood flow across the implantation site during implantation procedure. When the outer sheath is retracted, the prosthetic valve assembly expands to an expanded position such that the valve and valve support expand at the implantation site and the anchor engages the lumen wall. Insertion of the catheter may optionally be performed over a transseptally delivered guidewire that has been externalized through the arterial vasculature. Such a guidewire provide dual venous and arterial access to the implantation site and allows additional manipulation of the implantation site after arterial implantation of the prosthetic valve. Additional expansion stents may be delivered by venous access to the valve.
Owner:MEDTRONIC COREVALVE
Assembly for setting a valve prosthesis in a corporeal duct
InactiveUS7682390B2Eliminate riskRisk is exacerbatedBalloon catheterHeart valvesCommissureBiomedical engineering
The invention concerns an assembly comprising a valve prosthesis to be implanted and a support receiving said valve. The support comprises: at least a tubular portion made of a pliable material slightly stretchable in the circumferential direction; means for fixing said tubular portion to the wall of the corporeal duct; and a plurality of elongated reinforcing elements, arranged on the circumference of said tubular portion and linked to said tubular portion independently of one another; the valve is linked at least partly to said elongated reinforcing elements, in particular at the commissures of its leaflets, and said elongated reinforcing elements jointly form, in extended position, a structure having a predetermined diameter that ensures sufficient extension of said valve.
Owner:MEDTRONIC COREVALVE
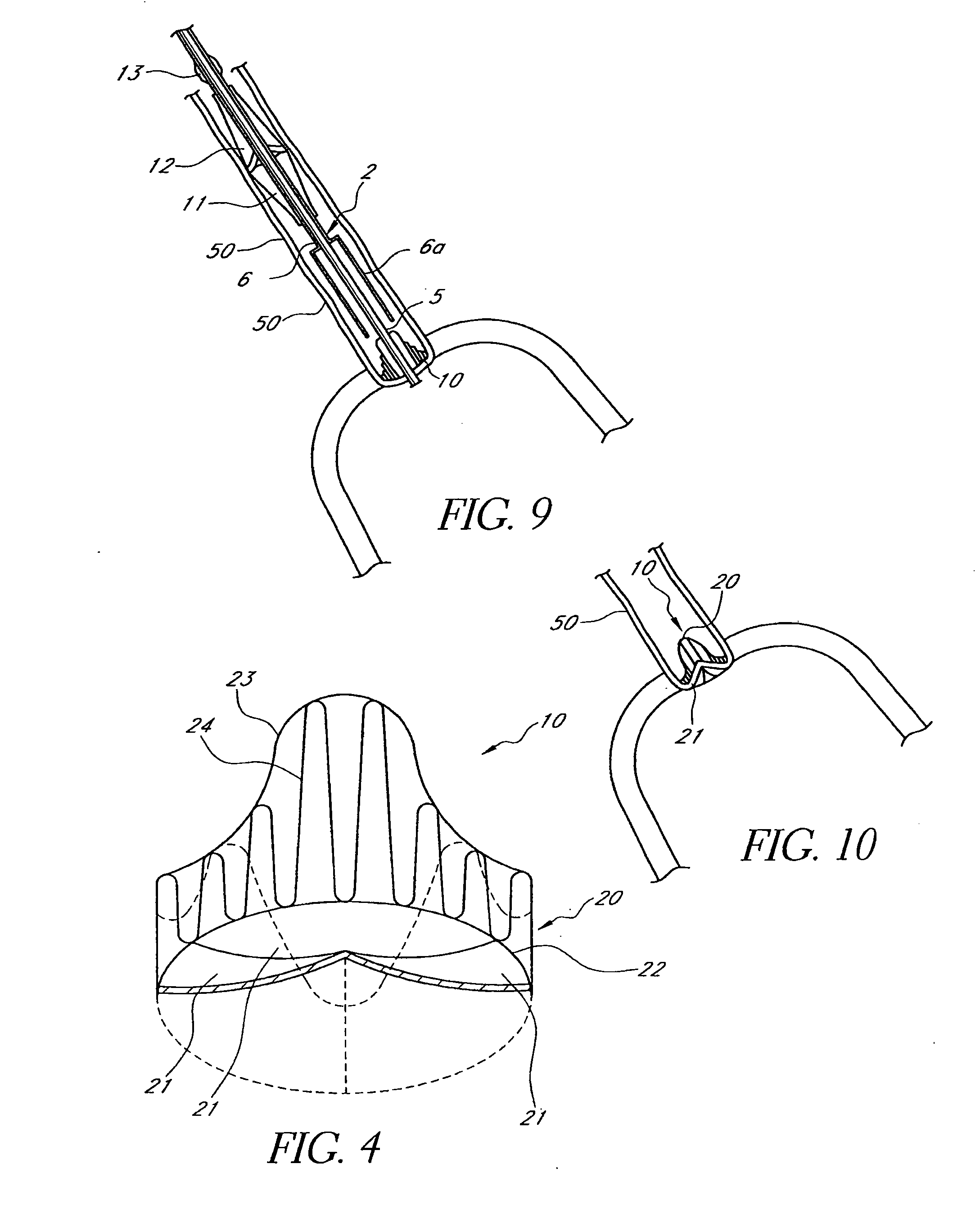
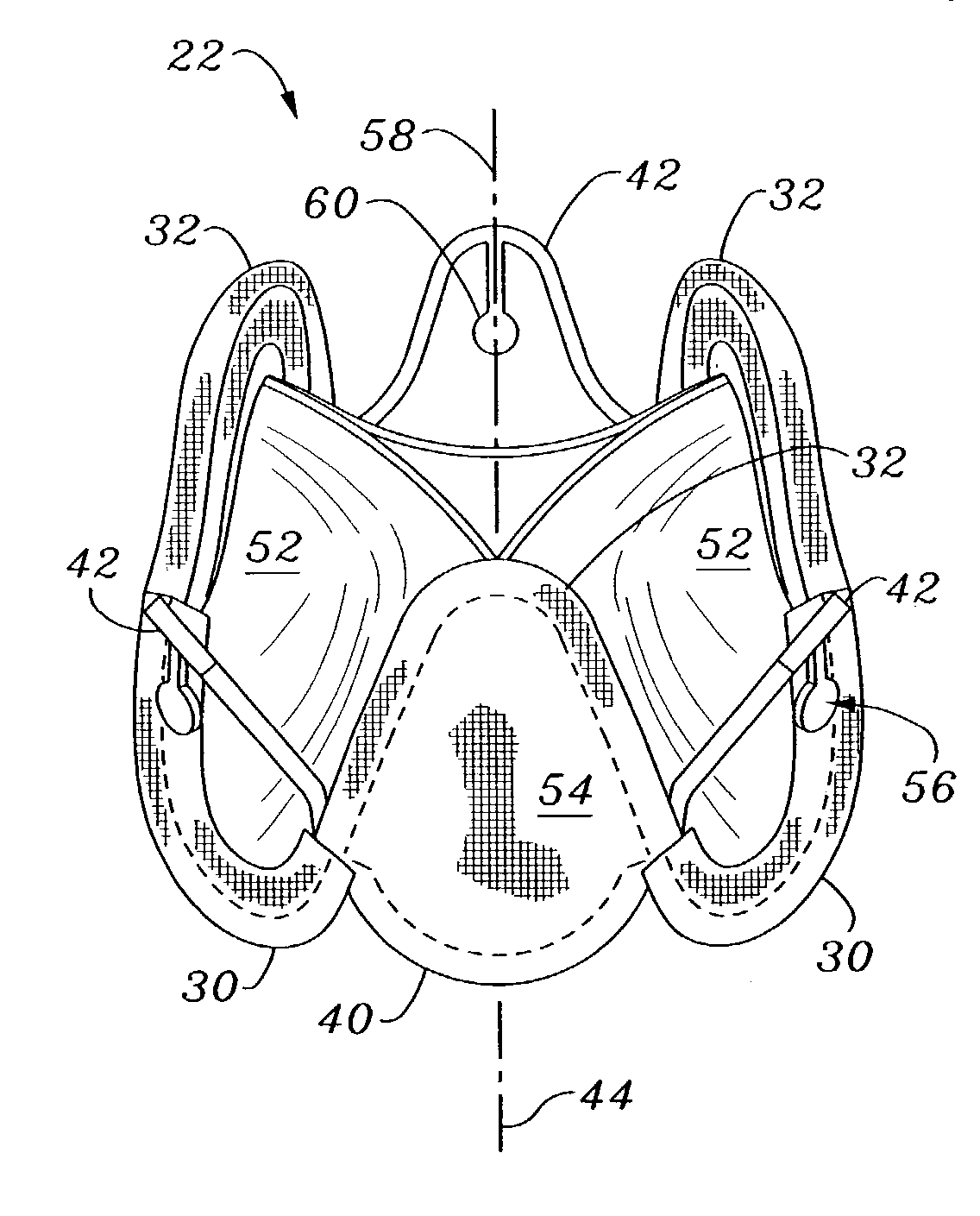
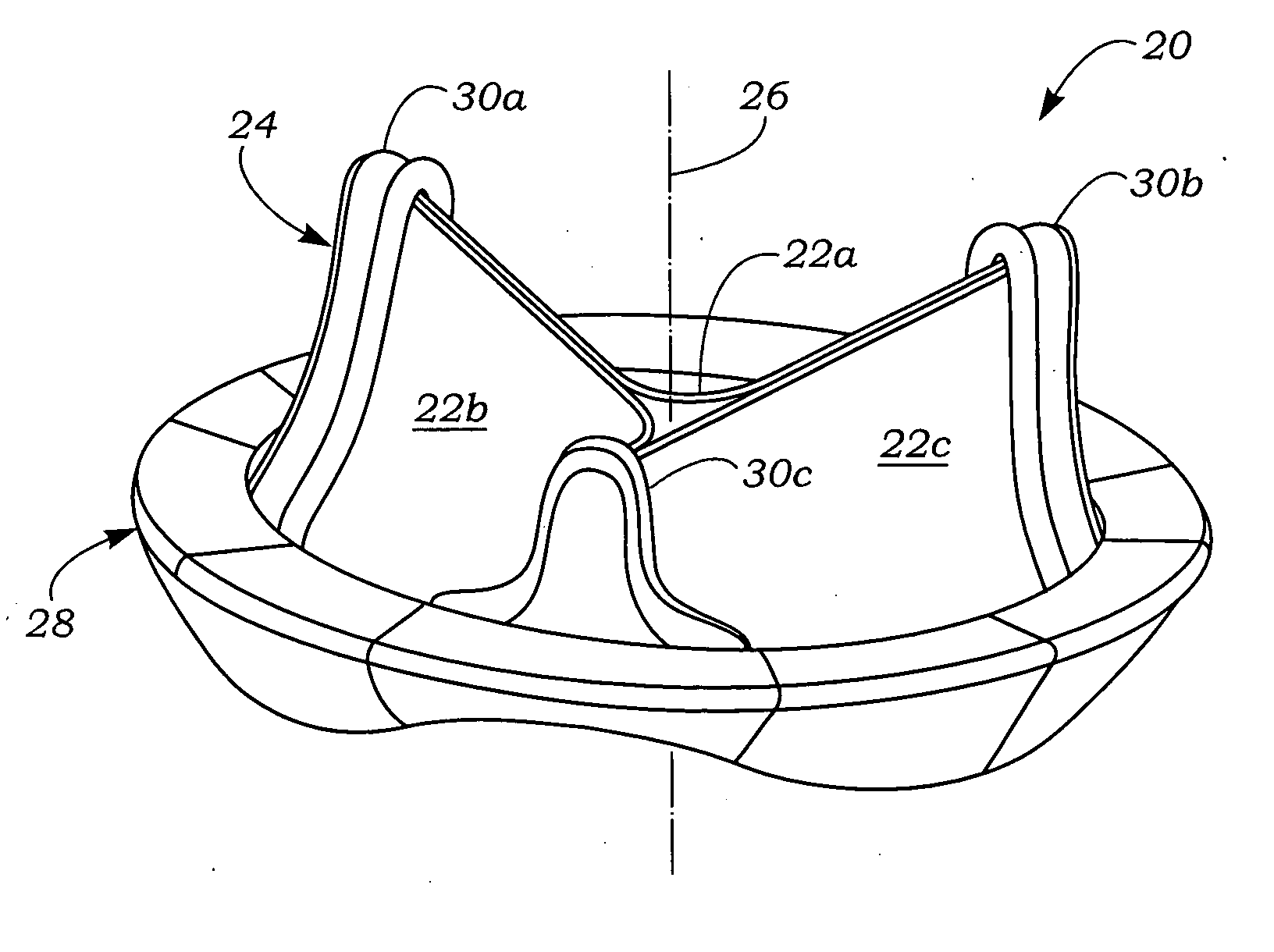
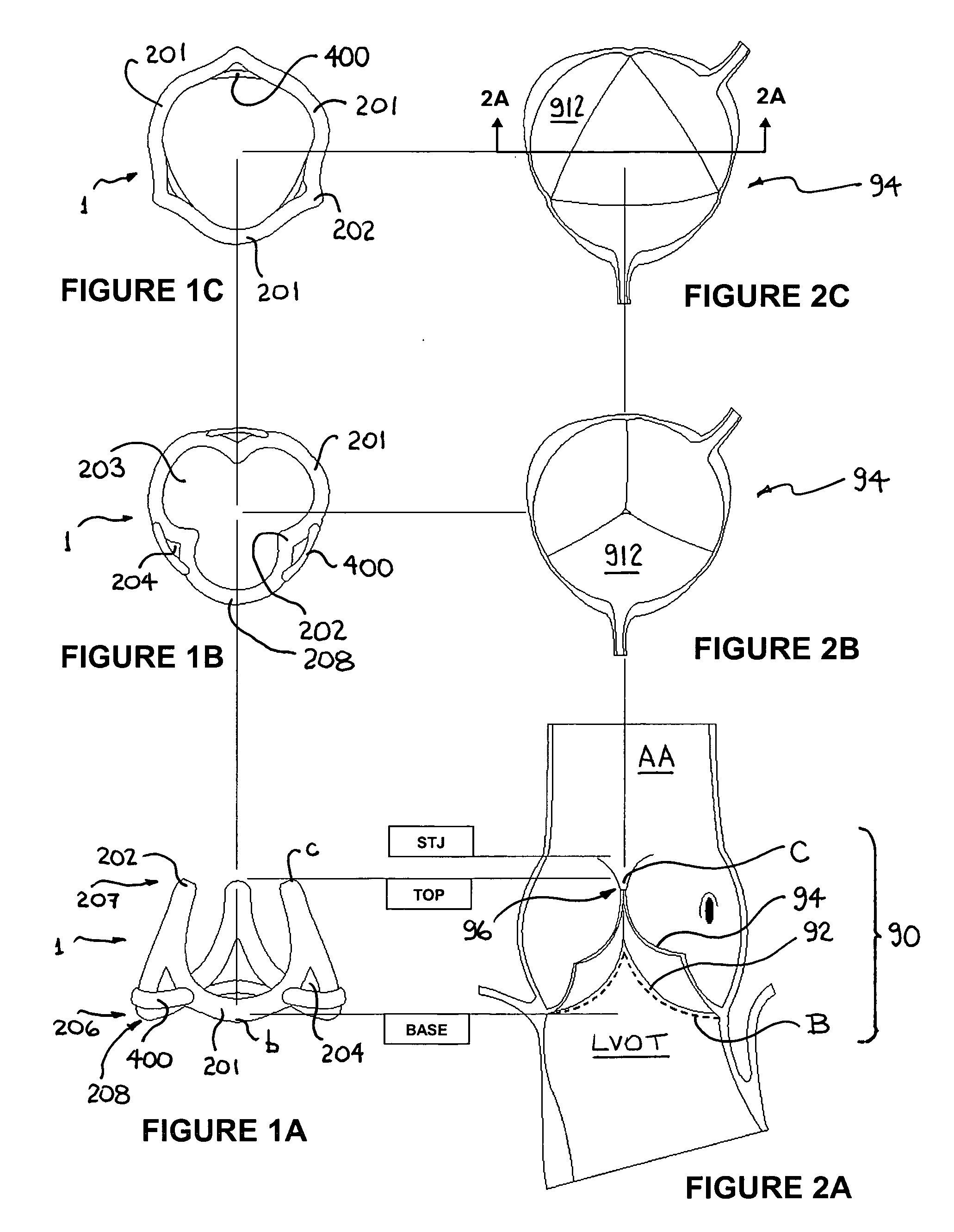
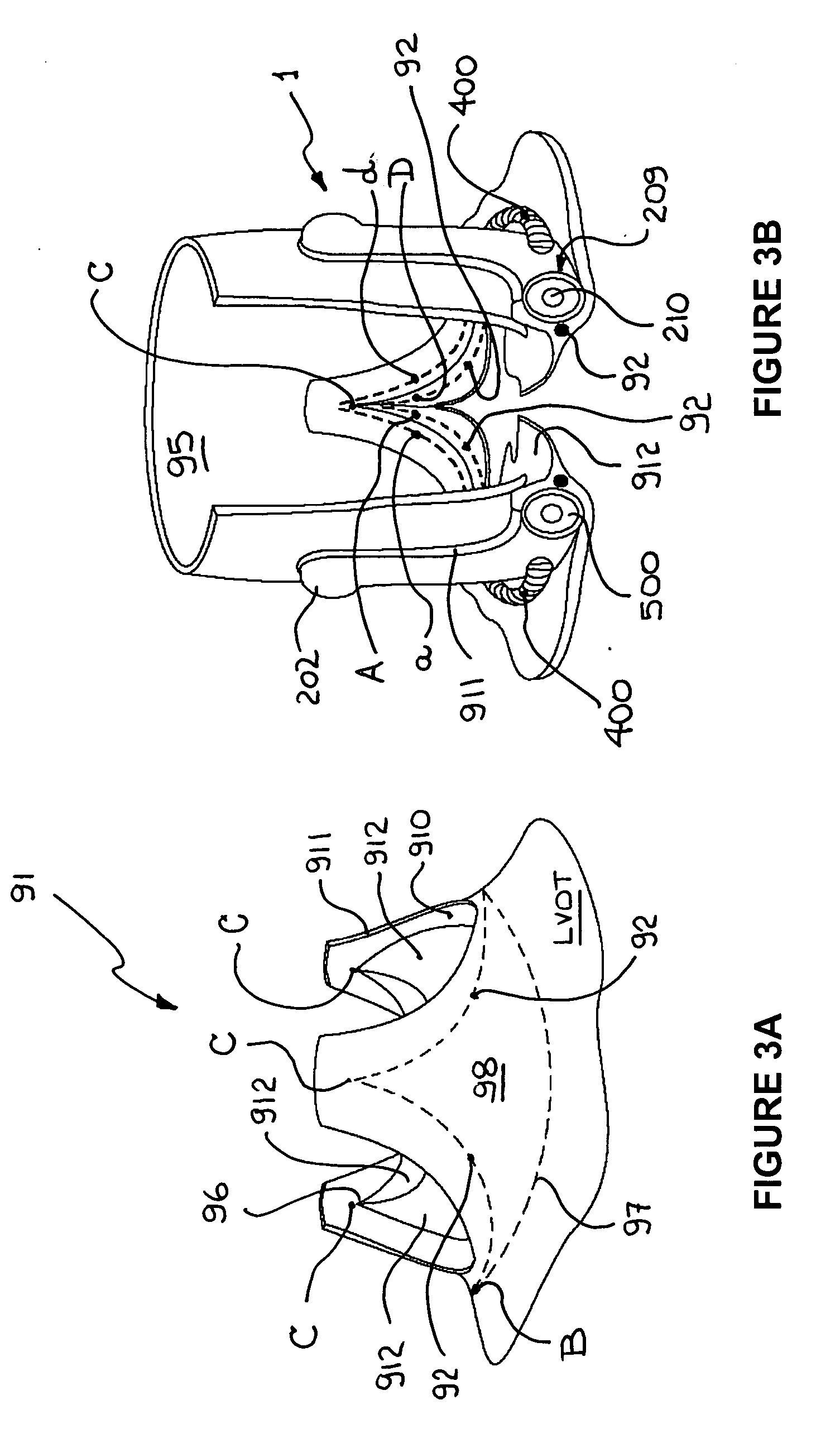
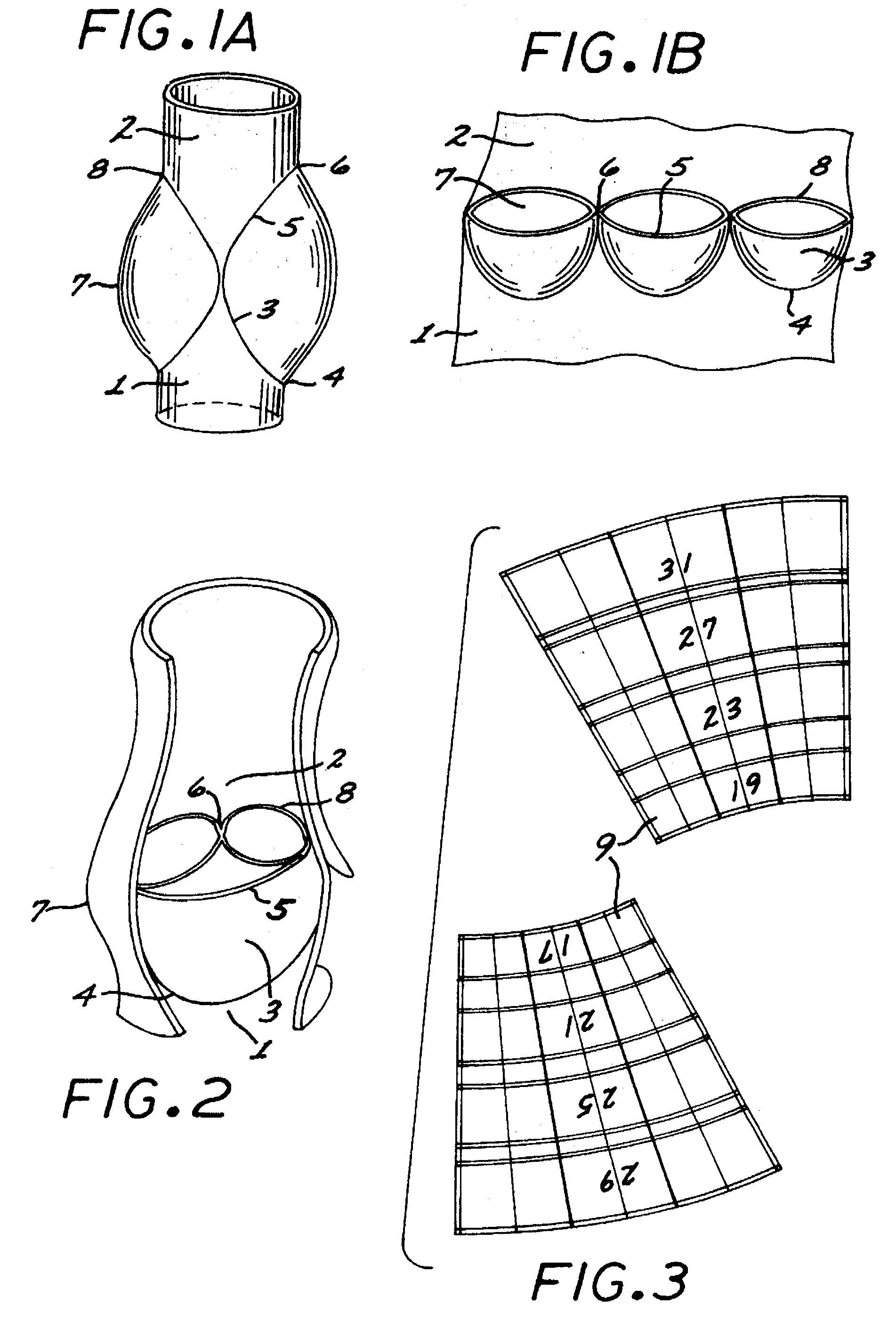
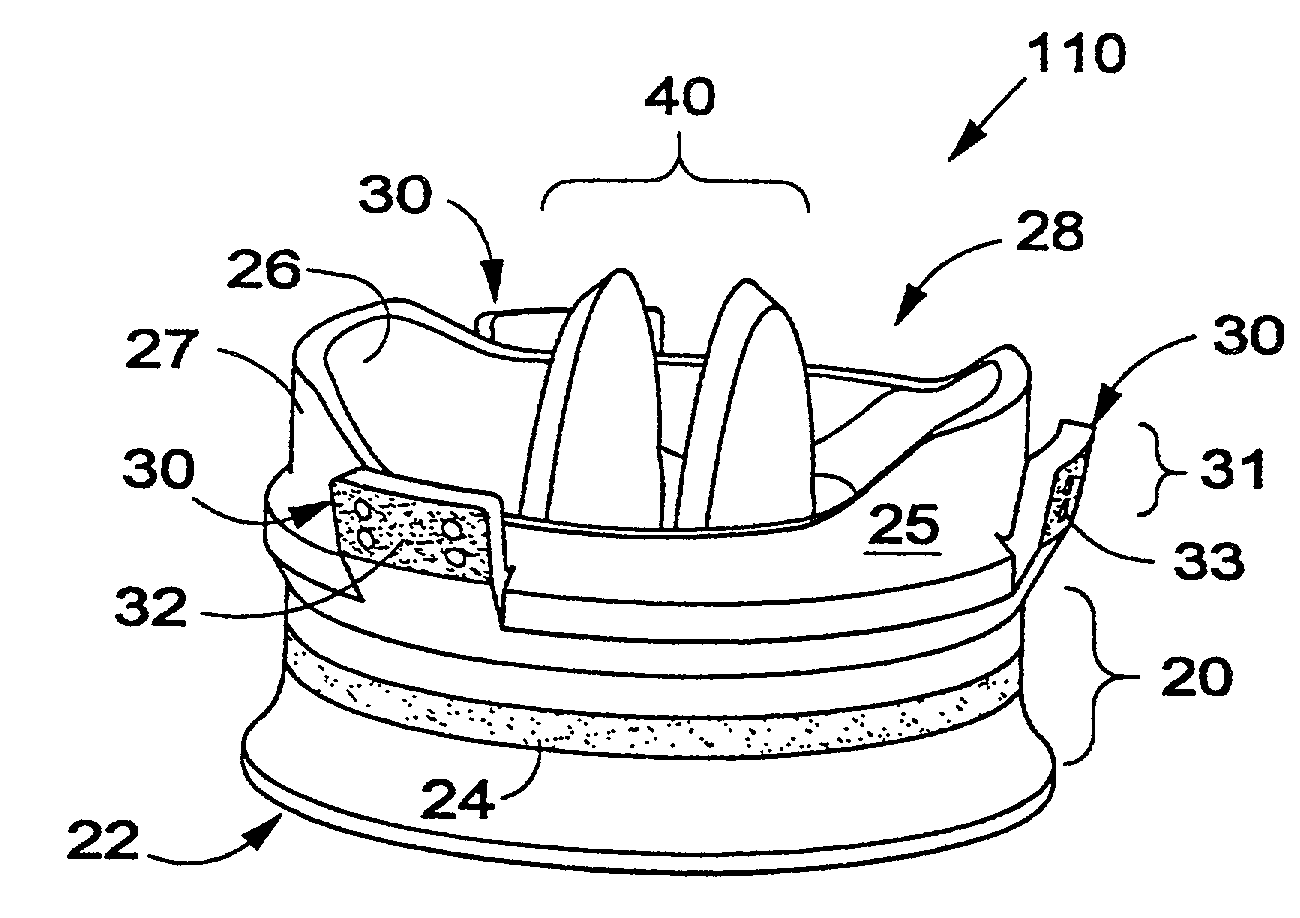
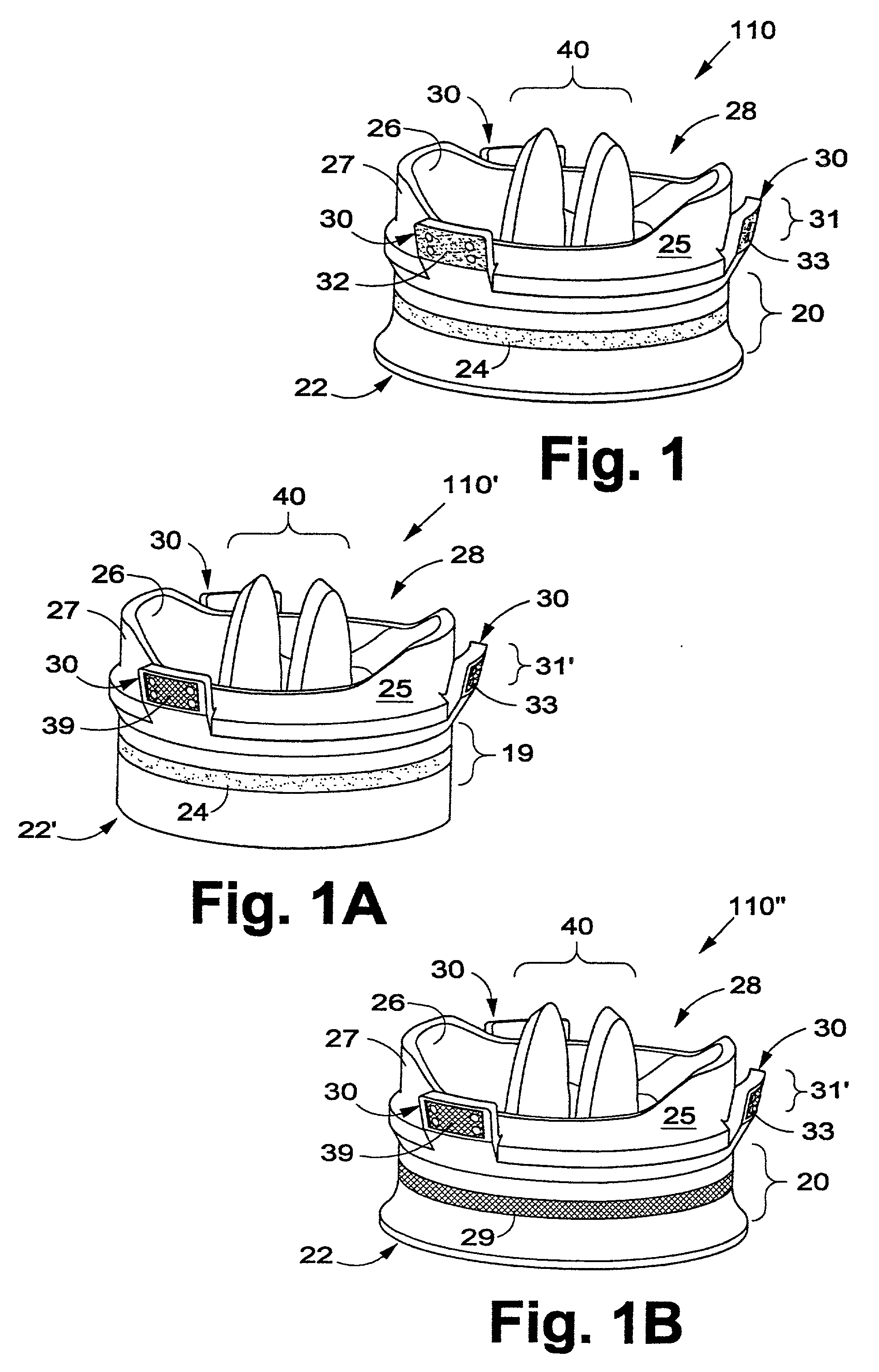
Minimally-invasive heart valve with cusp positioners
A prosthetic heart valve having an internal support frame with a continuous, undulating leaflet frame defined therein. The leaflet frame has three cusp regions positioned at an inflow end intermediate three commissure regions positioned at an outflow end thereof. The leaflet frame may be cloth covered and flexible leaflets attached thereto form occluding surfaces of the valve. The support frame further includes three cusp positioners rigidly fixed with respect to the leaflet frame and located at the outflow end of the support frame intermediate each pair of adjacent commissure regions. The valve is desirably compressible so as to be delivered in a minimally invasive manner through a catheter to the site of implantation. Upon expulsion from catheter, the valve expands into contact with the surrounding native valve annulus and is anchored in place without the use of sutures. In the aortic valve position, the cusp positioners angle outward into contact with the sinus cavities, and compress the native leaflets if they are not excised, or the aortic wall if they are. The support frame may be formed from a flat sheet of Nitinol that is bent into a three-dimensional configuration and heat set. A holder having spring-like arms connected to inflow projections of the valve may be used to deliver, reposition and re-collapse the valve, if necessary.
Owner:EDWARDS LIFESCIENCES CORP
Cardiac valve procedure methods and devices
The present invention discloses devices and methods for performing intravascular procedures with out cardiac bypass. The devices include various embodiments of temporary filter devices, temporary valves, and prosthetic valves. The temporary filter devices have one or more cannulae which provide access for surgical tools for effecting repair of the cardiac valves. A cannula may have filters of various configurations encircling the distal region of the cannula, which prevent embolitic material from entering the coronary arteries and aorta. The temporary valve devices may also have one or more cannulae which guide the insertion of the valve into the aorta. The valve devices expand in the aorta to occupy the entire flow path of the vessel. In one embodiment, the temporary valve is a disc of flexible, porous, material that acts to filter blood passing therethrough. A set of valve leaflets extend peripherally from the disc. These leaflets can alternately collapse to prevent blood flow through the valve and extend to permit flow. The prosthetic valves include valve fixation devices which secure the prosthetic valve to the wall of the vessel. In one embodiment, the prosthetic valves have at least one substantially rigid strut, at least two expandable fixation rings located about the circumference of the base of the apex of the valve, and one or more commissures and leaflets. The prosthetic valves are introduced into the vascular system a compressed state, advanced to the site of implantation, expanded and secured to the vessel wall.
Owner:MEDTRONIC INC
Minimally-invasive heart valve with cusp positioners
A prosthetic heart valve having an internal support frame with a continuous, undulating leaflet frame defined therein. The leaflet frame has three cusp regions positioned at an inflow end intermediate three commissure regions positioned at an outflow end thereof. The leaflet frame may be cloth covered and flexible leaflets attached thereto form occluding surfaces of the valve. The support frame further includes three cusp positioners rigidly fixed with respect to the leaflet frame and located at the outflow end of the support frame intermediate each pair of adjacent commissure regions. The valve is desirably compressible so as to be delivered in a minimally invasive manner through a catheter to the site of implantation. Upon expulsion from catheter, the valve expands into contact with the surrounding native valve annulus and is anchored in place without the use of sutures. In the aortic valve position, the cusp positioners angle outward into contact with the sinus cavities, and compress the native leaflets if they are not excised, or the aortic wall if they are. The support frame may be formed from a flat sheet of Nitinol that is bent into a three-dimensional configuration and heat set. A holder having spring-like arms connected to inflow projections of the valve may be used to deliver, reposition and re-collapse the valve, if necessary.
Owner:EDWARDS LIFESCIENCES CORP
Sigmoid valve and method for its percutaneous implantation
A multi-leaflet valve adapted to serve as a prosthesis for diseased native valve of a mammal is incorporated in self-expandable or inflatable endovascular stents or stents to form a combination which is introduced on a catheter with a guide wire into the circulatory system of the mammal to replace the diseased native valve. Once the combination is at the desired location the stent is caused to expand and affix itself to the patient's vessel wall. The prosthetic valve has the shape of a truncated cone that has an inflow and an outflow orifice with leaflets forming the outflow orifice and forming a plurality of commissures. A first flexible circular support is affixed in a substantially circular fashion around the truncated cone in proximity of the inflow orifice, and a second flexible circular support is affixed at the location of the commissures to form a circle around the truncated cone in proximity of the outflow orifice. The circular supports maintain the shape of the valve during the surgical implantation procedure and thereafter.
Owner:THE INT HEART INST OF MONTANA FOUND
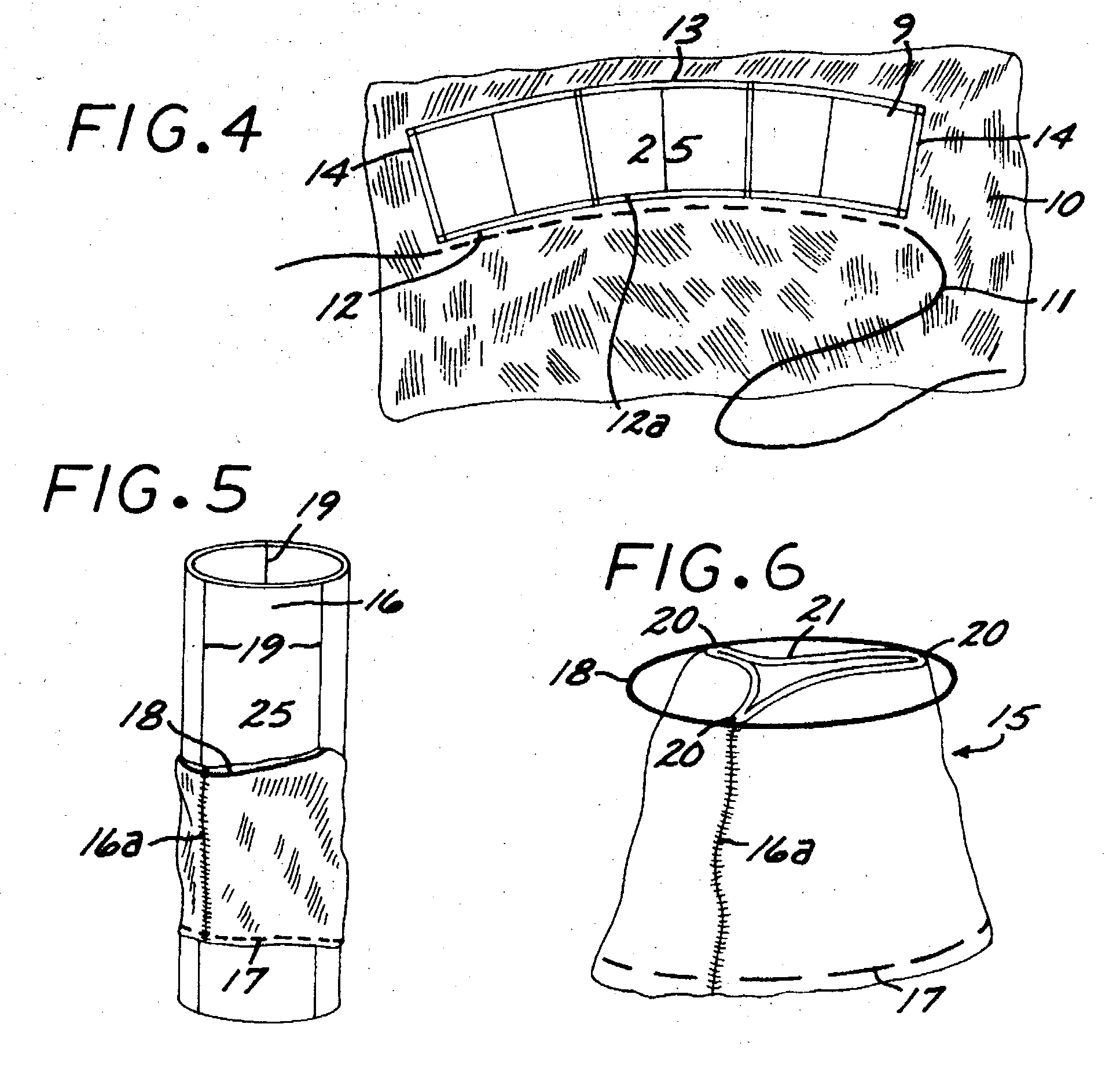
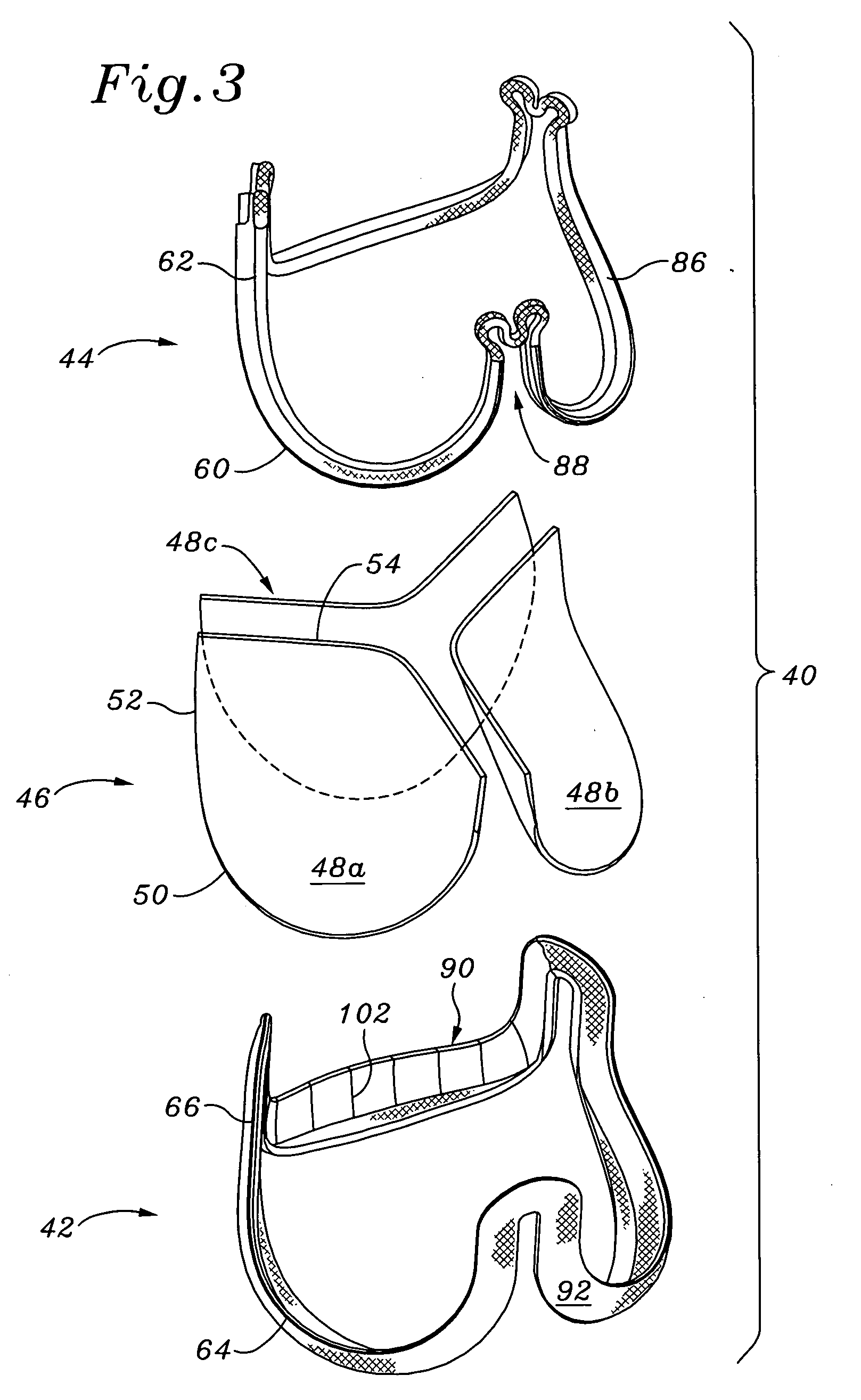
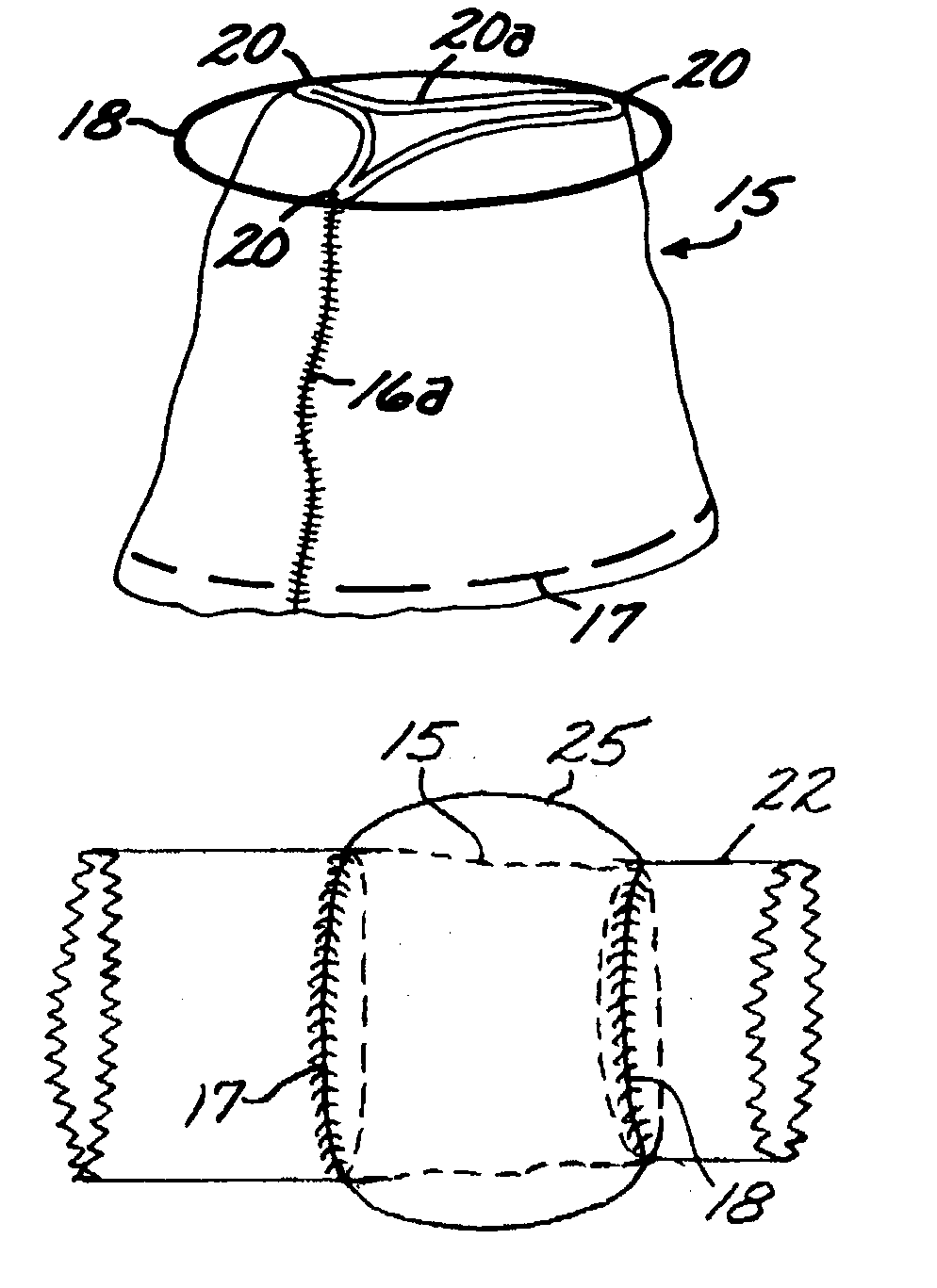
Highly flexible heart valve connecting band
ActiveUS20060229719A1Facilitates supra-annular attachmentIncrease flexibilityHeart valvesInsertion stentTissues types
A connecting band for a highly flexible tissue-type heart valve having a stent with cusps and commissures that are permitted to move radially. The connecting band follows the cusps and commissures and extends outwardly. The valve is connected to the natural tissue along the undulating connecting band using conventional techniques, such as sutures. The connecting band may be a cloth-covered inner suture-permeable member and attaches to the underside of the valve at the cusps to provide support to the stent and to the outer side of the valve at the commissures. The connecting band includes commissure portions defining generally axial gaps that help permit flexing of the valve. The inner member may include one or more slits along the cusps to enhance flexibility. The inner member may further include a continuous outwardly projecting sewing ridge around its periphery which includes a series of ribs separated by grooves around the inflow edge of the cusps. The sewing ridge enables supra-annular implant of a valve constructed with the connecting band.
Owner:EDWARDS LIFESCIENCES CORP
Prosthetic valve for transluminal delivery
InactiveUS8016877B2Preventing substantial migrationEliminate the problemBalloon catheterHeart valvesProsthesisCommissure
A method for deploying a prosthetic valve assembly is provided. The prosthetic valve assembly replaces a deficient native valve and comprises a replacement valve supported on an expandable valve support. The valve support, which entirely supports the valve annulus, valve leaflets, and valve commissure points, is configured to be collapsible for transluminal delivery and expandable to contact the anatomical annulus of the native valve when the assembly is properly positioned. Portions of the valve support may expand to a preset diameter to maintain coaptivity of the replacement valve and to prevent occlusion of the coronary oslia. The prosthetic valve assembly is compressible about a catheter, and restrained from expanding by an outer sheath. The catheter may be inserted inside a lumen within the body, such as the femoral artery, and delivered to a desired location, such as the heart.
Owner:MEDTRONIC COREVALVE
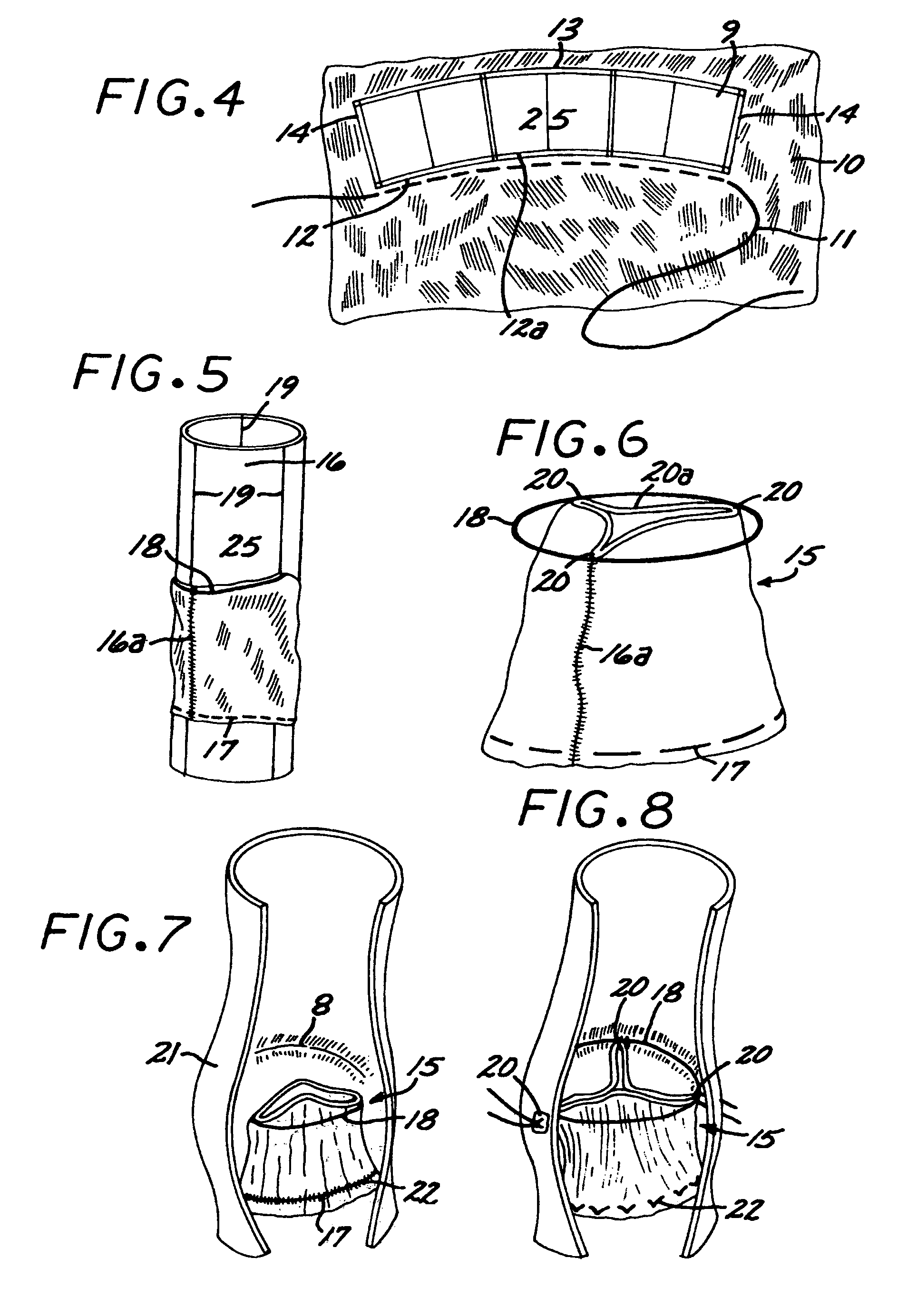
Flexible heart valve and associated connecting band
A highly flexible tissue-type heart valve is disclosed having a structural stent in a generally cylindrical configuration with cusps and commissures that are permitted to move radially. The stent commissures are constructed so that the cusps are pivotably or flexibly coupled together at the commissures to permit relative movement therebetween.
Owner:EDWARDS LIFESCIENCES CORP
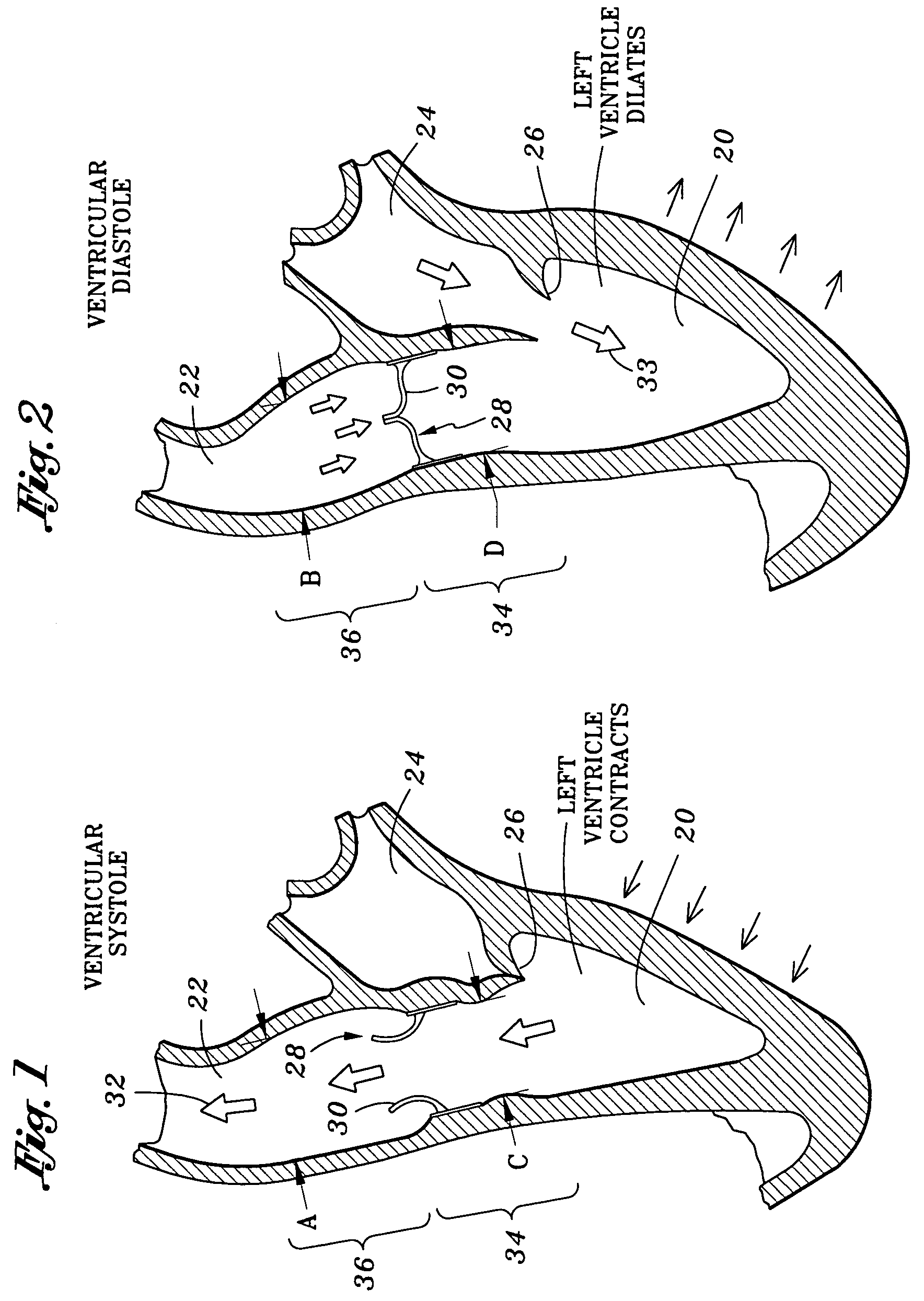
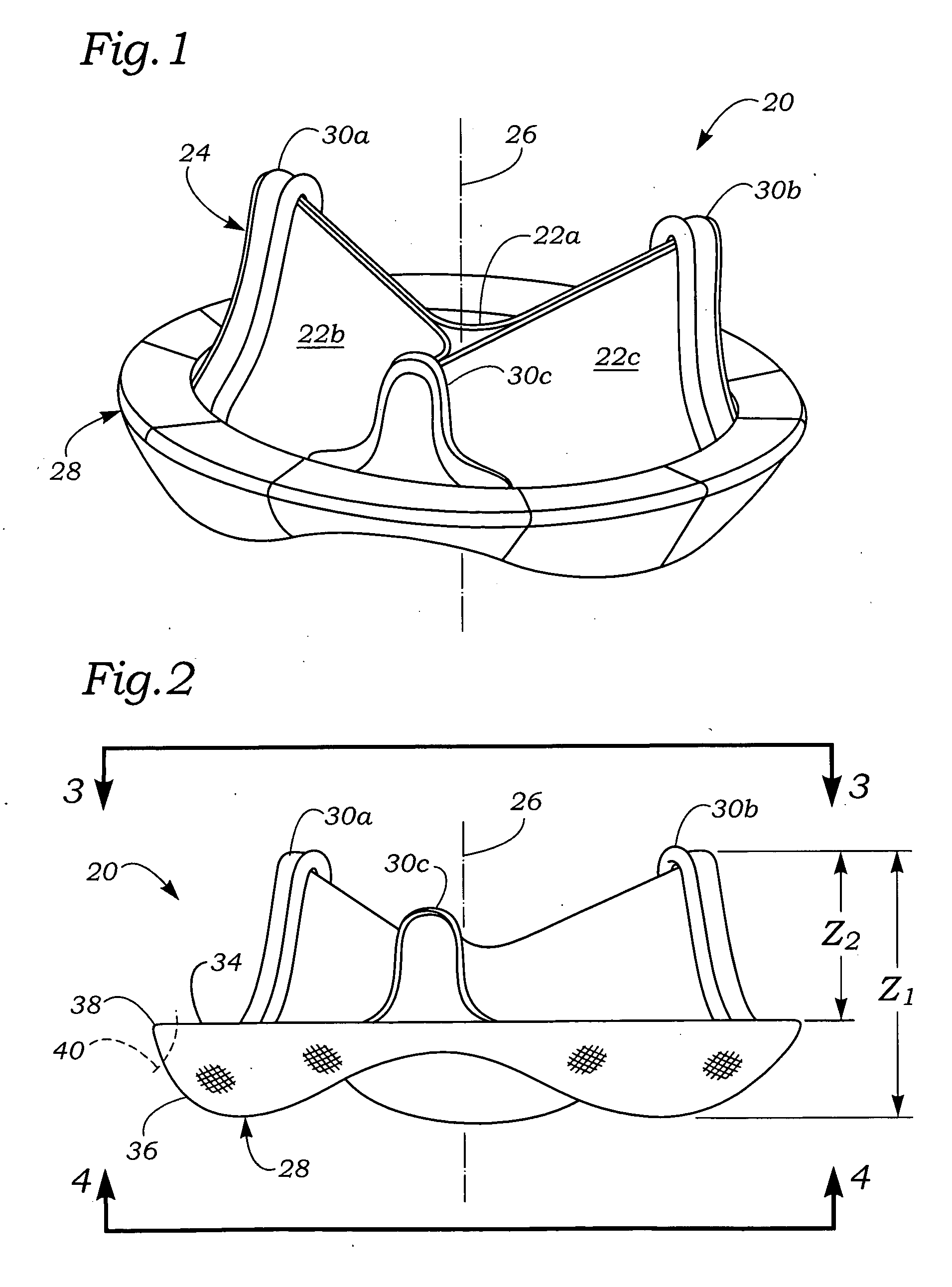
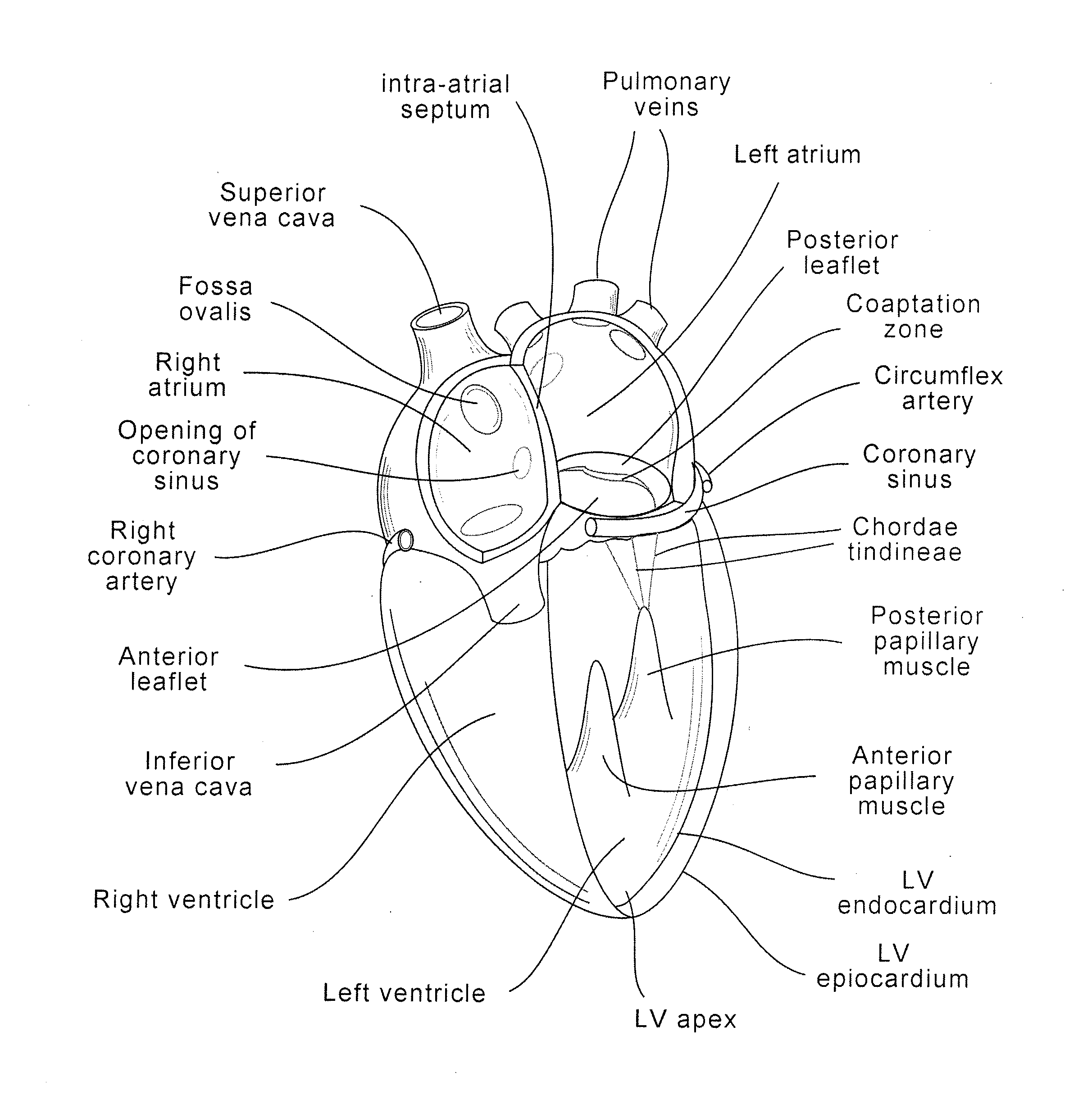
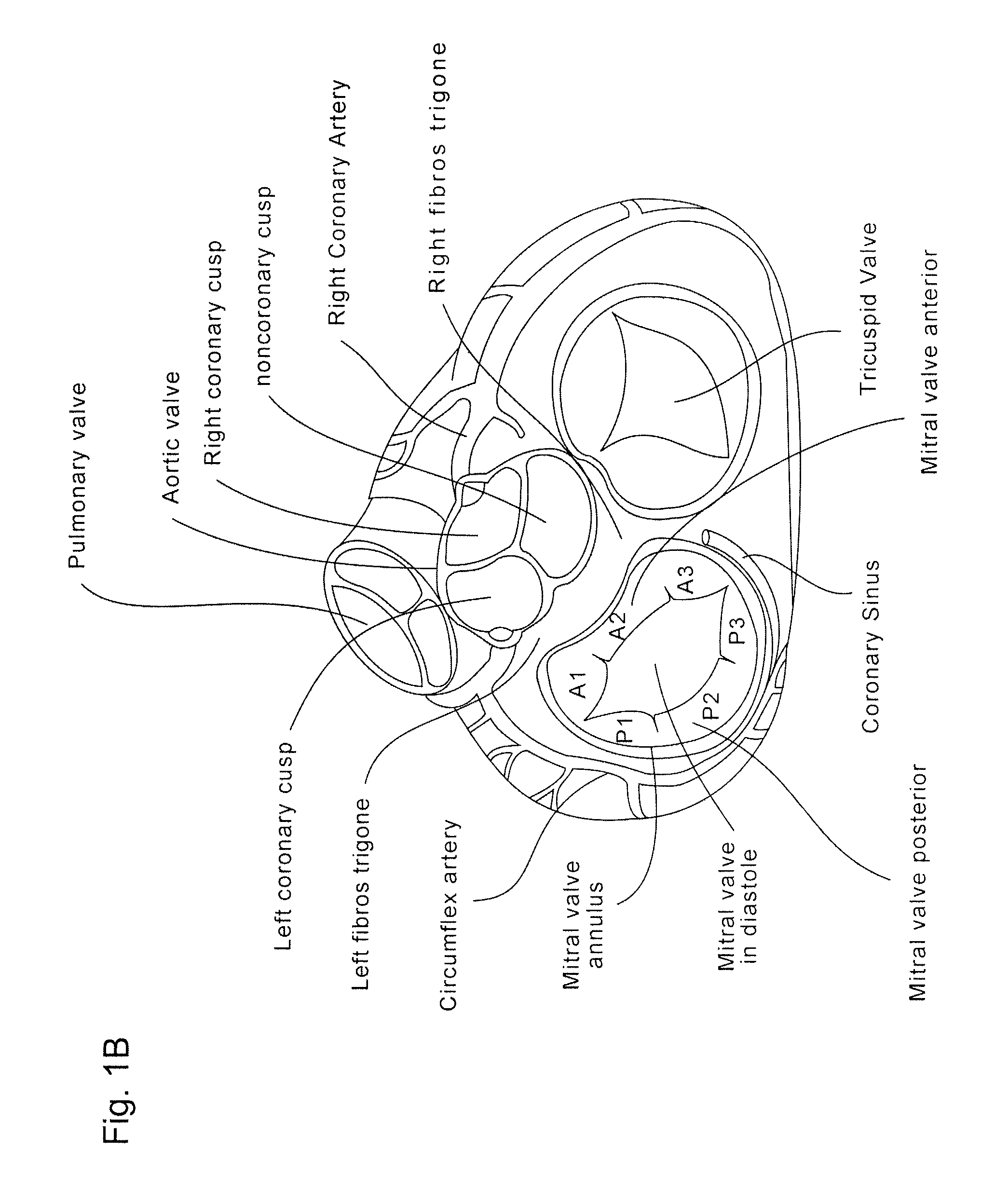
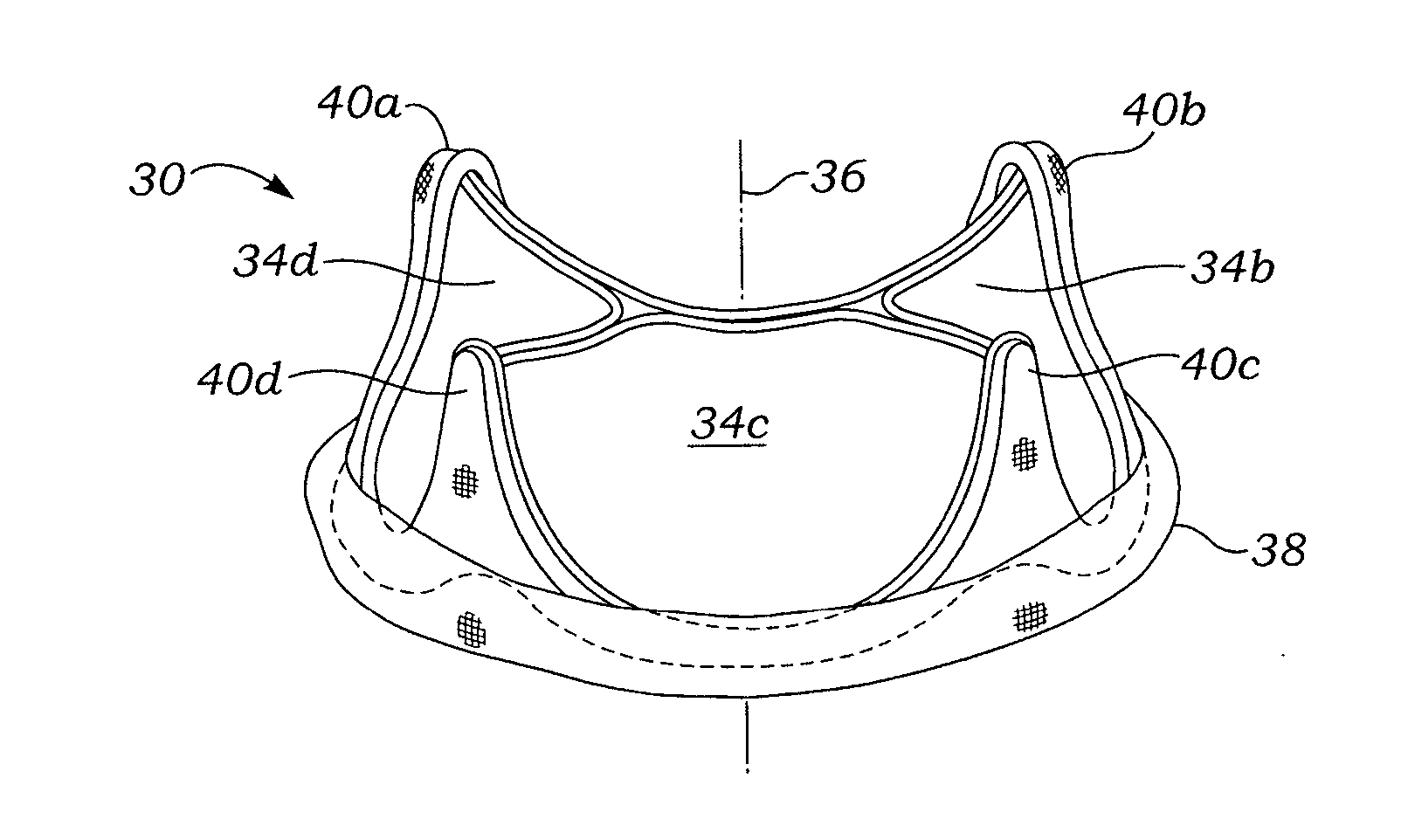
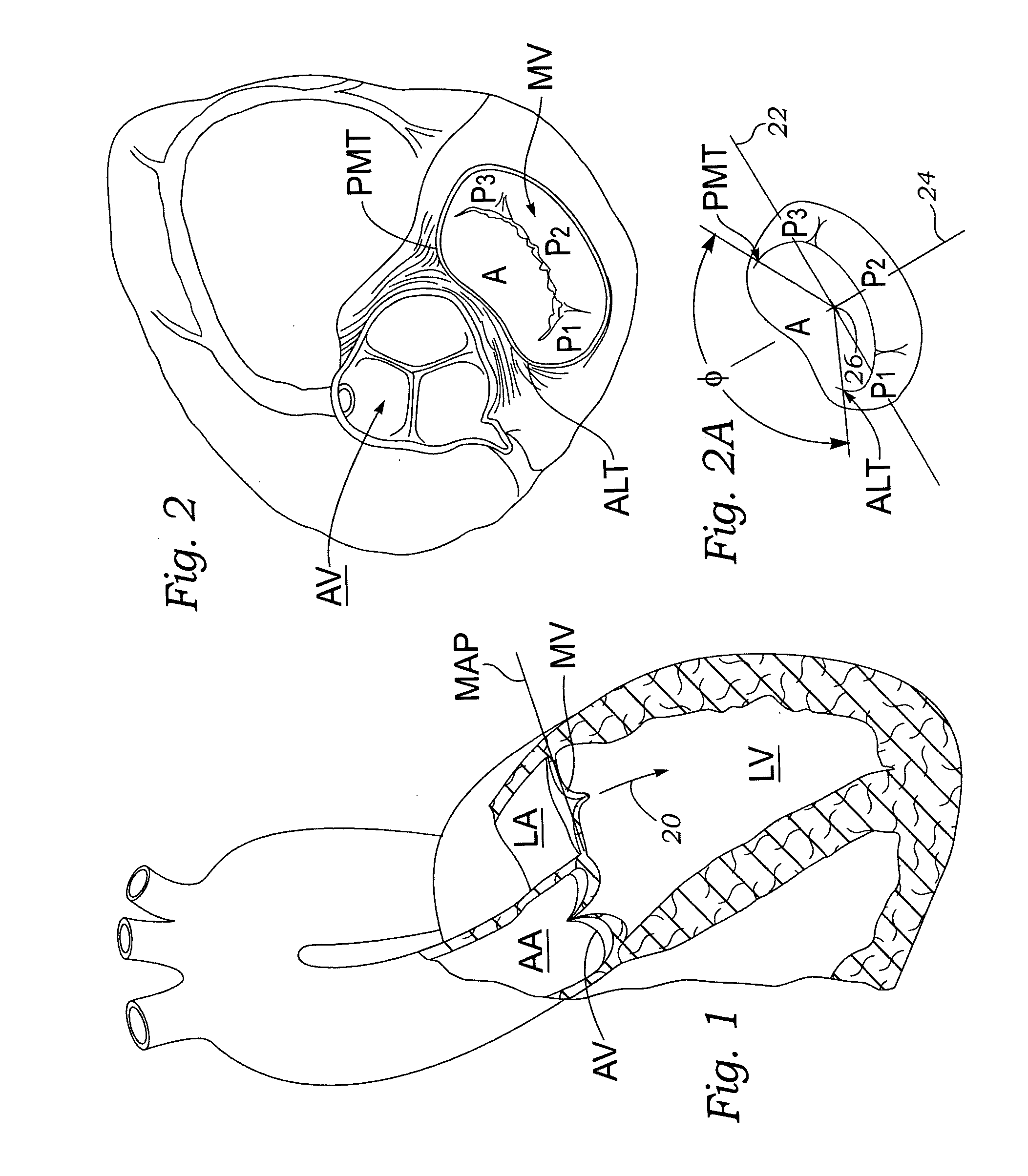
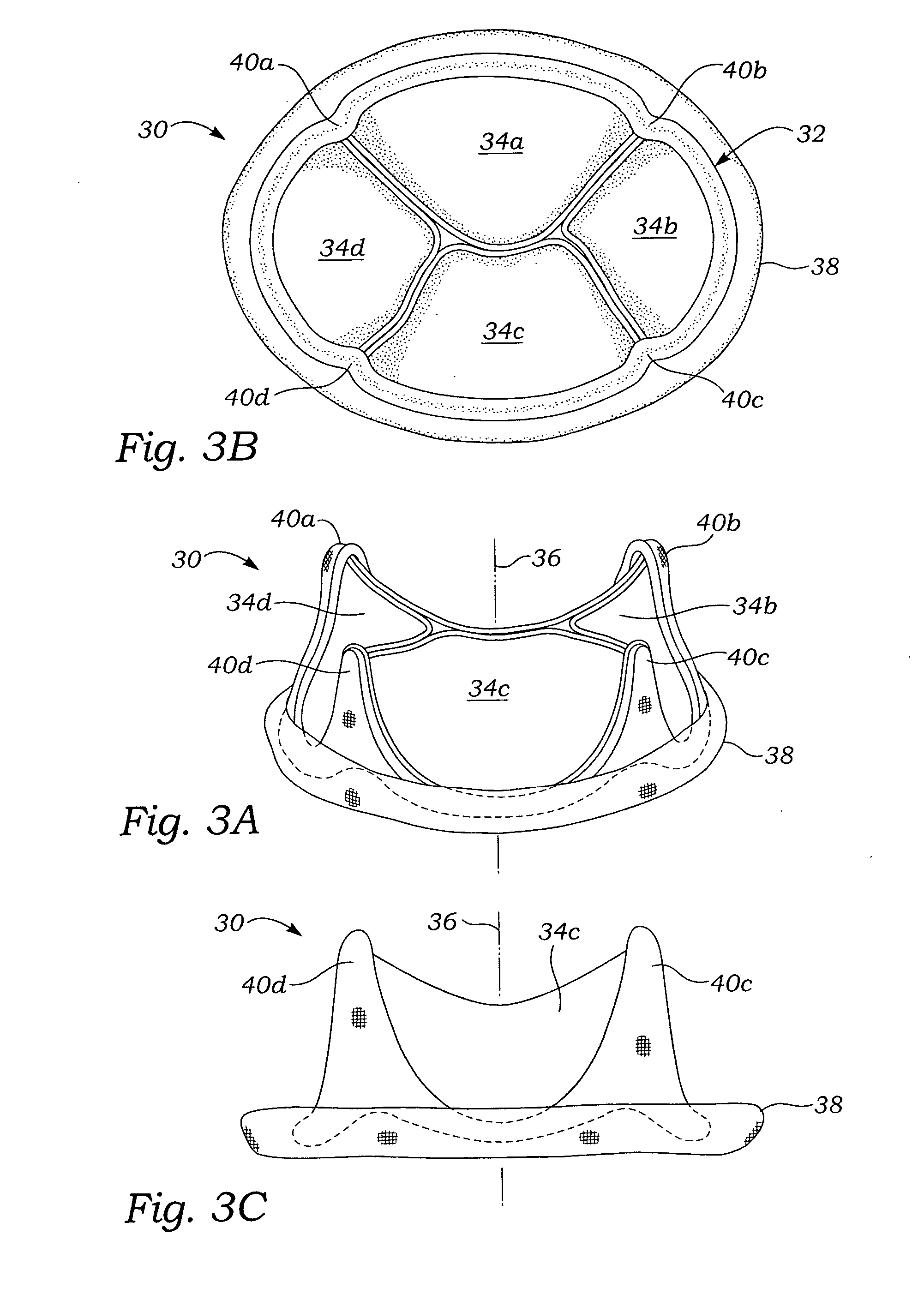
Anatomically approximate prosthetic mitral heart valve
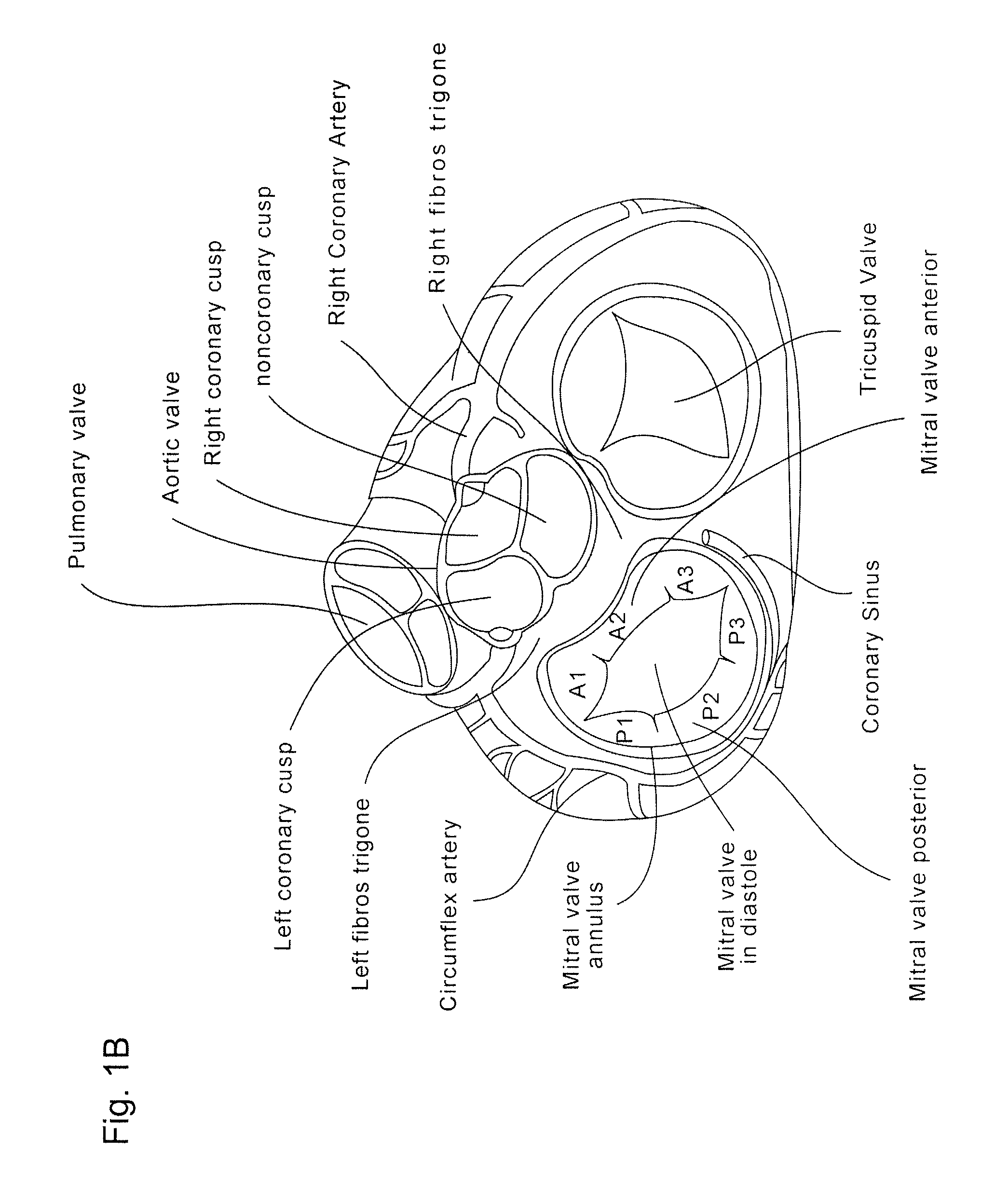
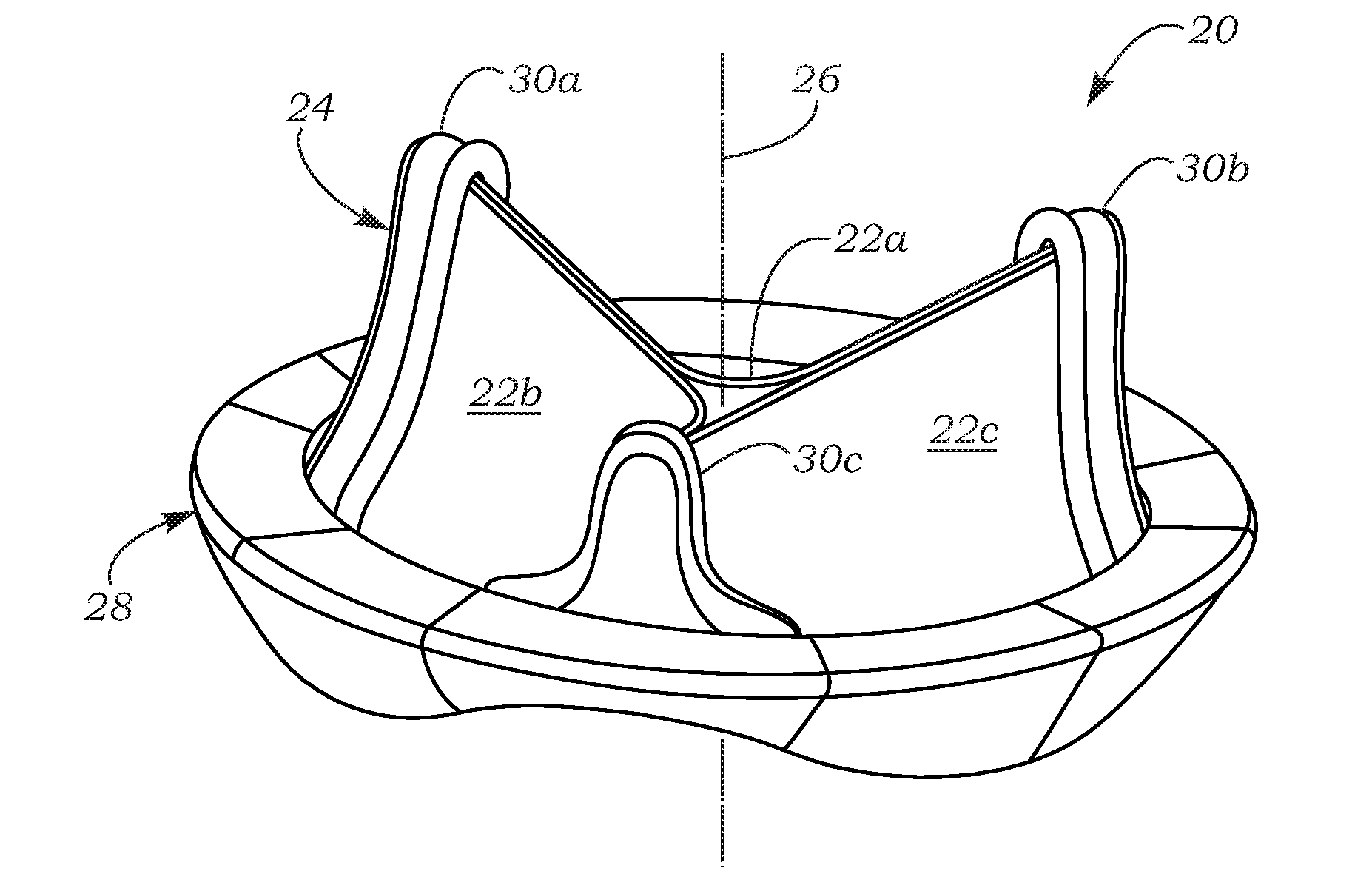
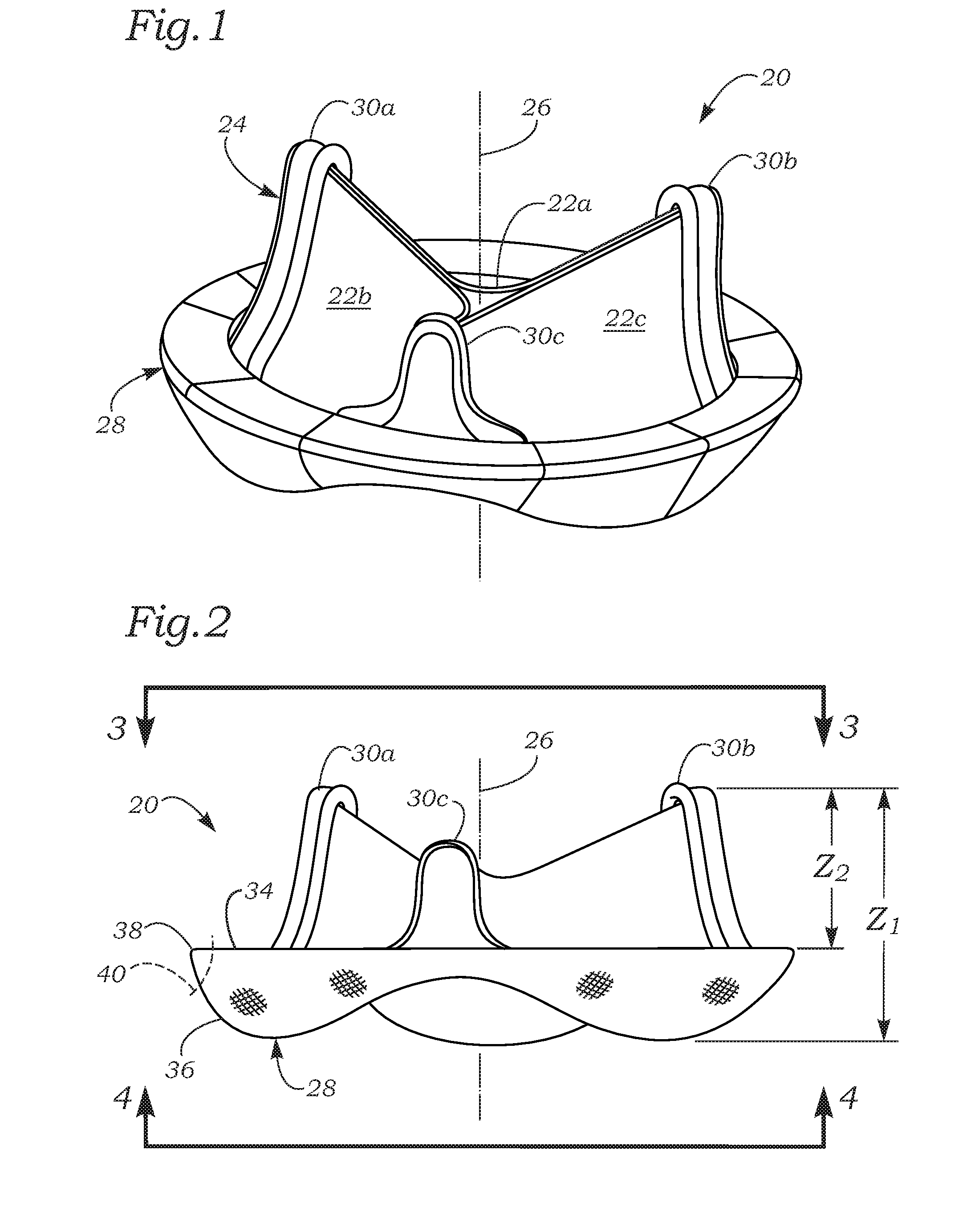
ActiveUS20060293745A1Increase the areaReduce the overall heightAnnuloplasty ringsAnterior leafletMitral annulus
An anatomically approximate prosthetic heart valve includes dissimilar flexible leaflets, dissimilar commissures and / or a non-circular flow orifice. The heart valve may be implanted in the mitral position and have one larger leaflet oriented along the anterior aspect so as to mimic the natural anterior leaflet. Two other smaller leaflets extend around the posterior aspect of the valve. A basic structure providing peripheral support for the leaflets includes two taller commissures on both sides of the larger leaflet, with a third, smaller commissure between the other two leaflets. The larger leaflet may be thicker and / or stronger than the other two leaflets. The base structure defines a flow orifice intended to simulate the shape of the mitral annulus during the systolic phase. For example, the flow orifice may be elliptical. A relatively wide sewing ring has a contoured inflow end and is attached to the base structure in such a way that the valve can be implanted in an intra-atrial position and the taller commissures do not extend too far into the left ventricle, therefore avoiding injury to the ventricle.
Owner:EDWARDS LIFESCIENCES CORP
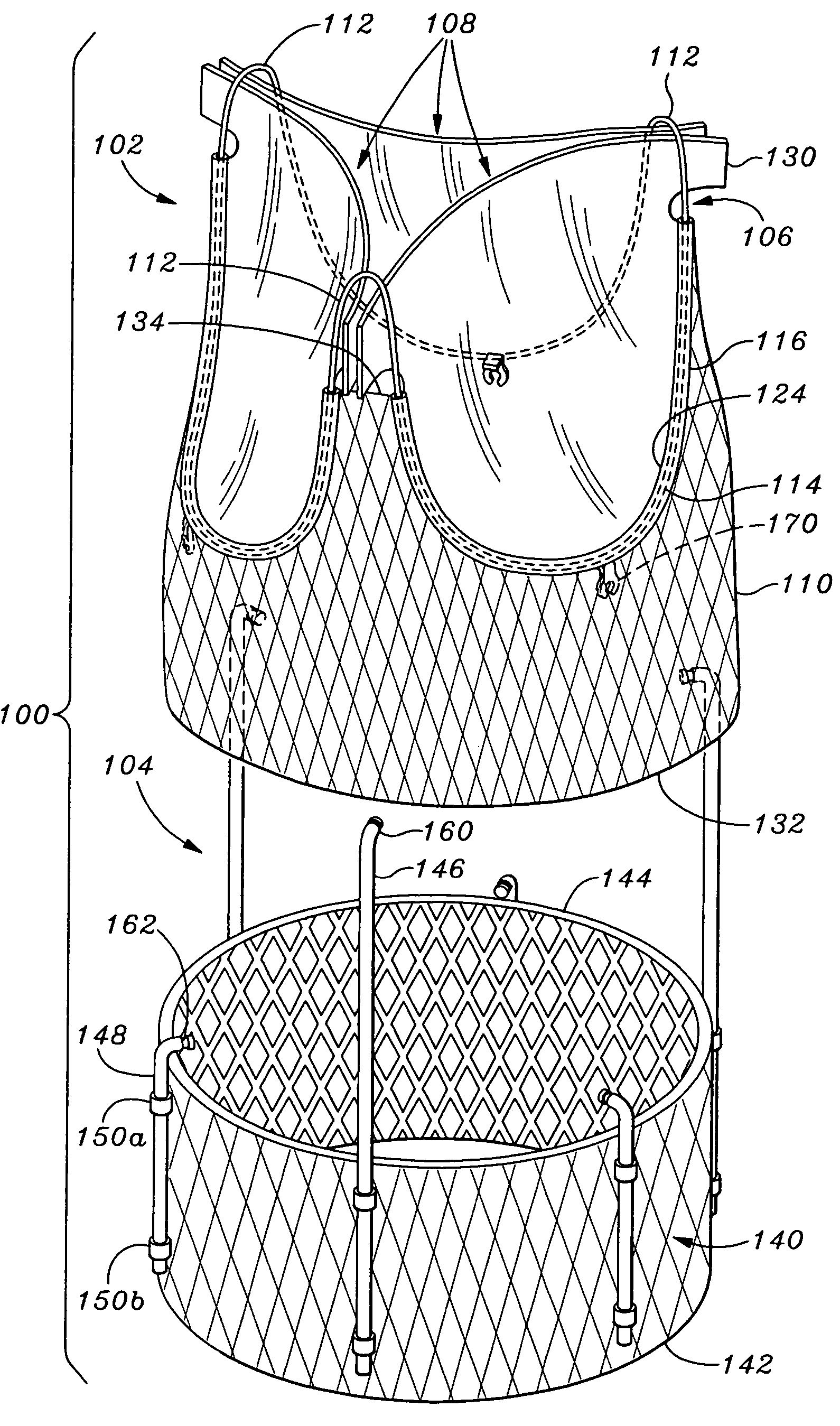
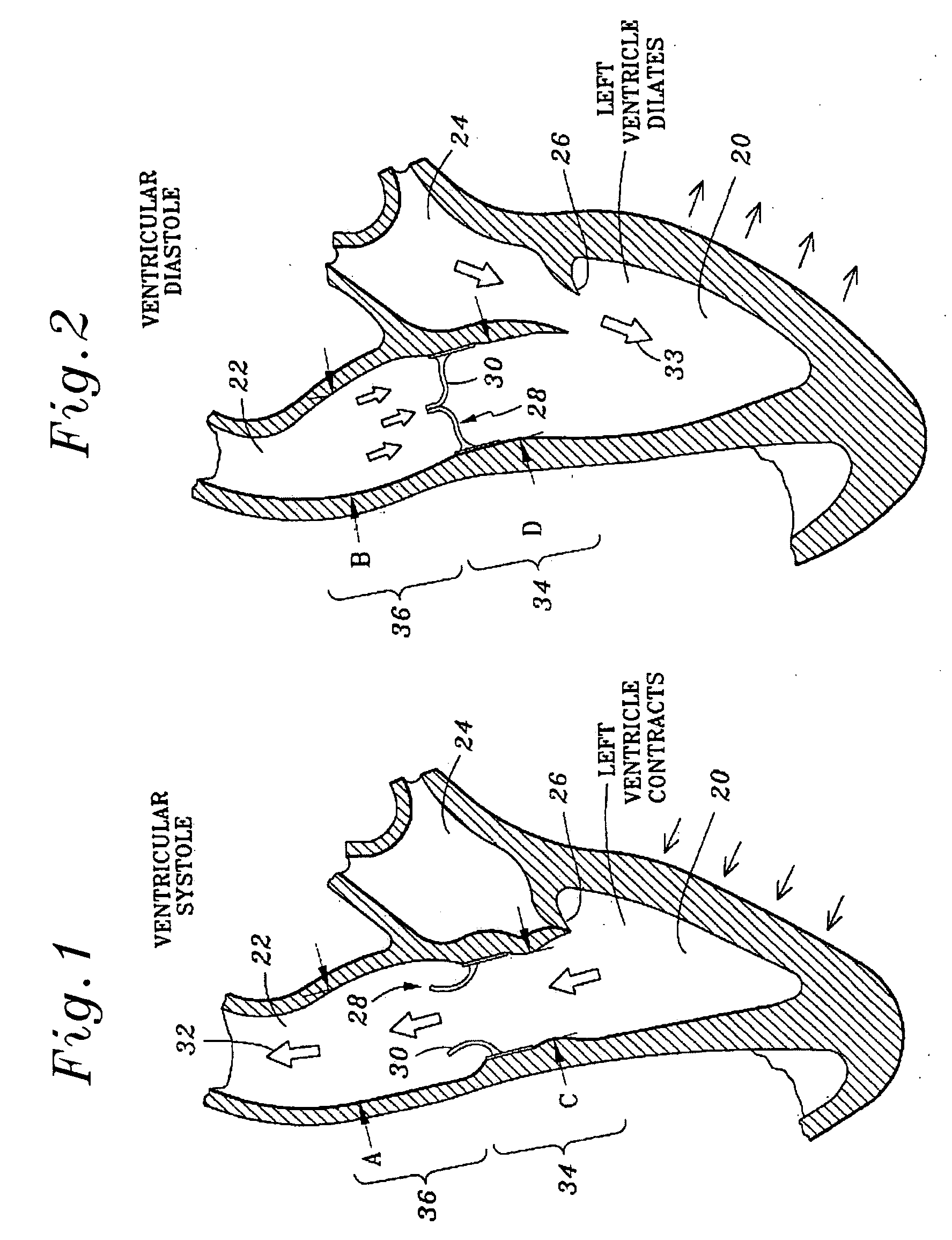
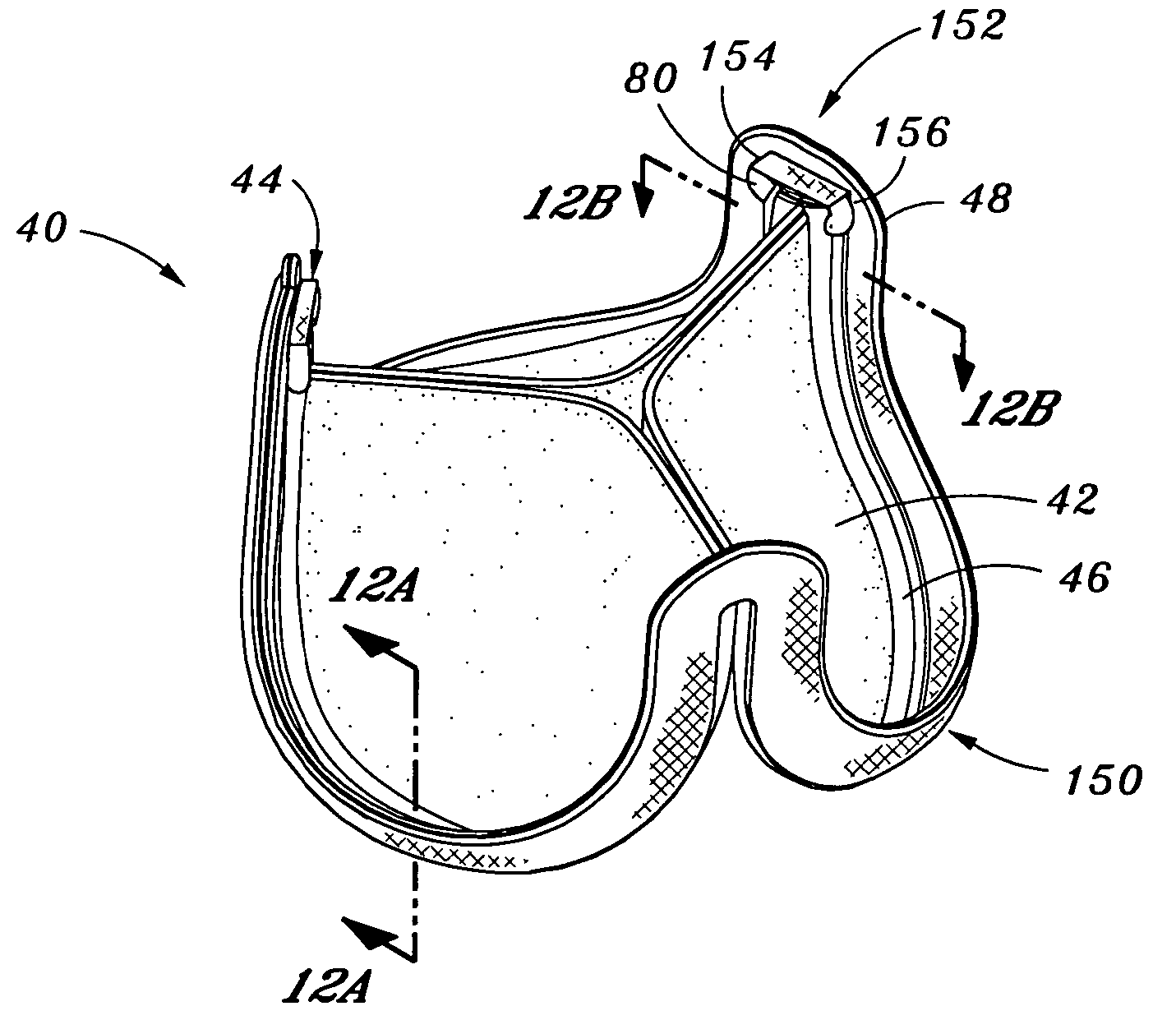
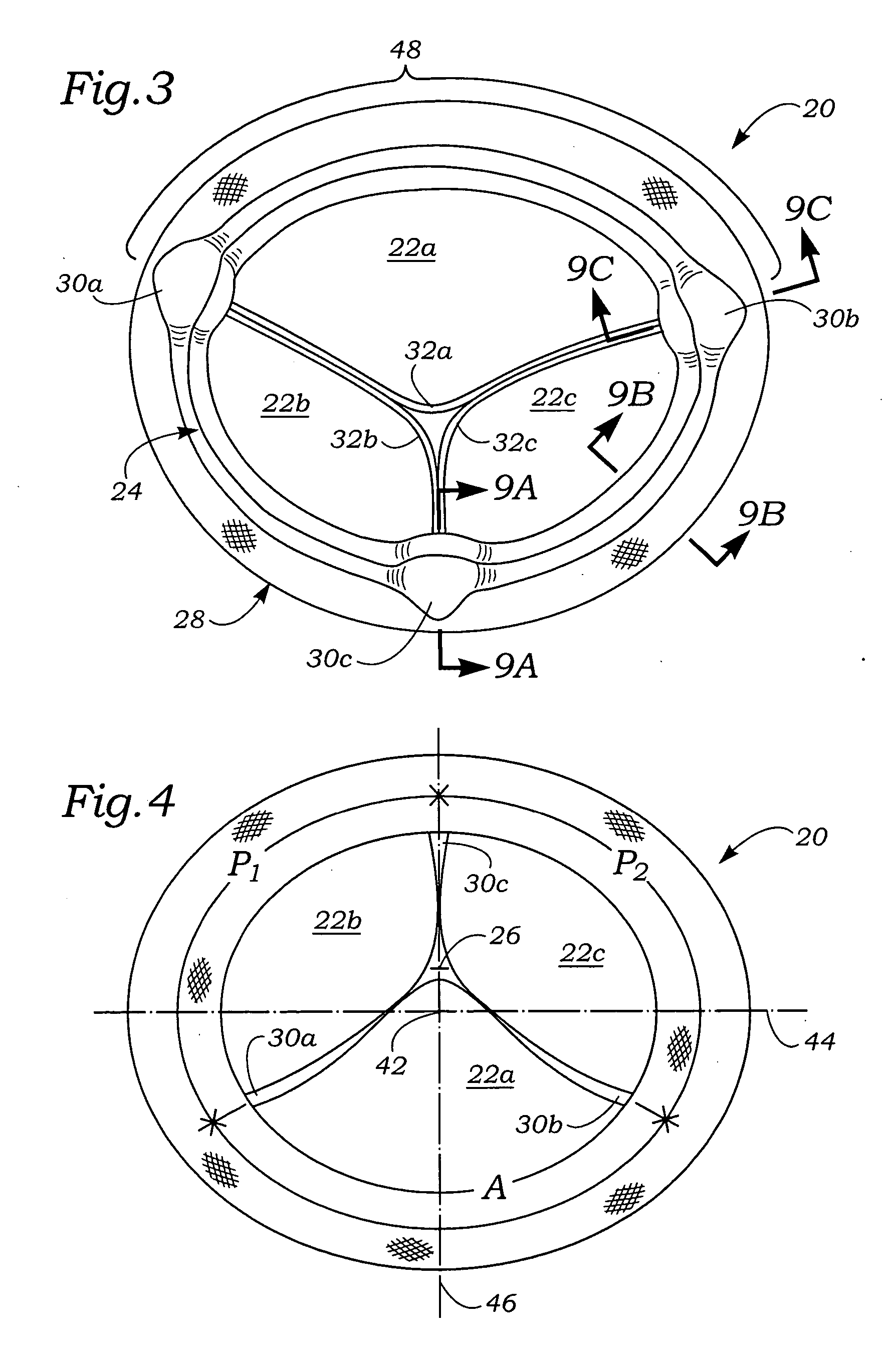
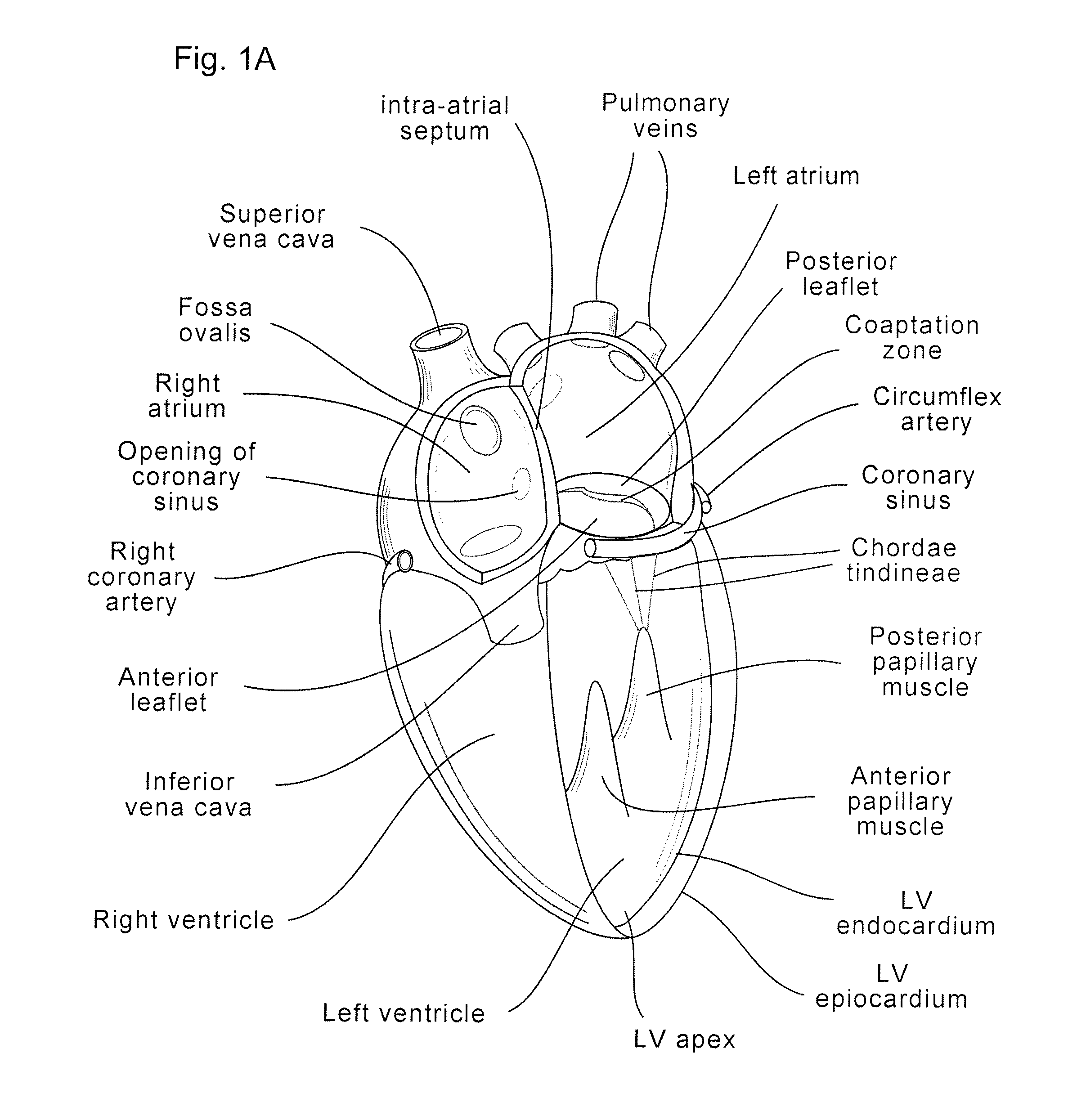
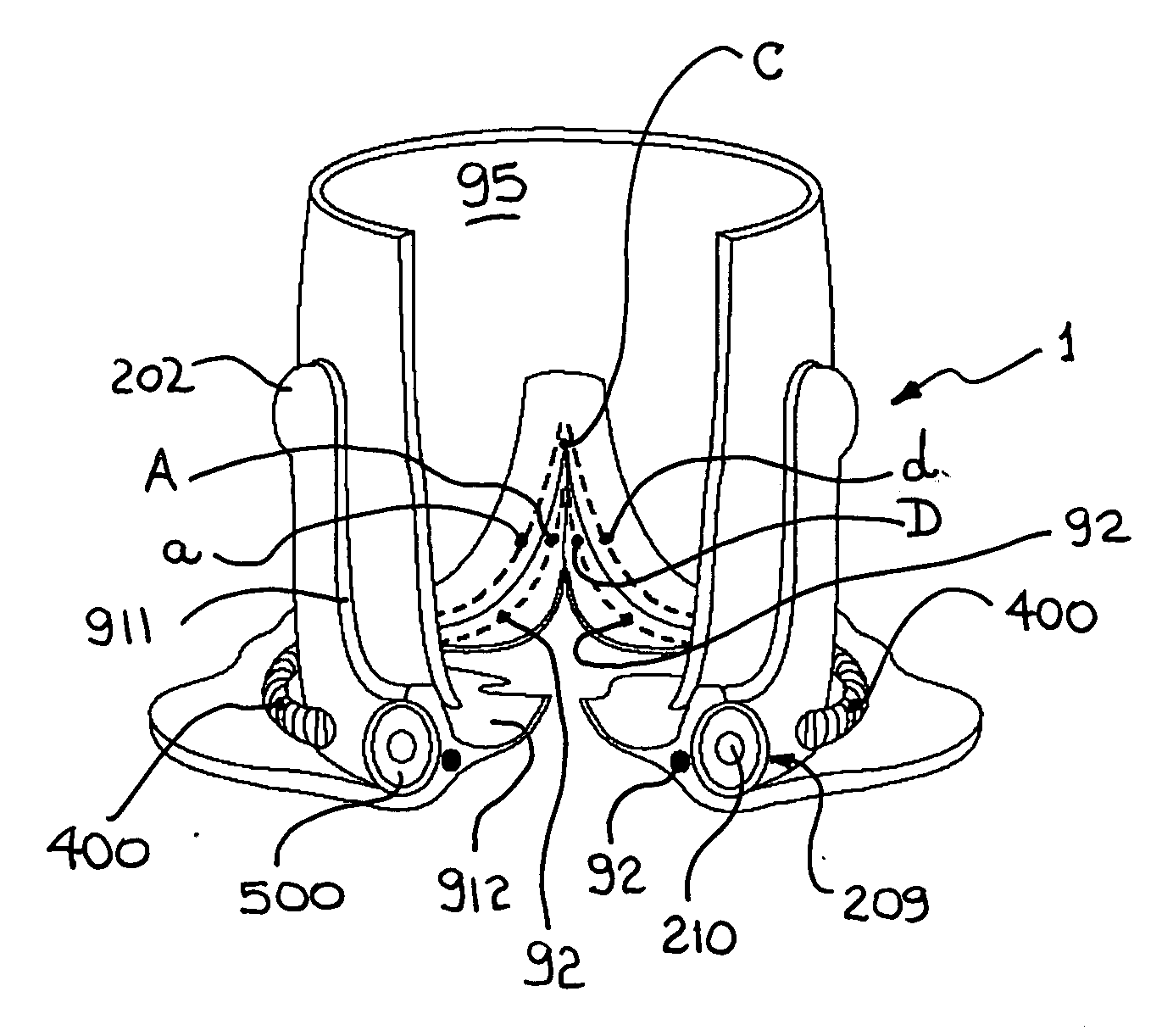
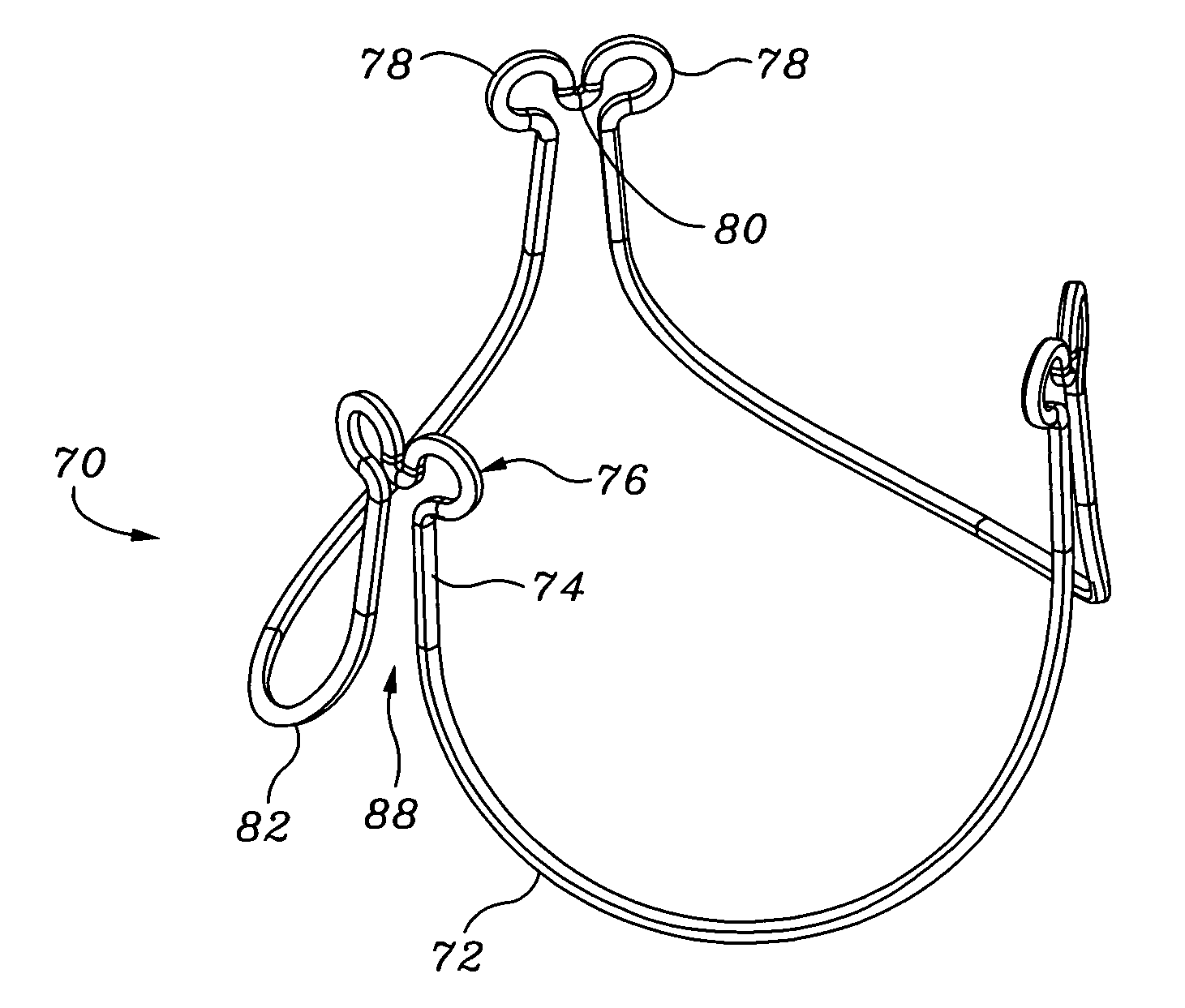
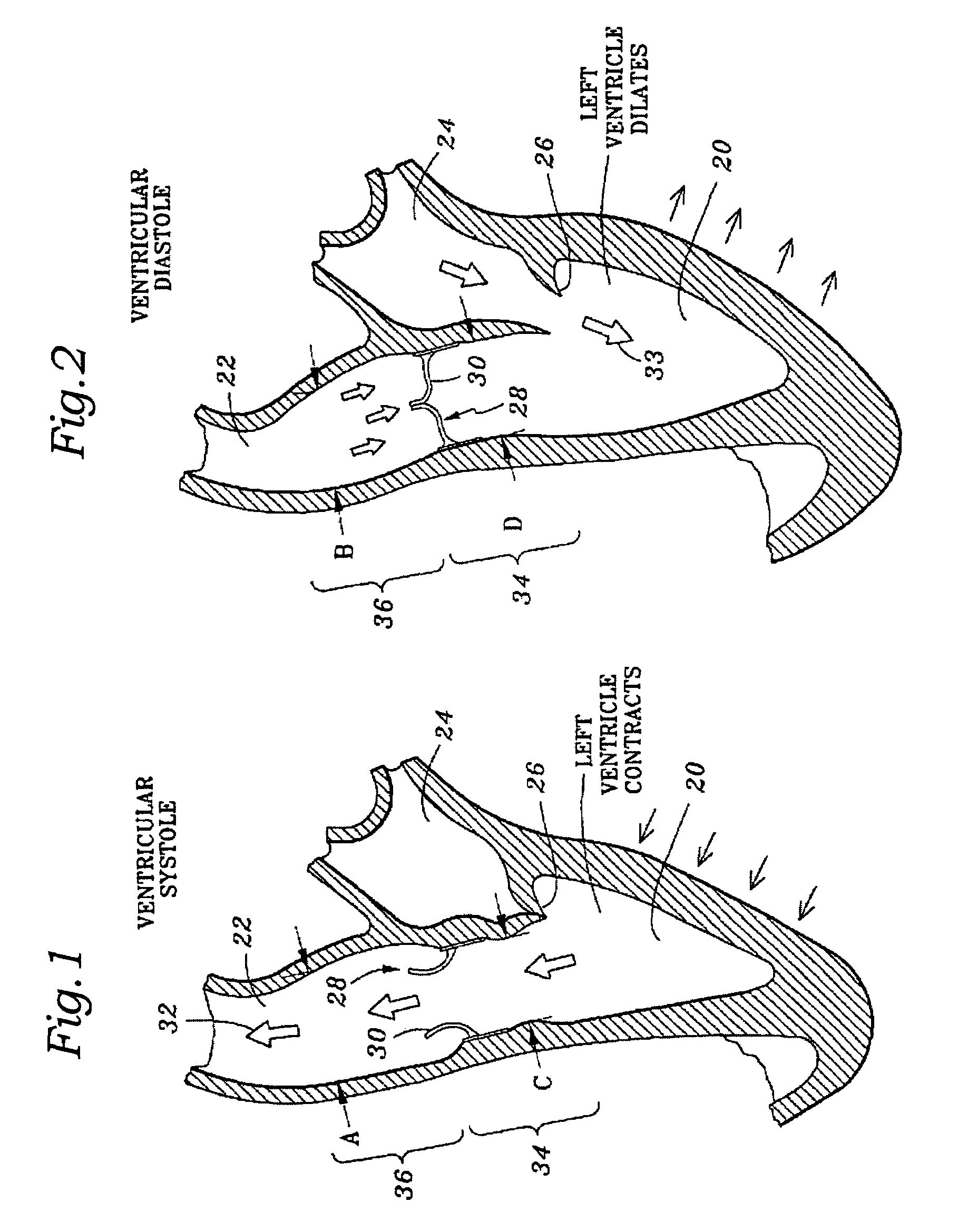
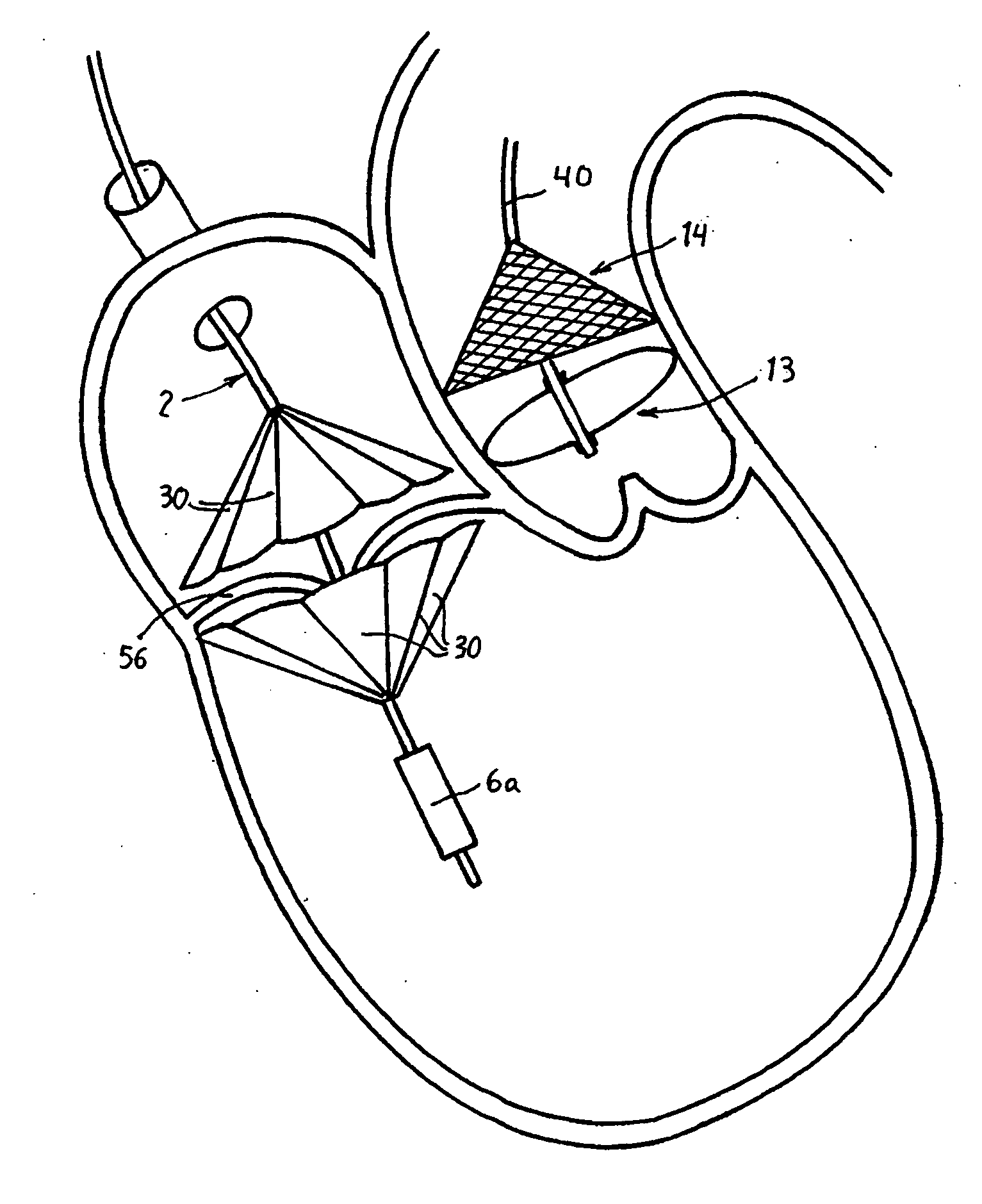
Coaptation enhancement implant, system, and method
ActiveUS8845717B2Safe and effective and operation of valveImprove sealingSuture equipmentsHeart valvesBody shapeCatheter
Implants, implant systems, and methods for treatment of mitral valve regurgitation and other valve diseases generally include a coaptation assist body which remains within the blood flow path as the leaflets of the valve move, the valve bodies often being relatively thin, elongate (along the blood flow path), and / or conformable structures which extend laterally from commissure to commissure, allowing the native leaflets to engage and seal against the large, opposed surfaces on either side of the valve body during the heart cycle phase when the ventricle contracts to empty that chamber of blood, and allows blood to pass around the valve body so that blood flows from the atrium to the ventricle during the filling phase of the heart cycle. Separate deployment of independent anchors near each of the commissures may facilitate positioning and support of an exemplary triangular valve body, with a third anchor being deployed in the ventricle. An outer surface of the valve body may accommodate tissue ingrowth or endothelialization, while a fluid-absorbing matrix can swell after introduction into the heart. The valve body shape may be selected after an anchor has been deployed, and catheter-based deployment systems may have a desirable low profile.
Owner:POLARES MEDICAL INC
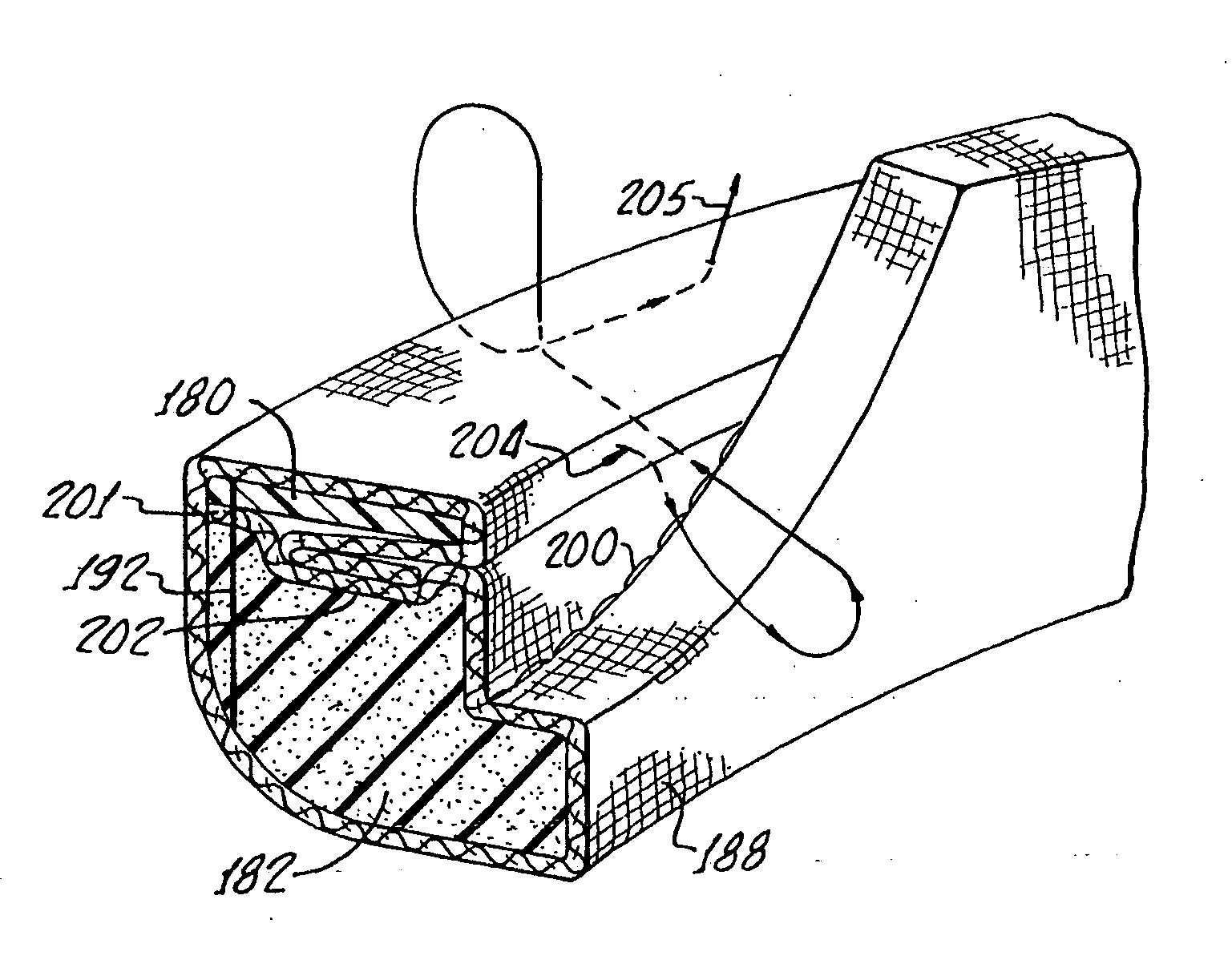
Aortic annuloplasty ring
ActiveUS20060015179A1Preserve and restore normal aortic rootPreserve and restore and valve leafletAnnuloplasty ringsBlood vesselsCardiac cycleAnnuloplasty rings
An annuloplasty ring to resize a dilated aortic root during valve sparing surgery includes a scalloped space frame having three trough sections connected to define three crest sections. The annuloplasty ring is mounted outside the aortic root, and extends in height between a base plane and a spaced apart commissure plane of the aortic root. At least two adjacent trough sections are coupled by an annulus-restraining member or tether that limits the maximum deflection of the base of the annuloplasty ring. In use, the tether is preferably located in proximity to the base plane of the aortic root. The annuloplasty ring is movable between a first, substantially conical configuration occurring during a diastolic phase of the cardiac cycle, and a second, substantially cylindrical configuration occurring during a systolic phase of the cardiac cycle. The attachment of the annuloplasty ring in proximity to the cardiac valve annulus allows the ring to regulate the dimensions of a dynamic aortic root during the different phases of the cardiac cycle.
Owner:CORONEO
Stress absorbing flexible heart valve frame
ActiveUS7473275B2Facilitate such flexionFacilitates a supra-annular implant techniqueHeart valvesMedicineProsthetic heart
A flexible support frame for a prosthetic heart valve having commissure tips that are shaped to even out stresses imposed during use. The support frame is an elongated wire-like element formed by a plurality, typically three, of arcuate cusp regions on an inflow end alternating with the same number of commissures terminating in tips on an outflow end. The commissure tips are elongated relative to more simple shapes. The commissure tips may be shaped with a complex curve having two enlarged convex flexure portions separated by a concave bridge portion at the midpoint of the commissure tip. The support frame may be fabricated by separating a two-dimensional blank from a sheet and then converting the blank into a three-dimensional support frame shape. The cross-sectional thickness of the support frame may be variable, such as by adjusting the thickness of the pattern of the two-dimensional blank in the sheet. Desirably, the radial thickness remains constant while the circumferential dimension varies with a maximum located at the commissure tips.
Owner:EDWARDS LIFESCIENCES CORP
Contoured heart valve suture rings
InactiveUS20060009842A1Improving long-term functionalityReduce pointsHeart valvesInsertion stentCatheter
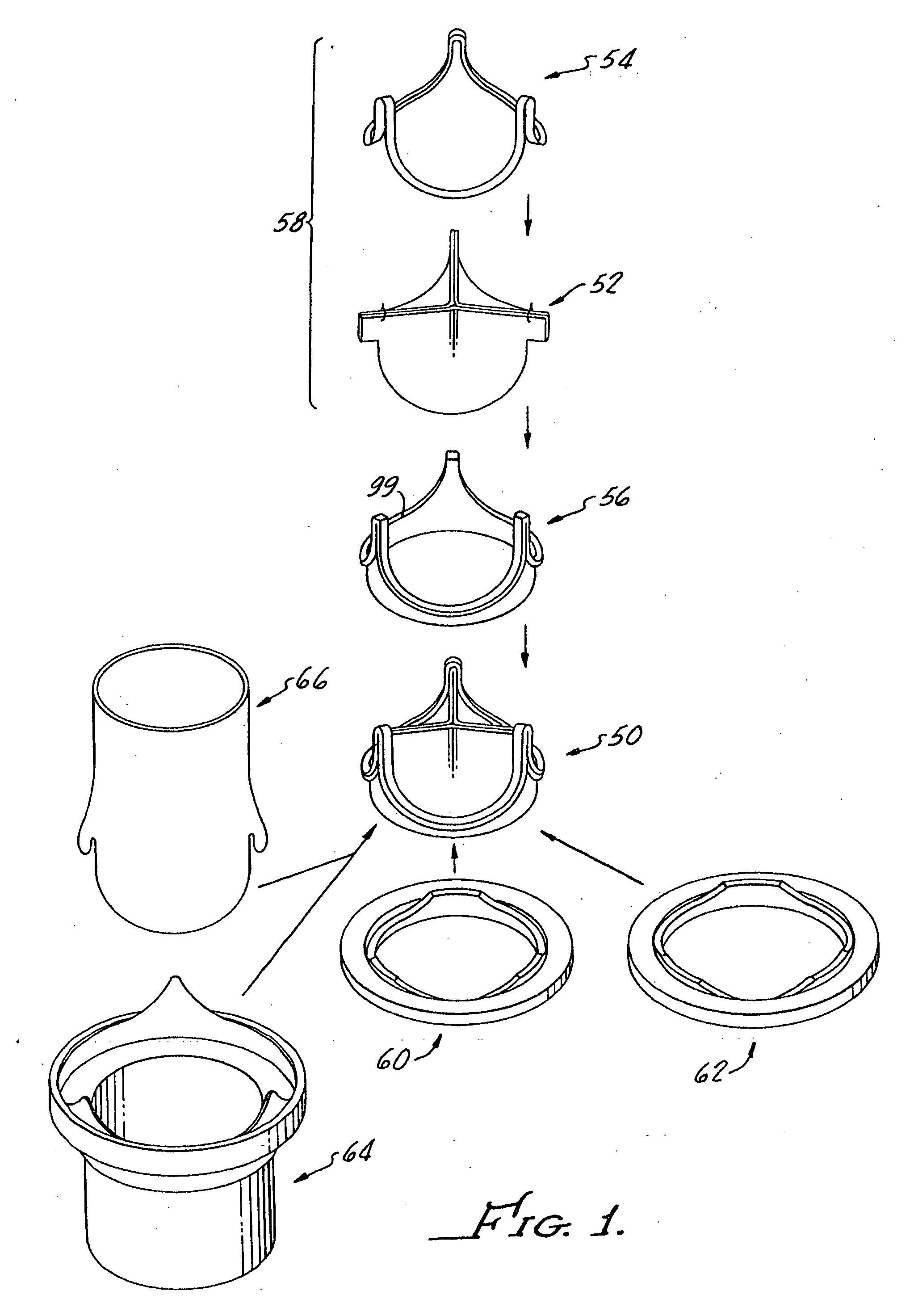
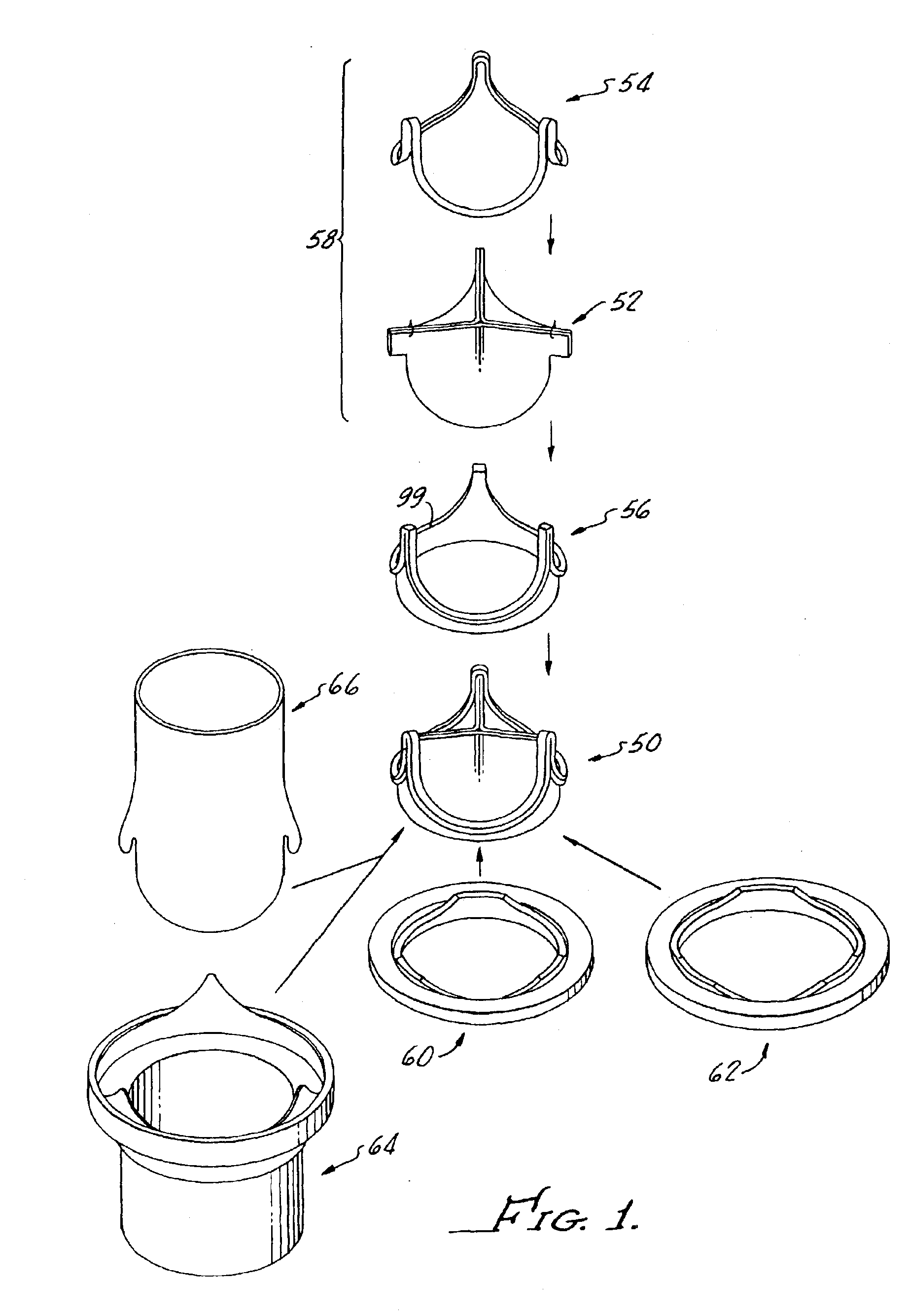
Improved, adaptable tissue-type heart valves and methods for their manufacture are disclosed wherein a dimensionally stable, pre-aligned tissue leaflet subassembly is formed and its peripheral edge clamped between and attached to an upper shaped wireform and a lower support stent. A variety of adaptable structural interfaces including suture rings, flanges, and conduits may be attached to the support stent with or without an outlet conduit disposed about the wireform to provide a tissue-type heart valve adaptable for use in either a natural heart or in mechanical pumping devices. The methods include forming individual leaflets with a template and using the template to attach the leaflets together to form a tissue leaflet subassembly. The template and leaflets include a straight edge terminating in oppositely directed tabs, and a curvilinear cusp edge extending opposite the straight edge. The template may include a guide slot in its straight edge and the assembly includes aligning two leaflet tabs with the template and passing sutures through the guide slot and through the leaflet tabs. The leaflet subassembly is mated to a wireform with the tabs extending through commissure posts of the wireform. A support stent having an upper surface matching the lower surface of the wireform sandwiches the edges of the leaflet subassembly therebetween. Separated tabs on the leaflet subassembly are passed through the wireform commissures and attached to adjacent stent commissures so as to induce clamping of the leaflet tabs between the stent commissures and wireform commissures upon a radially inward force being applied to the leaflets.
Owner:EDWARDS LIFESCIENCES CORP
Heart valves and suture rings therefor
InactiveUS6945997B2Reduce stress pointImproving long-term functionalityHeart valvesInsertion stentTissues types
Improved, adaptable tissue-type heart valves and methods for their manufacture are disclosed wherein a dimensionally stable, pre-aligned tissue leaflet subassembly is formed and its peripheral edge clamped between and attached to an upper shaped wireform and a lower support stent. A variety of adaptable structural interfaces including suture rings, flanges, and conduits may be attached to the support stent with or without an outlet conduit disposed about the wireform to provide a tissue-type heart valve adaptable for use in either a natural heart or in mechanical pumping devices. The methods include forming individual leaflets with a template and using the template to attach the leaflets together to form a tissue leaflet subassembly. The template and leaflets include a straight edge terminating in oppositely directed tabs, and a curvilinear cusp edge extending opposite the straight edge. The template may include a guide slot in its straight edge and the assembly includes aligning two leaflet tabs with the template and passing sutures through the guide slot and through the leaflet tabs. The leaflet subassembly is mated to a wireform with the tabs extending through commissure posts of the wireform. A support stent having an upper surface matching the lower surface of the wireform sandwiches the edges of the leaflet subassembly therebetween. Separated tabs on the leaflet subassembly are passed through the wireform commissures and attached to adjacent stent commissures so as to induce clamping of the leaflet tabs between the stent commissures and wireform commissures upon a radially inward force being applied to the leaflets.
Owner:EDWARDS LIFESCIENCES CORP
Coaptation enhancement implant, system, and method
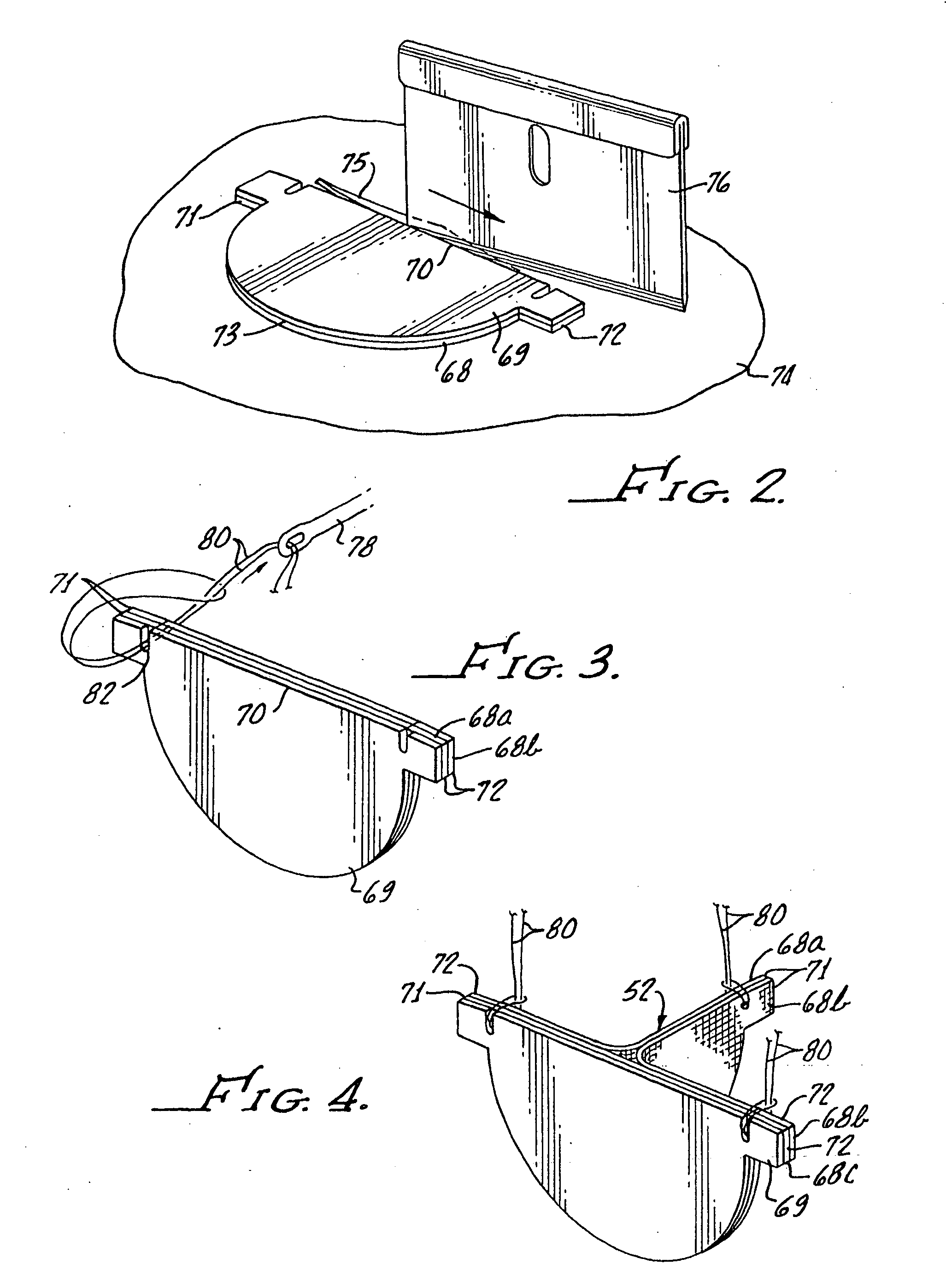
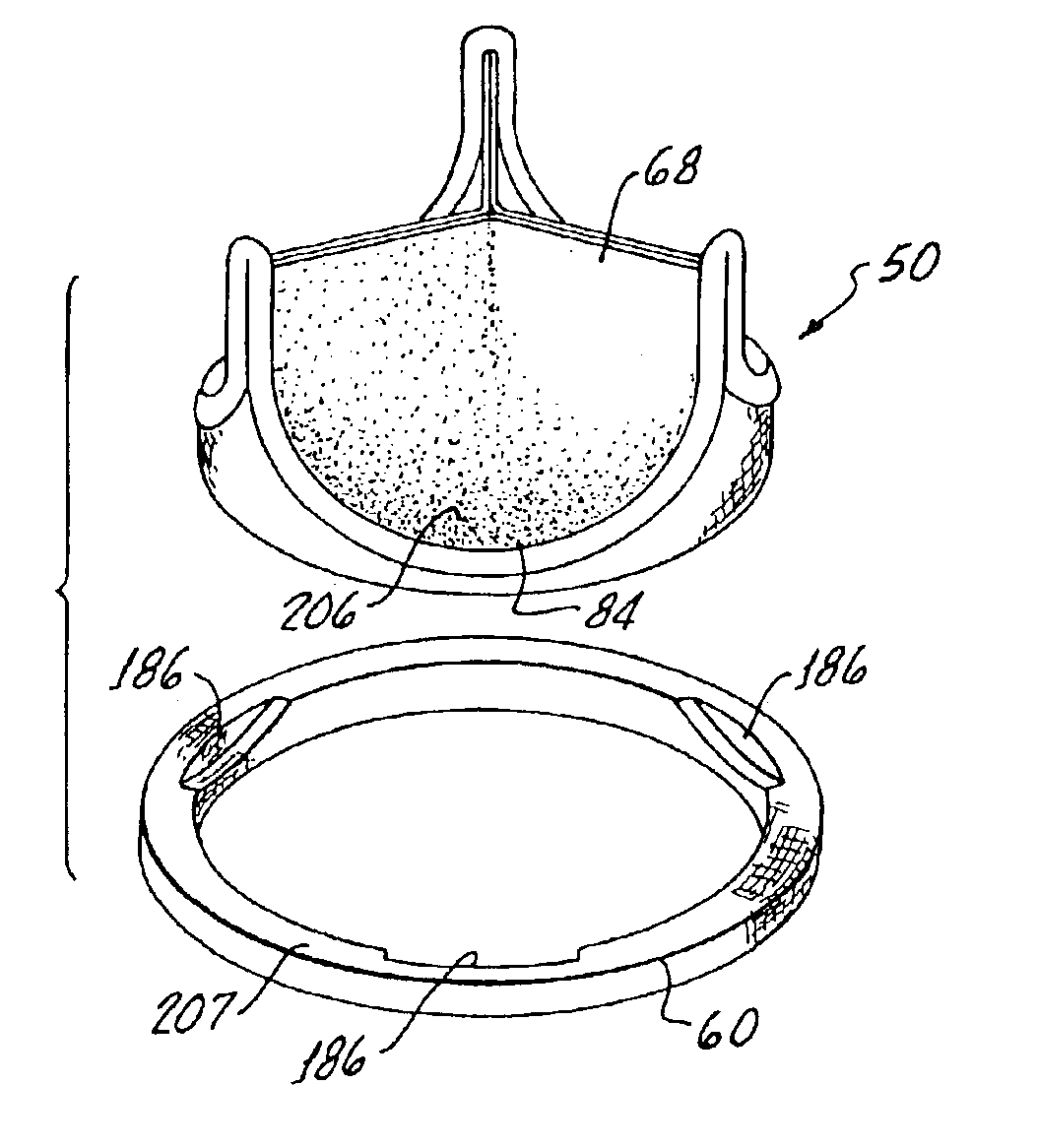
ActiveUS20120197388A1Mal-coaptation is mitigatedImprove valve functionSuture equipmentsBone implantBody shapeAbdominal cavity
Implants, implant systems, and methods for treatment of mitral valve regurgitation and other valve diseases generally include a coaptation assist body which remains within the blood flow path as the leaflets of the valve move, the valve bodies often being relatively thin, elongate (along the blood flow path), and / or conformable structures which extend laterally from commissure to commissure, allowing the native leaflets to engage and seal against the large, opposed surfaces on either side of the valve body during the heart cycle phase when the ventricle contracts to empty that chamber of blood, and allows blood to pass around the valve body so that blood flows from the atrium to the ventricle during the filling phase of the heart cycle. Separate deployment of independent anchors near each of the commissures may facilitate positioning and support of an exemplary triangular valve body, with a third anchor being deployed in the ventricle. An outer surface of the valve body may accommodate tissue ingrowth or endothelialization, while a fluid-absorbing matrix can swell after introduction into the heart. The valve body shape may be selected after an anchor has been deployed, and catheter-based deployment systems may have a desirable low profile.
Owner:POLARES MEDICAL INC
Sigmoid valve and method for its percutaneous implantation
Owner:THE INT HEART INST OF MONTANA FOUND
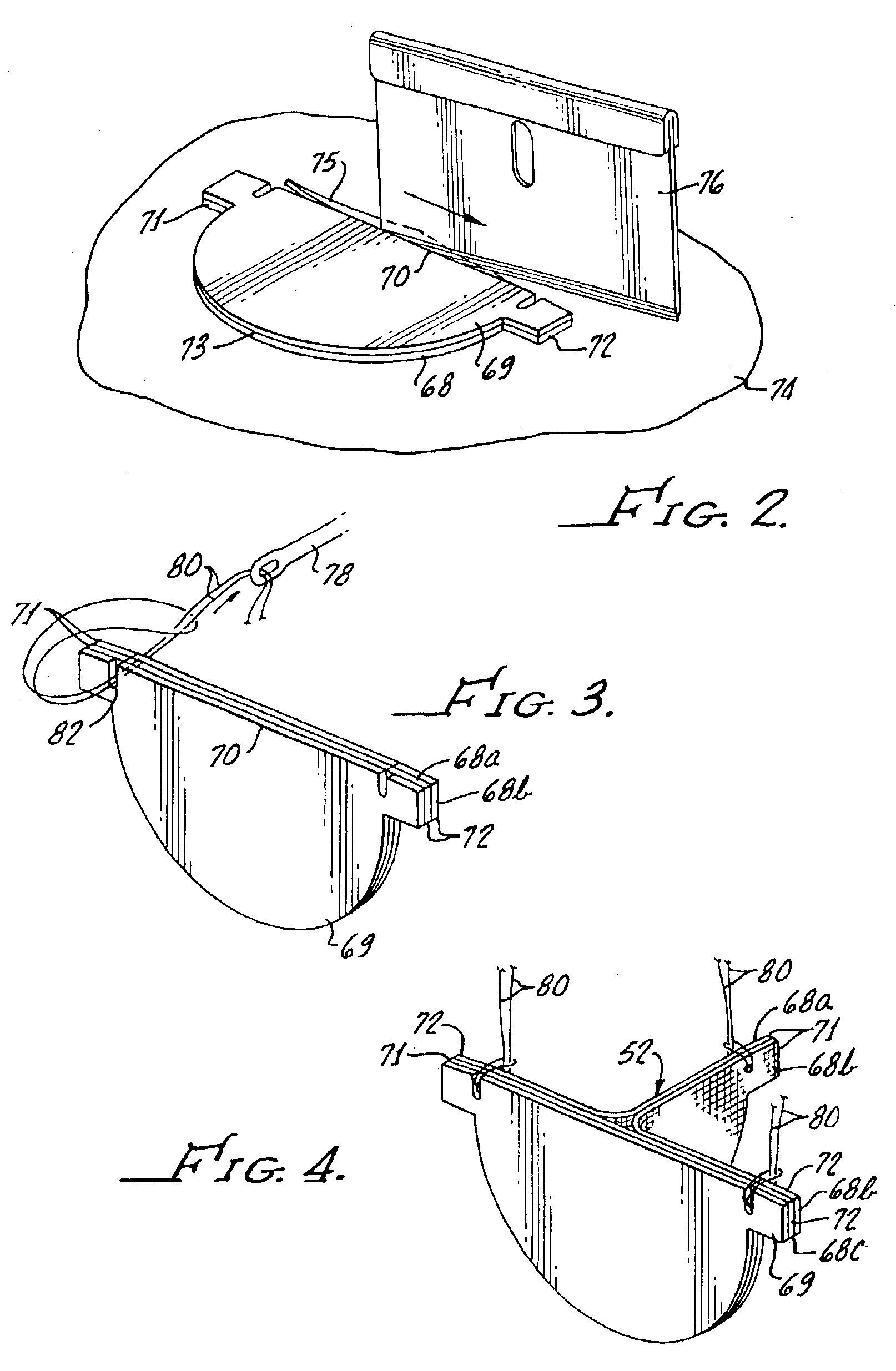
Heart valve holder and method for resisting suture looping
An improved holder and method for implanting a tissue-type prosthetic mitral heart valve that prevents suture looping and may also constrict the commissure posts of the valve. An upstanding or shaft member axially positioned on the holder causes the lengths of attachment sutures to extend axially beyond the commissure post tips to create a tent and prevent looping of any of an array of pre-implanted sutures around the tips during deployment of the valve. The shaft member may be axially movable such that it can be initially retracted and then actuated just prior to valve deployment. The shaft member may have notches on its distal tip for capturing the attachment sutures, which are crossed over along the valve axis to ensure engagement by the notches. The attachment sutures may be strands or filaments, or may be wider bands of flexible biocompatible material. If bands are used, they desirably cover the commissure post tips to further help prevent suture looping thereover. The flexible lengths of material extend directly between commissures of the valve, or may extending radially inward from each commissure to a central upstanding member.
Owner:EDWARDS LIFESCIENCES CORP
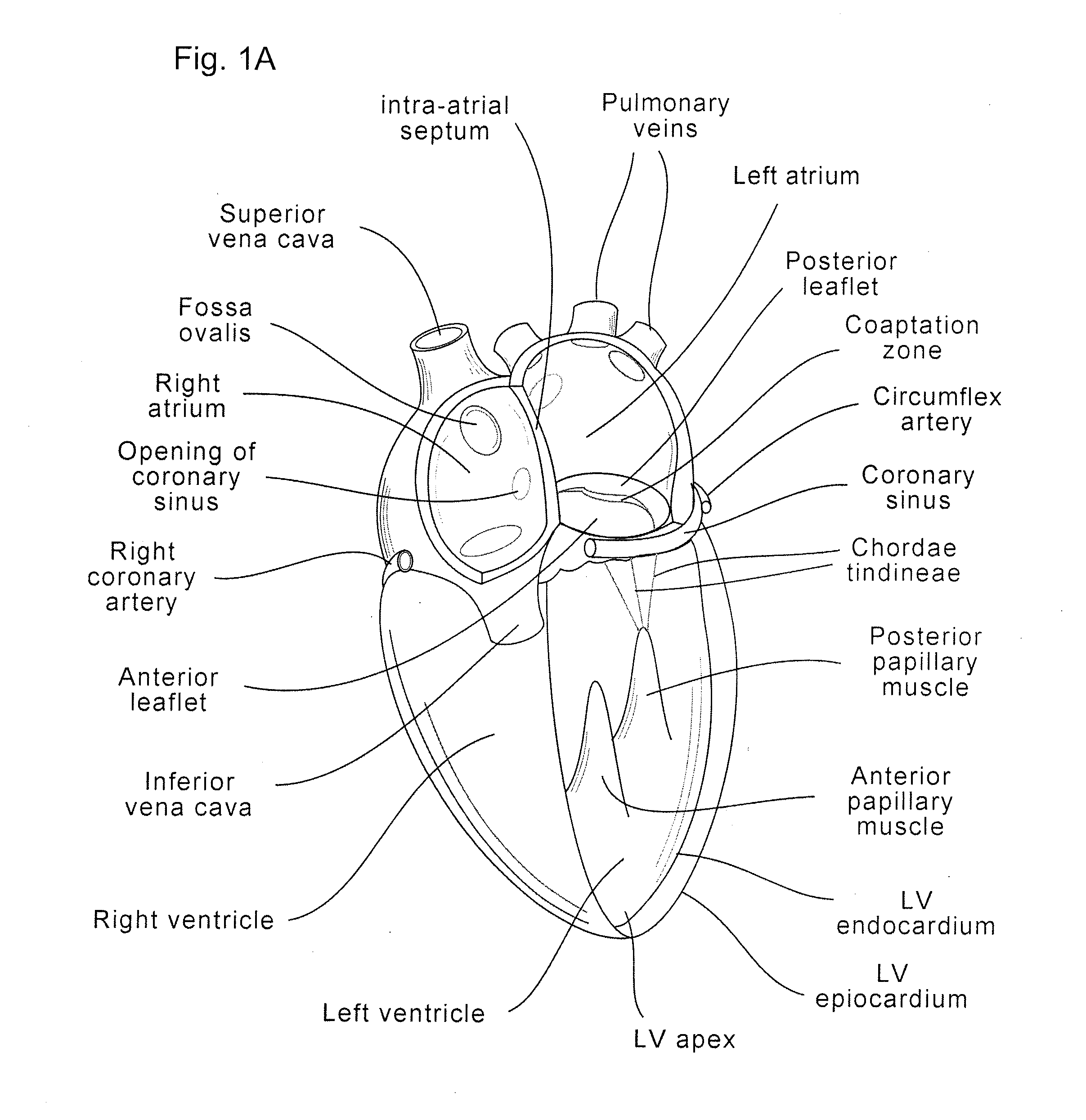
Anatomically Approximate Prosthetic Mitral Valve
ActiveUS20110015731A1Increase the areaReduce the overall heightAnnuloplasty ringsProsthetic heartLeft ventricle wall
An anatomically approximate prosthetic heart valve includes dissimilar flexible leaflets, dissimilar commissures and / or a non-circular flow orifice. The heart valve may be implanted in the mitral position and have one larger leaflet oriented along the anterior aspect so as to mimic the natural anterior leaflet. Two other smaller leaflets extend around the posterior aspect of the valve. A basic structure providing peripheral support for the leaflets includes two taller commissures on both sides of the larger leaflet, with a third, smaller commissure between the other two leaflets. The larger leaflet may be thicker and / or stronger than the other two leaflets. The base structure defines a flow orifice intended to simulate the shape of the mitral annulus during the systolic phase. For example, the flow orifice may be elliptical. A relatively wide sewing ring has a contoured inflow end and is attached to the base structure in such a way that the valve can be implanted in an intra-atrial position and the taller commissures do not extend too far into the left ventricle, therefore avoiding injury to the ventricle.
Owner:EDWARDS LIFESCIENCES CORP
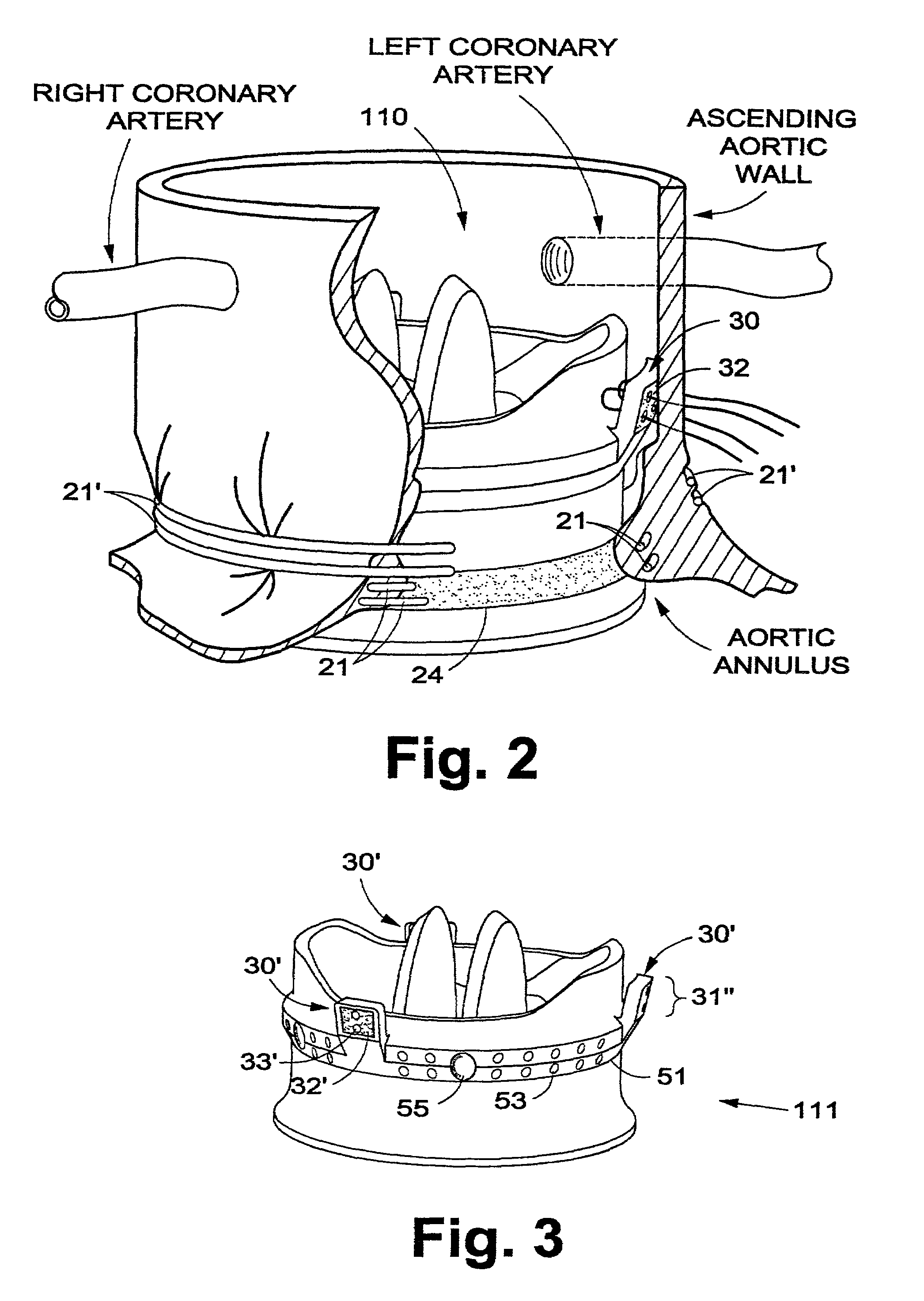
Prosthetic aortic valve
InactiveUS6951573B1Eliminating and minimizing riskHigh mechanical strengthHeart valvesBlood vesselsAscending aortaCoronary arteries
A prosthetic aortic valve is designed to be implanted in the natural aortic annulus and to extend into the ascending aorta to a point short of the right and left coronary arteries. Blood leakage around the valve is prevented by tension in one or more circumferential cords drawing annular tissue into sealing contact with an external sealing ring on the valve body. The security of the valve's attachment to a patient is assured with a plurality of interrupted sutures between a semirigid flange on the valve outer surface and the patient's aortic commissures and / or the patient's ascending aortic wall. The sutures are preferably attached to posts or cleats on the semirigid sewing flange, the flange being spaced apart from the valve inlet by the sealing ring.
Owner:DILLING EMERY W
Four-leaflet stented mitral heart valve
A prosthetic mitral heart valve having four separate flexible leaflets. The heart valve includes a support frame that may be non-circular, for example elliptical or “D-shaped”. The support frame may have an undulating outflow edge defined by four inflow cusps and four outflow commissures to which each of the flexible leaflets attaches. The support frame may comprise an undulating wireform and a surrounding stent defining a structure having four cantilevered posts projecting in the outflow direction to support the four leaflets. The heart valve is designed to be secured in the annulus and function as a standalone unit without papillary muscle connections to the leaflets. The four leaflets may be arranged in two opposed pairs, one pair being smaller than the other pair. The larger pair of leaflets may be identical, or differently sized. Existing sizes of heart valve leaflets may be utilized with the smaller leaflets being at least two leaflet sizes smaller than the larger leaflets in odd millimeter increments.
Owner:EDWARDS LIFESCIENCES CORP
Prosthetic valve for transluminal delivery
InactiveUS20060129235A1Preventing substantial migrationEliminate the problemBalloon catheterHeart valvesProsthesisCommissure
A prosthetic valve assembly for use in replacing a deficient native valve comprises a replacement valve supported on an expandable valve support. If desired, one or more anchor may be used. The valve support, which entirely supports the valve annulus, valve leaflets, and valve commissure points, is configured to be collapsible for transluminal delivery and expandable to contact the anatomical annulus of the native valve when the assembly is properly positioned. The anchor engages the lumen wall when expanded and prevents substantial migration of the valve assembly when positioned in place. The prosthetic valve assembly is compressible about a catheter, and restrained from expanding by an outer sheath. The catheter may be inserted inside a lumen within the body, such as the femoral artery, and delivered to a desired location, such as the heart. When the outer sheath is retracted, the prosthetic valve assembly expands to an expanded position such that the valve and valve support expand within the deficient native valve, and the anchor engages the lumen wall.
Owner:MEDTRONIC COREVALVE
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com