Patents
Literature
991 results about "Cardiac Ventricle" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
The larger chamber(s) of the heart that receives blood from an atrium and pushes it out of the heart into the peripheral circulation and/or the lungs.
Systems for heart treatment
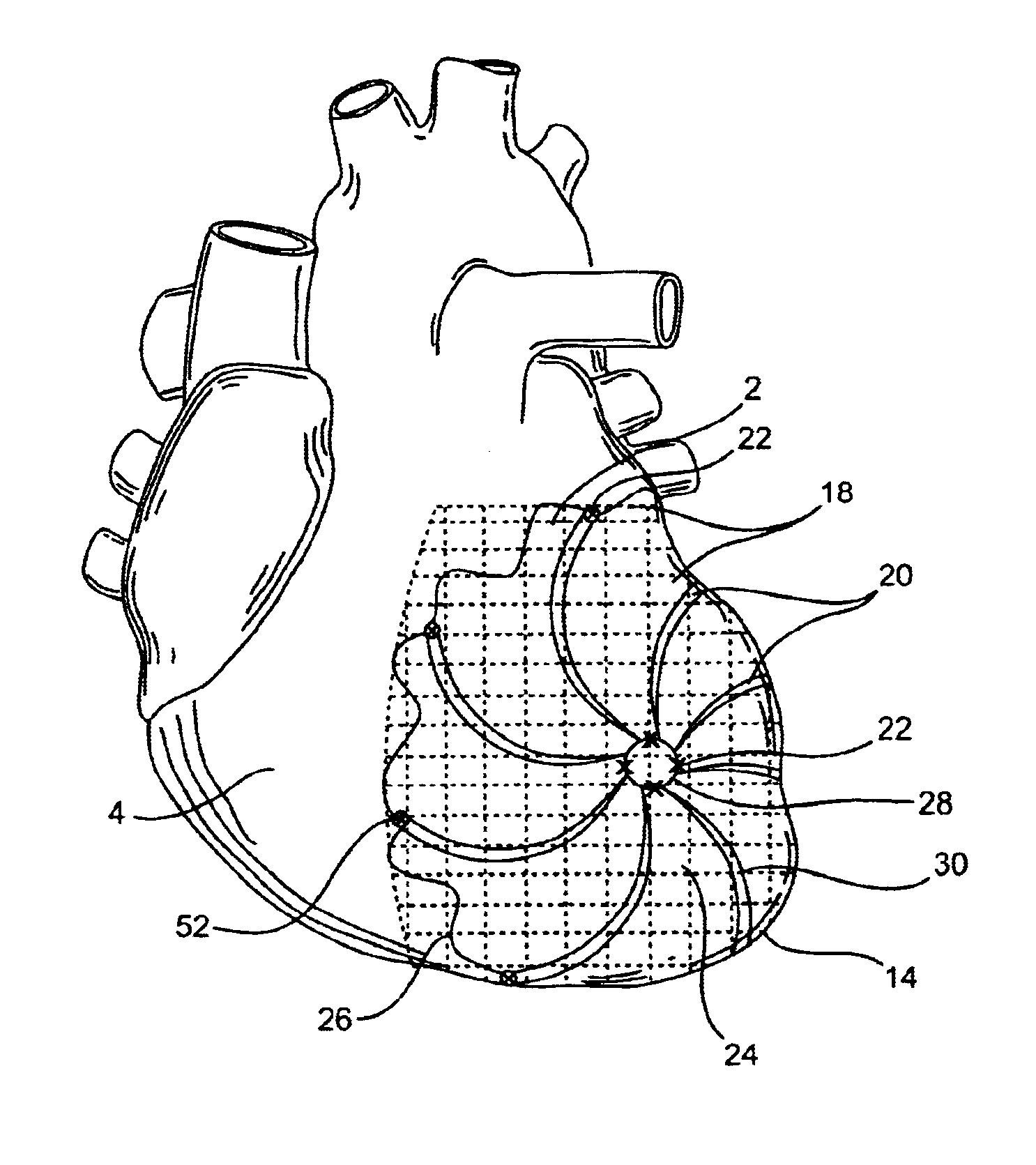
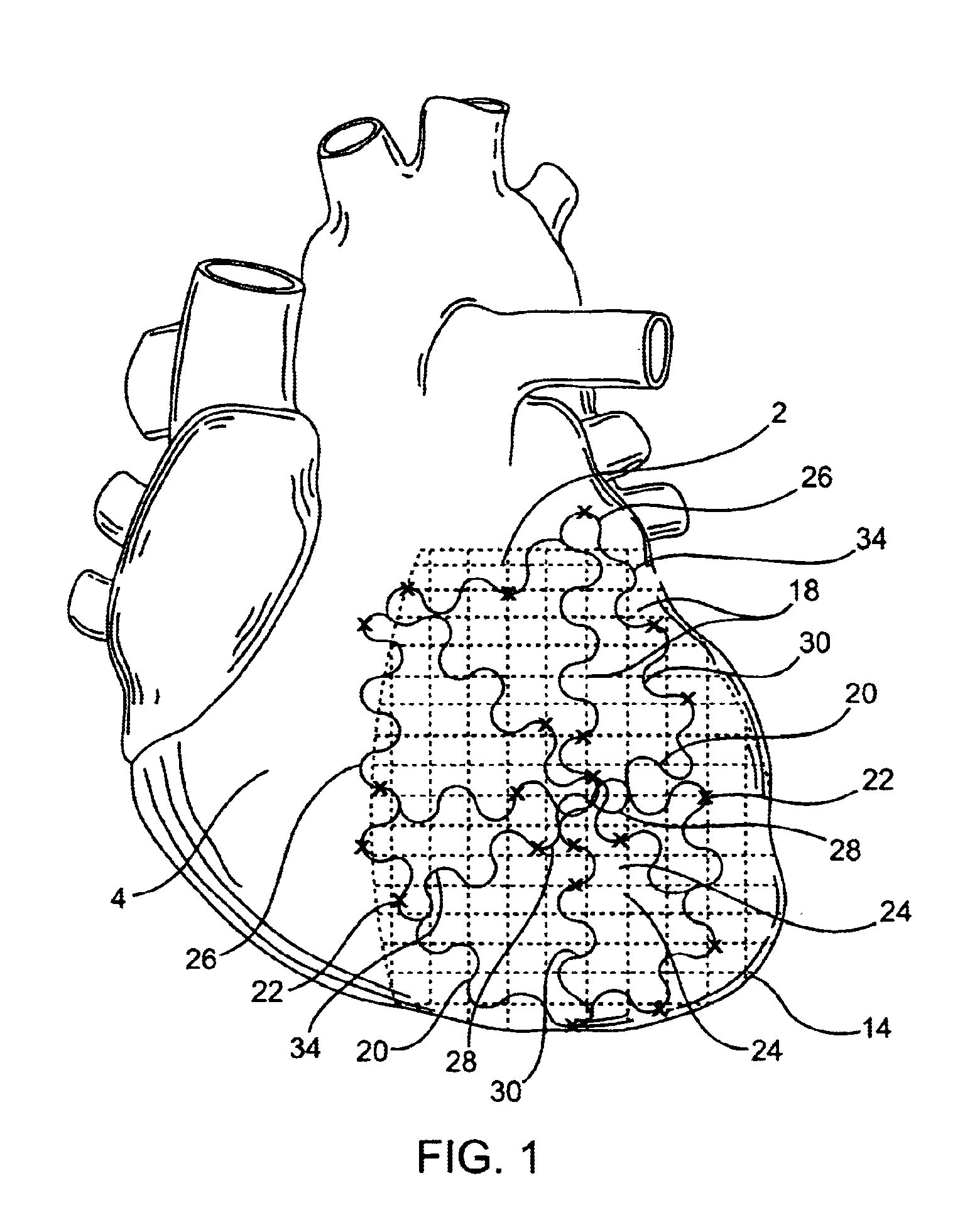
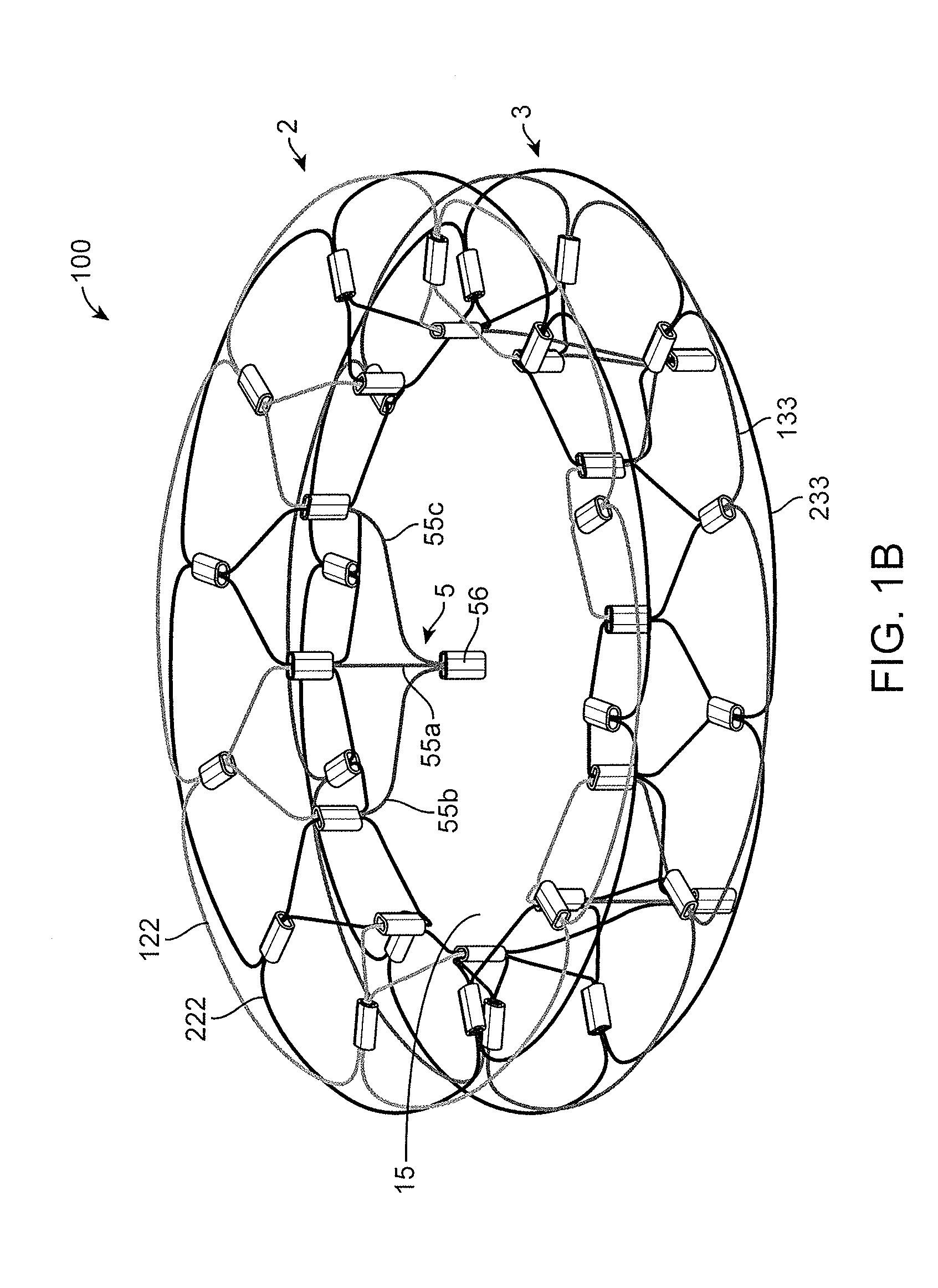
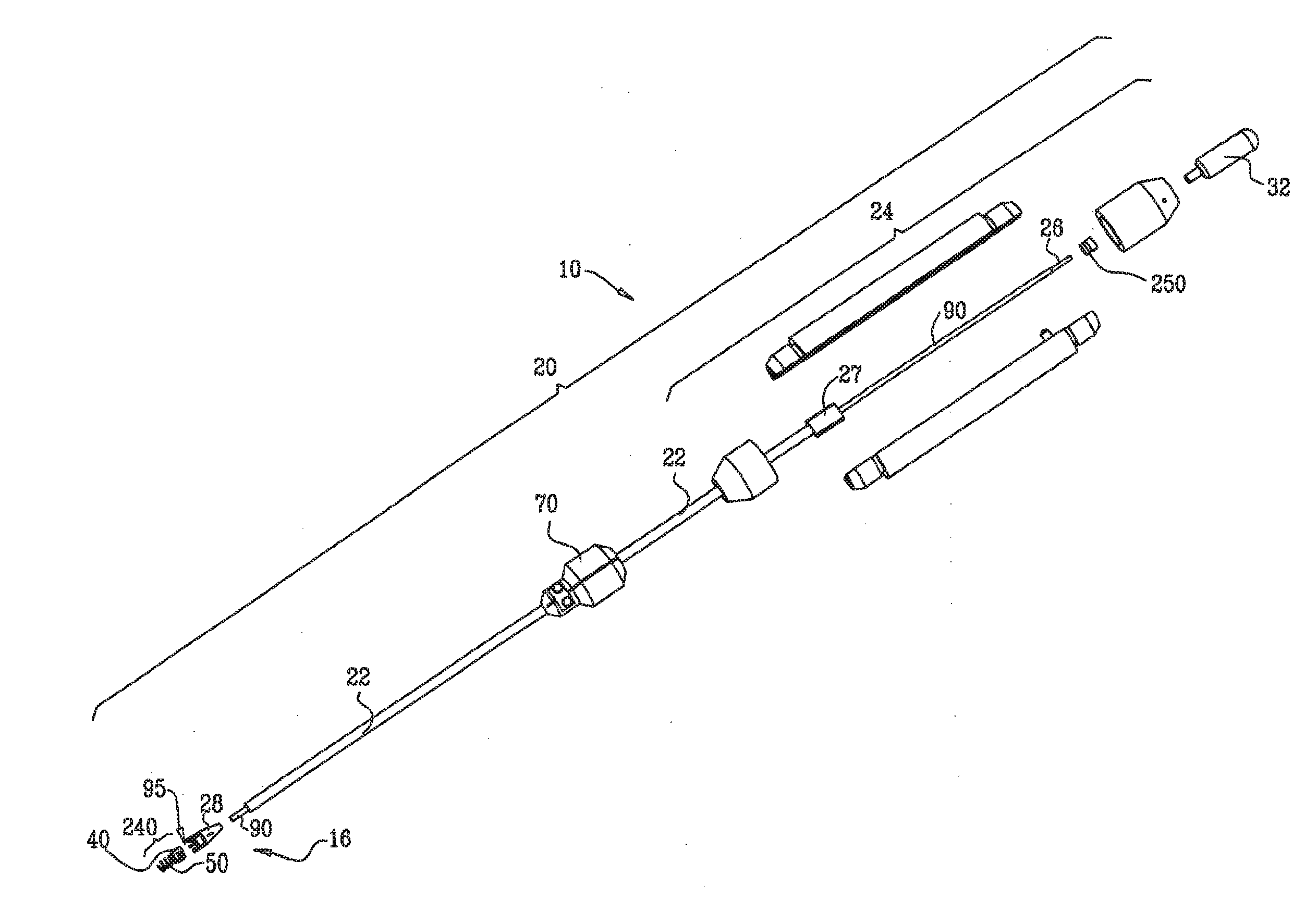
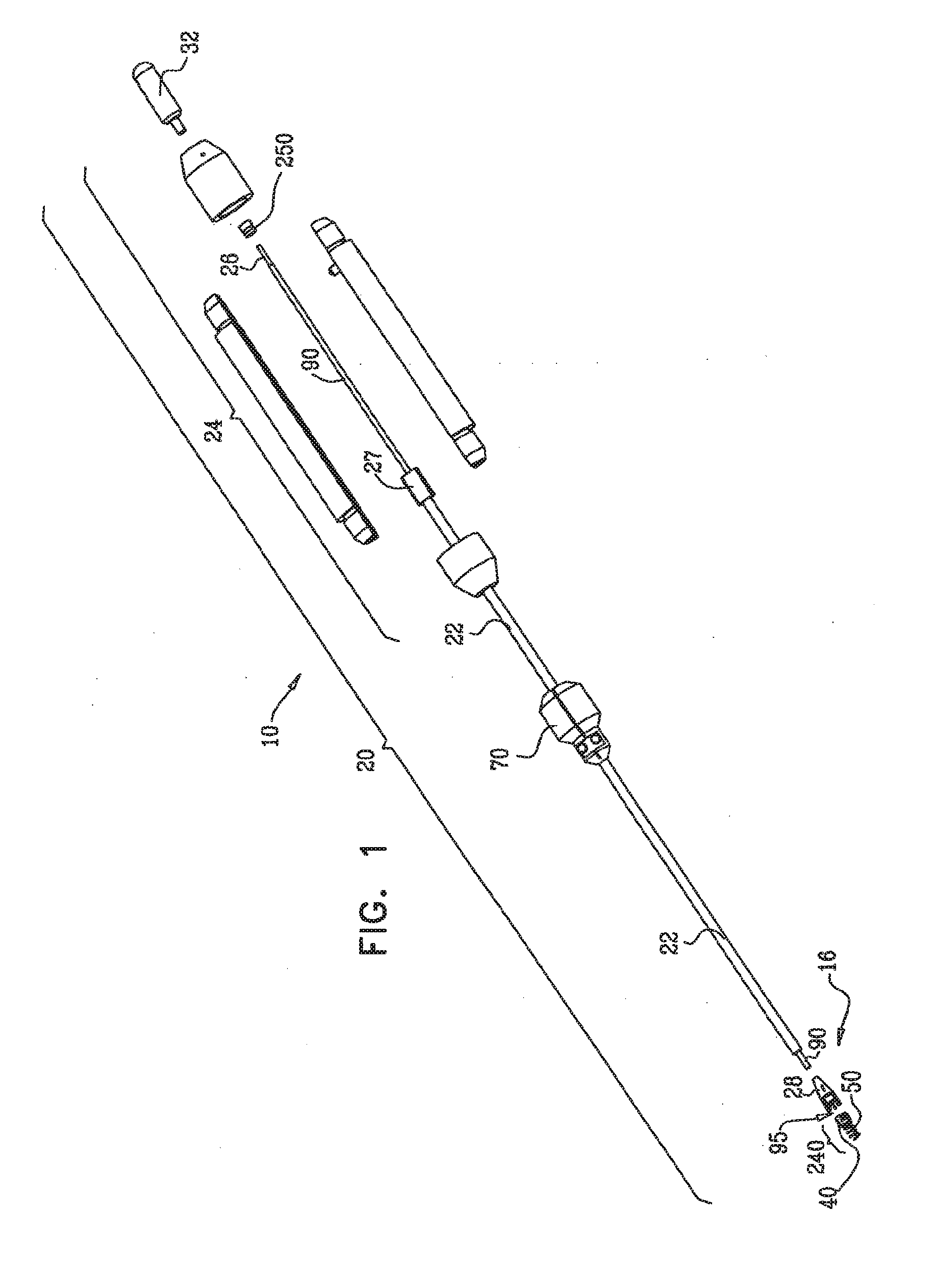
InactiveUS20050197694A1Reduce stressReduce/limit volumeSuture equipmentsElectrotherapyLeft ventricular sizeTherapeutic treatment
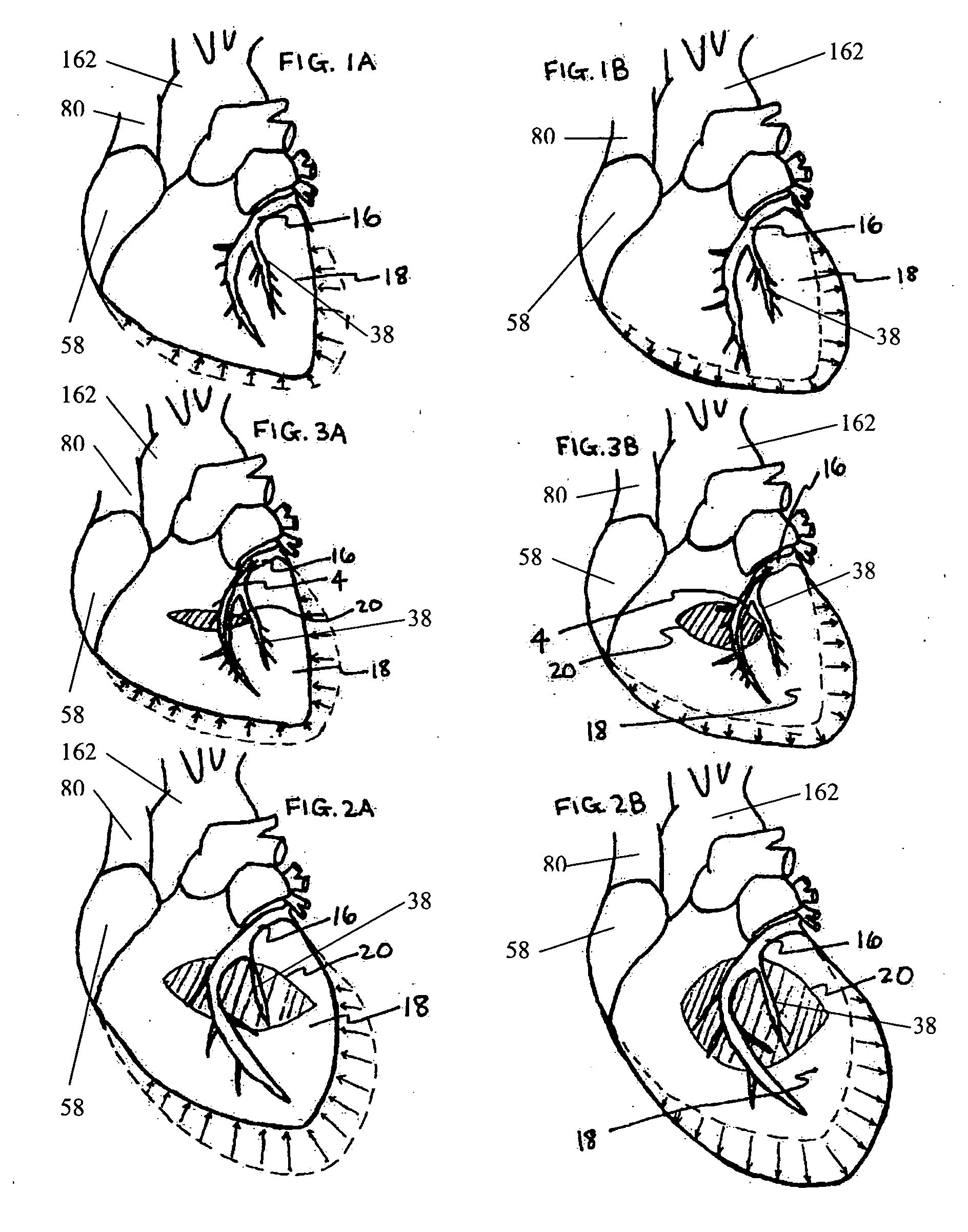
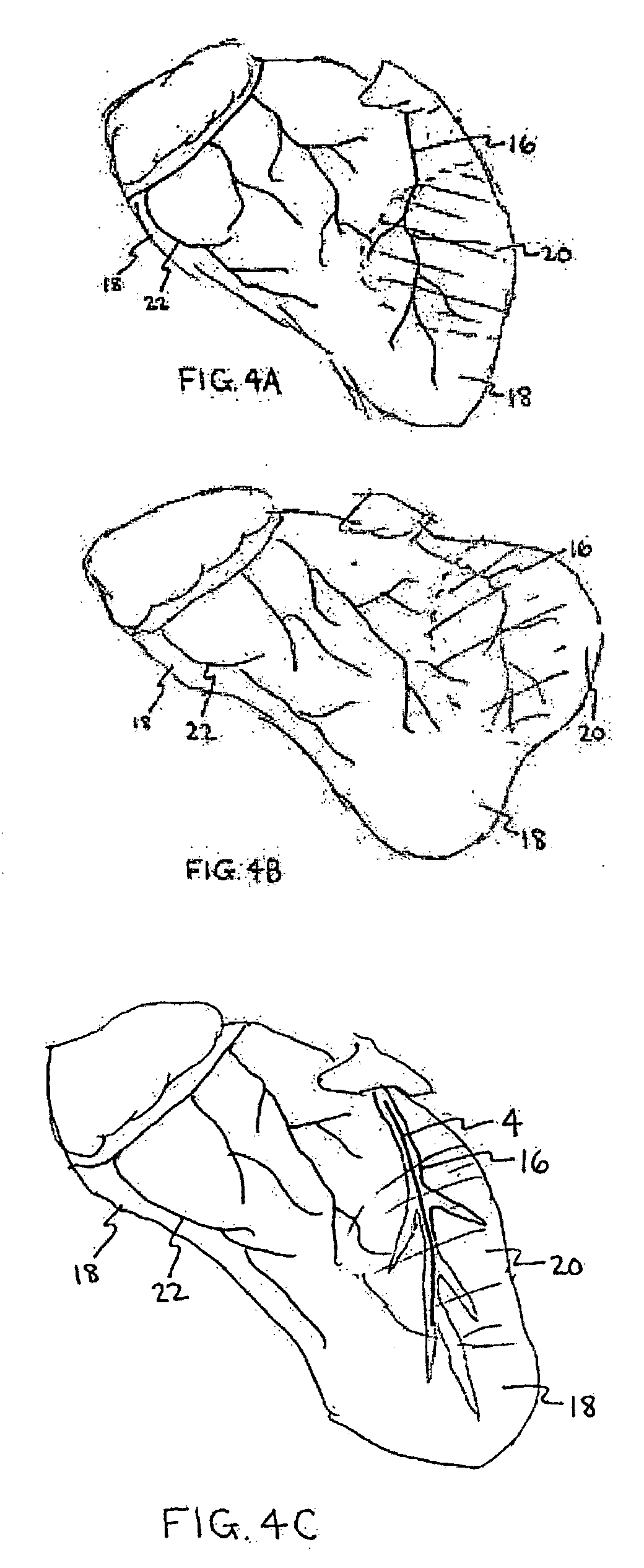
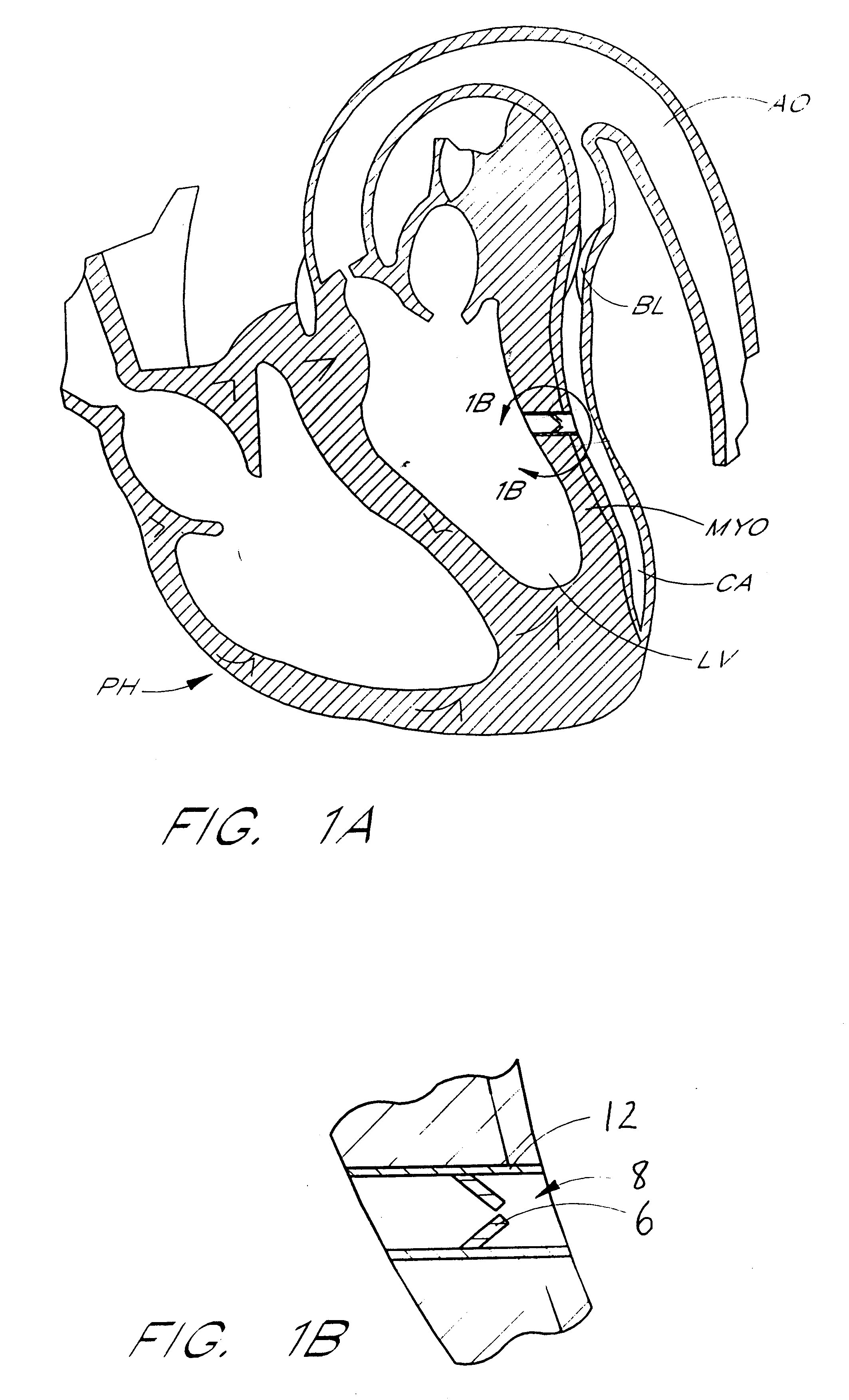
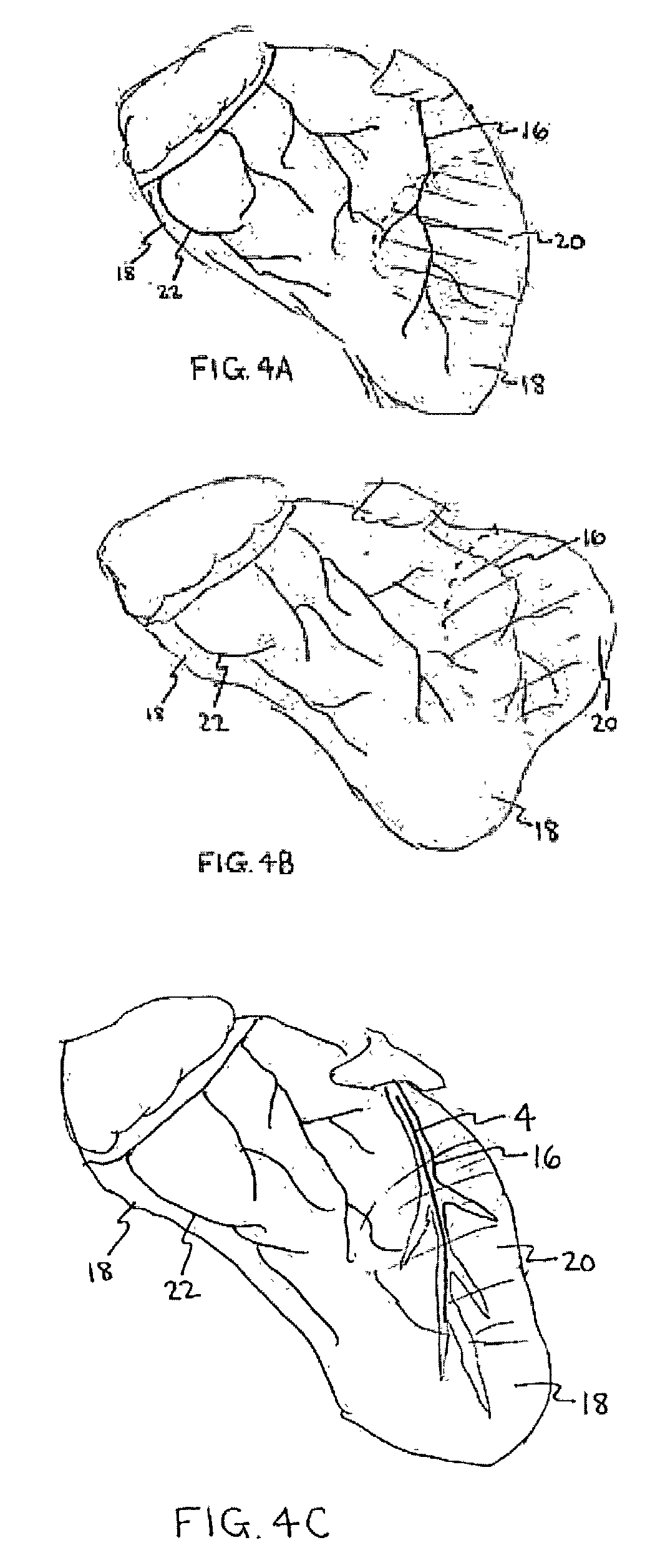
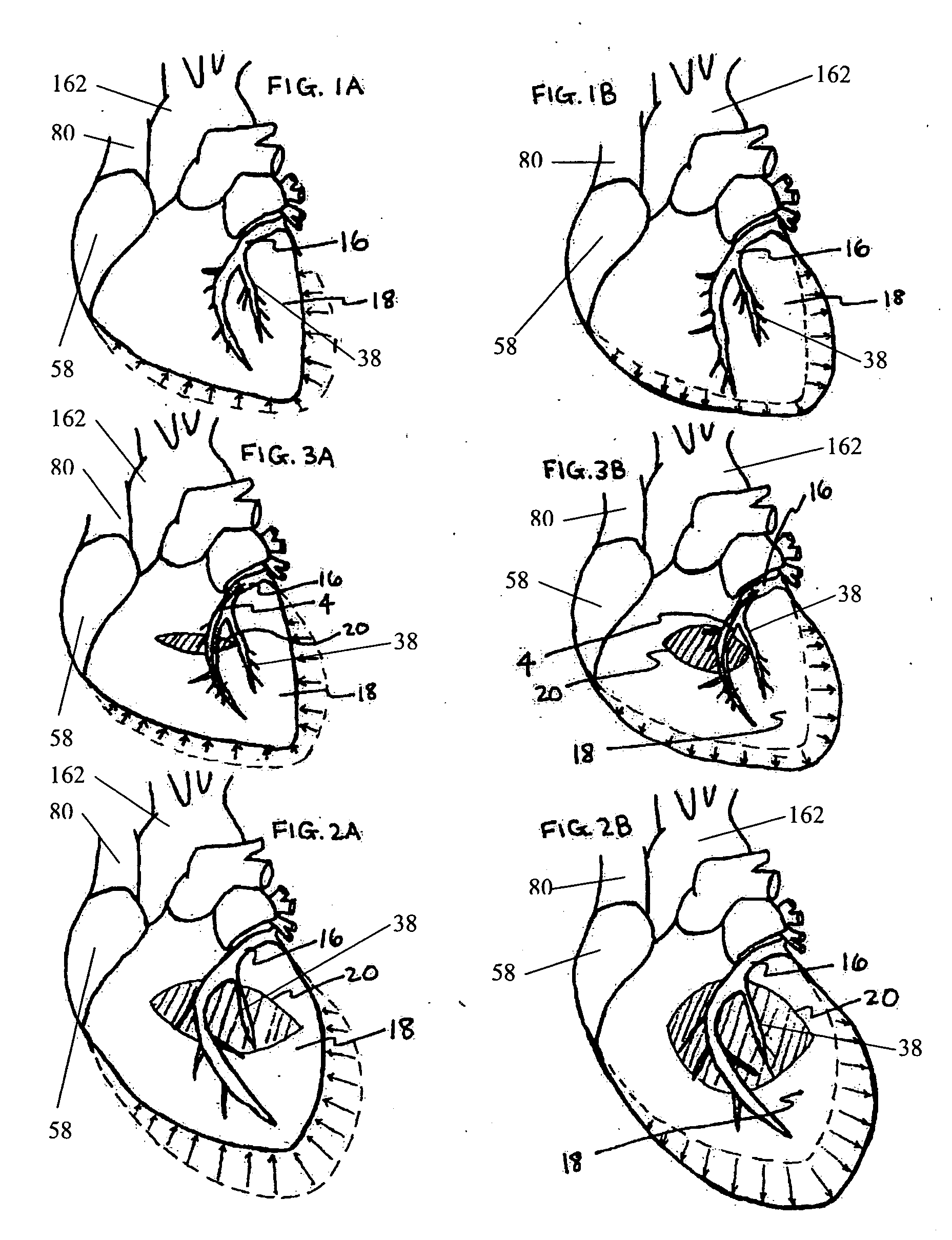
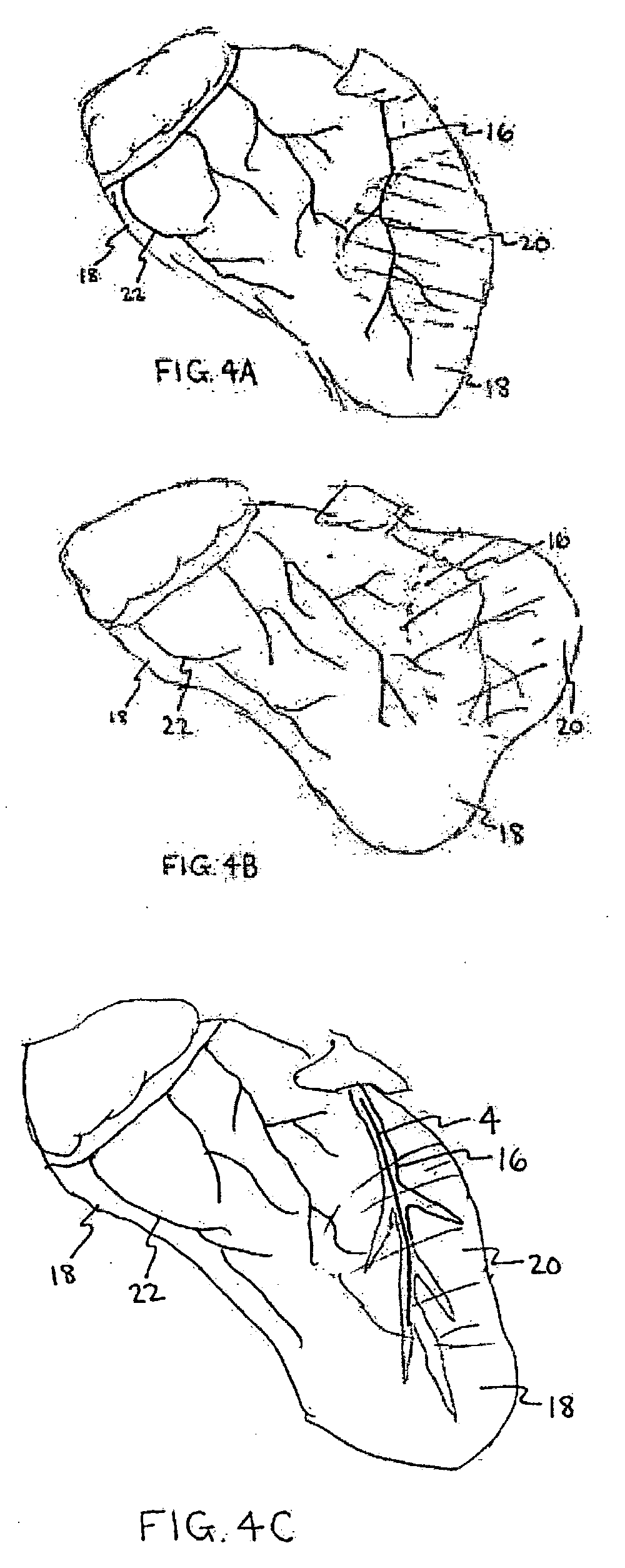
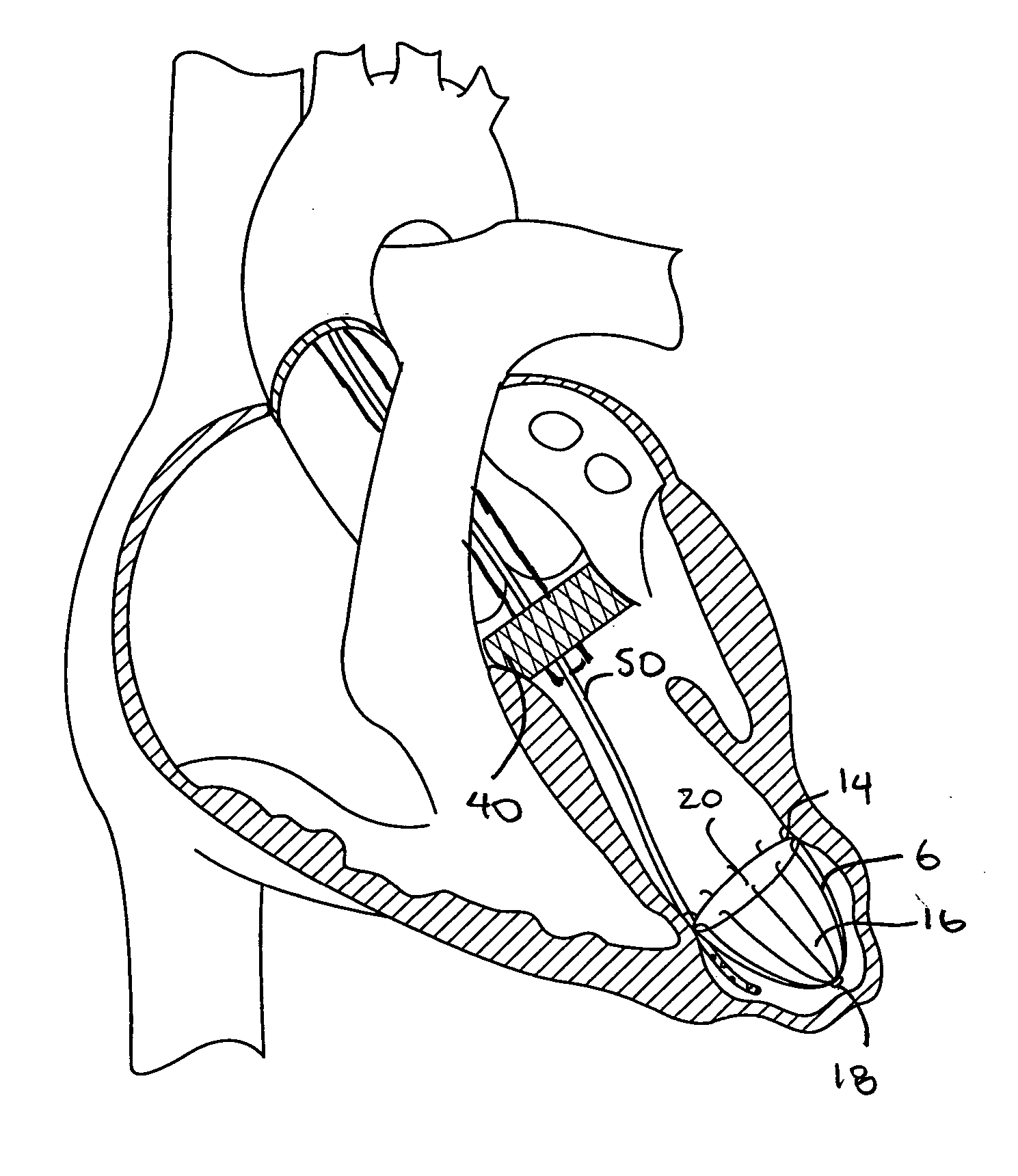
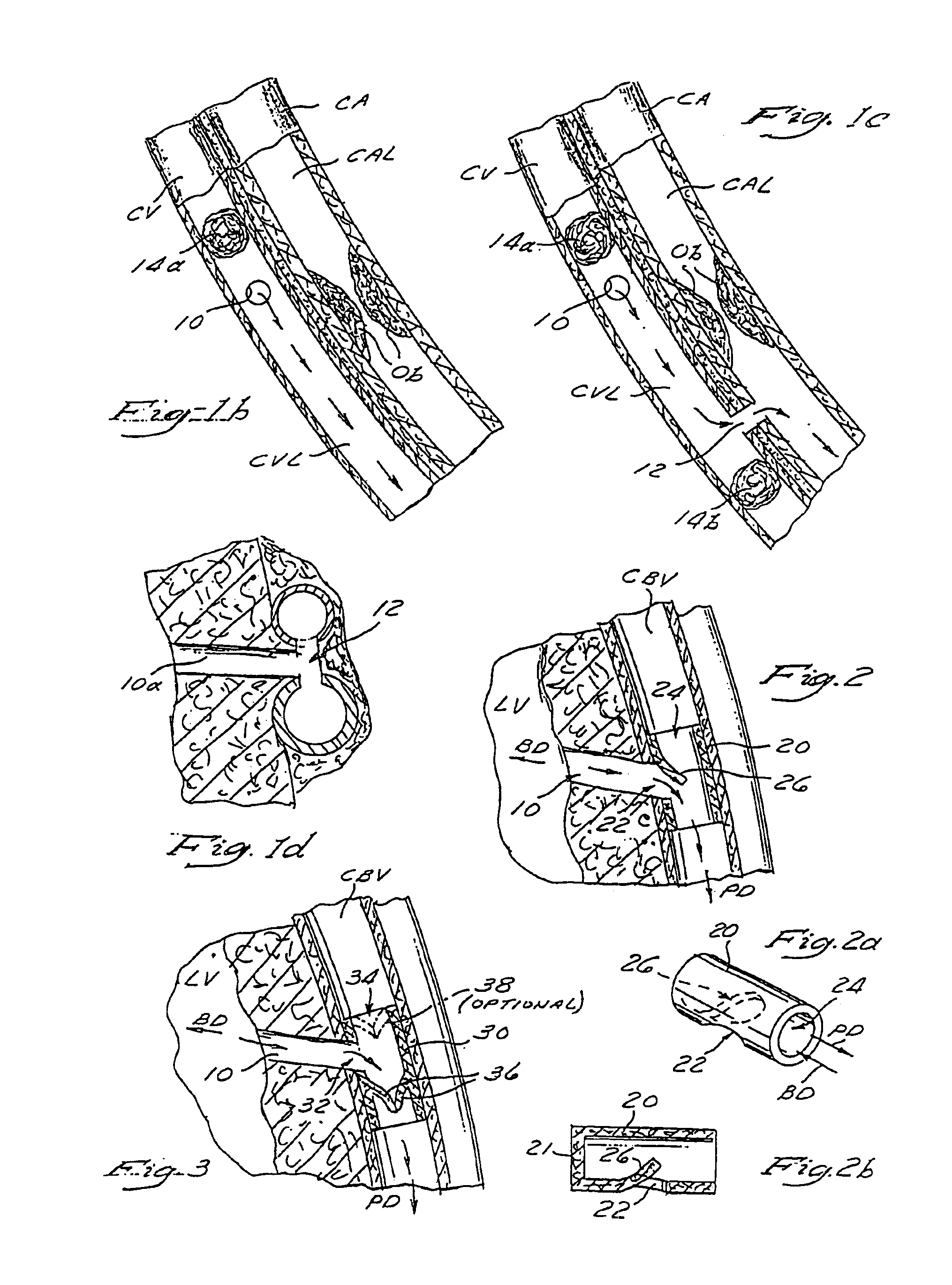
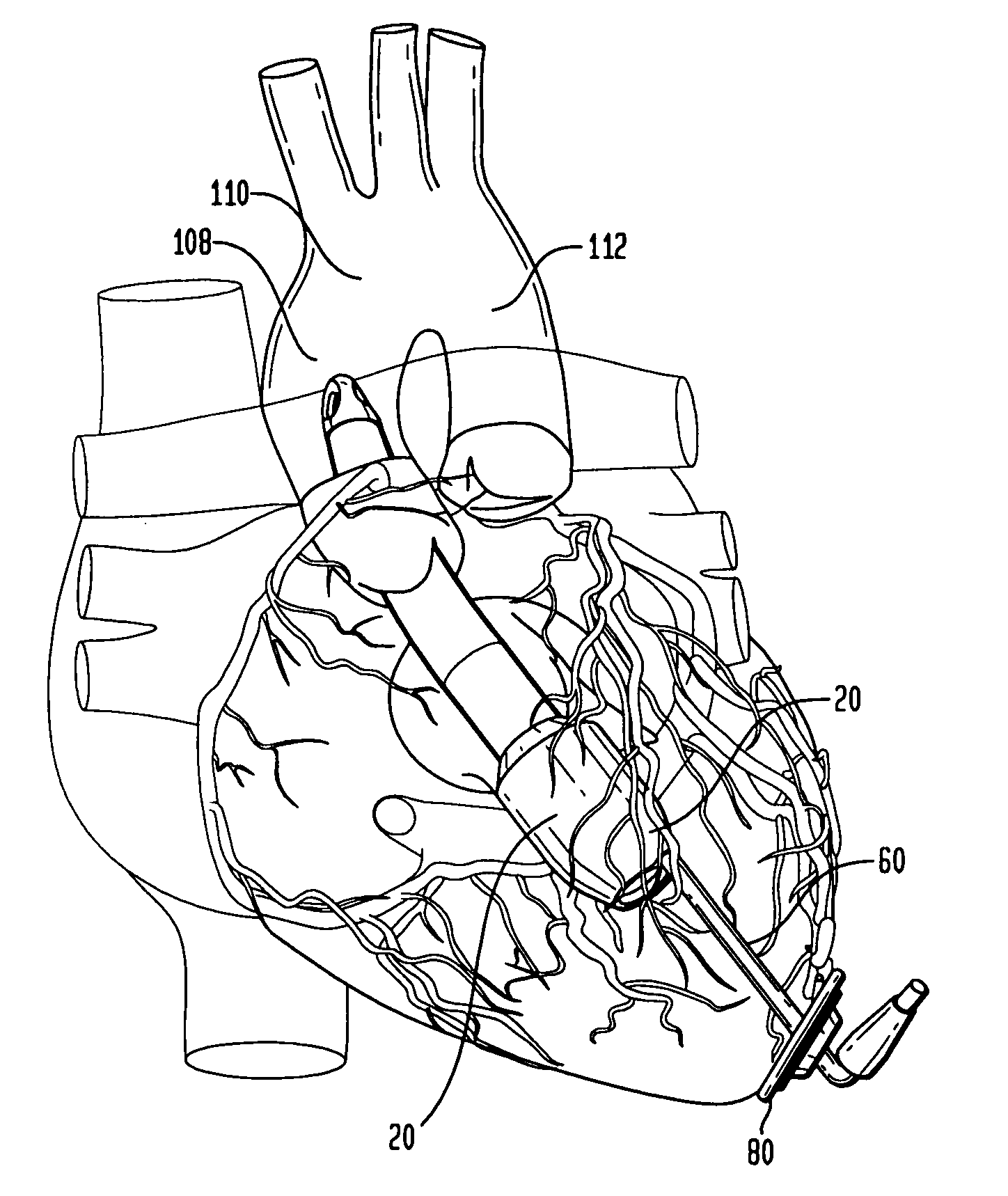
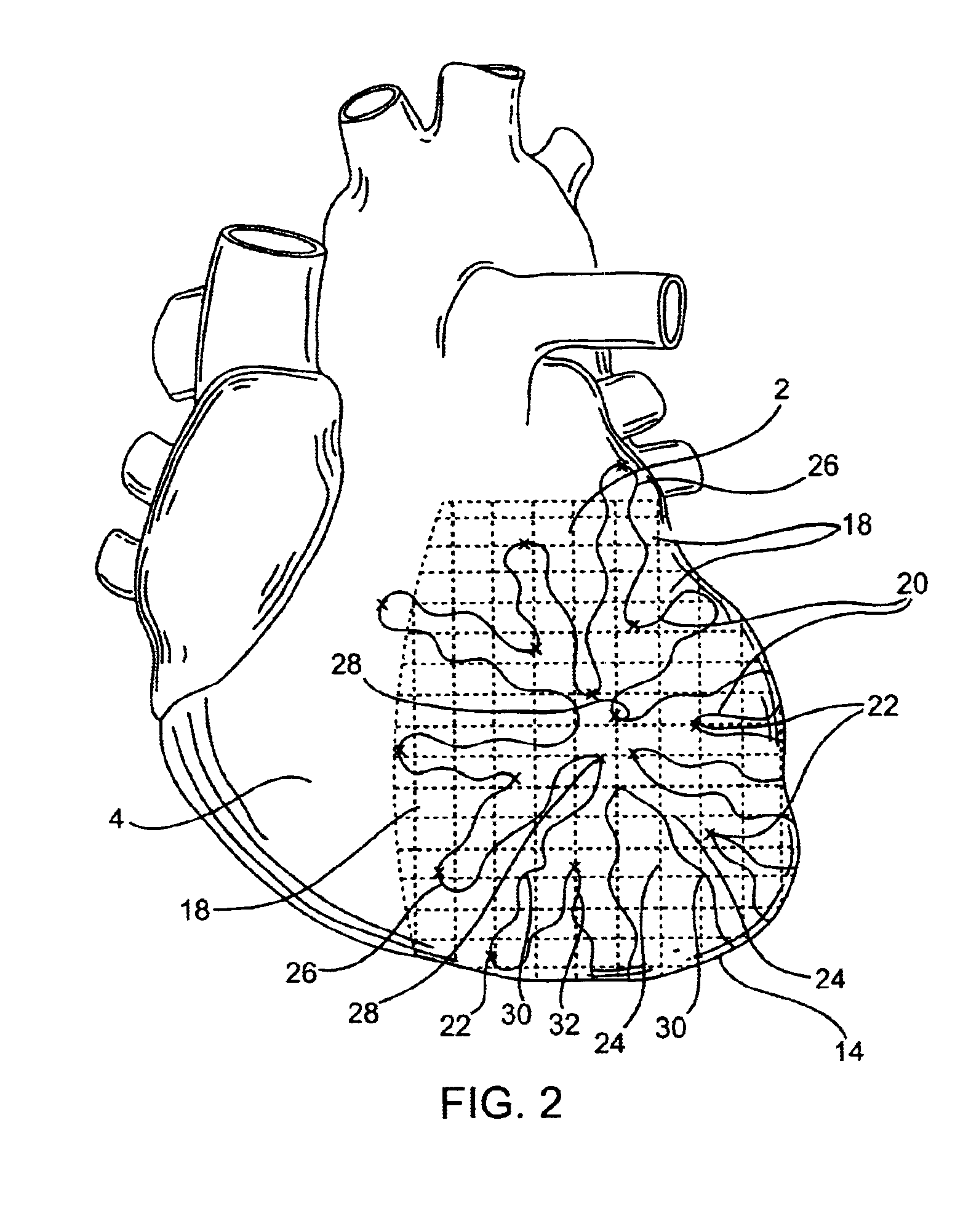
Described are devices and methods for treating degenerative, congestive heart disease and related valvular dysfunction. Percutaneous and minimally invasive surgical tensioning structures offer devices that mitigate changes in the ventricular structure (i.e., remodeling) and deterioration of global left ventricular performance related to tissue damage precipitating from ischemia, acute myocardial infarction (AMI) or other abnormalities. These tensioning structures can be implanted within various major coronary blood-carrying conduit structures (arteries, veins and branching vessels), into or through myocardium, or into engagement with other anatomic structures that impact cardiac output to provide tensile support to the heart muscle wall which resists diastolic filling pressure while simultaneously providing a compressive force to the muscle wall to limit, compensate or provide therapeutic treatment for congestive heart failure and / or to reverse the remodeling that produces an enlarged heart.
Owner:EXTENSIA MEDICAL
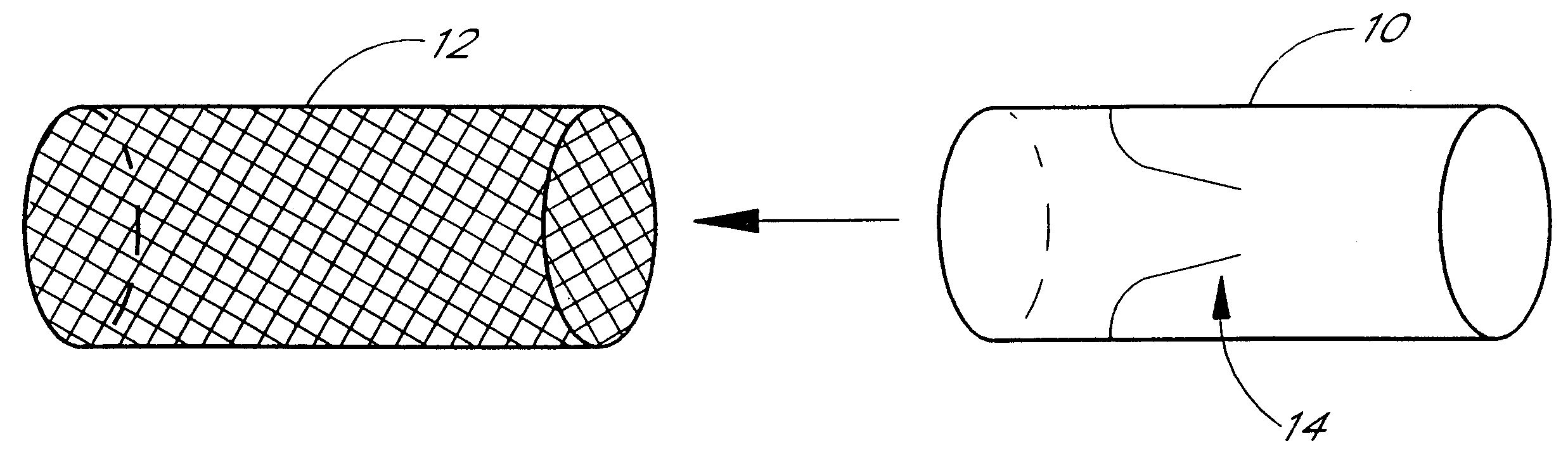
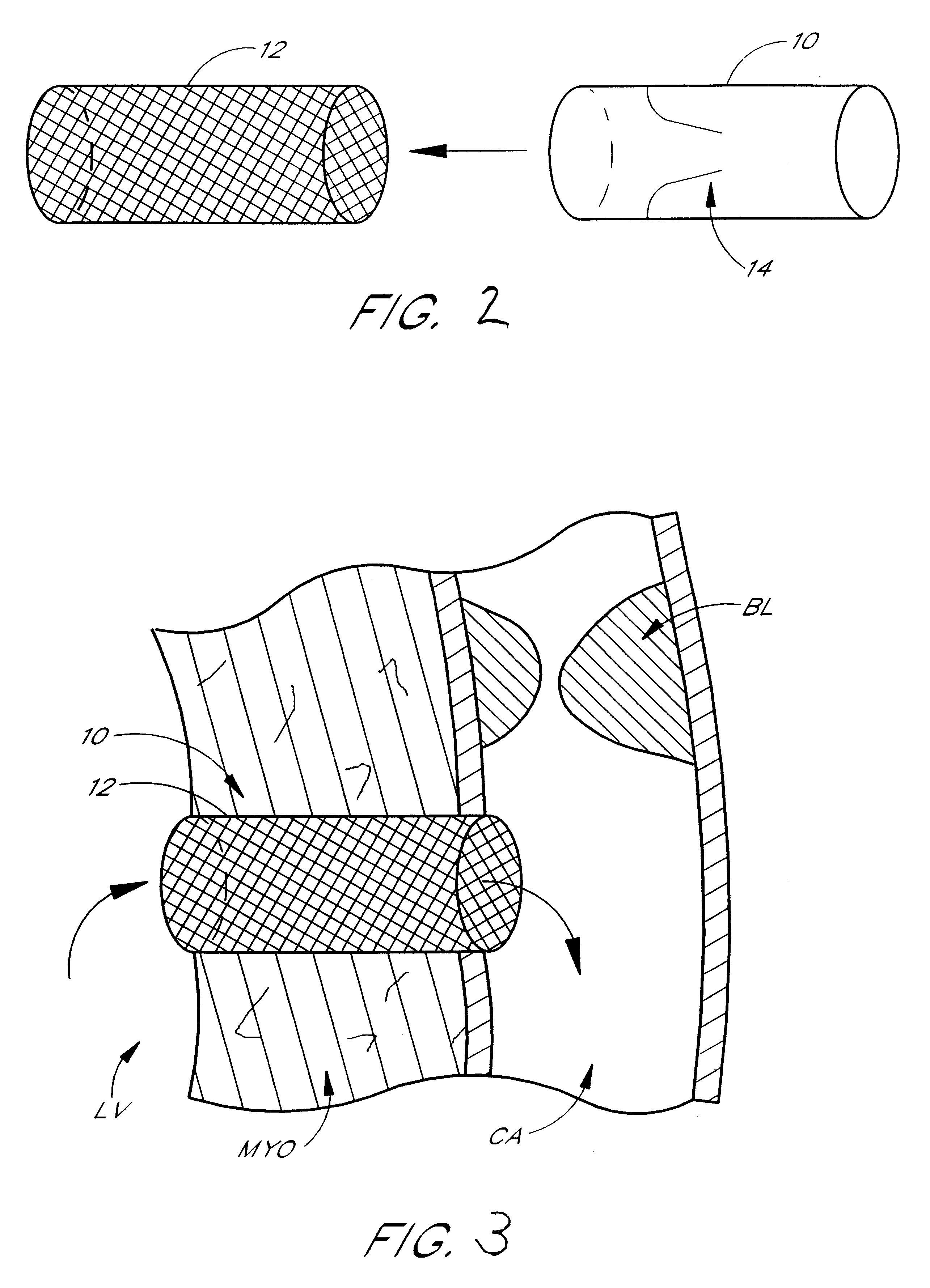
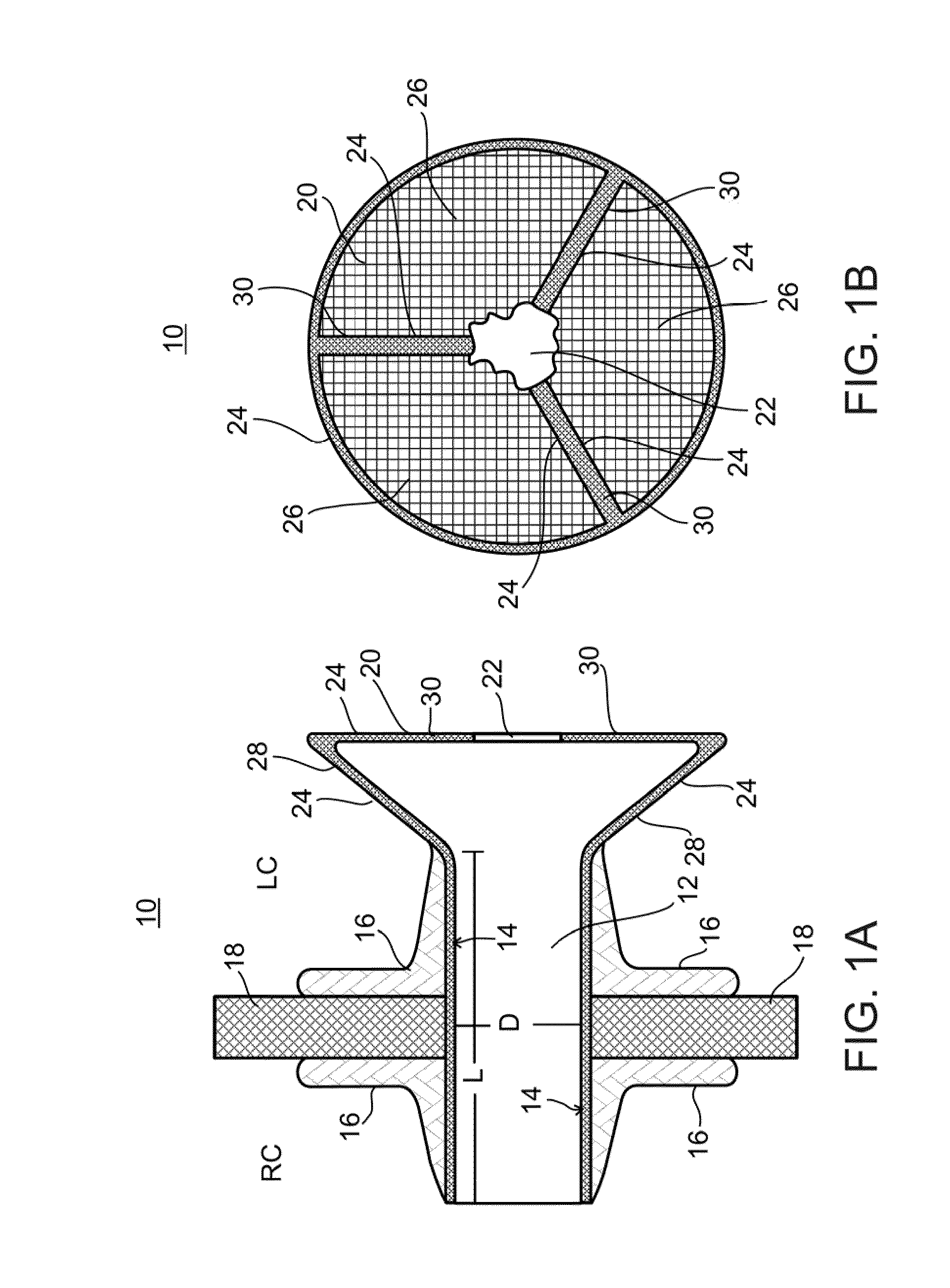
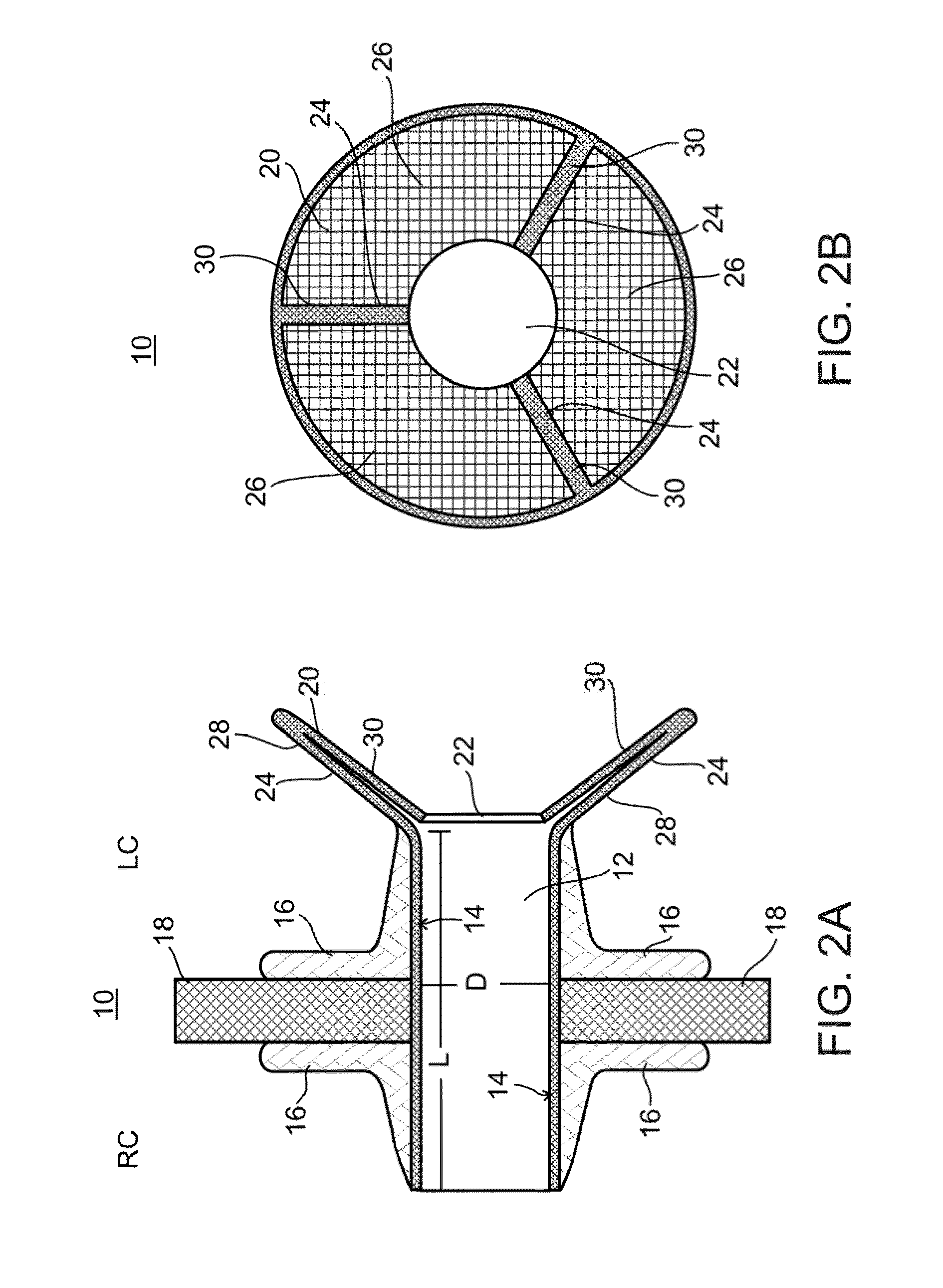
Conduit with valved blood vessel graft
Disclosed is a conduit that provides a bypass around an occlusion or stenosis in a coronary artery. The conduit is a tube adapted to be positioned in the heart wall to provide a passage for blood to flow between a heart chamber and a coronary artery, at a site distal to the occlusion or stenosis. The conduit has a section of blood vessel attached to its interior lumen which preferably includes at least one naturally occurring one-way valve positioned therein. The valve prevents the backflow of blood from the coronary artery into the heart chamber.
Owner:HORIZON TECH FUNDING CO LLC +1
Systems for heart treatment
InactiveUS7144363B2Reduce stressReduce/limit volumeSuture equipmentsHeart valvesLeft ventricular sizeTherapeutic treatment
Owner:BAY INNOVATION GROUP
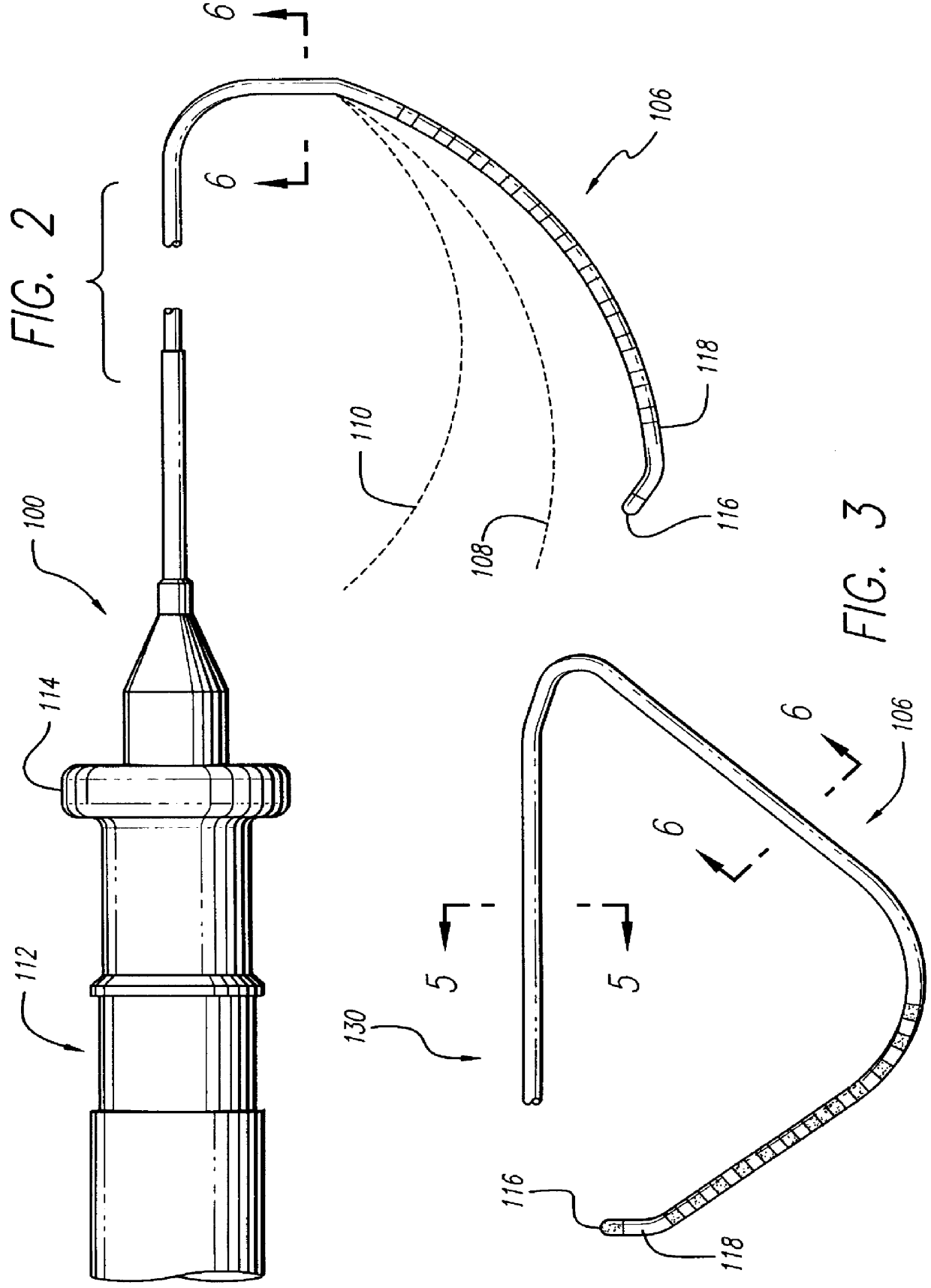
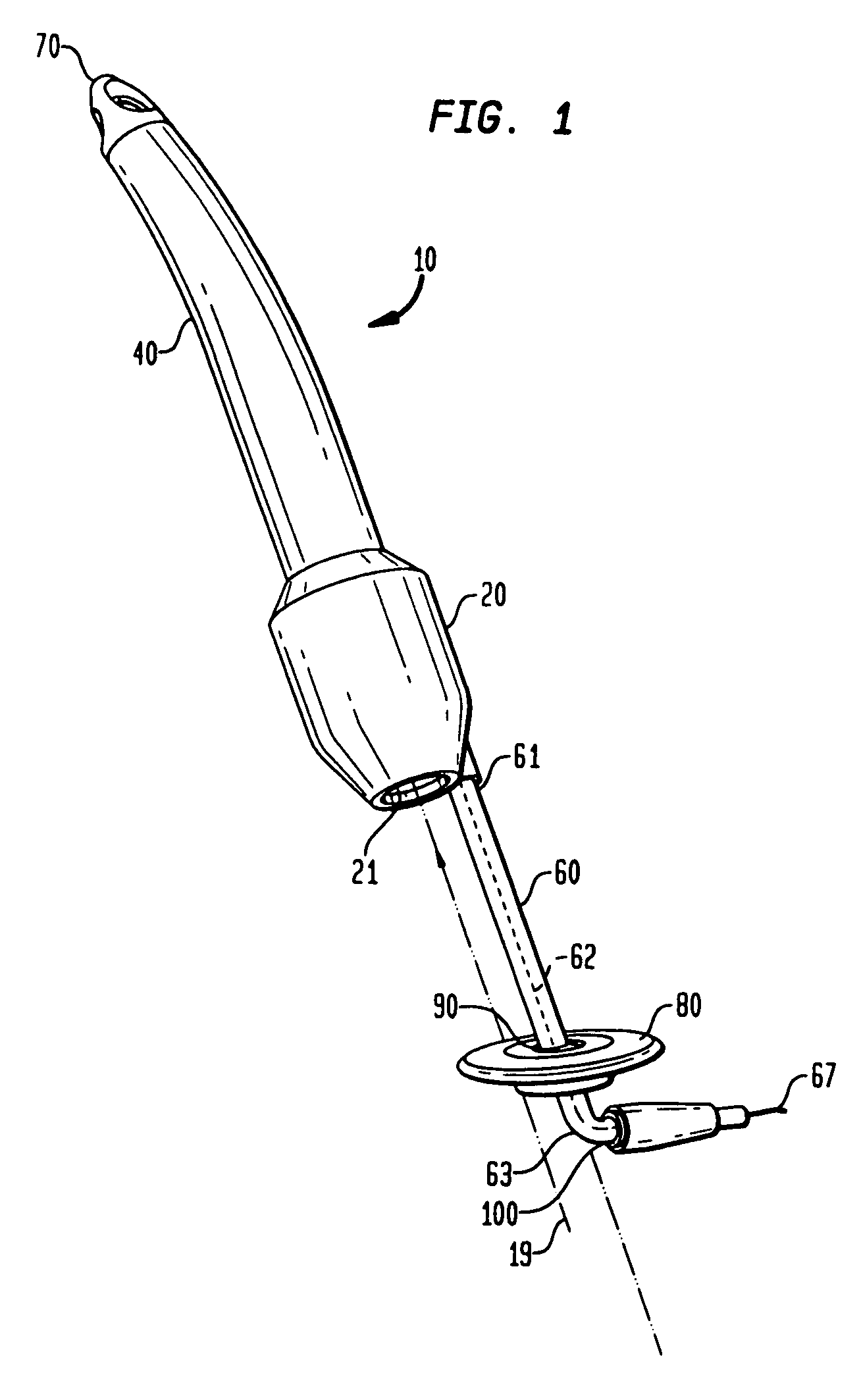
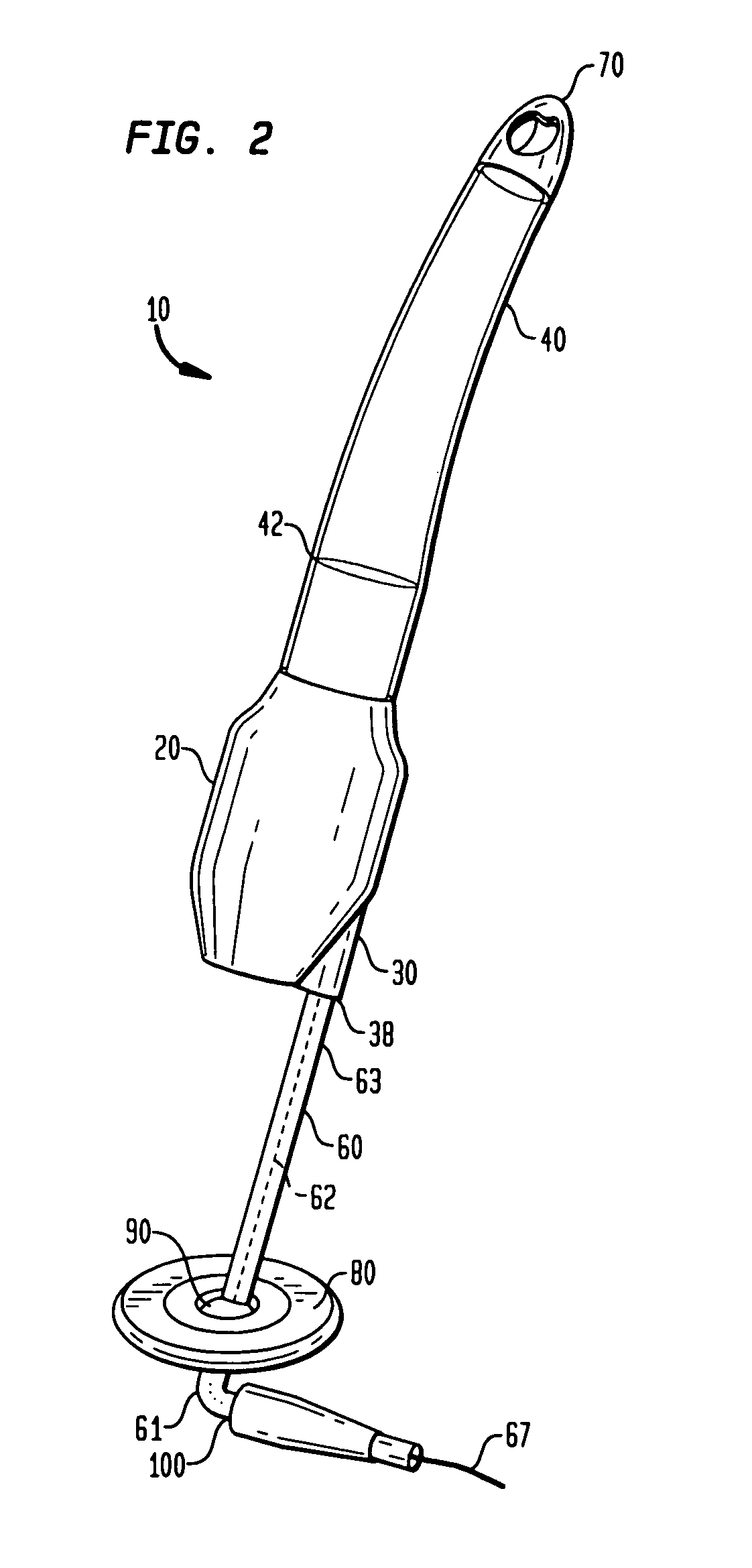
Steerable catheter with preformed distal shape and method for use
InactiveUS6096036AReduce curvatureTransvascular endocardial electrodesSurgical instrument detailsHeart chamberCurve shape
A catheter has a stylet formed of a shape-retentive and resilient material having a preformed curved shape at its distal end resulting in the catheter sheath having the preformed curved shape. The catheter sheath has a plurality of electrodes at its distal end for contacting selected biological tissue for imparting ablation energy thereto. The catheter sheath also has an axially mounted tendon for causing deflection of the distal end. The stylet material permits straightening the catheter sheath during insertion into the patient and advancing the electrodes to the target tissue. Upon removal of the straightening forces, such as by entry into a chamber of the heart, the stylet material resumes its preformed curved distal shape thereby forcing the catheter distal end with the electrodes into the same preformed curved shape. The operator may place the curved distal end into contact with the target tissue and axially move the tendon as desired to gain greater control over the bend in the distal end of the catheter sheath to adjust the radius of curvature of the distal end to obtain greater contact of the electrodes with the heart tissue. Preferably, the stylet is formed of nitinol.
Owner:CARDIAC PACEMAKERS INC
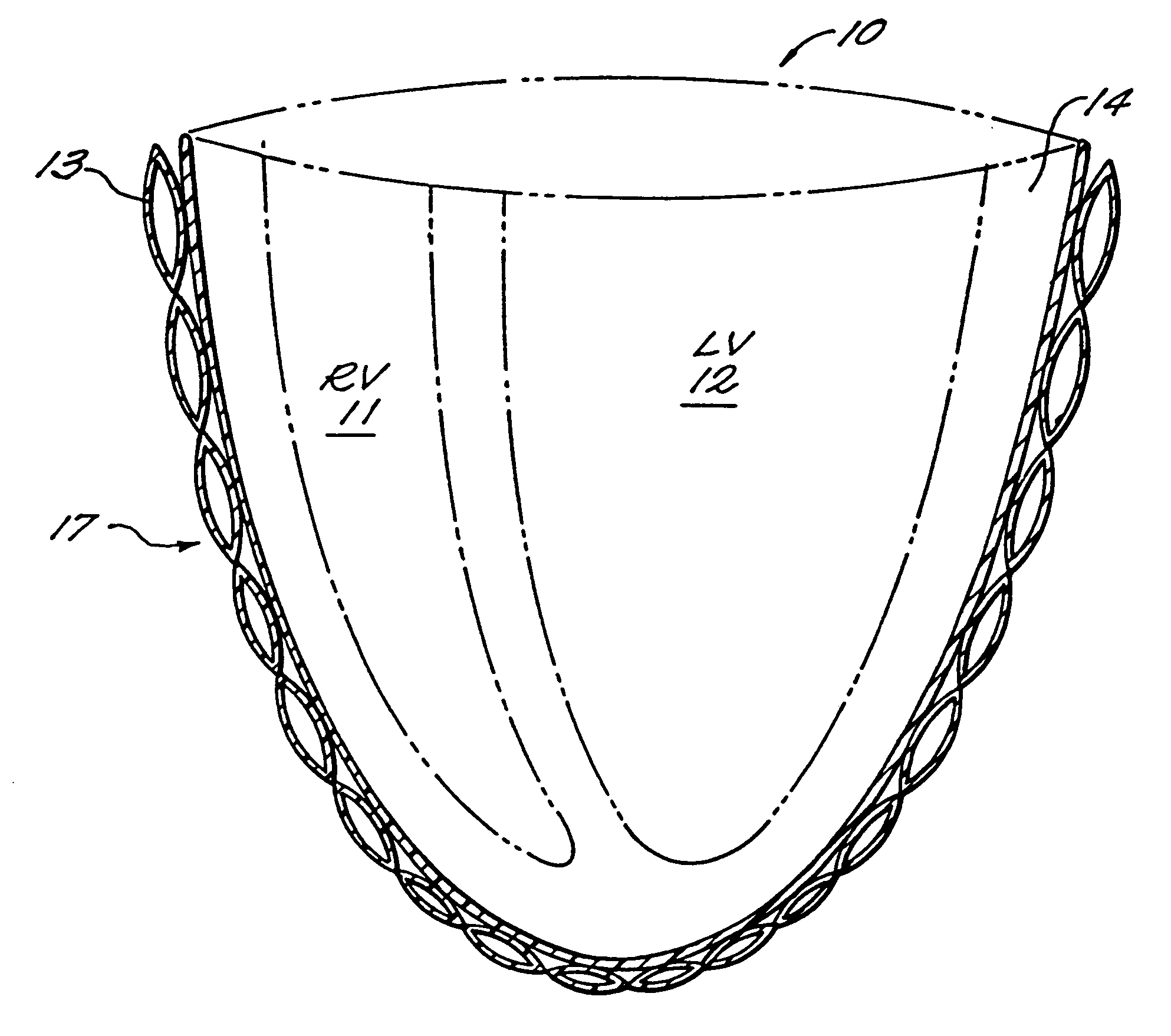
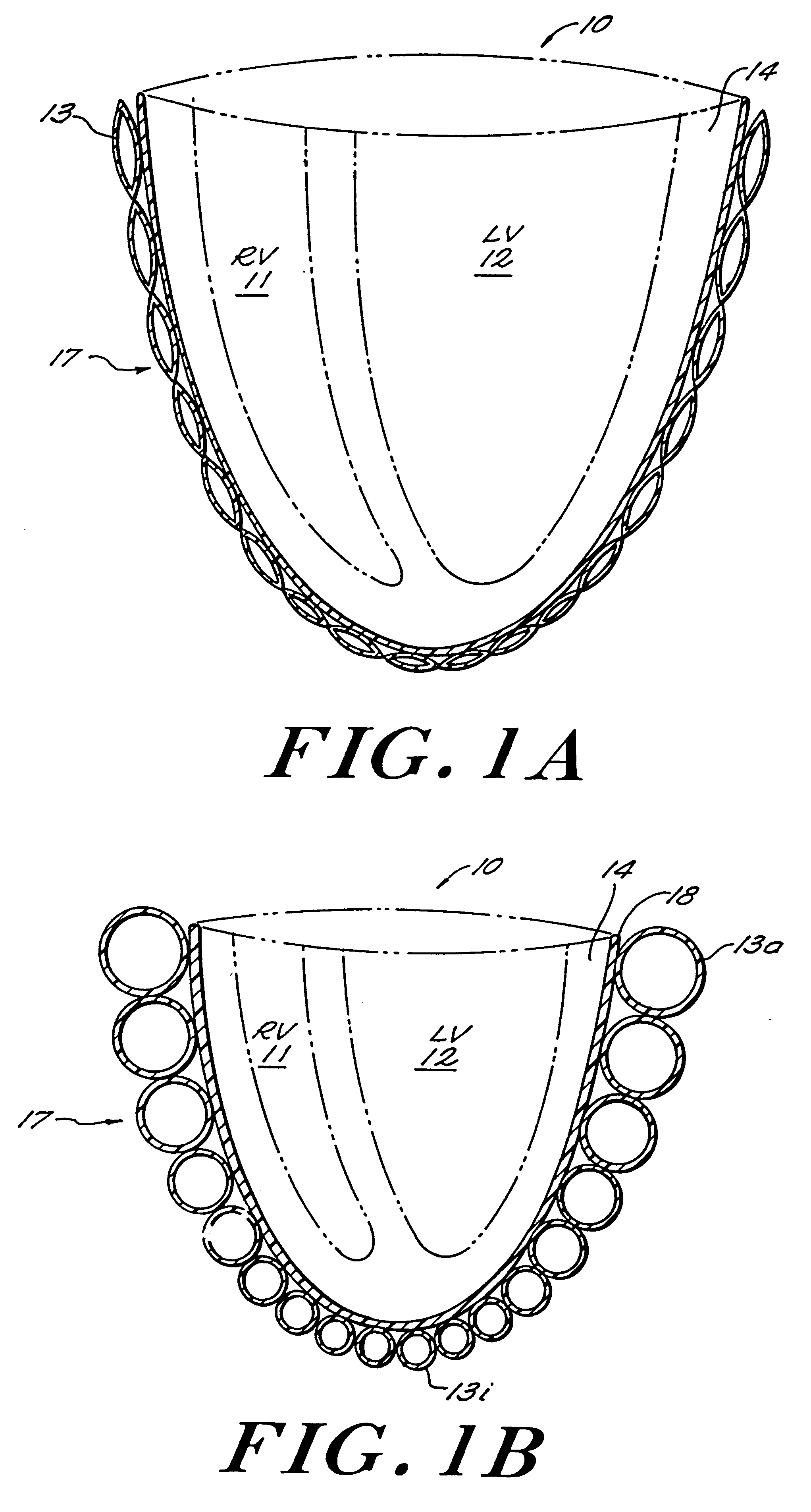
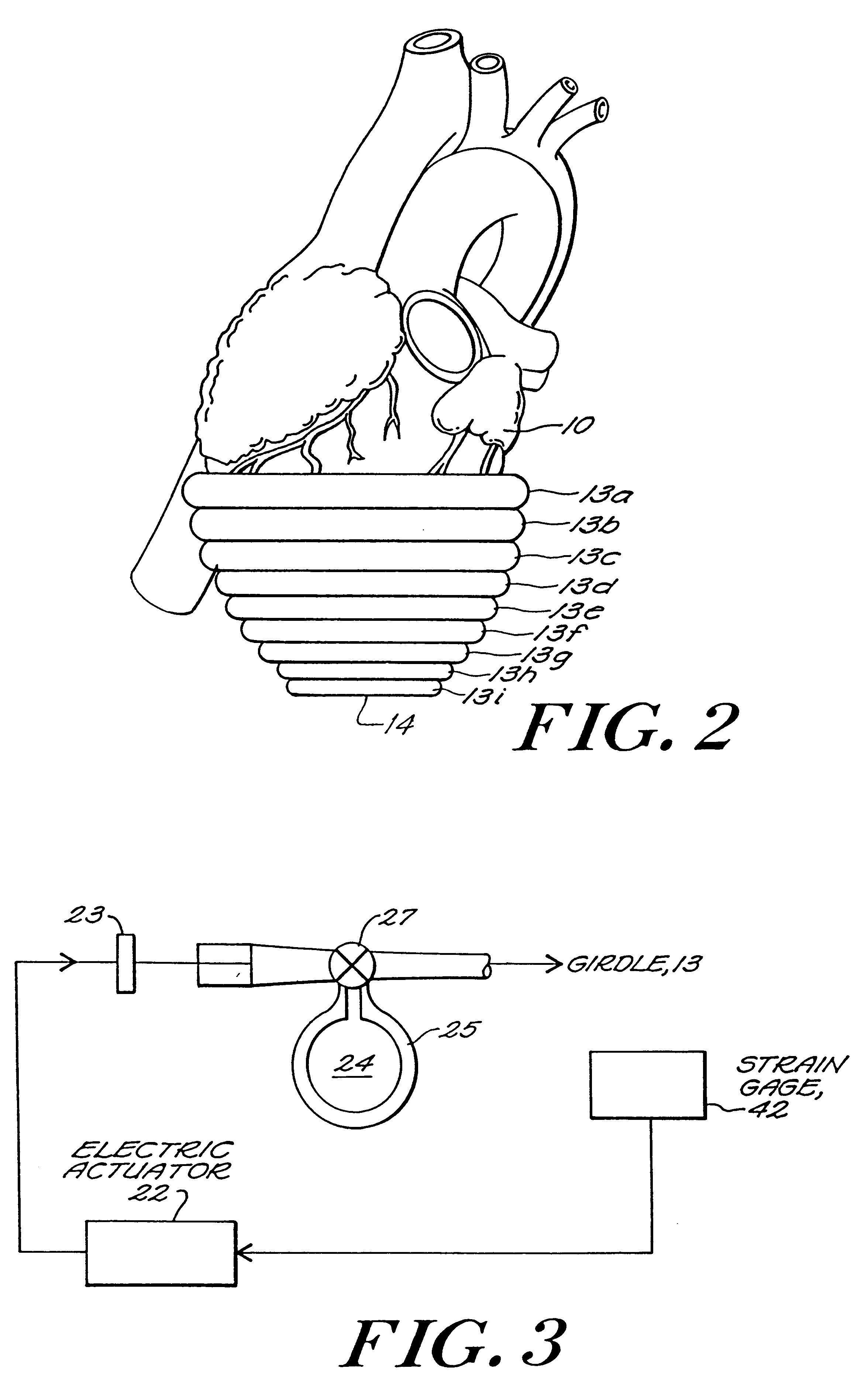
Passive girdle for heart ventricle for therapeutic aid to patients having ventricular dilatation
InactiveUS6224540B1Increased oxygen consumptionLarge increases in the tension-time integralHeart valvesControl devicesVentricular dilatationCardiac muscle
A passive girdle is wrapped around a heart muscle which has dilatation of a ventricle to conform to the size and shape of the heart and to constrain the dilatation during diastole. The girdle is formed of a material and structure that does not expand away from the heart but may, over an extended period of time be decreased in size as dilatation decreases.
Owner:ABIOMED
Systems for heart treatment
InactiveUS20050197692A1Decreasing wall stressReinforce wallSuture equipmentsElectrotherapyLeft ventricular sizeTherapeutic treatment
Described are devices and methods for treating degenerative, congestive heart disease and related valvular dysfunction. Percutaneous and minimally invasive surgical tensioning structures offer devices that mitigate changes in the ventricular structure (i.e., remodeling) and deterioration of global left ventricular performance related to tissue damage precipitating from ischemia, acute myocardial infarction (AMI) or other abnormalities. These tensioning structures can be implanted within various major coronary blood-carrying conduit structures (arteries, veins and branching vessels), into or through myocardium, or into engagement with other anatomic structures that impact cardiac output to provide tensile support to the heart muscle wall which resists diastolic filling pressure while simultaneously providing a compressive force to the muscle wall to limit, compensate or provide therapeutic treatment for congestive heart failure and / or to reverse the remodeling that produces an enlarged heart.
Owner:EXTENSIA MEDICAL
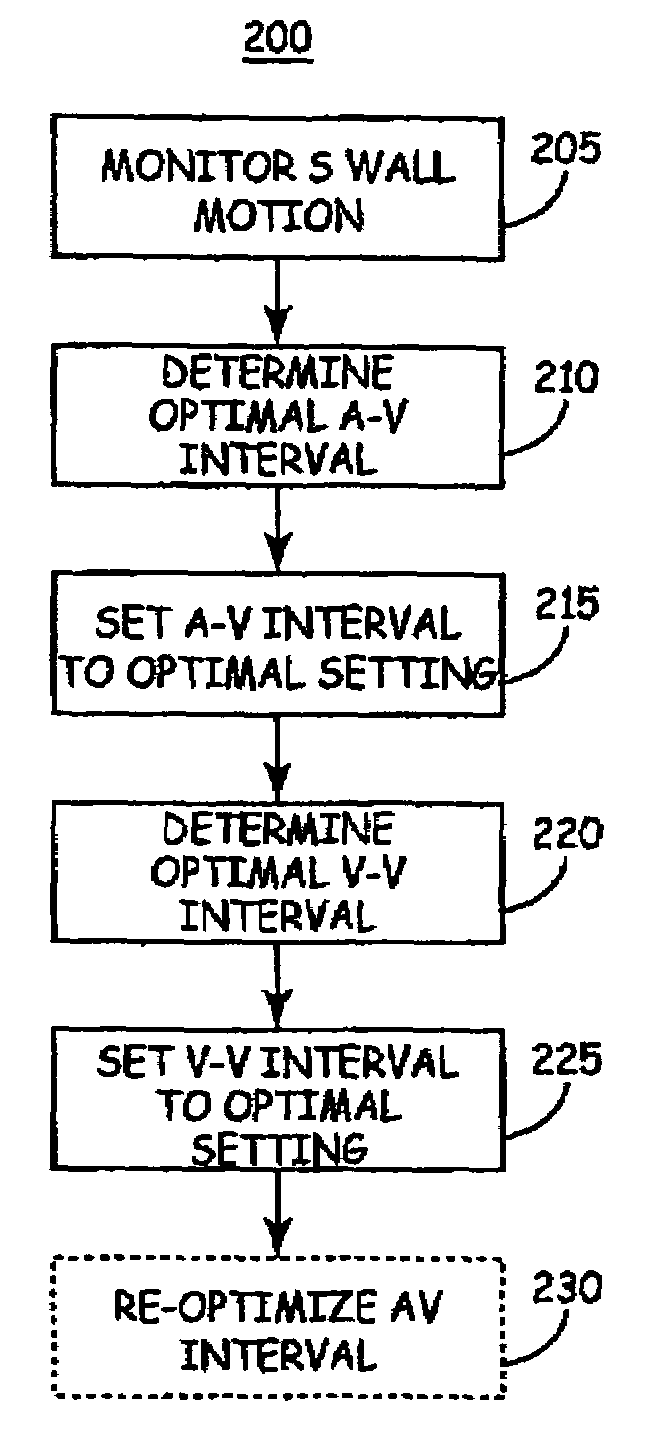
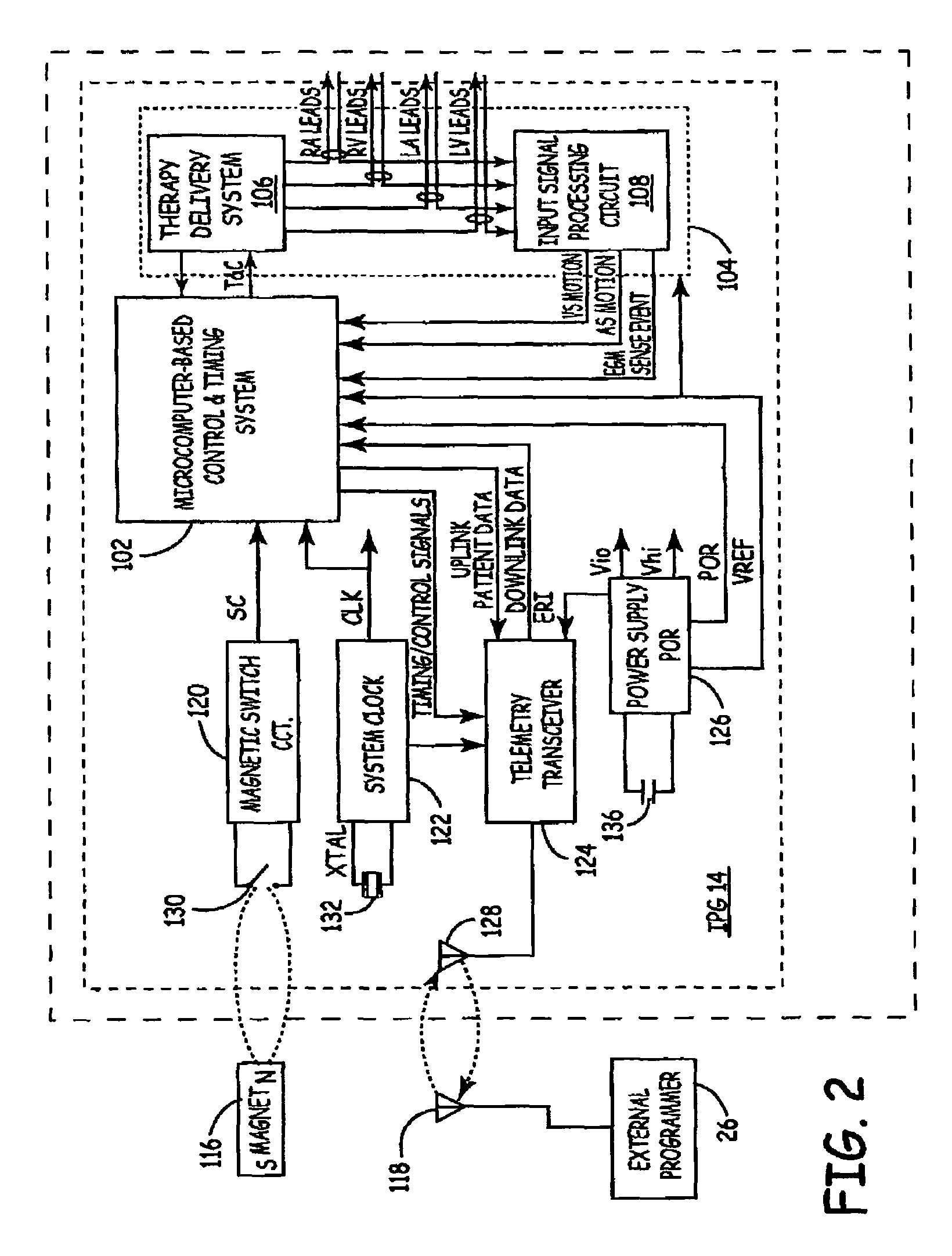
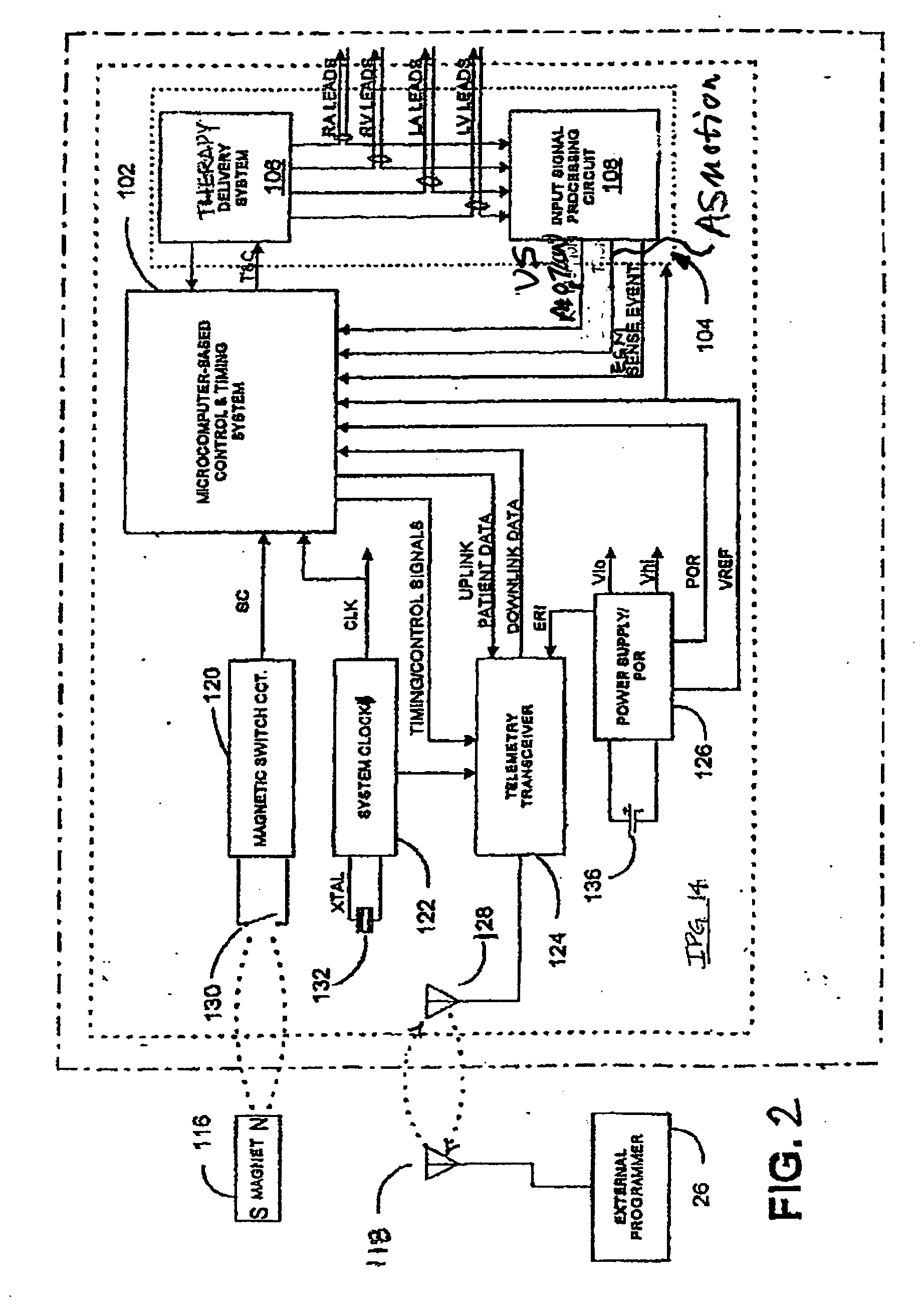
Method of optimizing cardiac resynchronization therapy using sensor signals of septal wall motion
Owner:MEDTRONIC INC
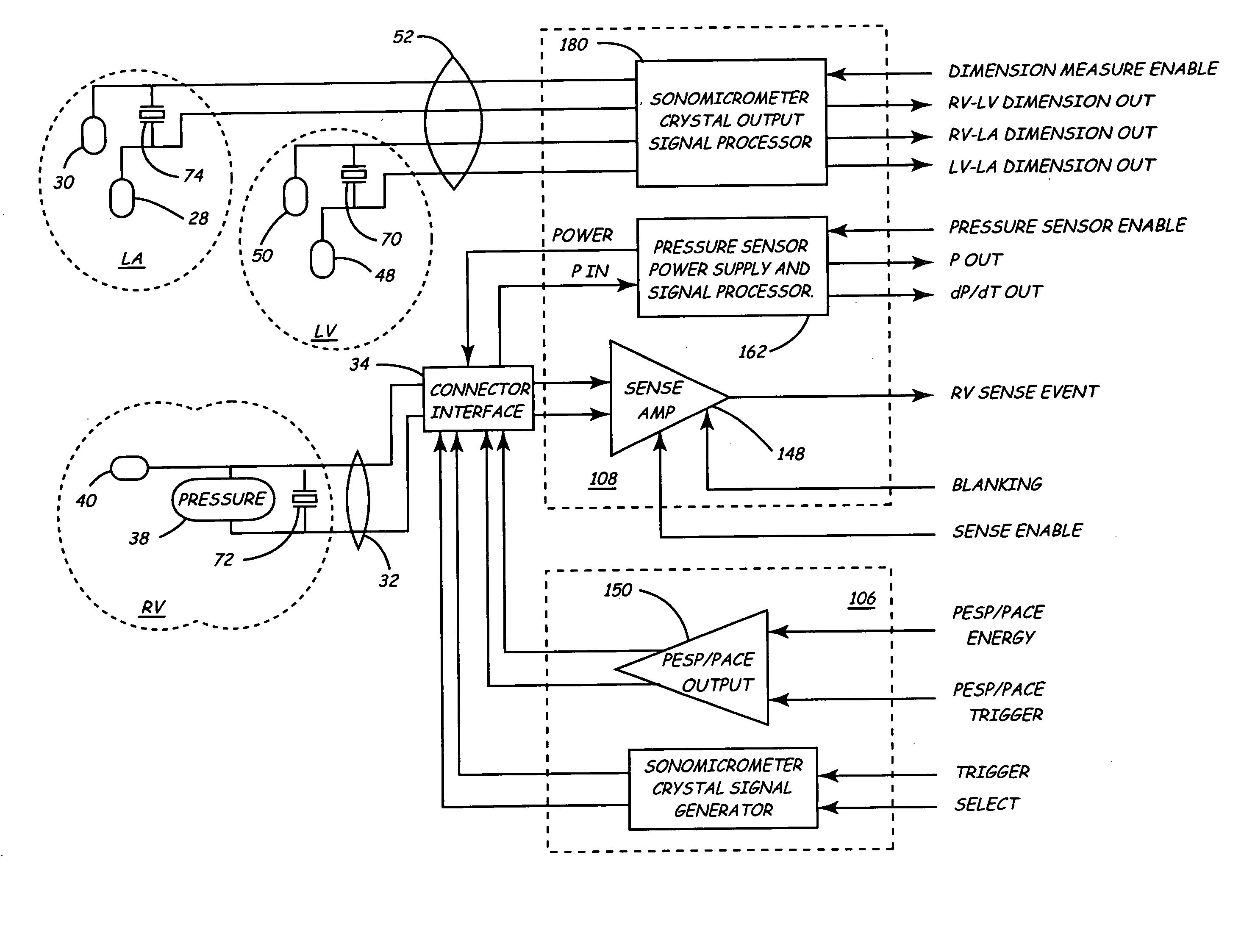
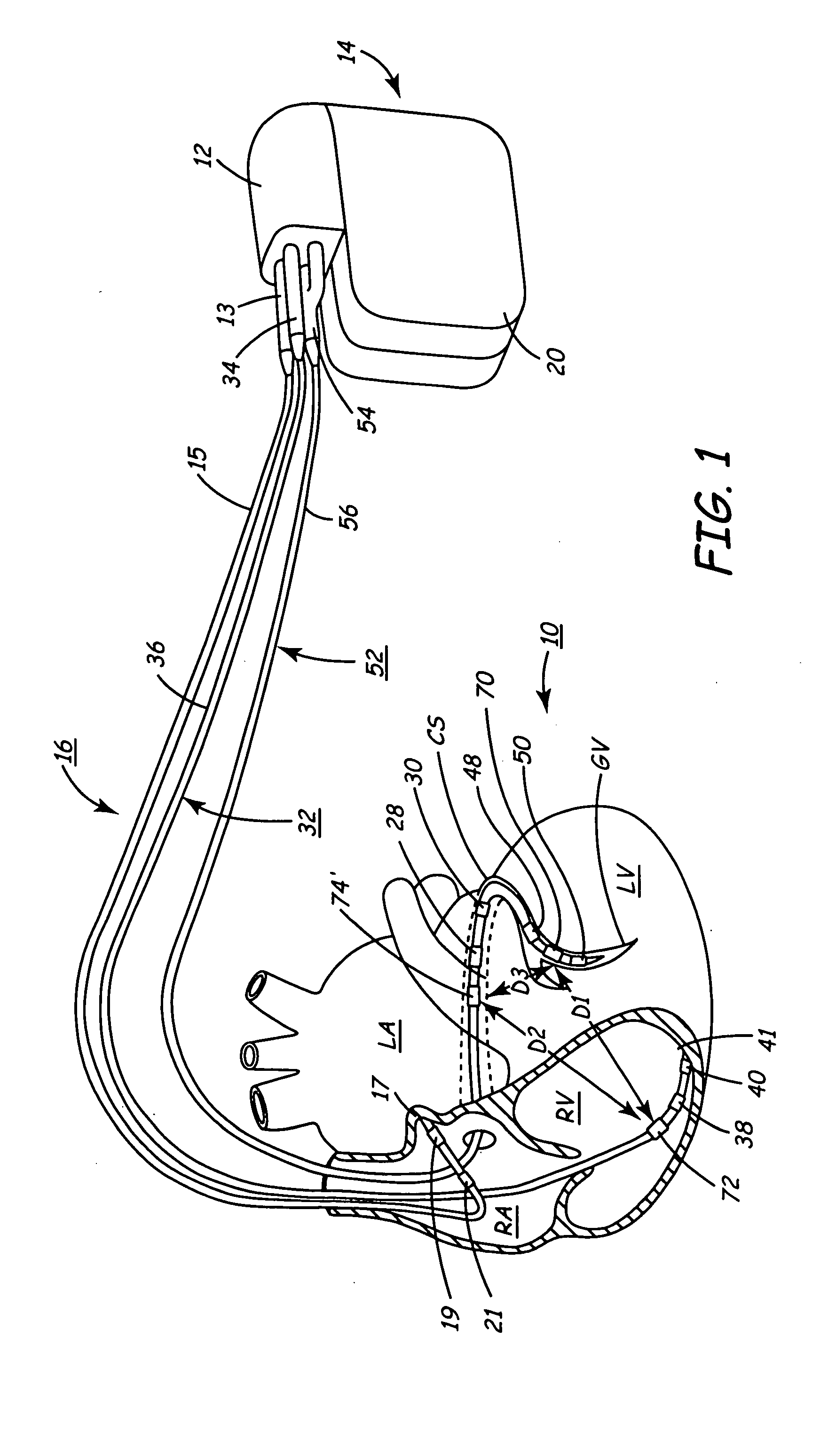
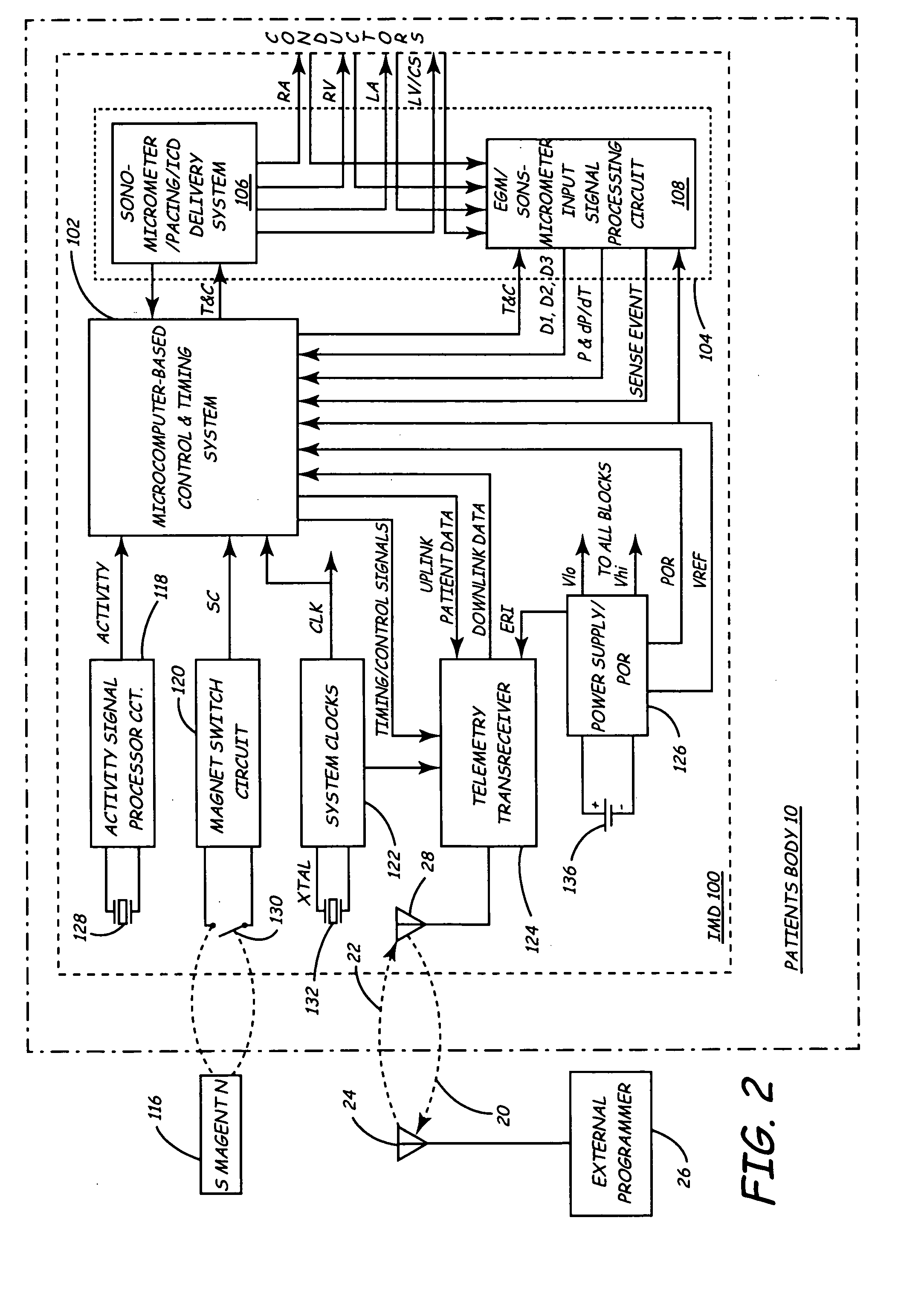
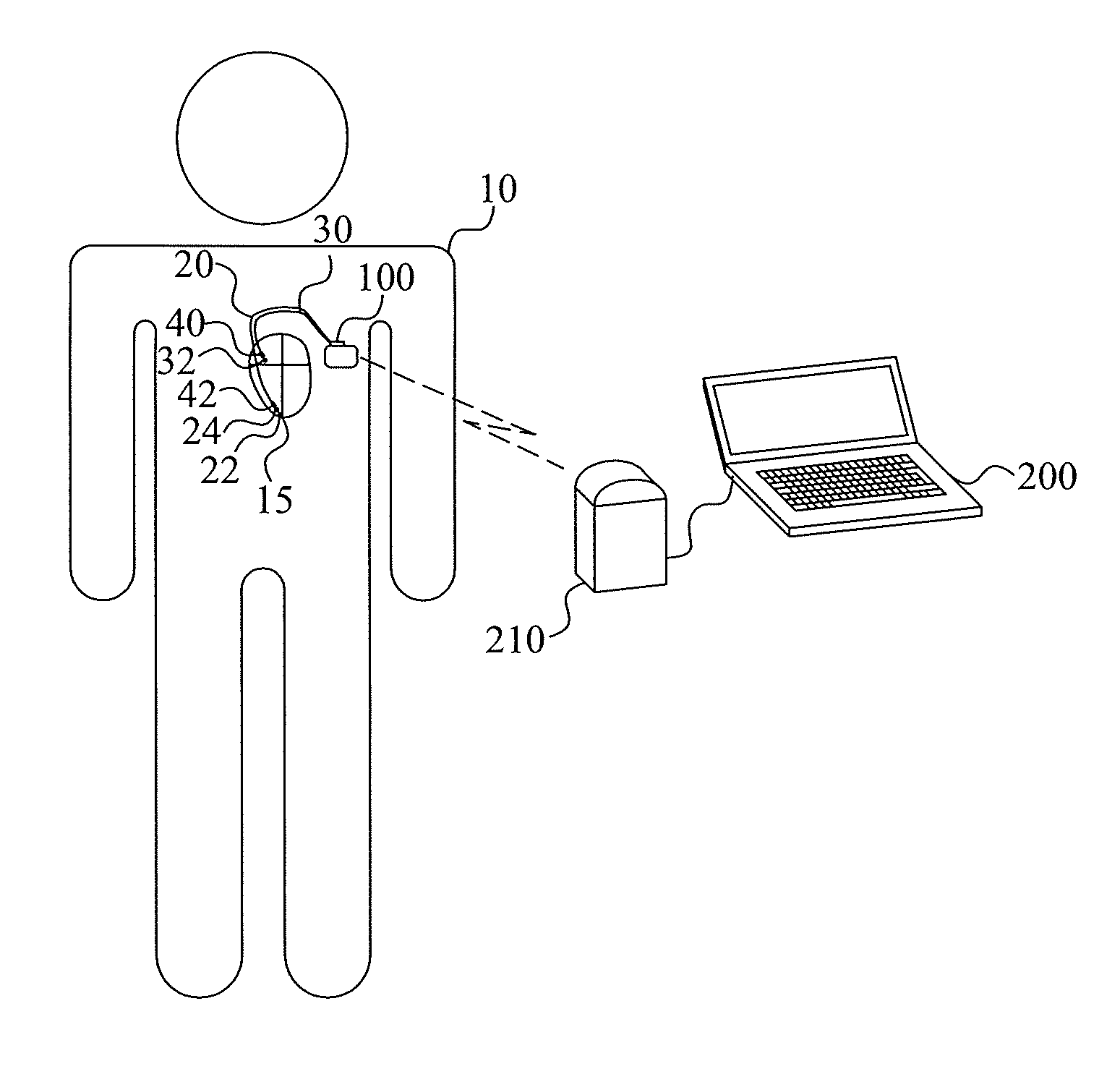
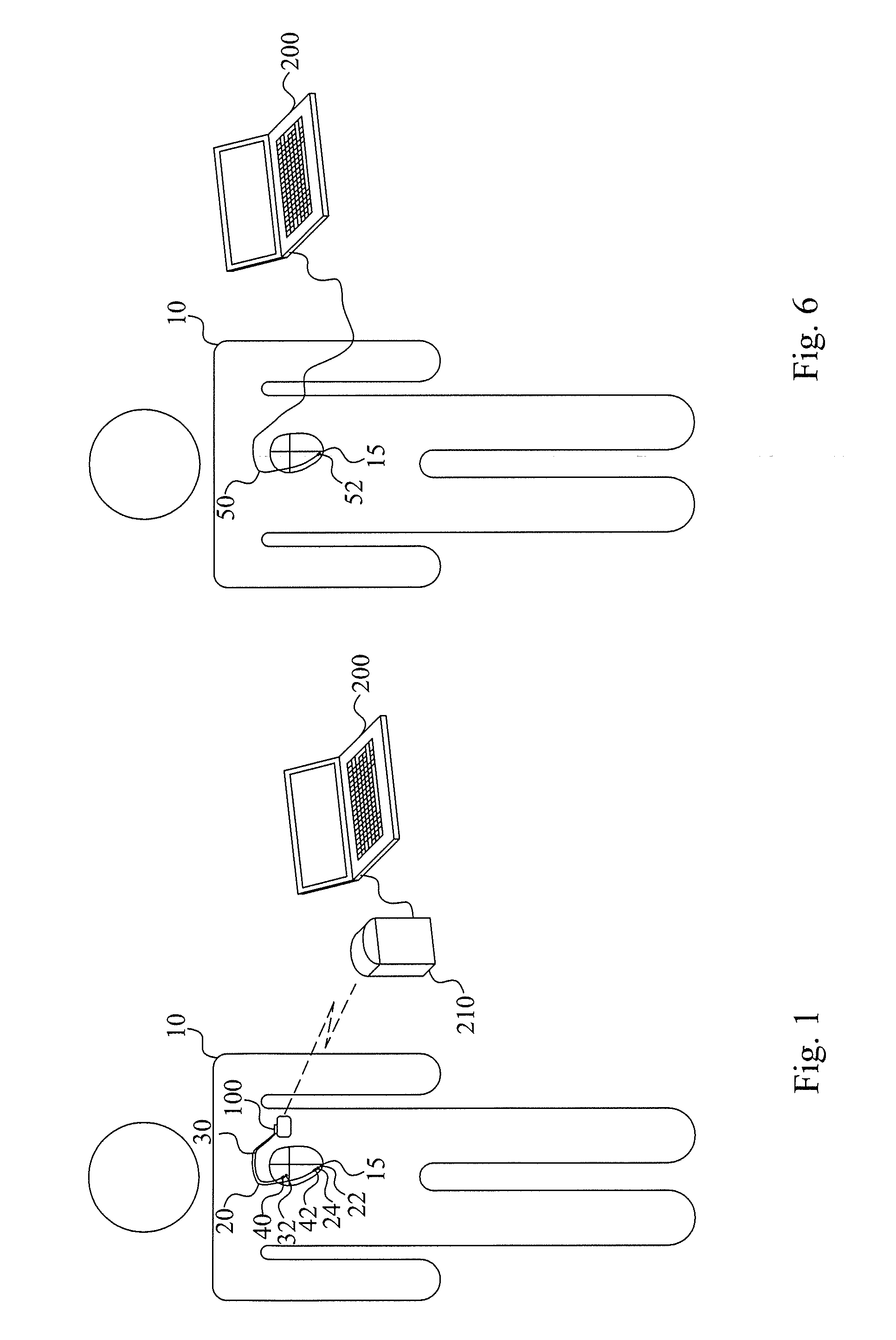
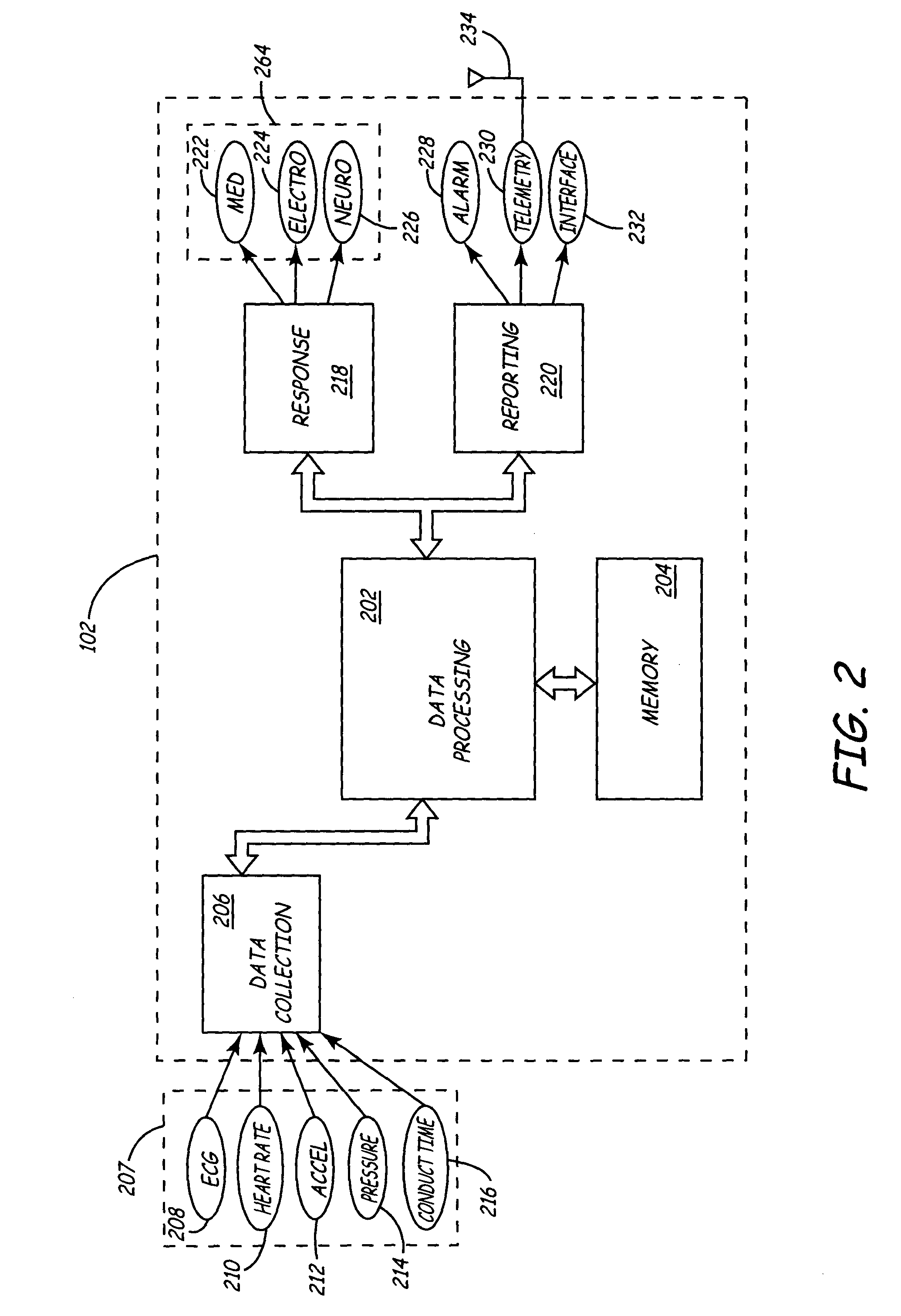
Implantable medical device for monitoring cardiac blood pressure and chamber dimension
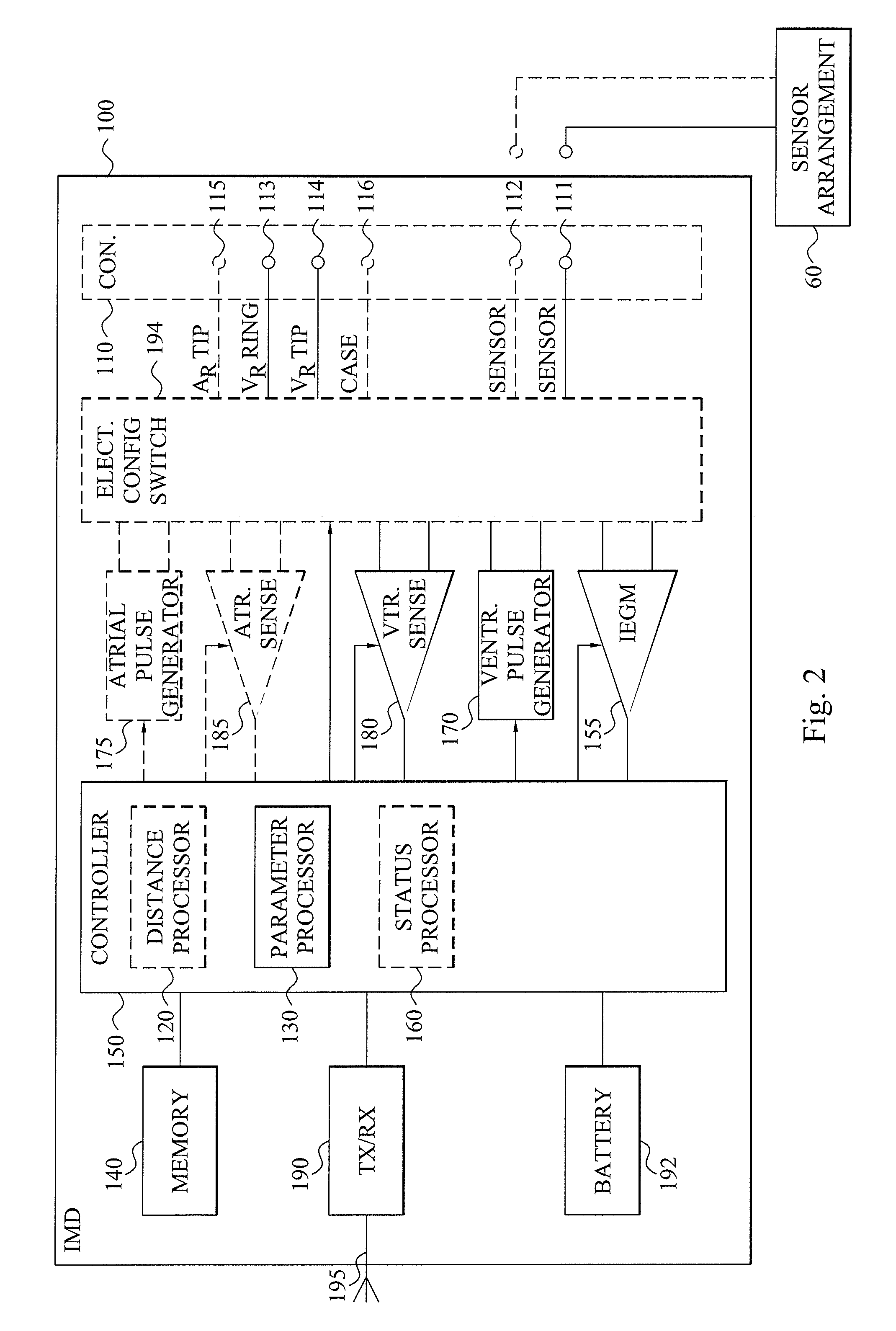
InactiveUS20050027323A1Maximize cardiac outputConvenient timeCatheterHeart stimulatorsSonificationHeart chamber
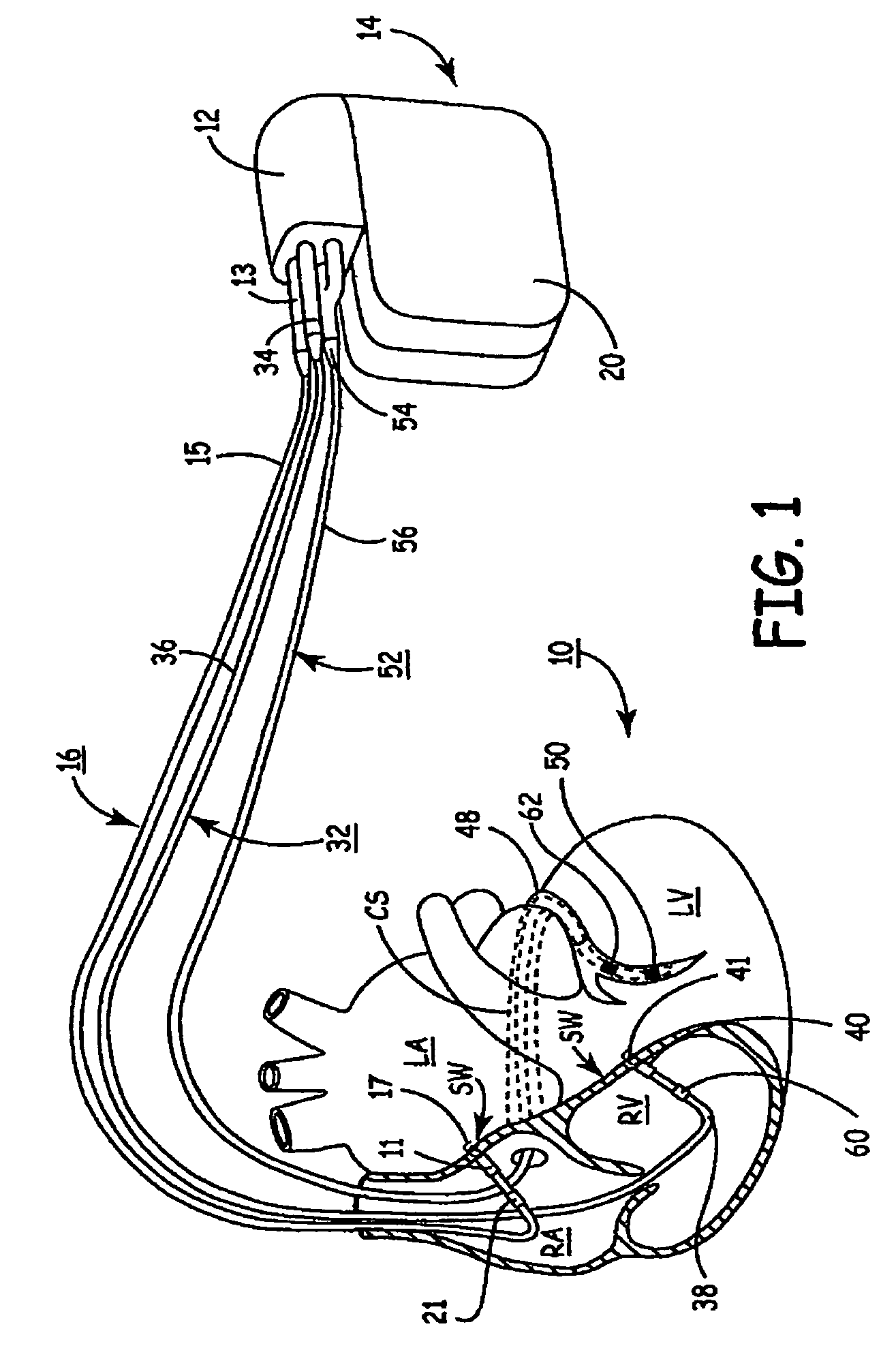
Implantable medical devices (IMDs) for monitoring signs of acute or chronic cardiac heart failure by measuring cardiac blood pressure and mechanical dimensions of the heart and providing multi-chamber pacing optimized as a function of measured blood pressure and dimensions are disclosed. The dimension sensor or sensors comprise at least a first sonomicrometer piezoelectric crystal mounted to a first lead body implanted into or in relation to one heart chamber that operates as an ultrasound transmitter when a drive signal is applied to it and at least one second sonomicrometer crystal mounted to a second lead body implanted into or in relation to a second heart chamber that operates as an ultrasound receiver. The ultrasound receiver converts impinging ultrasound energy transmitted from the ultrasound transmitter through blood and heart tissue into an electrical signal. The time delay between the generation of the transmitted ultrasound signal and the reception of the ultrasound wave varies as a function of distance between the ultrasound transmitter and receiver which in turn varies with contraction and expansion of a heart chamber between the first and second sonomicrometer crystals. One or more additional sonomicrometer piezoelectric crystal can be mounted to additional lead bodies such that the distances between the three or more sonomicrometer crystals can be determined. In each case, the sonomicrometer crystals are distributed about a heart chamber such that the distance between the separated ultrasound transmitter and receiver crystal pairs changes with contraction and relaxation of the heart chamber walls.
Owner:MEDTRONIC INC
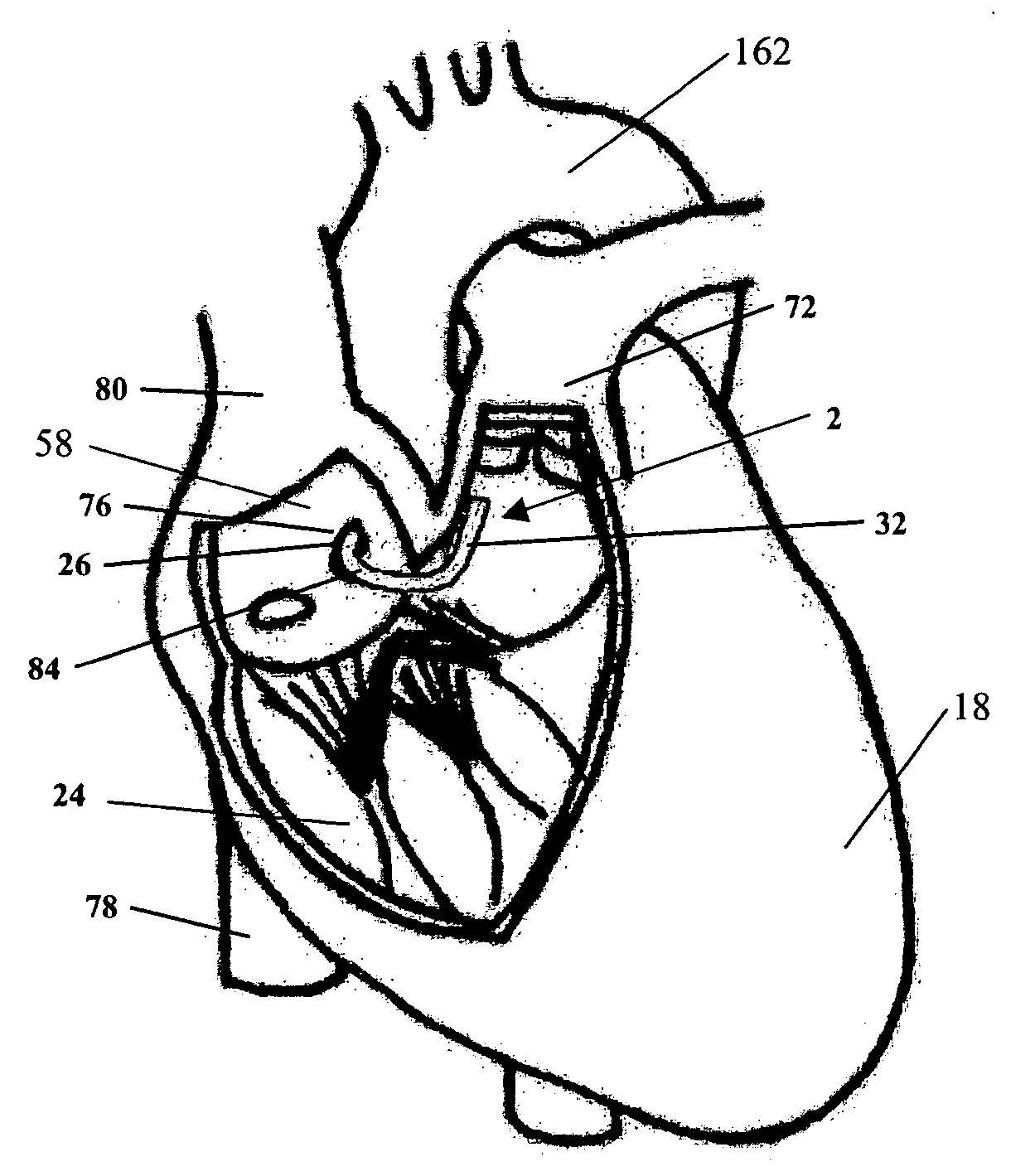
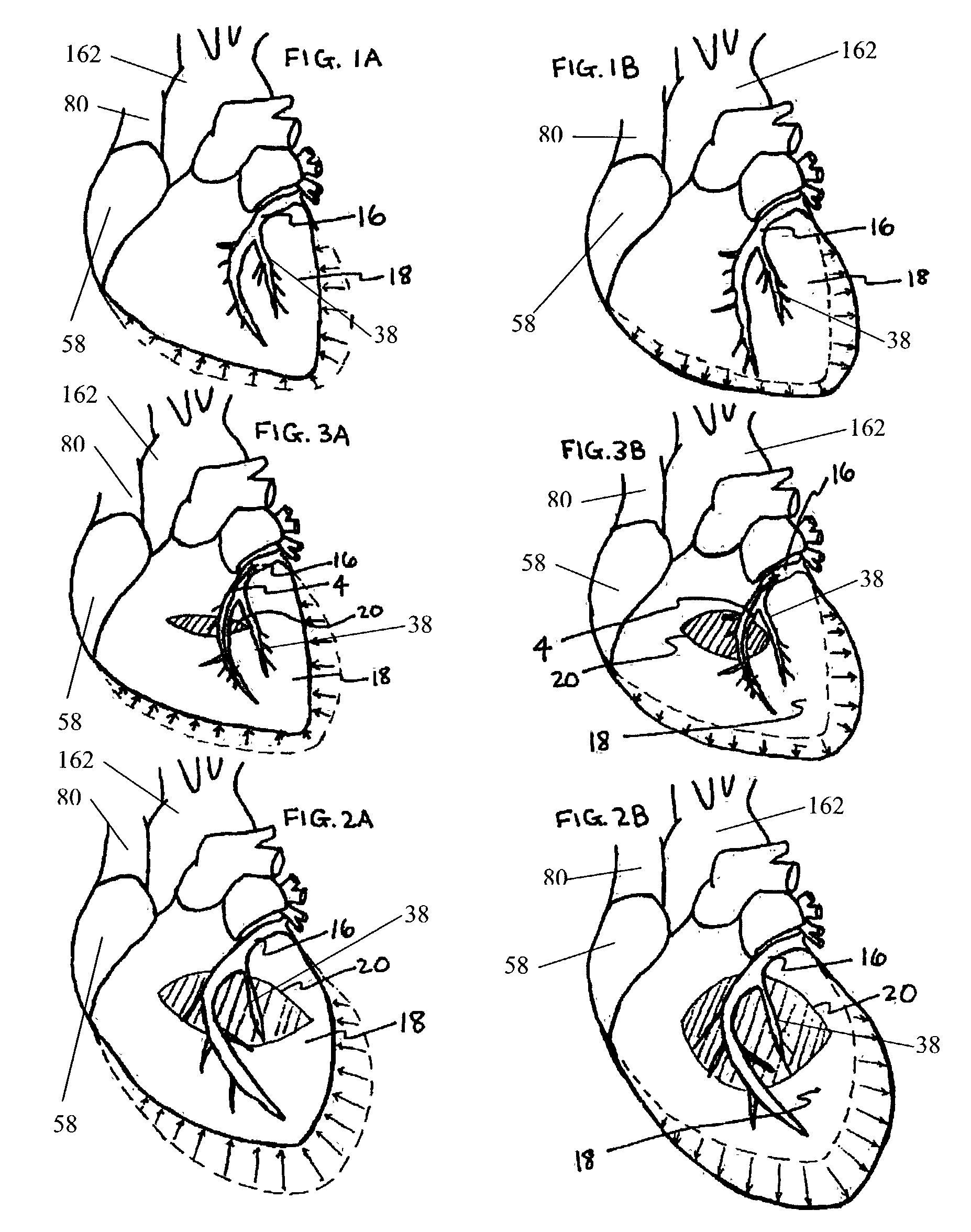
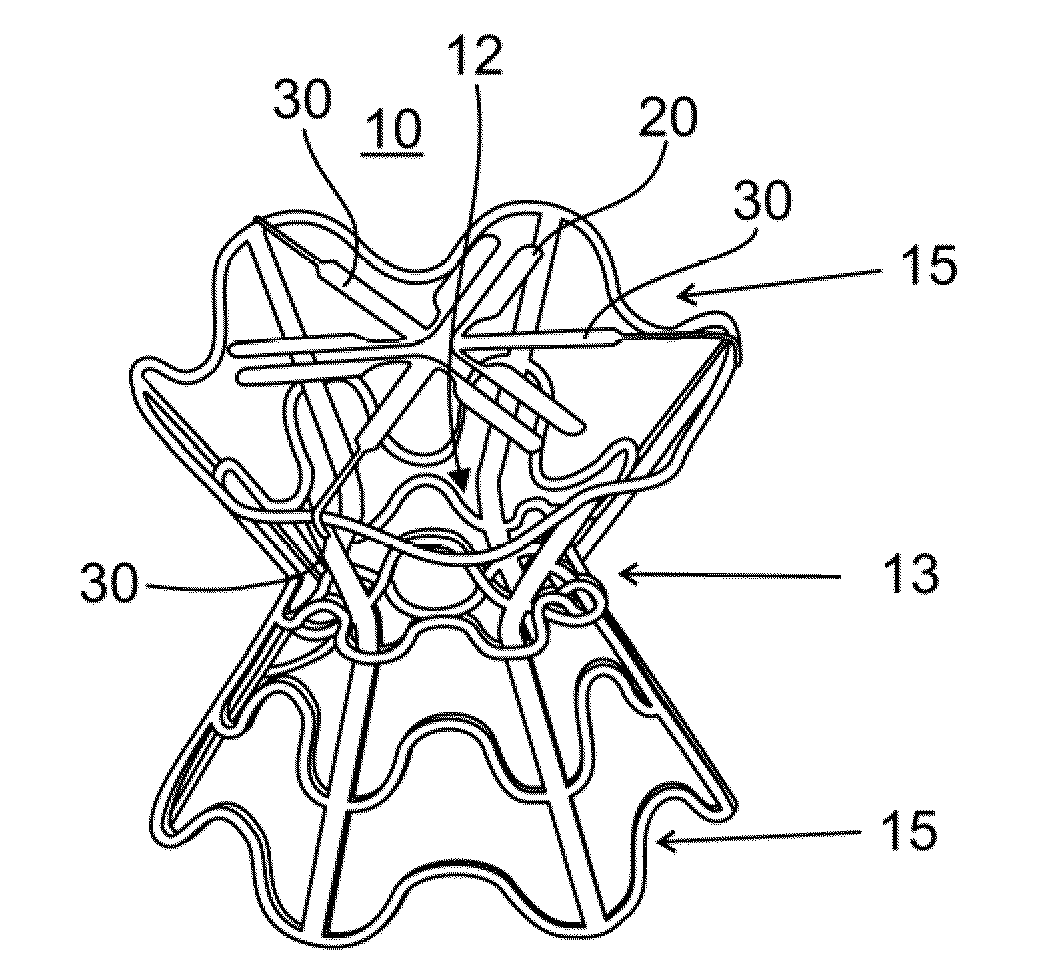
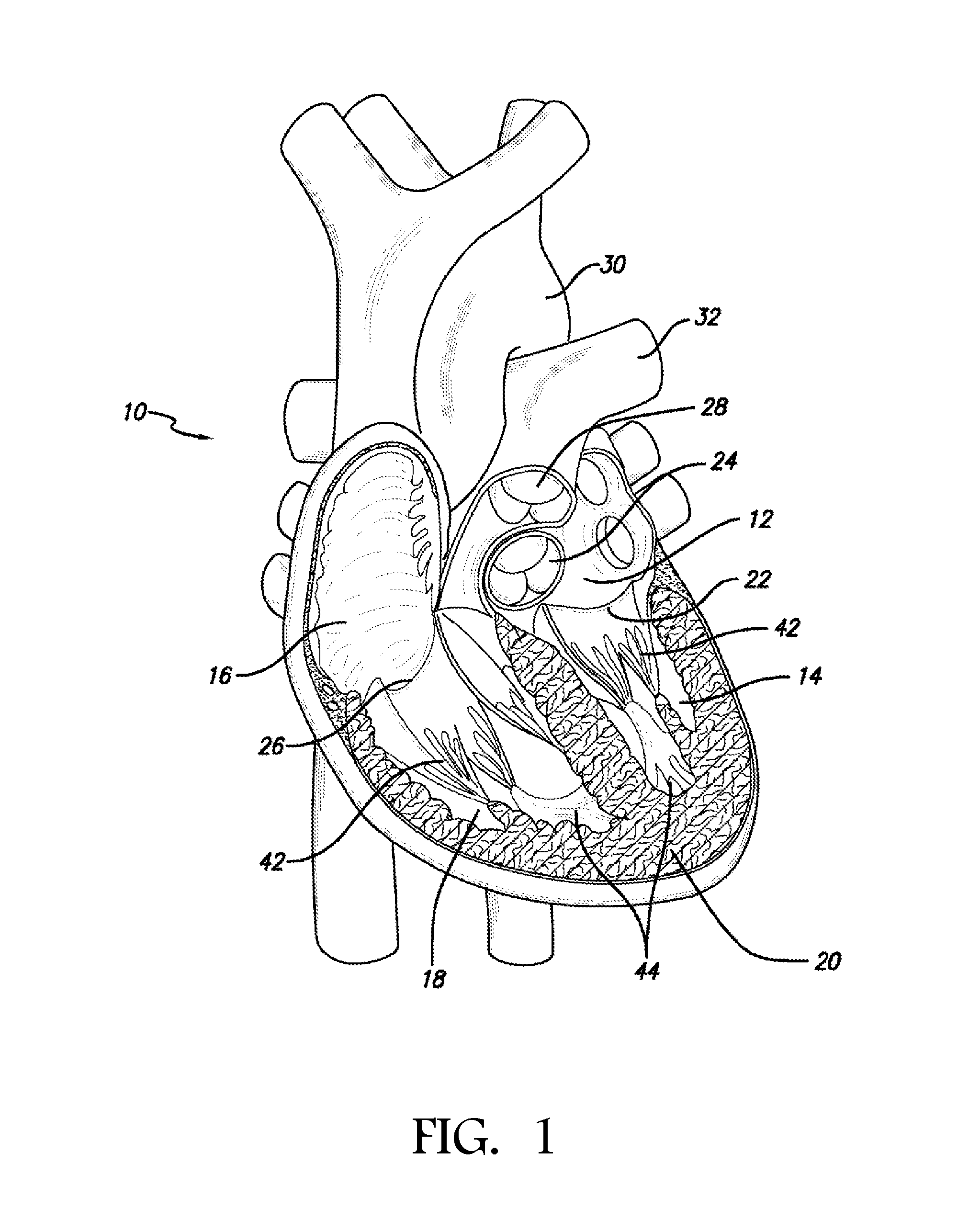
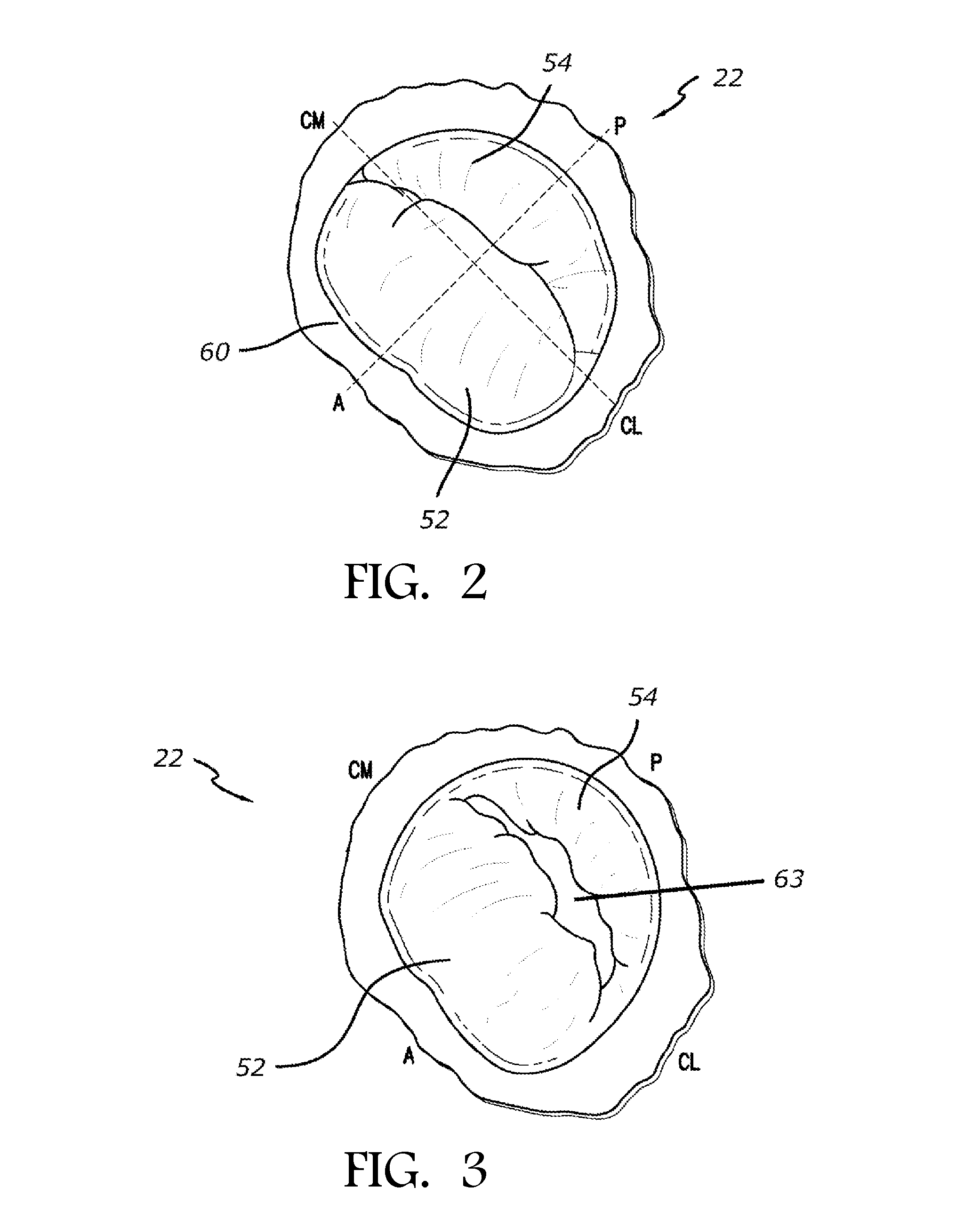
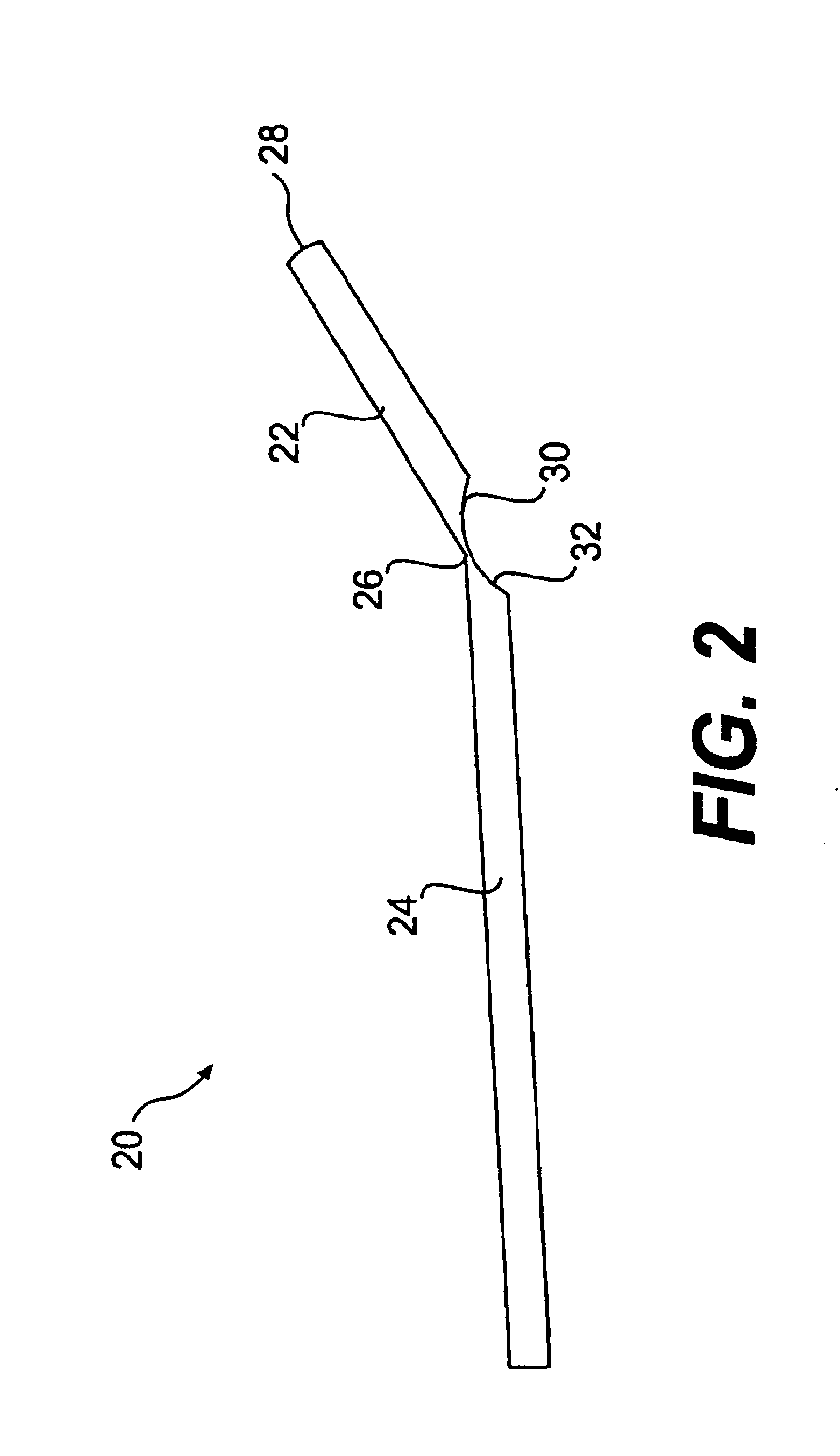
Mitral valve treatment techniques
ActiveUS8608797B2Enhance fibrosisReduce distanceBone implantAnnuloplasty ringsCouplingMitral valve leaflet
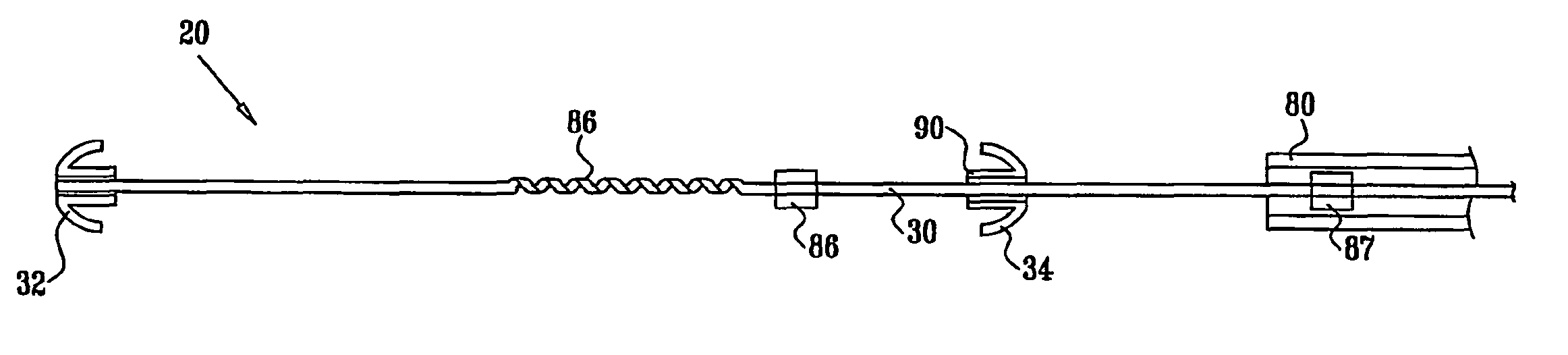
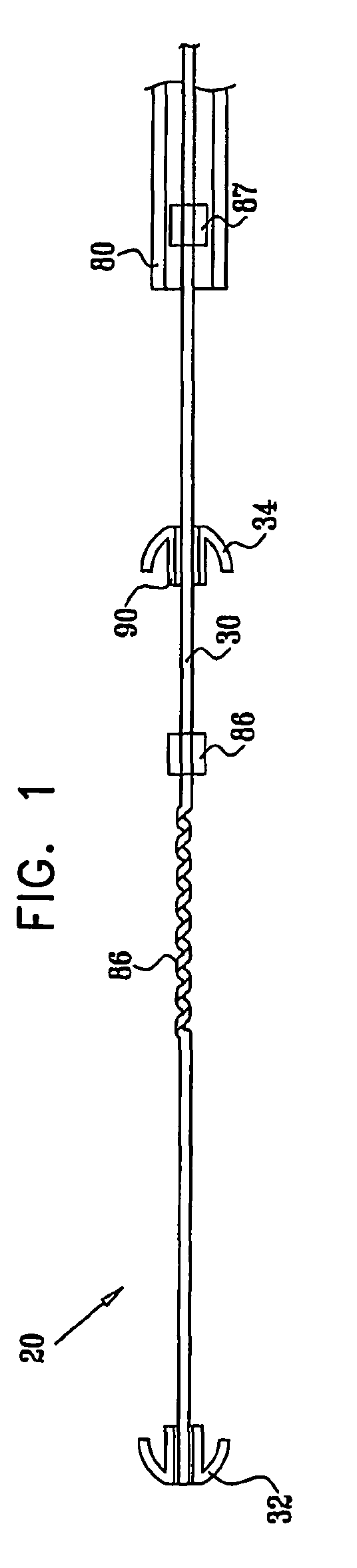
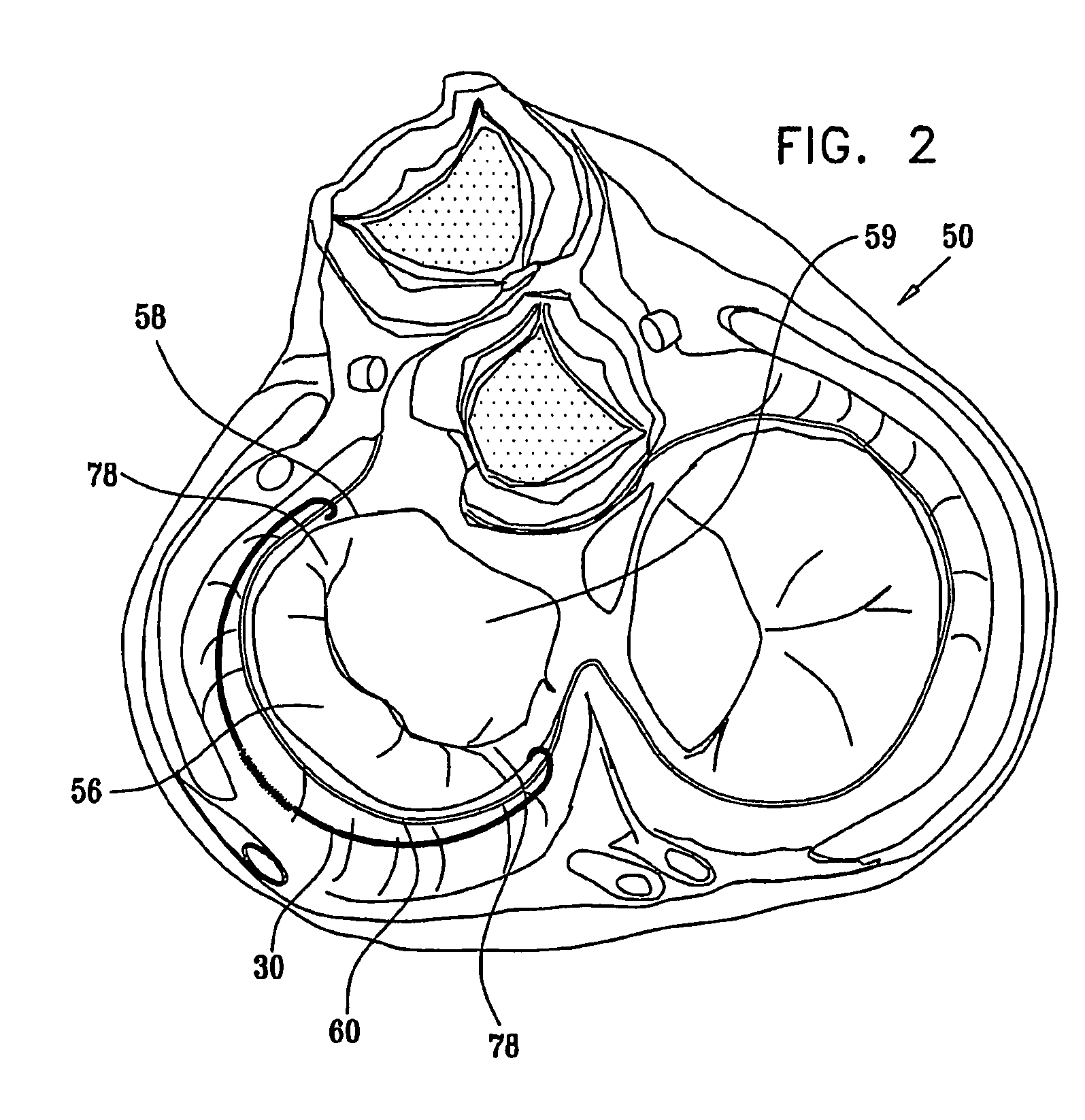
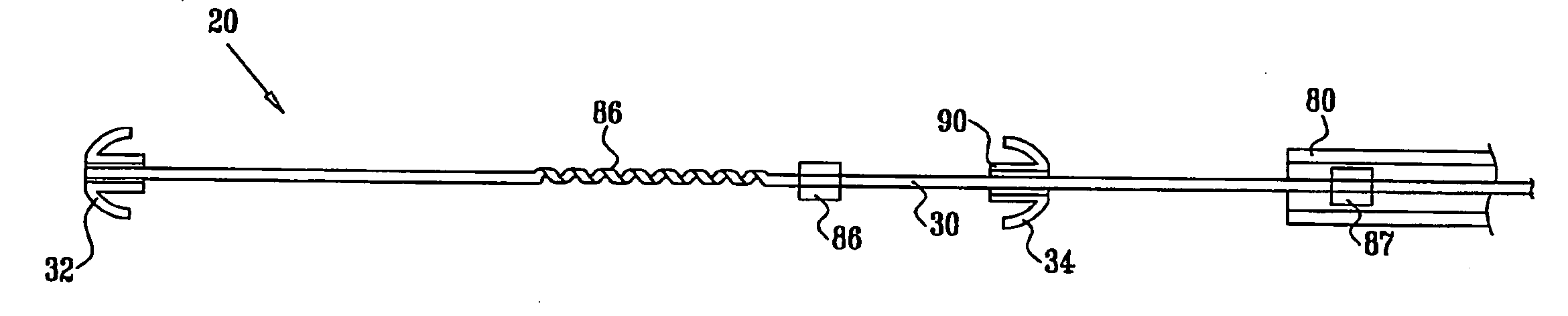
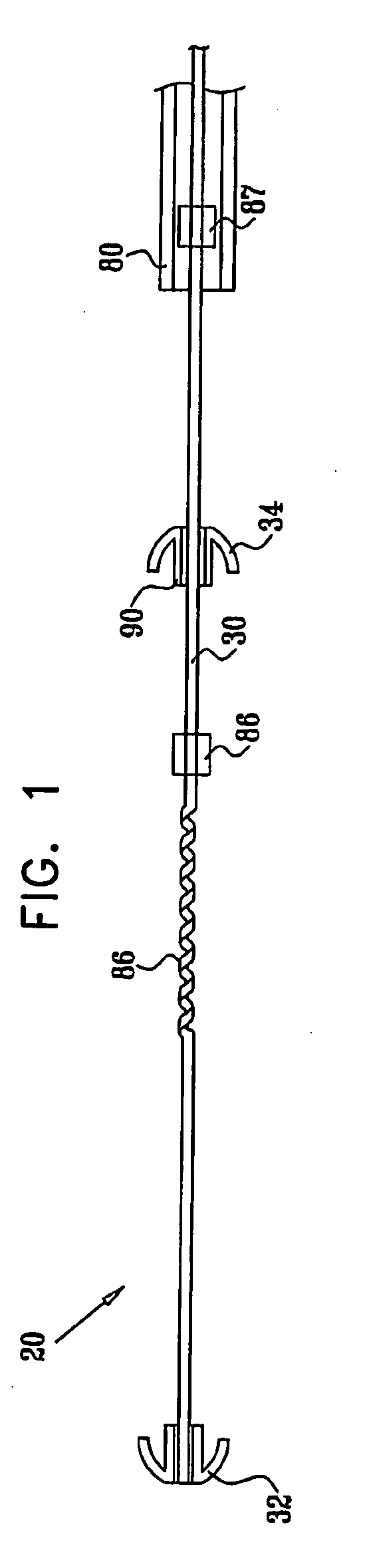
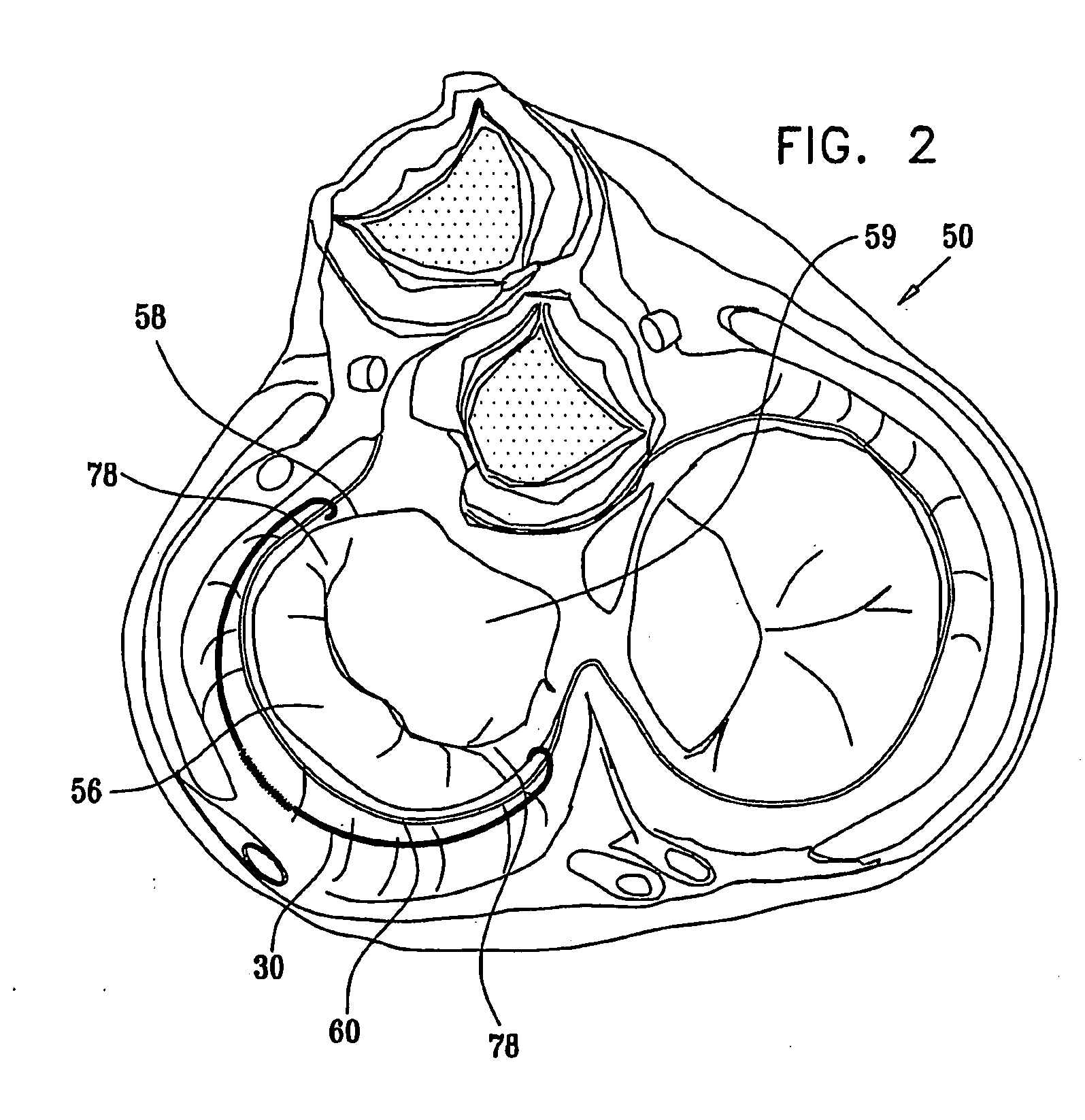
Apparatus (20) is provided for treating mitral valve regurgitation, including a band (30) having distal and proximal ends, the band (30) adapted to be placed: around between 90 and 270 degrees of a mitral valve (58), including around at least a portion of a posterior cusp (56) of the valve (58), in a space defined by (a) a ventricular wall (70), (b) a ventricular surface of the posterior cusp (56) in a vicinity of an annulus (60) of the mitral valve (58), and (c) a plurality of third-order chordae tendineae (74). The apparatus (20) further includes distal and proximal coupling elements (32, 34), coupled to the band (30) at the distal and proximal ends thereof, respectively, and adapted to be coupled to a first chorda tendinea and a second chorda tendinea, respectively, each of the first and second chordae tendineae selected from the group consisting of: one of the plurality of third-order chordae tendineae (74), and a first-order chorda tendinea that inserts on a commissural cusp (78) of the mitral valve (58). Additional embodiments are also described.
Owner:VALTECH CARDIO LTD
Methods and devices for altering blood flow through the left ventricle
ActiveUS20050015109A1Lower the volumeInefficient geometry for pumpingHeart valvesDilatorsBlood flowMaterial Perforation
An element is expanded in the left ventricle to isolate part of the left ventricle. The element has a generally convex outer surface and an apex which together define a desired geometry of the left ventricle. The isolated part of the wall of the left ventricle may be left so that the wall naturally forms around the element or the isolated portion of the ventricle may be evacuated and / or filled. The element may also be used to isolate part of the left ventricle containing a ventricular septal defect or other perforation or opening in the ventricular wall.
Owner:KARDIUM
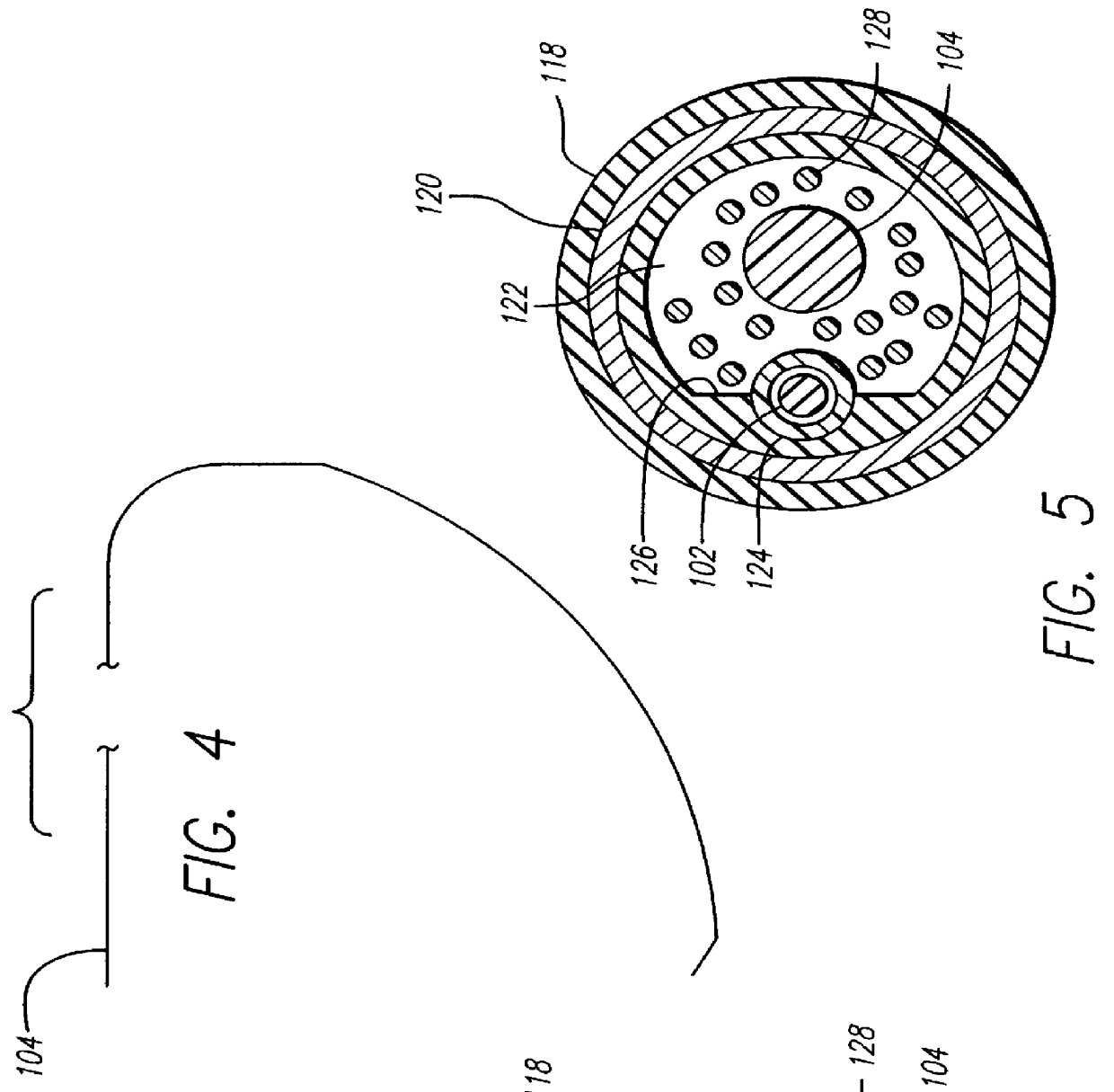
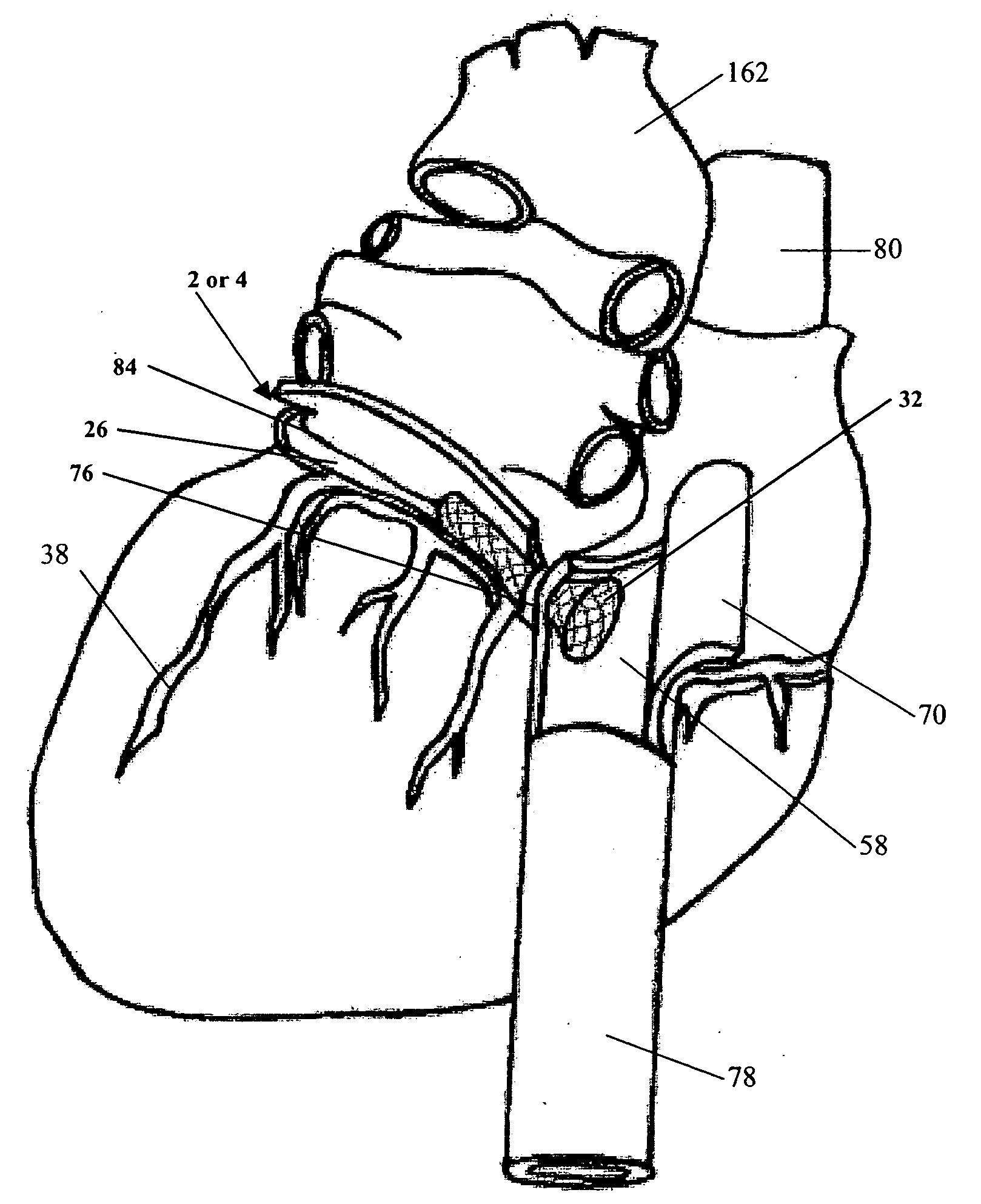
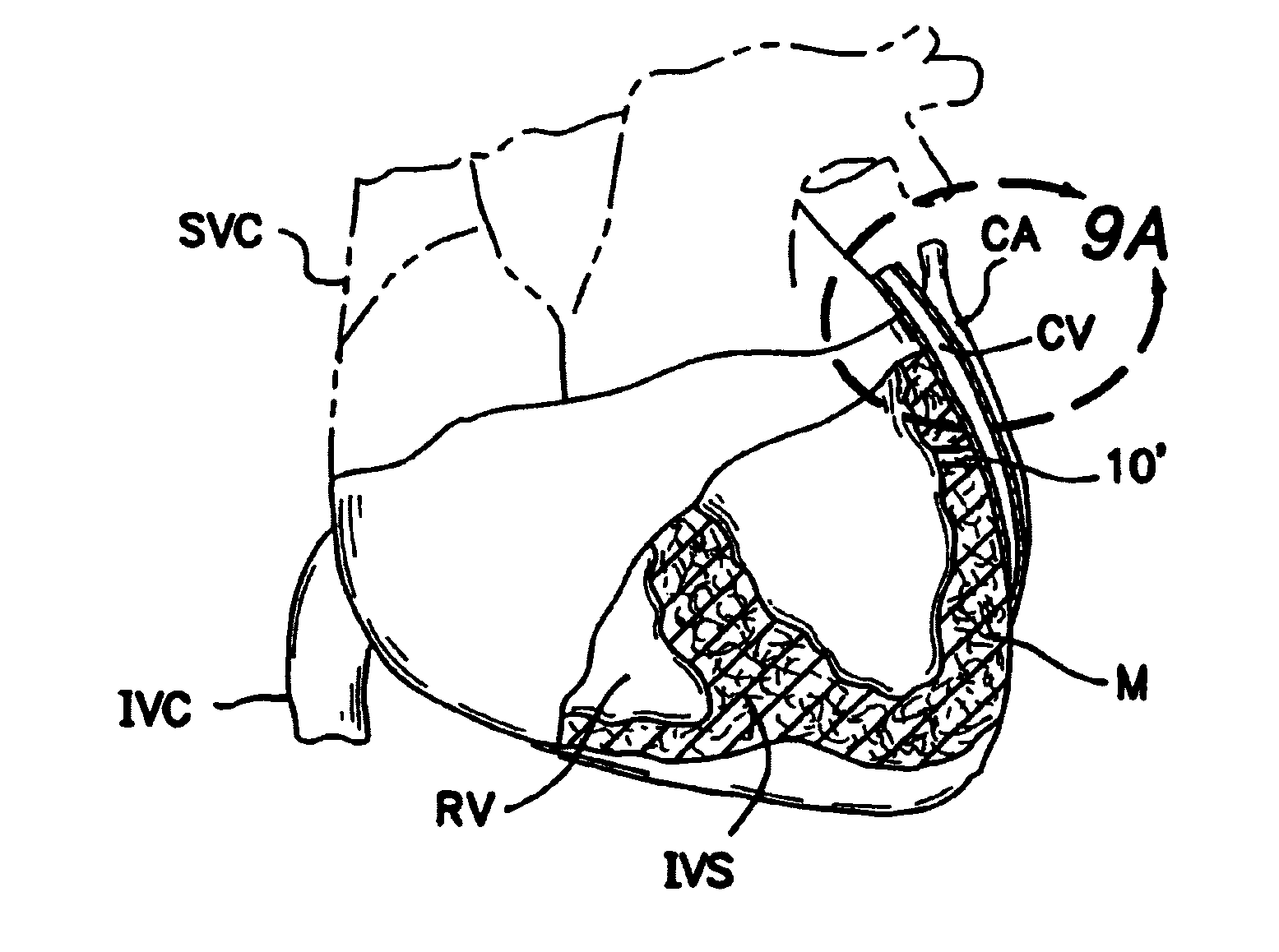
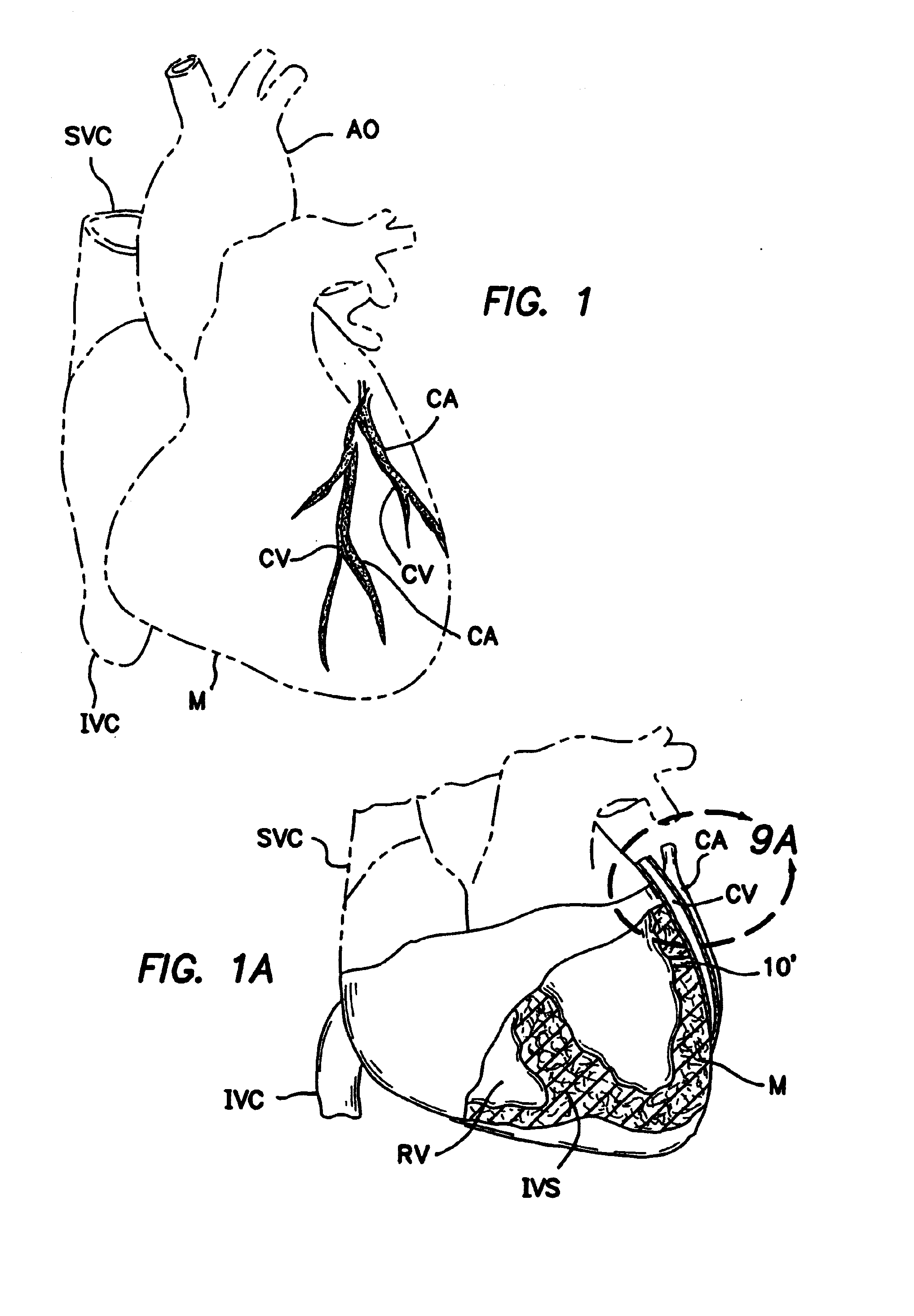
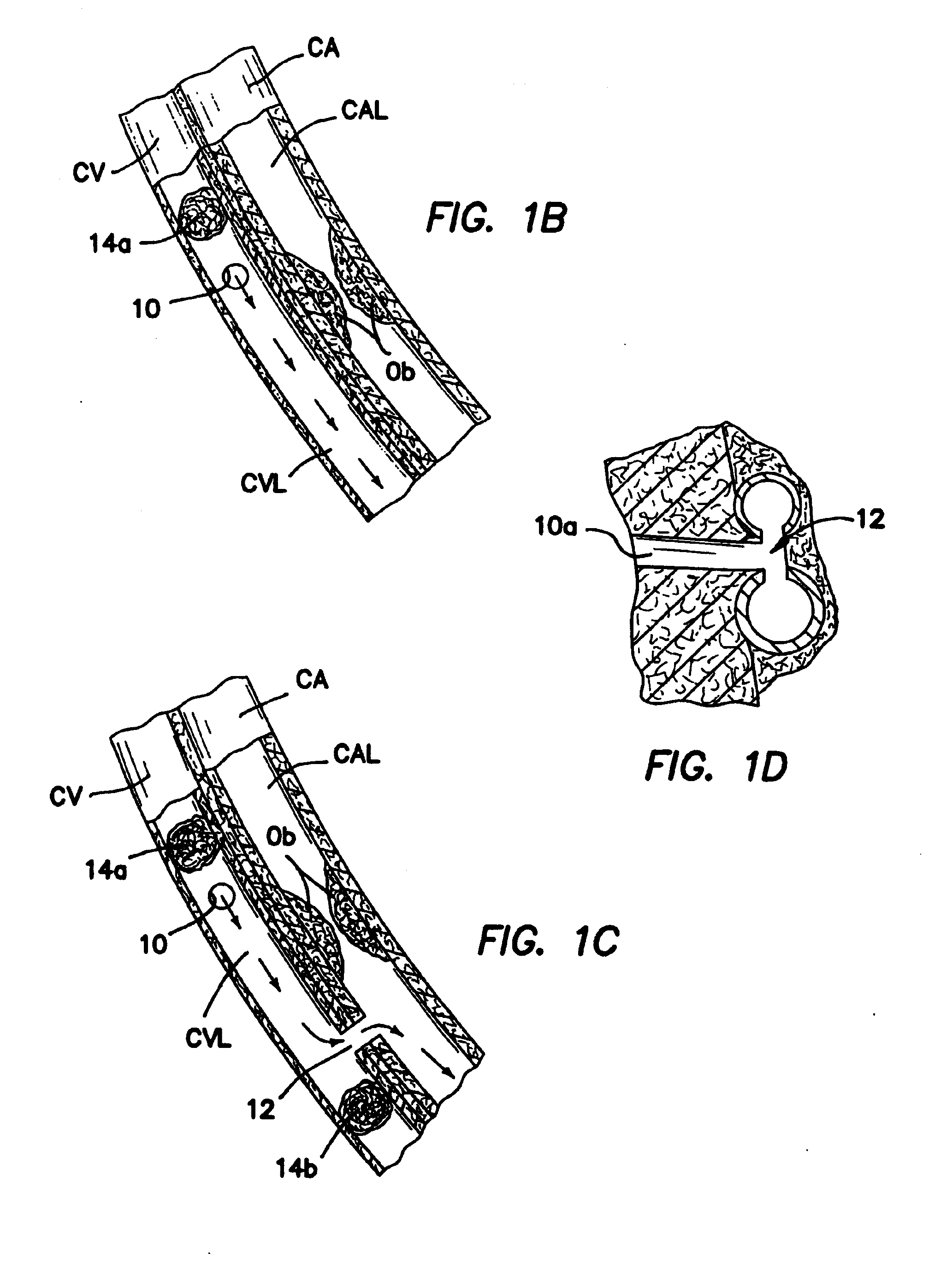
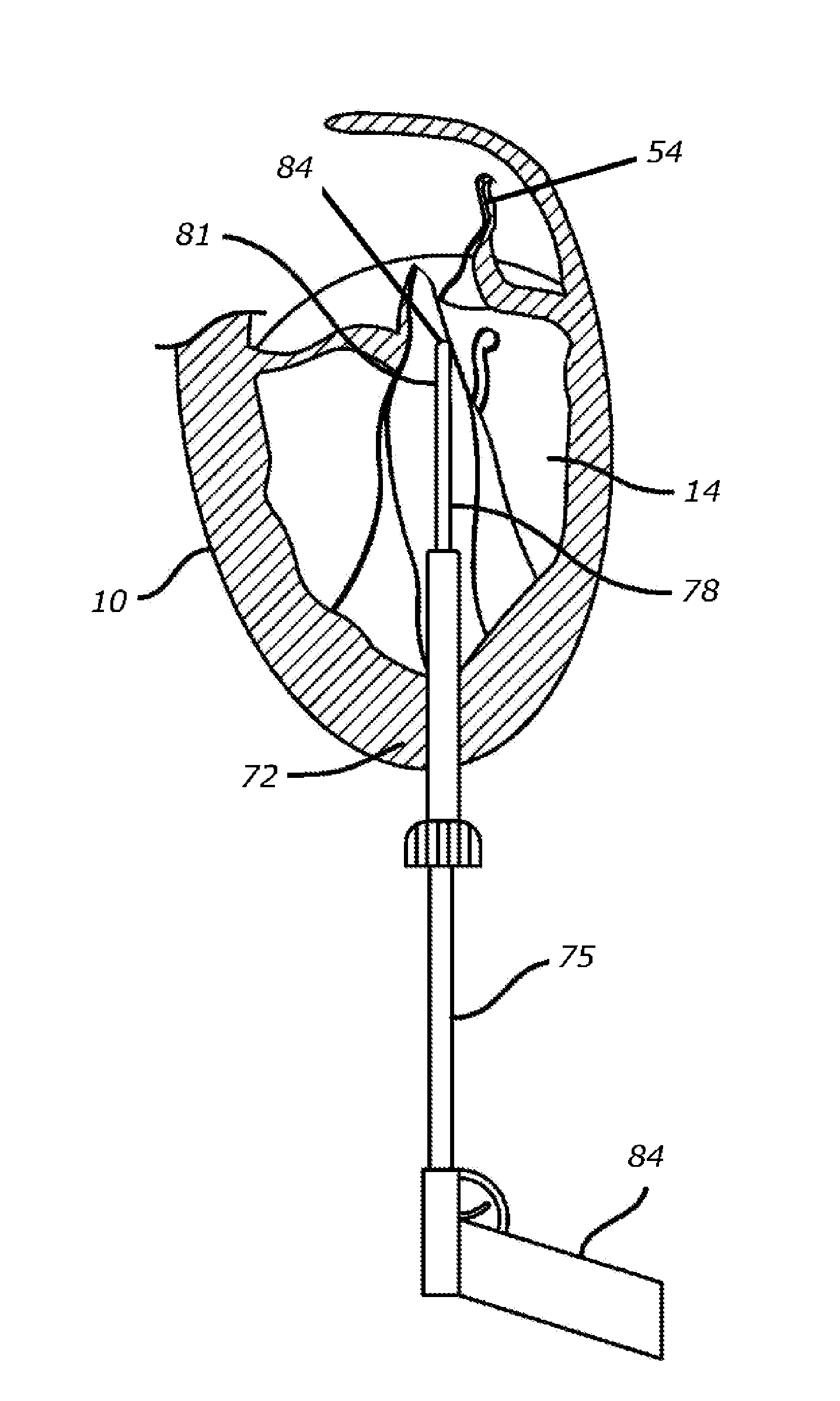
Method and apparatus for transmyocardial direct coronary revascularization
InactiveUS6929009B2Facilitate valvingShortening and thickeningEar treatmentCannulasVeinHeart chamber
Methods and apparatus for direct coronary revascularization wherein a transmyocardial passageway is formed between a chamber of the heart and a coronary blood vessel to permit blood to flow therebetween. In some embodiments, the transmyocardial passageway is formed between a chamber of the heart and a coronary vein. The invention includes unstented transmyocardial passageways, as well as transmyocardial passageways wherein protrusive stent devices extend from the transmyocardial passageway into an adjacent coronary vessel or chamber of the heart. The apparatus of the present invention include protrusive stent devices for stenting of transmyocardial passageways, intraluminal valving devices for valving of transmyocardial passageways, intracardiac valving devices for valving of transmyocardial passageways, endogenous tissue valves for valving of transmyocardial passageways, and ancillary apparatus for use in conjunction therewith.
Owner:MEDTRONIC VASCULAR INC
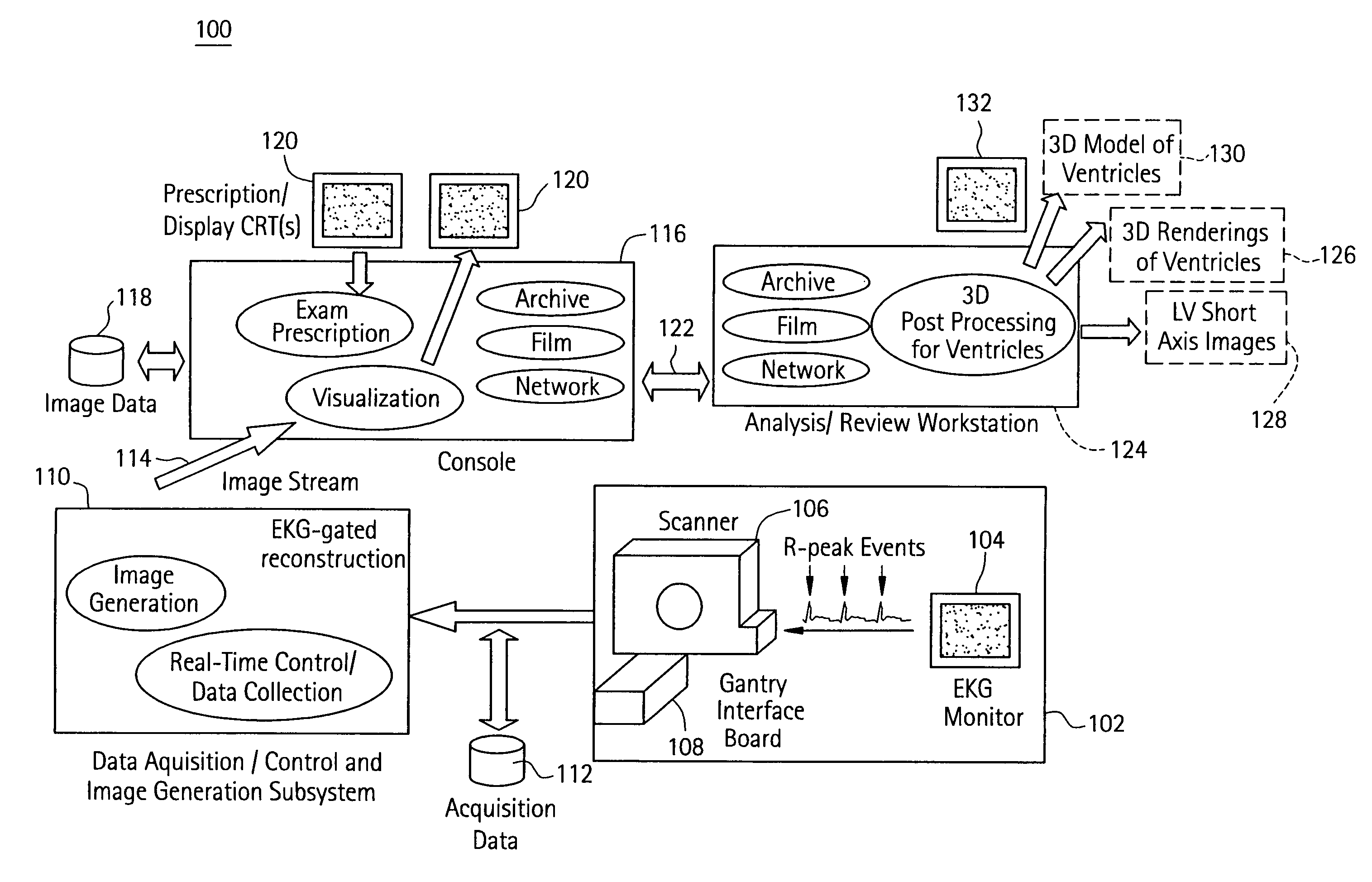
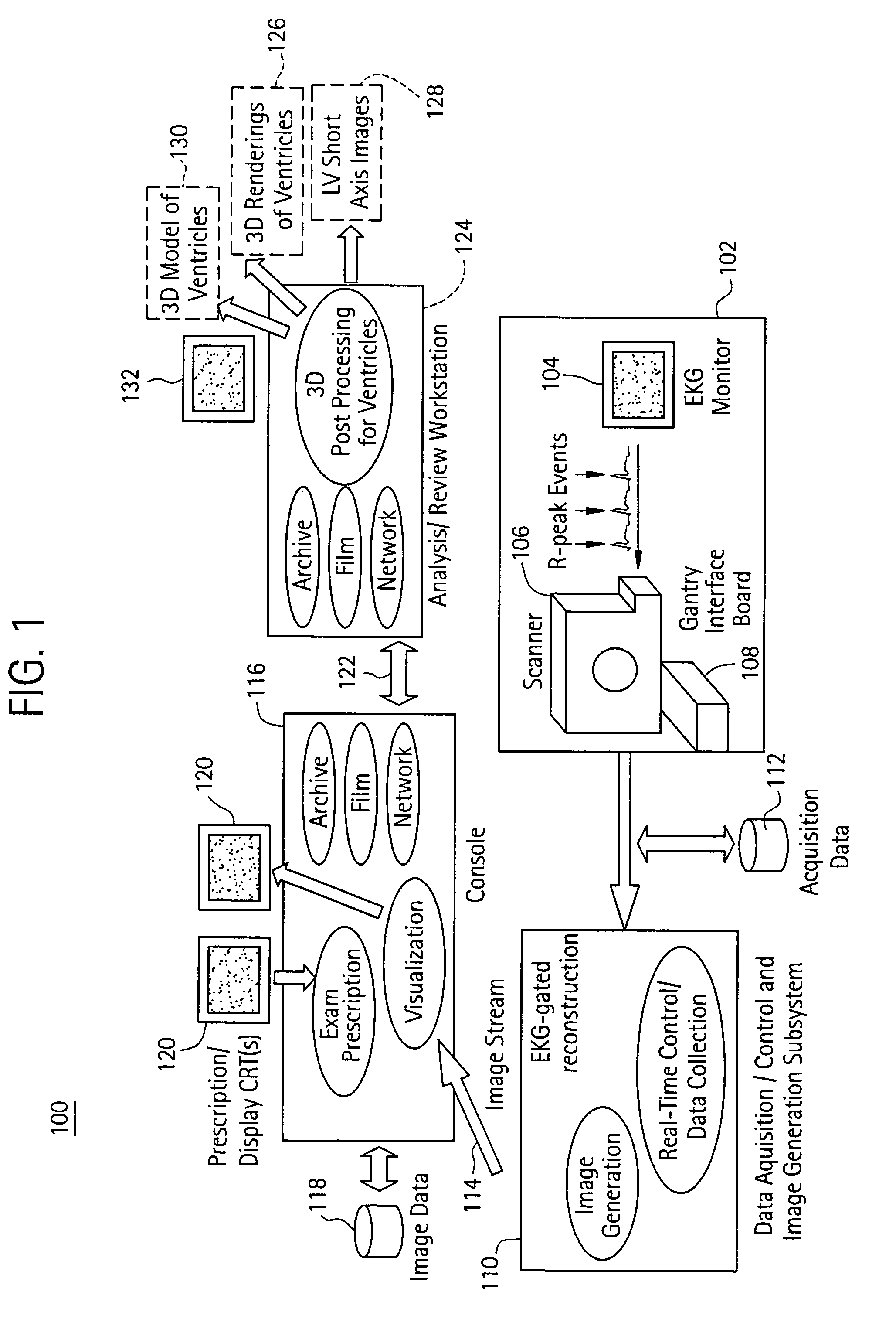
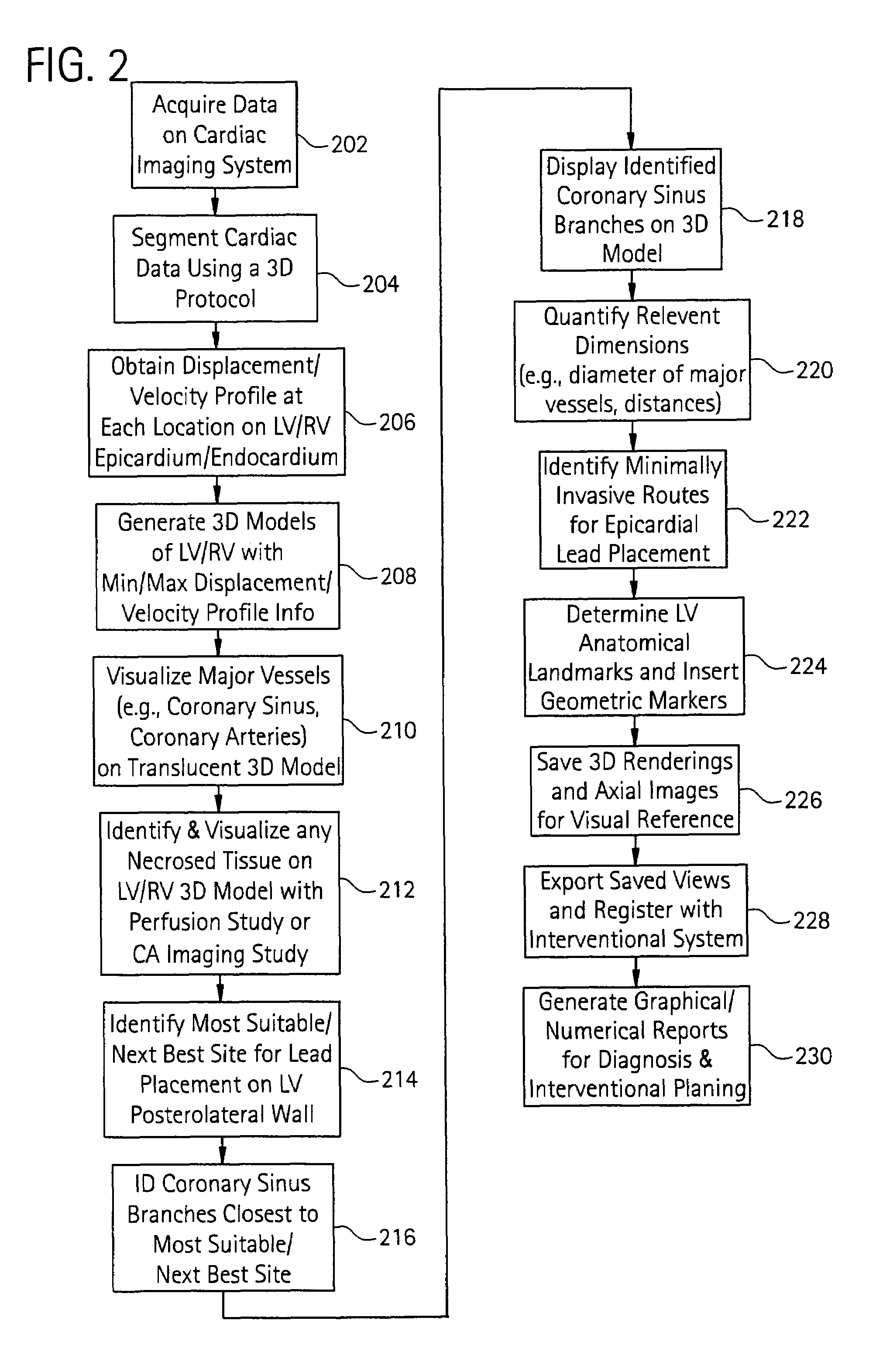
Cardiac imaging system and method for quantification of desynchrony of ventricles for biventricular pacing
A method for quantifying cardiac desynchrony of the right and left ventricles includes obtaining cardiac acquisition data from a medical imaging system, and determining a movement profile from the cardiac acquisition data. The movement profile is directed toward identifying at least one of a time-based contraction parameter for a region of the left ventricle (LV), and a displacement-based contraction parameter for a region of the LV. The determined movement profile is visually displayed by generating a 3D model therefrom.
Owner:APN HEALTH +1
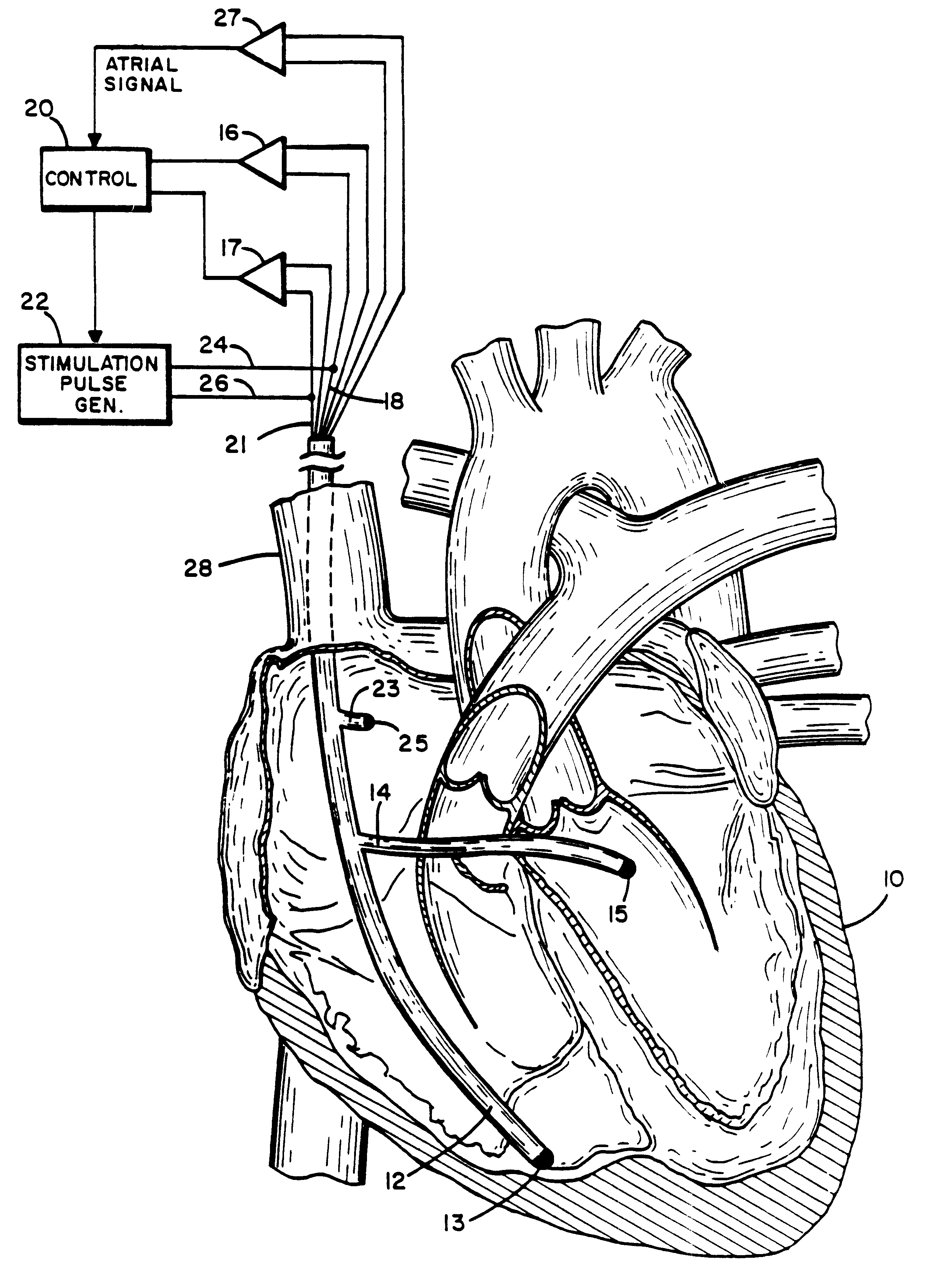
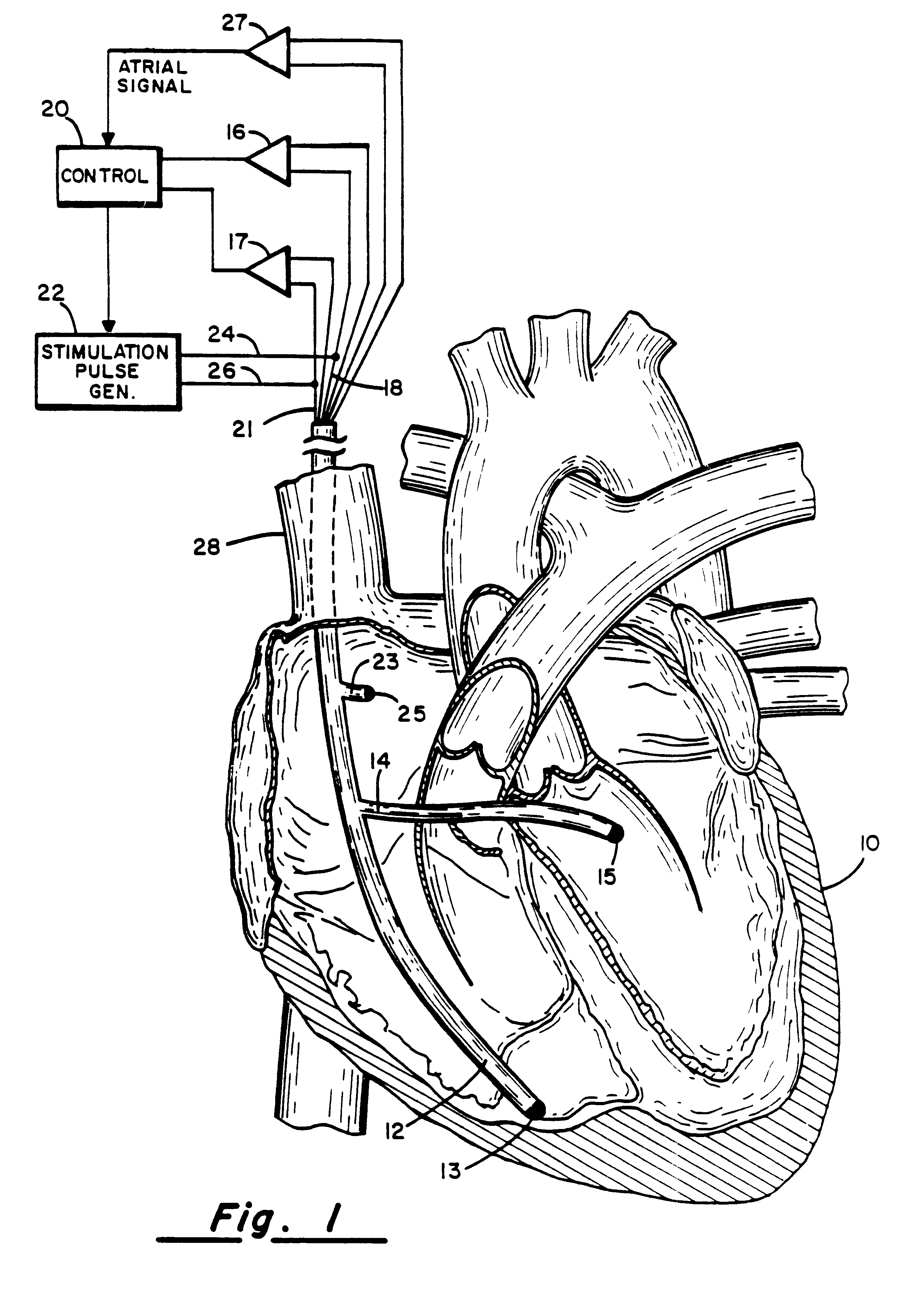
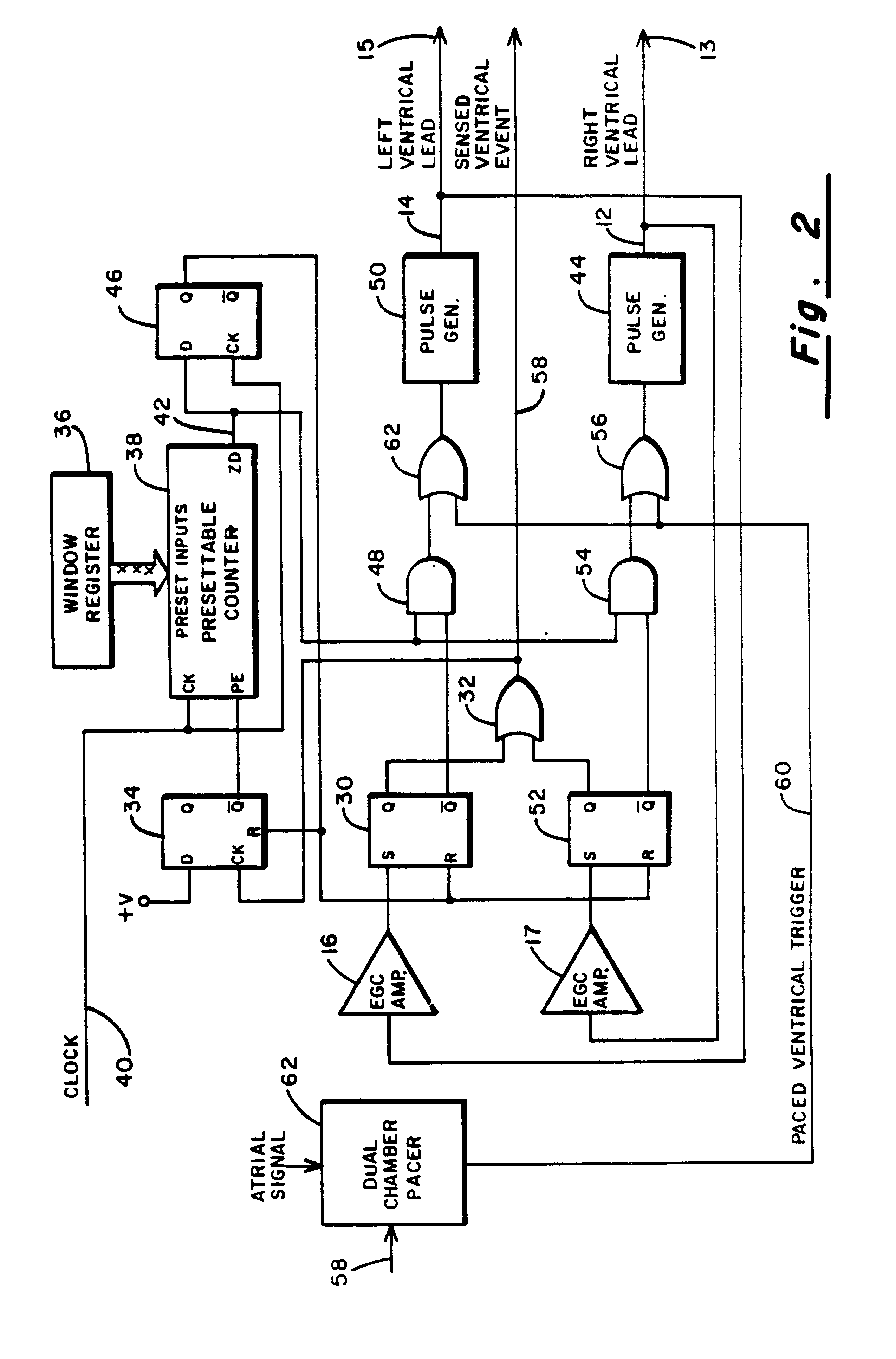
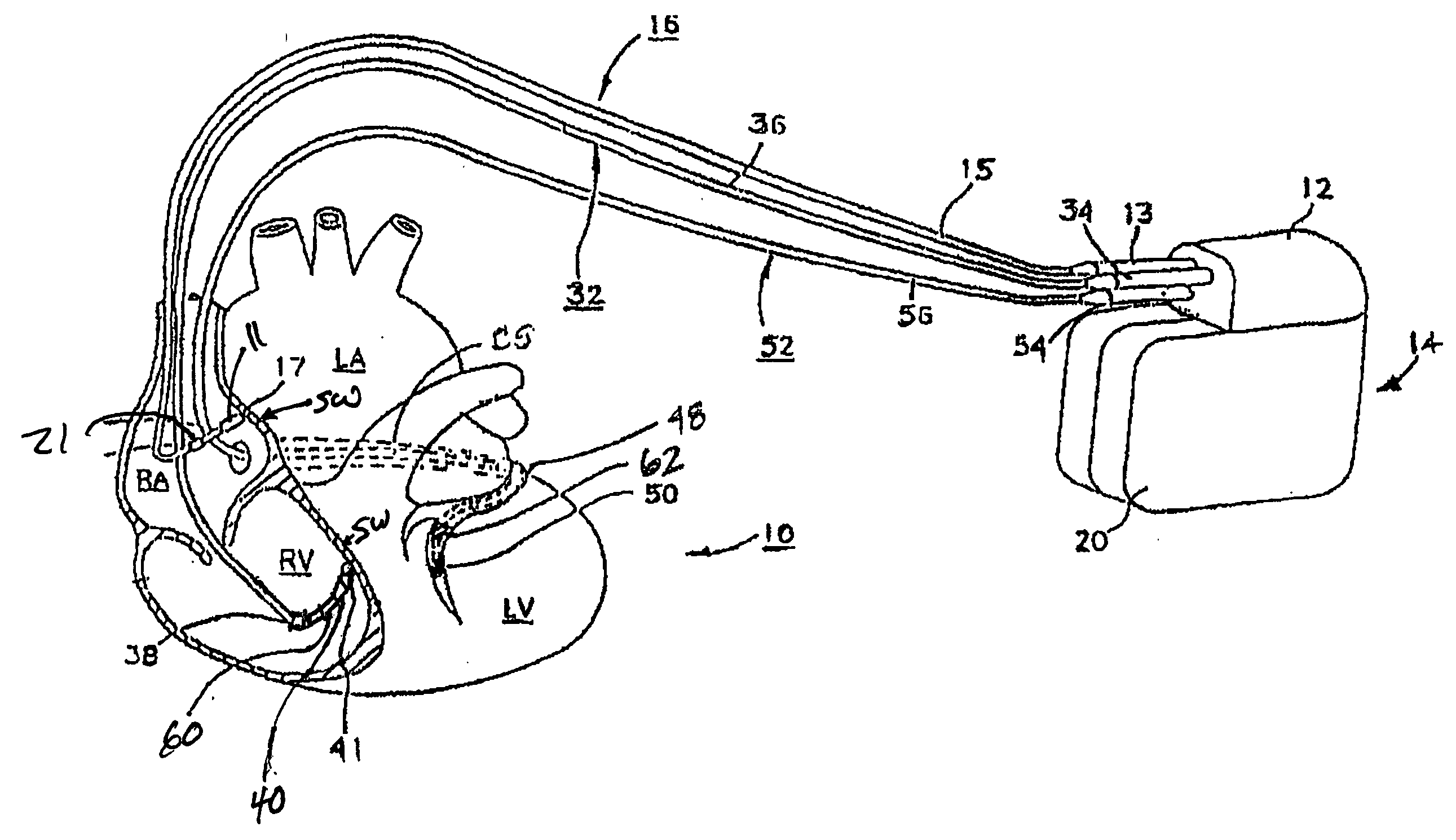
Method and apparatus for treating hemodynamic disfunction
A method of treating hemodynamic disfunction by simultaneously pacing both ventricles of a heart. At least one ECG amplifier is arranged to separately detect contraction of each ventricle and a stimulator is then activated for issuing stimulating pulses to both ventricles in a manner to assure simultaneous contraction of both ventricles, thereby to assure hemodynamic efficiency. A first ventricle is stimulated simultaneously with contraction of a second ventricle when the first fails to properly contract. Further, both ventricles are stimulated after lapse of a predetermined A-V escape interval. One of a pair of electrodes, connected in series, is placed through the superior vena cava into the right ventricle and a second is placed in the coronary sinus about the left ventricle. Each electrode performs both pacing and sensing functions. The pacer is particularly suitable for treating bundle branch blocks or slow conduction in a portion of the ventricles.
Owner:MIROWSKI FAMILY VENTURES LLC
Ventricular assist device for intraventricular placement
A ventricular assist device includes a pump such as an axial flow pump, an outflow cannula connected to the outlet of the pump, and an anchor element. The anchor element is physically connected to the pump, as by an elongate element. The pump is implanted within the left ventricle with the outflow cannula projecting through the aortic valve but desirably terminating short of the aortic arch. The anchor element is fixed to the wall of the heart near the apex of the heart so that the anchor element holds the pump and outflow cannula in position.
Owner:HEARTWARE INC
Contraction status assessment
An implantable medical device receives at least one sensor signal representing inter-movement between a basal region of a heart ventricle and a ventricle apex during at least a portion of a systolic phase of a cardiac cycle. A parameter processor calculates a contraction status parameter value based on the at least one sensor signal. This contraction status parameter value represents an elongation of the ventricle following onset of ventricular activation during a cardiac cycle. The contraction status parameter value is stored in a memory as a diagnostic parameter representing a current contraction status of a subject's heart.
Owner:ST JUDE MEDICAL
Mitral valve treatment techniques
ActiveUS20090149872A1Enhance fibrosisReduce distanceAnnuloplasty ringsNon-surgical orthopedic devicesCouplingMitral valve leaflet
Apparatus (20) is provided for treating mitral valve regurgitation, including a band (30) having distal and proximal ends, the band (30) adapted to be placed: around between 90 and 270 degrees of a mitral valve (58), including around at least a portion of a posterior cusp (56) of the valve (58), in a space defined by (a) a ventricular wall (70), (b) a ventricular surface of the posterior cusp (56) in a vicinity of an annulus (60) of the mitral valve (58), and (c) a plurality of third-order chordae tendineae (74). The apparatus (20) further includes distal and proximal coupling elements (32, 34), coupled to the band (30) at the distal and proximal ends thereof, respectively, and adapted to be coupled to a first chorda tendinea and a second chorda tendinea, respectively, each of the first and second chordae tendineae selected from the group consisting of: one of the plurality of third-order chordae tendineae (74), and a first-order chorda tendinea that inserts on a commissural cusp (78) of the mitral valve (58). Additional embodiments are also described.
Owner:VALTECH CARDIO LTD
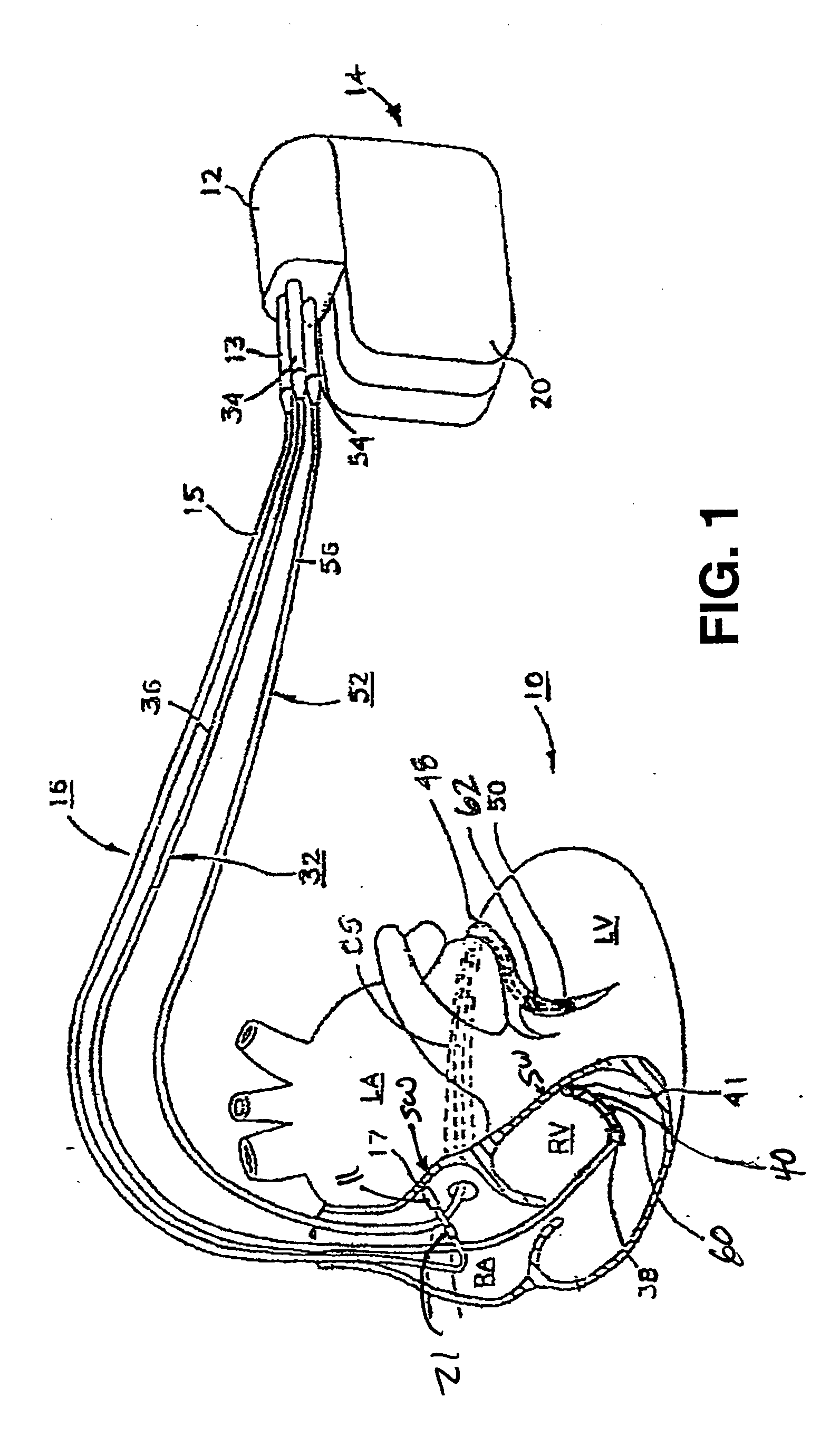
Four chamber pacer for dilated cardiomyopthy
An endocardial apparatus for pacing four chambers of a heart, comprising: a power source housed in an implantable can, first, second and third leads having proximal and distal ends, each lead being electrically connected to the power source at its proximal end and extending into a vein proximal the heart, the first lead connecting at its distal end to an electrode that is in electrical contact with the right atrium of the heart, the second lead connecting at its distal end to an electrode that is in electrical contact with the right ventricle of the heart, the third lead connecting at a point proximal its distal end to a first electrode that is in electrical contact with the inside of the coronary sinus and oriented so as to stimulate the left atrium of the heart and connecting at its distal end to a second electrode that is in electrical contact with the inside of the great cardiac vein and oriented so as to stimulate the left ventricle of the heart. Devices are also disclosed for orienting and maintaining the position of the electrodes on the third lead.
Owner:INTERMEDICS
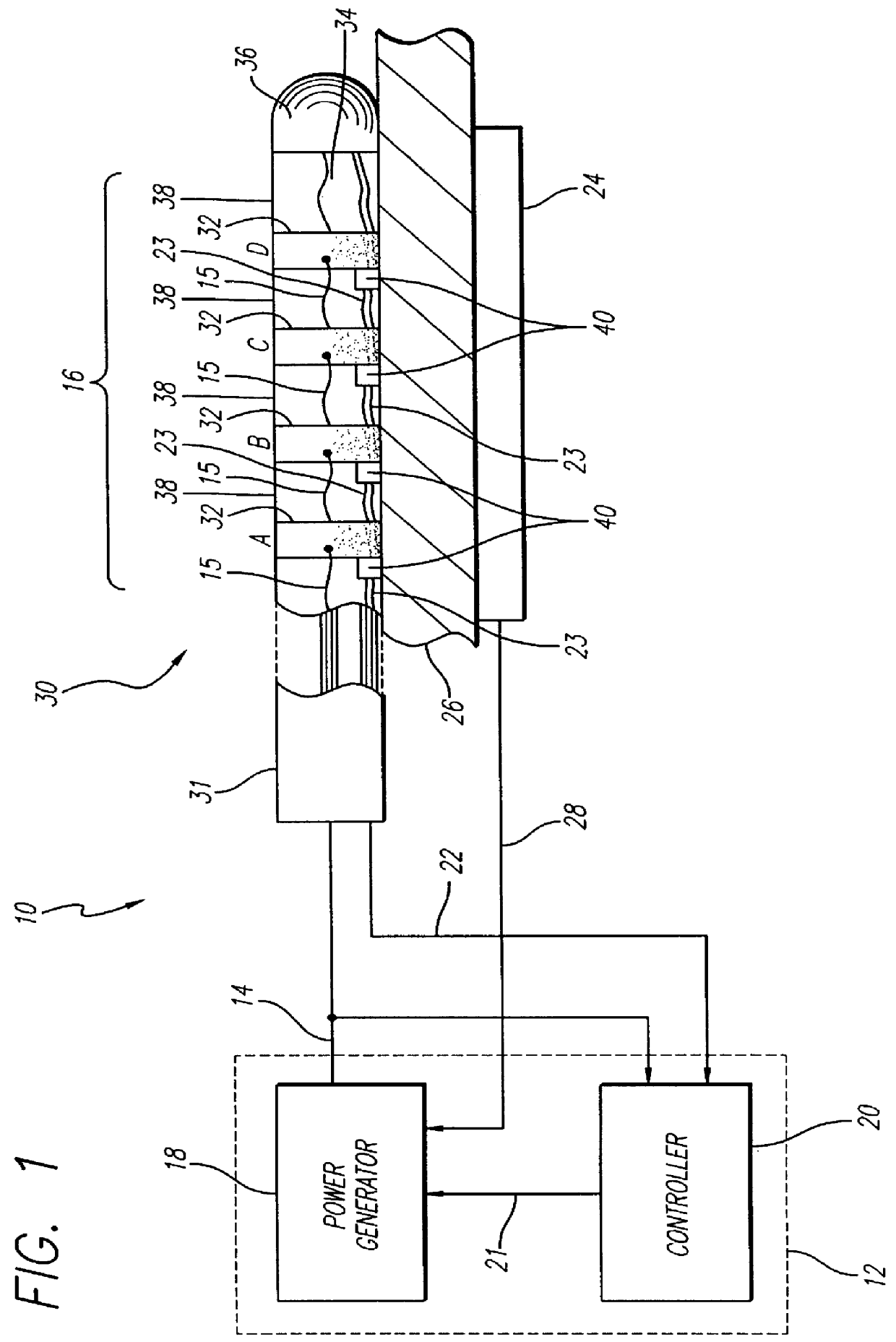
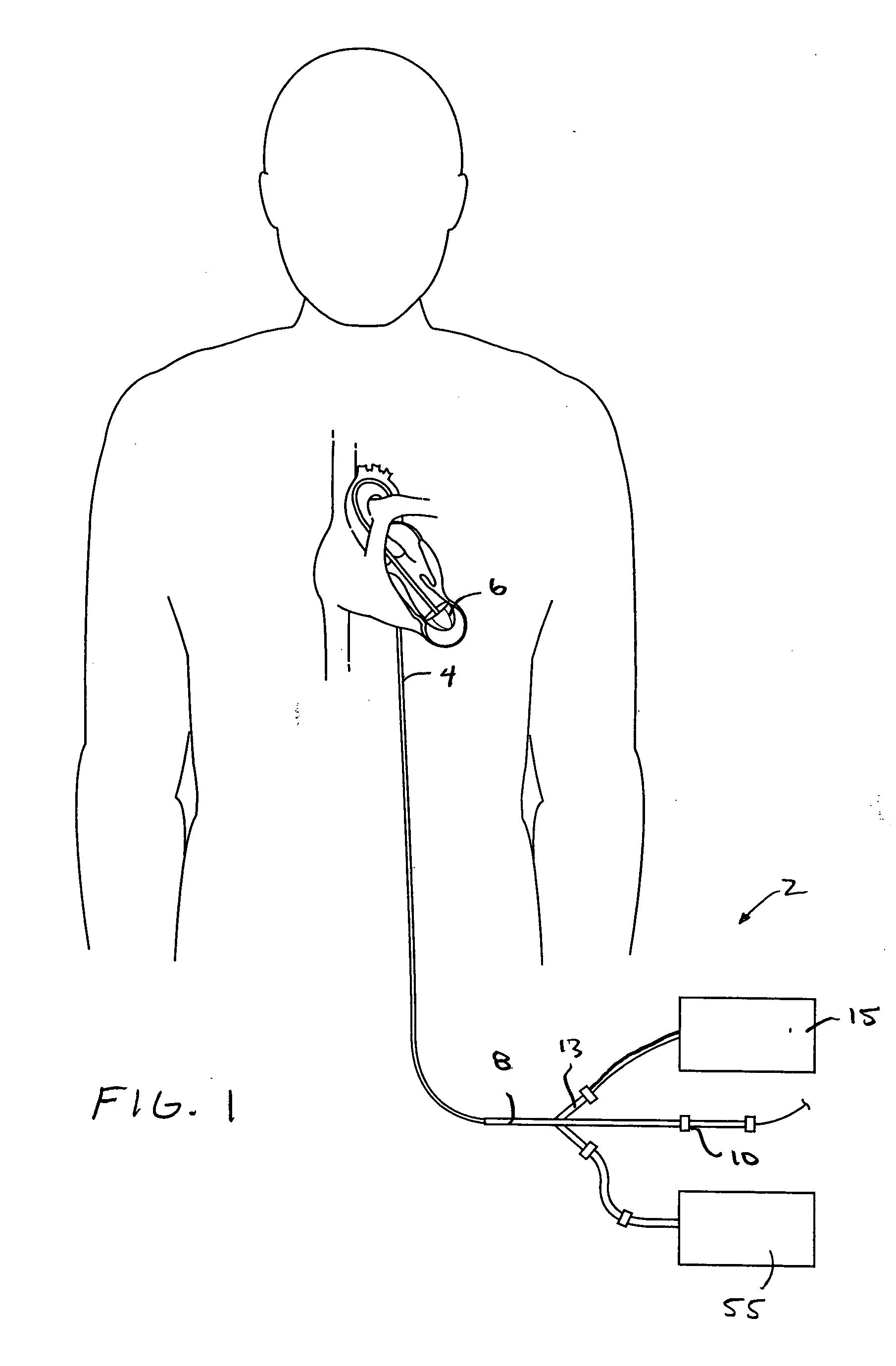
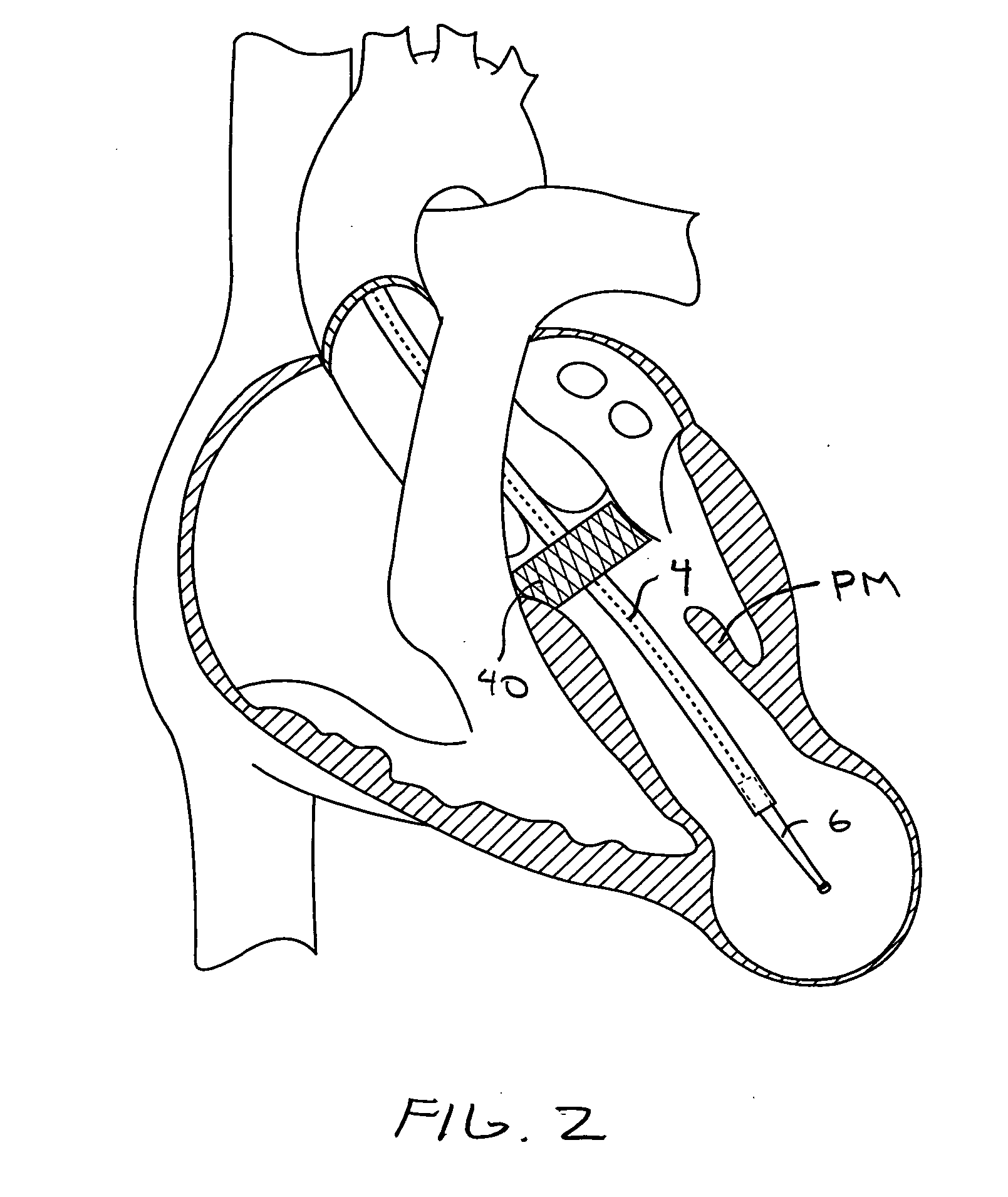
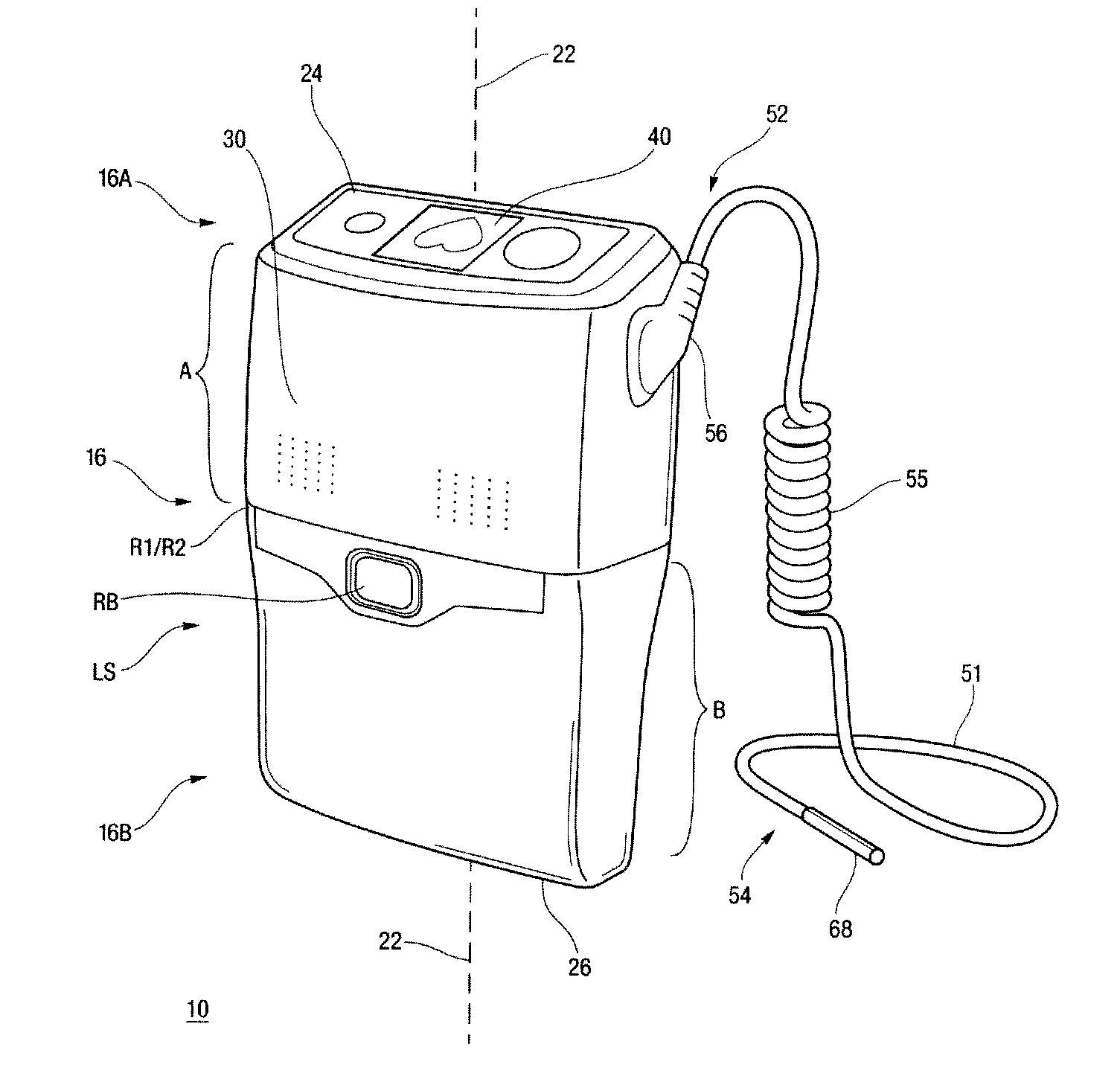
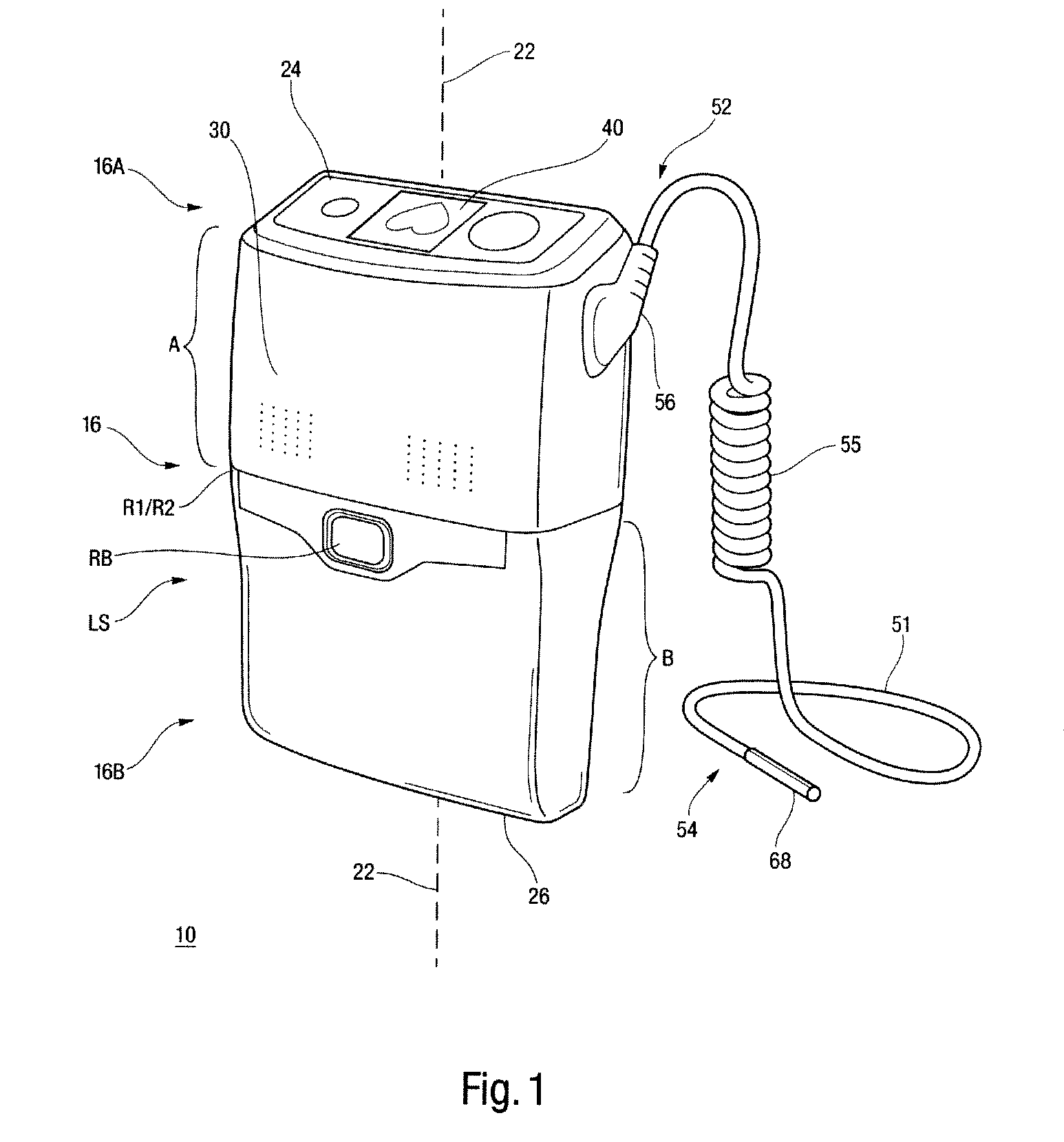
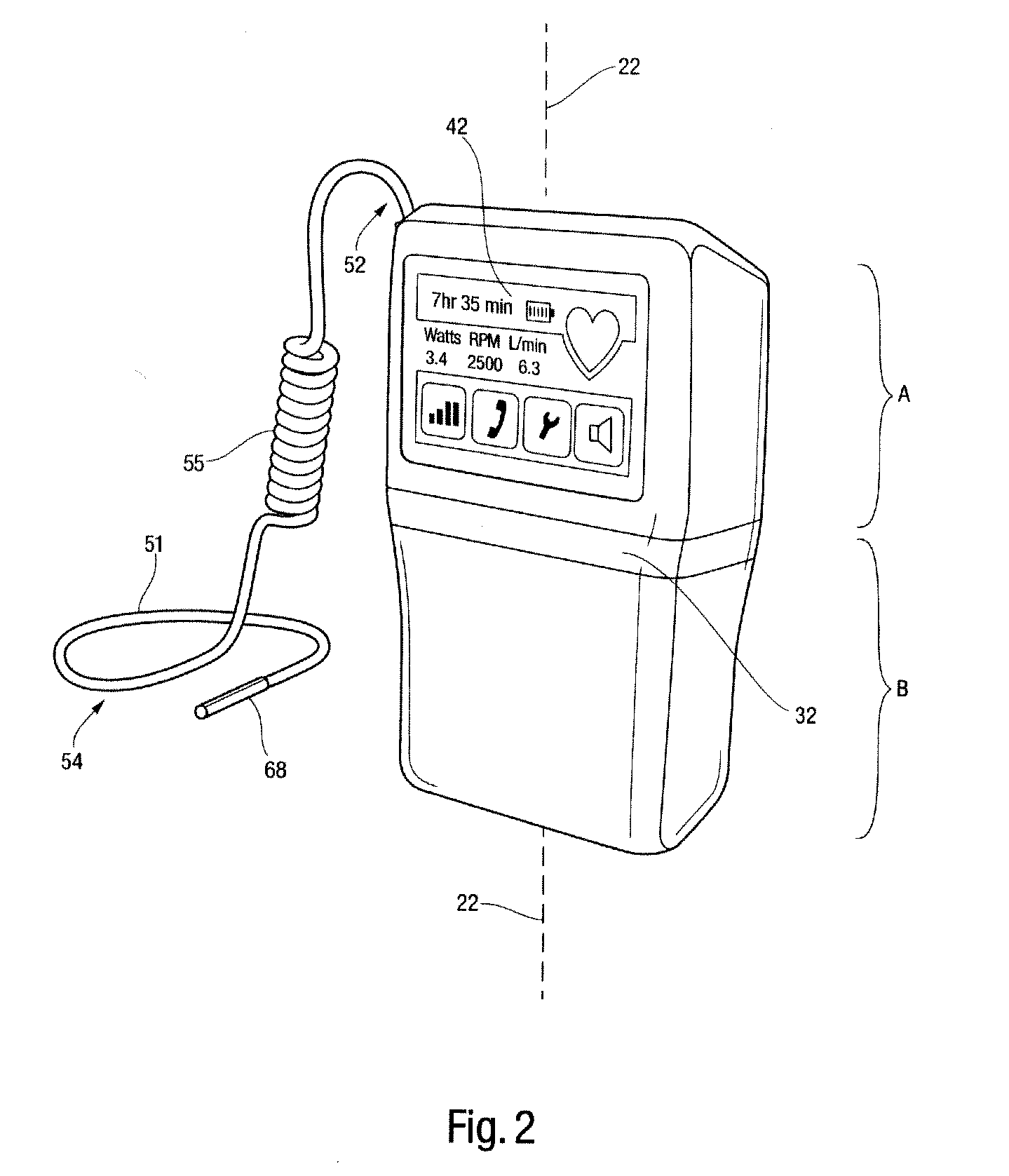
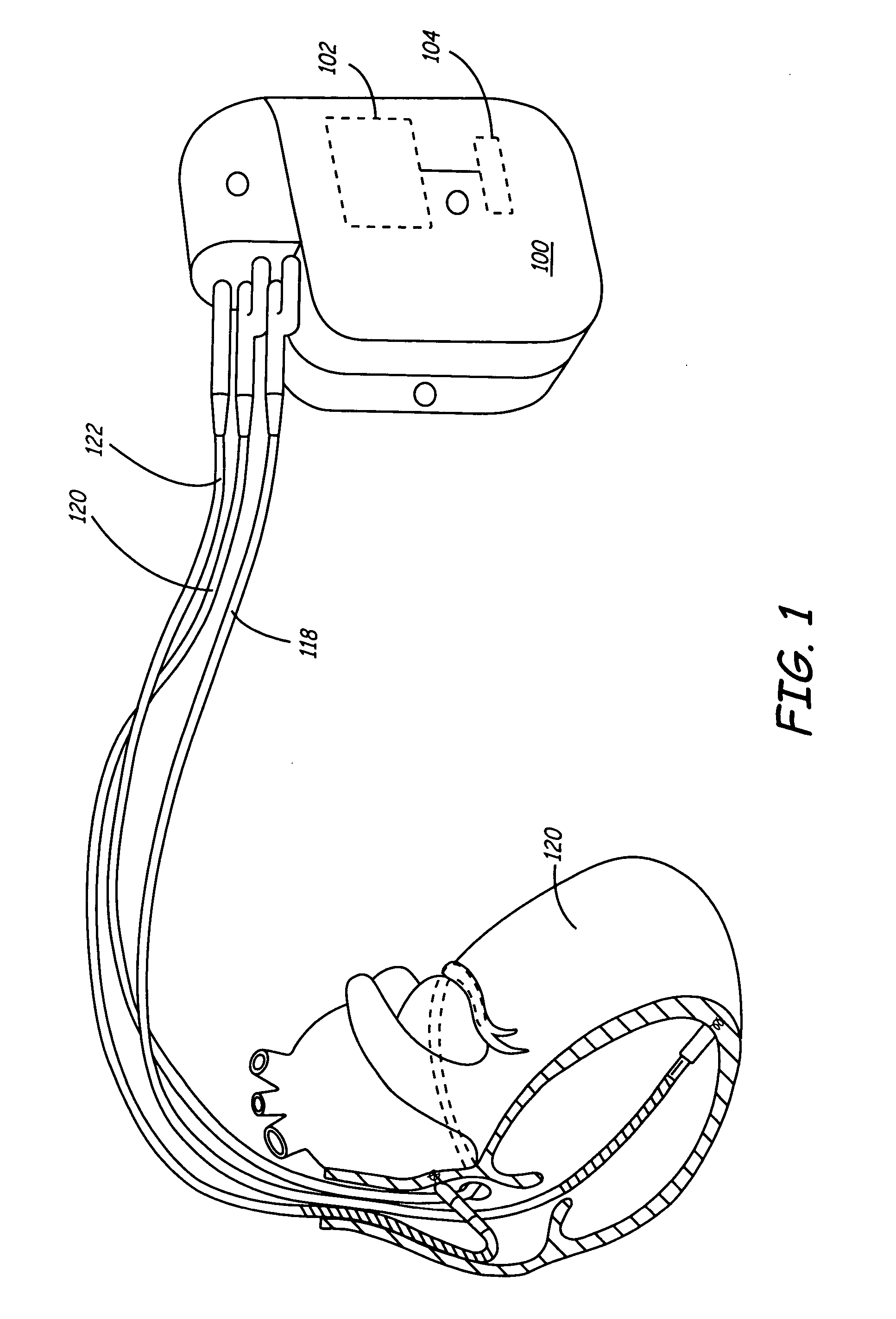
Controller and power source for implantable blood pump
Methods and apparatus for controlling the operation of, and providing power for and to, implantable ventricular assist devices which includes a pump employing a brushless DC motor-driven blood pump, are disclosed. In one embodiment, a control system for driving an implantable blood pump is provided. The digital processor is responsive to data associated with the operation of the pump received at the data transfer pump, and from program data stored in the memory, (i) to determine therefrom, the identity of the pump, (ii) to determine therefrom, electrical characteristics and features of the identified pump, and (iii) to adaptively generate and apply to the data port, control signals for driving the identified pump.
Owner:HEARTWARE INC
Method of optimizing cardiac resynchronization therapy using sensor signals of septal wall motion
The present invention relates to monitoring septal wall motion of the atrial and / or ventricular chambers of a heart for optimizing cardiac pacing intervals based on signals derived from said wall motion. At least one lead of medical device is equipped with a motion sensor adapted to couple to septal tissue. The device receives and may post-process (e.g., suitably filter, rectify and / or integrate) motion signals to determine acceleration, velocity or displacement. During pacing interval optimization the wall motion is measured for many pacing intervals and the pacing interval setting(s) that produce minimal wall motion are implemented for therapy delivery. In addition, the present invention provides methods for periodically determining whether to cease or resume delivery of a bi-ventricular pacing therapy to a patient that may have experienced beneficial reverse remodeling of the heart.
Owner:MEDTRONIC INC
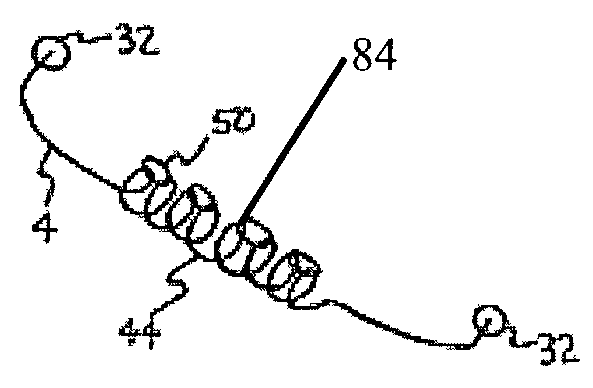
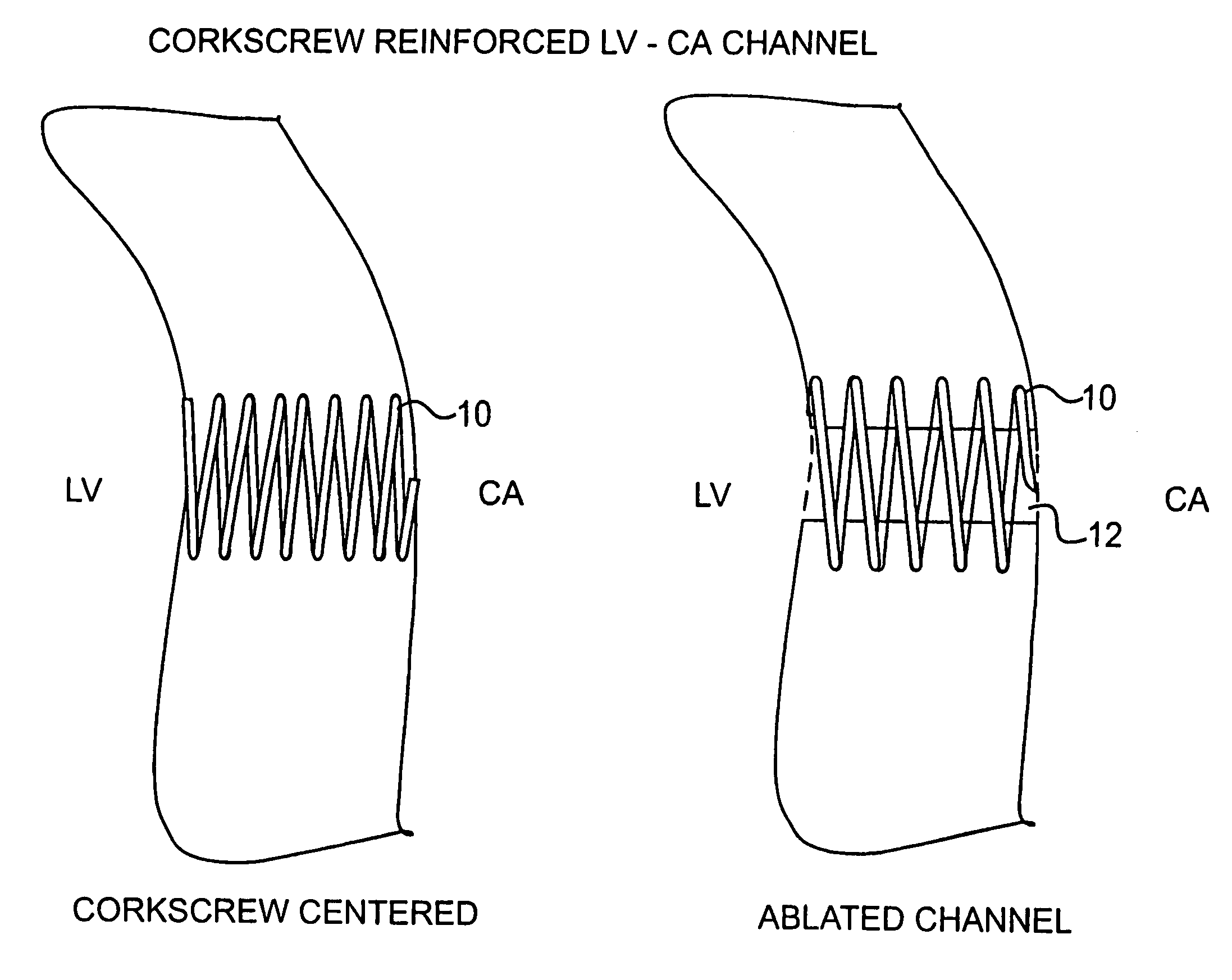
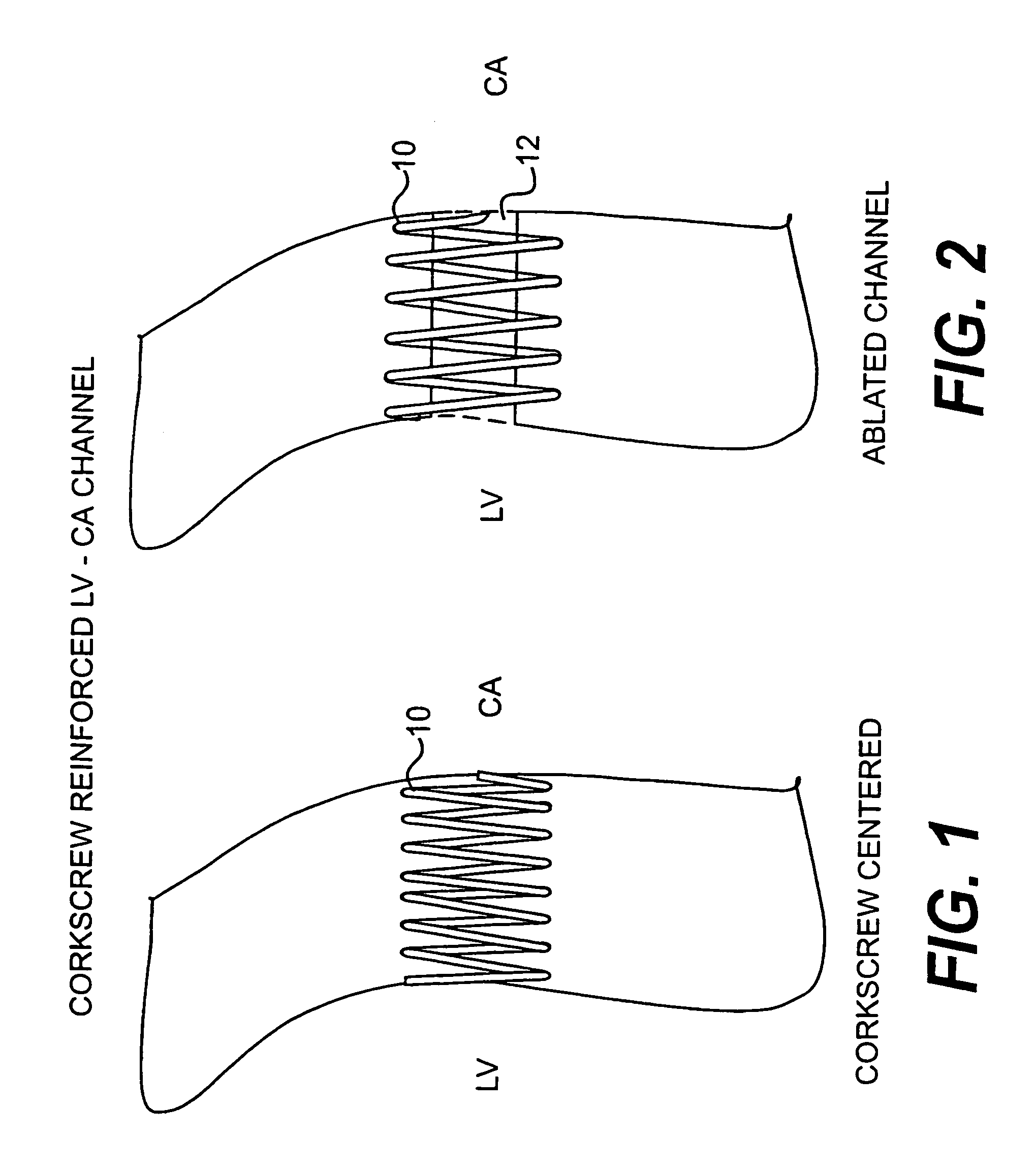
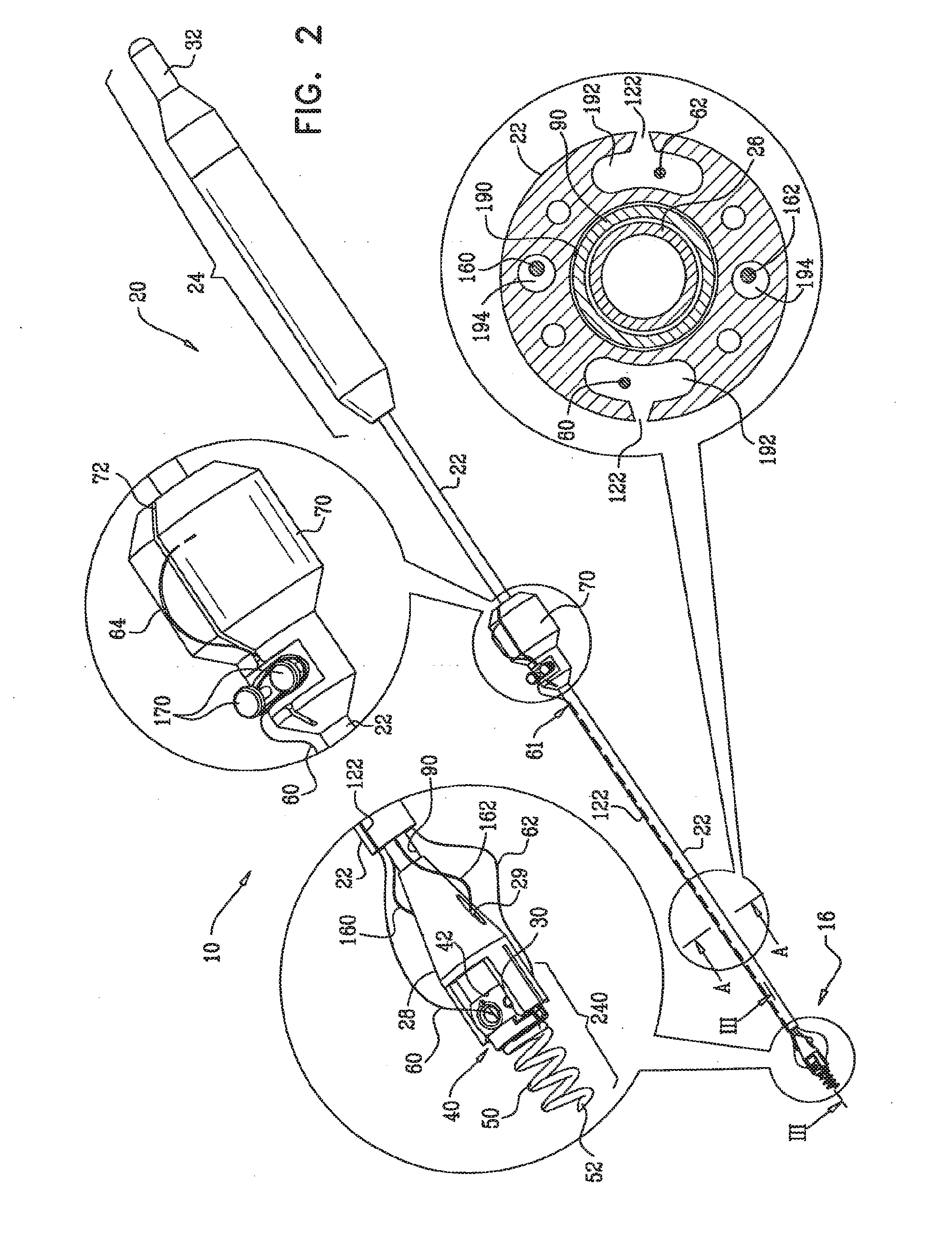
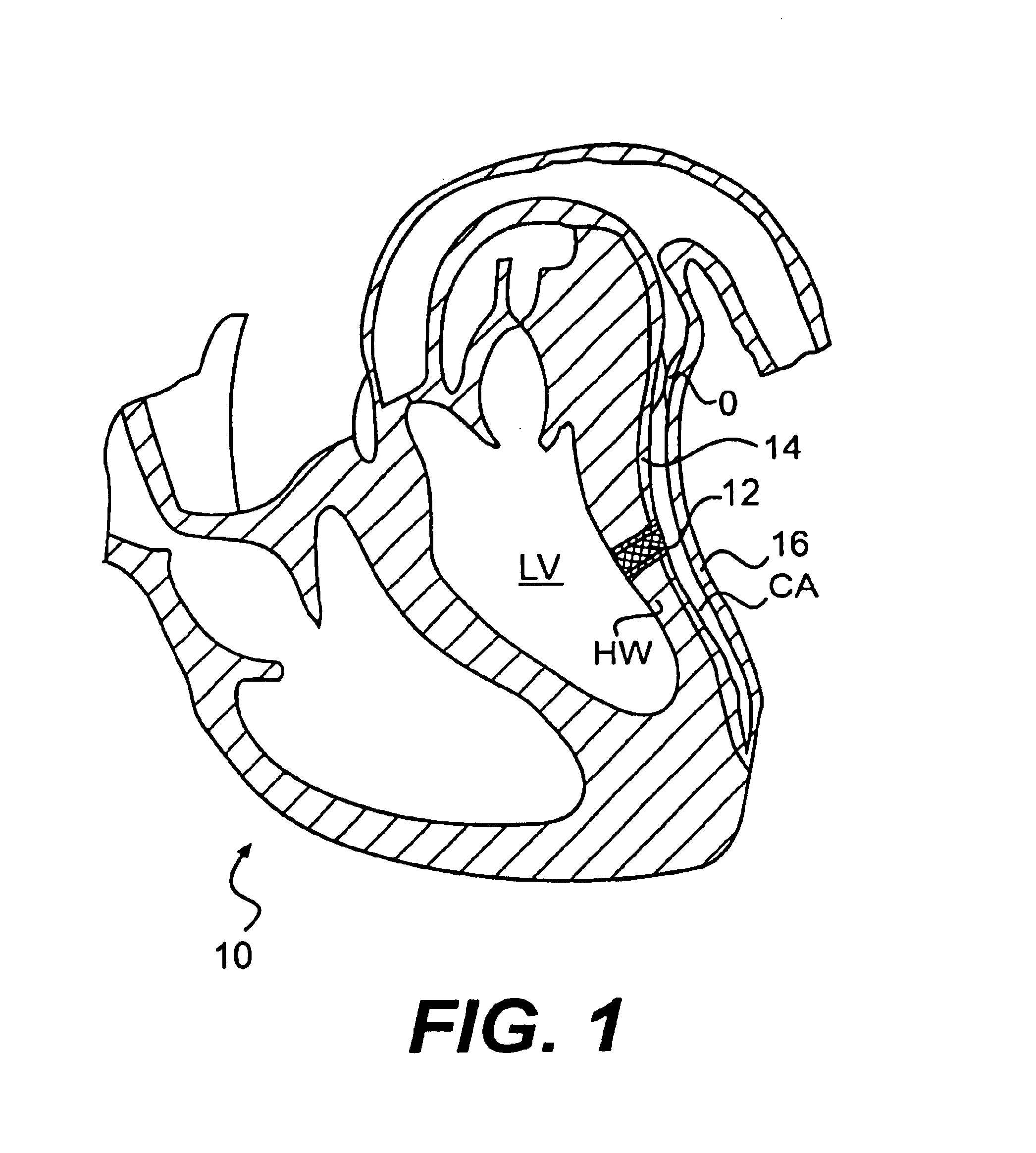
Corkscrew reinforced left ventricle to coronary artery channel
InactiveUS7033372B1Improve stabilityWithout significant tissue traumaDiagnosticsSurgical needlesCoronary arteriesHeart wall
A coil is screwed into the heart wall HW between the left ventricle and coronary artery, followed by forming of a channel with laser, plasma, electrical, or mechanical device therethrough.
Owner:HORIZON TECH FUNDING CO LLC
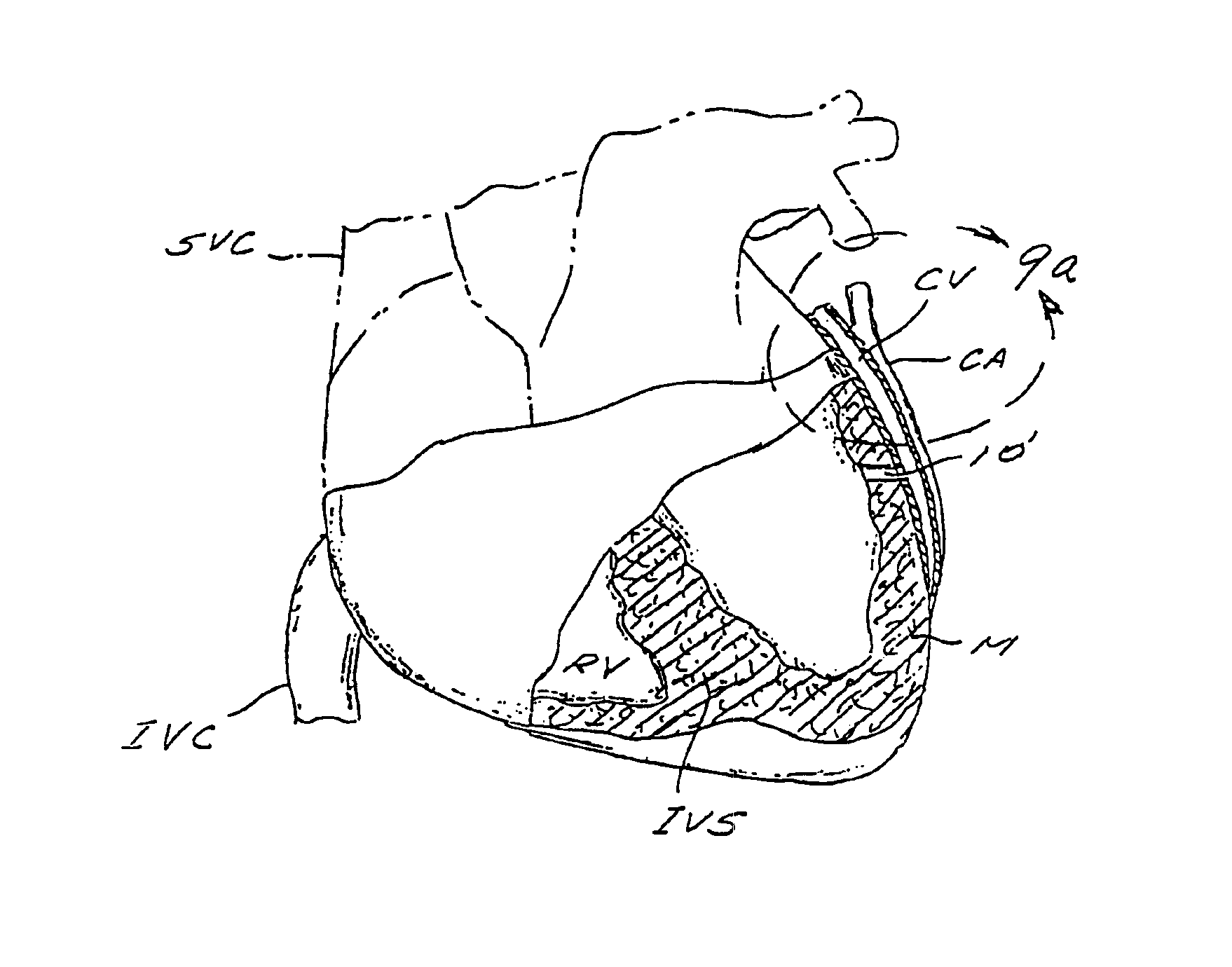
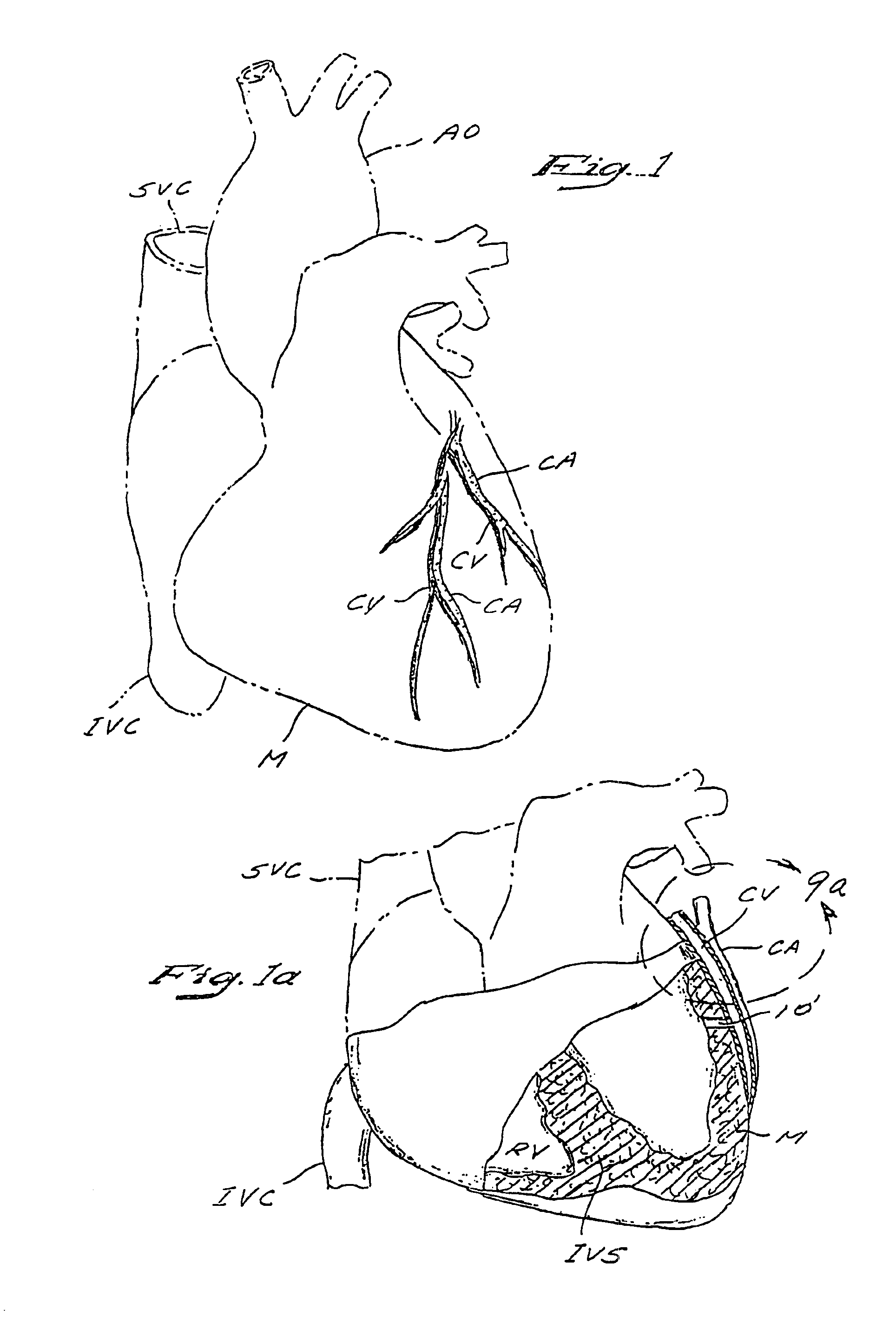
Methods and apparatus for transmyocardial direct coronary revascularization
InactiveUS7159592B1Easy to movePromote formationEar treatmentCannulasCoronary revascularizationCoronary revascularisation
Methods and apparatus for direct coronary revascularization wherein a transmyocardial passageway is formed between a chamber of the heart and a coronary blood vessel to permit blood to flow therebetween. In some embodiments, the transmyocardial passageway is formed between a chamber of the heart and a coronary vein. The invention includes unstented transmyocardial passageways, as well as transmyocardial passageways wherein protrusive stent devices extend from the transmyocardial passageway into an adjacent coronary vessel or chamber of the heart. The apparatus of the present invention include protrusive stent devices for stenting of transmyocardial passageways, intraluminal valving devices for valving of transmyocardial passageways, intracardiac valving devices for valving of transmyocardial passageways, endogenous tissue valves for valving of transmyocardial passageways, and ancillary apparatus for use in conjunction therewith.
Owner:MEDTRONIC VASCULAR INC
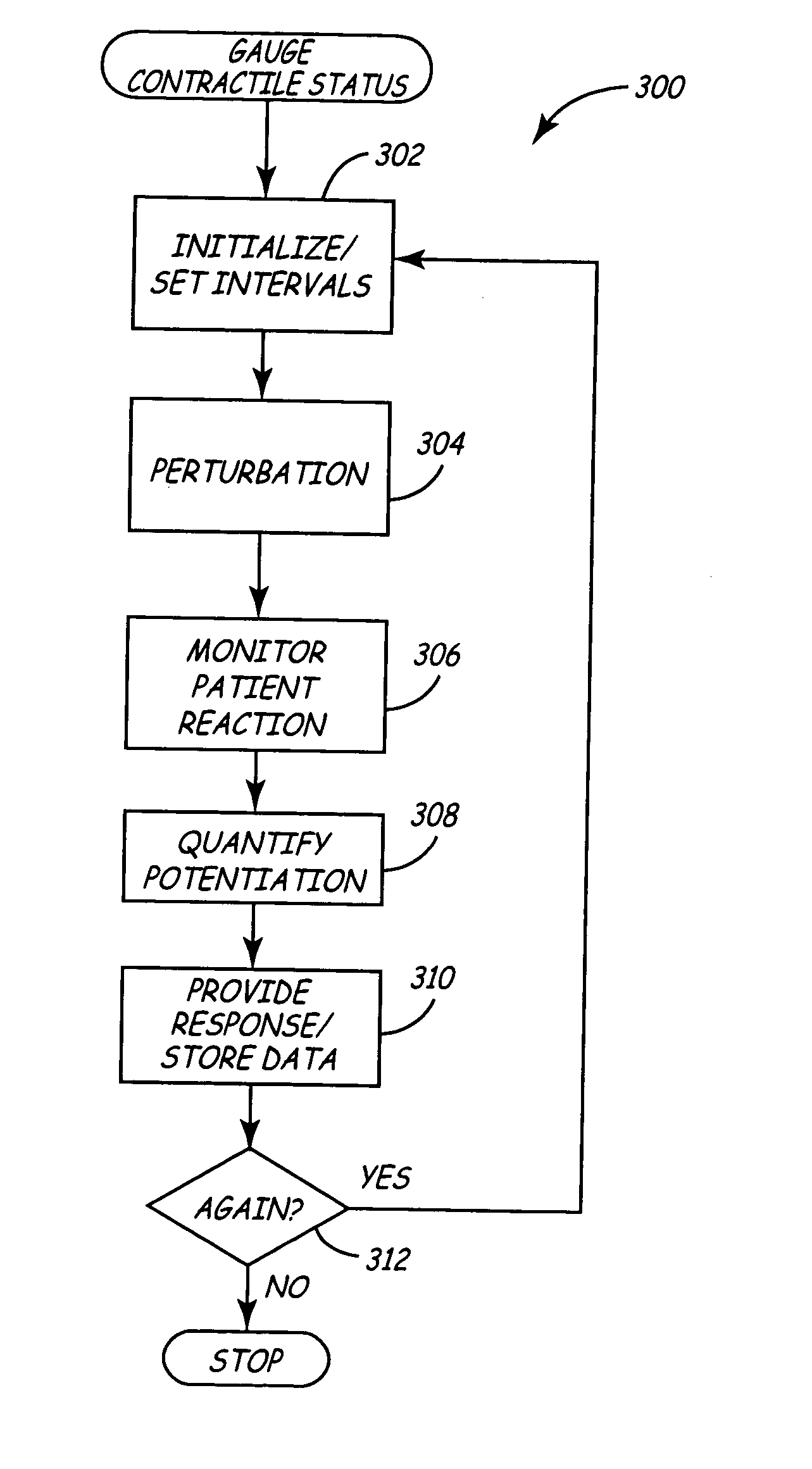
Method and apparatus for improving ventricular status using the force interval relationship
Methods and devices for improving ventricular contractile status of a patient suitably exploit changes in ventricular pressure and / or dP / dtmax to provide and / or optimize a response to a patient. The ventricular pressure may be appropriately correlated to intracellular calcium regulation, which is indicative of contractile status. To assess ventricular contractile status, the device suitably observes a cardiac perturbation of the patient and measures force interval potentiation following the perturbation. The contractile potentiation can then be stored and / or quantified in the implantable medical device to determine the ventricular contractile status of the patient, and an appropriate response may be provided to the patient as a function of the ventricular contractile status. Examples of responses may include administration of drug or neuro therapies, modification of a pacing rate, or the like. Force interval potentiation may also be used to optimize or improve a parameter for a response provided by the implantable medical device.
Owner:MEDTRONIC INC
Heart support to prevent ventricular remodeling
InactiveUS6887192B1Reducing end-diastolic diameterRelieve stressHeart valvesControl devicesSystoleCardiac functioning
This is a support device that prevents, reduces, and delays remodeling of diseased cardiac tissue, and also decreases the impact of such remodeling on collateral tissue is disclosed. The invention further reinforces abnormal tissue regions to prevent over-expansion of the tissue due to increased afterload and excessive wall tension. As a result, the support device prevents phenomenon such as systolic stretch from occurring and propagating. The support structure maintains and restores diastolic compliance, wall motion, and ejection fraction to preserve heart functionality. As such, the support device prevents and treats cardiomyopathy and congestive heart failure.
Owner:CONVERGE MEDICAL
In-vivo method and device for improving diastolic function of the left ventricle
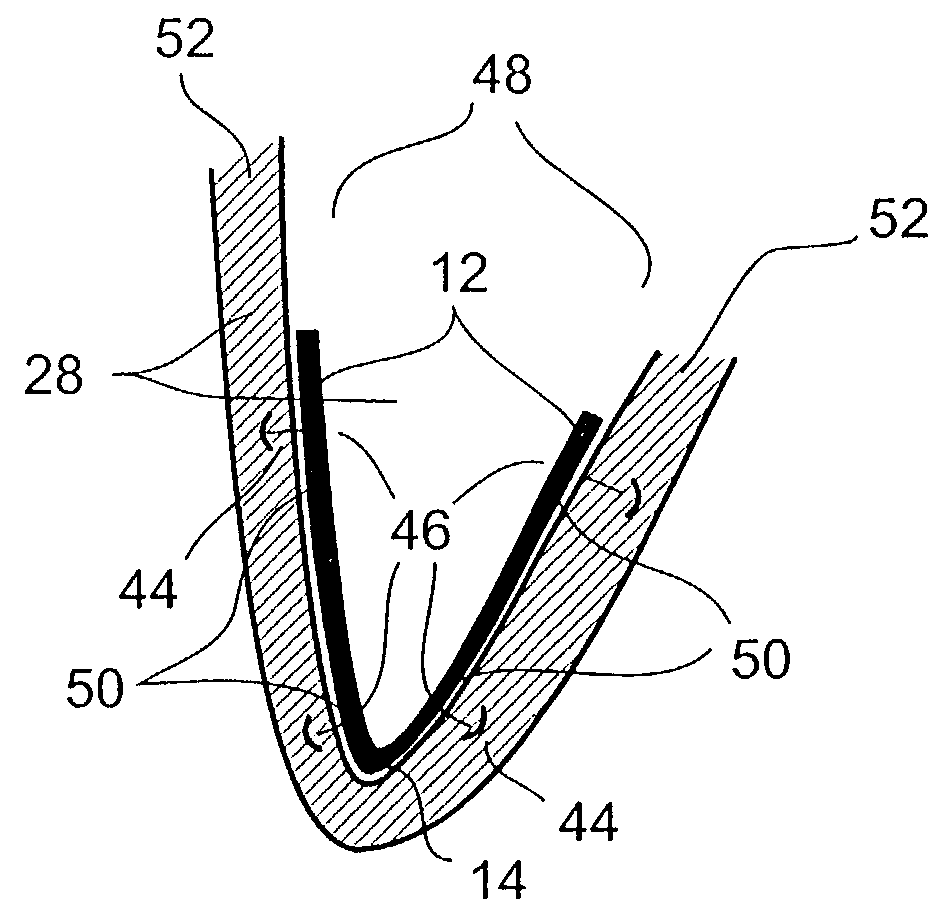
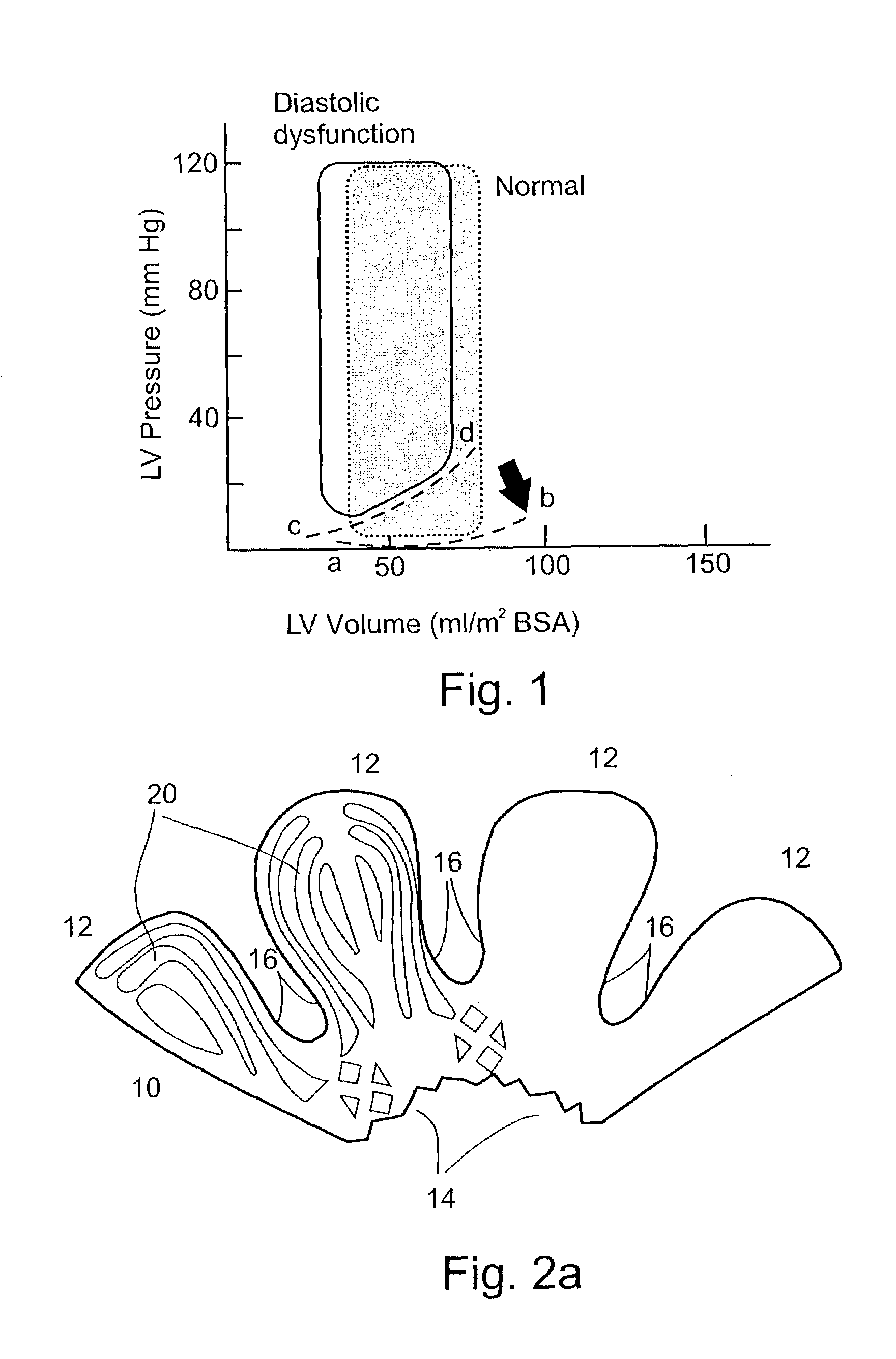
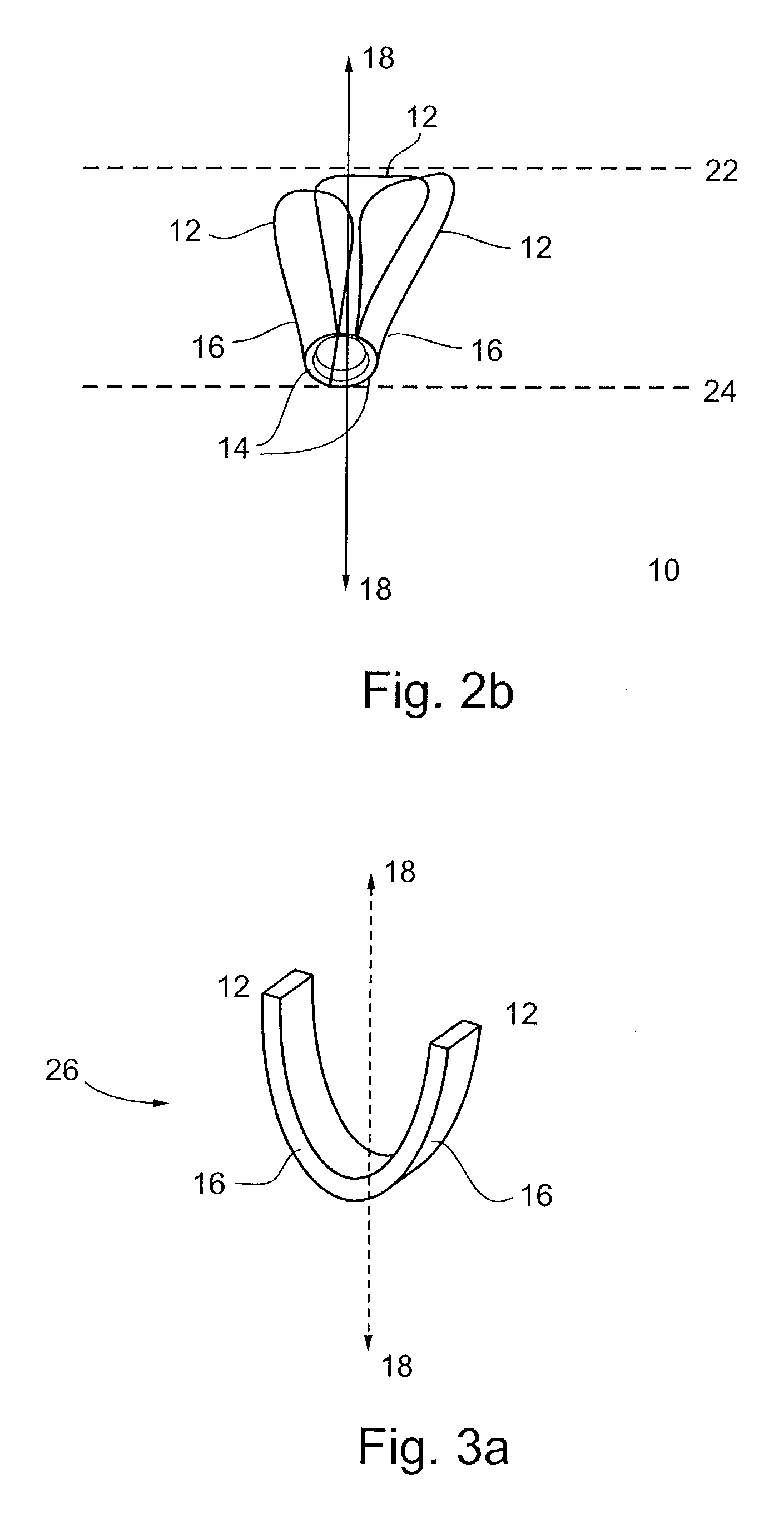
InactiveUS7186210B2Function increaseReduce hydrostatic pressureSuture equipmentsHeart valvesLeft ventricular sizeCardiac cycle
A method and device featuring at least one component providing a potential to kinetic converted elastic, magnetic repulsion, or, an elastic and magnetic repulsion, pushing, pulling, or, pulling and pushing, type of radially outward expansive force or pressure to an inner, outer, intermediate, and, combination thereof, wall region of the left ventricle, for reducing intraluminal hydrostatic pressure of the left ventricle (LV filling pressure) during the ventricular diastolic stage of the cardiac cycle, thereby, improving diastolic function of the left ventricle of the heart in subjects having a condition of diastolic heart failure (DHF), while minimally disturbing systolic function of the heart. The expansive force or pressure is in a range of about 5–40 mm Hg, whereby, left ventricular end diastolic pressure (LVEDP) is reduced down to the normal range of about 6–12 mm Hg, during ventricular diastole of the heart.
Owner:RELAXIS
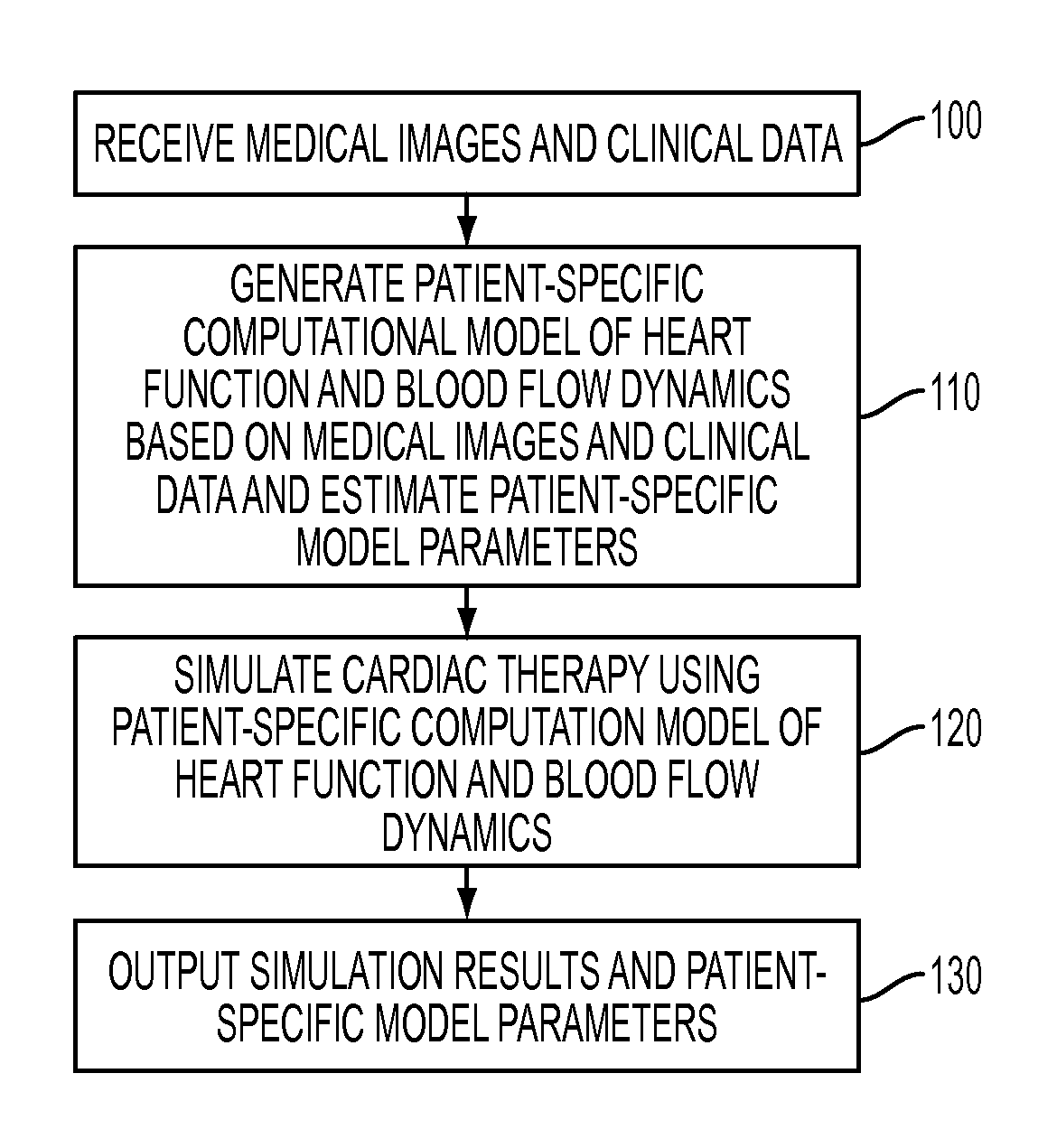
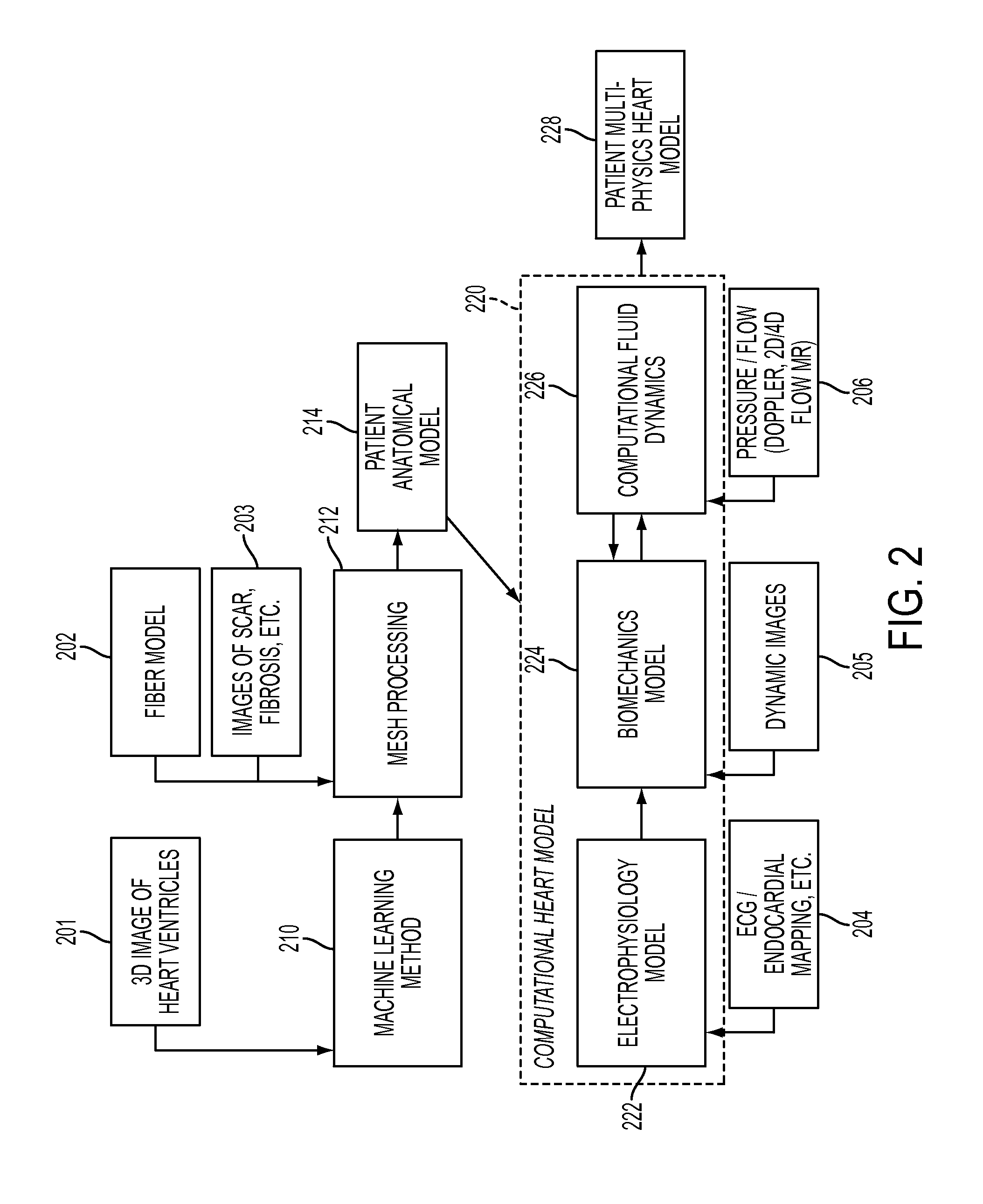
Method and System for Advanced Measurements Computation and Therapy Planning from Medical Data and Images Using a Multi-Physics Fluid-Solid Heart Model
ActiveUS20130197884A1Exact reproductionMedical simulationUltrasonic/sonic/infrasonic diagnosticsComputational modelPatient data
Method and system for computation of advanced heart measurements from medical images and data; and therapy planning using a patient-specific multi-physics fluid-solid heart model is disclosed. A patient-specific anatomical model of the left and right ventricles is generated from medical image patient data. A patient-specific computational heart model is generated based on the patient-specific anatomical model of the left and right ventricles and patient-specific clinical data. The computational model includes biomechanics, electrophysiology and hemodynamics. To generate the patient-specific computational heart model, initial patient-specific parameters of an electrophysiology model, initial patient-specific parameters of a biomechanics model, and initial patient-specific computational fluid dynamics (CFD) boundary conditions are marginally estimated. A coupled fluid-structure interaction (FSI) simulation is performed using the initial patient-specific parameters, and the initial patient-specific parameters are refined based on the coupled FSI simulation. The estimated model parameters then constitute new advanced measurements that can be used for decision making.
Owner:SIEMENS HEALTHCARE GMBH
Device and method for regulating pressure in a heart chamber
A device for regulating blood pressure in a heart chamber is provided. The device includes a shunt positionable within a septum of the heart. The shunt is designed for enabling blood flow between a left heart chamber and a right heart chamber, wherein the flow rate capacity of the device is mostly a function of pressure in the left heart chamber.
Owner:WAVE LTD V
System and method for cardiac valve repair and replacement
A method of delivering a prosthetic mitral valve includes delivering a distal anchor from a delivery sheath such that the distal anchor self-expands inside a first heart chamber on a first side of the mitral valve annulus, pulling proximally on the distal anchor such that the distal anchor self-aligns within the mitral valve annulus and the distal anchor rests against tissue of the ventricular heart chamber, and delivering a proximal anchor from the delivery sheath to a second heart chamber on a second side of the mitral valve annulus such that the proximal anchor self-expands and moves towards the distal anchor to rest against tissue of the second heart chamber. The self-expansion of the proximal anchor captures tissue of the mitral valve annulus therebetween.
Owner:CEPHEA VALVE TECH
Transapical mitral valve repair device
Methods and devices for repairing a cardiac valve. A minimally invasive procedure includes creating an access in the apex region of the heart through which one or more instruments may be inserted. The device can implant artificial heart valve chordae tendineae into cardiac valve leaflet tissues to restore proper leaflet function and prevent reperfusion. The device punctures the apex of the heart and travels through the ventricle. The tip of the device rests on the defective valve and punctures the valve leaflet. A suture or a suture / guide wire combination is inserted, securing the top of the leaflet to the apex of the heart. A resilient element or shock absorber mechanism adjacent to the outside of the apex of the heart minimizes the linear travel of the device in response to the beating of the heart or opening / closing of the valve.
Owner:UNIV OF MARYLAND BALTIMORE
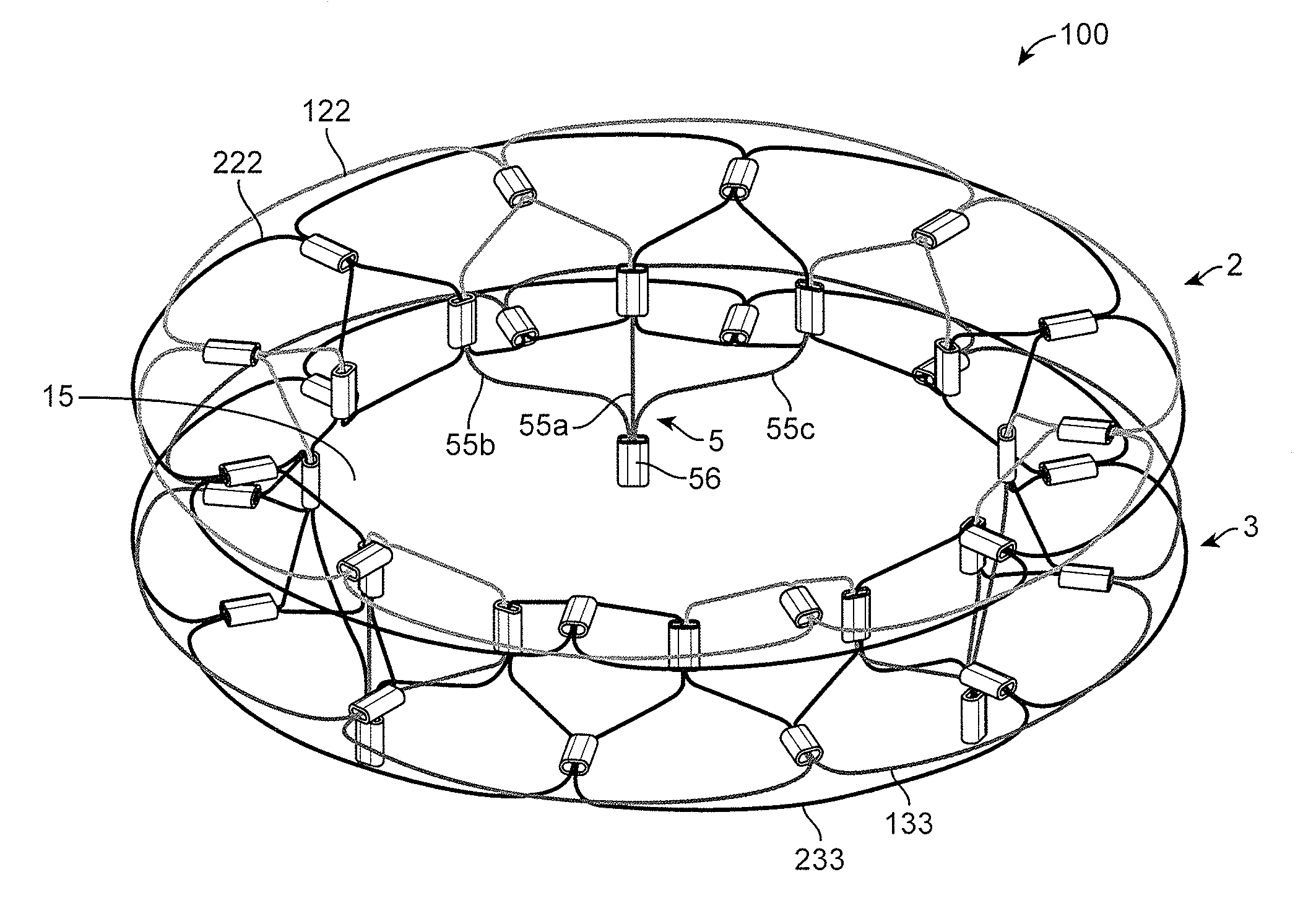
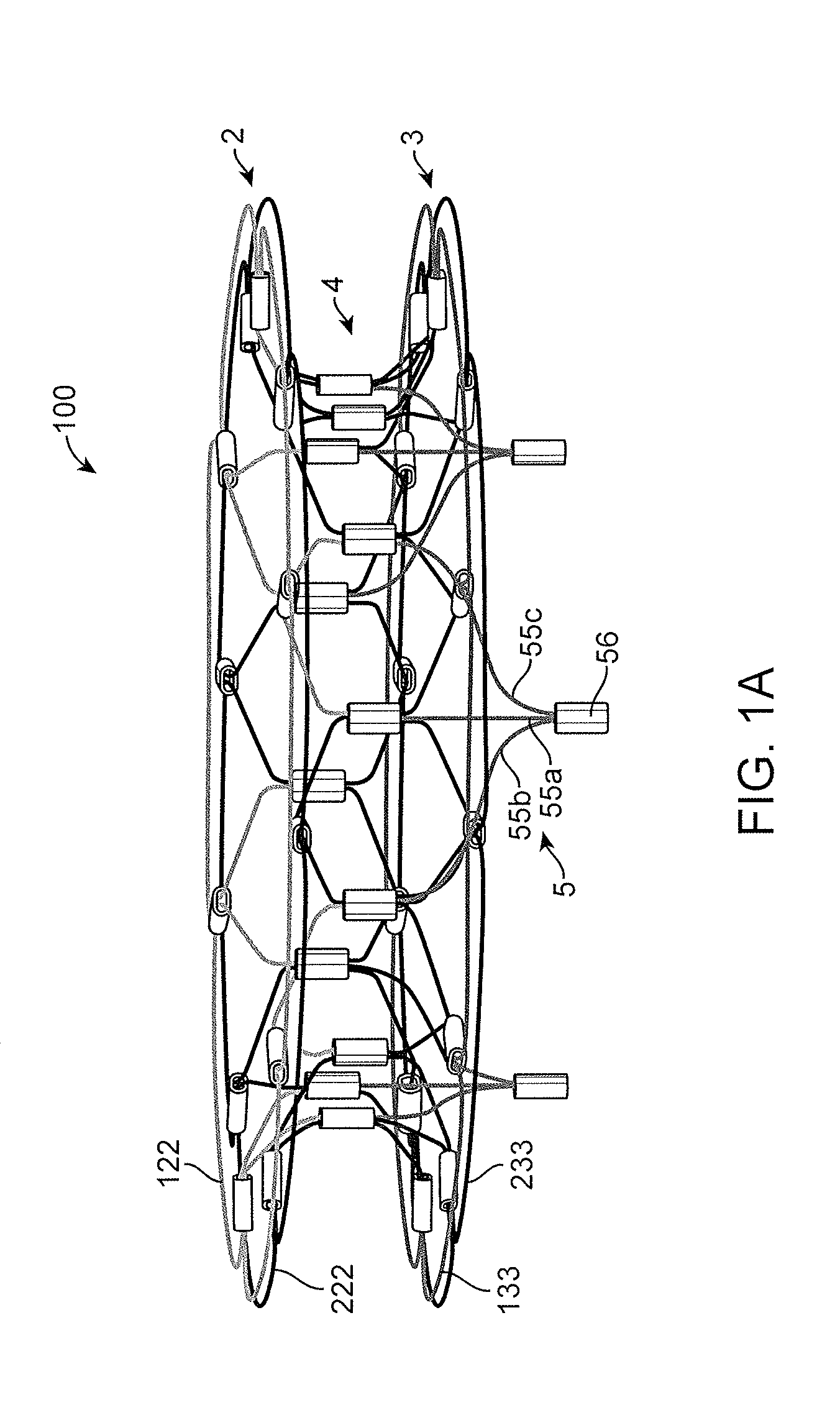
Implantation of repair chords in the heart
ActiveUS20160158008A1Reduce the overall diameterEasy to implantSuture equipmentsHeart valvesCardiac VentricleTissue Part
Apparatus is provided, including first and second longitudinal members coupled at respective first portions thereof to tissue surrounding the ventricle. The first portion of at least the first longitudinal member is coupled to a tissue anchor, and respective second portions of the first and second longitudinal members are coupled to respective first and second leaflets of a cardiac valve. The longitudinal members are arranged with respect to the tissue anchor and the portion of tissue surrounding the ventricle in a manner which facilitates adjustment of a degree of tension of the first and second longitudinal members to draw the first and second leaflets together. A longitudinal-member-coupling device is coupled to the first and second longitudinal members, and is advanceable toward a ventricular surface of the first and second leaflets, and responsively to draw together the first and second longitudinal members. Other applications are also described.
Owner:VALTECH CARDIO LTD
Methods and devices for delivering a ventricular stent
A method, and related tools for performing the method, of delivering a stent or other like device to the heart to connect the left ventricle to the coronary artery to thereby supply blood directly from the ventricle to the coronary artery may be used to bypass a total or partial occlusion of a coronary artery. The method may include placing a guide device and a dilation device through an anterior wall and a posterior wall of the coronary vessel and through a heart wall between the heart chamber and the coronary vessel. The dilation device may be used to form a passageway in the heart wall at a location defined by the guide device. The method may then include placing a stent within the passageway.
Owner:HORIZON TECH FUNDING CO LLC
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com