Patents
Literature
211 results about "Left ventricular Stroke volume" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
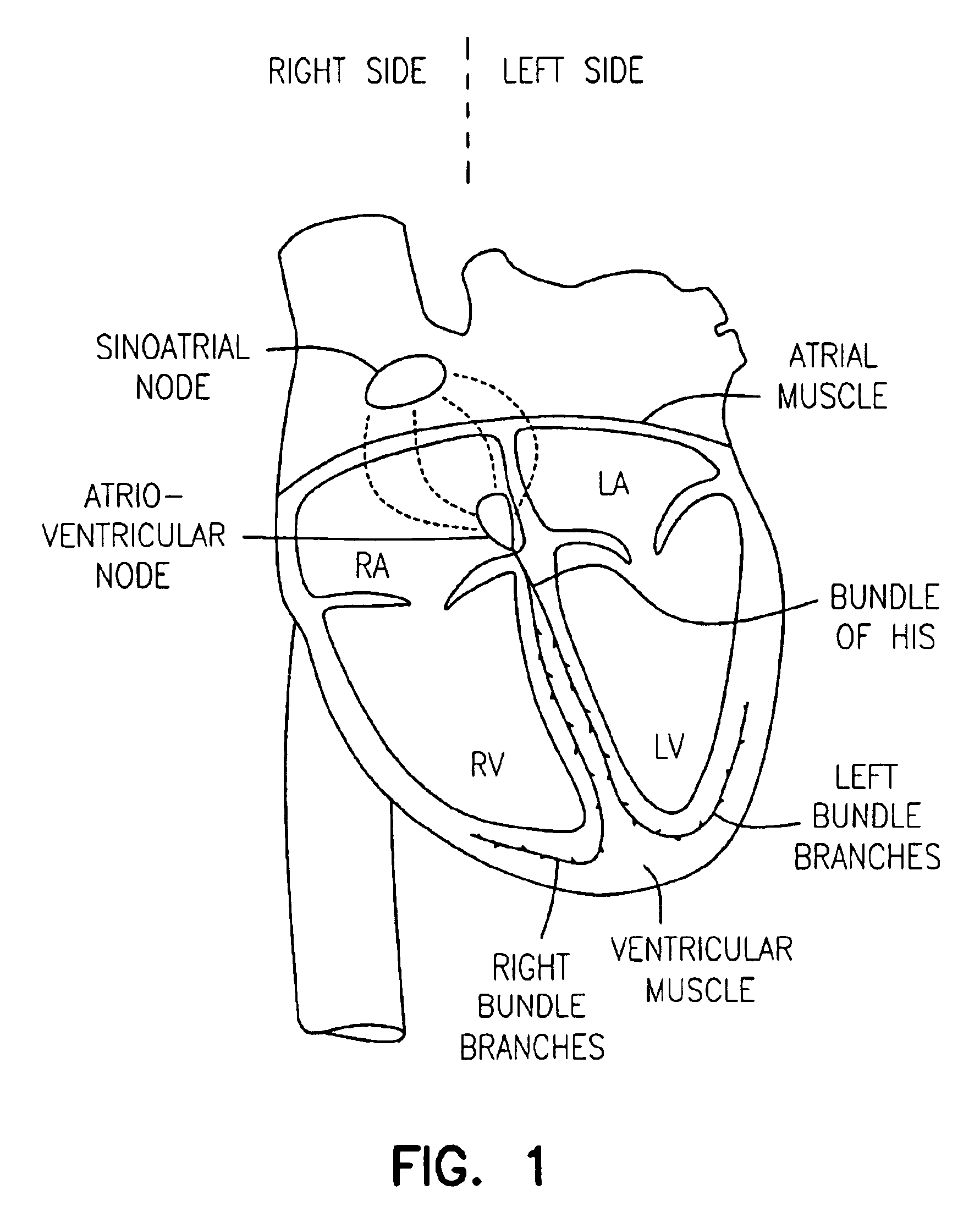
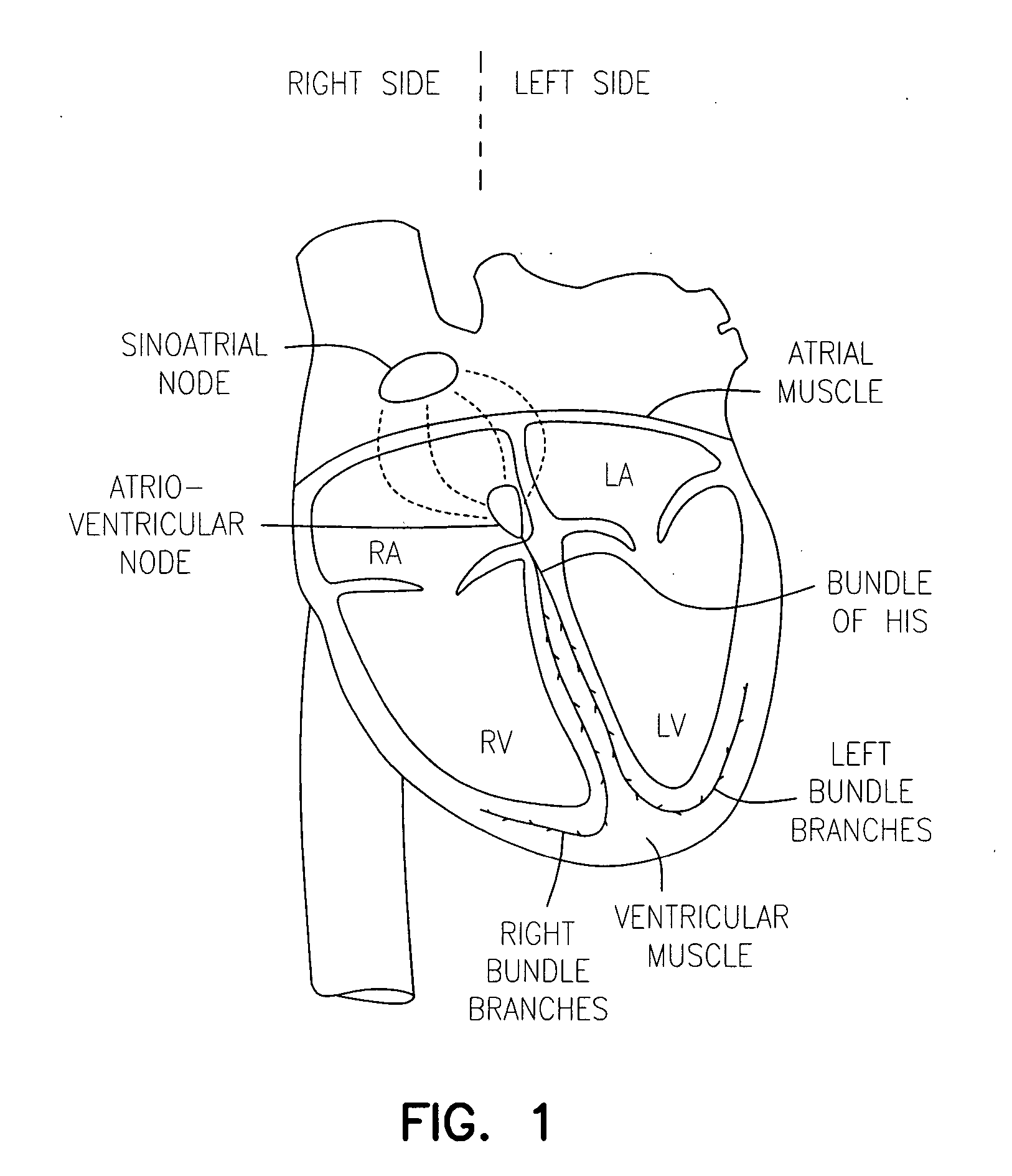
The term stroke volume can apply to each of the two ventricles of the heart, although it usually refers to the left ventricle. The stroke volumes for each ventricle are generally equal, both being approximately 70 mL in a healthy 70-kg man.
Device for diagnosing physiological state and device for controlling the same
PCT No. PCT / JP96 / 01254 Sec. 371 Date Apr. 2, 1997 Sec. 102(e) Date Apr. 2, 1997 PCT Filed May 13, 1996 PCT Pub. No. WO96 / 35368 PCT Pub. Date Nov. 14, 1996The present invention relates to a device for diagnosing physiological state based on blood pulse waves detected in the body. It is the objective of the present invention to provide a device which correctly diagnoses the current physiological state based on changes in physiological state measured over a specified period of time in the past while taking into consideration the cyclical variation exhibited in physiological state. In order to realize this objective, the device according to the present invention has as its main components: blood pulse wave detector 381 and stroke-volume-per-beat measurer 382 which respectively detect blood pulse wave and stroke volume in the body; blood pulse wave extraction memory 386 which extracts characteristic information from the detected blood pulse wave; memory 383 in which the physiological state calculated from the stroke volume and this characteristic information is stored; output portion 385 which outputs an alarm; and microcomputer 387 which controls each part inside the device. The microcomputer calculates the circulatory parameters based on characteristic information obtained from the waveform extraction memory, and stores the parameters in memory at specified time intervals. At these times, microcomputer 387 calculates the circulatory parameters from the stroke volume per beat and the characteristic information of the blood pulse wave at specified time intervals, and stores the parameters in memory 383. Further, microcomputer 387 reads out from memory 383 the circulatory parameters from a specified time interval in the past, and calculates the average value and standard deviation. Microcomputer 387 then determines whether or not the current circulatory parameters are within a specified range determined by their average value and standard deviation. When the circulatory parameters are determined to be outside this range, microcomputer 387 controls output portion 385 to sound an alarm.
Owner:SEIKO EPSON CORP
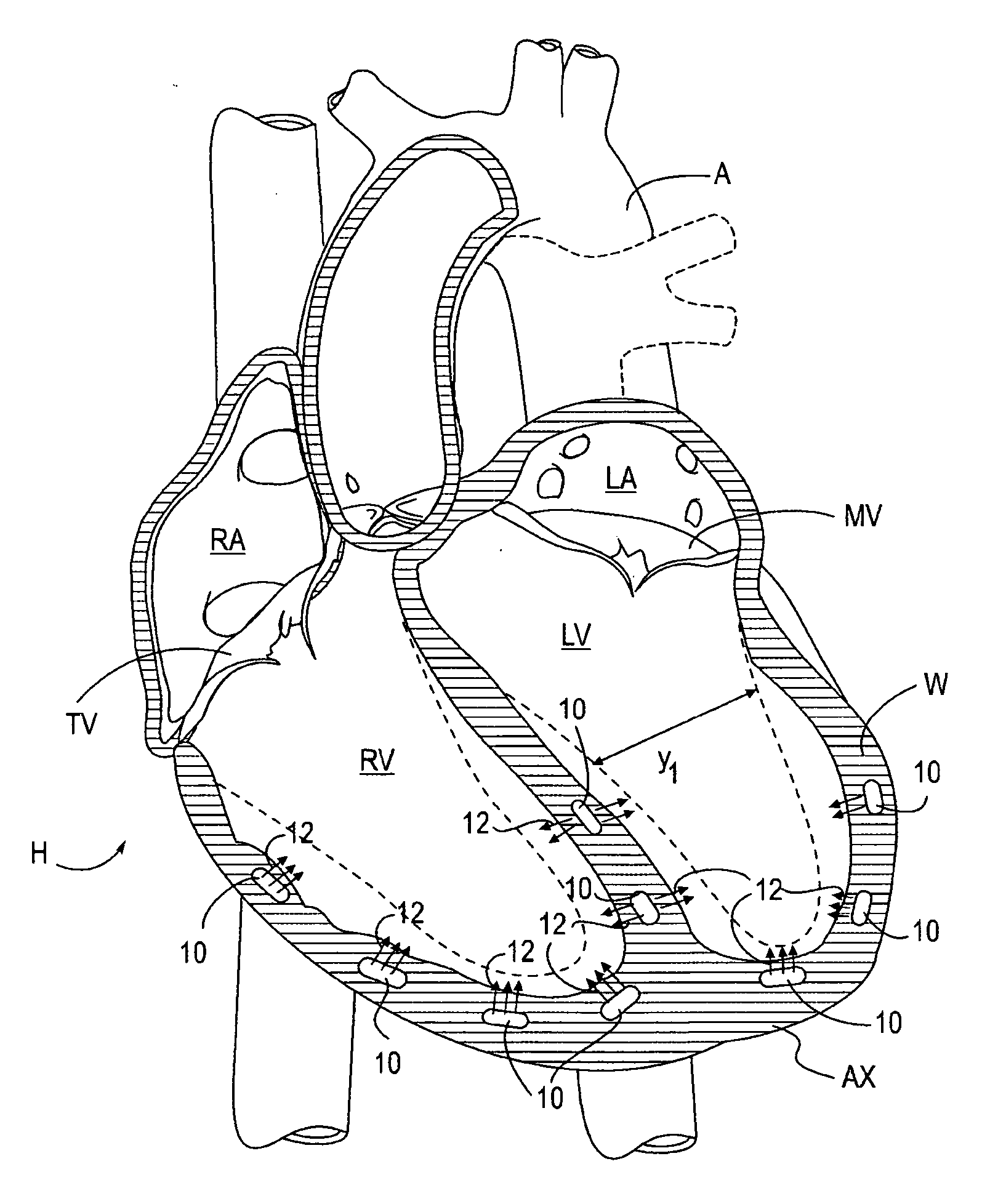
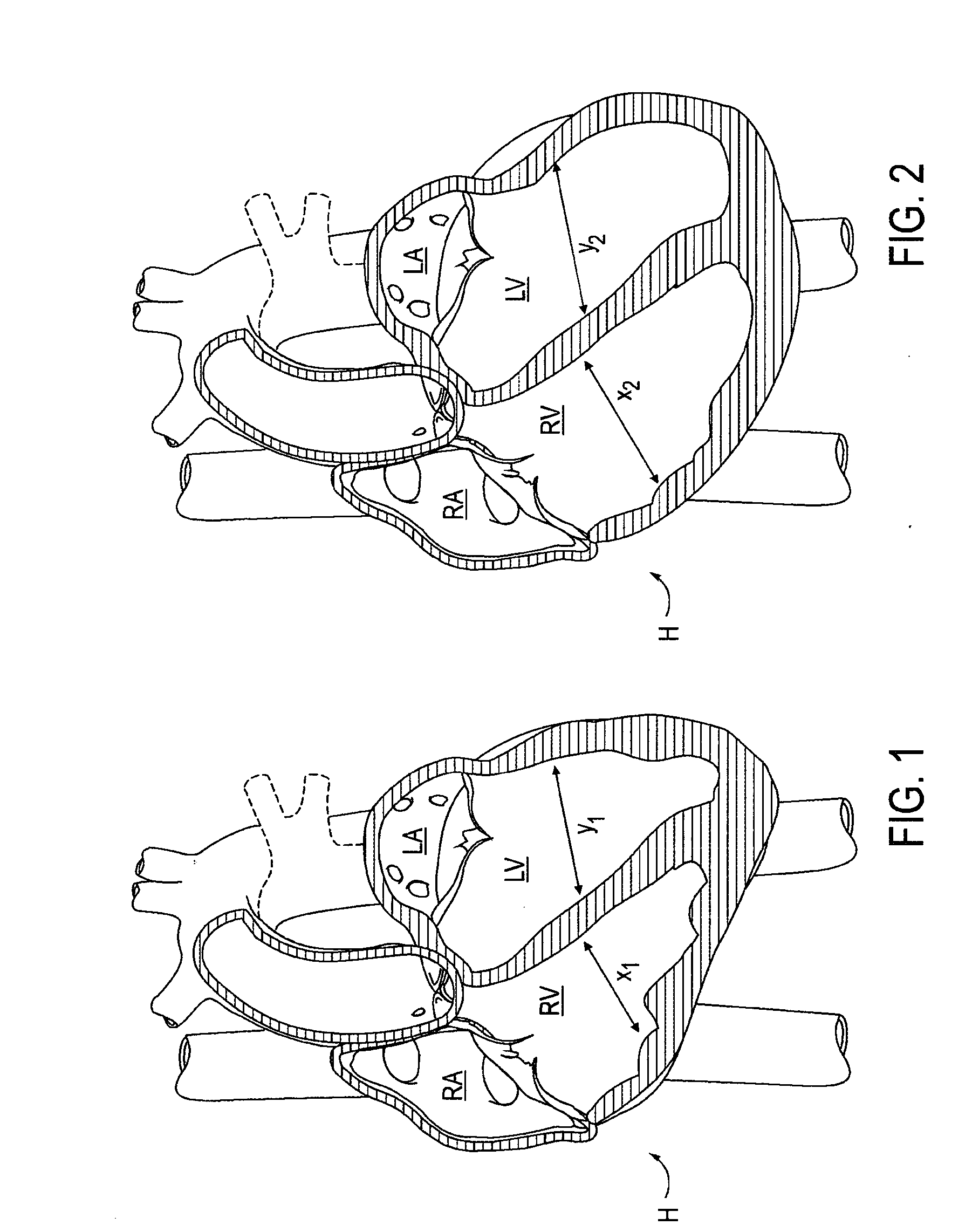
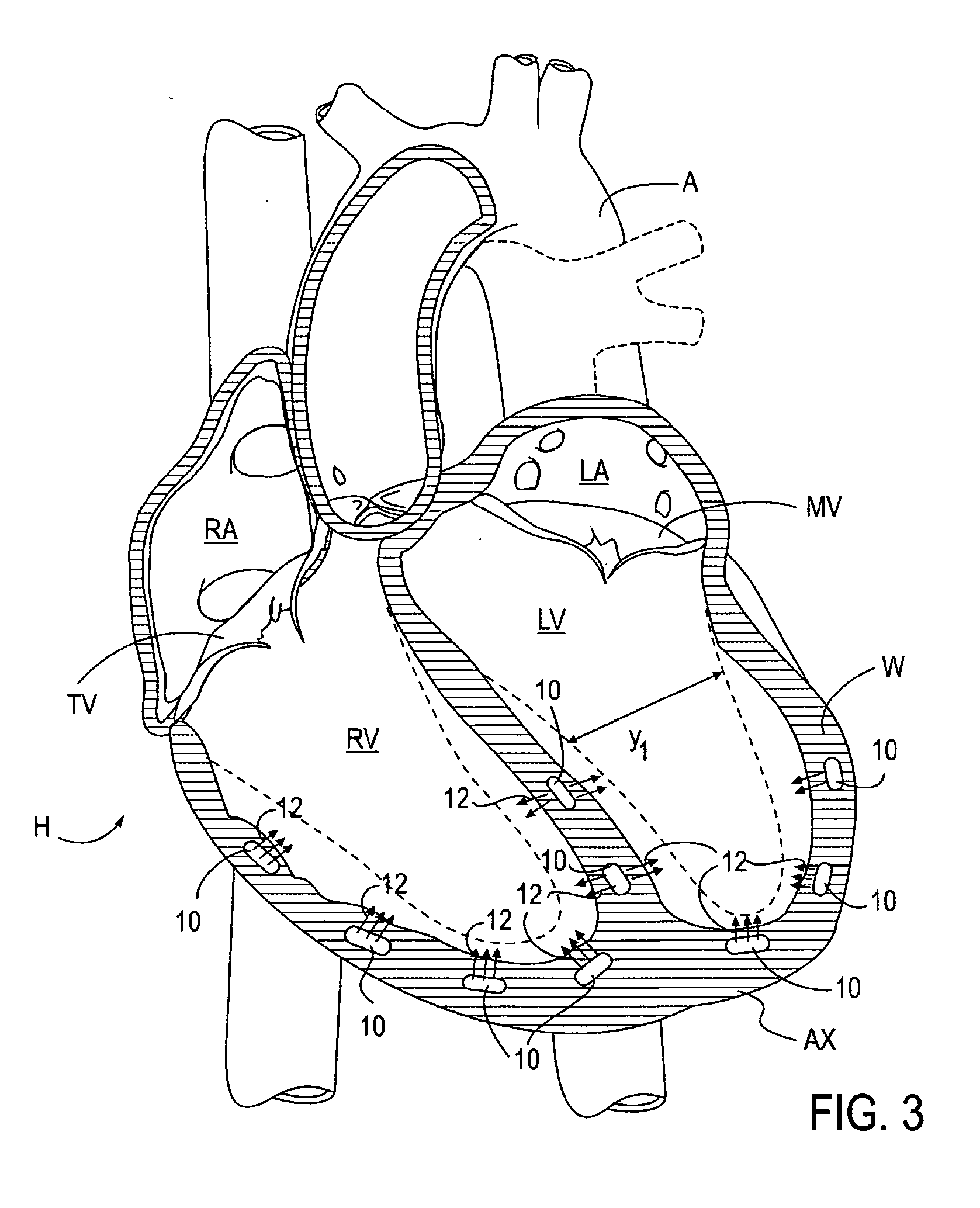
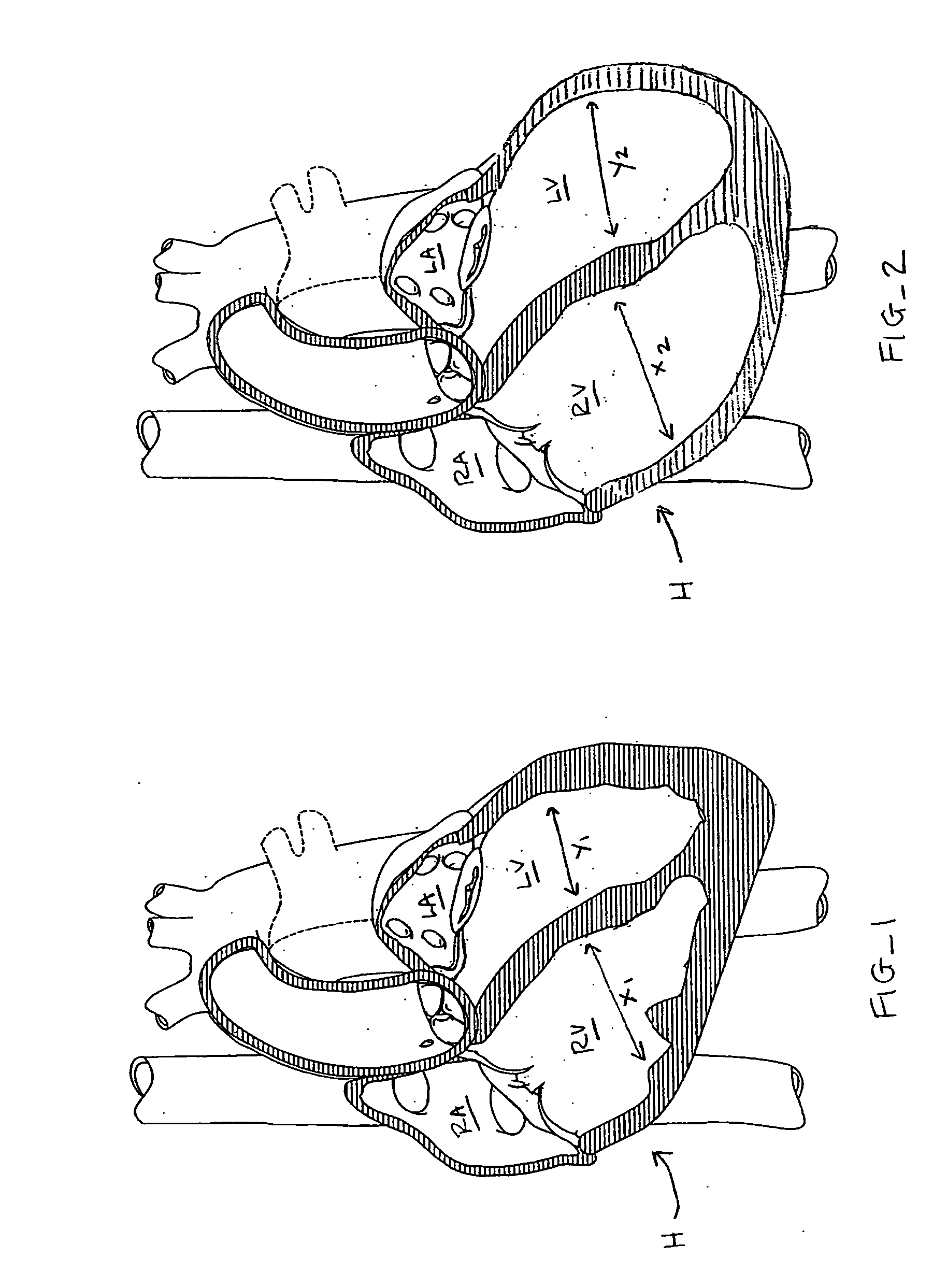
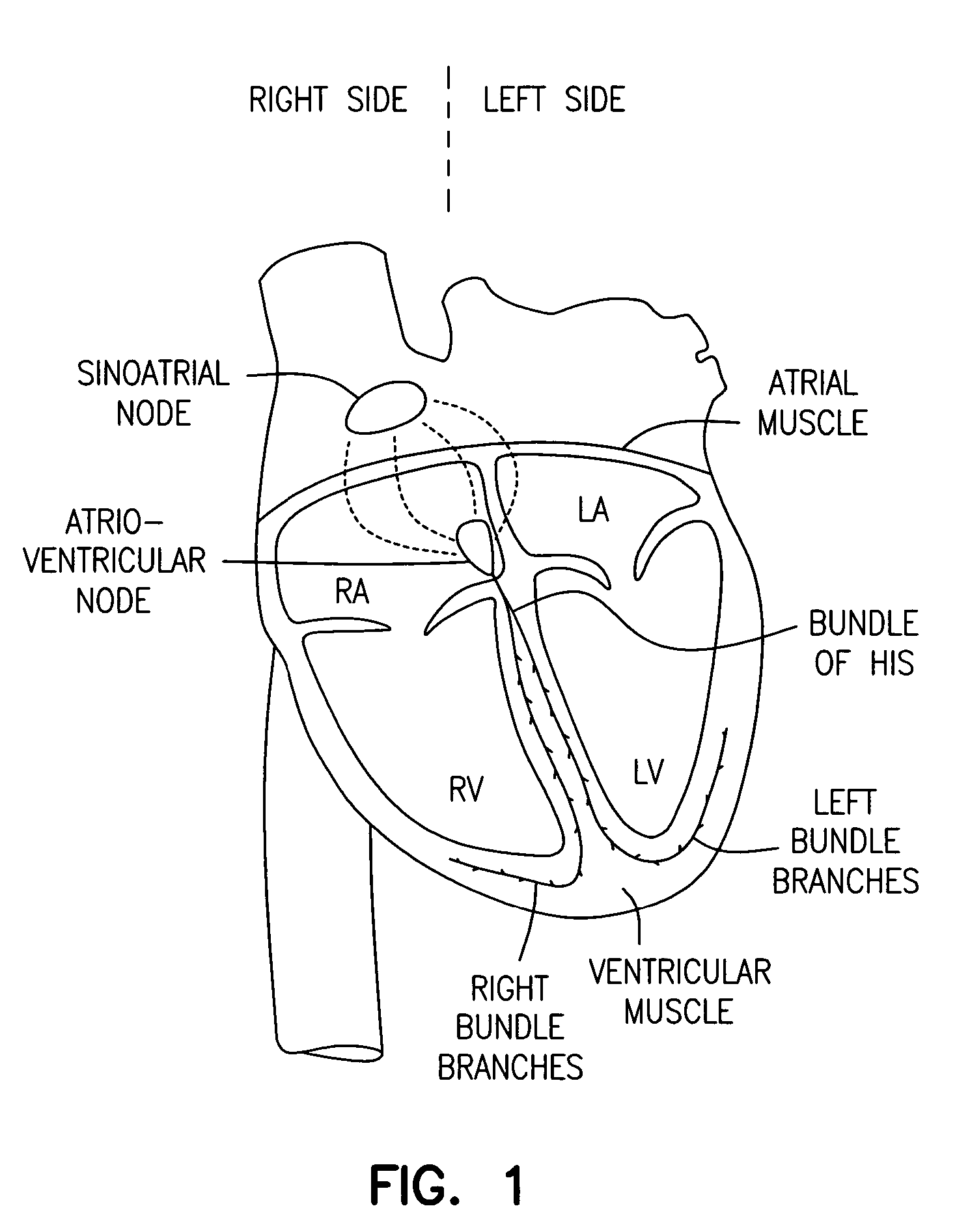
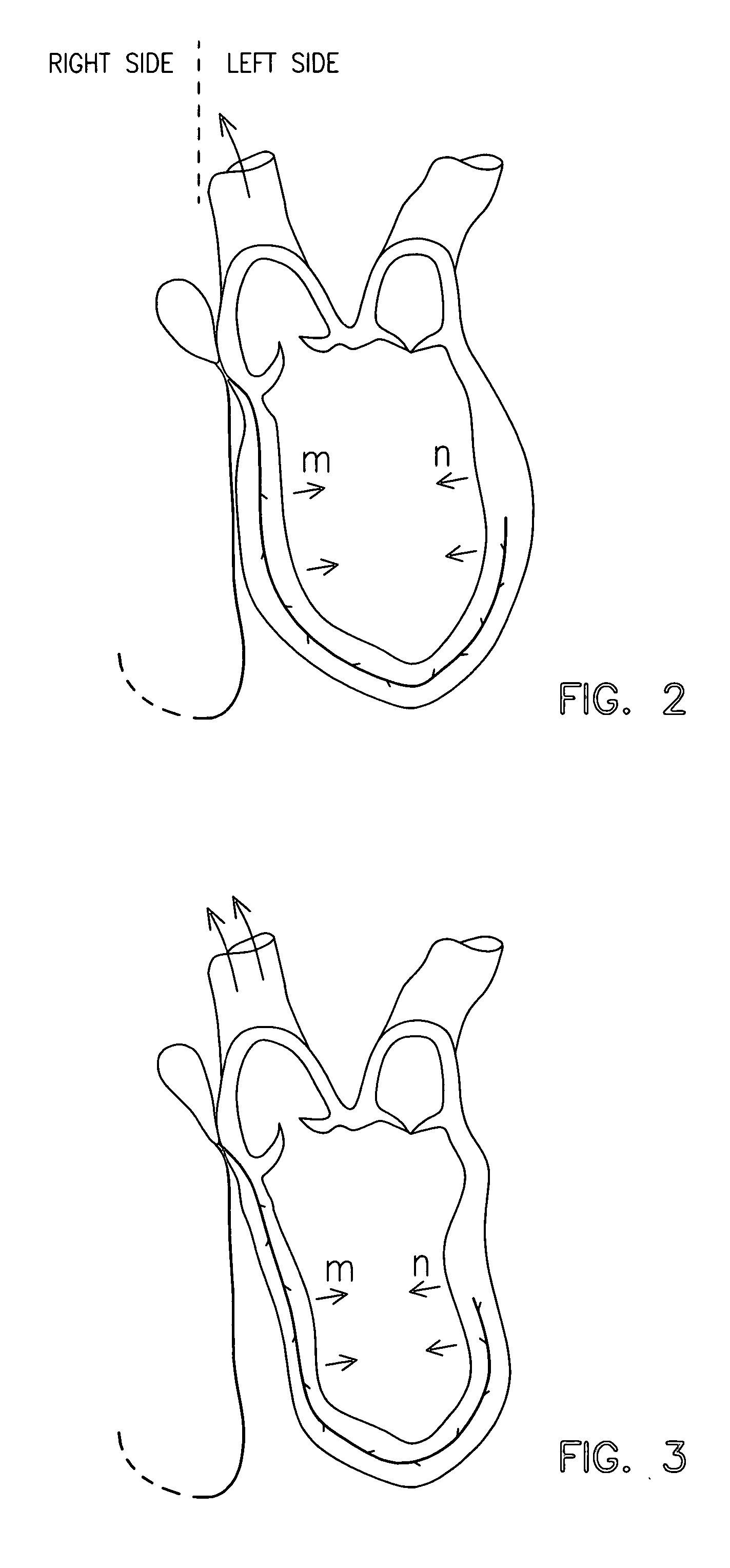
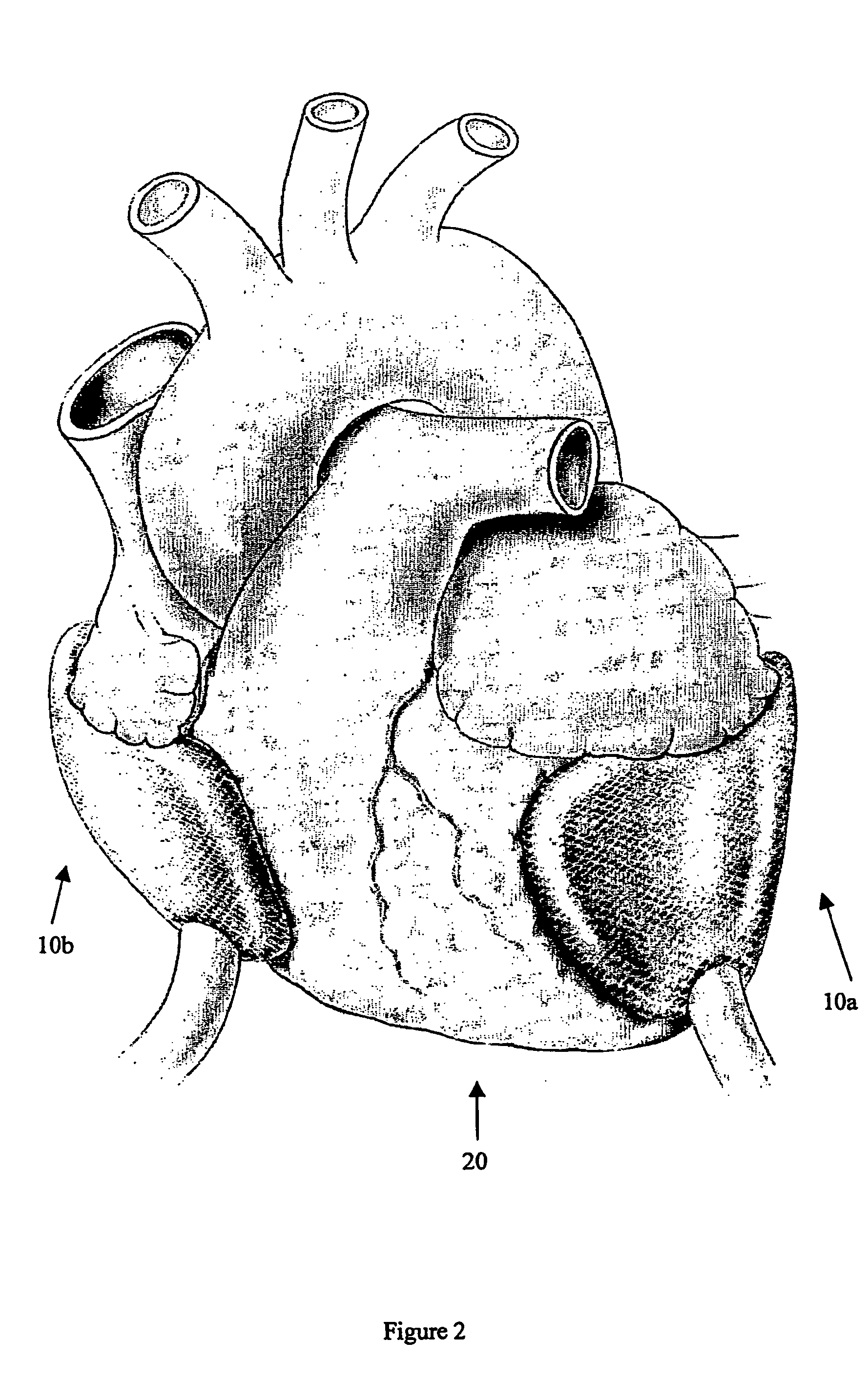
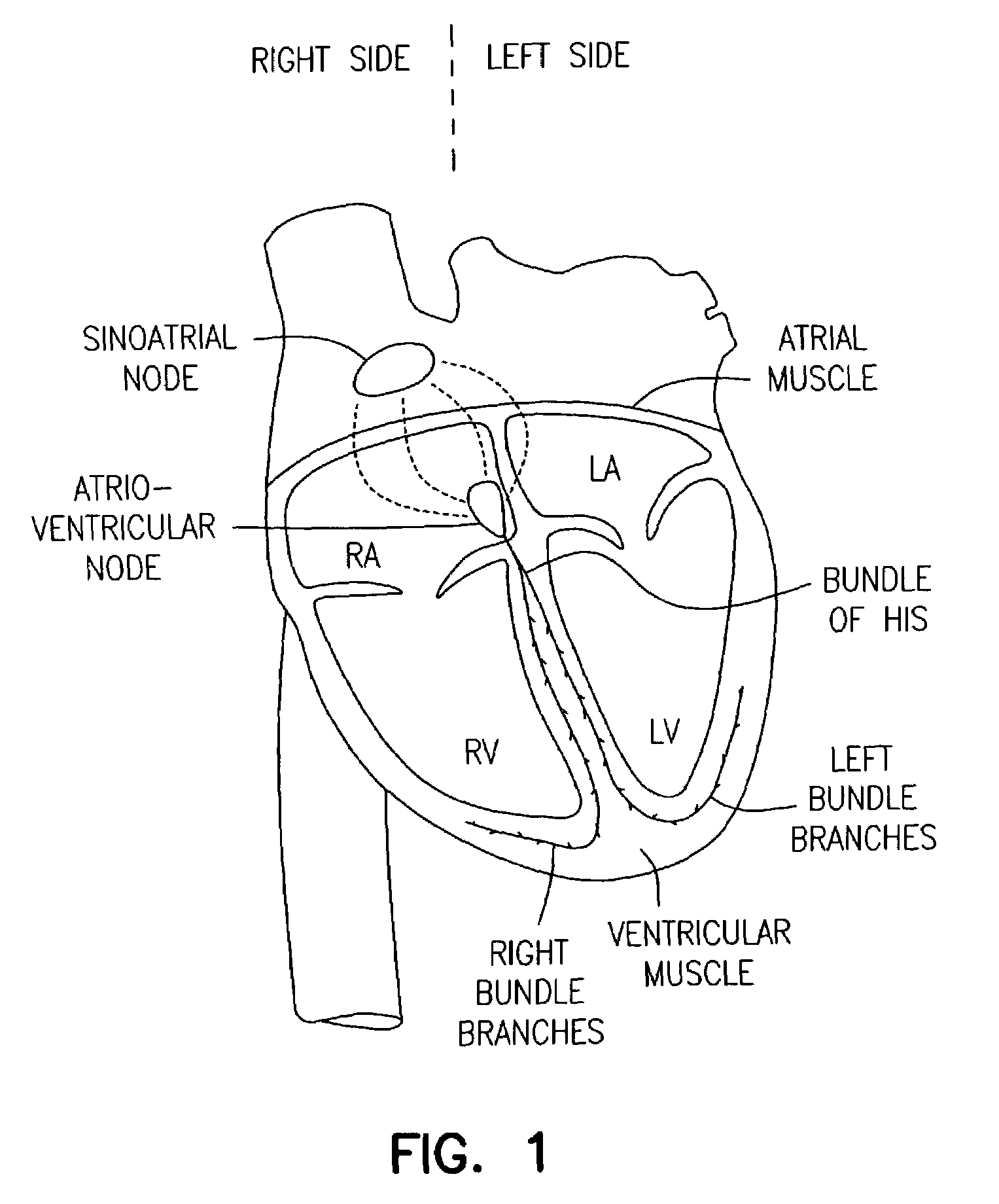
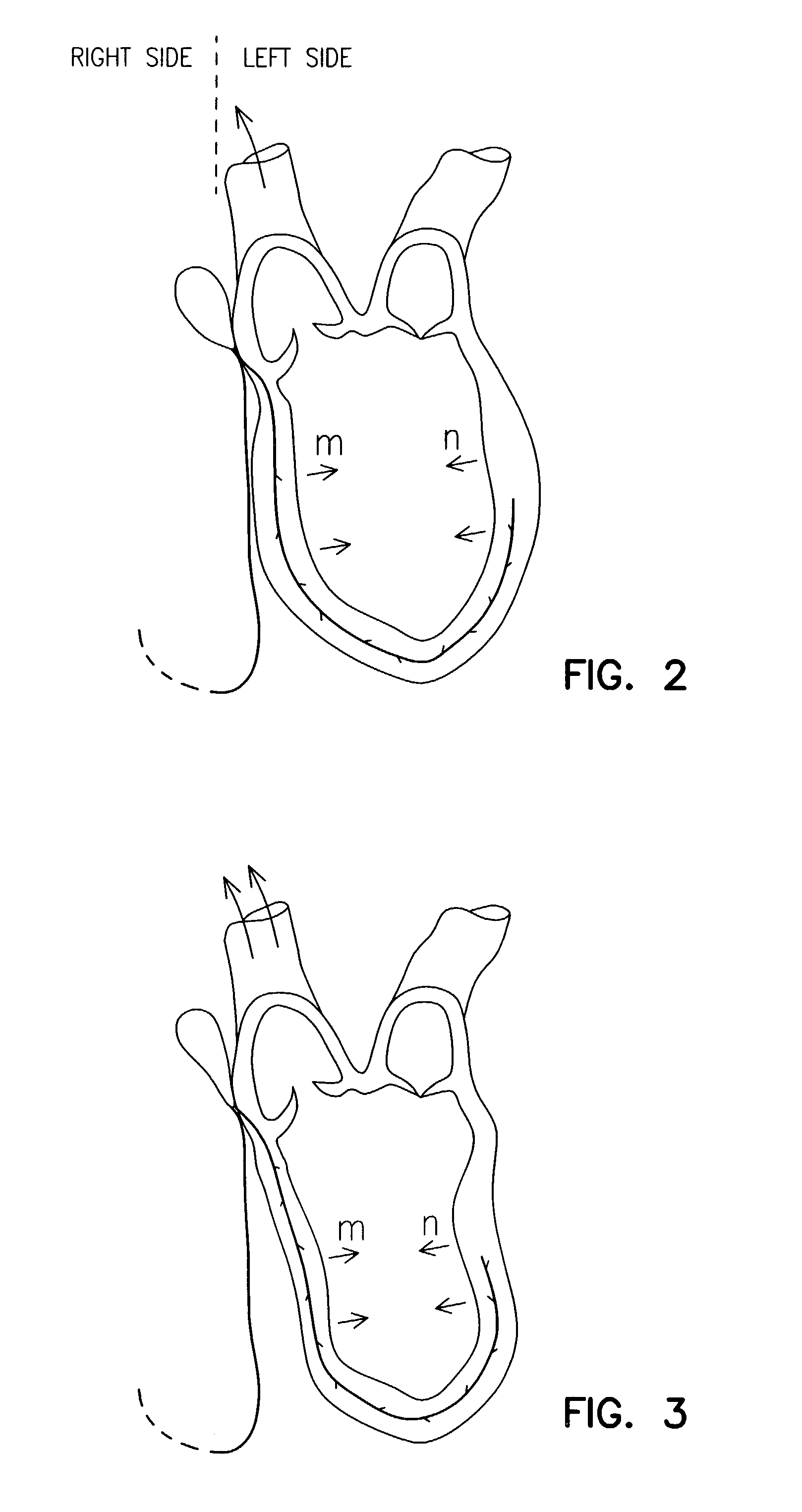
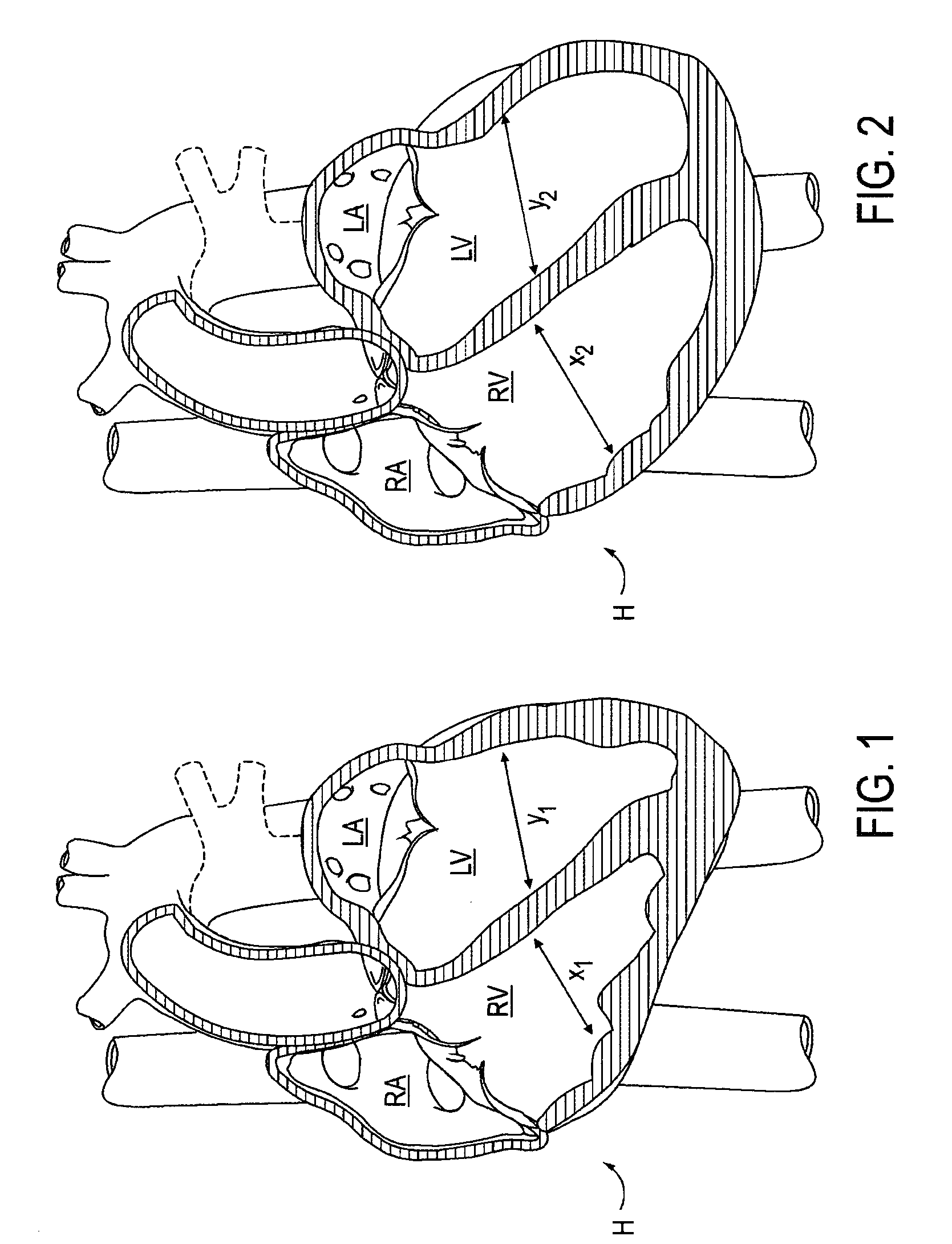
Magnetic devices and methods for reshaping heart anatomy
InactiveUS20060015003A1Improve shrinkageIncreased total stroke volumeElectrotherapyHeart valvesCardiac surfaceHeart Part
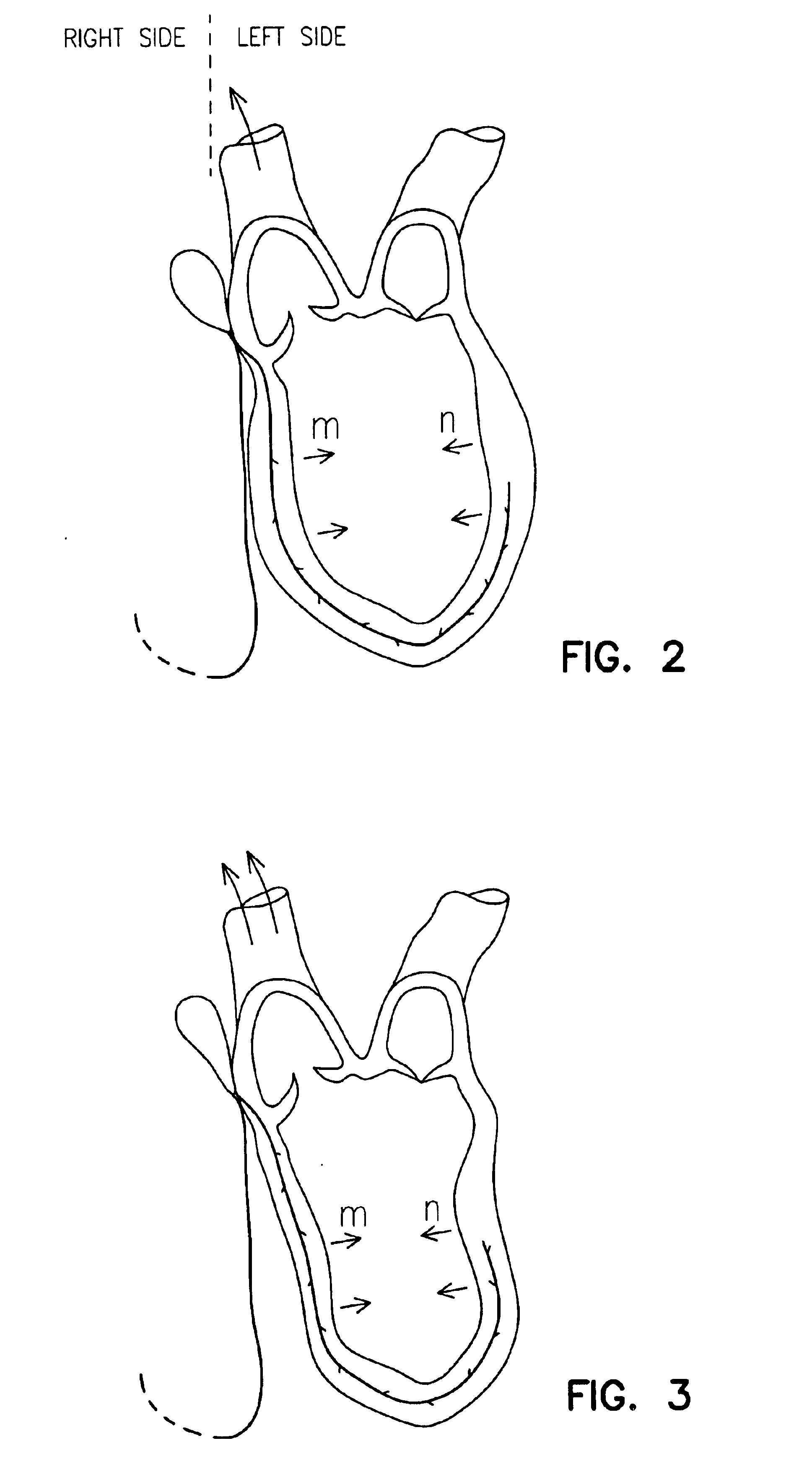
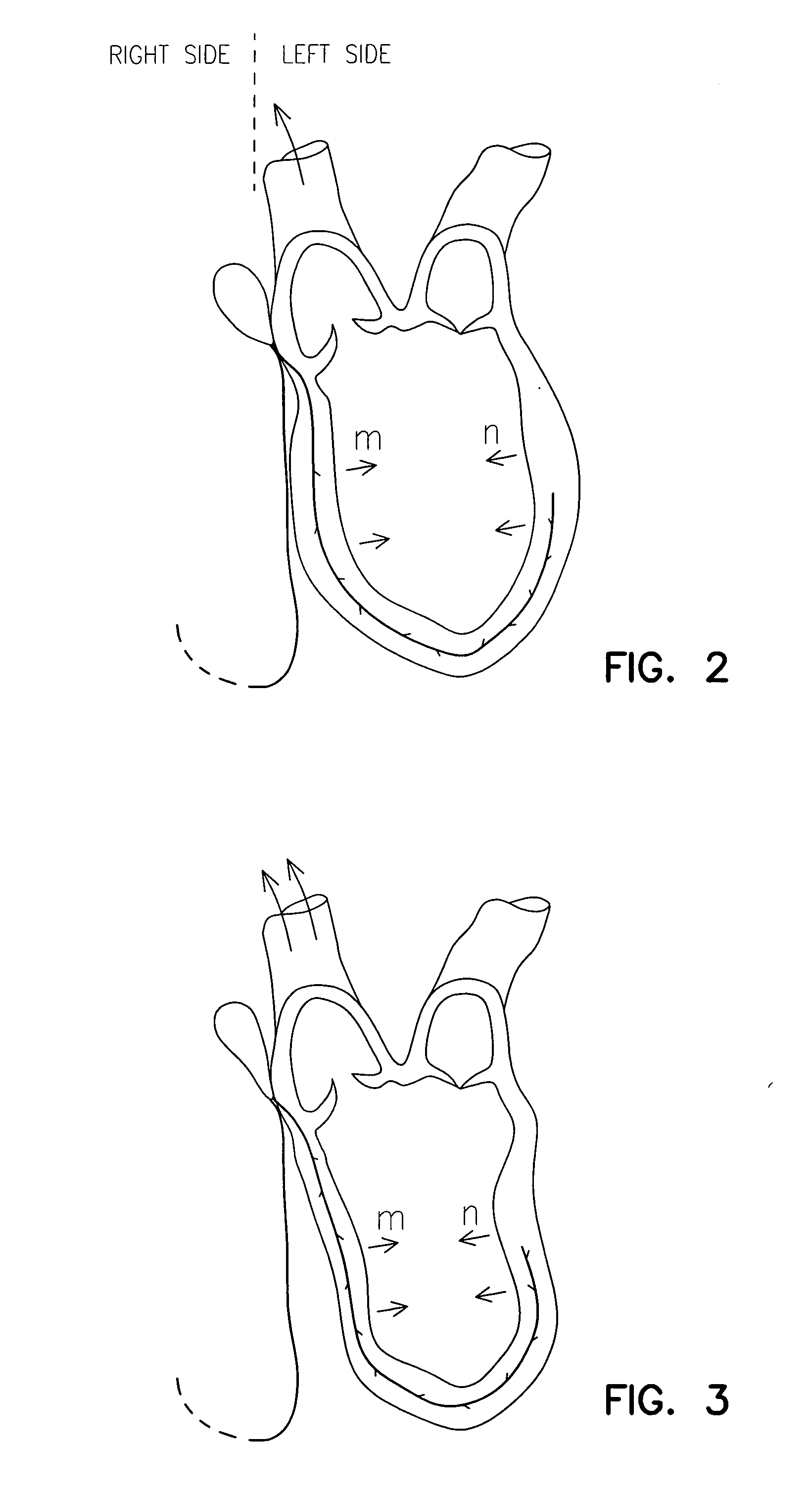
Systems, methods and devices are provided for treating heart failure patients suffering from various levels of heart dilation. Heart dilation treated by reshaping the heart anatomy with the use of magnetic forces. Such reshaping changes the geometry of portions of the heart, particularly the right or left ventricles, to increase contractibility of the ventricles thereby increasing the stroke volume which in turn increases the cardiac output of the heart. The magnetic forces are applied with the use of one or more magnetic elements which are implanted within the heart tissue or attached externally and / or internally to a surface of the heart. The various charges of the magnetic forces interact causing the associated heart tissue areas to readjust position, such as to decrease the width of the ventricles. Such repositioning is maintained over time by the force of the magnetic elements, allowing the damaging effects of heart dilation to slow in progression or reverse.
Owner:MICARDIA CORP
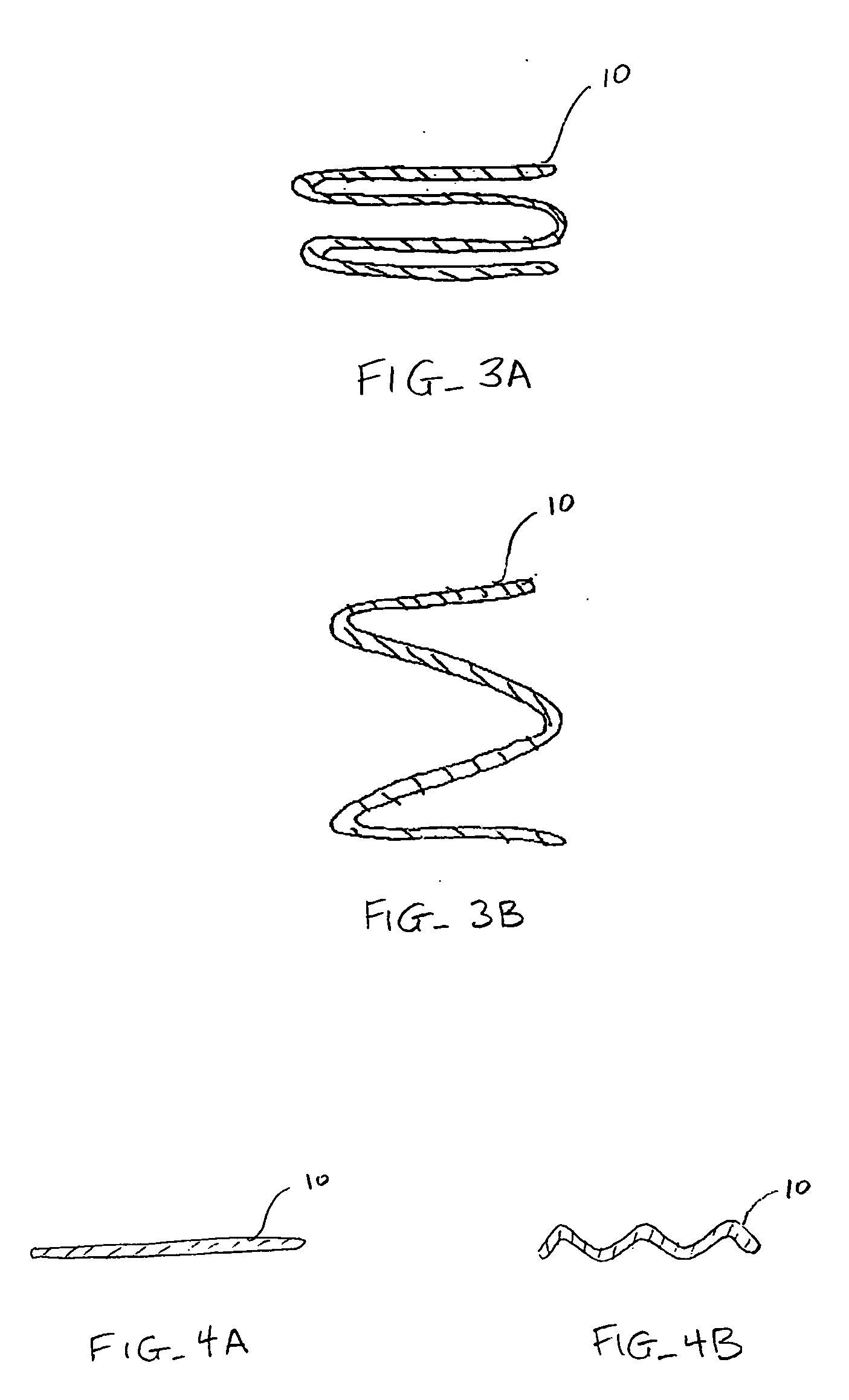
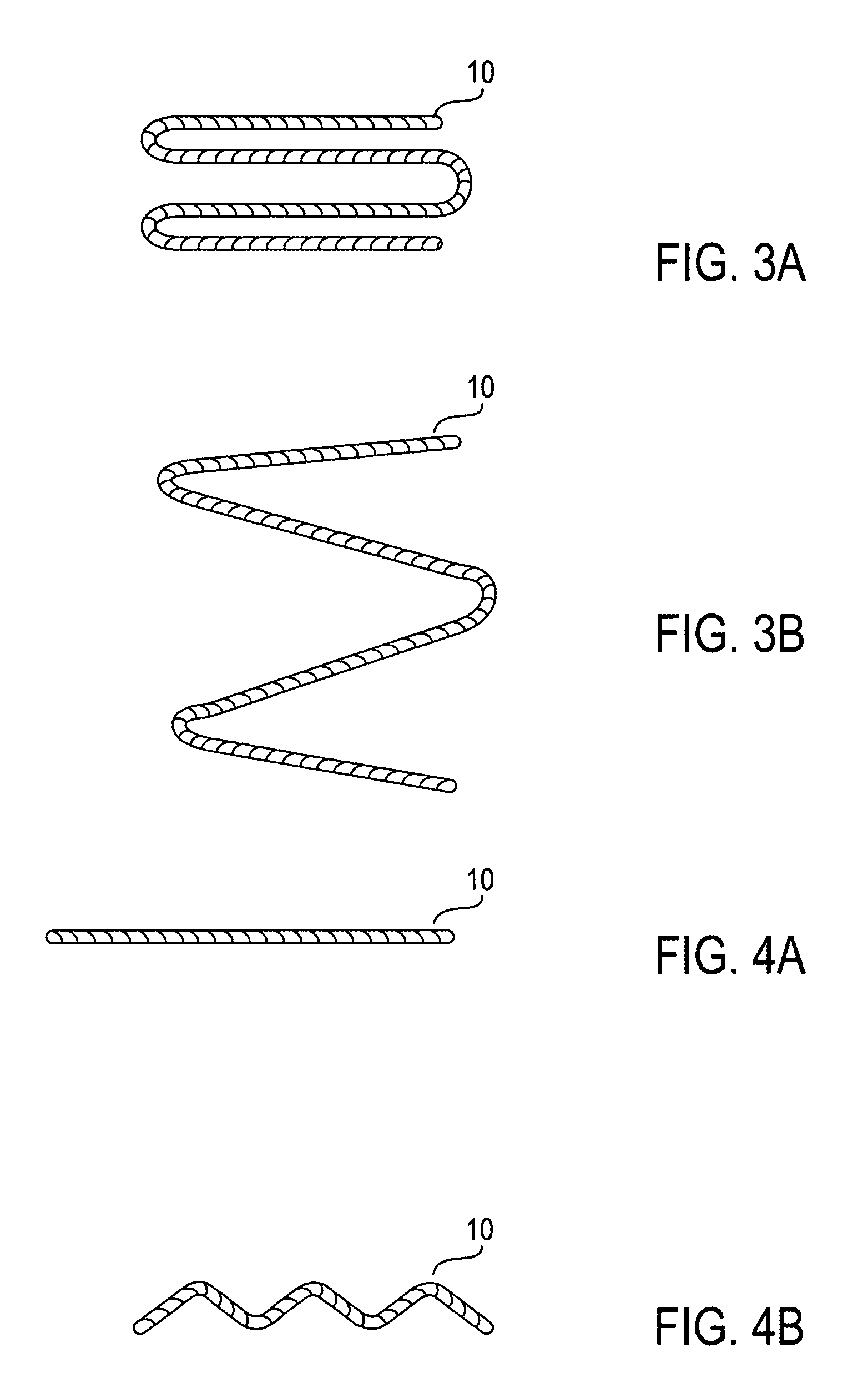
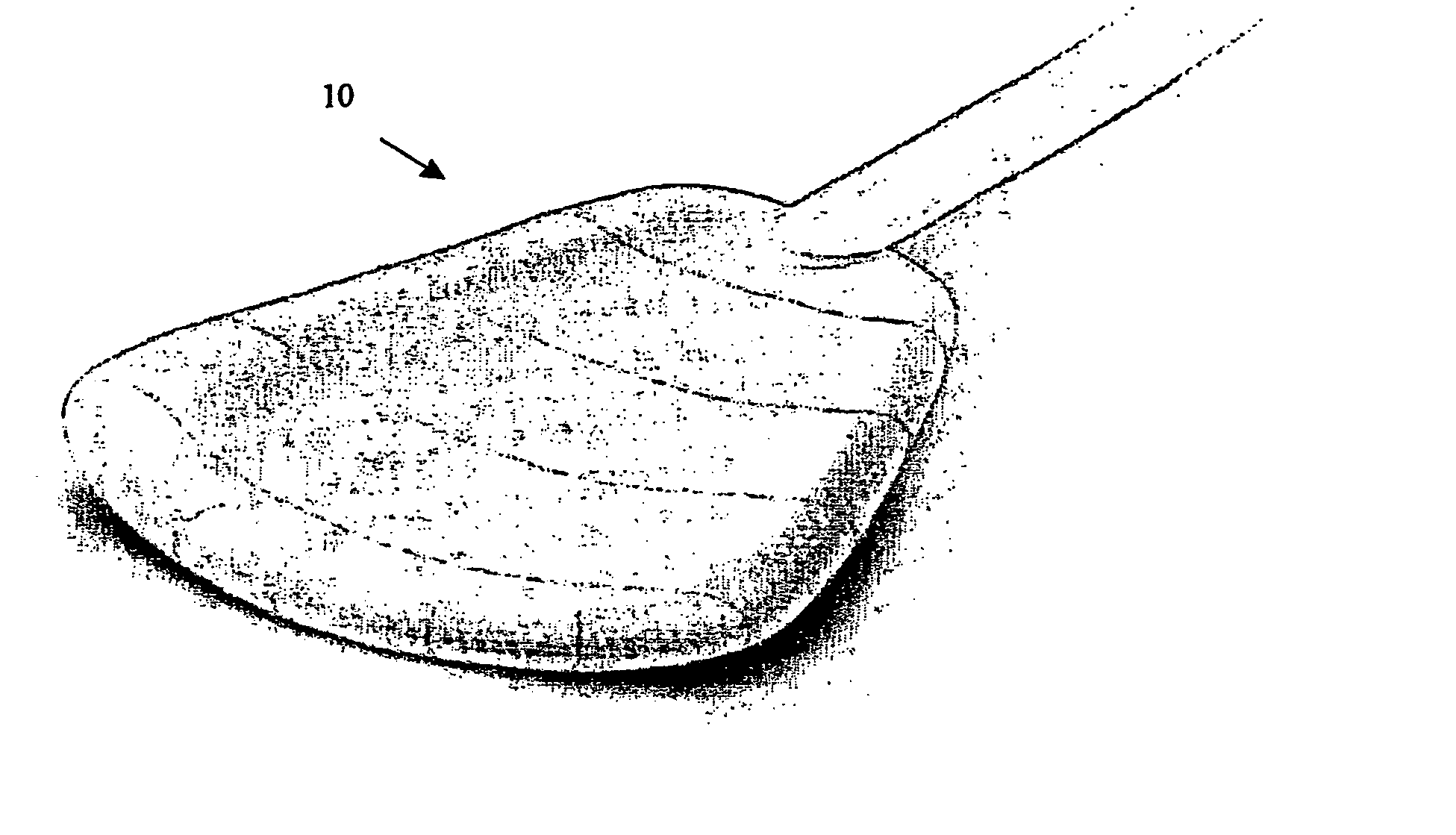
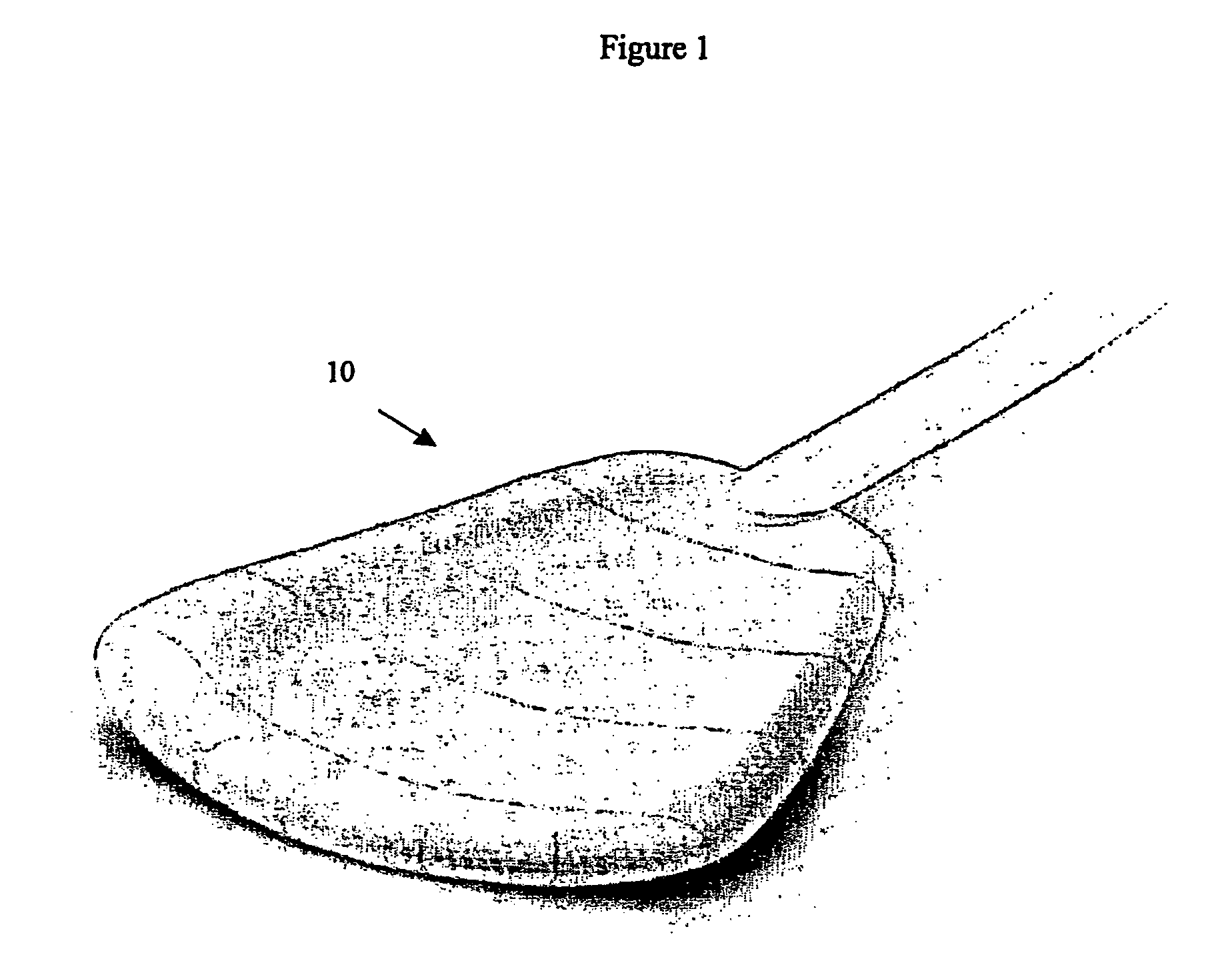
Shape memory devices and methods for reshaping heart anatomy
InactiveUS20060015002A1Improve shrinkageReduce widthSuture equipmentsSurgical needlesCardiac surfaceHeart anatomy
Systems, methods and devices are provided for treating heart failure patients suffering from various levels of heart dilation. Such heart dilation is treated by reshaping the heart anatomy with the use of shape memory elements. Such reshaping changes the geometry of portions of the heart, particularly the right or left ventricles, to increase contractibility of the ventricles thereby increasing the stroke volume which in turn increases the cardiac output of the heart. The shape memory elements have an original shape and at least one memory shape. The elements are implanted within the heart tissue or attached externally and / or internally to a surface of the heart when in the original shape. The elements are then activated to transition from the original shape to one of the at least one memory shapes. Transitioning of the elements cause the associated heart tissue areas to readjust position, such as to decrease the width of the ventricles. Such repositioning is maintained over time by the elements, allowing the damaging effects of heart dilation to slow in progression or reverse.
Owner:MICARDIA CORP
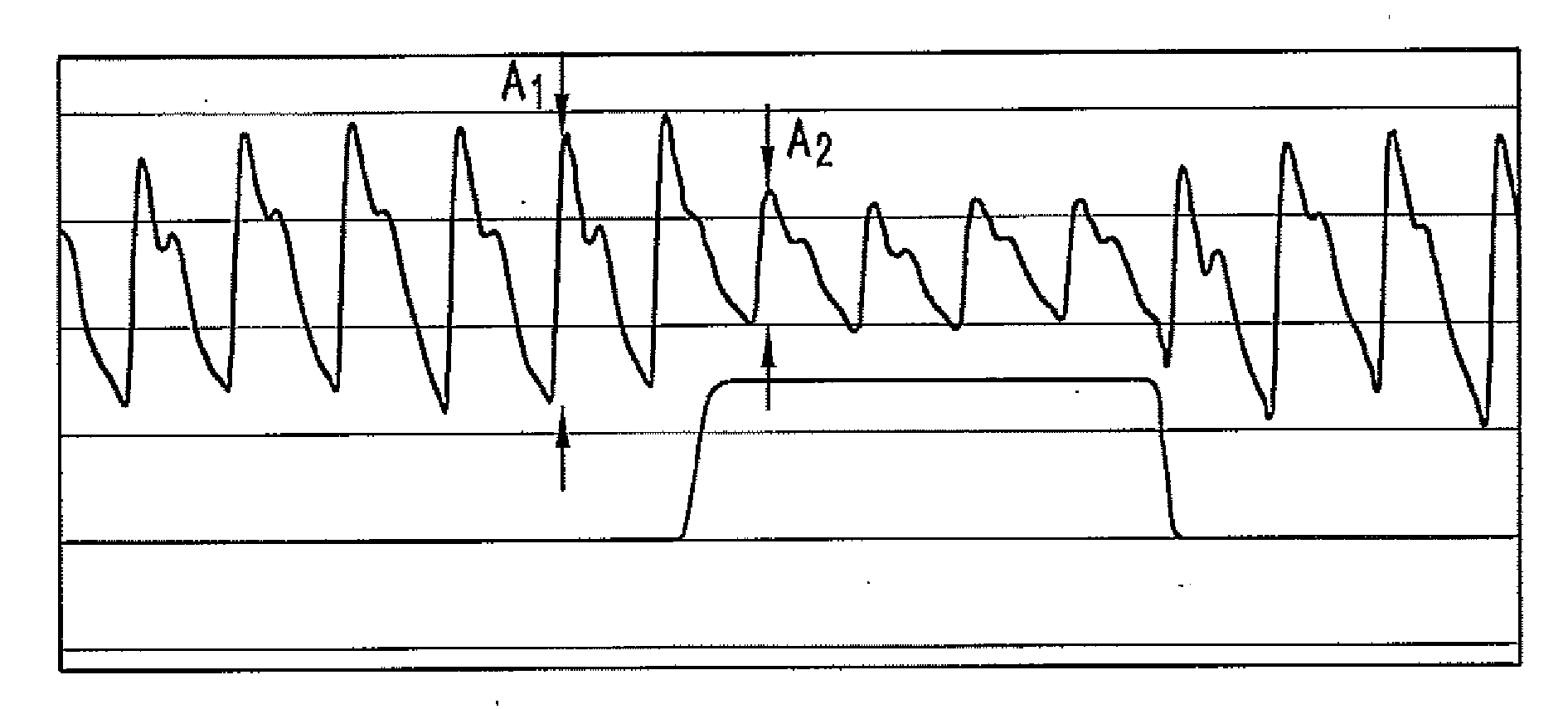
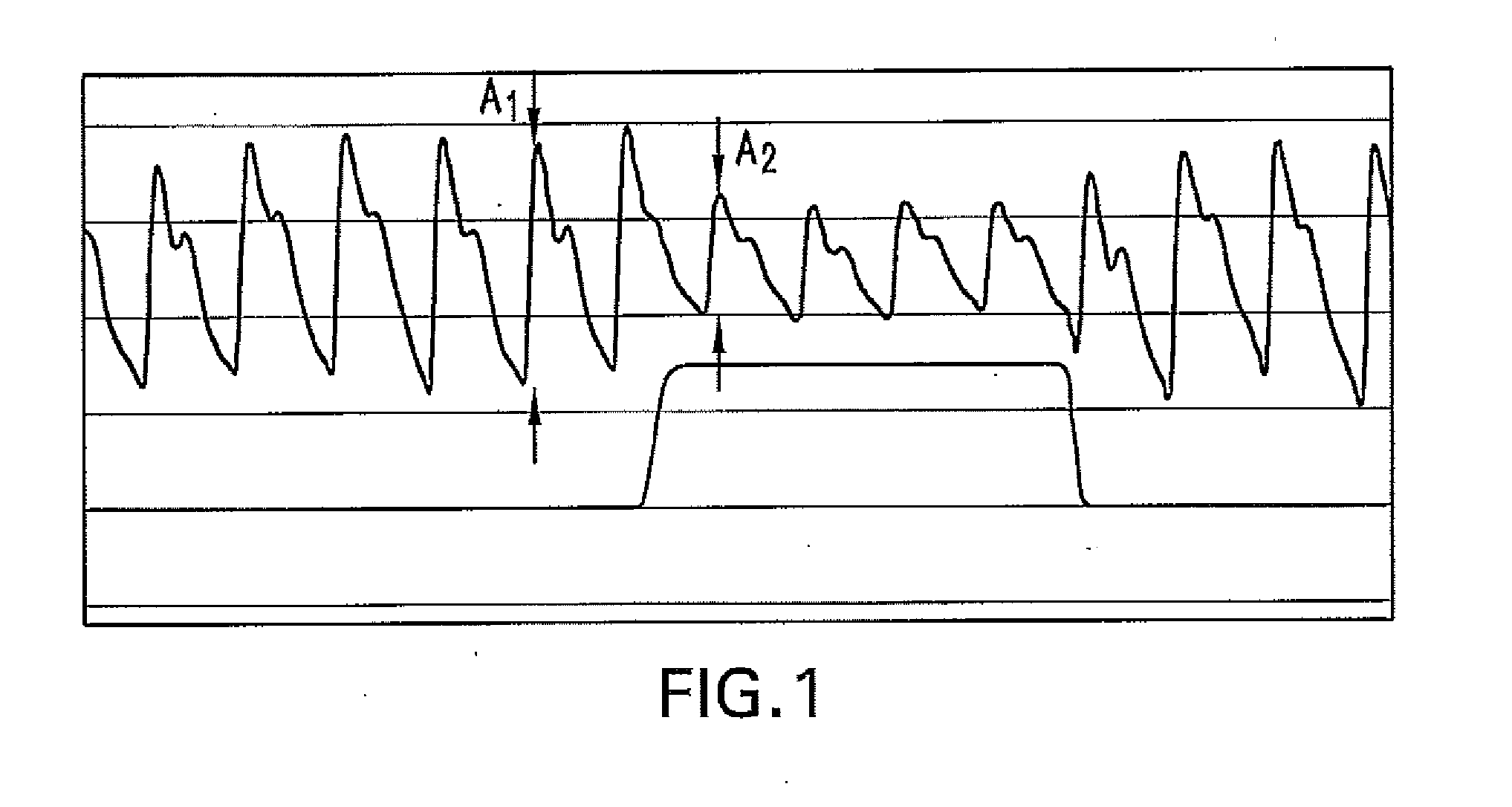
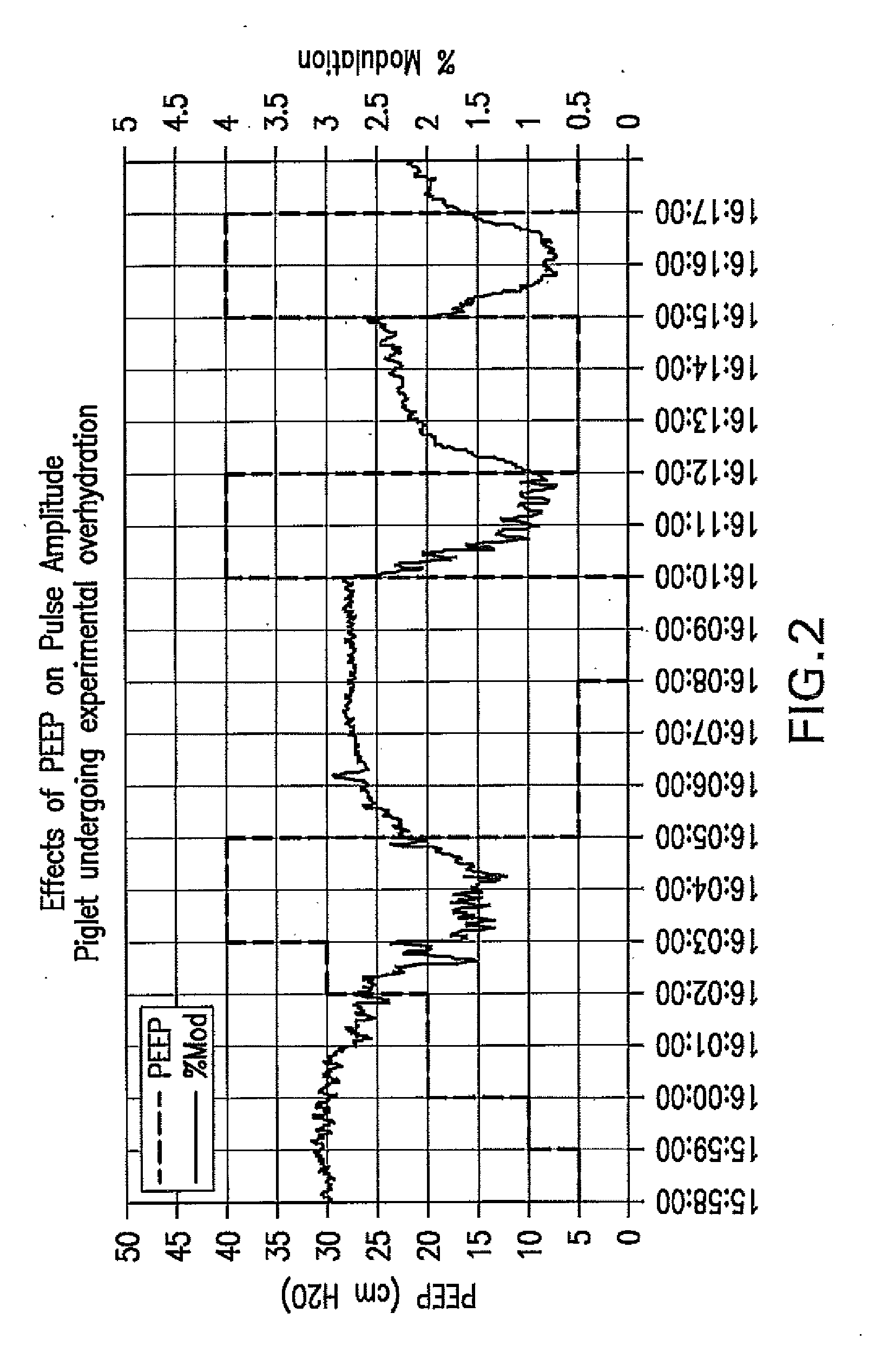
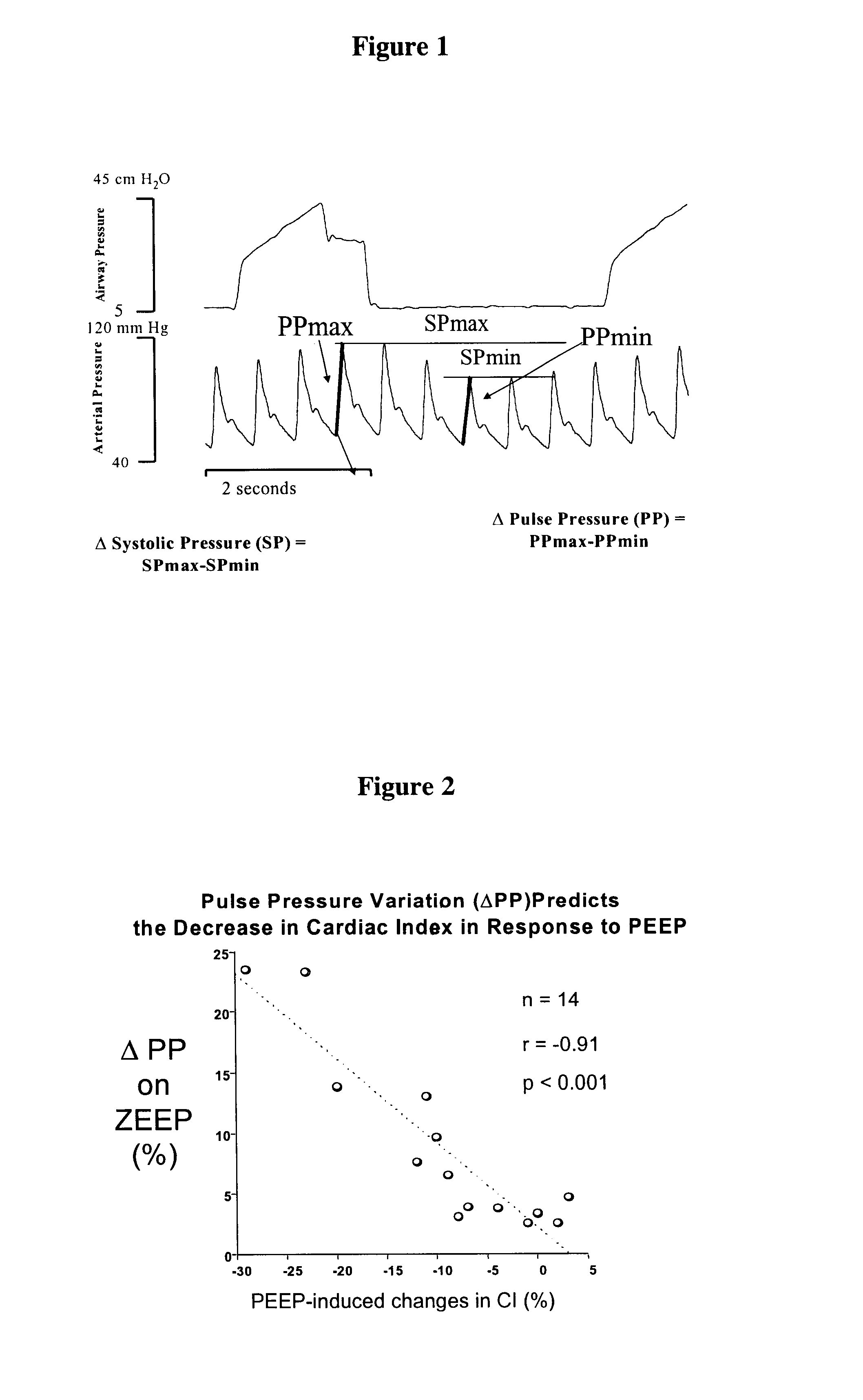
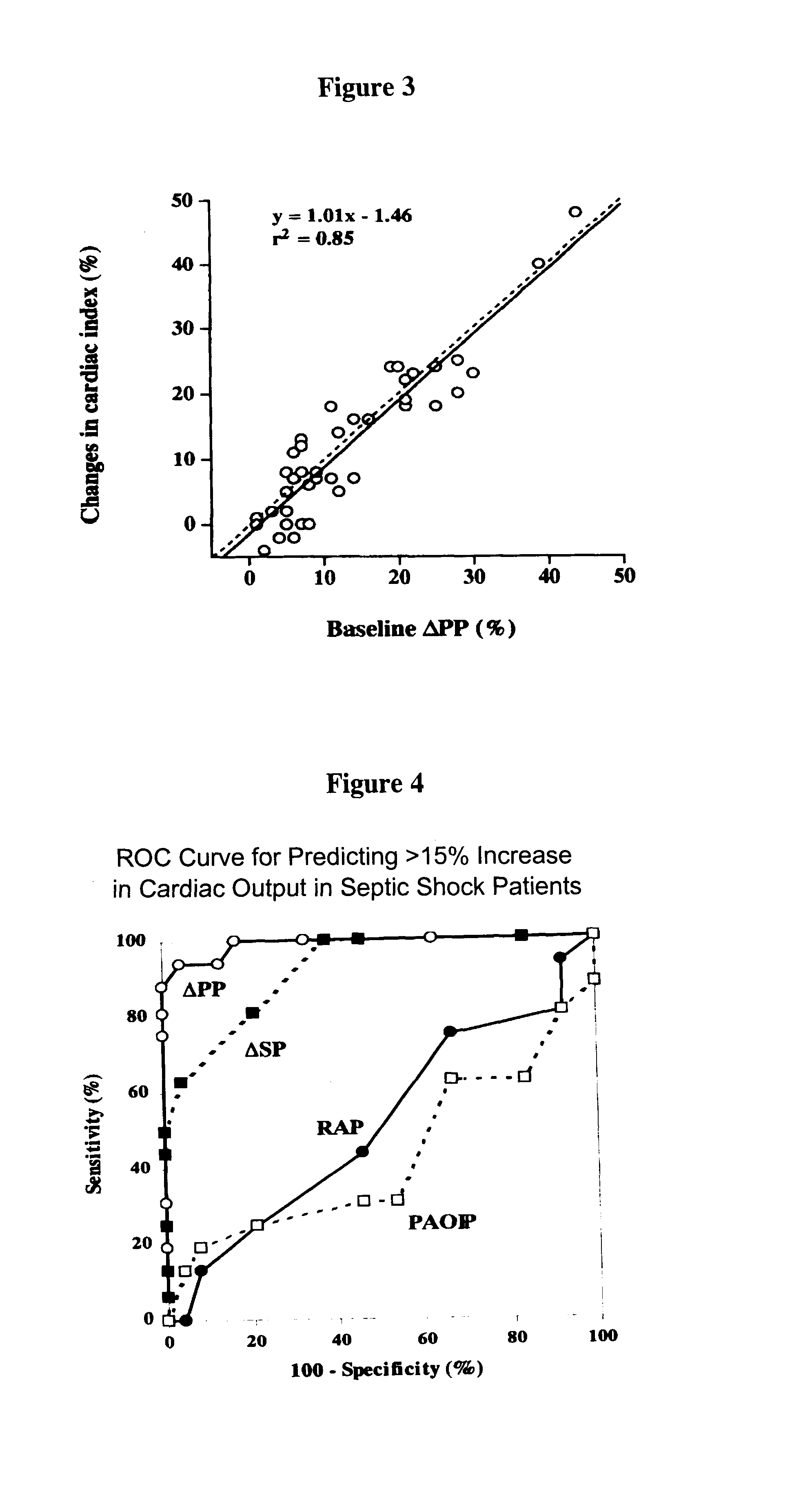
Method For Determining Hemodynamic Effects Of Positive Pressure Ventilation
The present disclosure relates, in some embodiments, to devices, systems, and / or methods for collecting, processing, and / or displaying stroke volume and / or cardiac output data. For example, a device for assessing changes in cardiac output and / or stroke volume of a subject receiving airway support may comprise a processor; an airway sensor in communication with the processor, wherein the airway sensor is configured and arranged to sense pressure in the subject's airway, lungs, and / or intrapleural space over time; a blood volume sensor in communication with the processor, wherein the blood volume sensor is configured and arranged to sense pulsatile volume of blood in a tissue of the subject over time; and a display configured and arranged to display a representative of an airway pressure, a pulsatile blood volume, a photoplethysmogram, a photoplethysmogram ratio, the determined cardiac output and / or stroke volume, or combinations thereof. A method of assessing changes in cardiac output or stroke volume of a subject receiving airway support from a breathing assistance system may comprise sensing pressure in the subject's airway as a function of time, sensing pulsatile volume of blood in a tissue of the subject as a function of time, producing a photoplethysmogram from the sensed pulsatile volume, determining the ratio of the amplitude of the photoplethysmogram during inhalation to the amplitude of the photoplethysmogram during exhalation, and determining the change in cardiac output or stroke volume of the subject using the determined ratio.
Owner:TYCO HEALTHCARE GRP LP
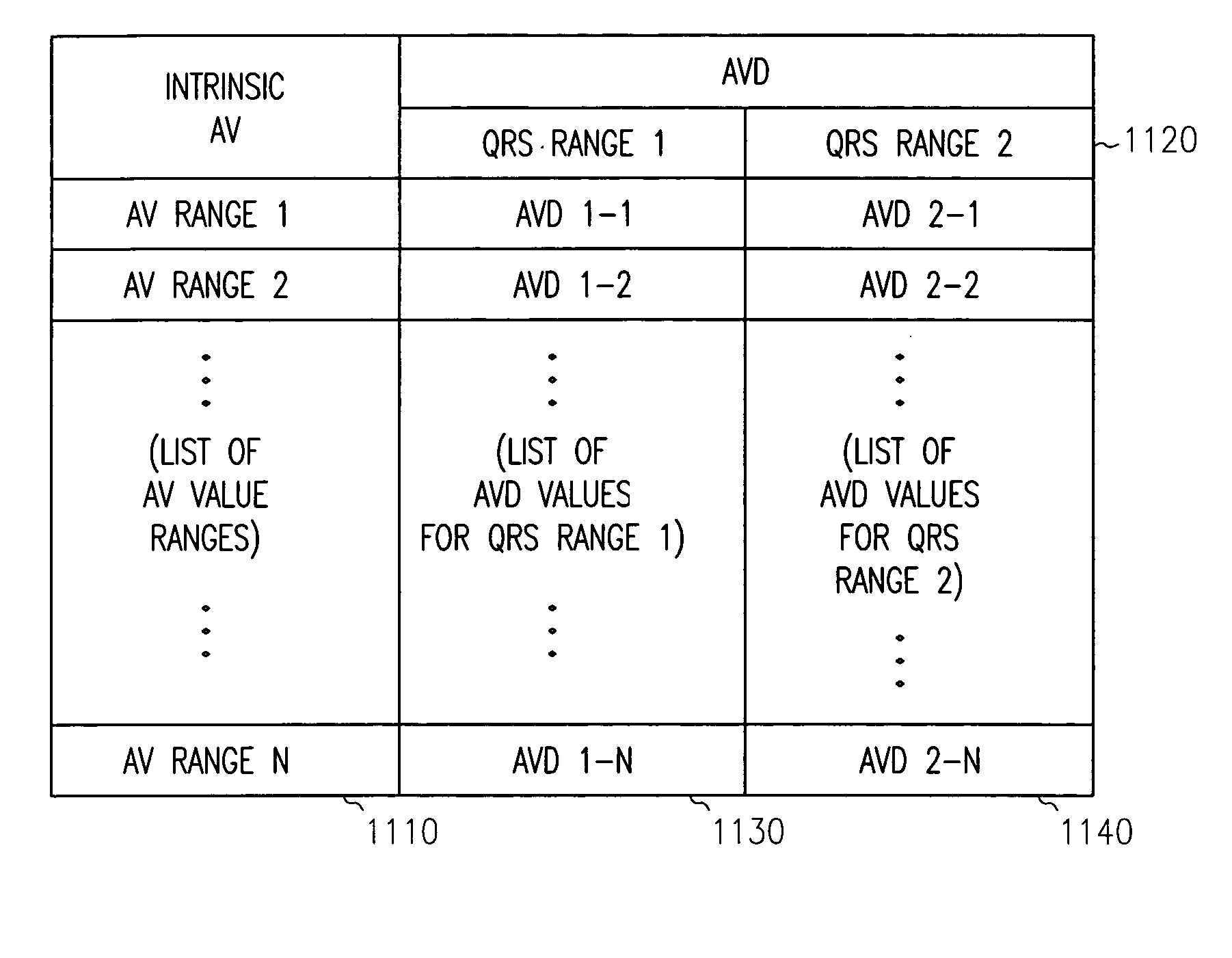
Method and apparatus for adjustable AVD programming using a table
Owner:CARDIAC PACEMAKERS INC
Non-invasive monitoring of hemodynamic parameters using impedance cardiography
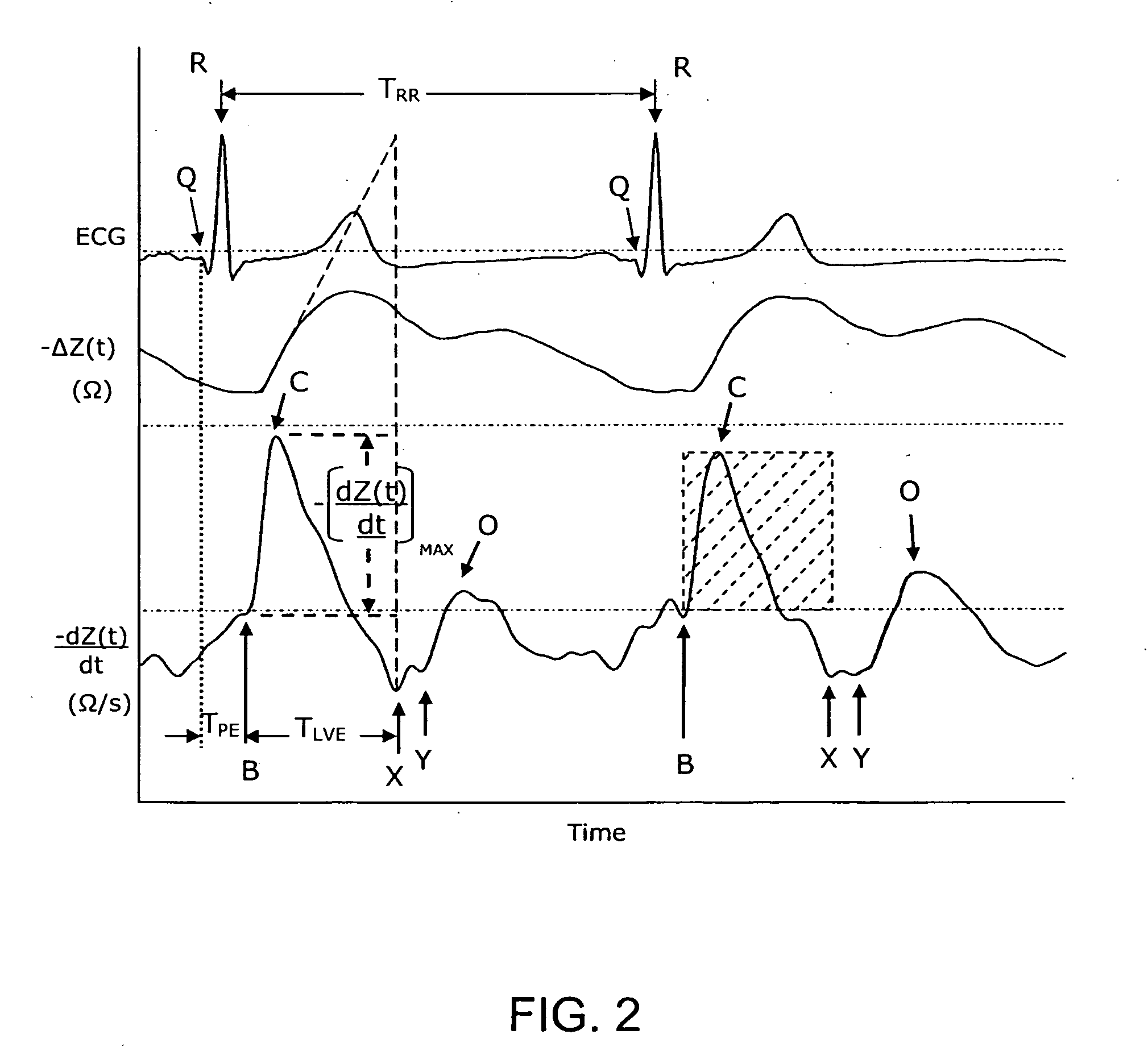
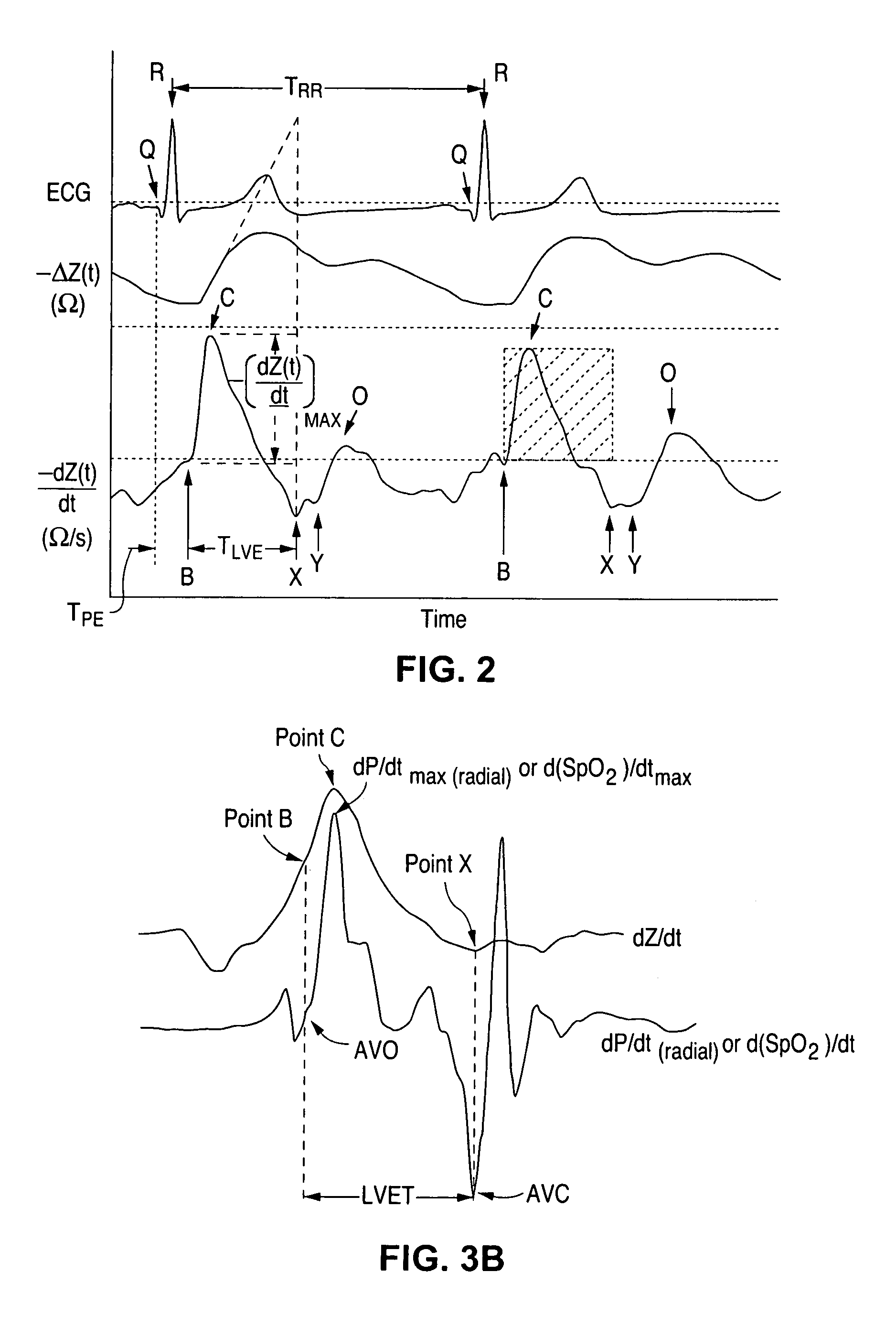
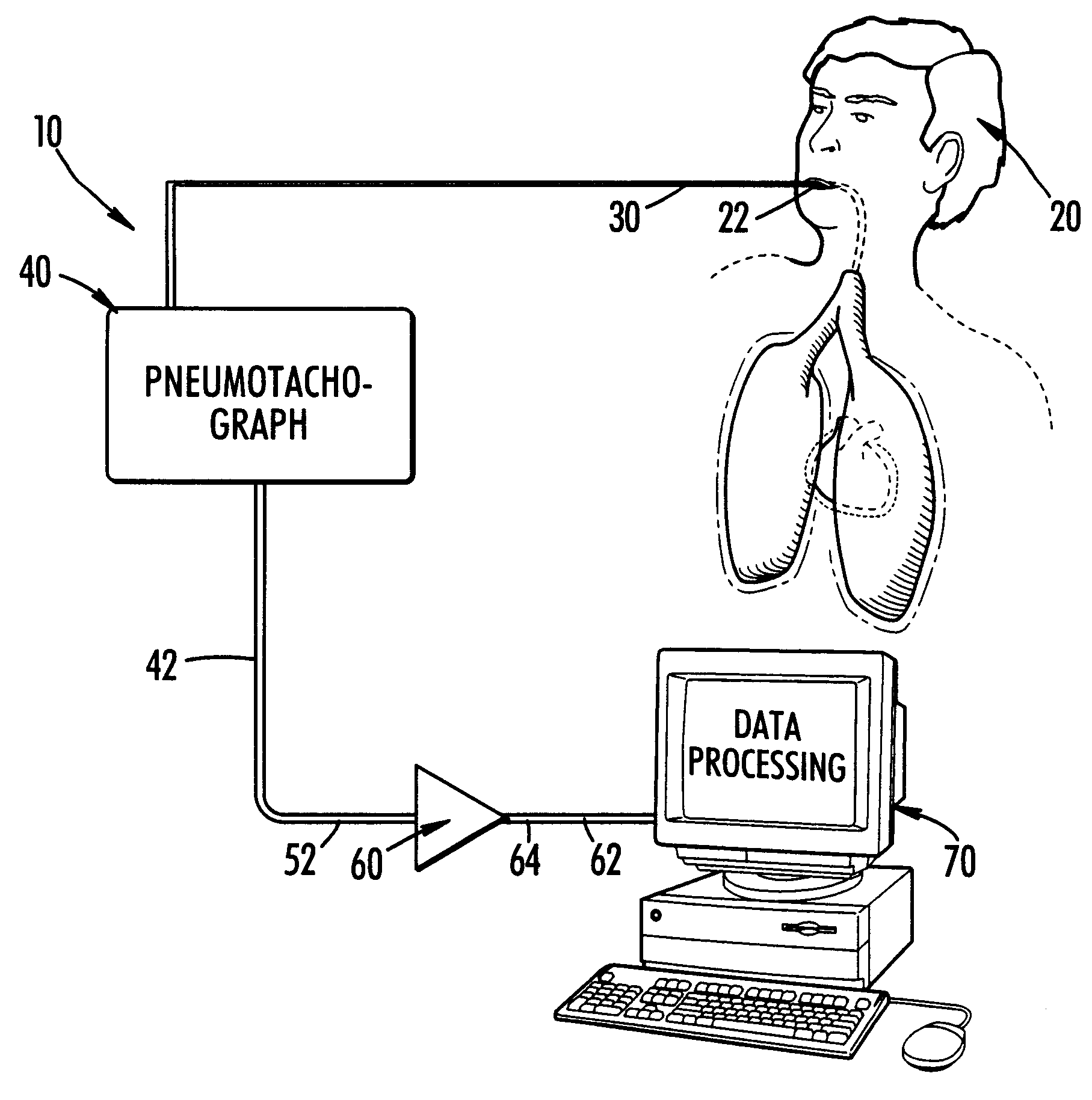
InactiveUS6161038AImprove accuracySimple processCatheterRespiratory organ evaluationLeft Ventricular Ejection TimeHarmonic
PCT No. PCT / SG97 / 00013 Sec. 371 Date Oct. 8, 1998 Sec. 102(e) Date Oct. 8, 1998 PCT Filed Apr. 7, 1997 PCT Pub. No. WO97 / 37591 PCT Pub. Date Oct. 16, 1997A method and apparatus for determination of heart rate, heart stroke volume, heart stroke volume, and cardiac output from thoracic bioimpedance signals and electrocardiograms. A unique bioimpedance electrode arrangement is employed, and the bioimpedance signals are corrected for gain-phase-frequency distortion through the use of sinusoidal test signals through the measuring or detection electrodes to identify distortions and correct for same during actual measurements. Time-derivative bioimpedance signals are employed, the power spectrum calculated, and a novel autoconvolution procedure used to emphasize the heart rate harmonic. Breath waves and other signals not indicative of the patient's cardiocycles are removed. Left ventricular ejection time is derived from the bioimpedance signals, and an improved version of Kubicek's equation is employed to derive heart stroke volume and thus cardiac output.
Owner:RHEO GRAPHIC PTE
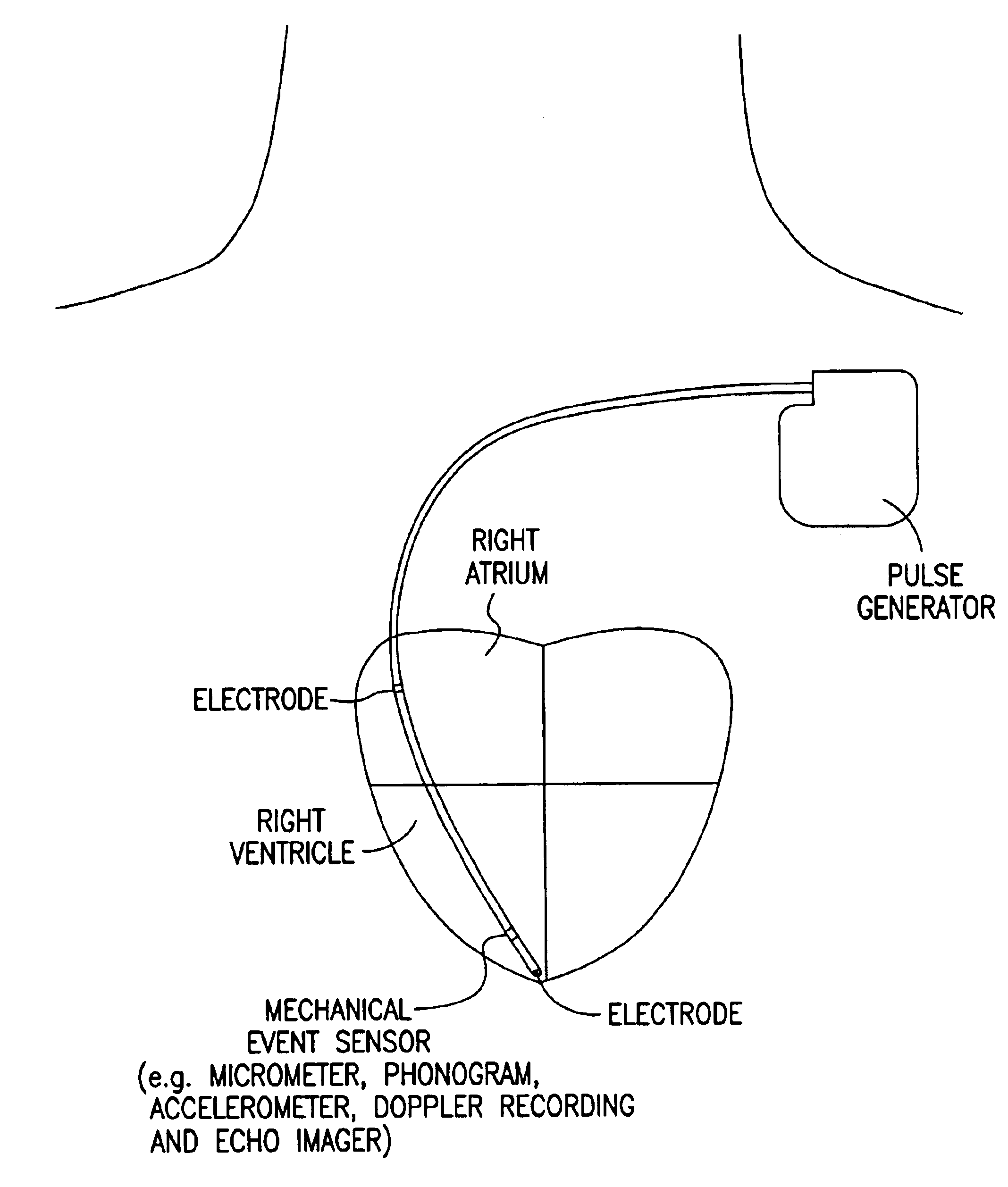
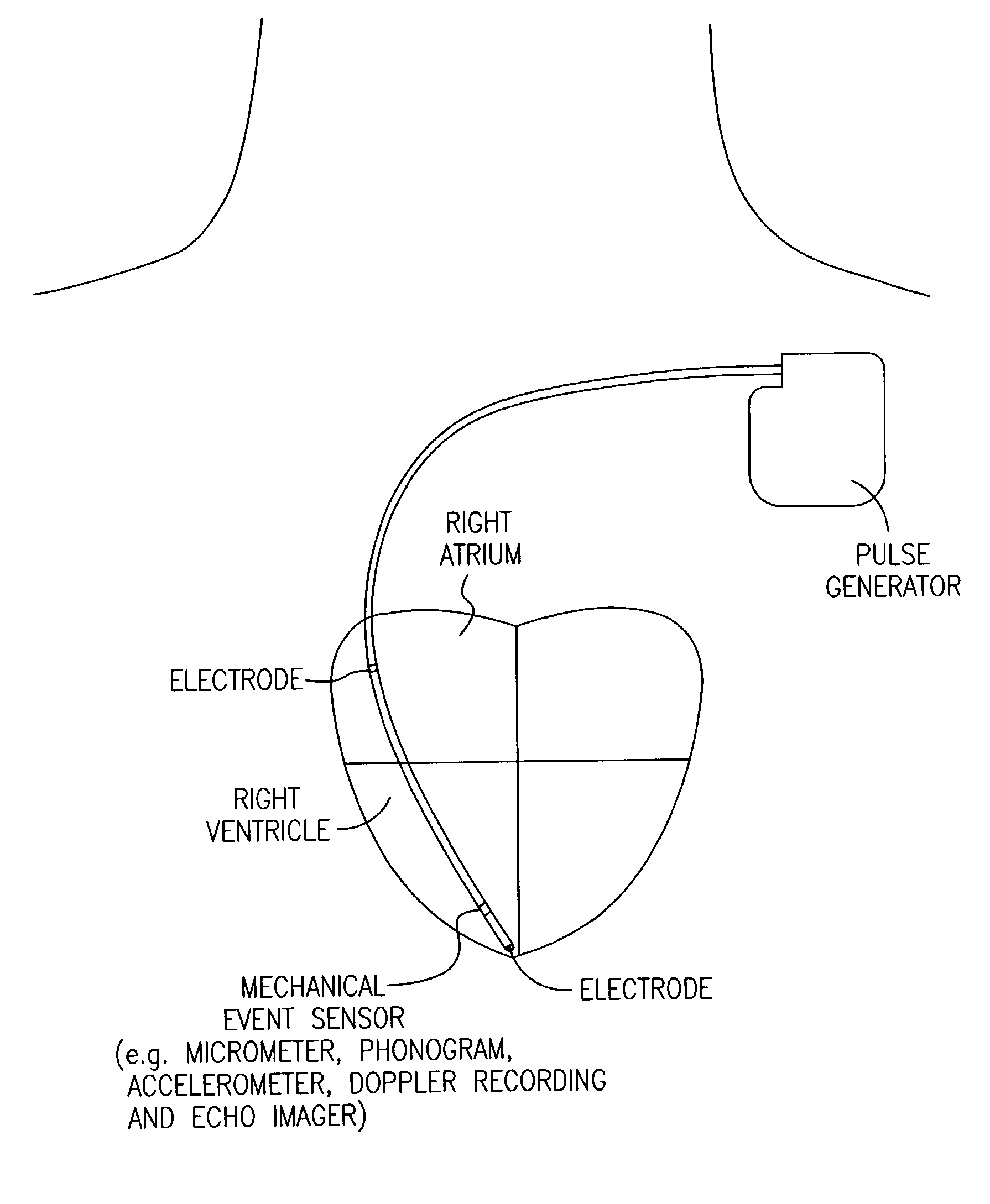
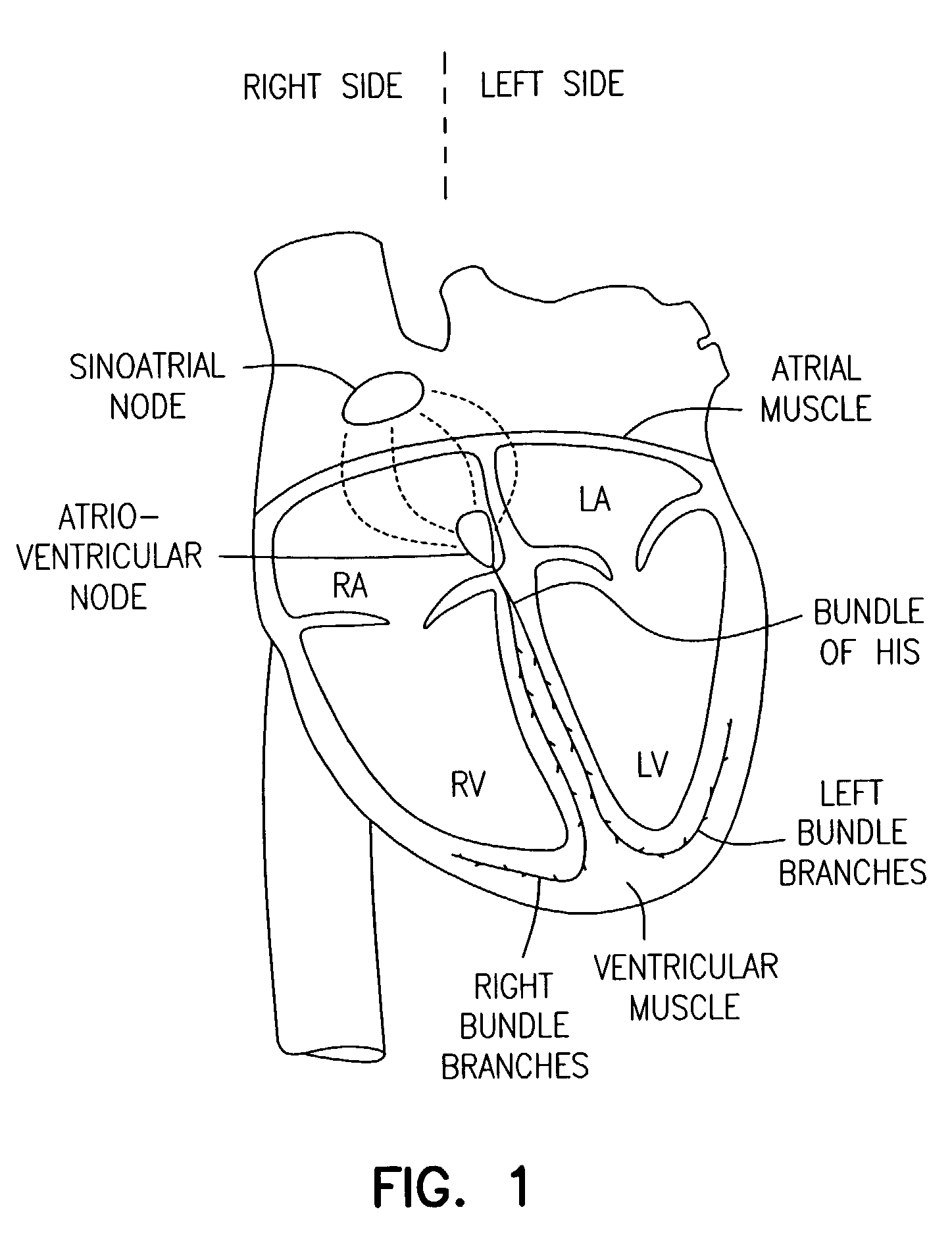
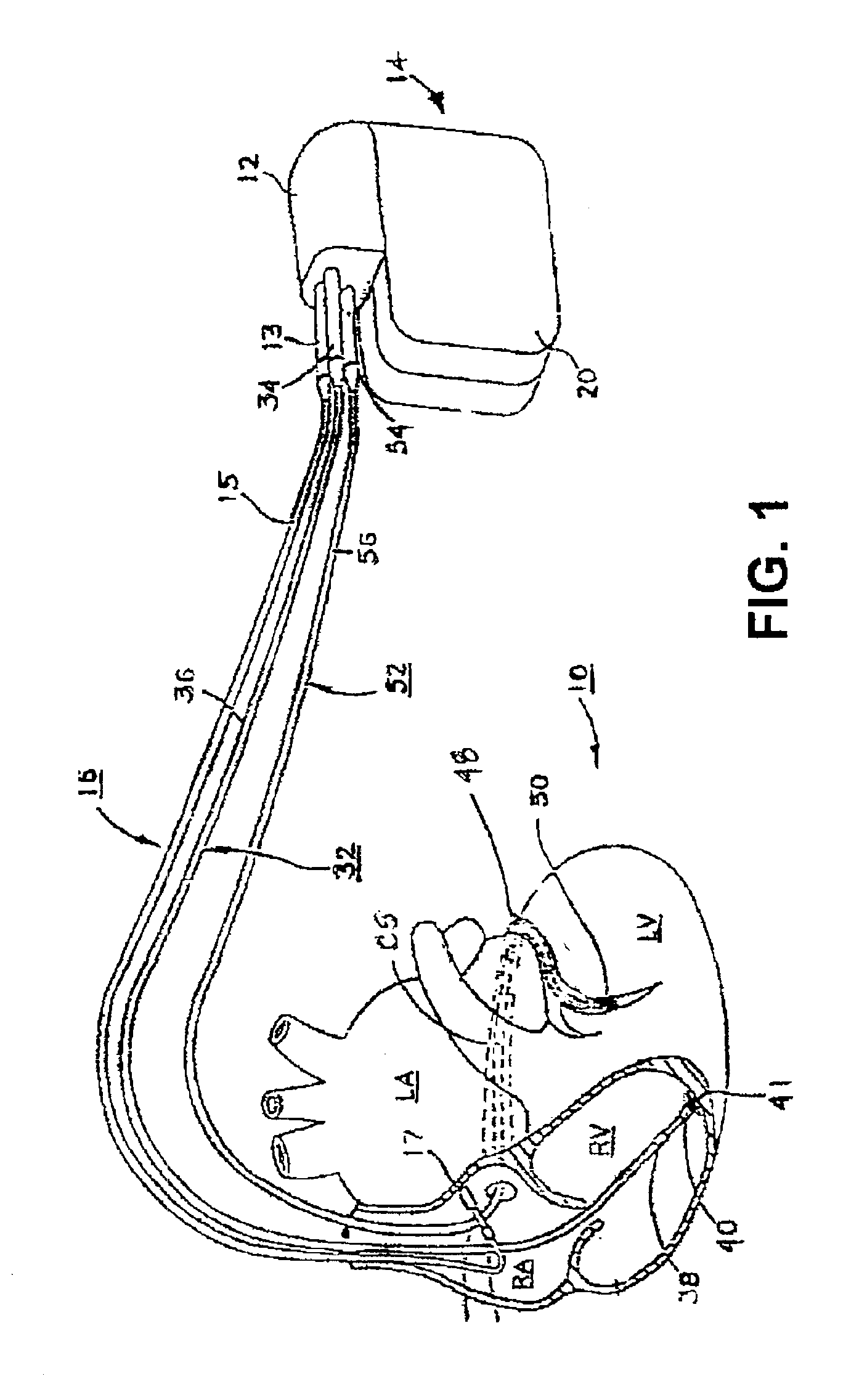
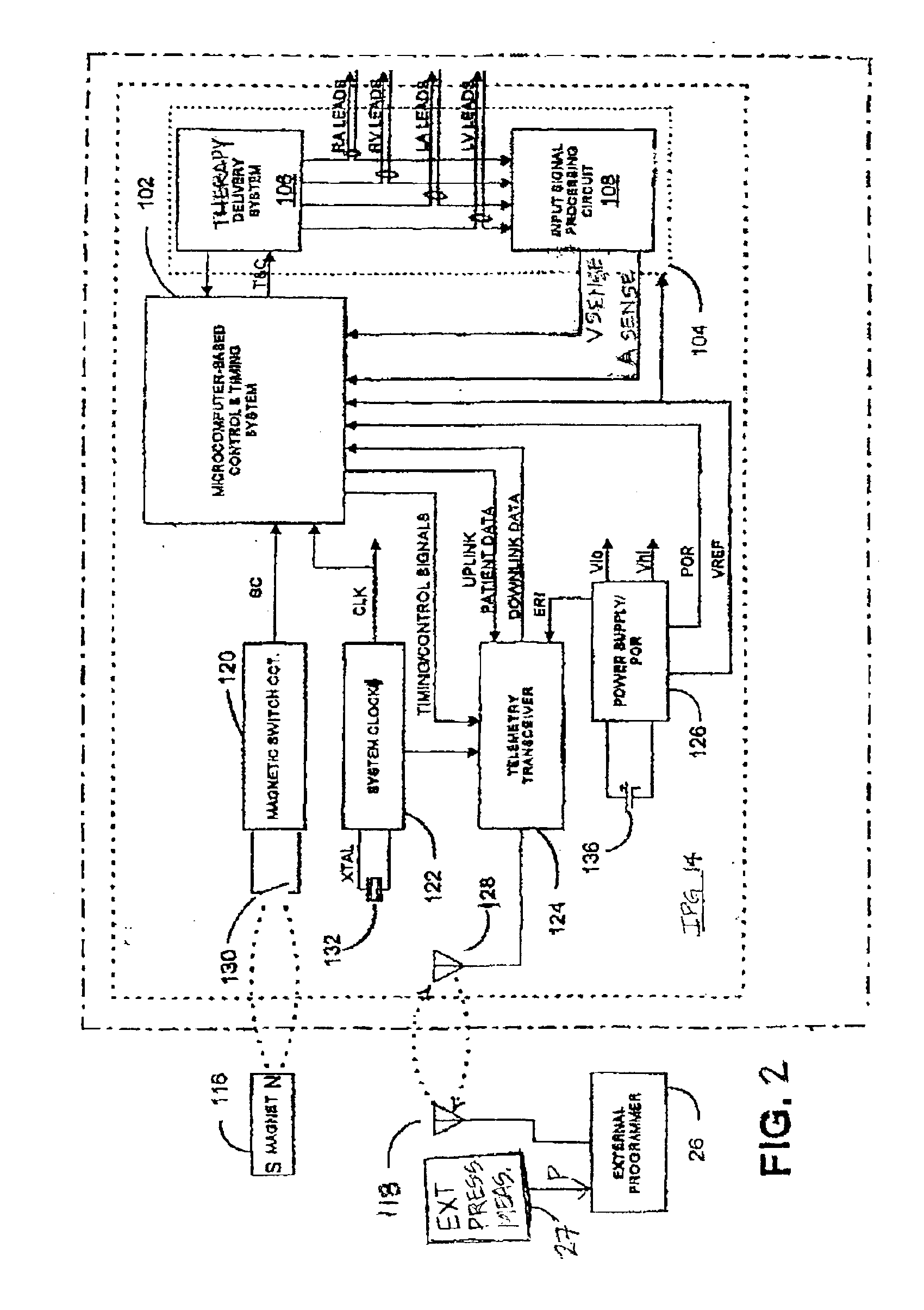
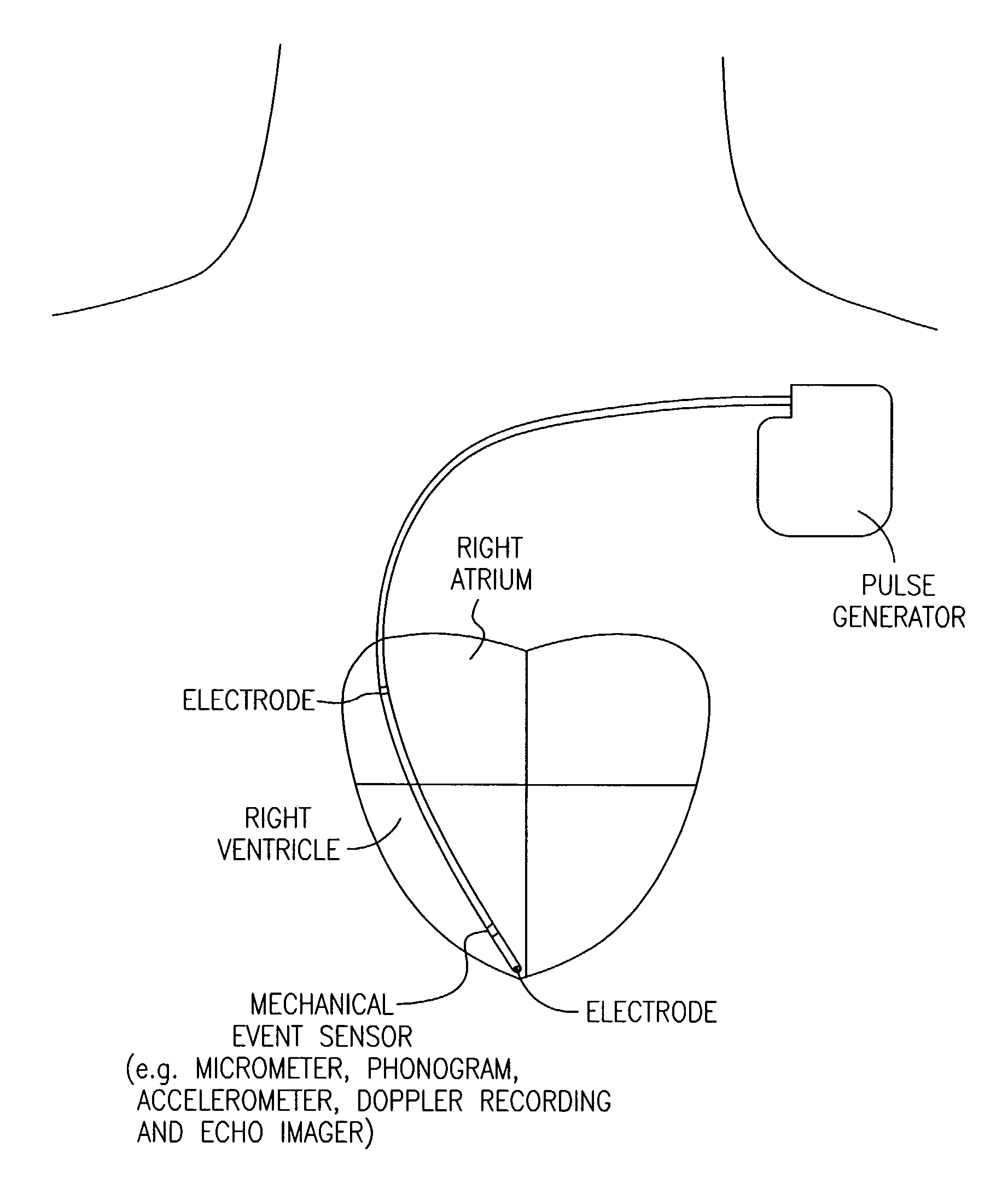
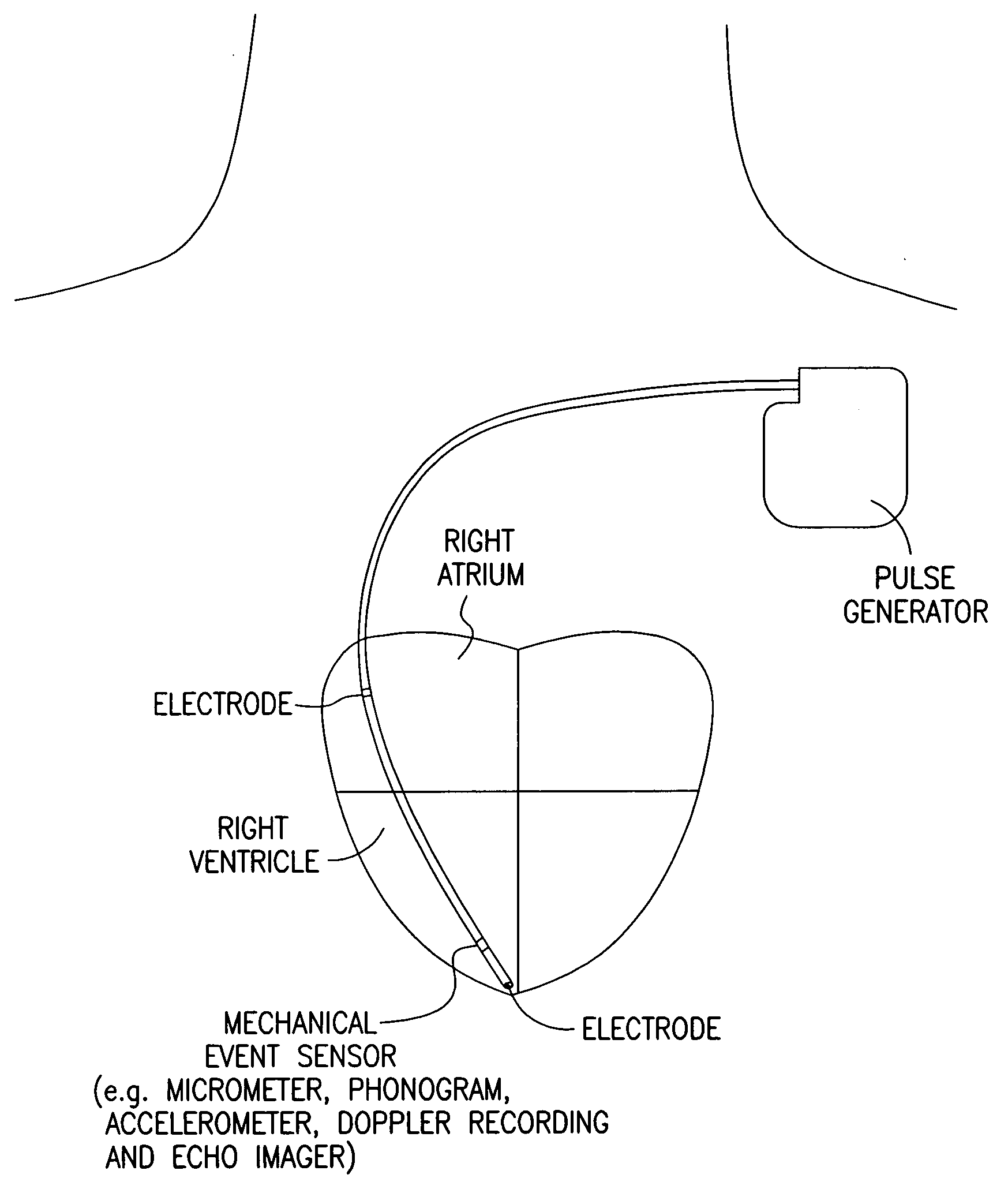
Cardiac pacing using adjustable atrio-ventricular delays
A pacing system for providing optimal hemodynamic cardiac function for parameters such as contractility (peak left ventricle pressure change during systole or LV+dp / dt), or stroke volume (aortic pulse pressure) using system for calculating atrio-ventricular delays for optimal timing of a ventricular pacing pulse. The system providing an option for near optimal pacing of multiple hemodynamic parameters. The system deriving the proper timing using electrical or mechanical events having a predictable relationship with an optimal ventricular pacing timing signal.
Owner:CARDIAC PACEMAKERS INC
Shape memory devices and methods for reshaping heart anatomy
InactiveUS7285087B2Improve shrinkageReduce widthSuture equipmentsSurgical needlesCardiac surfaceHeart Part
Owner:MICARDIA CORP
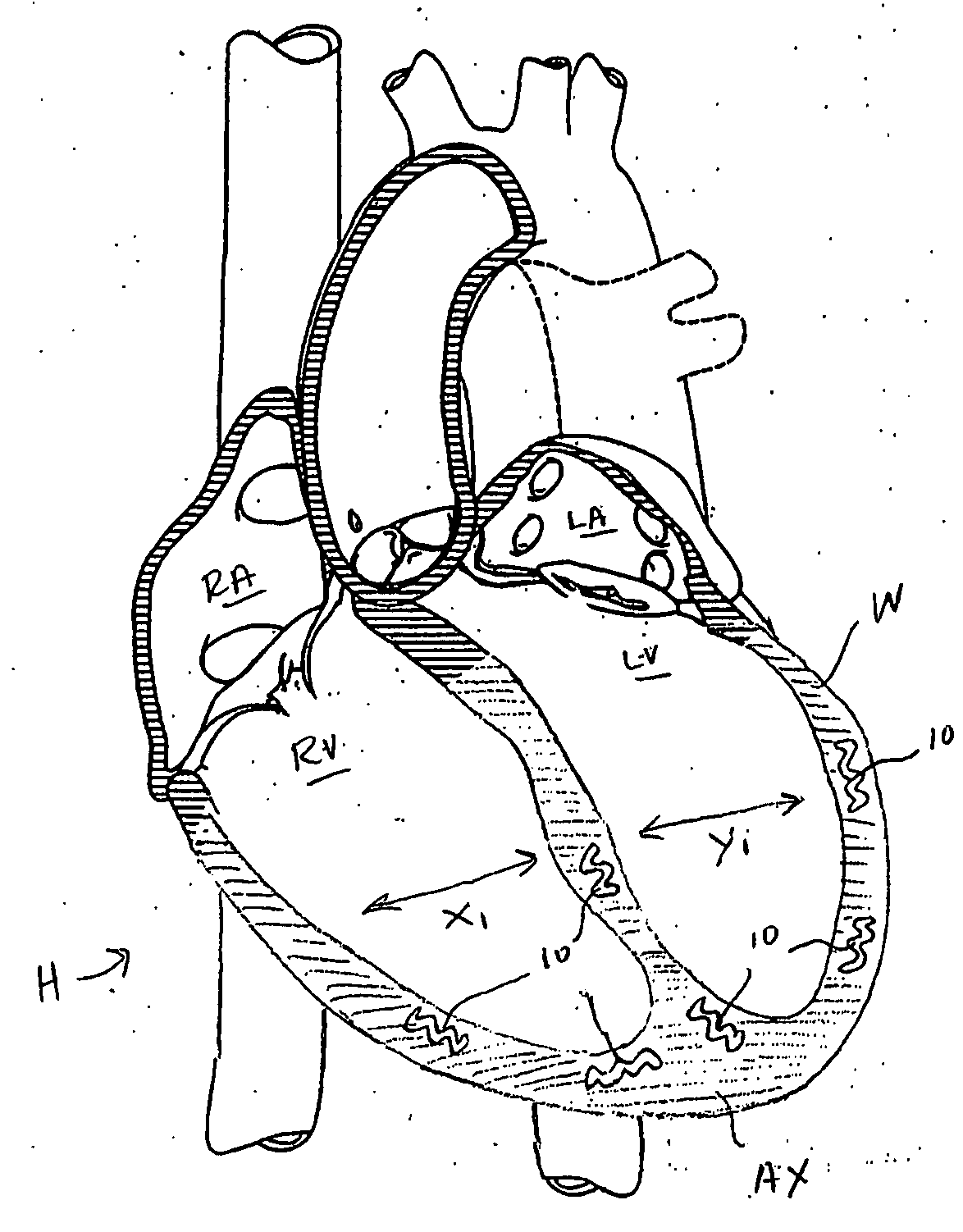
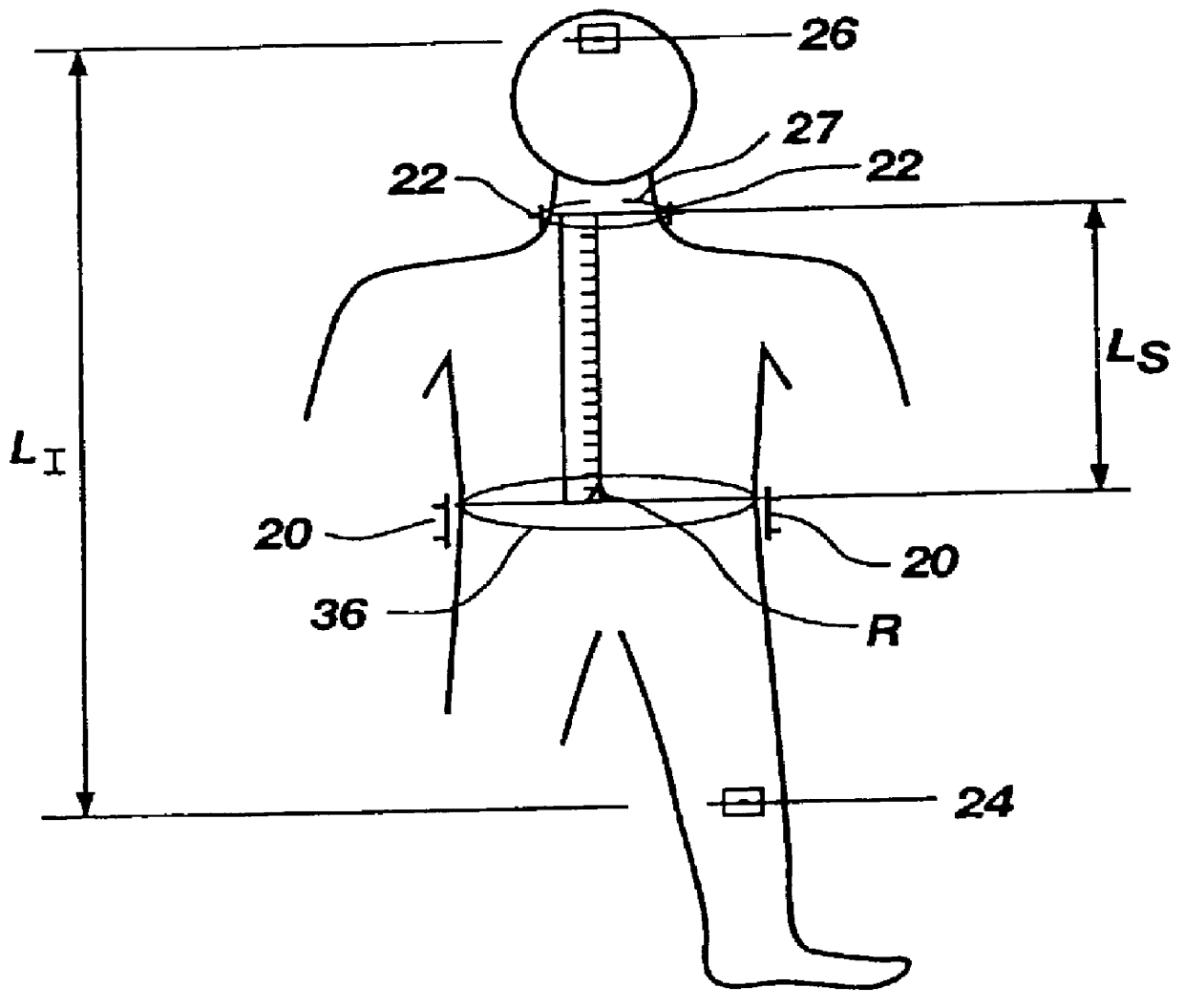
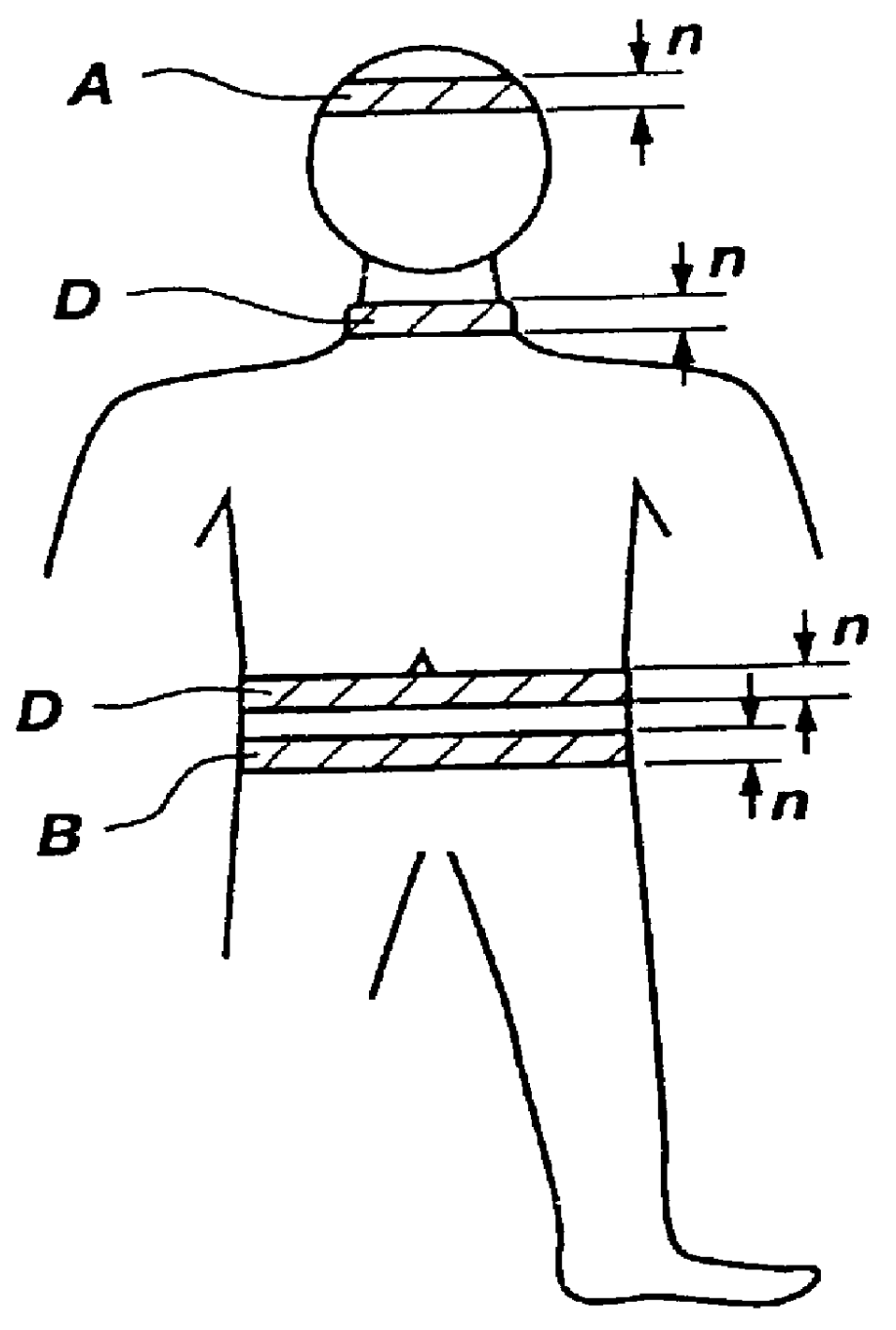
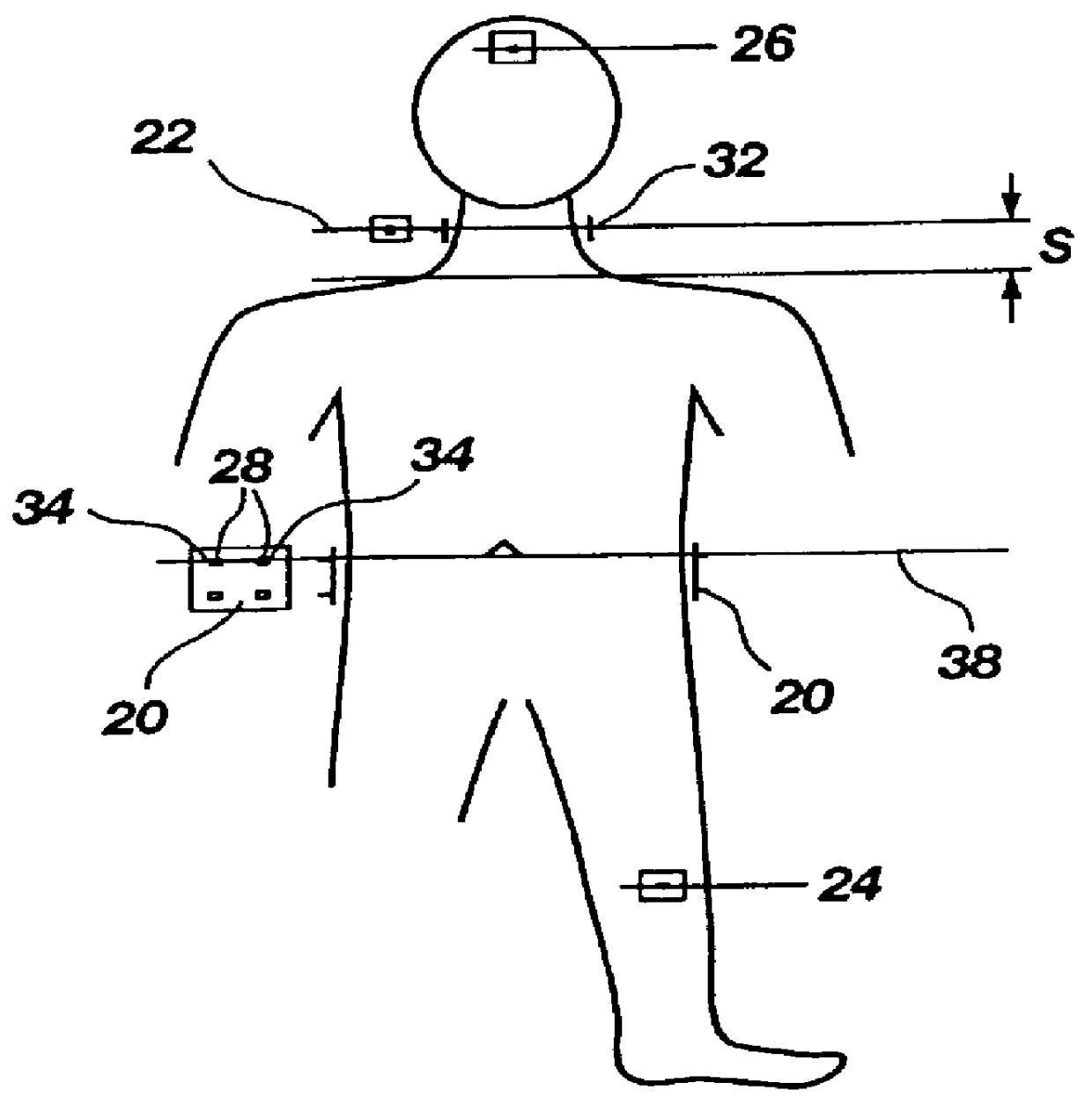
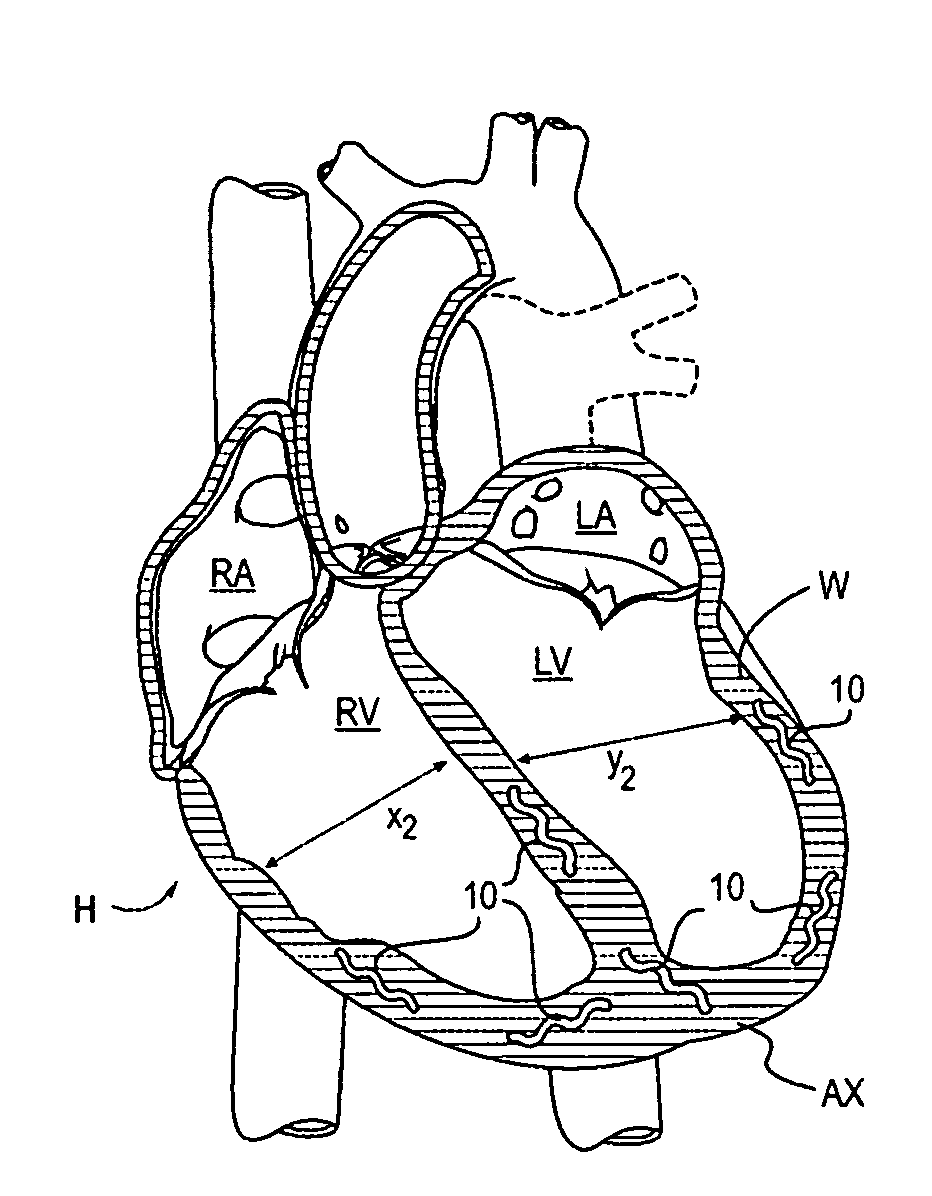
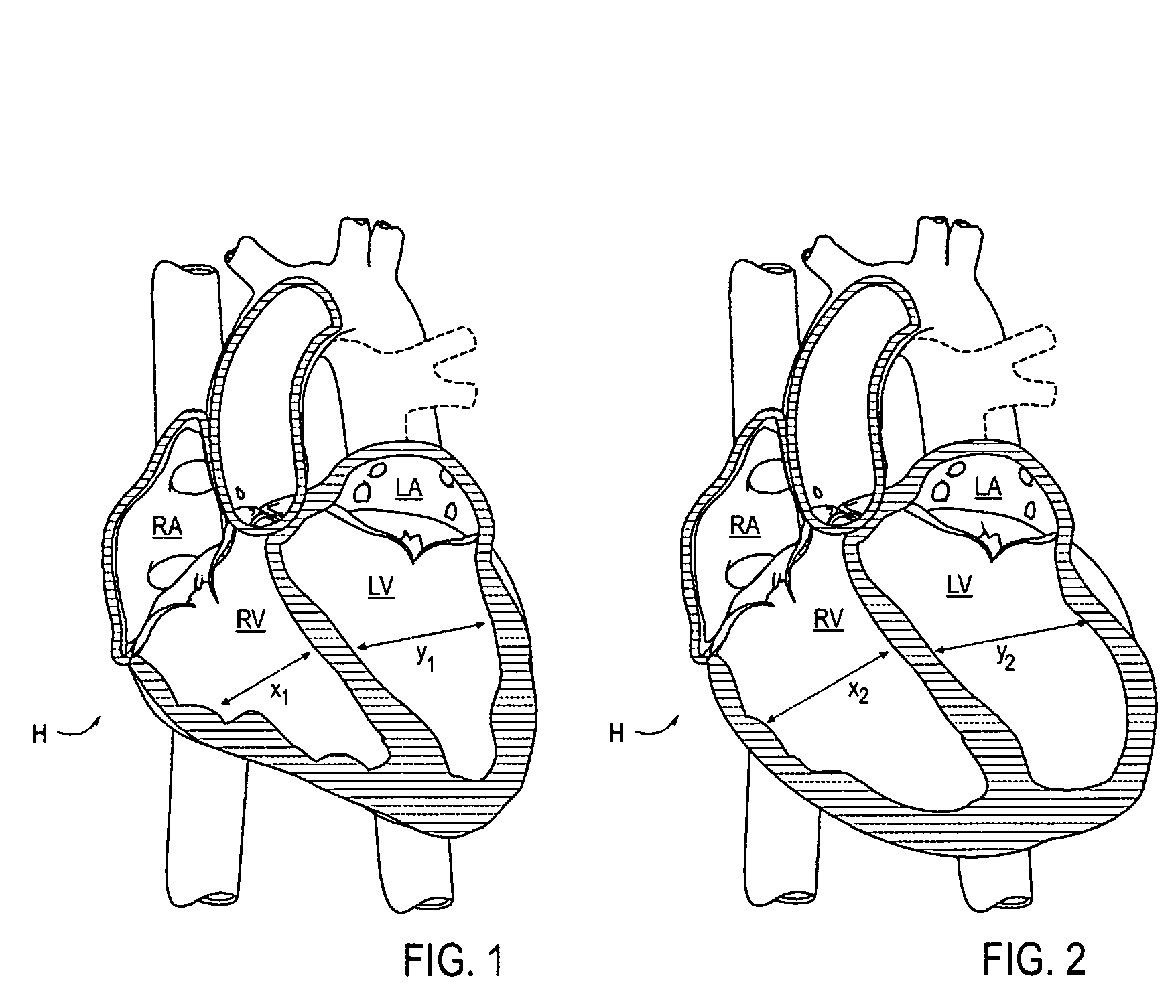
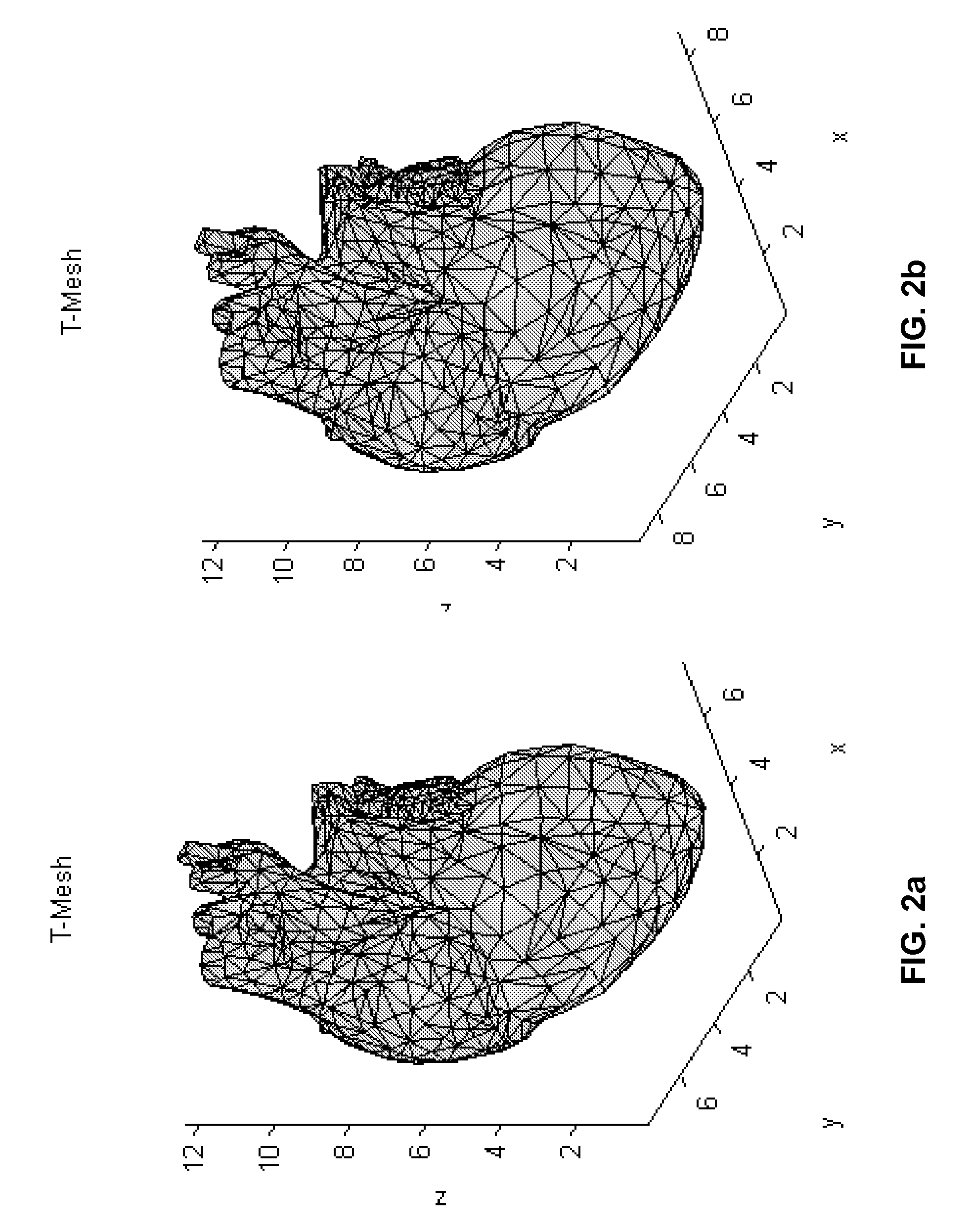
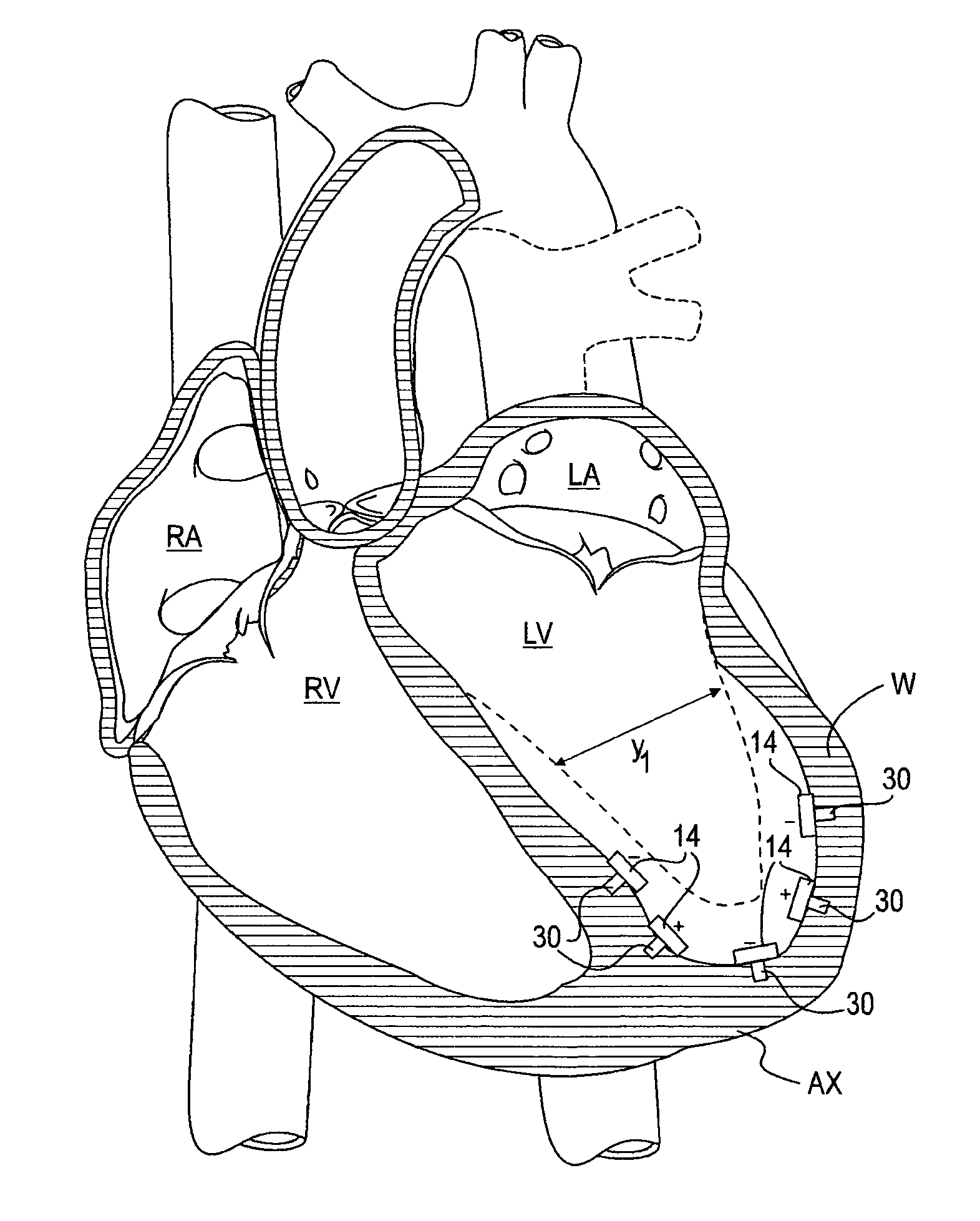
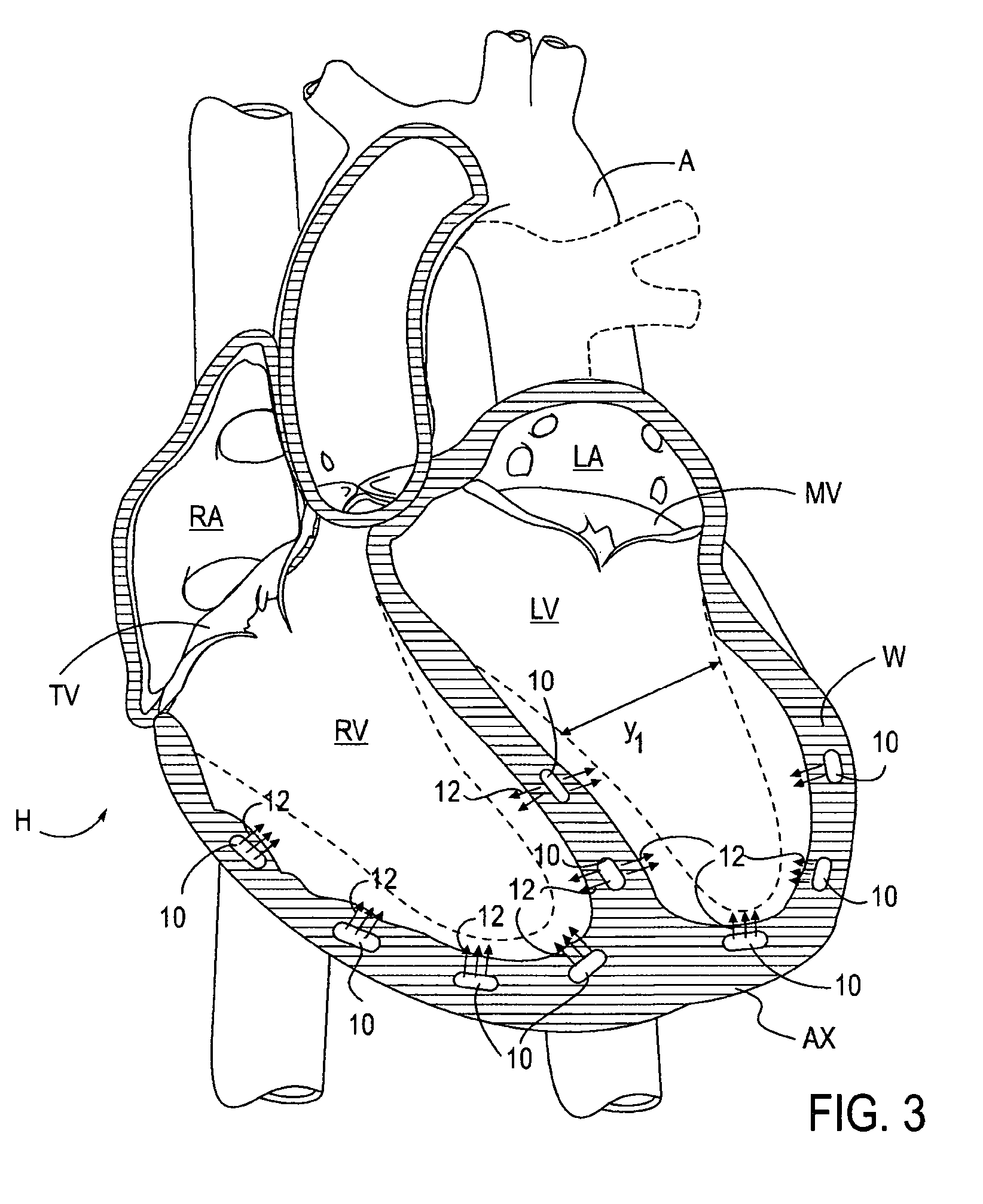
Determining the volume of a normal heart and its pathological and treated variants by using dimension sensors
InactiveUS20040106871A1Improve accuracyReduce in quantityUltrasonic/sonic/infrasonic diagnosticsCatheterVentricular volumeCardiac surface
A method and system measure the instantaneous volume of blood contained within a chamber of a heart, irrespective of its shape, whereby stroke volume and cardiac output volume can be continuously monitored and feedback to a non-blood contacting cardiac assist device. In a preferred form the device uses the distances between the sensors which are implanted in a biomaterial that integrates with a heart surface to determine changes in heart volume. Sonomicrometry crystal measurements are disclosed as a preferred mode of obtaining distance readings. A computer readable medium carries instructions to convert data from dimension sensors into sensor positions within a predetermined coordinate system. Ventricular volume is based on the sensor positions.
Owner:HEART ASSIST TECH PTY LTD
Method and apparatus for optimizing stroke volume during DDD resynchronization therapy using adjustable atrio-ventricular delays
InactiveUS7158830B2Convenient timeMaximizes ventricular performanceHeart stimulatorsSystoleHemodynamics
A pacing system for providing optimal hemodynamic cardiac function for parameters such as ventricular synchorny or contractility (peak left ventricle pressure change during systole or LV+dp / dt), or stroke volume (aortic pulse pressure) using system for calculating atrio-ventricular delays for optimal timing of a ventricular pacing pulse. The system providing an option for near optimal pacing of multiple hemodynamic parameters. The system deriving the proper timing using electrical or mechanical events having a predictable relationship with an optimal ventricular pacing timing signal.
Owner:CARDIAC PACEMAKERS INC
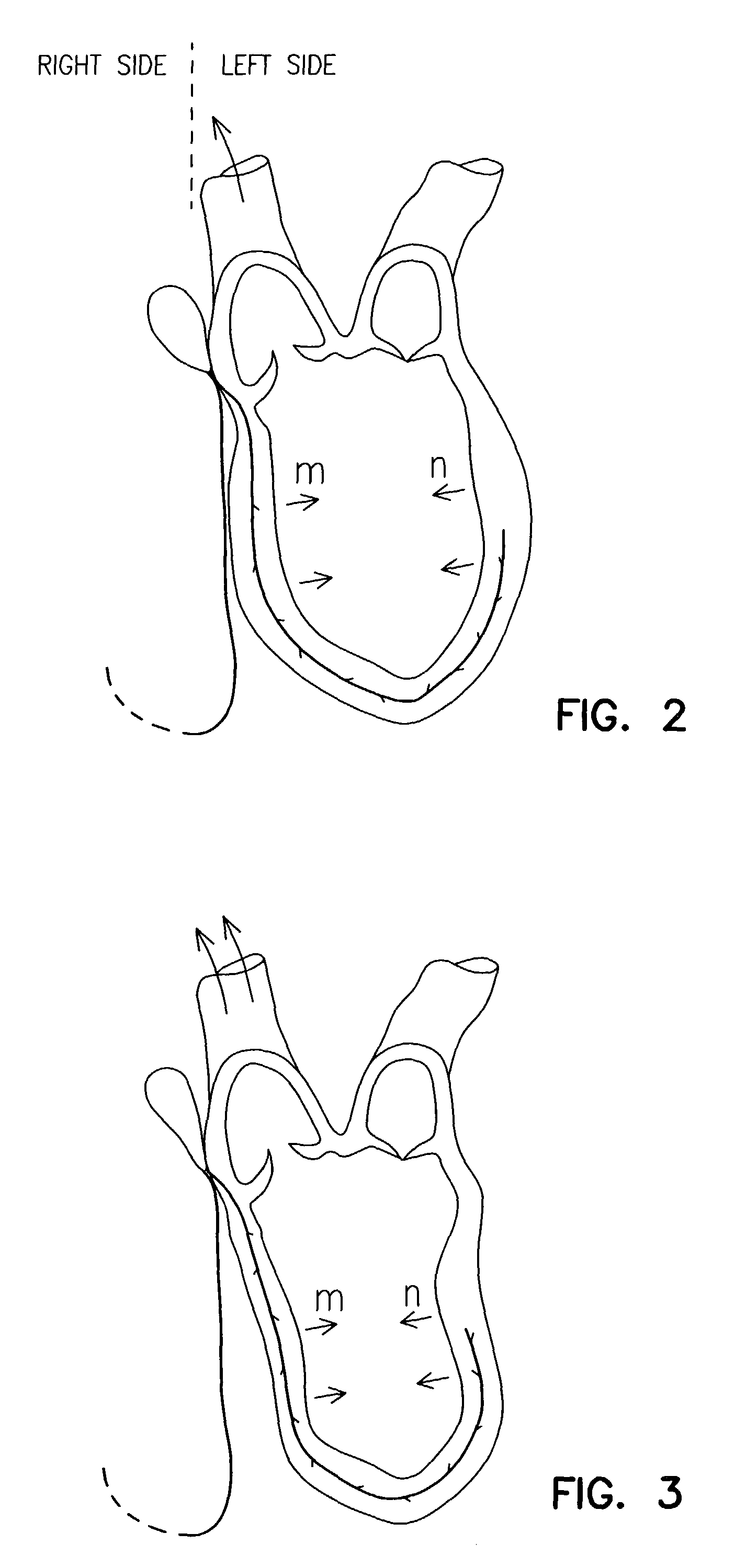
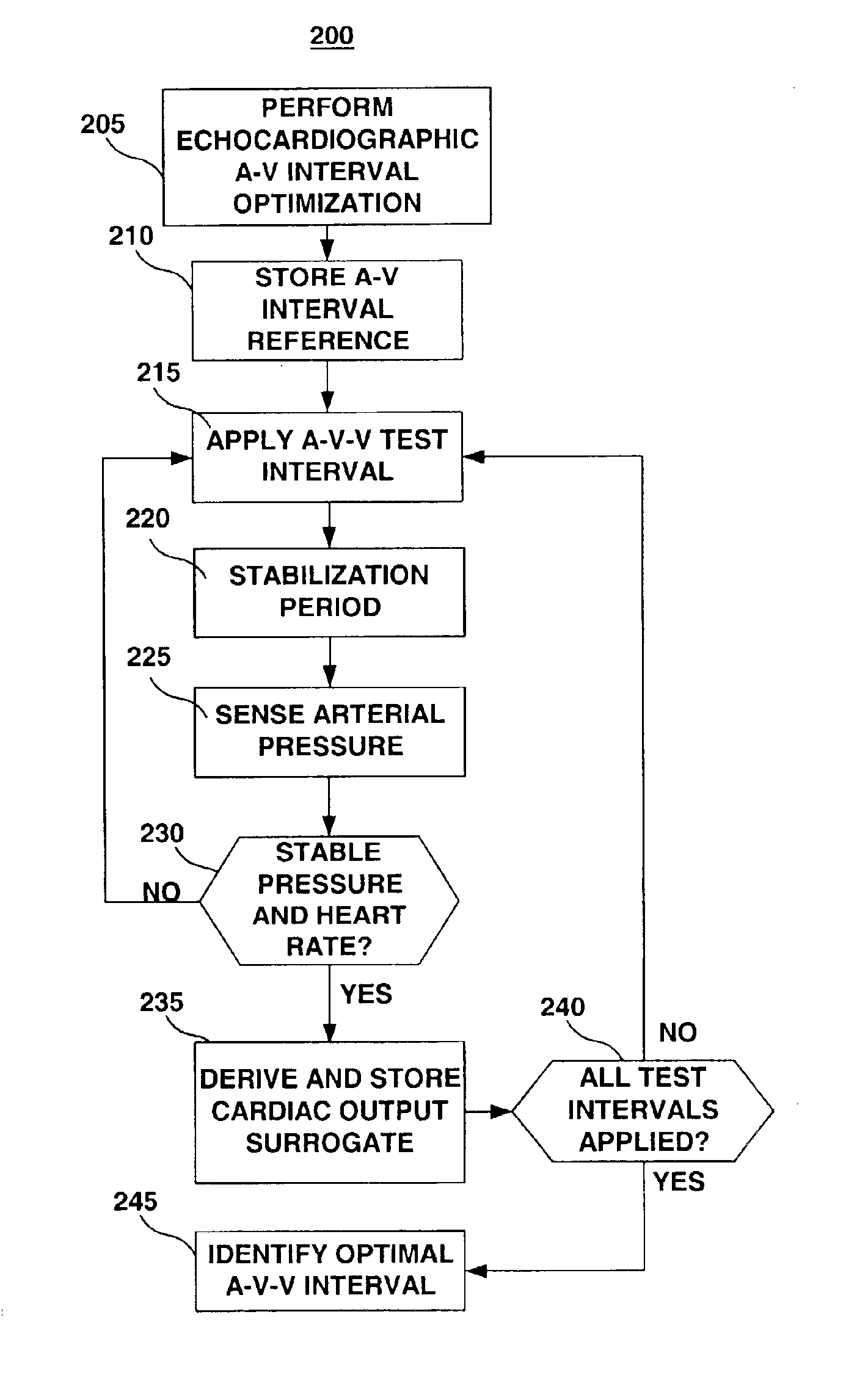
Method and apparatus for optimizing cardiac resynchronization therapy
InactiveUS6871088B2Shorten the timeLower requirementCatheterHeart stimulatorsBlood flowBlood pressure
A method and apparatus for optimizing cardiac resynchronization therapy are provided. An iterative optimization procedure is performed to test the systolic hemodynamic effects of varying A-V-V timing schemes. The hemodynamic effect is assessed based on a surrogate of stroke volume. The stroke volume surrogate is derived from a sensor signal proportional to the blood pressure in the aorta or a major artery. The A-V-V timing scheme corresponding to the greatest stroke volume, as indicated by the stroke volume surrogate, is identified and automatically programmed to maintain optimal A-V-V settings acutely and chronically.
Owner:MEDTRONIC INC
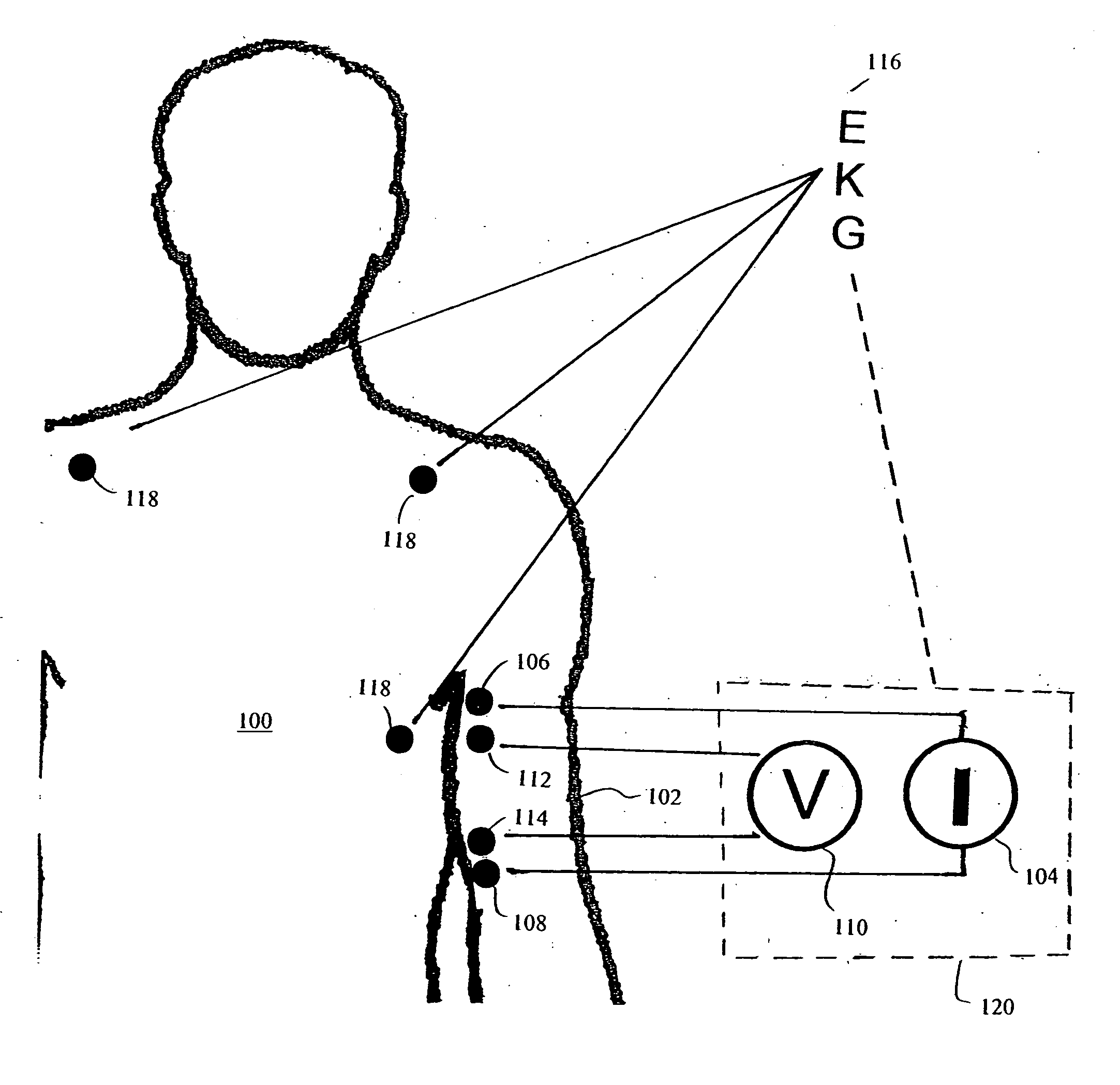
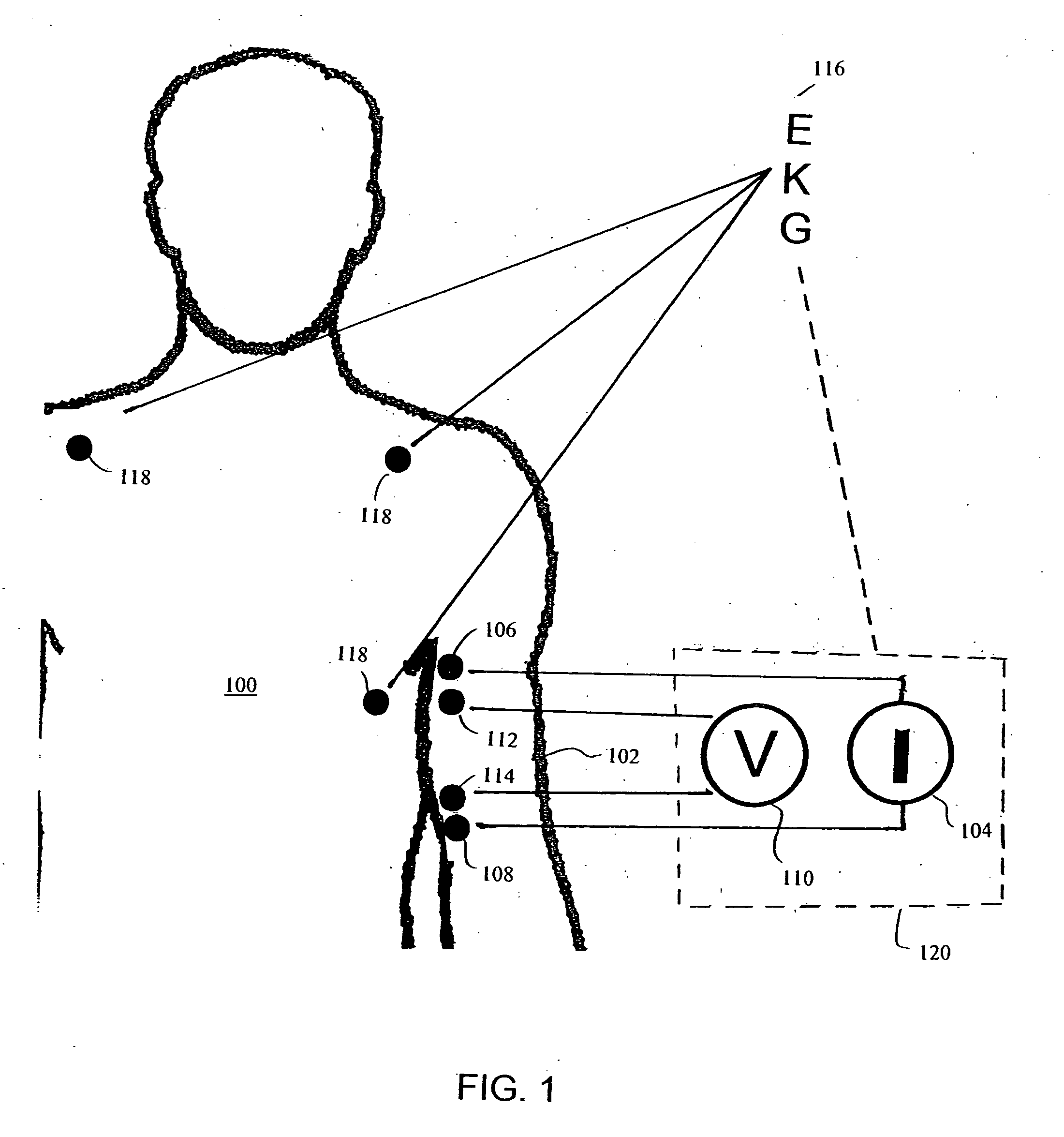
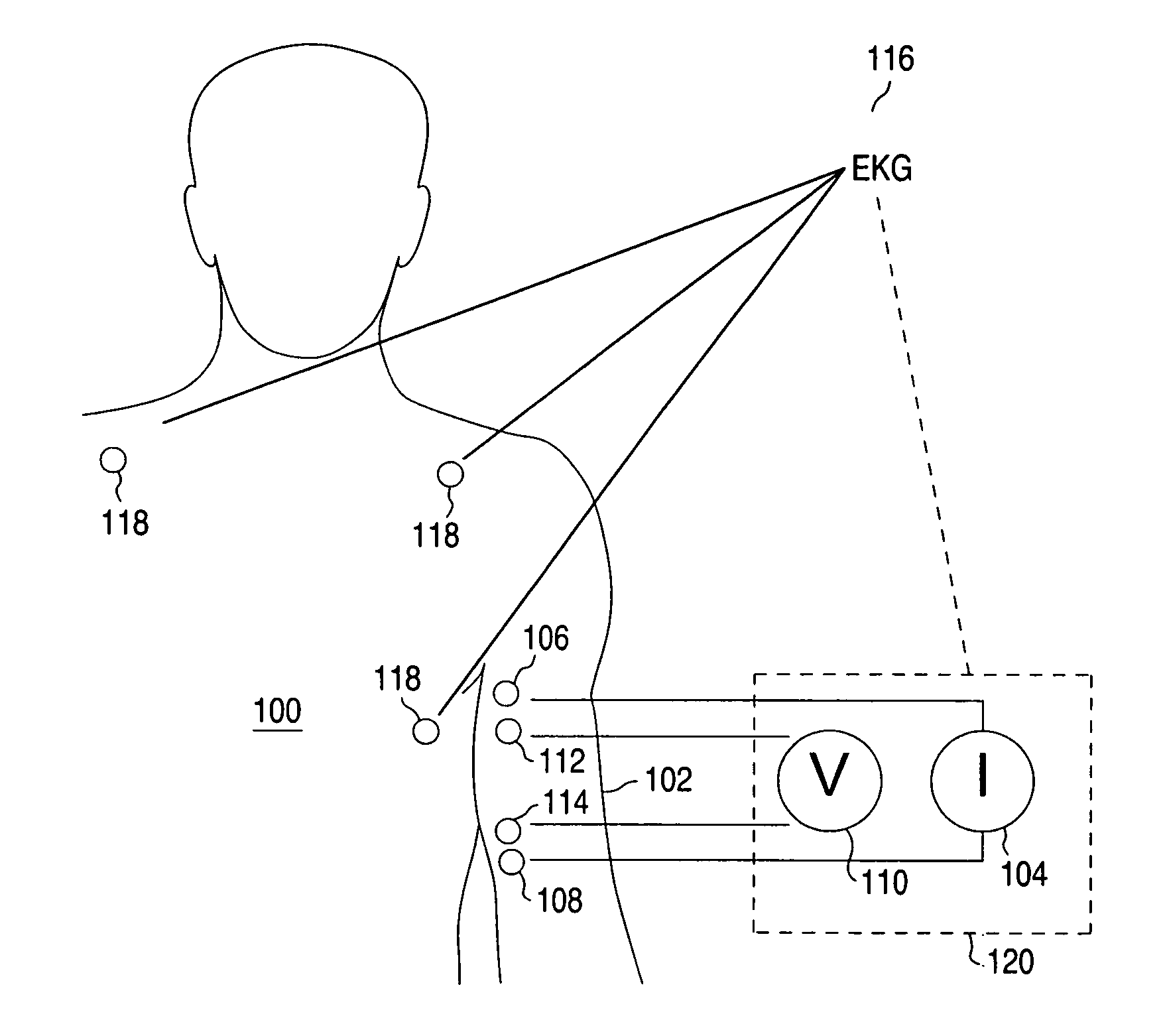
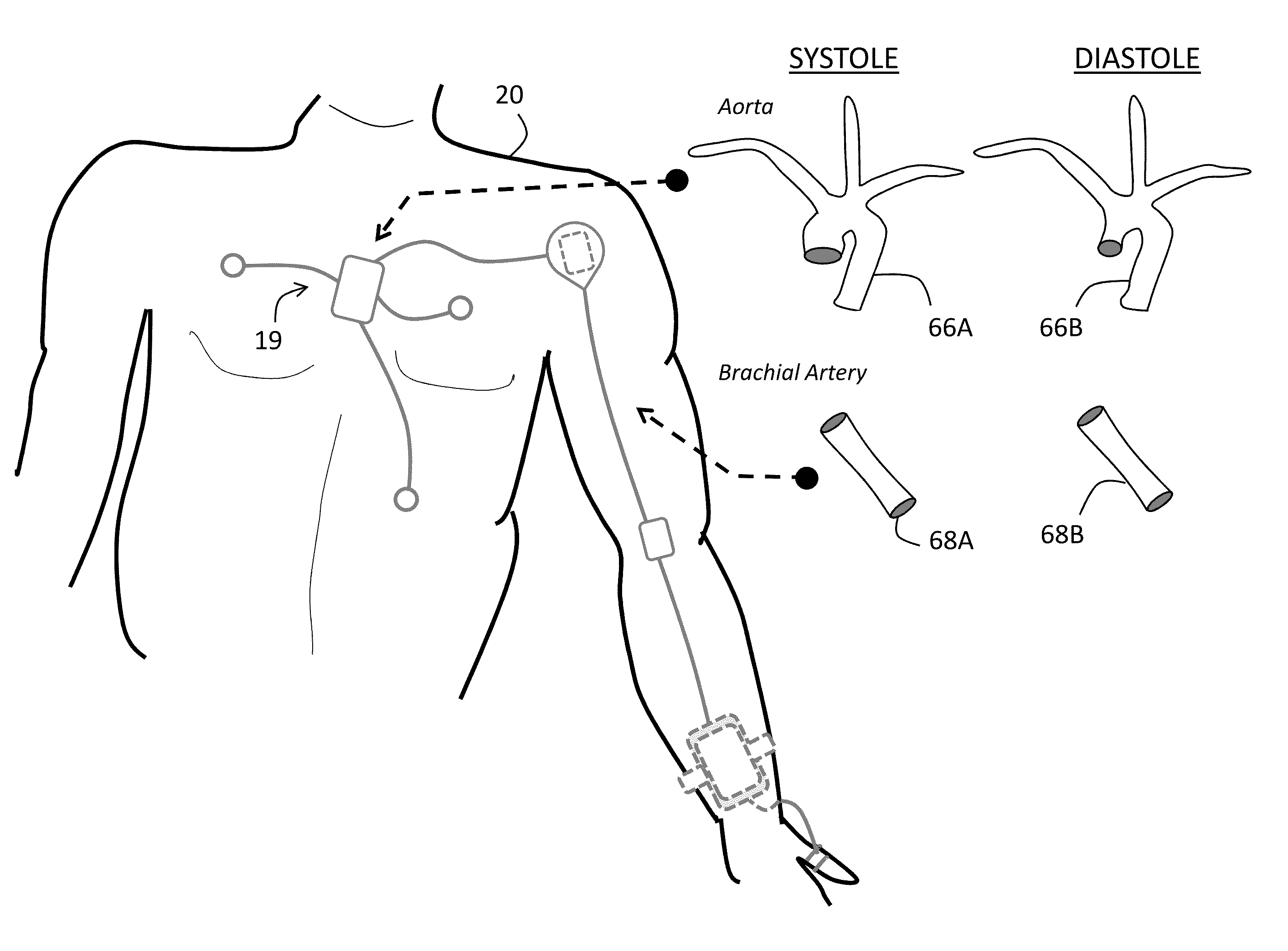
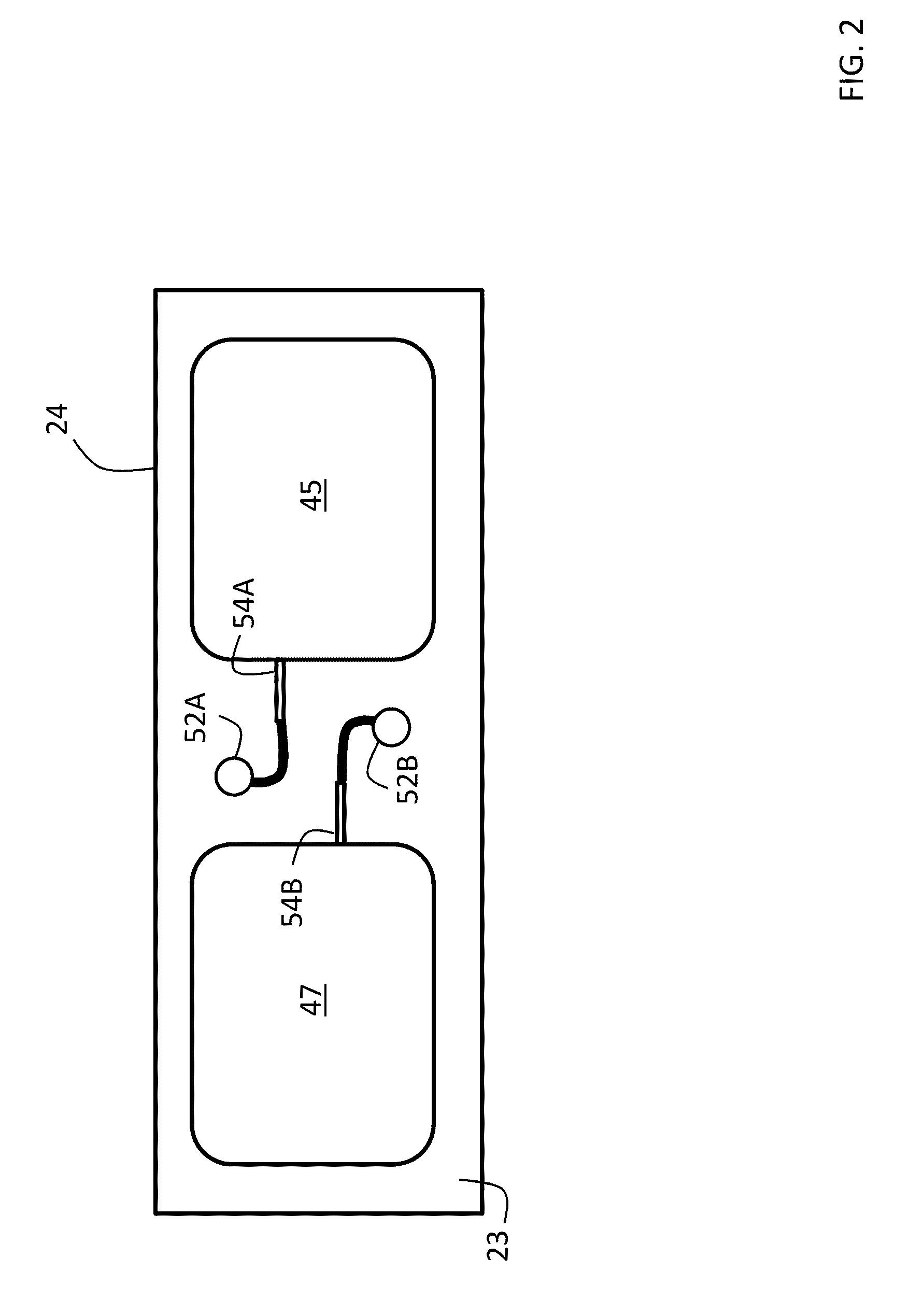
Apparatus and method for determination of stroke volume using the brachial artery
Provided herein are methods and apparatus for stroke volume determination by bioimpedance from a patient's upper arm, or brachium, utilizing pulsations of the brachial artery contained therein. The apparatus includes two or more spaced apart alternating current flow electrodes positioned on the patient's arm proximate the brachial artery and two or more spaced apart voltage sensing electrodes positioned on the patient's arm proximate the brachial artery. The voltage sensing electrodes are positioned between the alternating current flow electrodes on the arm. An alternating current source is electrically connected to the alternating current flow electrodes and a voltmeter electrically is connected to the voltage sensing electrodes. A data input device is provided along with a processing unit in communication with the data input device, the alternating current source, alternating current flow electrodes, the voltmeter, and voltage sensing electrodes. The processing unit is capable of using data from the data input device and voltage sensing electrodes to calculate the stroke volume of the patient.
Owner:BERSTEIN DONALD P
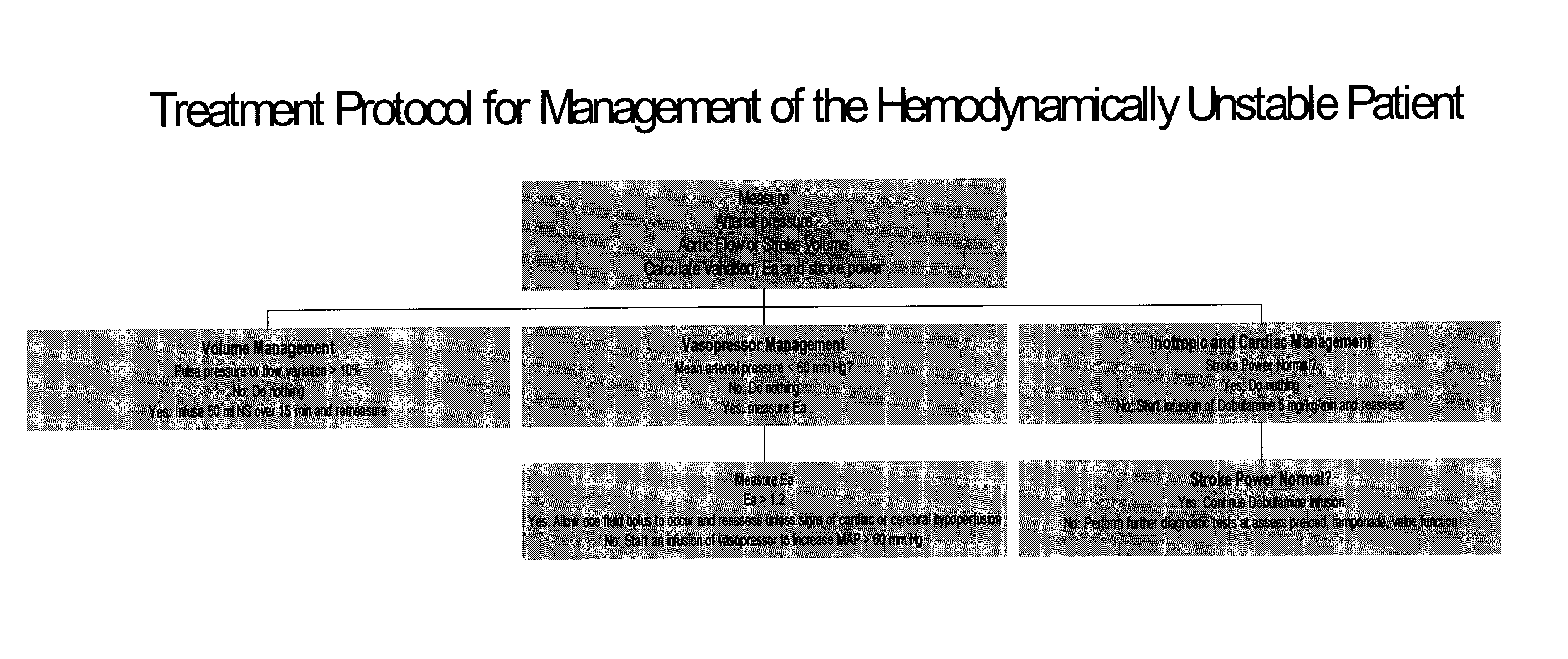
Use of aortic pulse pressure and flow in bedside hemodynamic management
InactiveUS6776764B2Evaluation of blood vesselsCatheterCritically illDecreased mean arterial pressure
Owner:UNIVERSITY OF PITTSBURGH
System and method for non-invasive instantaneous and continuous measurement of cardiac chamber volume.
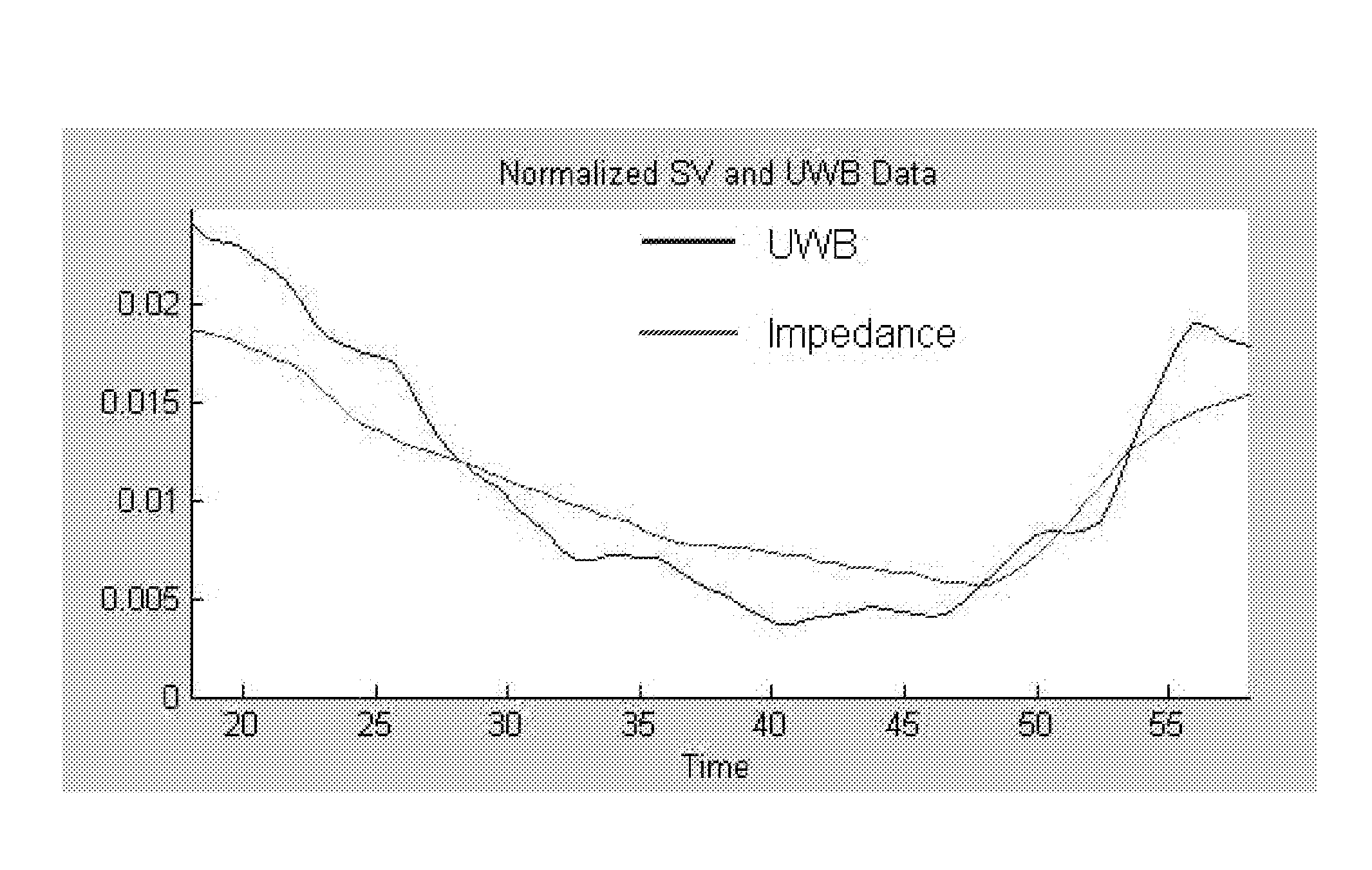
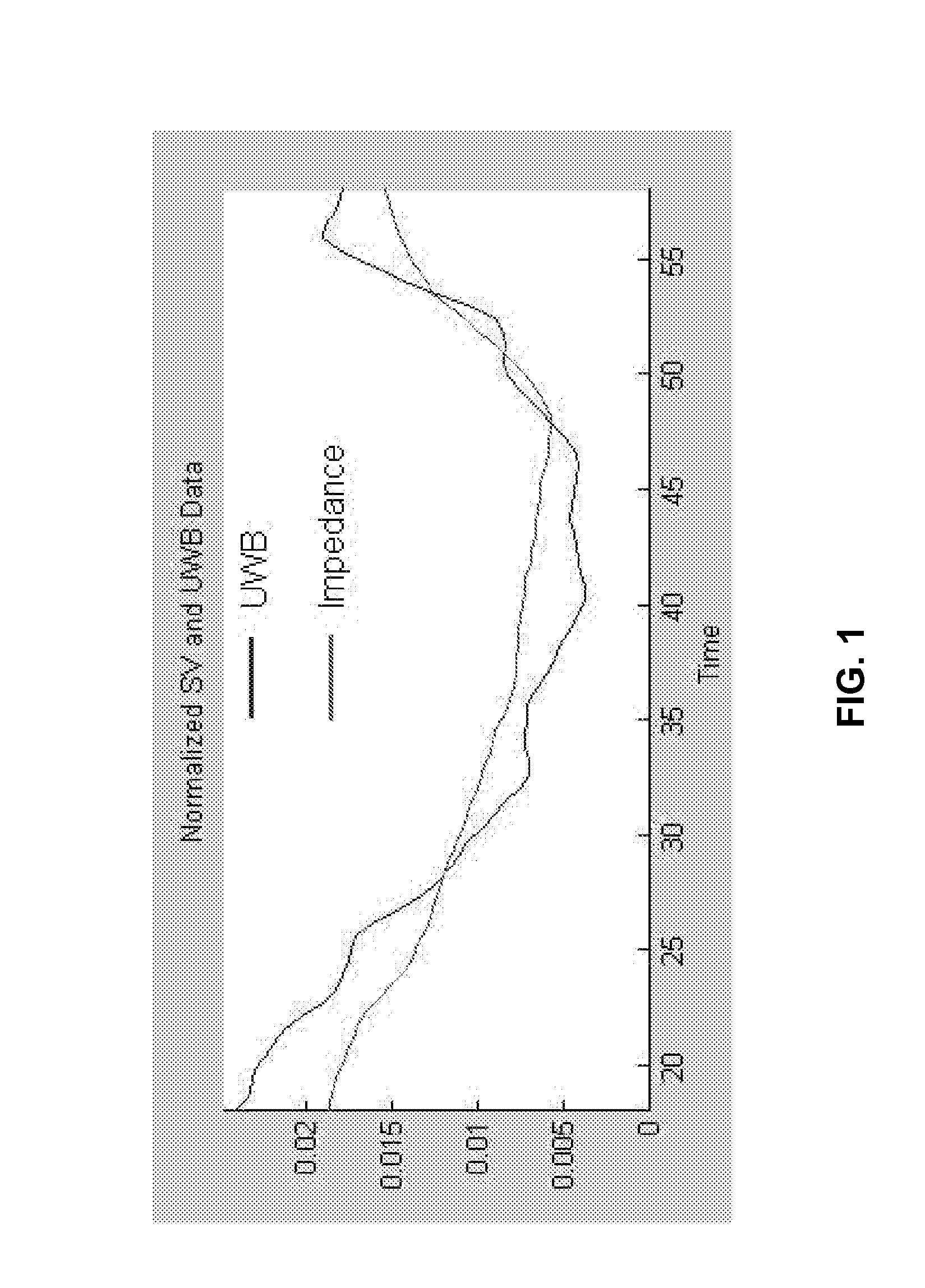
A system and method for non-invasive and continuous measurement of cardiac chamber volume and derivative parameters including stroke volume, cardiac output and ejection fraction comprising an ultrawideband radar system having a trans-mitting and receiving antenna for applying ultrawideband radio signals to a target area of a subject's anatomy wherein the receiving antenna collects and transmits signal returns from the target area which are then delivered to a data processing unit, such as an integrated processor or PDA, having software and hardware used to process the signal returns to produce a value for cardiac stroke volume and changes in cardiac stroke volume supporting multiple diagnostic requirements for emergency response and medical personnel whether located in the battlefield, at a disaster site or at a hospital or other treatment facility.
Owner:LIFEWAVE BIOMEDICAL
Method and apparatus for optimizing ventricular synchrony during DDD resynchronization therapy using adjustable atrio-ventricular delays
InactiveUS7110817B2Convenient timeMaximizes ventricular performanceTransvascular endocardial electrodesHeart stimulatorsSystoleCardiac functioning
A pacing system for providing optimal hemodynamic cardiac function for parameters such as ventricular synchorny or contractility (peak left ventricle pressure change during systole or LV+dp / dt), or stroke volume (aortic pulse pressure) using system for calculating atrio-ventricular delays for optimal timing of a ventricular pacing pulse. The system providing an option for near optimal pacing of multiple hemodynamic parameters. The system deriving the proper timing using electrical or mechanical events having a predictable relationship with an optimal ventricular pacing timing signal.
Owner:CARDIAC PACEMAKERS INC
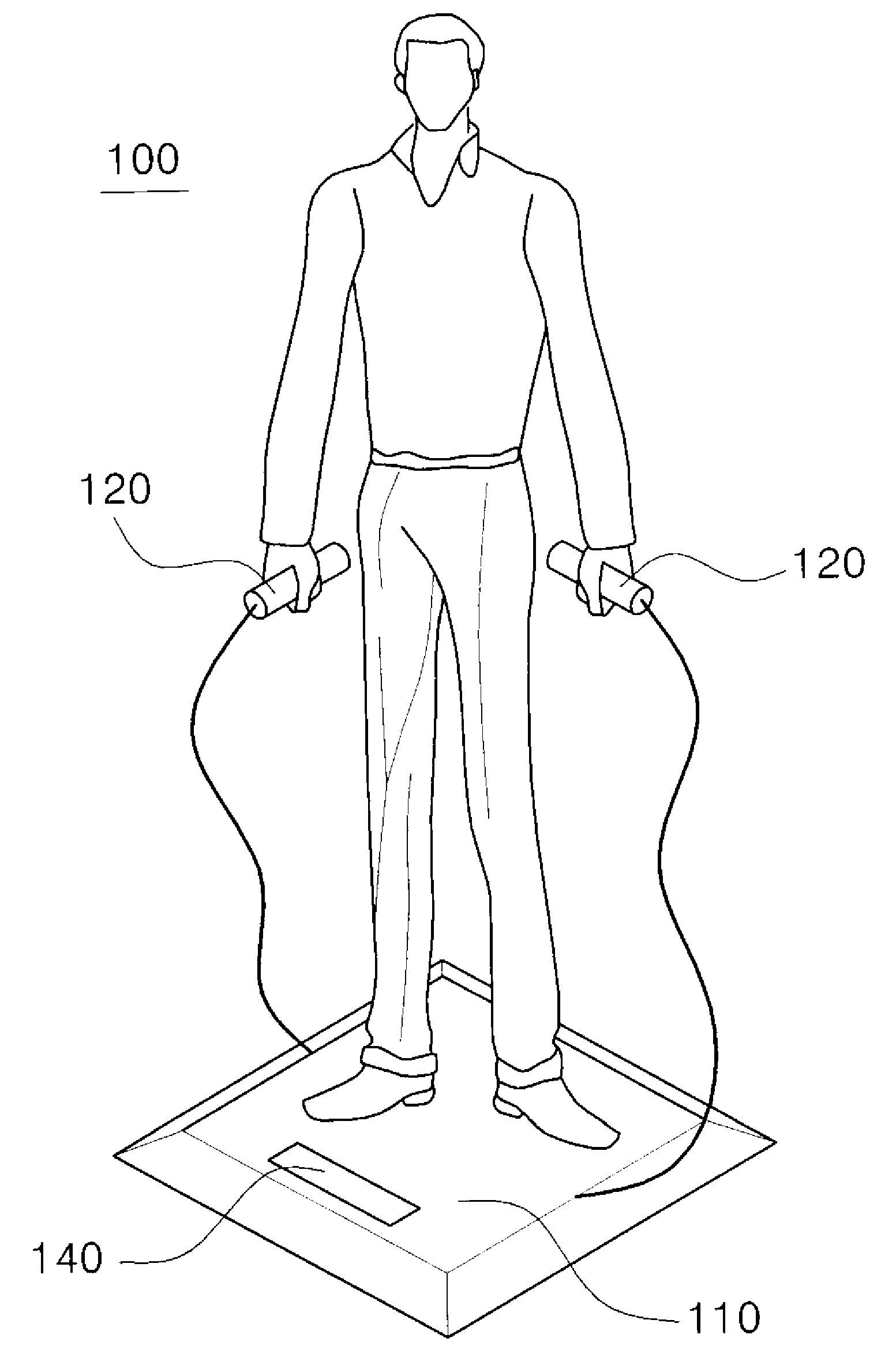
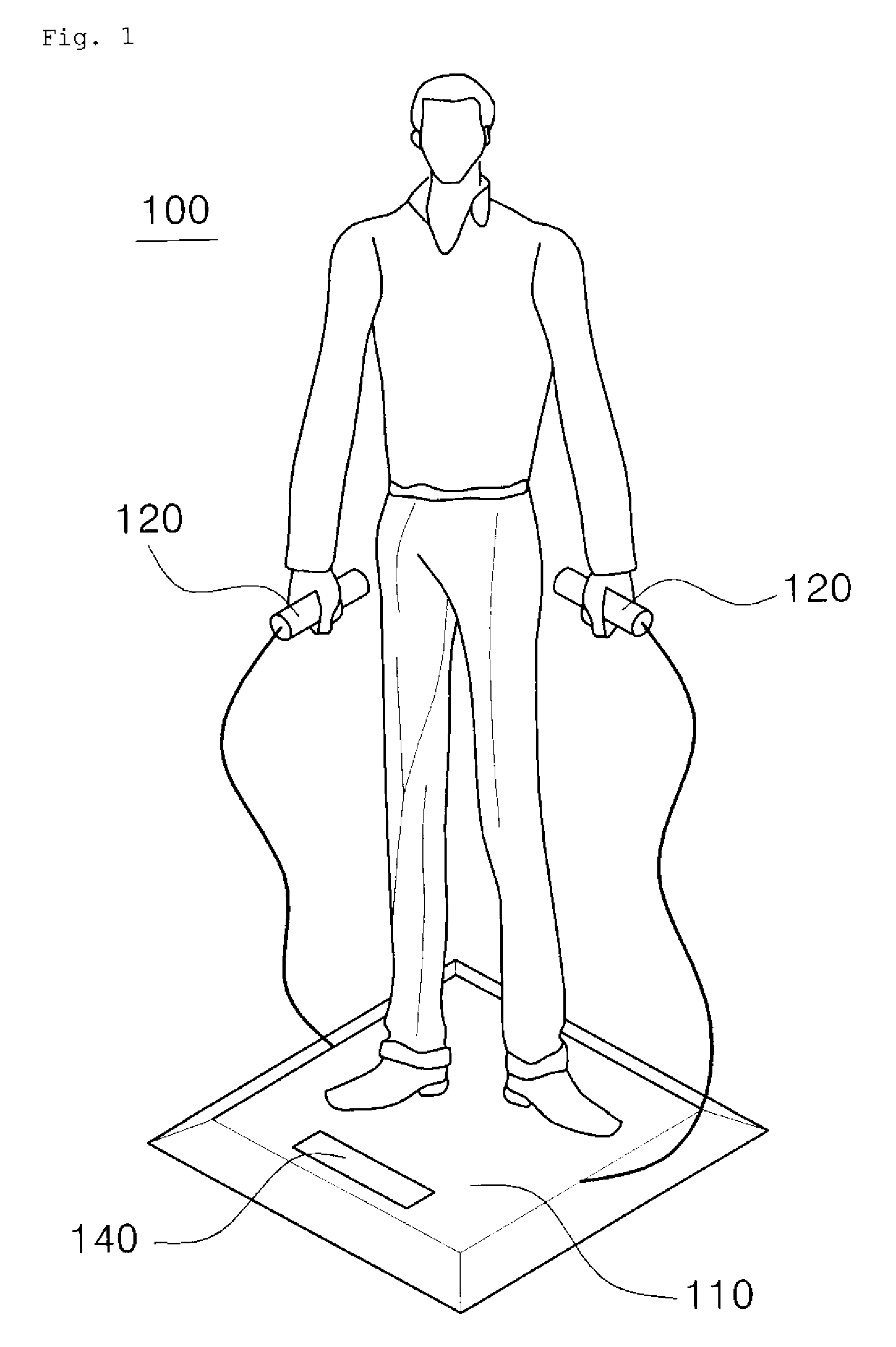
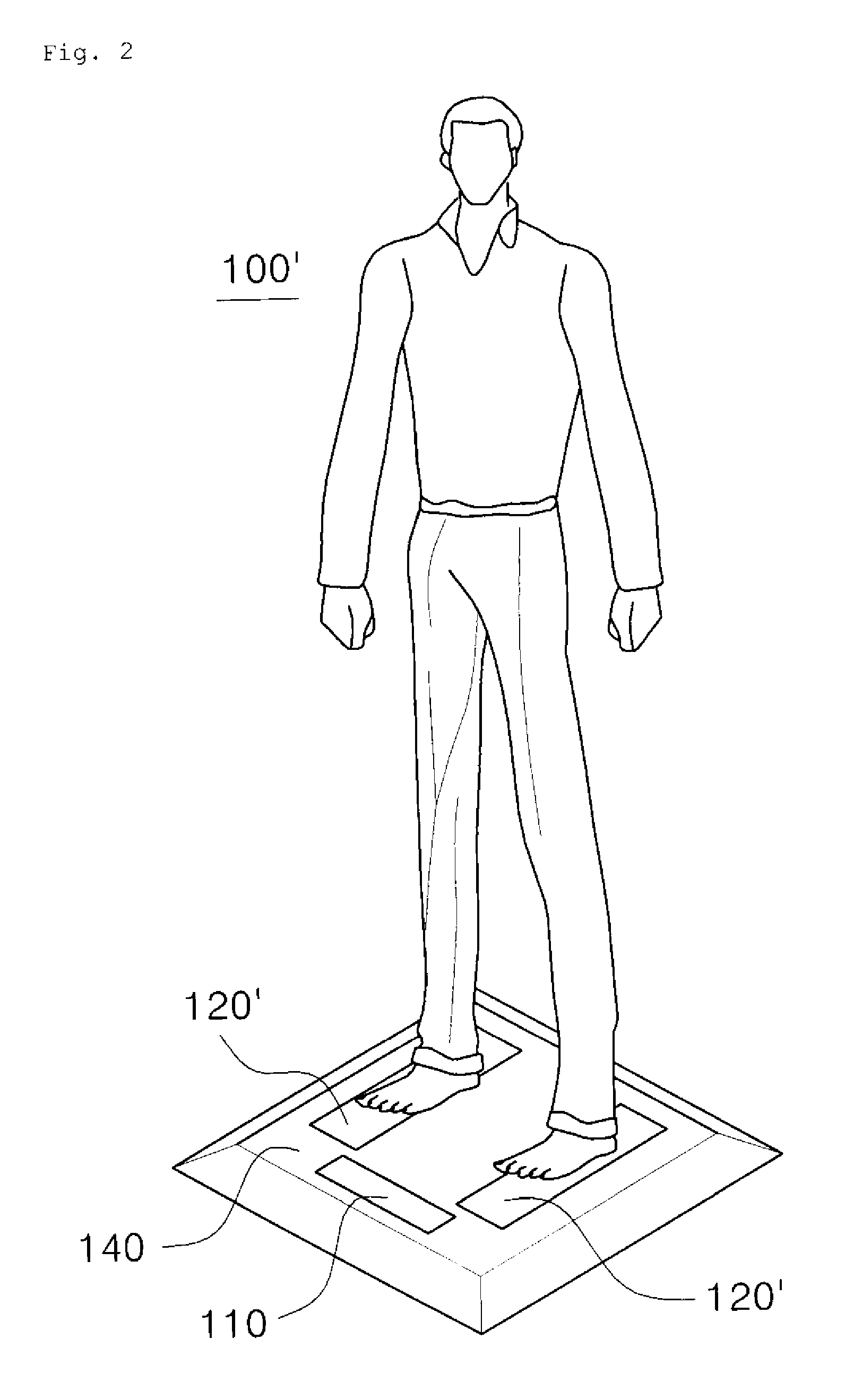
Scale-type nonconstrained health condition evaluating apparatus and method
ActiveUS20100210921A1Easily monitor cardiovascular health conditionMeasure securityElectrocardiographyCatheterHealth conditionLoad cell
A scale-type nonconstrained health condition evaluating apparatus includes a load cell sensor for sensing a ballistocardiogram signal and a weight signal from a measured person, an electrocardiogram sensor for sensing an electrocardiogram signal from the measured person, and a signal processor for calculating at least one of the heart rate, normalized stroke volume force, blood pressure and equilibrium sense abnormality of the measured person from the ballistocardiogram, weight and electrocardiogram signals sensed by the load cell sensor and the electrocardiogram sensor.
Owner:SEOUL NAT UNIV R&DB FOUND
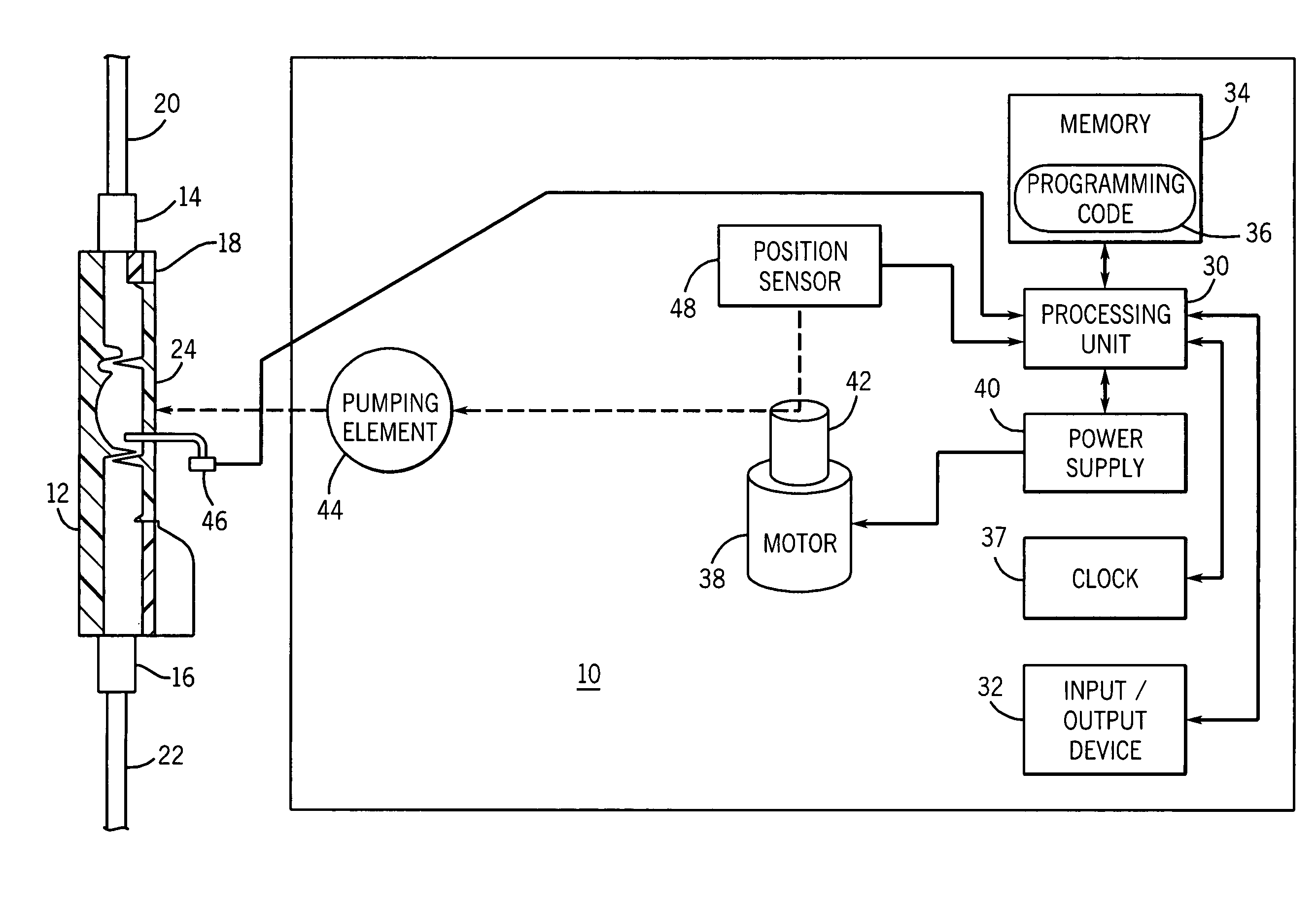
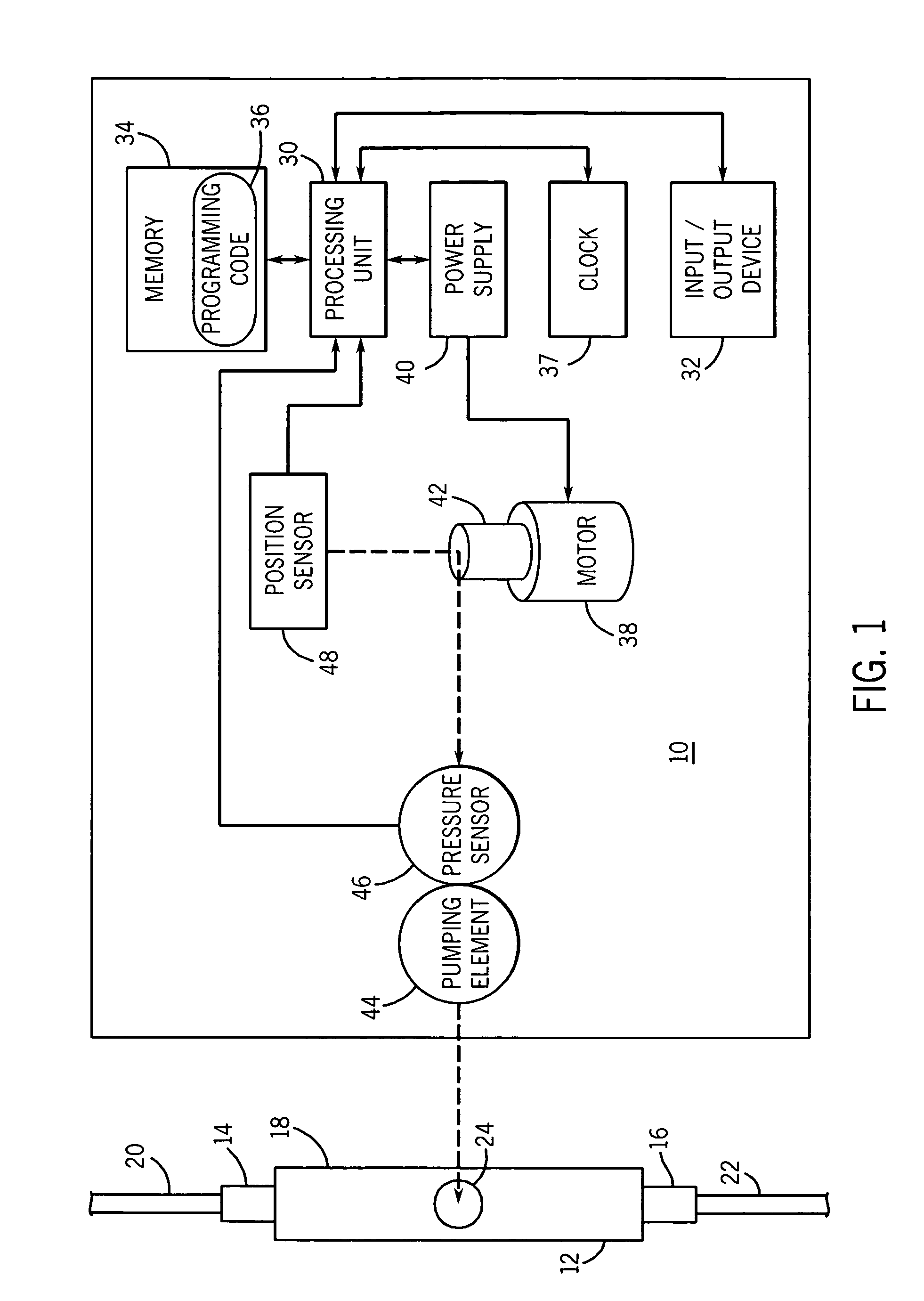
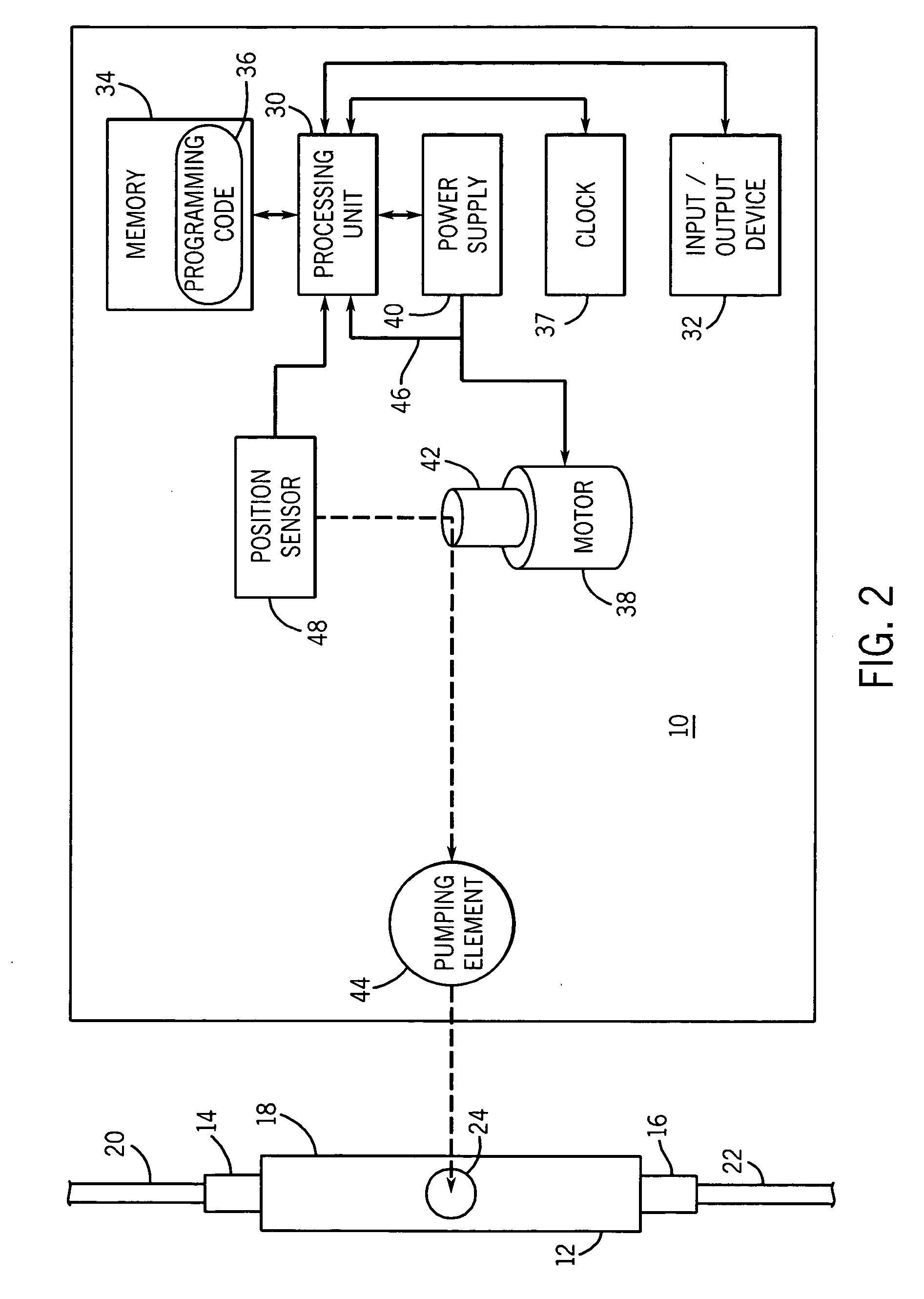
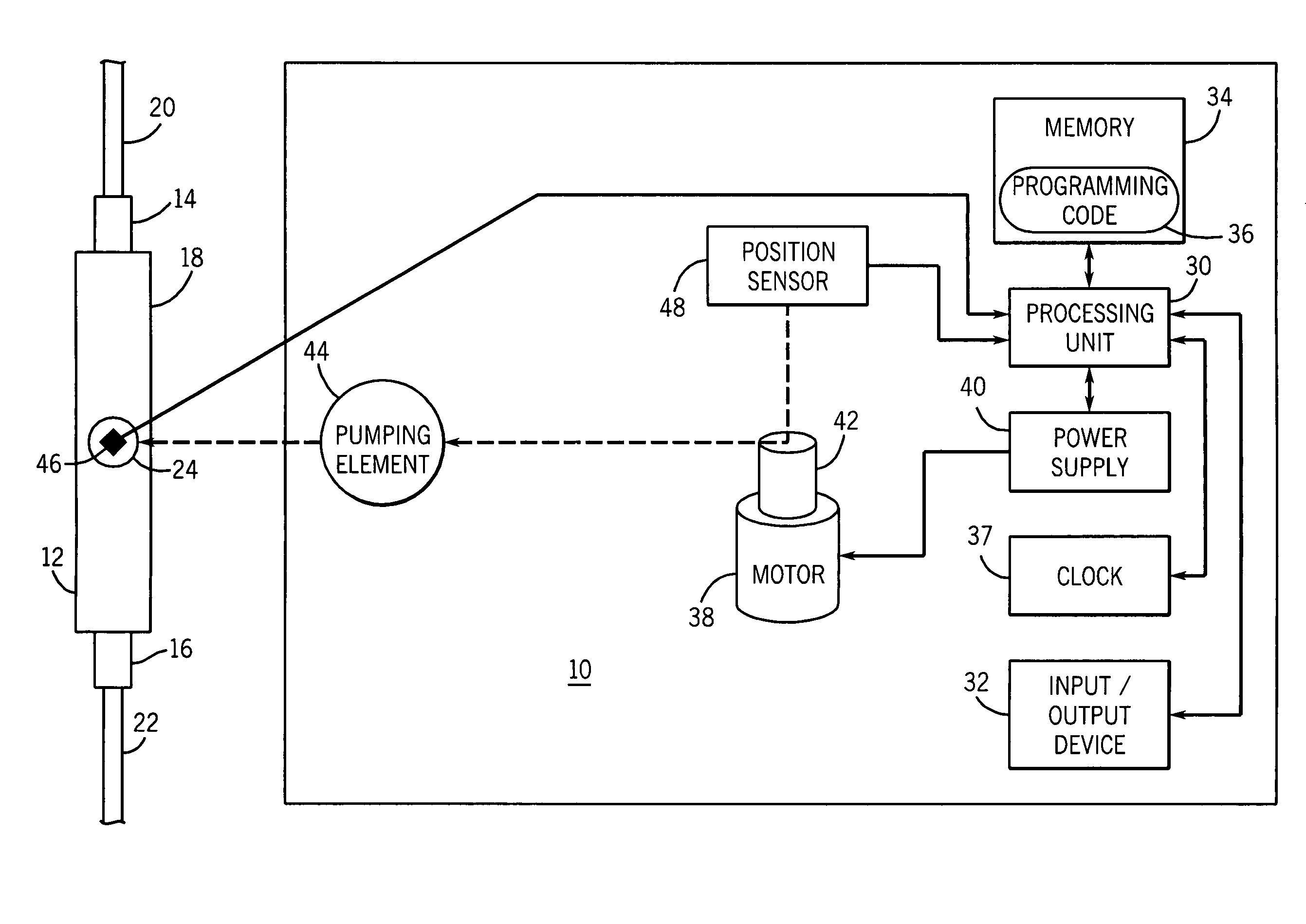
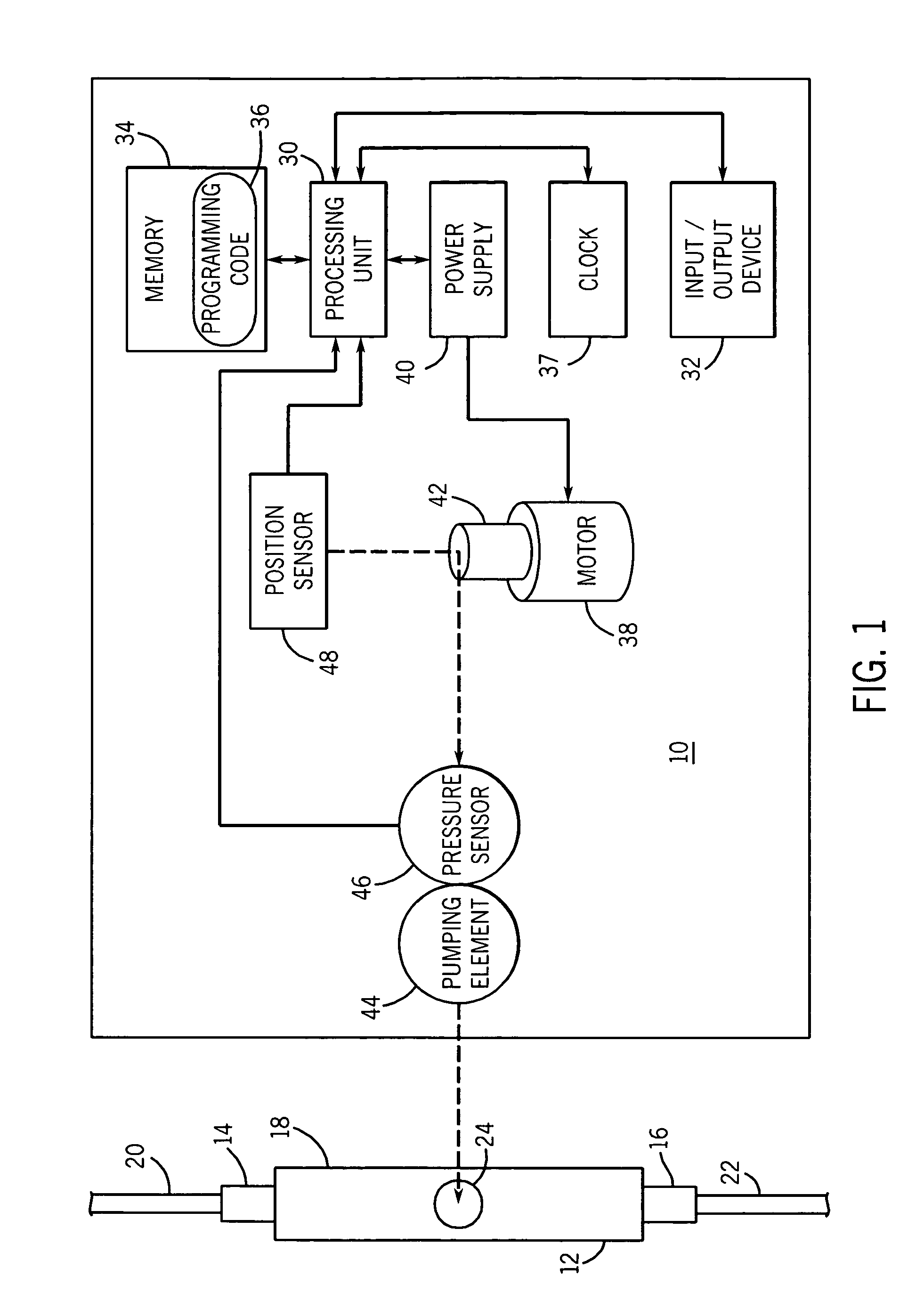
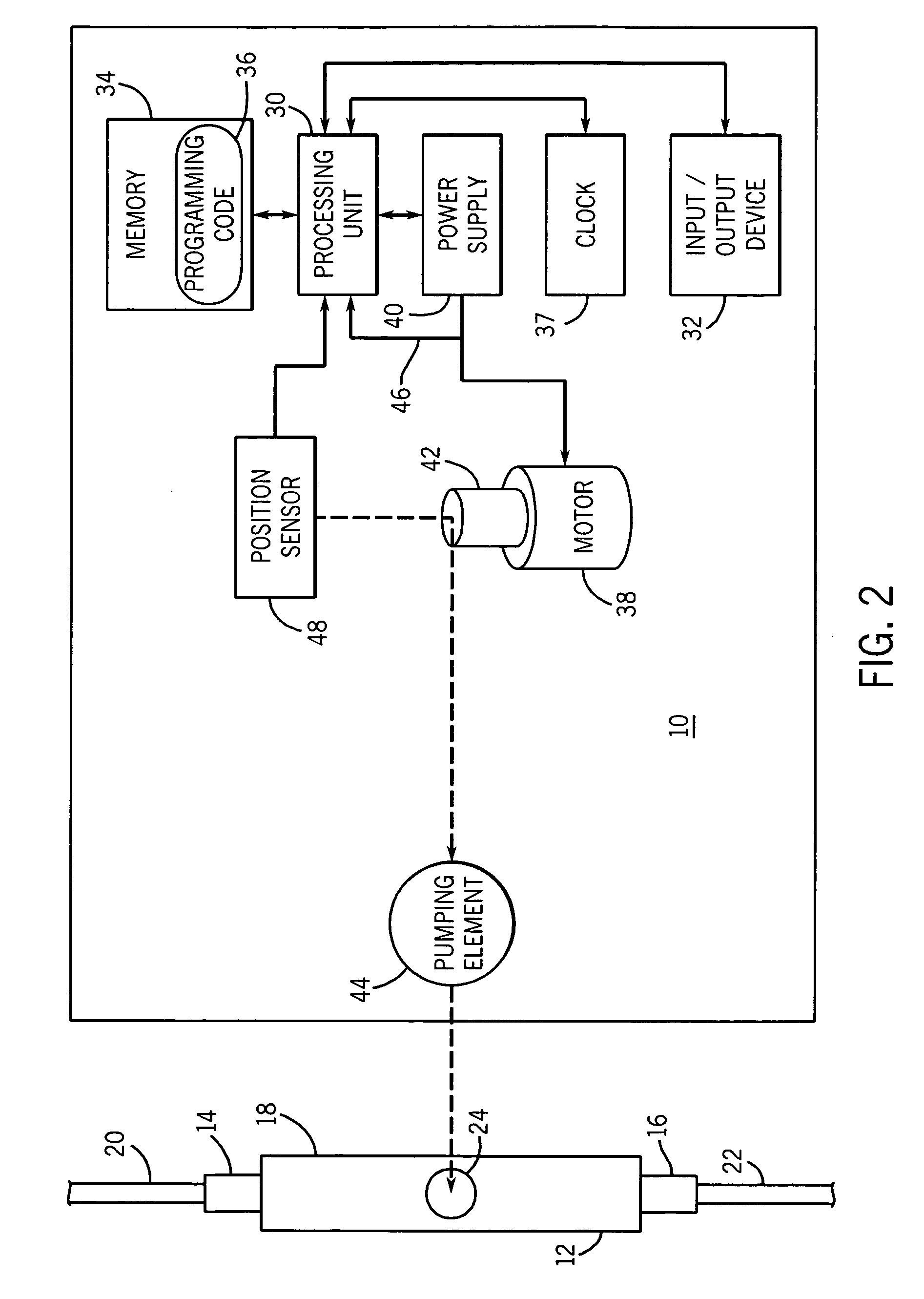
Medical infusion pump with closed loop stroke feedback system and method
ActiveUS20050214129A1Flexible member pumpsMedical devicesLeft ventricular Stroke volumeStroke frequency
A medical pump with a closed loop stroke feedback system and method, for use with a pumping chamber, for example in a cassette, is disclosed. The pump includes a pumping element that intermittently pressurizes a pumping chamber during a pumping cycle. A pressure sensor detects the pressure exerted by the pumping element on the pumping chamber. A position sensor detects the position of the pumping element. A processing unit processes pressure data from the pressure sensor and position data from the position sensor to determine a calculated stroke volume of the pump for a pump cycle, and to adjust a stroke frequency of the pump to compensate for variation in the stroke volume.
Owner:ICU MEDICAL INC +1
Cardiac pacing using adjustable atrio-ventricular delays
A pacing system for providing optimal hemodynamic cardiac function for parameters such as contractility (peak left ventricle pressure change during systole or LV+dp / dt), or stroke volume (aortic pulse pressure) using system for calculating atrio-ventricular delays for optimal timing of a ventricular pacing pulse. The system providing an option for near optimal pacing of multiple hemodynamic parameters. The system deriving the proper timing using electrical or mechanical events having a predictable relationship with an optimal ventricular pacing timing signal.
Owner:CARDIAC PACEMAKERS INC
Medical infusion pump with closed loop stroke feedback system and method
A medical pump with a closed loop stroke feedback system and method, for use with a pumping chamber, for example in a cassette, is disclosed. The pump includes a pumping element that intermittently pressurizes a pumping chamber during a pumping cycle. A pressure sensor detects the pressure exerted by the pumping element on the pumping chamber. A position sensor detects the position of the pumping element. A processing unit processes pressure data from the pressure sensor and position data from the position sensor to determine a calculated stroke volume of the pump for a pump cycle, and to adjust a stroke frequency of the pump to compensate for variation in the stroke volume.
Owner:ICU MEDICAL INC +1
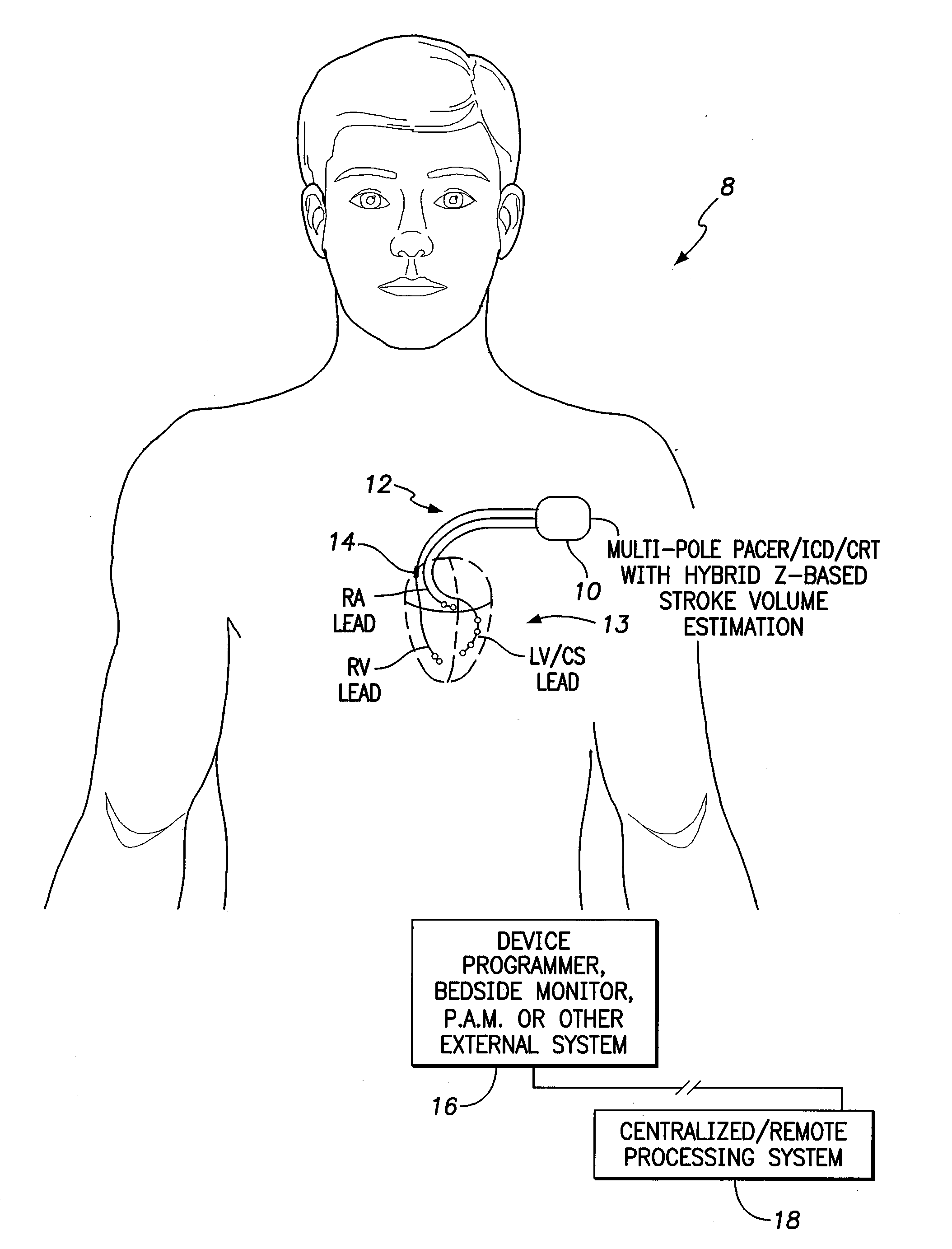
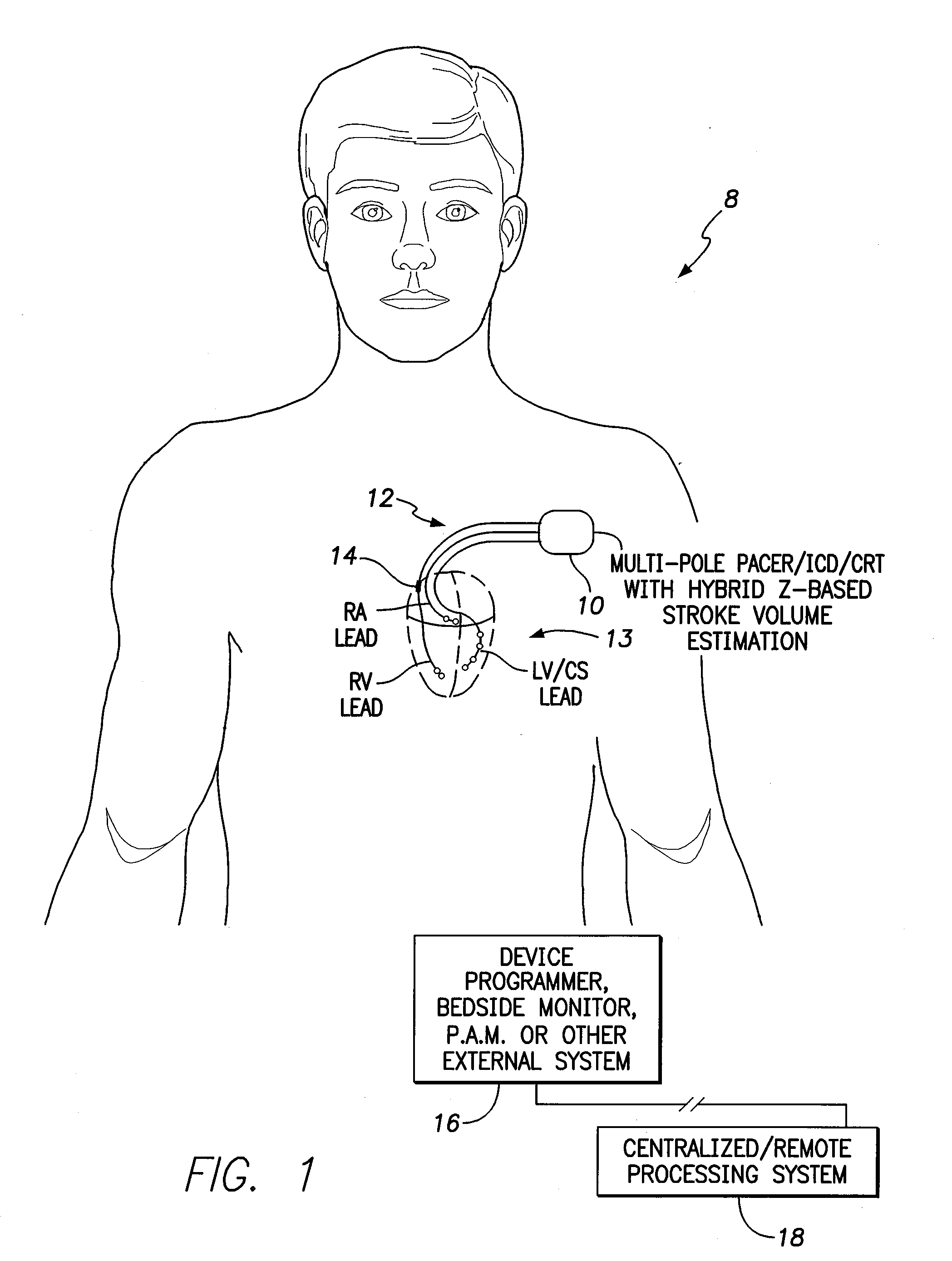
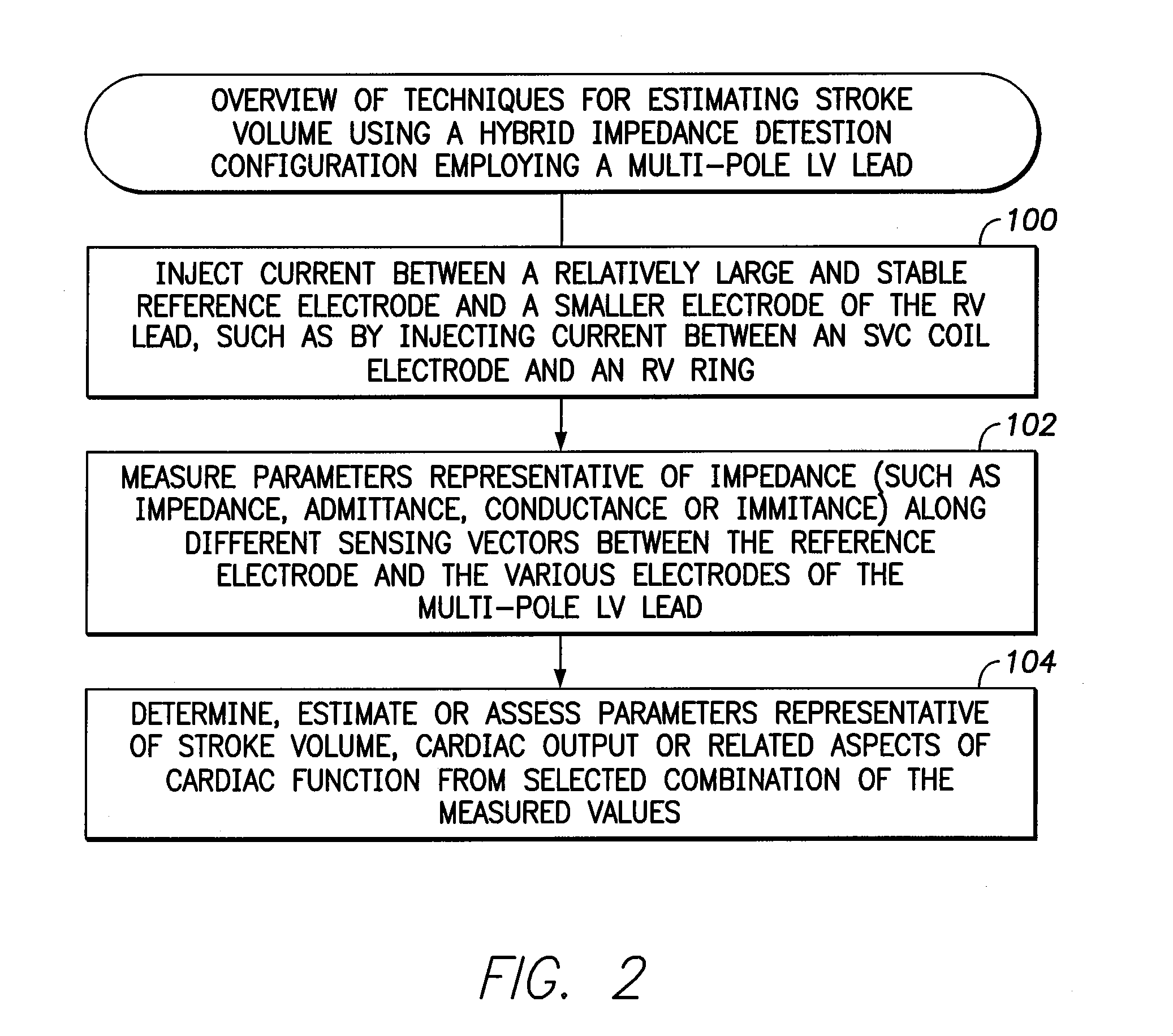
Systems and methods for tracking stroke volume using hybrid impedance configurations employing a multi-pole implantable cardiac lead
ActiveUS20120203090A1Wide electrical fieldLarge and stableElectrocardiographyHeart stimulatorsElectrical impedanceLeft ventricle wall
Techniques are provided for use with an implantable medical device for assessing stroke volume or related cardiac function parameters such as cardiac output based on impedance signals obtained using hybrid impedance configurations that exploit a multi-pole cardiac pacing / sensing lead implanted near the left ventricle. In one example, current is injected between a large and stable reference electrode and a ring electrode in the RV. The reference electrode may be, e.g., a coil electrode implanted within the superior vena cava (SVC). Impedance values are measured along a set of different sensing vectors between the reference electrode and each of the electrodes of the multi-pole LV lead. Stroke volume is then estimated and tracked within the patient using the impedance values. In this manner, a hybrid impedance detection configuration is exploited whereby one vector is used to inject current and other vectors are used to measure impedance.
Owner:PACESETTER INC
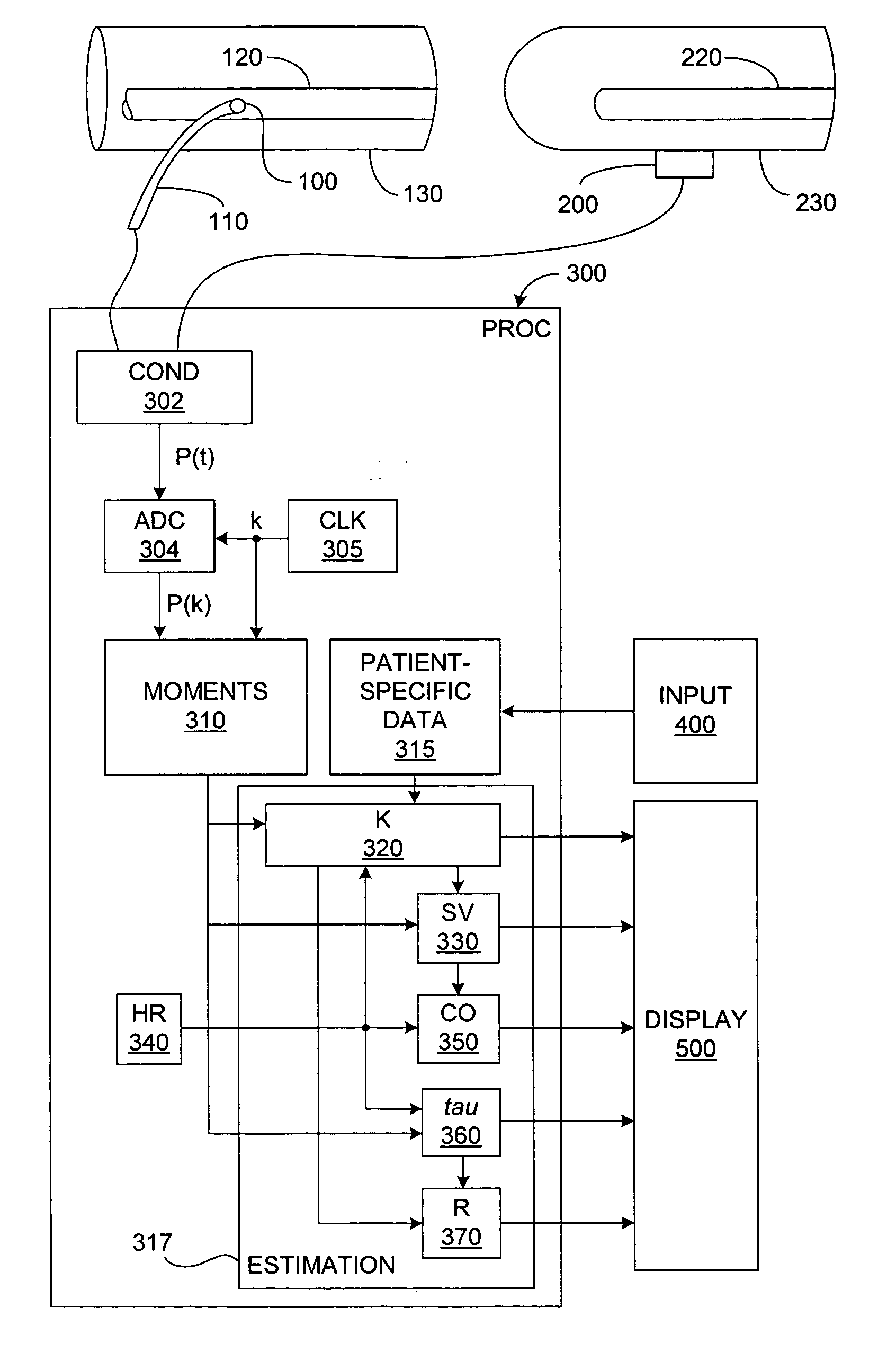
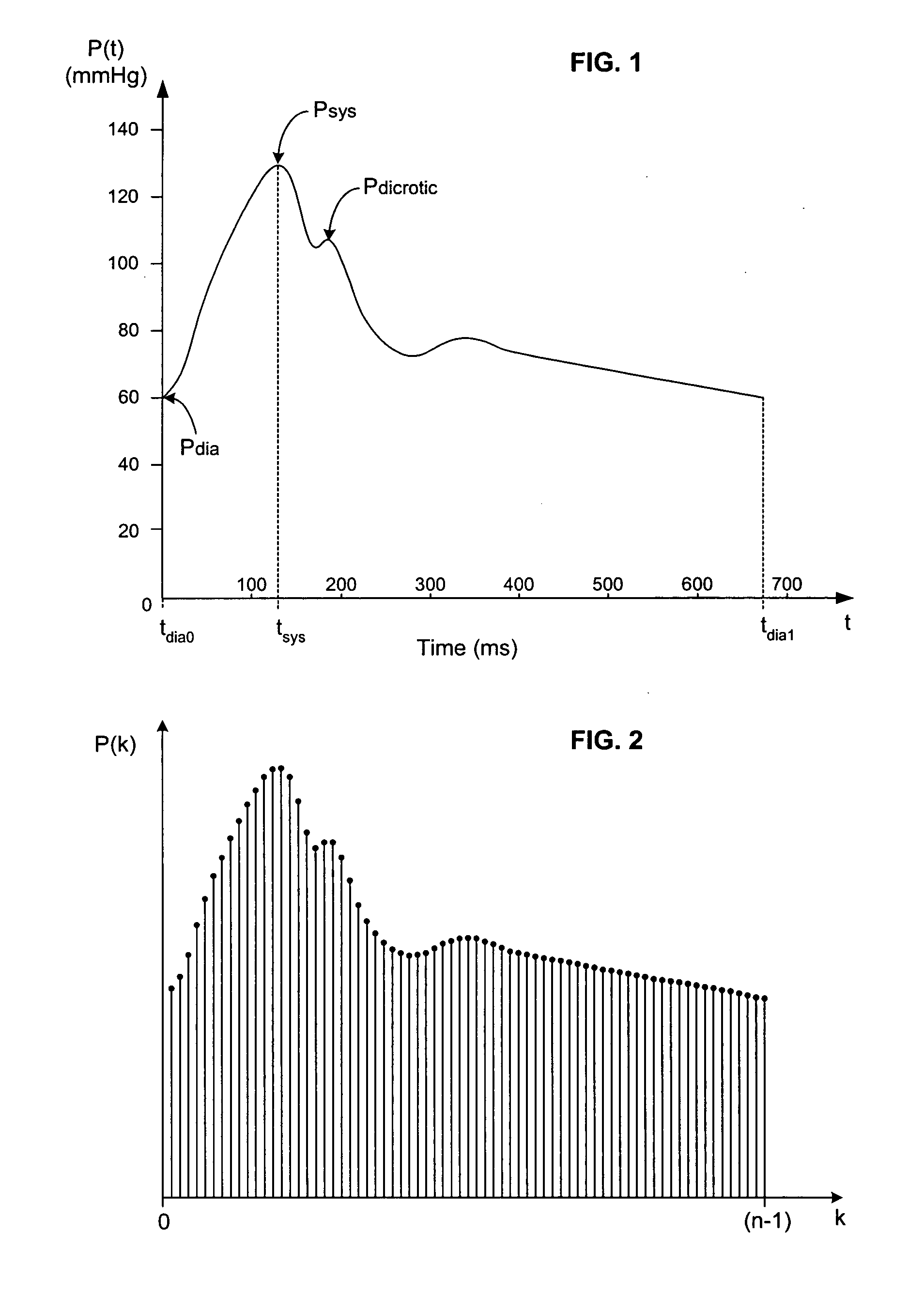
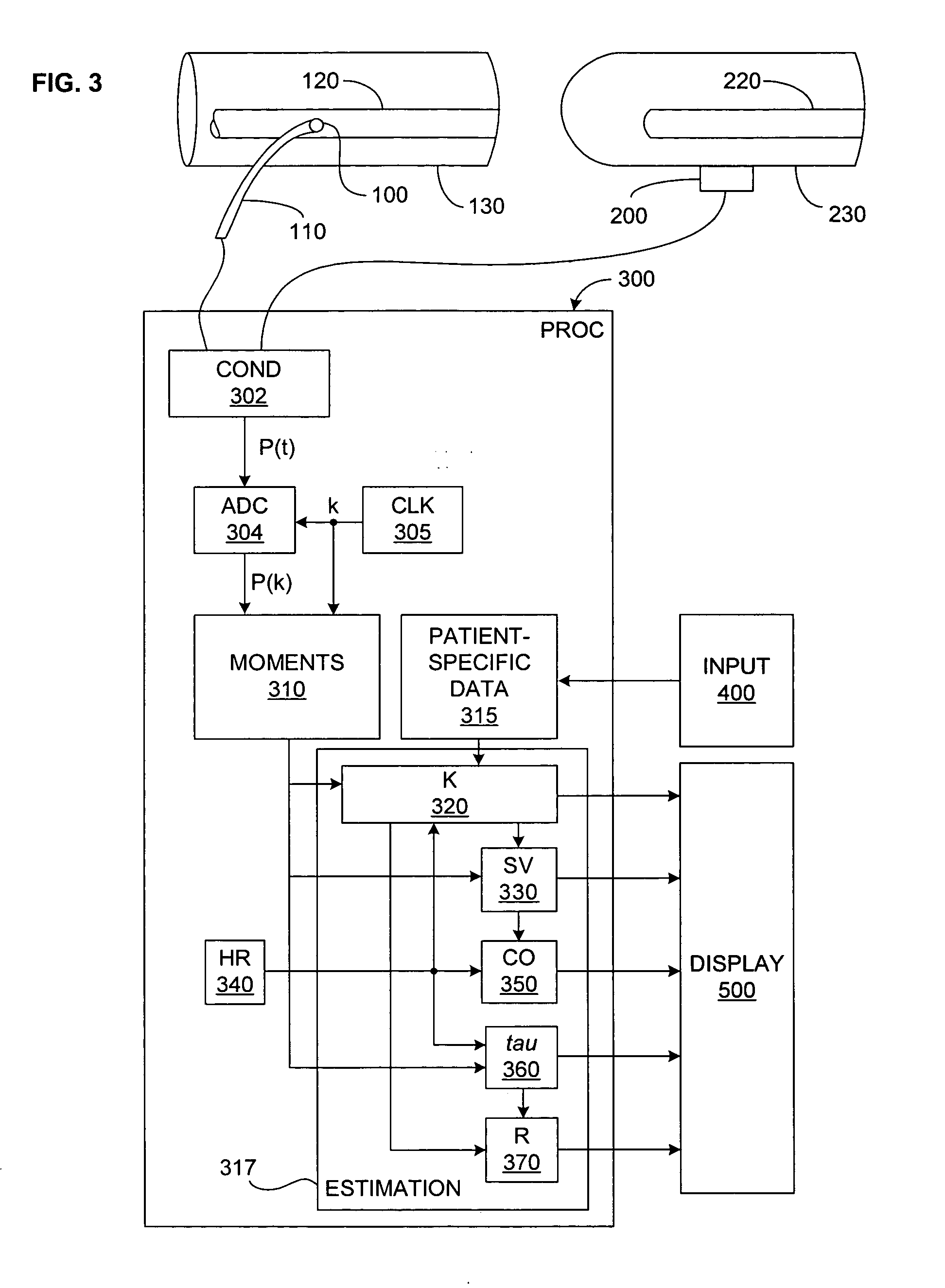
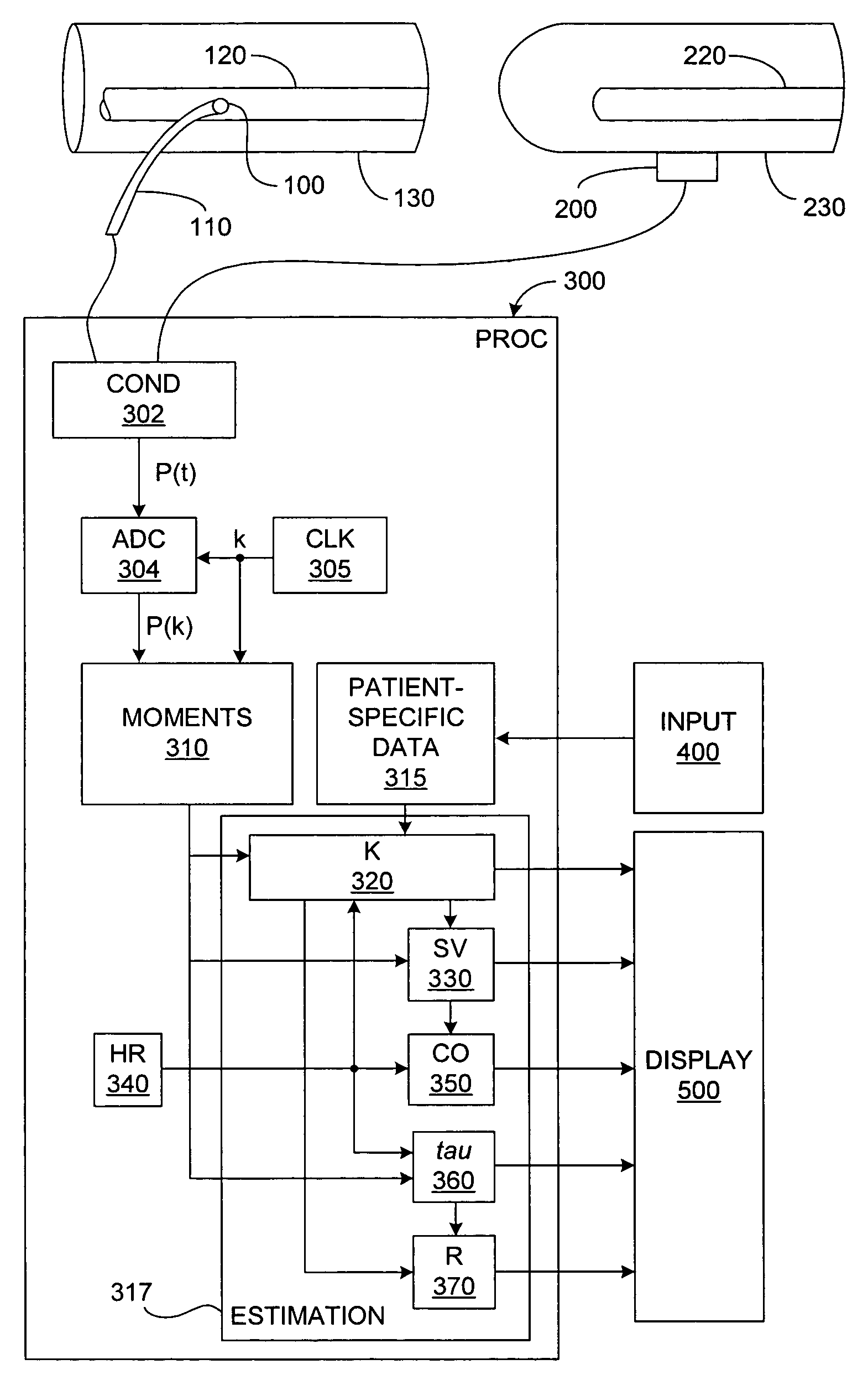
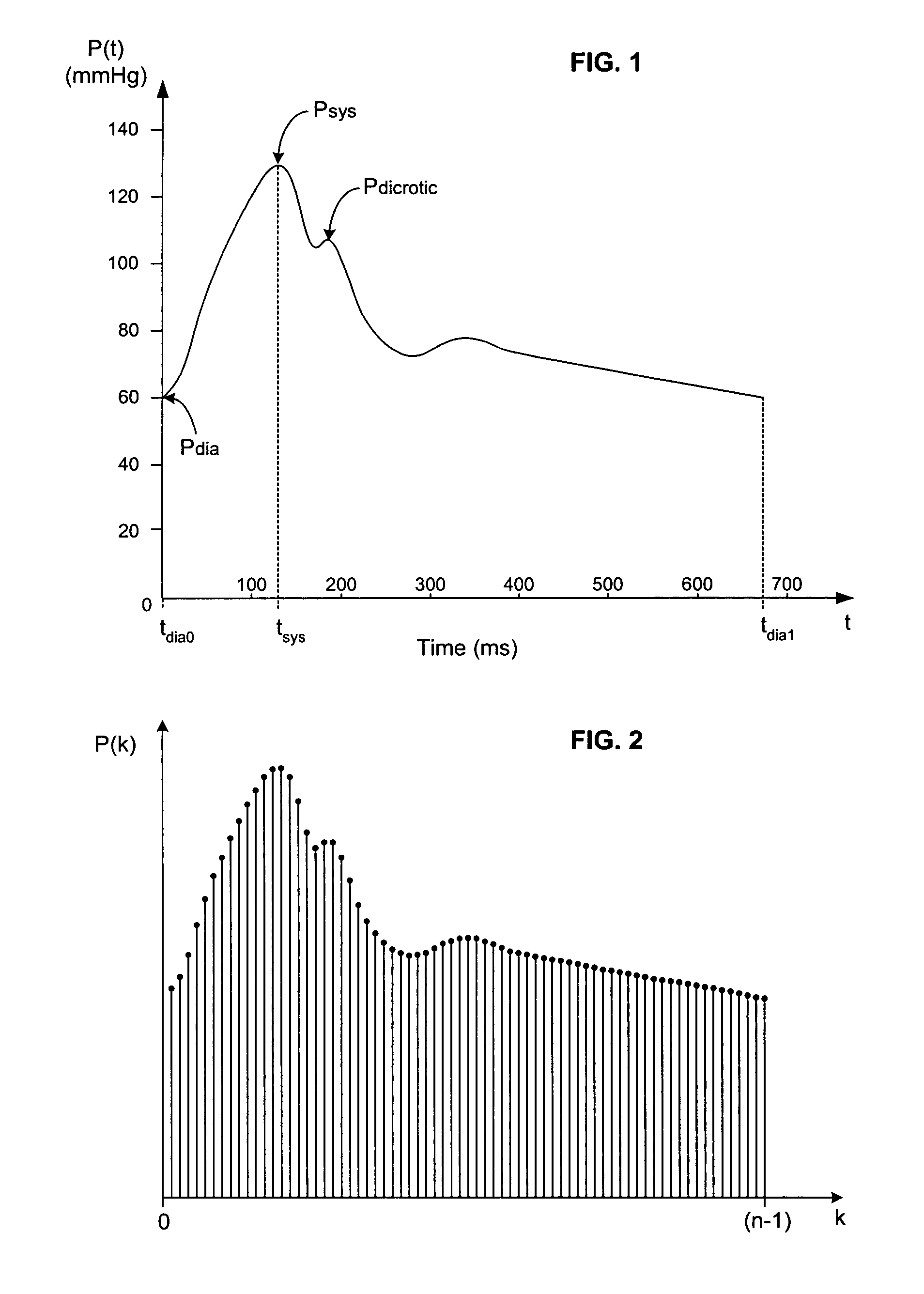
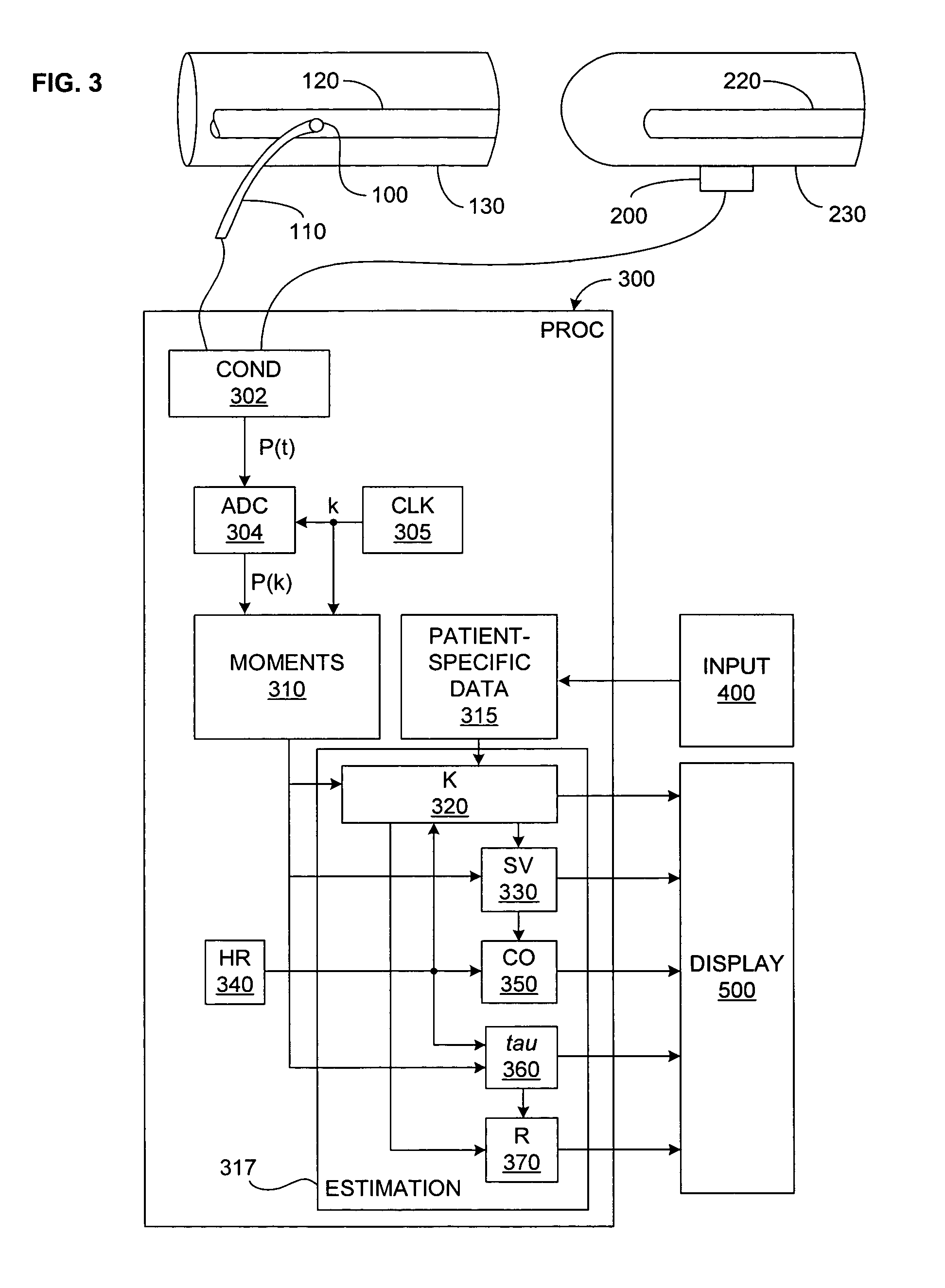
Arterial pressure-based, automatic determination of a cardiovascular parameter
One or more cardiovascular parameters is estimated as a function of the arterial pressure waveform, in particular, using at least one statistical moment of pressure waveform having an order greater than one. Arterial compliance, the exponential pressure decay constant, vascular resistance, cardiac output, and stroke volume are examples of cardiovascular parameters that can be estimated using various aspects of the invention. In one embodiment of the invention, not only are the first four moments (mean, standard deviation, skewness, and kurtosis) of the pressure waveform used to estimate the cardiovascular parameter(s) of interest, but also heart rate, statistical moments of a set of pressure-weighted time values, and certain anthropometric patient measurements such as age, sex, body surface area, etc.
Owner:EDWARDS LIFESCIENCES CORP
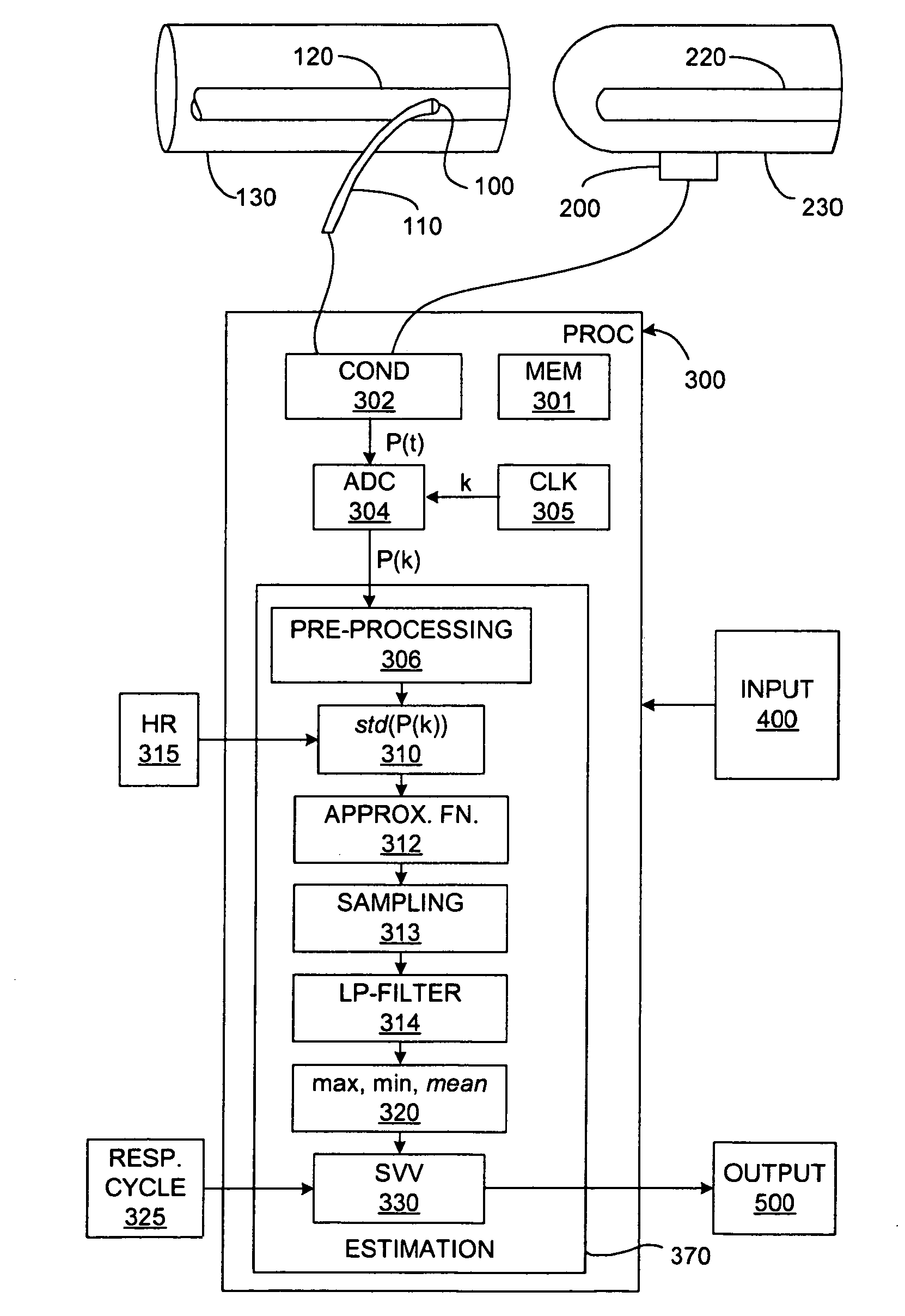
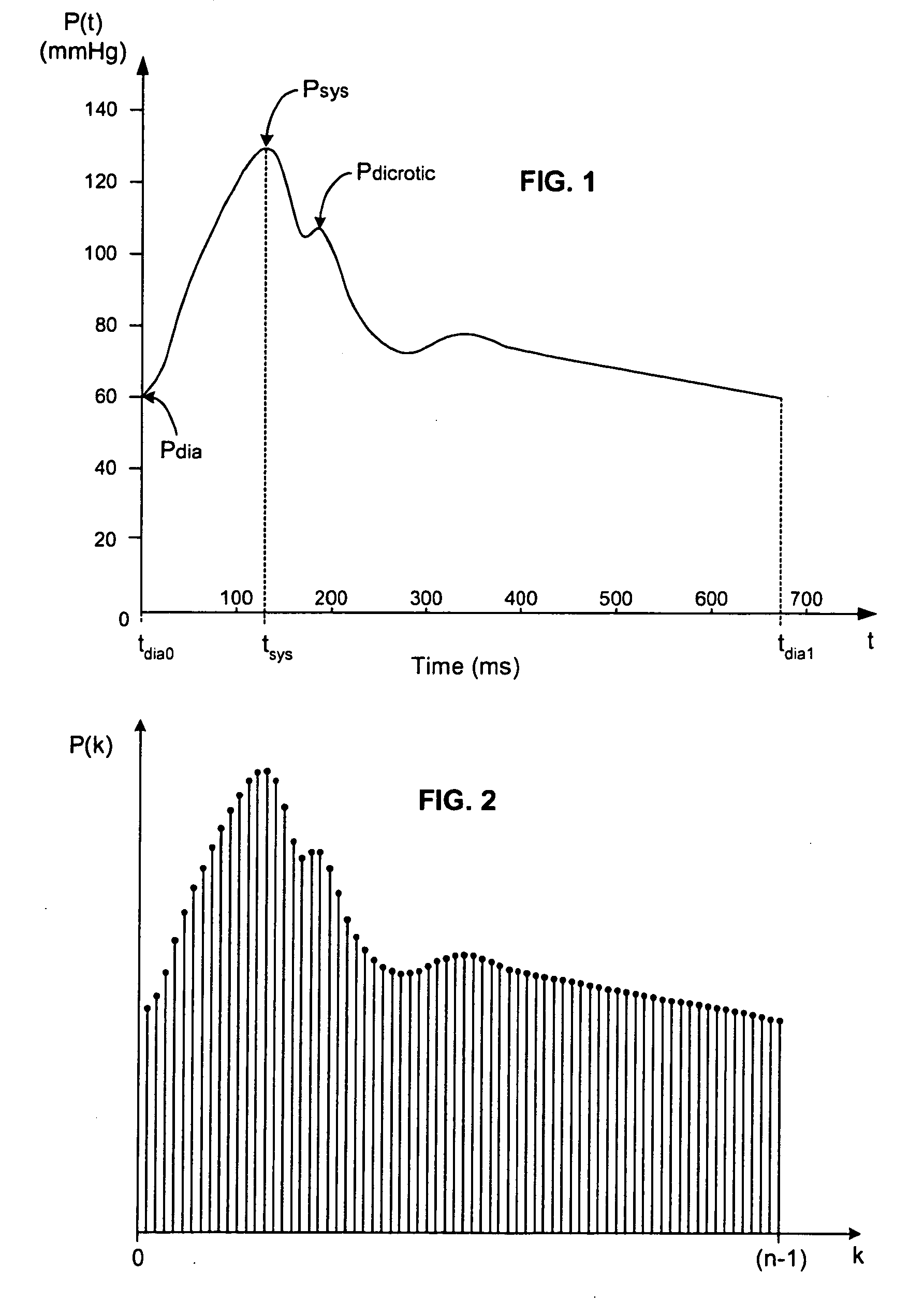
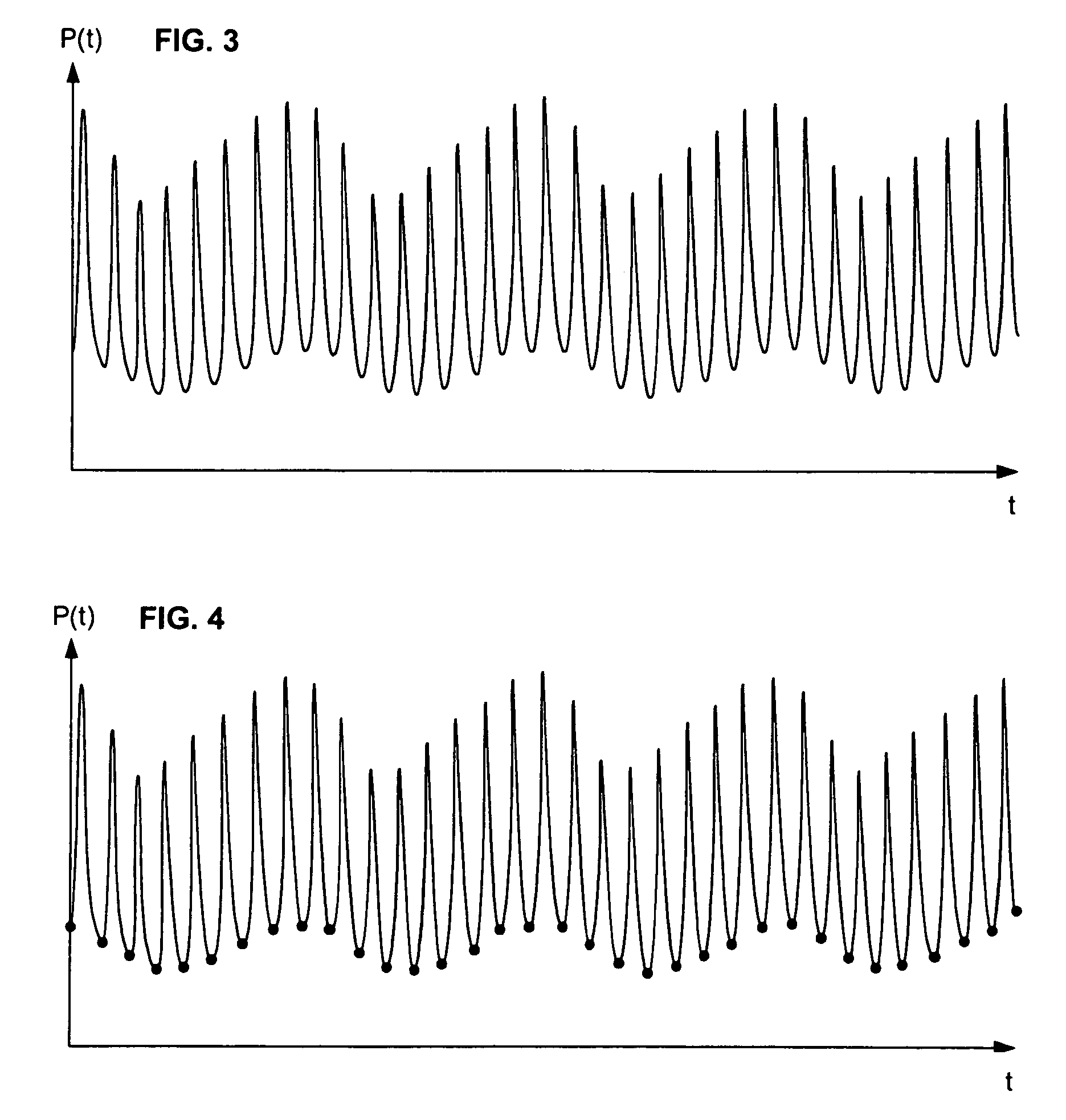
Real-time measurement of ventricular stroke volume variations by continuous arterial pulse contour analysis
Ventricular stroke volume variation (SVV) is estimated as a function of the standard deviation of arterial blood pressure value measured over each of at least two cardiac cycles, preferably over each of the cardiac cycles in a computation interval covering a full respiratory cycle. In one embodiment, maximum and minimum standard deviation values are determined over the computation interval. SVV is then estimated proportional to the ratio of the difference between the maximum and minimum standard deviation values and the mean of the standard deviation values. In another embodiment, SVV is then estimated proportional to the ratio of the standard deviation of the standard deviation values and the mean standard deviation over the entire computation interval. A pre-processing arrangement for improving reliability of estimates of more general cardiac or hemodynamic parameters is also disclosed and involves smoothing with an approximating function, and sampling and low-pass filtering at an adjustable rate.
Owner:EDWARDS LIFESCIENCES CORP
Magnetic devices and methods for reshaping heart anatomy
InactiveUS7402134B2Improve shrinkageIncrease volumeHeart valvesSurgical needlesCardiac surfaceHeart Part
Systems, methods and devices are provided for treating heart failure patients suffering from various levels of heart dilation. Heart dilation treated by reshaping the heart anatomy with the use of magnetic forces. Such reshaping changes the geometry of portions of the heart, particularly the right or left ventricles, to increase contractibility of the ventricles thereby increasing the stroke volume which in turn increases the cardiac output of the heart. The magnetic forces are applied with the use of one or more magnetic elements which are implanted within the heart tissue or attached externally and / or internally to a surface of the heart. The various charges of the magnetic forces interact causing the associated heart tissue areas to readjust position, such as to decrease the width of the ventricles. Such repositioning is maintained over time by the force of the magnetic elements, allowing the damaging effects of heart dilation to slow in progression or reverse.
Owner:MICARDIA CORP
Apparatus for determination of stroke volume using the brachial artery
Provided herein are methods and apparatus for stroke volume determination by bioimpedance from a patient's upper arm, or brachium, utilizing pulsations of the brachial artery contained therein. The apparatus includes two or more spaced apart alternating current flow electrodes positioned on the patient's arm proximate the brachial artery and two or more spaced apart voltage sensing electrodes positioned on the patient's arm proximate the brachial artery. The voltage sensing electrodes are positioned between the alternating current flow electrodes on the arm. An alternating current source is electrically connected to the alternating current flow electrodes and a voltmeter electrically is connected to the voltage sensing electrodes. A data input device is provided along with a processing unit in communication with the data input device, the alternating current source, alternating current flow electrodes, the voltmeter, and voltage sensing electrodes. The processing unit is capable of using data from the data input device and voltage sensing electrodes to calculate the stroke volume of the patient.
Owner:BERSTEIN DONALD P
Method and system for continuously monitoring cardiac output
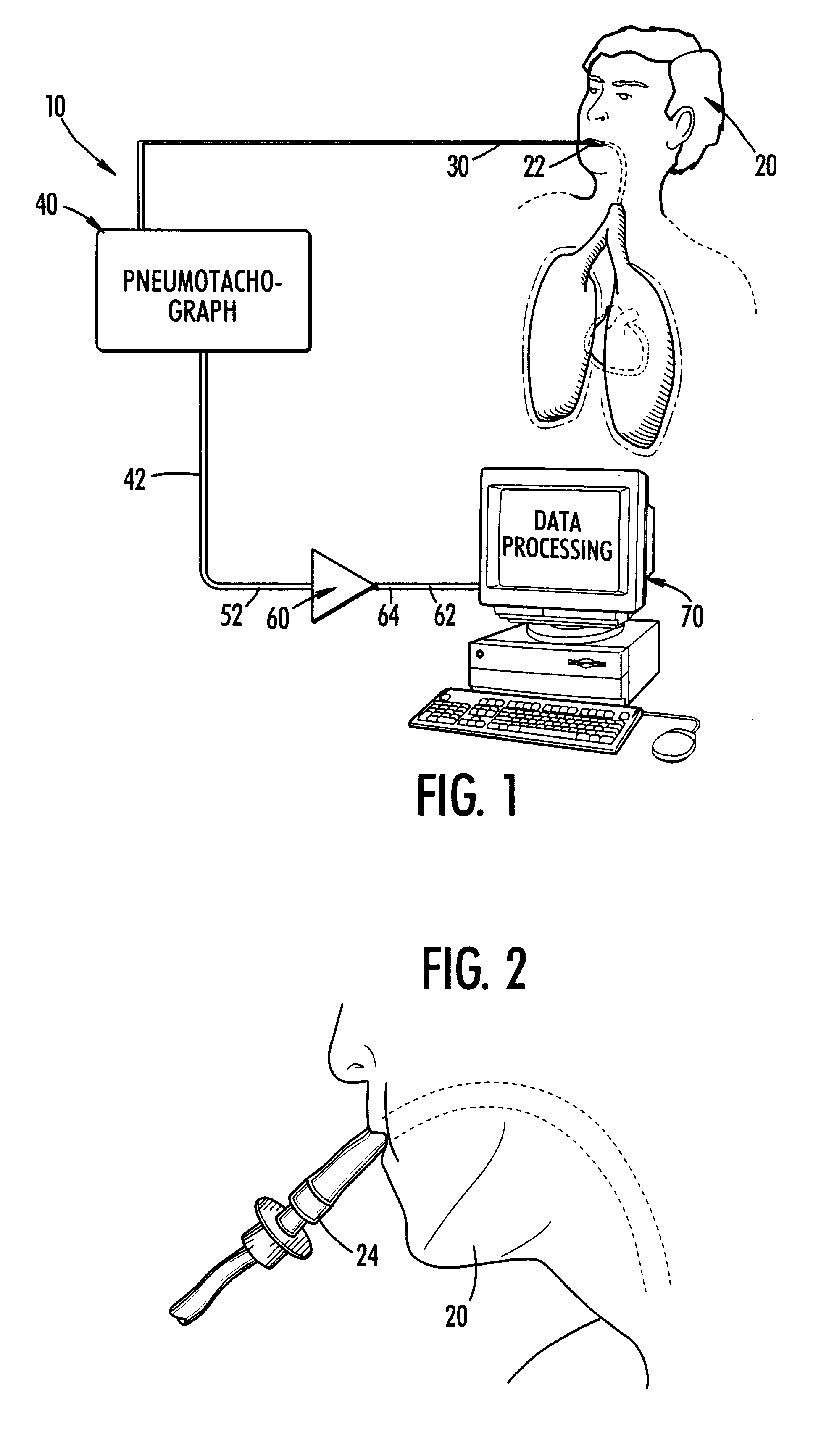
InactiveUS6186956B1Easily moved to patient and transportedLight weightCatheterRespiratory organ evaluationDigital dataAir volume
The present invention is a method and system for continuously monitoring cardiac output. In a preferred embodiment, the method and system of the present invention comprises a pneumotachograph, differential pressure transducer, and a signal amplifier / conditioner interconnected to a programmed digital computer. A patient, preferably, inserts the pneumotachograph in his mouth or, alternatively, the pneumotachograph is connected to a patient's tracheal cannula. As the patient exhales and inhales the differential pressure transducer measures the drop in pressure as air flows through the pneumotachograph thereby producing a weak electrical signal non-linearly proportional to flow. Next, the weak signal is directed through the amplifier / signal conditioner which increases the amplitude and removes some of the noise contained in the transducer output. A digital computer is then utilized to convert the analog time varying electrical signal into a stream of digital data, store it on disk, display it in real time and processes the signal using an experimentally determined correlation factor and mathematical equations relating the fluctuations in air flow with stroke volume to obtain the cardiac output.
Owner:UNIVERSITY OF SOUTH CAROLINA
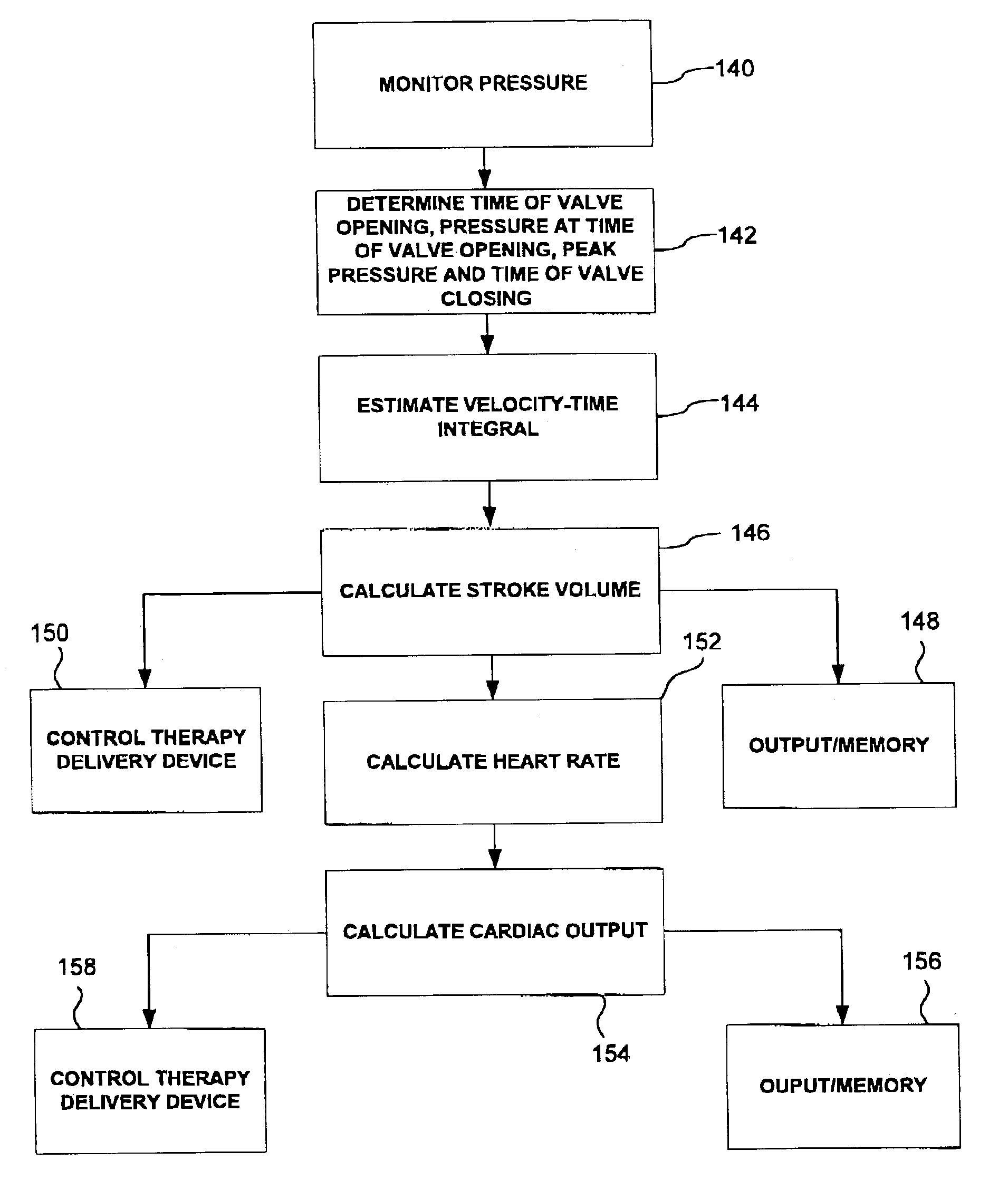
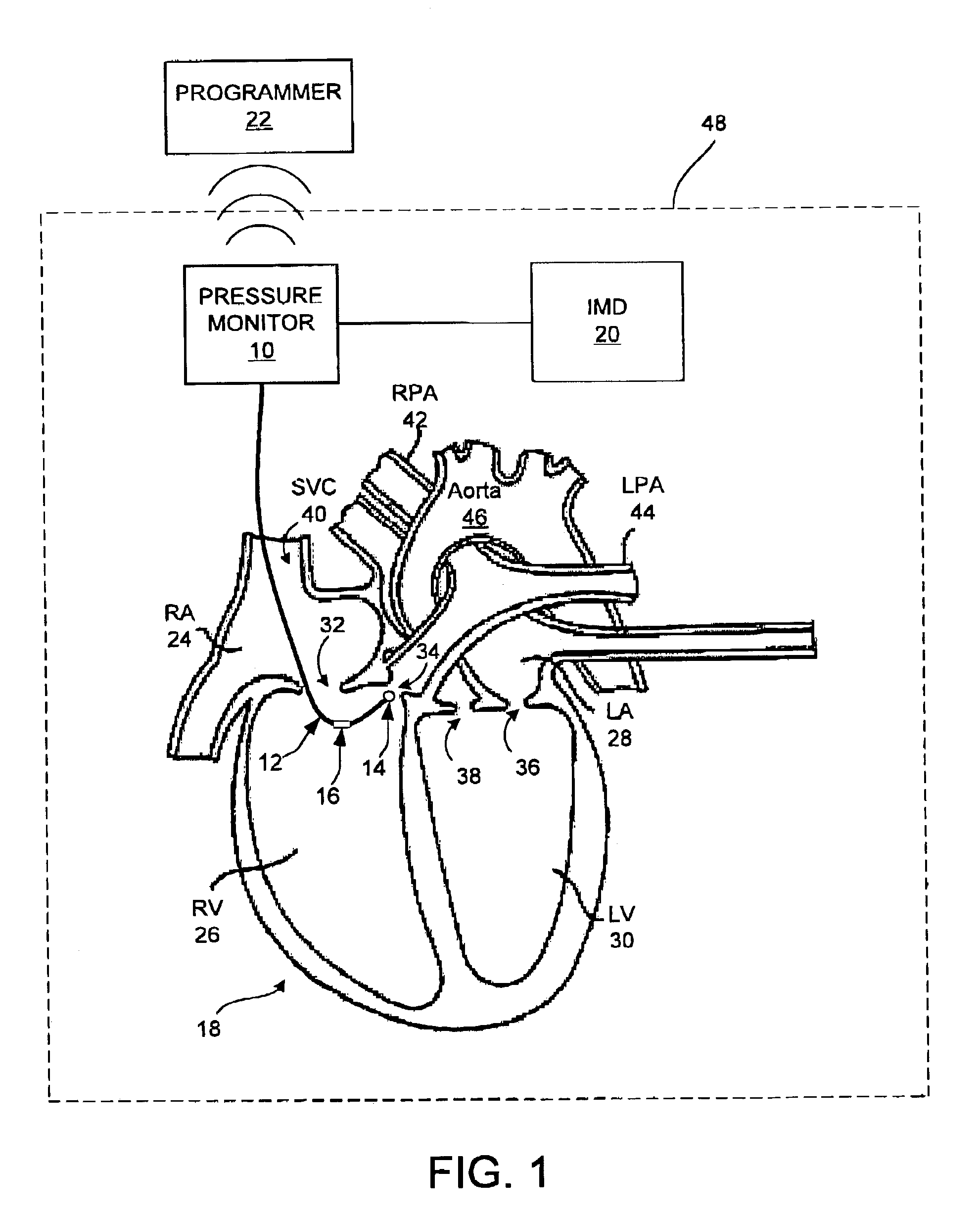
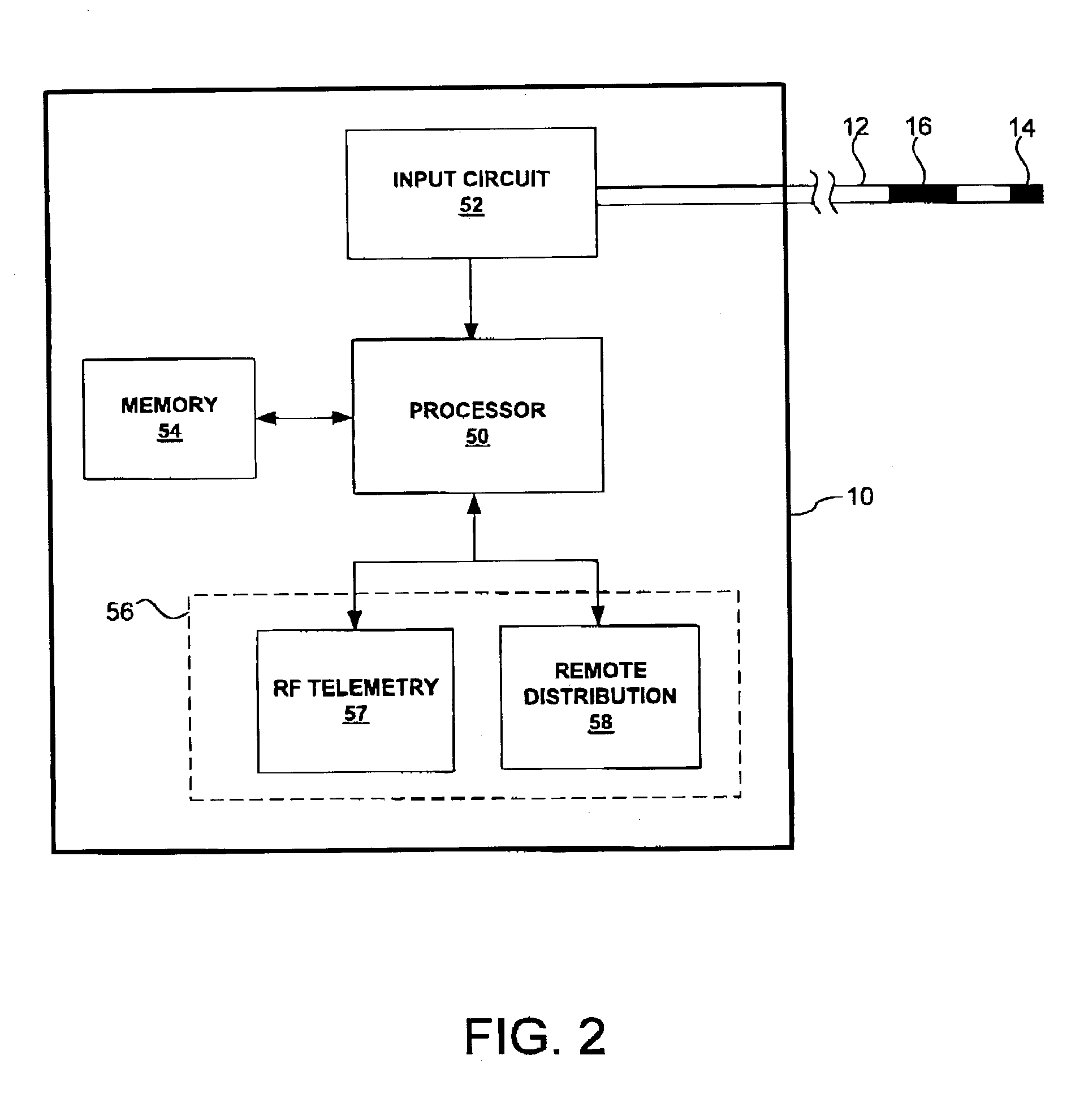
Estimation of stroke volume cardiac output using an intracardiac pressure sensor
InactiveUS7024244B2Similar level of accuracyMore accurate or less resource intensive estimationHeart stimulatorsSensorsTime functionVelocity time integral
Techniques are described for estimating a rate of blood flow from a heart, such as a stroke volume or a cardiac output, as a function of a pressure in the heart. A pressure monitor may measure pressure values, and identify the times at which pressure values and valve opening and closing occur. The pressure monitor may estimate a velocity-time function as a function of the measured pressures and identified times, and may calculate a velocity-time integral by integrating the velocity-time function. The pressure monitor may also calculate an estimated velocity-time integral directly as a function of the measured pressures and the identified times. The pressure monitor may calculate the stroke volume or cardiac output using the velocity-time integral. The pressure monitor may control a delivery of therapy by an implantable medical device as a function of the stroke volume or cardiac output.
Owner:MEDTRONIC INC
Arterial pressure-based, automatic determination of a cardiovascular parameter
One or more cardiovascular parameters is estimated as a function of the arterial pressure waveform, in particular, using at least one statistical moment of pressure waveform having an order greater than one. Arterial compliance, the exponential pressure decay constant, vascular resistance, cardiac output, and stroke volume are examples of cardiovascular parameters that can be estimated using various aspects of the invention. In one embodiment of the invention, not only are the first four moments (mean, standard deviation, skewness, and kurtosis) of the pressure waveform used to estimate the cardiovascular parameter(s) of interest, but also heart rate, statistical moments of a set of pressure-weighted time values, and certain anthropometric patient measurements such as age, sex, body surface area, etc.
Owner:EDWARDS LIFESCIENCES CORP
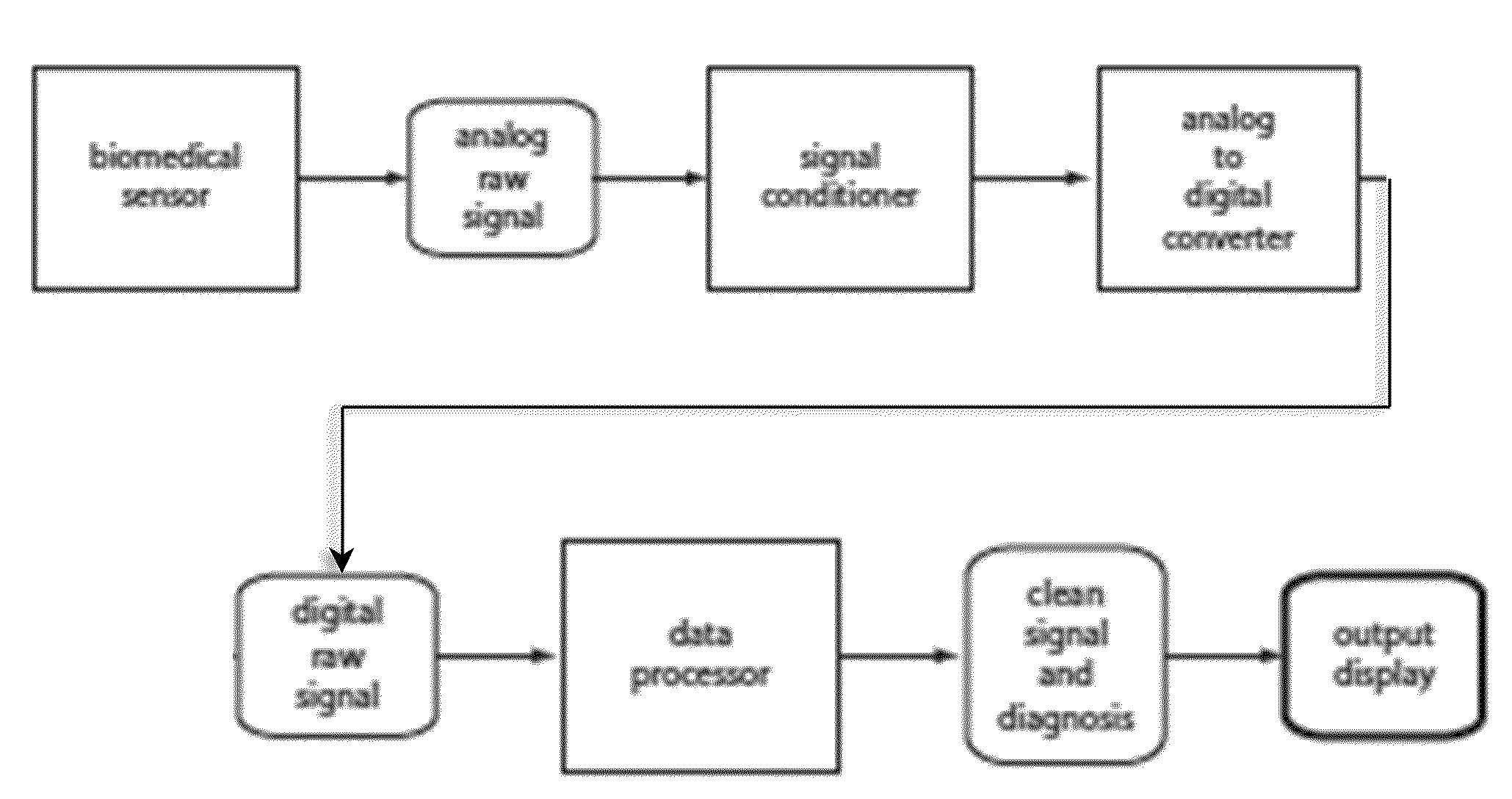
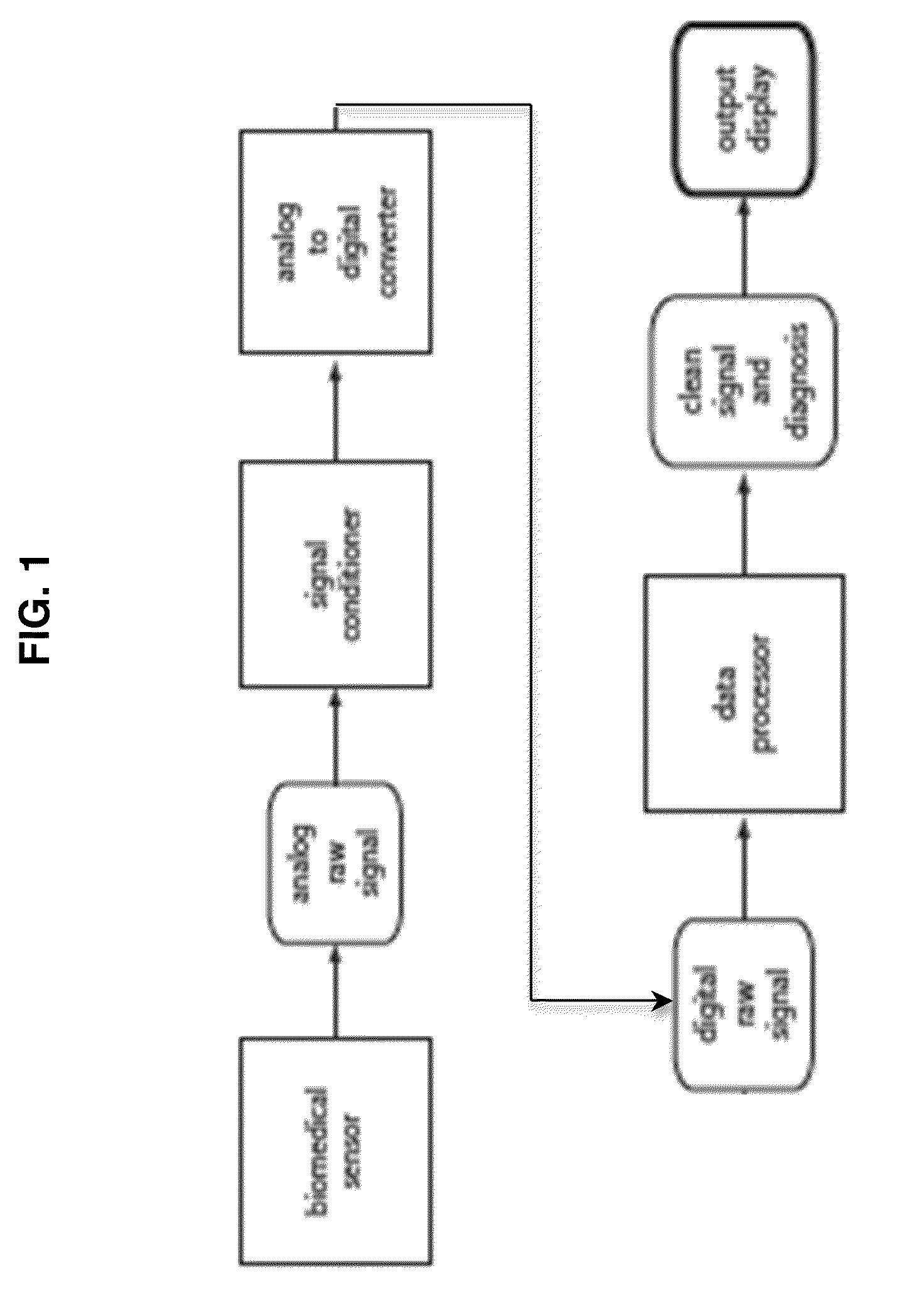
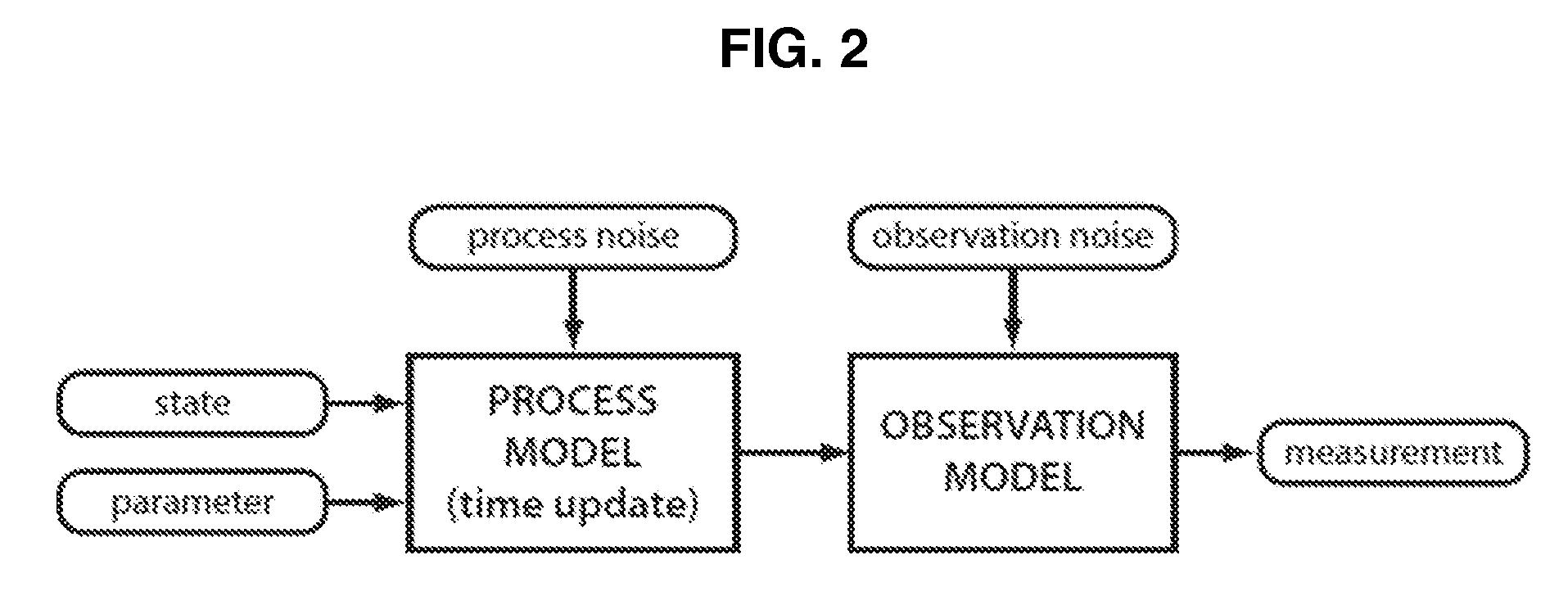
Processing Physiological Sensor Data Using a Physiological Model Combined with a Probabilistic Processor
InactiveUS20100274102A1Reliable and accurate measurementCharacter and pattern recognitionDiagnostic recording/measuringPulse oximetersSigma point
A pulse oximeter system comprises a data processor configured to perform a method that combines a sigma point Kalman filter (SPKF) or sequential Monte Carlo (SMC) algorithm with Bayesian statistics and a mathematical model comprising a cardiovascular model and a plethysmography model to remove contaminating noise and artifacts from the pulse oximeter sensor output and measure blood oxygen saturation, heart rate, left-ventricular stroke volume, aortic pressure and systemic pressures.
Owner:VITAL METRIX INC
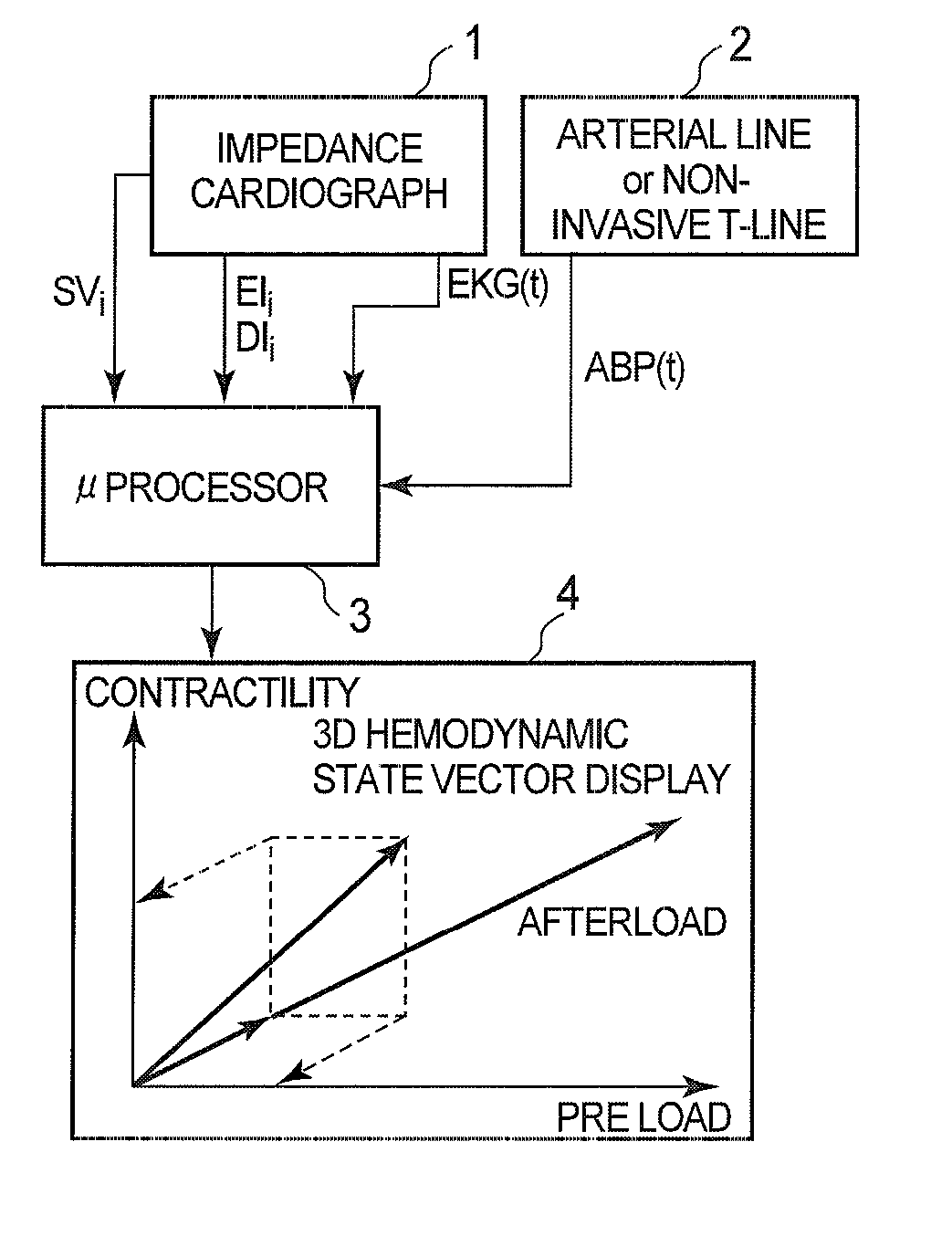
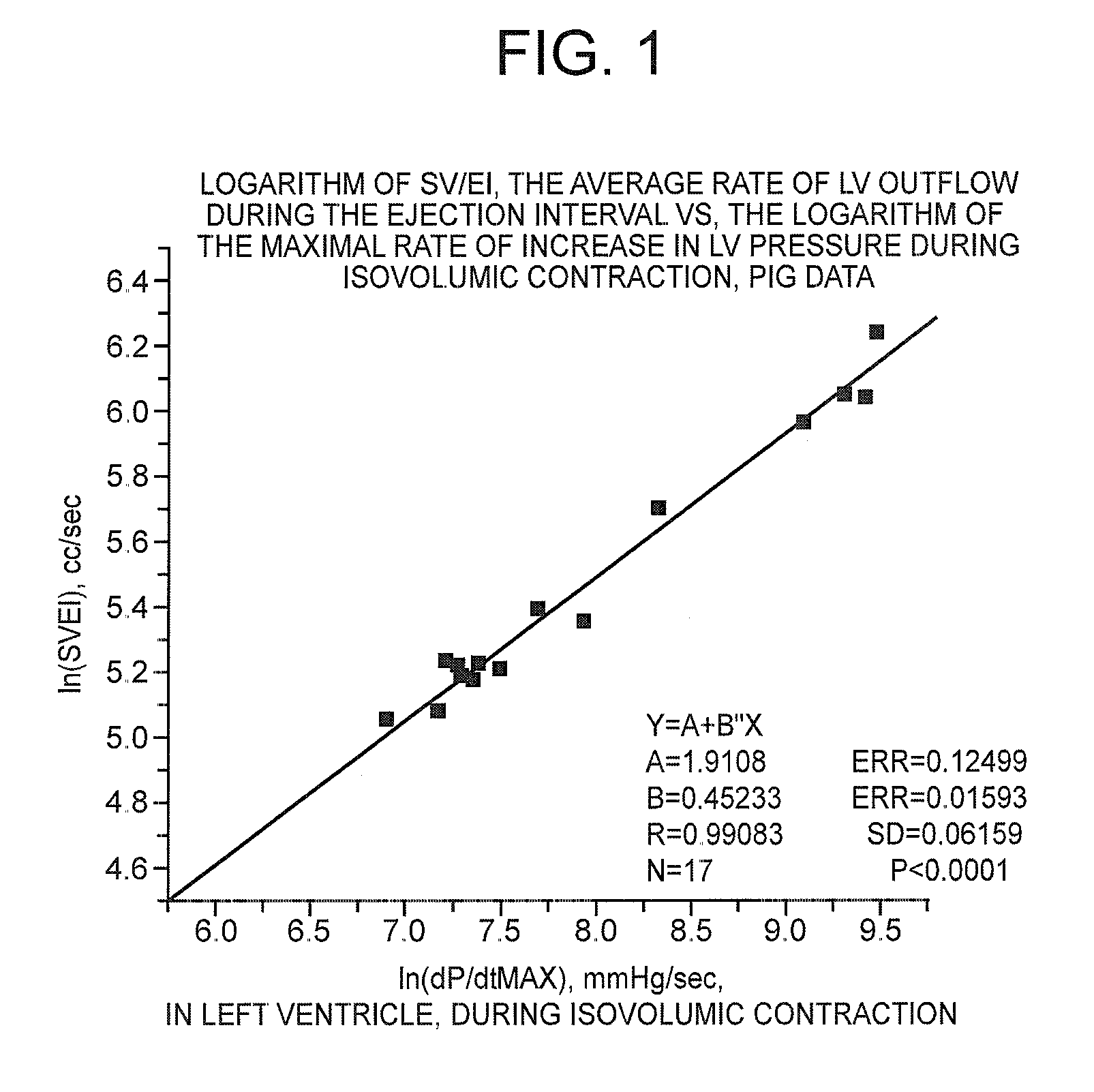
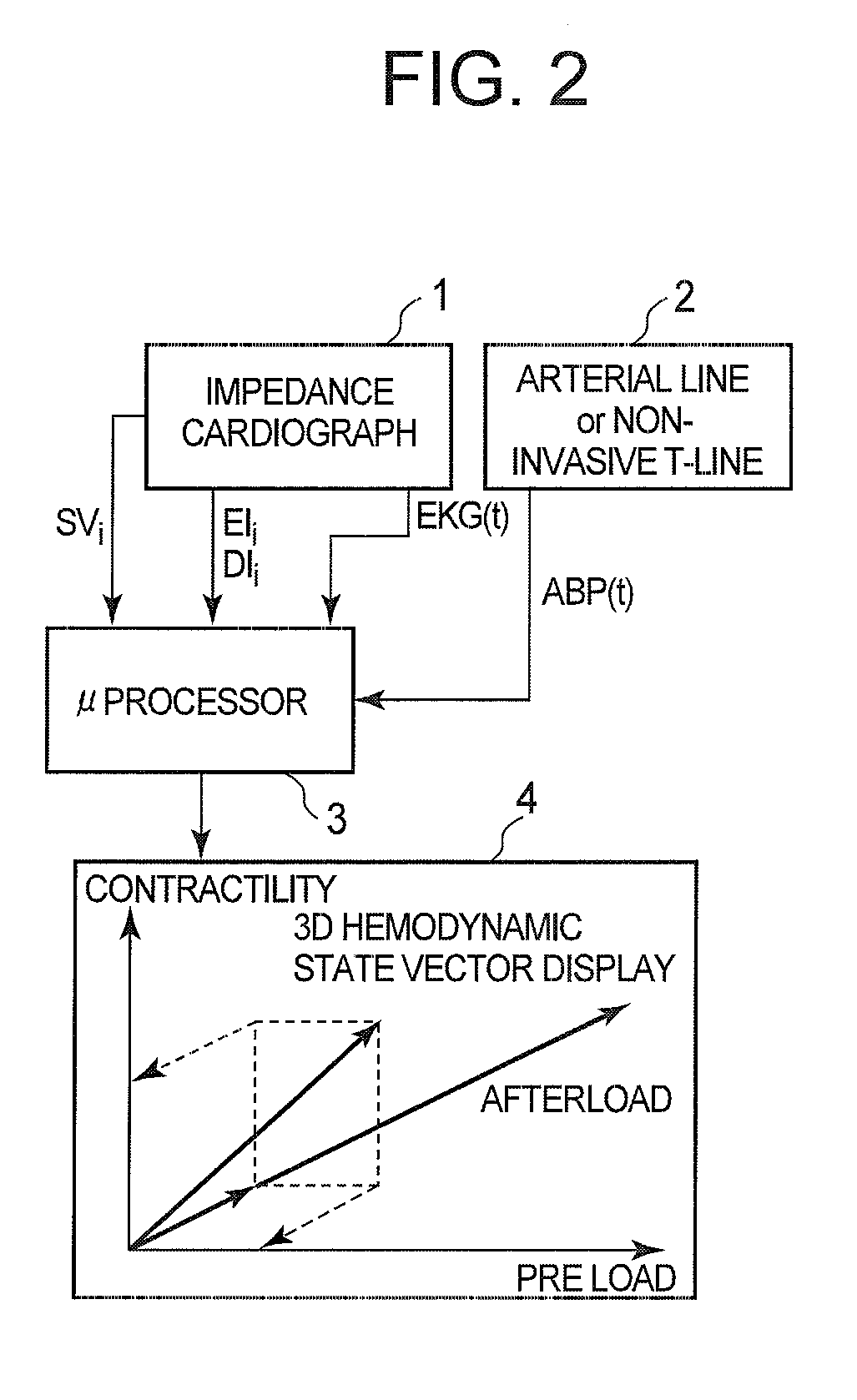
Non-invasive method and device to monitor cardiac parameters without use of electrical-mechanical interval
InactiveUS20070191724A1Easy to measureSimple processElectrocardiographyBlood flow measurement devicesDiastolic intervalCardiac cycle
A method of and a device for non-invasively measuring the hemodynamic state of a subject or a human patient involve steps and units of non-invasively or minimally invasively measuring cardiac cycle period, mean arterial pressure, stroke volume, diastolic interval and ejection interval and converting the measured mean arterial pressure, stroke volume, diastolic interval and ejection interval into the cardiac parameters such as Preload, Afterload and Contractility, which are the common cardiac parameters used by an anesthesiologist. In the current invention, the use of electrical-mechanical interval has been eliminated for various advantageous reasons. The converted hemodynamic state of a patient is displayed on a screen as a three-dimensional vector with each of its three coordinates respectively representing Preload, Afterload and Contractility. Therefore, a medical practitioner looks at the screen and—quickly obtains the important and necessary information.
Owner:HIRSH ROBERT
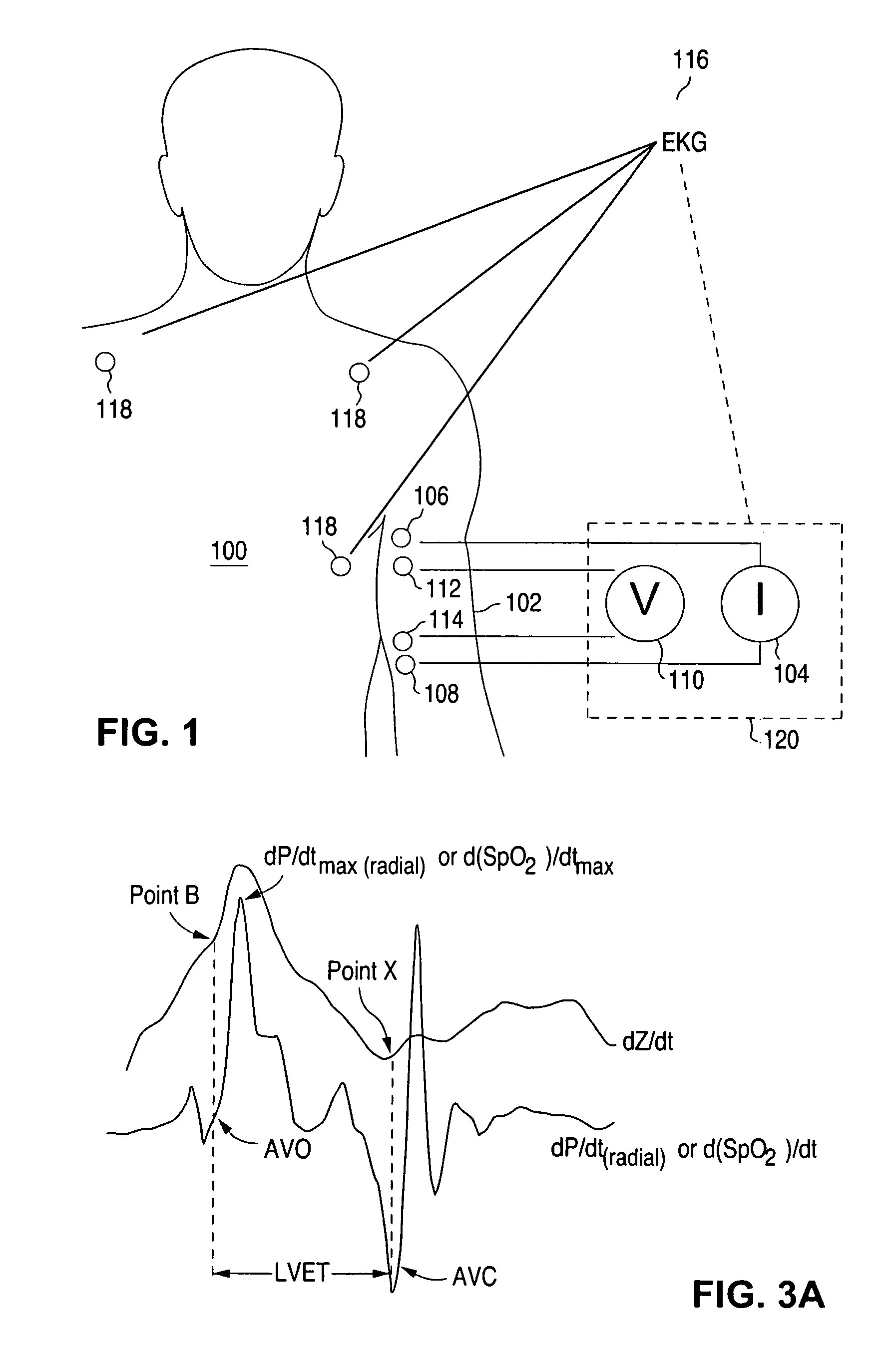
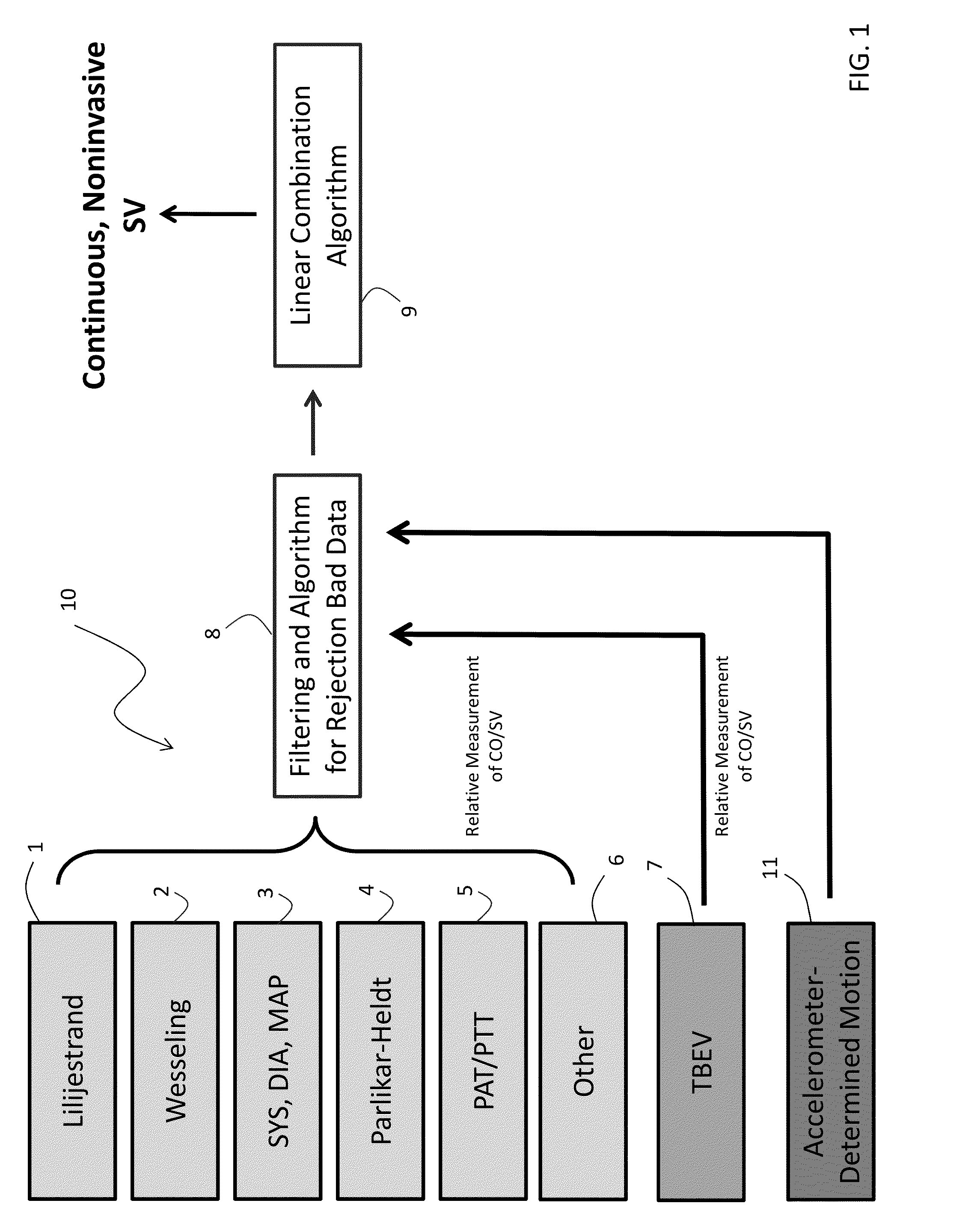
Body-worn system for continuous, noninvasive measurement of cardiac output, stroke volume, cardiac power, and blood pressure
ActiveUS20140249431A1Accurate estimateEffective monitoringDiagnostic signal processingEvaluation of blood vesselsEcg signalBlood pressure
The invention provides a system for measuring stroke volume (SV), cardiac output (CO), and cardiac power (CP) from a patient that features: 1) an impedance sensor connected to at least two body-worn electrodes and including an impedance circuit that processes analog signals from the electrodes to measure an impedance signal (e.g. TBEV waveform); 2) an ECG sensor connected to at least two chest-worn electrodes and including an ECG circuit that processes analog signals from the electrodes to measure and ECG signal; 3) an optical sensor connected to a body-worn optical probe and including an optical circuit that processes signals from the probe to measure at least one optical signal (e.g. a PPG waveform) from the patient; 4) a processing system, typically worn on the patient's wrist and connected through a wired interface to the optical sensor, and through either a wired or wireless interface to the TBEV and ECG sensors.
Owner:SOTERA WIRELESS
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com