Patents
Literature
384 results about "Tissues types" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
In humans, there are four basic types of tissue: epithelial, connective, muscular, and nervous tissue. There may be various sub-tissues within each of the primary tissues. Epithelial tissue covers the body surface and forms the lining for most internal cavities.
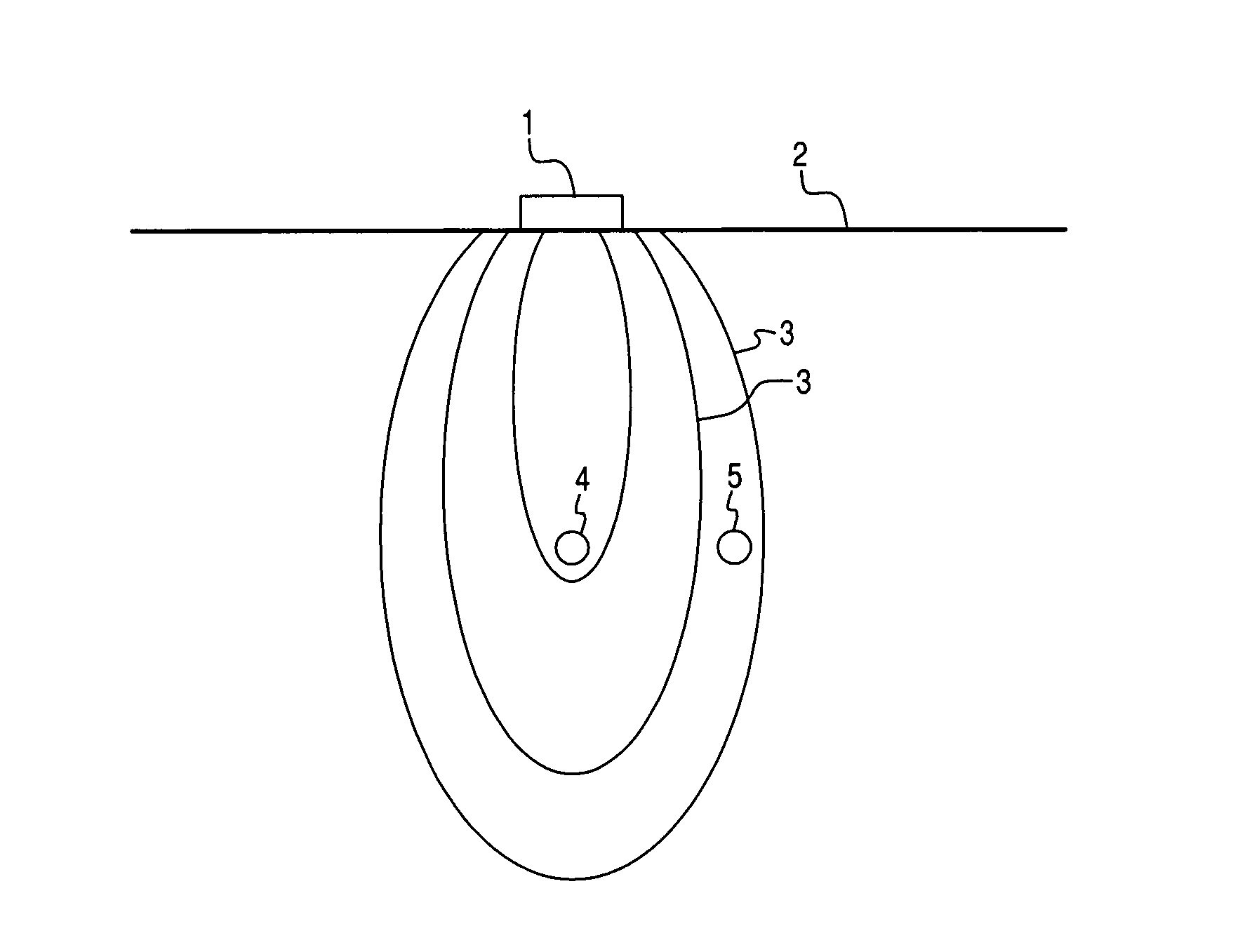
Active electrode, bio-impedance based, tissue discrimination system and methods of use
InactiveUS20060085049A1Accurate identificationAvoid problemsElectrotherapyDiagnostic recording/measuringElectricityTissues types
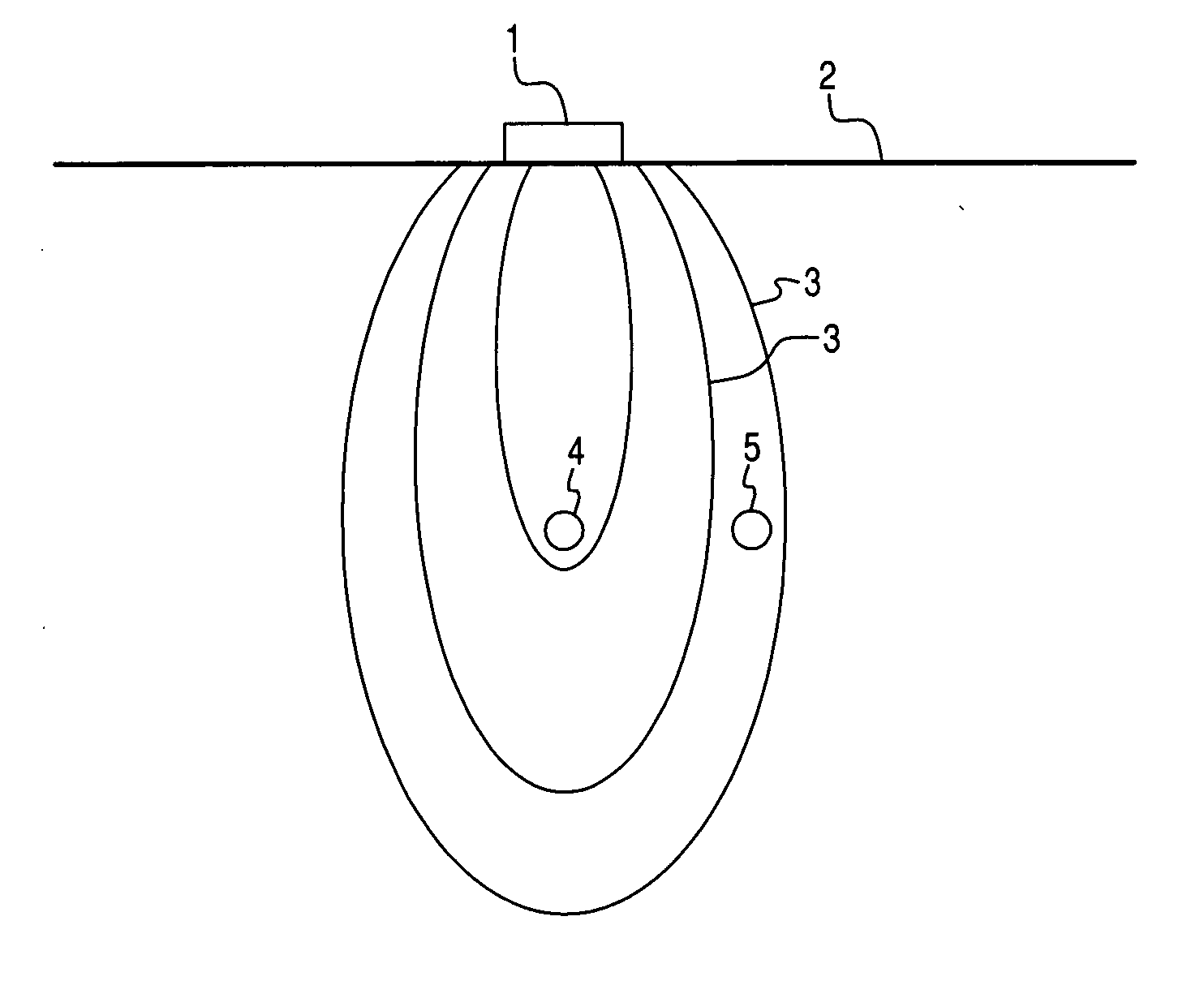
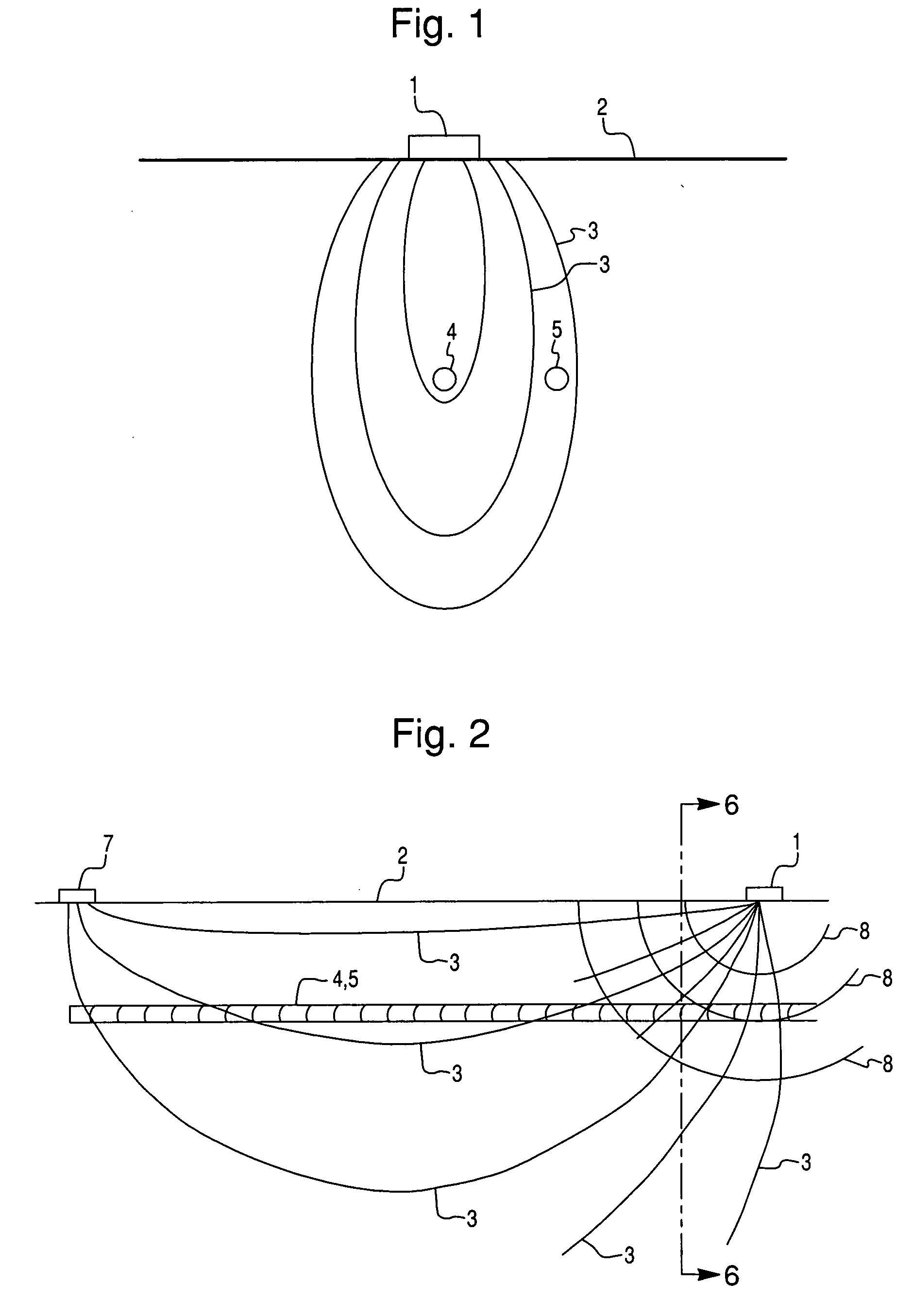
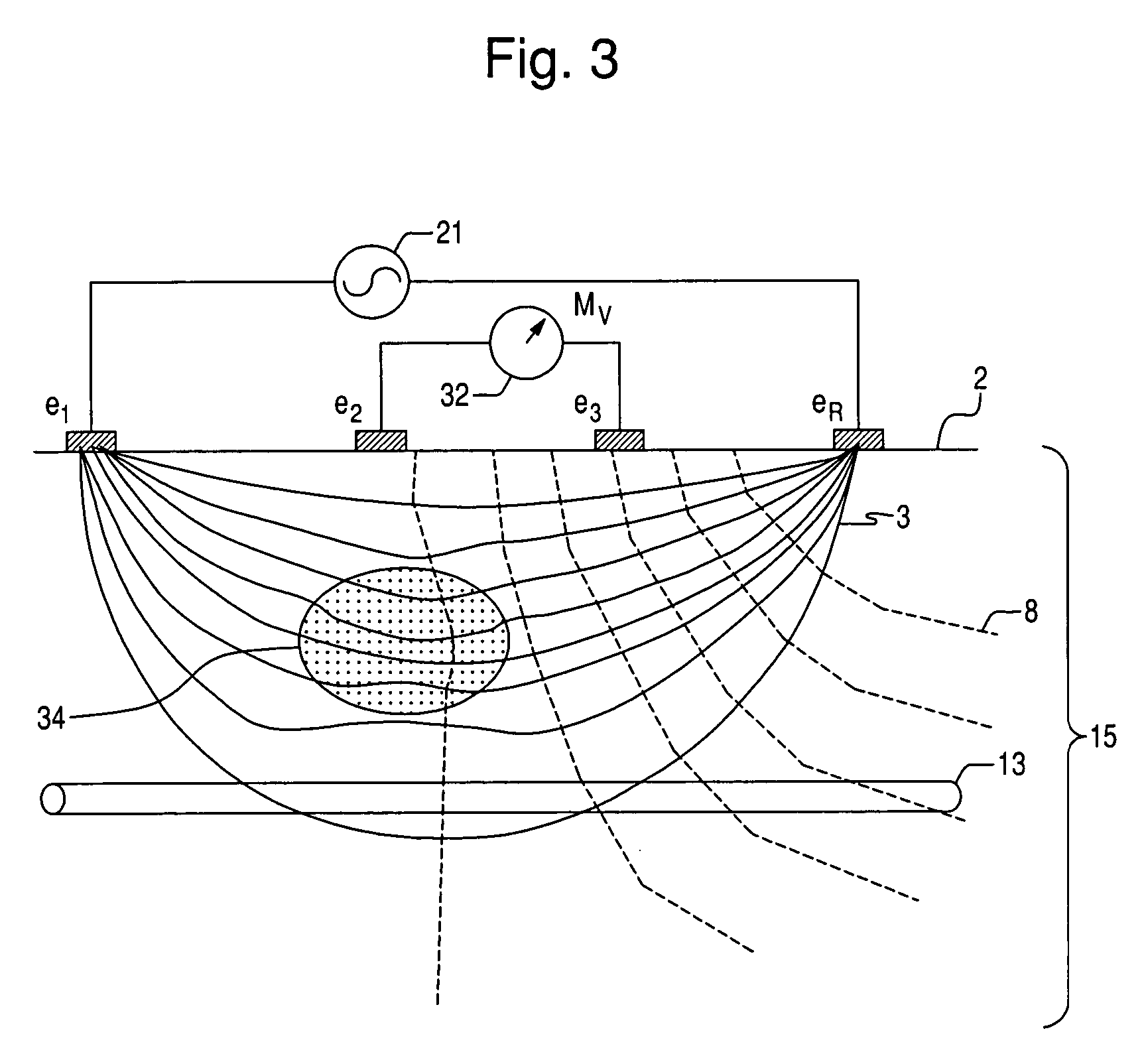
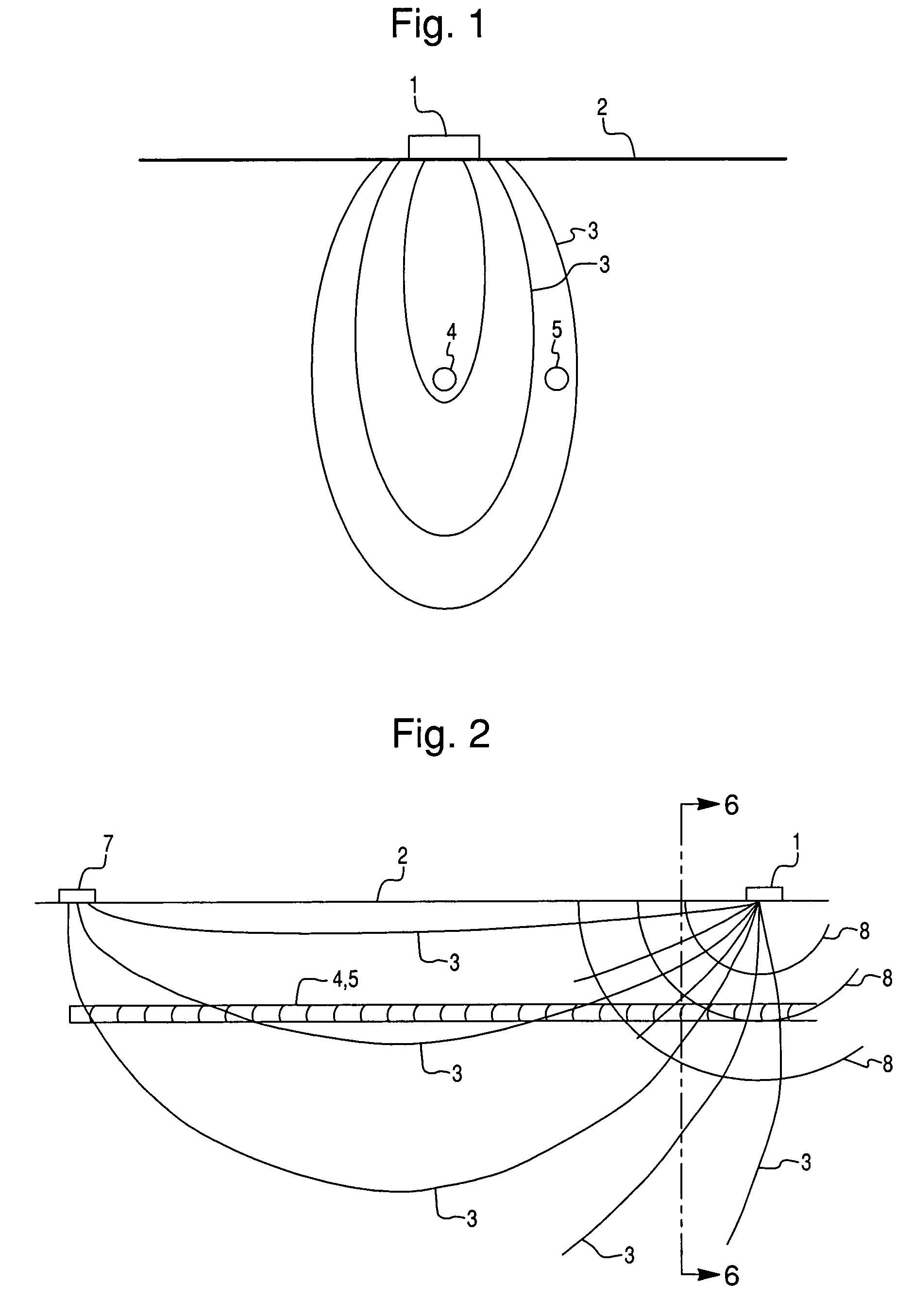
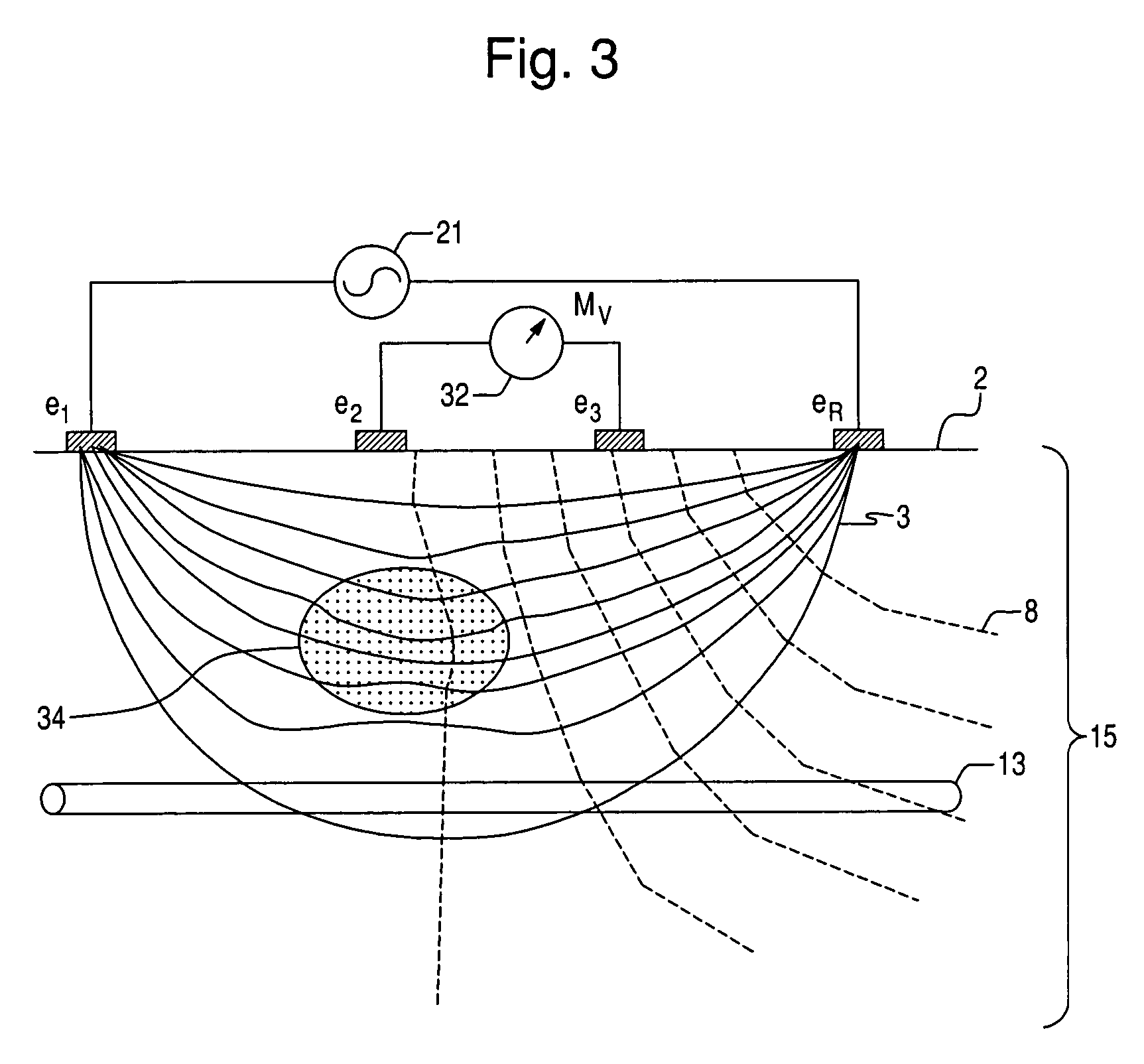
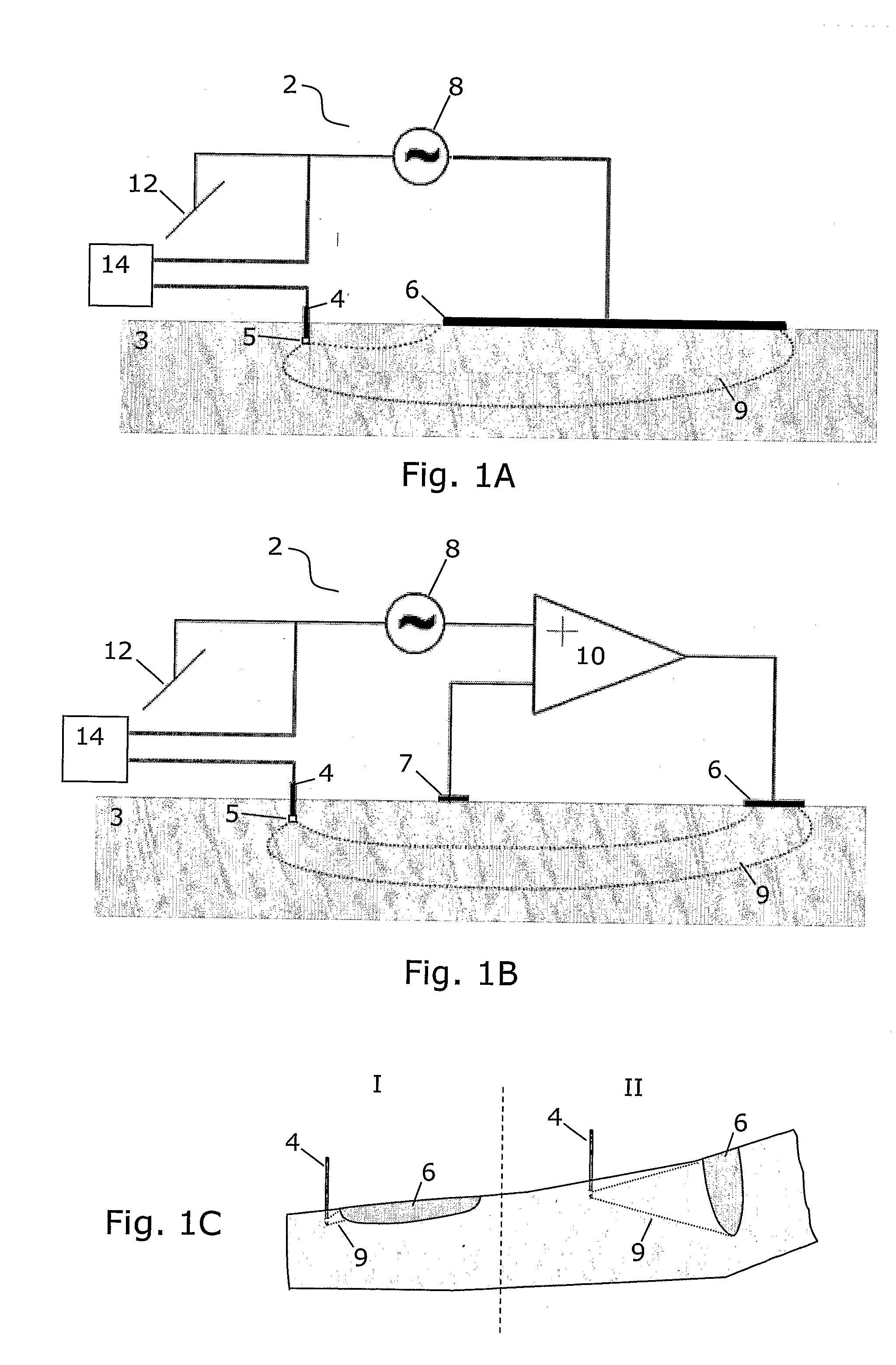
Systems and methods for discriminating and locating tissues within a body involve applying a waveform signal to tissue between two electrodes and measuring the electrical characteristics of the signal transmitted through the tissue. At least one of the electrodes is constrained in area so that localized electrical characteristics of the tissue are measured. Such localized electrical characteristics are determined over a portion of a body of the subject by using an array of electrodes or electrodes that can be moved over the body. A controller may implement the process and perform calculations on the measured data to identify tissue types and locations within the measured area, and to present results in graphical form. Results may be combined with other tissue imaging technologies and with image-guided systems.
Owner:NERVONIX INC
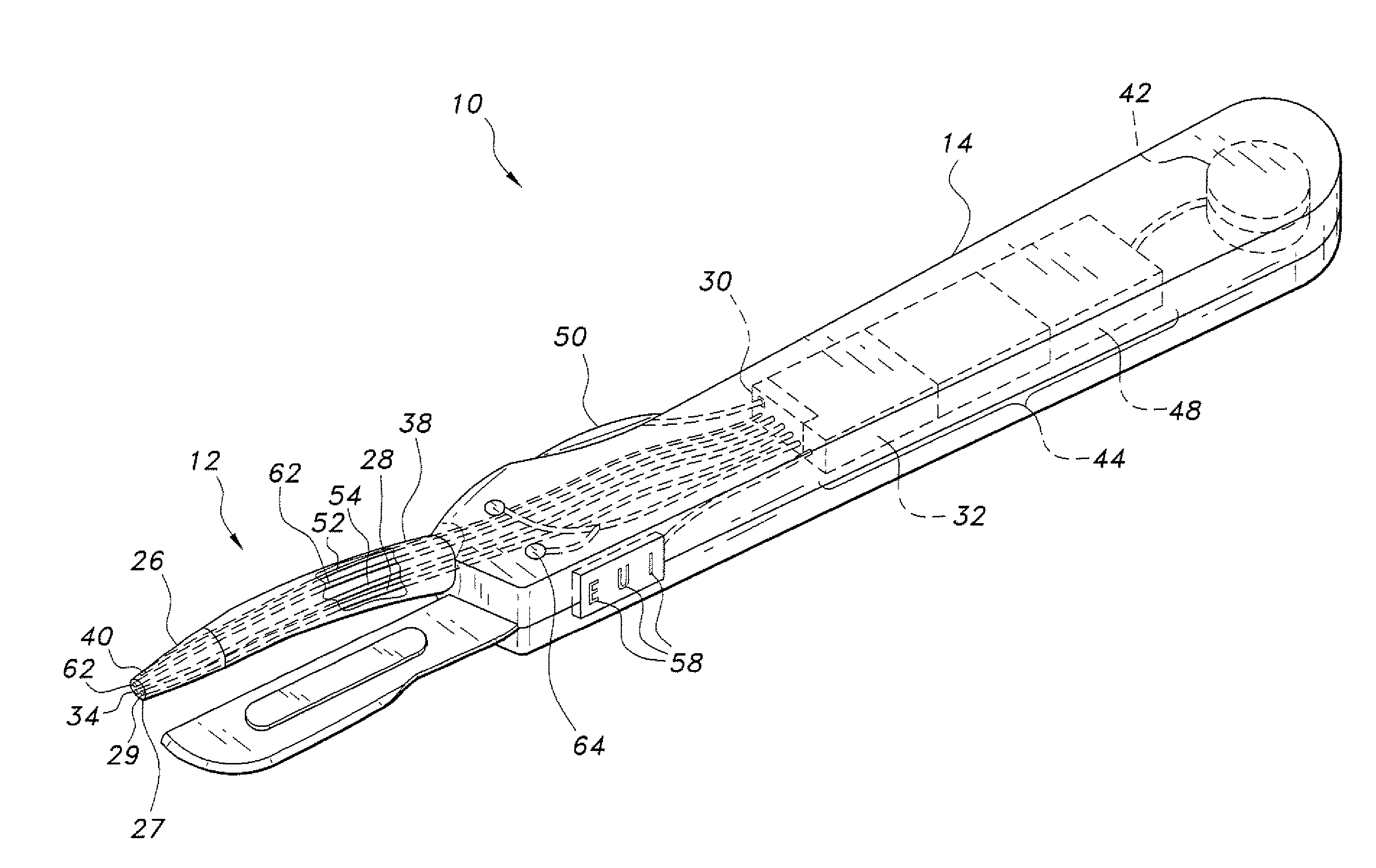
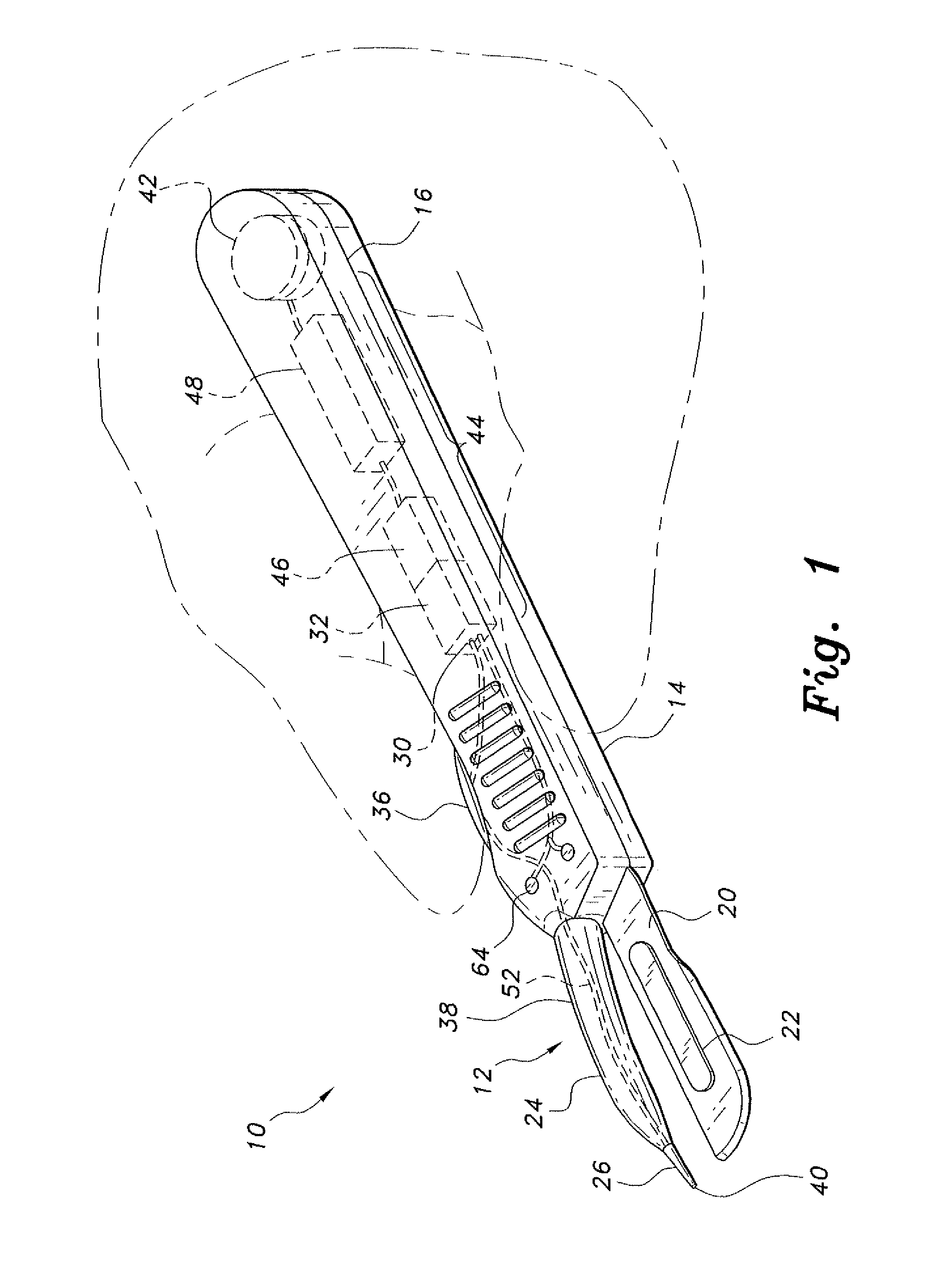
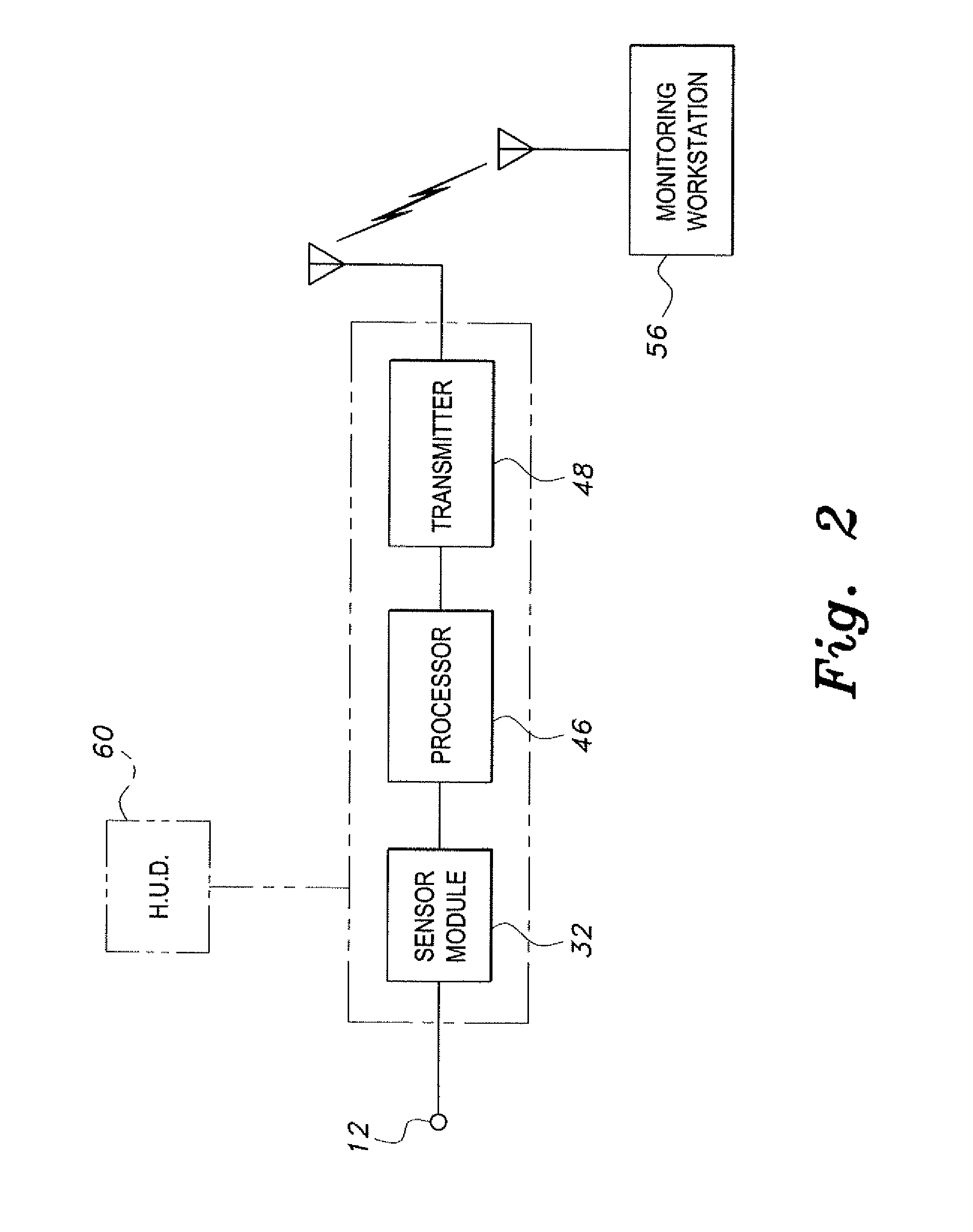
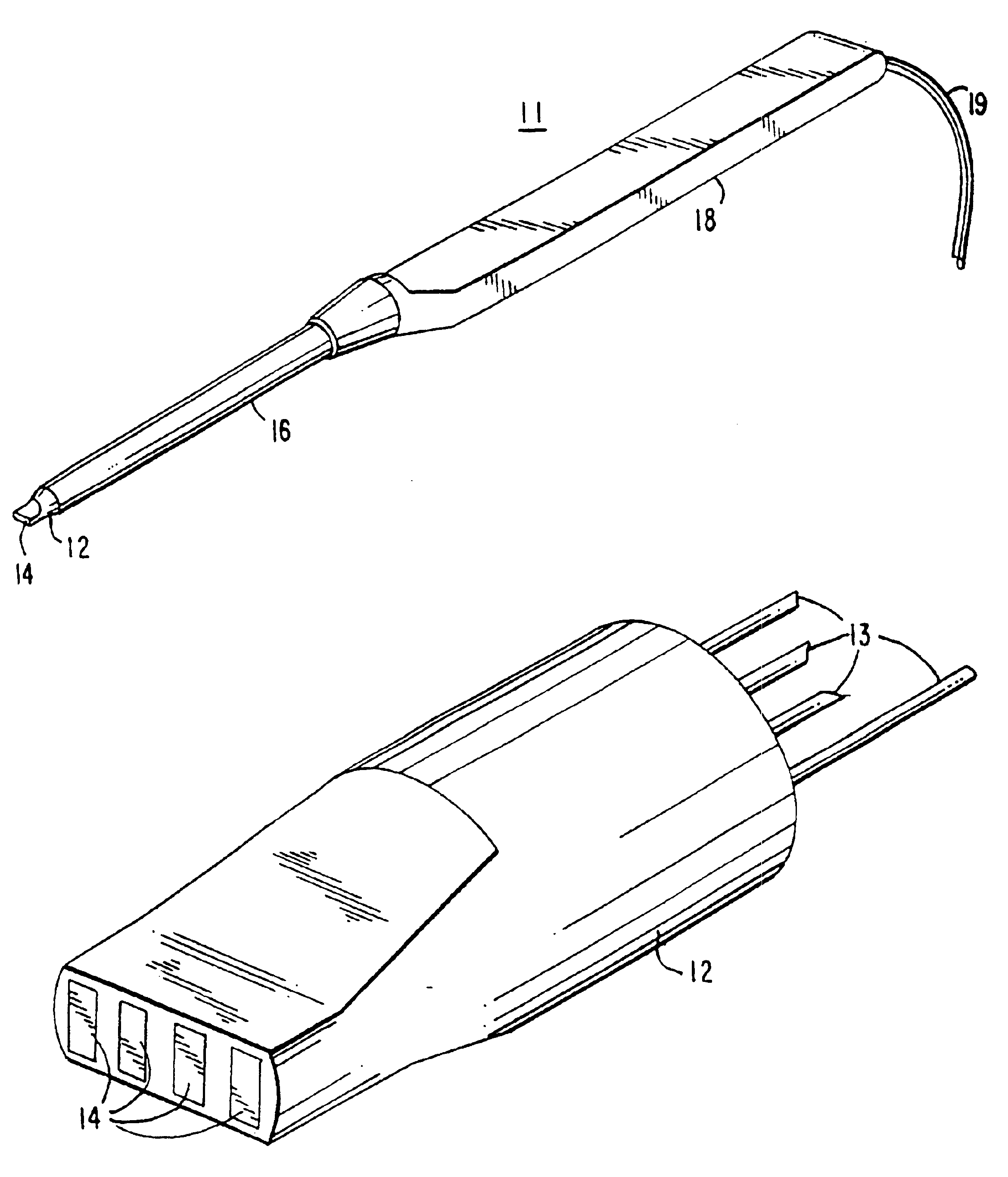
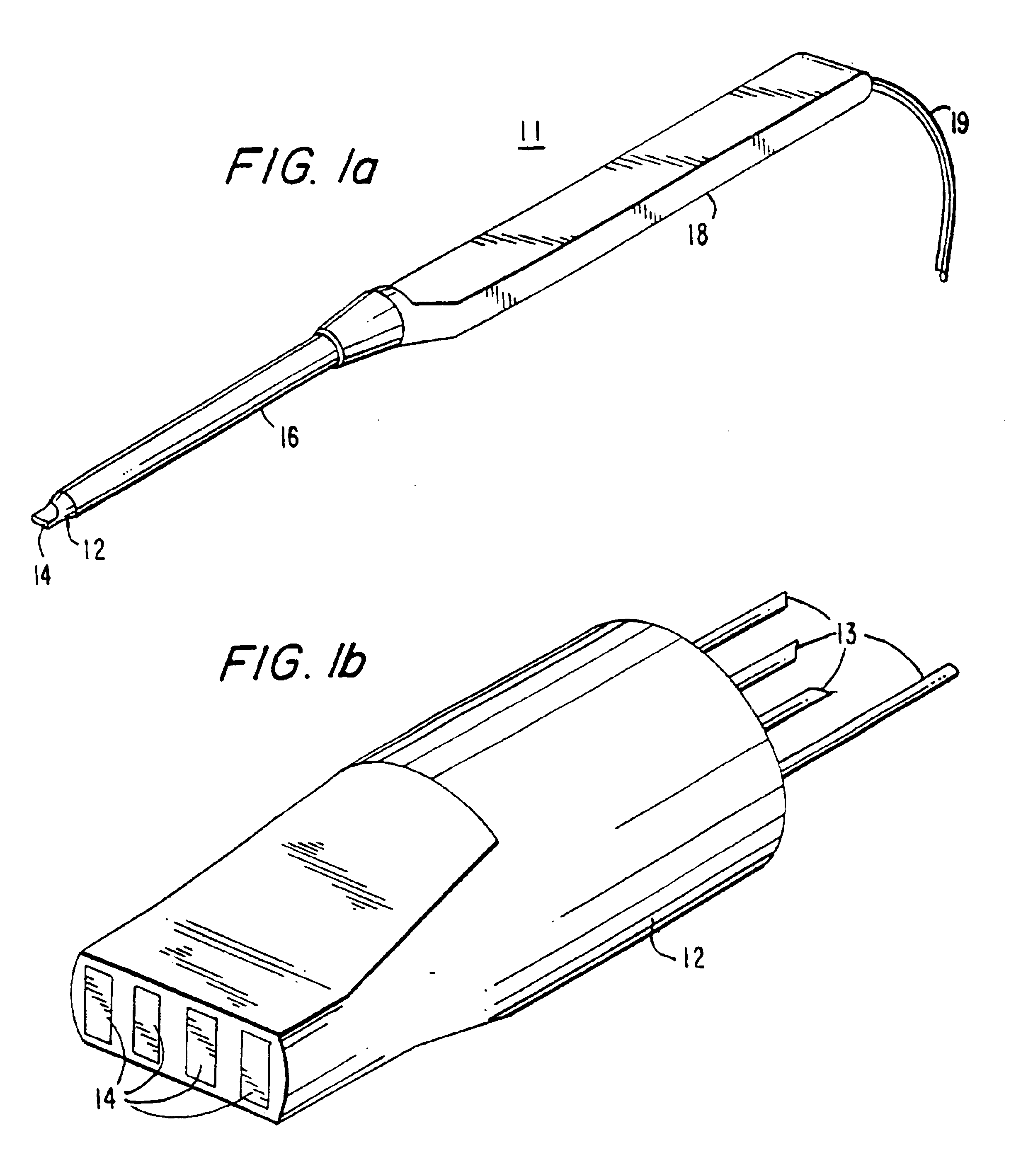
Tissue-identifying surgical instrument
The tissue-identifying surgical instrument includes a surgical instrument having a handle and an integral probe operatively connected to the handle. The probe senses a tissue of interest to identify the type of tissue, e.g., nerve, muscle, vein or other. The interior of the handle includes a control assembly connected to a power source for operation of the tissue identification function. The control assembly displays and wirelessly transmits tissue identification data to a monitoring workstation to inform the surgeon of the type of tissue contacted by the probe.
Owner:SOLOMON CLIFFORD T +1
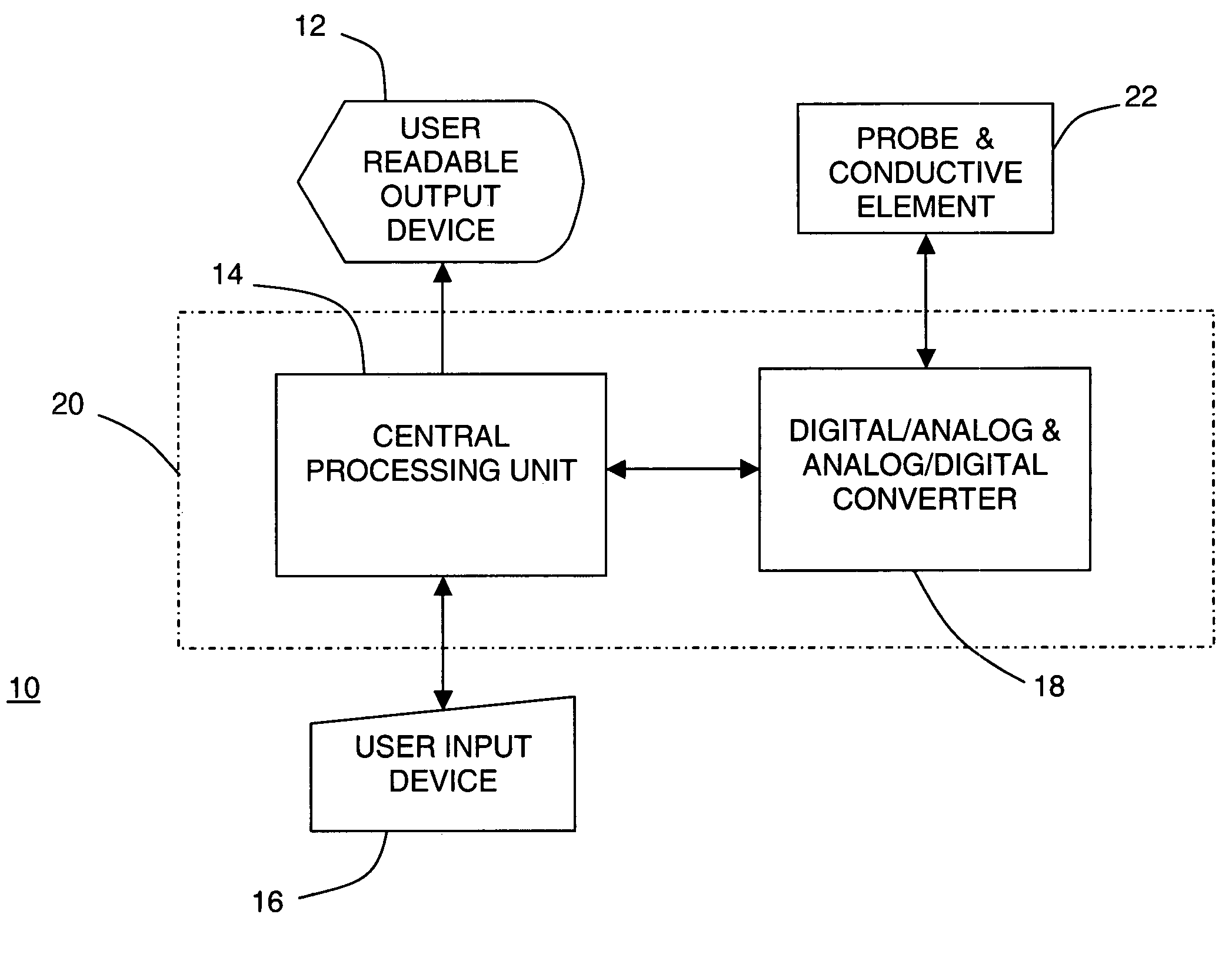
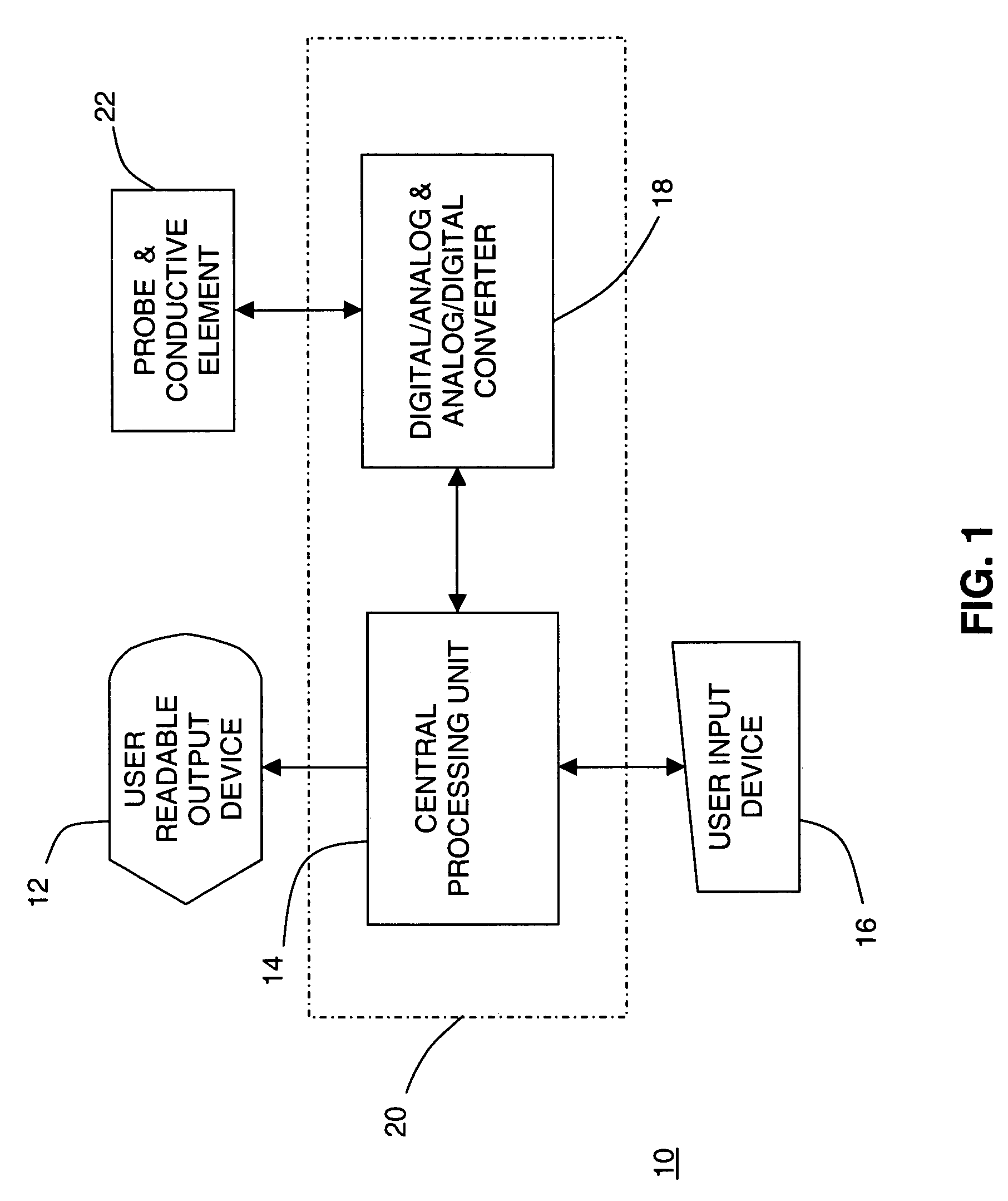
Tissue discrimination and applications in medical procedures
InactiveUS7050848B2Different transmission propertyDifferent capacitanceElectrotherapyInternal osteosythesisTissues typesBone Cortex
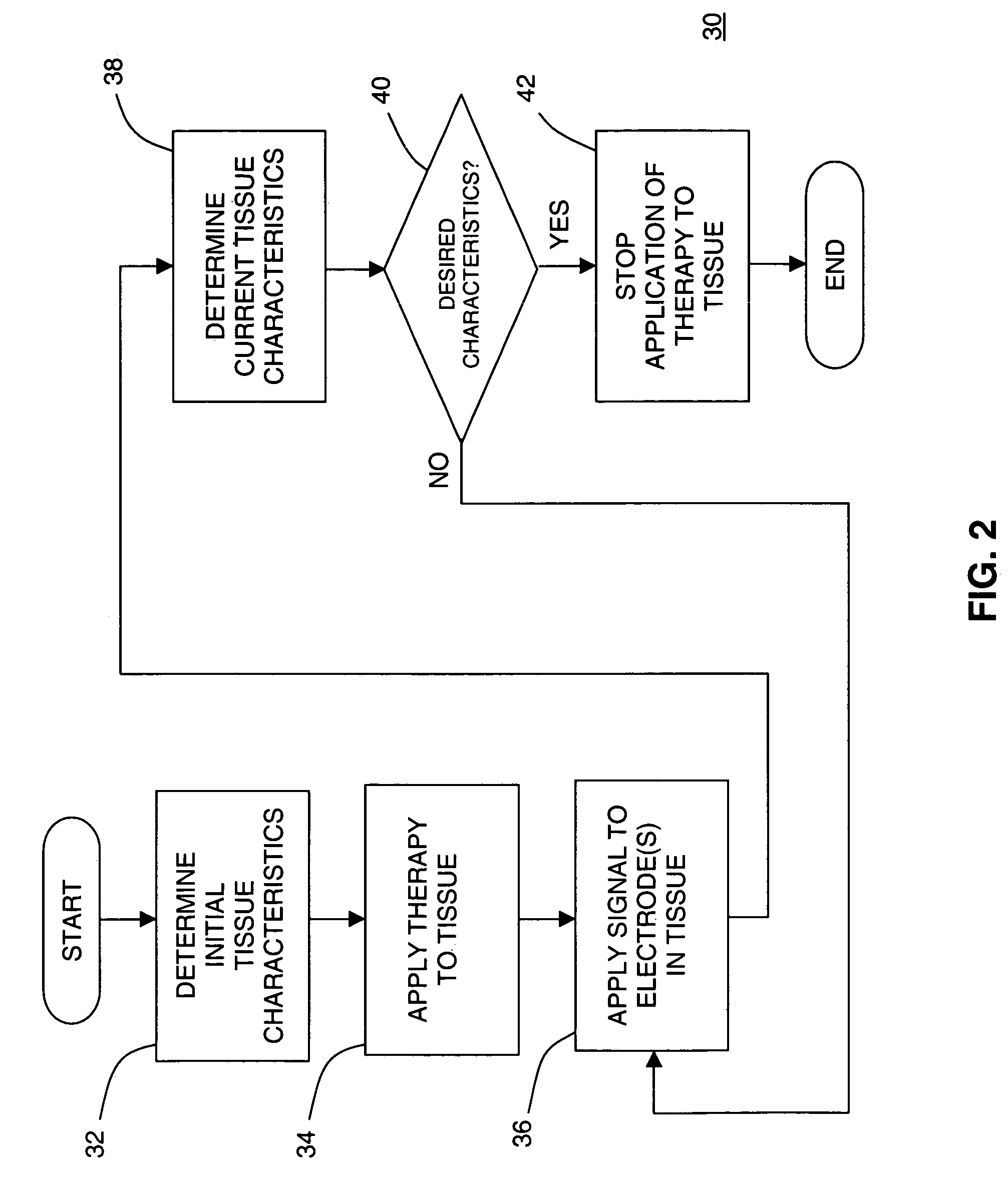
A system and method for discriminating tissue types, controlling the level of therapy to tissue, and determining the health or a known tissue by measuring the characteristics an electrical signal applied to conductive element located within or by the tissue. Additionally, the system and method may be used for determining whether the conductive tip of a pedicle probe or pedicle screw is located in one of cortical bone, cancellous bone, and cortical bone near a boundary with soft tissue, whether the conductive tip of a cannula is located adjacent to one of nerve tissue and annulus tissue, and whether the conductive tip of a cathode is located adjacent to one of nerve tissue and prostate gland tissue.
Owner:NUVASIVE
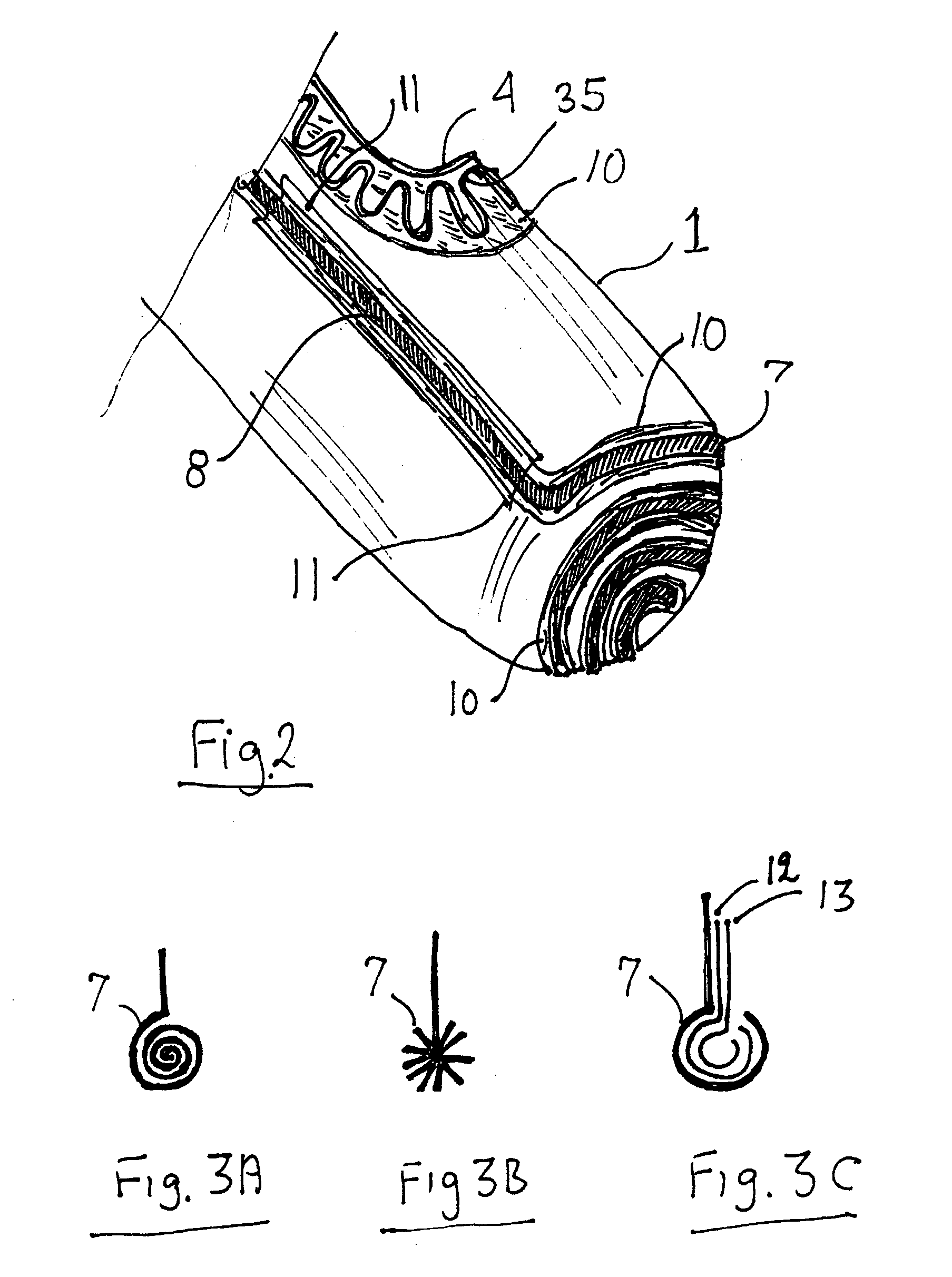
Highly flexible heart valve connecting band
ActiveUS20060229719A1Facilitates supra-annular attachmentIncrease flexibilityHeart valvesInsertion stentTissues types
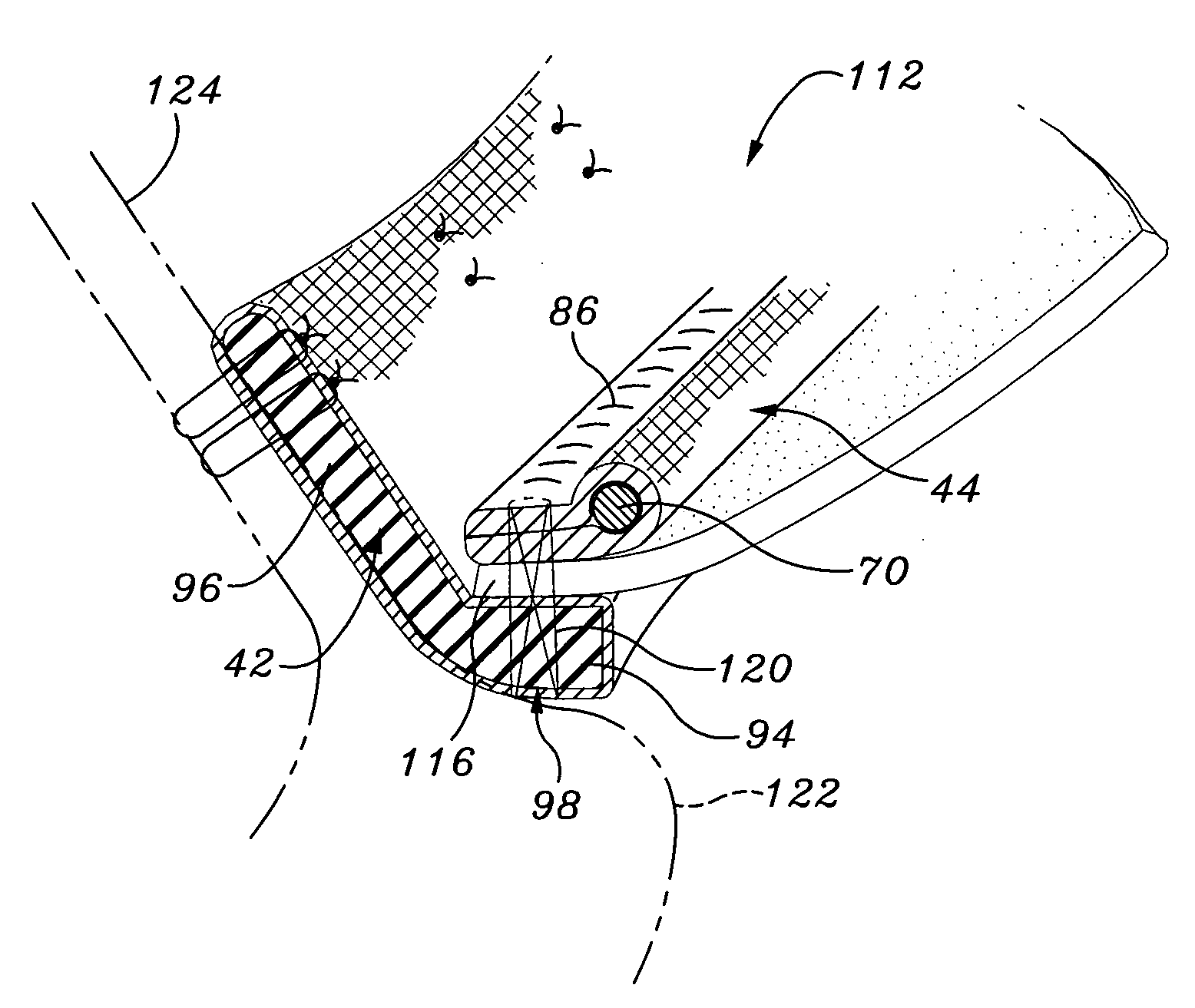
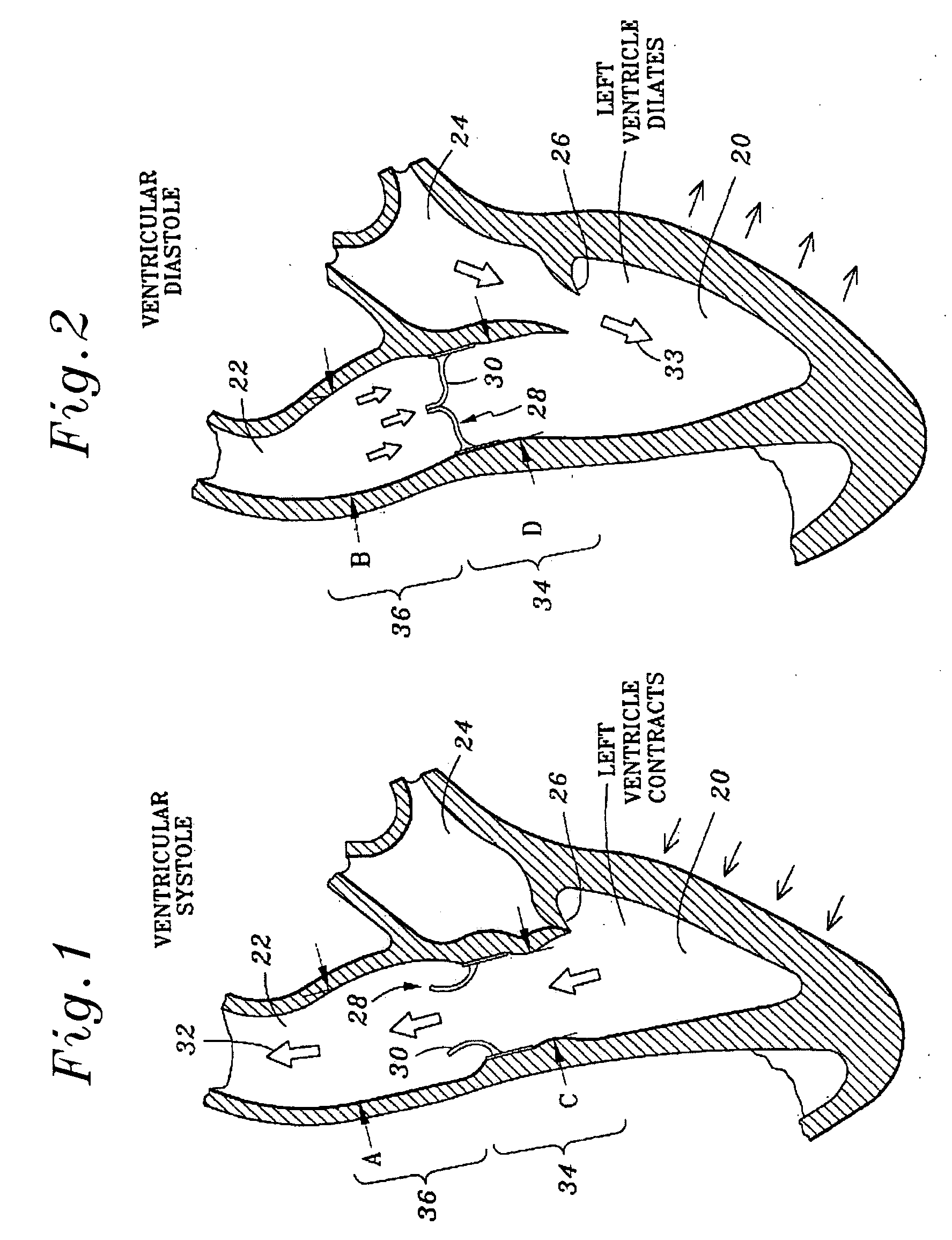
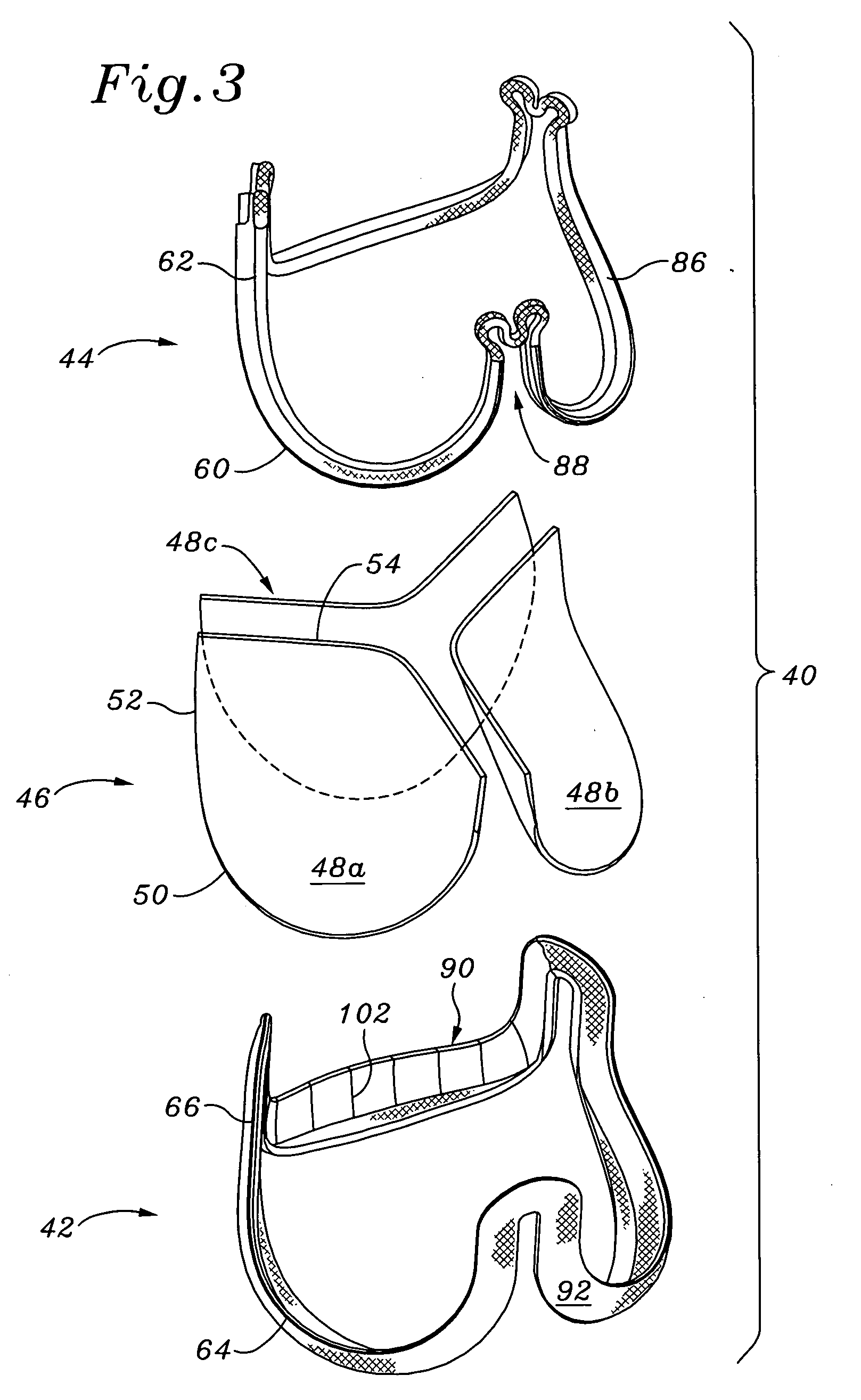
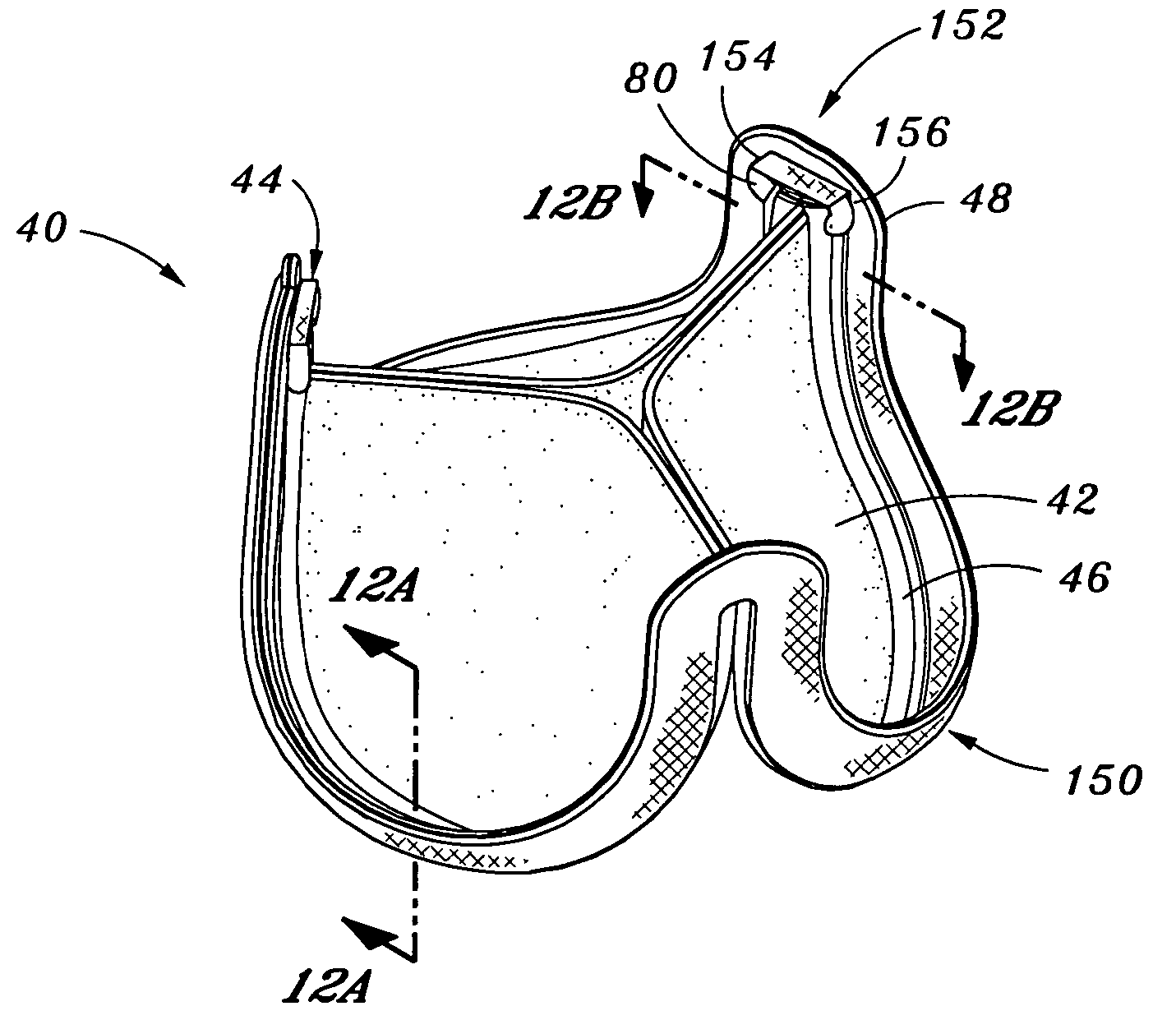
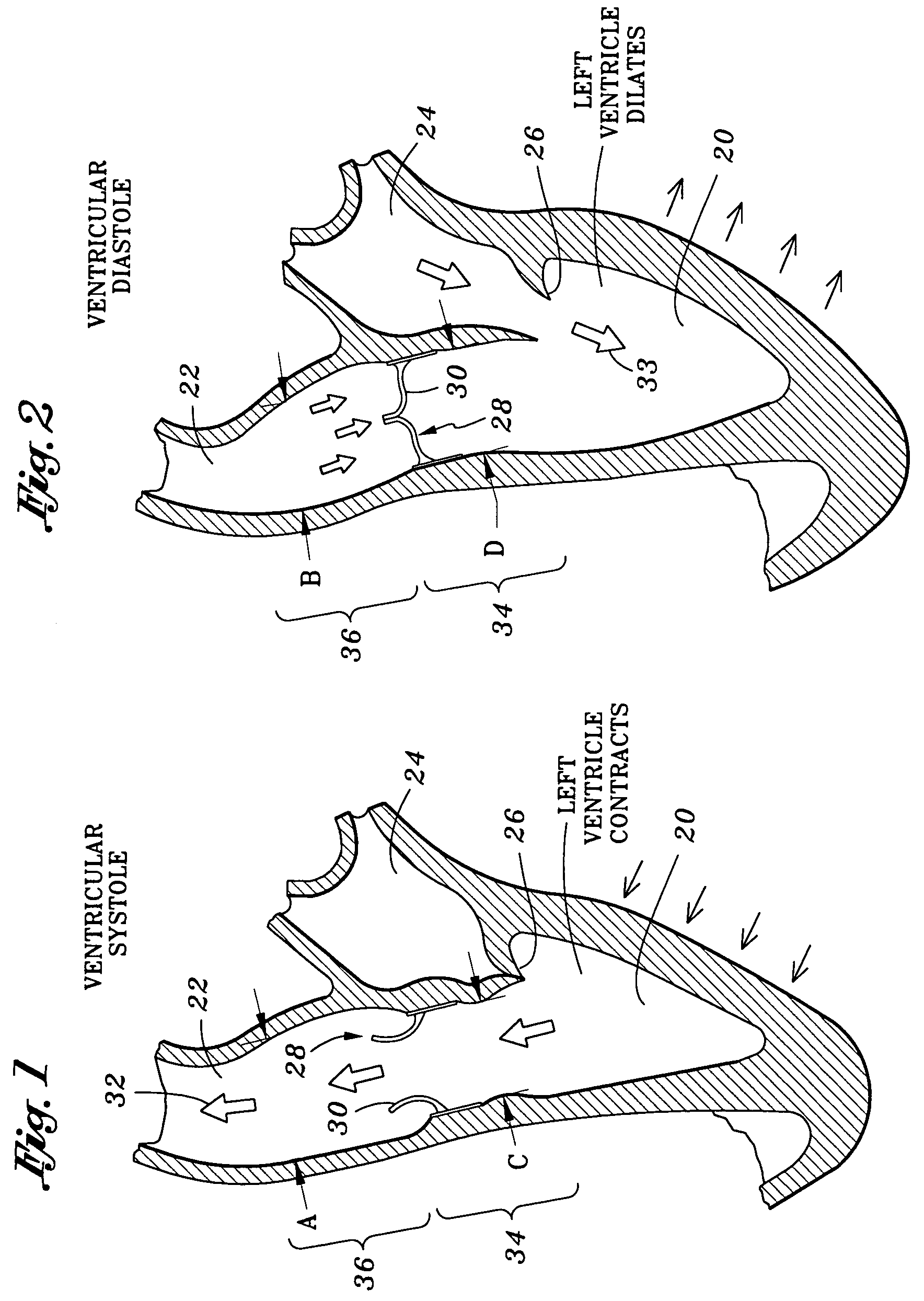
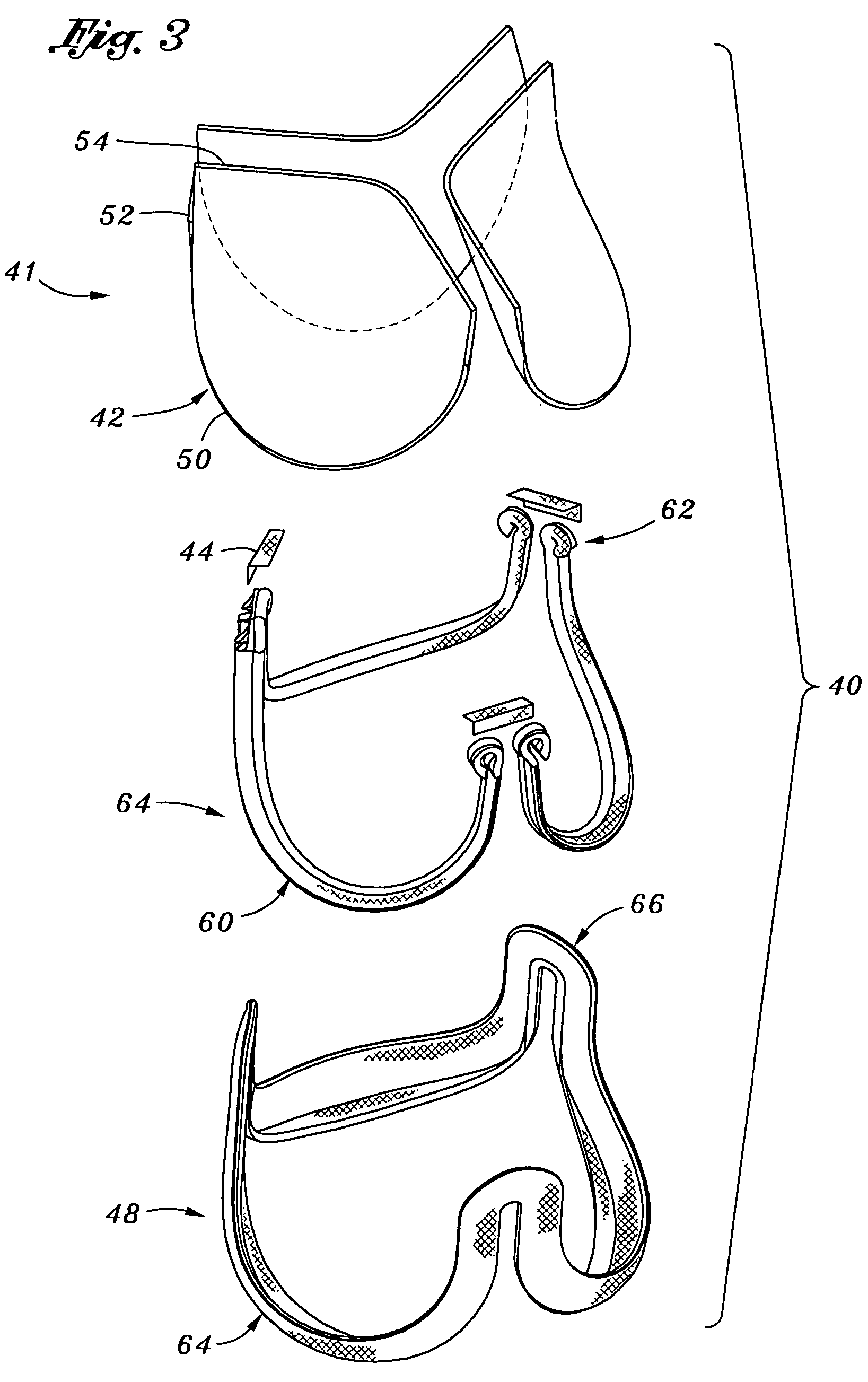
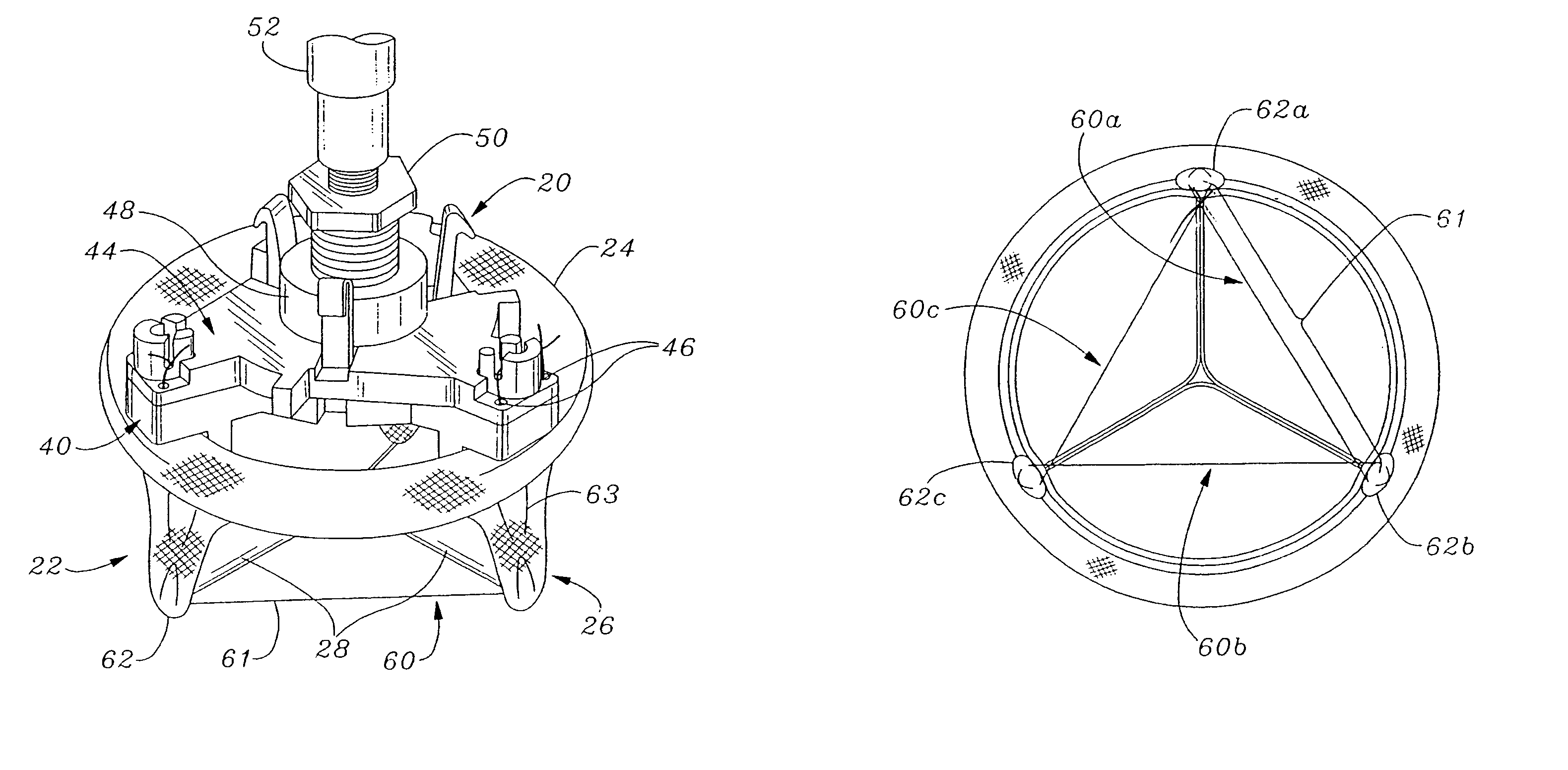
A connecting band for a highly flexible tissue-type heart valve having a stent with cusps and commissures that are permitted to move radially. The connecting band follows the cusps and commissures and extends outwardly. The valve is connected to the natural tissue along the undulating connecting band using conventional techniques, such as sutures. The connecting band may be a cloth-covered inner suture-permeable member and attaches to the underside of the valve at the cusps to provide support to the stent and to the outer side of the valve at the commissures. The connecting band includes commissure portions defining generally axial gaps that help permit flexing of the valve. The inner member may include one or more slits along the cusps to enhance flexibility. The inner member may further include a continuous outwardly projecting sewing ridge around its periphery which includes a series of ribs separated by grooves around the inflow edge of the cusps. The sewing ridge enables supra-annular implant of a valve constructed with the connecting band.
Owner:EDWARDS LIFESCIENCES CORP
Flexible heart valve and associated connecting band
A highly flexible tissue-type heart valve is disclosed having a structural stent in a generally cylindrical configuration with cusps and commissures that are permitted to move radially. The stent commissures are constructed so that the cusps are pivotably or flexibly coupled together at the commissures to permit relative movement therebetween.
Owner:EDWARDS LIFESCIENCES CORP
Method and system for knowledge guided hyperintensity detection and volumetric measurement
InactiveUS6430430B1High sensitivityHigh detectionImage enhancementImage analysisAnatomical structuresTissues types
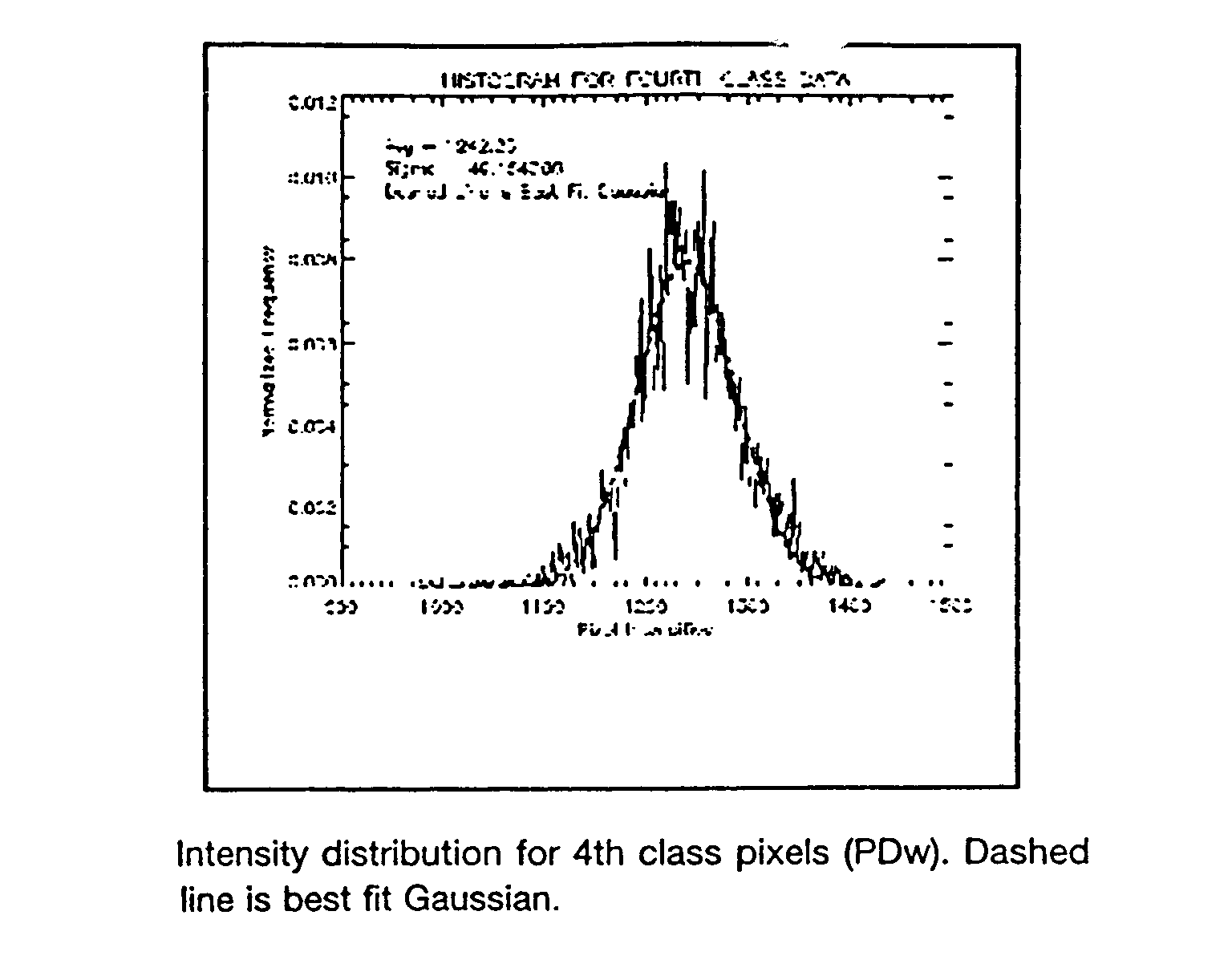
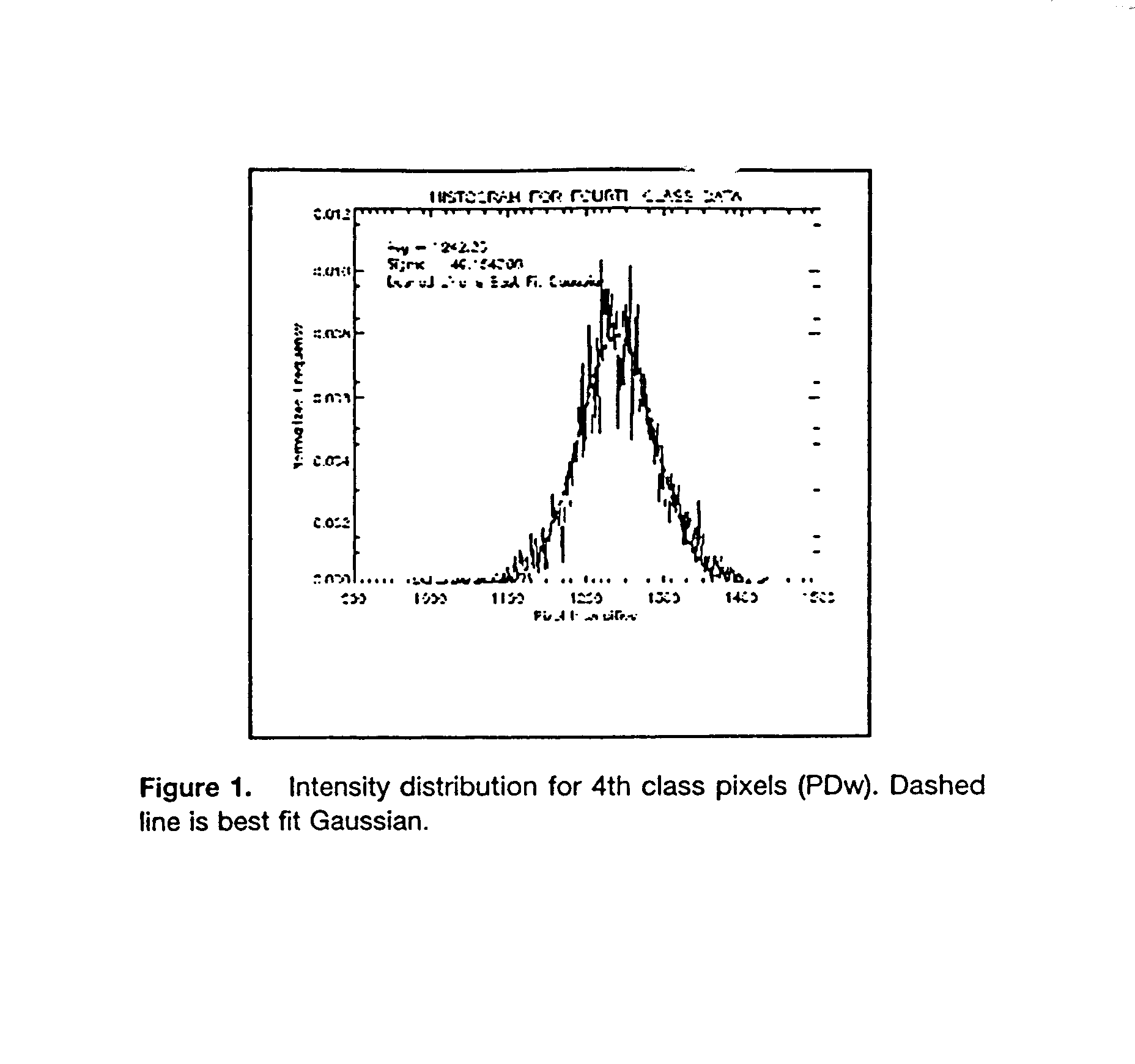
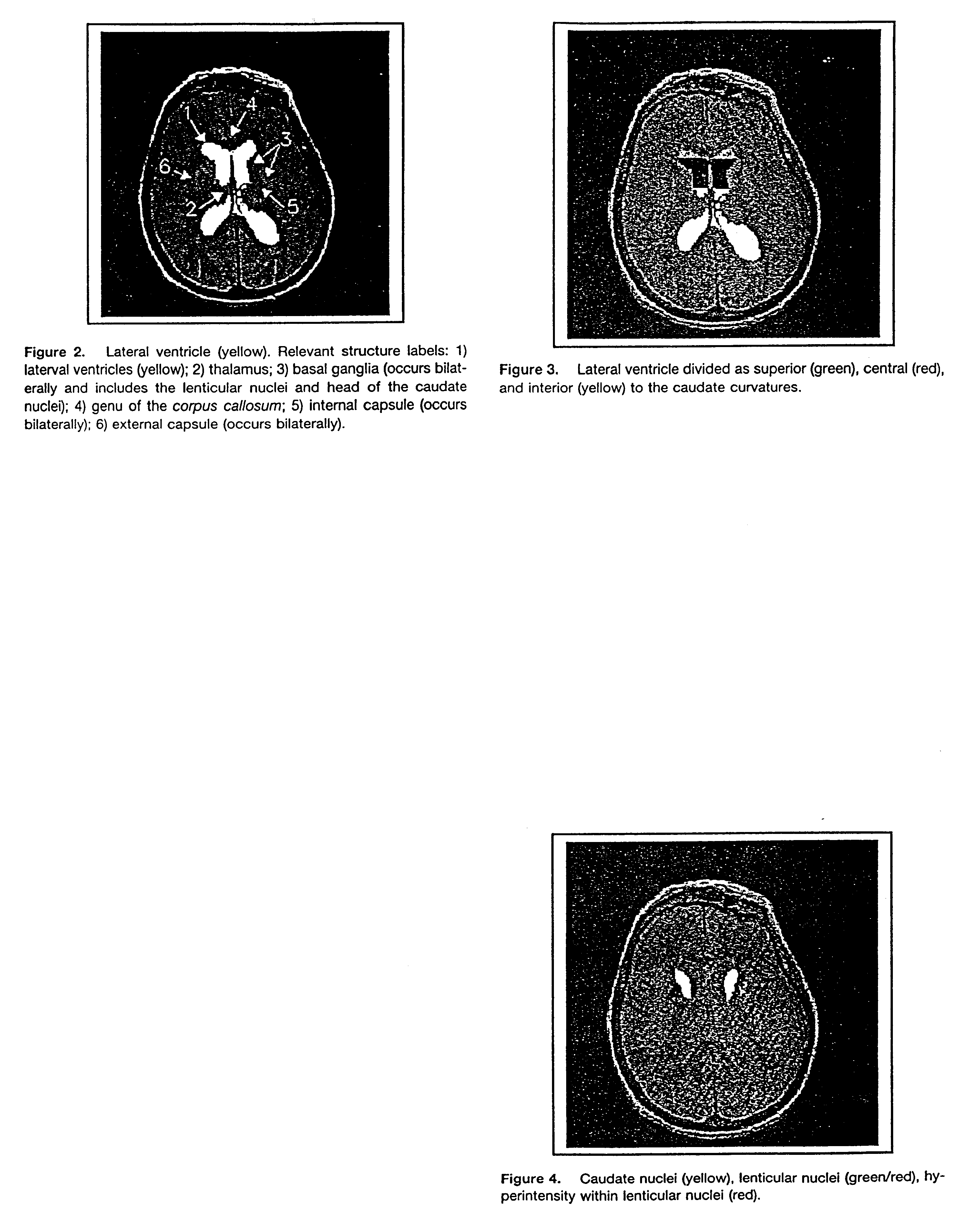
An automated method and / or system for identifying suspected lesions in a brain is provided. A processor (a) provides a magnetic resonance image (MRI) of a patient's head, including a plurality of slices of the patient's head, which MRI comprises a multispectral data set that can be displayed as an image of varying pixel intensities. The processor (b) identifies a brain area within each slice to provide a plurality of masked images of intracranial tissue. The processor (c) applies a segmentation technique to at least one of the masked images to classify the varying pixel intensities into separate groupings, which potentially correspond to different tissue types. The processor (d) refines the initial segmentation into the separate groupings of at least the first masked image obtained from step (c) using one or more knowledge rules that combine pixel intensities with spatial relationships of anatomical structures to locate one or more anatomical regions of the brain. The processor (e) identifies, if present, the one or more anatomical regions of the brain located in step (d) in other masked images obtained from step (c). The processor (f) further refines the resulting knowledge rule-refined images from steps (d) and (e) to locate suspected lesions in the brain.
Owner:UNIV OF SOUTH FLORIDA
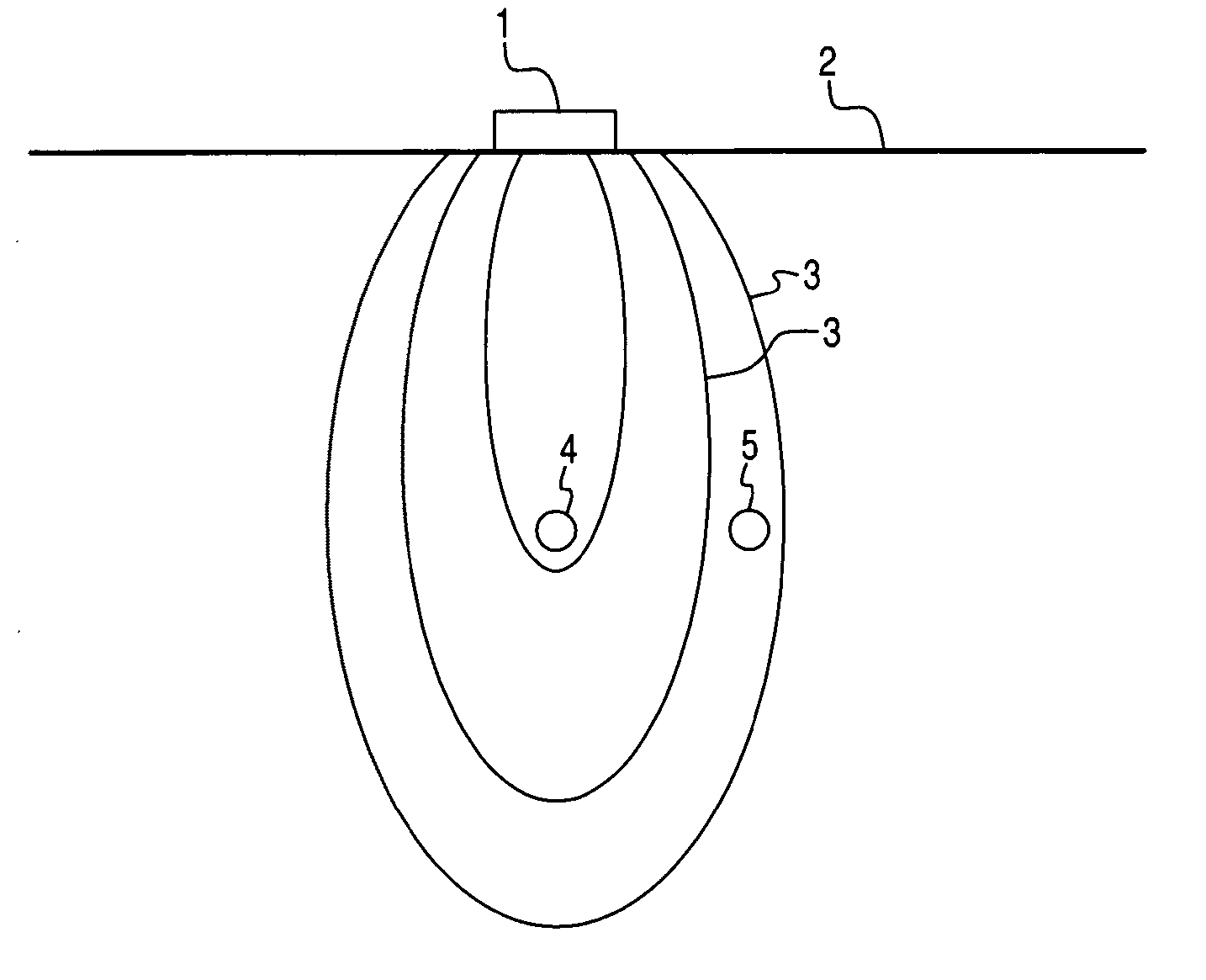
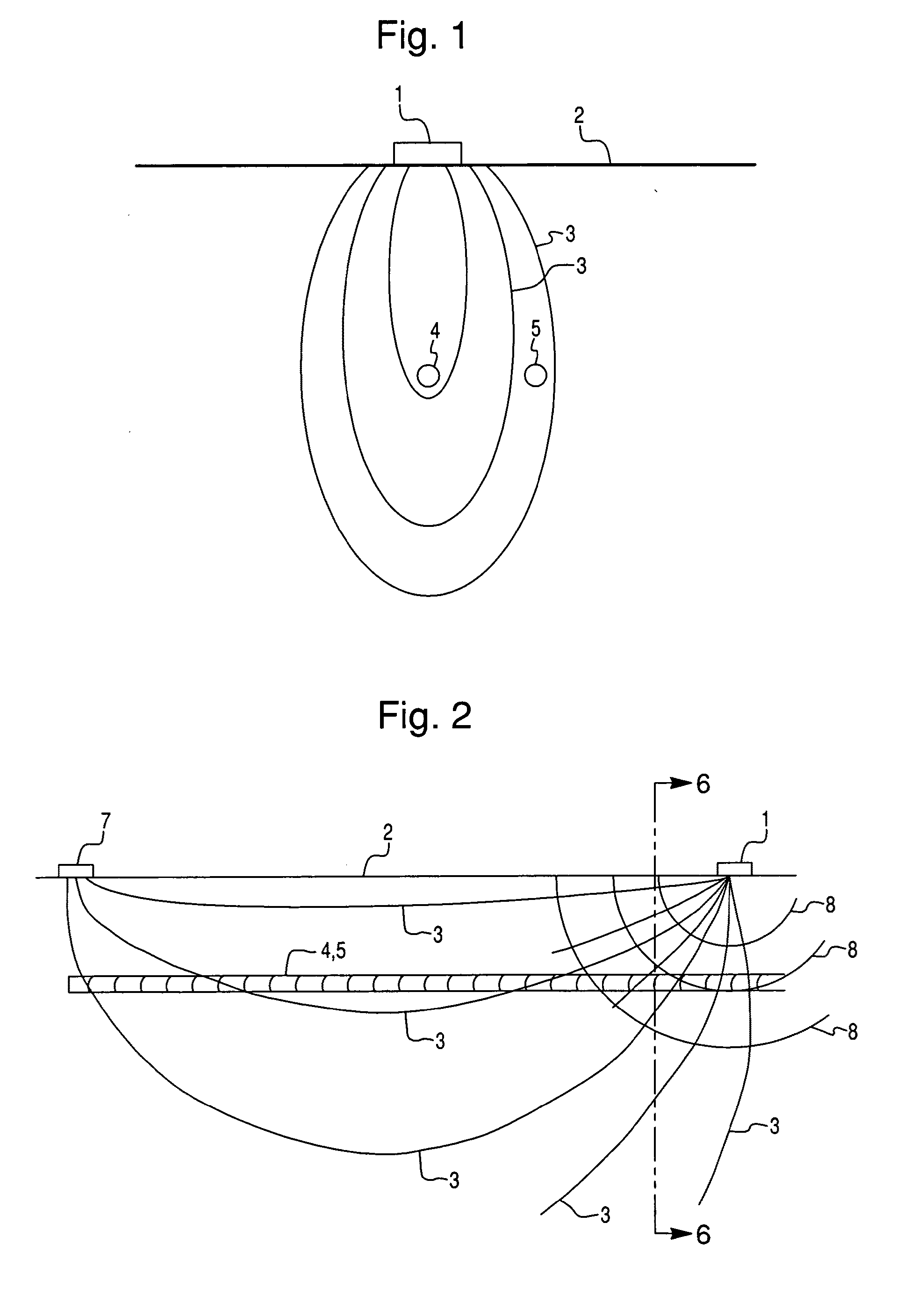
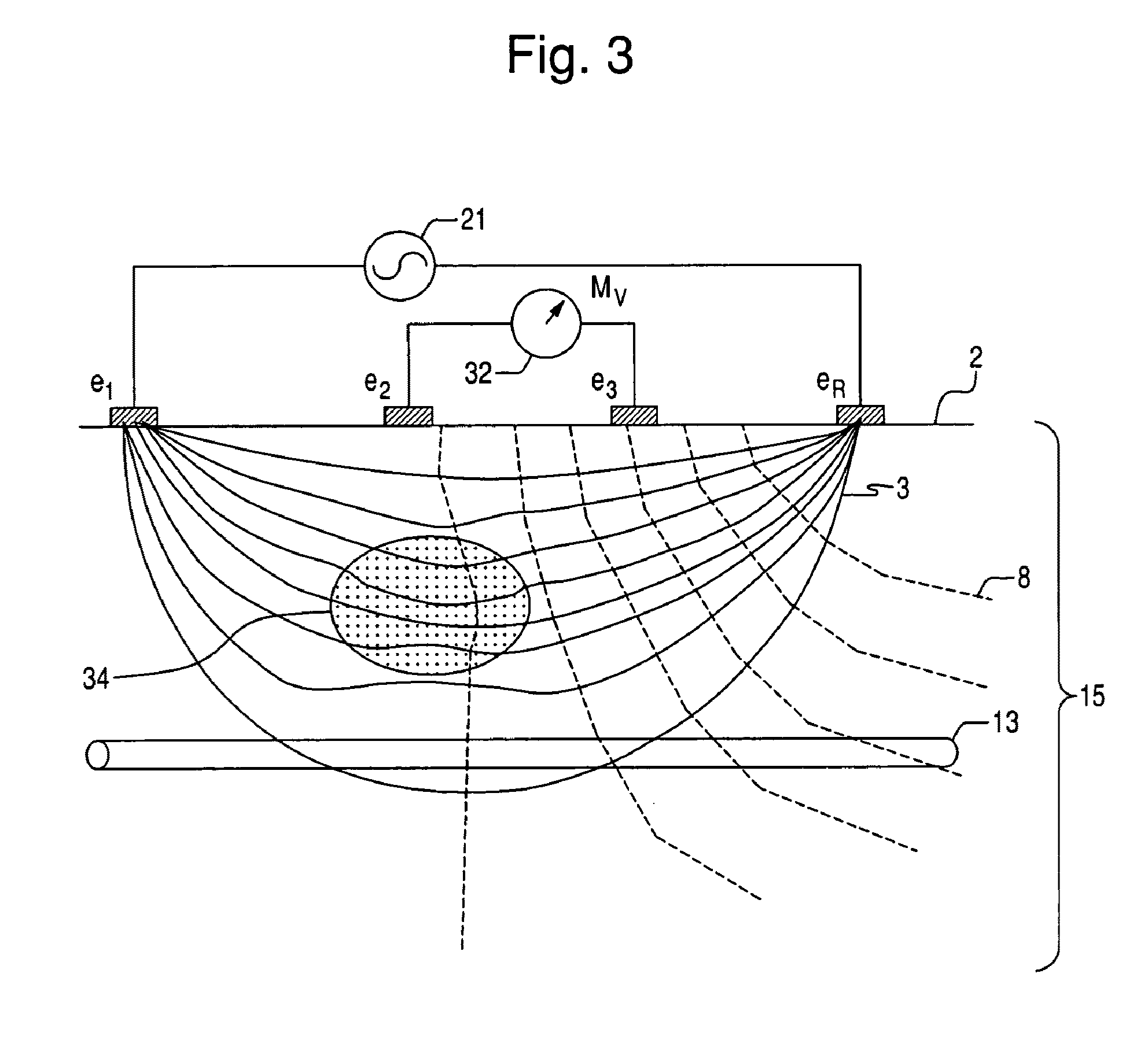
Tissue characterization based on impedance images and on impedance measurements
InactiveUS7141019B2Improved and uniform and repeatable contactMinimal operator expertiseUltrasonic/sonic/infrasonic diagnosticsSurgical needlesDisplay deviceTissues types
Apparatus for aiding in the identification of tissue type for an anomalous tissue in an impedance image comprising a first device providing a polychromic immitance map of a portion of the body; a second devise determining a plurality of polychromic measures from one or both of a portion of the body; and a display which displays an indication based on the plurality of polychromic measures.
Owner:TRANSSCAN MEDICAL
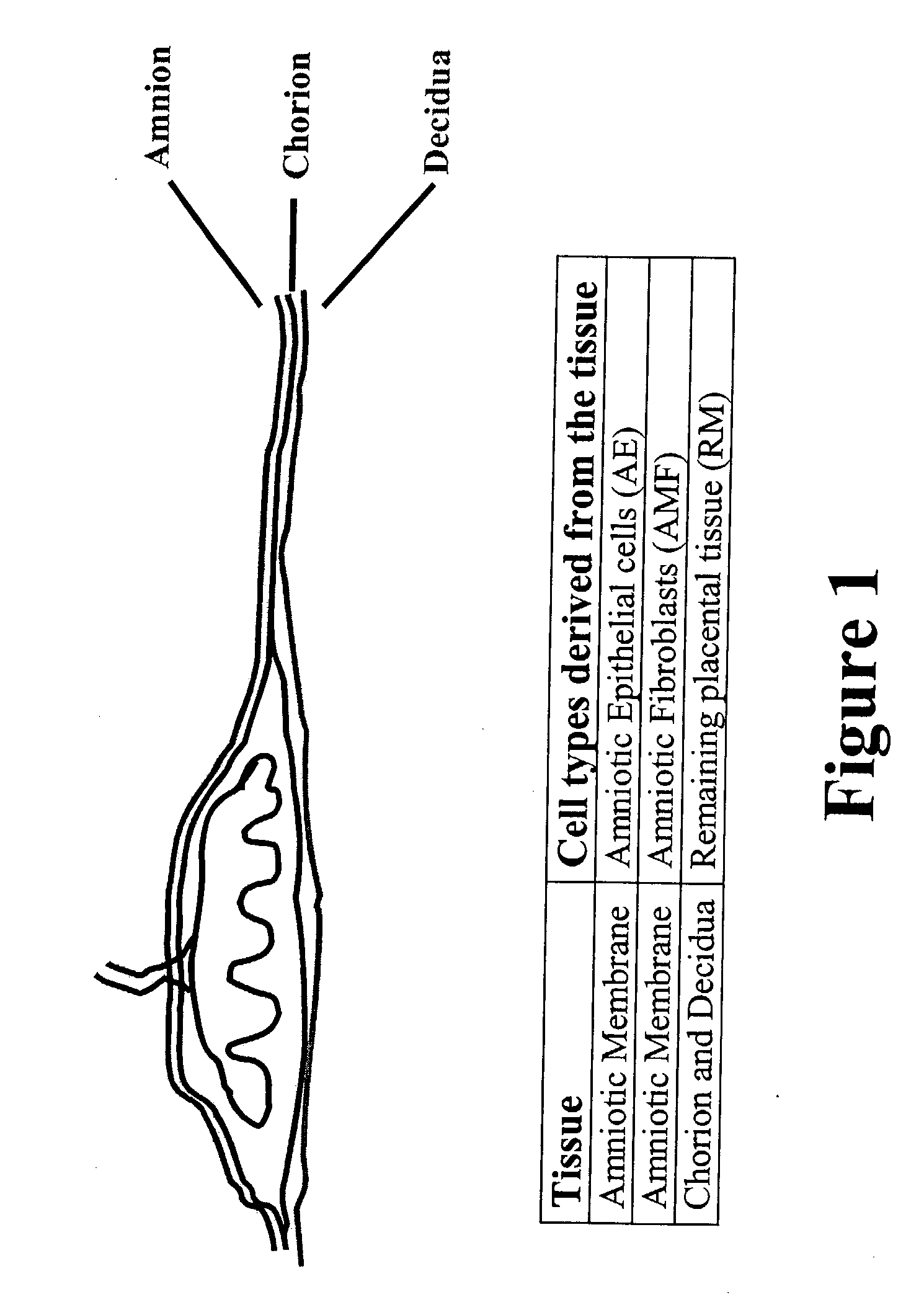
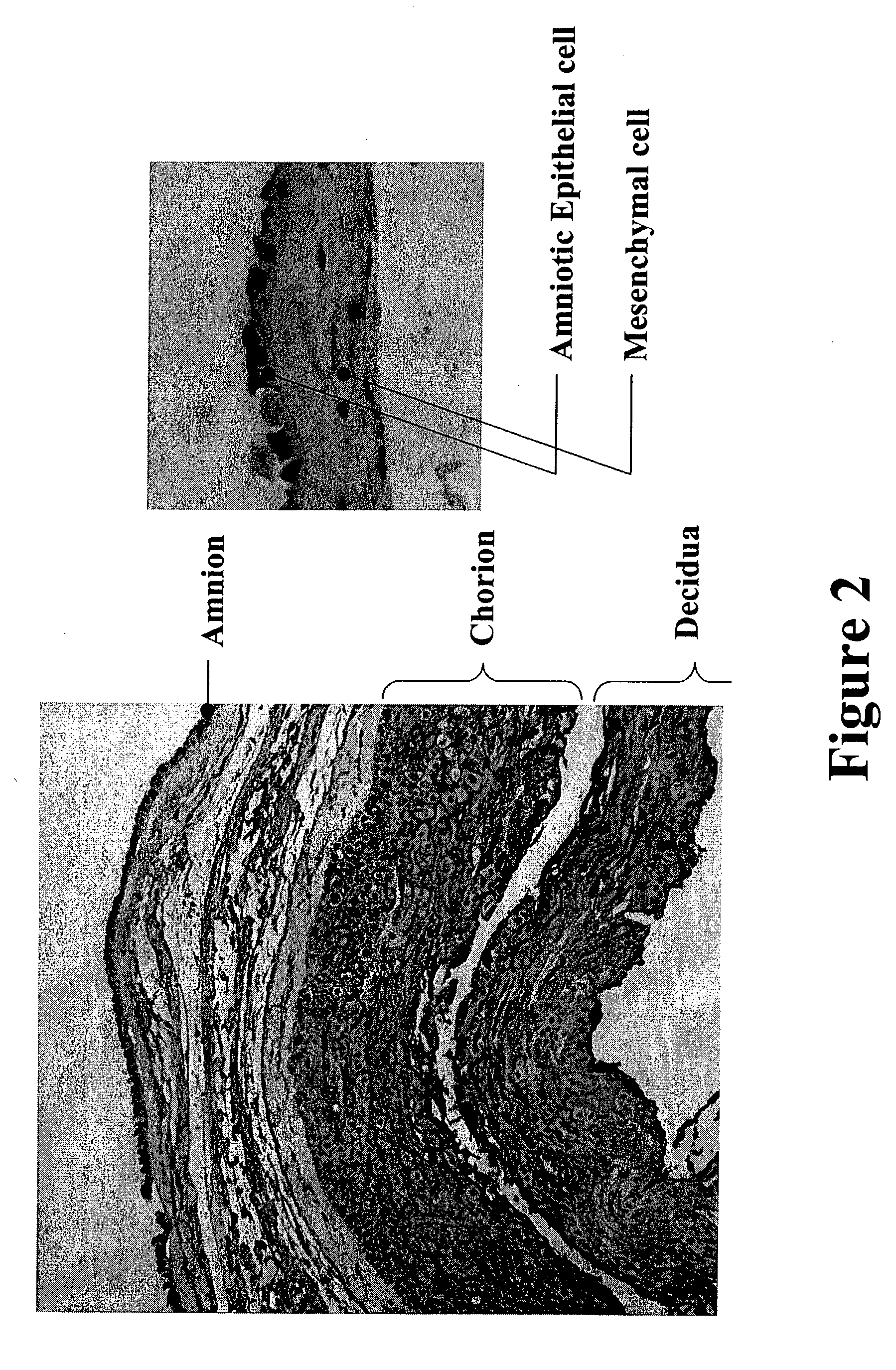
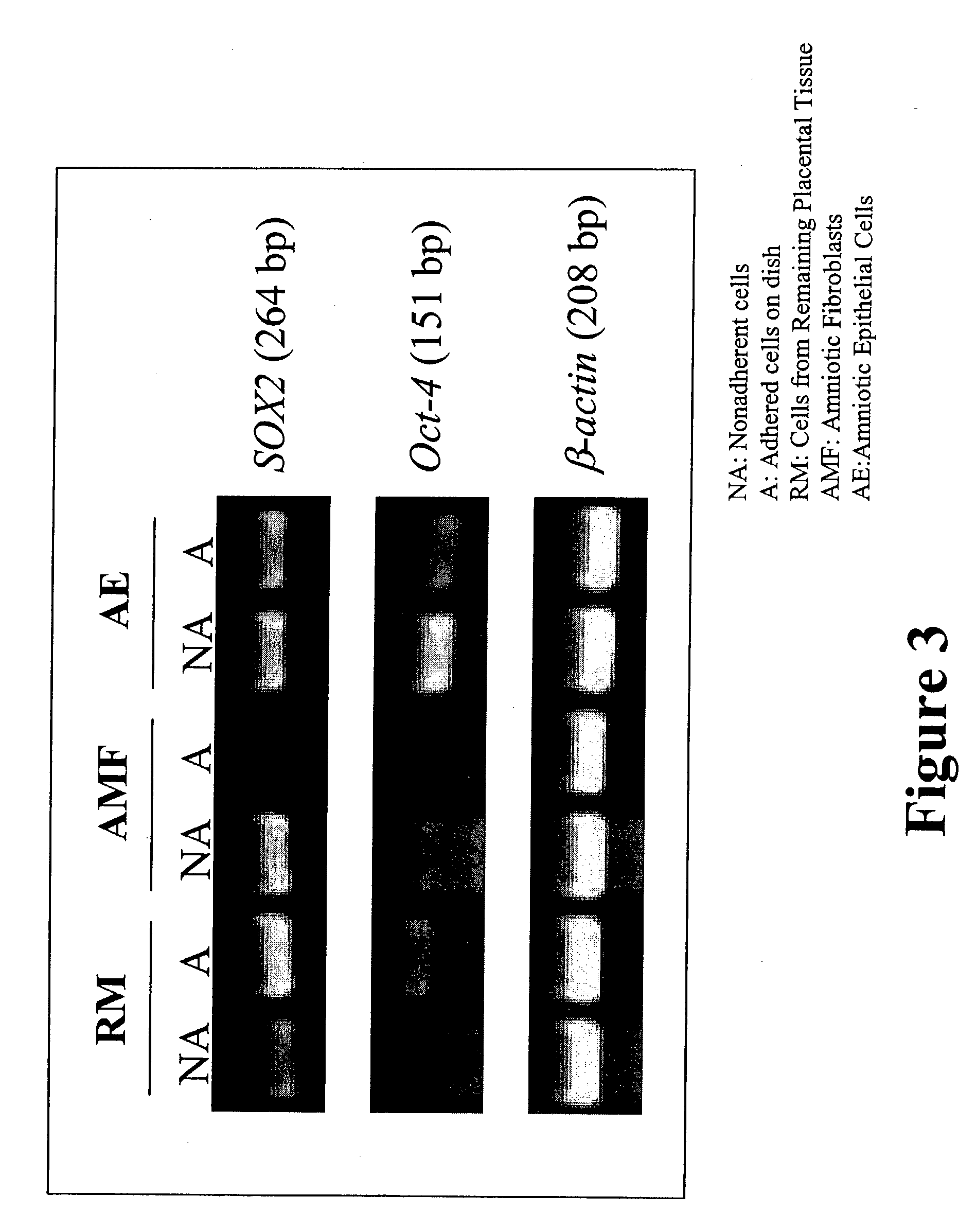
Placental derived stem cells and uses thereof
The present invention features novel placental derived stem cells and provides methods and compositions for the therapeutic uses of placental derived stem cells or placental derived stem cells that have been induced to differentiate into a desired tissue type into a recipient host in amounts sufficient to result in production of the desired cell type, i.e., hepatic, pancreatic, neuronal, or nervous tissue.
Owner:UNIVERSITY OF PITTSBURGH
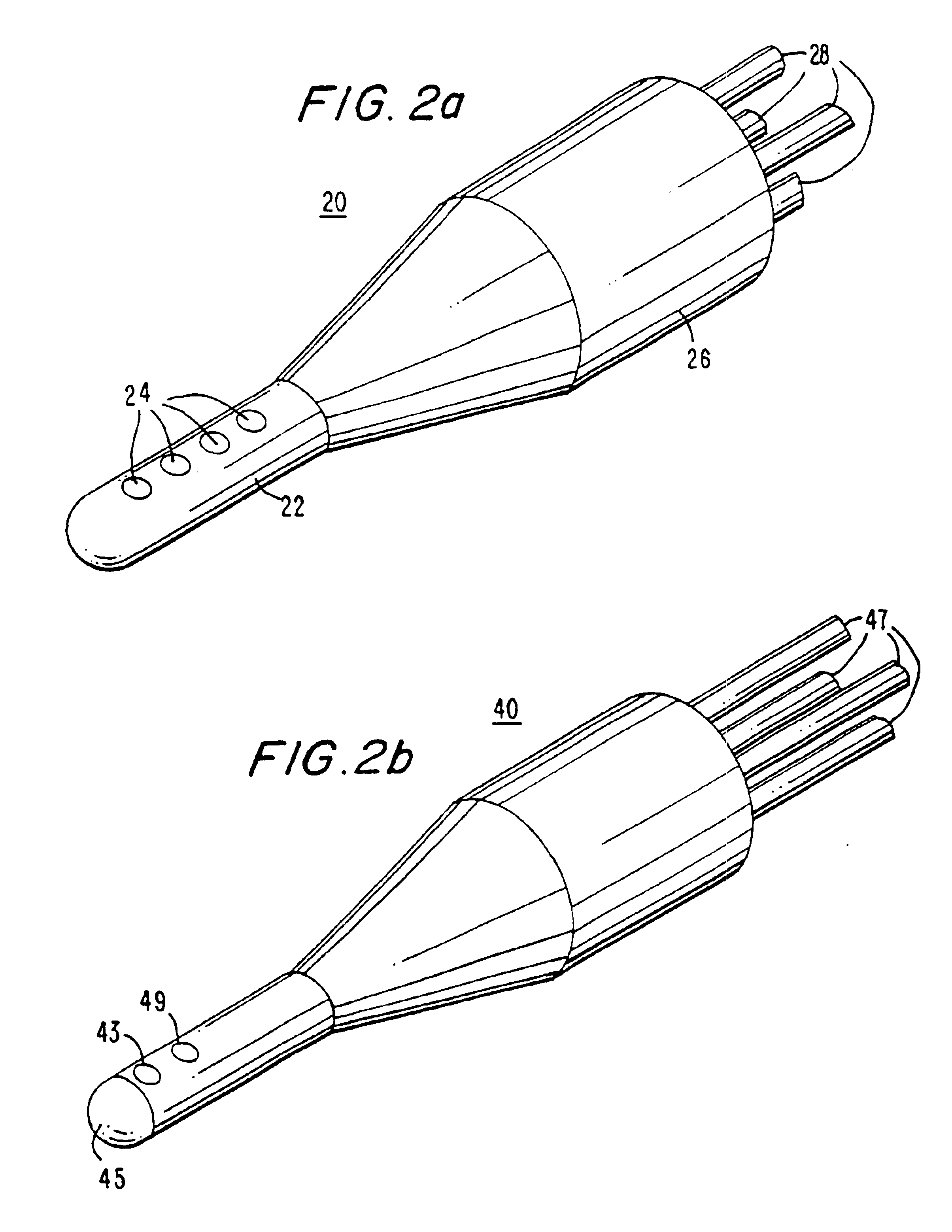
Apparatus for recognizing tissue types
InactiveUS6845264B1Remove the ambiguity of any one measurementPerson identificationSurgical instruments for heatingPower flowMedicine
A method and apparatus for recognizing tissue types measures at least two separate and distinct properties of a tissue specimen using a probe tip containing electrodes coupled to circuitry that applies a measuring current and obtains values of electrical properties of the tissue such as conductivity and potential difference. An algorithm then uses the values to determine the tissue's type and condition.
Owner:SKLADNEV VICTOR +2
Active electrode, bio-impedance based, tissue discrimination system and methods of use
InactiveUS7865236B2Accurate identificationElectrotherapyDiagnostic recording/measuringElectricityTissues types
Systems and methods for discriminating and locating tissues within a body involve applying a waveform signal to tissue between two electrodes and measuring the electrical characteristics of the signal transmitted through the tissue. At least one of the electrodes is constrained in area so that localized electrical characteristics of the tissue are measured. Such localized electrical characteristics are determined over a portion of a body of the subject by using an array of electrodes or electrodes that can be moved over the body. A controller may implement the process and perform calculations on the measured data to identify tissue types and locations within the measured area, and to present results in graphical form. Results may be combined with other tissue imaging technologies and with image-guided systems.
Owner:NERVONIX INC
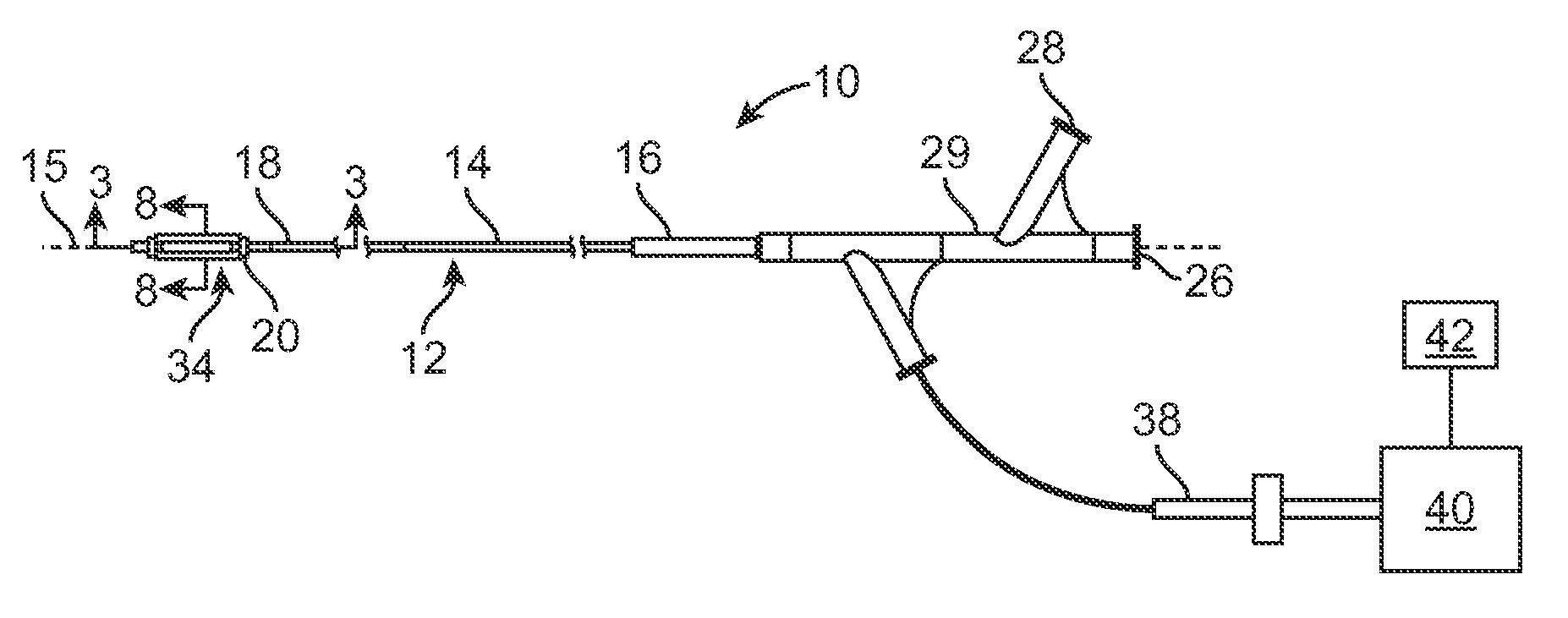
Tissue biopsy and treatment apparatus and method
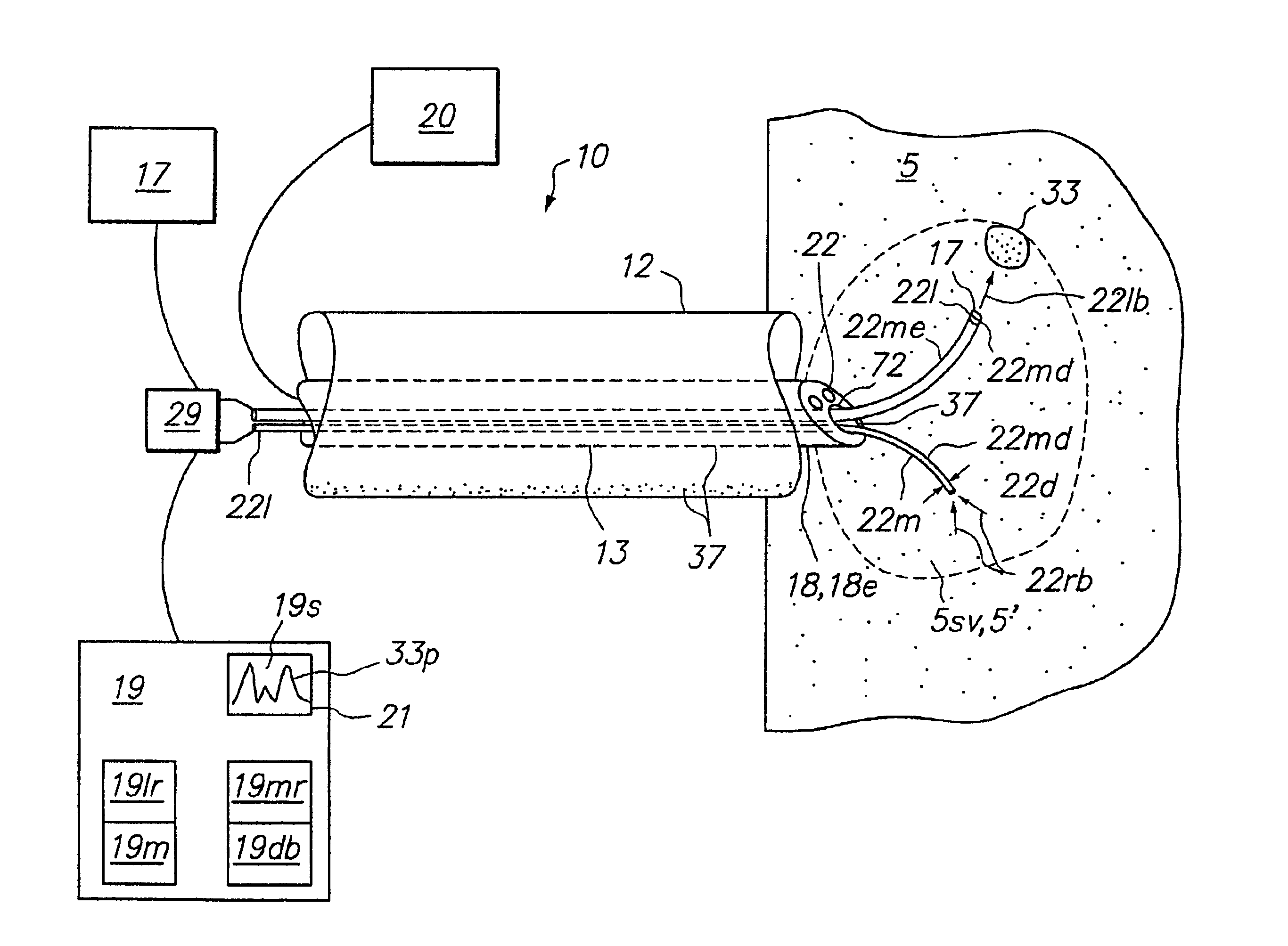
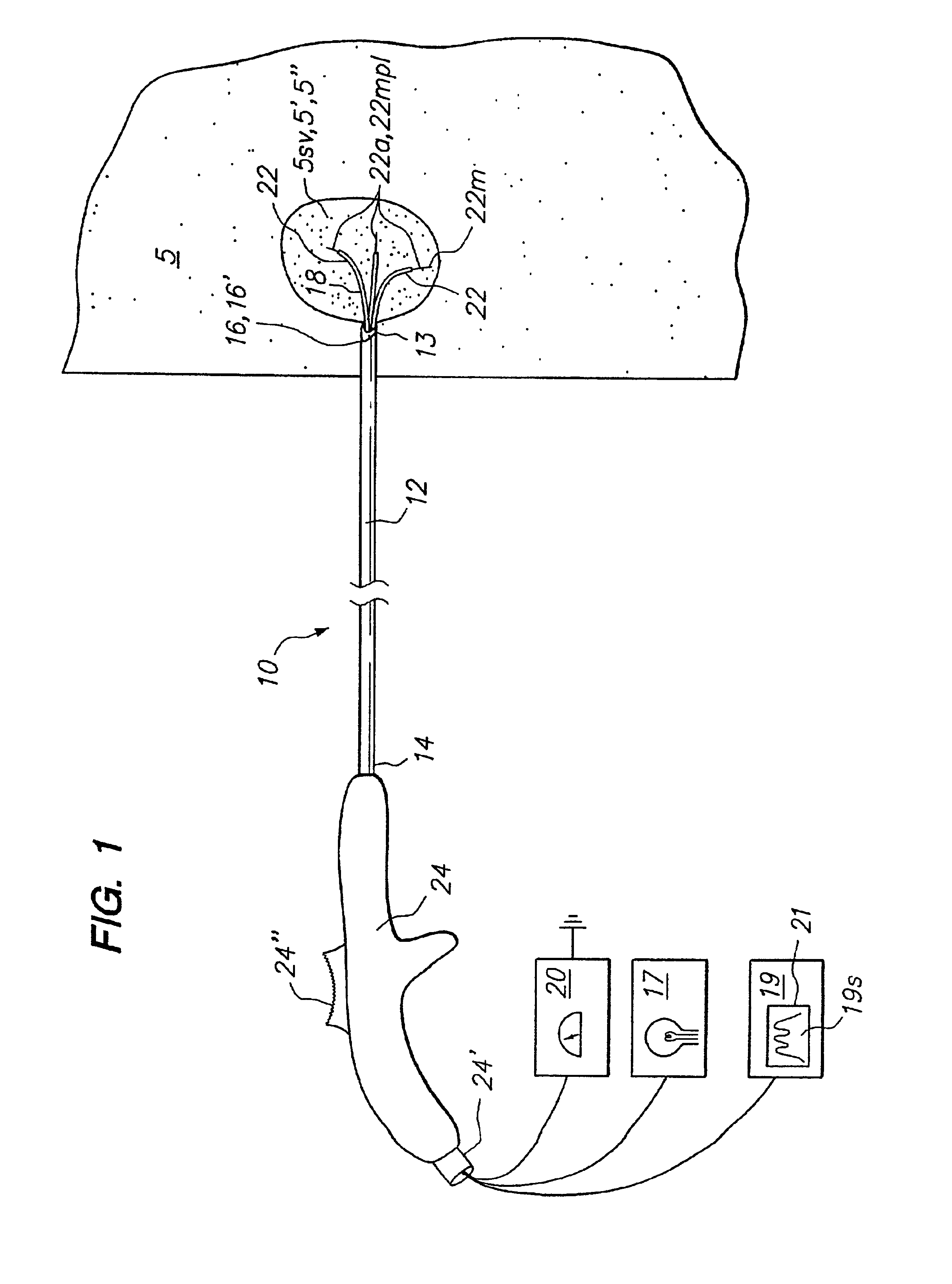
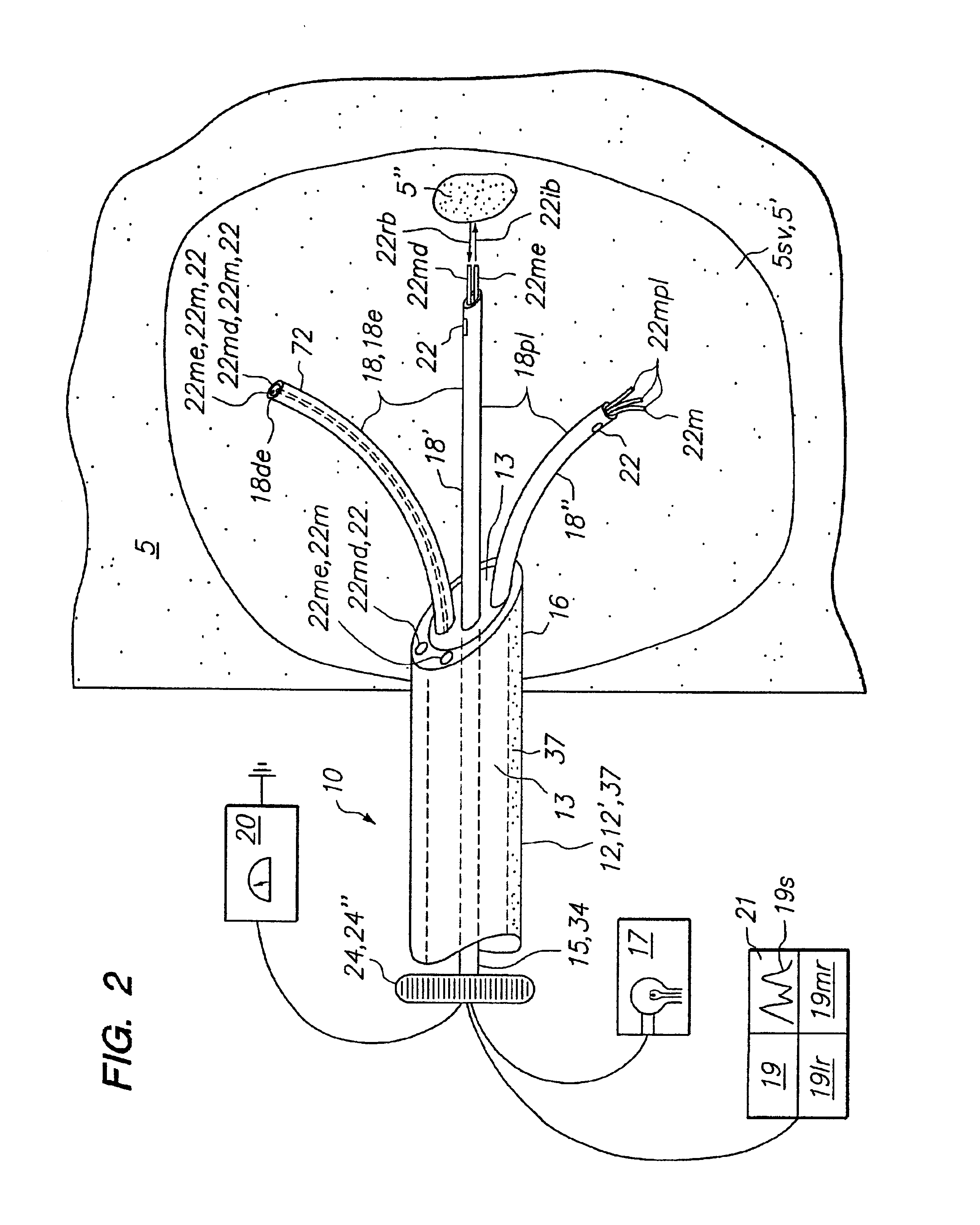
InactiveUS7025765B2Improve clinical outcomesPrecise positioningElectrotherapySurgical needlesSensor arrayTissue biopsy
A method of treating a tumor includes providing a tissue biopsy and treatment apparatus that includes an elongated delivery device that has a lumen and is maneuverable in tissue. A sensor array having a plurality of resilient members is deployable from the elongated delivery device. At least one of the plurality of resilient members is positionable in the elongated delivery device in a compacted state and deployable with curvature into tissue from the elongated delivery device in a deployed state. At least one of the plurality of resilient members includes at least one of a sensor, a tissue piercing distal end or a lumen. The sensor array has a geometric configuration adapted to volumetrically sample tissue at a tissue site to differentiate or identify tissue at the tissue site. At least one energy delivery device is coupled to one of the sensor array, at least one of the plurality of resilient members or the elongated delivery device. The apparatus is then introduced into a target tissue site. The sensor array is then utilized to distinguish a tissue type. The tissue type information derived from the sensor array is utilized to position the energy delivery device to ablate a tumor volume. Energy is then delivered from the energy delivery device to ablate or necrose at least a portion of the tumor volume. The sensor array is then utilized to determine an amount of tumor volume ablation.
Owner:ANGIODYNAMICS INC
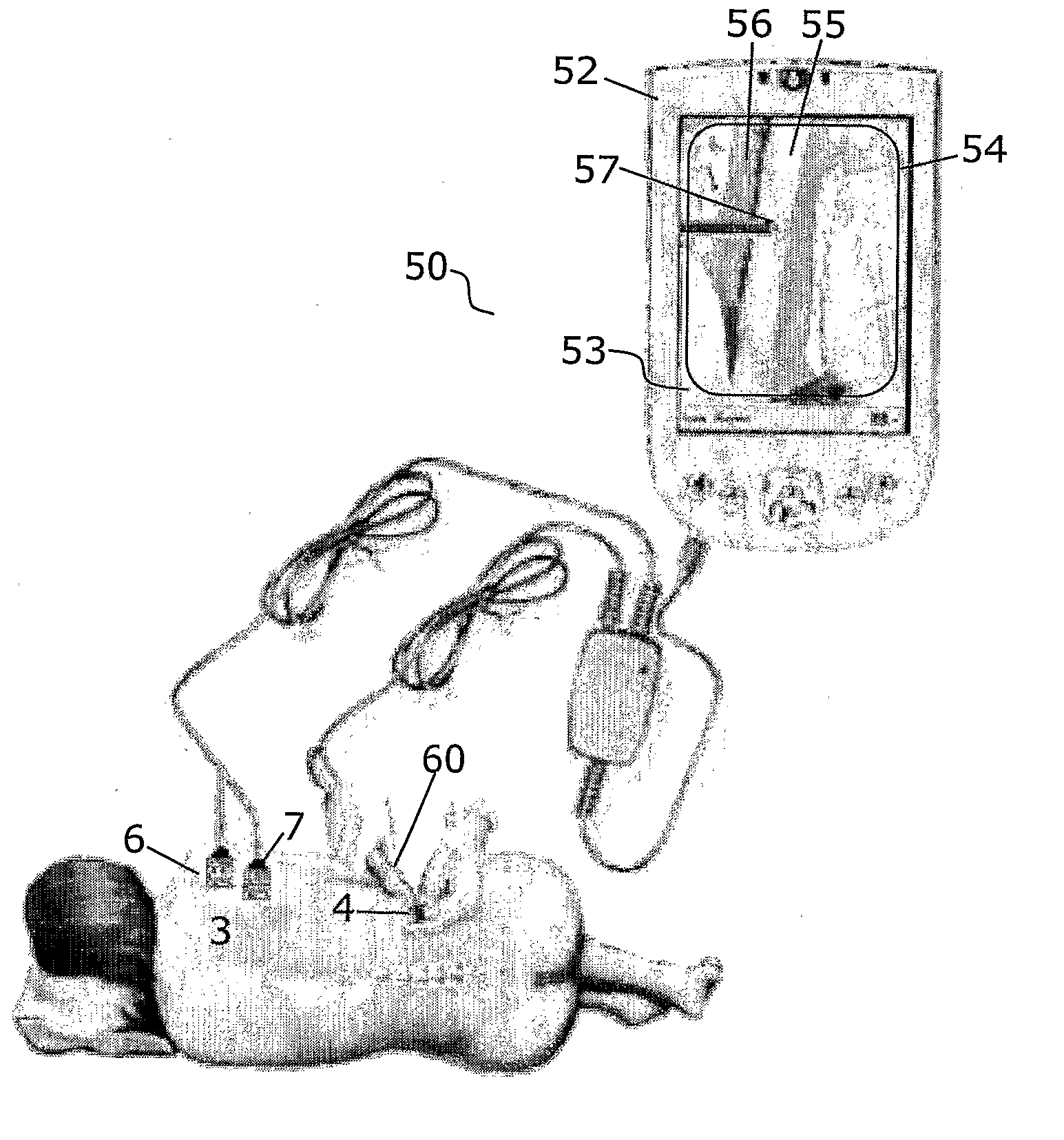
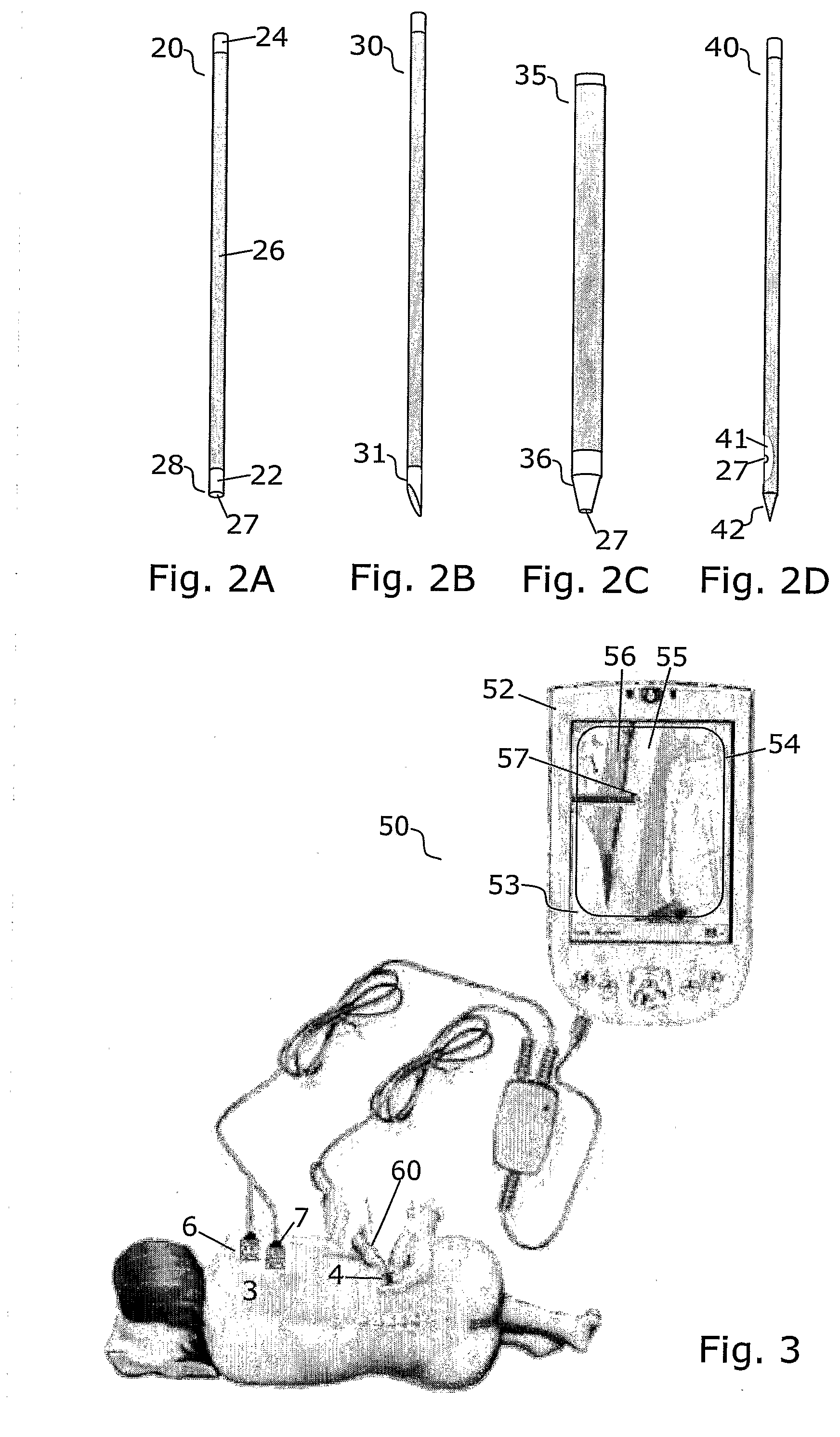
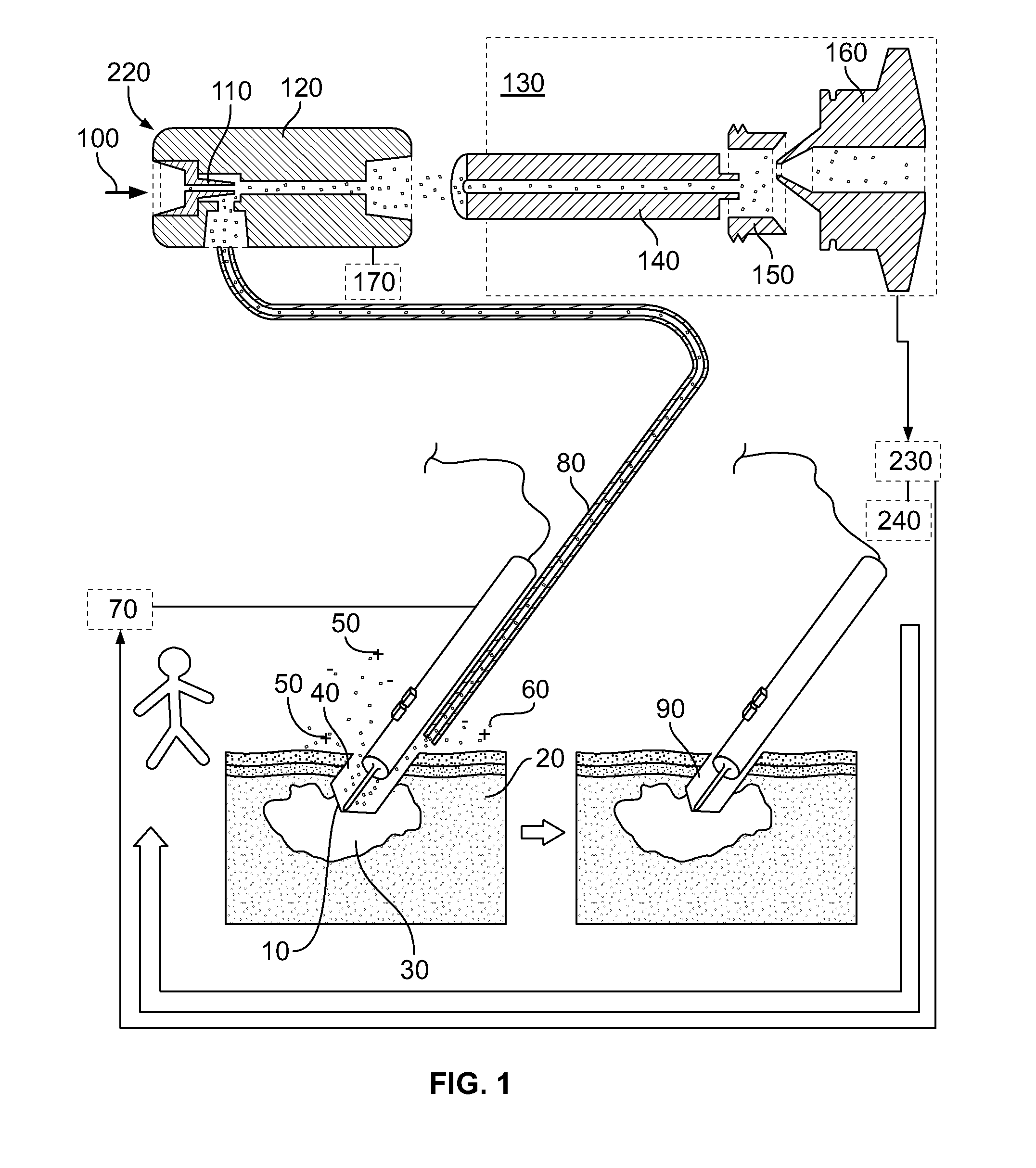
Method and apparatus for determining local tissue impedance for positioning of a needle
InactiveUS20090036794A1Eliminate impedanceGood distinctionDiagnostic recording/measuringSensorsTissues typesSubcutaneous tissue
The invention relates to apparatus and methods for measuring local tissue impedance for subcutaneous tissue surrounding a needle tip inserted into a subject, impedance spectra and / or complex impedance values are determined. The invention applies a monopolar impedance measuring setup with a needle, a current-carrying electrode, an optional reference electrode. The setup is configured to eliminate contributions from the current-carrying electrode in order to measure local impedance of tissue in the close neighbourhood of the needle tip instead of an averaged value over the volume or current path between the needle and the electrode(s). The determined impedance can be correlated with either a tissue type or state, or with a position of the needle tip in the subject, and can thereby provide an insertion history to the operator in the form of impedance or corresponding tissue type as a function of insertion depth or time.
Owner:UNIV OSLO HF
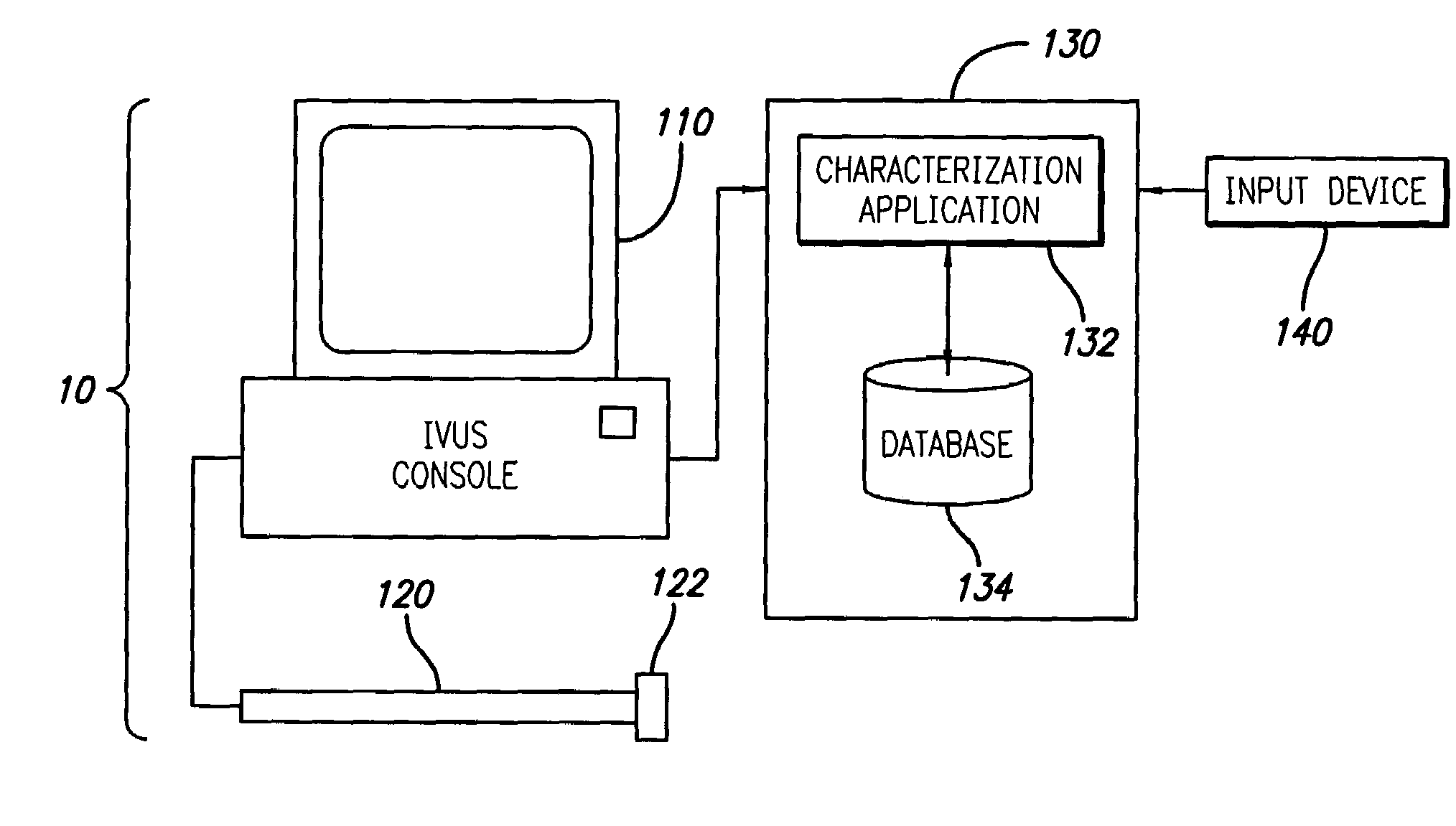
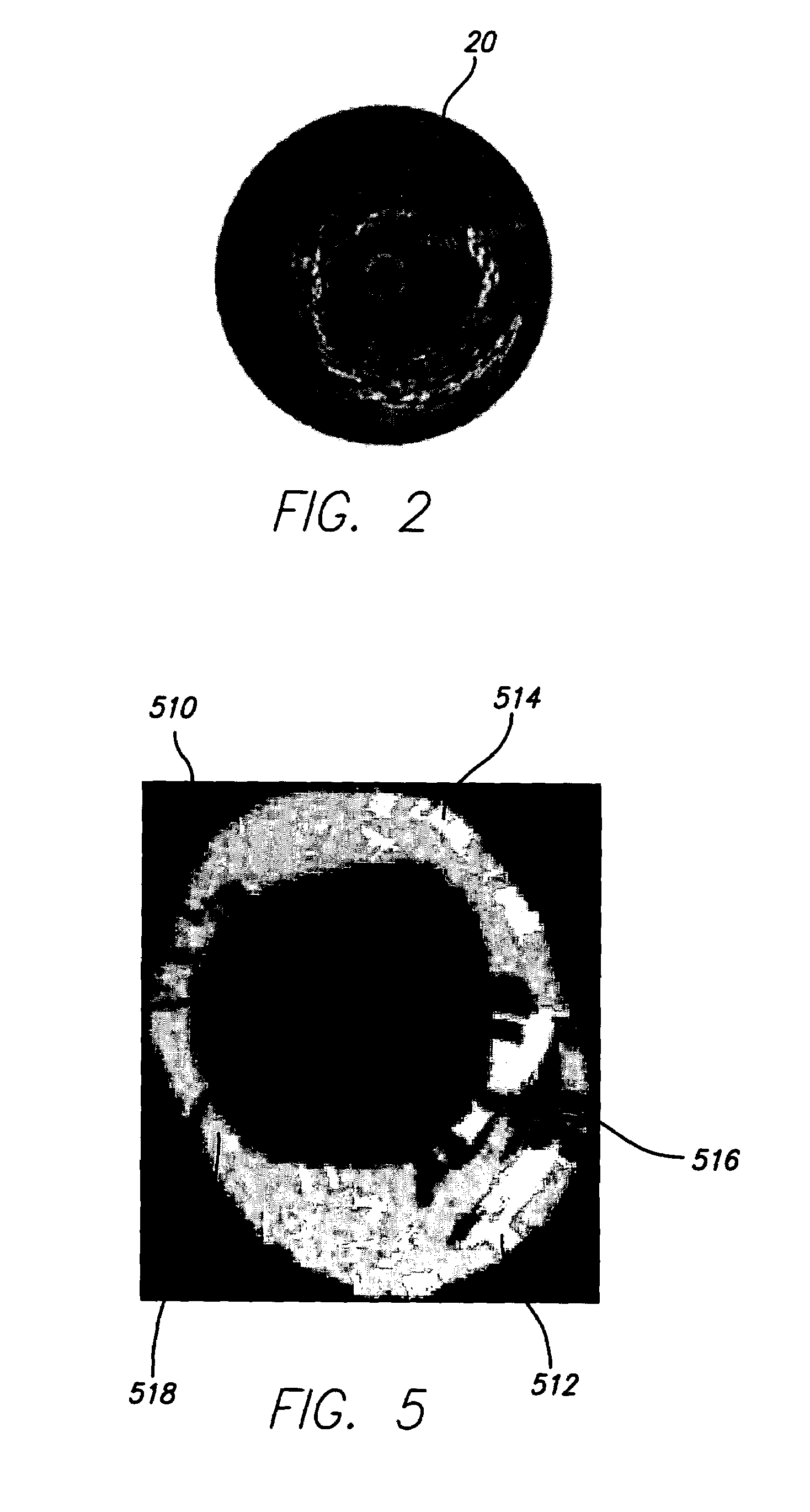
System and method of characterizing vascular tissue
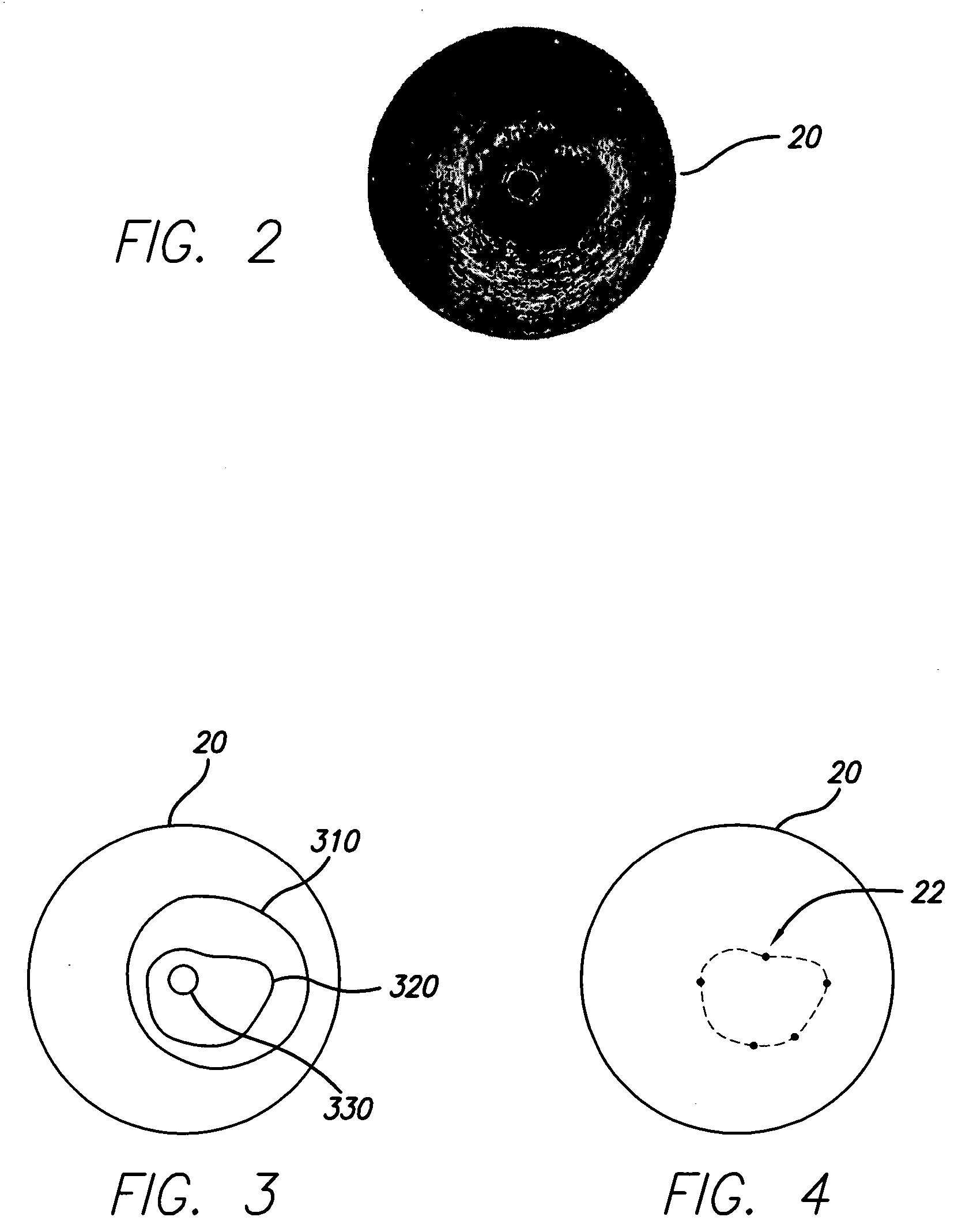
A system and method is provided for using backscattered data and known parameters to characterize vascular tissue. Specifically, in one embodiment of the present invention, an ultrasonic device is used to acquire RF backscattered data (i.e., IVUS data) from a blood vessel. The IVUS data is then transmitted to a computing device and used to create an IVUS image. The blood vessel is then cross-sectioned and used to identify its tissue type and to create a corresponding image (i.e., histology image). A region of interest (ROI), preferably corresponding to the identified tissue type, is then identified on the histology image. The computing device, or more particularly, a characterization application operating thereon, is then adapted to identify a corresponding region on the IVUS image. To accurately match the ROI, however, it may be necessary to warp or morph the histology image to substantially fit the contour of the IVUS image. After the corresponding region is identified, the IVUS data that corresponds to this region is identified. Signal processing is then performed and at least one parameter is identified. The identified parameter and the tissue type (e.g., characterization data) is stored in a database. In another embodiment of the present invention, the characterization application is adapted to receive IVUS data, determine parameters related thereto (either directly or indirectly), and use the parameters stored in the database to identify a tissue type or a characterization thereof.
Owner:THE CLEVELAND CLINIC FOUND
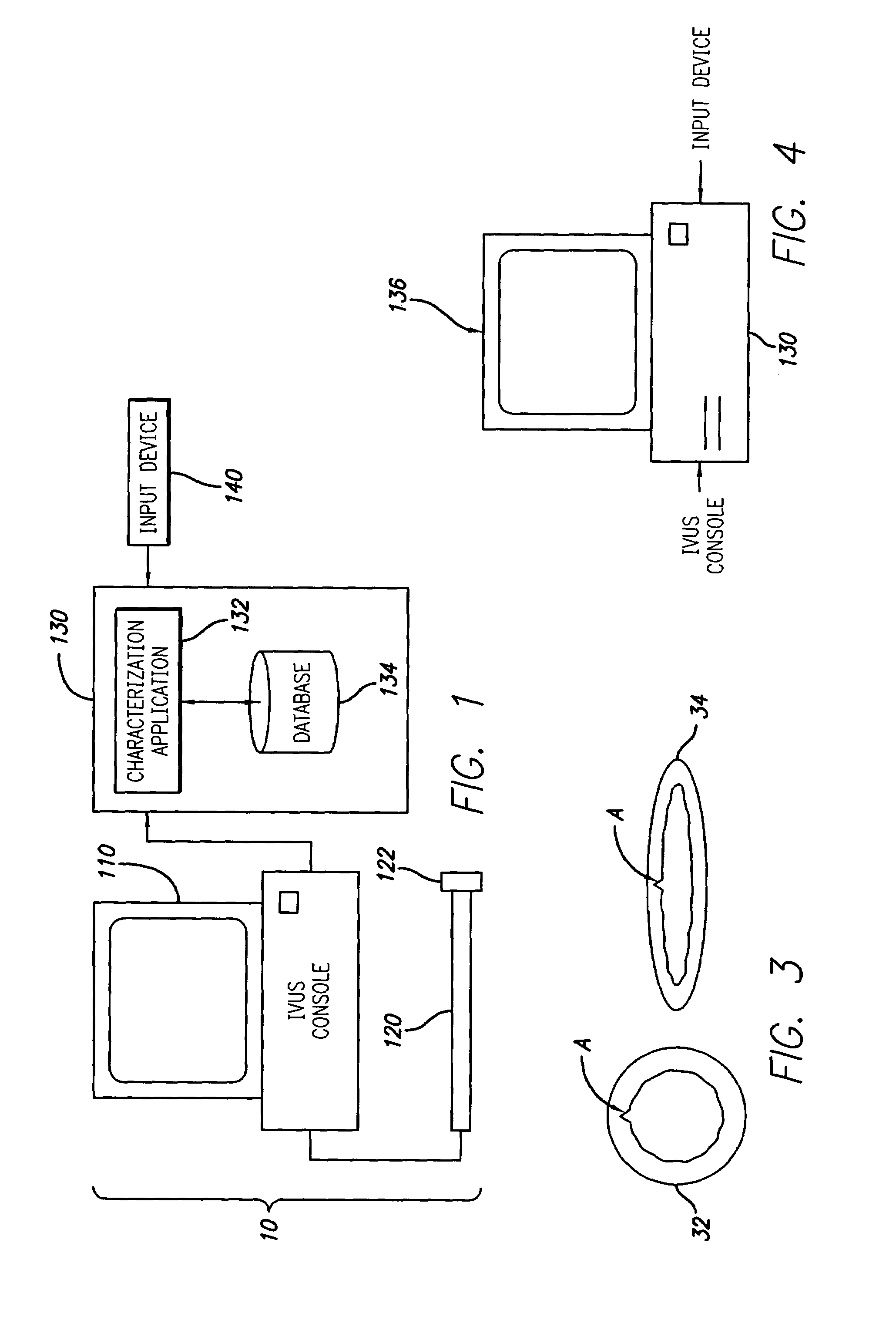
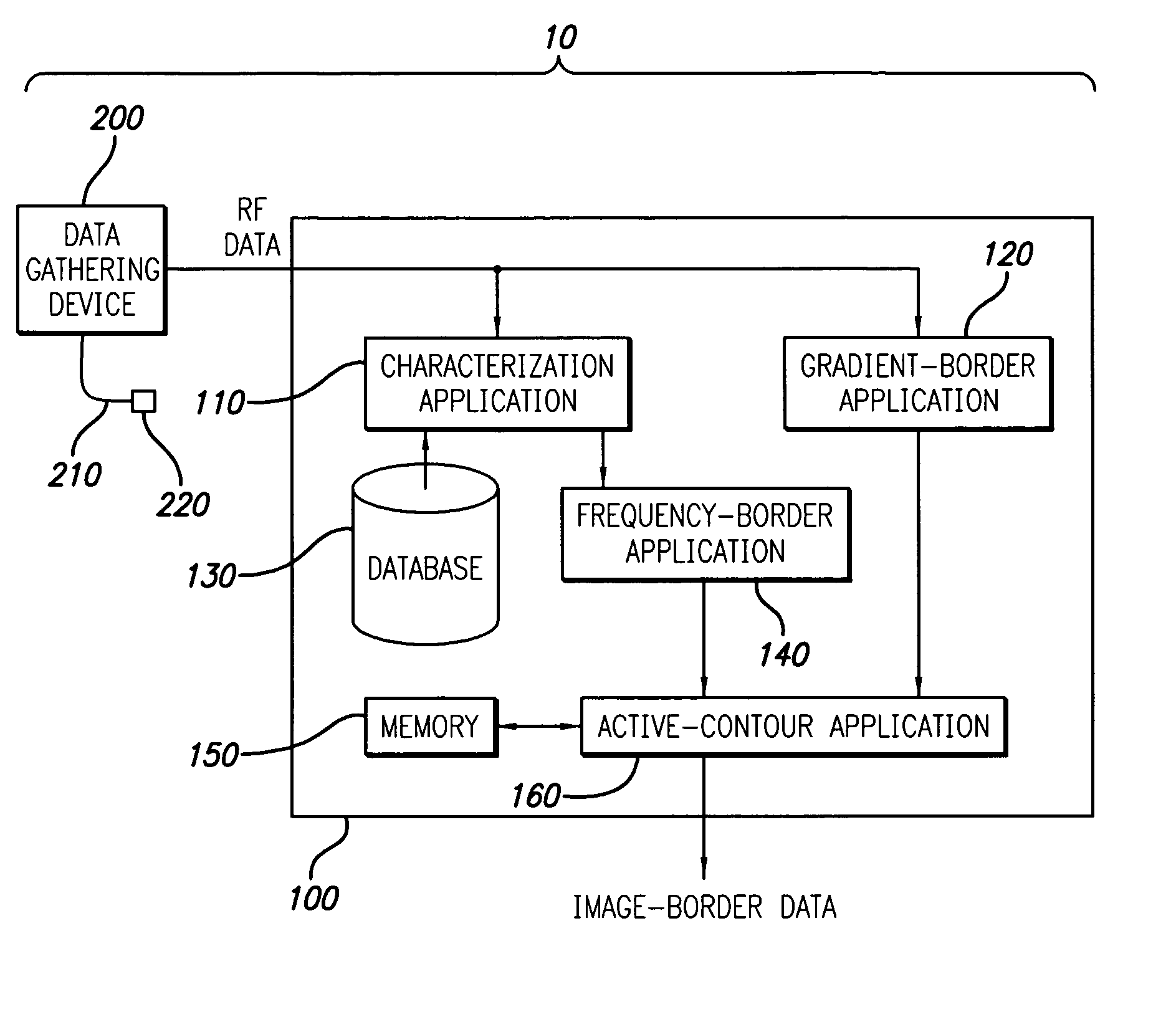
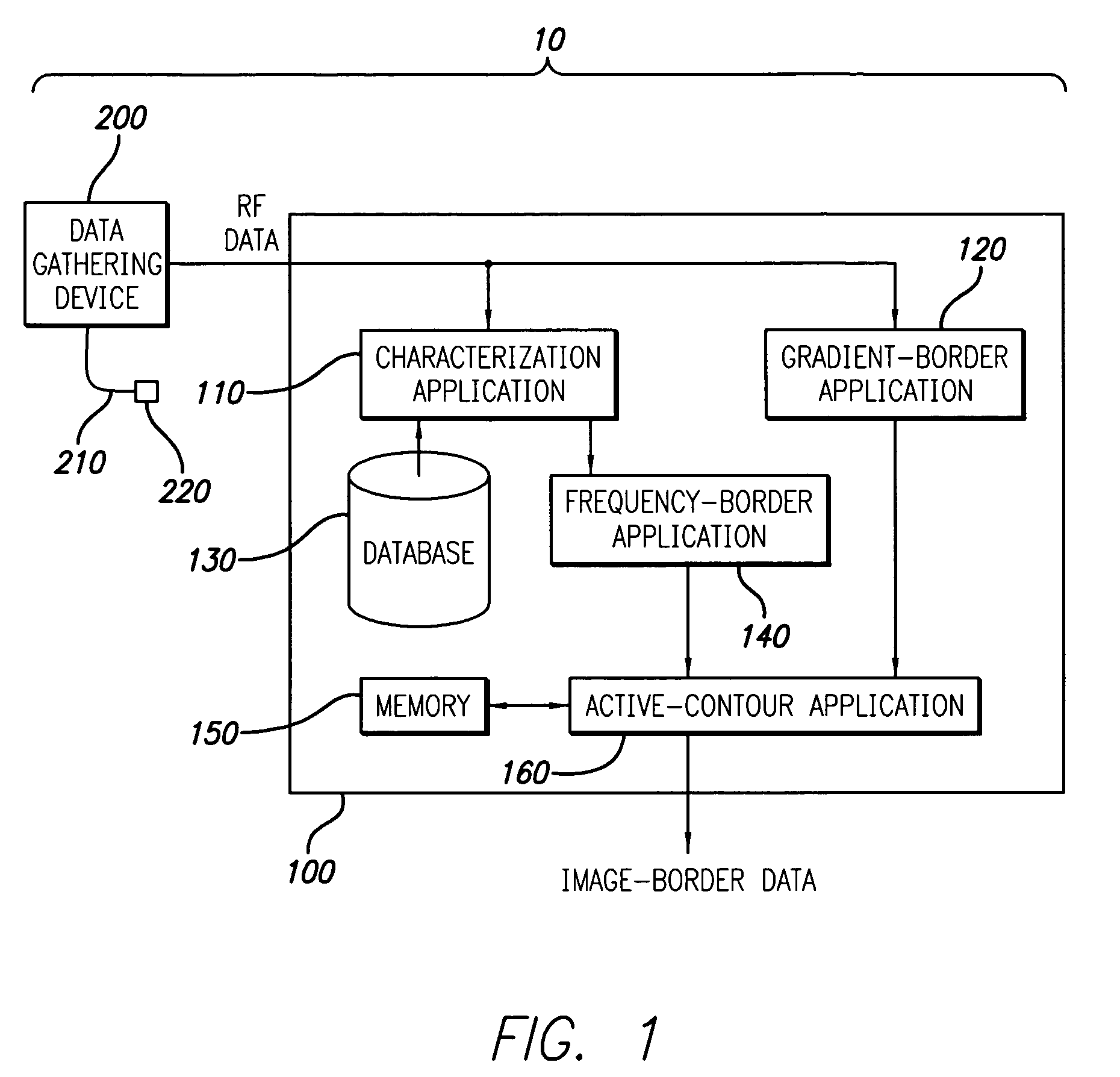
System and method for vascular border detection
A system and method is provided for using the frequency spectrum of a radio frequency (RF) signal backscattered from vascular tissue to identify at least one border (e.g., tissue interface, etc.) on a vascular image. Embodiments of the present invention operate in accordance with a data gathering device (e.g., an intra-vascular ultrasound (IVUS) device, etc.) electrically connected to a computing device and a transducer via a catheter. The transducer is used to gather radio frequency (RF) data backscattered from vascular tissue. The RF data is then provided to (or acquired by) the computing device via the data-gathering device. In one embodiment of the present invention, the computing device includes (i) at least one data storage device (e.g., database, memory, etc.) for storing a plurality of tissue types and parameters related thereto and (ii) at least one application (e.g., a characterization application, a gradient-border application, a frequency-border application and / or an active-contour application). The characterization application is used to convert (or transform) the RF data into the frequency domain and to identify a plurality of parameters associated therewith. The identified parameters are then compared to the parameters stored in the data storage device to identify the corresponding tissue type. This information (e.g., tissue type, corresponding RF data, etc.) is then used, either alone or together with other border-related information (e.g., gradient information, other-border information, etc.), to determine at least one border on a vascular image.
Owner:THE CLEVELAND CLINIC FOUND
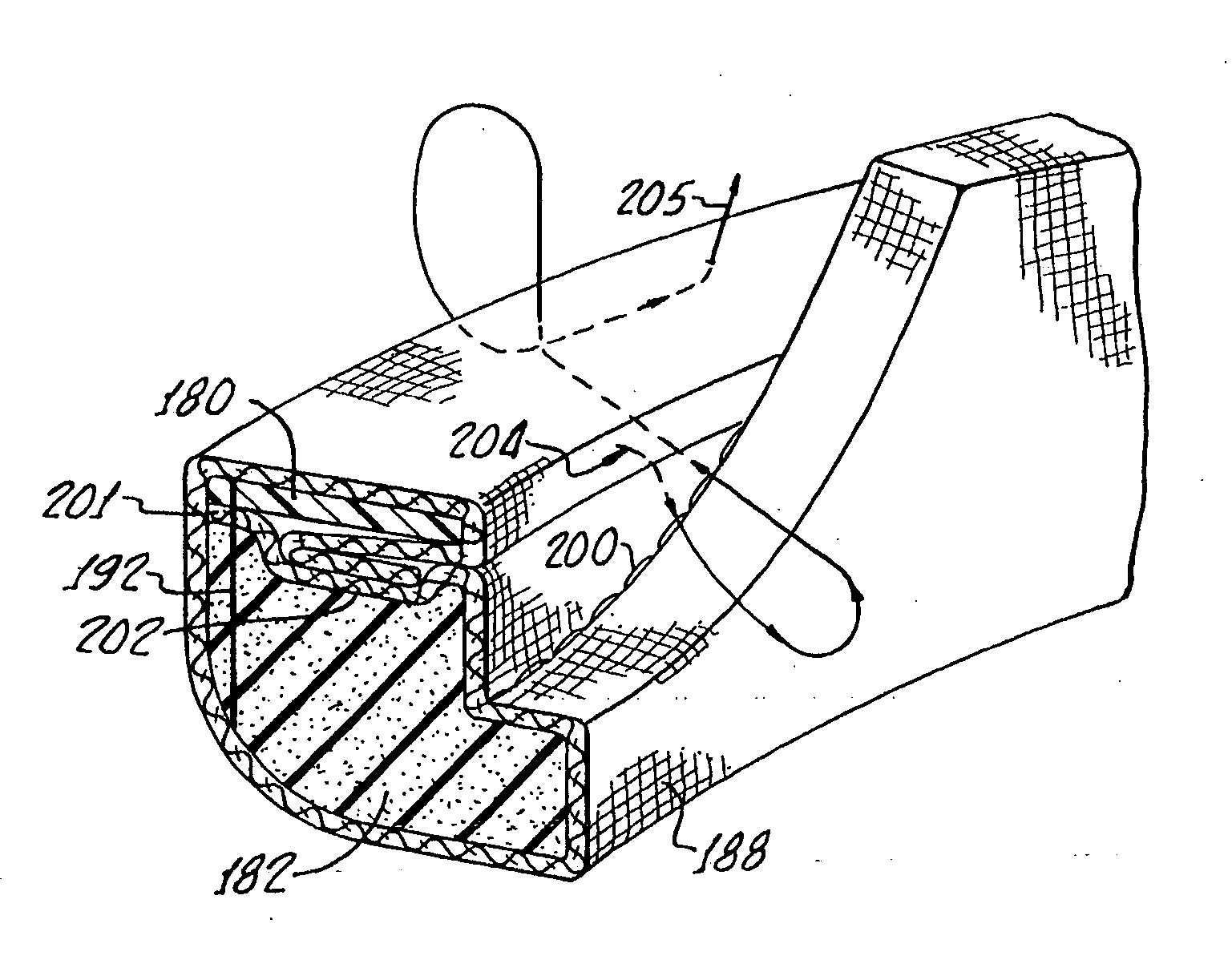
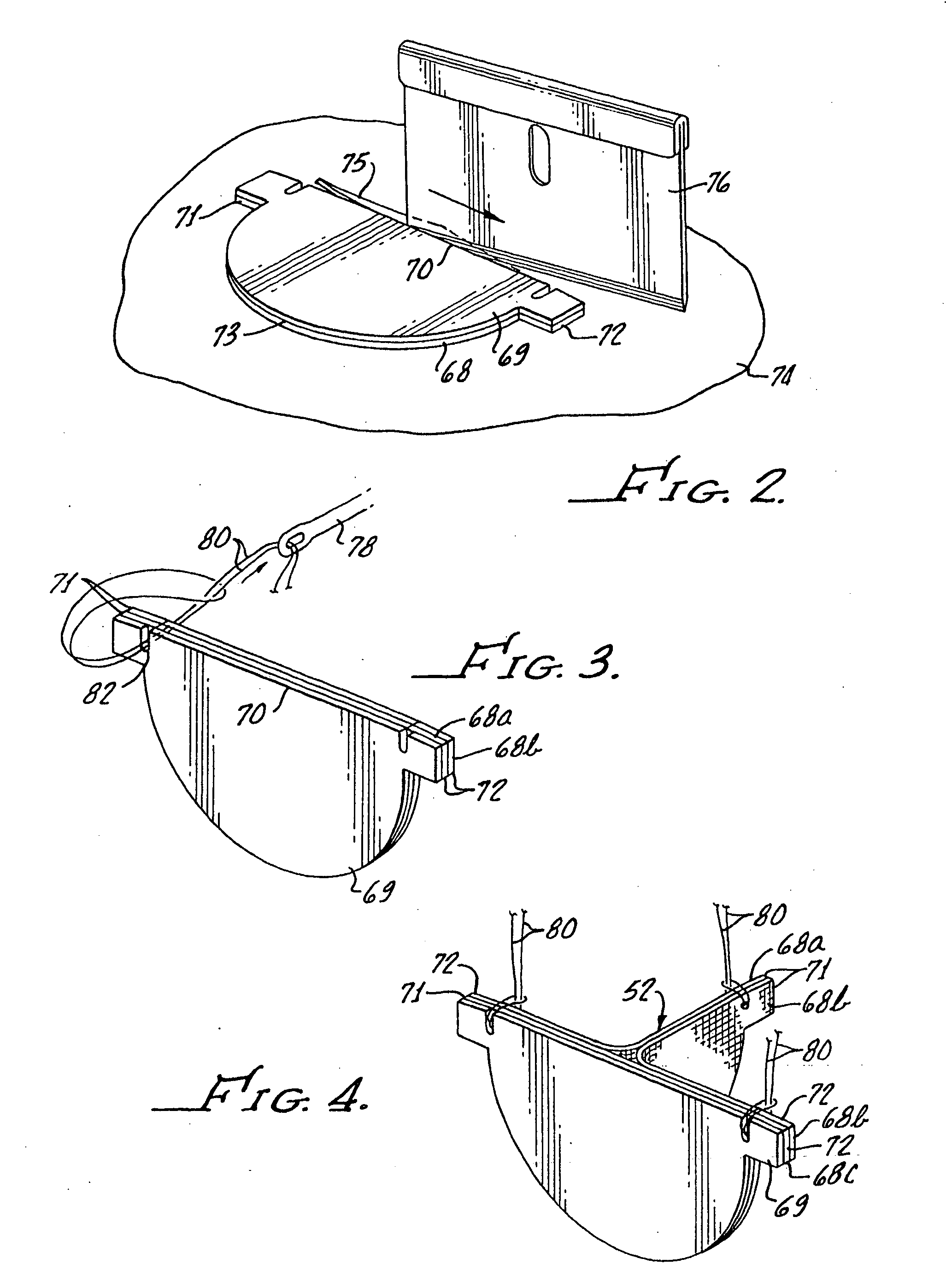
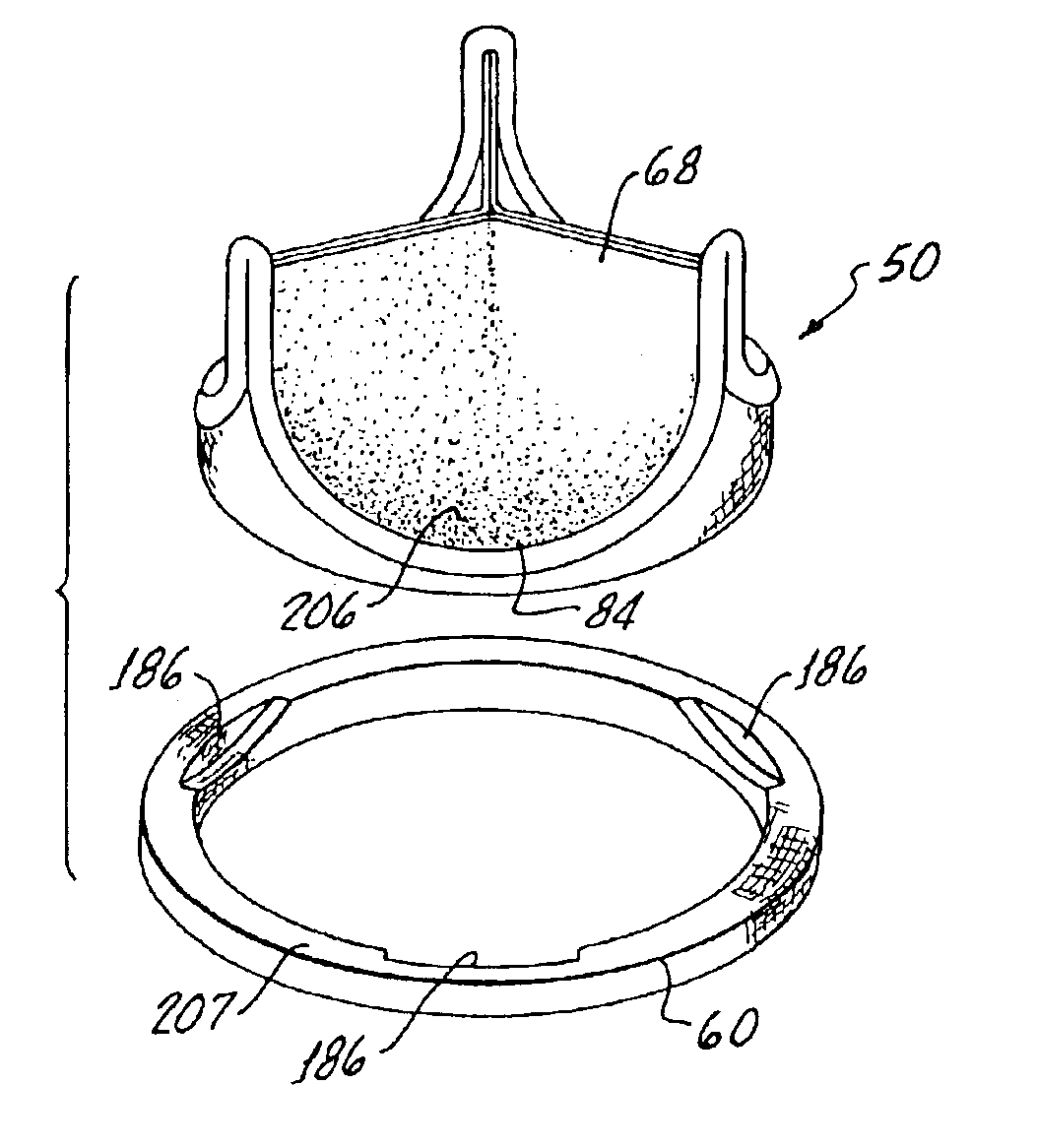
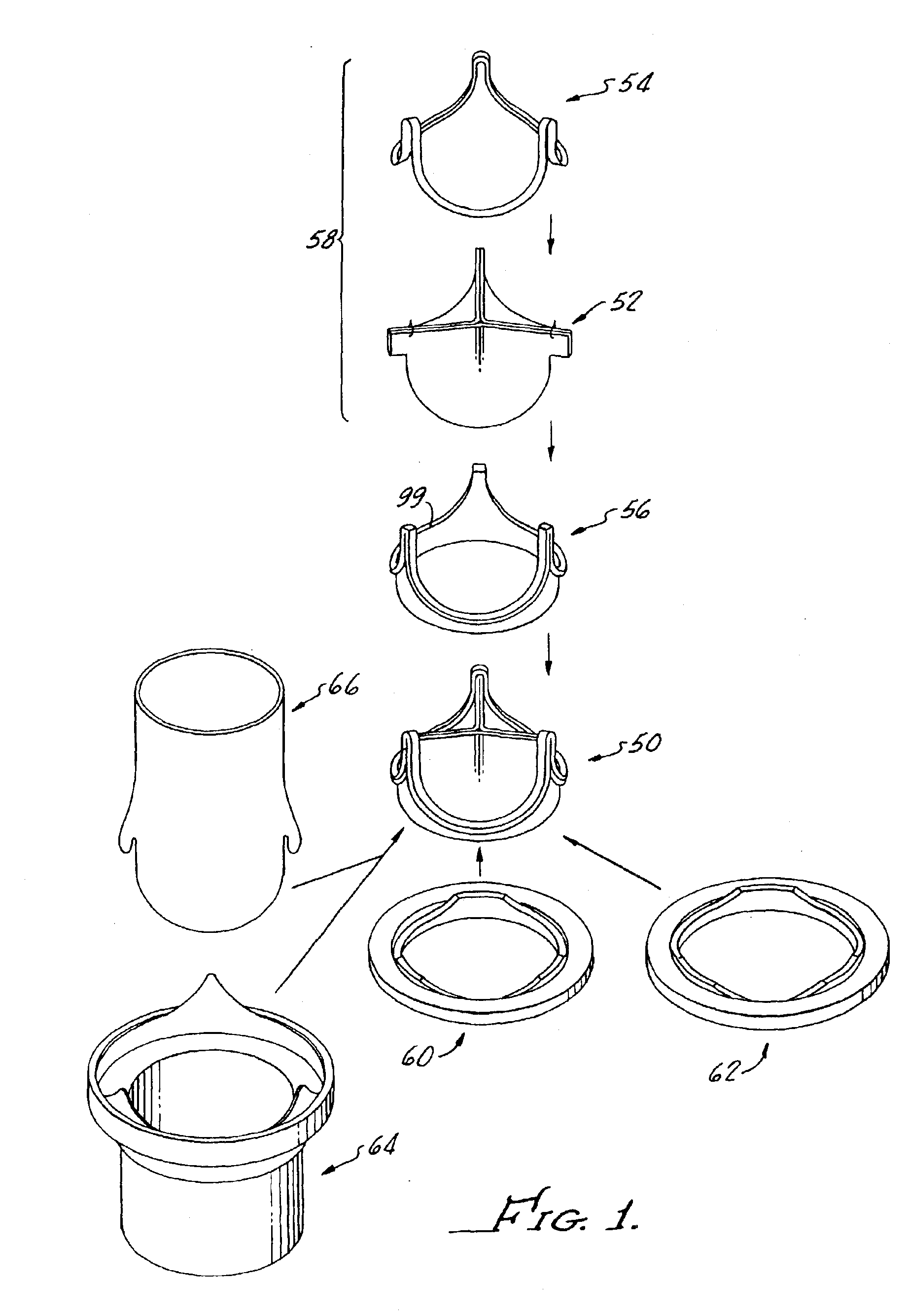
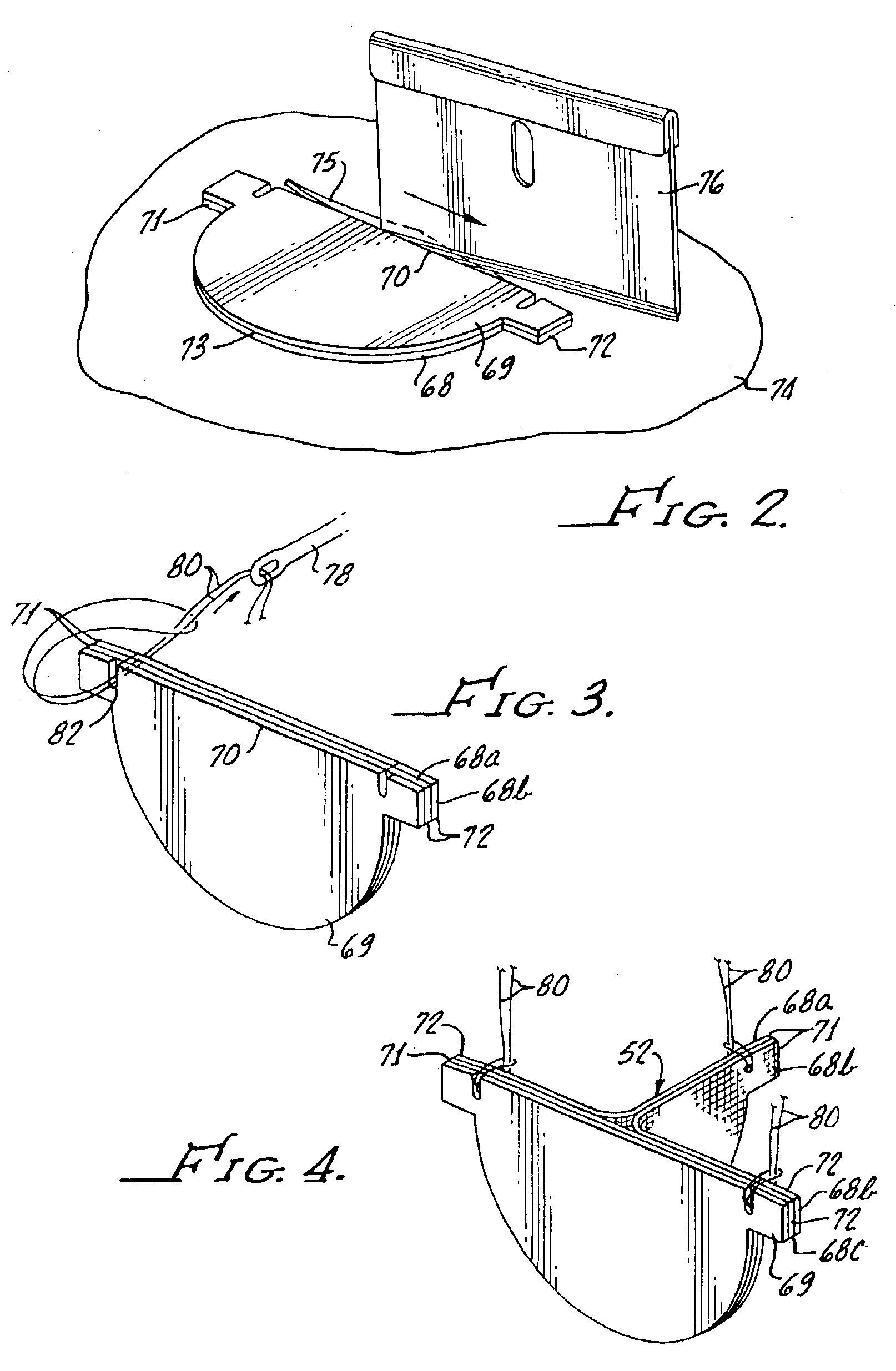
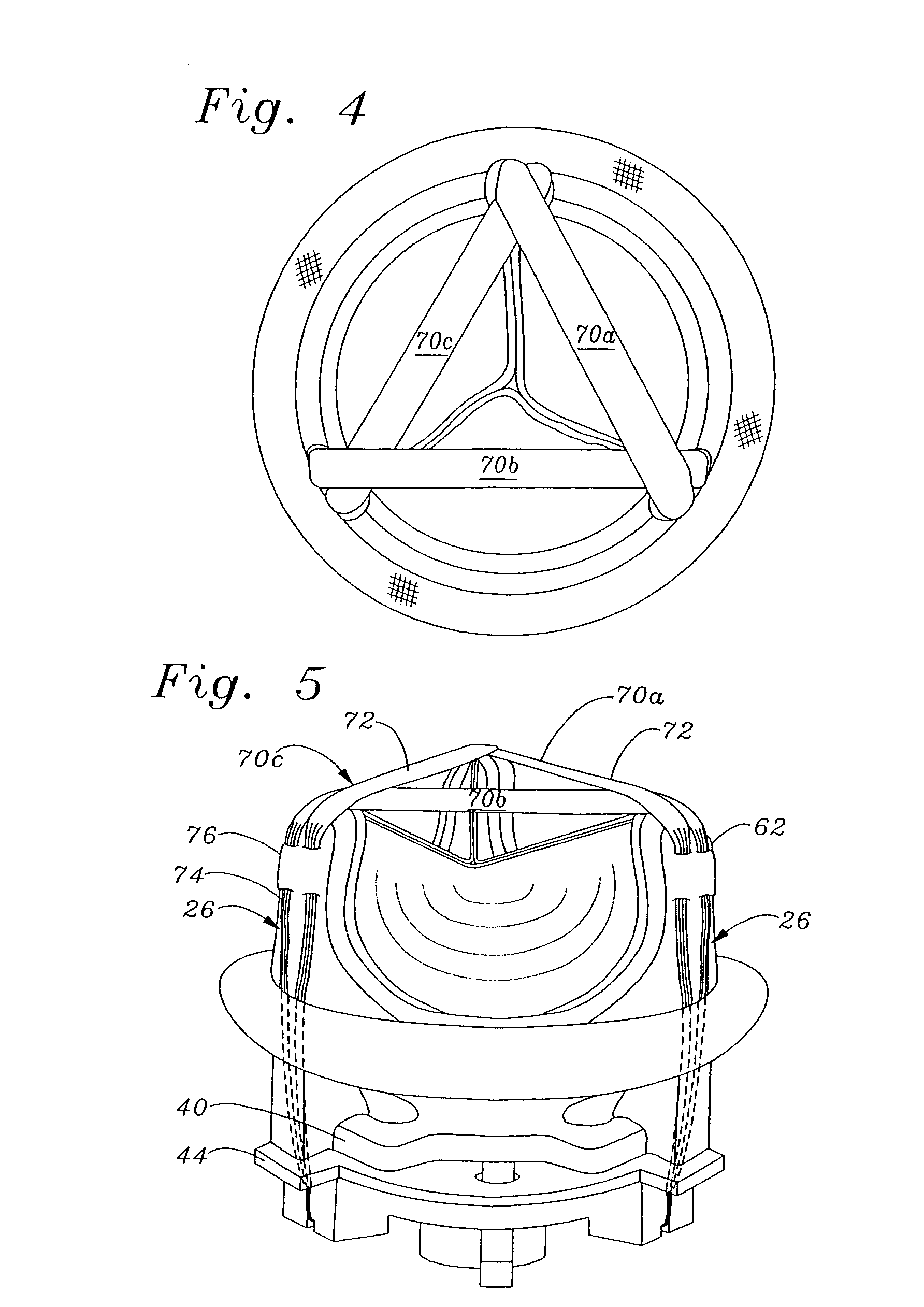
Contoured heart valve suture rings
InactiveUS20060009842A1Improving long-term functionalityReduce pointsHeart valvesInsertion stentCatheter
Improved, adaptable tissue-type heart valves and methods for their manufacture are disclosed wherein a dimensionally stable, pre-aligned tissue leaflet subassembly is formed and its peripheral edge clamped between and attached to an upper shaped wireform and a lower support stent. A variety of adaptable structural interfaces including suture rings, flanges, and conduits may be attached to the support stent with or without an outlet conduit disposed about the wireform to provide a tissue-type heart valve adaptable for use in either a natural heart or in mechanical pumping devices. The methods include forming individual leaflets with a template and using the template to attach the leaflets together to form a tissue leaflet subassembly. The template and leaflets include a straight edge terminating in oppositely directed tabs, and a curvilinear cusp edge extending opposite the straight edge. The template may include a guide slot in its straight edge and the assembly includes aligning two leaflet tabs with the template and passing sutures through the guide slot and through the leaflet tabs. The leaflet subassembly is mated to a wireform with the tabs extending through commissure posts of the wireform. A support stent having an upper surface matching the lower surface of the wireform sandwiches the edges of the leaflet subassembly therebetween. Separated tabs on the leaflet subassembly are passed through the wireform commissures and attached to adjacent stent commissures so as to induce clamping of the leaflet tabs between the stent commissures and wireform commissures upon a radially inward force being applied to the leaflets.
Owner:EDWARDS LIFESCIENCES CORP
Heart valves and suture rings therefor
InactiveUS6945997B2Reduce stress pointImproving long-term functionalityHeart valvesInsertion stentTissues types
Improved, adaptable tissue-type heart valves and methods for their manufacture are disclosed wherein a dimensionally stable, pre-aligned tissue leaflet subassembly is formed and its peripheral edge clamped between and attached to an upper shaped wireform and a lower support stent. A variety of adaptable structural interfaces including suture rings, flanges, and conduits may be attached to the support stent with or without an outlet conduit disposed about the wireform to provide a tissue-type heart valve adaptable for use in either a natural heart or in mechanical pumping devices. The methods include forming individual leaflets with a template and using the template to attach the leaflets together to form a tissue leaflet subassembly. The template and leaflets include a straight edge terminating in oppositely directed tabs, and a curvilinear cusp edge extending opposite the straight edge. The template may include a guide slot in its straight edge and the assembly includes aligning two leaflet tabs with the template and passing sutures through the guide slot and through the leaflet tabs. The leaflet subassembly is mated to a wireform with the tabs extending through commissure posts of the wireform. A support stent having an upper surface matching the lower surface of the wireform sandwiches the edges of the leaflet subassembly therebetween. Separated tabs on the leaflet subassembly are passed through the wireform commissures and attached to adjacent stent commissures so as to induce clamping of the leaflet tabs between the stent commissures and wireform commissures upon a radially inward force being applied to the leaflets.
Owner:EDWARDS LIFESCIENCES CORP
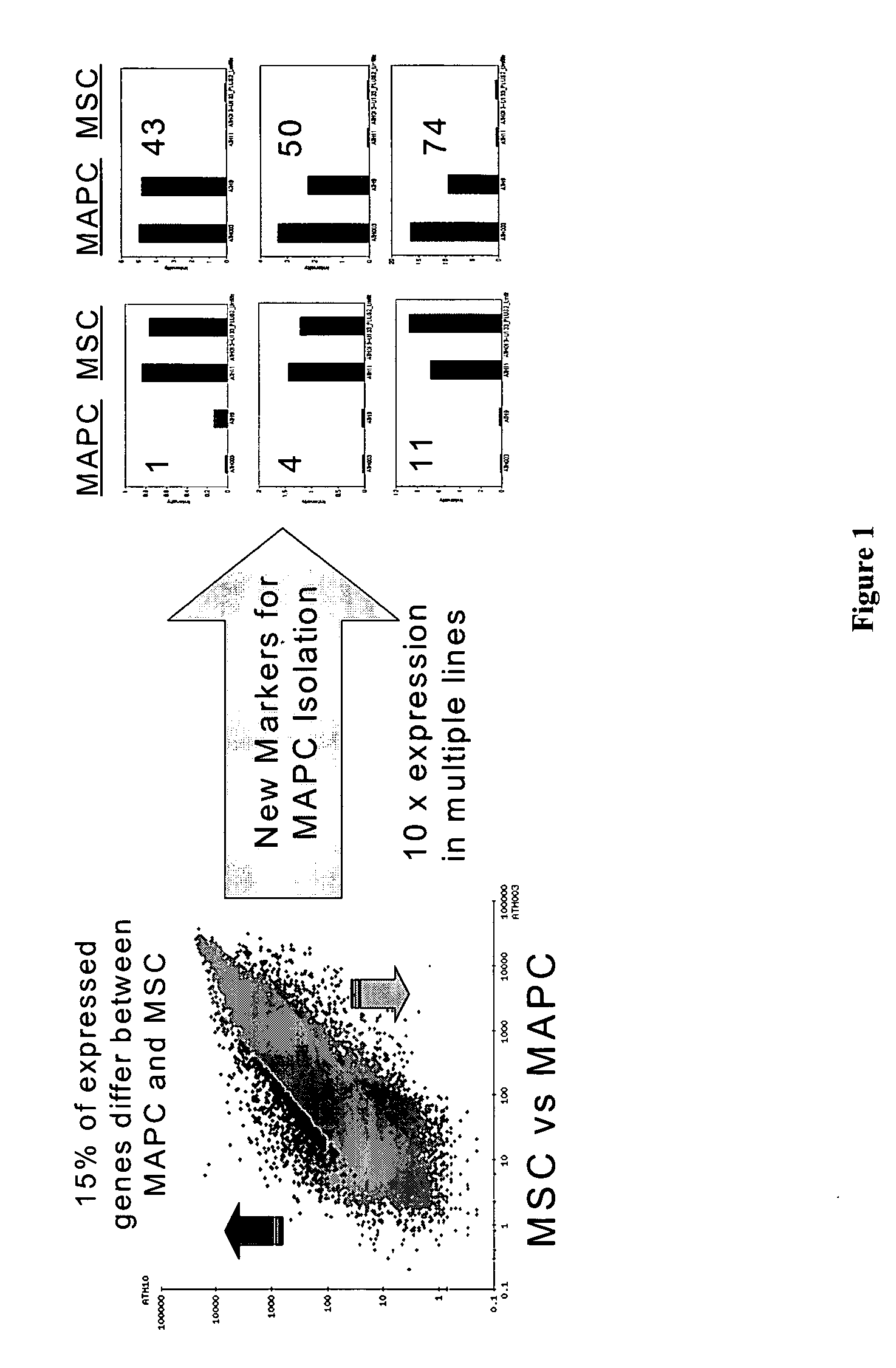
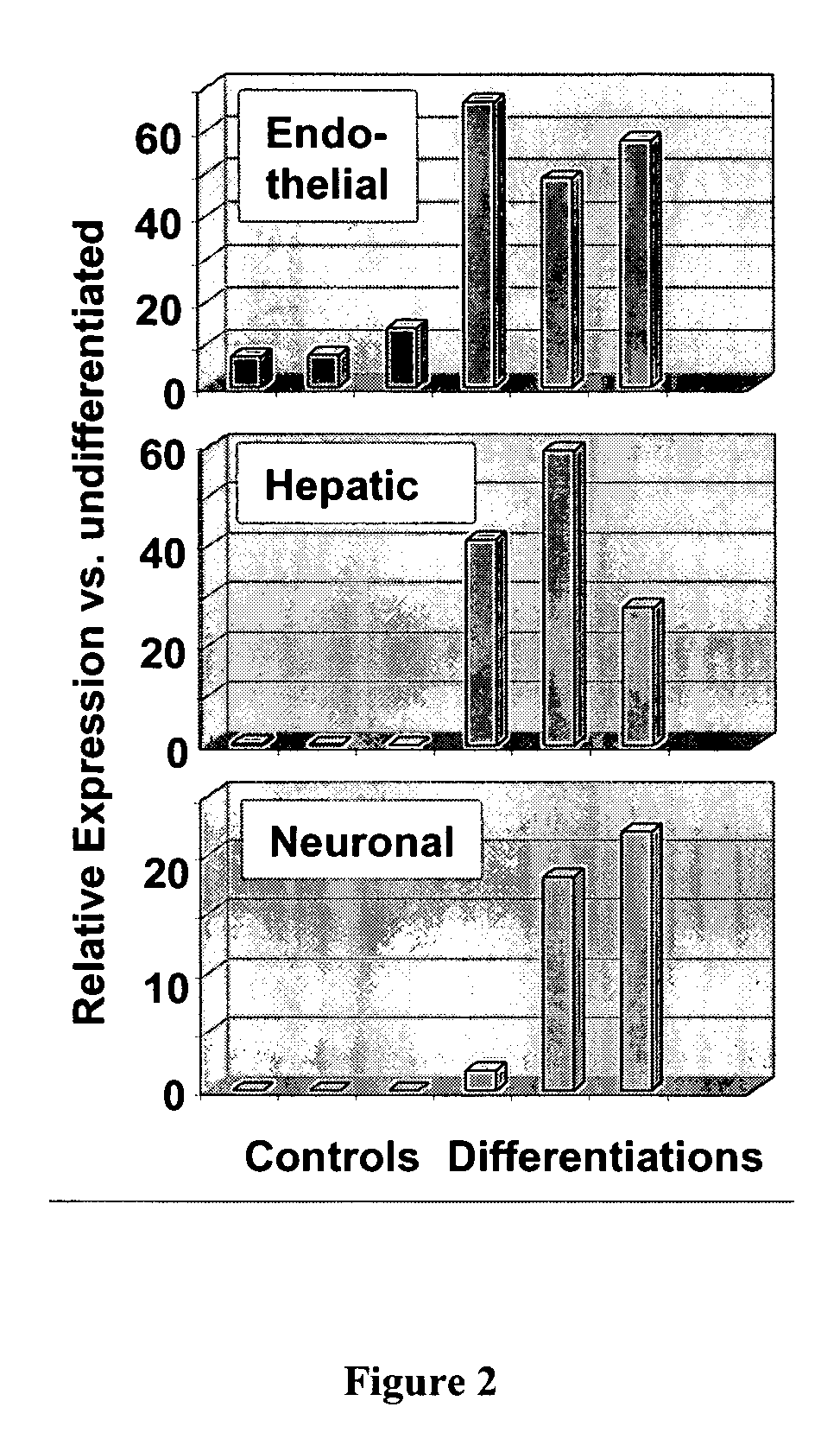
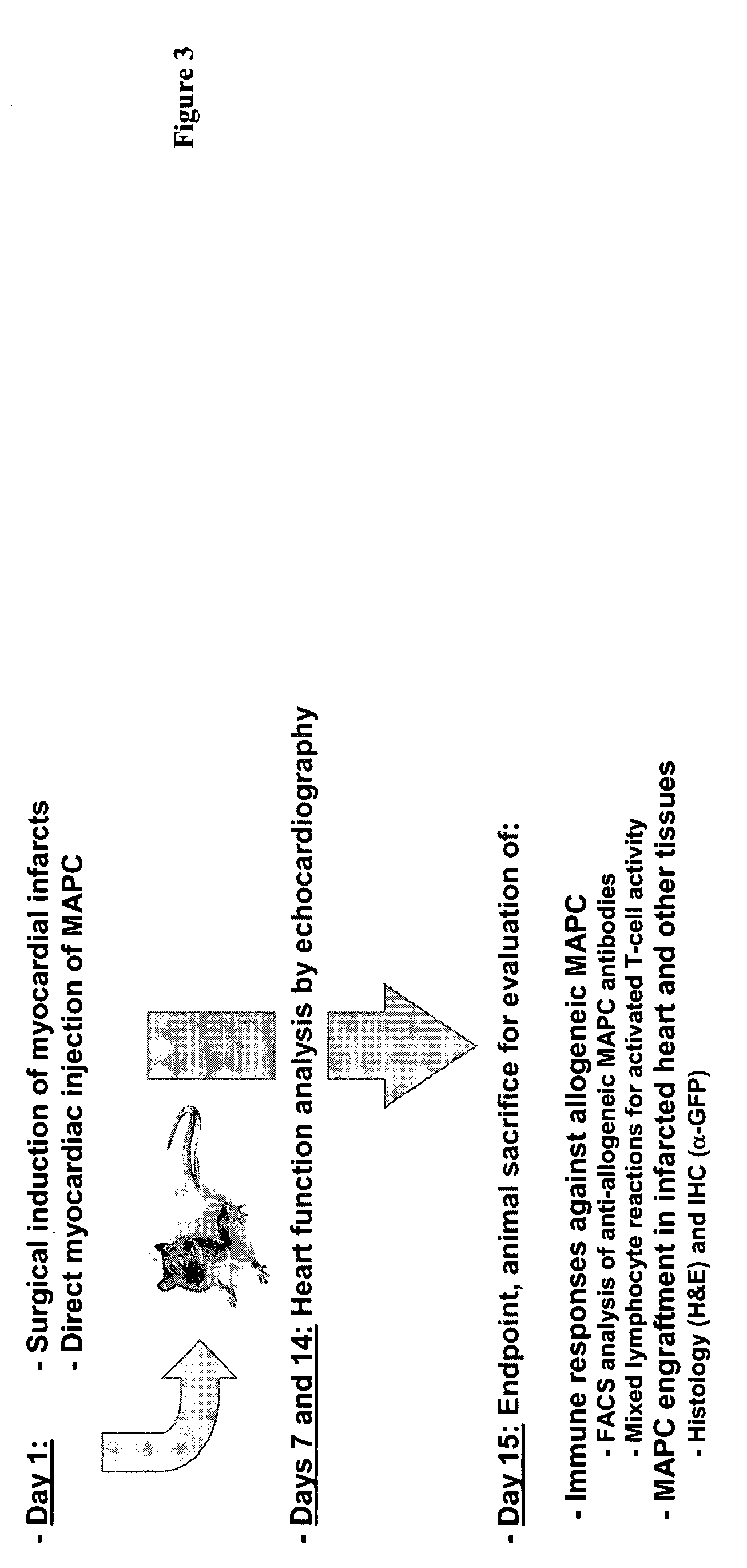
Use of multipotent adult stem cells in treatment of myocardial infarction and congestive heart failure
ActiveUS20060008450A1Restore and enhance cardiac muscle functionRapid responseBiocideGenetic material ingredientsTissues typesEmbryo
Owner:RGT UNIV OF MINNESOTA
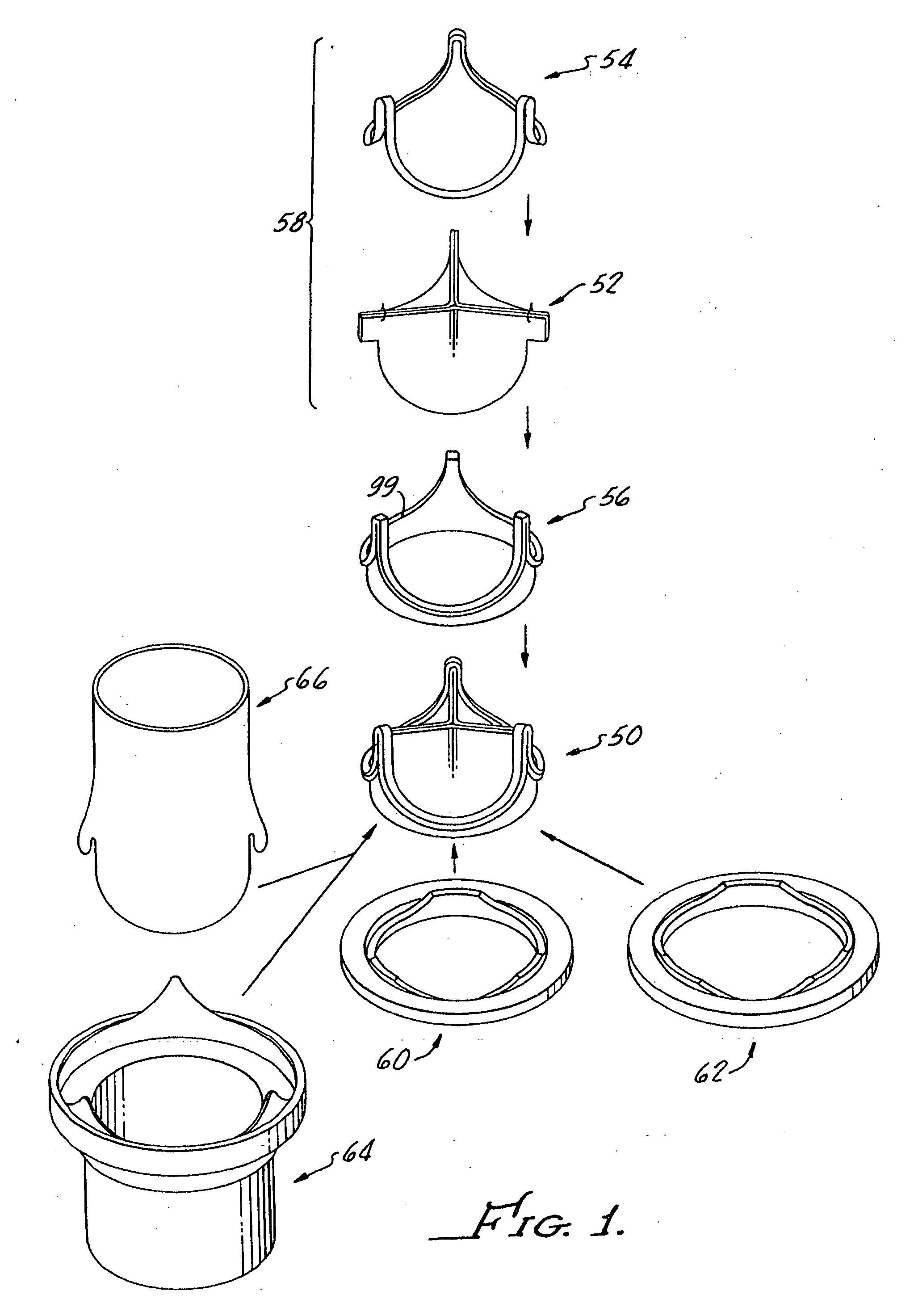
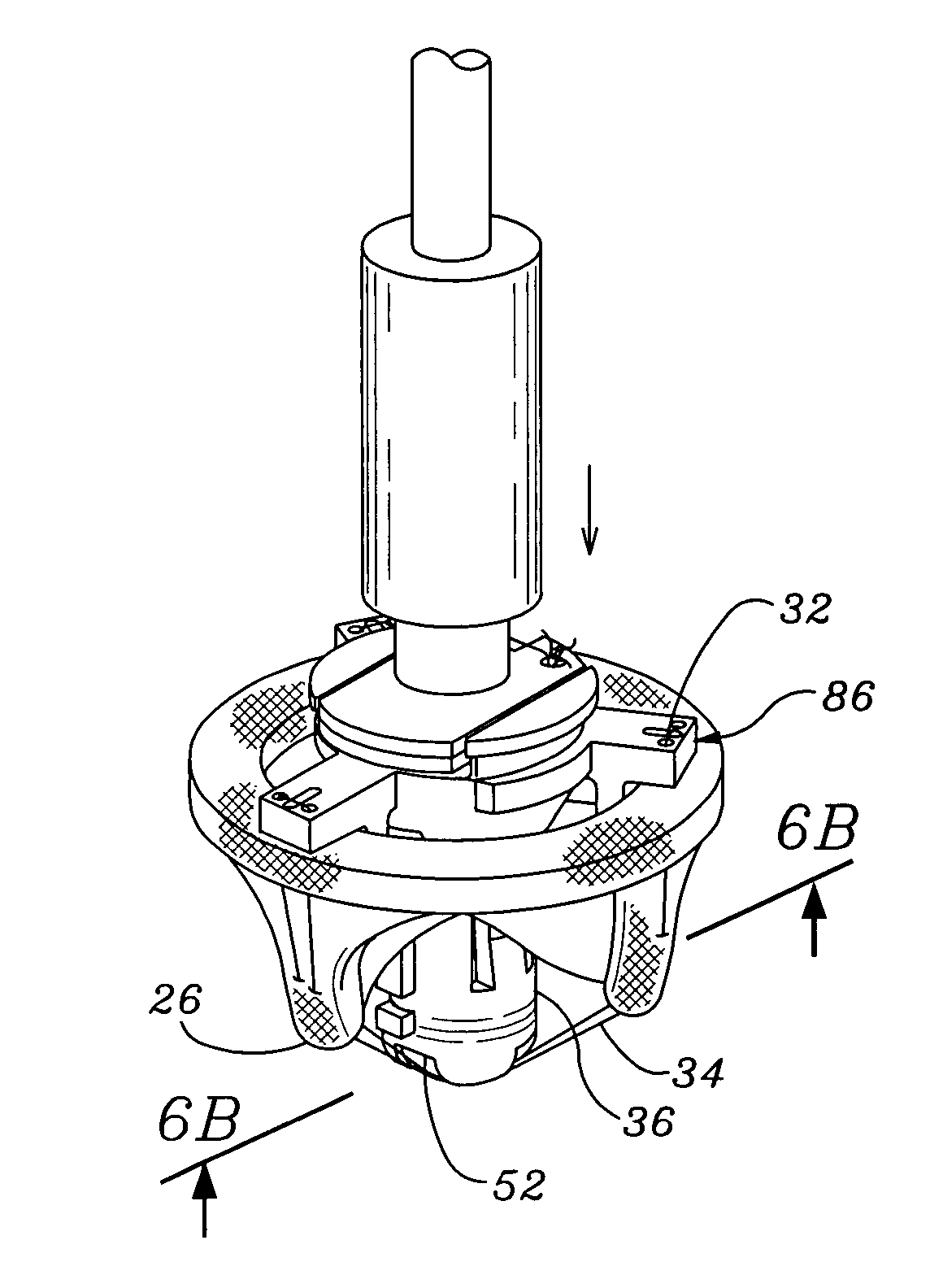
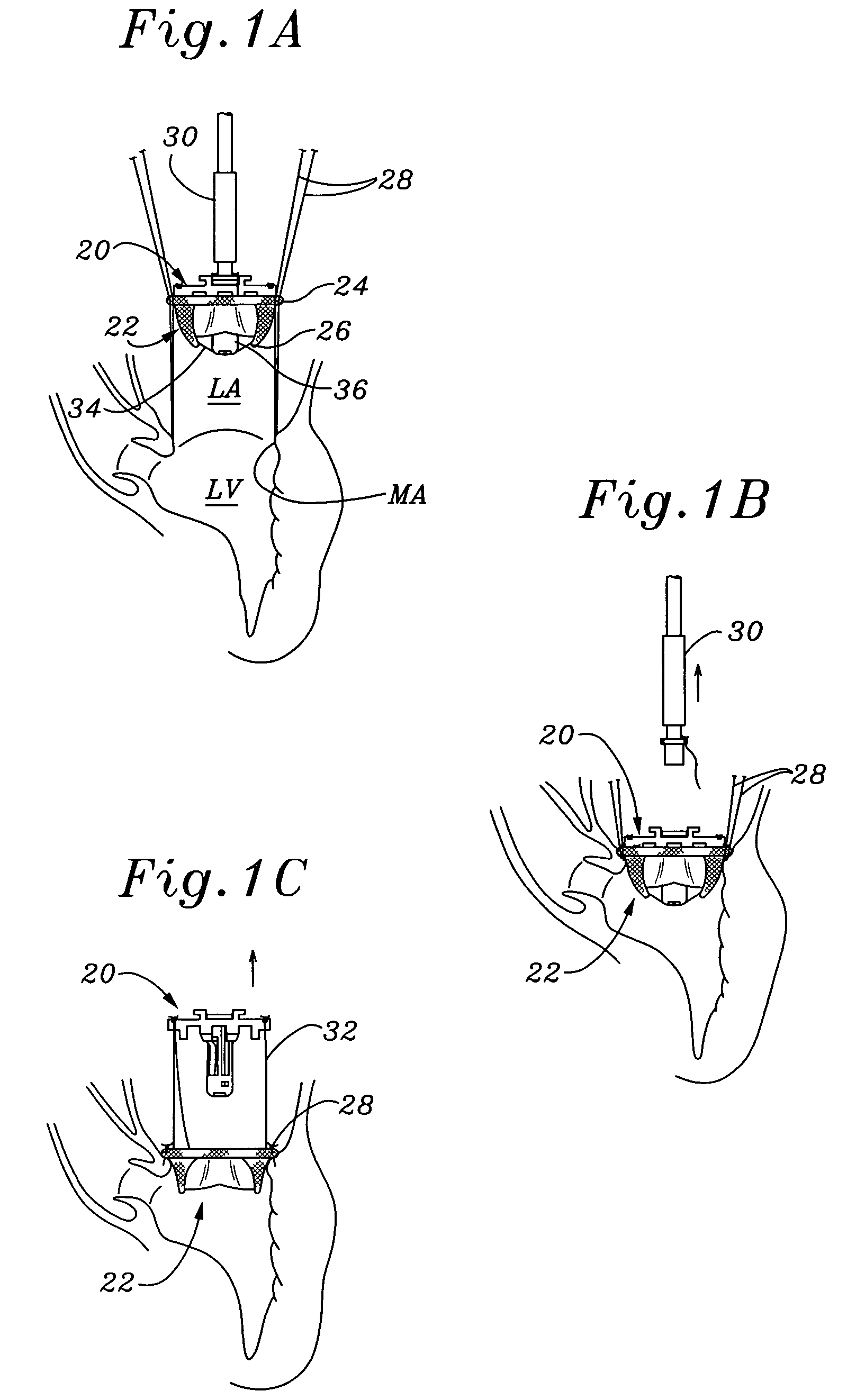
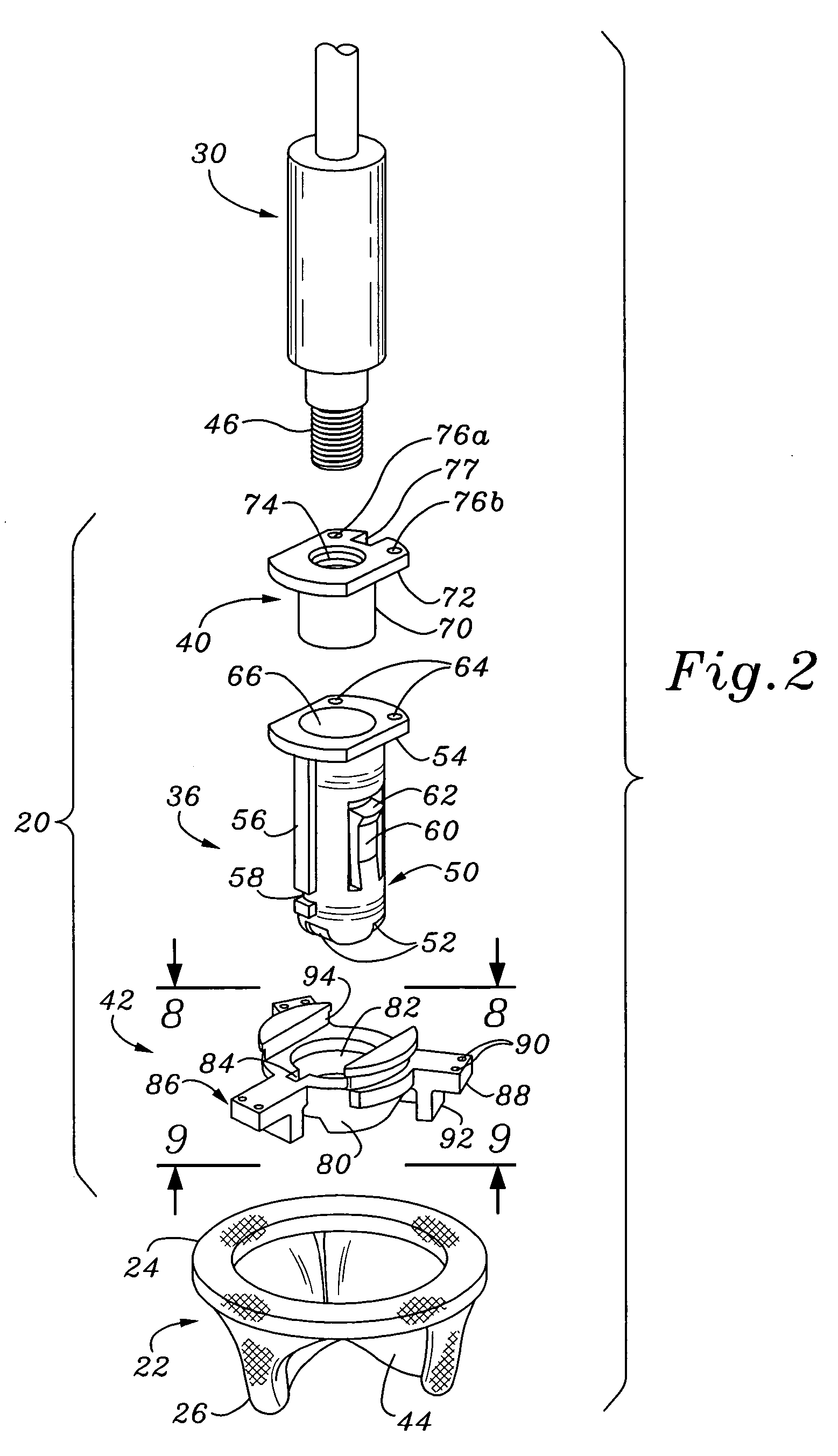
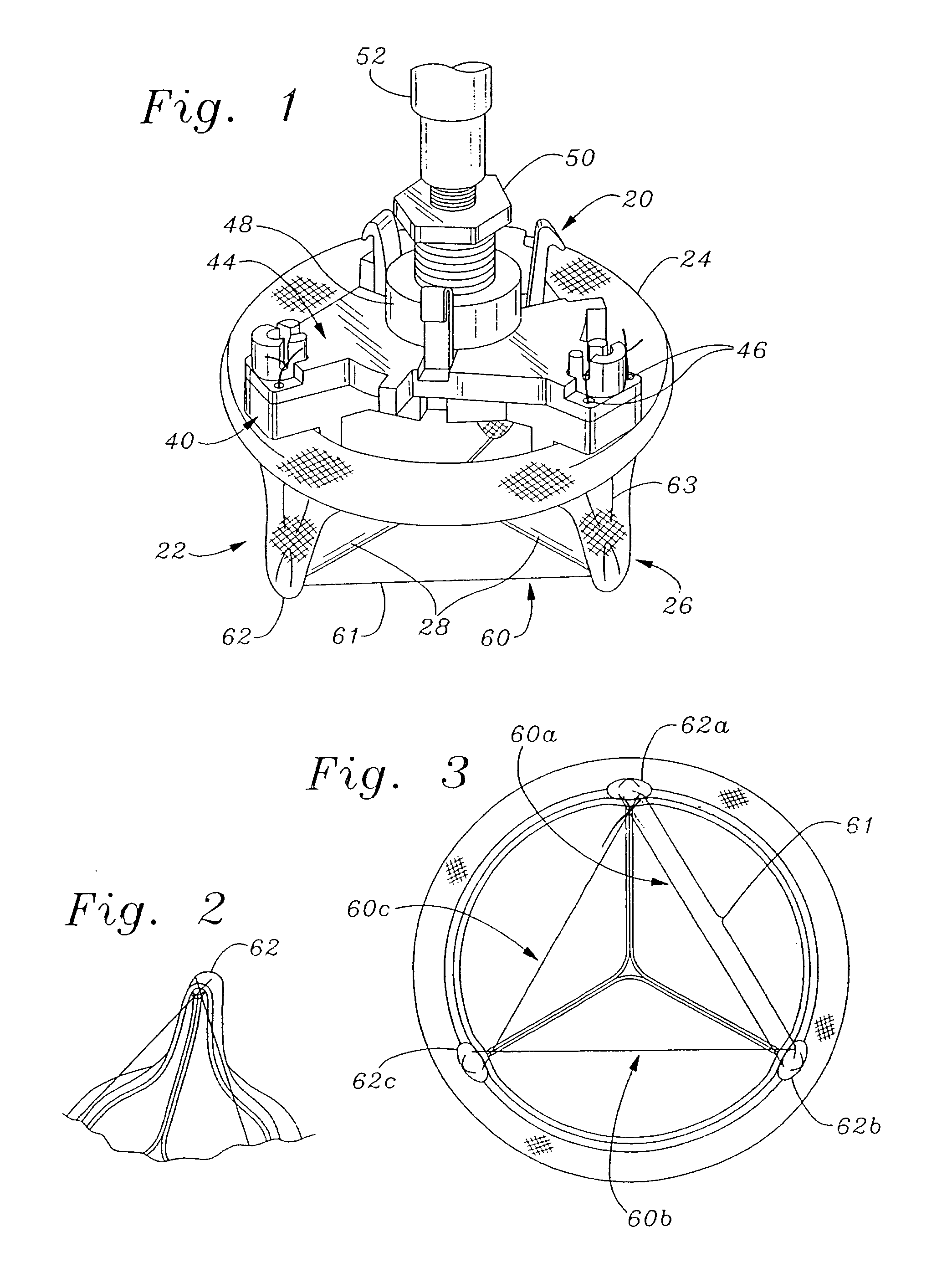
Heart valve holder and method for resisting suture looping
An improved holder and method for implanting a tissue-type prosthetic mitral heart valve that prevents suture looping and may also constrict the commissure posts of the valve. An upstanding or shaft member axially positioned on the holder causes the lengths of attachment sutures to extend axially beyond the commissure post tips to create a tent and prevent looping of any of an array of pre-implanted sutures around the tips during deployment of the valve. The shaft member may be axially movable such that it can be initially retracted and then actuated just prior to valve deployment. The shaft member may have notches on its distal tip for capturing the attachment sutures, which are crossed over along the valve axis to ensure engagement by the notches. The attachment sutures may be strands or filaments, or may be wider bands of flexible biocompatible material. If bands are used, they desirably cover the commissure post tips to further help prevent suture looping thereover. The flexible lengths of material extend directly between commissures of the valve, or may extending radially inward from each commissure to a central upstanding member.
Owner:EDWARDS LIFESCIENCES CORP
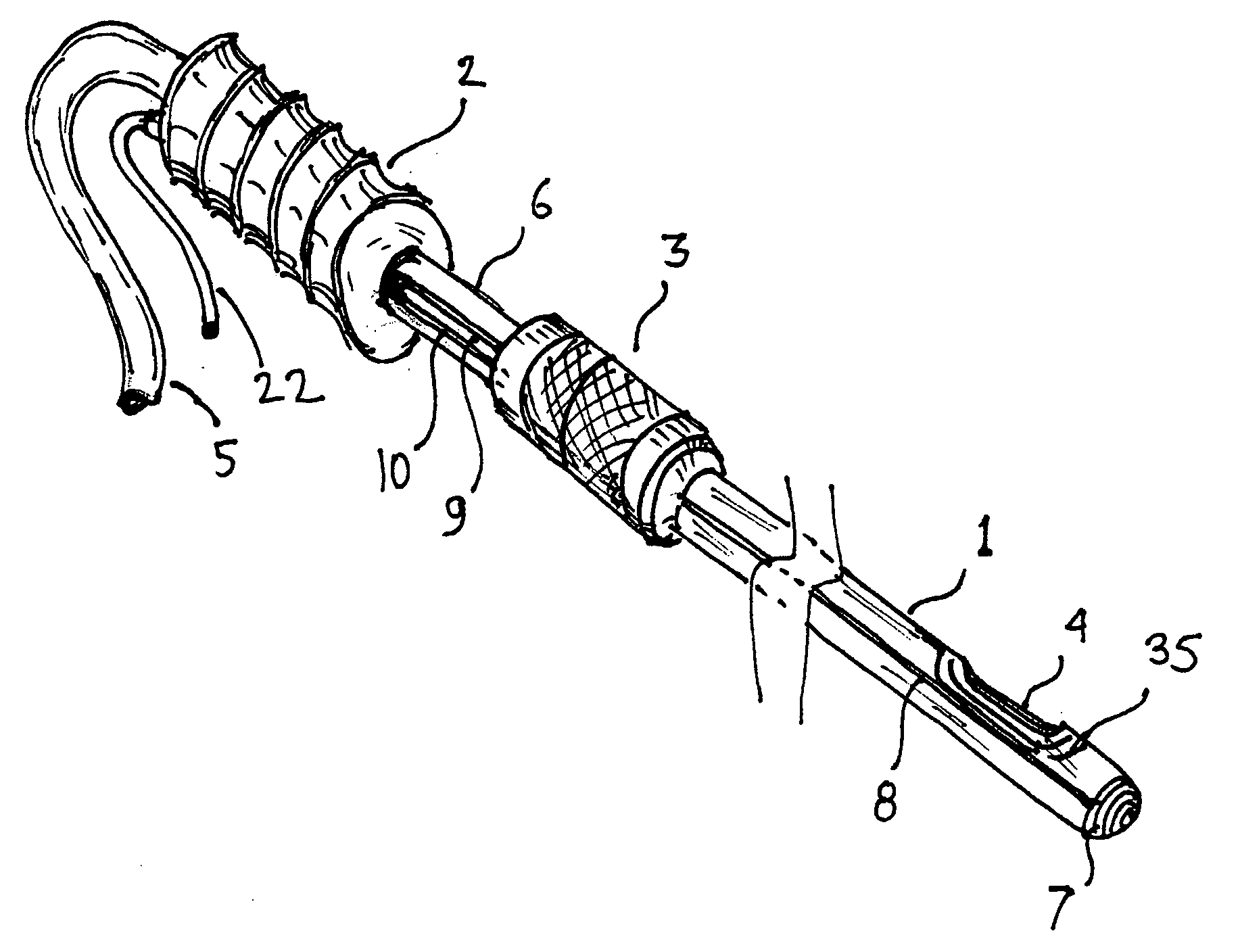
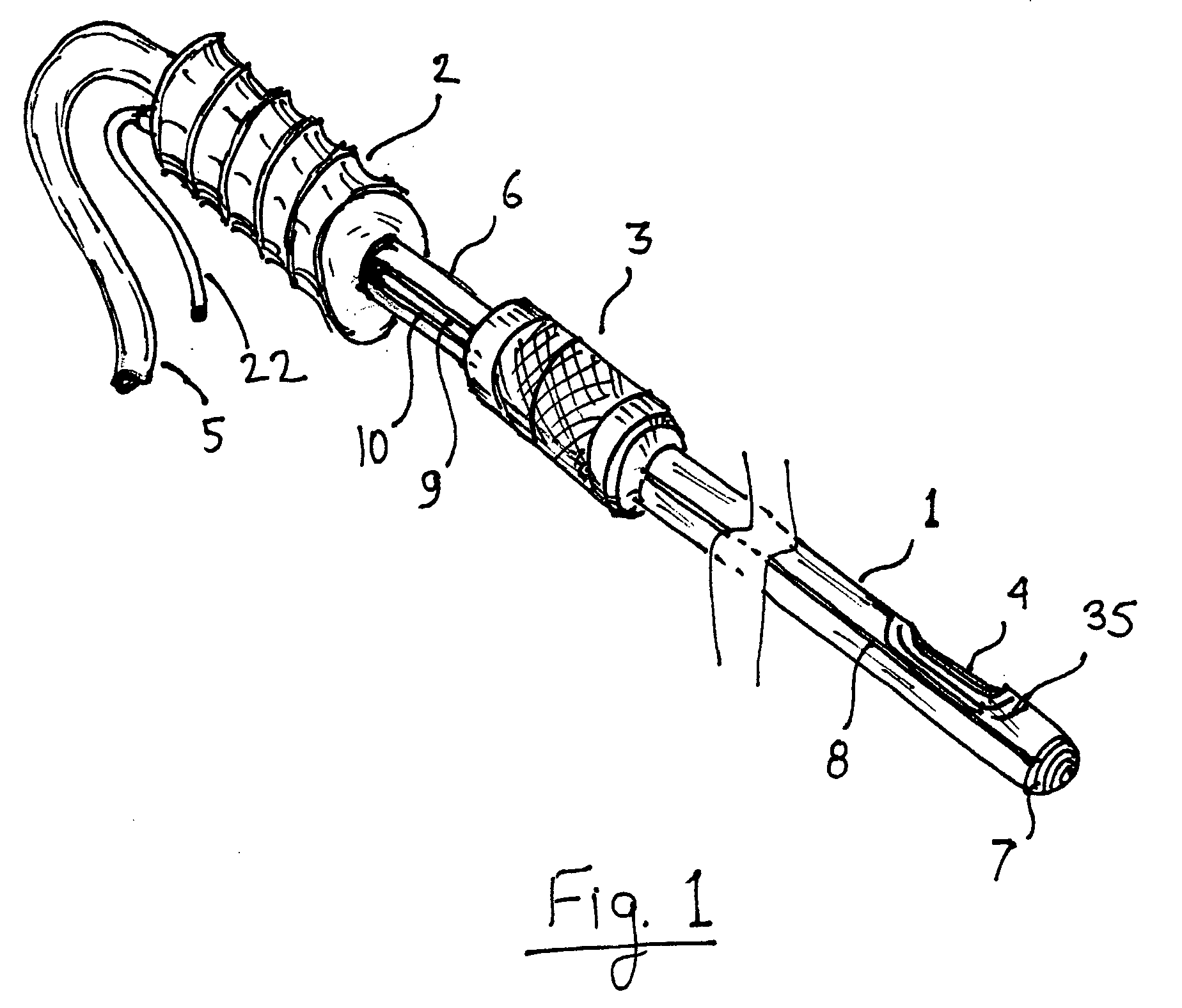
Liposuction system
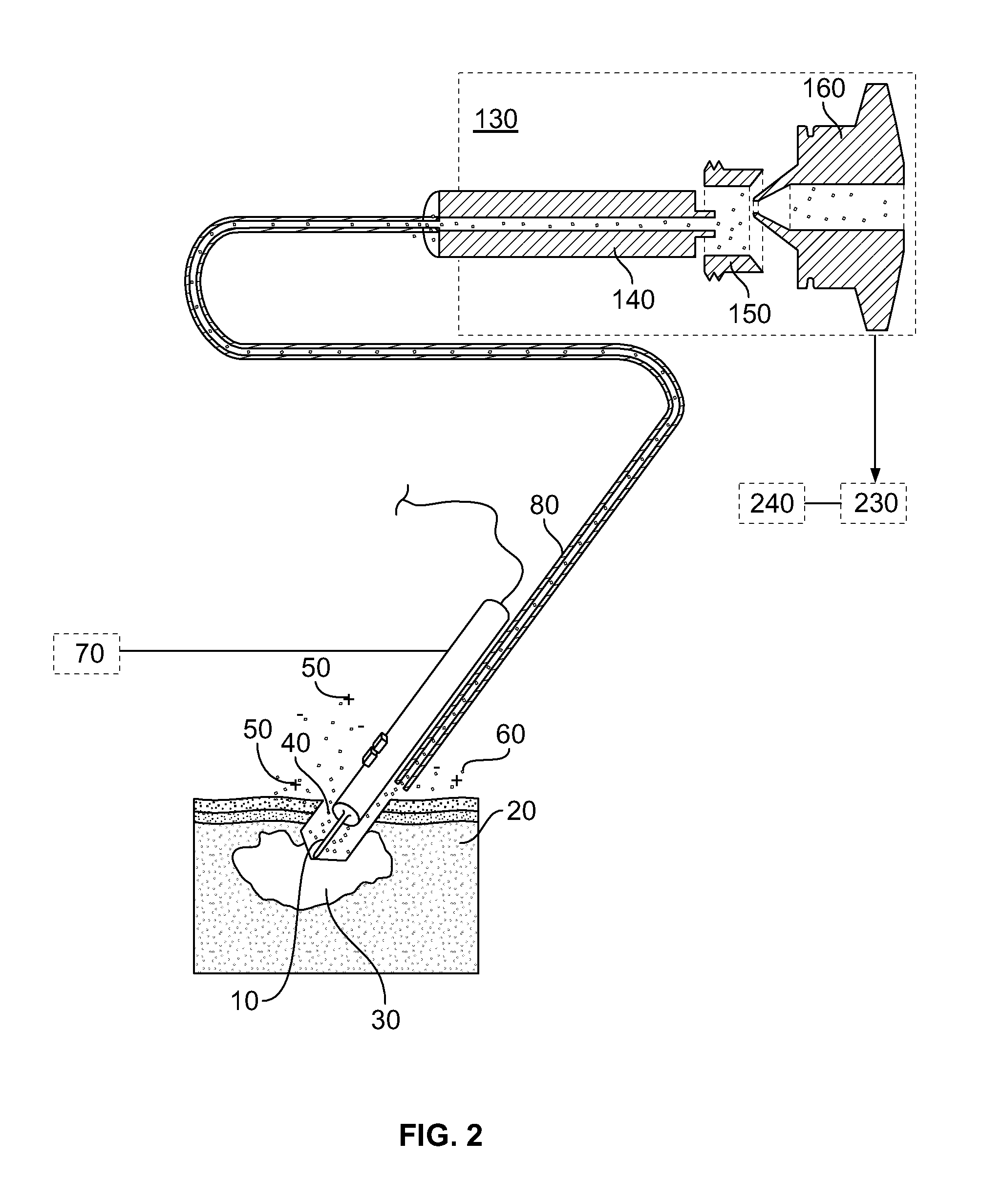
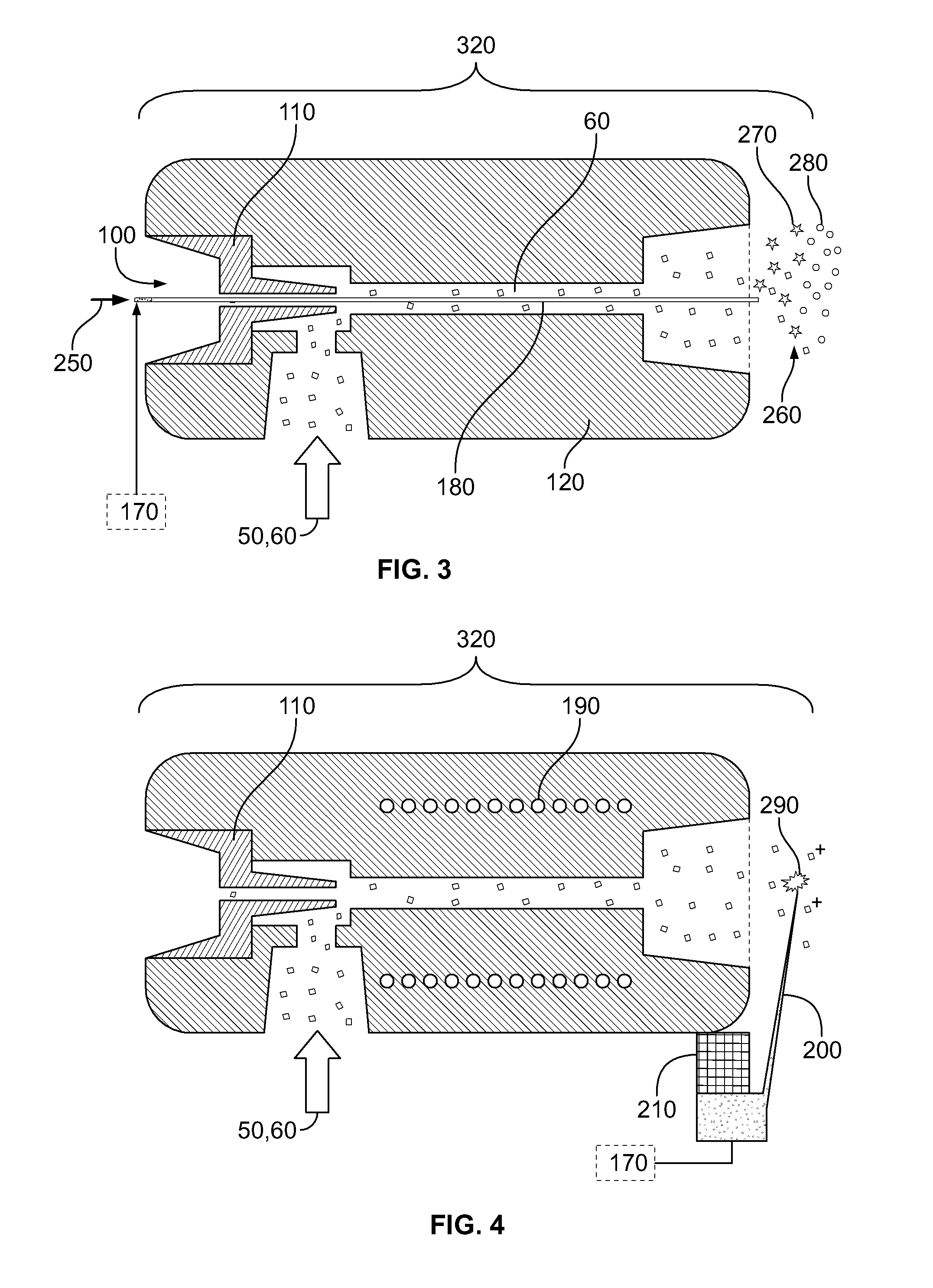
ActiveUS20090192441A1Minimize inertiaStopping actionElectrotherapyChiropractic devicesLiposuctionEngineering
A surgical tool such as a liposuction cannula is equipped with a sensor at the tool tip. The sensor continuously analyzes the type of tissue in contact with the tip based on the electrical properties of the tissue. When encountering a tissue type that should not be disturbed, the action of the surgical tool is stopped automatically. When used for liposuction, the cannula is mechanically decoupled from the handle when the wrong type of tissue is detected thus minimizing the inertia of the part that needs to be stopped. Besides electrical sensing, other sensors, such as mechanical or ultrasonic, can be used at the tip of the surgical tool or cannula to differentiate between tissue types
Owner:KARDIUM
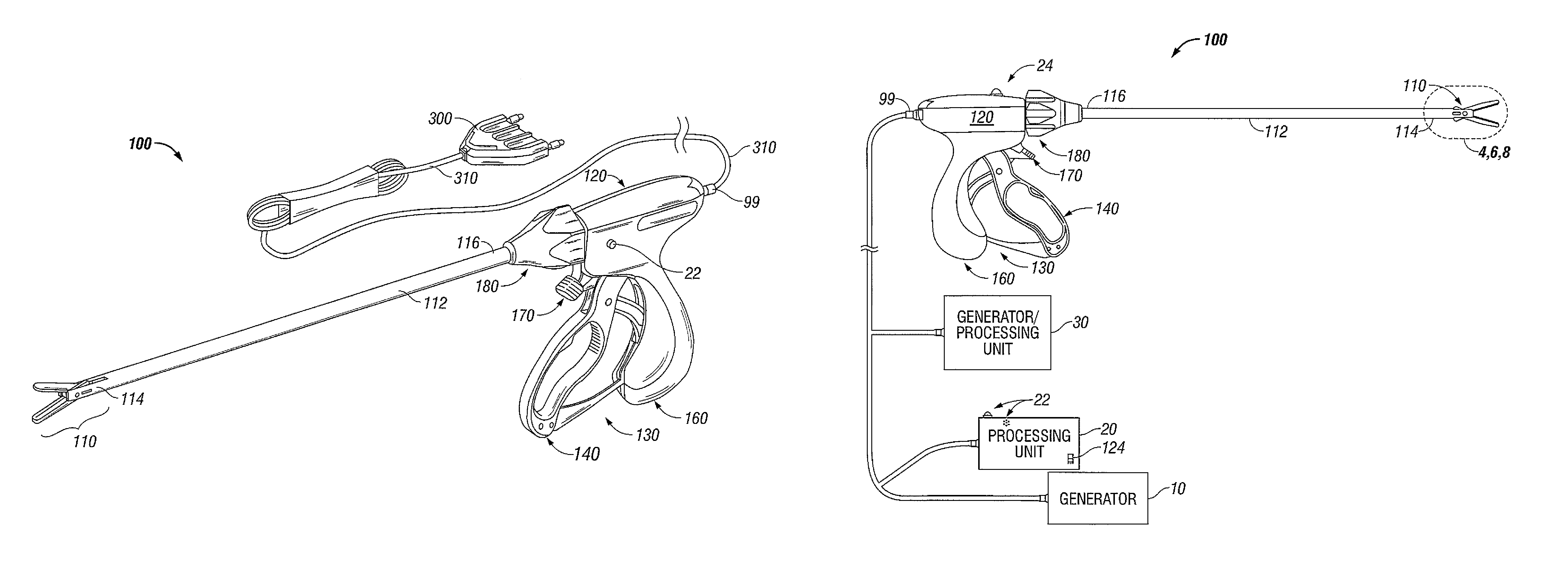
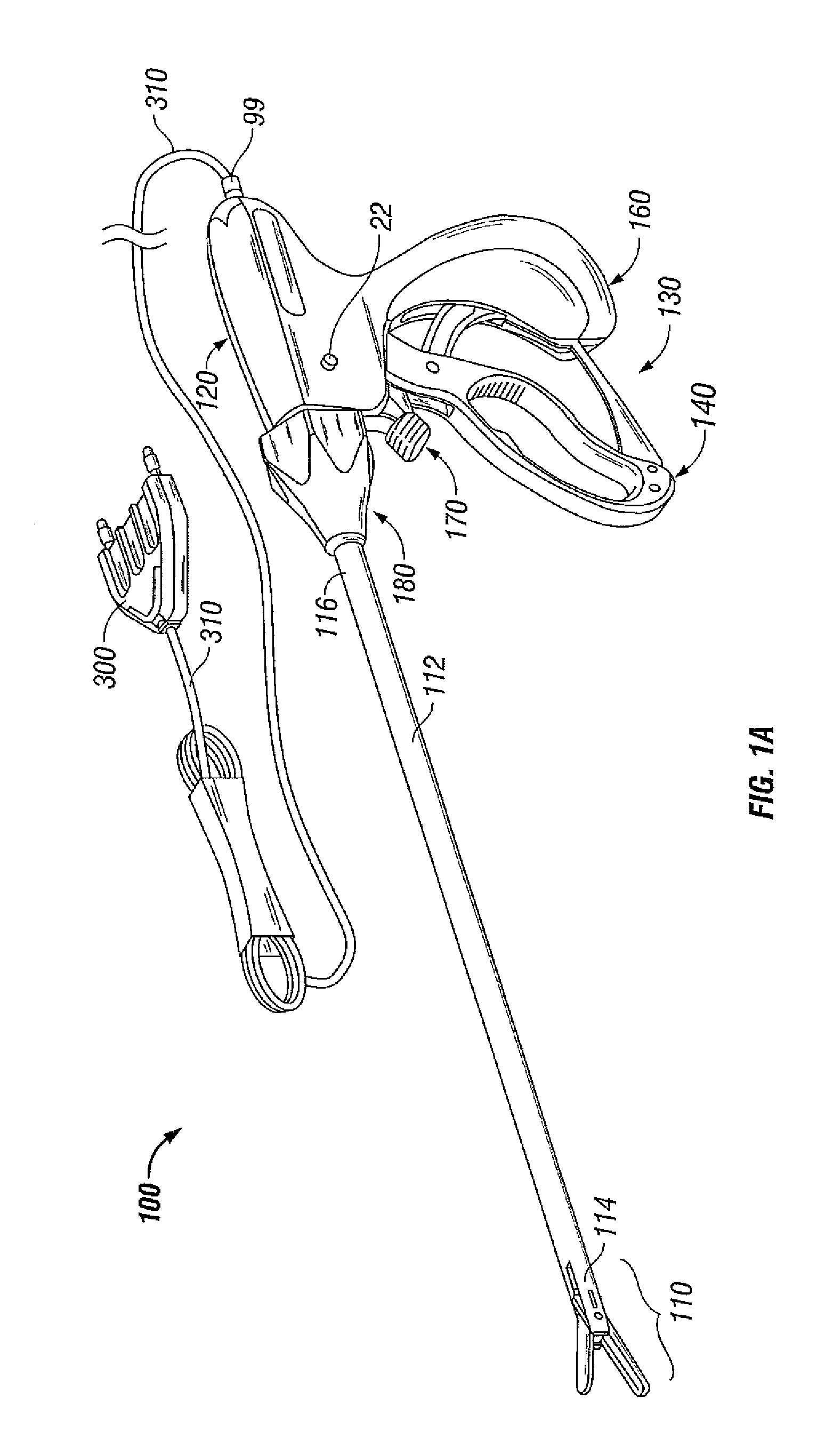
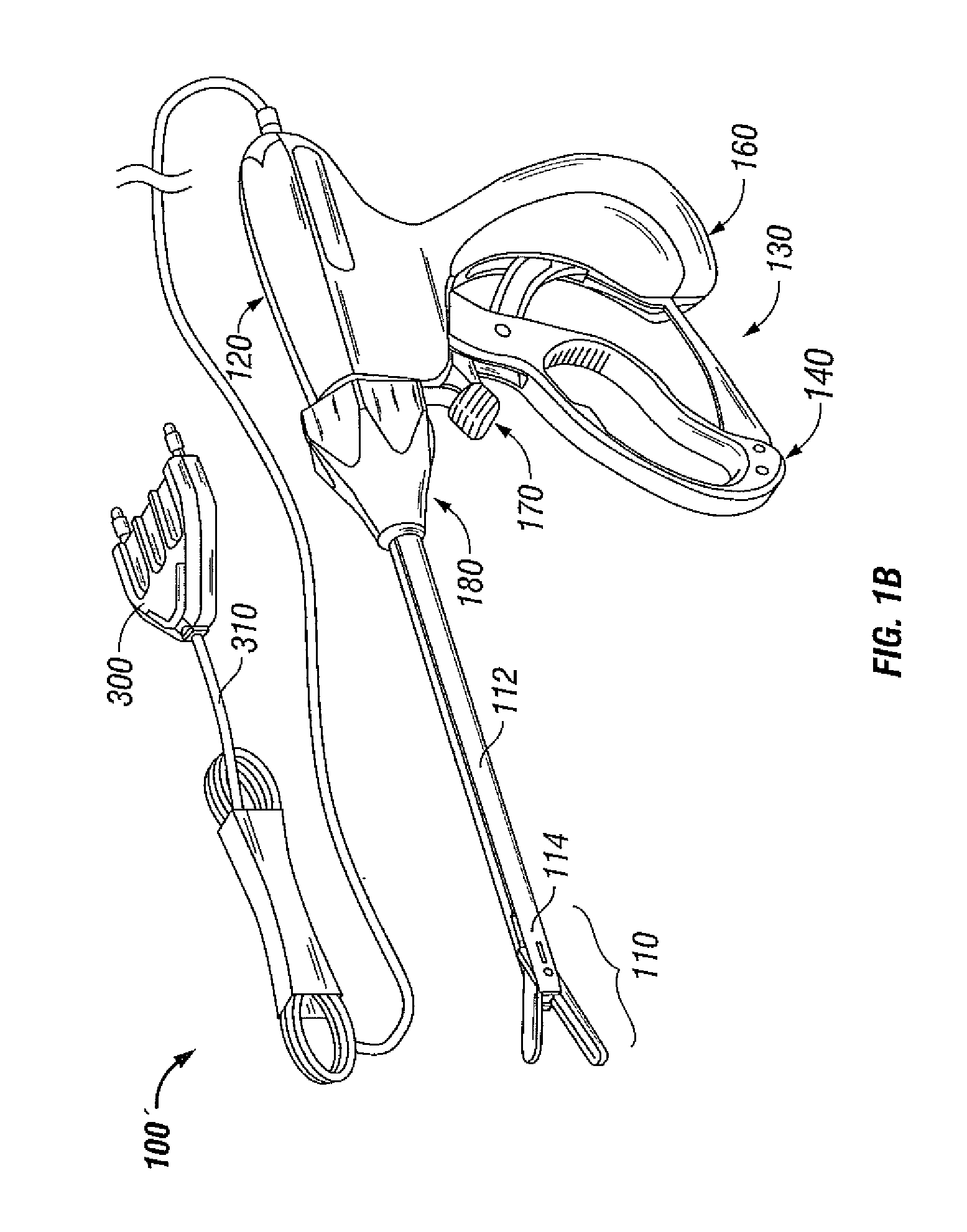
Endoscopic instrument for tissue identification
The present disclosure relates to various apparatus, systems and methods of identifying and treating tissue using at least one electrical property of tissue. Provided is a method for identifying and treating tissue, the method including providing a electrosurgical treatment device including an electrode assembly for measuring one or more electrical properties of a target tissue, the electrode assembly being mounted on a distal end thereof, measuring the one or more electrical characteristics of the target tissue, comparing the measured electrical property values of the target tissue against electrical property values of known tissue types, identifying a tissue type of the target tissue, adjusting an energy delivery configuration of the electrosurgical treatment device to the type of target tissue, and activating the electrosurgical treatment device to treat the target tissue.
Owner:TYCO HEALTHCARE GRP LP
Multipotent adult stem cells and methods for isolation
ActiveUS20050181502A1Improve the level ofLong telomereGenetically modified cellsDiagnosticsTissues typesEmbryo
Owner:ABT HOLDING COMPANY +1
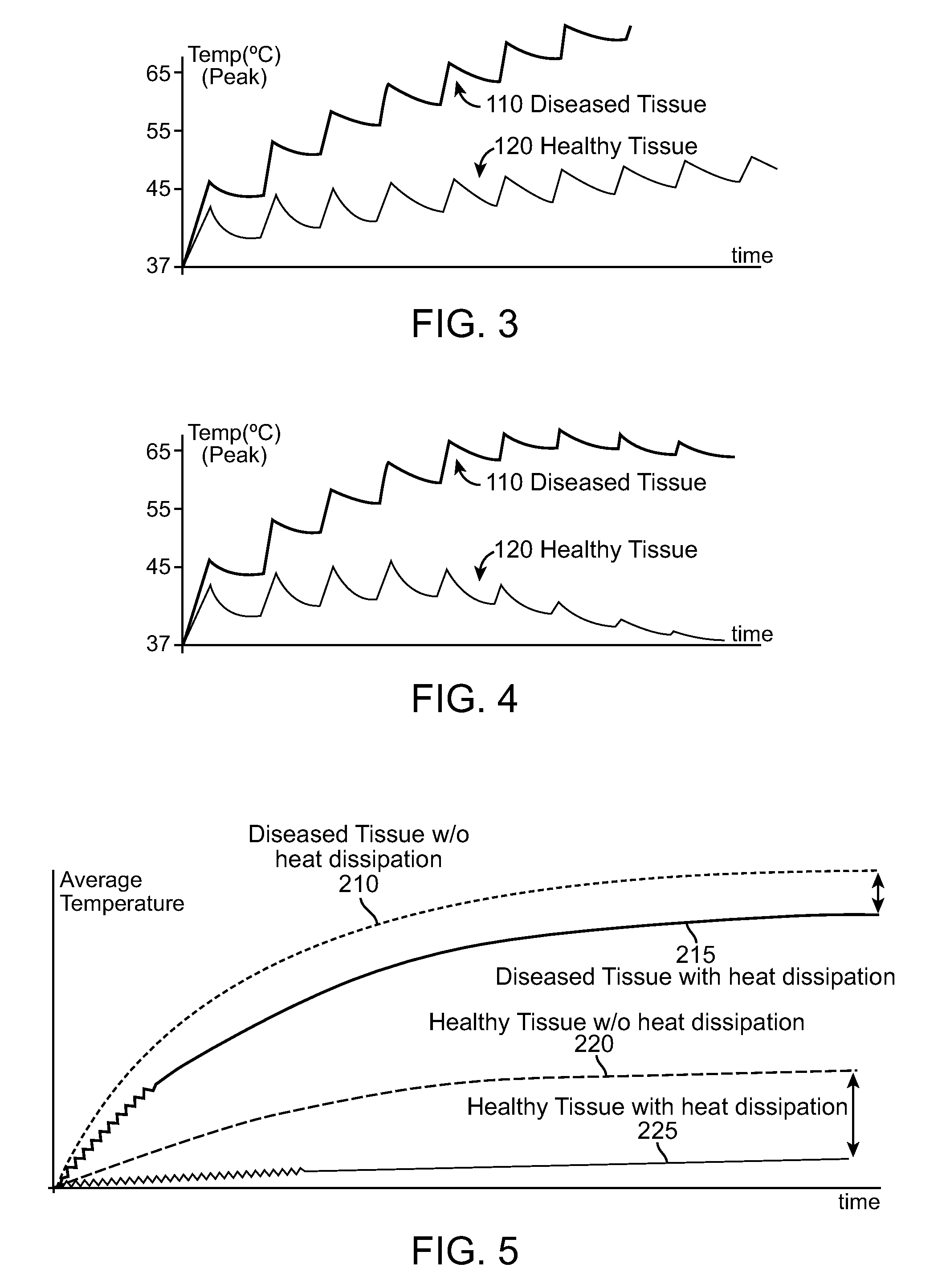
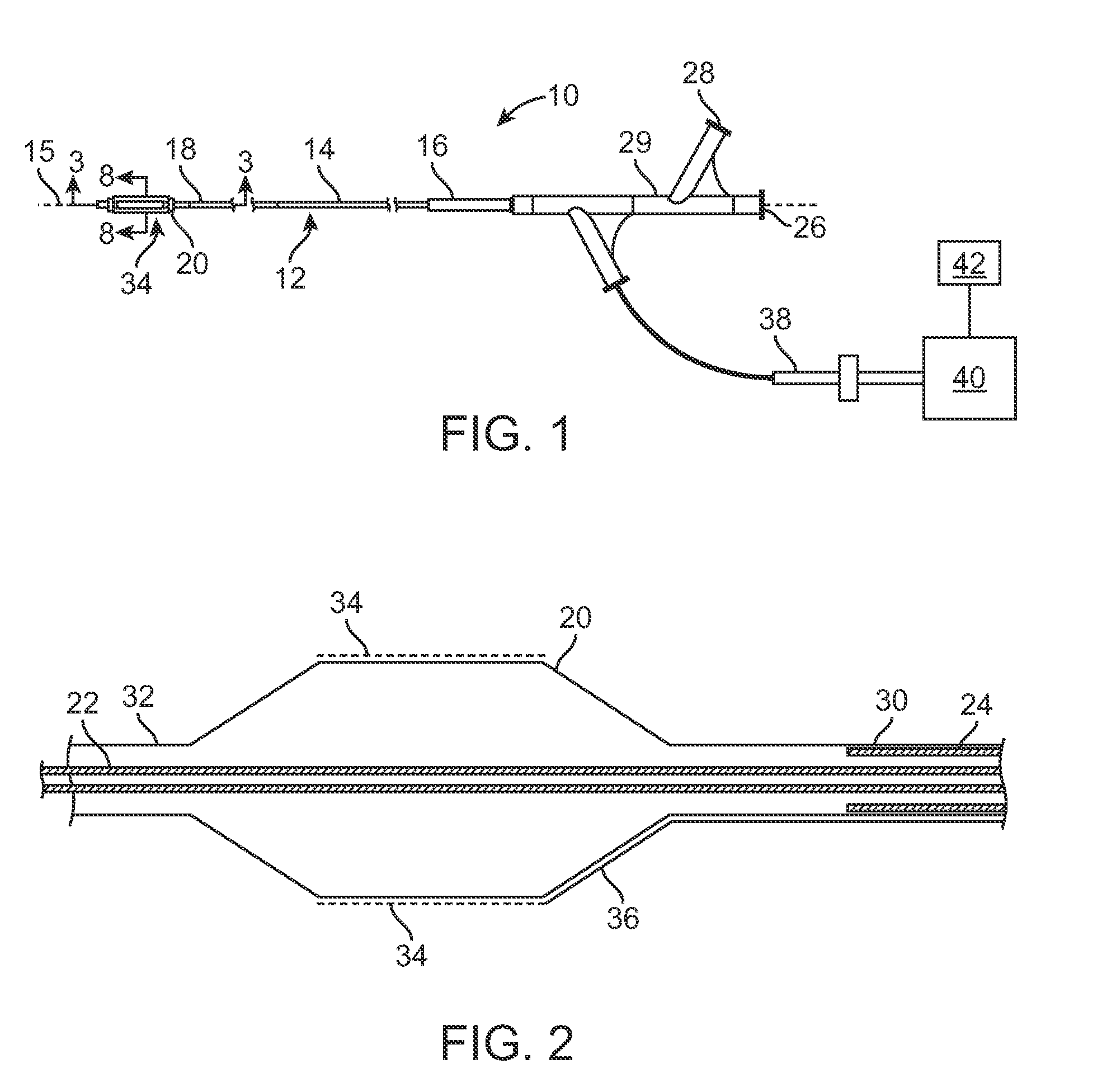
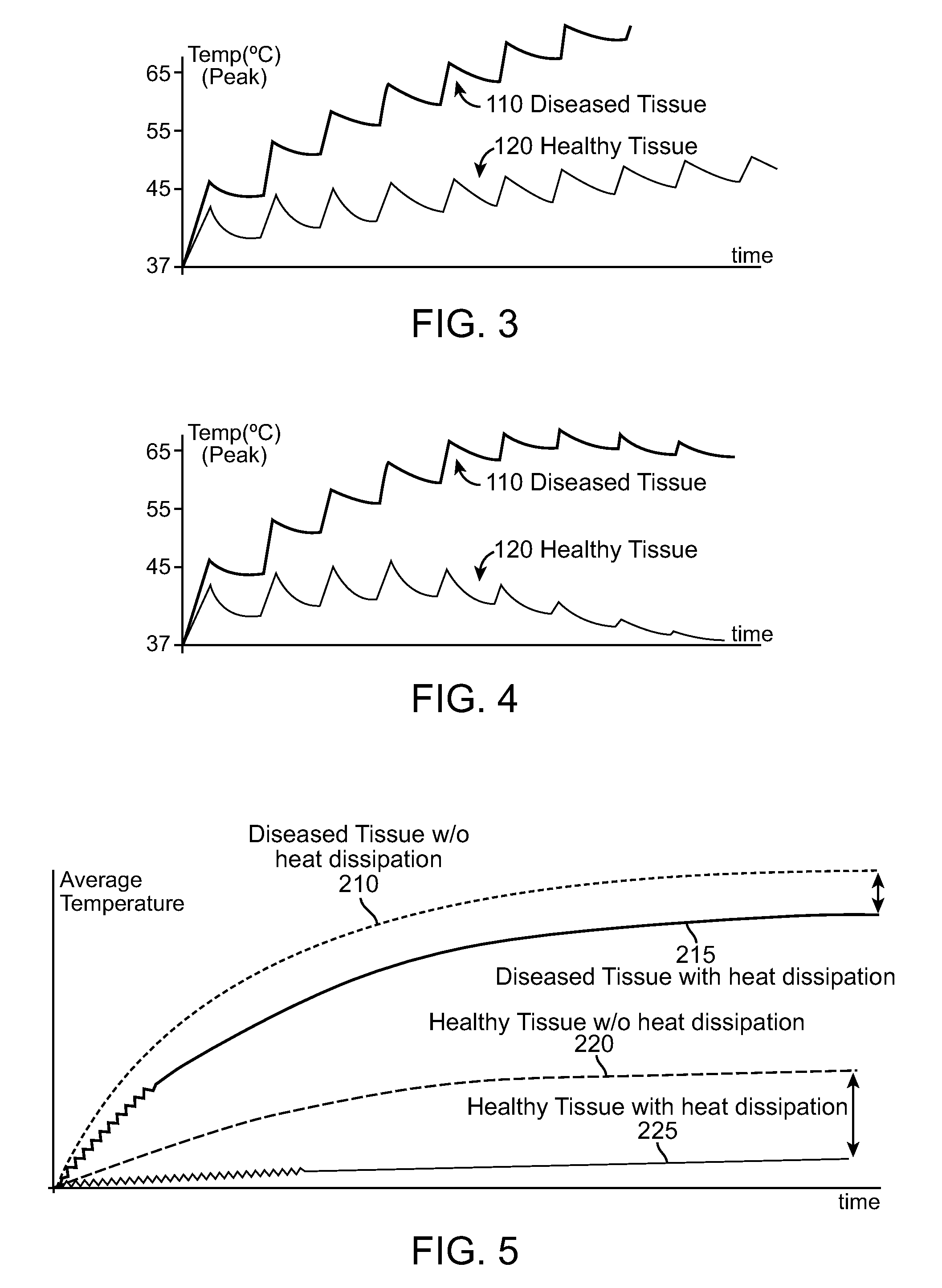
Selective accumulation of energy with or without knowledge of tissue topography
ActiveUS8401667B2Avoids significant thermal damageSignificant thermal damageUltrasound therapyChiropractic devicesMedicinePulse energy
Methods and systems for heating a body tissue region adjacent a body lumen using selective accumulation of energy without knowledge of tissue topography. Methods include positioning an energy delivery portion of a catheter within the lumen adjacent the body tissue region, determining a pulse characteristic in response to a thermal property of a first tissue type and applying pulsed energy with the characteristic to treat a second tissue type within the region by drawing heat from the first tissue at a rate that inhibits thermal damage to the first tissue while building-up heat in the second tissue. Systems include a catheter body having an energy delivery portion processor configured to control a pulse characteristic of pulsed energy to therapeutically treat the second tissue by drawing heat from the first tissue at a rate that inhibits thermal damage to the first tissue while building-up heat in the second tissue.
Owner:BOSTON SCI SCIMED INC
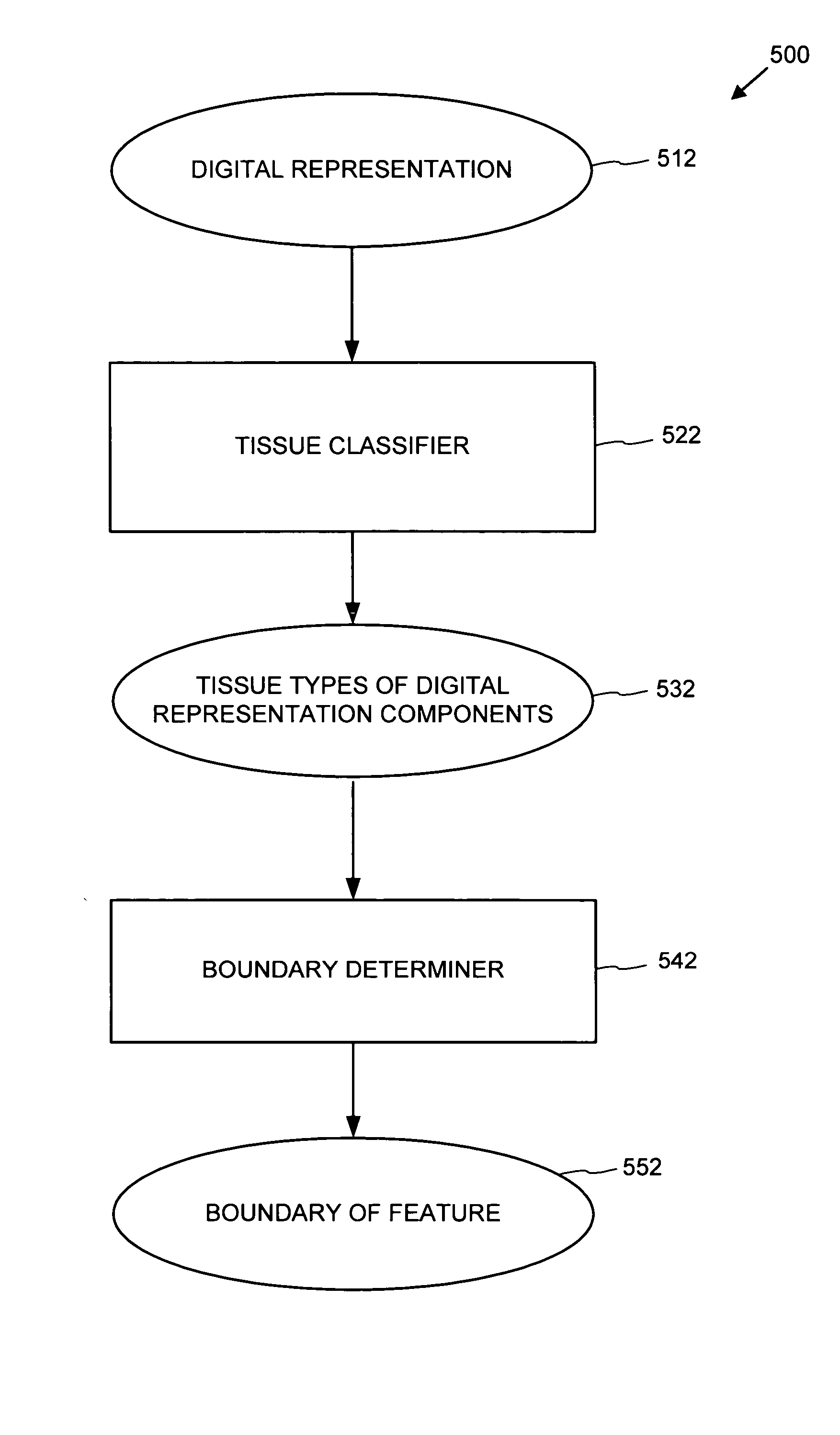
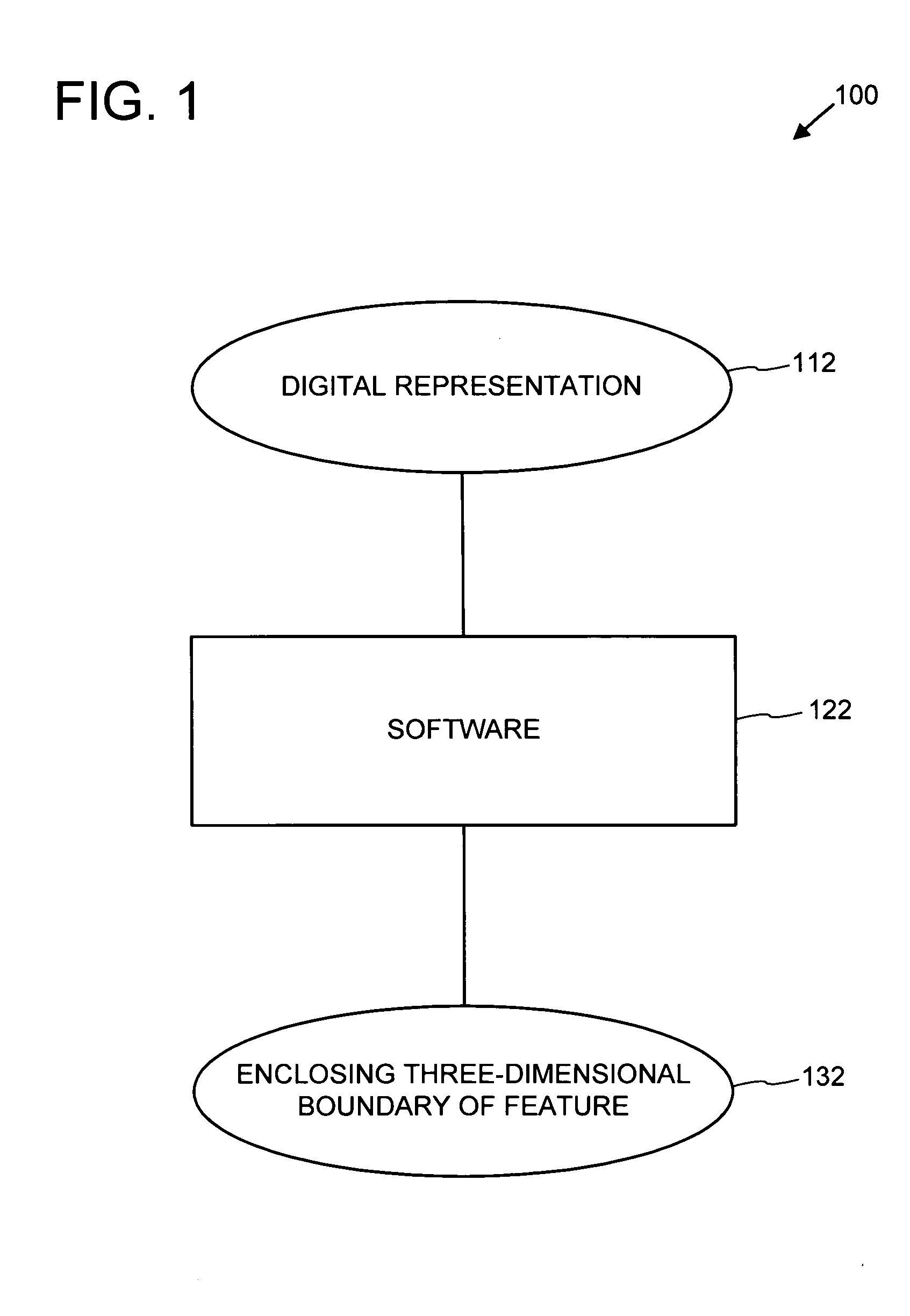
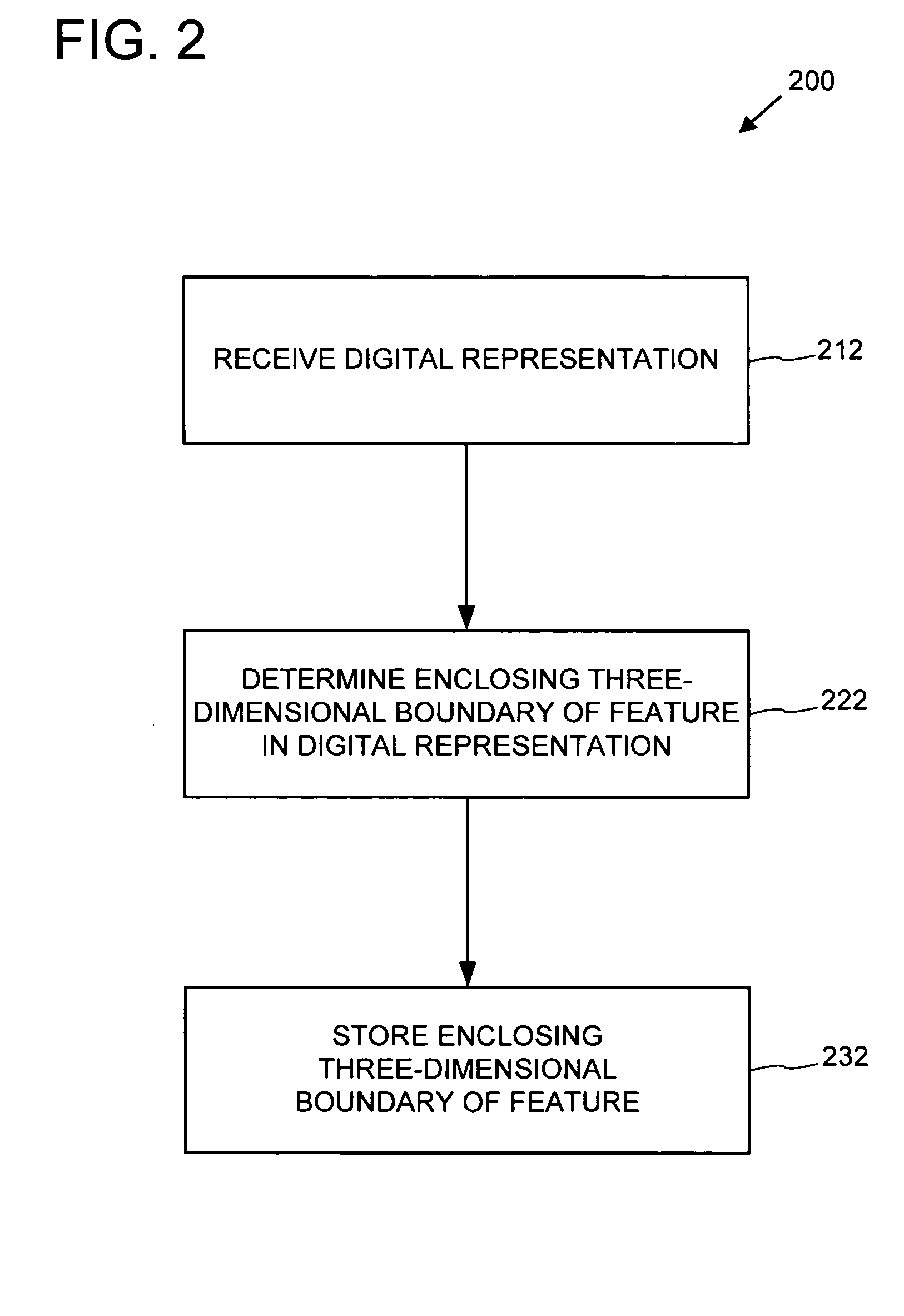
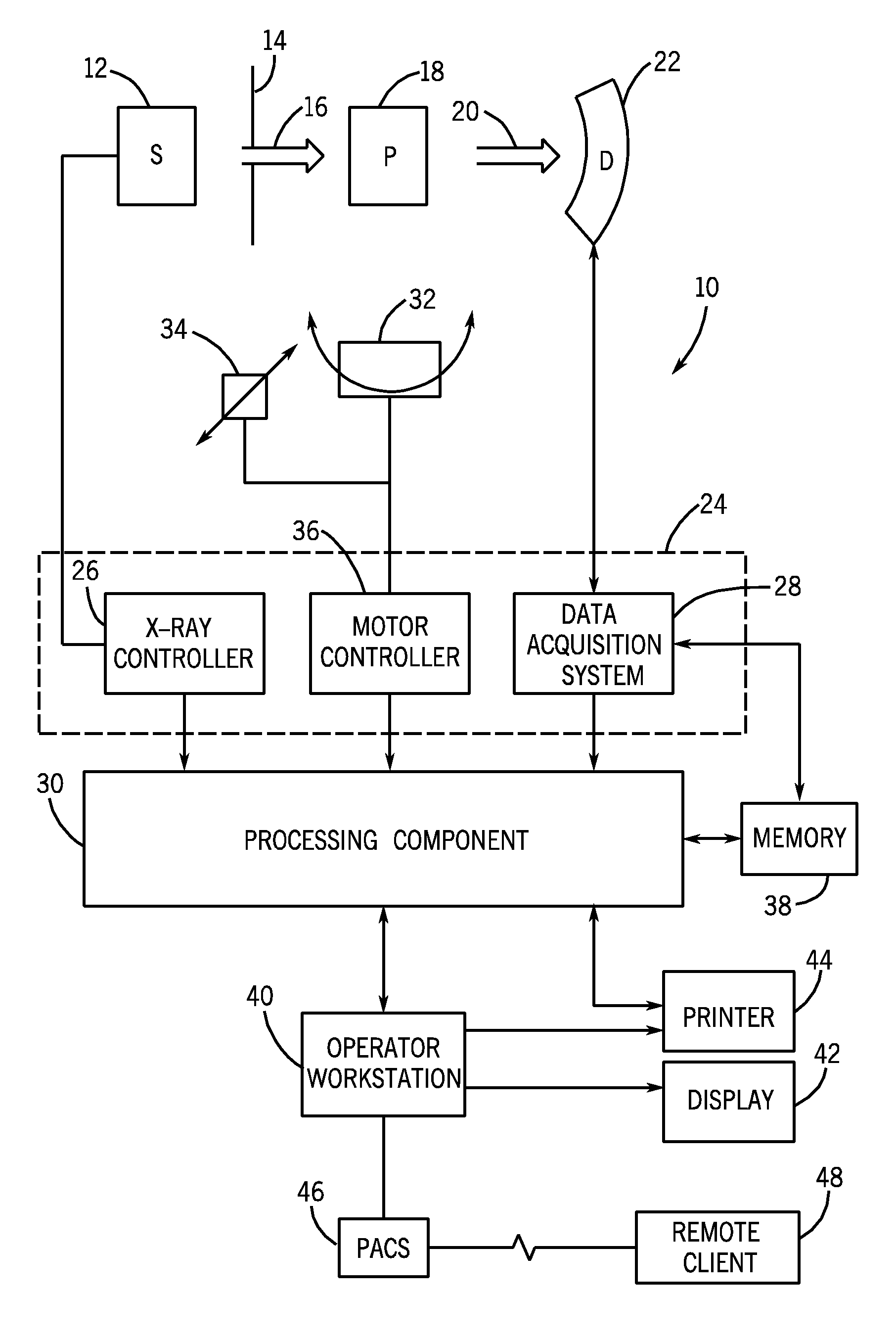
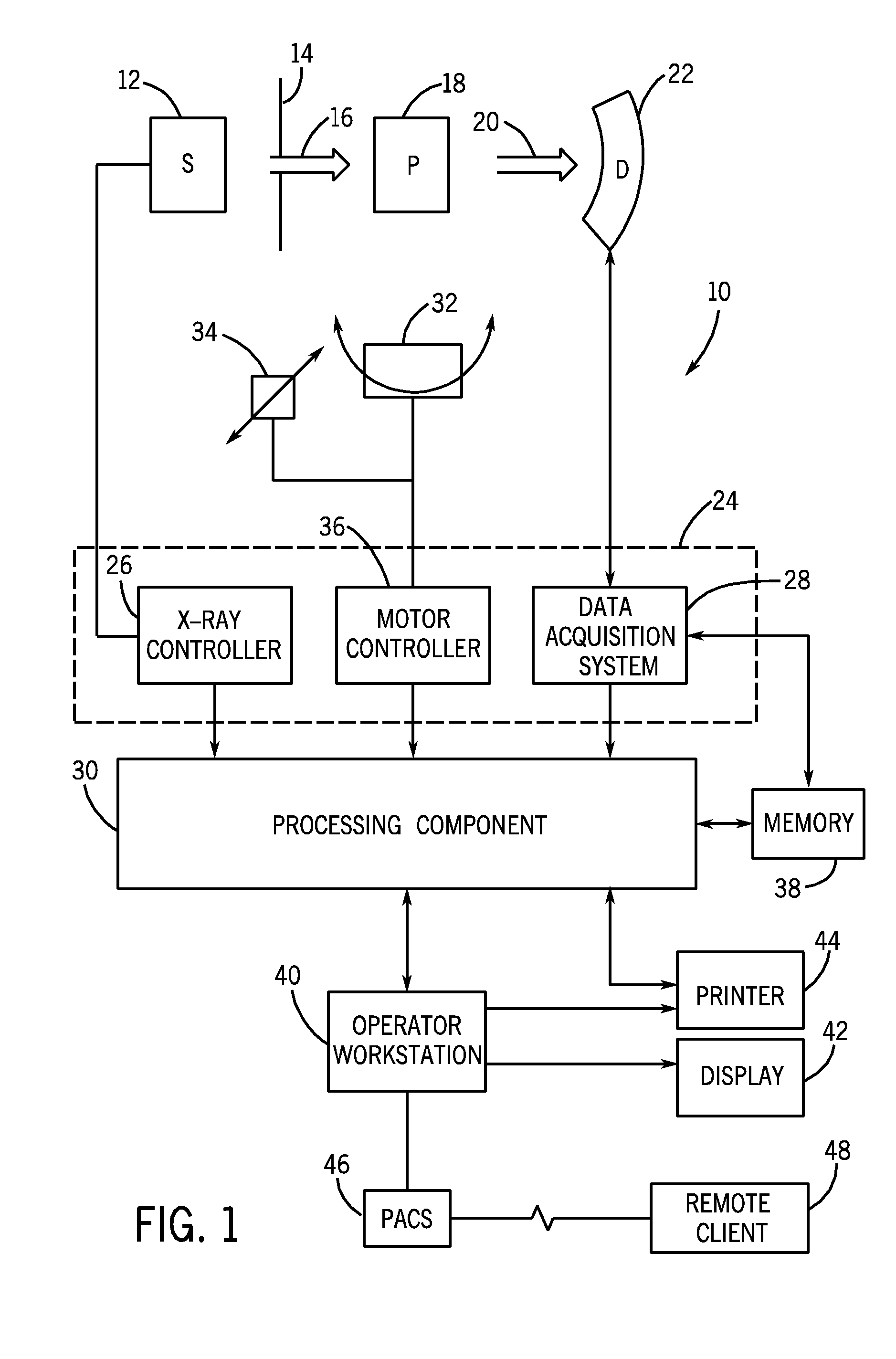
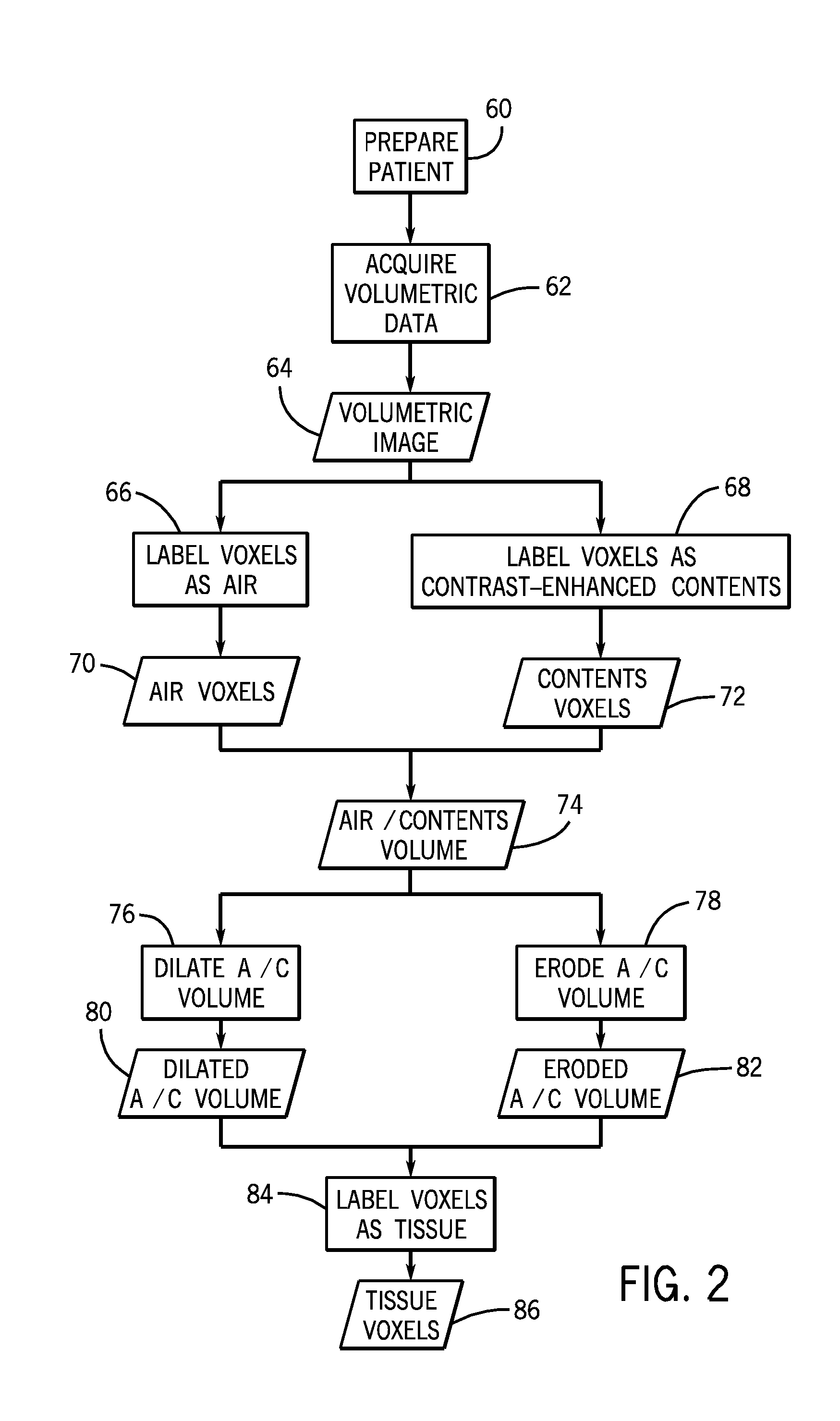
Determination of feature boundaries in a digital representation of an anatomical structure
A virtual anatomical structure can be analyzed to determine enclosing three-dimensional boundaries of features therein. Various techniques can be used to determine tissue types in the virtual anatomical structure. For example, tissue types can be determined via an iso-boundary between lumen and air in the virtual anatomical structure and a fuzzy clustering approach. Based on the tissue type determination, a deformable model approach can be used to determine an enclosing three-dimensional boundary of a feature in the virtual anatomical structure. The enclosing three-dimensional boundary can be used to determine characteristics of the feature and classify it as of interest or not of interest.
Owner:UNITED STATES OF AMERICA
Tissue classification in medical images
Owner:GENERAL ELECTRIC CO
Displaying image data using automatic presets
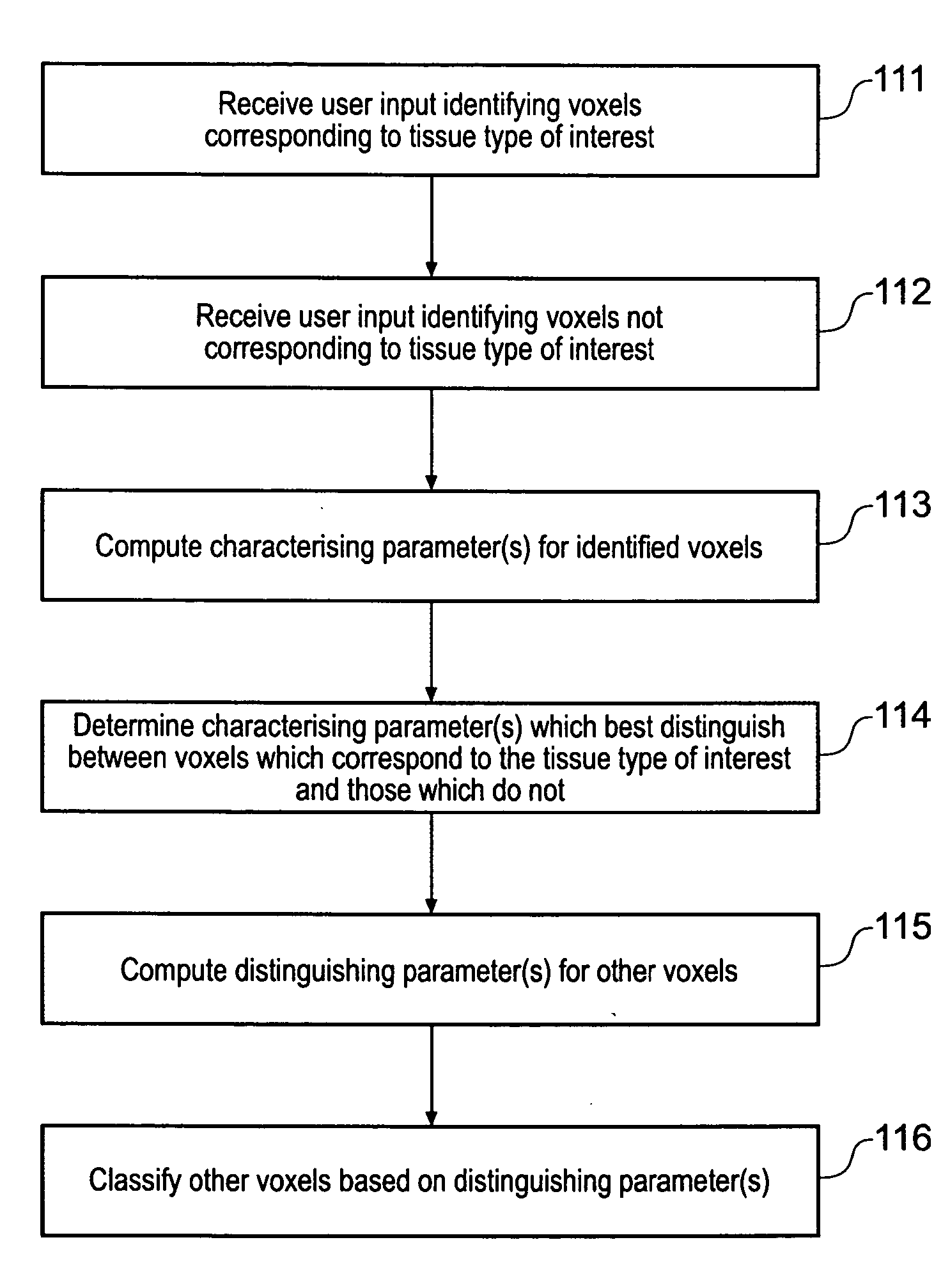
InactiveUS20050017972A1Easy and intuitiveAccurate classificationUltrasonic/sonic/infrasonic diagnosticsImage enhancementPattern recognitionVoxel
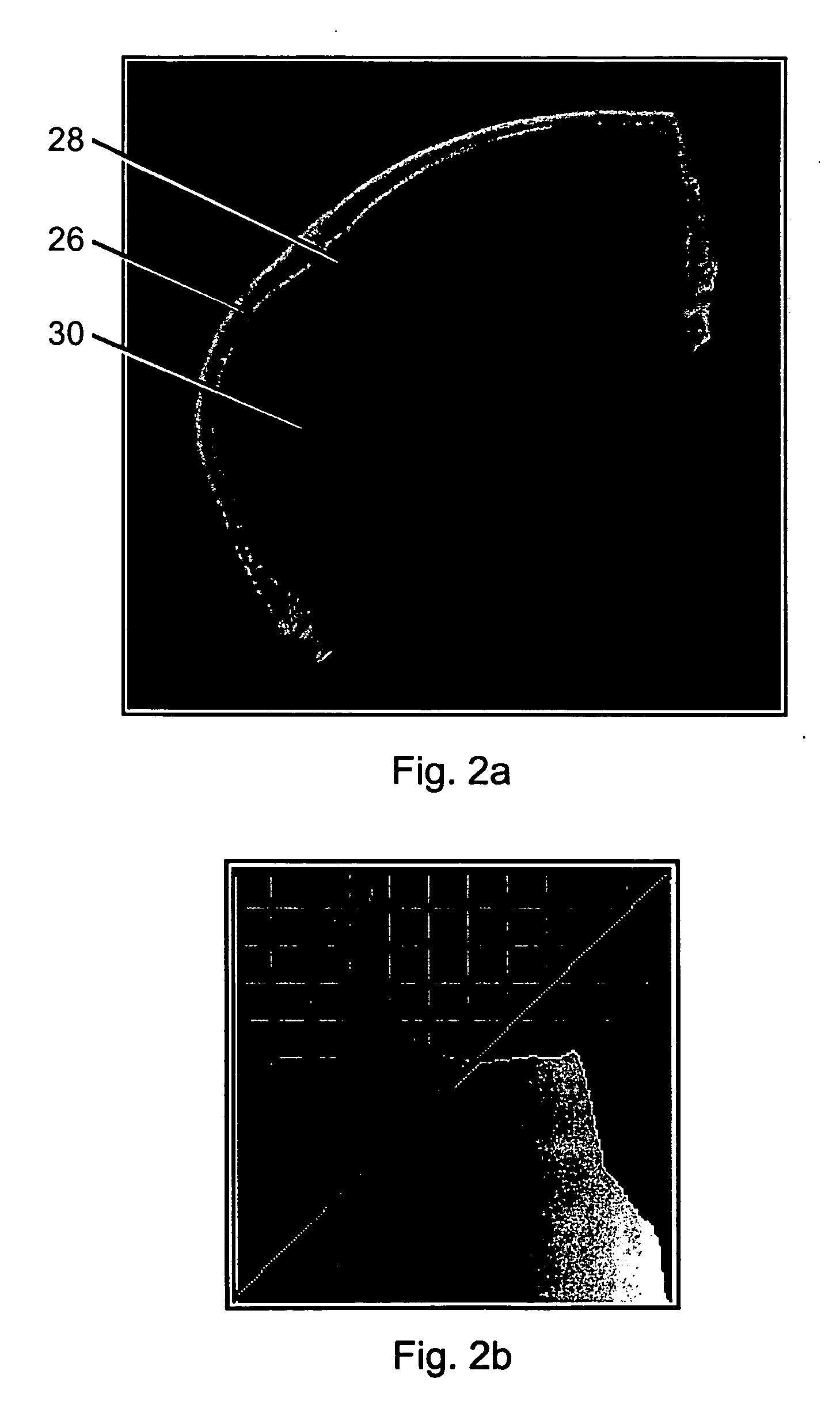
A computer automated method that applies supervised pattern recognition to classify whether voxels in a medical image data set correspond to a tissue type of interest is described. The method comprises a user identifying examples of voxels which correspond to the tissue type of interest and examples of voxels which do not. Characterizing parameters, such as voxel value, local averages and local standard deviations of voxel value are then computed for the identified example voxels. From these characterizing parameters, one or more distinguishing parameters are identified. The distinguishing parameter are those parameters having values which depend on whether or not the voxel with which they are associated corresponds to the tissue type of interest. The distinguishing parameters are then computed for other voxels in the medical image data set, and these voxels are classified on the basis of the value of their distinguishing parameters. The approach allows tissue types which differ only slightly to be distinguished according to a user's wishes.
Owner:VOXAR
Heart valve holder that resist suture looping
An improved holder, system and method for implanting a tissue-type prosthetic mitral heart valve that prevents suture looping and may also constrict the commissure posts of the valve. The holder may include two relatively movable plates, one of which attaches to the valve sewing on the inflow end of the valve ring and the other which attaches via sutures or similar expedient to the valve commissures on the outflow end. Separation of the plates places the sutures in tension and constricts the commissures. The sutures may be strands or filaments, or may be wider bands of flexible biocompatible material. If bands are used, they desirably cover the commissure post tips to further help prevent suture looping thereover. The flexible lengths of material extend directly between commissures of the valve, or may extending radially inward from each commissure to a central upstanding member. Desirably, a slide is created by the flexible lengths of material adjacent each commissure post, for example by crossing over suture filaments at or radially inward from the commissure posts. If an upstanding member is used, the lengths of suture extend axially beyond the commissure post tips to create a tent that wards off sutures that otherwise might loop around the tips during advancement of the valve along an array of pre-implanted sutures.
Owner:EDWARDS LIFESCIENCES CORP
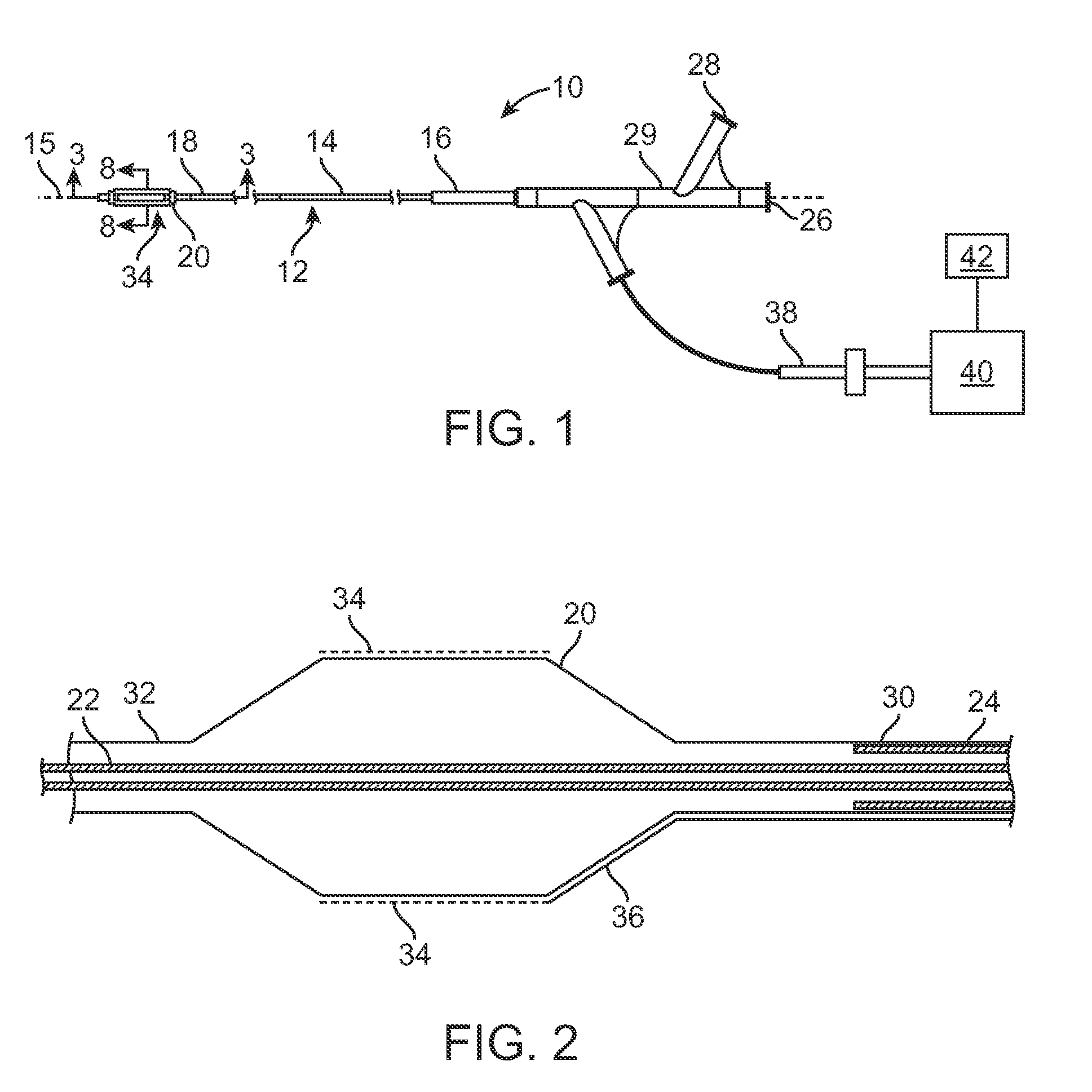
Selective Accumulation of Energy With or Without Knowledge of Tissue Topography
ActiveUS20100125268A1Avoids significant thermal damageSignificant thermal damageUltrasound therapyChiropractic devicesPulse energyPulse characteristics
Methods and systems for heating a body tissue region adjacent a body lumen with diseased and healthy portions using selective accumulation of energy in the artery tissue with or without knowledge of tissue topography. The method includes positioning an energy delivery portion of a catheter body within the lumen adjacent the body tissue region to be heated, determining a pulse characteristic in response to a thermal property of a first tissue type and applying pulsed energy with the pulse characteristic from the energy delivery portion so as to therapeutically treat the second tissue type within the body tissue region by drawing heat from the first tissue type at a rate that avoids significant thermal damage to the first tissue type while building-up heat in the second tissue type. The system includes an elongate flexible catheter body having a proximal end and a distal end with an axis therebetween, an energy delivery portion proximate the distal end, an energy source coupled to the energy delivery portion and a processor coupled to the energy source, the processor configured to control a pulse characteristic of pulsed energy transmitted from the energy source to the energy delivery portion so as to therapeutically treat the second tissue type within the body tissue region by drawing heat from the first tissue type at a rate that avoids significant thermal damage to the first tissue type while building-up heat in the second tissue type.
Owner:BOSTON SCI SCIMED INC
Active Electrode, Bio-Impedance Based, Tissue Discrimination System and Methods of Use
InactiveUS20110082383A1Accurate identificationDiagnostic recording/measuringSensorsElectricityTissues types
Owner:NERVONIX INC
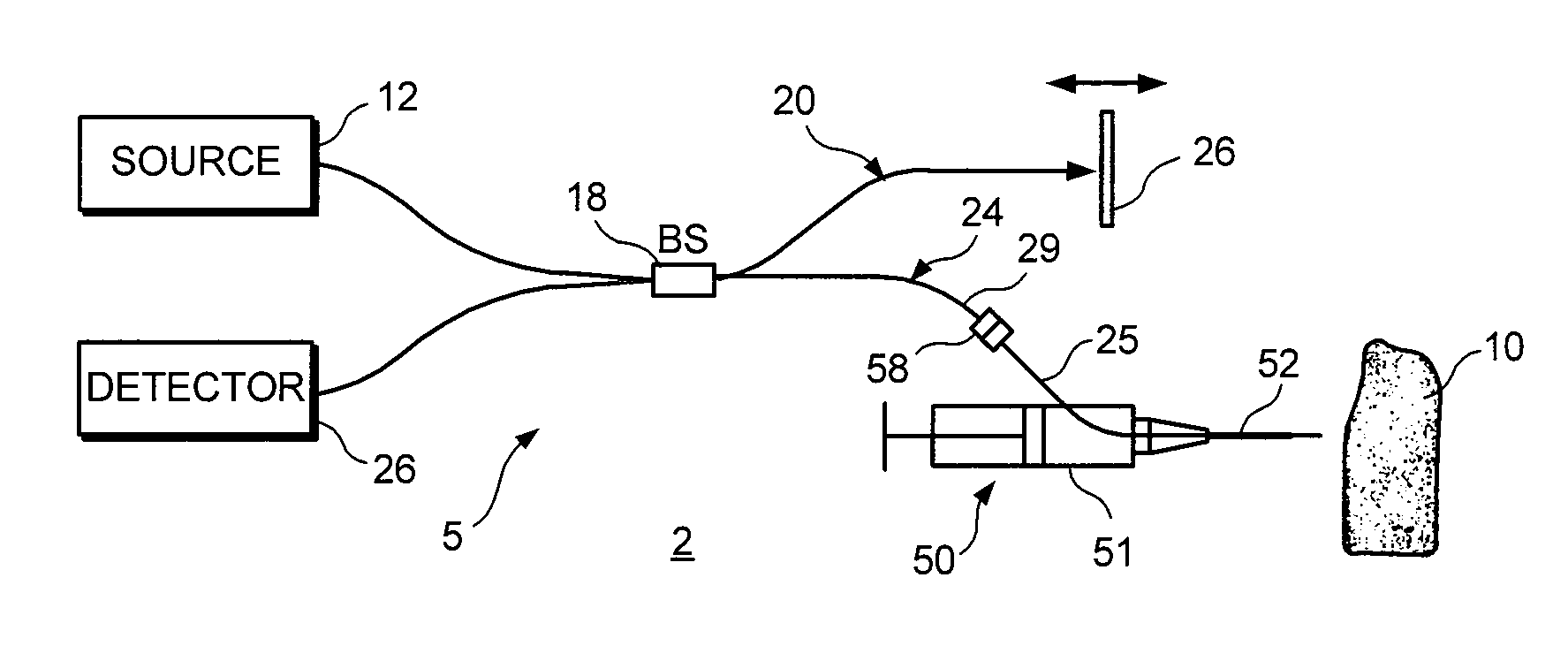
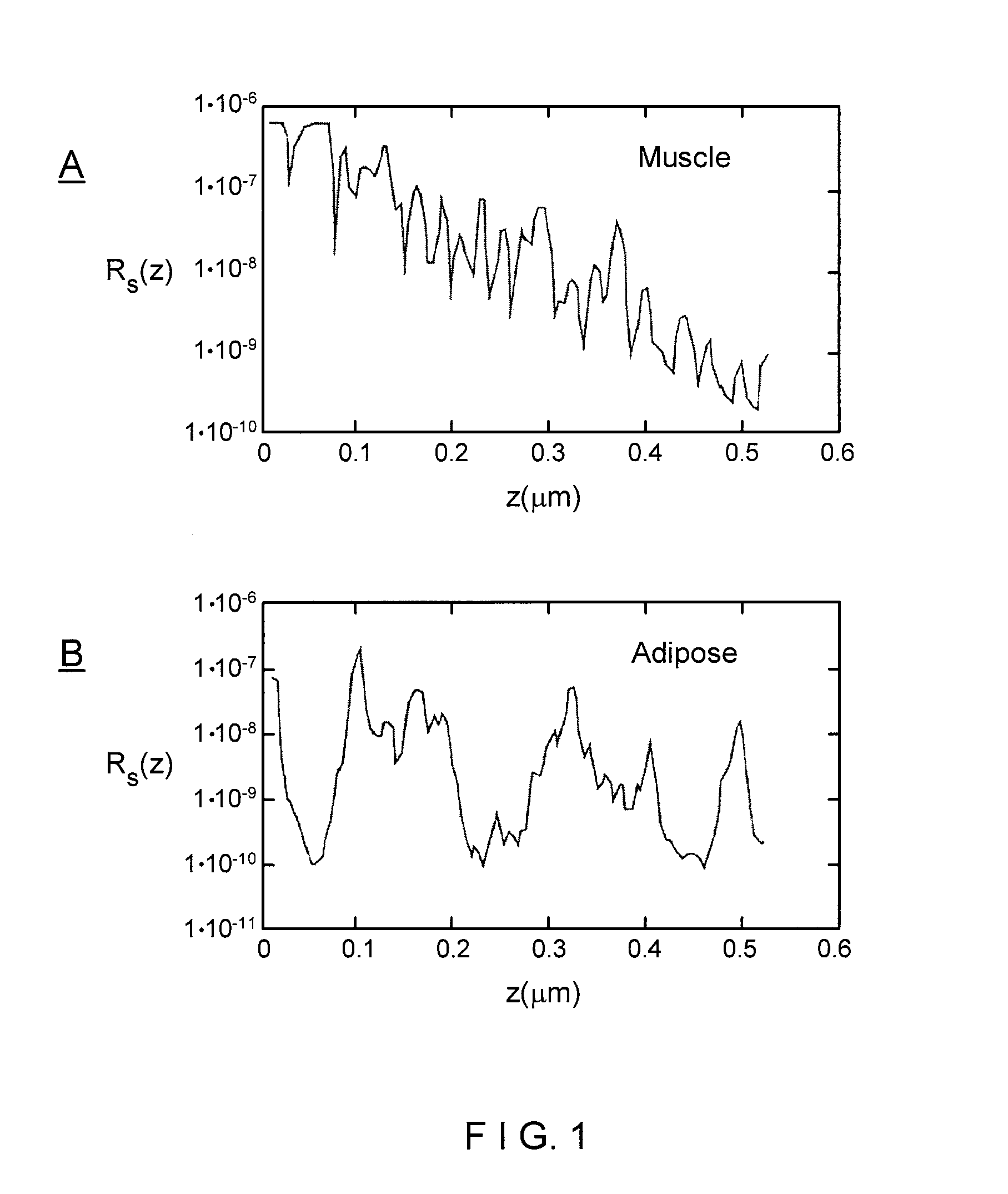
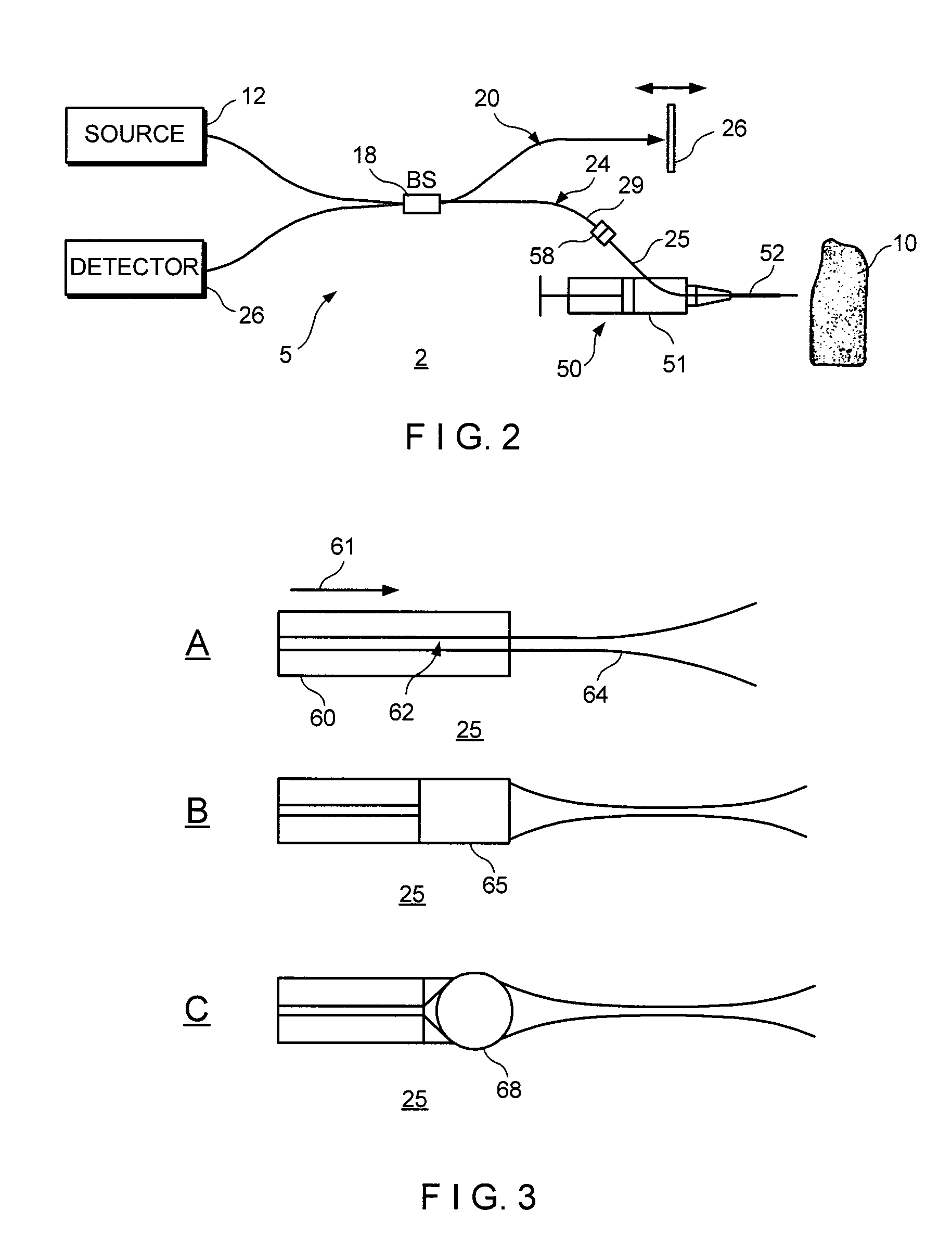
System and method for identifying tissue using low-coherence interferometry
ActiveUS7761139B2Image degradationLower requirementCatheterDiagnostic recording/measuringFiberBiopsy procedure
Owner:THE GENERAL HOSPITAL CORP
System and method for identification of biological tissues
ActiveUS20120156712A1Easy to detectOverall light weightBioreactor/fermenter combinationsBiological substance pretreatmentsCombined useTissue sample
The present invention provides for a system, method, and device for analyzing, localizing and / or identifying tissue types. The method includes analyzing, localizing and / or identifying one or more tissue samples, characterized in that the method comprises: (a) generating gaseous tissue particles from a site in the one or more tissue samples, (b) transporting the gaseous tissue particles from the site to an analyser, (c) using the analyser for generating tissue-related data based on the gaseous tissue particles, and (d) analyzing, localizing and / or identifying the one or more tissue samples based on the tissue-related data. The invention can either be used in close conjunction with a surgical procedure, when one or more surgical tools are an integrated part of ionization, or as a separate mass spectrometric probe for the analysis of one or more tissue parts.
Owner:MICROMASS UK LTD +1
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com