Patents
Literature
170 results about "Alveolar ridge" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
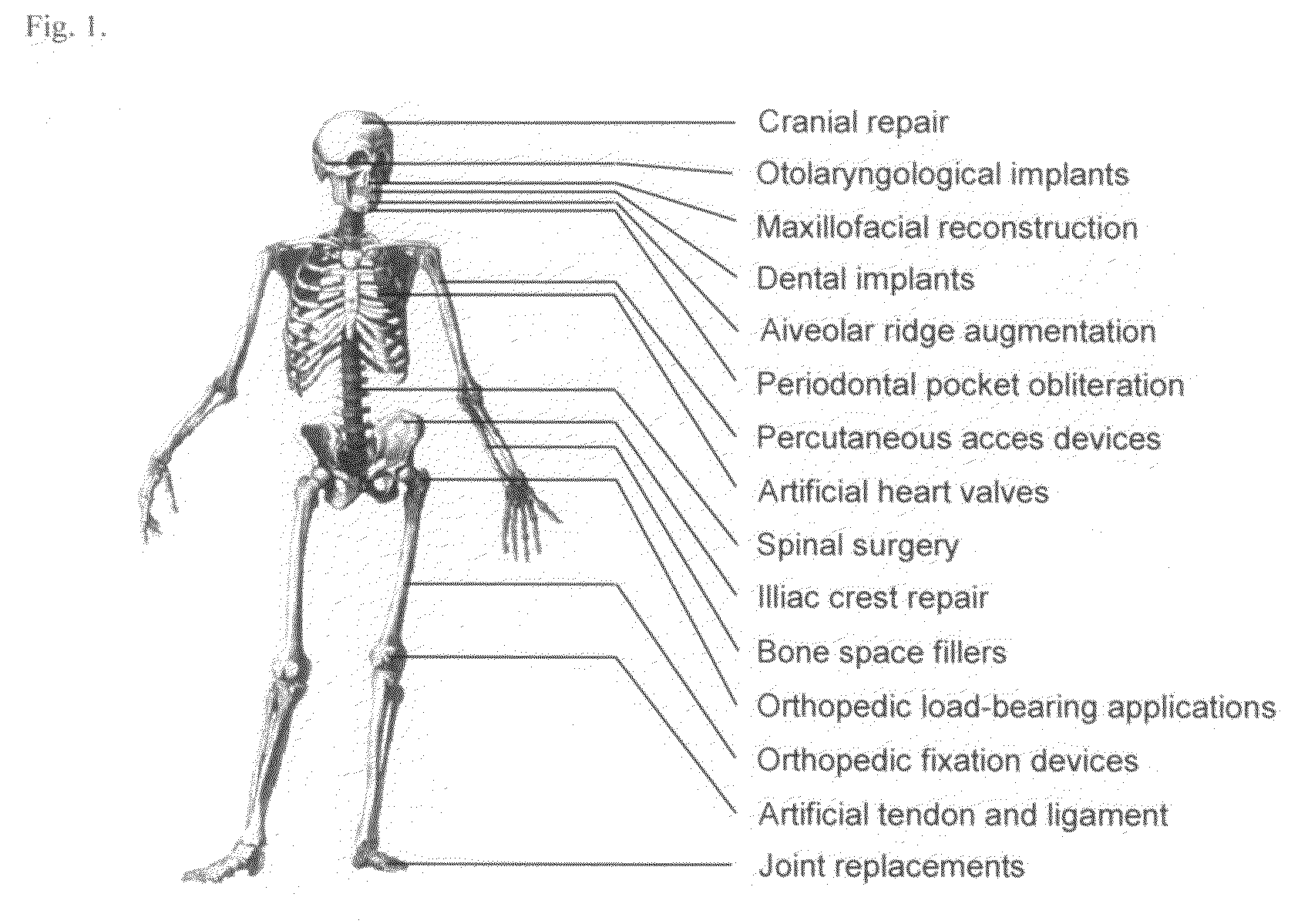
The alveolar ridge (/ˌælviˈoʊlər, ælˈviːələr, ˈælviələr/; also known as the alveolar margin) is one of the two jaw ridges, extensions of the mandible or maxilla, either on the roof of the mouth between the upper teeth and the hard palate or on the bottom of the mouth behind the lower teeth. Most of the roof of one's mouth is the hard palate and the soft palate. The alveolar ridges contain the sockets (alveoli, singular "alveolus") of the teeth. They can be felt with the tongue in the area right above the top teeth or below the bottom teeth. Its surface is covered with little ridges.
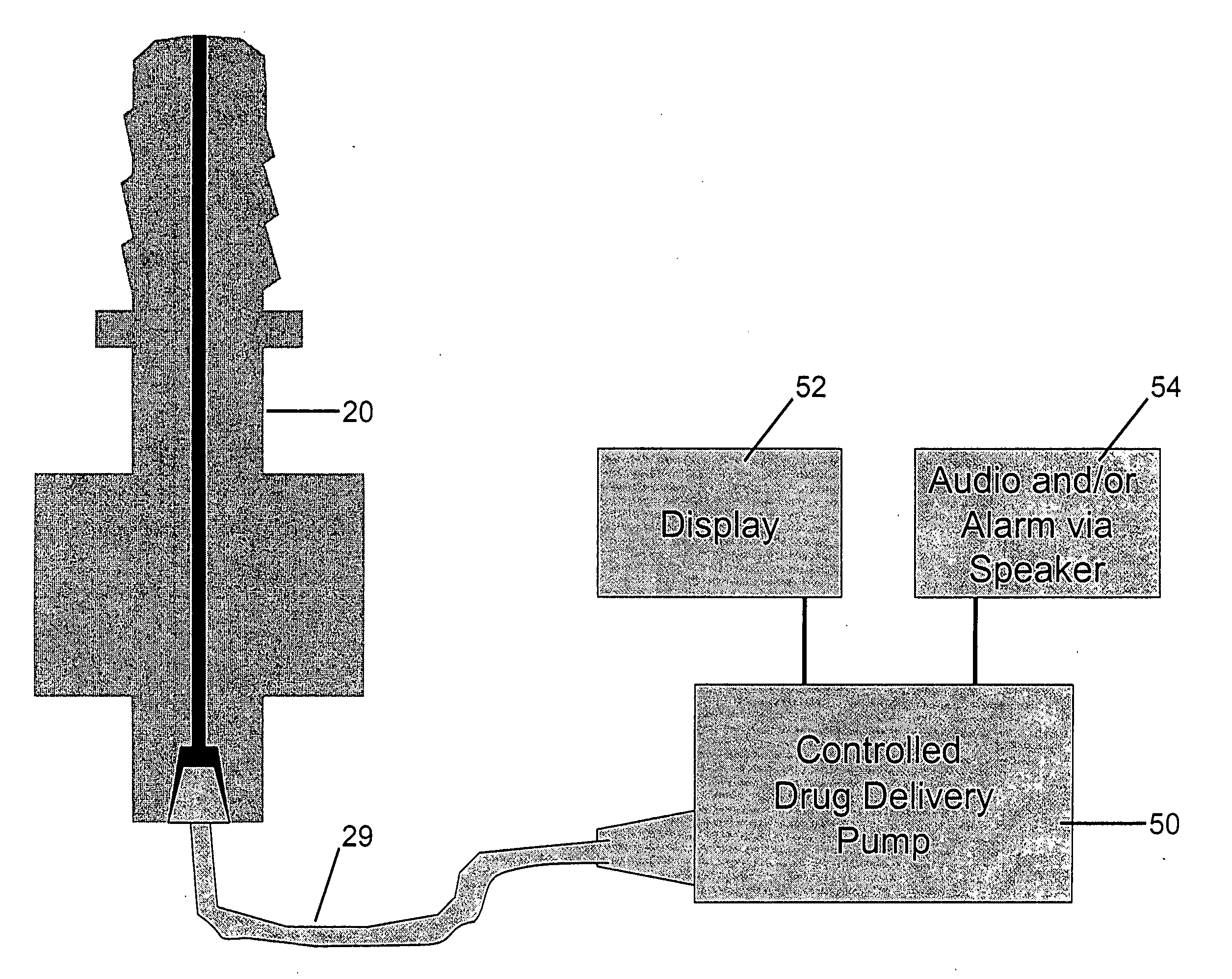
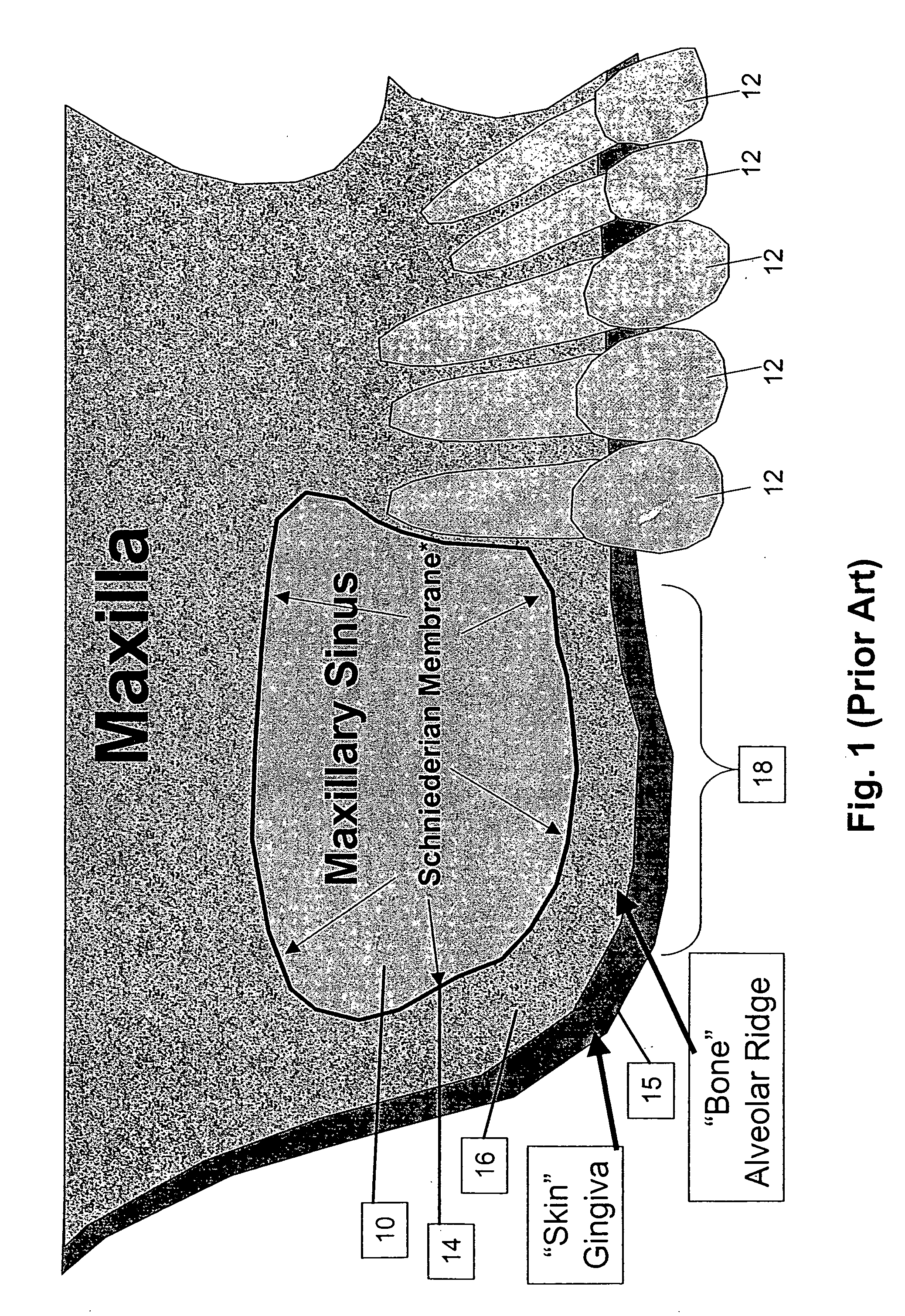
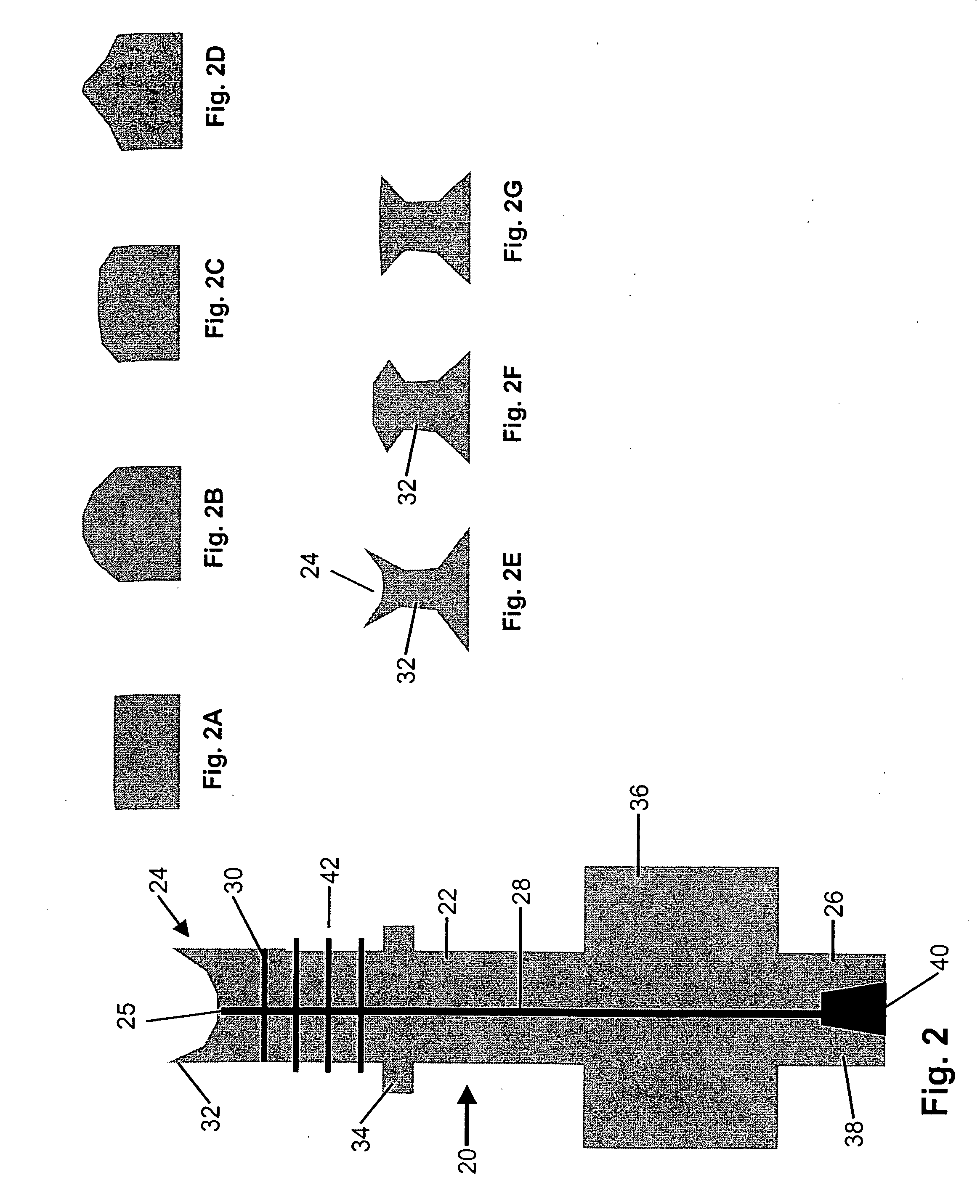
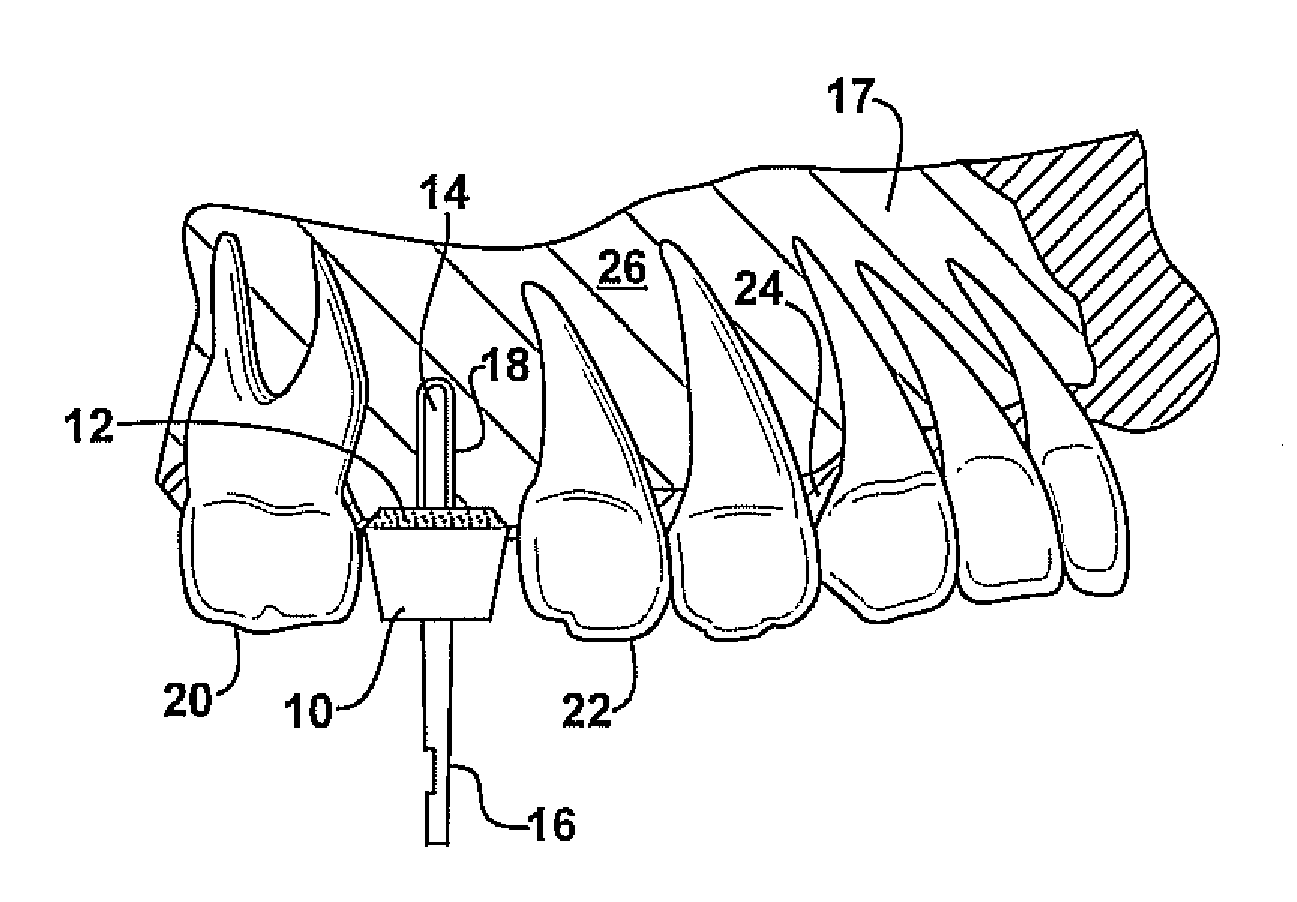
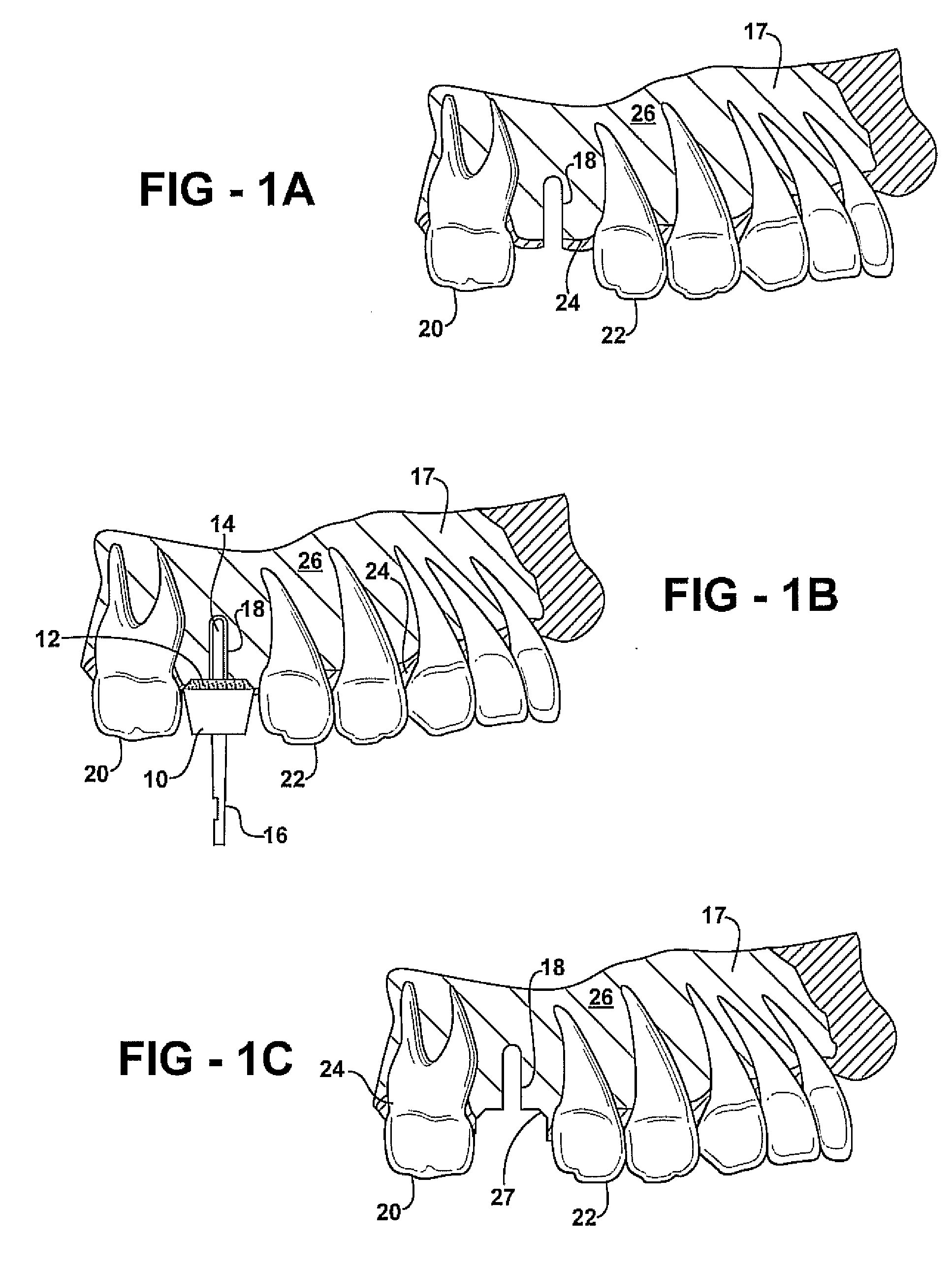
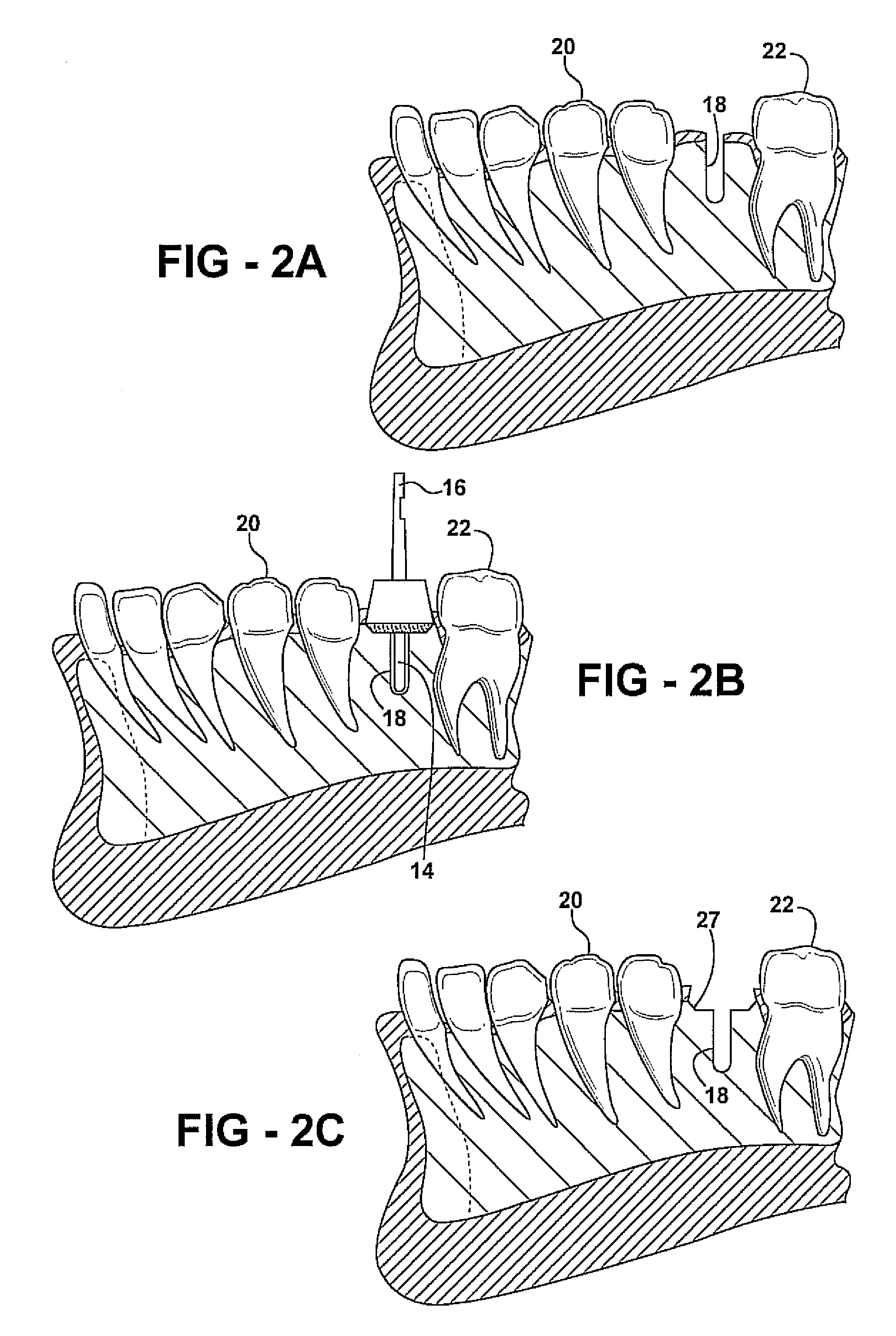
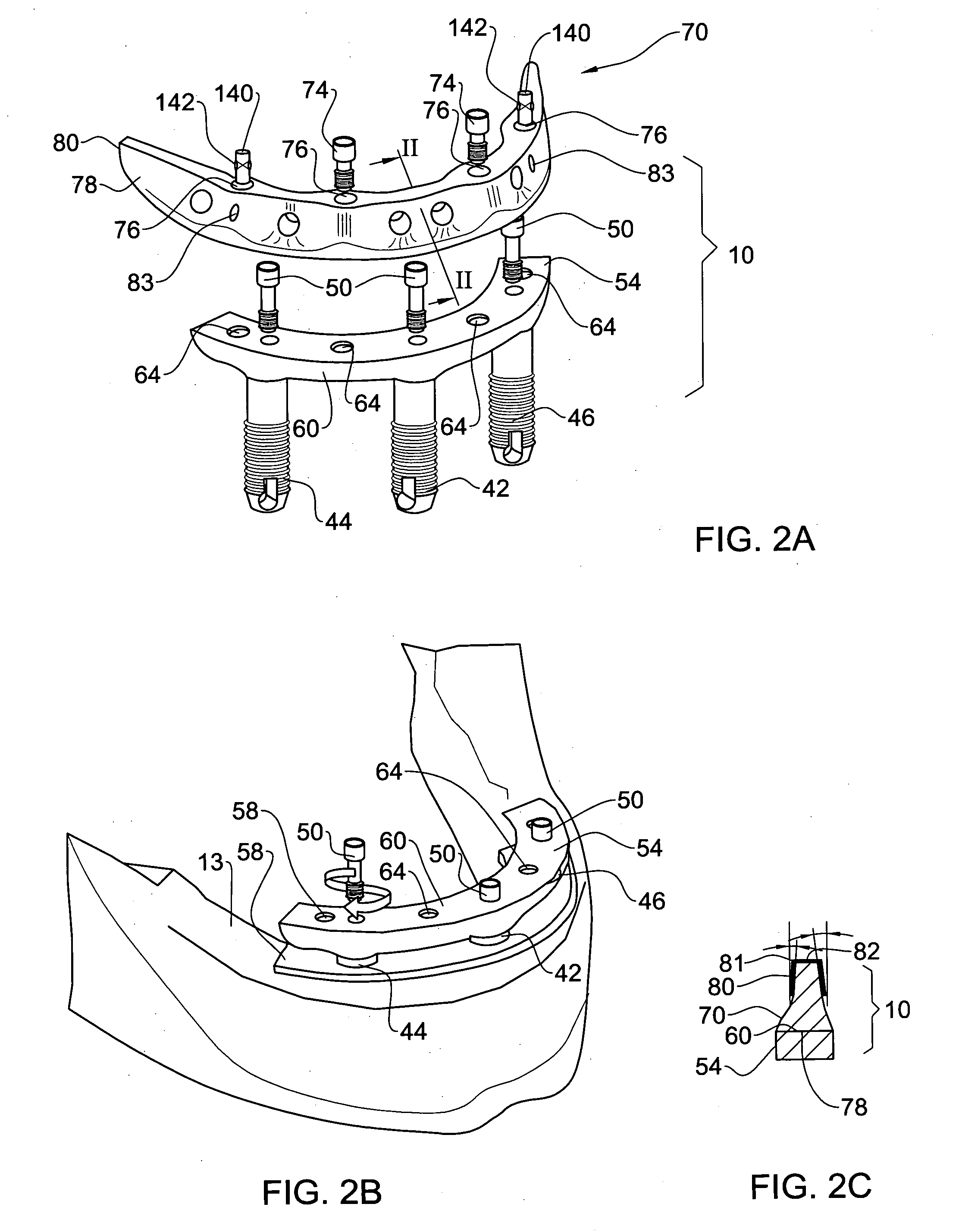
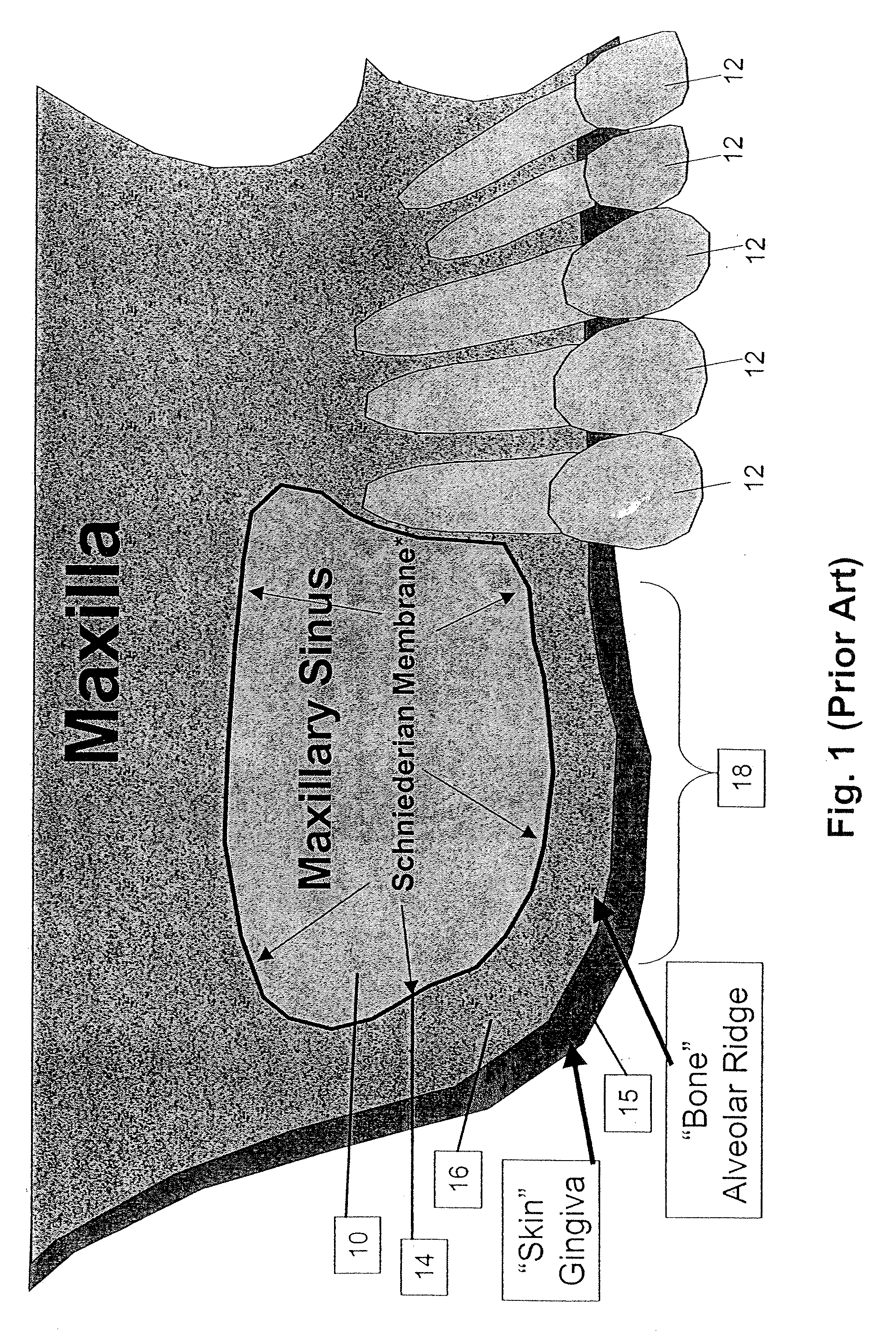
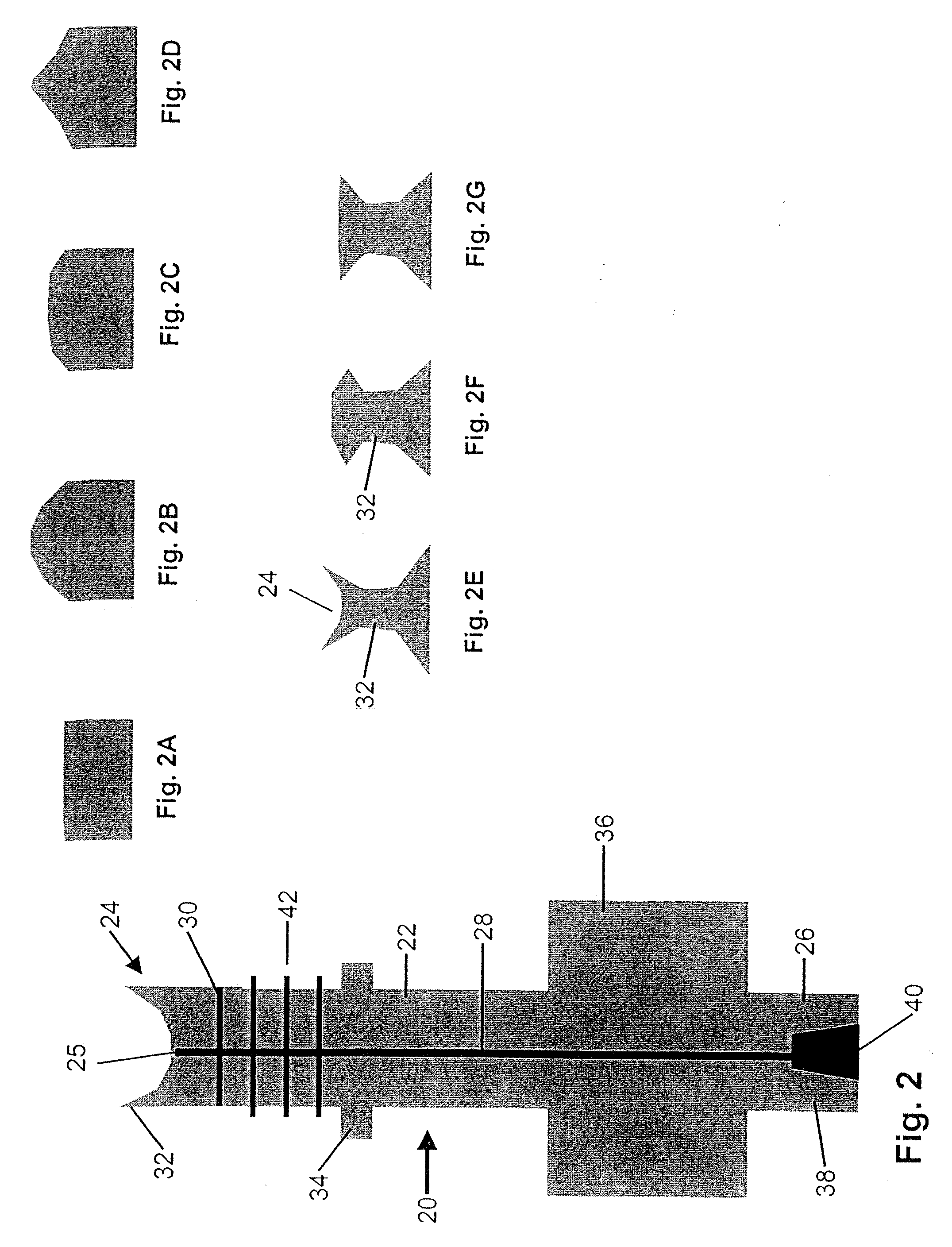
Method and apparatus for performing maxillary sinus elevation
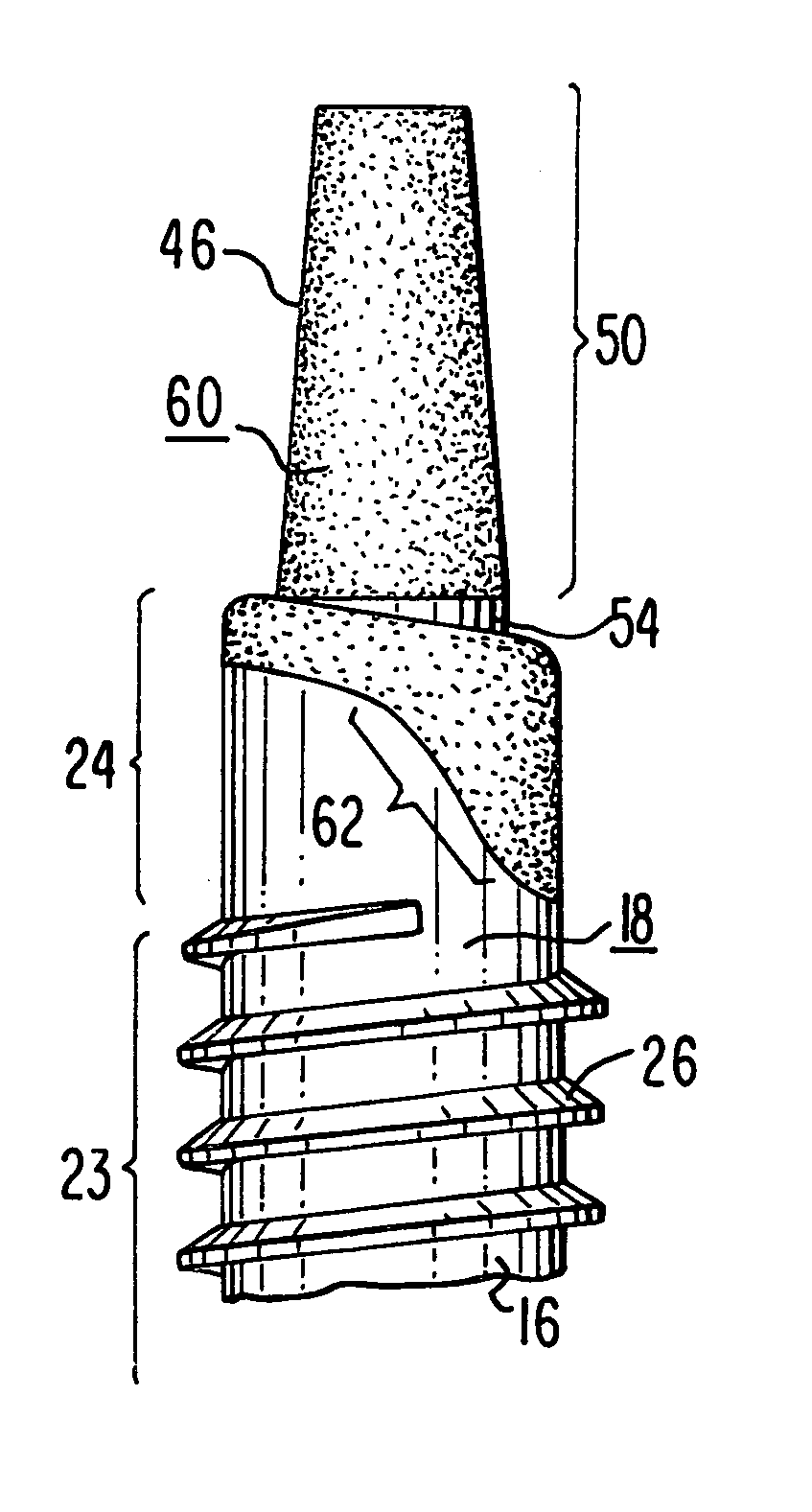
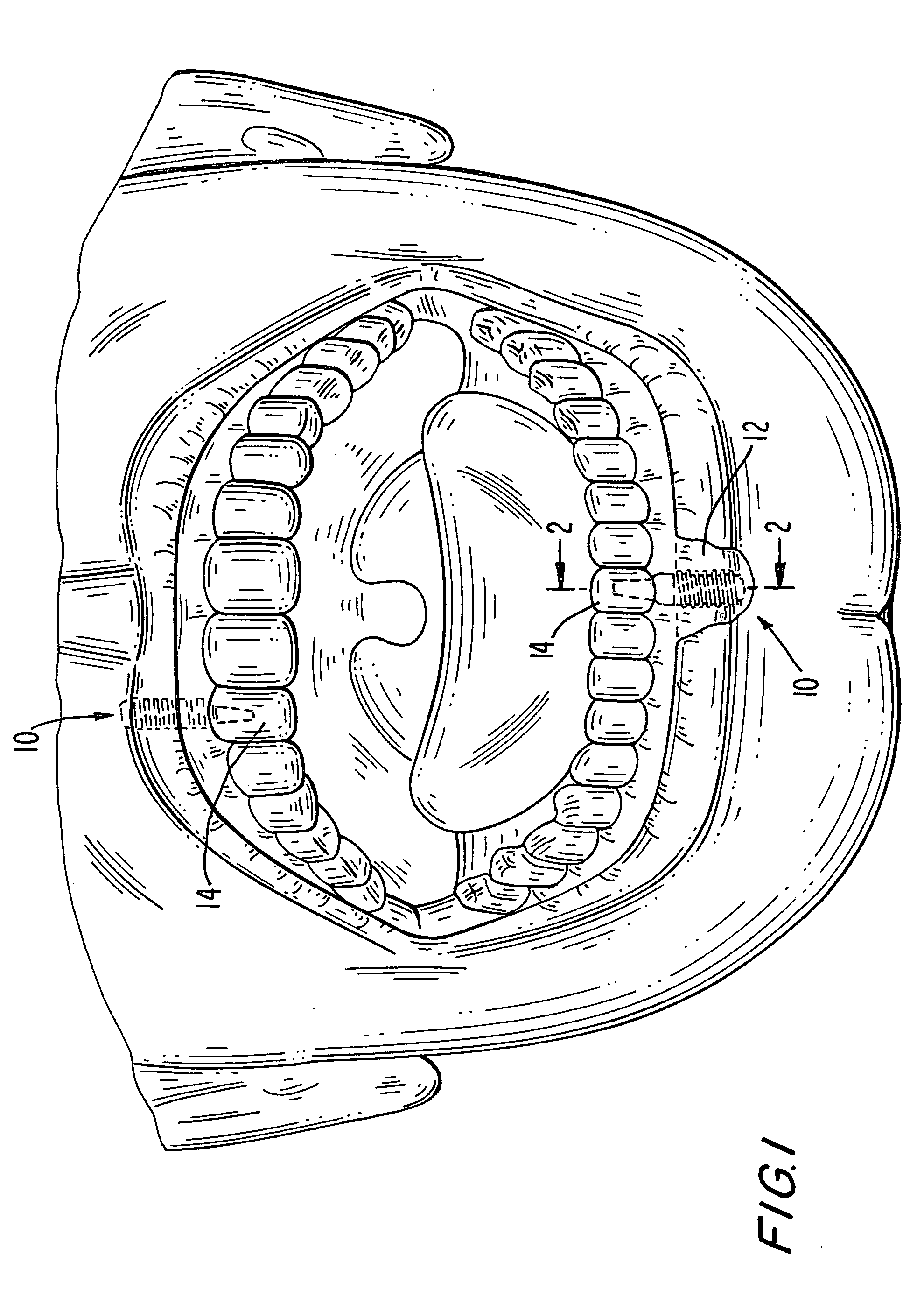
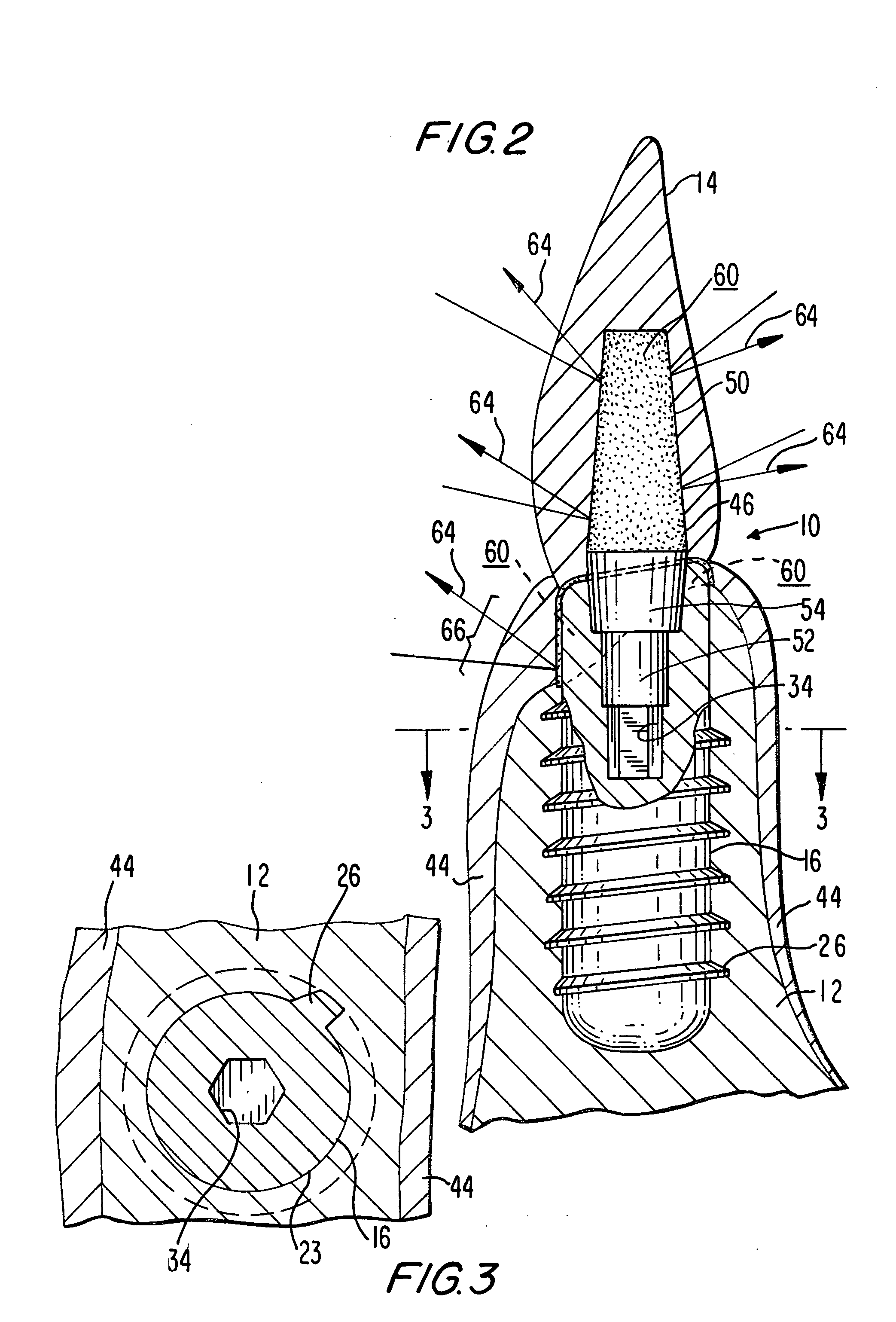
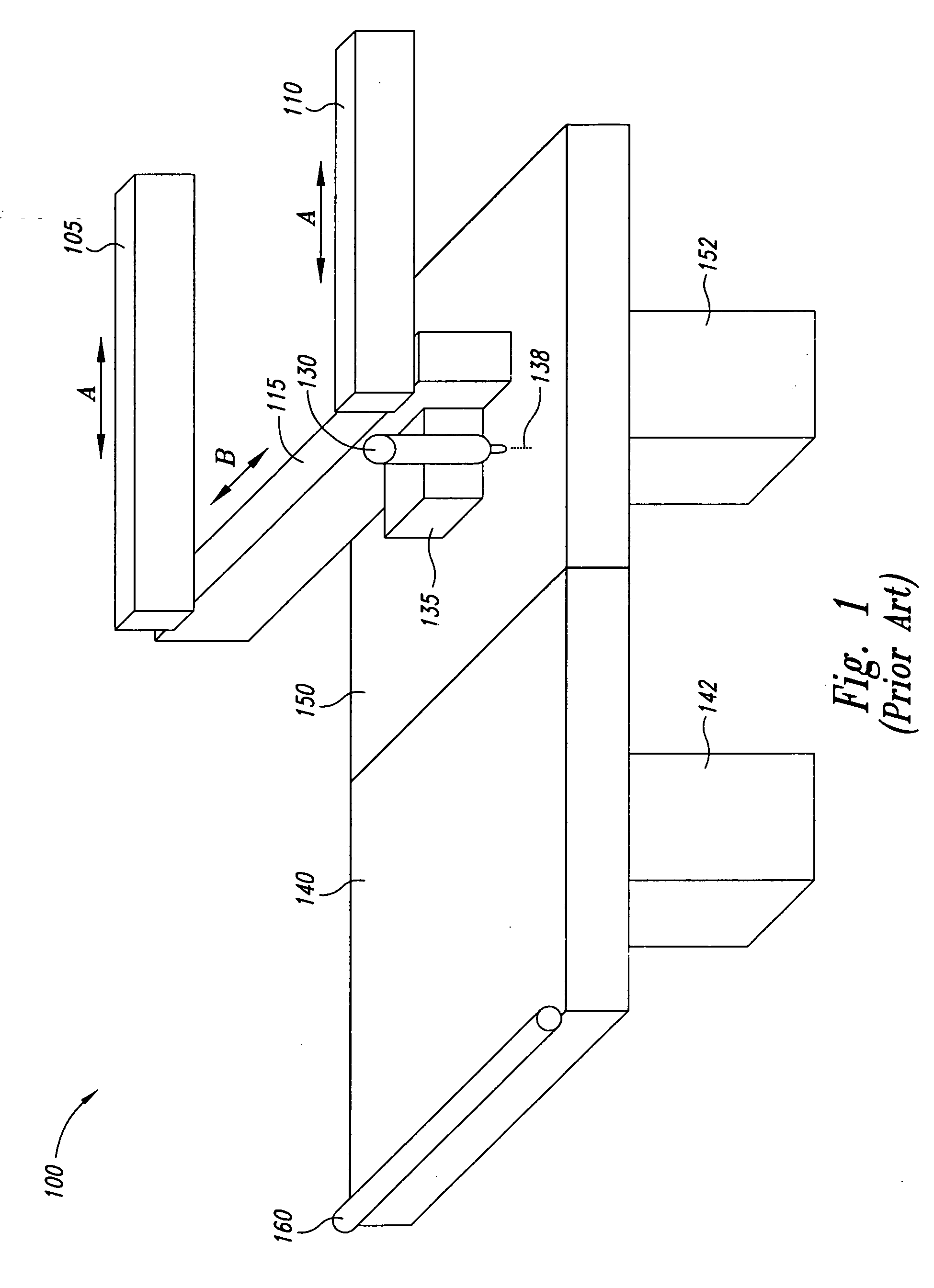
InactiveUS20060084034A1Miss massEffective placementDental implantsFastening prosthesisBone growth stimulatorBiomedical engineering
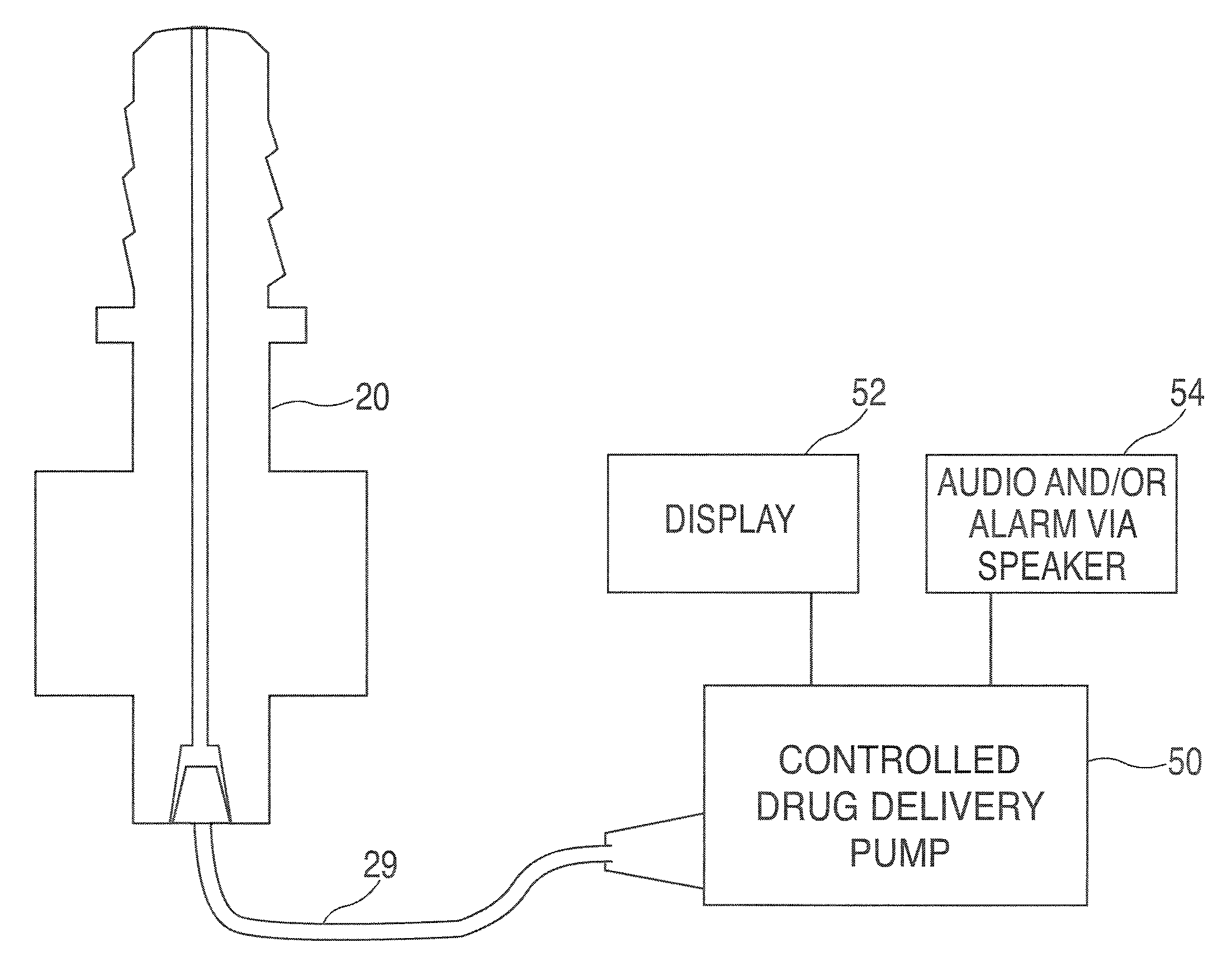
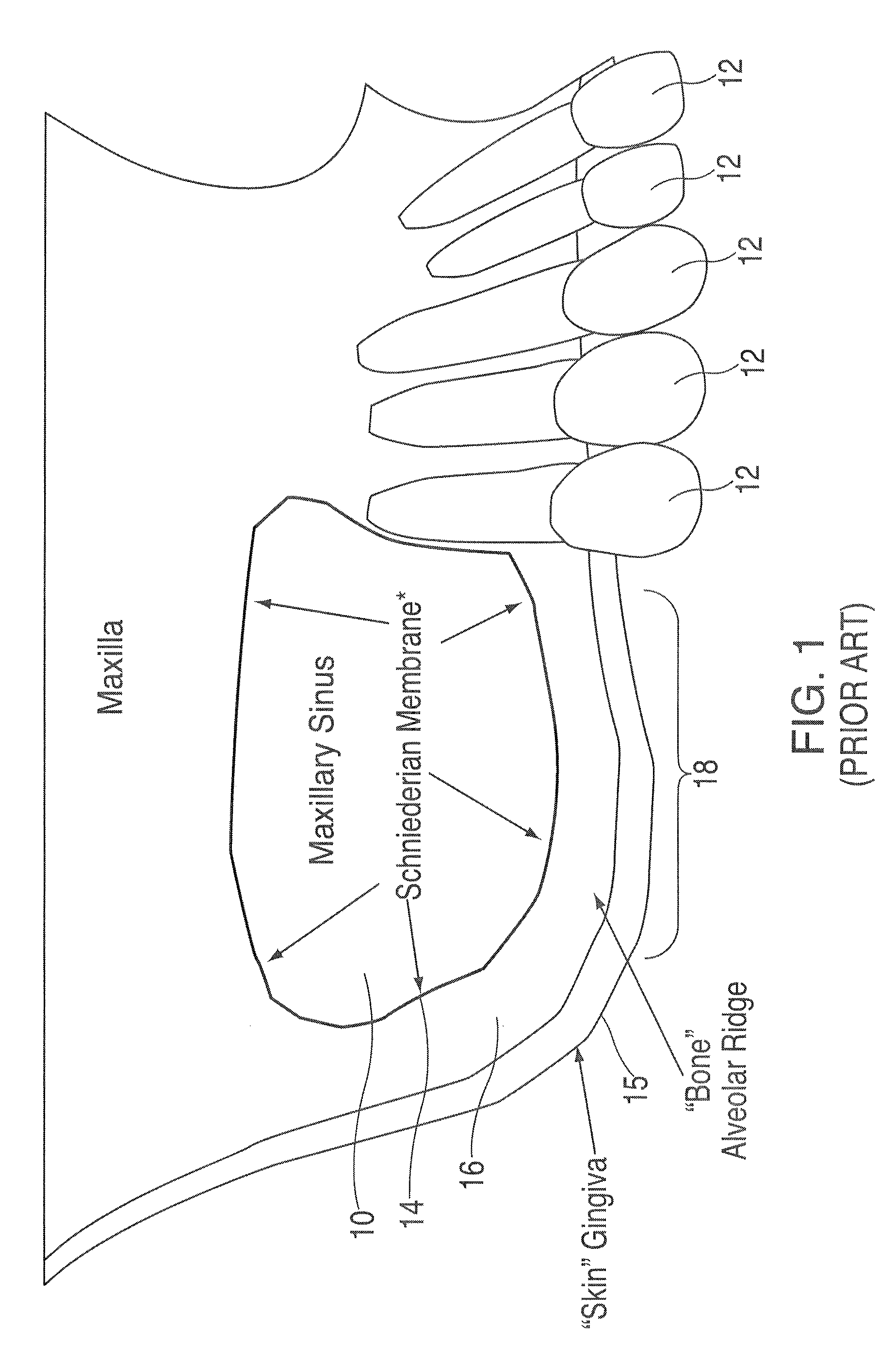
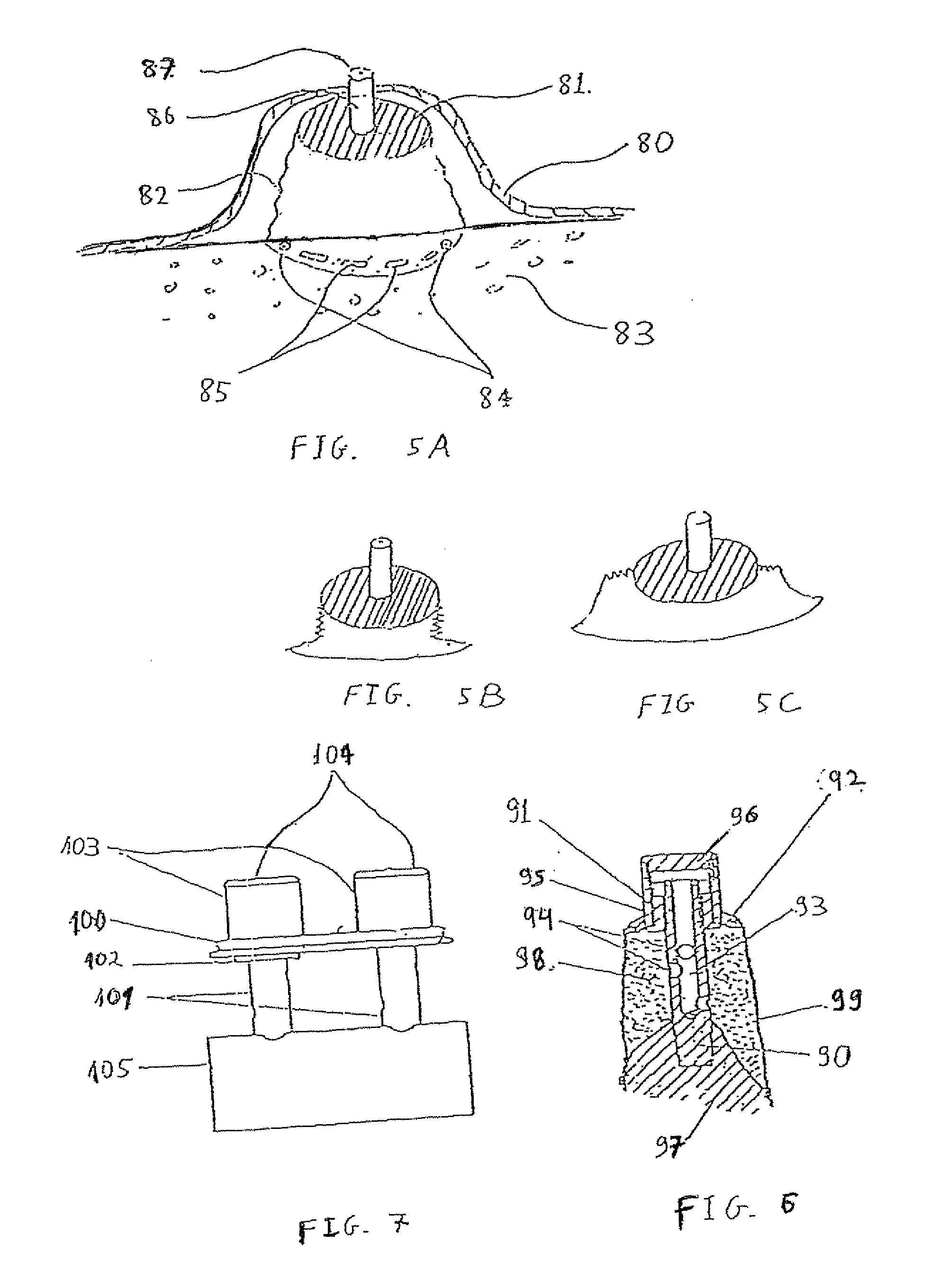
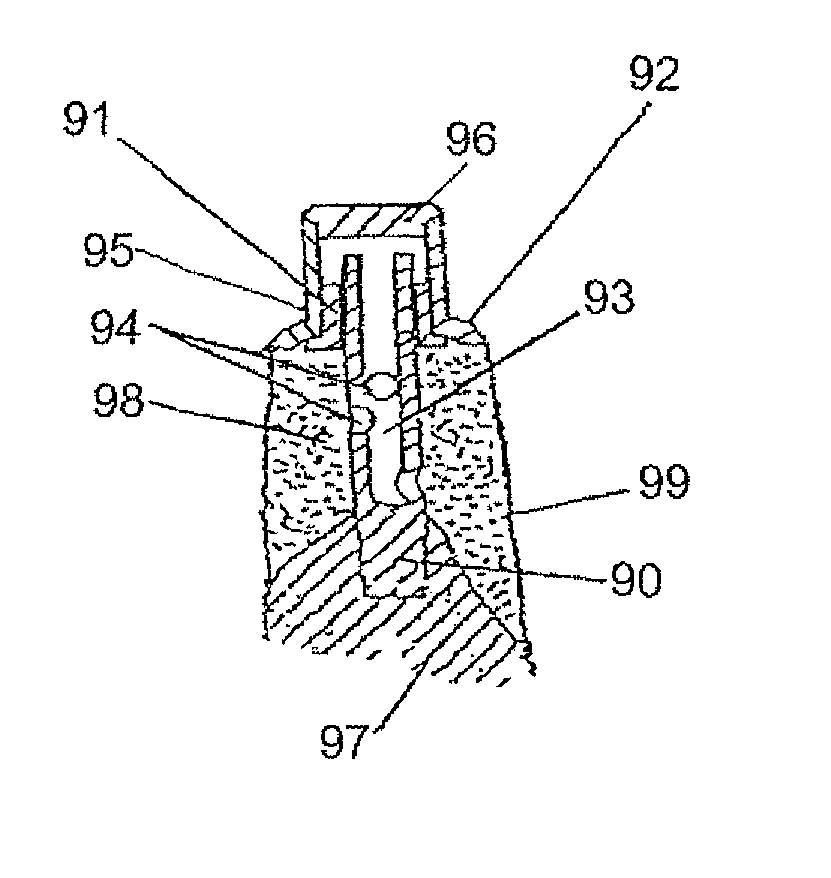
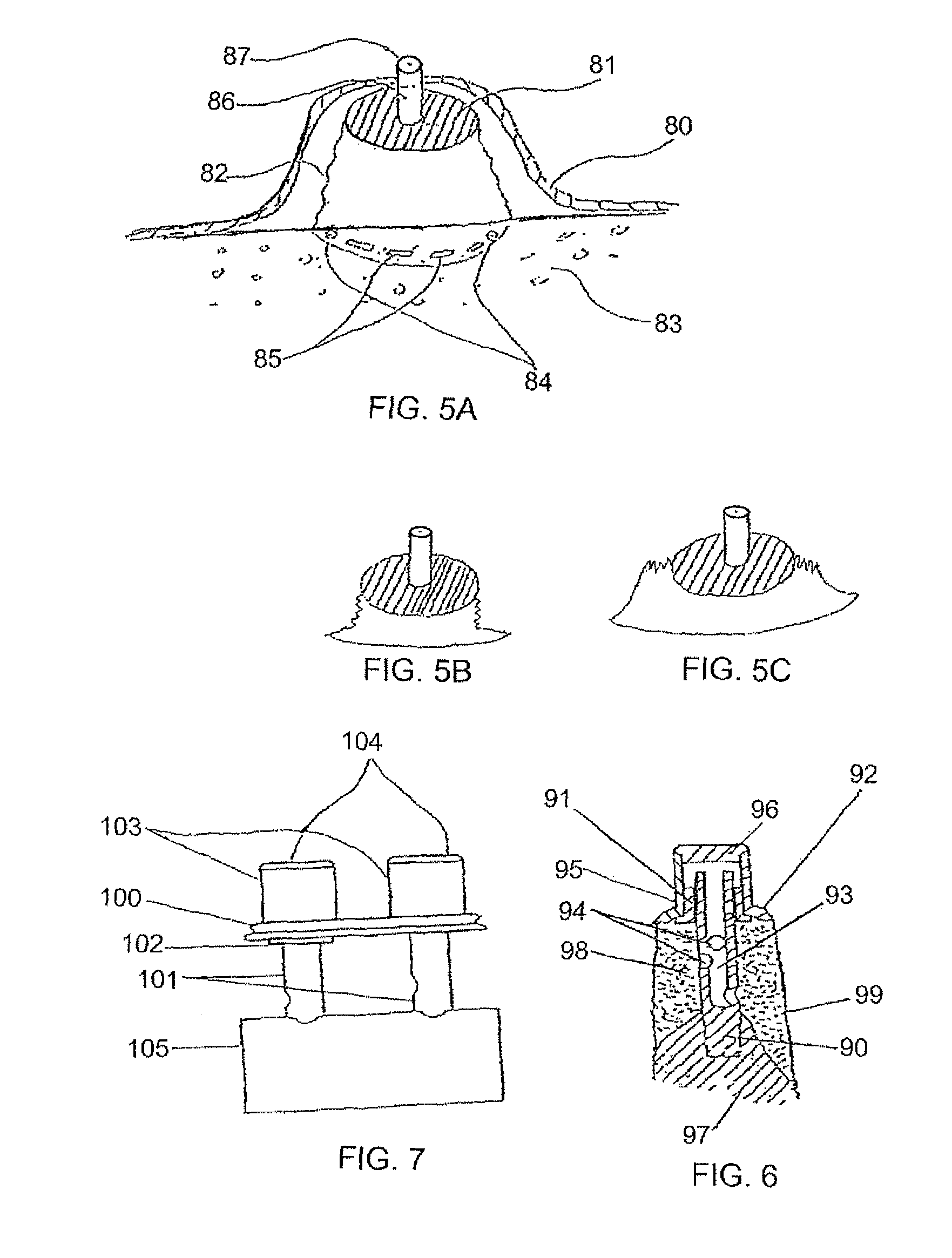
A method and apparatus is disclosed for providing implants in the upper jaws of a person. A sleeve is inserted through the alveolar ridge to the maxillary sinus. The sleeve is used to raise the subantral membrane and form a cavity. A filler, such as a bone growth stimulant is injected through the sleeve into the cavity. In the process, the sleeve also can cut and / or condense the bone around itself so that the bone can hold an implant. Optionally, the bone growth stimulant is also introduced into the bone surrounding the sleeve. During the injection, the pressure within the sleeve or the cavity is monitored to detect and prevent the rupture of the subantral membrane.
Owner:HOCHMAN MARK N
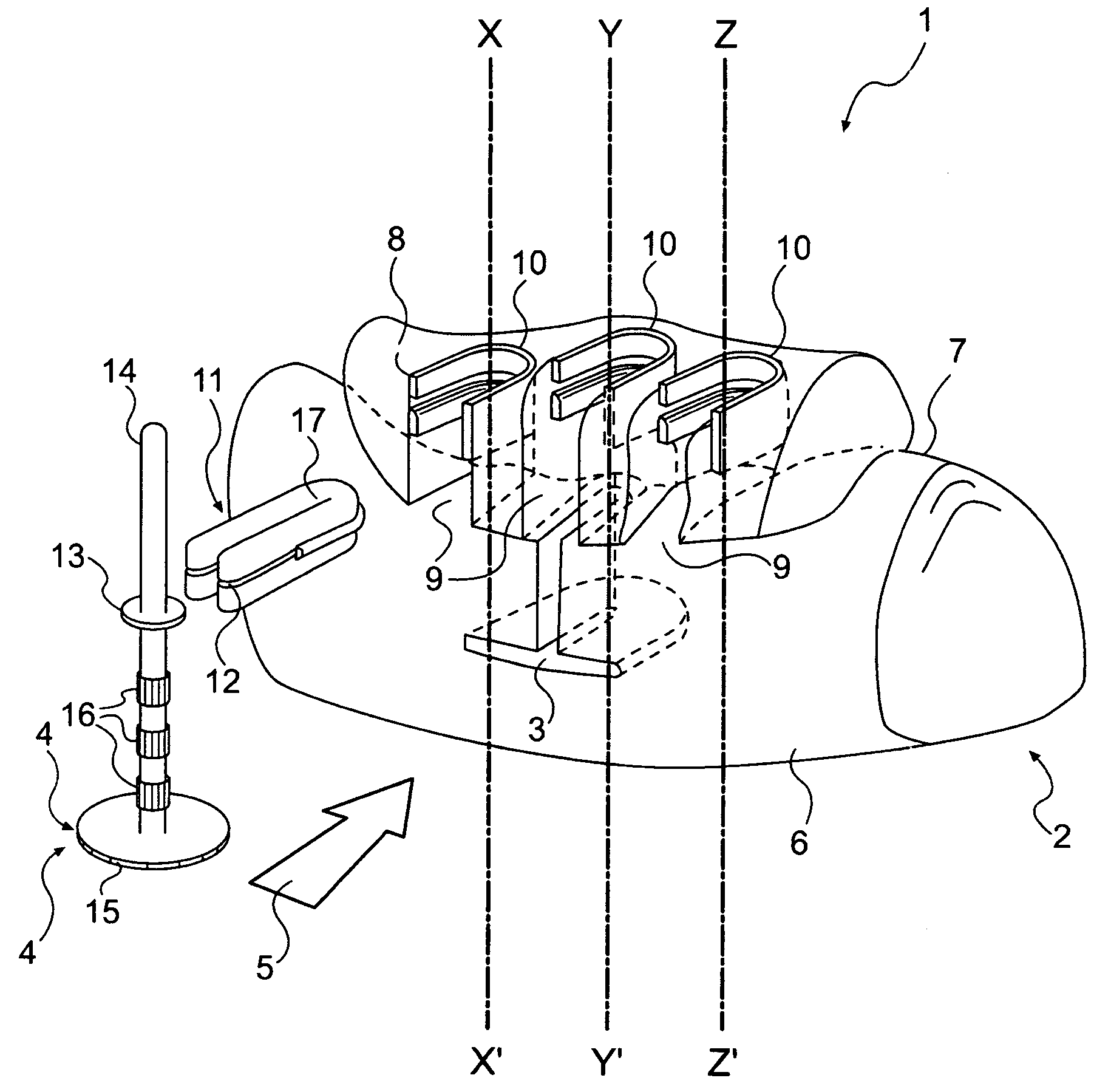
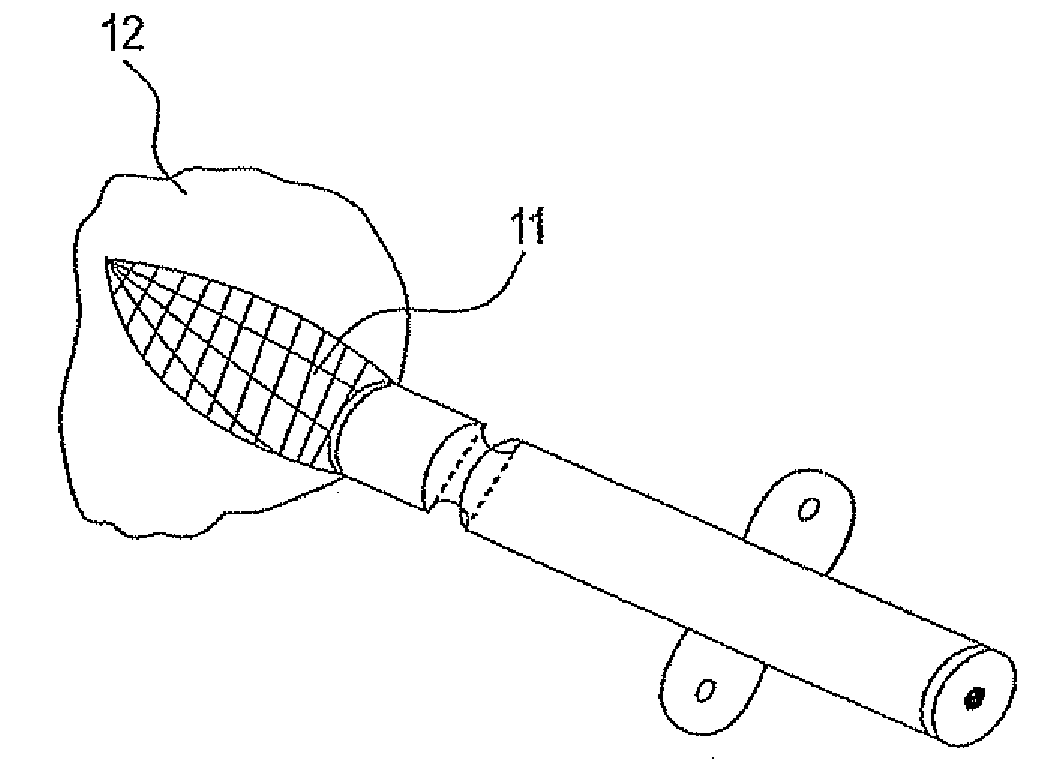
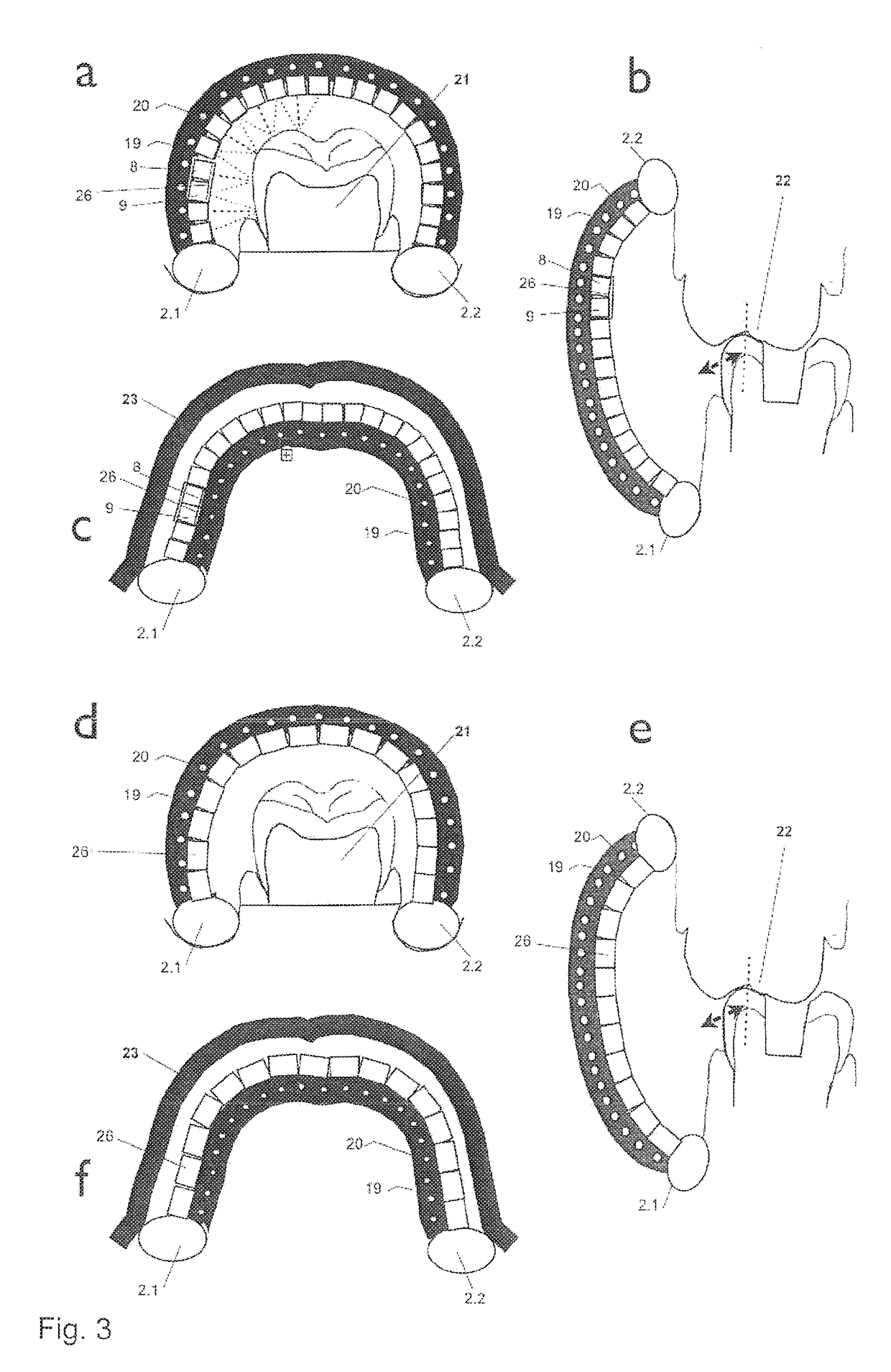
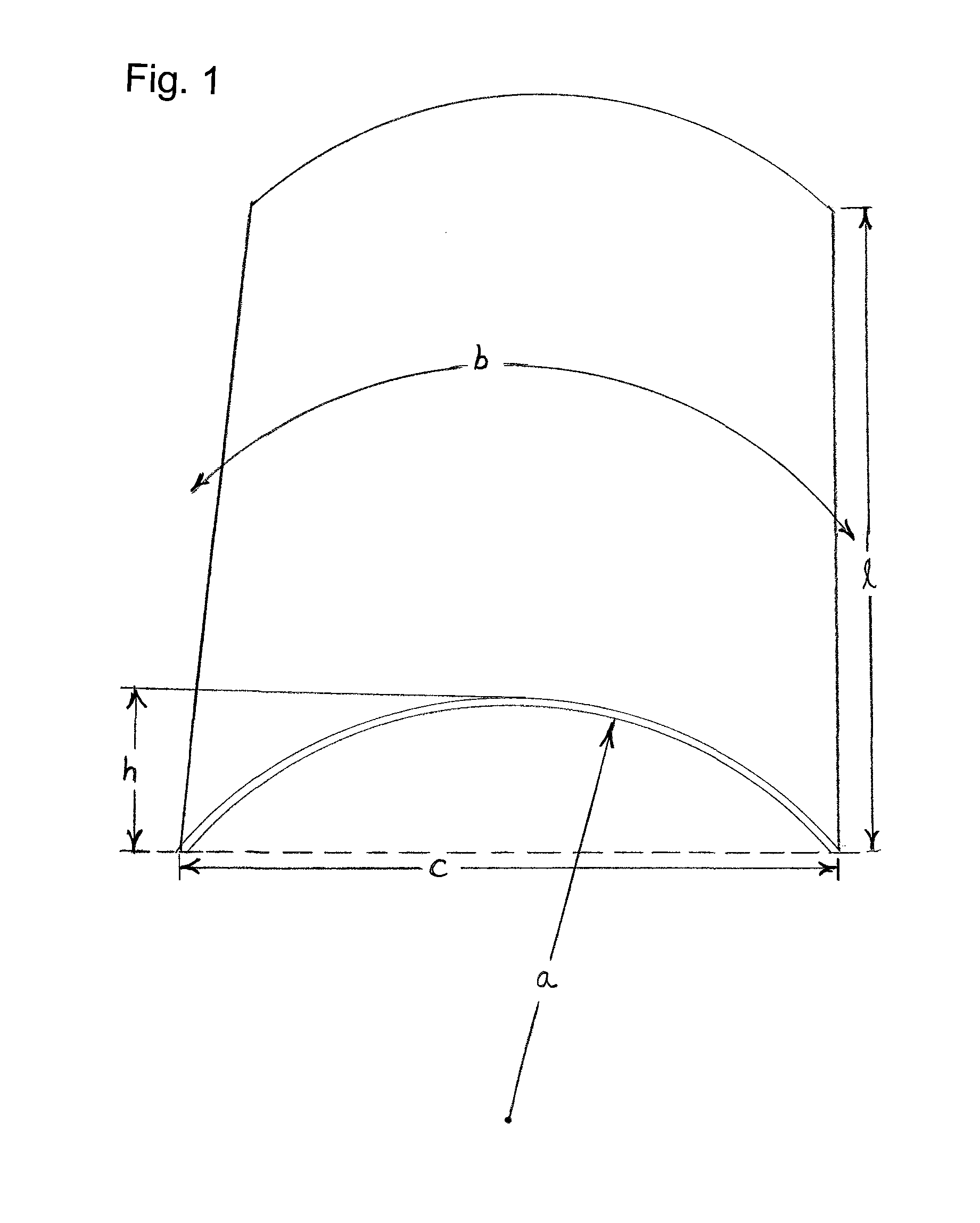
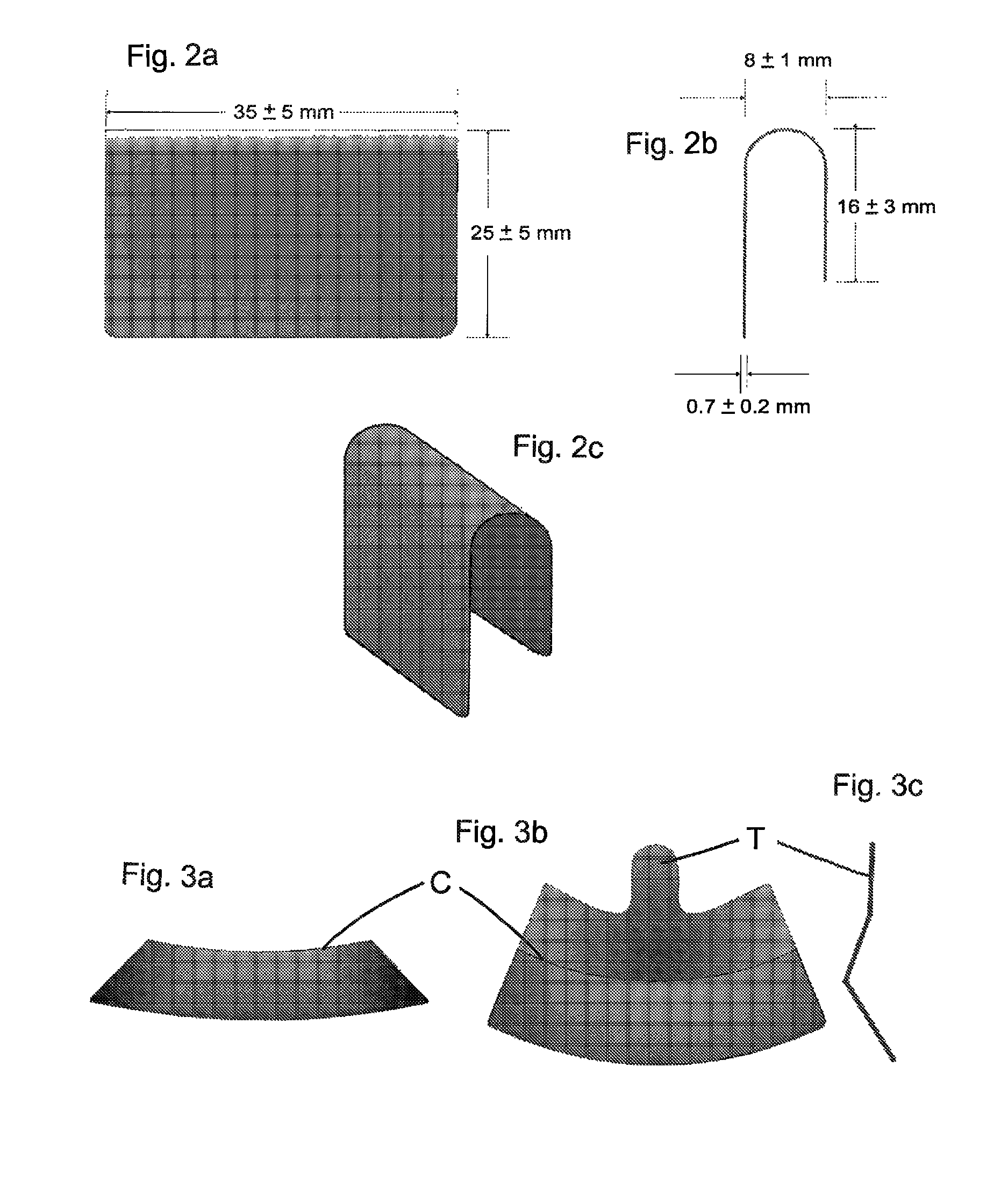
Custom-fit implant surgery guide and associated milling cutter, method for their production, and their use
InactiveUS7824181B2Ensure total axial stabilityEnsure stabilityDental implantsAdditive manufacturing apparatusMilling cutterEngineering
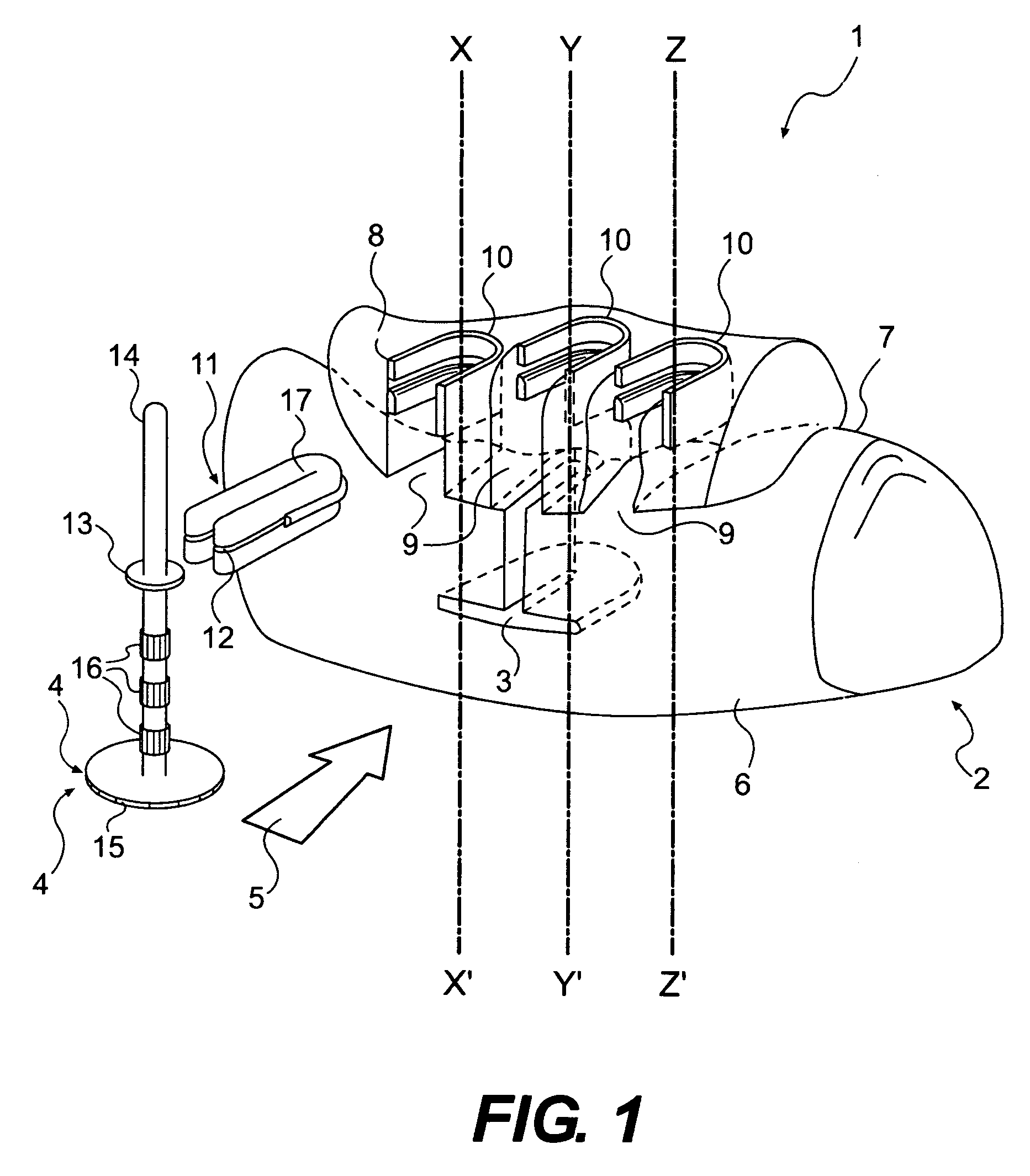
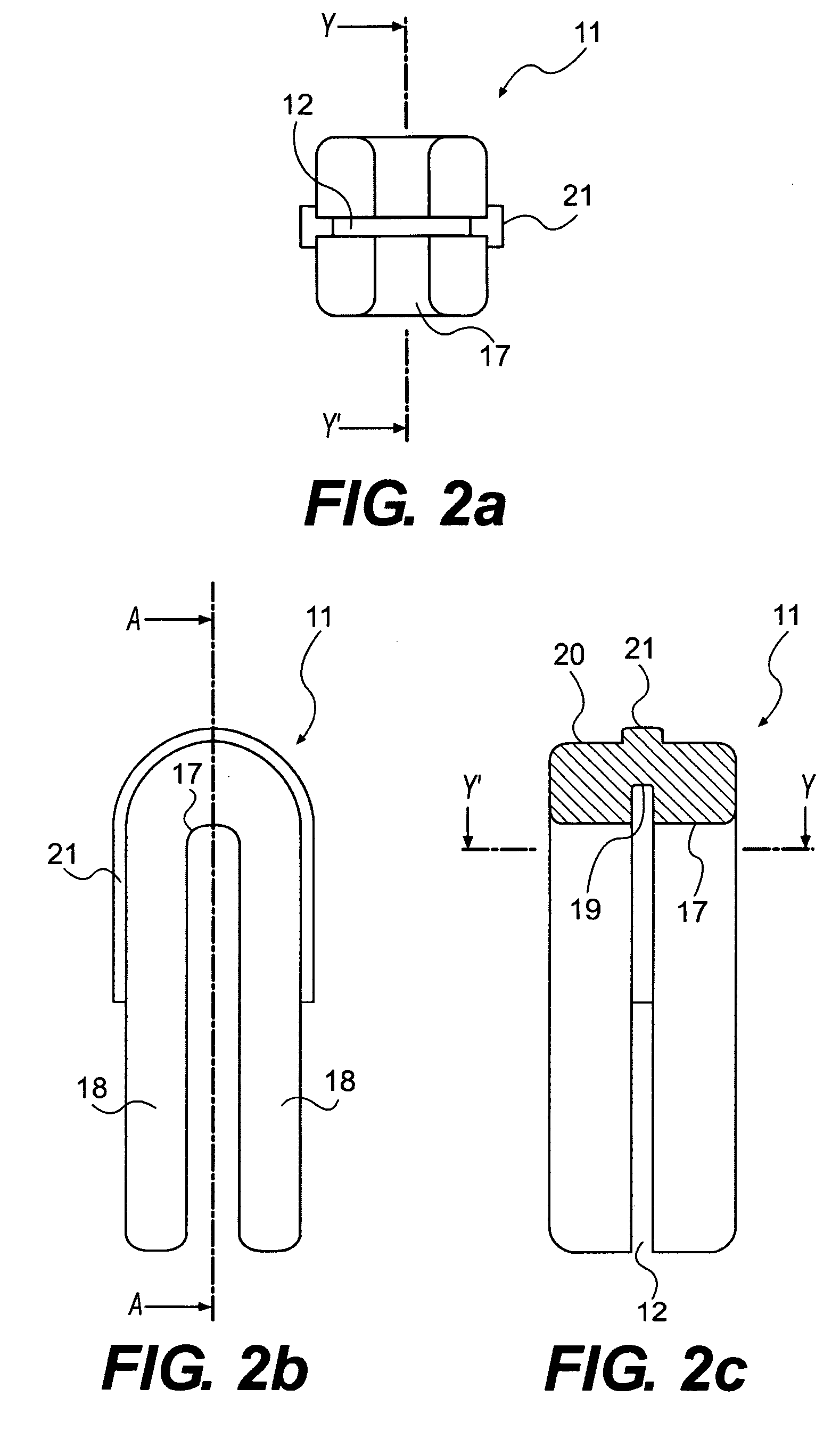
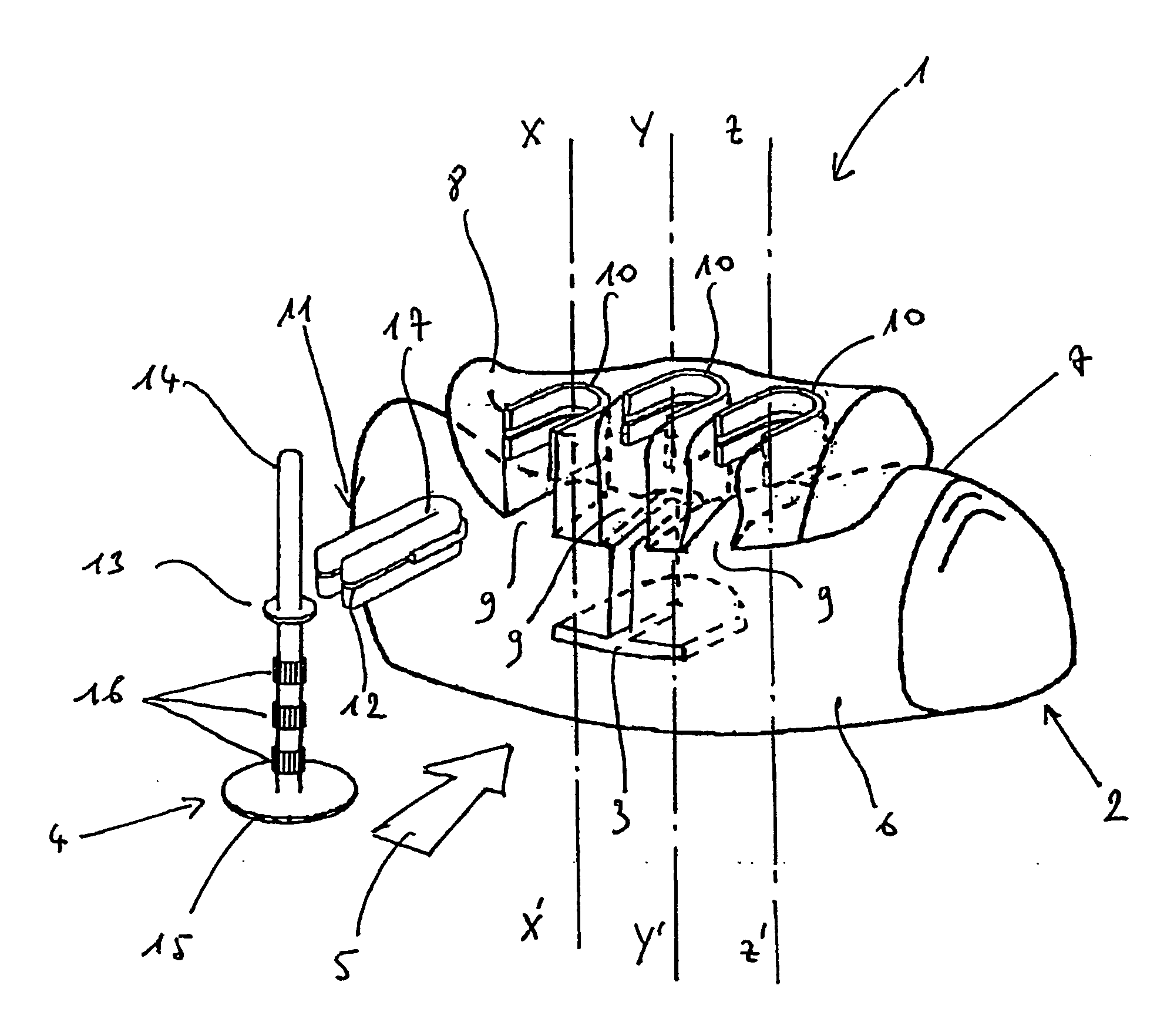
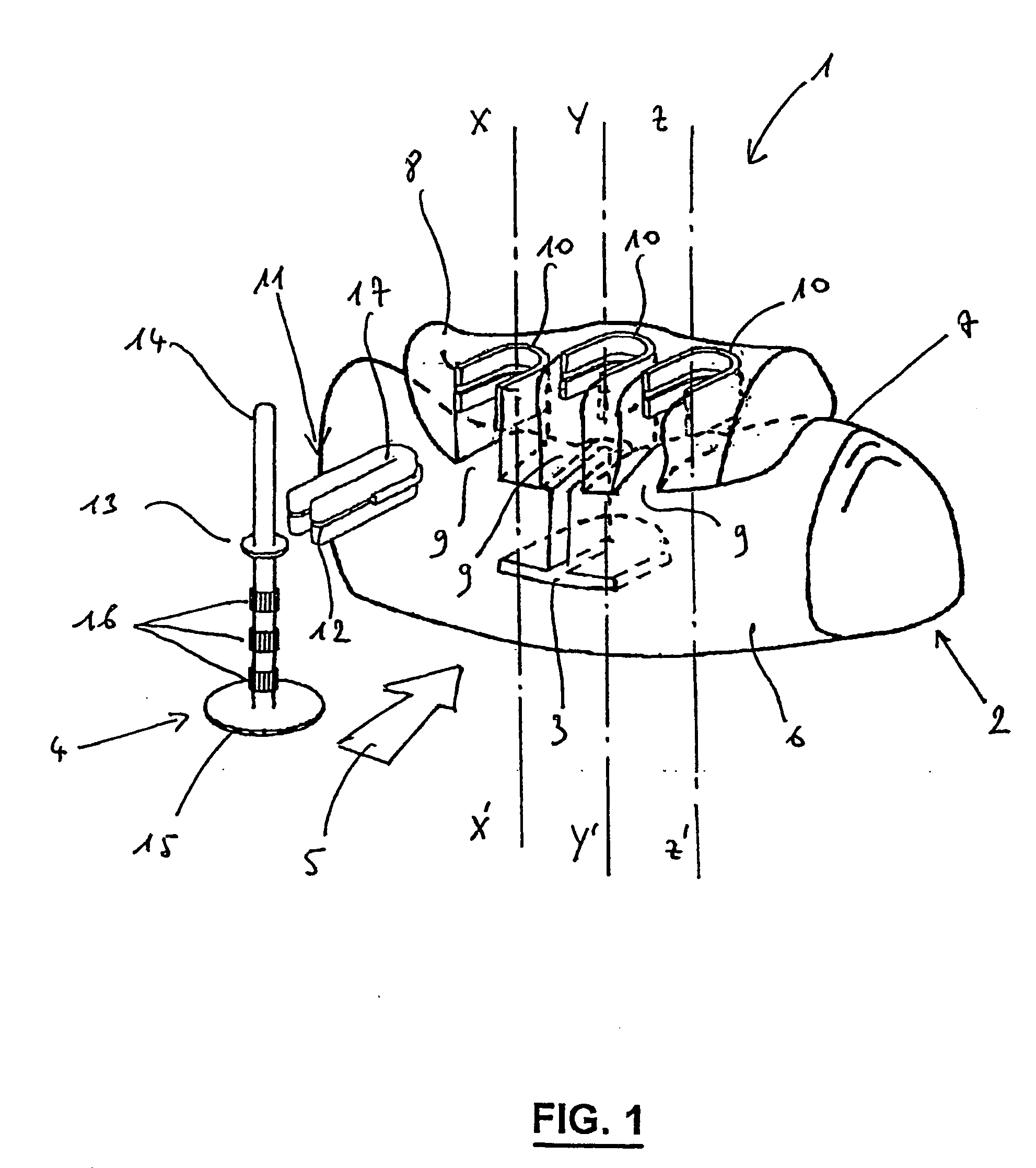
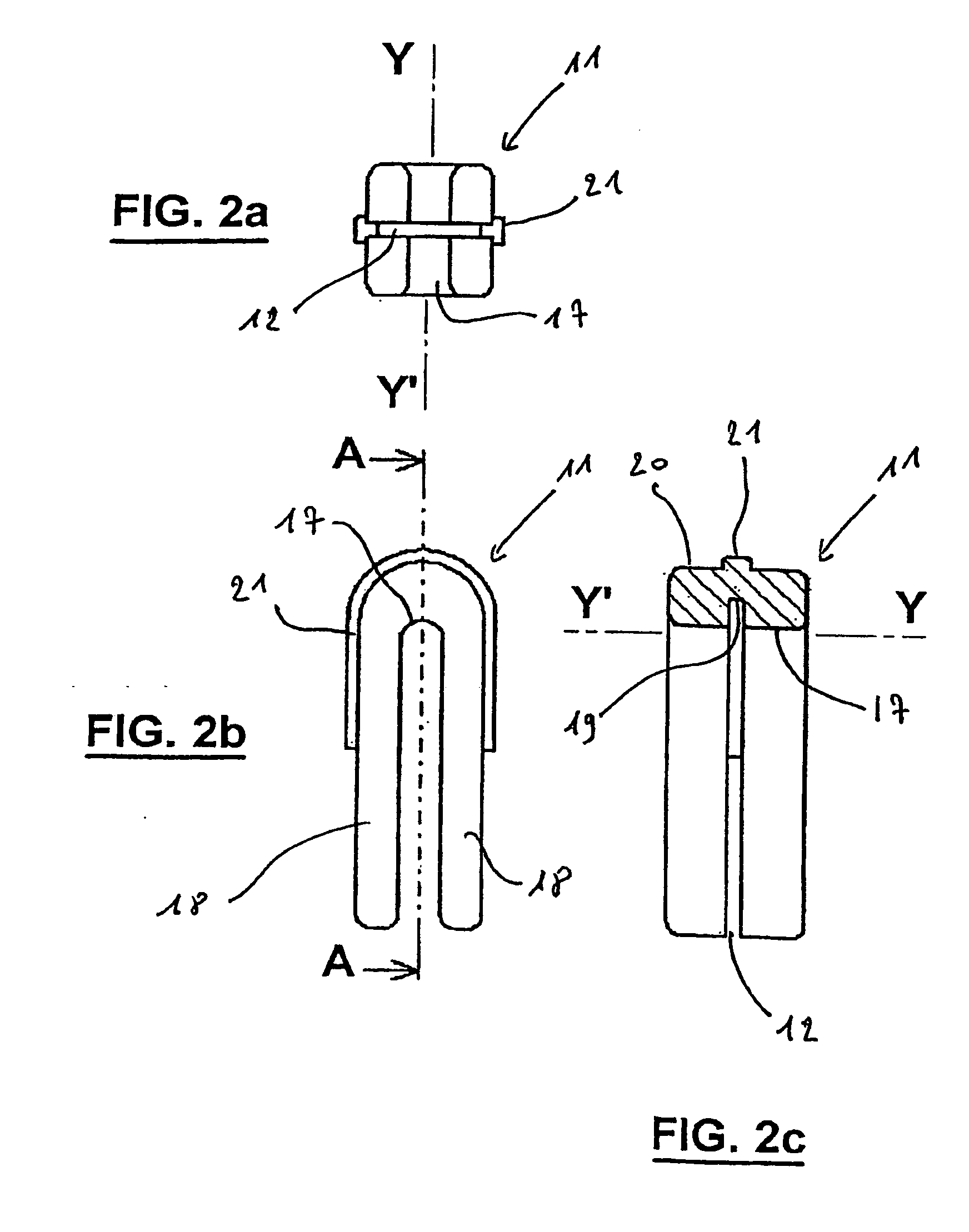
The invention relates to a custom-fit implantable surgical guide (1) and an associated milling tool (4), which is positioned in straddling on the alveolar ridge (7) of a maxillary or mandible arch (2) and comprises at least one drilling barrel (11) for axially guiding said milling tool (4), wherein said barrel (11) is laterally open and at least one part of the internal surface thereof (17) and at least one part of the external surface of the milling tool (4) interact and axially maintain the entire milling tool (4) with respect to the barrel (11). Said invention makes it possible to carry out high precision osteotomies for lateral insertion dental implants.
Owner:MATERIALISE DENTAL NV
Custom-Fit Implantable Surgical Guide and Associated Milling Tool, Method for the Production and Use Thereof
InactiveUS20080287953A1Ensure total axial stabilityEnsure stabilityDental implantsAdditive manufacturing apparatusMilling cutterOsteotomy
The invention relates to a custom-fit implantable surgical guide (1) and an associated milling tool (4), which is positioned in straddling on the alveolar ridge (7) of a maxillary or mandible arch (2) and comprises at least one drilling barrel (11) for axially guiding said milling tool (4), wherein said barrel (11) is laterally open and at least one part of the internal surface thereof (17)and at least one part of the external surface of the milling tool (4) interact and axially maintain the entire milling tool (4) with respect to the barrel (11). Said invention makes it possible to carry out high precision osteotomies for lateral insertion dental implants.
Owner:MATERIALISE DENTAL NV
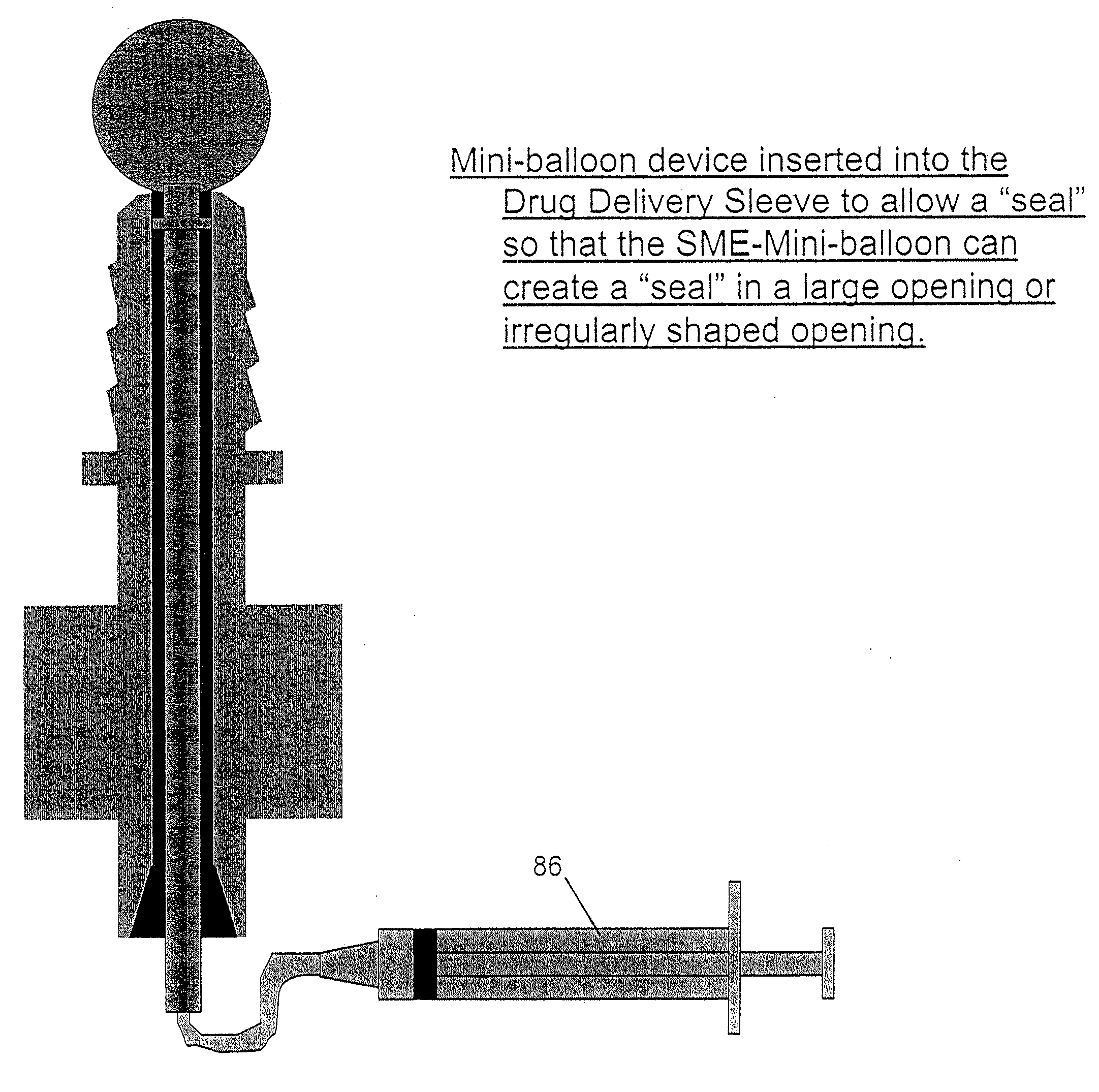
Method and apparatus for performing maxillary sinus elevation
InactiveUS7510397B2Miss massEffective placementDental implantsFastening prosthesisPeritoneumBiomedical engineering
A method and apparatus is disclosed for providing implants in the upper jaws of a person. A sleeve is inserted through the alveolar ridge to the maxillary sinus. The sleeve is used to raise the subantral membrane and form a cavity. A filler, such as a bone growth stimulant is injected through the sleeve into the cavity. In the process, the sleeve also can cut and / or condense the bone around itself so that the bone can hold an implant. Optionally, the bone growth stimulant is also introduced into the bone surrounding the sleeve. During the injection, the pressure within the sleeve or the cavity is monitored to detect and prevent the rupture of the subantral membrane.
Owner:HOCHMAN MARK N
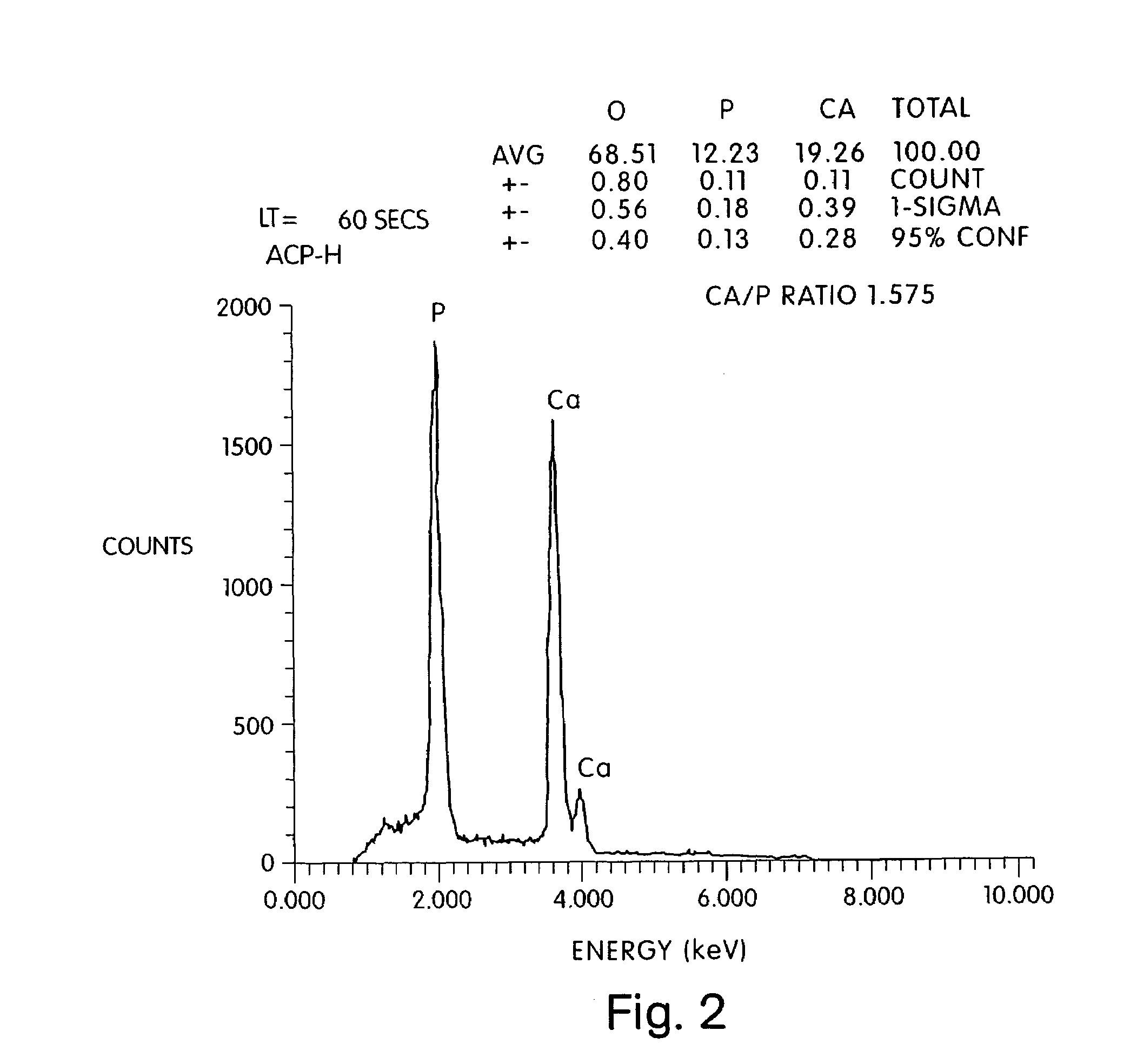
Method of preparing a poorly crystalline calcium phosphate and methods of its use
InactiveUS7517539B1Readily injectableHigh strengthBiocideSurgical adhesivesOsteoporotic boneIntervertebral spaces
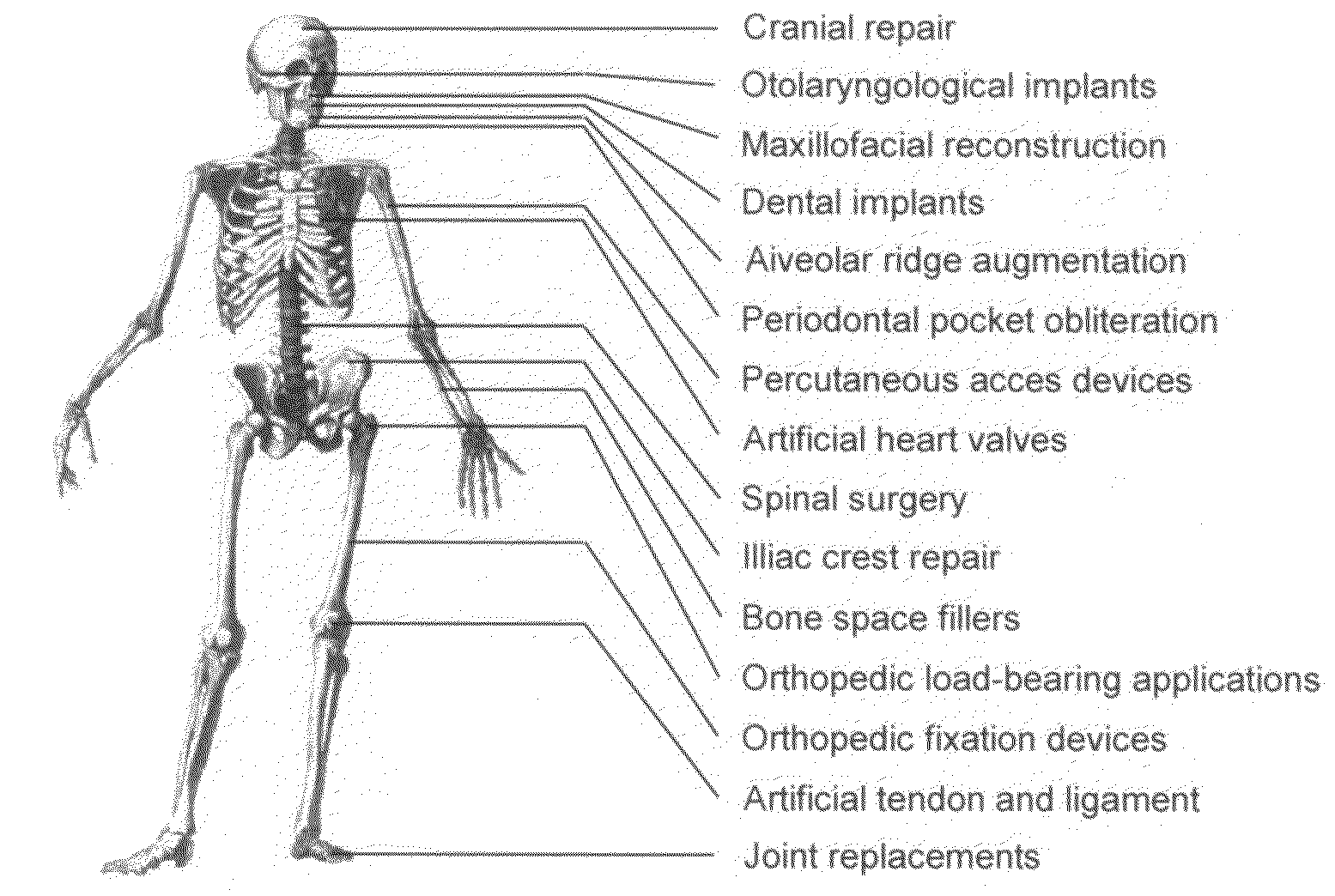
The present invention provides a novel process for producing a calcium phosphate cement or filler which hardens in a temperature dependent fashion in association with an endothermic reaction. In the reaction a limited amount of water is mixed with dry calcium phosphate precursors to produce a hydrated precursor paste. Hardening of the paste occurs rapidly at body temperature and is accompanied by the conversion of one or more of the reactants to poorly crystalline apatitic calcium phosphate. The hardened cements, fillers, growth matrices, orthopedic and delivery devices of the invention are rapidly resorbable and stimulate hard tissue growth and healing. A composite material is provided including a strongly bioresorbable, poorly crystalline apatitic calcium phosphate composite and a supplementary material. The supplementary material is in intimate contact with the hydroxyapatite material in an amount effective to impart a selected characteristic to the composite. The supplemental material may be biocompatible, bioresorbable or non-resorbable. A method for treating a bone defect also is provided by identifying a bone site suitable for receiving an implant, and introducing a strongly resorbable, poorly crystalline apatitic calcium phosphate at the implant site, whereby bone is formed at the implant site. The implant site may be a variety of sites, such as a tooth socket, non-union bone, bone prosthesis, an osteoporotic bone, an intervertebral space, an alveolar ridge or a bone fracture.
Owner:LIFE SCI ENTERPRISES
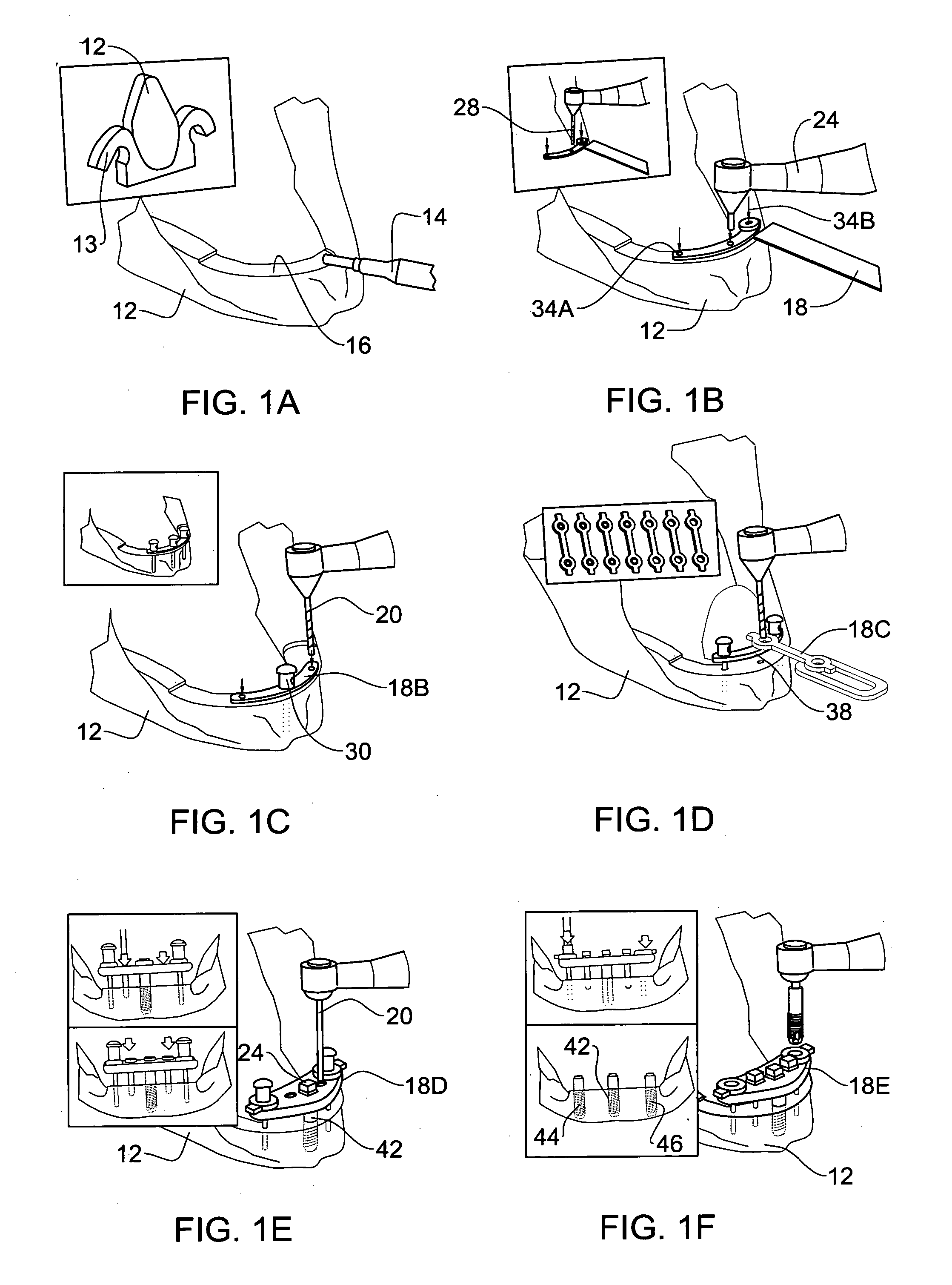
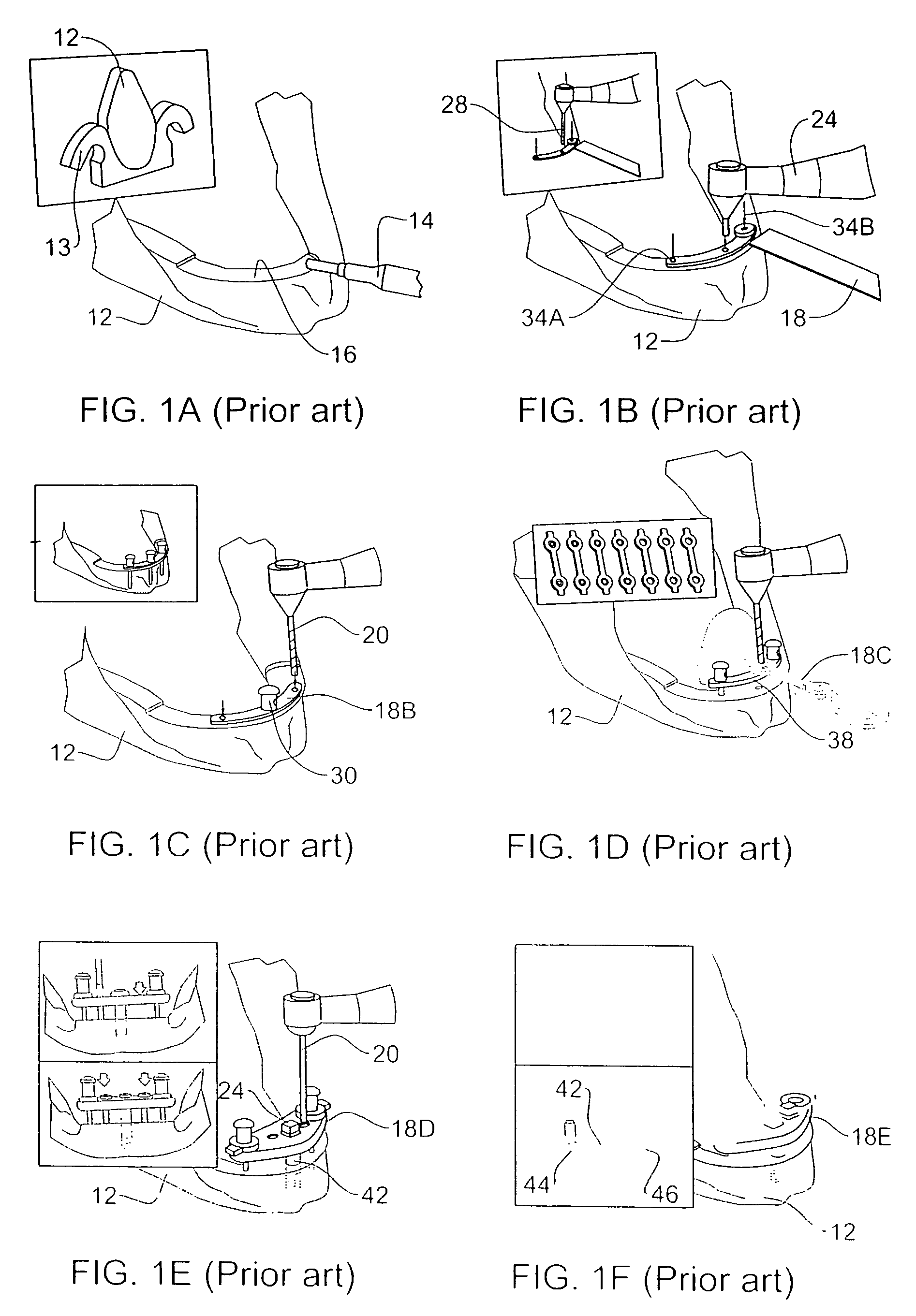
Method and apparatus for performing dental implantation
InactiveUS20070065777A1Reduce irregularitiesProcedure is difficultDental implantsDental toolsPilot holeEngineering
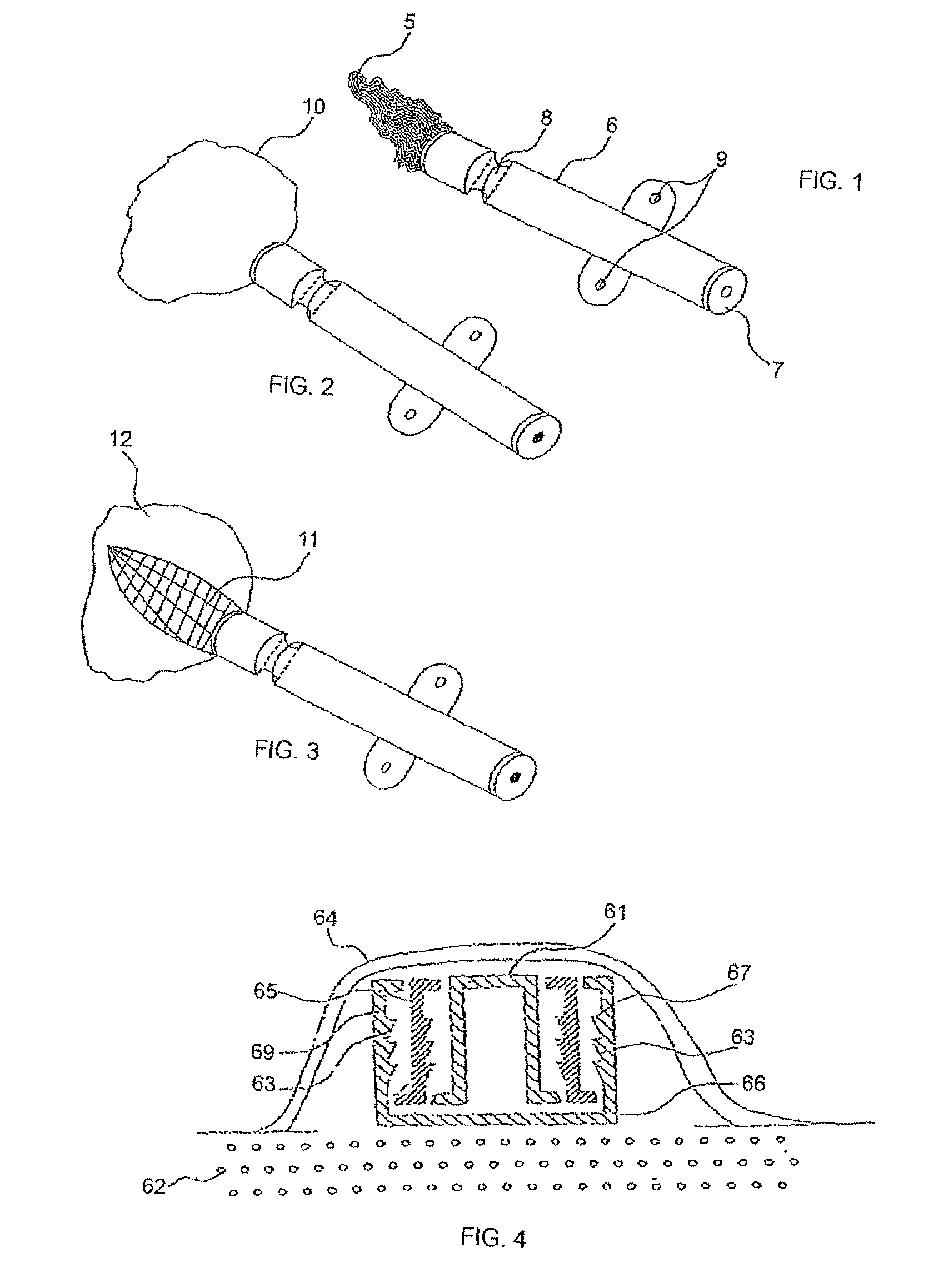
In a dental implantation, after exposure of the alveolar crest and drilling a pilot hole into the crest, a novel mill having an axial guide pin which extends into the pilot hole is used to form clearance for a cover screw or temporary healing abutment. The pilot hole is then enlarged to form clearance for the implant and the screw or abutment is attached.
Owner:BECKER ROBERT
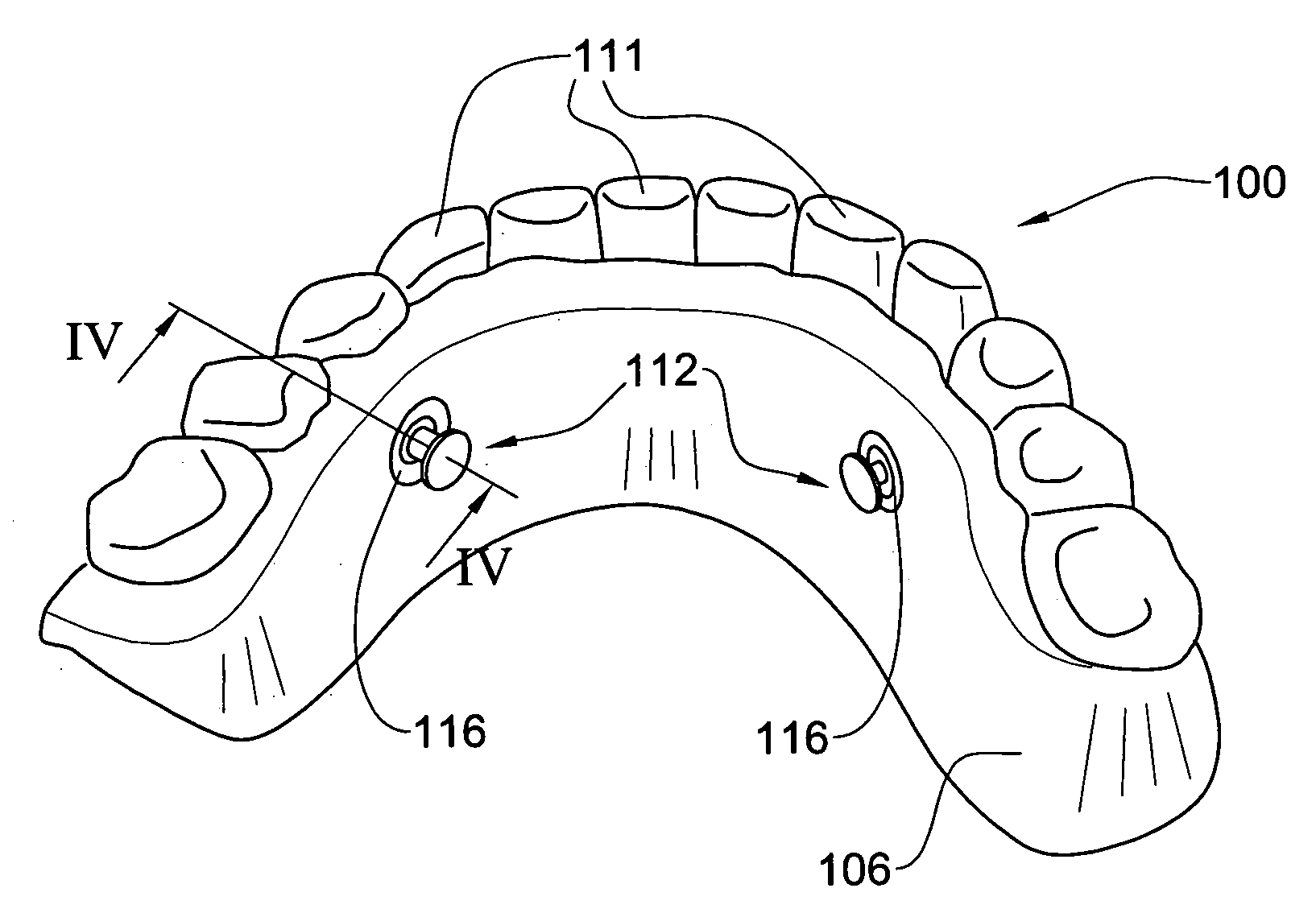
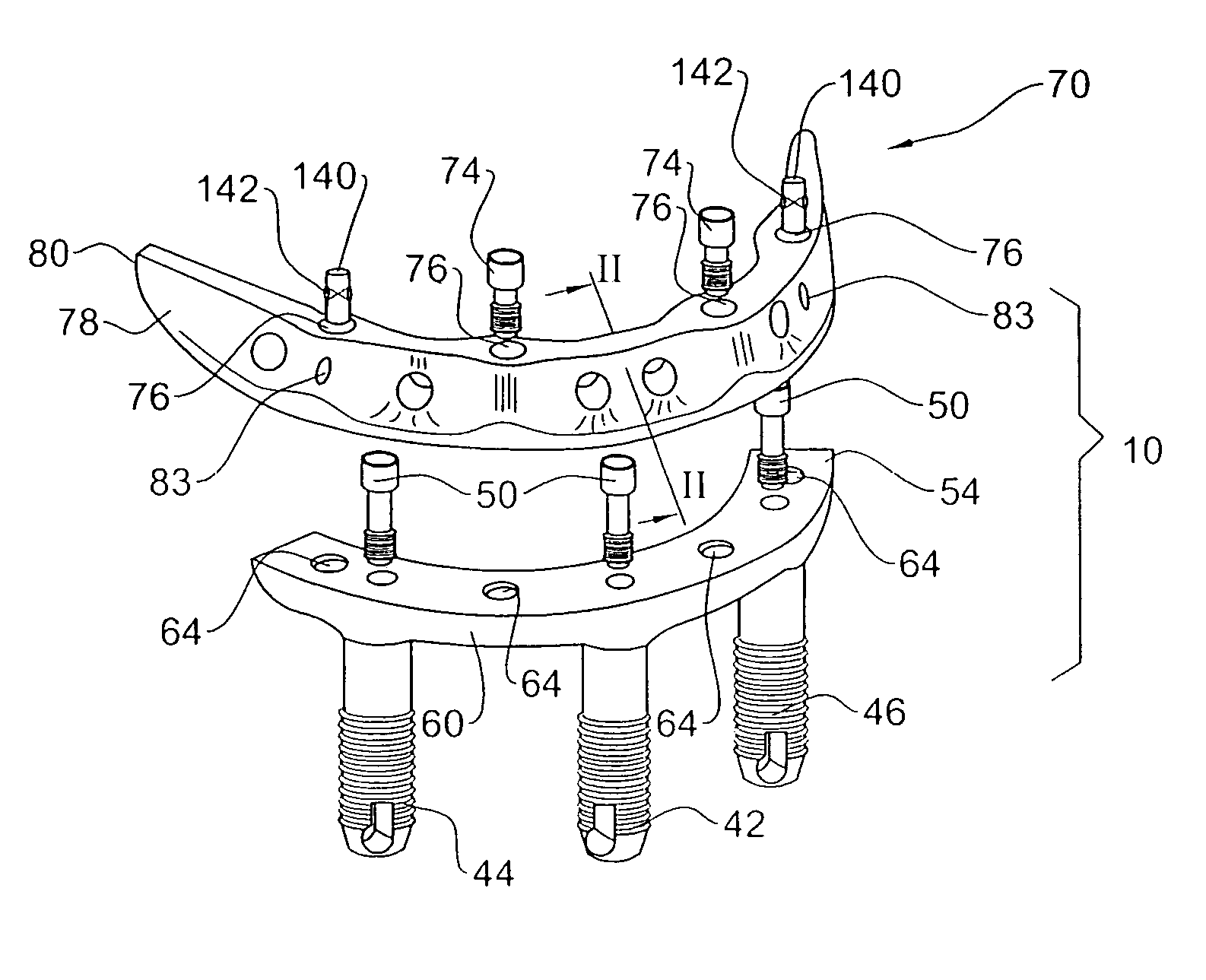
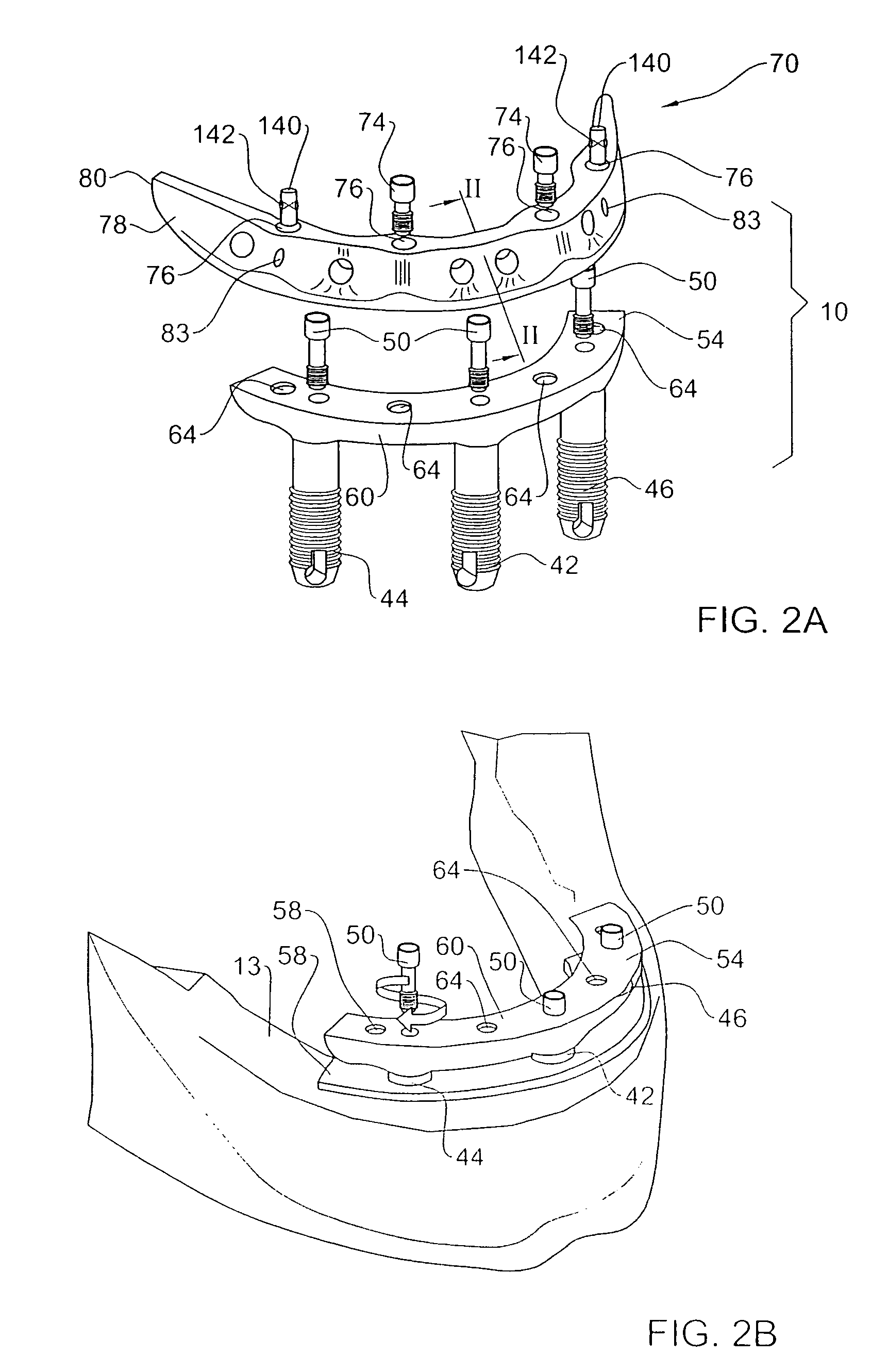
Method and system for fixing removable dentures
ActiveUS20060223029A1Preventing unintentional disengagementTight toleranceDental implantsFastening prosthesisEngineeringDental implant
A removable denture system comprising a support beam fixedly attached to the individual's alveolar ridge above the mucous membrane by a plurality of dental implants, and a denture generally conforming with the dental parameters of the individual and integrated with a supper-structure. The supper-structure comprises at least a portion shaped in confirmation with the support beam, and a denture locking arrangement for removably though fixedly articulating the denture to the support beam preventing unintentional disengagement of the denture.
Owner:BIO DENTAL SOLUTIONS
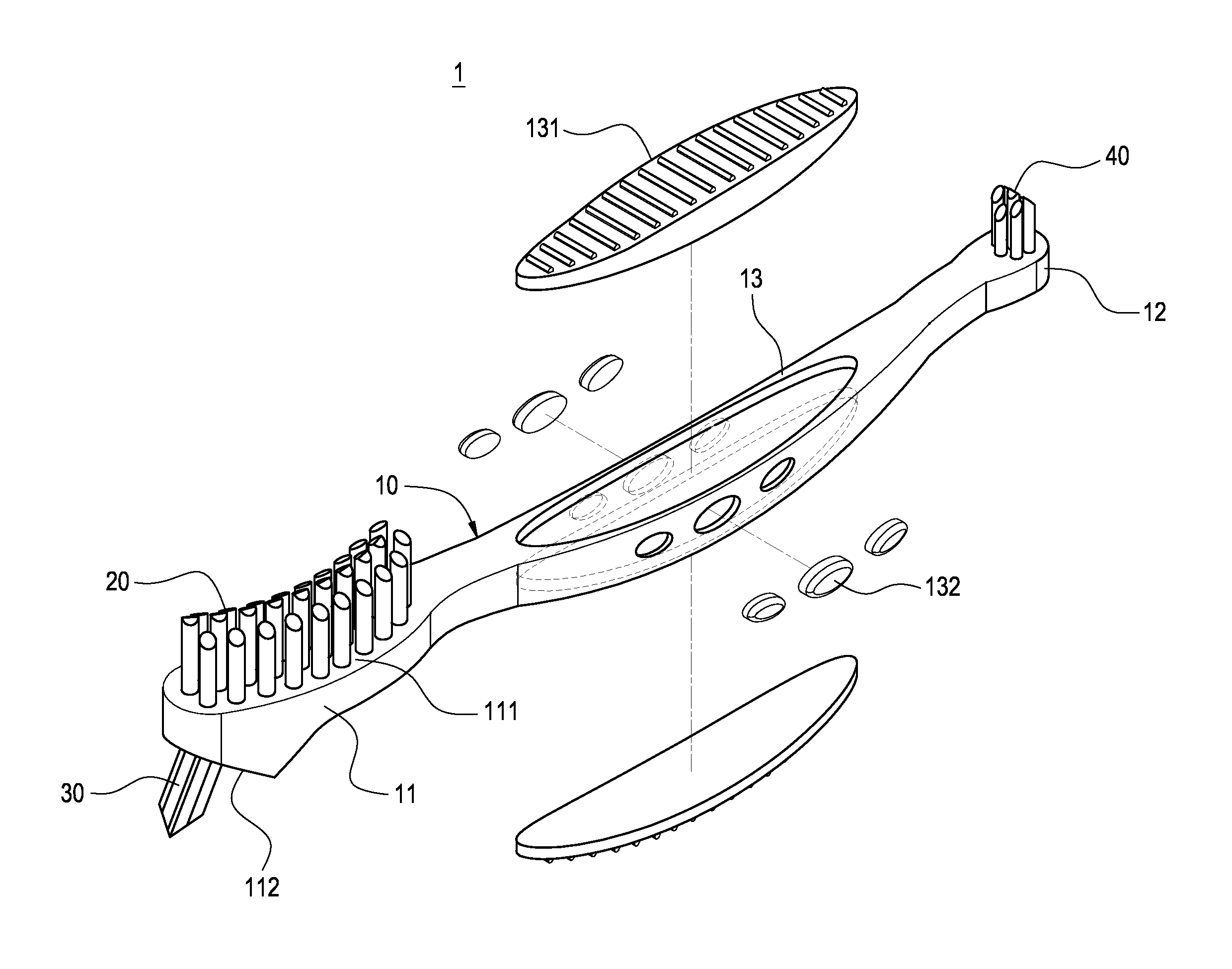
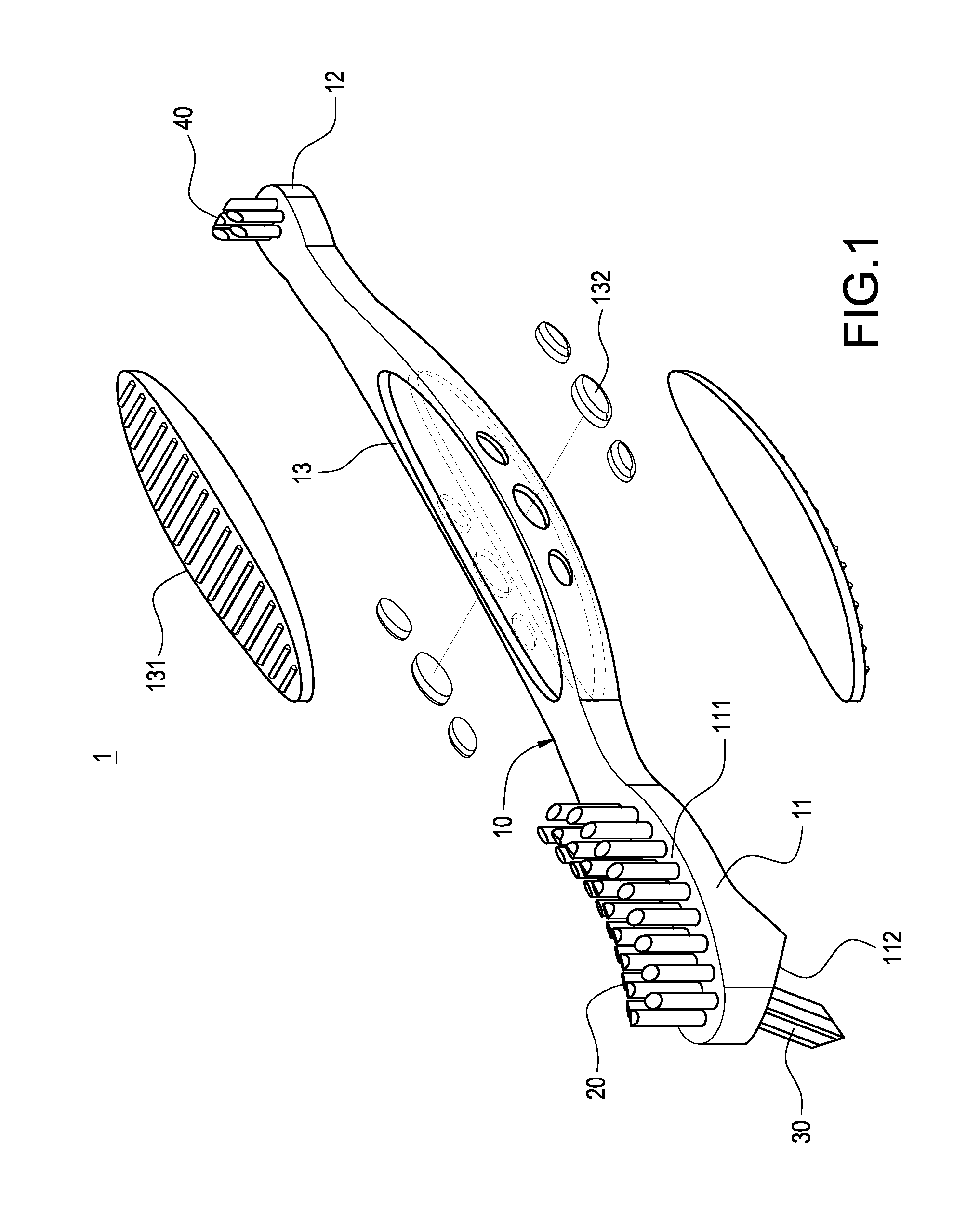
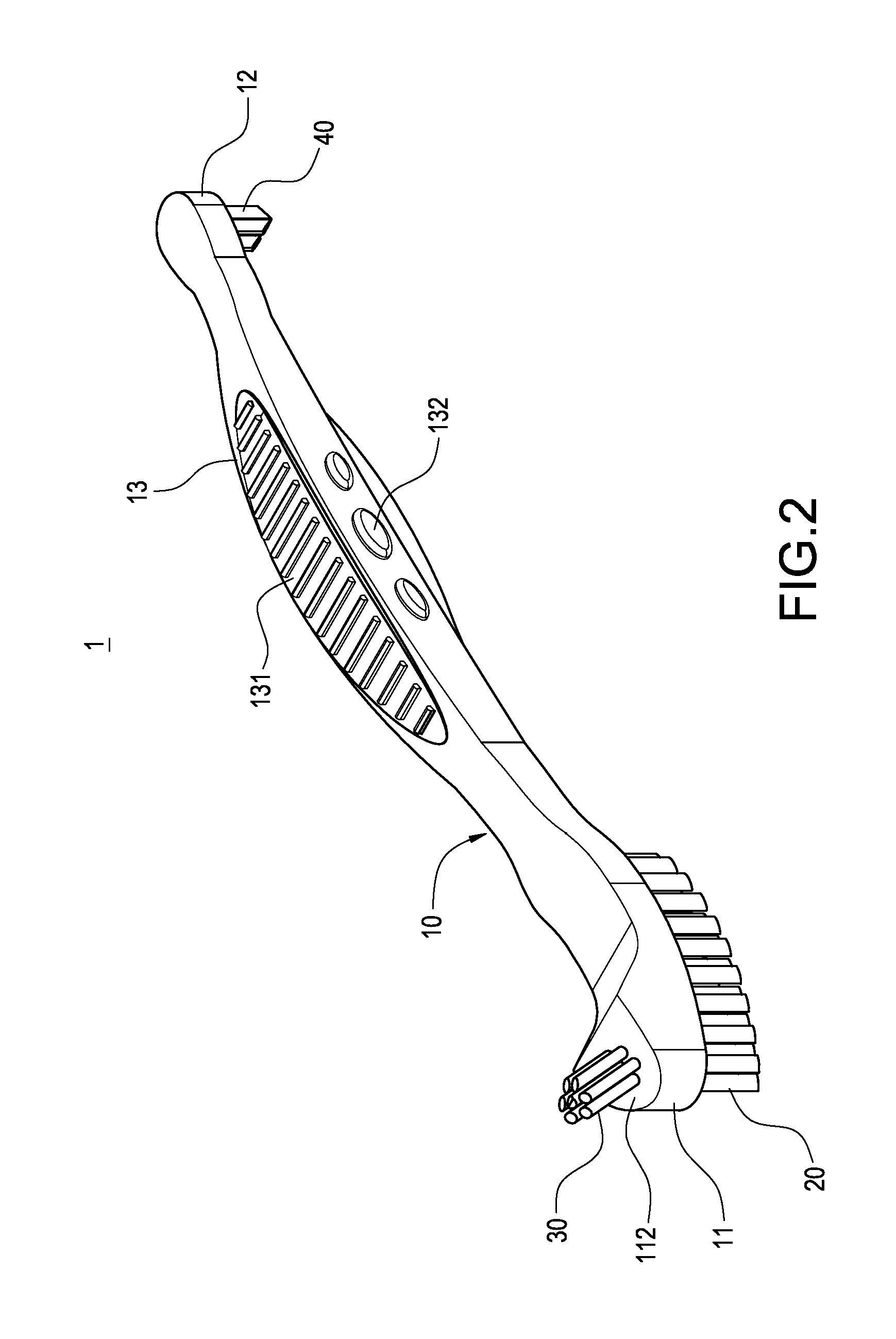
Multi-function brush for overdenture
Owner:CHEN MING SHEH
Ultrasonic dental implant tool set
An ultrasonic dental implant tool set includes an ultrasonic machine, a hand piece connected to the ultrasonic machine and tool members selectively mounted on the hand piece for providing vibrations and a compressed fluid. Each tool member has a connection base, a pole and a cutter tip. The spray nozzle has a connection base, a pole extends from the connection base and having a longitudinal fluid passage for the passing of a fluid and a fluid injection hole for injecting a fluid into a vertical hole made on the alveolar ridge of the patient to be treated, and an operating tip located on one end of the pole remote from the connection base and for insertion into the vertical hole made on the alveolar bone of the patient to transfer ultrasonic vibrations to the fluid applied to the inside of the vertical hole on the alveolar bone of the patient.
Owner:CHEN CHUN LEON
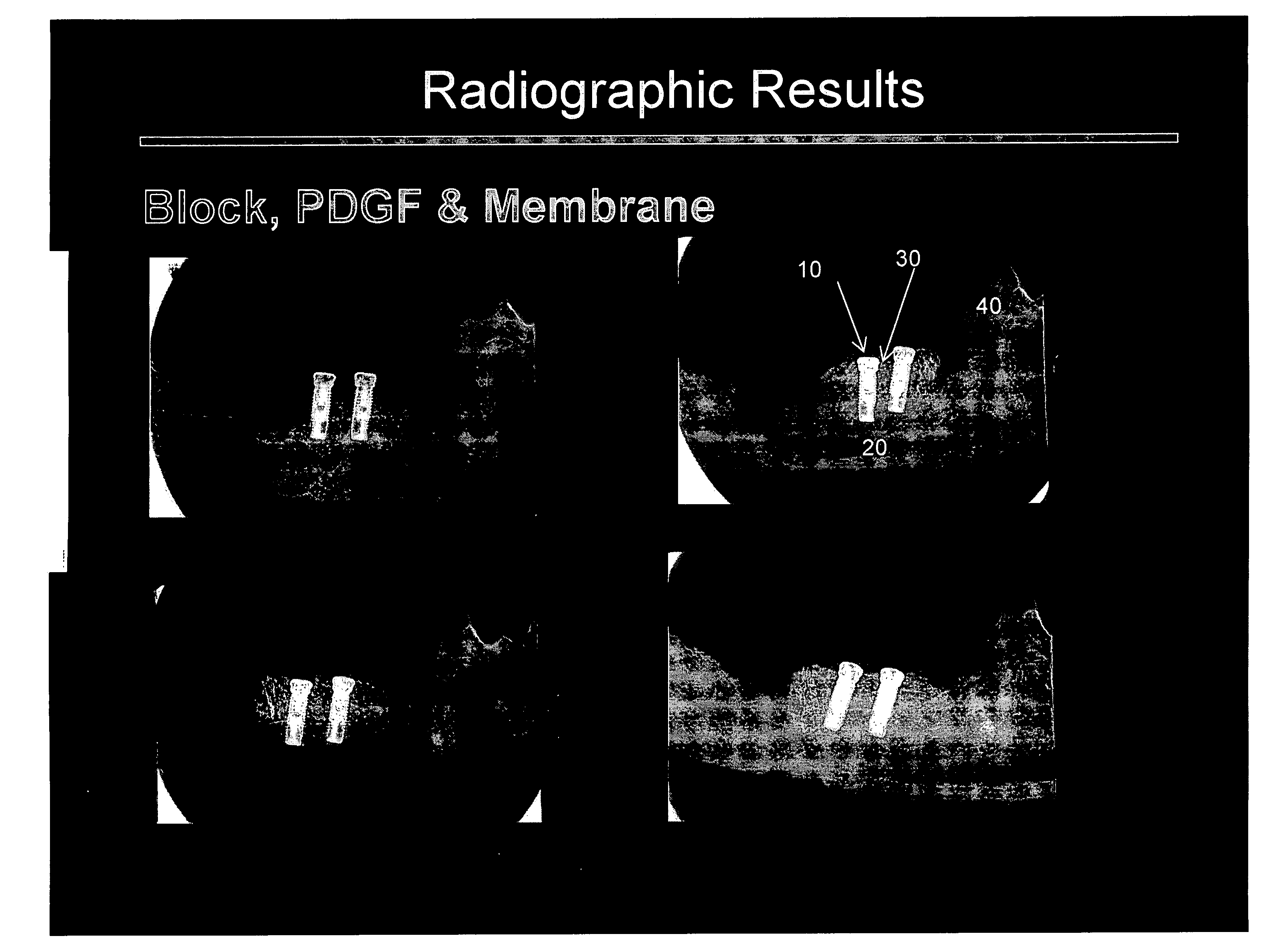
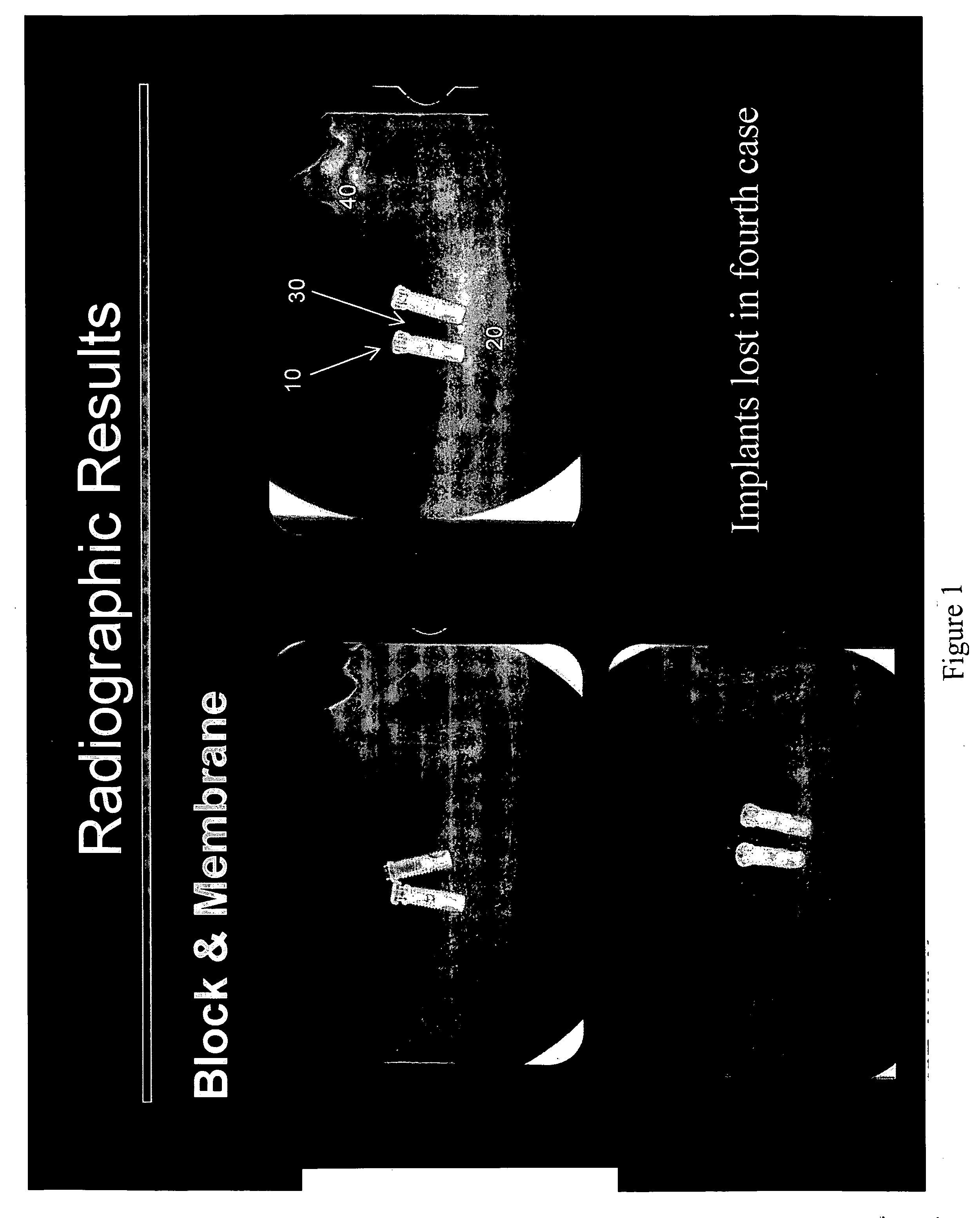
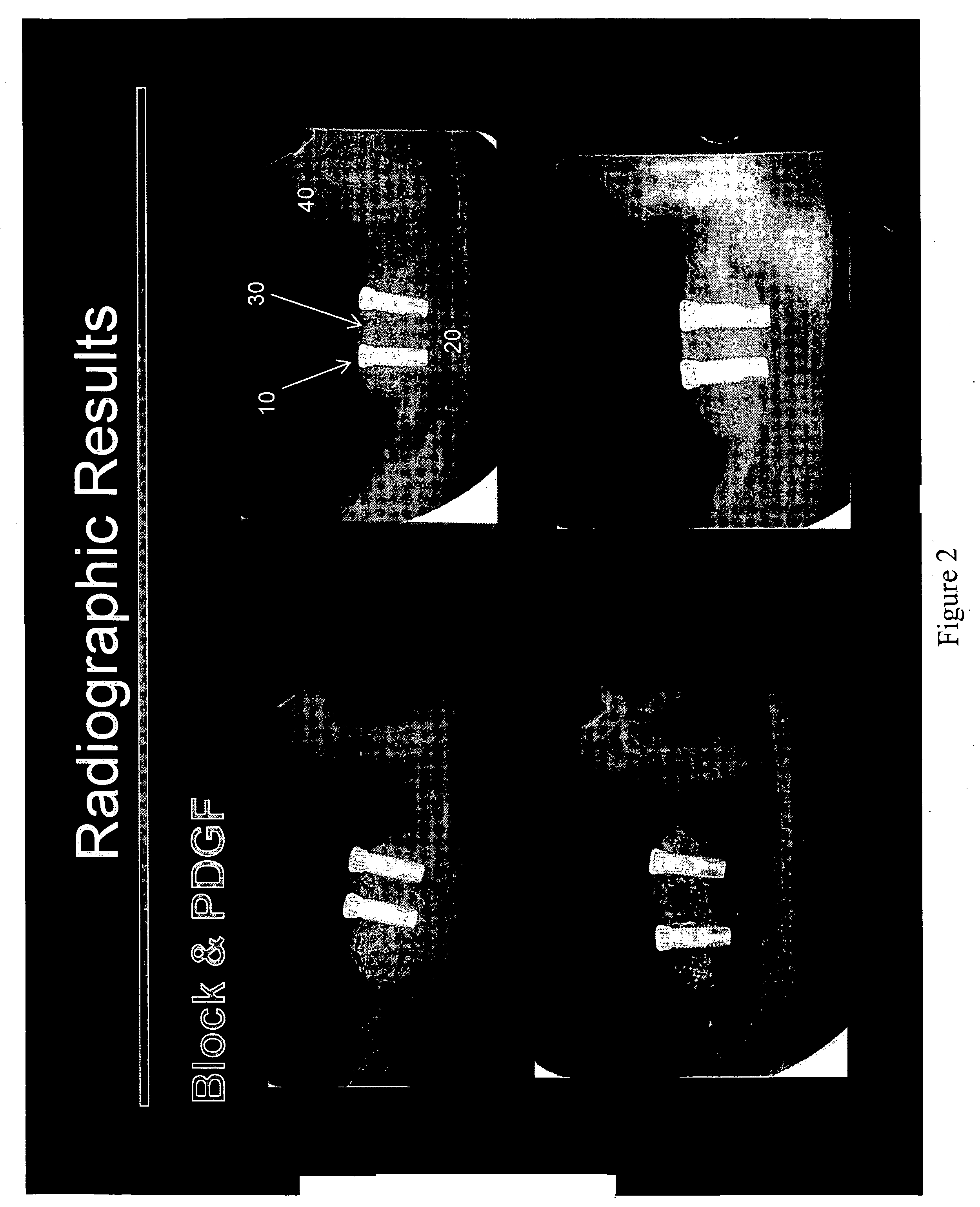
Maxillofacial bone augmentation using rhPDGF-BB and a biocompatible matrix
ActiveUS20070129807A1Facilitating bone augmentationFacilitating maxillofacial bone augmentationPowder deliveryDental implantsPresent methodBioresorbable membrane
The present invention provides effective new methods and materials for maxillofacial bone augmentation, particularly alveolar ridge augmentation, that are free of problems associated with prior art methods. In one embodiment, these materials include human recombinant platelet derived growth factor (rhPDGF-BB) and a biocompatible matrix. In another embodiment, these materials include rhPDGF-BB, a deproteinized bone block or calcium phosphate, and a bioresorbable membrane. The use of these materials in the present method is effective in regenerating maxillofacial bones and facilitating achievement of stable osseointegrated implants. The mandible and maxilla are preferred bones for augmentation, and enhancement of the alveolar ridge is a preferred embodiment of the present invention.
Owner:BIOMIMETIC THERAPEUTICS INC
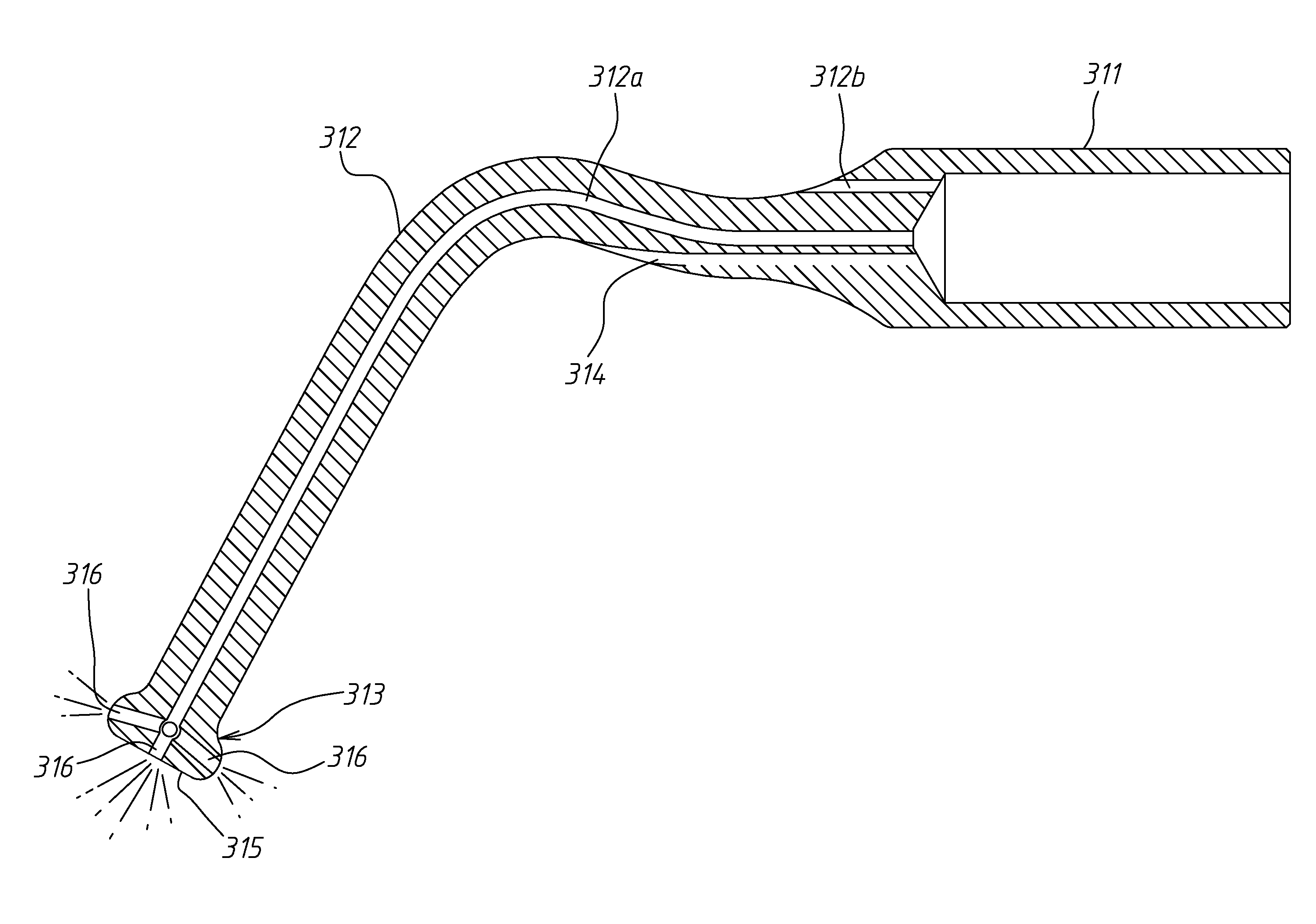
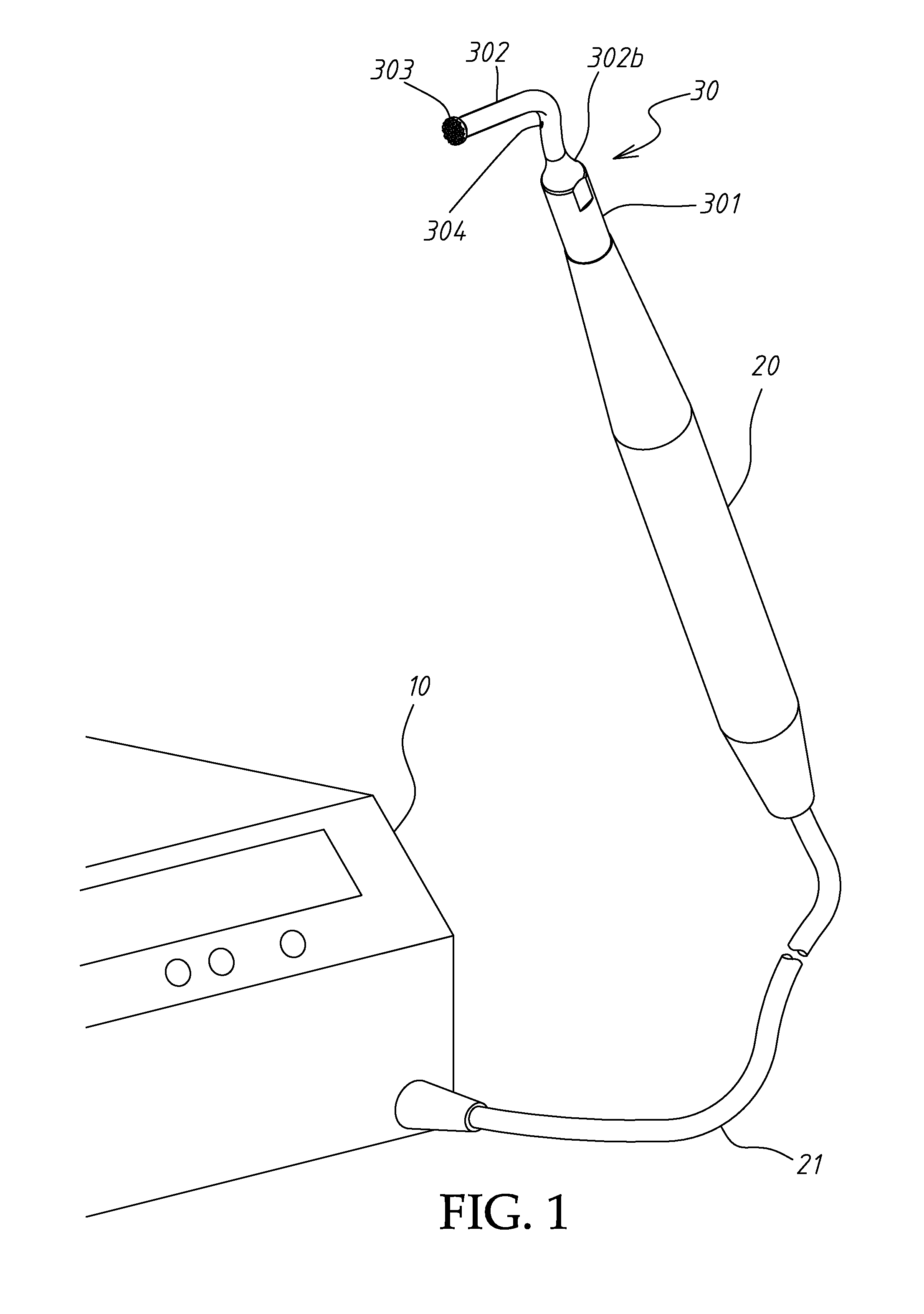
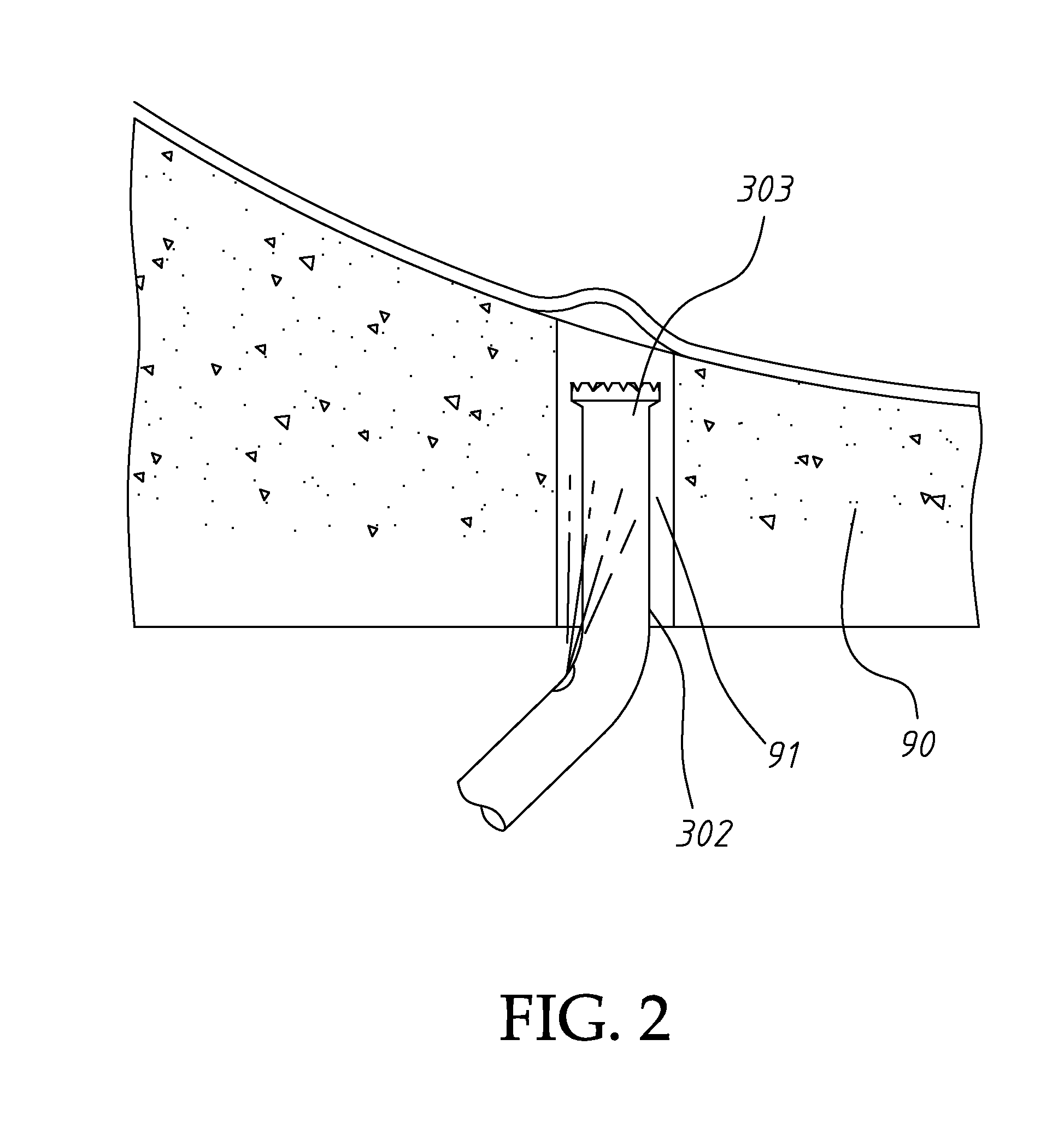
Method and apparatus for performing maxillary sinus elevation
InactiveUS20080213729A1Miss massEffective placementDental implantsTeeth fillingPeritoneumBiomedical engineering
A method and apparatus is disclosed for providing implants in the upper jaws of a person. A sleeve is inserted through the alveolar ridge to the maxillary sinus. The sleeve is used to raise the subantral membrane and form a cavity. A filler, such as a bone growth stimulant is injected through the sleeve into the cavity. In the process, the sleeve also can cut and / or condense the bone around itself so that the bone can hold an implant. Optionally, the bone growth stimulant is also introduced into the bone surrounding the sleeve. During the injection, the pressure within the sleeve or the cavity is monitored to detect and prevent the rupture of the subantral membrane.
Owner:HOCHMAN MARK N
Method and system for fixing removable dentures
ActiveUS7806691B2Preventing unintentional disengagementTight toleranceDental implantsFastening prosthesisSuper structureEngineering
A removable denture system comprising a support beam fixedly attached to the individual's alveolar ridge above the mucous membrane by a plurality of dental implants, and a denture generally conforming with the dental parameters of the individual and integrated with a super-structure. The super-structure comprises at least a portion shaped in confirmation with the support beam, and a denture locking arrangement for removably though fixedly articulating the denture to the support beam preventing unintentional disengagement of the denture.
Owner:BIO DENTAL SOLUTIONS
Aesthetic dental implant fixture and abutment system
InactiveUS20050244789A1Sustains optimal peri-implant healthGood for healthDental implantsDental surgeryPeri implant bone
A dental implant fixture and abutment system for use in restorative dental surgery comprises a thin coating, preferably of gold, applied to certain regions of the implant fixture and to certain regions of the abutment post, so as to mask or camouflage the unattractive dark root and crown appearance of prior art dental restorations which is caused primarily by the innate gray-black chroma of the titanium alloys out of which such restorations are conventionally fabricated. Optionally, the implant fixture may also be shaped such that, upon placement in the mouth, the transgingival portions of the implant fixture are more coronal on the palatal aspect and more apical on the facial aspect, thereby accommodating the differences in the residual alveolar ridge morphology and allowing for maintenance of peri-implant bone height post implant placement. Both one-stage and two-stage dental implant systems having such characteristics are disclosed, as are dental restoration systems in which a prosthetic tooth device or crown is combined with a one-stage or two-stage dental implant having such a characteristics.
Owner:CROHIN CONSTANT C +1
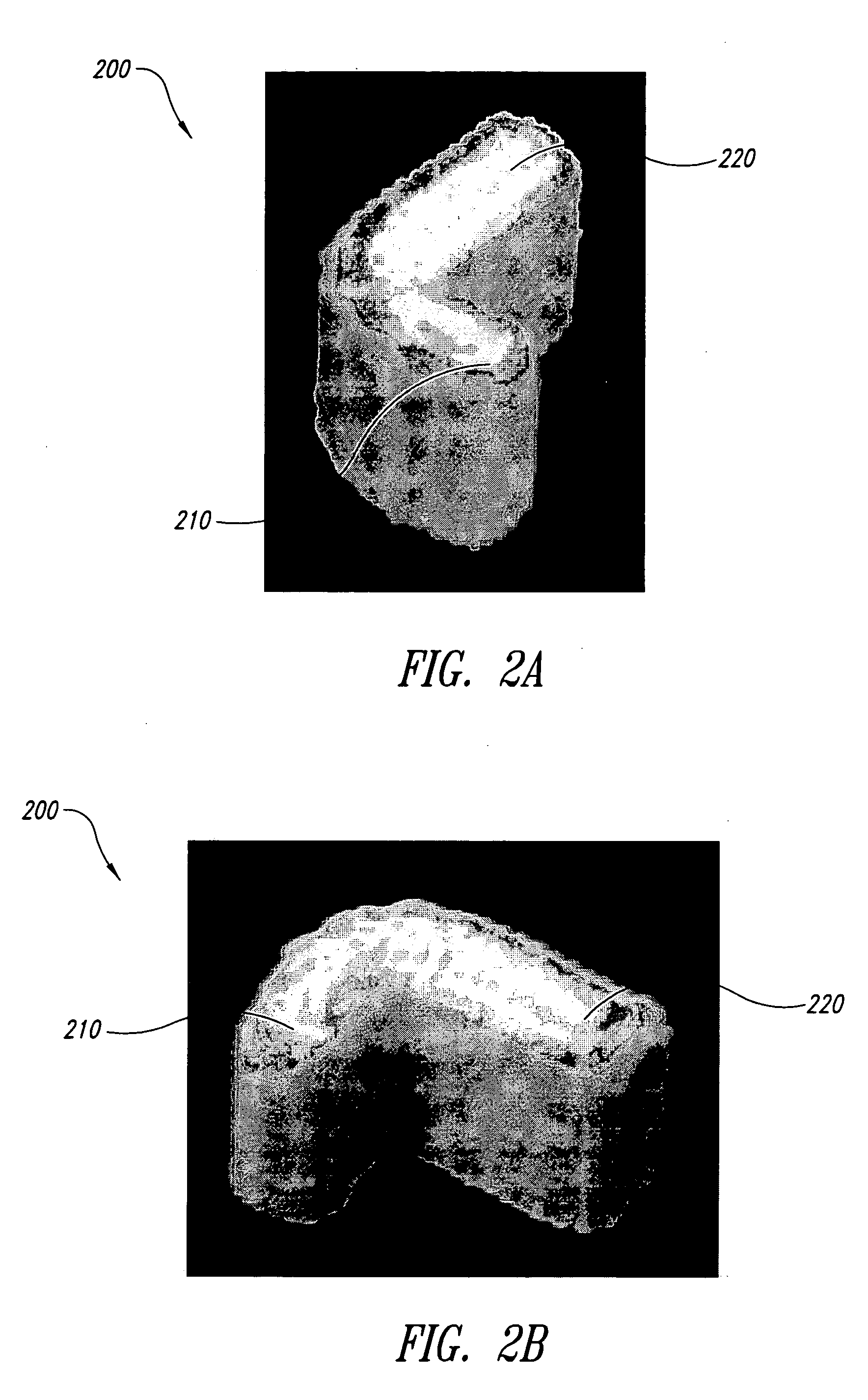
Method of manufacture, installation, and system for an alveolar ridge augmentation graft
A bone graft that is made at least partially of synthetic material or demineralized bone matrix and is manufactured in suitable shape and / or dimensions to augment an alveolar ridge. The bone graft may be such as to augment both a portion of the crest of the alveolar ridge and a portion of at least one side of the alveolar ridge. The graft may include at least one hole for the intended position of an implant base, and / or at least one hole for attachment hardware. The graft may be manufactured to standard dimensions or it may be manufactured to patient-unique dimensions which may be determined radiographically prior to surgery and prior to manufacturing of the bone graft. The bone graft may be able to be carved for dimensional adjustment during surgery. The bone graft may have composition and / or local geometry which varies from one place to another, and may have a particular composition and / or local geometry at places intended to adjoin natural bone.
Owner:THERICS
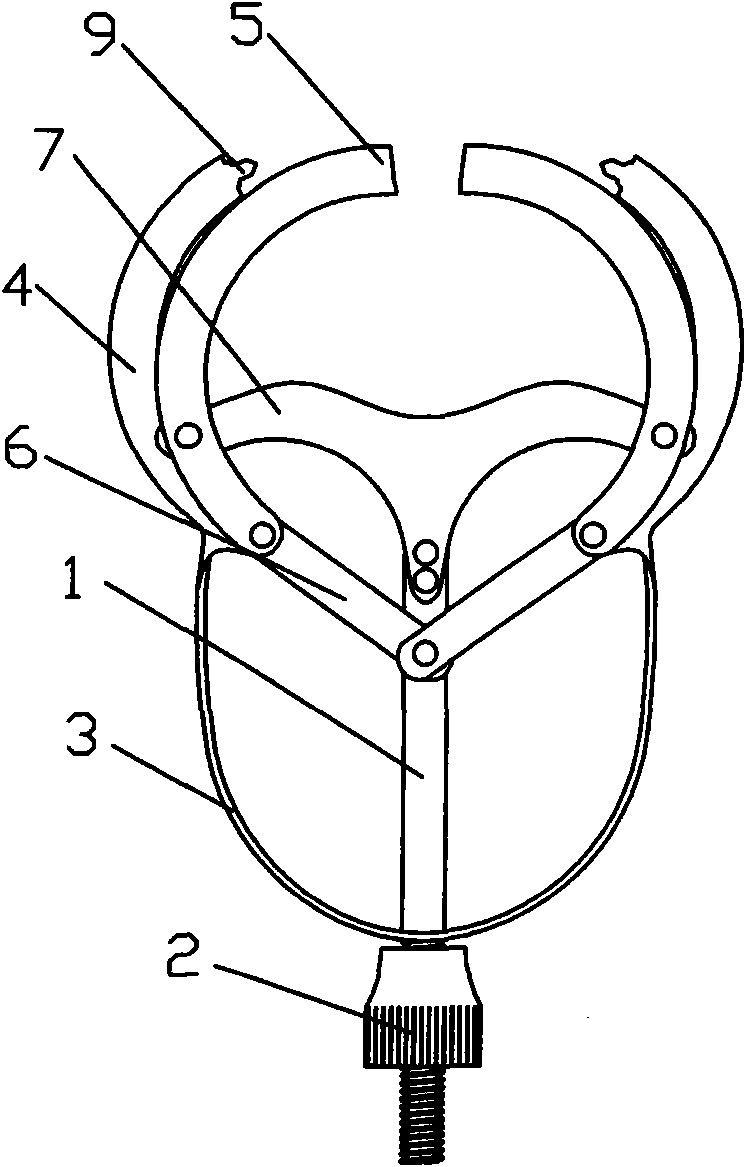
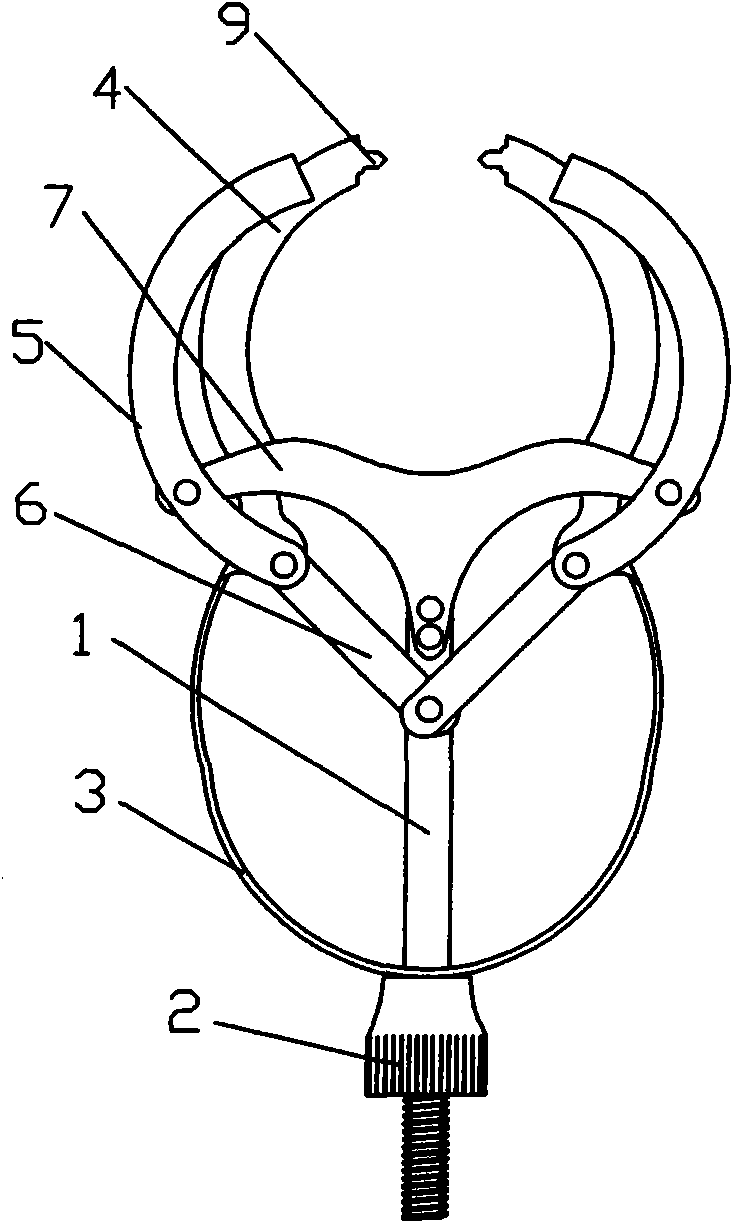
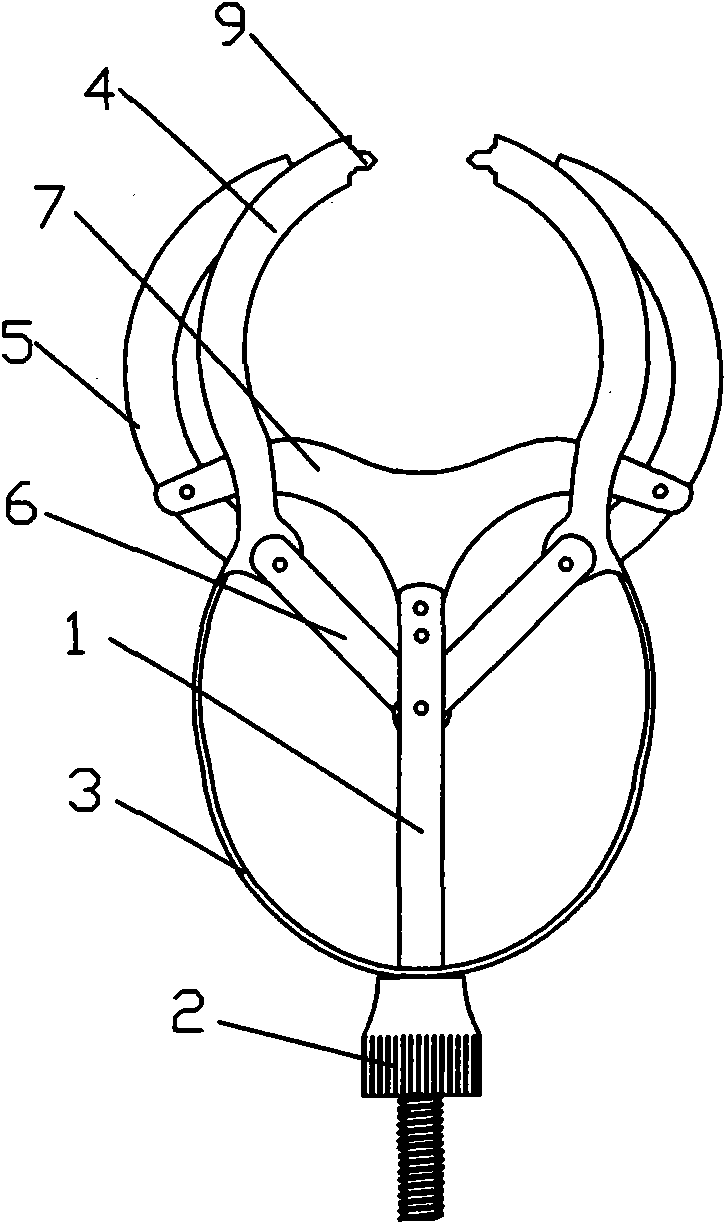
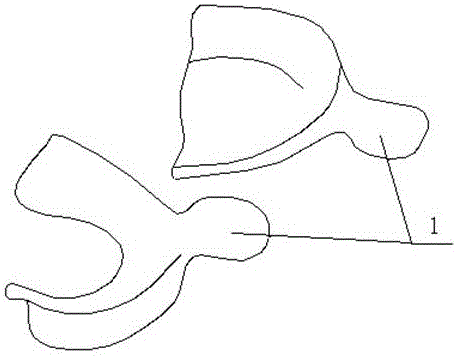
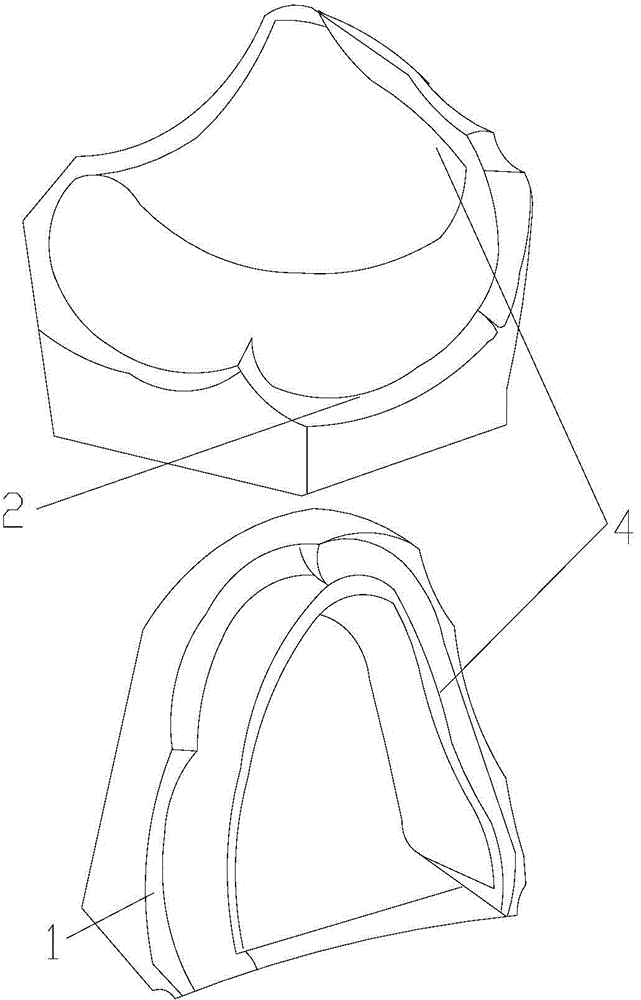
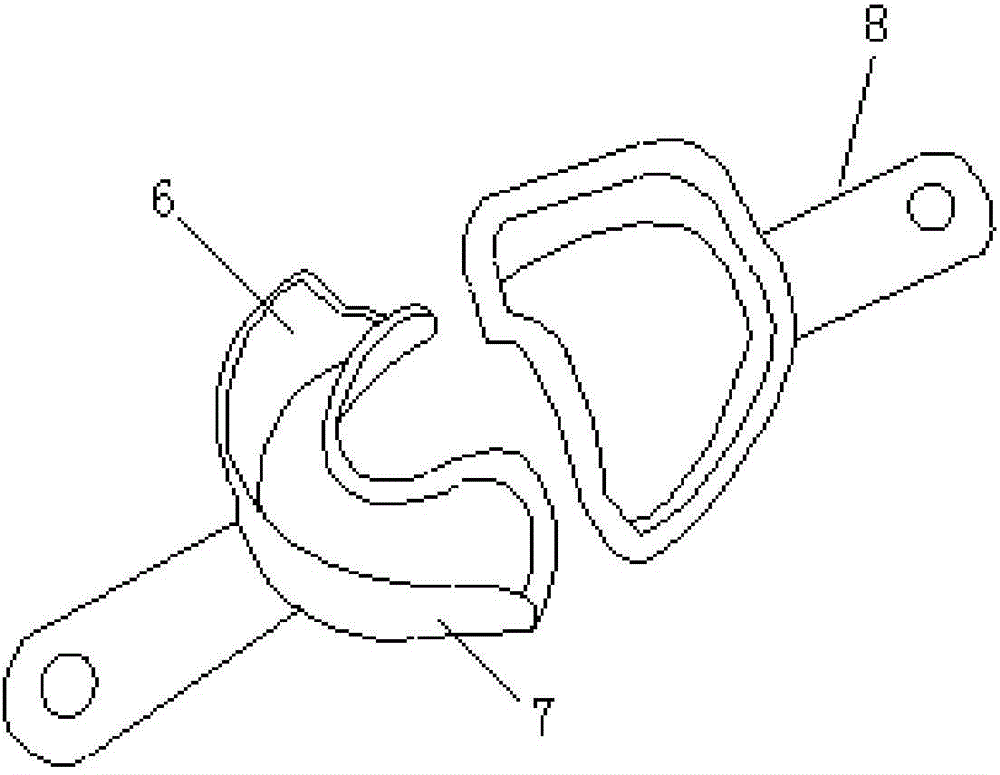
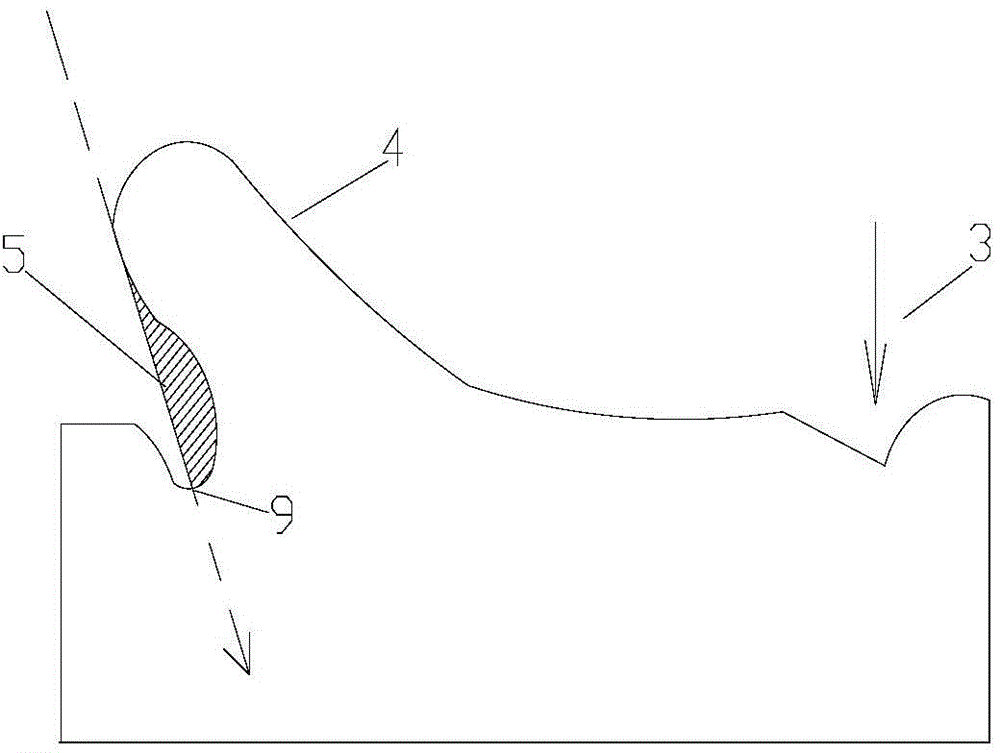
Mandibular gingival flap stretching fixation clamp
The invention relates to a mandibular gingival flap stretching fixation clamp which has simple structure, is convenient to use and is used in gingival flap implant operation. When in use, a left alveolar bone fixing arm and a right alveolar bone fixing arm clamp the alveolar bone from the left and right sides, a left gingival flap stretching arm and a right gingival flap stretching arm can move oppositely, gingival flap stretching plates on the left and right gingival flap stretching arms stretch the gingival flap to the left and right sides so that the surgical site on the top of the alveolar bone can be fully exposed for operation, the dental drill for holing and the implant can not contact the gingival soft tissue, and the soft tissue can not be carried into the cavity to affect synosteosis; and after the gingival flap is stretched by the stretching fixation clamp, the hands of the doctor can be free and the operation can be performed smoothly. The mandibular gingival flap stretching fixation clamp is mainly used to stretch and fix the gingival flap after gingival is flapped in the mandibular teeth implant operation and can also be used in the mandibular teeth alveolar ridge trimming and forming operation.
Owner:THE FIRST AFFILIATED HOSPITAL OF WENZHOU MEDICAL COLLEGE
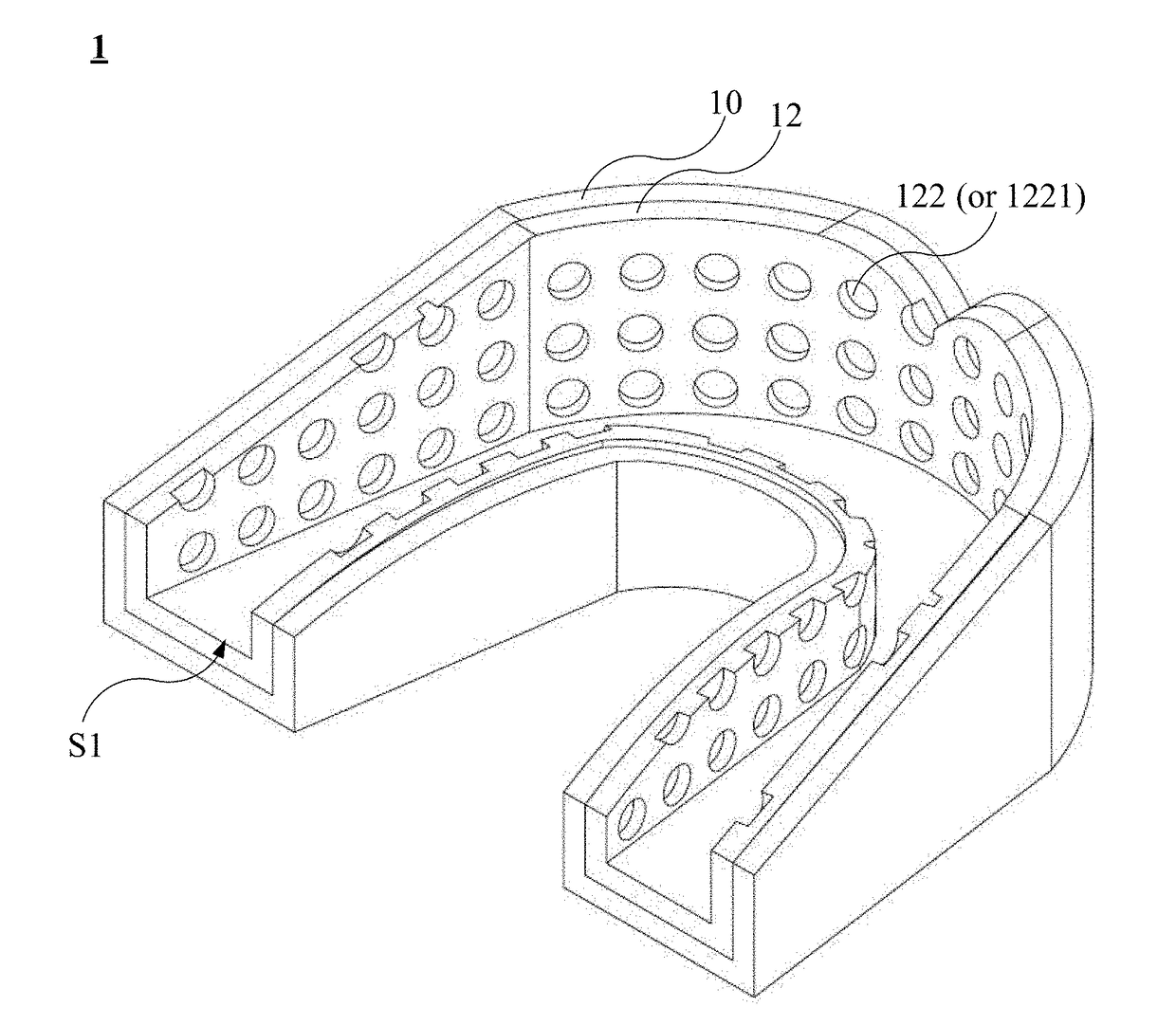
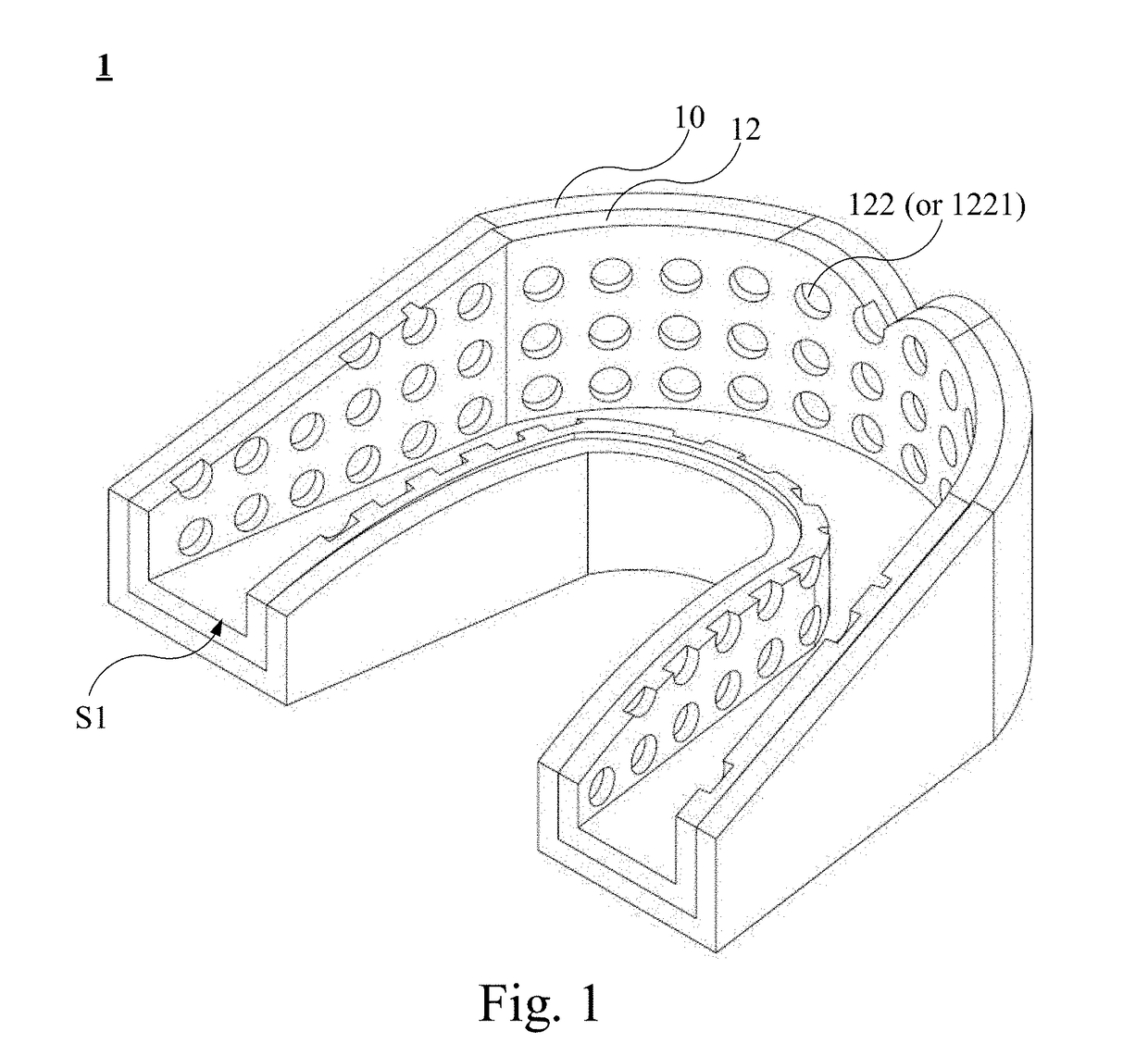
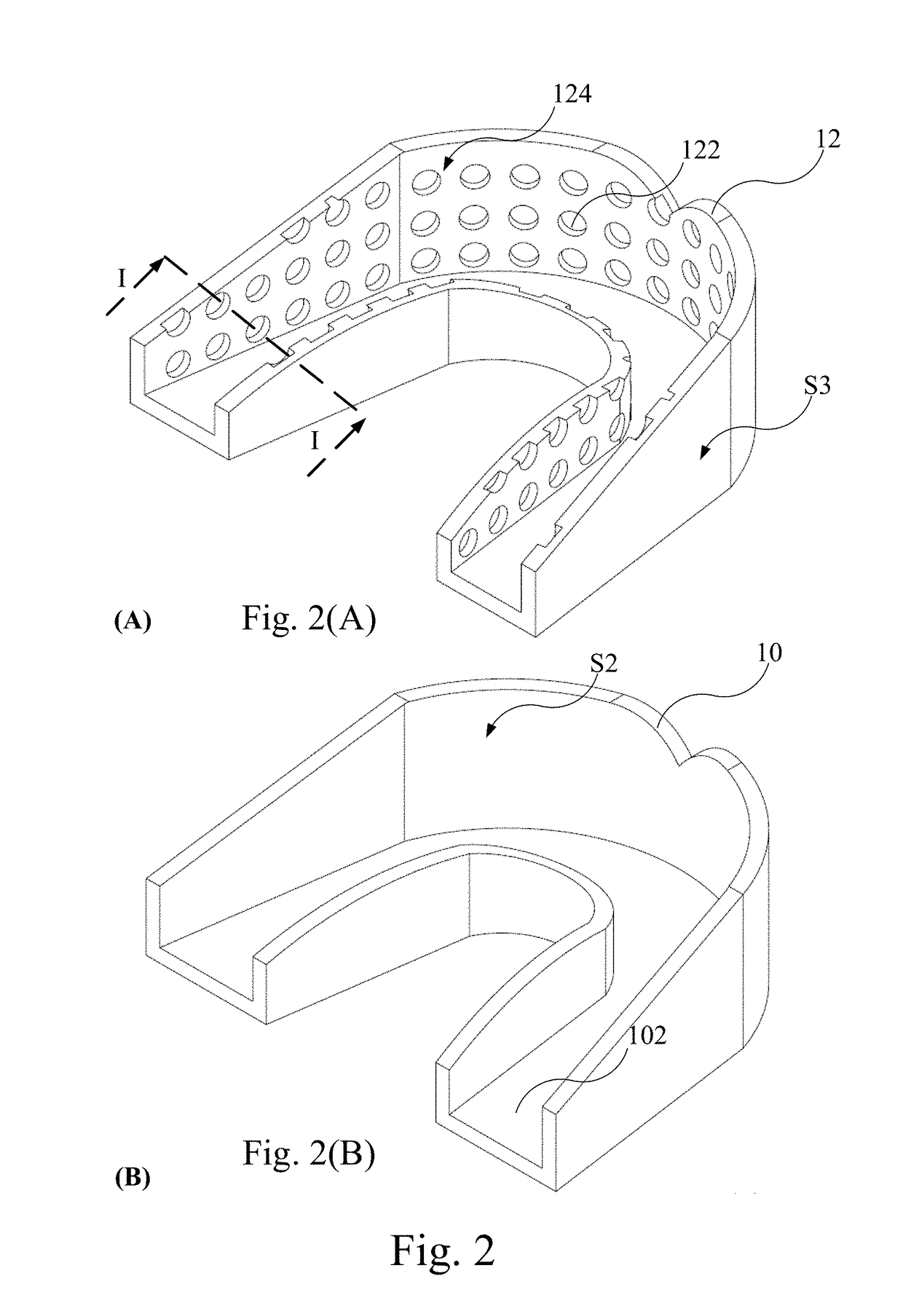
Dental Carrier
InactiveUS20170172717A1Improve fitnessHigh mechanical strengthImpression capsOthrodonticsPeriodontal tissueOrthodontic retainer
A dental carrier comprises a thermoplastic carrier. The thermoplastic carrier has a pattern structure. After heating the thermoplastic carrier, the thermoplastic carrier is provided with a user to be impressed by teeth or alveolar ridge for forming teeth or alveolar ridge model of the user. Compared to the prior art, the dental carrier of the present invention can provide the dental medicament contained in the pattern structure to be precisely applied and hold onto the treatment area and the medicament can be evenly coated on the teeth, root, or periodontal tissue for the treatment of teeth. When the dental carrier is not used to carry medicament, the pattern structure can improve the mechanical strength and fitness of the dental carrier to be used as a biteplate, orthodontic retainer, periodontal dressing for treatment or protection or mouth guard in sports.
Owner:TAIPEI MEDICAL UNIV +1
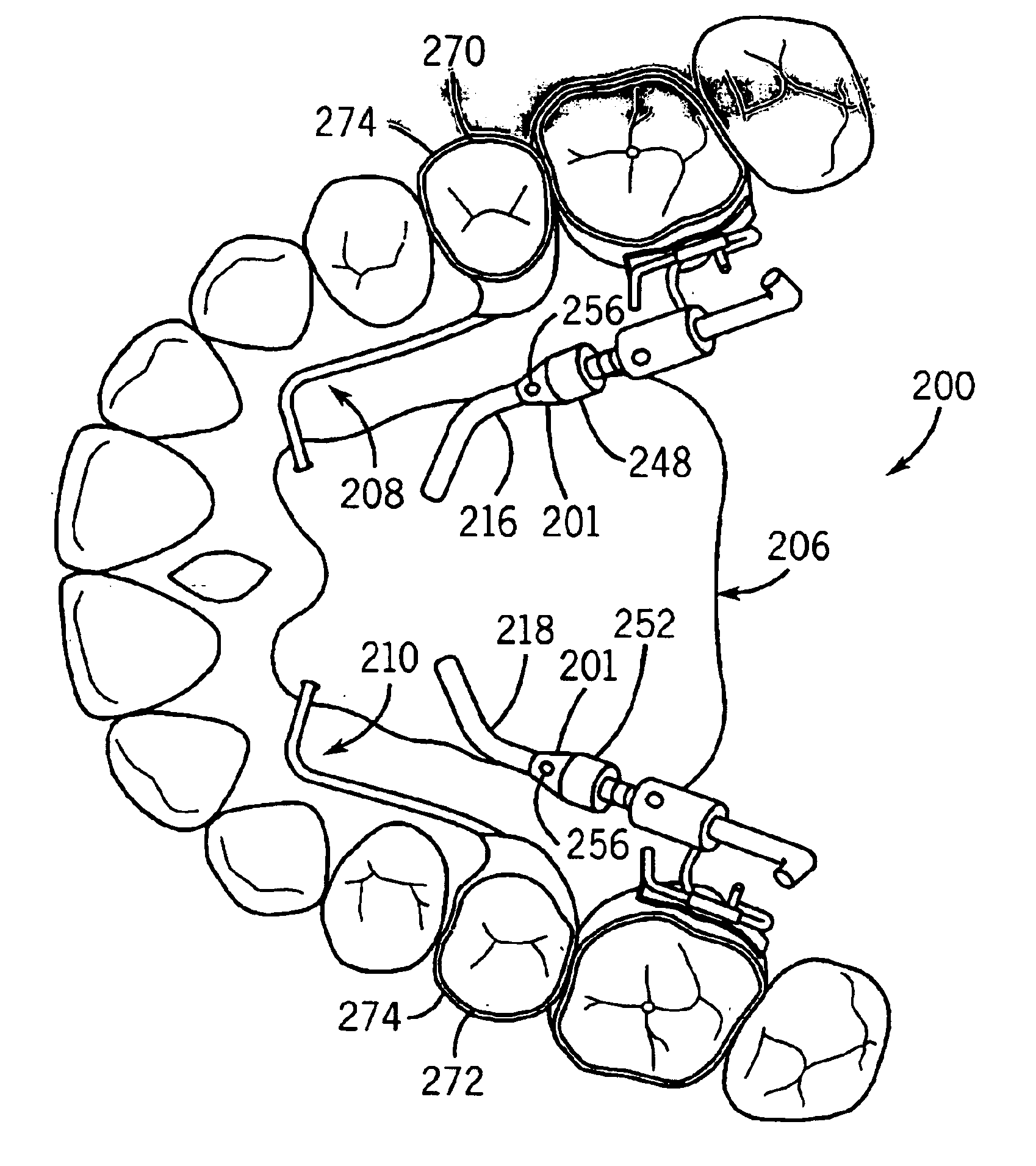
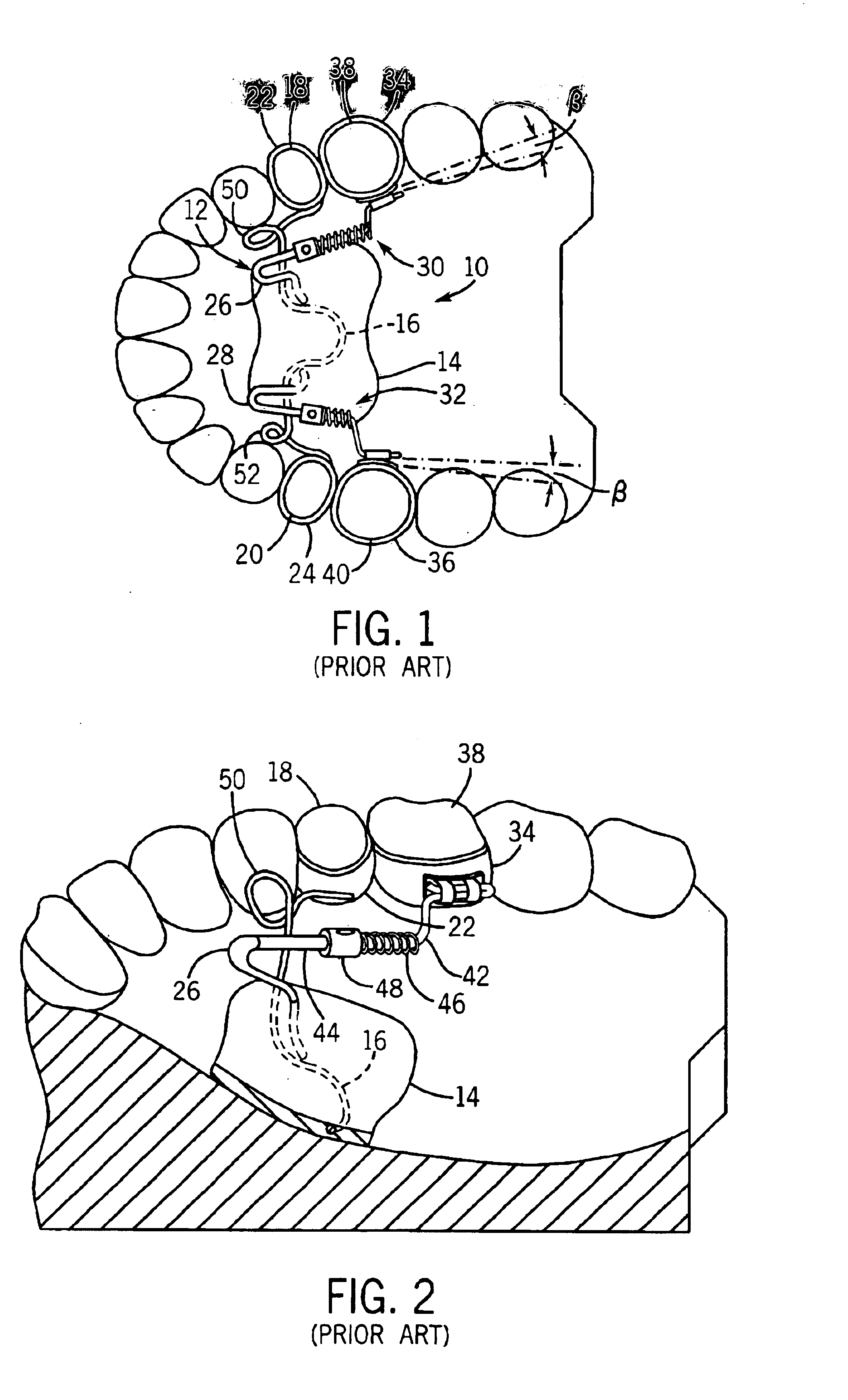
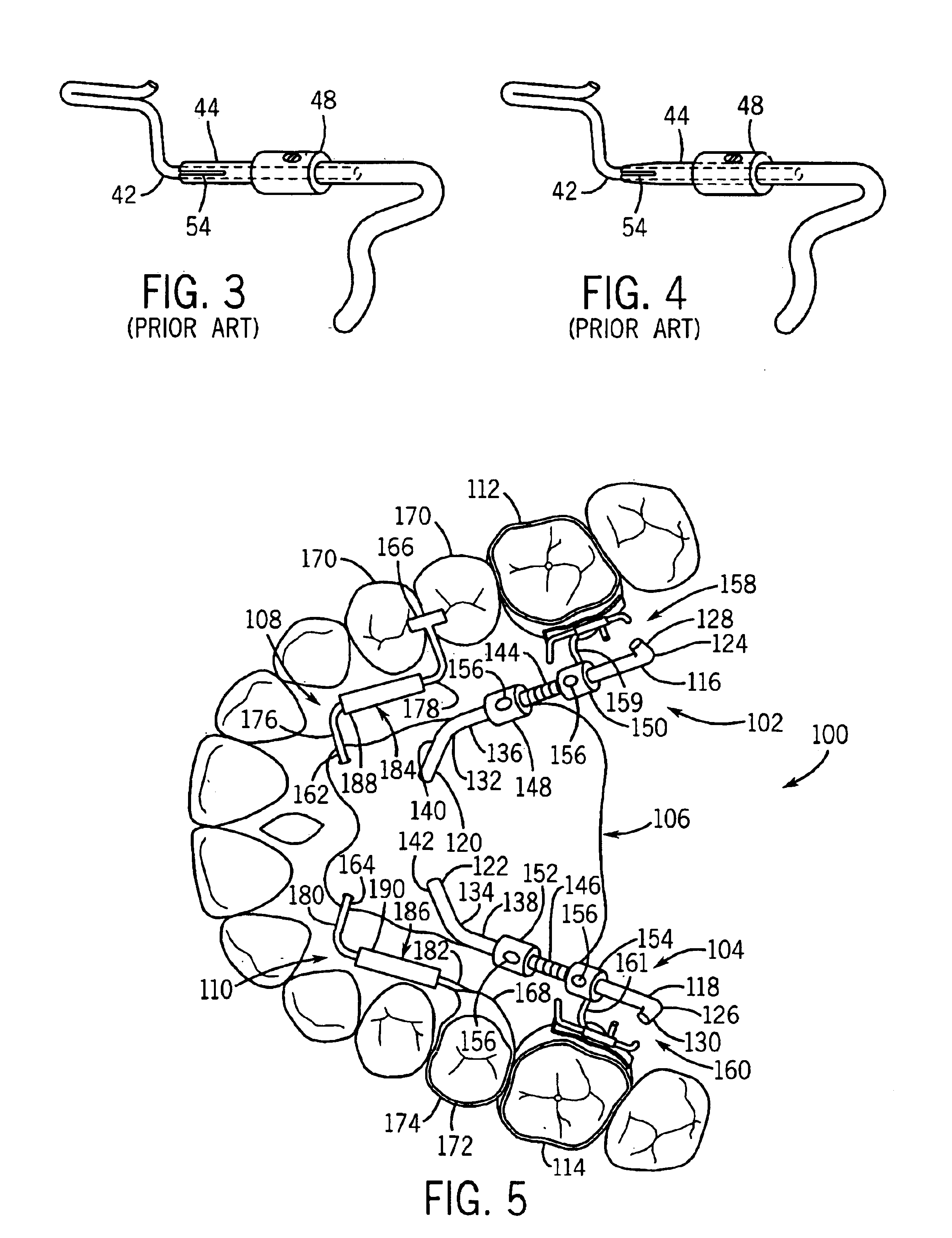
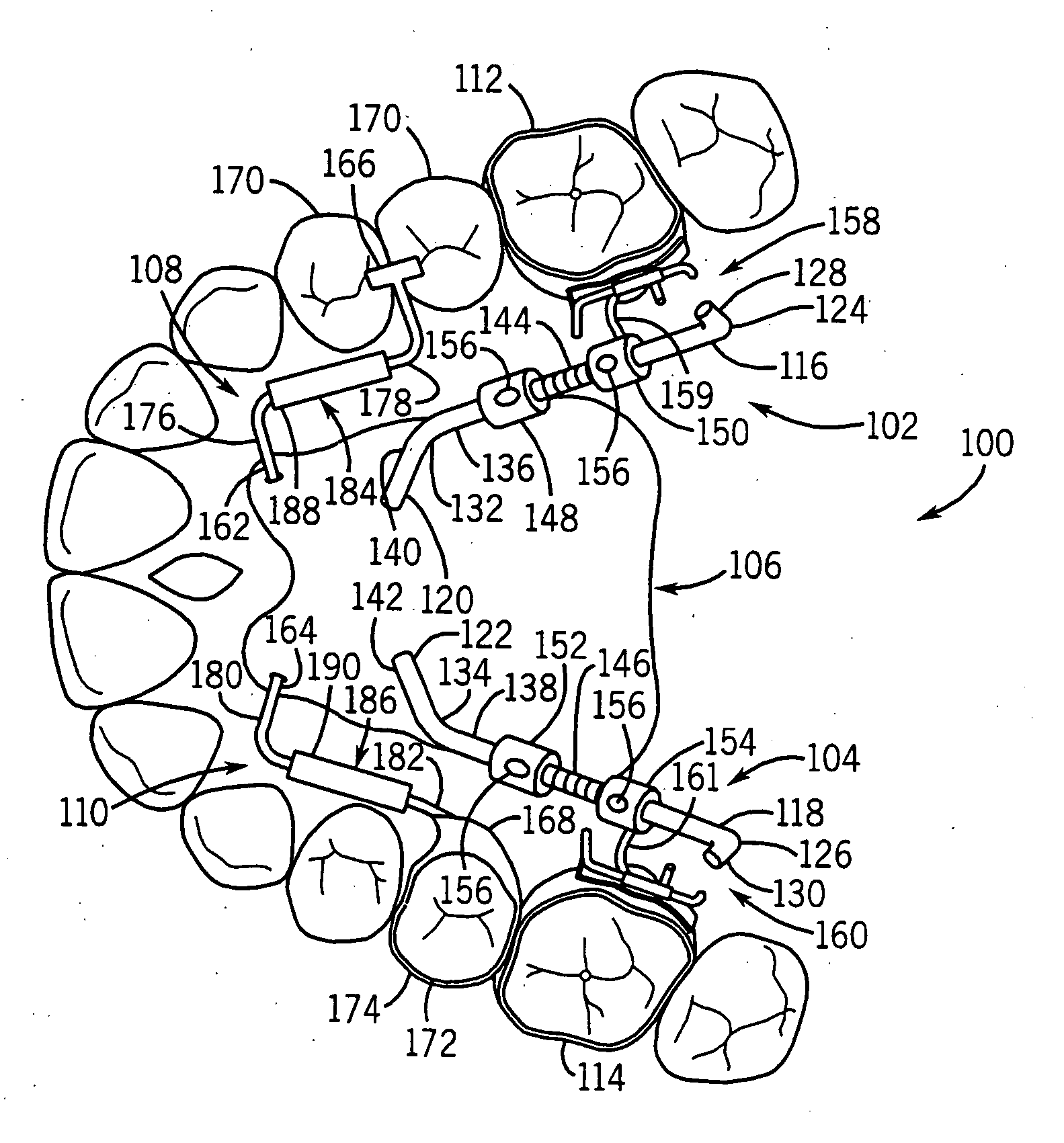
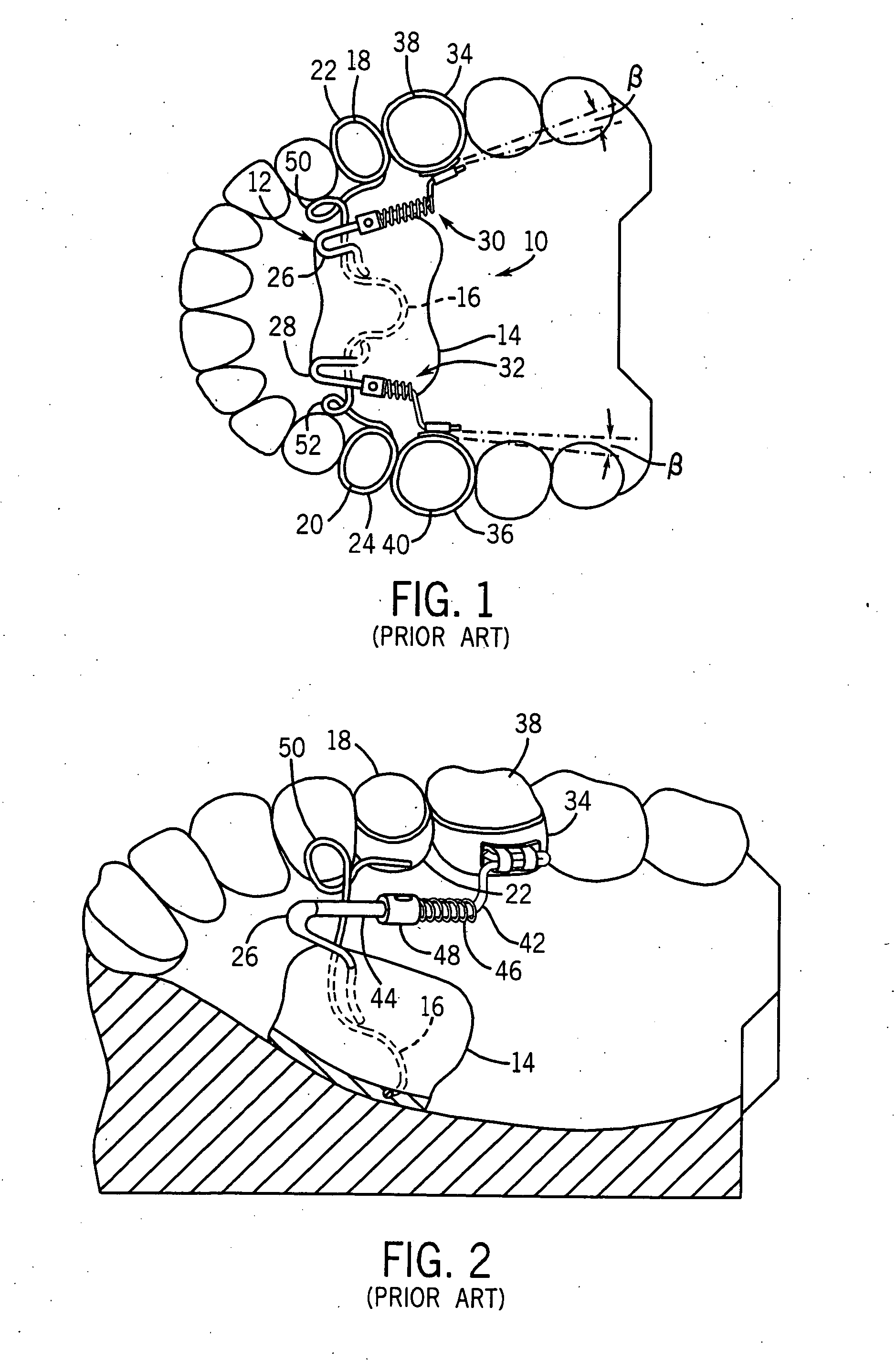
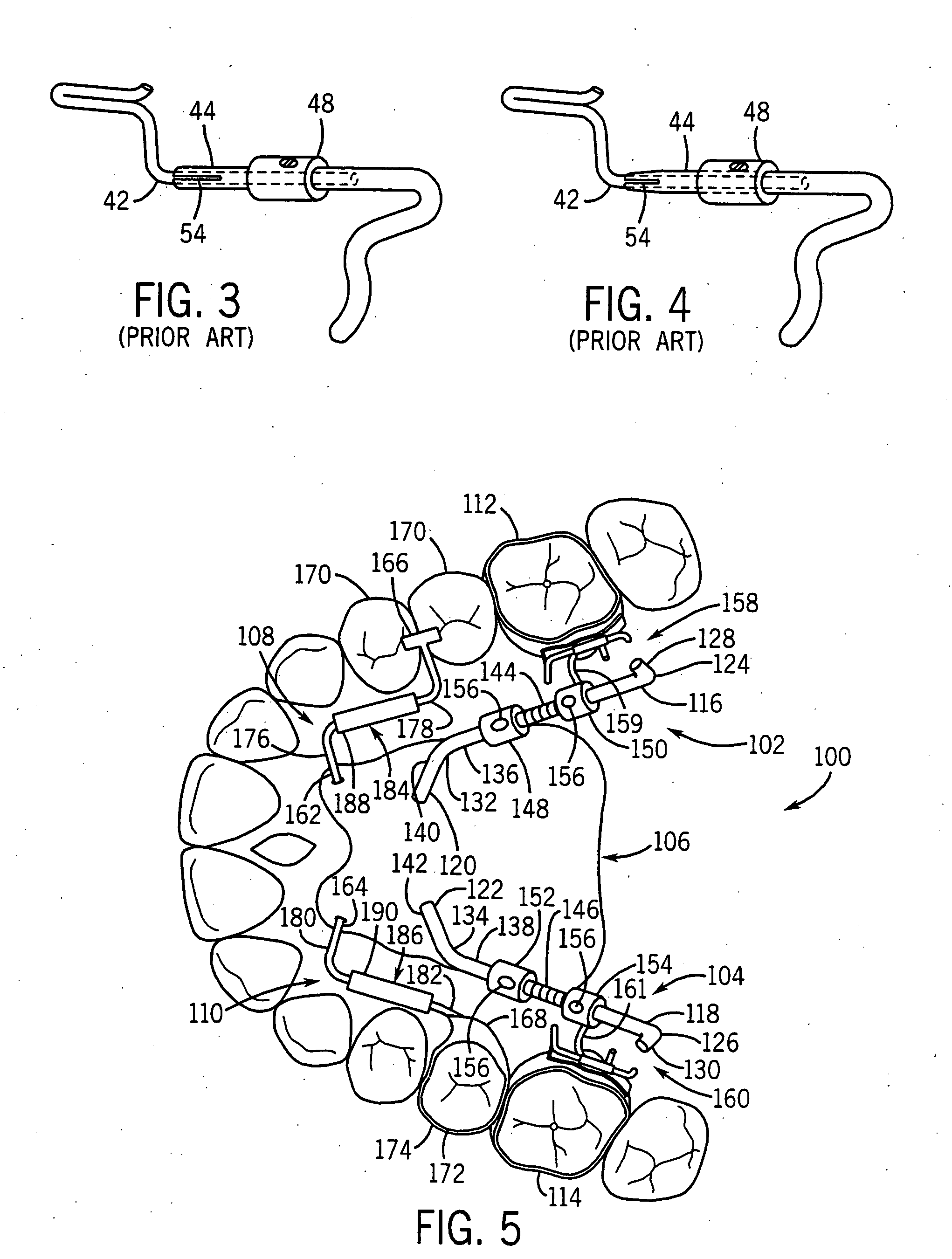
Orthodontic distalizing apparatus
An orthodontic distalizing apparatus comprises at least one force generating element positioned intermediate a force dissipating element secured to the hard palate and / or alveolar ridge and a first tooth (e.g., a molar) that is being distalized. The at least one force generating element is positioned to apply a distalizing force on the molar in a direction substantially along a longitudinal axis of the dental arch and at a low level of the basal gingiva. The at least one force generating element may be configured to prevent inadvertent disassembly thereof during installation, adjustment and / or conversion of the apparatus between an active and a passive state. In addition, the at least one force generating element may be configured to be reversibly convertible between an active state and a passive state without requiring removal of the device from the patient's mouth. Moreover, the at least one force generating element may be configured to provide a continuous activation force of substantially constant magnitude during distalization of the molar. The apparatus may also be constructed so that the force dissipating element is connected to at least one anchoring tooth by a slidable coupling that absorbs all reaction forces transmitted substantially along a direction of the longitudinal arch. A second force dissipating element may be positioned intermediate the force dissipating element and a second tooth (e.g., a bicuspid) to facilitate the closing of any gaps that are created following distalization of the molar. A method of converting an orthodontic distalizing apparatus between an active and a passive state is also provided.
Owner:AMERICAN ORTHODONTICS
Hydrogel sheets and shapes for oral care
InactiveUS20070122362A1Enhanced inhibitory effectReduce releaseCosmetic preparationsToilet preparationsCross-linkBeam energy
A hydrogel for use in oral care. The hydrogel is ion beam cross-linked, the hydrogel is adapted to be disposed in the oral cavity and may be adapted to provide a denture fixative or may be loaded with a whitening agent for use in whitening one or more teeth and disposed on or adjacent one or more teeth and the whitening agent is slow-released to whiten the one or more teeth. Other loading materials may include materials for treatment of alveolitis or malodor, inter alia. The present invention is a new hydrophilic oral and dental cohesive hydrogel sheet designed to securely grip and cushion prosthetic devices in the human mouth with the further ability to slow release antimicrobial or other orally desirable agents. Additionally, the invention also provides a method of making an orally cohesive device that: 1) is easily adapted and applied to a removable dental prosthesis; 2) bonds well to alveolar ridge / palatal mucosa and denture acrylic materials; and 3) releases cleanly, with no tacky or thixotropic residue when the prosthesis is removed. The cohesive hydrogel gel device is a hydrogel-forming polymer mixed with water, optionally surrounding an internal scrim, and uses an electron-beam energy source to cause cross-linking. The method does not need any chemical additive to affect the cross-linking. Furthermore the beam energy can be adjusted to optimize the cohesive properties of either side of the device, as well as to compensate for addition of orally active agents, if any are chosen. The hydrogel sheets are pre-cut to fit most sizes of maxillary and mandibular full denture prostheses, but can be easily trimmed with a scissors by the end user for the ideal custom fit of any full or partial denture, in either arch.
Owner:GINIGER MARTIN S +1
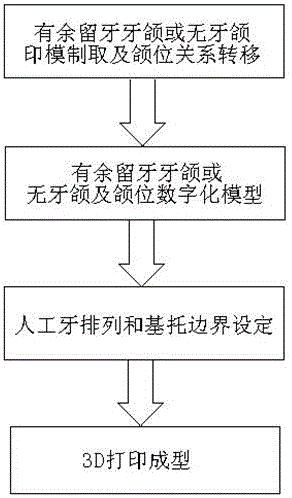
Method for producing immediate complete or half denture based on 3D printing technique
ActiveCN106037967AComfortable to wearSimple preparation steps3D printingDental prostheticsDenture baseBite registration
The invention discloses a method for producing an immediate complete or half denture based on a 3D printing technique. The method comprises the steps of preparing an impression with a remaining tooth jaw or a tooth-free jaw, transferring a jaw position relation, acquiring digital models of the remaining tooth jaw or the tooth-free jaw and the jaw position relation, setting the arrangement and the denture border of artificial teeth of the immediate complete or half denture corresponding to the form of the remaining tooth jaw or the tooth-free jaw and the jaw position relation, invoking data in a preset database, designing the artificial teeth and polishing surfaces of the artificial teeth, regulating the occlusion of the teeth to enable alveolar ridge supporting tissues to bear proper pressure distribution, and manufacturing a three-dimensional model of the immediate complete or half denture by virtue of a photo-healing three-dimensional printing technique in the 3D printing technique. The method has the advantages that the production steps are simple, the production time is short, the precision is high, the denture can be conformably worn by a patient, and meanwhile, the production cost is lowered.
Owner:AFFILIATED STOMATOLOGICAL HOSPITAL OF NANJING MEDICAL UNIV
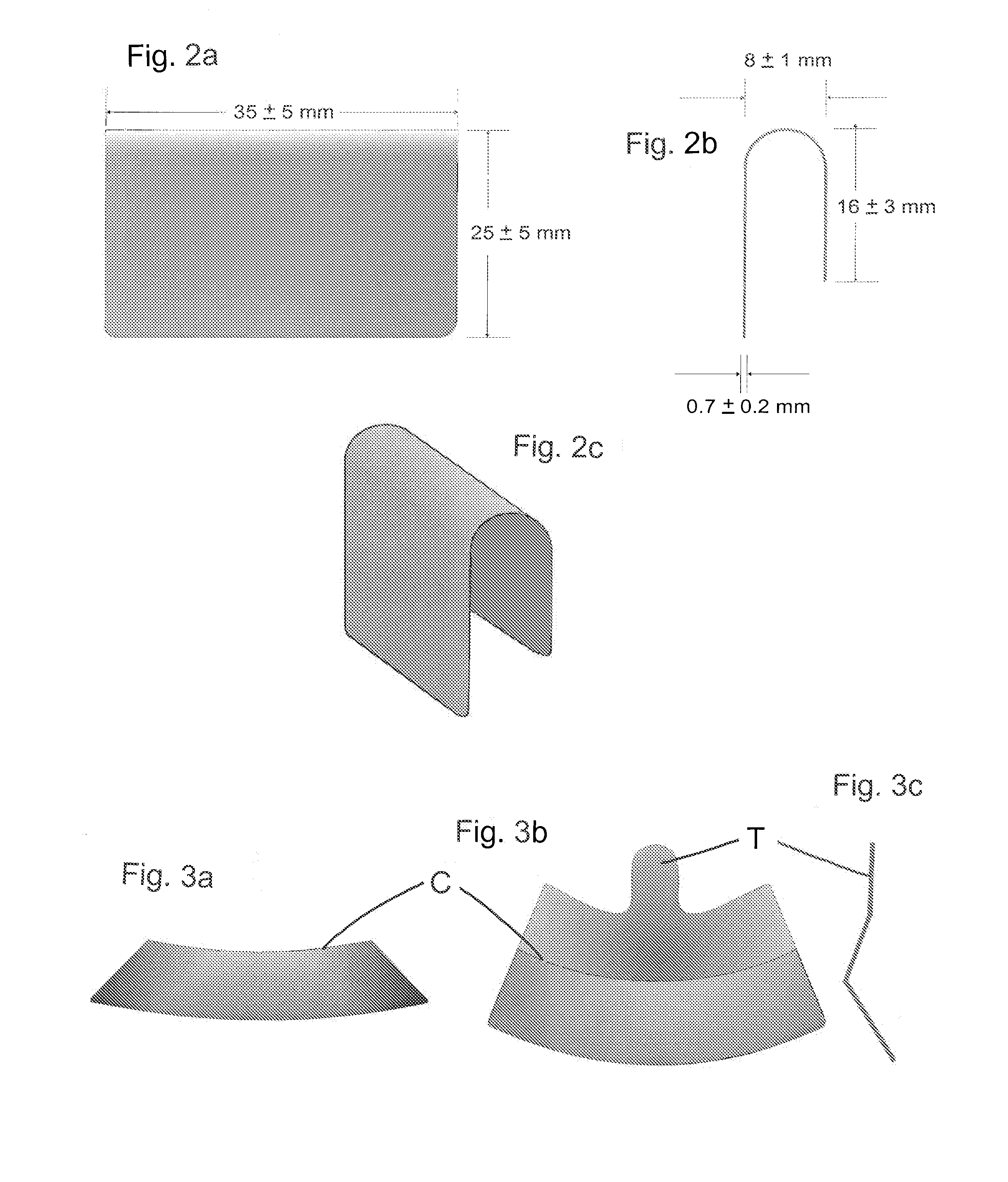
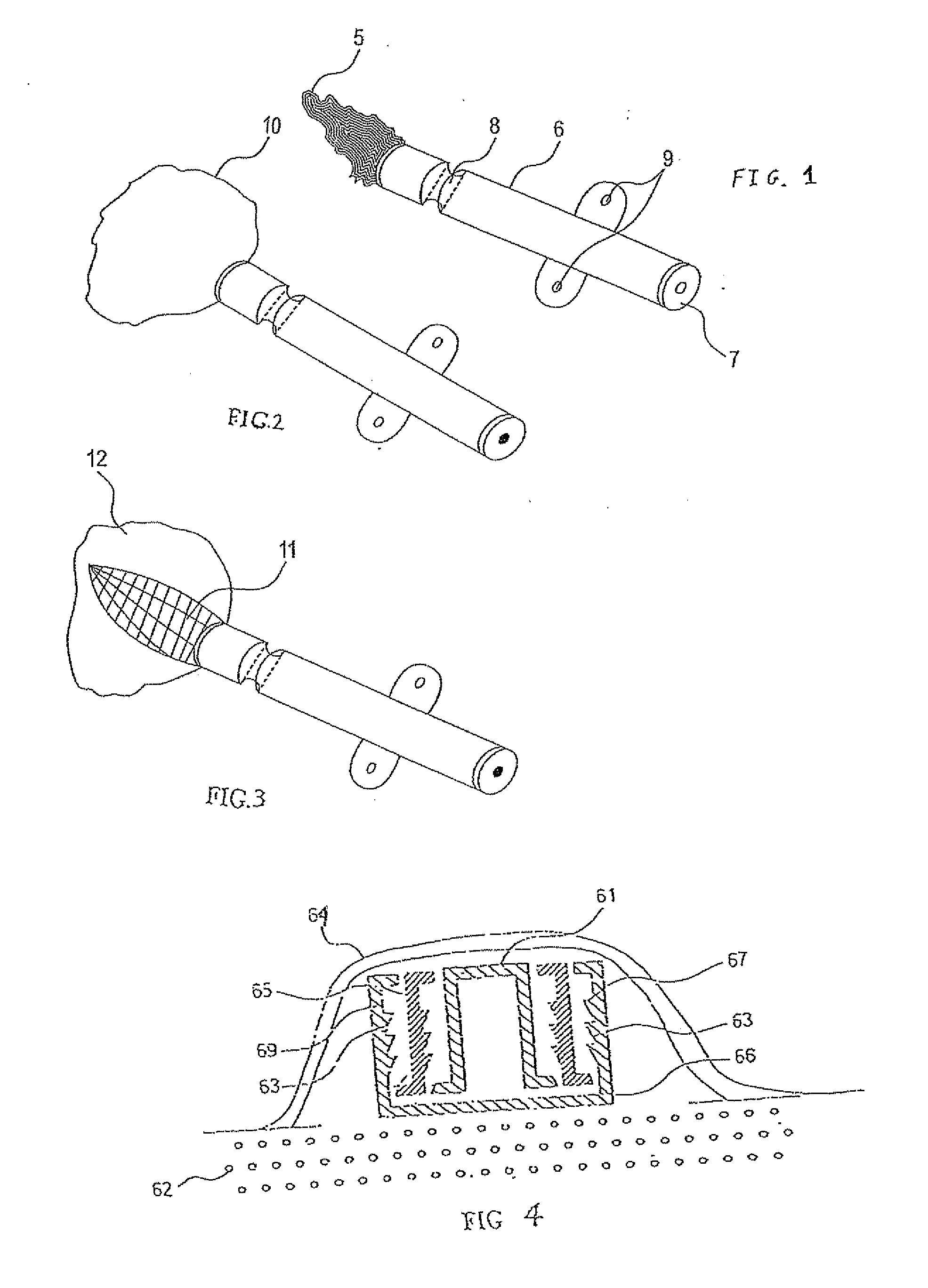
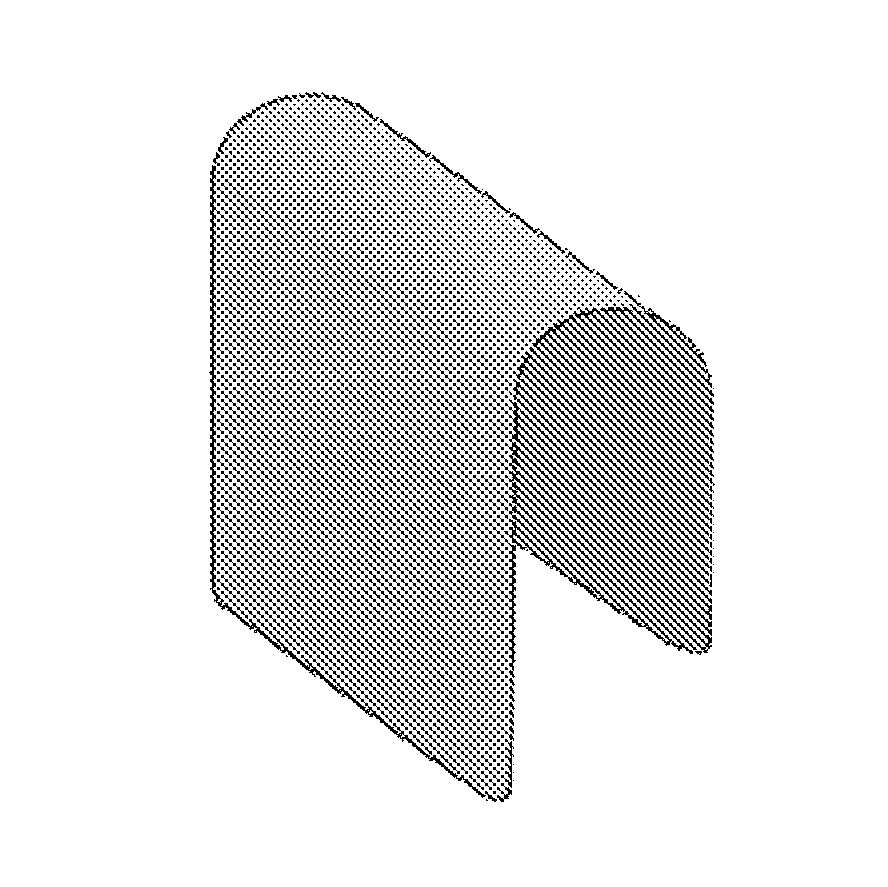
Self-Supporting Collagen Tunnel for Guided Tissue Regeneration and Method of Using Same
InactiveUS20110035024A1Stronger/stifferHigh strengthBiocidePeptide/protein ingredientsIliac screwBiomedical engineering
Owner:CARDOSO RONALD
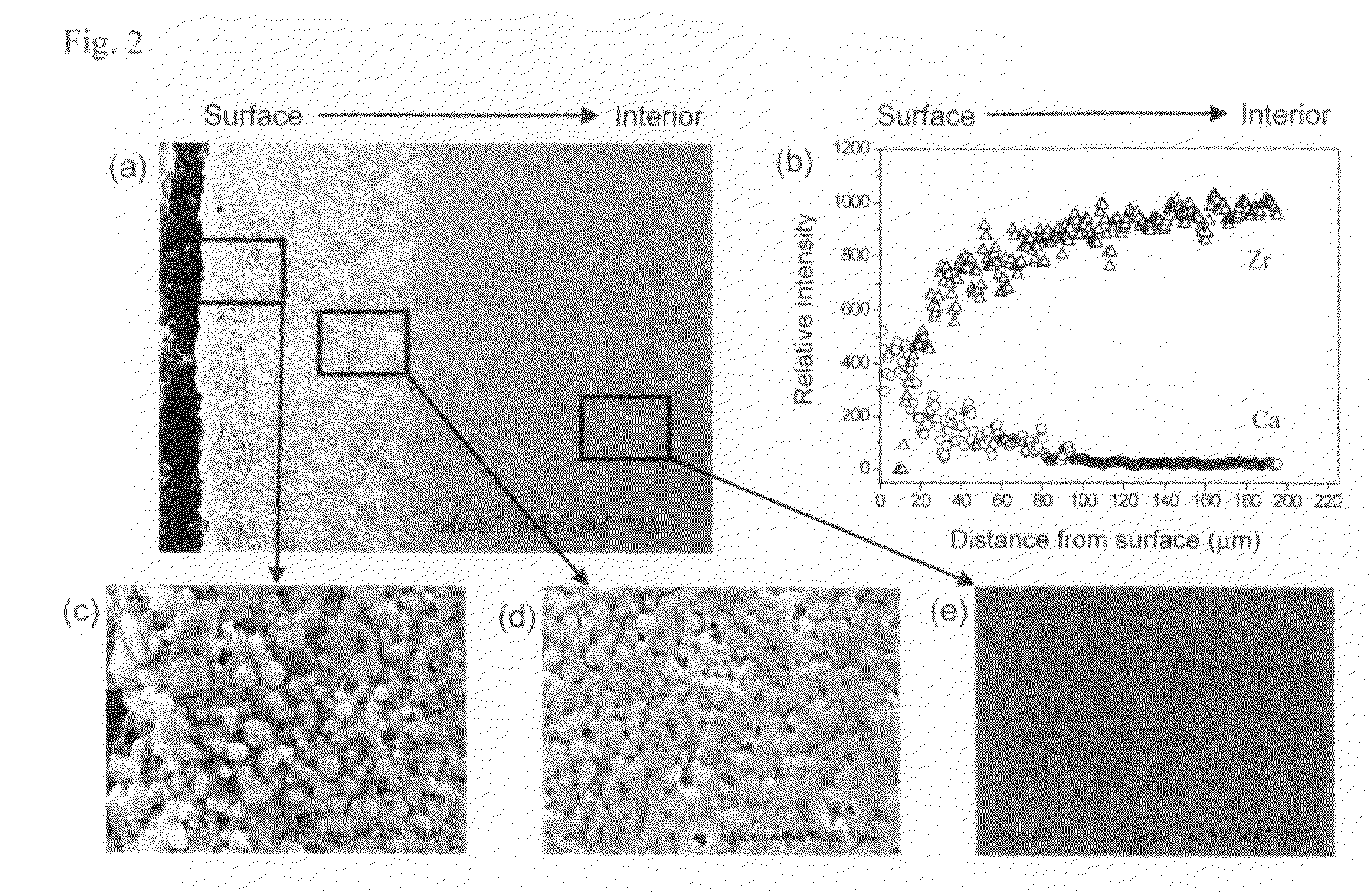
Bioactive graded zirconia-based structures
The present invention provides a functionally graded bioactive glass / ceramic composite structure or bioactive glass / ceramic / bioactive glass sandwich structure for use in such applications as damage resistant, ceramic dental implants, immediate tooth replacement, endodontic posts, orthopedic prostheses, orthopedic stems, bone substitutes, bone screws, plates, and anchors, nonunion fractures repair, alveolar ridge augmentation, missing small bone parts (e.g. fingers, toes, etc), maxilla facial reconstruction, spinal fusion, and scaffolds for bone regeneration, comprising a residual bioactive glass or glass-ceramic layer at all accessible surfaces, followed by an underlying graded glass-ceramic layer, and then an dense interior ceramic. The residual bioactive glass or glass-ceramic layer can be further transformed to a carbonate apatite (CHA) layer by immersing in calcifying solution or simulated body fluid (SBF) with electrolyte composition similar to that of serum. The interior ceramic preferably contains yttria-tetragonal zirconia polycrystal (Y-TZP) or ceria stabilized tetragonal zirconia polycrystal (Ce-TZP) or magnesia stabilized zirconia (Mg-PSZ) or calcia stabilized zirconia (Ca-PSZ) or alumina or zirconia-alumina composites. Further, the invention provides methods for making the same functionally graded bioactive glass / ceramic composite structure or graded bioactive glass / ceramic / bioactive glass sandwich structure.
Owner:NEW YORK UNIV
Expandable devices and methods for tissue expansion, regeneration and fixation
InactiveUS20100266979A1Less fear of punctureLess fear of leakageDental implantsInternal osteosythesisFilling materialsTissue expansion
A device which allows the insertion of a flowable filling material through at least part of a dental implant inside the body to touch the bone. The implant can be hollow and to have a side perforation connecting the space inside the implant with the surrounding of the implant. This perforation can be placed initially outside the alveolar ridge. The device can allow immediate direct contact between the filling material and the tissue and for the displacement of the soft tissues covering the bone.
Owner:KARMON BEN ZION
Method for enlarging a jaw bone using a hollow dental implant having a side perforation
InactiveUS8622739B2High viscous or rigid substanceDirect contact guaranteeDental implantsInternal osteosythesisJaw boneDental implant
A method for inserting a flowable material adjacent the alveolar ridge bone through an elongated tube having an a side perforation. The elongated tube can be a dental implant.
Owner:KARMON BEN ZION
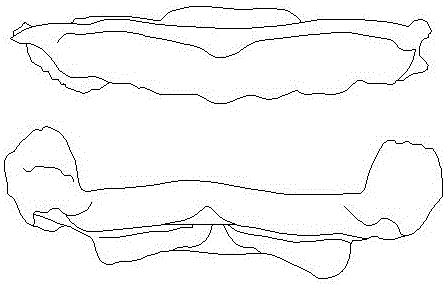
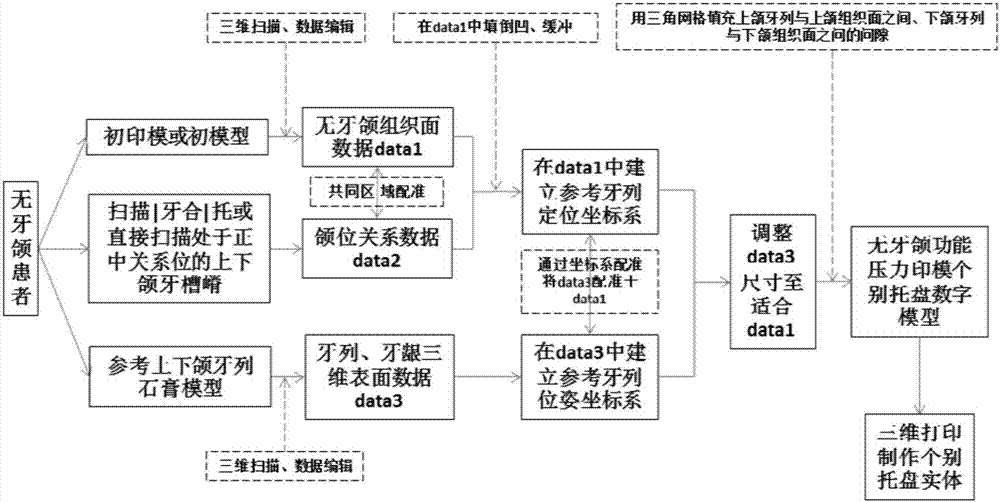
Digital preparation method of edentulous jaw individual impression tray
ActiveCN105078598AImproving the technical level of clinical treatment operationImprove the efficiency of diagnosis and treatmentImpression capsPoint cloudImpression trays
The invention relates to a digital preparation method of an edentulous jaw individual impression tray. The method comprises the following steps: preparing a preliminary impression, or forming a plaster model by pouring; scanning the preliminary impression or scanning the plaster model; introducing scanning data into reverse engineering software and intercepting tissue surface point cloud data of the edentulous jaw preliminary impression; acquiring point cloud data of undercut-free alveolar ridge surface; uniformly enlarging the alveolar ridge surface by 1-2mm in the normal direction of the alveolar ridge surface so as to obtain a virtual tray inner surface; uniformly thickening the virtual tray inner surface by 2mm in the normal direction thereof; designing an upper jaw virtual tray handle and a lower jaw virtual tray handle; and fusing data boundaries of the inner and outer surfaces of the virtual tray as well as the handle and saving the data in an STL format, importing the data into a computer system connected to 3D printing equipment, and making the edentulous jaw individual impression tray from a polymethyl methacrylate (PMMA) material by virtue of the 3D printing equipment. The digital designing and manufacturing method of the edentulous jaw individual impression tray can replace traditional hand-made manufacturing method.
Owner:PEKING UNIV SCHOOL OF STOMATOLOGY
Digital designing and making method of individual tray without edentulous jaw function pressure
ActiveCN107198586AImproving the technical level of clinical treatment operationImprove the efficiency of diagnosis and treatmentImpression capsEngineeringDentition
The invention relates to a digital designing and making method of an individual tray without edentulous jaw function pressure. The method includes: making an edentulous jaw preliminary impression; scanning the impression or a model to obtain data 1; scanning alveolar ridges of upper and lower jaws to obtain jaw position relation data 2; registering the data 1 to the data 2; completing undercut filling and buffering on the surfaces of the alveolar ridges of the upper and lower jaws; creating a dentition positioning coordinate system in the data 1; scanning a pair of upper-lower jaw dentition reference gypsum models to acquire data 3; creating a dentition posture coordinate system in the data 3; registering the data 3 to the data 1 through coordinate system registering; using a triangular grid to fill gaps between upper and lower jaw data 1 and the data 3 to acquire STL data of the individual tray; printing upper-lower jaw trays. The method replaces complex steps of conventional manual making, clinical operation steps are simplified, operation difficulty is lowered, and clinical diagnosis and treatment efficiency of edentulous jaw complete denture repair is improved.
Owner:PEKING UNIV SCHOOL OF STOMATOLOGY
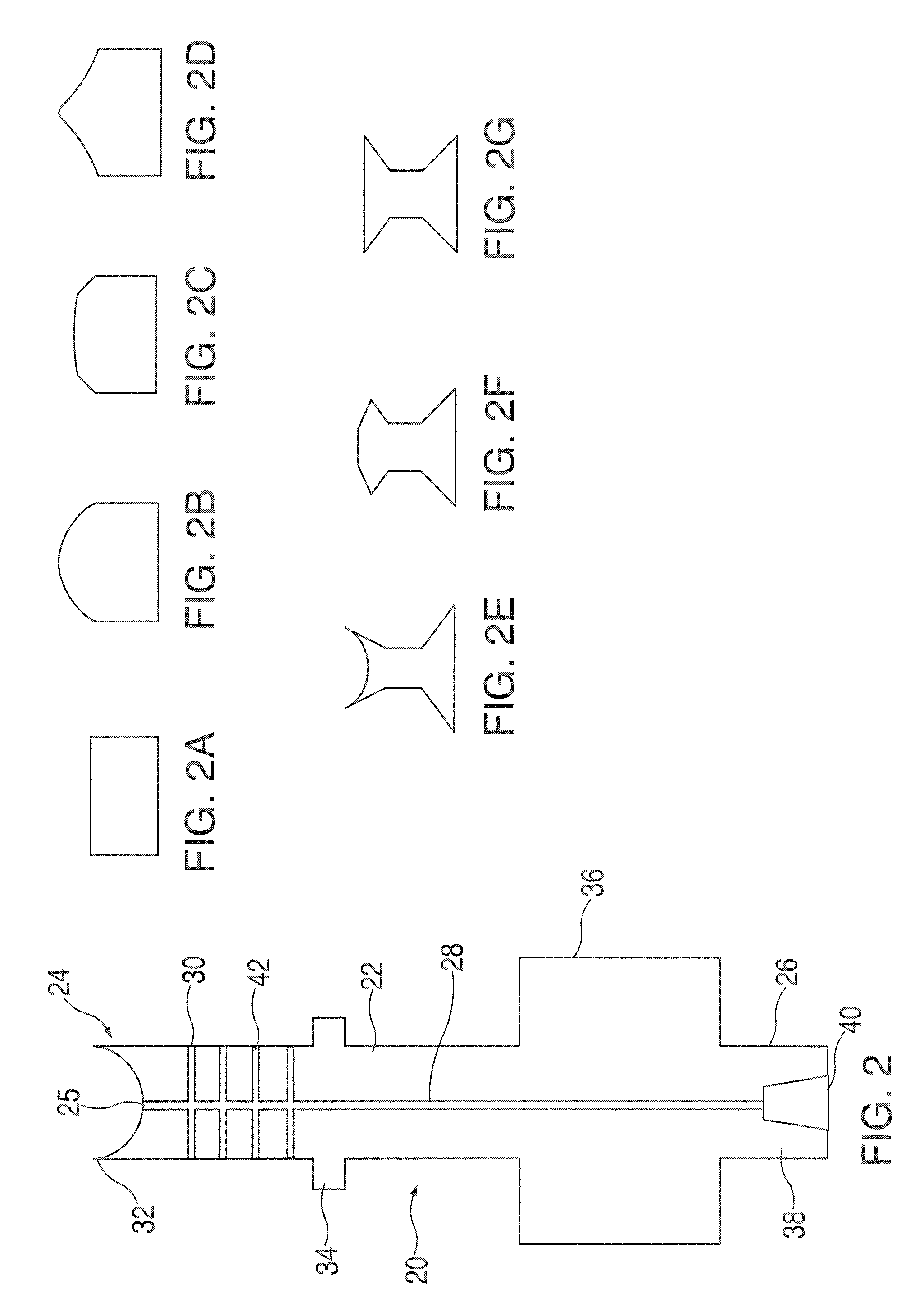
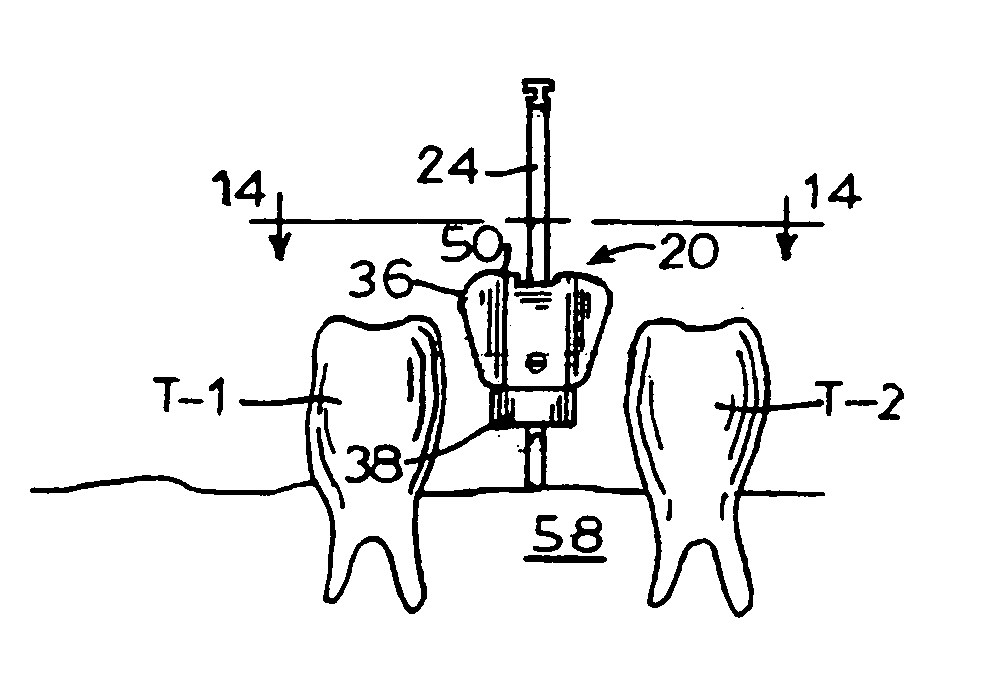
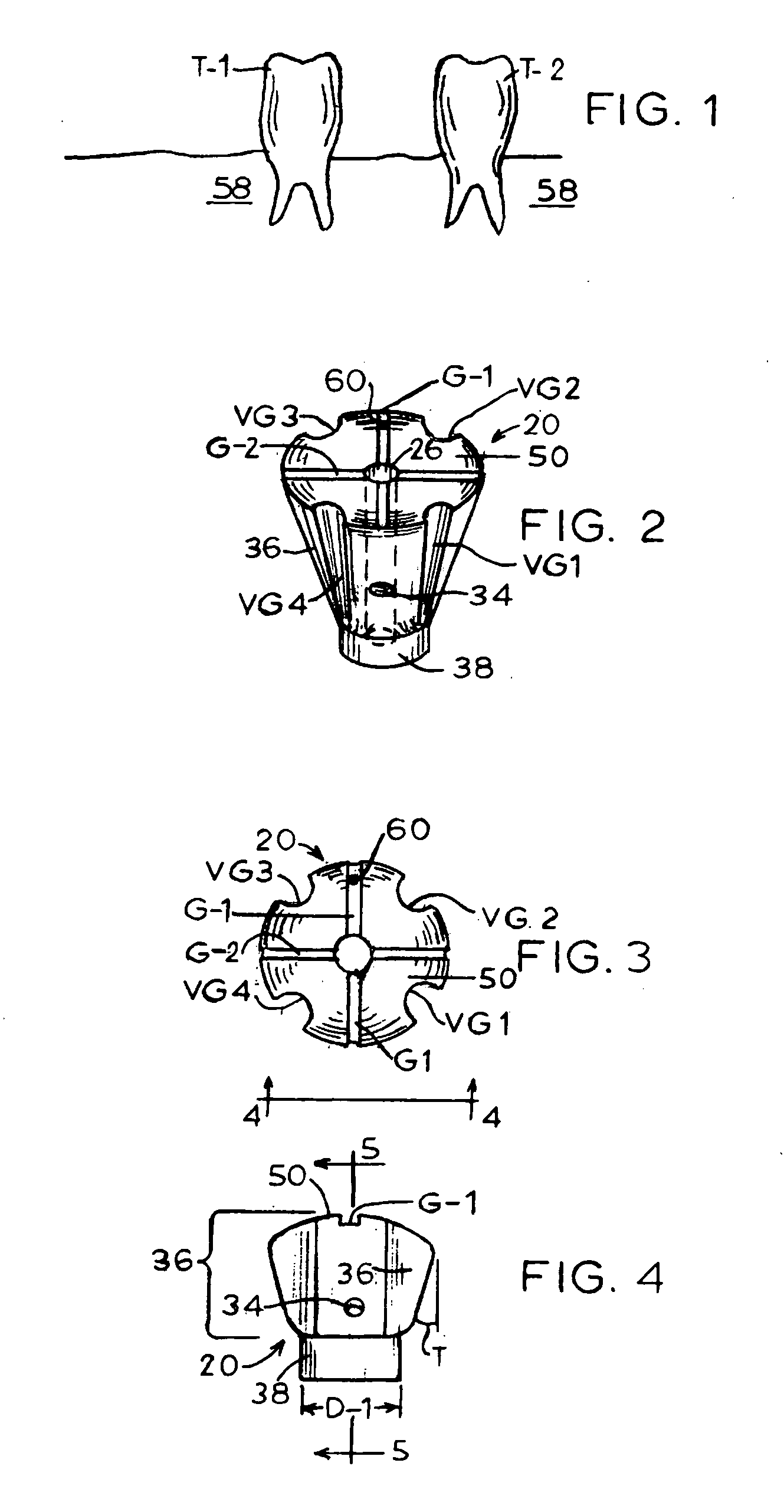
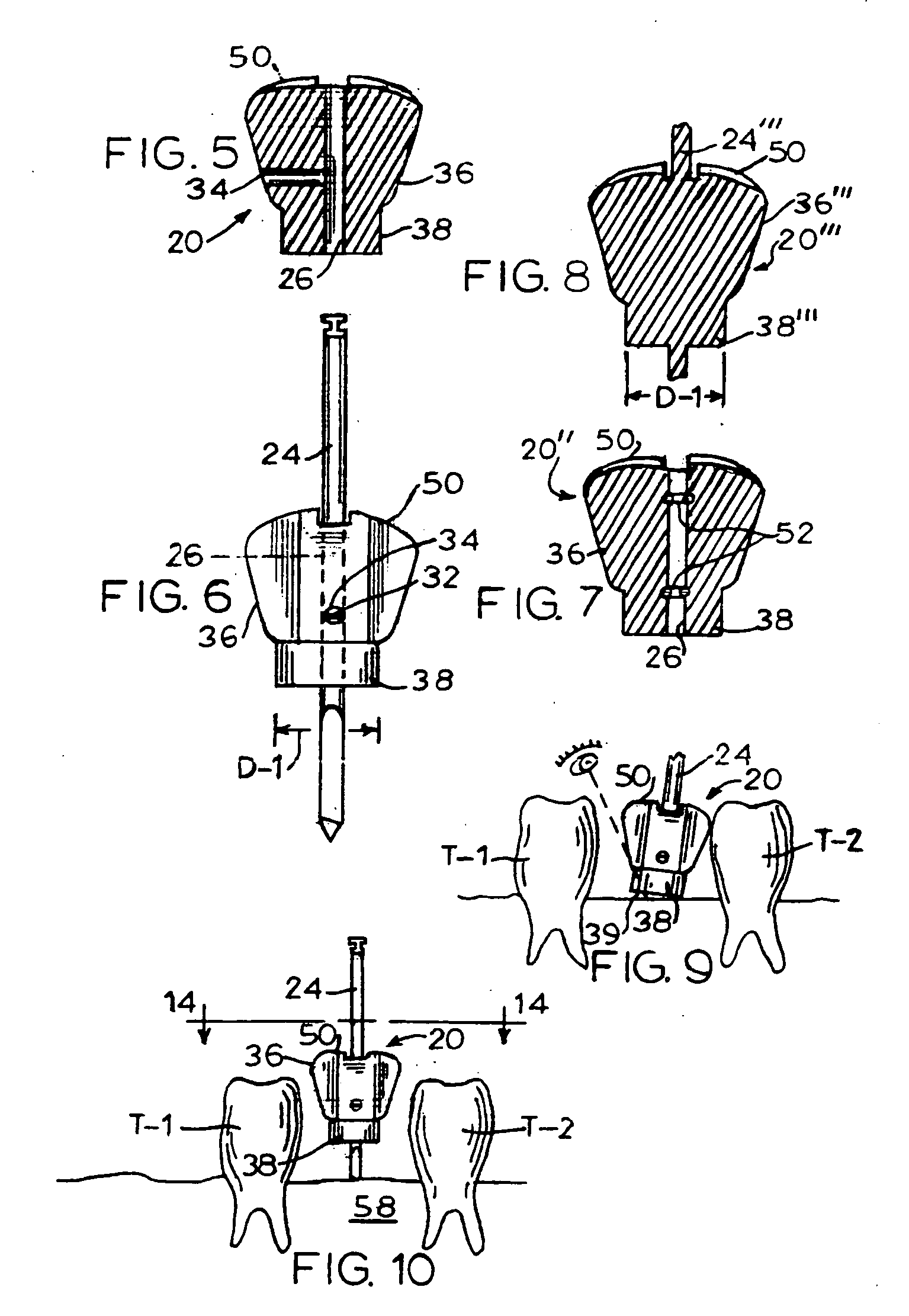
Dental implant drill apparatus and method
InactiveUS20090286201A1Effectively “ see ”Easy to drillDental toolsBoring toolsDenturesVisual comparison
A device is operatively associated with a drill used in connection with forming a hole in which a dental implant is to be installed. The device is made in multiple sizes suitable for accommodating differences in spacing between existing teeth between which one or more new prosthetic teeth are to be installed as well as accommodating differences in the bucco-lingual alveolar ridge width and the mesio-distal alveolar ridge length between the existing teeth where the implant is to be installed. The device is formed in such a way as to aid correct placement of the dental drill during implant surgery. The device permits the size of the proposed implant to be evaluated by visual comparison with the size of the selected implant site. The device further permits locating the dental implant pilot drill correctly so as to achieve successful implant placement.
Owner:CHOE MIKE WANSIK
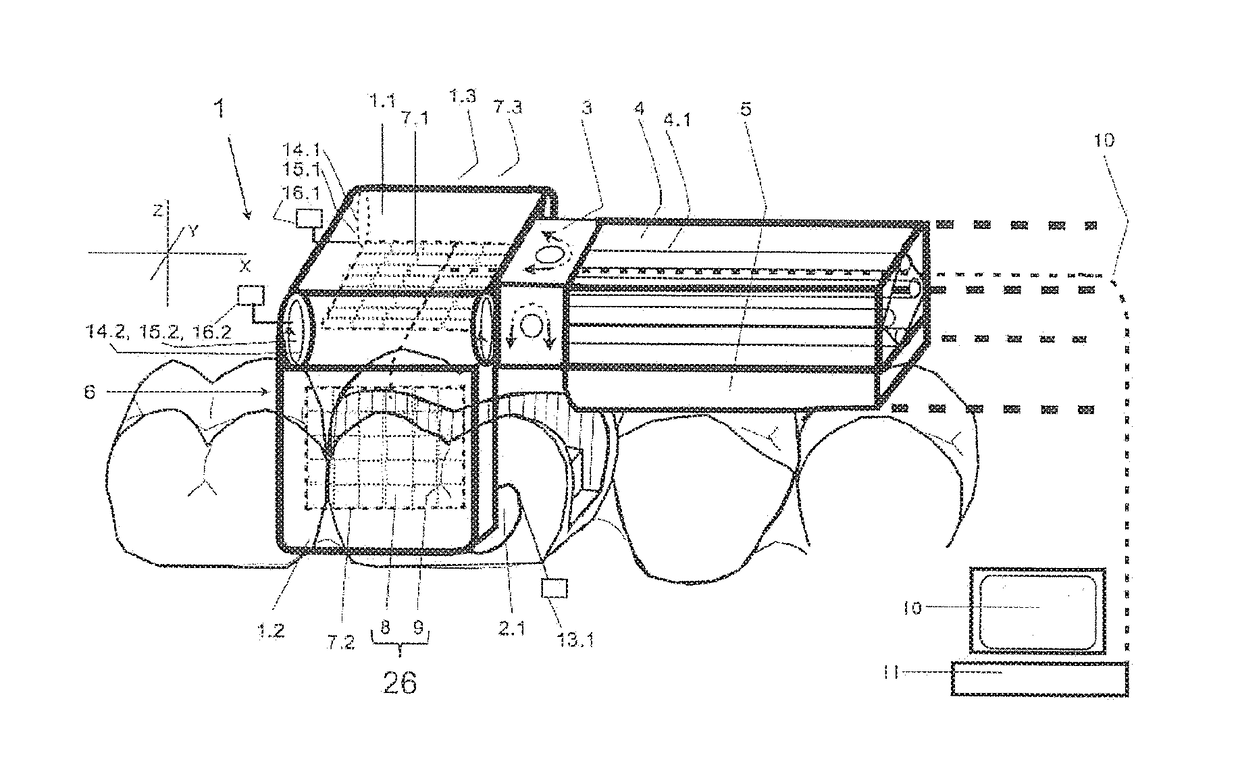
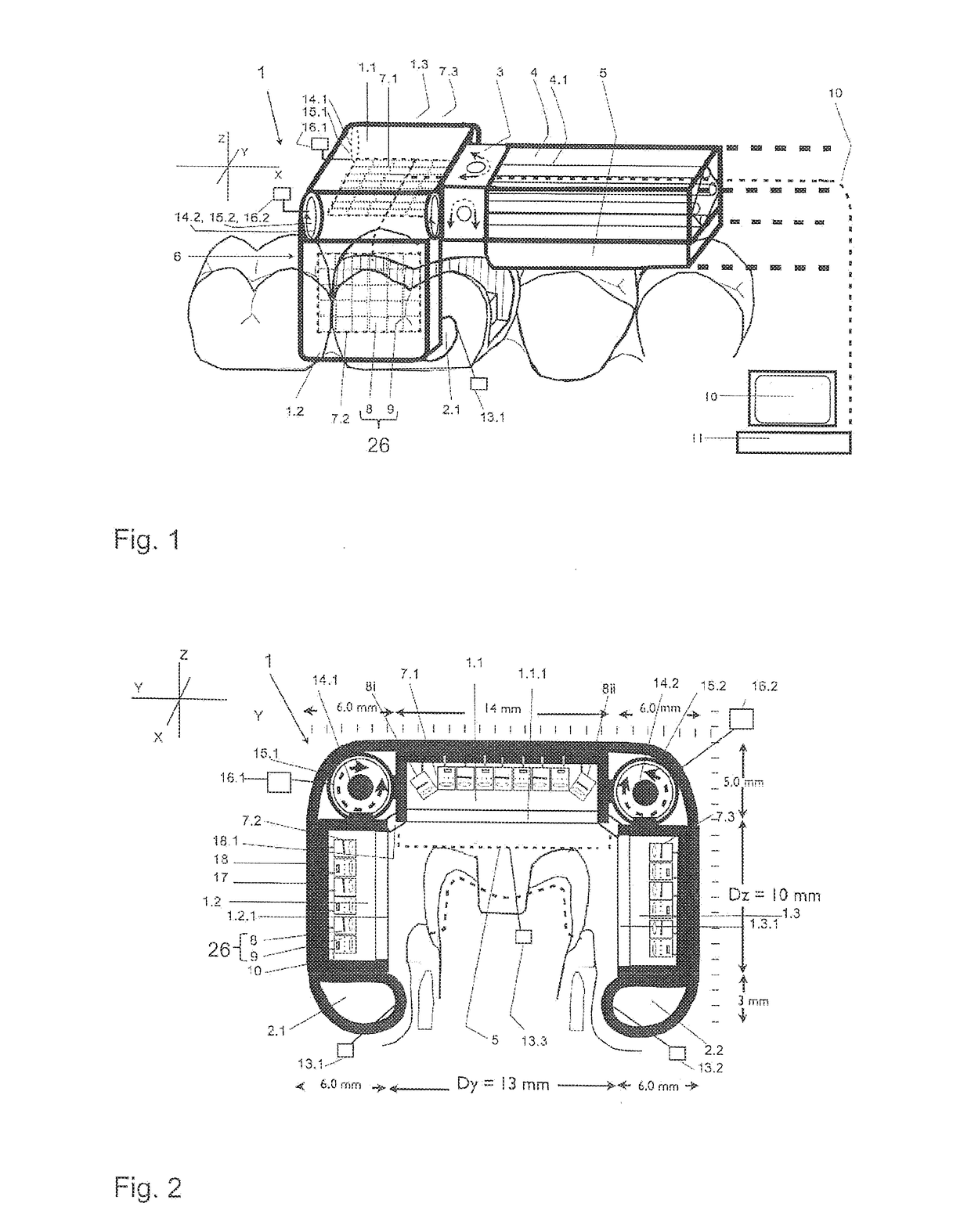
Measuring apparatus and method for three-dimensional measurement of an oral cavity
ActiveUS20170119505A1Fast and complete measurementShort measurement timeImpression capsSomatoscopeAutomatic controlMeasurement device
Disclosed is a measuring apparatus for three-dimensionally measuring a row of teeth, the rows of teeth of the maxilla and mandible, buccally, during articulation and during terminal occlusion, an alveolar ridge or the palate in the oral cavity, the measuring apparatus comprising an autonomously movable measuring head (1) on a shaft (4), said measuring head (1) consisting of a central measuring member (1.1) and at least two lateral measuring members (1.2, 1.3) which are movably interconnected and define a variable measurement space (6). The measuring head (1) can be placed on the row of teeth and is be guided therealong using guiding elements (1.1.1, 2.1, 2.2, 5); contact sensors (13) and angle sensors (16) ensure that the lateral measuring members are laterally guided and the angles thereof are adjusted to the topology of the alveolar ridge while the central guiding element (1.1.1) and / or a support (5) of the shaft (4) can rest on the row of teeth. Measuring units (26) for measuring the structures in the measurement space (6) are provided in the measuring members (1.1, 1.2, 1.3). Measurements are taken from multiple solid angle positions of the measuring units, said positions being preset in the measuring members (1.1, 1.2, 1.3), being adjusted by moving the measuring members (1.1, 1.2, 1.3), being taken by having mirrors move, in a controlled manner, the beam path generated by the measuring units, or being aligned by changing the angular position of the measuring head (1) relative to the shaft (4) in an automatically controlled manner.
Owner:QUARZ PARTNERS
Orthodontic distalizing apparatus
Owner:AMERICAN ORTHODONTICS
Self-supporting collagen tunnel for guided tissue regeneration and method of using same
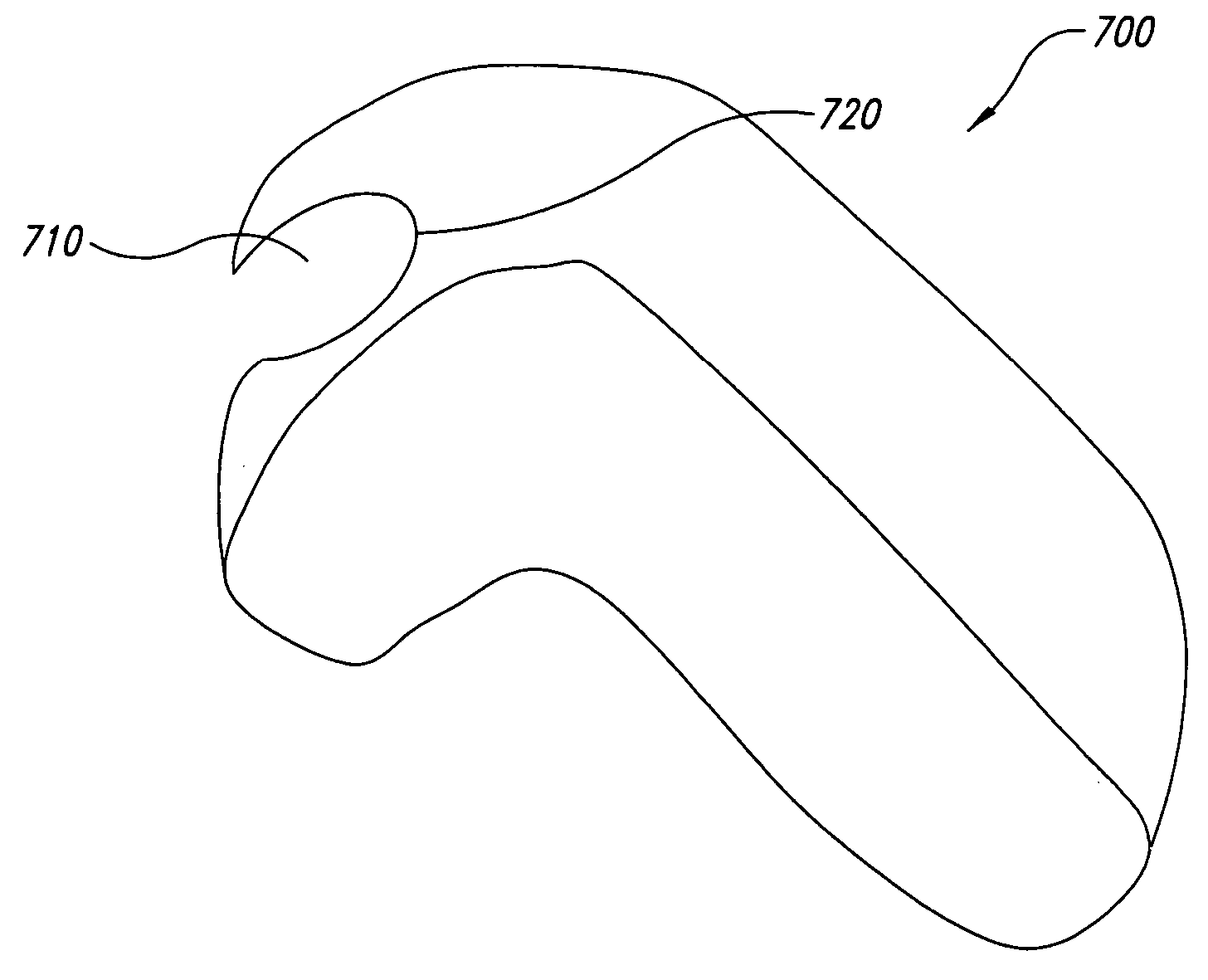
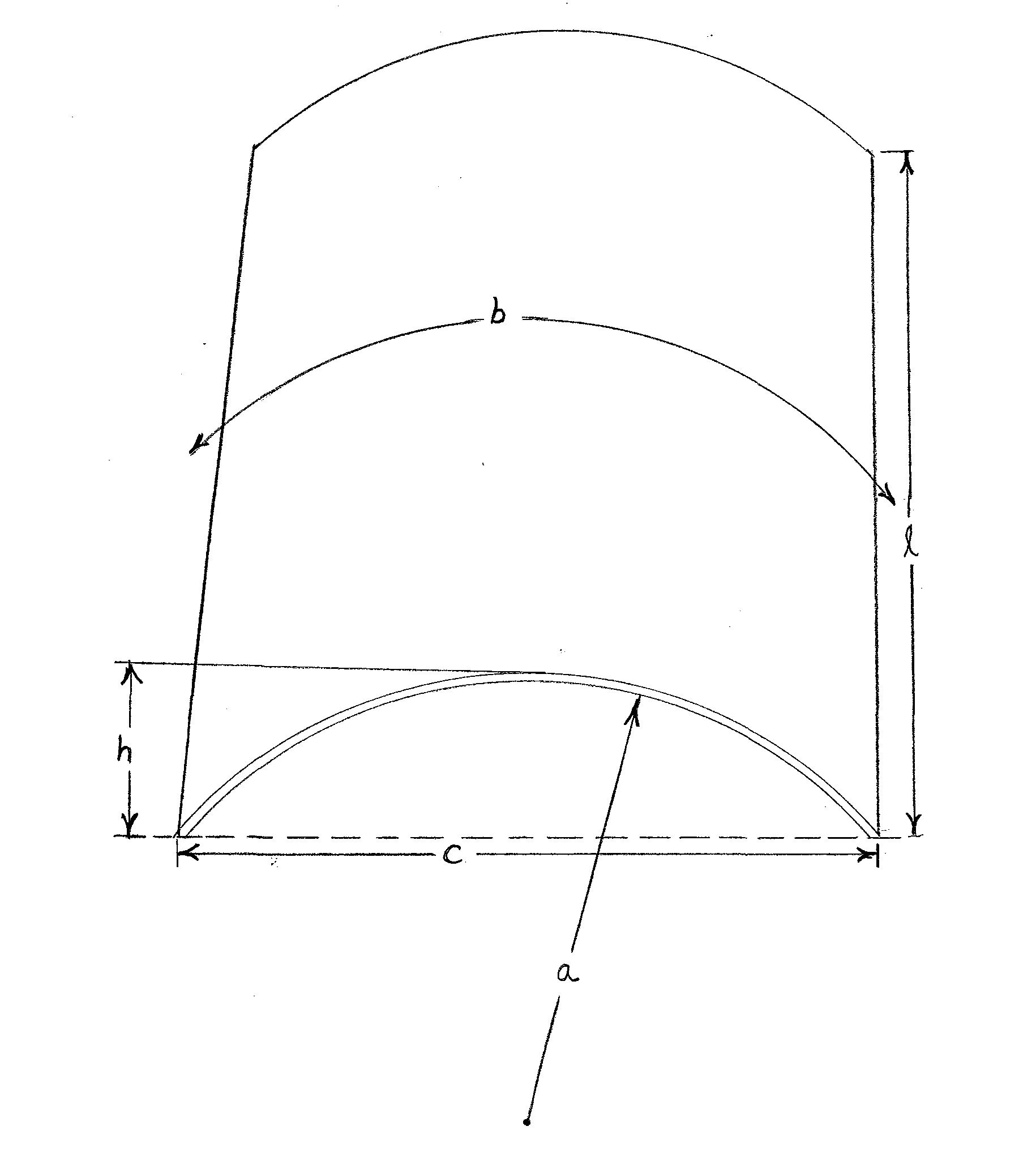
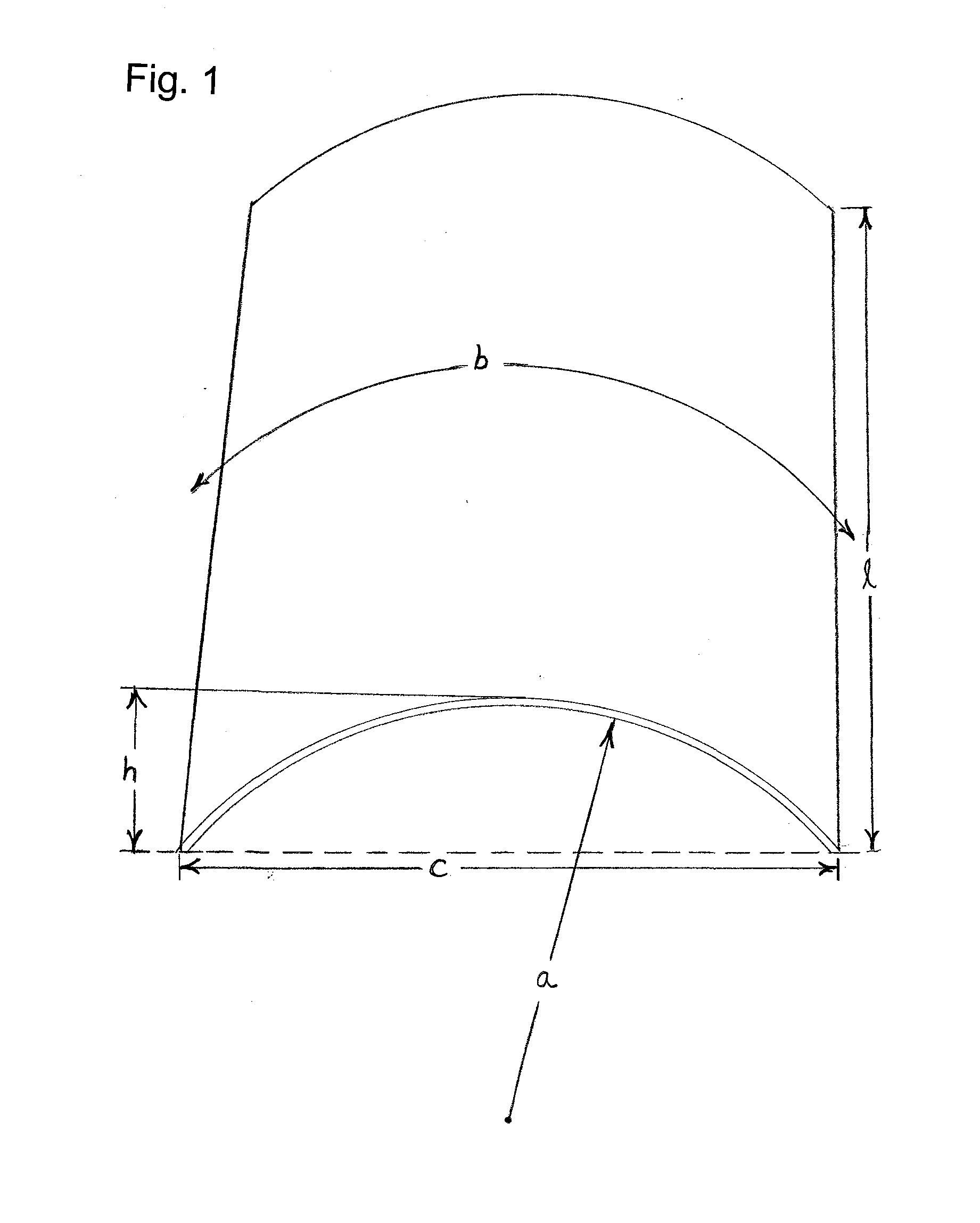
InactiveUS8353967B2For accurate placementPrecise positioningBiocidePeptide/protein ingredientsIliac screwBiomedical engineering
A biocompatible, self-supporting, curved, collagen membrane adapted to be secured by bone tacks or bone screws over exposed bone at a desired bone graft site in the alveolar ridge of a patient such that the membrane defines a space having a predetermined height and width over the exposed bone, in which the membrane maintains its structural integrity for at least 4 months after implantation at the bone graft site and then naturally breaks down and is resorbed by the patient's body, a method of making such a membrane, and a method of using such a membrane for vertical augmentation of the alveolar ridge of the patient.
Owner:CARDOSO RONALD
Bone repair putty
ActiveUS8876532B2Promote bone growthSpeed up the repair processPowder deliveryBiocideParticulatesHigh concentration
A bone repair material is described that is of putty-like consistency, particularly useful for repairing dental bony defects such as those caused by bone loss resulting from moderate or severe periodontitis, augmenting of bony defects of the alveolar ridge, filling tooth extraction sites, or sinus elevation grafting. The repair material includes a porous, resorbable particulate that is bone-derived or derived from bone-like hydroxyapatite or synthetic hydroxyapatite; and, a resorbable carrier, such as high molecular weight polysaccharides, such as hyaluronic acid. A high concentration of particulate in the putty enhances bone repair and requires a high concentration of carrier to retain the putty at the defect site. For a particulate density of about 1.2 g / cc such as PEPGEN P-15® Bone Graft, a preferred formulation comprises about 55% percent by weight of the putty suspended in a hyaluronic acid gel of about 1.4×106 daltons molecular weight and a final concentration of about 56 mg / cc which material adheres to a bony periodontal defect and does not excessively expand or migrate from the defect when held in place by a conventional flap closure.
Owner:DENTSPLY SIRONA INC
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com