Patents
Literature
230 results about "Decreased mean arterial pressure" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
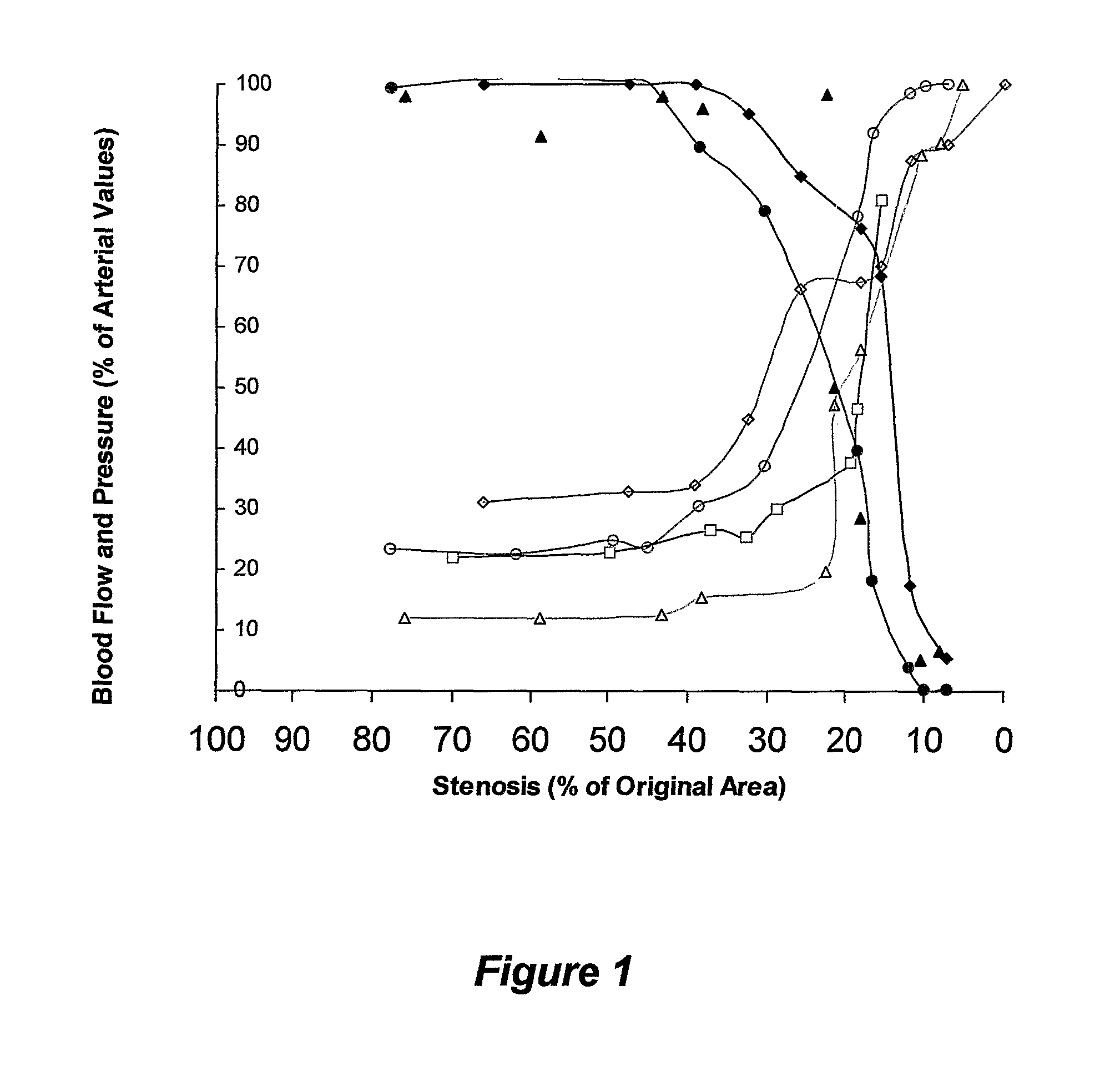
When arterial pressure and blood flow decrease beyond a certain point, the perfusion of the brain becomes critically decreased (i.e., the blood supply is not sufficient), causing lightheadedness, dizziness, weakness or fainting.
Methods and systems for treating ischemia
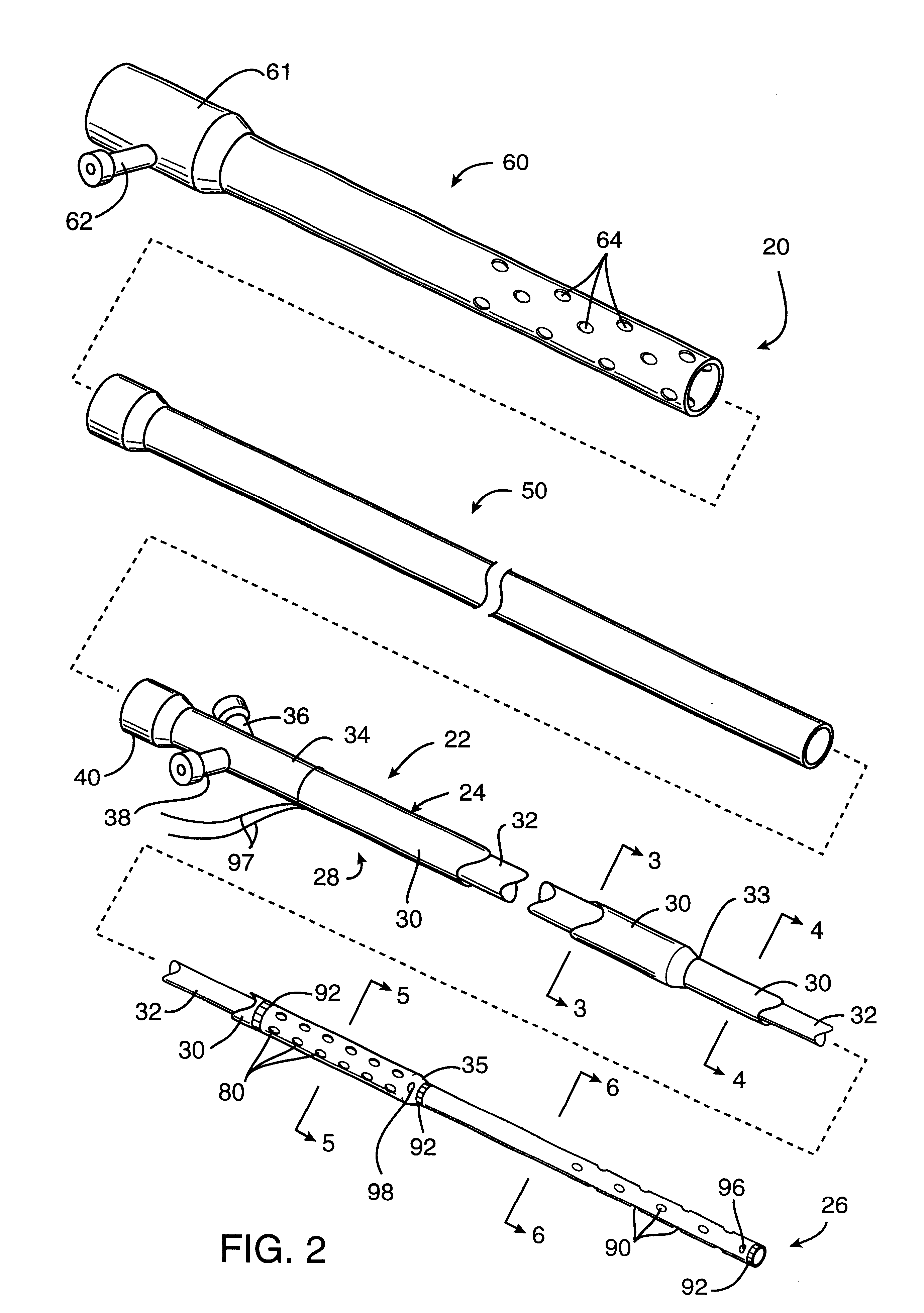
InactiveUS6295990B1Promote dissolution and removalMinimize and prevent ischemiaStentsBalloon catheterControl mannerDecreased mean arterial pressure
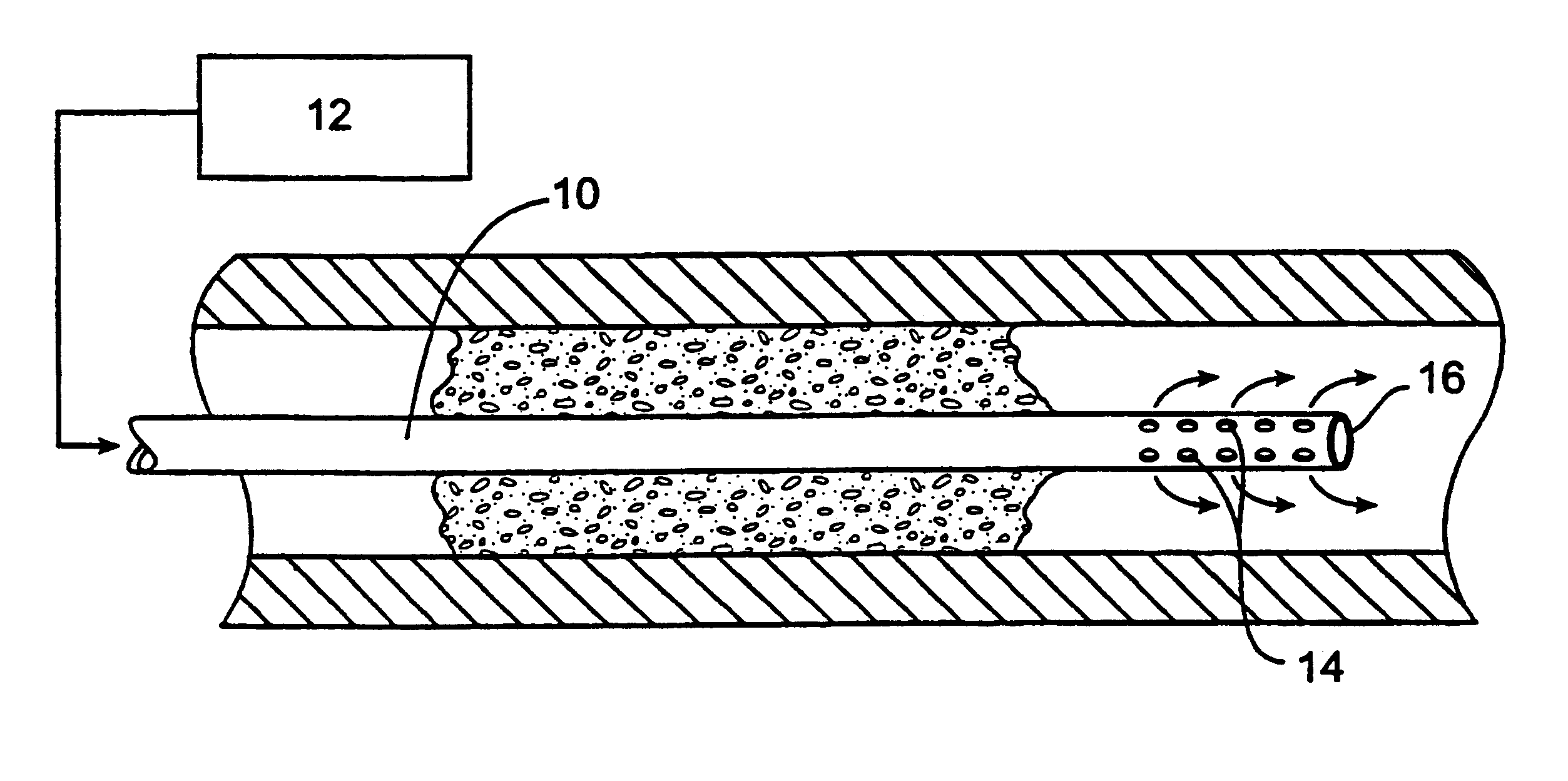
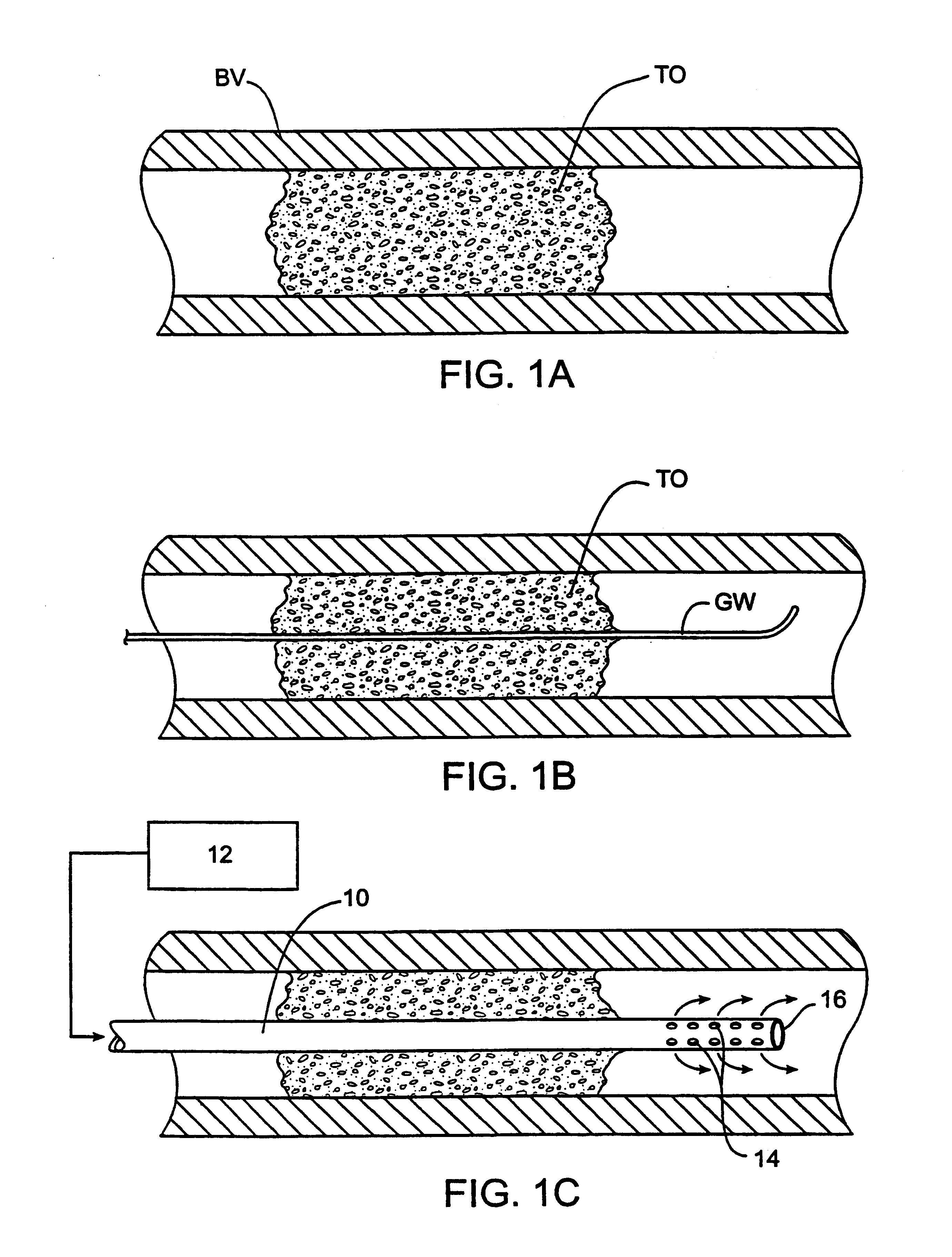
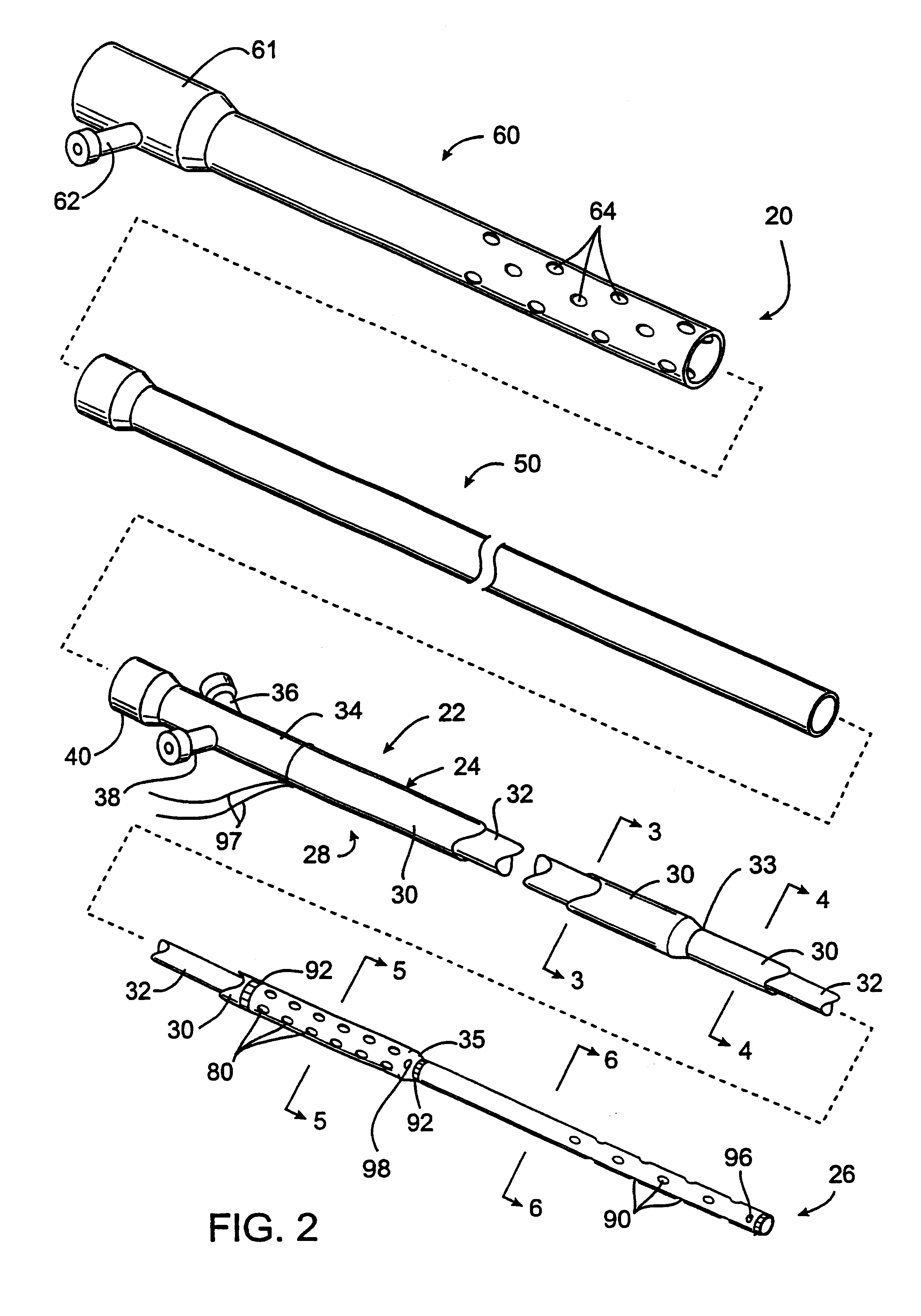
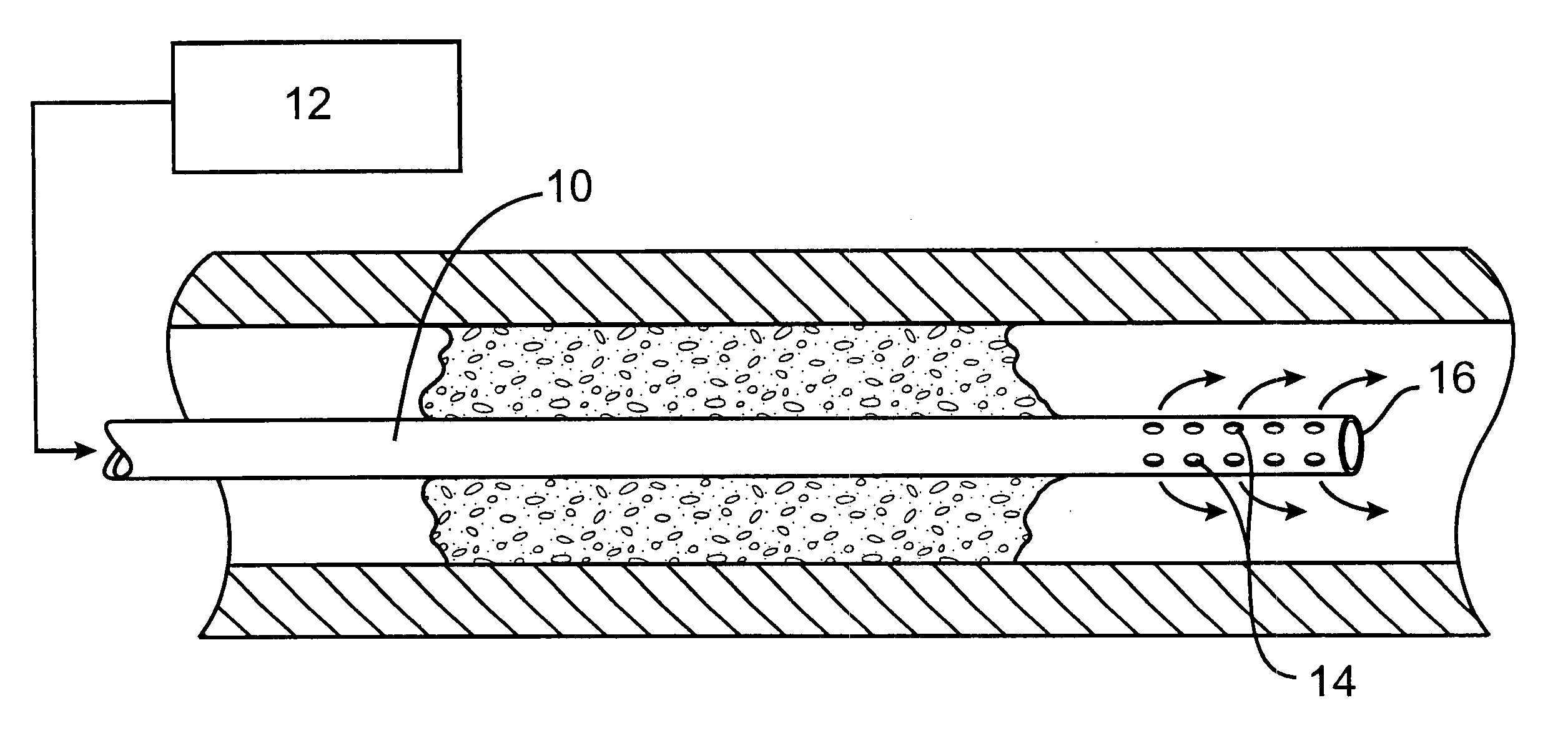
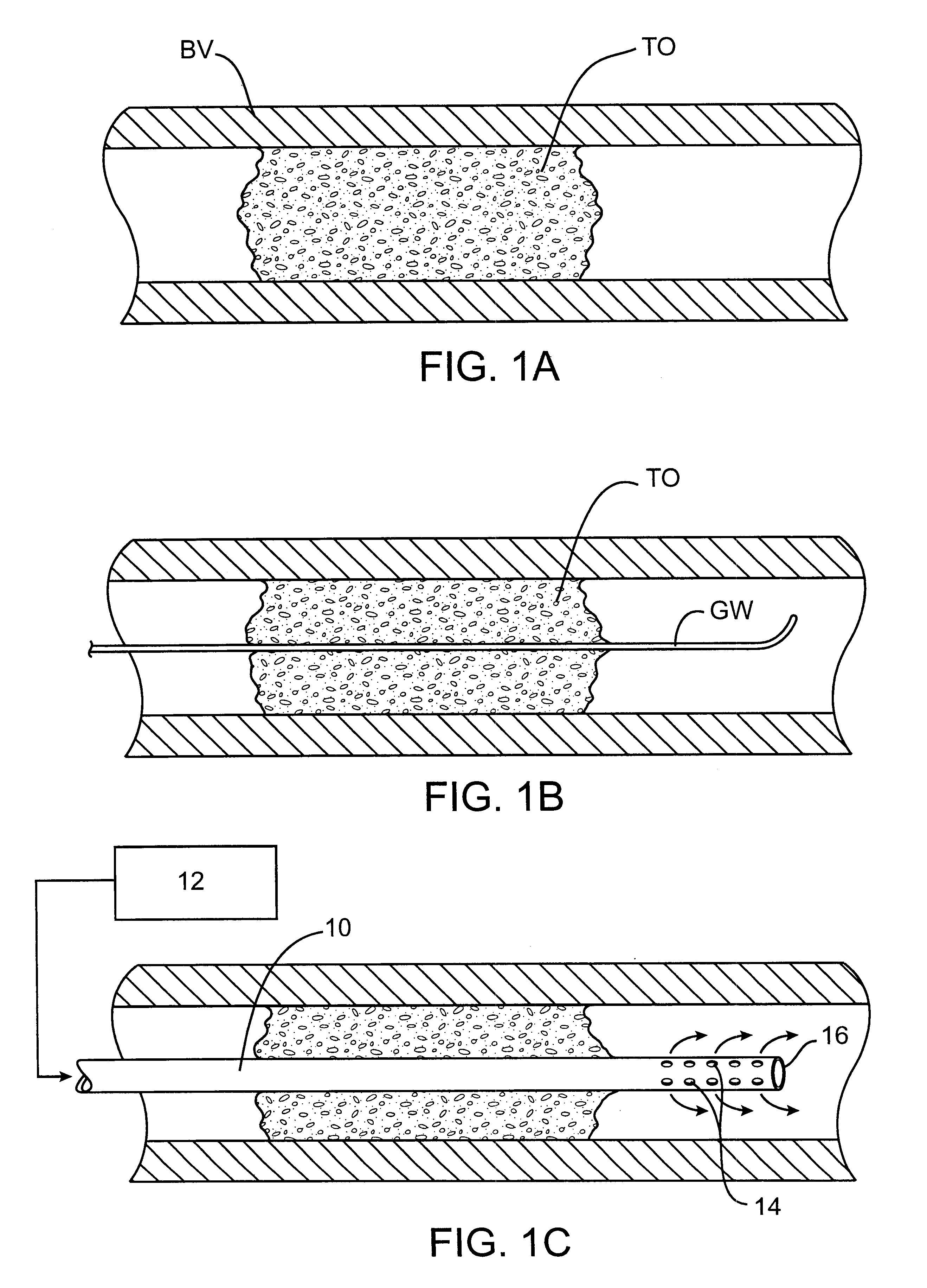
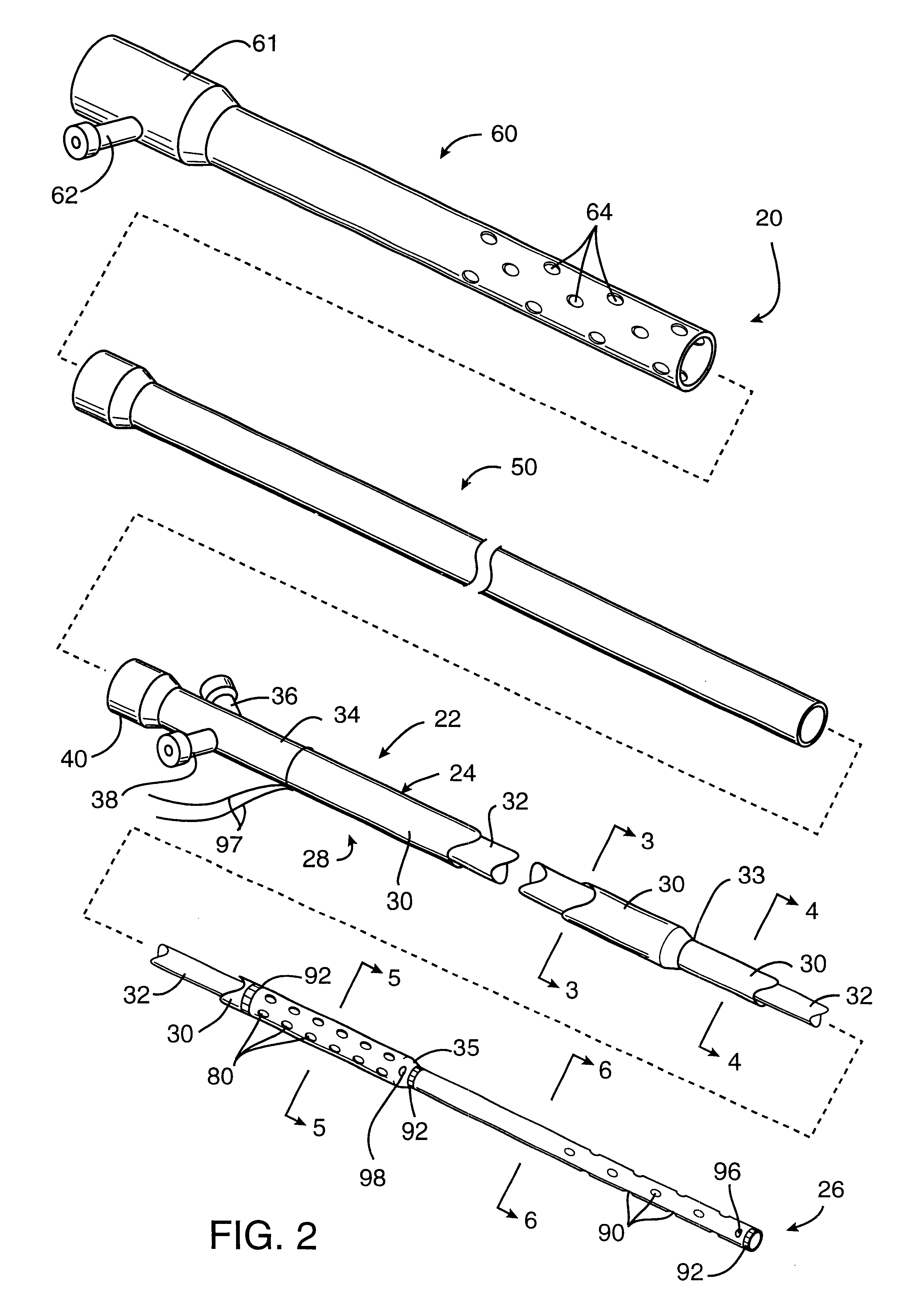
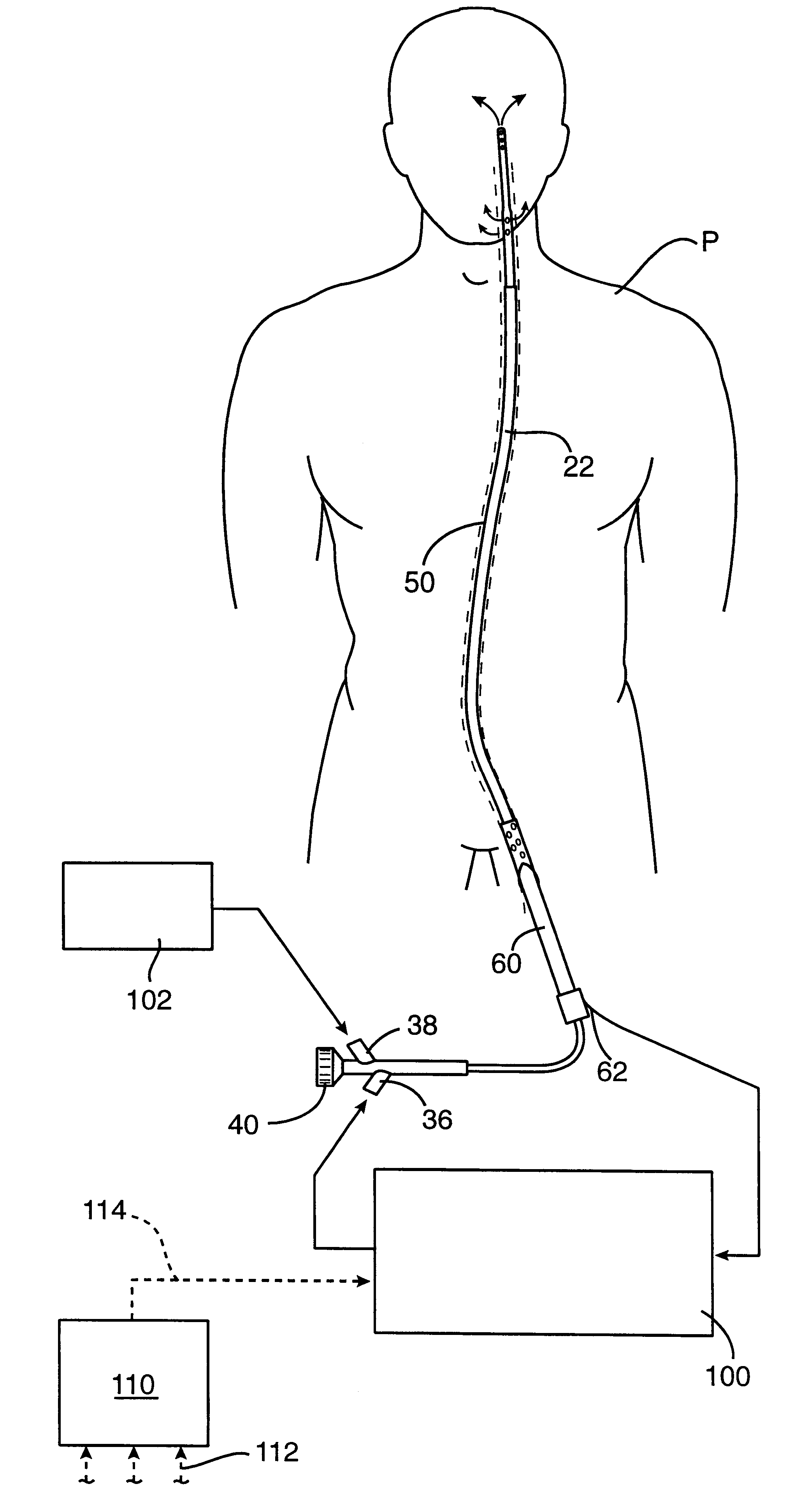
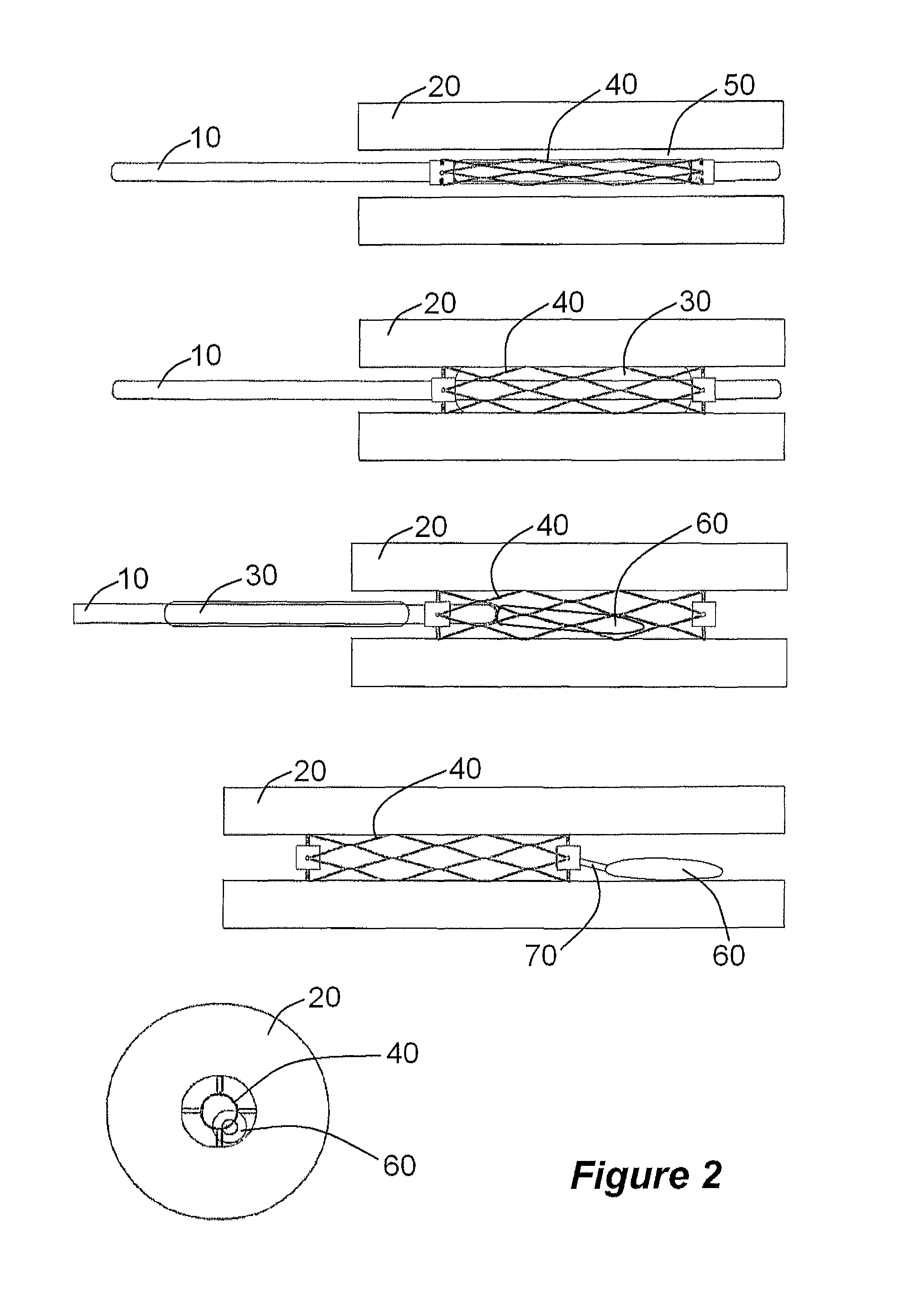
Methods for treating total and partial occlusions employ a perfusion conduit which is penetrated through the occlusive material. Oxygenated blood or other medium is then perfused through the conduit in a controlled manner, preferably at a controlled pressure below the arterial pressure, to maintain oxygenation and relieve ischemia in tissue distal to the occlusion. In another aspect, interventional devices, such as stents or balloon catheters, are passed through the perfusion catheter to remove obstructions. Optionally, the occlusion may be treated while perfusion is maintained, typically by introducing a thrombolytic or other agent into the occlusive material using the perfusion conduit or by employing mechanical means to remove the obstruction. Such methods are particularly suitable for treating acute stroke to prevent damage to the cerebral tissue.
Owner:SALIENT INTERVENTIONAL SYST
Methods and systems for treating ischemia
InactiveUS6435189B1Promote dissolution and removalMinimize and prevent ischemiaStentsBalloon catheterControl mannerDecreased mean arterial pressure
Methods for treating total and partial occlusions employ a perfusion conduit which is penetrated through the occlusive material. Oxygenated blood or other medium is then perfused through the conduit in a controlled manner, preferably at a controlled pressure below the arterial pressure, to maintain oxygenation and relieve ischemia in tissue distal to the occlusion. In another aspect, interventional devices, such as stents or balloon catheters, are passed through the perfusion catheter to remove obstructions. Optionally, the occlusion may be treated while perfusion is maintained, typically by introducing a thrombolytic or other agent into the occlusive material using the perfusion conduit or by employing mechanical means to remove the obstruction. Such methods are particularly suitable for treating acute stroke to prevent damage to the cerebral tissue.
Owner:SALIENT INTERVENTIONAL SYST
Methods and systems for treating ischemia
InactiveUS6436087B1Promote dissolution and removalMinimize and prevent ischemiaStentsBalloon catheterControl mannerThrombus
Methods for treating total and partial occlusions employ a perfusion conduit which is penetrated through the occlusive material. Oxygenated blood or other medium is then perfused through the conduit in a controlled manner, preferably at a controlled pressure below the arterial pressure, to maintain oxygenation and relieve ischemia in tissue distal to the occlusion. In another aspect, interventional devices, such as stents or balloon catheters, are passed through the perfusion catheter to remove obstructions. Optionally, the occlusion may be treated while perfusion is maintained, typically by introducing a thrombolytic or other agent into the occlusive material using the perfusion conduit or by employing mechanical means to remove the obstruction. Such methods are particularly suitable for treating acute stroke to prevent damage to the cerebral tissue.
Owner:SALIENT INTERVENTIONAL SYST
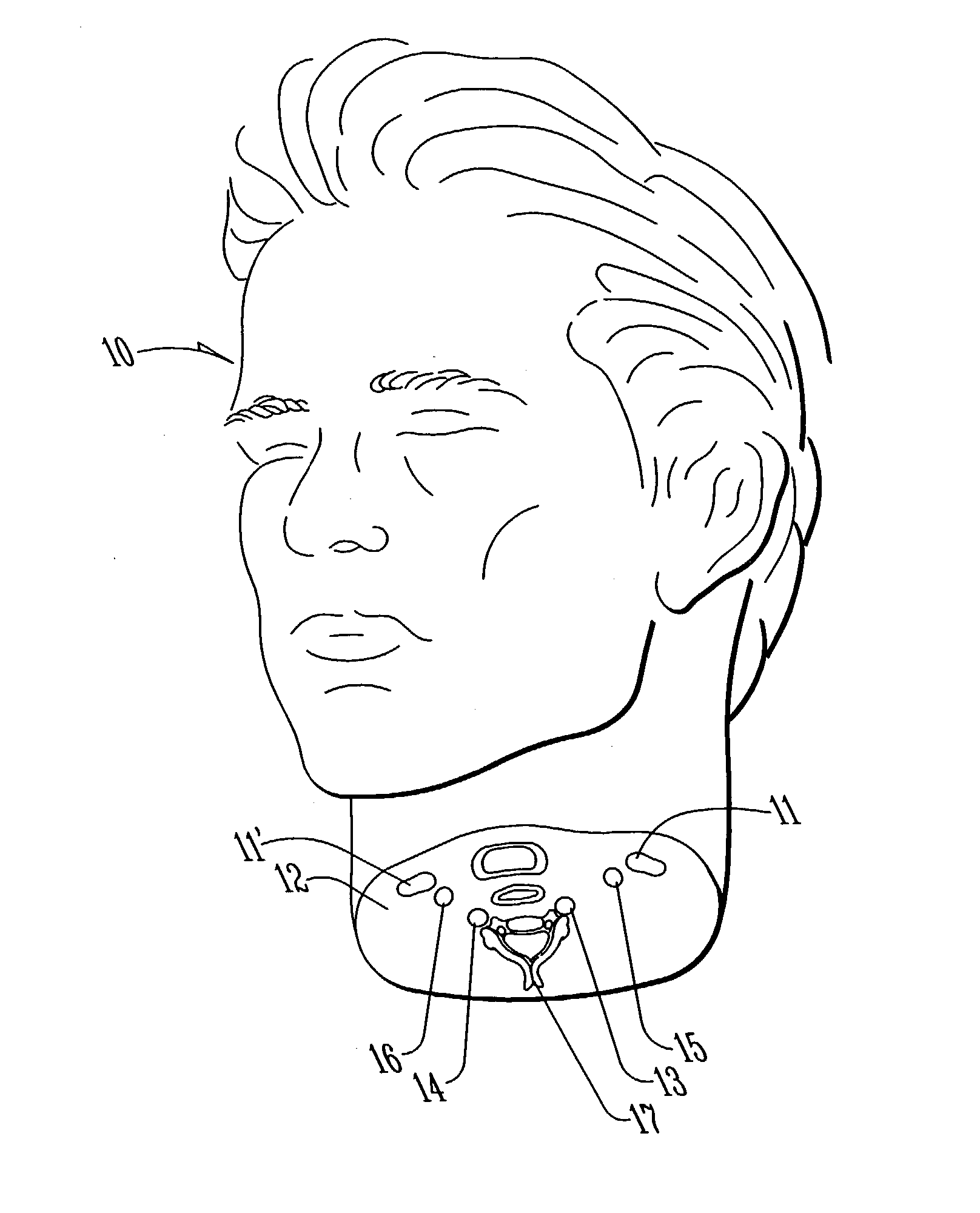
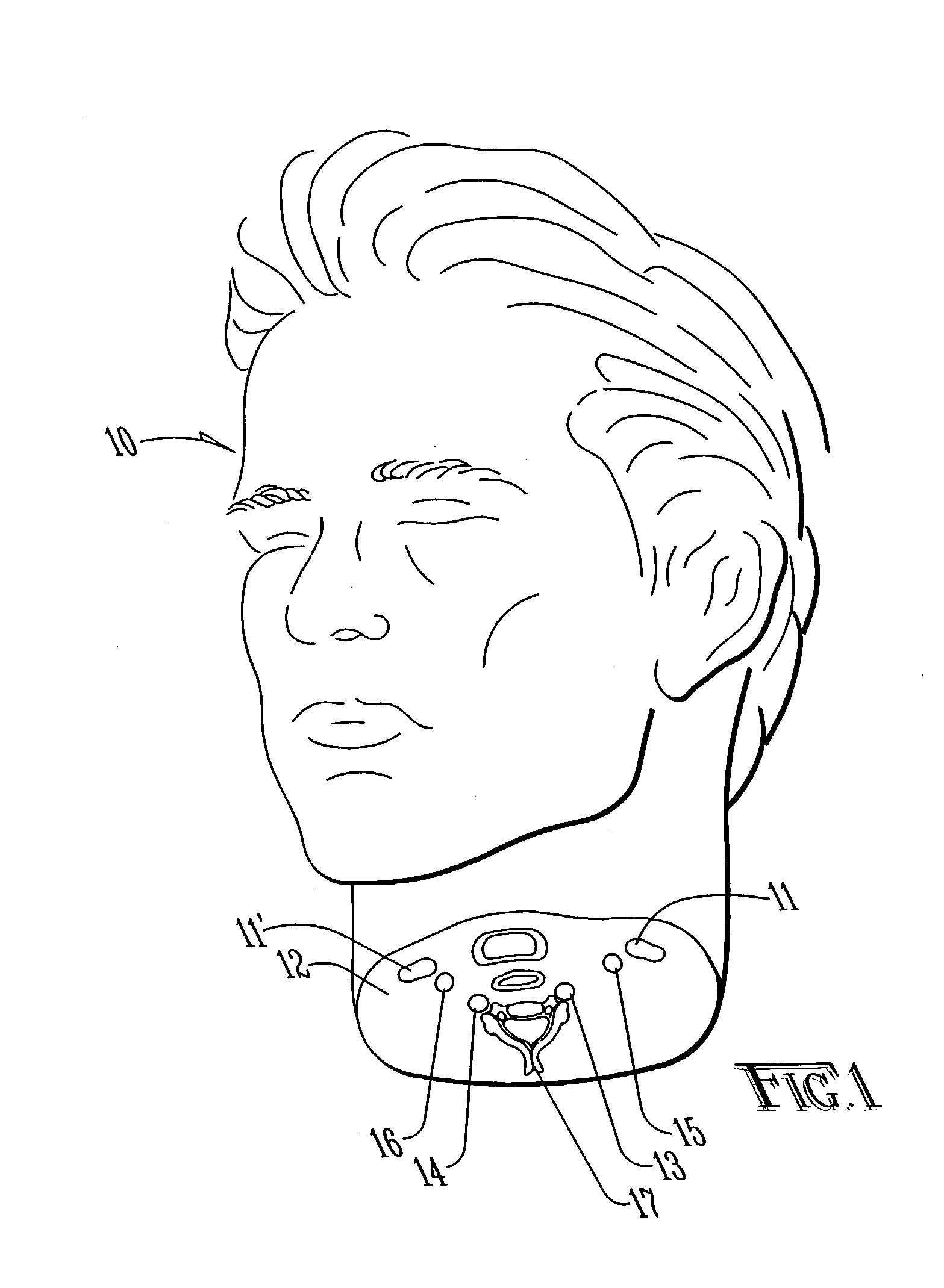
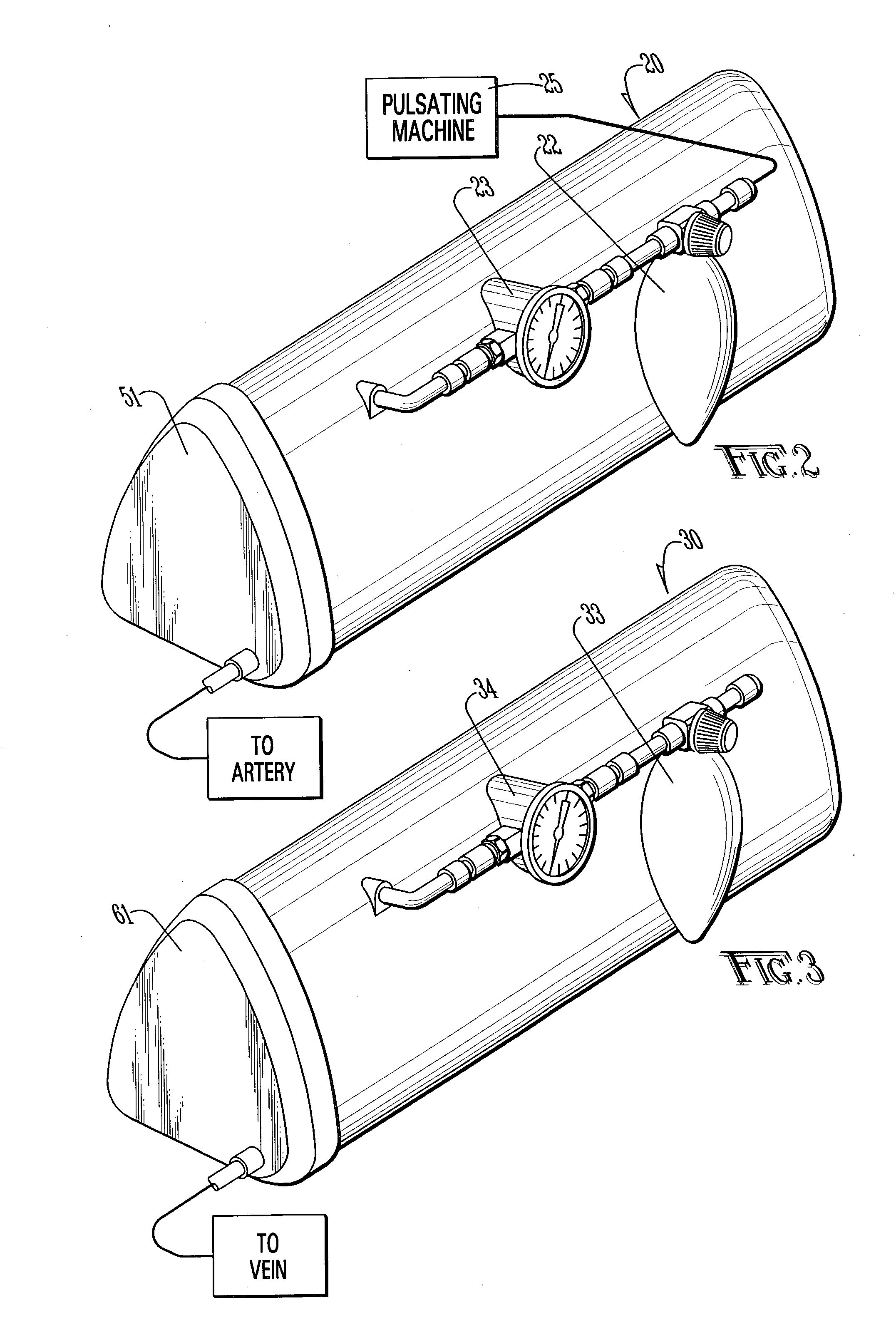
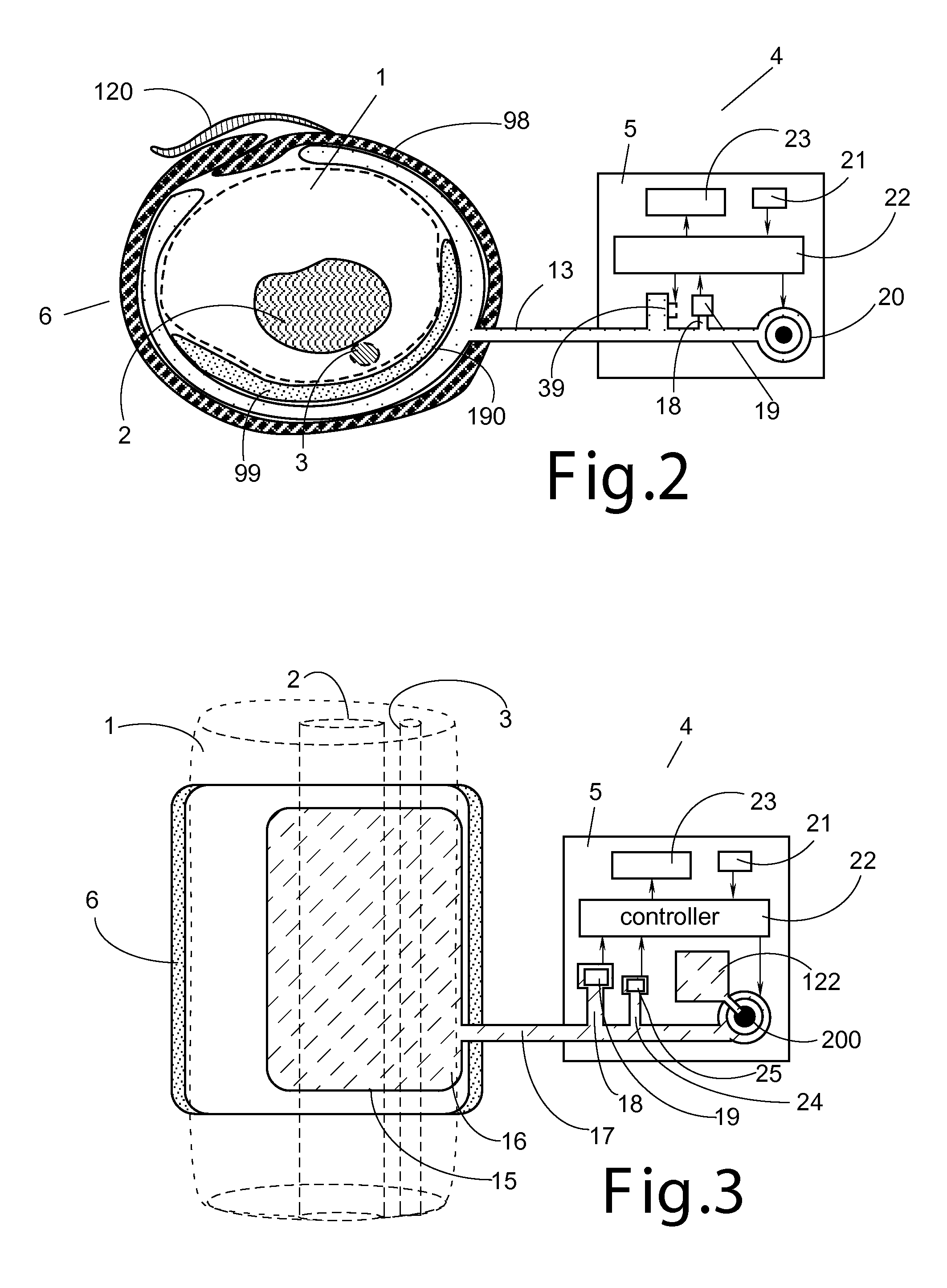
Method and apparatus for surgical training
An apparatus and method for microsurgical training using cadaveric anatomy with filling of the vascular system by fluids under pressure to simulate the appearance and function of live surgery. One or more arteries on the specimen of cadaveric anatomy are cannulated and connected to an arterial reservoir having a flexible container holding an arterial fluid simulating the appearance of blood circulating in the arteries of the living organism from which the cadaveric anatomy is derived. Suitable static pressure simulating the arterial pressure appropriate to that of the living organism is applied to the air in an air-tight space surrounding the flexible container in the arterial reservoir. A pulsating machine provides air pulsations to the space surrounding the flexible fluid container to simulate the normal pulsations of the arterial system. One or more veins on the specimen are also cannulated and connected to a venous reservoir having a flexible container holding a venous fluid simulating the appearance of blood circulating in the veins of the living organism. Suitable static pressure simulating the venous pressure appropriate to that of the living organism is applied to the air in an air-tight space surrounding the flexible container in the venous reservoir. Optionally, if the specimen includes at least a portion of spinal canal, a clear fluid reservoir can be connected to the specimen through the spinal canal to simulate cerebrospinal fluid.
Owner:ABOUD GHAITH +1
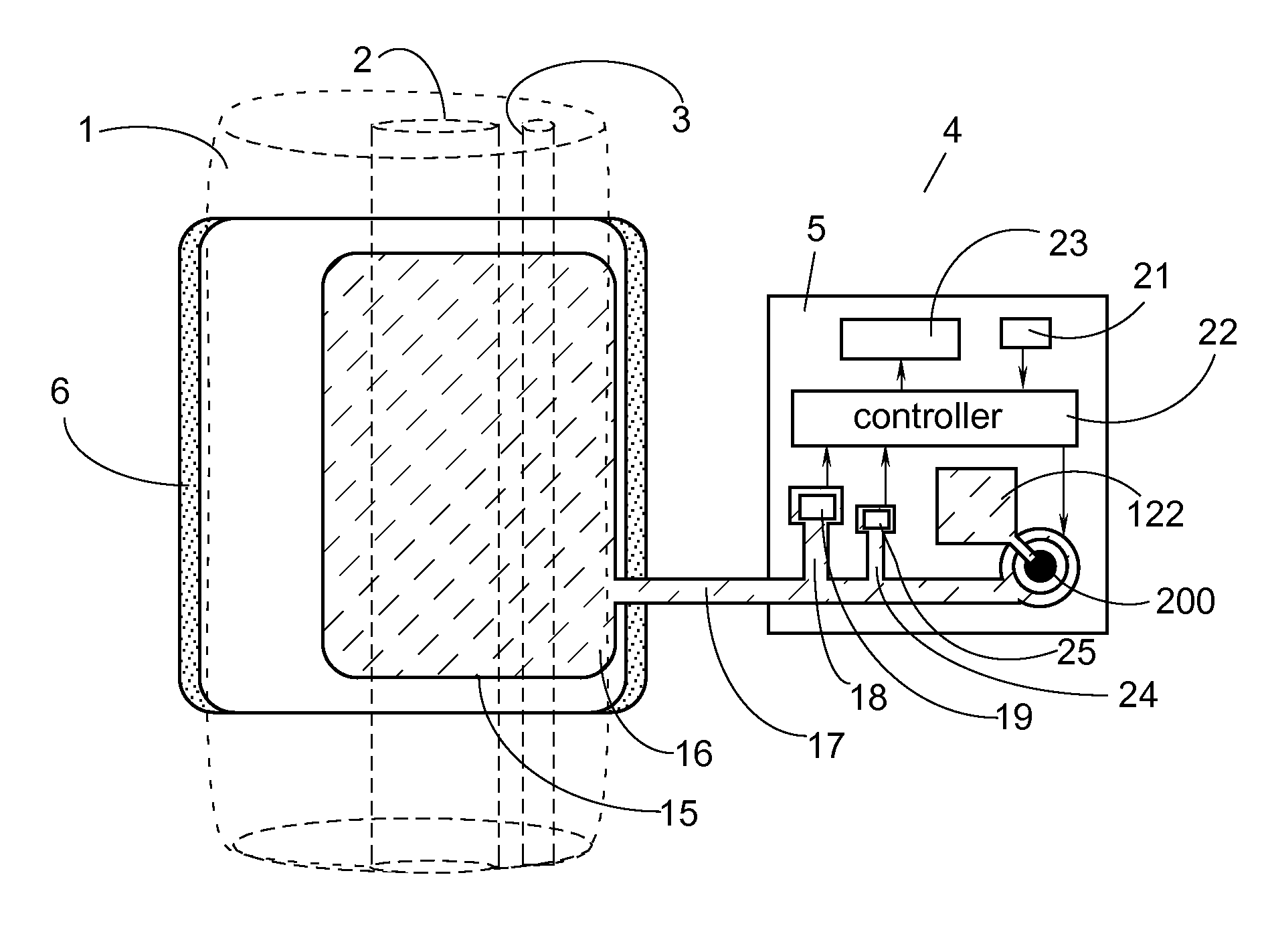
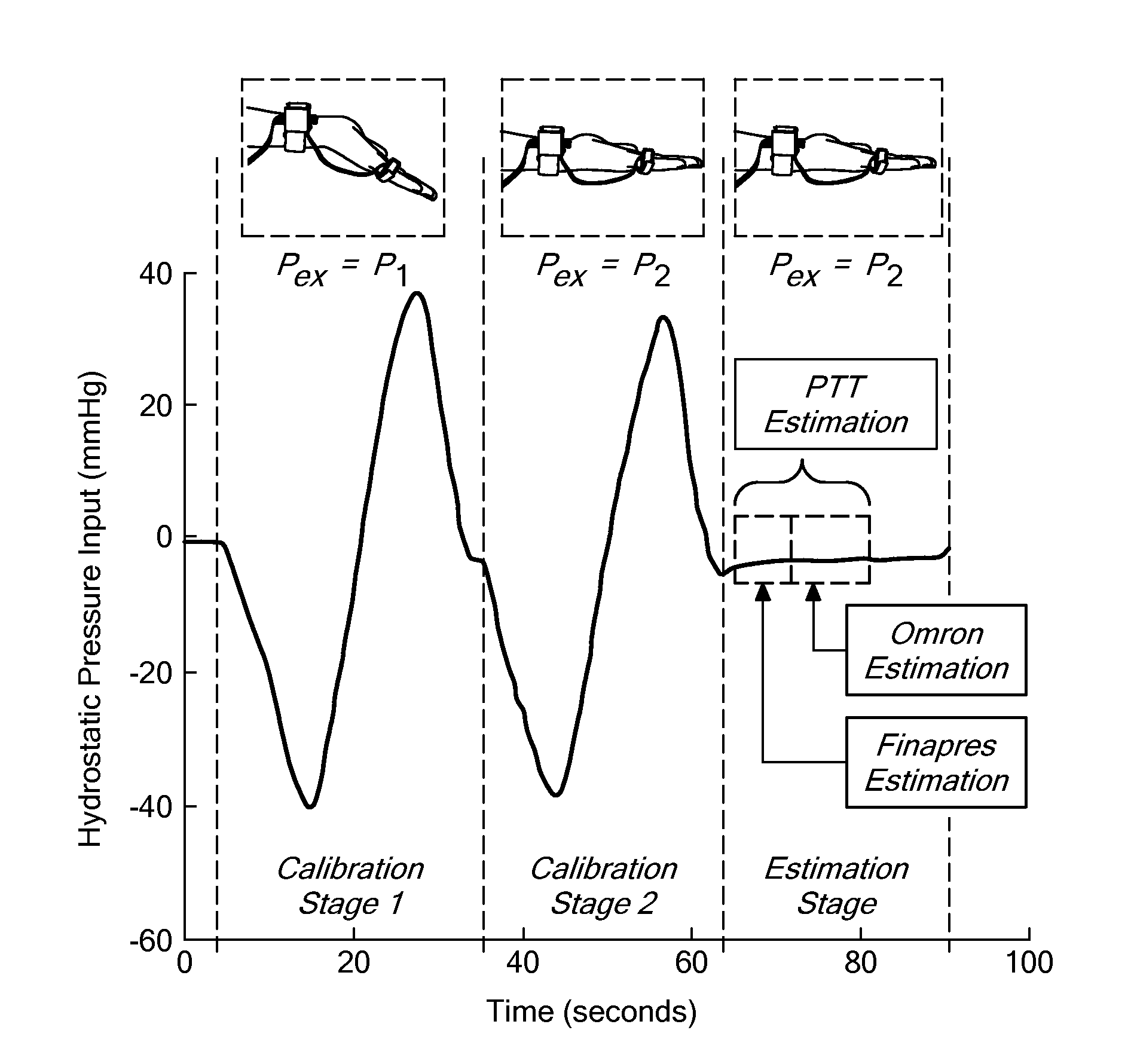
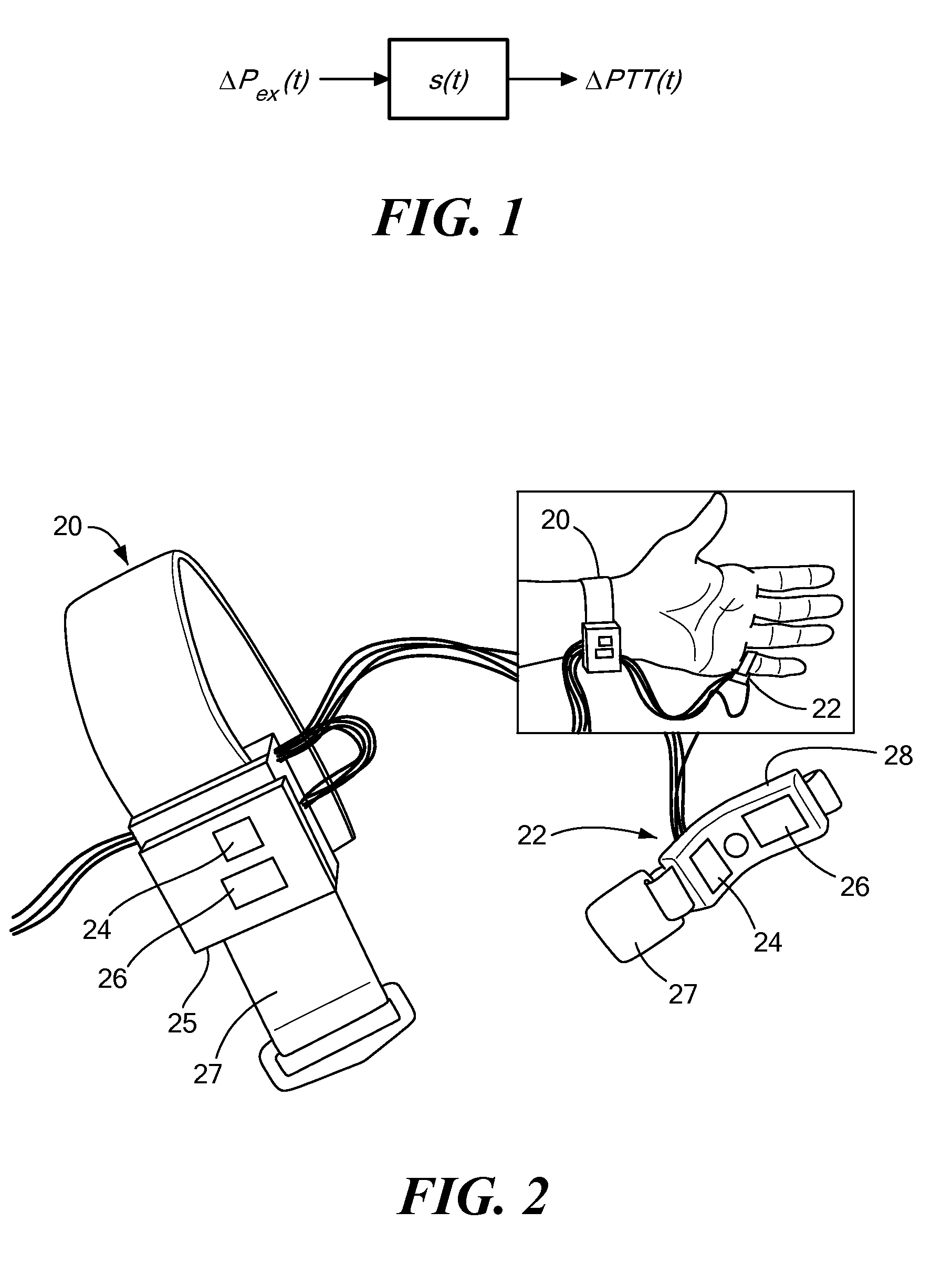
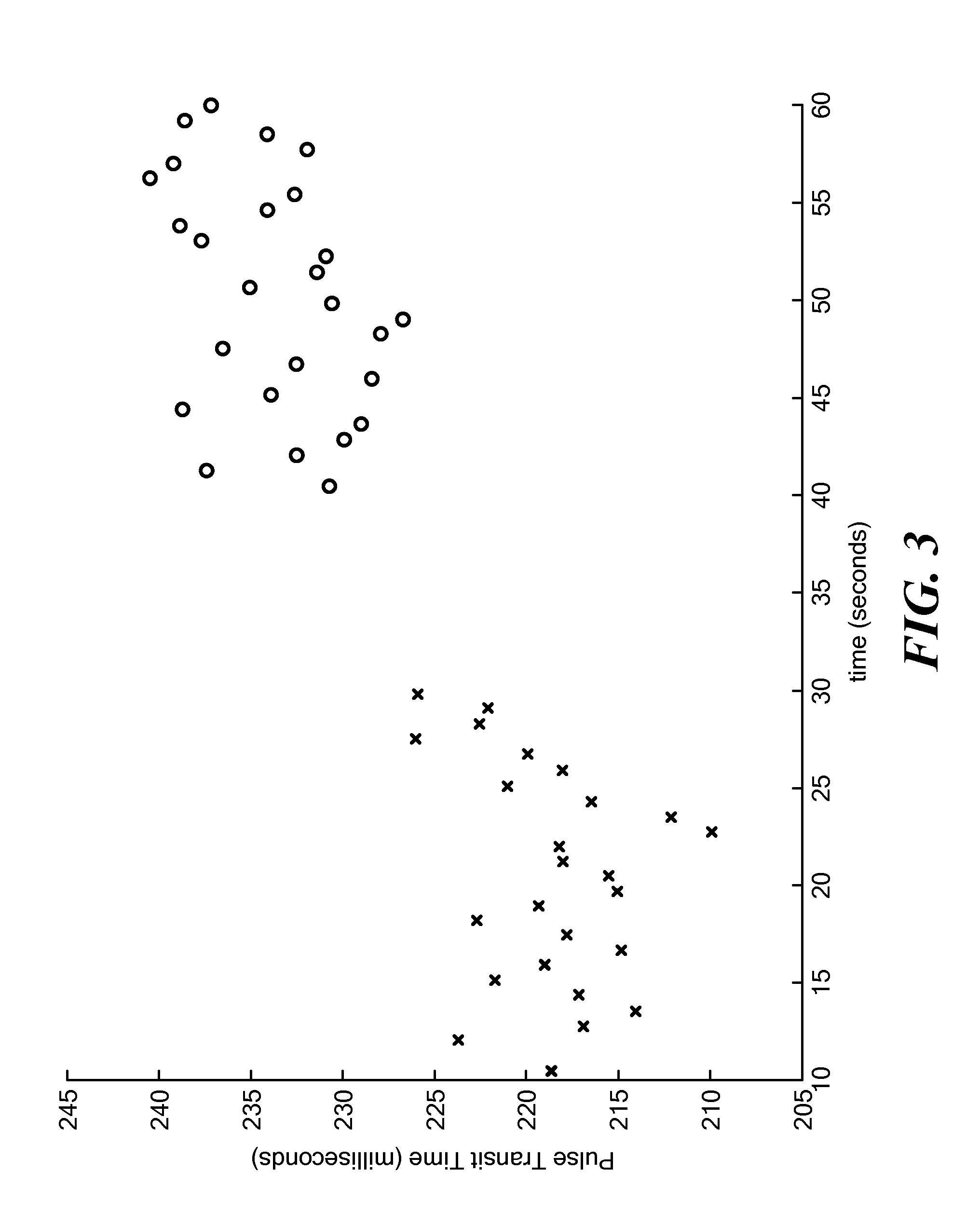
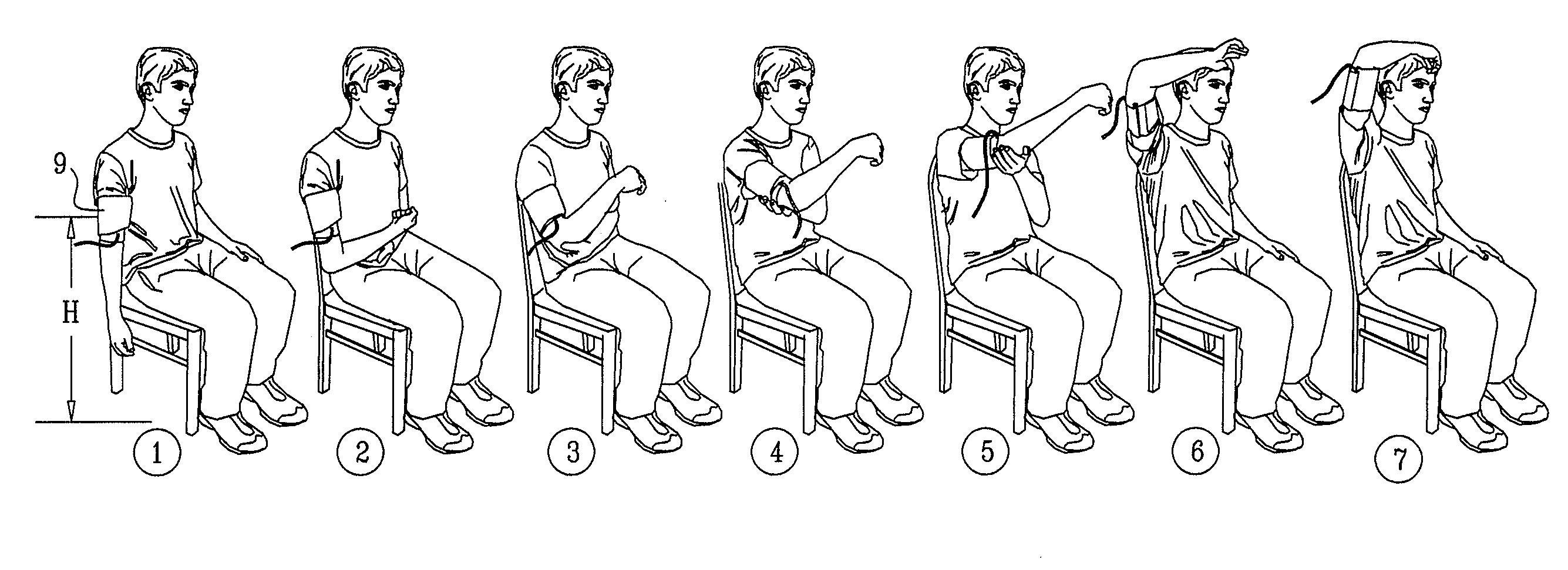
Calibration of Pulse Transit Time Measurements to Arterial Blood Pressure using External Arterial Pressure Applied along the Pulse Transit Path
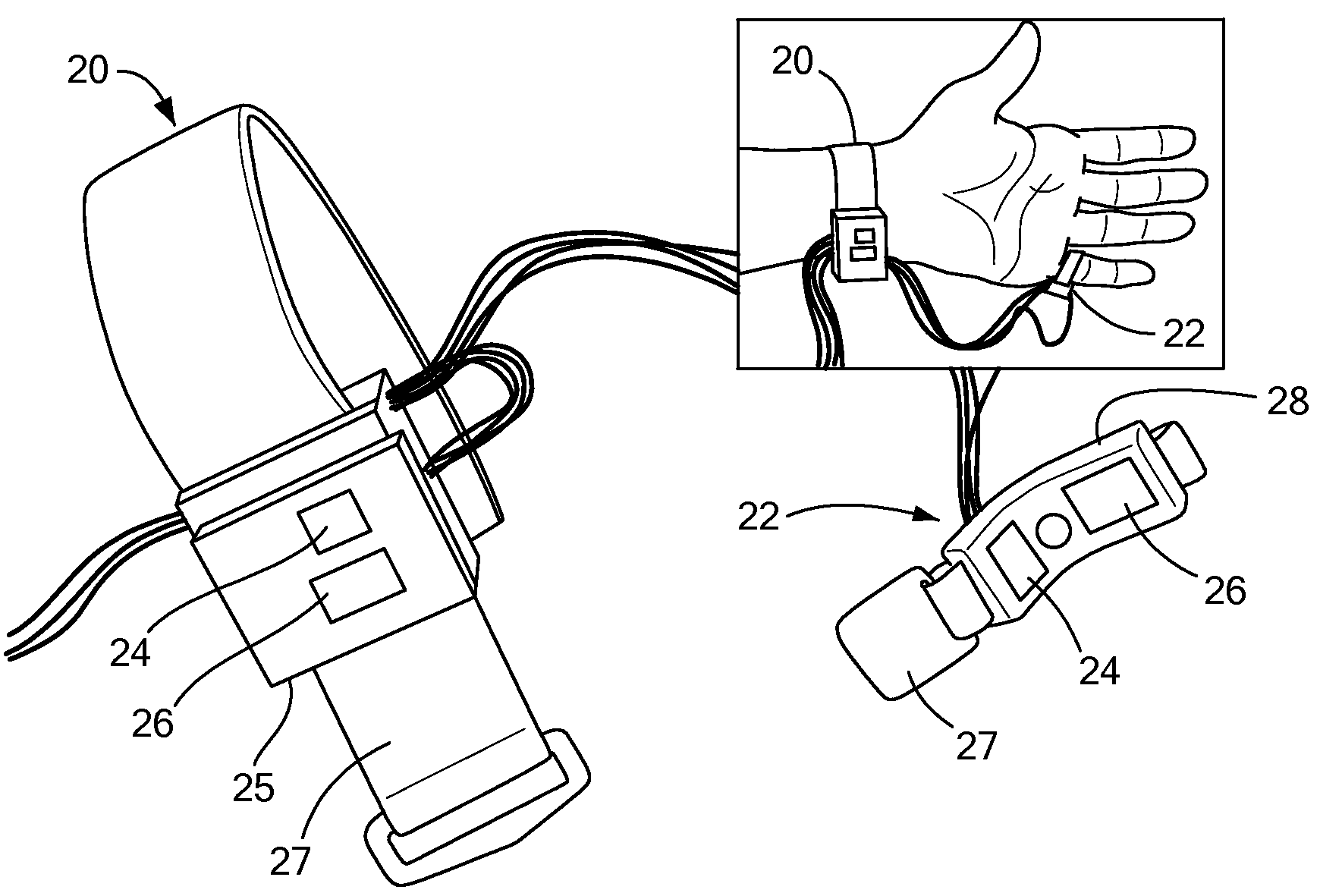
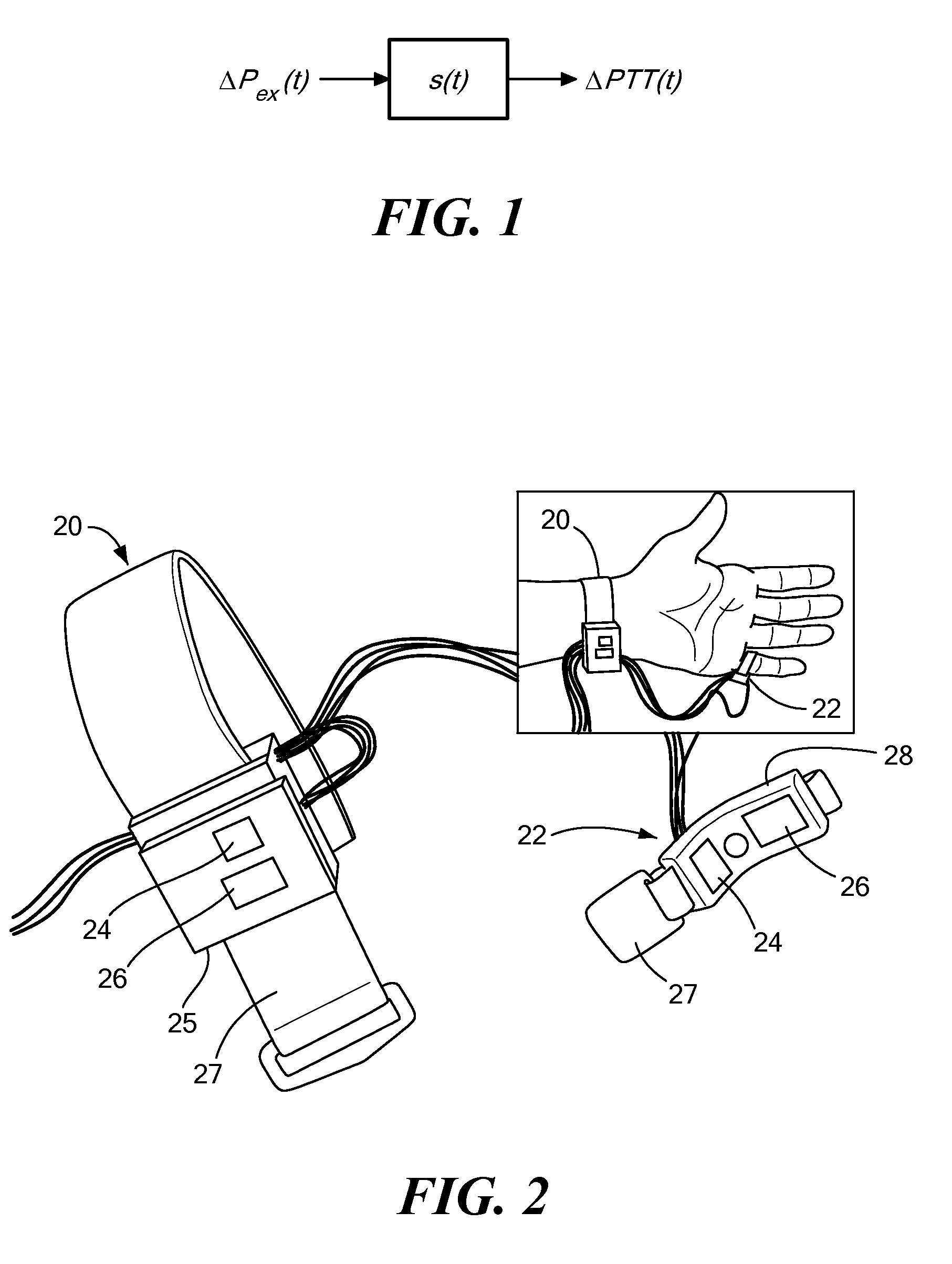
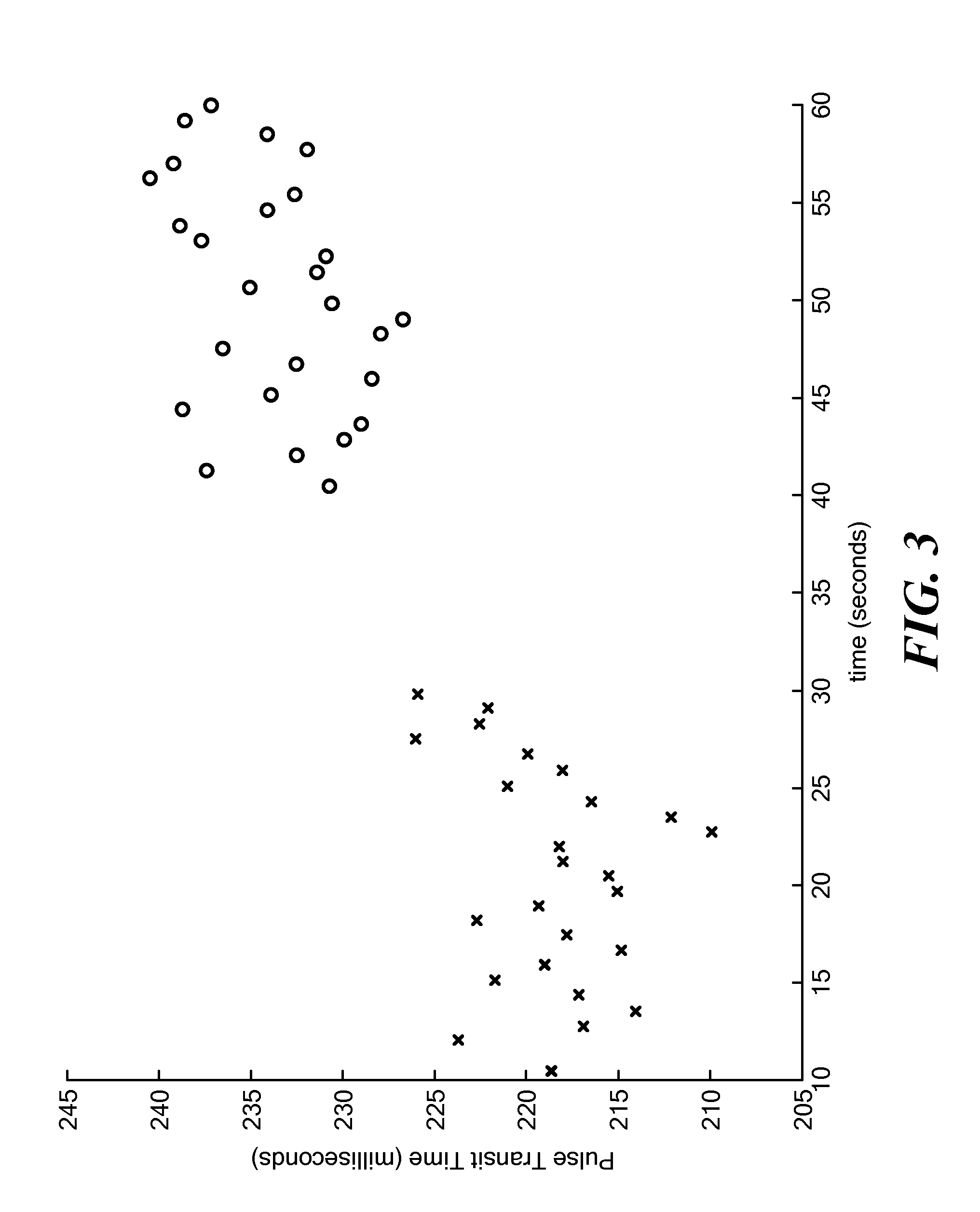
An apparatus and methods for adaptive and autonomous calibration of pulse transit time measurements to obtain arterial blood pressure using arterial pressure variation. The apparatus and methods give pulse transit time (PTT) devices an ability to self-calibrate. The methods apply a distributed model with lumped parameters, and may be implemented, for example, using pulse transit time measurements derived from a wearable photoplethysmograph (PPG) sensor architecture with an intervening pressurizing mechanism.
Owner:MASSACHUSETTS INST OF TECH
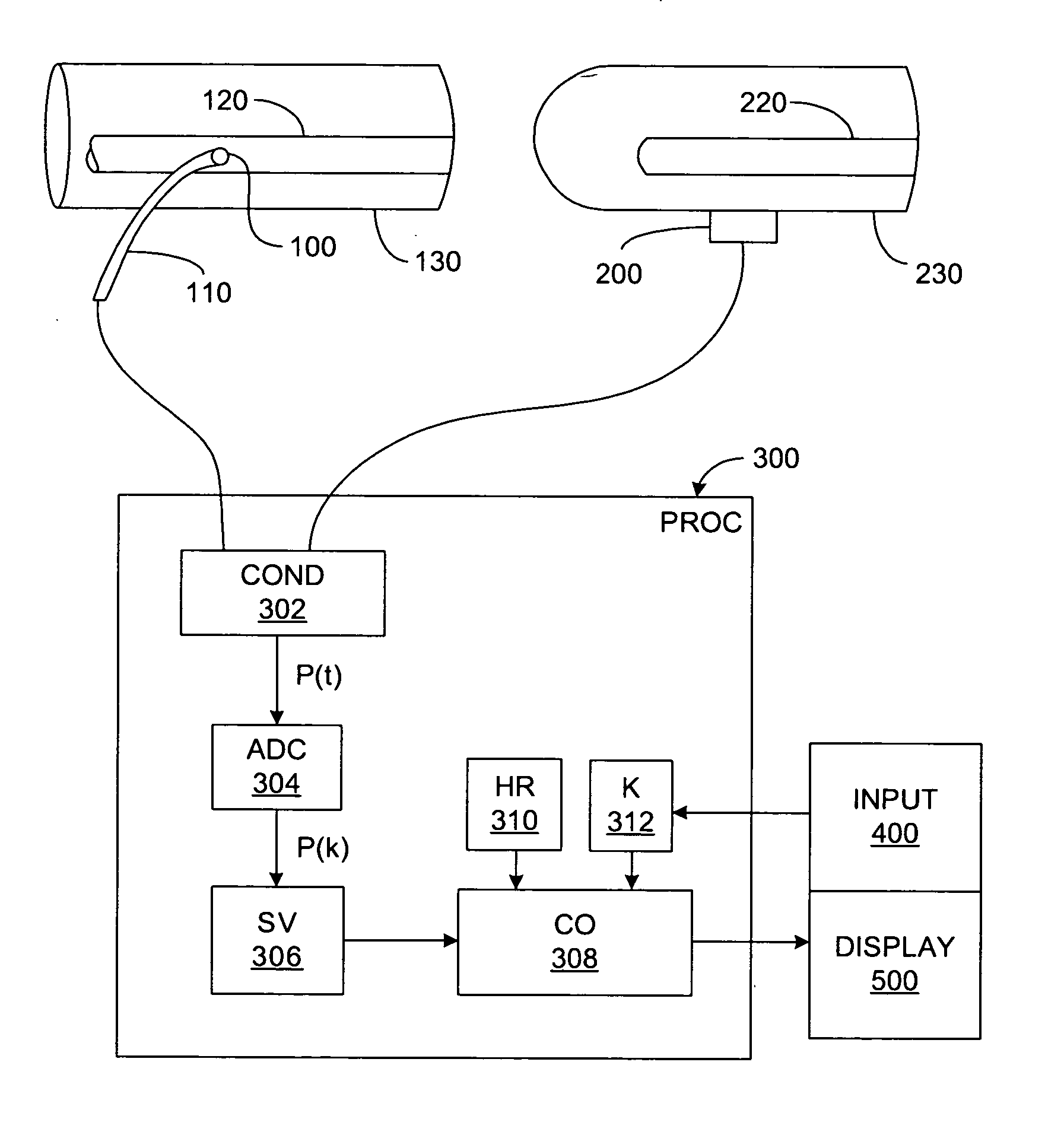
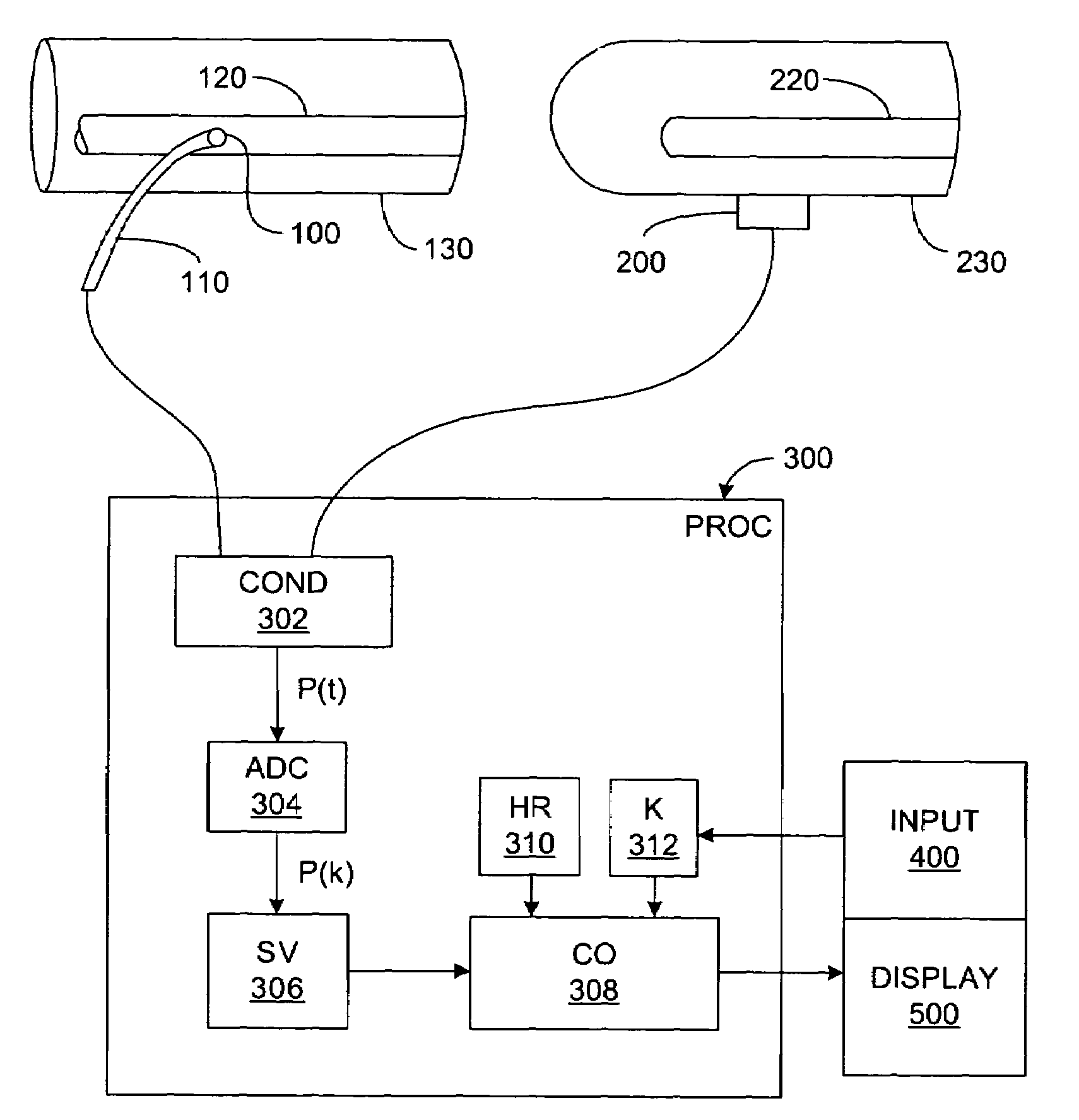
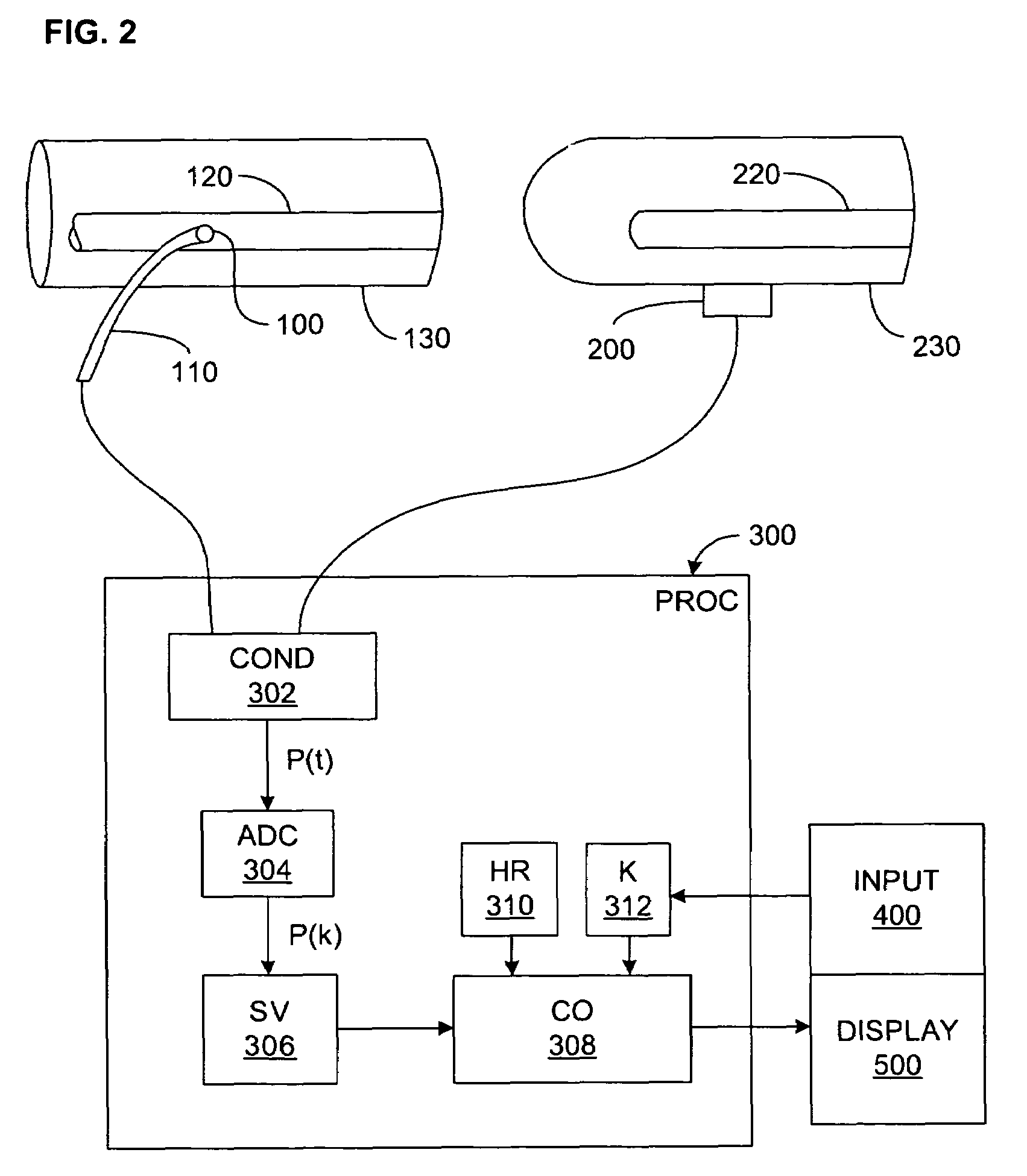
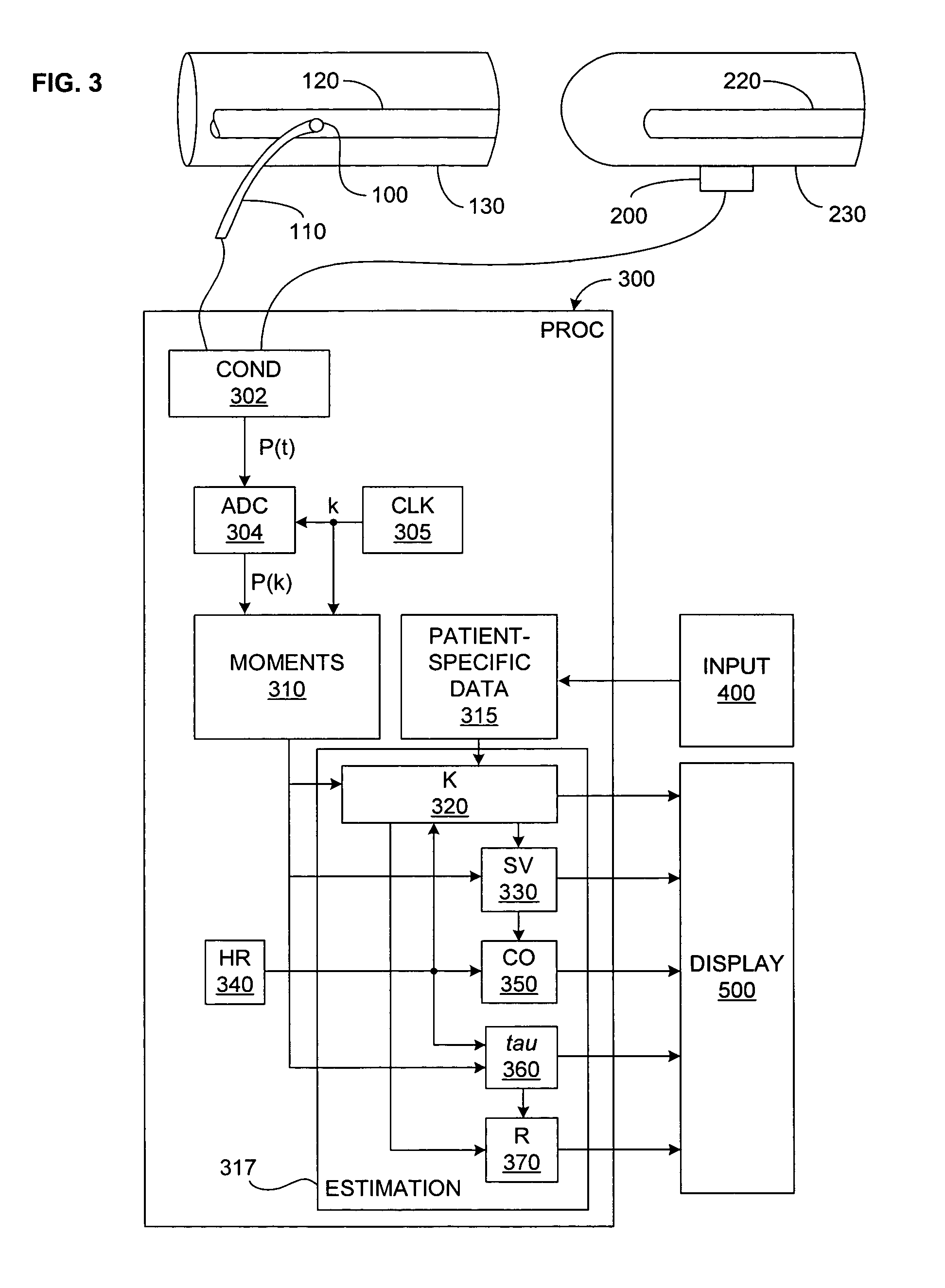
Pressure-based system and method for determining cardiac stroke volume
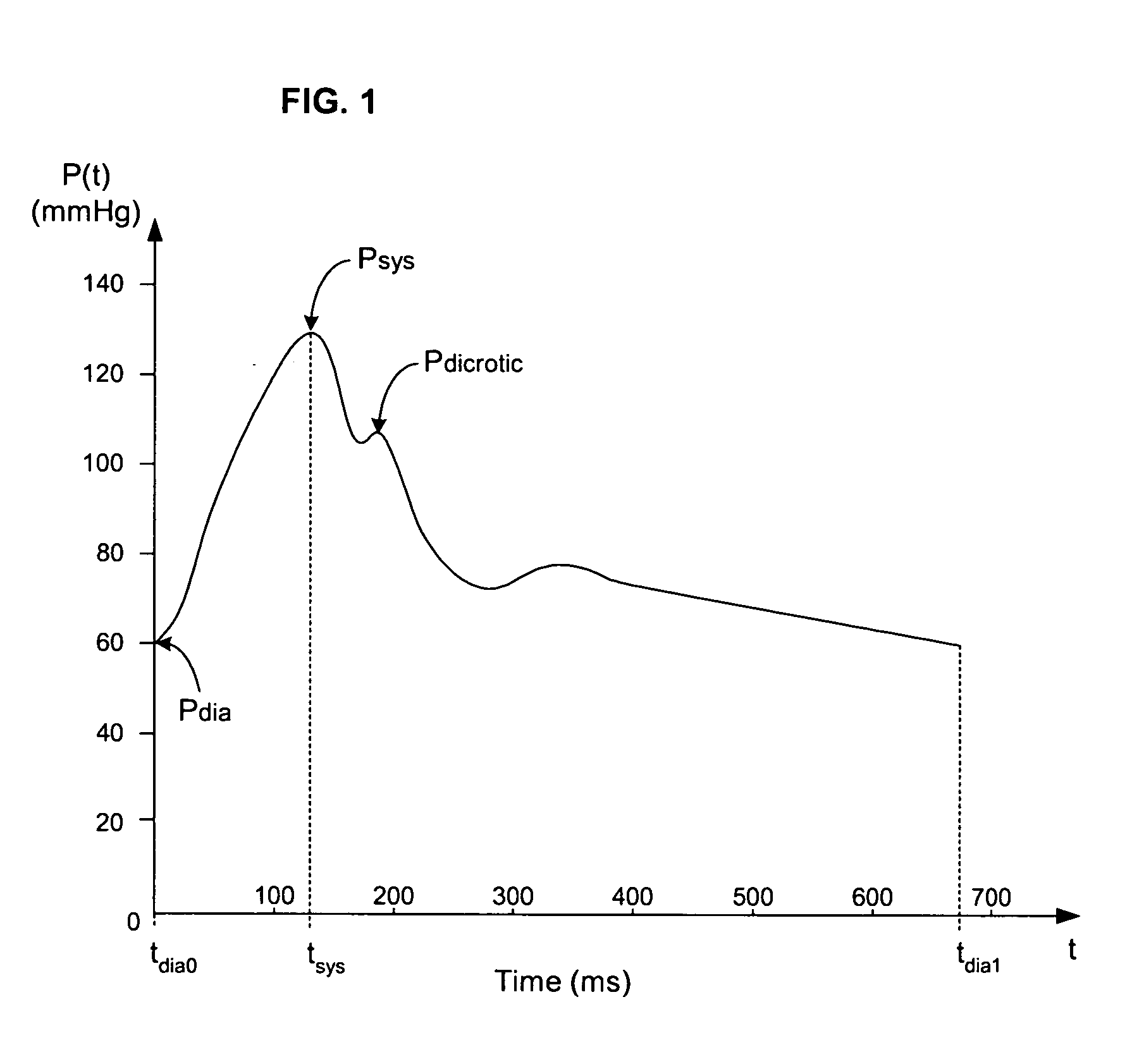
ActiveUS20050124903A1Potent effectEvaluation of blood vesselsCatheterArterial pressure waveformDecreased mean arterial pressure
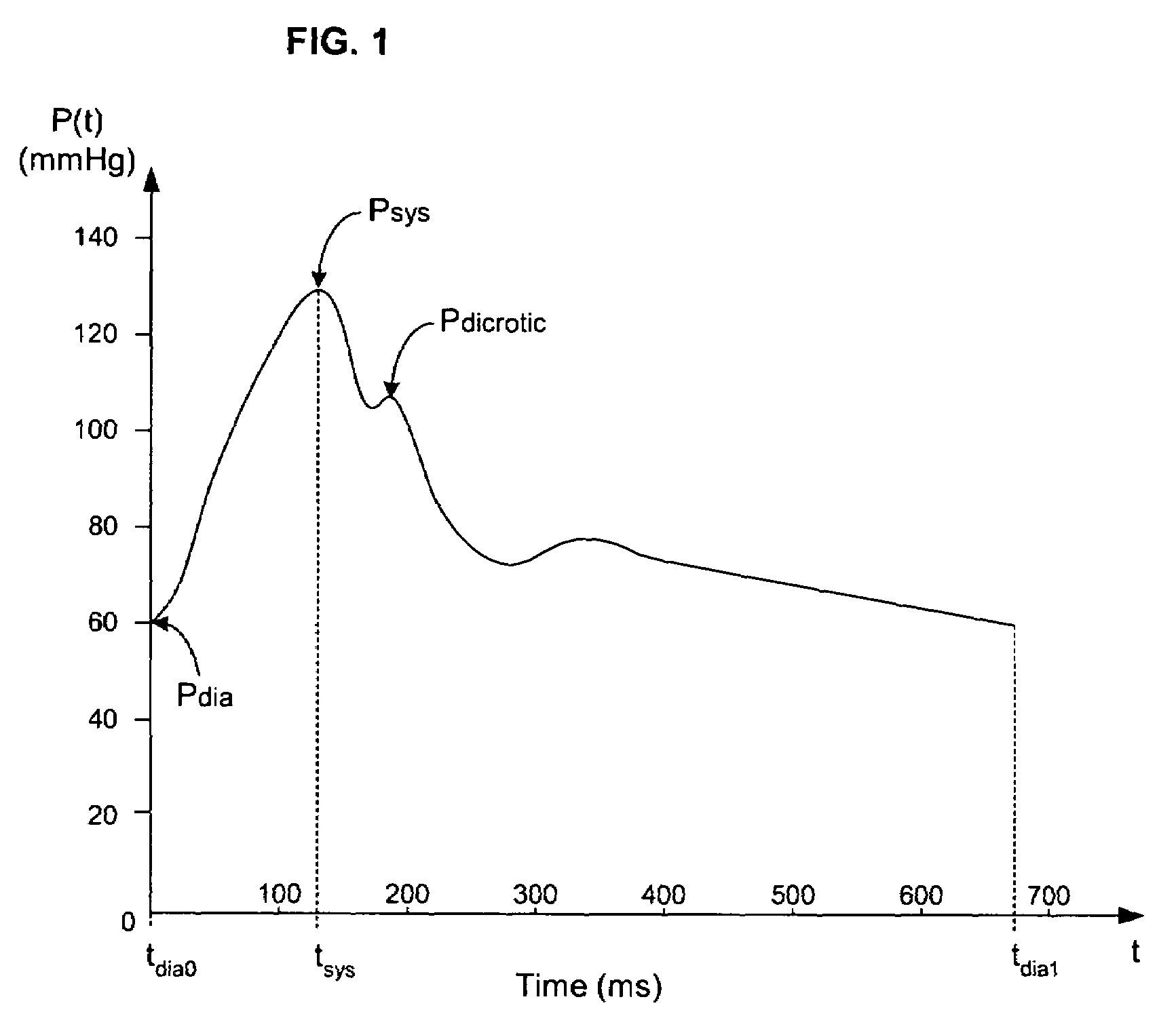
Cardiac stroke volume (SV) of a subject is estimated as a function of a value derived from a measured arterial pressure waveform. The value may be the standard deviation, or a function of the difference between maximum and minimum pressure values, or a function of either the maximum value of the first time derivative or the absolute value of the minimum of the first time derivative of the pressure waveform, or both, or a function of the magnitude of one or more spectral components of the pressure waveform at a frequency corresponding to the heart rate. Cardiac output is then estimated as the product of the subject's heart rate and SV, scaled by a calibration constant. Arterial pressure may be measured invasively or non-invasively.
Owner:EDWARDS LIFESCIENCES CORP
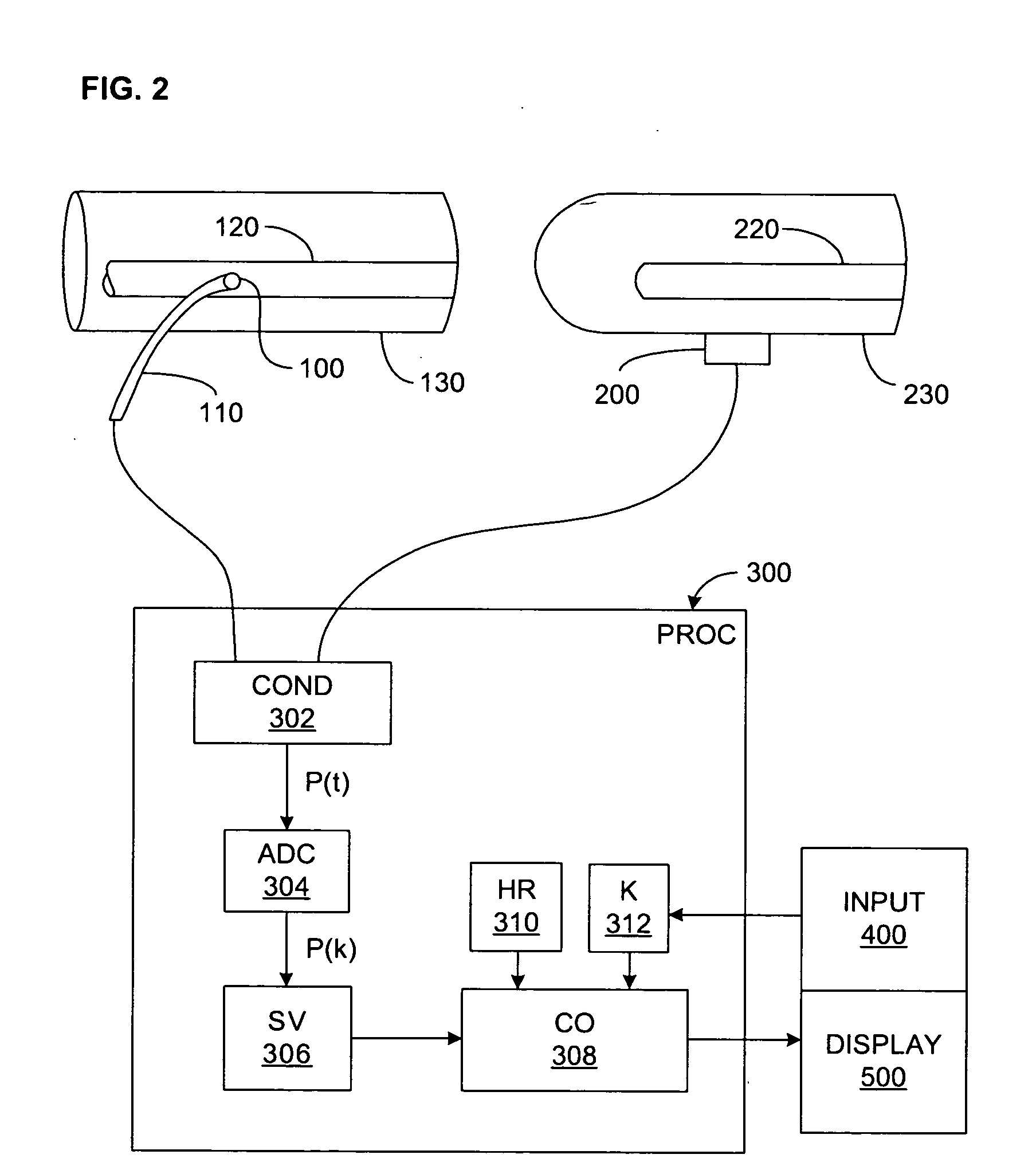
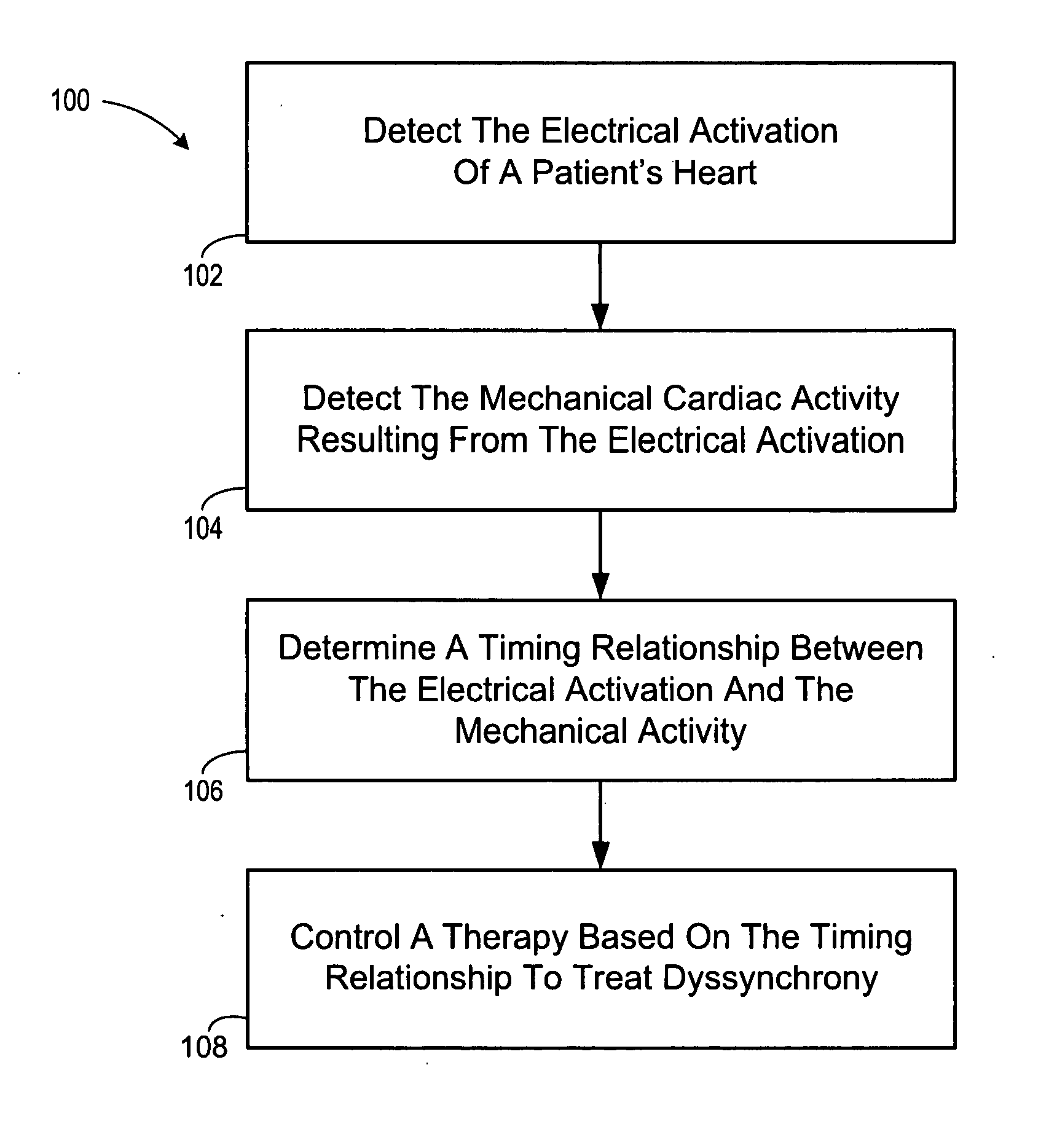
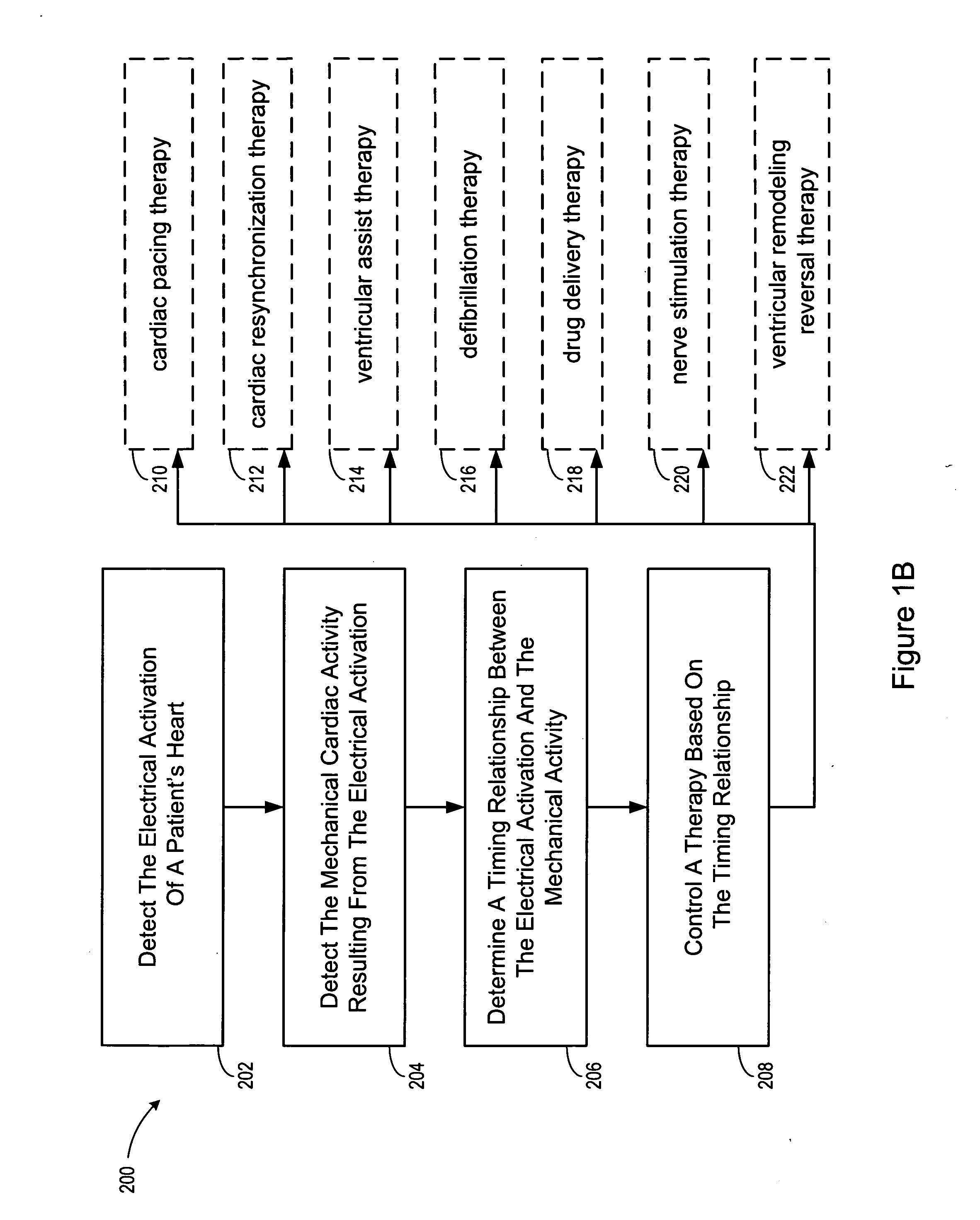
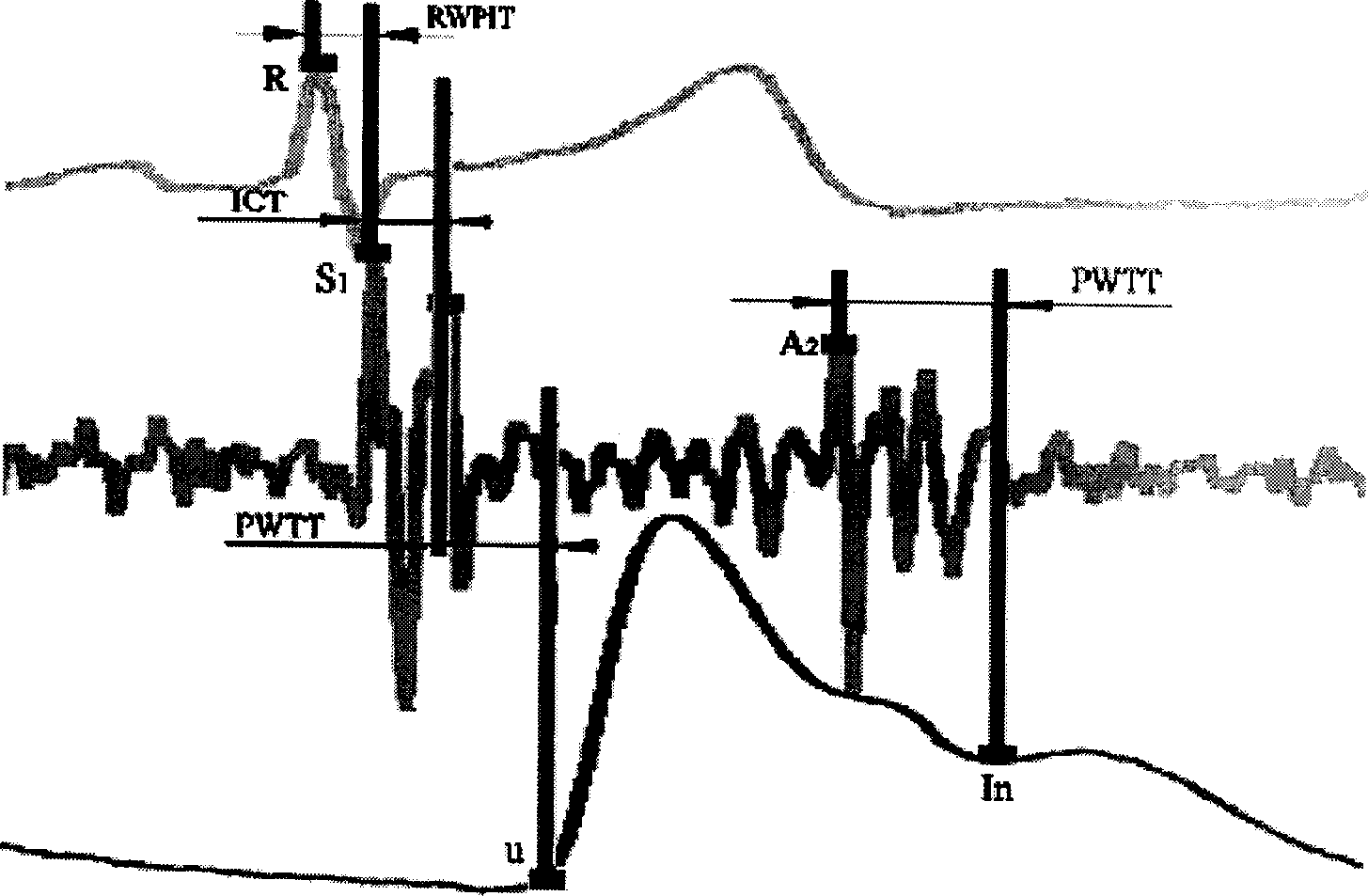
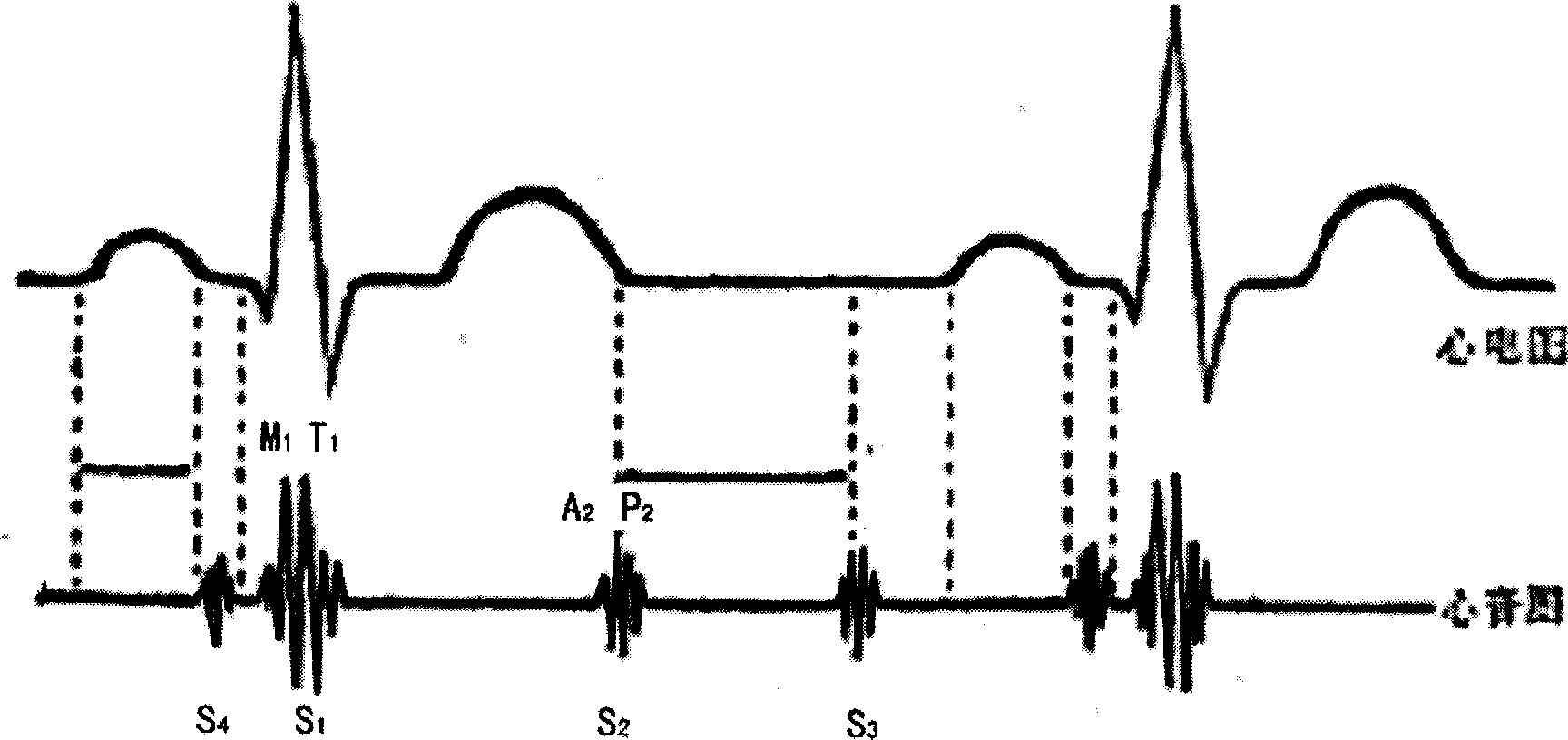
Method and apparatus for controlling cardiac therapy based on electromechanical timing
Devices and methods for therapy control based on electromechanical timing involve detecting electrical activation of a patient's heart, and detecting mechanical cardiac activity resulting from the electrical activation. A timing relationship is determined between the electrical activation and the mechanical activity. A therapy is controlled based on the timing relationship. The therapy may improve intraventricular dyssynchrony of the patient's heart, or treat at least one of diastolic and systolic dysfunction and / or dyssynchrony of the patient's heart, for example. Electrical activation may be detected by sensing delivery of an electrical stimulation pulse to the heart or sensing intrinsic depolarization of the patient's heart. Mechanical activity may be detected by sensing heart sounds, a change in one or more of left ventricular impedance, ventricular pressure, right ventricular pressure, left atrial pressure, right atrial pressure, systemic arterial pressure and pulmonary artery pressure.
Owner:CARDIAC PACEMAKERS INC
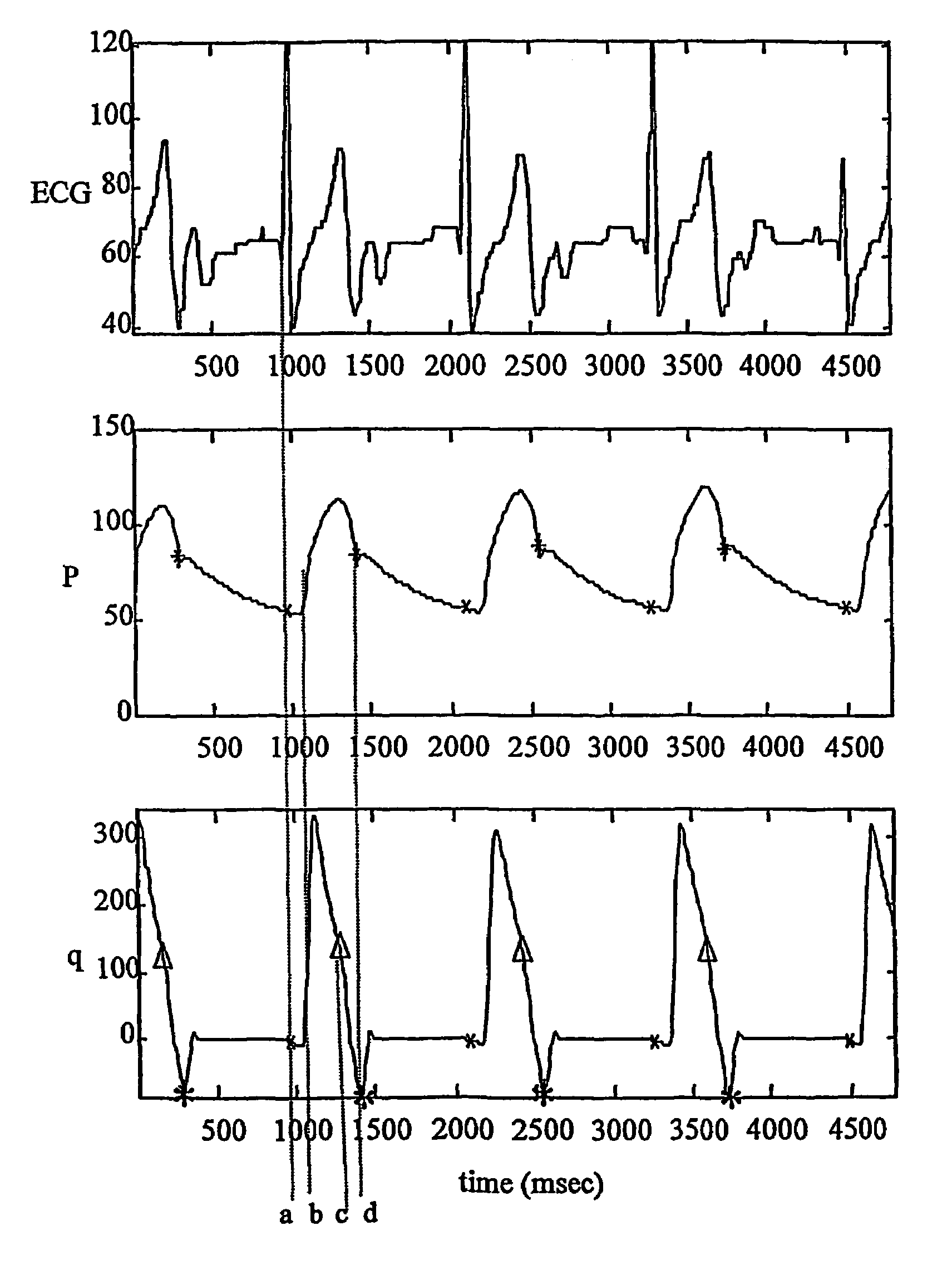
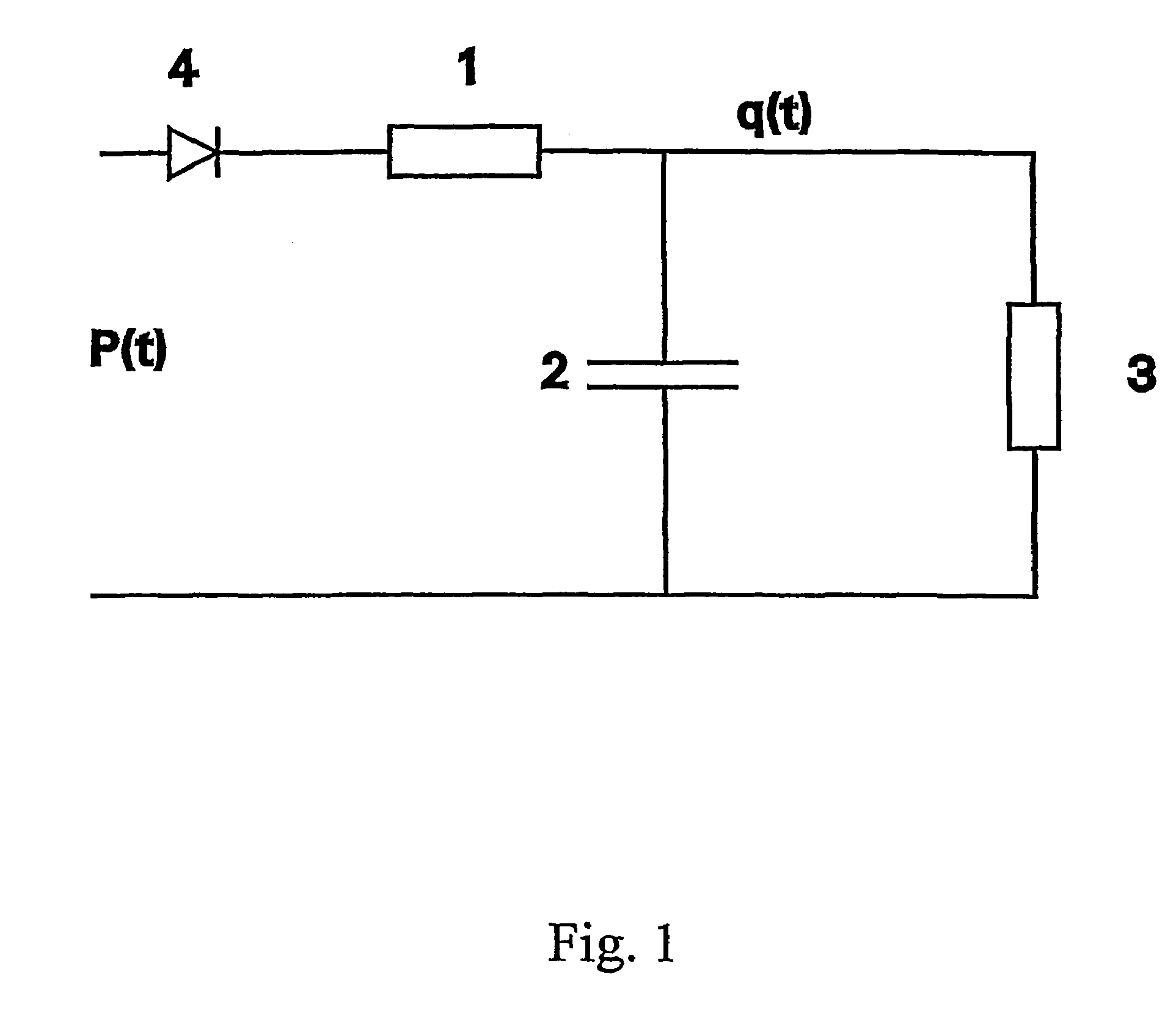
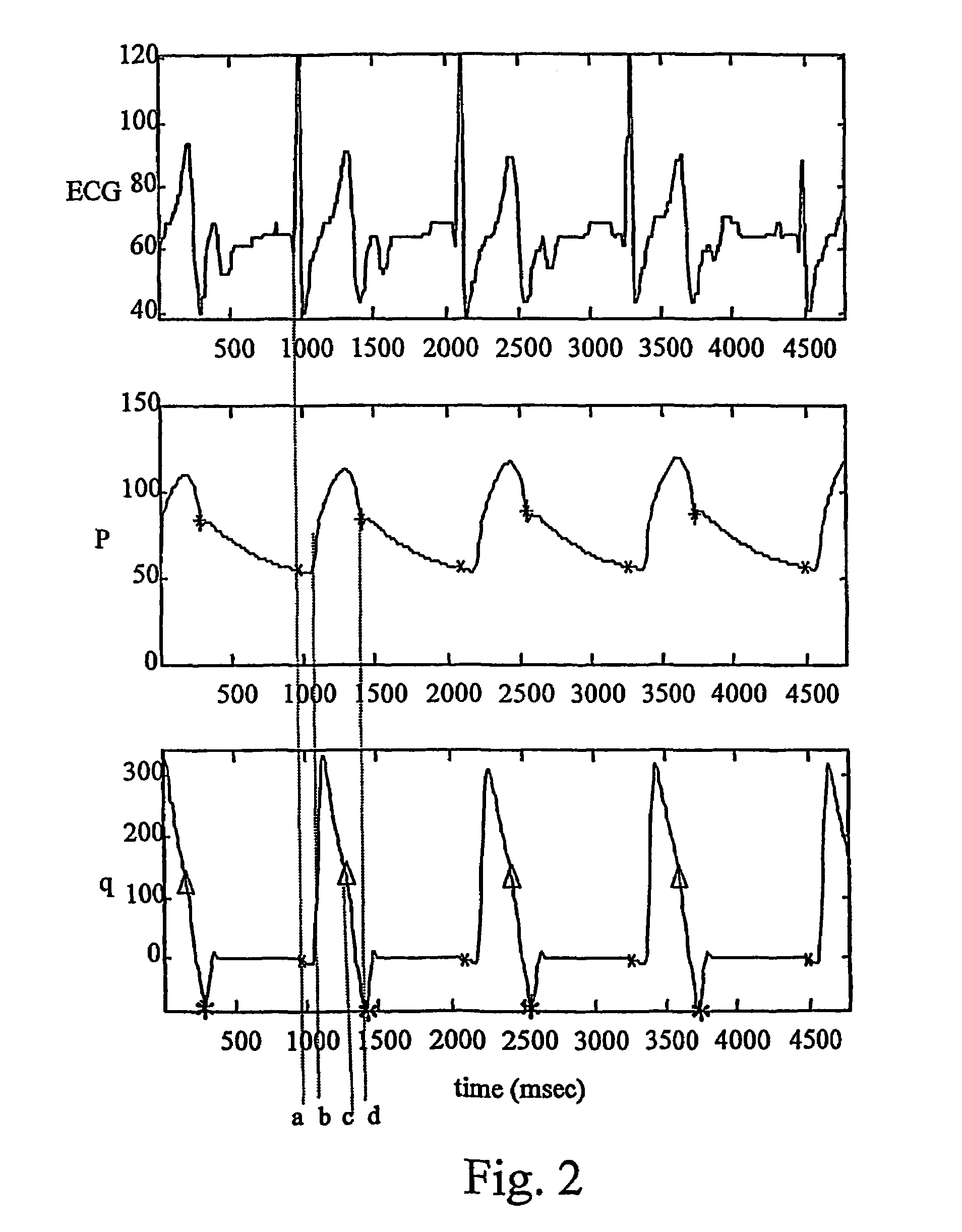
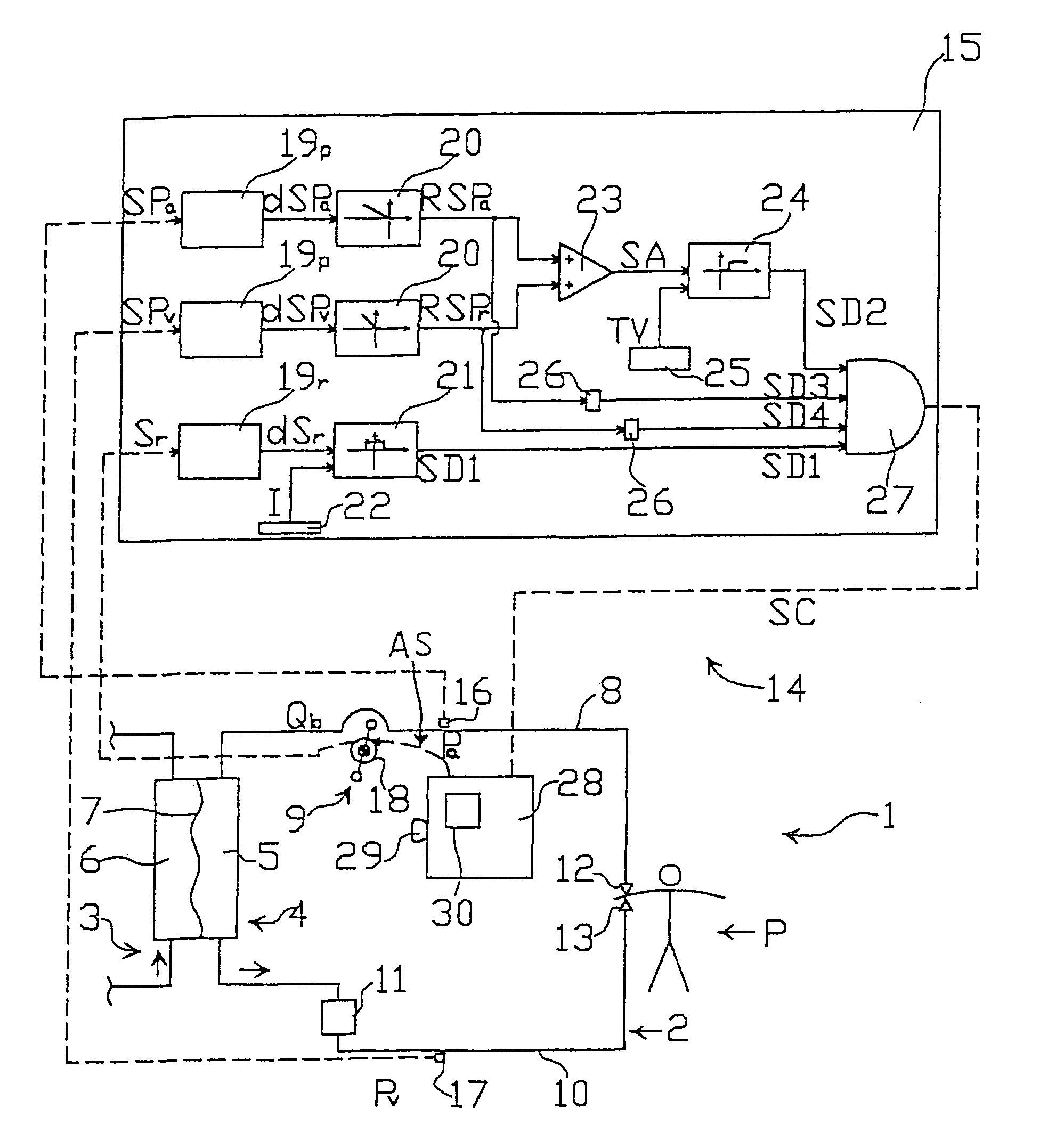
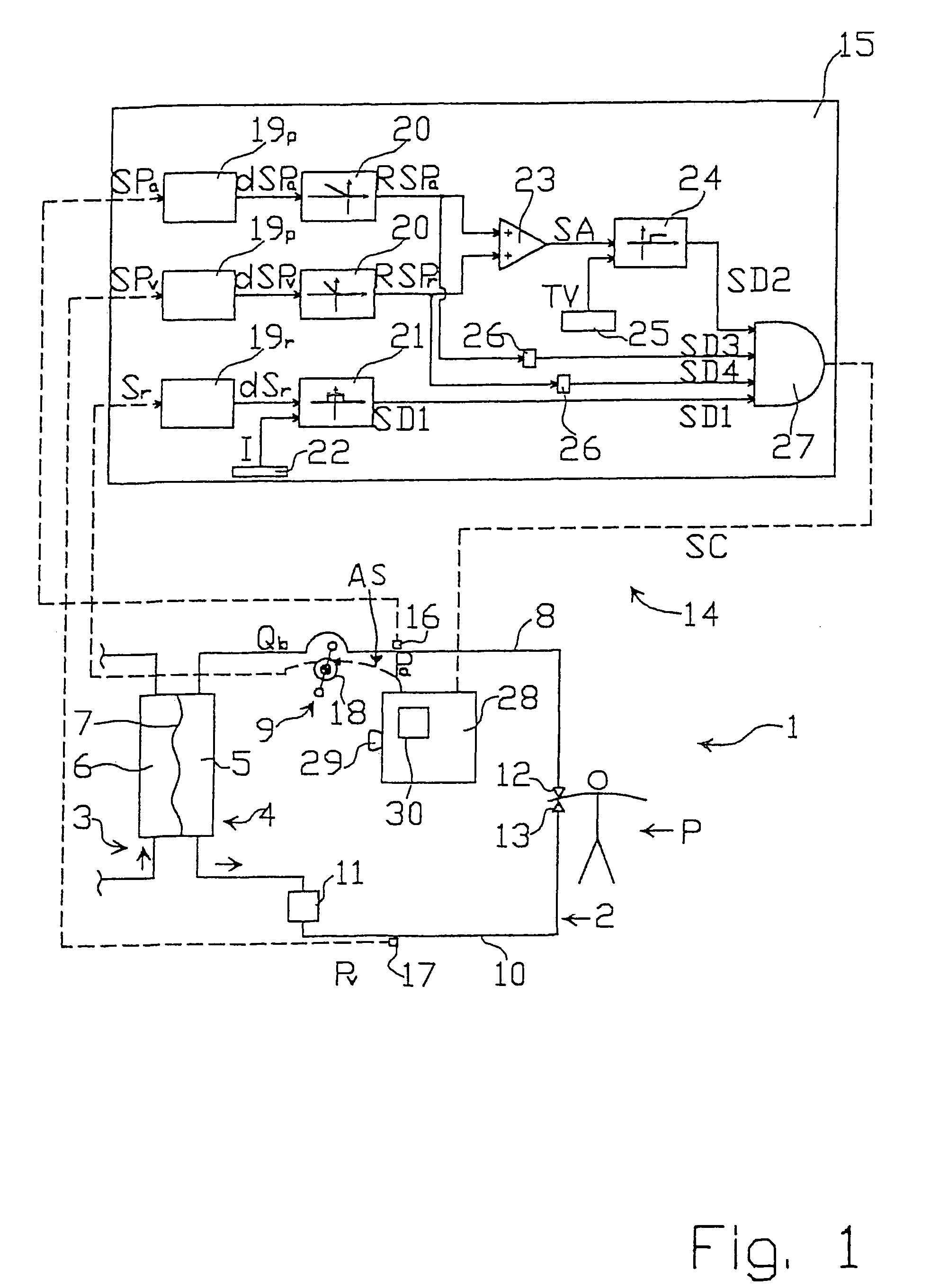
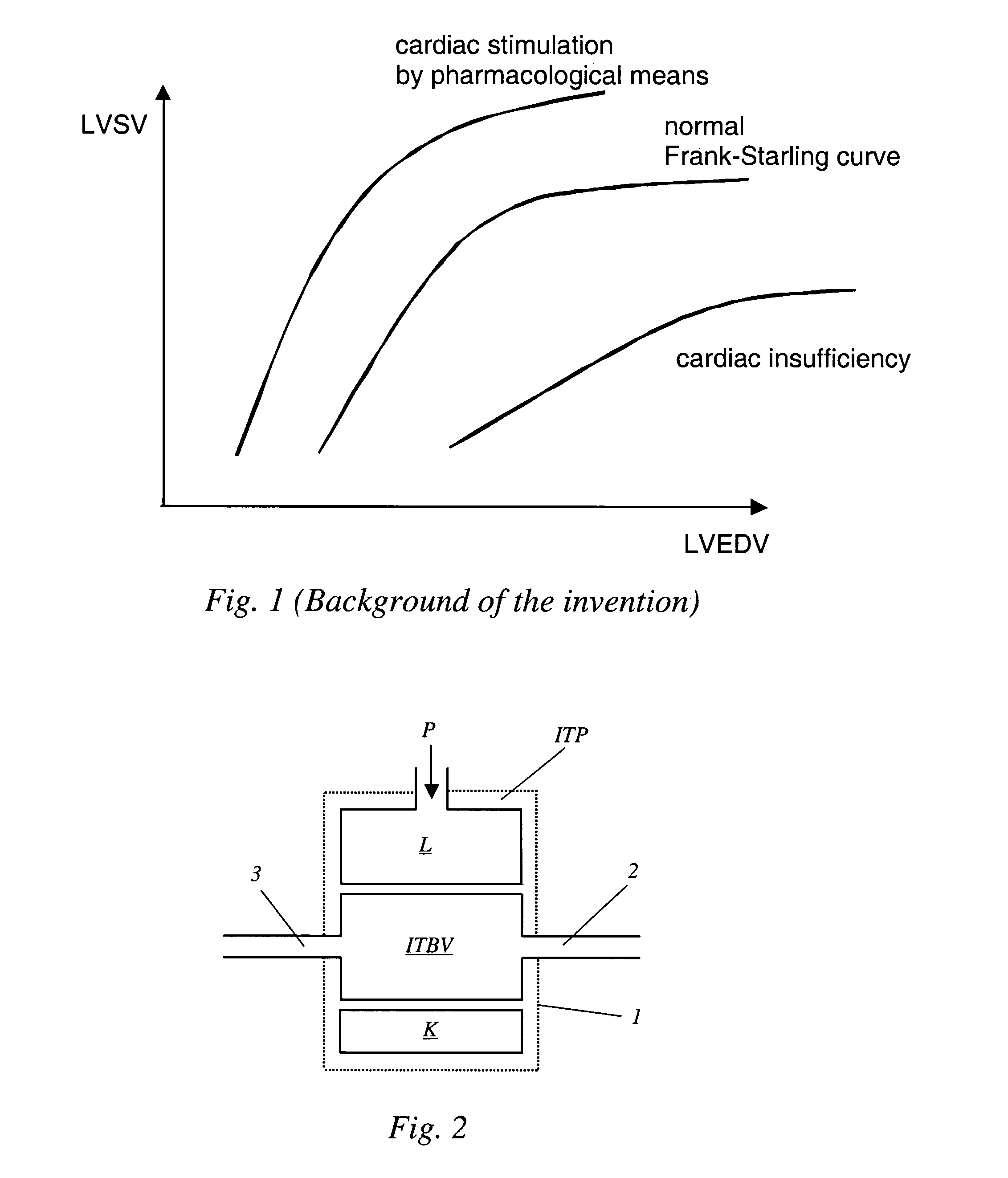
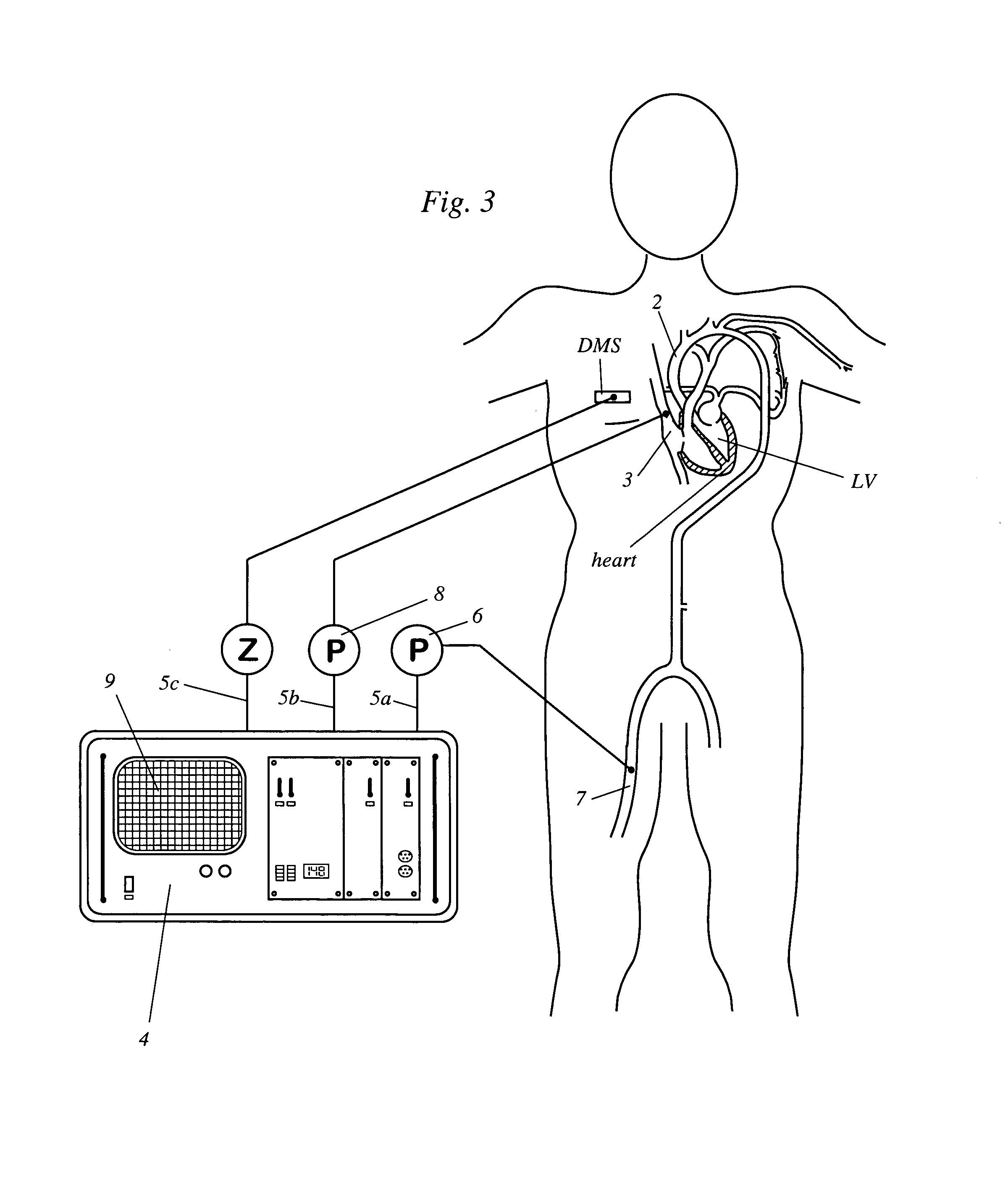
Methods and apparatus for controlling heart assist devices
InactiveUS7169109B2Improve accuracyElectrocardiographyOther blood circulation devicesDecreased mean arterial pressurePulse pressure
An apparatus for a heart assist device, comprising a processing unit for computing the blood flow rate from the arterial pressure curve and for predicting at every heartbeat the closing time of the heart valve from the curve of the blood flow rate. The processing unit is adapted to deliver a signal for controlling a heart assist device at a point in time, a period ahead in time of the closing time of the heart valve, wherein the mechanical properties of the said heart assist device are taken into account in determining the period. The apparatus adapts itself to changes in a patient's heart frequency and aortic pressure.
Owner:ARROW INT INC
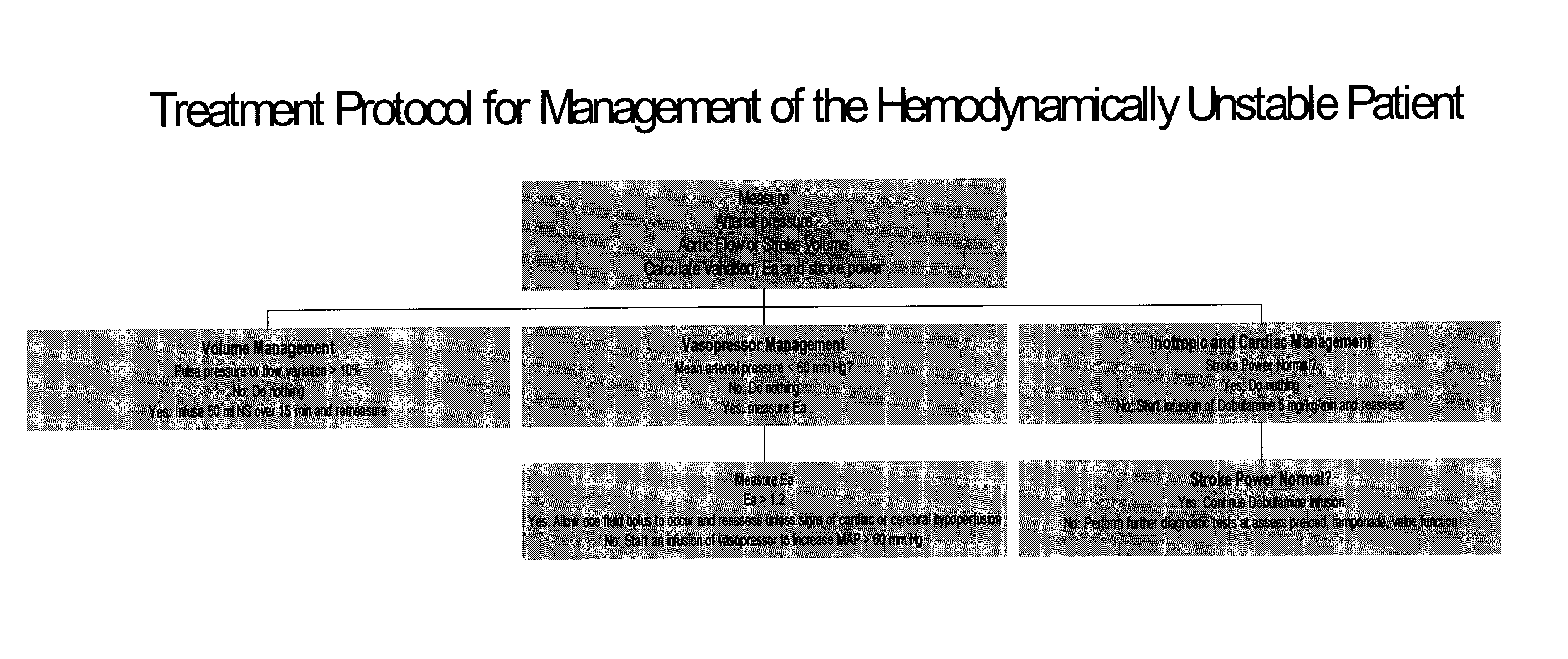
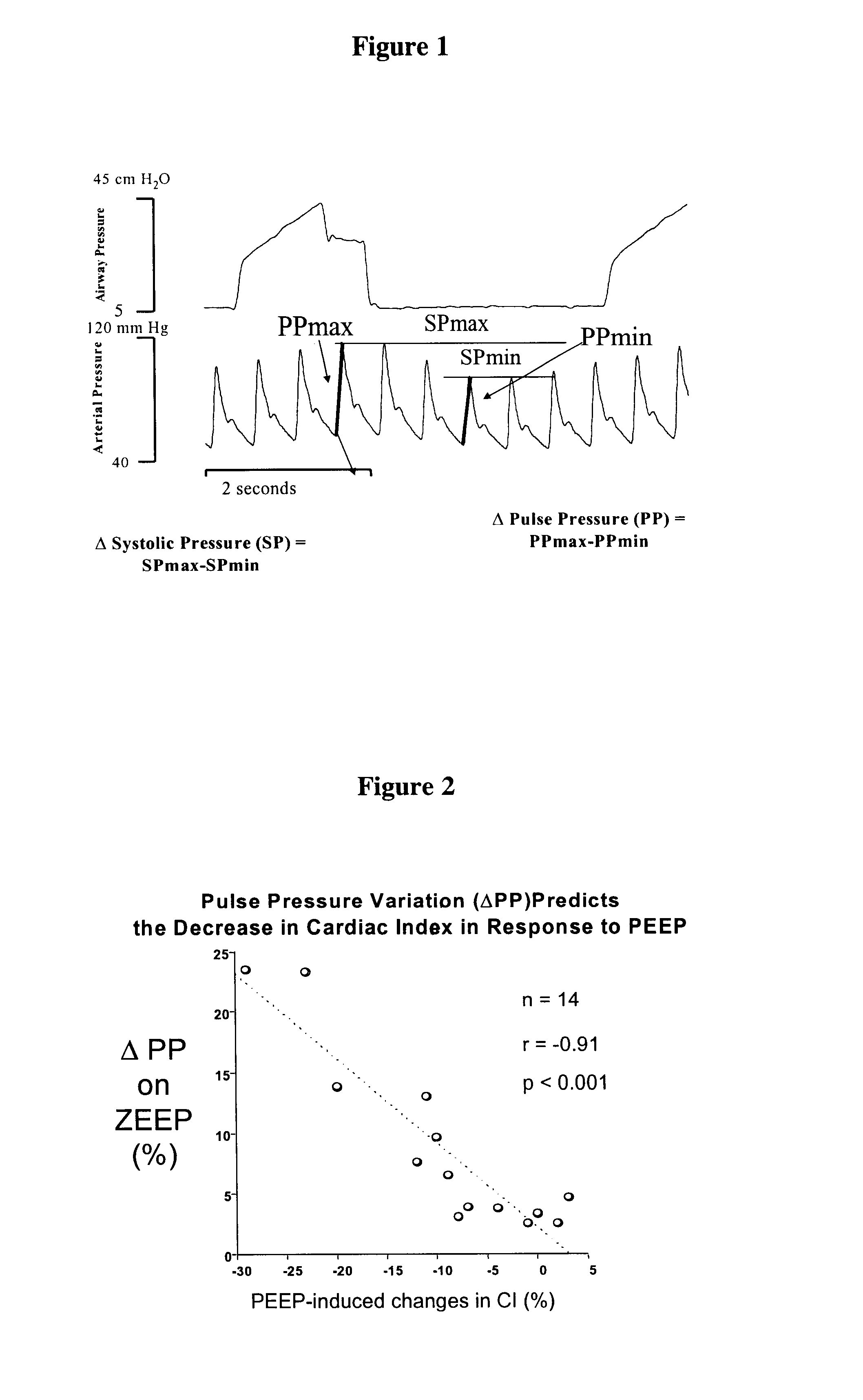
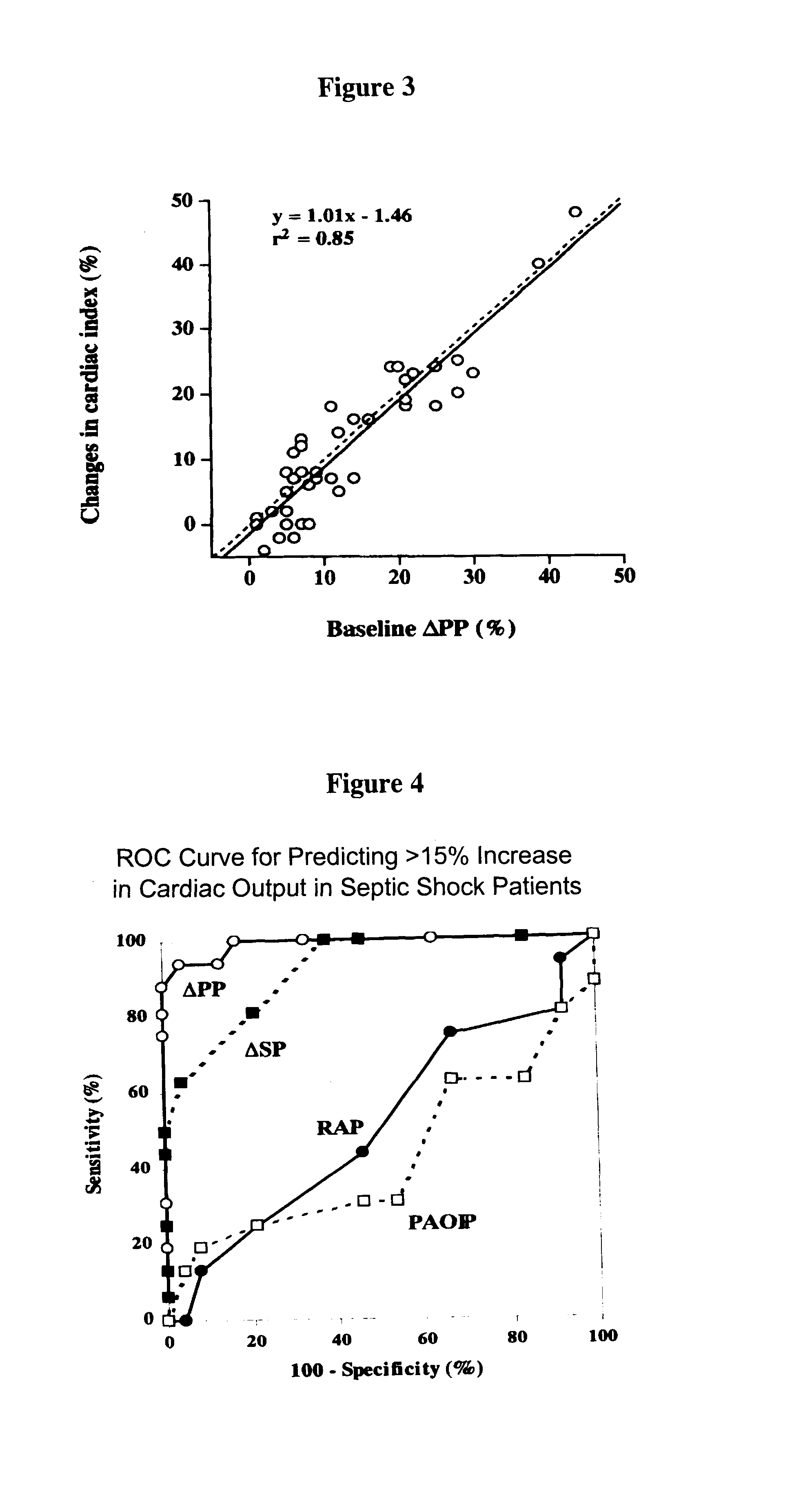
Use of aortic pulse pressure and flow in bedside hemodynamic management
InactiveUS6776764B2Evaluation of blood vesselsCatheterCritically illDecreased mean arterial pressure
Owner:UNIVERSITY OF PITTSBURGH
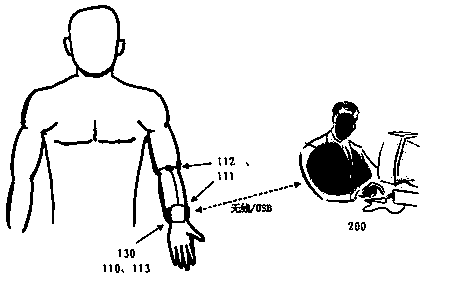
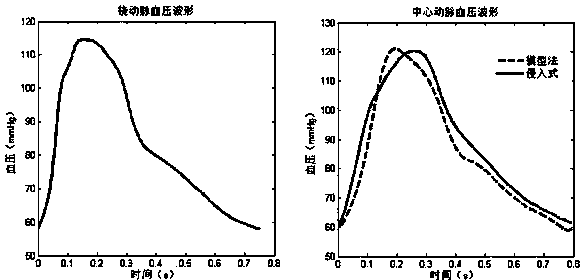
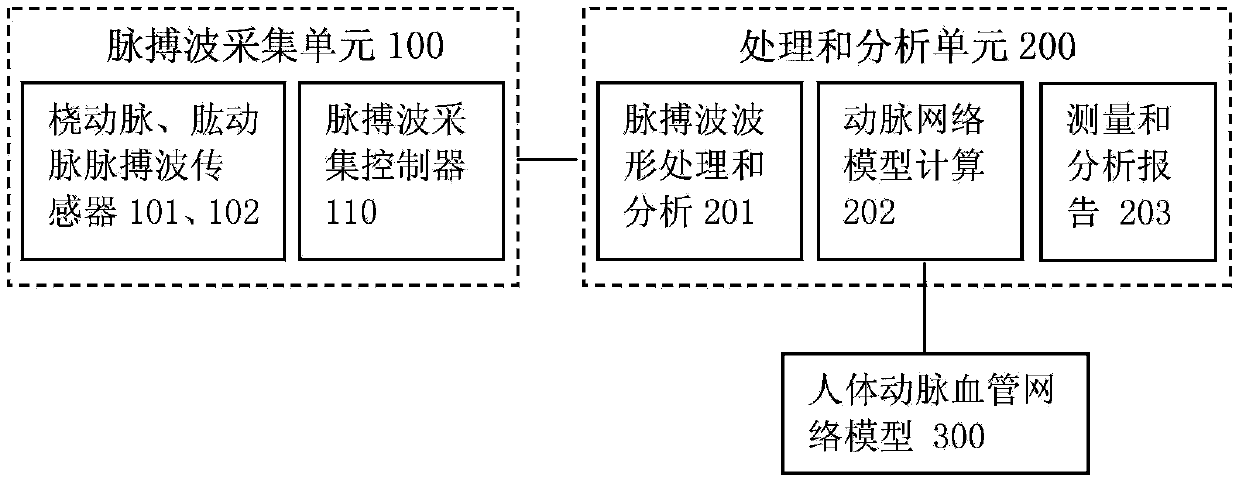
Noninvasive continuous arterial blood pressure measuring method and equipment
ActiveCN104138253ADiagnostic recording/measuringSensorsCoronary heart diseaseDecreased mean arterial pressure
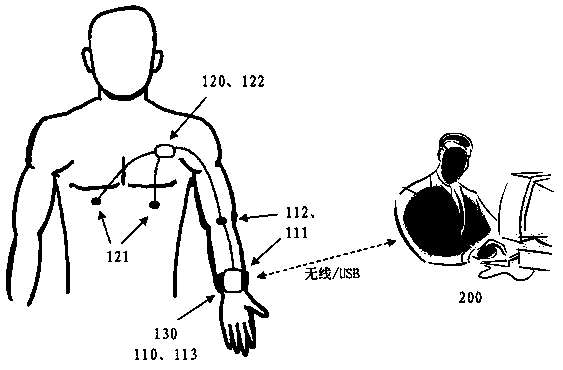
The invention discloses a noninvasive continuous human body arterial blood pressure measuring method and equipment. The noninvasive continuous human body central arterial blood pressure measuring method comprises the steps as follows: calculating individualization parameters of a to-be-measured person artery blood vessel network model according to acquired pulse wave forms of radial arteries and brachial arteries; calculating radial artery blood pressure systolic pressure, diastolic pressure and blood pressure wave forms according to radial artery pulse wave speeds and artery blood vessel network parameters; calculating ascending aorta-radial artery transfer functions; further calculating central arterial blood pressure. The noninvasive continuous human body central arterial blood pressure measuring equipment consists of a signal processing and analyzing unit, a pulse wave and motion signal acquisition unit worn on the wrist as well as an electro-cardio and motion signal acquisition unit worn in front of the chest. According to the method and the equipment, electrocardiograms, the radial artery blood pressure, the central arterial blood pressure as well as motions and postures are monitored simultaneously, heart rate and electro-cardio morphological parameters are analyzed in various motion states, artery network model parameters and blood pressure parameters, particularly central arterial pressure wave form parameters, are analyzed, and the method and the equipment have great significance for prevention and control on cardiovascular diseases, particularly for prevention and control on high-risk diseases such as the hypertension, the coronary heart disease and the like.
Owner:南京茂森电子技术有限公司
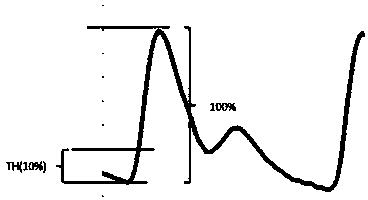
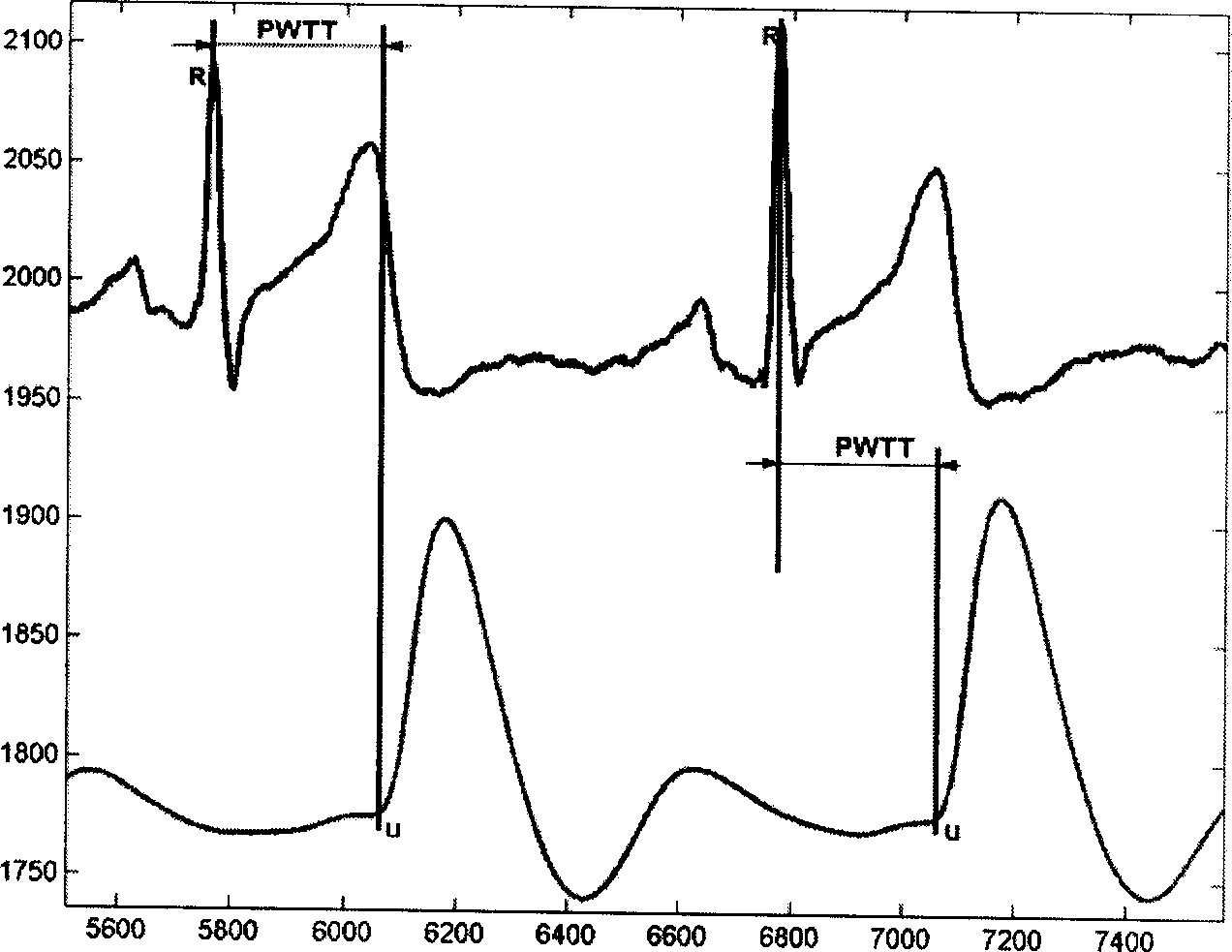
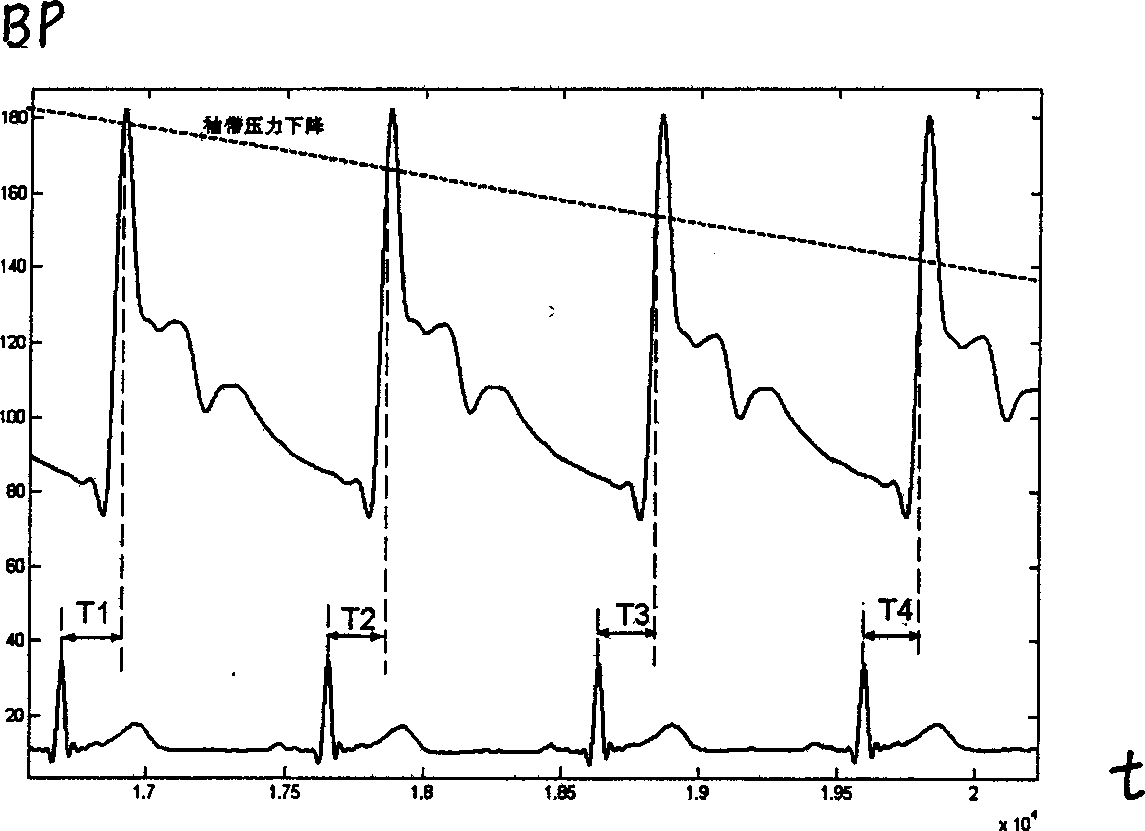
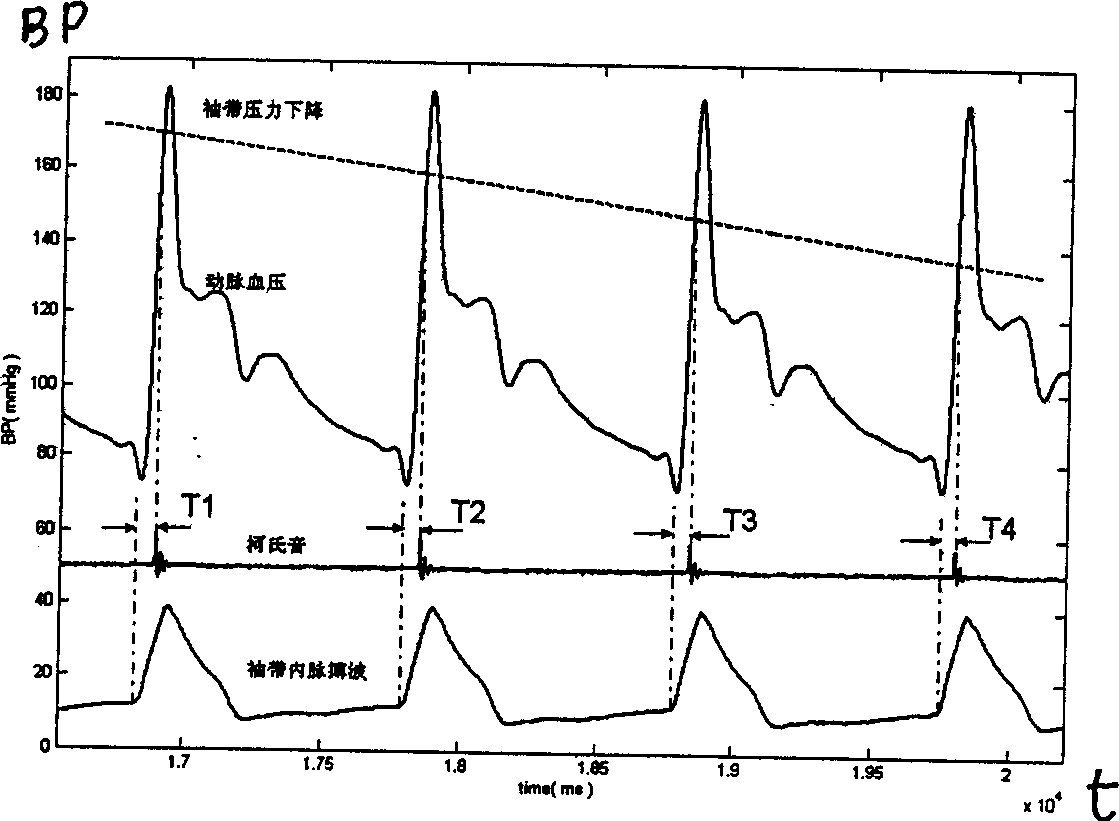
Method and apparatus for continuously measuring blood pressure
InactiveCN1849998AExclude positiveEliminate distractionsEvaluation of blood vesselsSensorsPersonalizationCardiac cycle
The present invention relates to a method for continuously measuring blood pressure and its equipment. Said method is characterized by that it creates a regression equation between pulse wave conduction time and arterial pressure: BP=a+b*PWTT for measurand person; and utilizes personalization correction technique to define intercept and regression coefficient b of measurand person. Besides, said invention also provides a method for continuously obtaining pulse wave conduction time PWTT by using pulse wave of human body, electrocardiogram signal and phonocardiogram signal and its concrete steps. Said method can raise accuracy for continuously measuring blood pressure, and can be used for measuring head blood pressure.
Owner:AVIATION MEDICINE INST AIR FORCE PLA +1
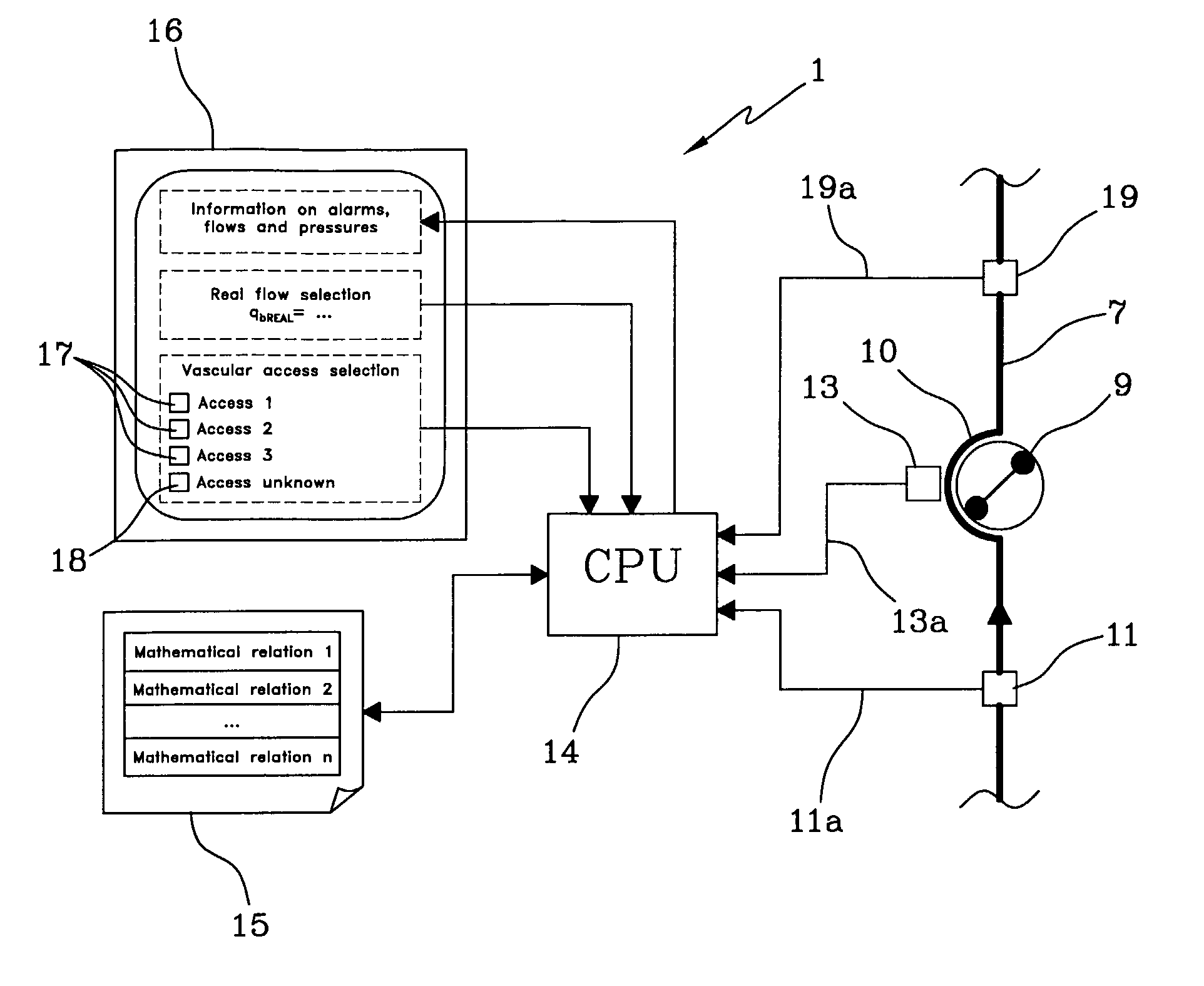
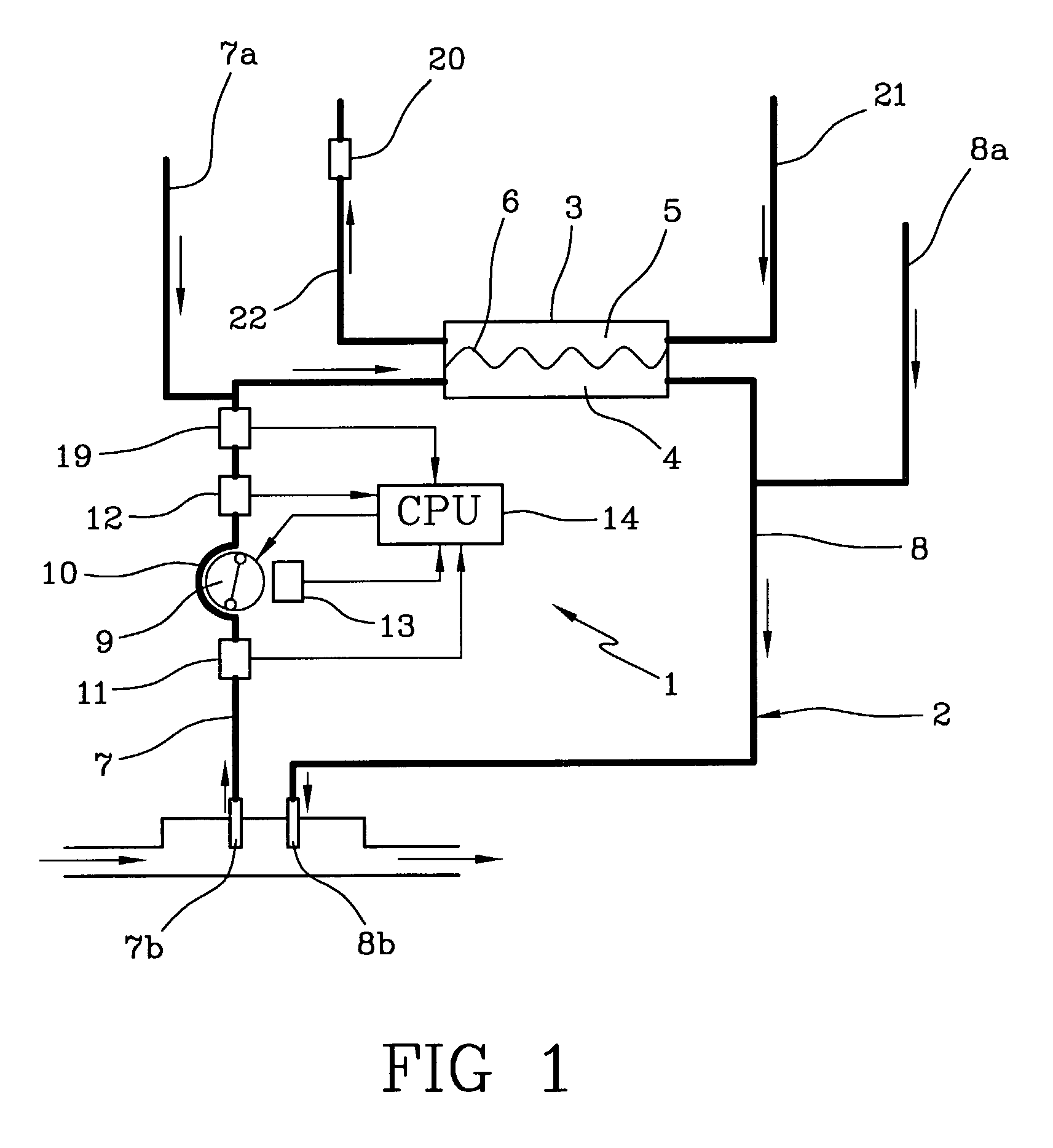
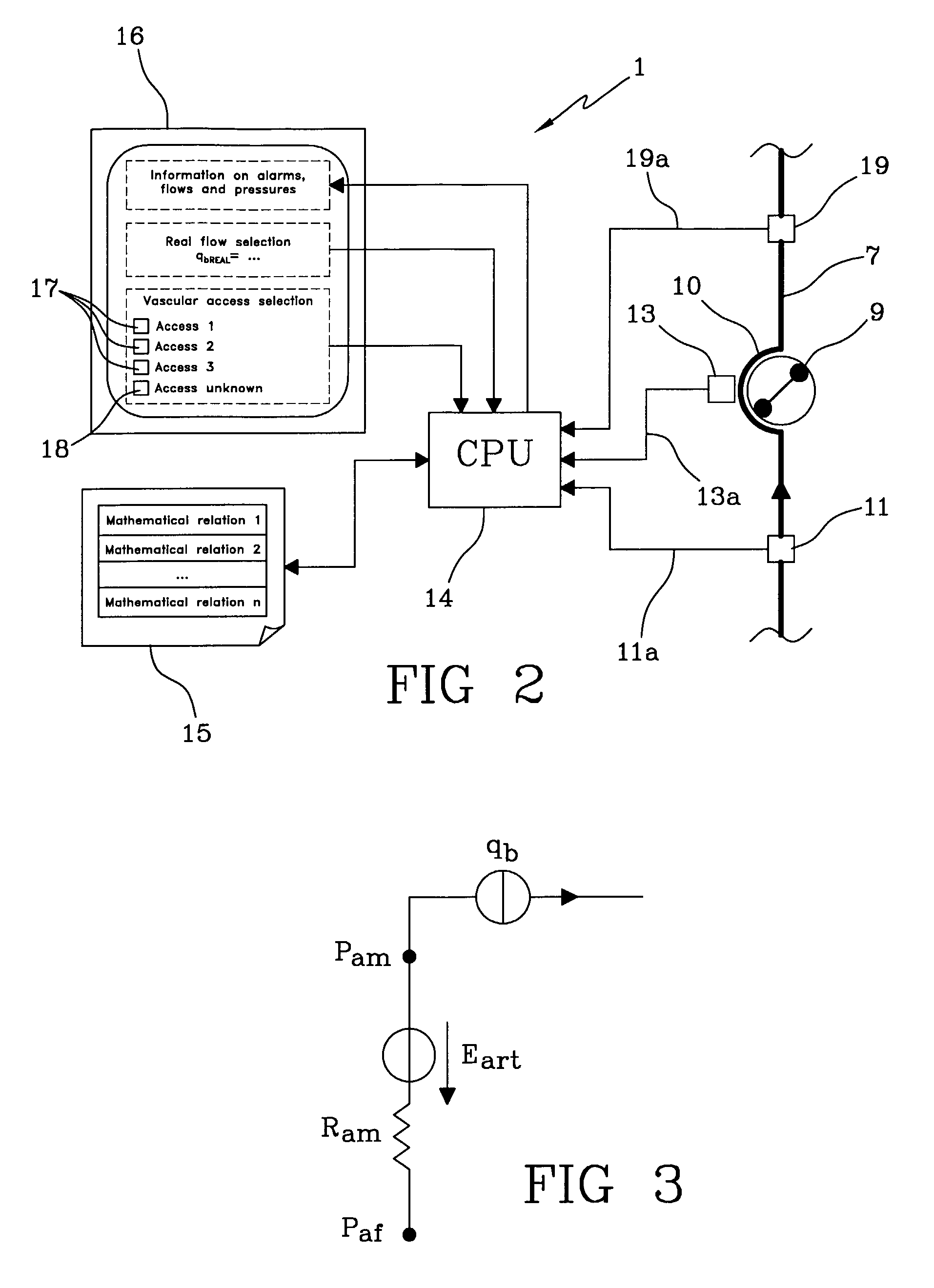
Apparatus for controlling blood flow in an extracorporeal circuit
ActiveUS7794419B2Semi-permeable membranesSolvent extractionExtracorporeal circulationAngular velocity
The apparatus for blood flow control in an extracorporeal circuit comprises: a user interface for setting a desired blood flow value (qbREAL) and a datum relating to the vascular access, a memory for recording a plurality of mathematical relations having mathematical expressions relating to the vascular access organ to be used, and a control unit. The control unit identifies the vascular access, selects, from among the plurality of mathematical relations present in the memory, a relation which corresponds to the vascular access identified, and calculates, as a mathematical function of the set value for the desired flow (qbREAL), a value at which to set the angular velocity of the pump associated to the extracorporeal circuit and / or a theoretical value of the arterial pressure upstream of the pump.
Owner:GAMBRO LUNDIA AB
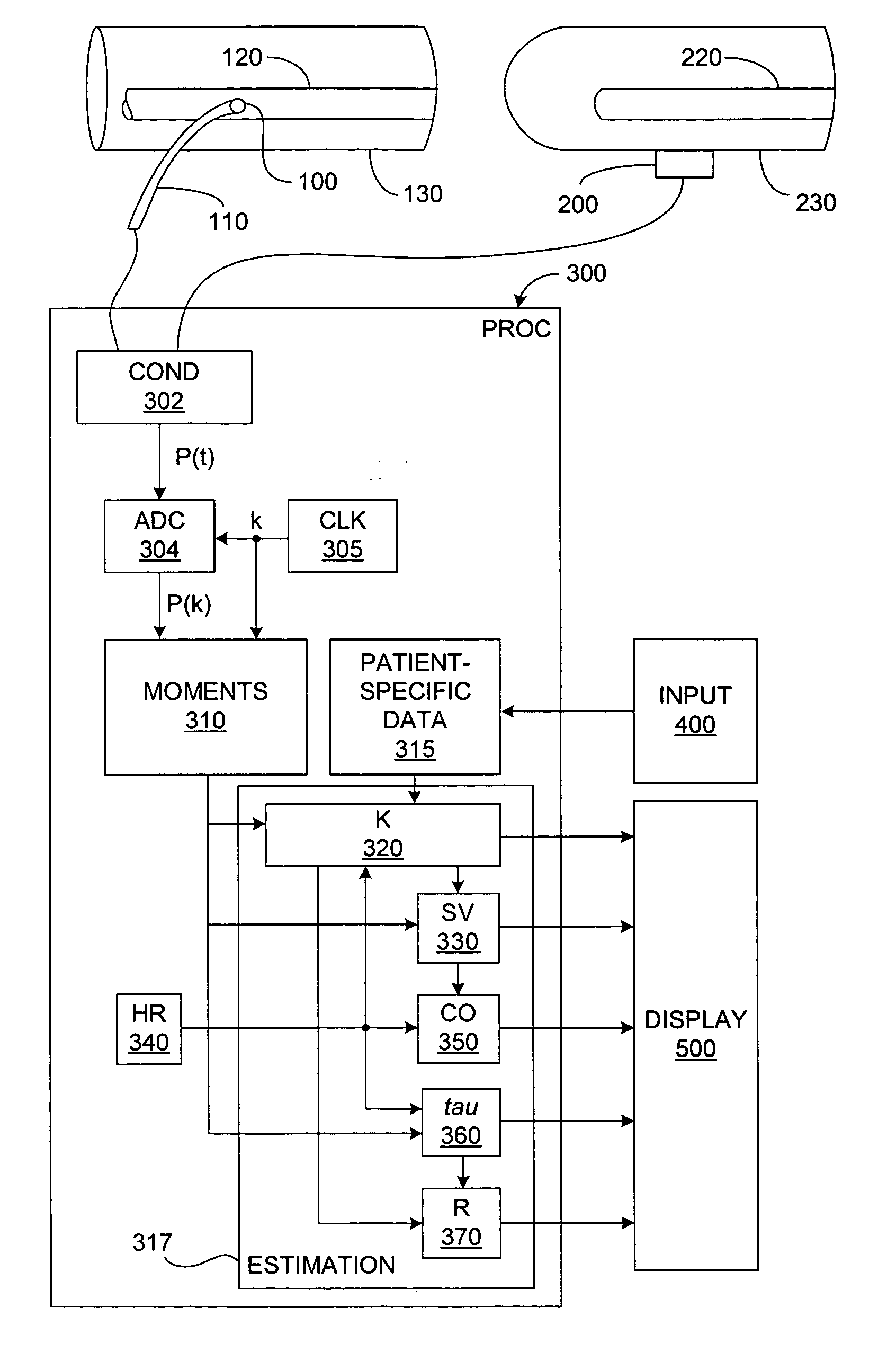
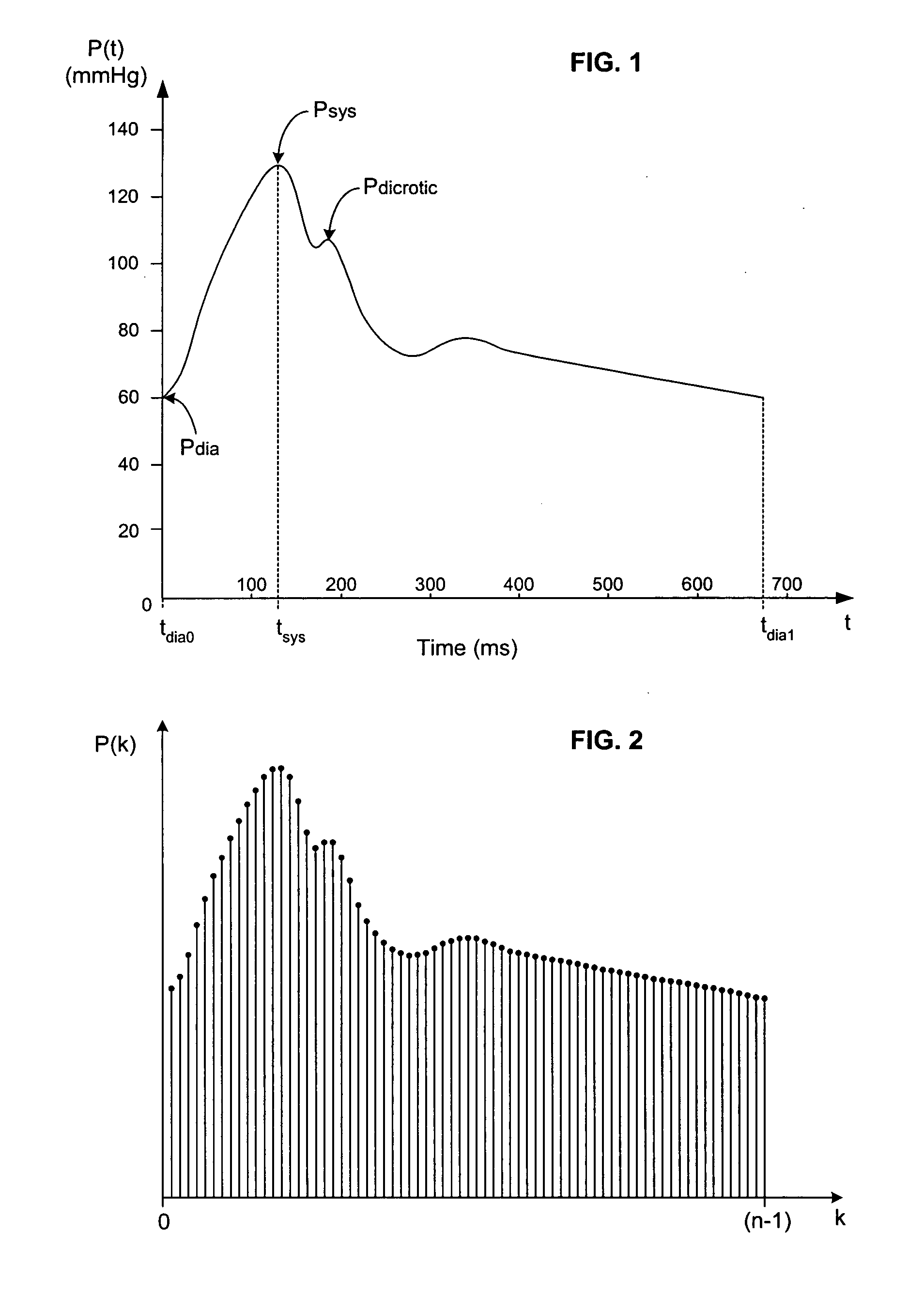
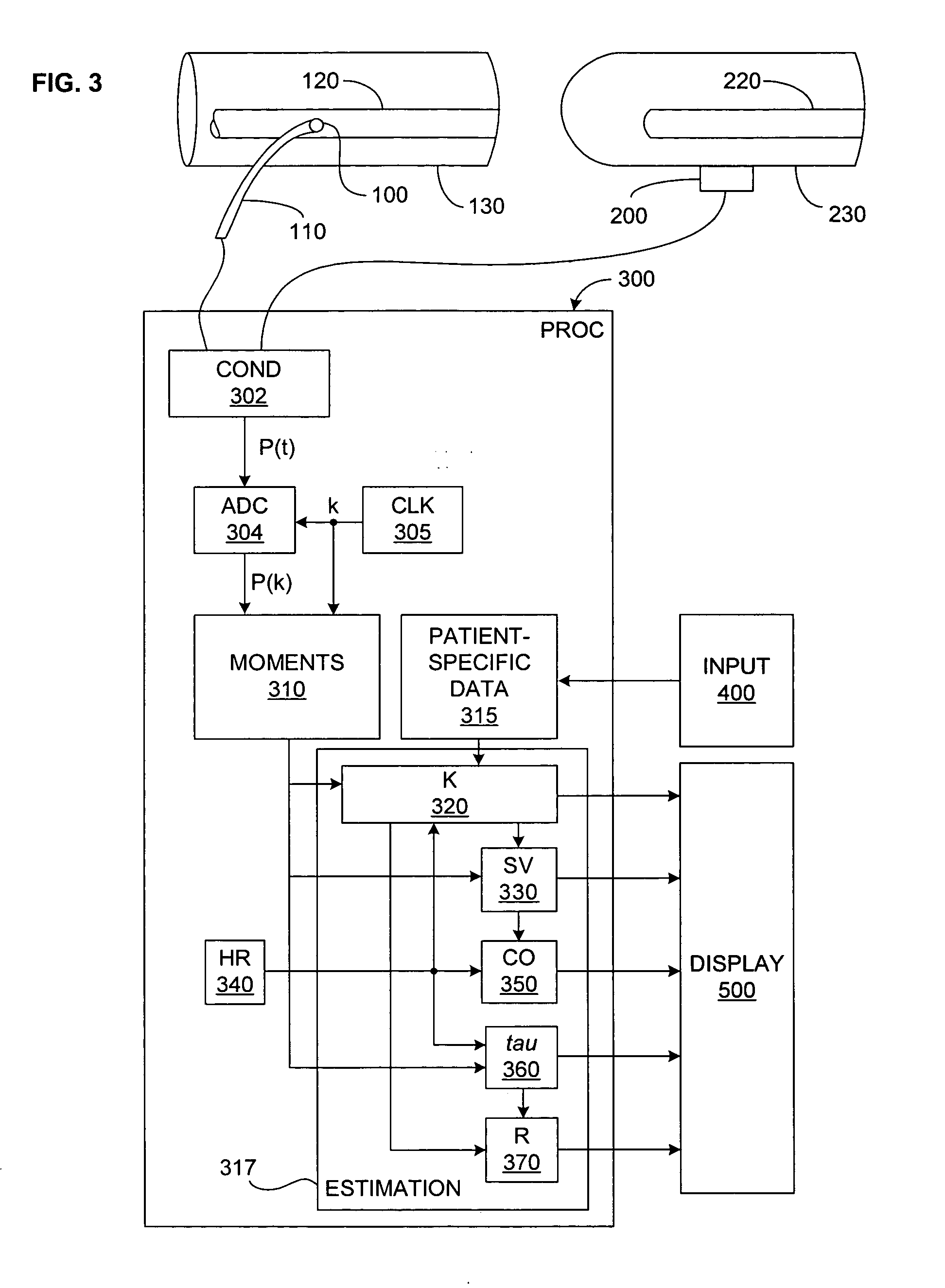
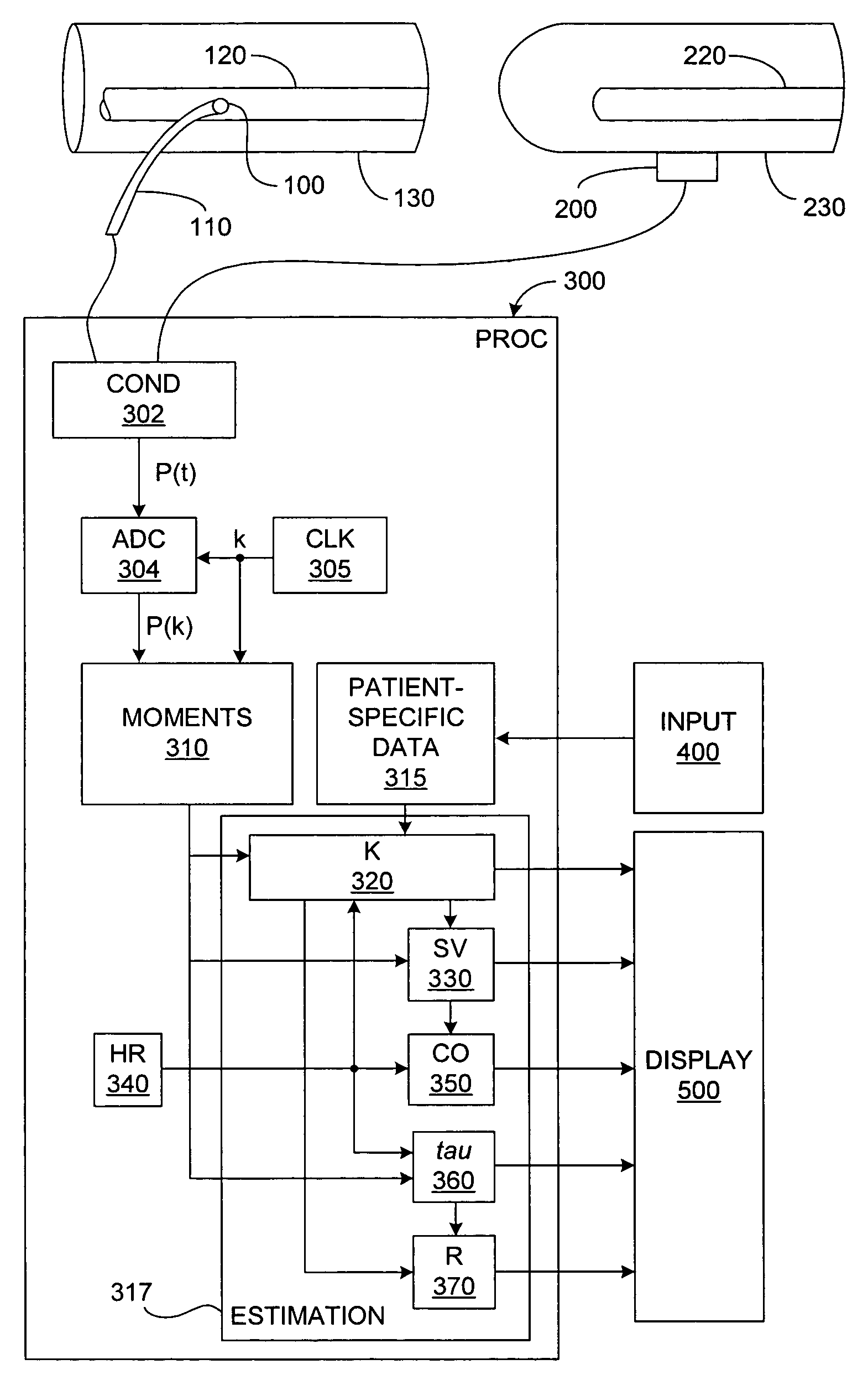
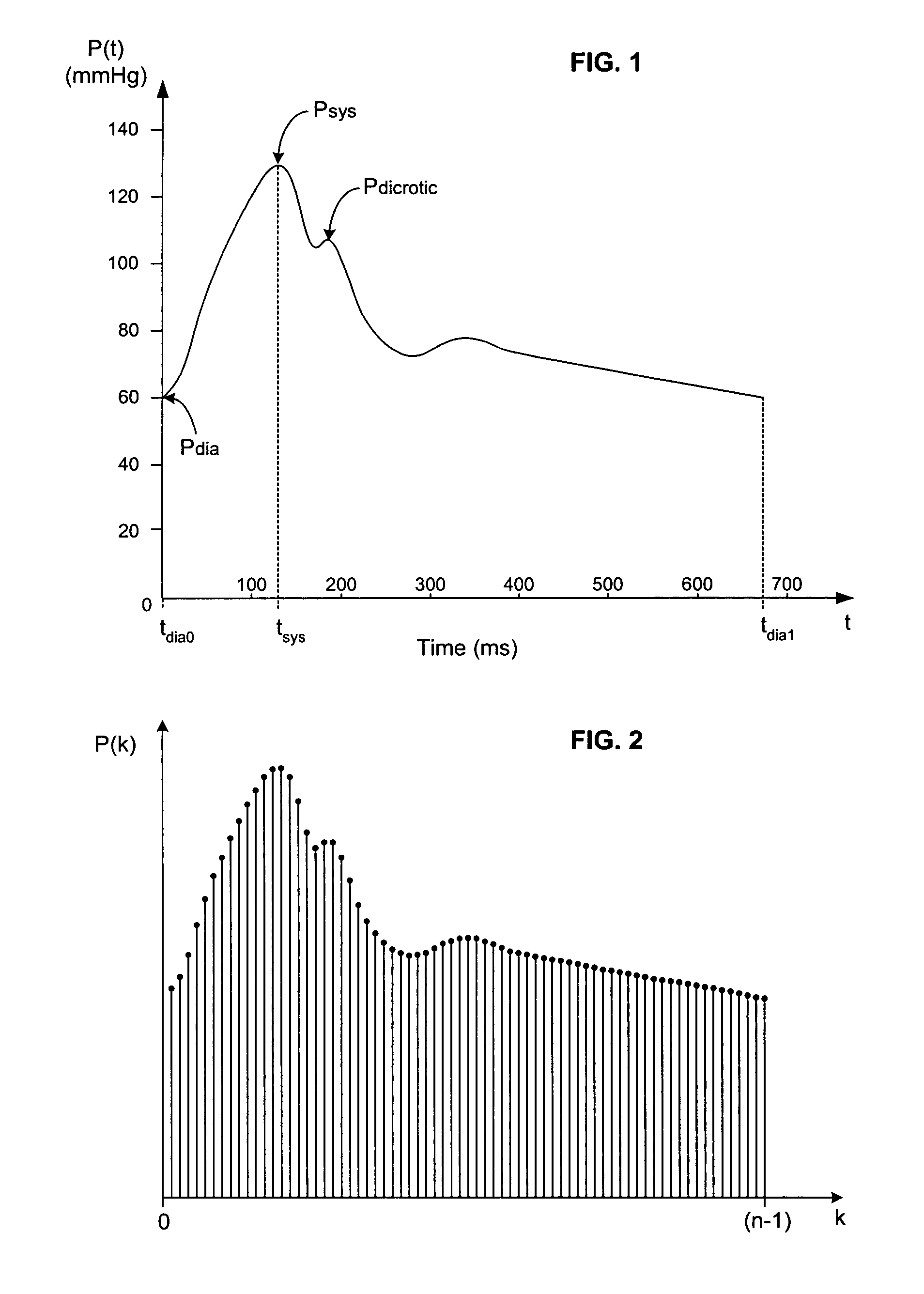
Arterial pressure-based, automatic determination of a cardiovascular parameter
One or more cardiovascular parameters is estimated as a function of the arterial pressure waveform, in particular, using at least one statistical moment of pressure waveform having an order greater than one. Arterial compliance, the exponential pressure decay constant, vascular resistance, cardiac output, and stroke volume are examples of cardiovascular parameters that can be estimated using various aspects of the invention. In one embodiment of the invention, not only are the first four moments (mean, standard deviation, skewness, and kurtosis) of the pressure waveform used to estimate the cardiovascular parameter(s) of interest, but also heart rate, statistical moments of a set of pressure-weighted time values, and certain anthropometric patient measurements such as age, sex, body surface area, etc.
Owner:EDWARDS LIFESCIENCES CORP
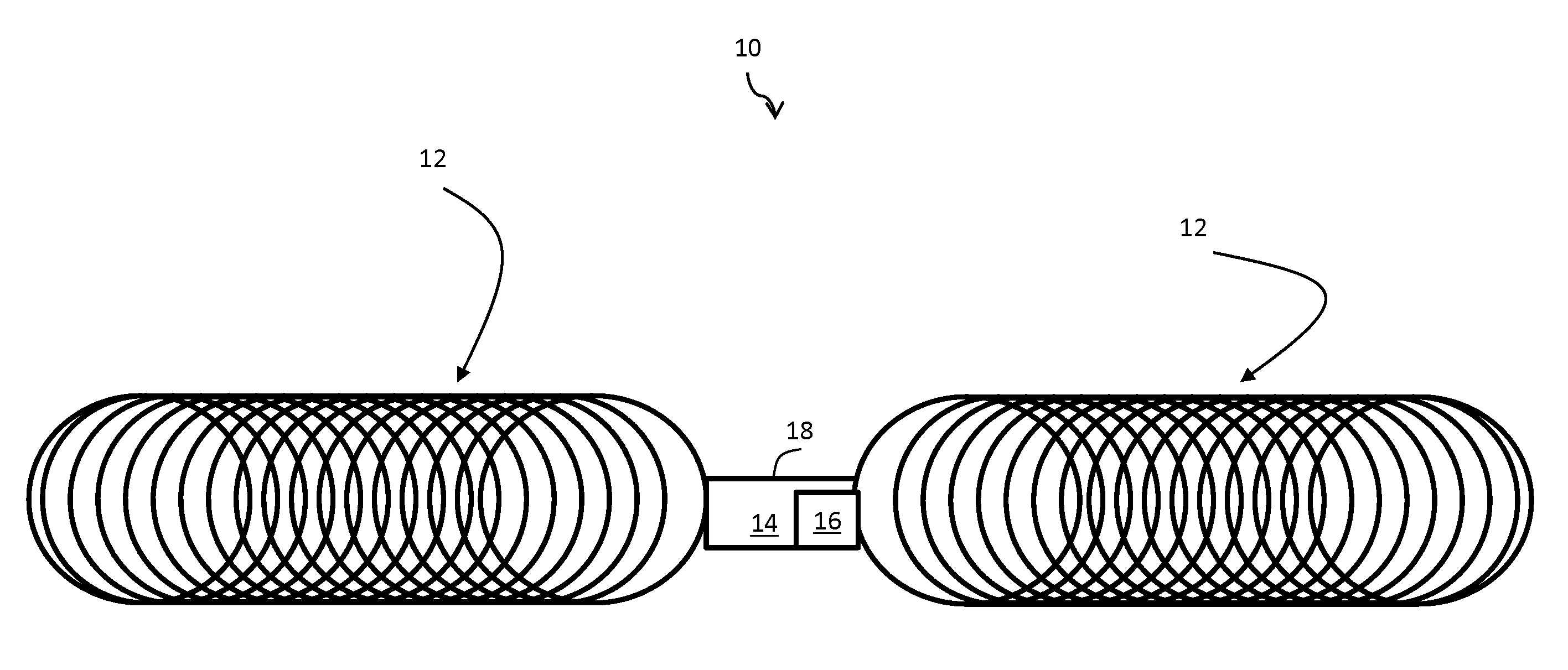
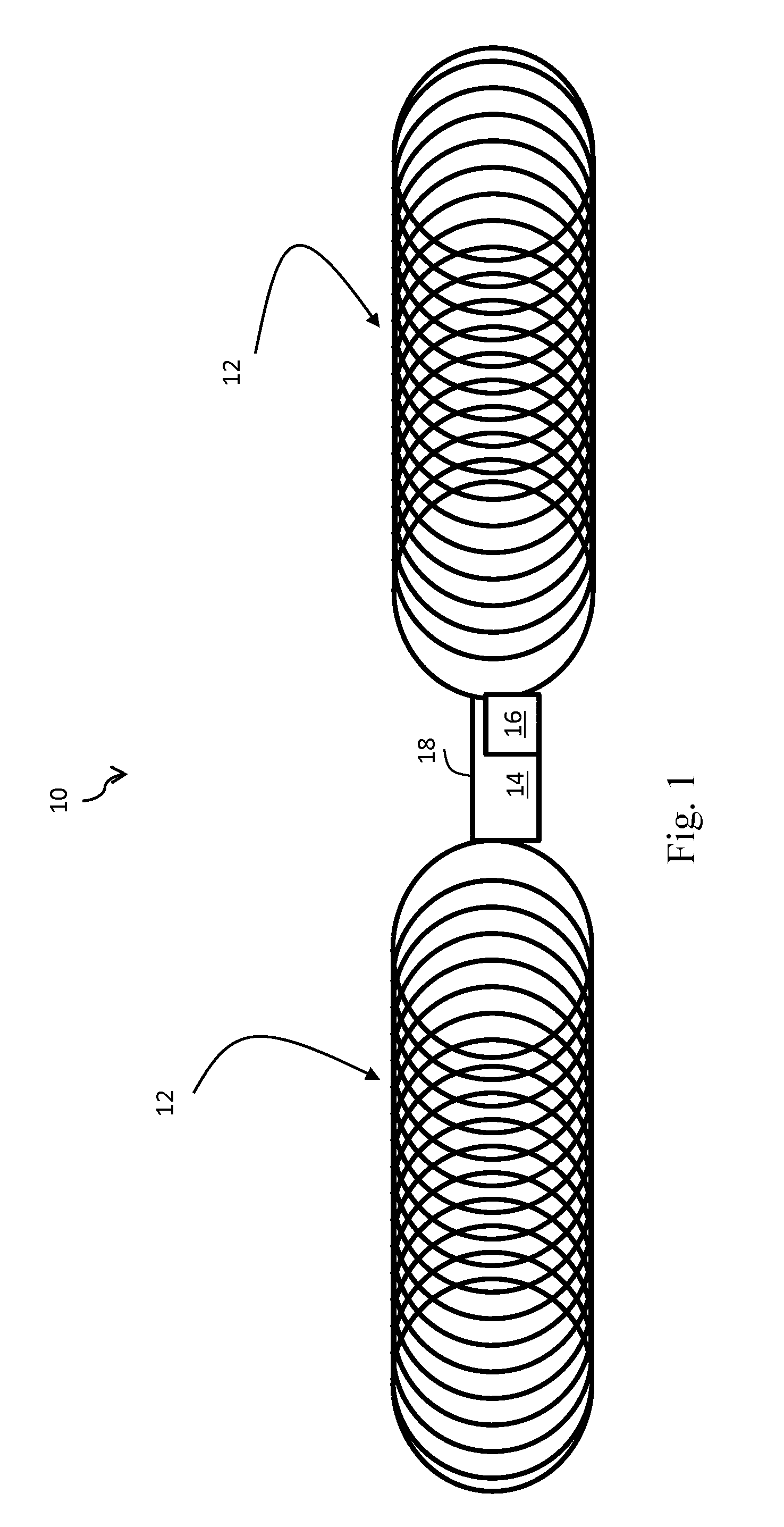
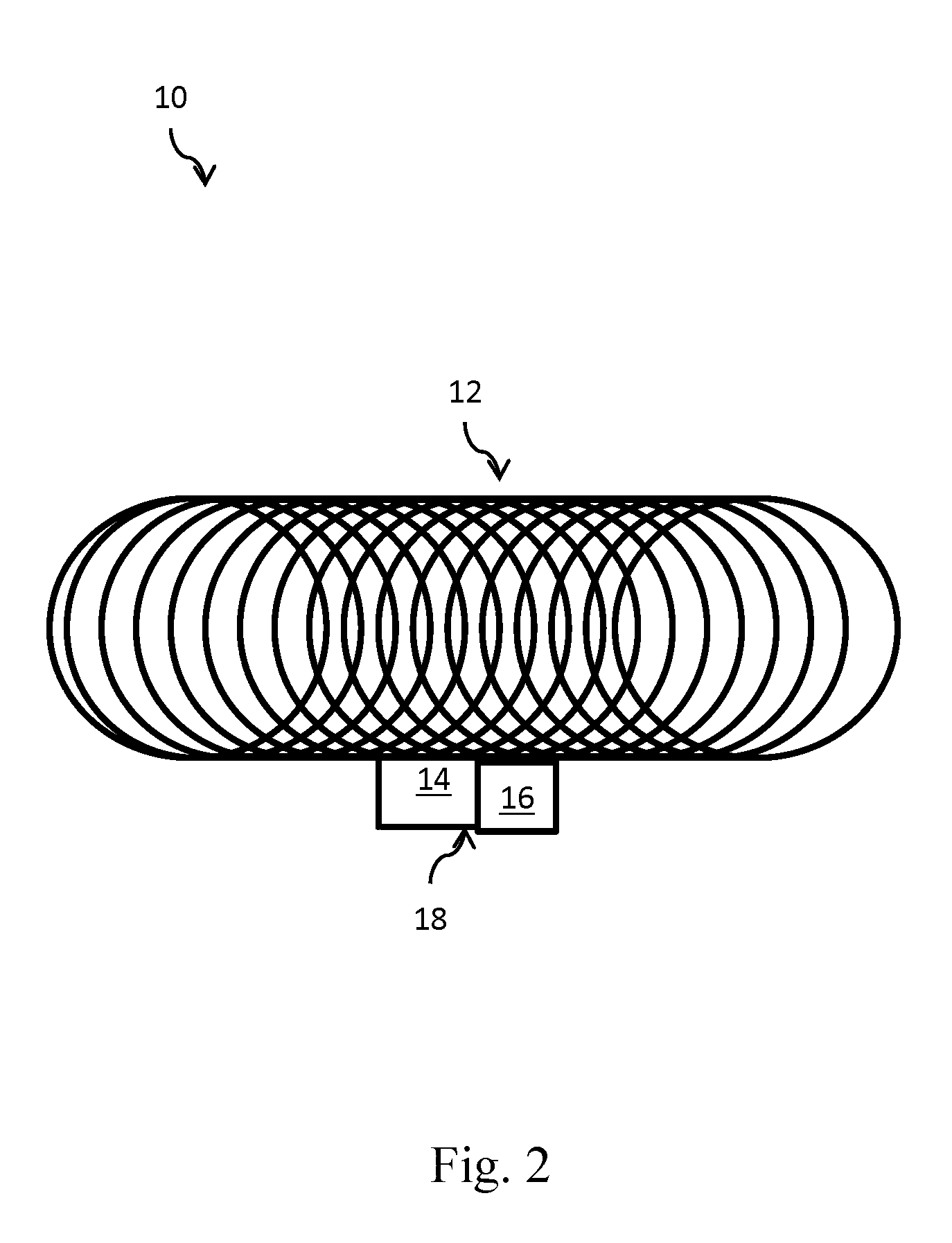
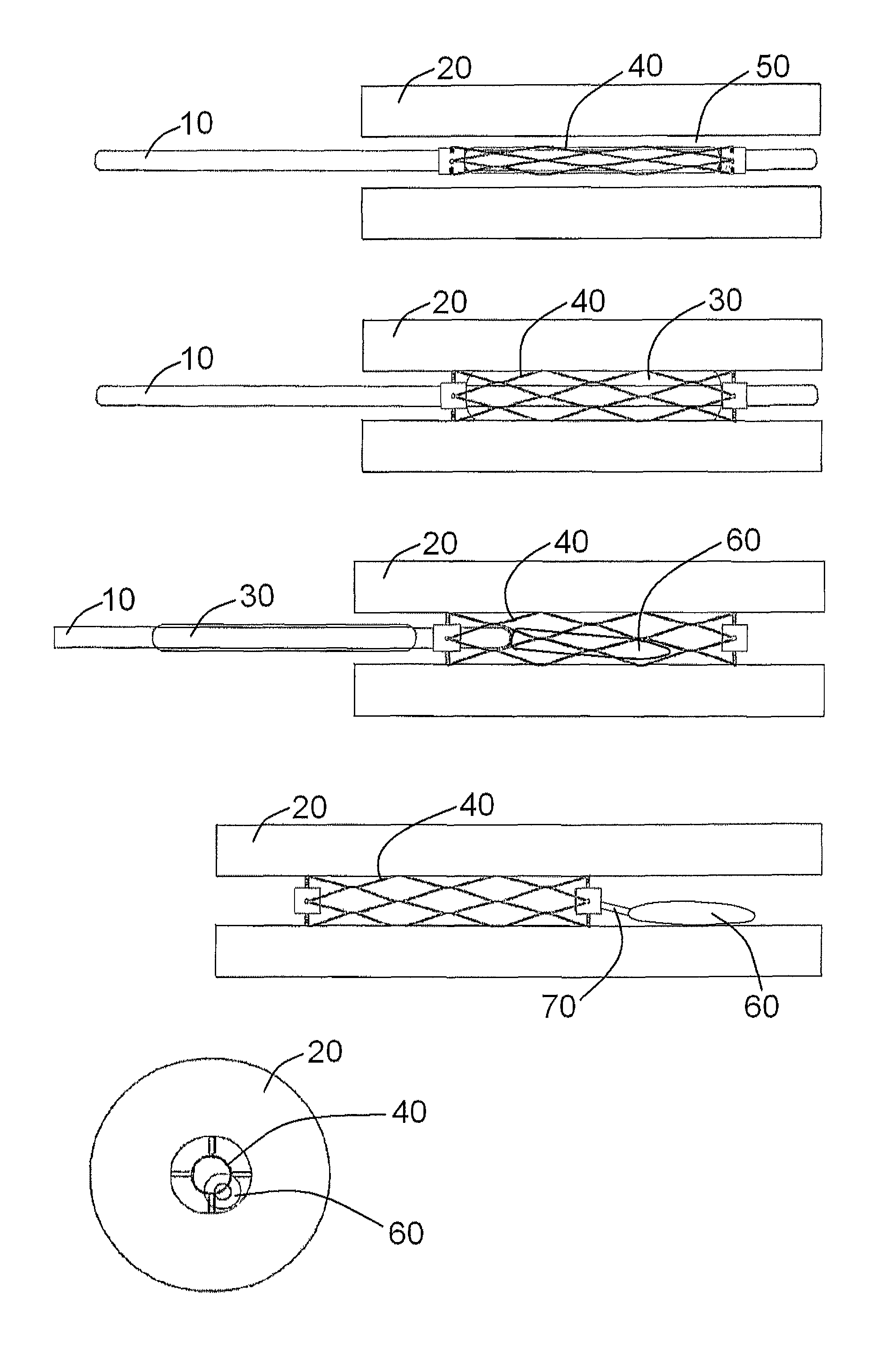
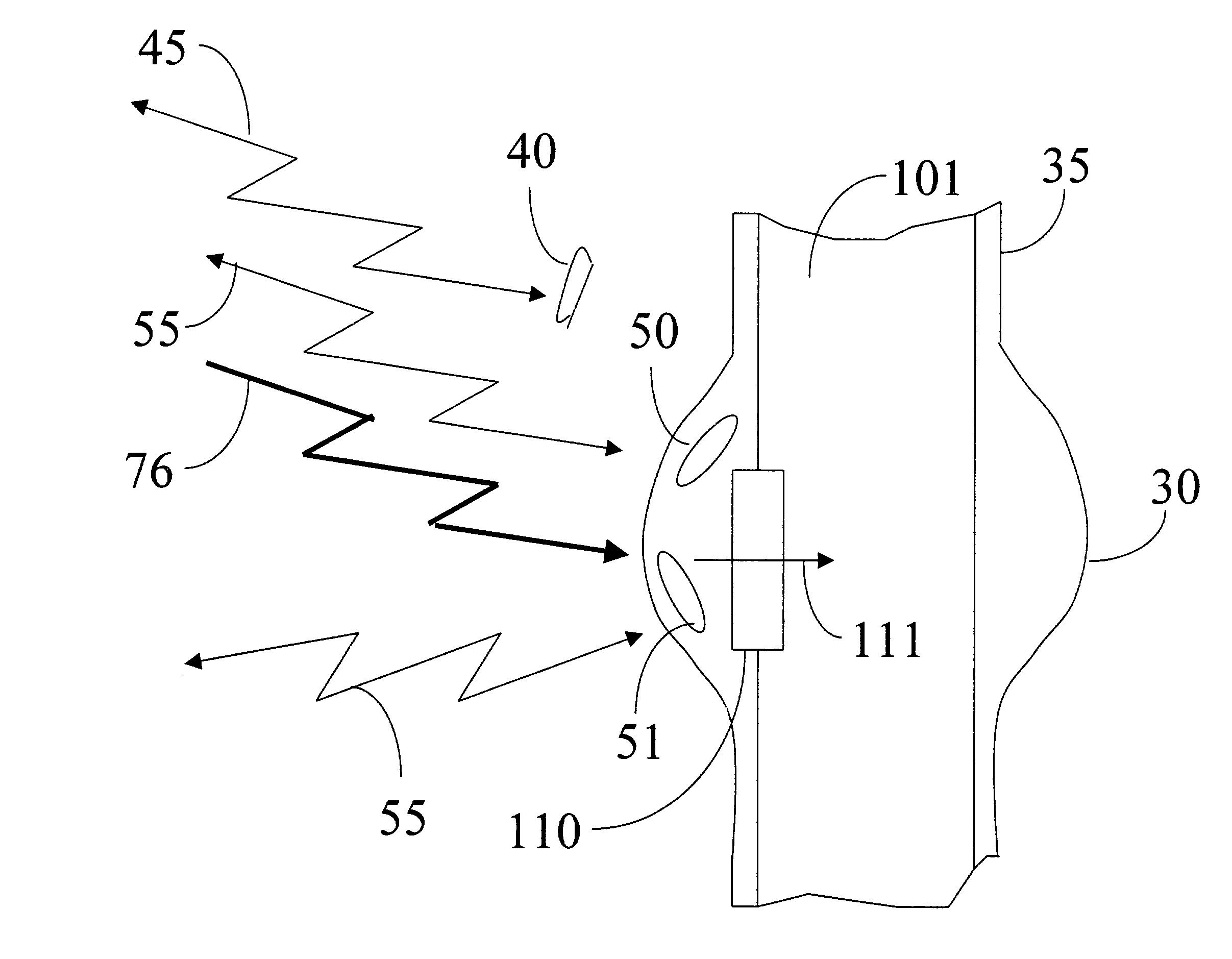
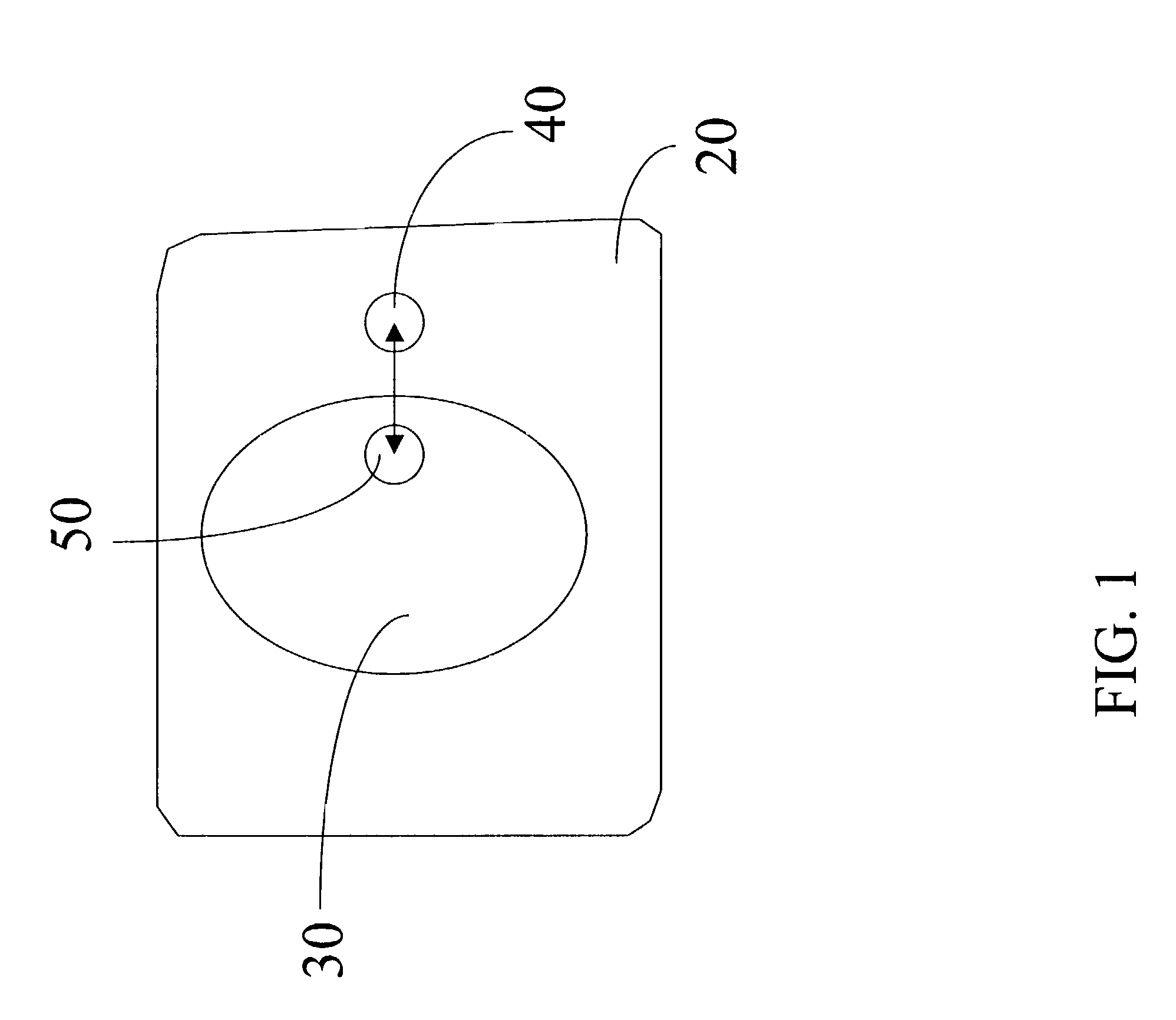
Miniature stent-based implantable wireless monitoring devices
A system is provided for the transmission of in vivo arterial pressure, the system comprising: an a pressure sensor whereby in vivo arterial pressure data is collected; a wireless transmitter, whereby the in vivo arterial pressure data is transmitted to be received disposed externally to a patient in which the system is disposed; a stent body, the stent body having an integral antenna, and a power source, whereby power is supplied to the system.
Owner:PURDUE RES FOUND INC
Pressure-based system and method for determining cardiac stroke volume
ActiveUS7220230B2Evaluation of blood vesselsCatheterArterial pressure waveformDecreased mean arterial pressure
Cardiac stroke volume (SV) of a subject is estimated as a function of a value derived from a measured arterial pressure waveform. The value may be the standard deviation, or a function of the difference between maximum and minimum pressure values, or a function of either the maximum value of the first time derivative or the absolute value of the minimum of the first time derivative of the pressure waveform, or both, or a function of the magnitude of one or more spectral components of the pressure waveform at a frequency corresponding to the heart rate. Cardiac output is then estimated as the product of the subject's heart rate and SV, scaled by a calibration constant. Arterial pressure may be measured invasively or non-invasively.
Owner:EDWARDS LIFESCIENCES CORP
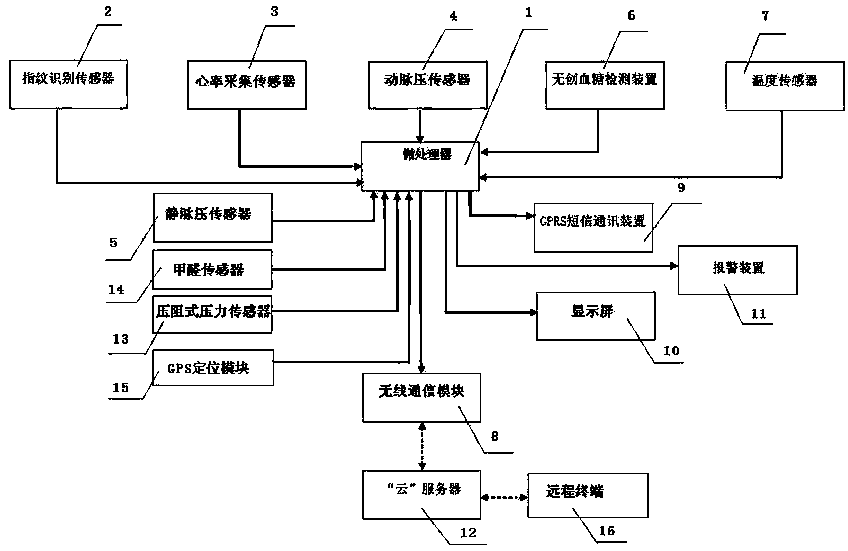
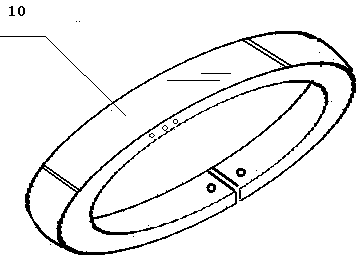
Physiological index detector
ActiveCN103393414AHigh densityImprove scalabilityDiagnostic recording/measuringSensorsCurve shapeDecreased mean arterial pressure
The invention discloses a physiological index detector. The physiological index detector comprises a microprocessor, a fingerprint identification sensor, a heart rate acquisition sensor, an arterial pressure sensor, a venous pressure sensor, a noninvasive blood glucose detection device, a temperature sensor, a wireless communication module, a GPRS short message communication device, a display screen and a warning device. The physiological index detector is a wristband-type structure fit to the wrist curve of the human body, components in the circuit portion are installed by using a flexible printed circuit (FPC), the FPC is mounted in the wristband-type physiological index detector in a circular arc shape, the display screen is an organic light emitting diode (OLED) which is arranged along the outer side of the wristband-type physiological index detector in an arc-shaped curve shape, and the wireless communication module transmits the acquired physiological index data of the human body to a cloud server for editing, preserving and processing. The physiological index detector is convenient to carry and measure and data are uploaded to the cloud, so that the physiological index data can be preserved for a long time, analyzed, tracked and warned.
Owner:JIANGSU HUITONG GRP
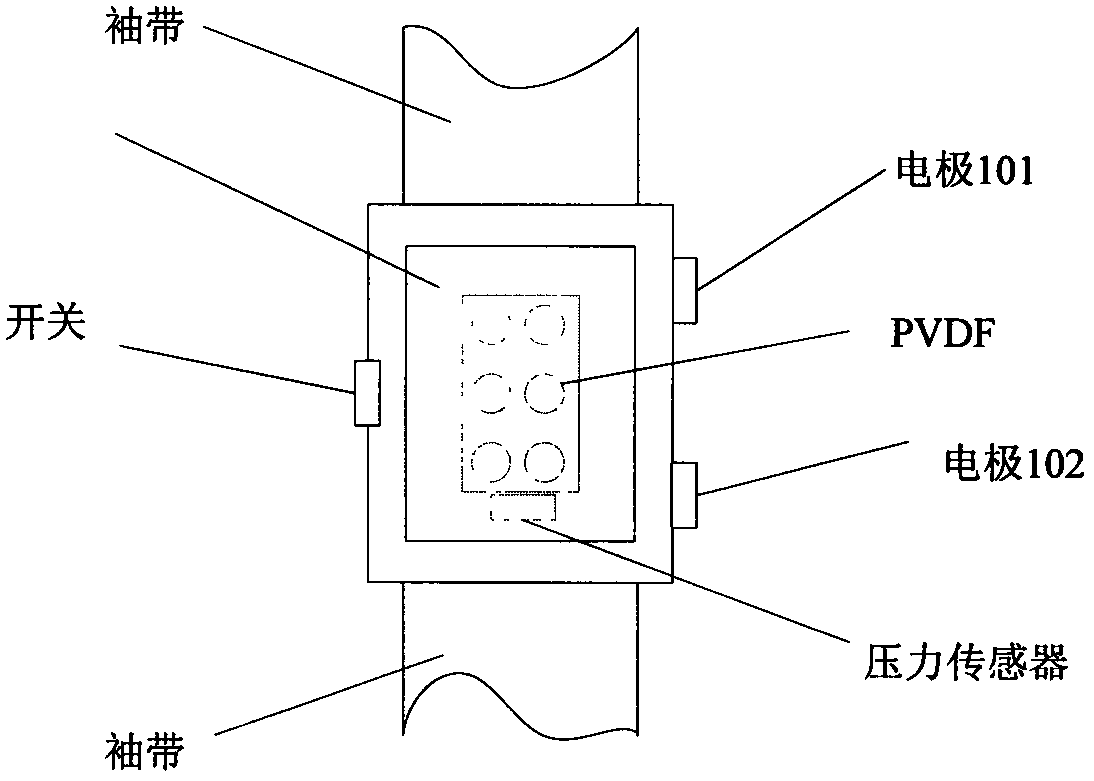
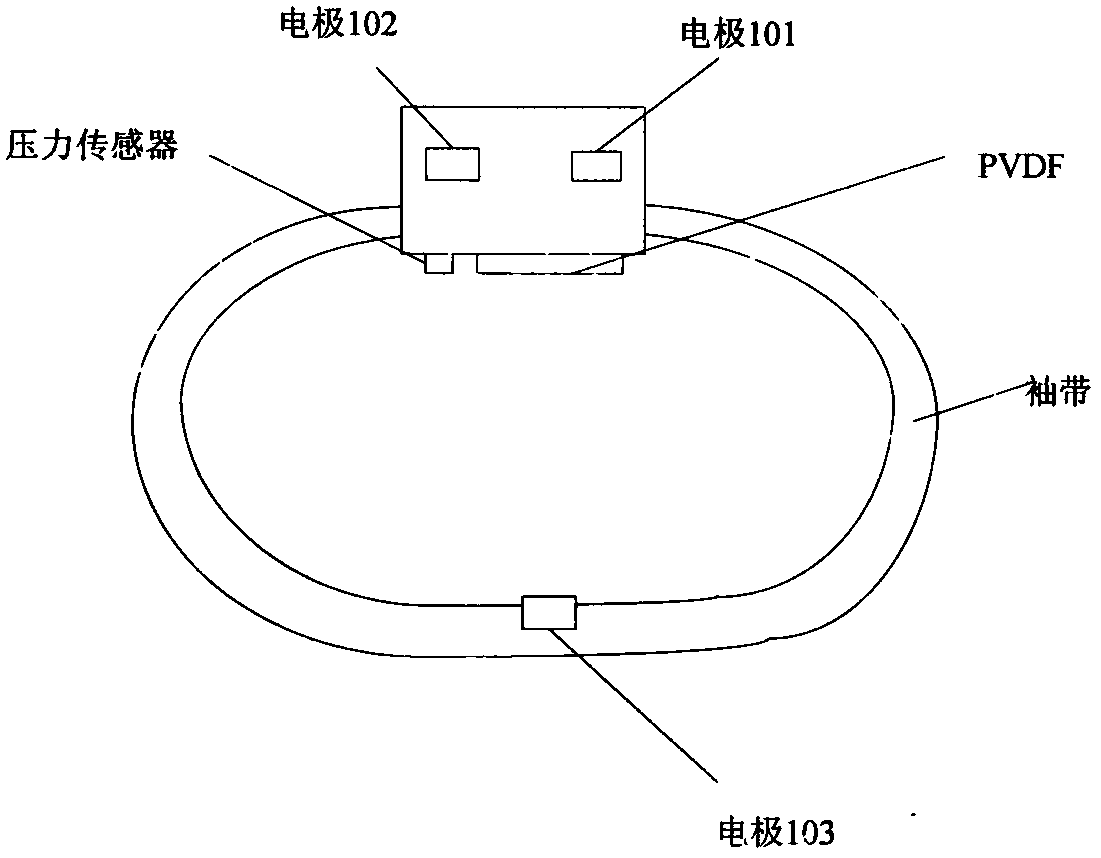
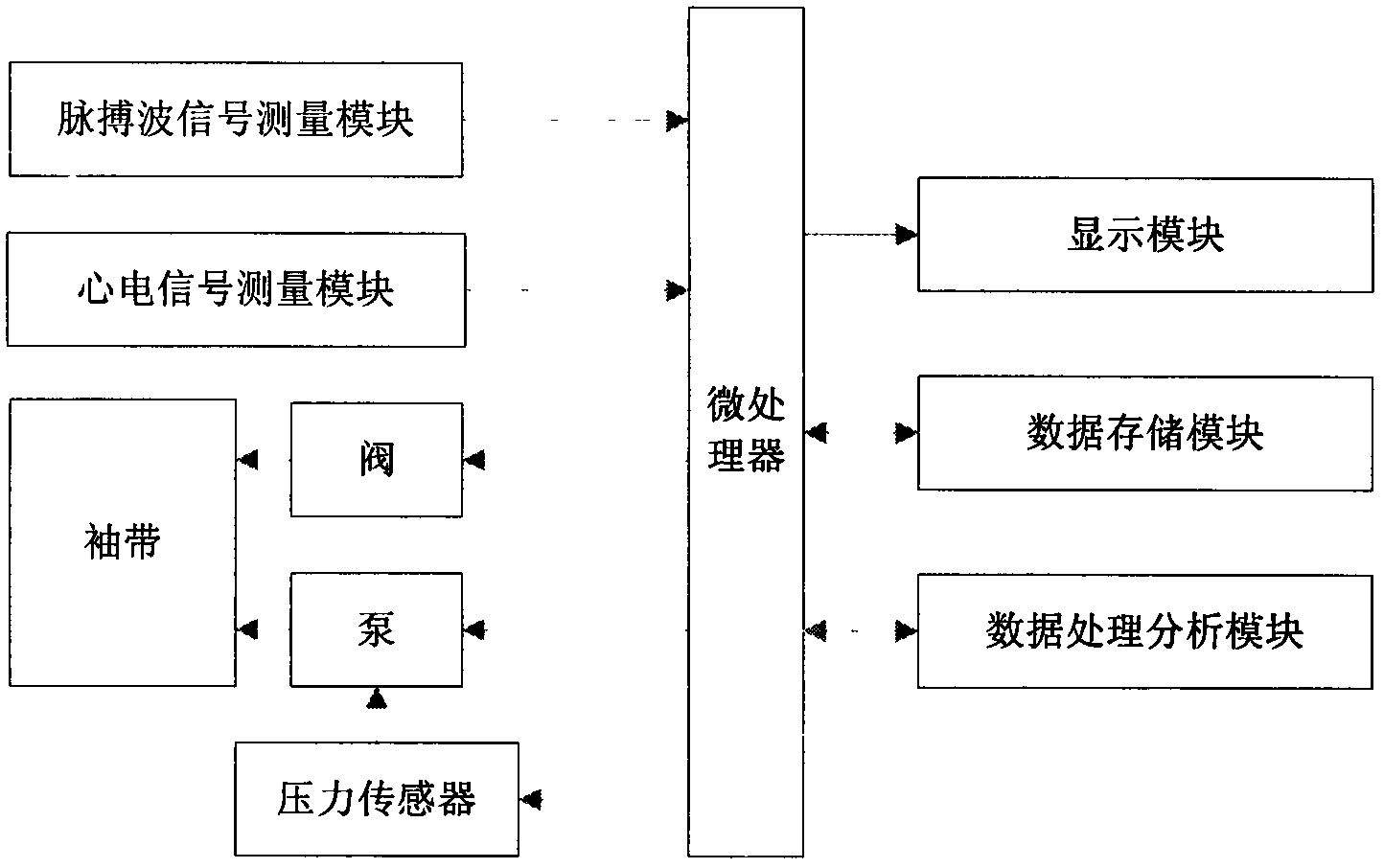
Research of dynamic blood pressure detection and calibration method of radial artery
InactiveCN104257371AImprove comfortSmall changes in body positionDiagnostic recording/measuringSensorsOscillometryEcg signal
The invention relates to a dynamic blood pressure detection and calibration method of a radial artery. The method comprises the following steps: measuring a blood pressure value BP1 to perform first calibration by using oscillography; measuring a blood pressure value BP2 to perform second calibration by using correlation of an electrocardiosignal, a pulse wave signal and human arterial pressure; finally performing continuous monitoring of blood pressure by using the linear relation between pulse wave transmission time difference PWT of two different parts on a wrist and the human arterial blood pressure which are measured at the same time.
Owner:TIANJIN POLYTECHNIC UNIV
Arterial blood pressure monitor with a liquid filled cuff
InactiveUS20100106029A1Mechanical couplingPositioning of criticalEvaluation of blood vesselsCatheterBLOOD FILLEDExhaust valve
A non-invasive arterial blood pressure monitor uses an inflatable cuff that incorporates the first bladder that is filled with non-compressible liquid or gel. The bladder can be pressurized by an action of a pressurizing device superimposed onto its outer surface. In a preferred embodiment, a pressurizing device is an air-filled second bladder being connected to an air pump and bleed valve. The first bladder is positioned between the patient's body and the second bladder. During operation, the second bladder compresses the first bladder, which, in turn, compresses the patient's artery against the supporting bone. The mechanical coupling between the blood-filled artery of a patient and the liquid-filled bladder of a dual-bladder cuff is improved for detecting pressure oscillations in a broad frequency range. The pressure sensor that is coupled to the first bladder also functions as a hydrophone for picking-up the mechanical oscillations from any part of the occluded limb or digit. This allows for improved computation of the arterial pressure.
Owner:HELEN OF TROY LIMITED
Arterial pressure-based, automatic determination of a cardiovascular parameter
One or more cardiovascular parameters is estimated as a function of the arterial pressure waveform, in particular, using at least one statistical moment of pressure waveform having an order greater than one. Arterial compliance, the exponential pressure decay constant, vascular resistance, cardiac output, and stroke volume are examples of cardiovascular parameters that can be estimated using various aspects of the invention. In one embodiment of the invention, not only are the first four moments (mean, standard deviation, skewness, and kurtosis) of the pressure waveform used to estimate the cardiovascular parameter(s) of interest, but also heart rate, statistical moments of a set of pressure-weighted time values, and certain anthropometric patient measurements such as age, sex, body surface area, etc.
Owner:EDWARDS LIFESCIENCES CORP
Calibration of pulse transit time measurements to arterial blood pressure using external arterial pressure applied along the pulse transit path
An apparatus and methods for adaptive and autonomous calibration of pulse transit time measurements to obtain arterial blood pressure using arterial pressure variation. The apparatus and methods give pulse transit time (PTT) devices an ability to self-calibrate. The methods apply a distributed model with lumped parameters, and may be implemented, for example, using pulse transit time measurements derived from a wearable photoplethysmograph (PPG) sensor architecture with an intervening pressurizing mechanism.
Owner:MASSACHUSETTS INST OF TECH
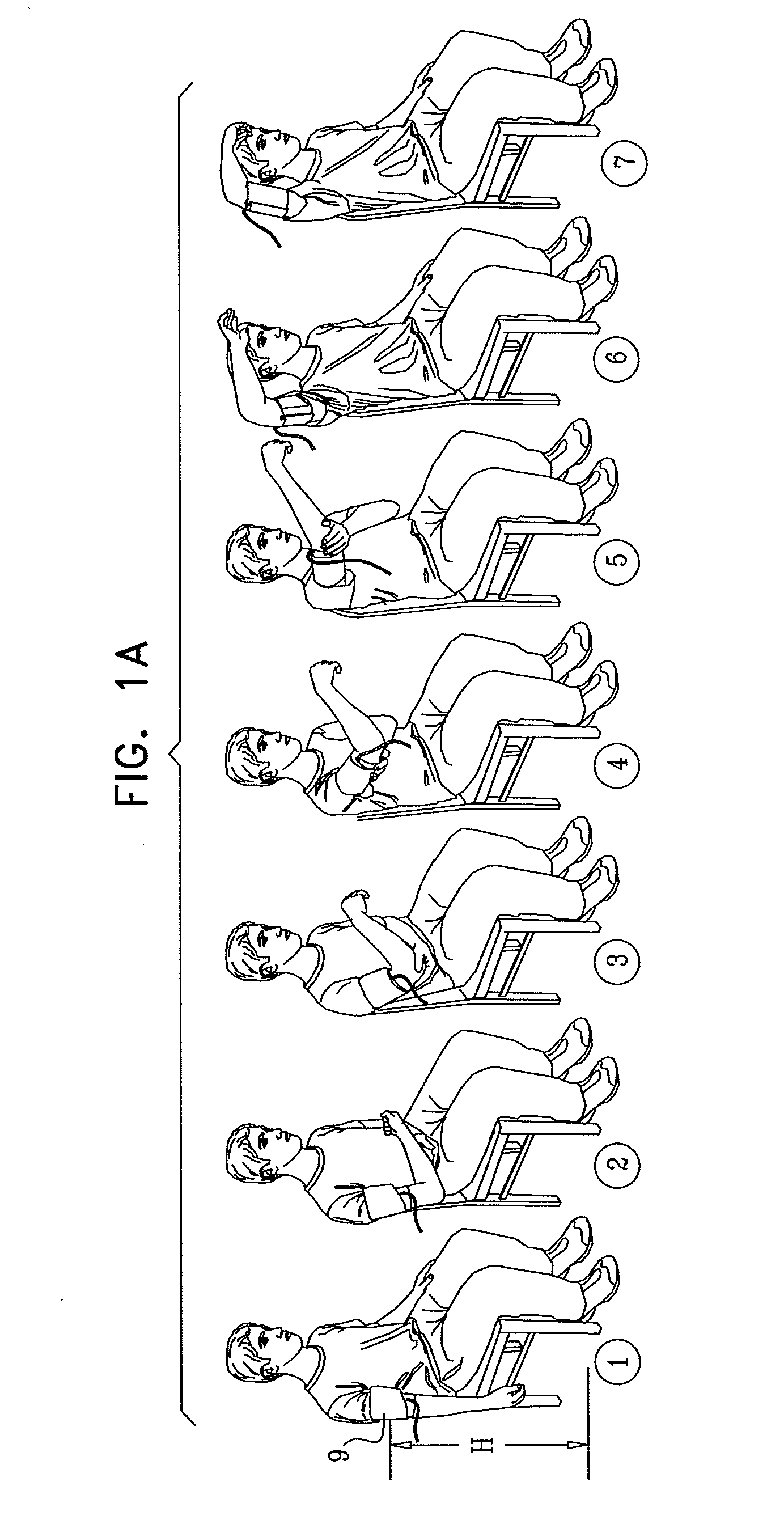
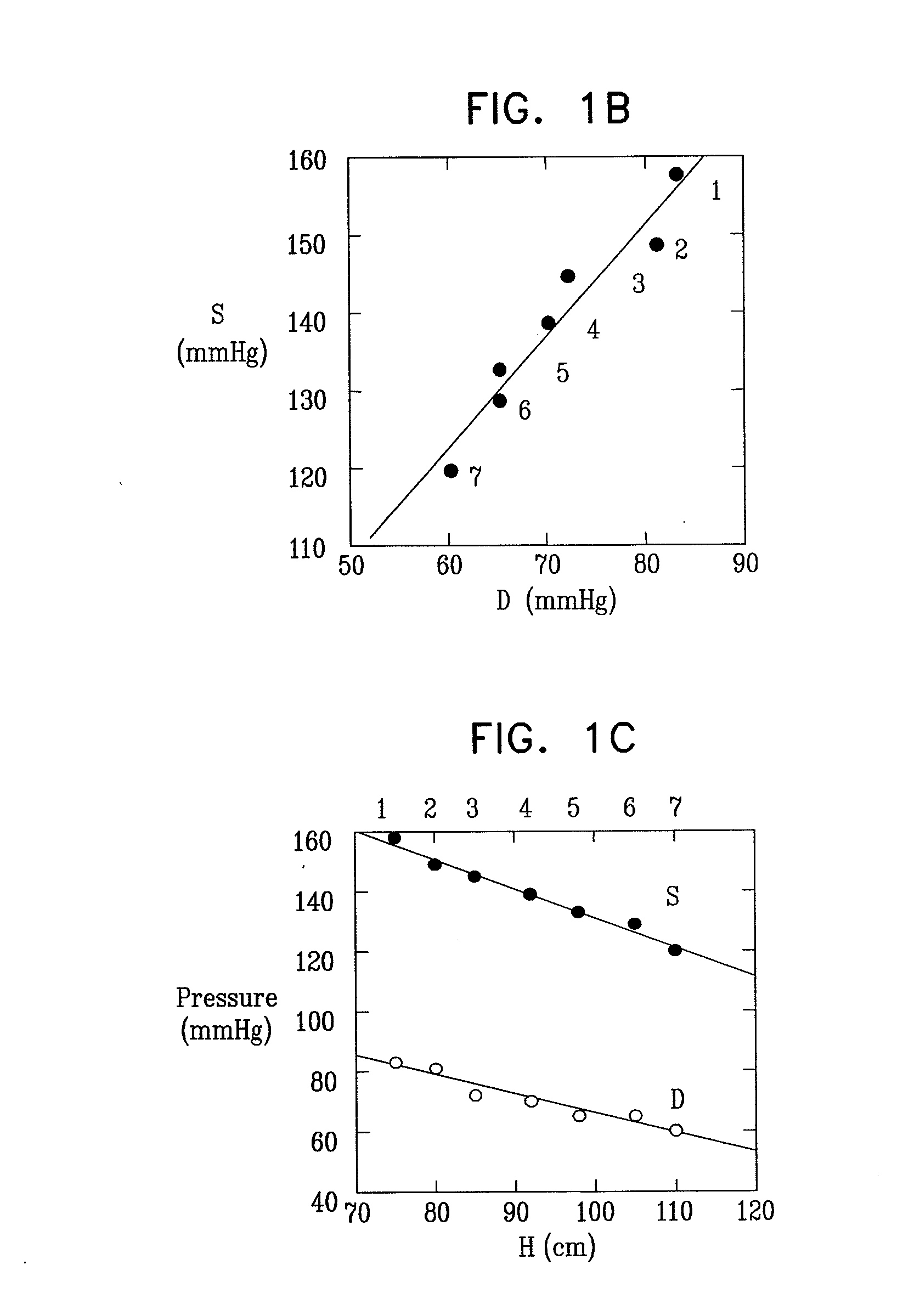
Determination of physiological parameters using repeated blood pressure measurements
InactiveUS20110009718A1Ultrasonic/sonic/infrasonic diagnosticsEvaluation of blood vesselsBlood pressureDecreased mean arterial pressure
A pulsewave detection unit is provided, at least a portion of the pulsewave detection unit being configured to be coupled to a portion of a subject's body, the pulsewave detection unit generating a signal that is responsive to arterial pressure of the portion of the subject's body. A pulsewave parameters determination unit receives respective first and second signals from the pulsewave detection unit, the signals being responsive to arterial pressure of the portion of the subject's body while the portion of the pulsewave detection unit that is coupled to the portion of the subject's body is at respective first and second heights, at respective times. An arterial parameters calculating unit determines an arterial property of the subject by processing the first and second signals, and generates an output in response to determining the arterial property. Other embodiments are also described.
Owner:GAVISH BENJAMIN
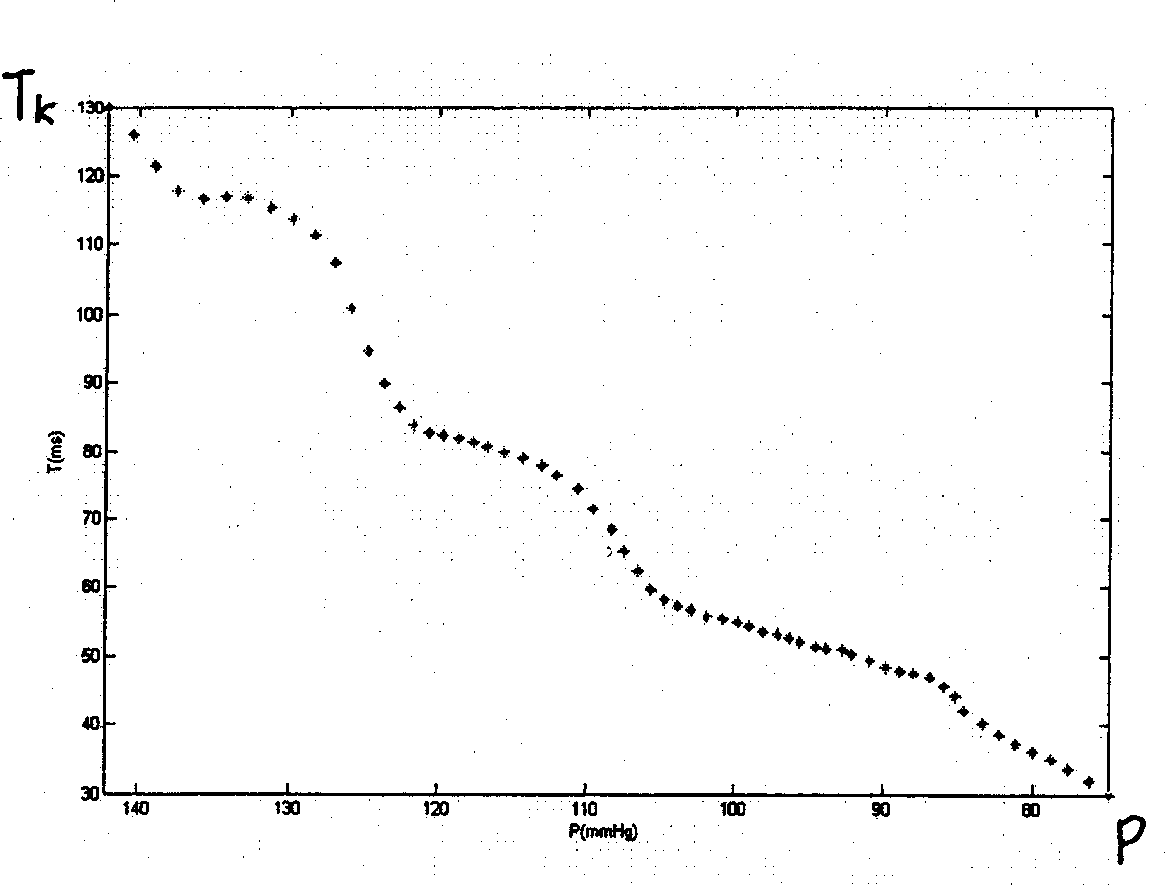
Method for measuring arterial pressure, apparatus and individual correction tech. therefor
InactiveCN1868399AHigh implementabilityReduce mistakesEvaluation of blood vesselsAngiographyContinuous measurementPhysical medicine and rehabilitation
A method and device for measuring the blood pressure of artery and its personalized correction technique are disclosed. A series of the pressure values (P) for sleeve band and the time delay values (Tk) of the relative remote Ke's sounds are obtained. The function relation Tk(P) between said pressure change and sound delay is in turn obtained. Measuring a Tk relative to a P can calculate out the blood pressure change. A regression equation for continuous measurements of arteral blood pressure is used to obtain a personalized correction coefficient.
Owner:BEIJING XINXING YANGSHENG TECHN CORP +1
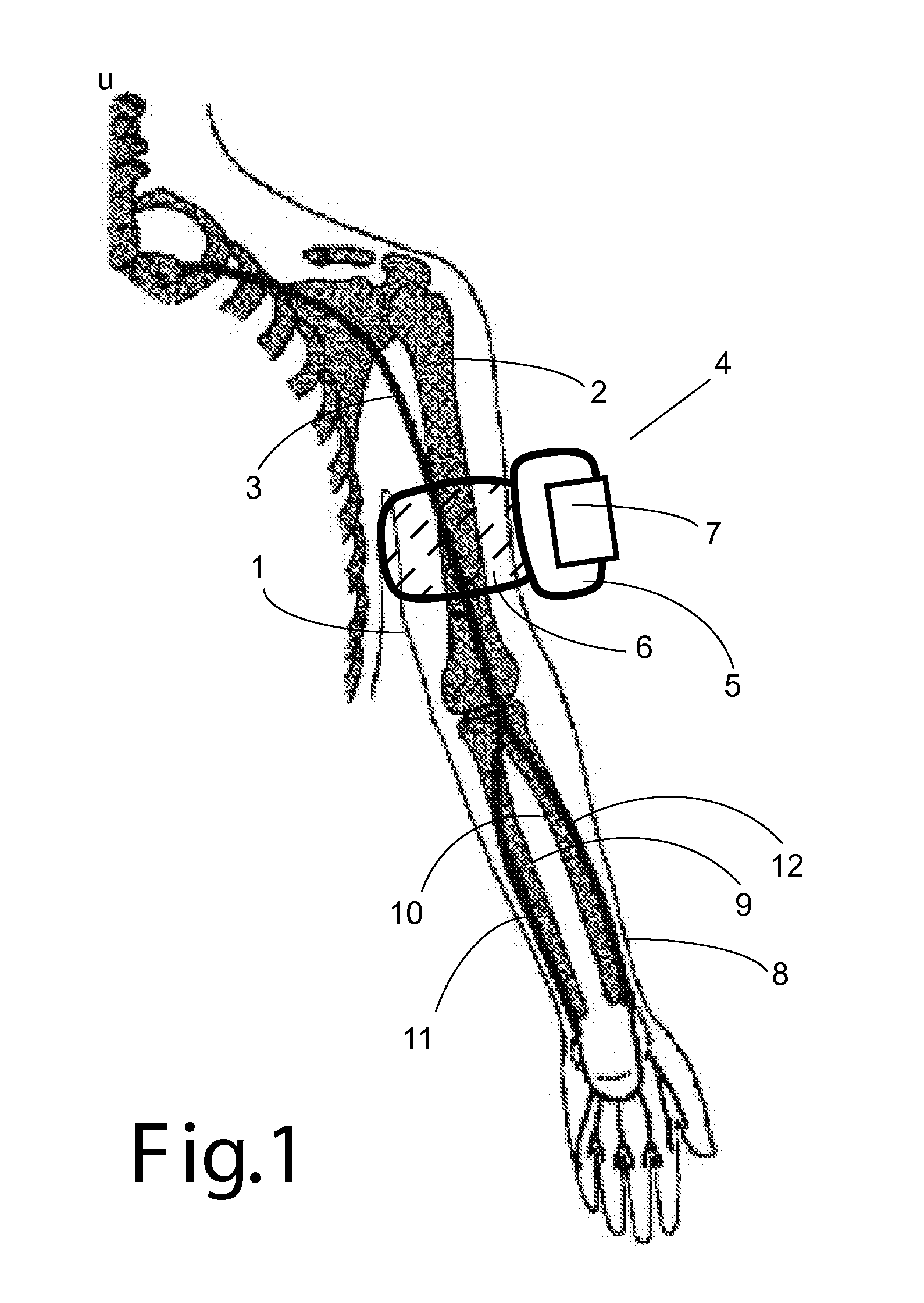
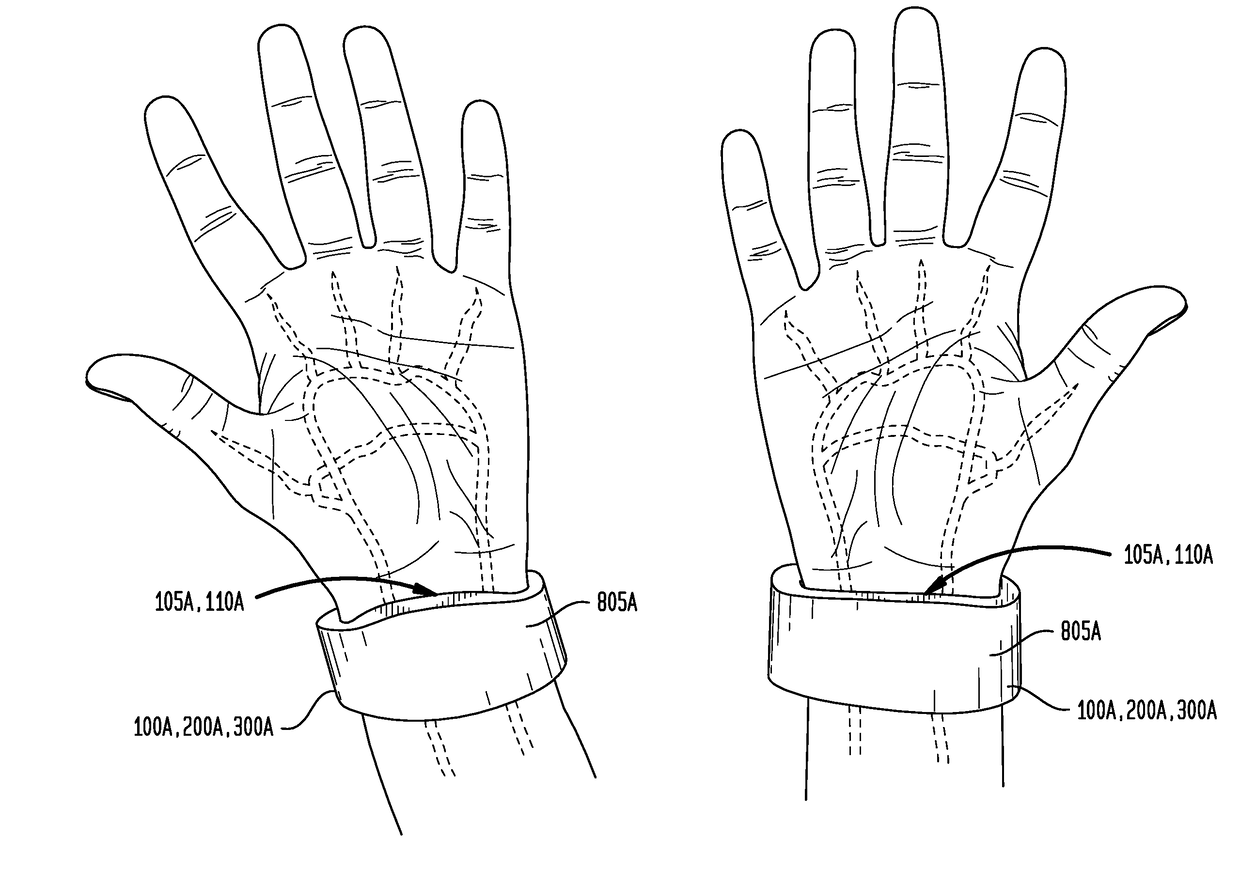
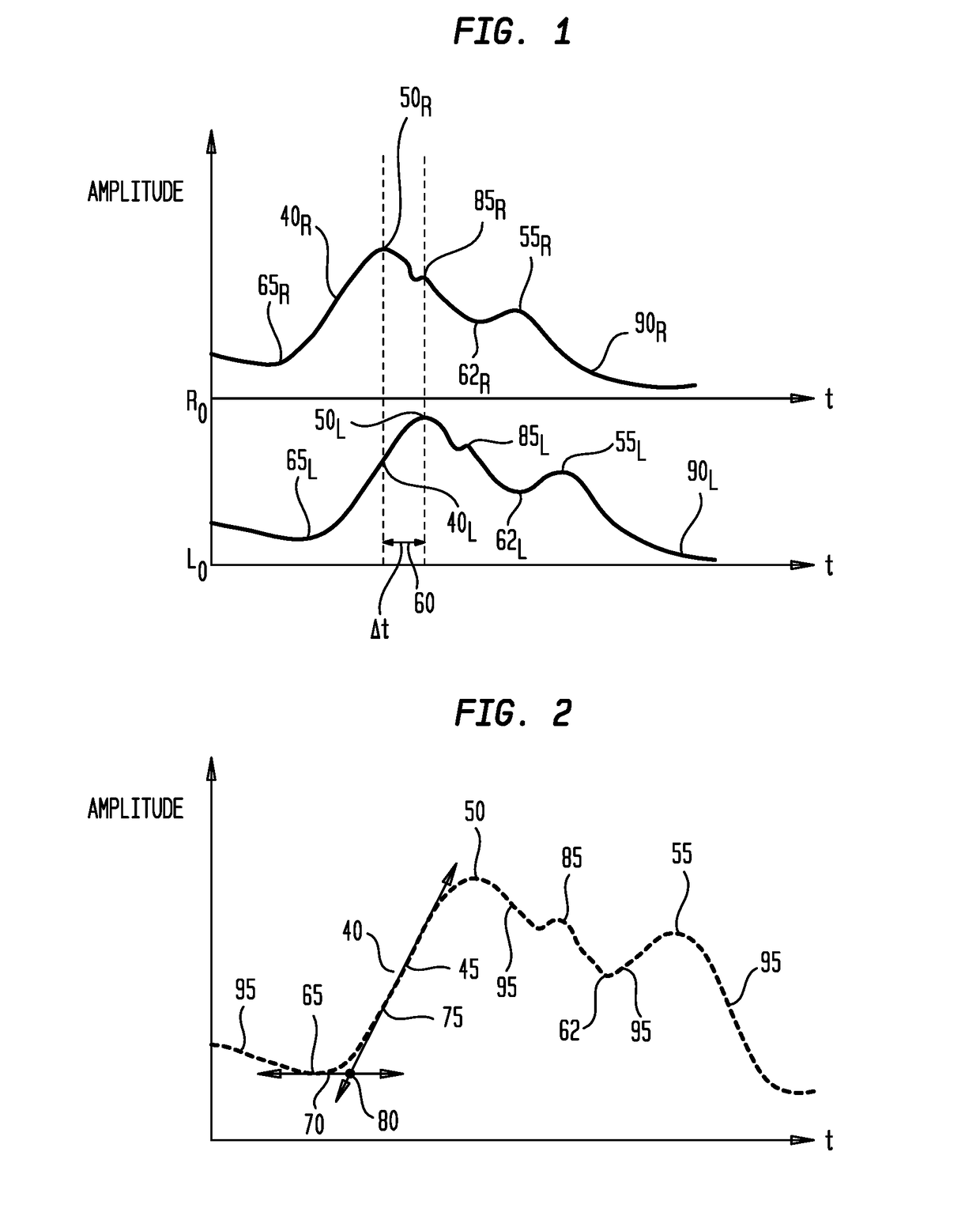
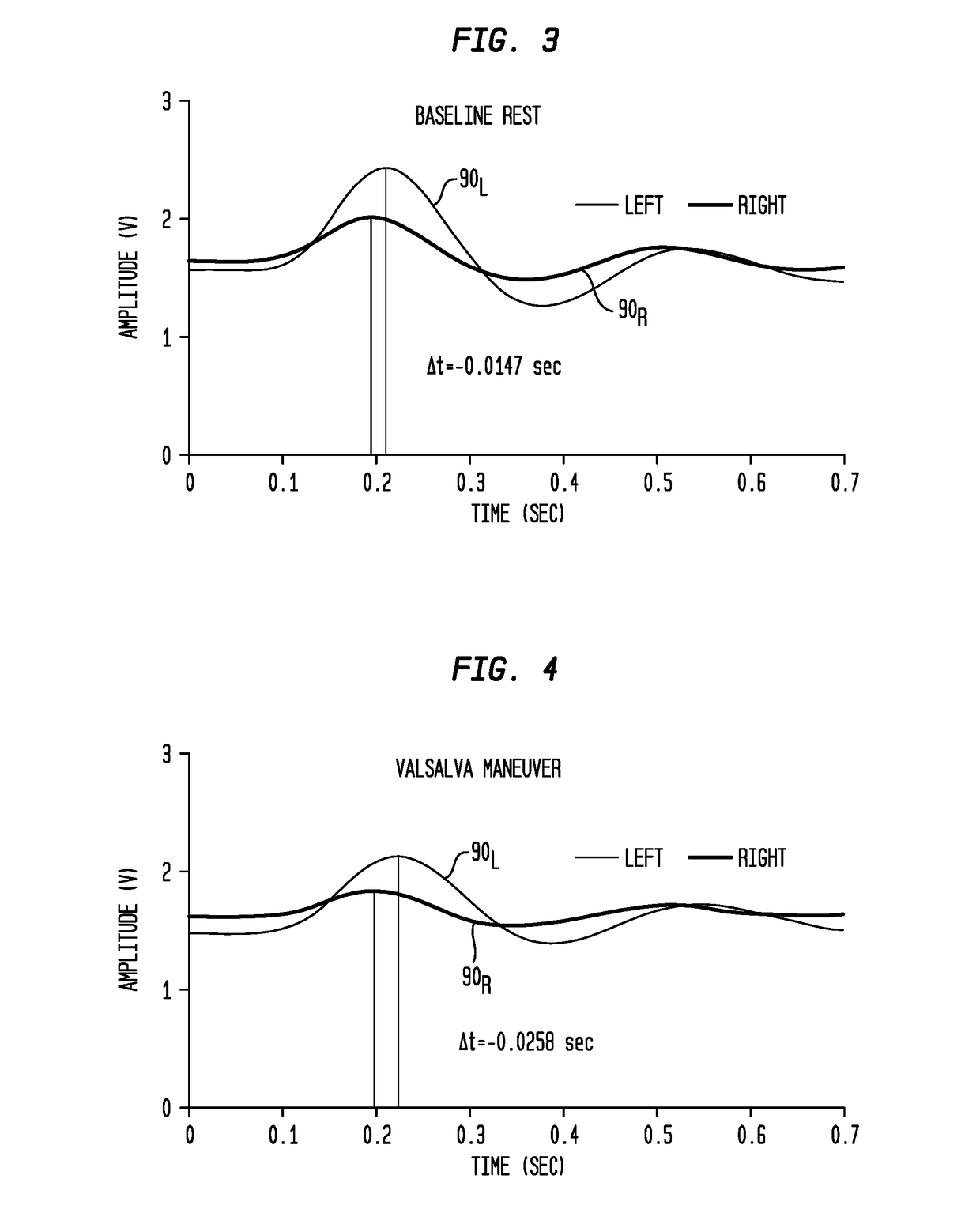
Ambulatory Blood Pressure and Vital Sign Monitoring Apparatus, System and Method
InactiveUS20180279965A1Fast BP acquisition timeImprove complianceAcoustic sensorsInertial sensorsDecreased mean arterial pressureEngineering
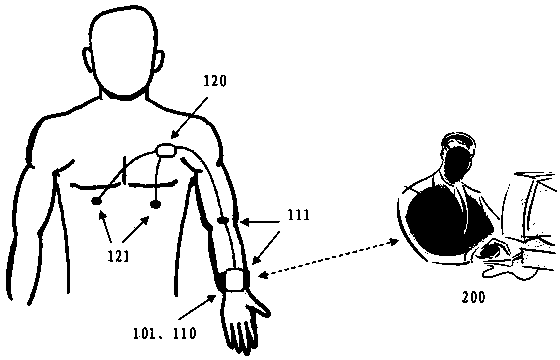
Representative methods, apparatus and systems are disclosed for determining one or more physiological parameters, such as for ambulatory blood pressure and other vital sign monitoring. A representative system comprises first and second wearable apparatuses to be worn on the user's left and right sides, and any of several types of central vital signs monitors. Another representative system is a handheld, singular apparatus to be held in both hands by the user. Another representative system comprises first and second wearable apparatuses without any additional central vital signs monitor. The various embodiments measure a differential pulse arrival time of left and right arterial pressure waves using corresponding determined features, such as a foot or systolic peak, and using the measured differential pulse arrival time and calibration data, determine at least one physiological parameter such as blood pressure, heart rate, stroke rate, and cardiac output.
Owner:NORTHWESTERN UNIV
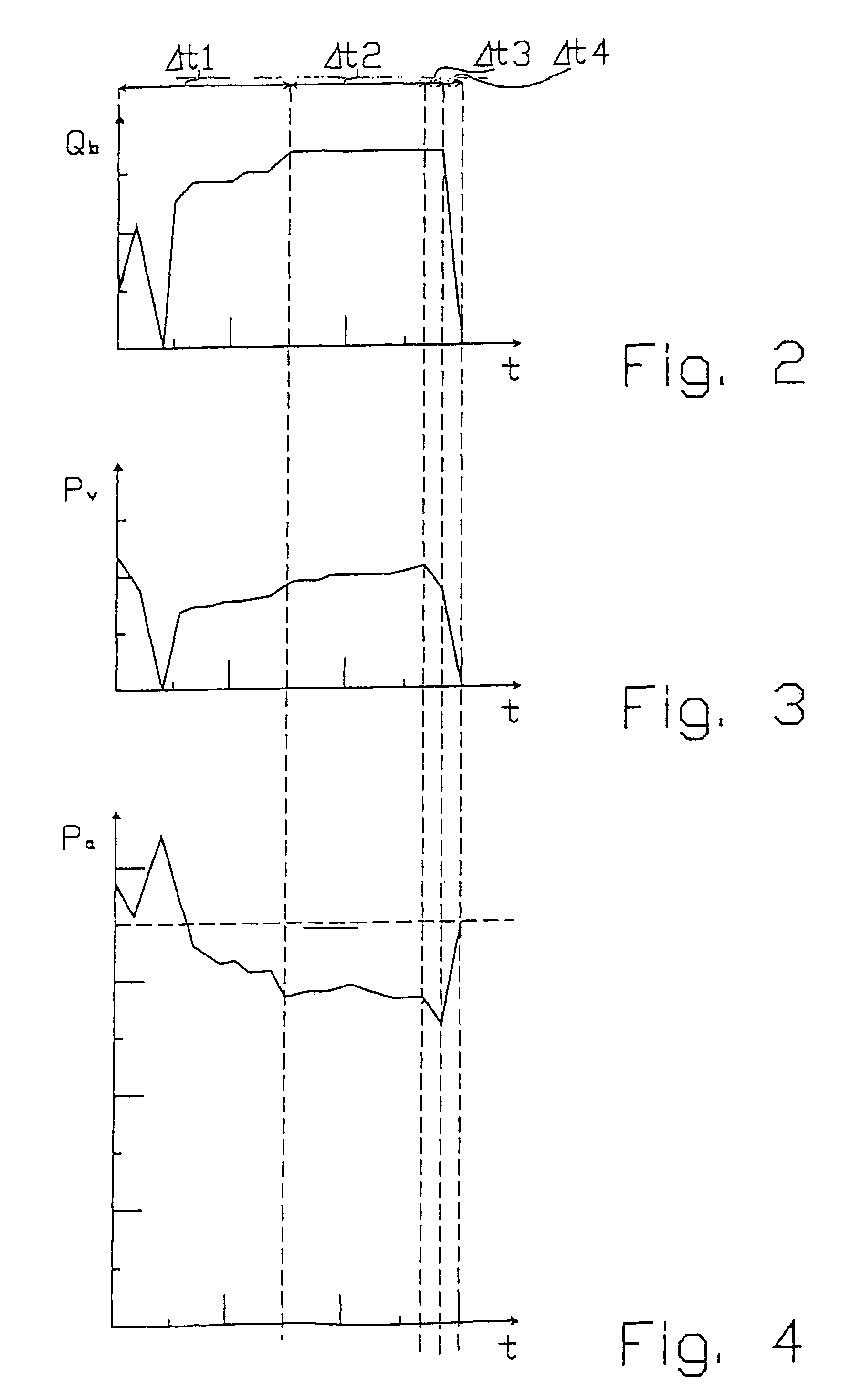
Method and device for detecting the detachment of the venous needle from a patient during dialysis
A method of detecting the detachment of the venous needle from a patient during an extracorporeal blood treatment in a dialysis machine having an extracorporeal blood circuit provided with an arterial branch and a venous branch. The arterial pressure (Pa) is measured in the arterial branch and the venous pressure (Pv) is measured in the venous branch, and the determination is made of whether or not decreases of the arterial pressures (Pa) and venous pressures (Pv) are occurring during the dialysis treatment in normal conditions.
Owner:GAMBRO LUNDIA AB
Devices, systems and methods for controlling local blood pressure
The present invention discloses devices, systems and methods for increasing blood pressure in a blood vessel by introducing an anchor within that traps a particle capable of increasing in volume as it is exposed to blood flow. As the particle increases in volume, it serves to decrease the cross sectional area of the blood vessel, resulting in decreased blood flow and increased blood pressure. This invention may be used to arterialize blood vessels in the venous system to prepare them for an exposure to arterial pressures.
Owner:DTHERAPEUTICS
Pressure monitoring system to prevent aneurismal sac rupture
An abdominal aortic aneurysm pressure monitoring system comprising at least one pressure sensor positioned in an aneurismal sac which optionally may be excluded from direct arterial pressure by an already implanted stent graft, at least one pressure sensor positioned in an abdominal region of the body at a location outside of the aneurismal sac, a controller in communication with the pressure sensors, where a pressure gradient between the abdominal region and the aneurismal sac is determined based on the pressures communicated to the controller from the aneurismal sac and abdominal region pressure sensors.
Owner:MEDTRONIC VASCULAR INC
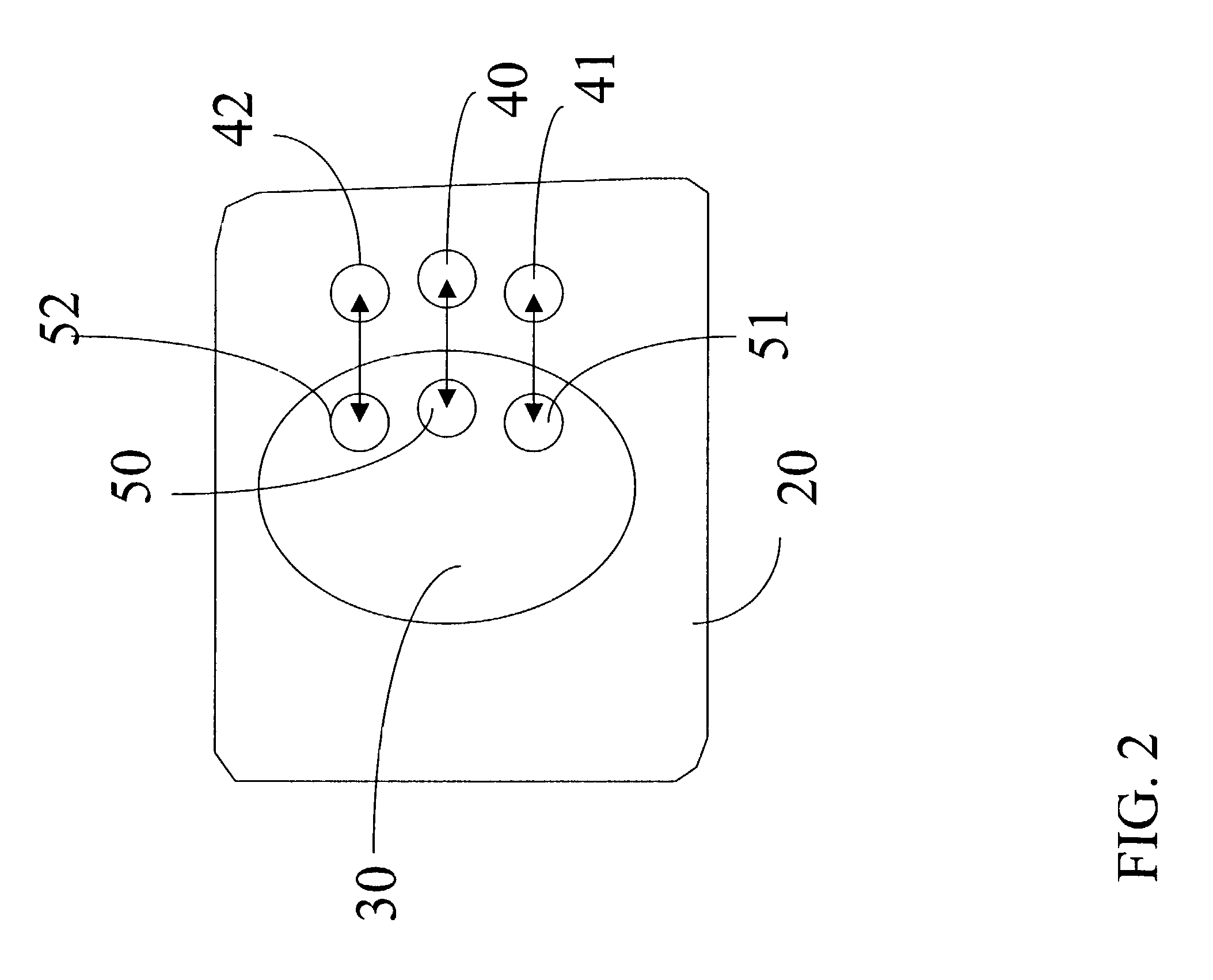
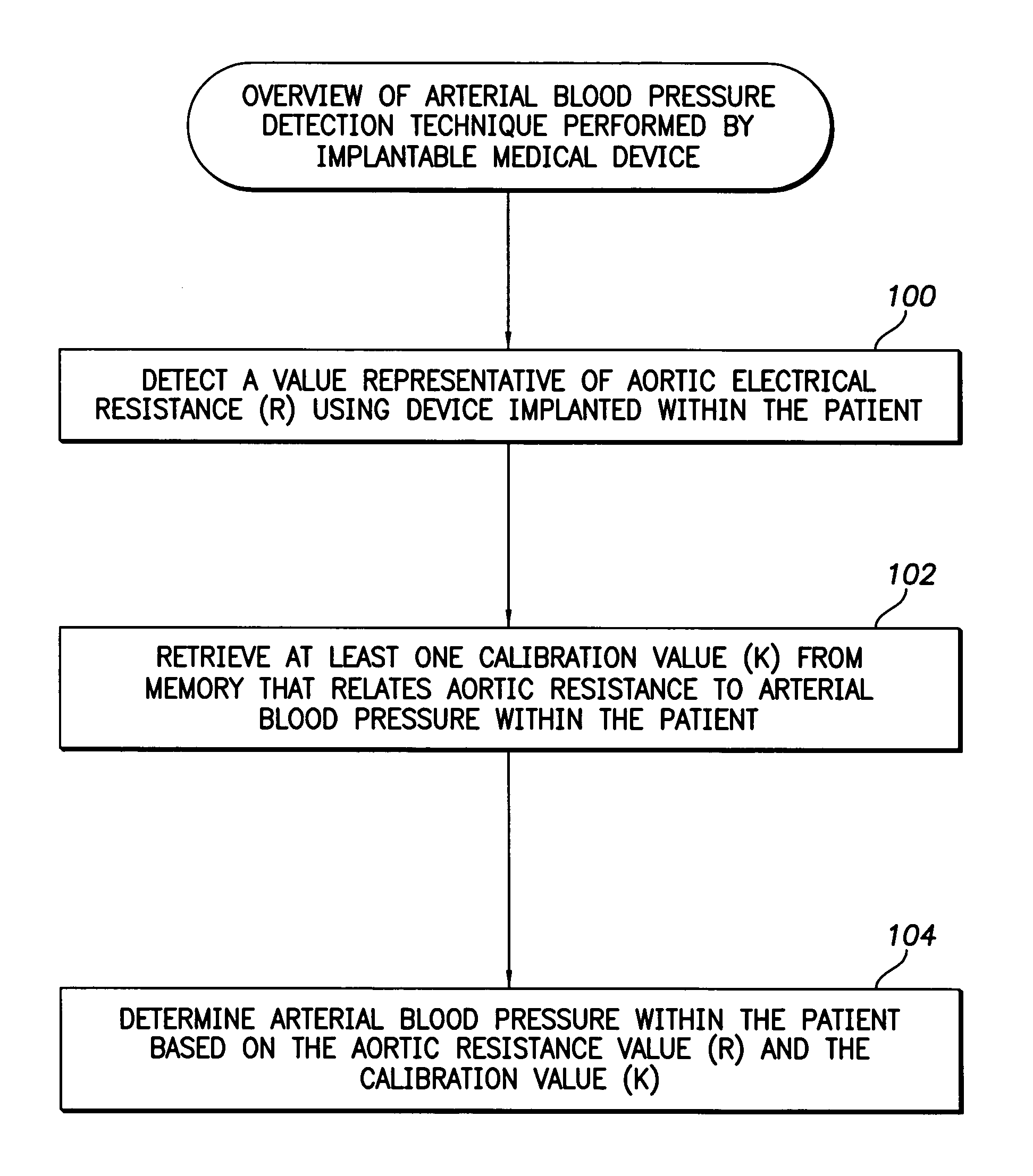
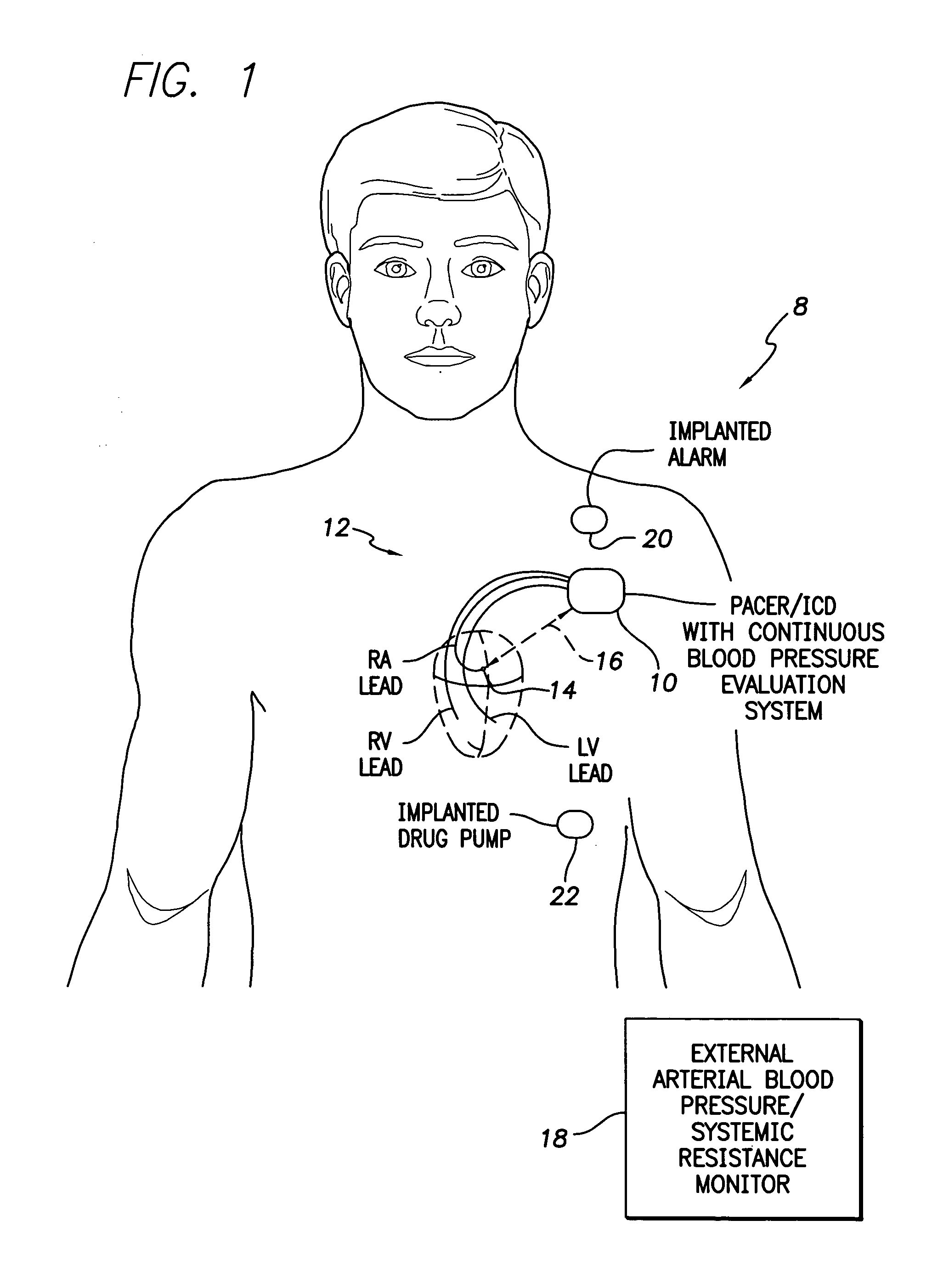
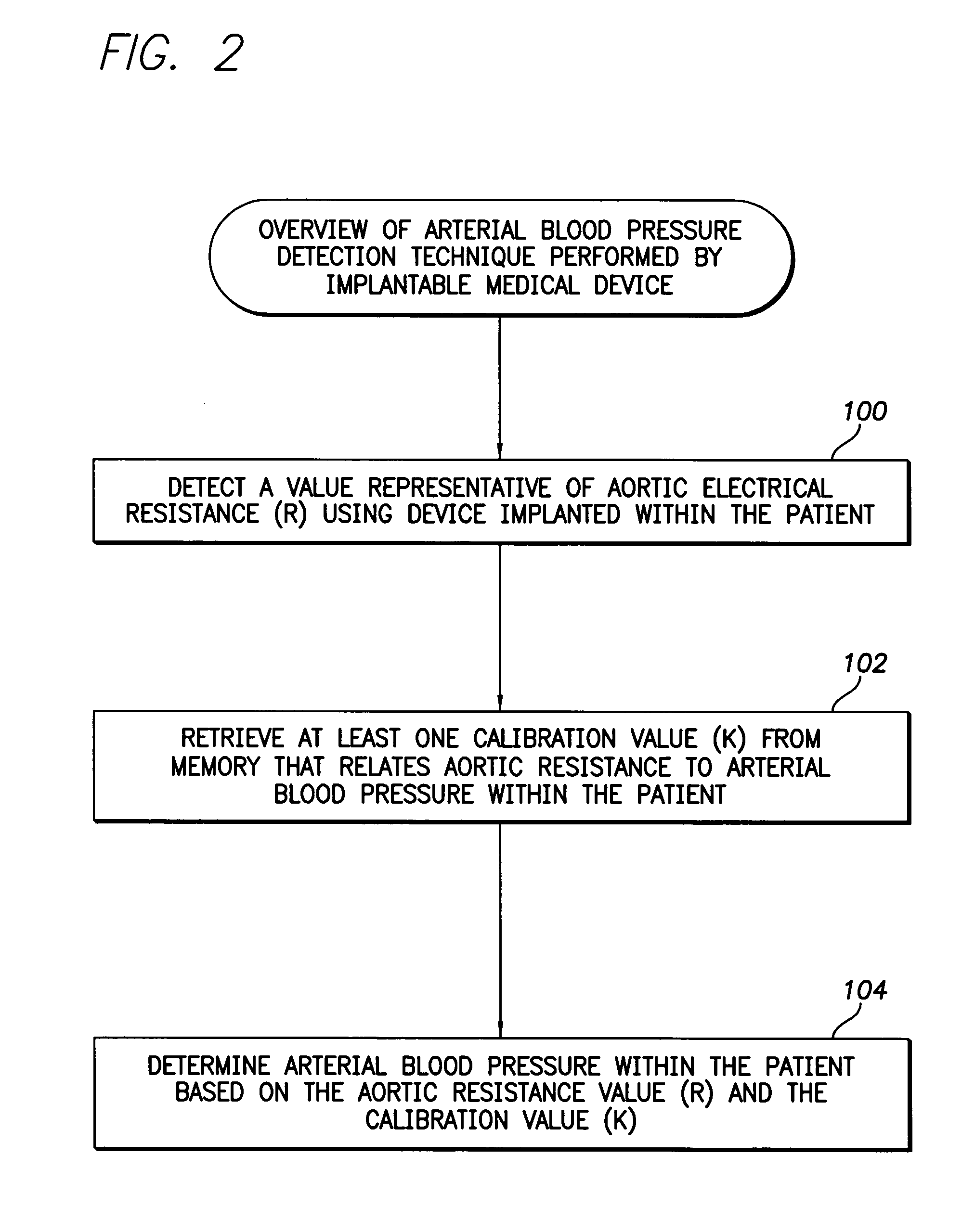
System and method for detecting arterial blood pressure based on aortic electrical resistance using an implantable medical device
Techniques are provided for use with a pacemaker or other implantable medical device for detecting arterial blood pressure. Briefly, the pacemaker detects aortic electrical resistance using sensing / pacing leads. Aortic electrical resistance pertains to the resistance to an electrical current passing through the aorta. The pacemaker then determines the arterial blood pressure of the patient based on the aortic resistance and a predetermined calibration value that relates aortic resistance to arterial pressure. The calibration value is updated monthly based on blood pressure values detected using an external blood pressure sensor employing a blood pressure cuff. Other techniques described herein pertain to the determination of other physiologic parameters such as stroke volume and cardiac output and to the detection of changes in hematocrit. Any of the various physiological parameters may then be used to trigger or control warning signals and responsive therapy.
Owner:PACESETTER INC
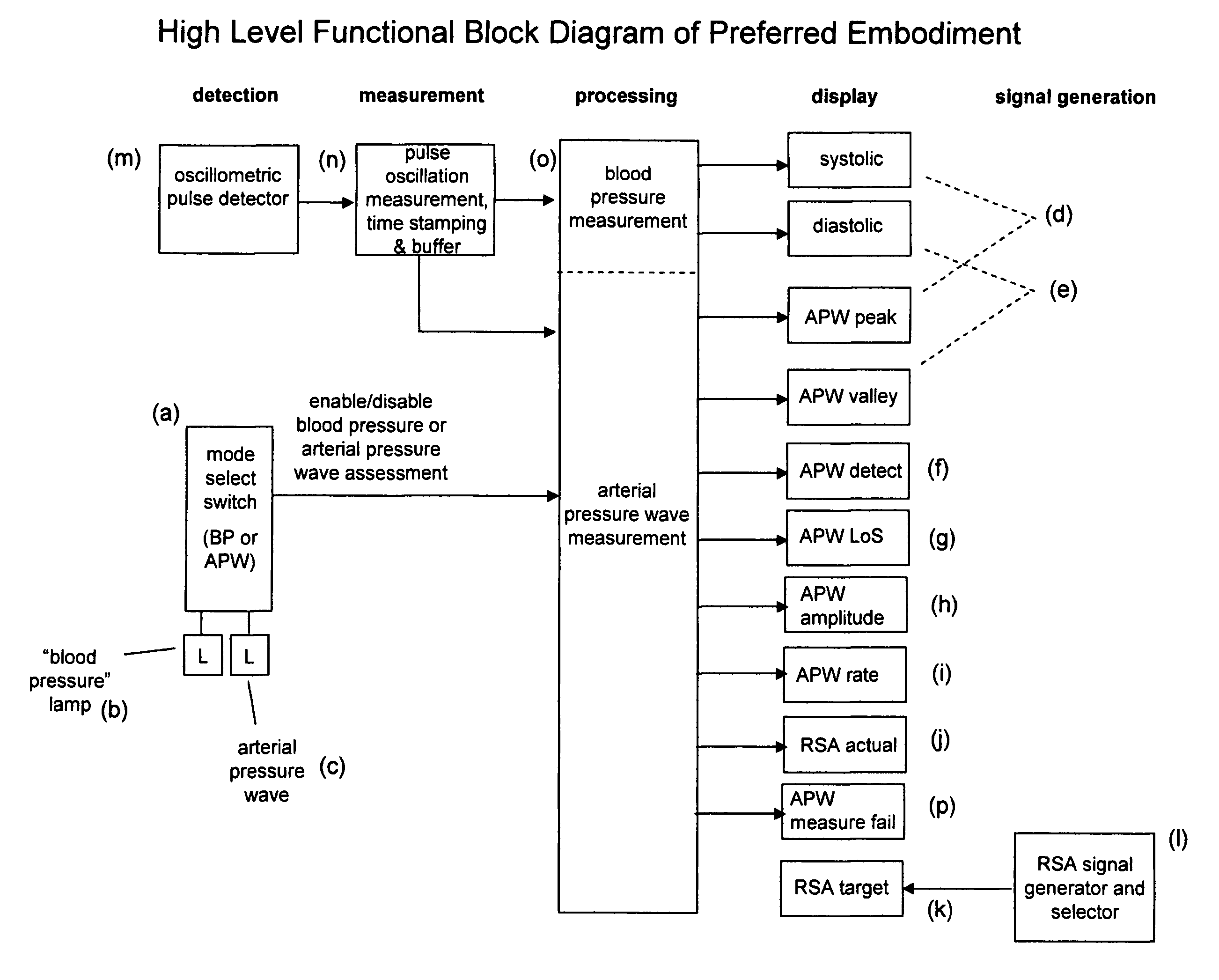
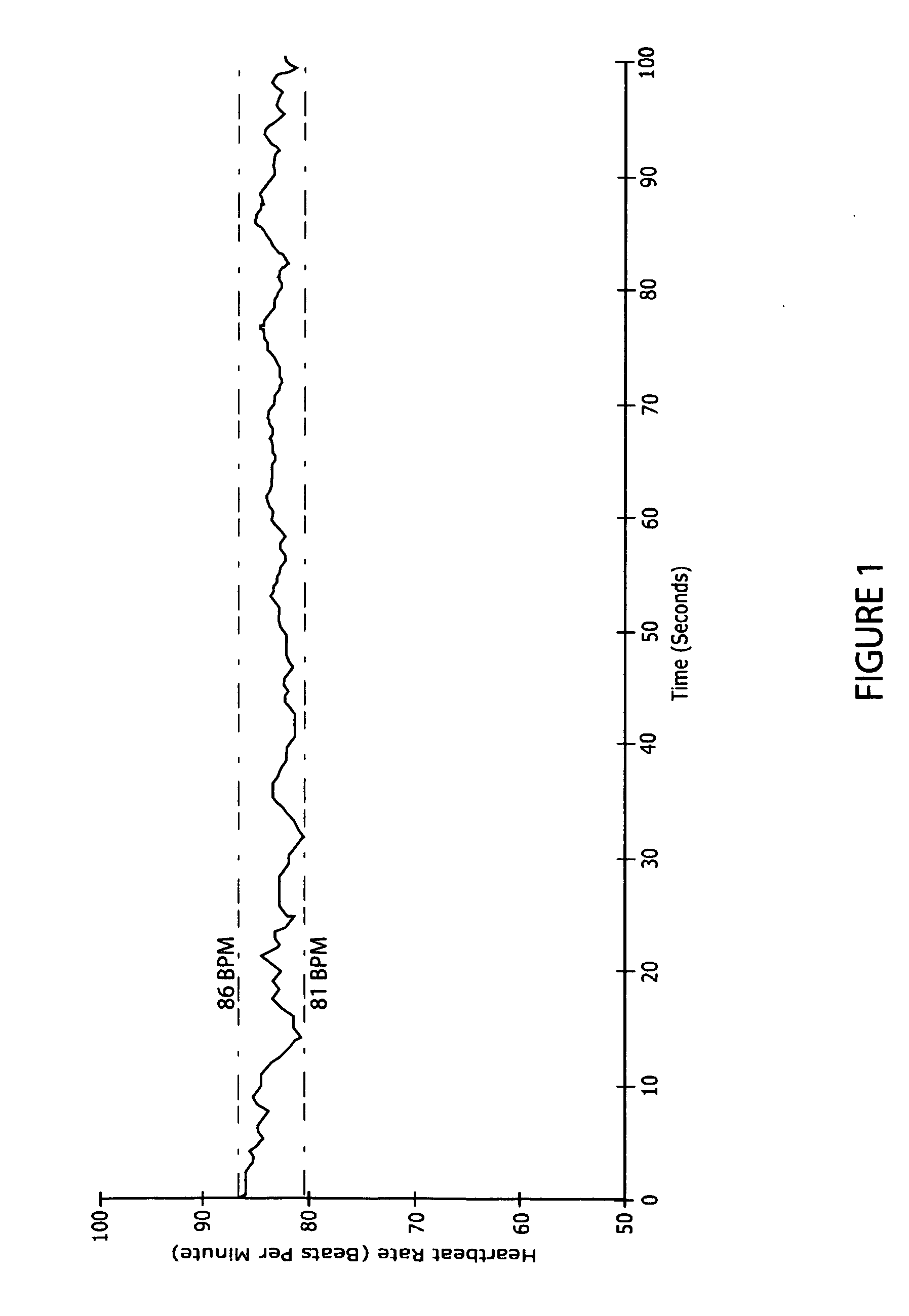
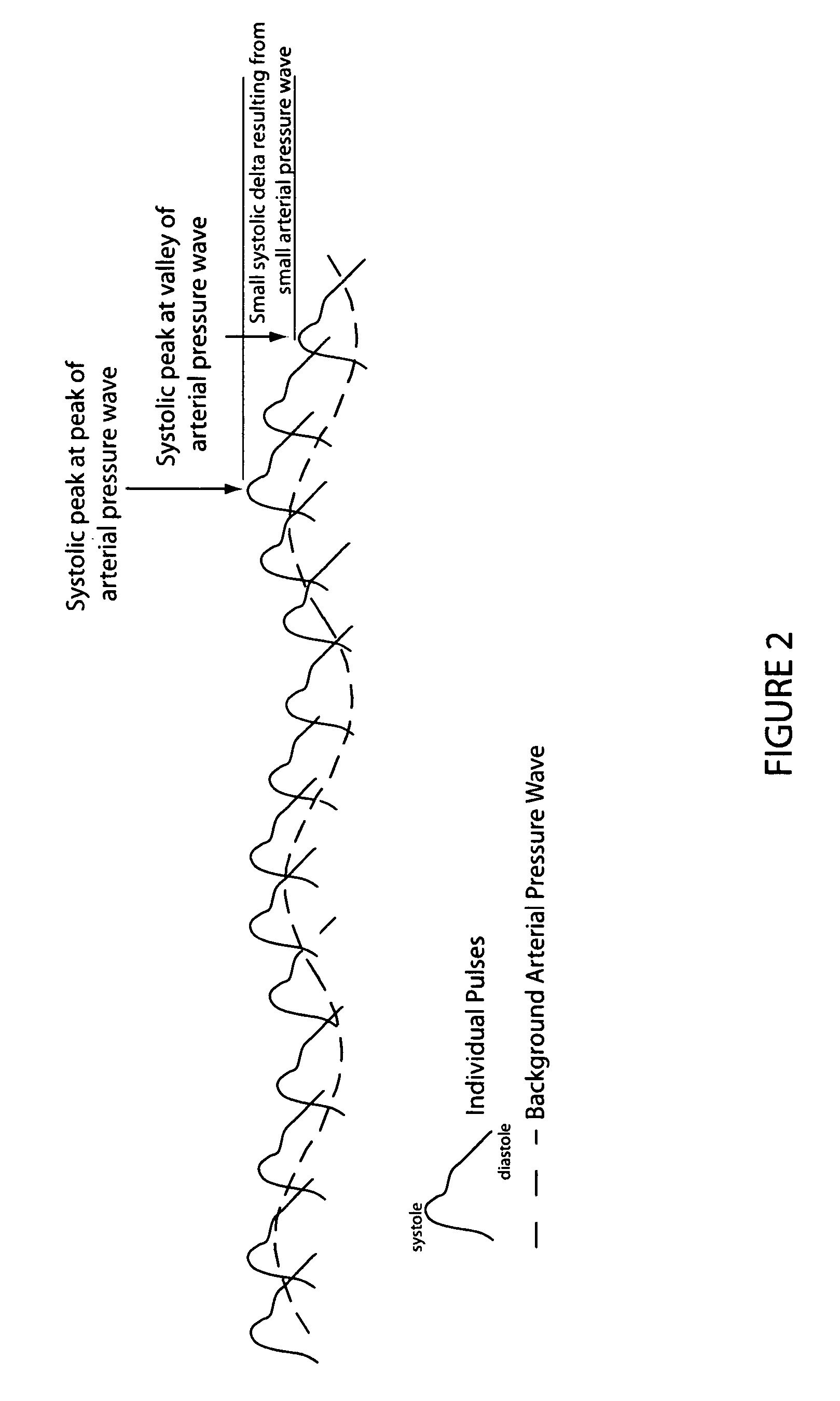
Method and system for assessing breathing effectiveness via assessment of the dynamic arterial pressure wave using the oscillometric measurement technique
The present invention specifies a method and system for assessing breathing effectiveness via dynamic assessment of respiratory sinus arrhythmia and the consequent arterial pressure wave using the oscillometric measurement technique. Arterial pressure wave peak pressure, valley pressure, amplitude, and rate are characterized and displayed for diagnostic and remedial purposes. The dynamic change in respiratory sinus arrhythmia and resultant arterial pressure wave is visually presented in real time as user biofeedback. A respiratory sinus arrhythmia generator generates varying frequencies to which the user synchronizes their breathing cycle for purposes of increasing arterial pressure wave amplitude with a consequent increase in breathing depth and decrease in breathing frequency. An instructive method in the application of the present invention is also specified.
Owner:COHERENCE
Non-invasive central aortic blood pressure measuring method and device
The invention discloses a non-invasive central aortic blood pressure measuring method and device. The non-invasive central aortic blood pressure measuring method includes, according to a human artery network model based on viscous fluid mechanics, a method of calculating artery network model personalized parameters of a measured person through measured radial artery and brachial artery pulse wave signals and arm blood pressure values, a method of calculating an ascending aorta-radial artery transfer function and a method of calculating central arterial pressure waveforms through measured central arterial pressures. The non-invasive central aortic blood pressure continuous measuring device comprises a pulse wave signal processing and analysis unit and a radial artery and brachial artery pulse wave signal acquisition unit worn on a wrist. The method is different from an existing general transfer function method, the artery network model parameters of each person to be measured are measured and calculated and the artery network model parameters are numerical characteristics of the cardiovascular system states of the person to be measured with the calculated central arterial pressure waveforms, and the method and device has important meanings in prevention, curing and control of cardiovascular diseases, especially high-risk diseases, such as hypertensions and coronary heart diseases.
Owner:南京茂森电子技术有限公司
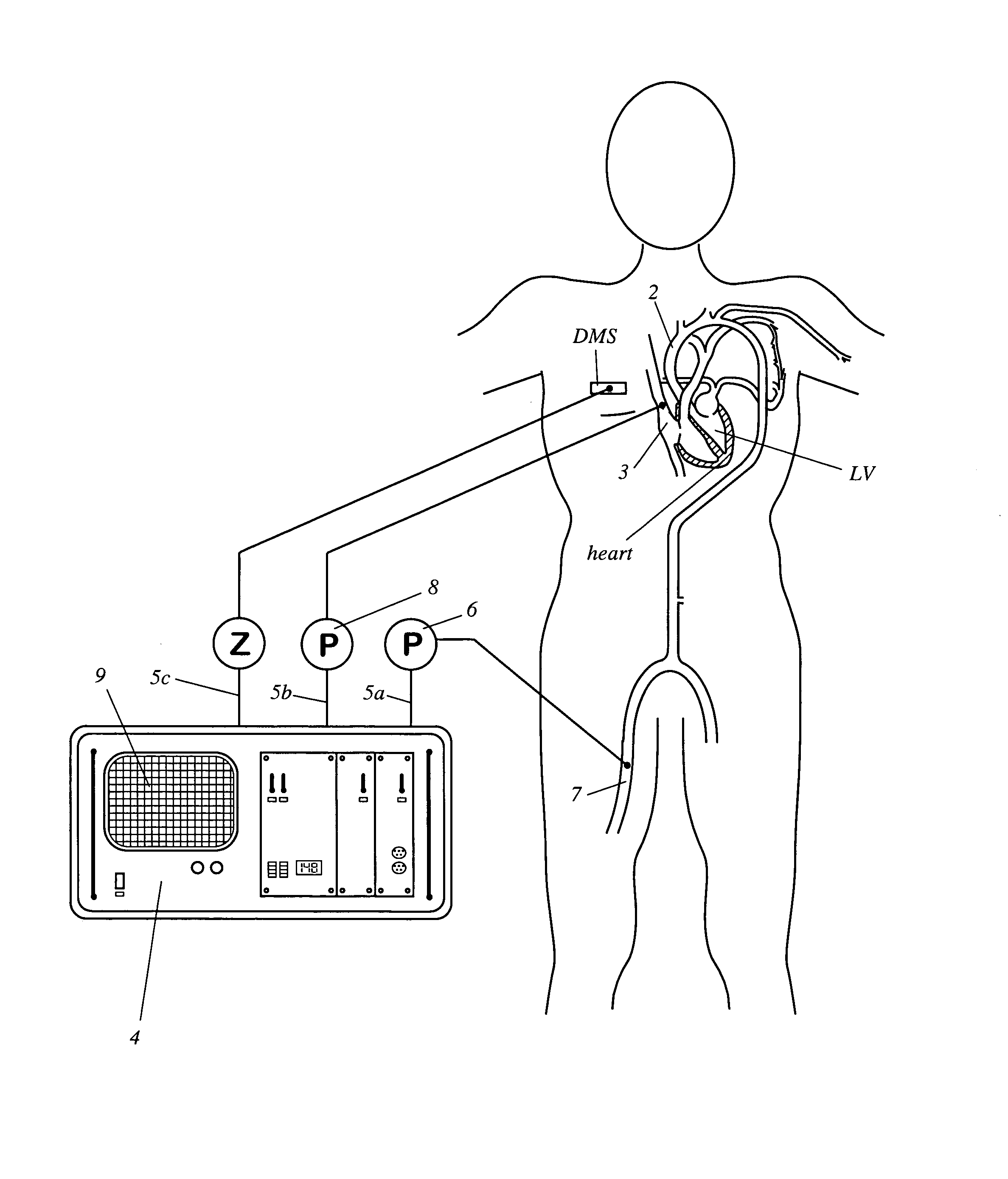
Apparatus for determining cardiovascular parameters
InactiveUS7314449B2Reduced effectivenessReliable assessmentRespiratorsSurgeryAutonomous breathingTransmural pressure
An apparatus that continuously monitors the arterial pressure measured by a pressure sensor in an artery, which pressure is regarded as the reading Pao that approximately corresponds to the aortal pressure. In principle, the arterial pressure can be measured in the aorta, near the aorta, or in the arterial tree. To provide a second reading, the apparatus, via the input channel, continuously monitors the central venous pressure (CVP), which is regarded as the reading PIT that approximately corresponds to the intrathoracic pressure (ITP). The third reading is provided via the input channel as a reading Z which expresses the thoracic compliance. Via known algorithms of the pulse contour analysis, the apparatus calculates the stroke volume variation, using as the determining pressure the transmural pressure which is calculated according to the formulaPtransmural=Pao−f(C)*PITThe cardiac volume responsiveness indicator (CVRI) is calculated for mechanical positive respiration according to the formulaCVRI=k*(SVV / ΔCVP)or for spontaneous breathing according to the formulaCVRI=l−m*(ΔCVP / SVV).
Owner:PULSION MEDICAL SYSTEMS SE
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com