Patents
Literature
403results about How to "Potential damage" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
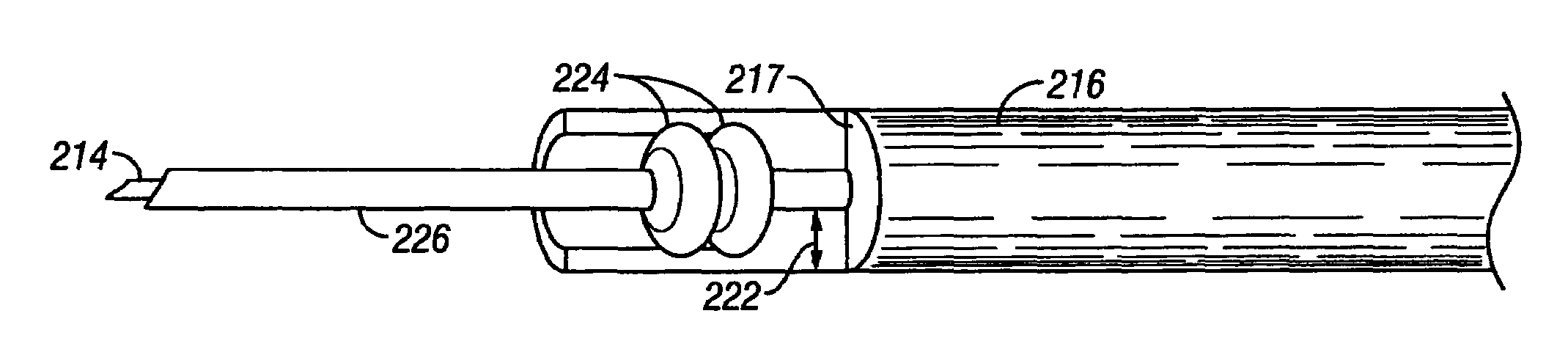
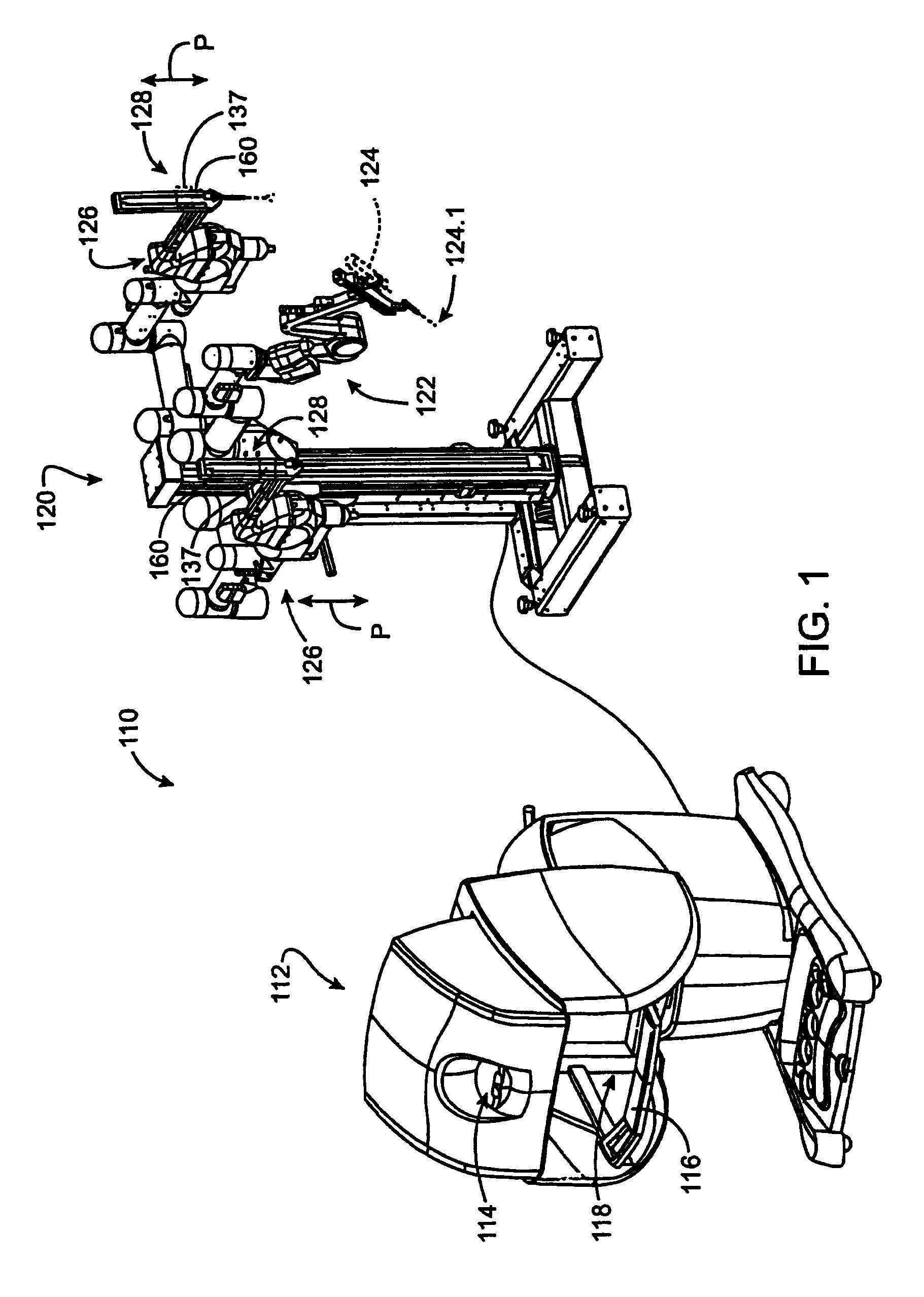
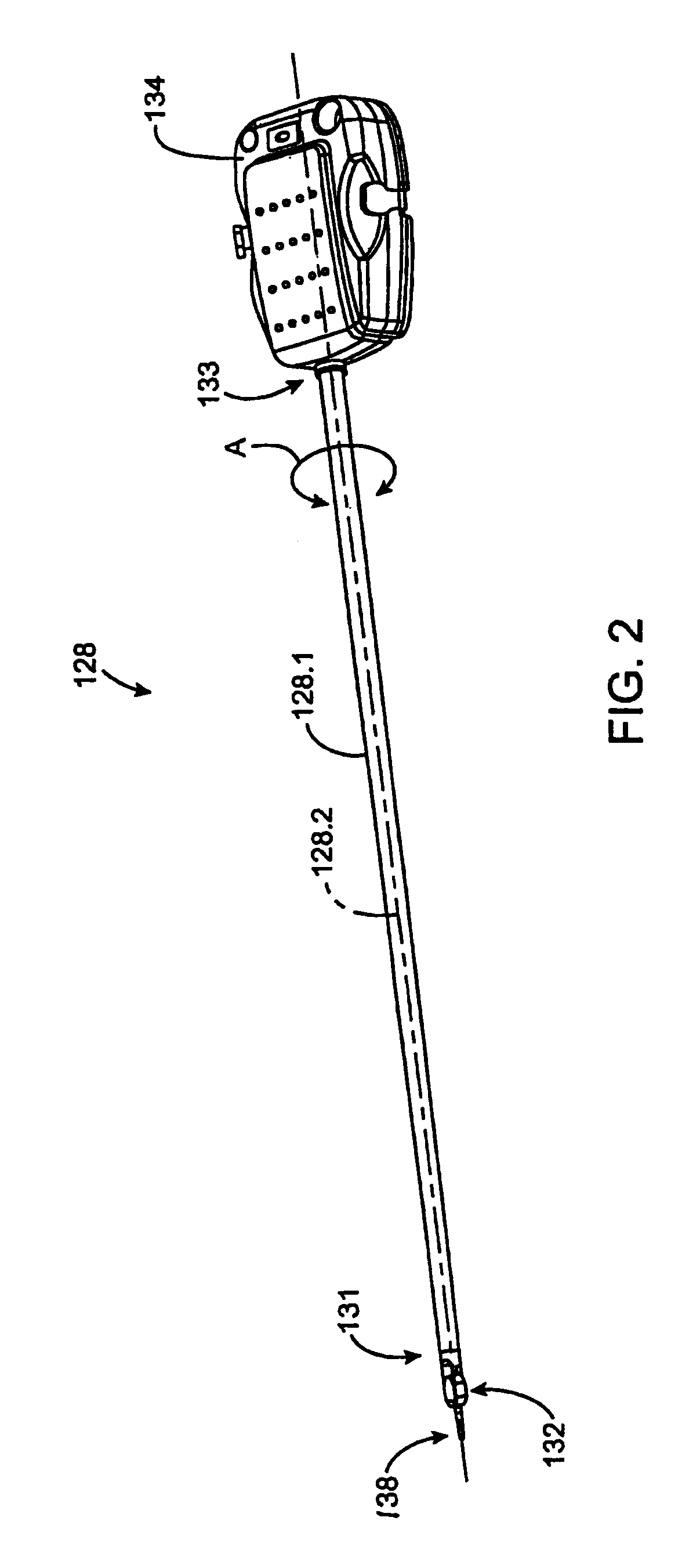
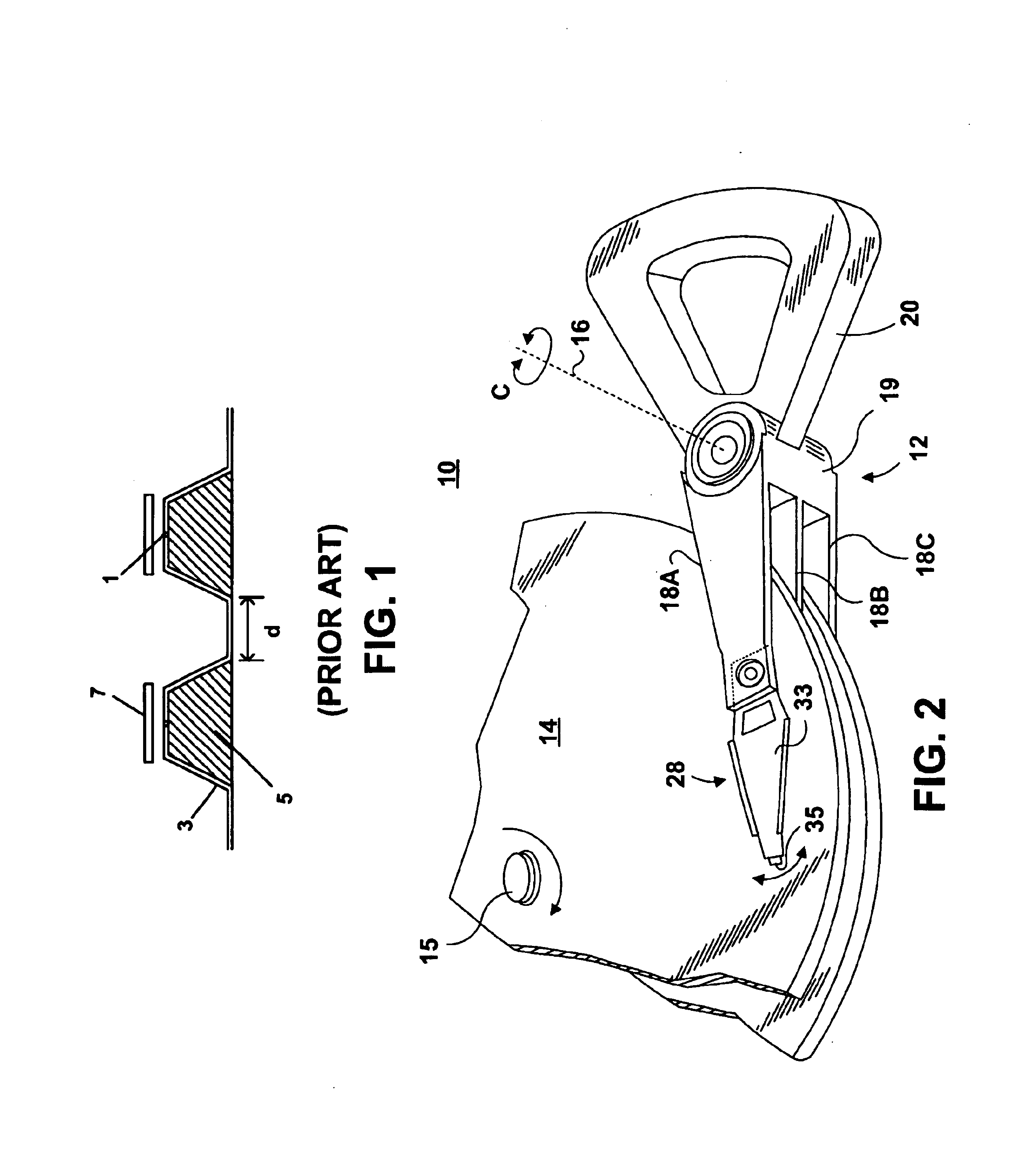
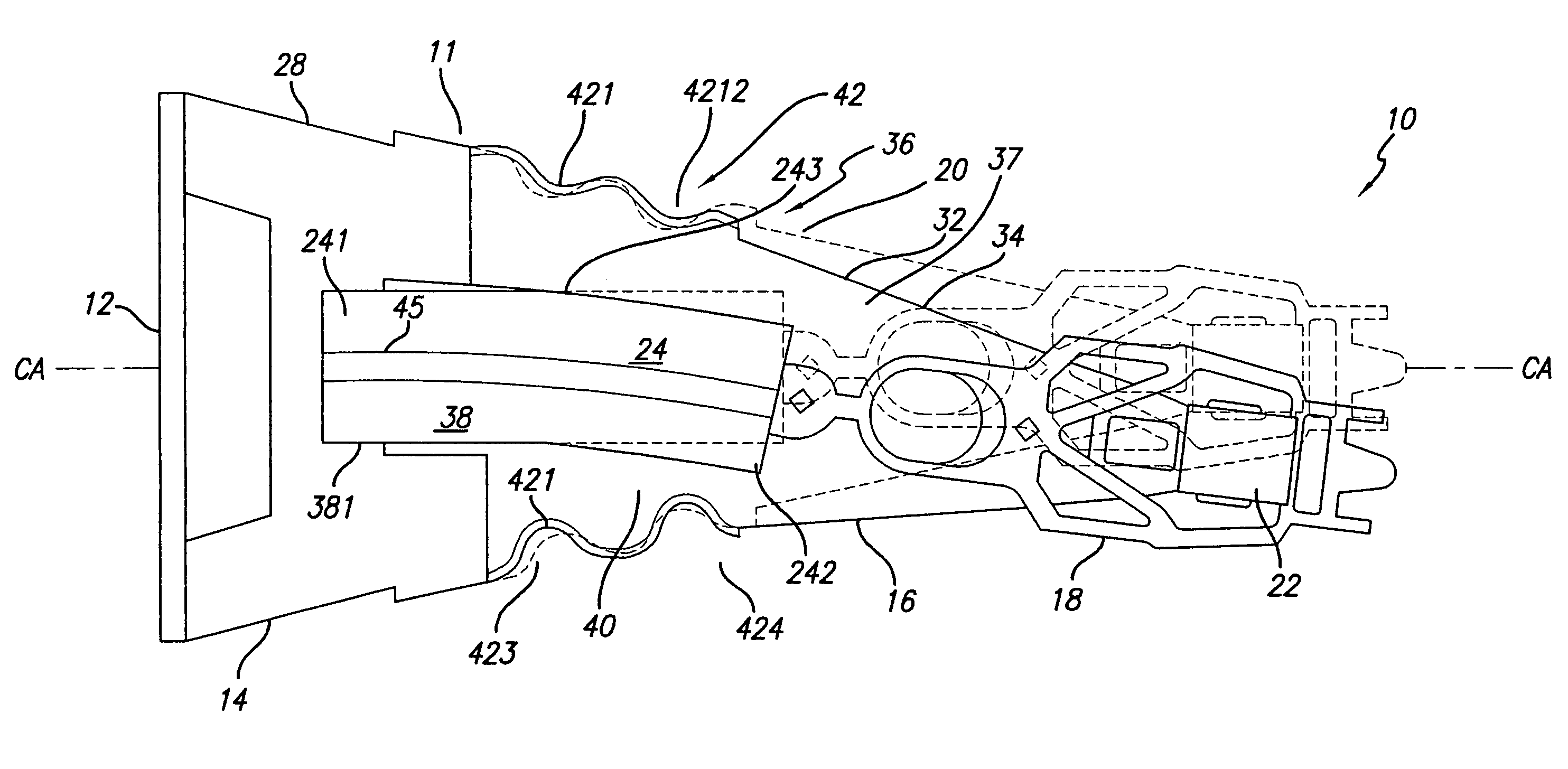
Surgical tool having electrocautery energy supply conductor with inhibited current leakage
InactiveUS7083615B2Low costEasy to manufactureDiagnosticsSurgical instruments for heatingCapacitanceElectrical conductor
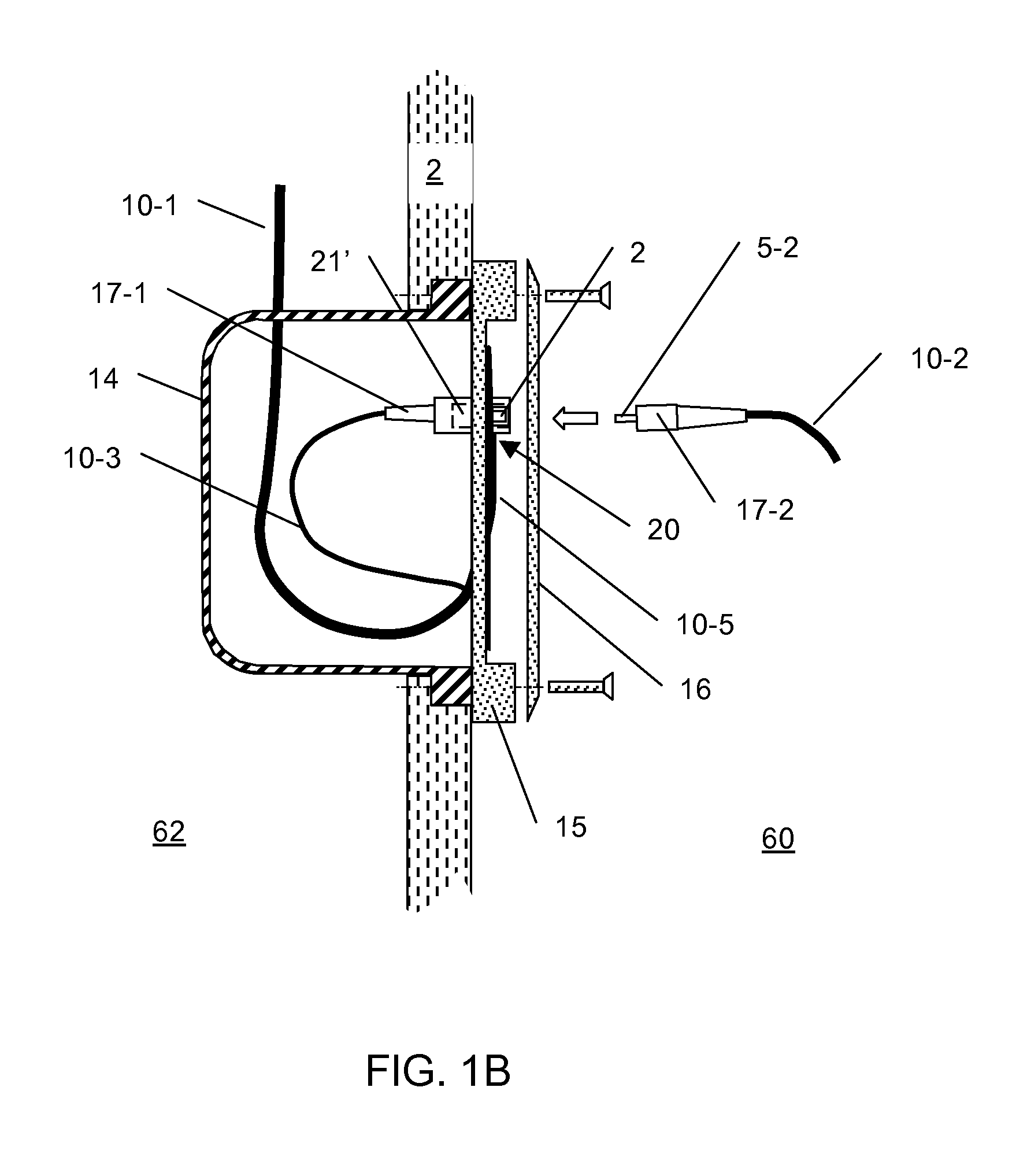
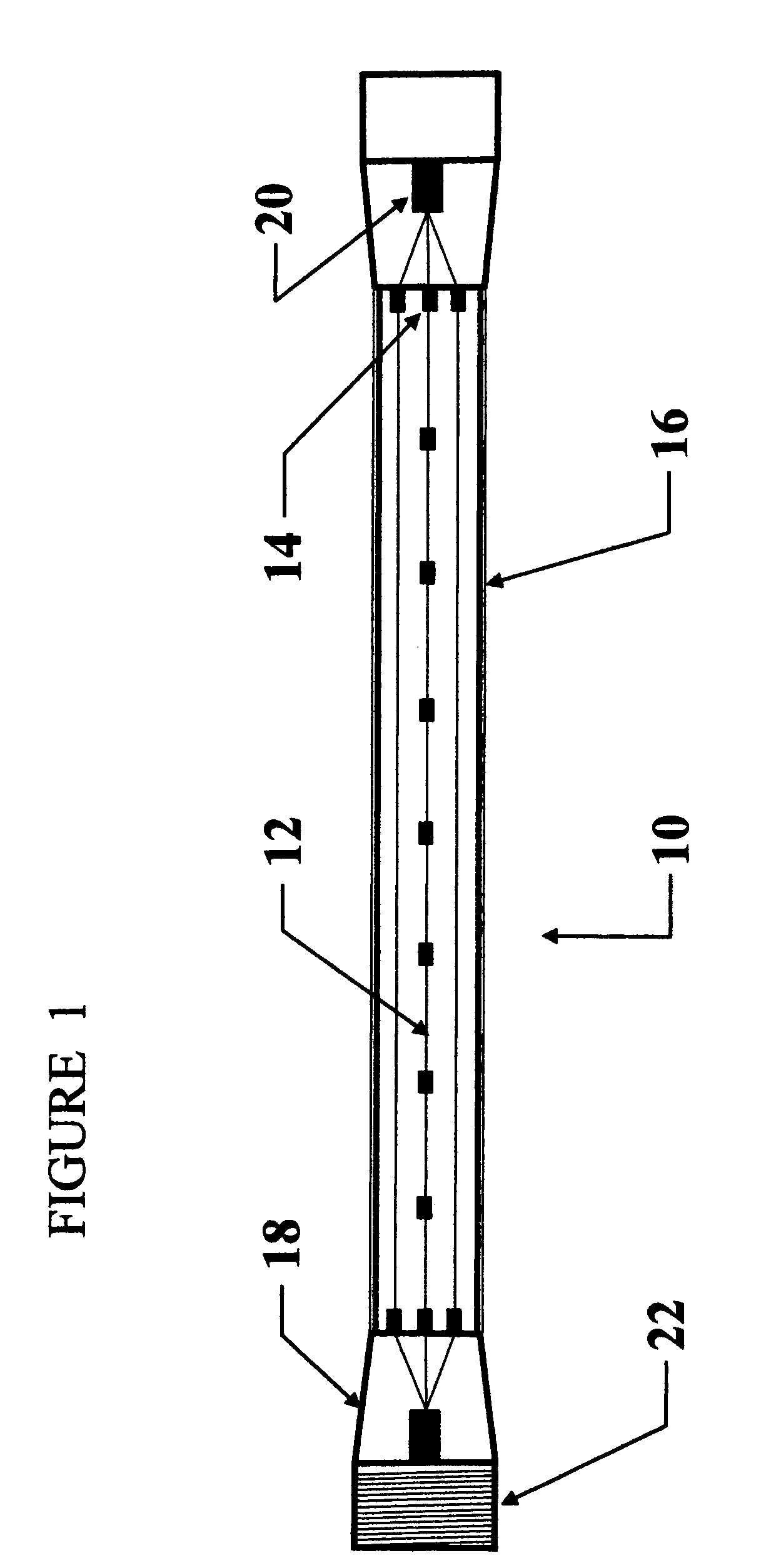
The present invention provides improved electrosurgical instruments and systems having electrocautery energy supply conductors that provide inhibited current leakage and methods of performing a robotically controlled minimally invasive surgical procedure while preventing unintended capacitive coupling. A surgical instrument generally comprises an elongate shaft having a proximal end and a distal end and defining an internal longitudinally extending passage. An electrocautery end effector is coupled to or disposed at the distal end of the shaft. An interface or tool base is coupled to or disposed at the proximal end of the shaft and removably connectable to the robotic surgical system. Typically, an independent electrical conductor extends from the interface to the end effector to transmit electrical energy to tissue engaged by the end effector. A sealed insulation tube extends within the passage and over the conductor. A separation is maintained between the sealed insulation tube and the conductor.
Owner:INTUITIVE SURGICAL OPERATIONS INC
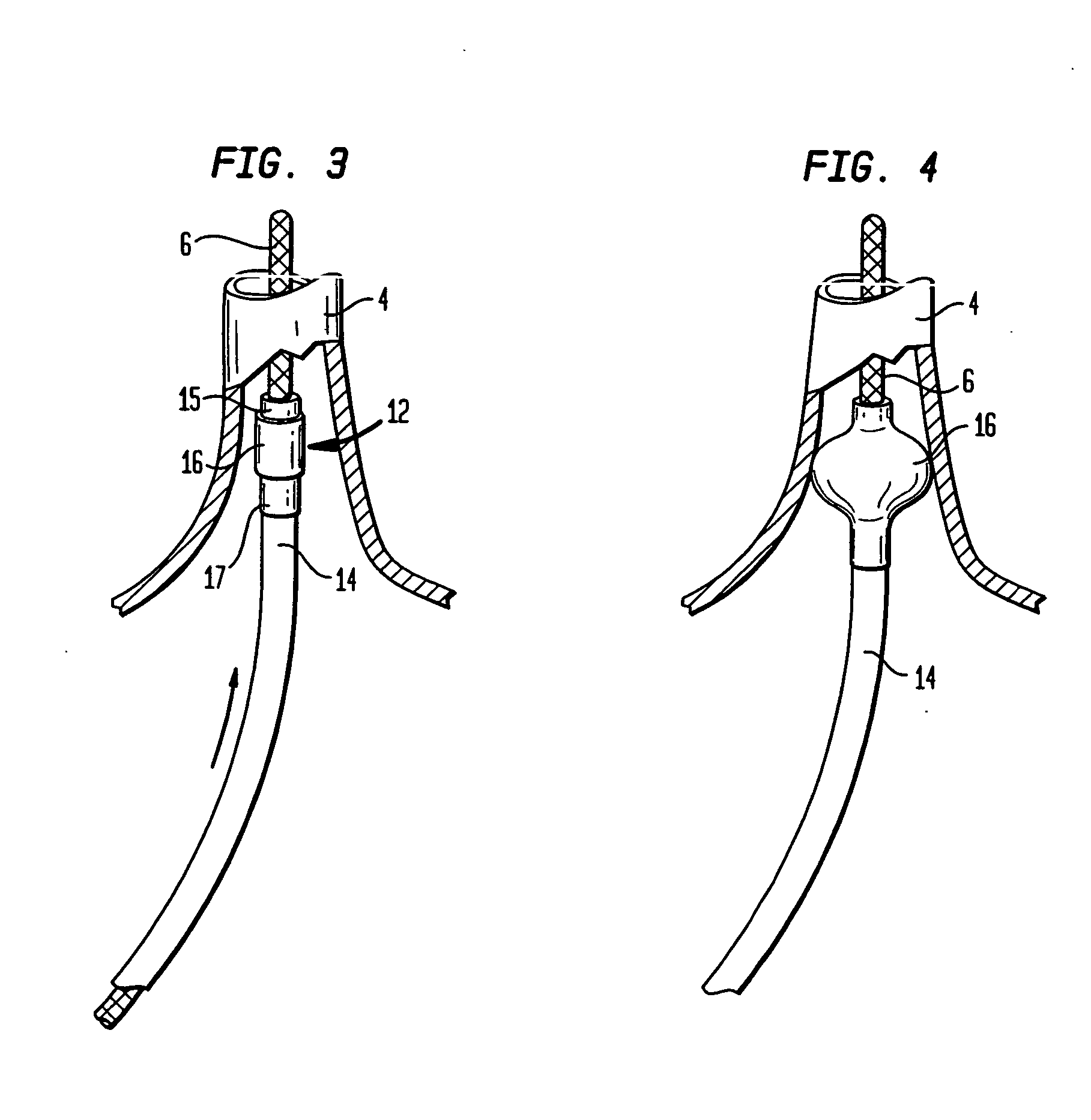
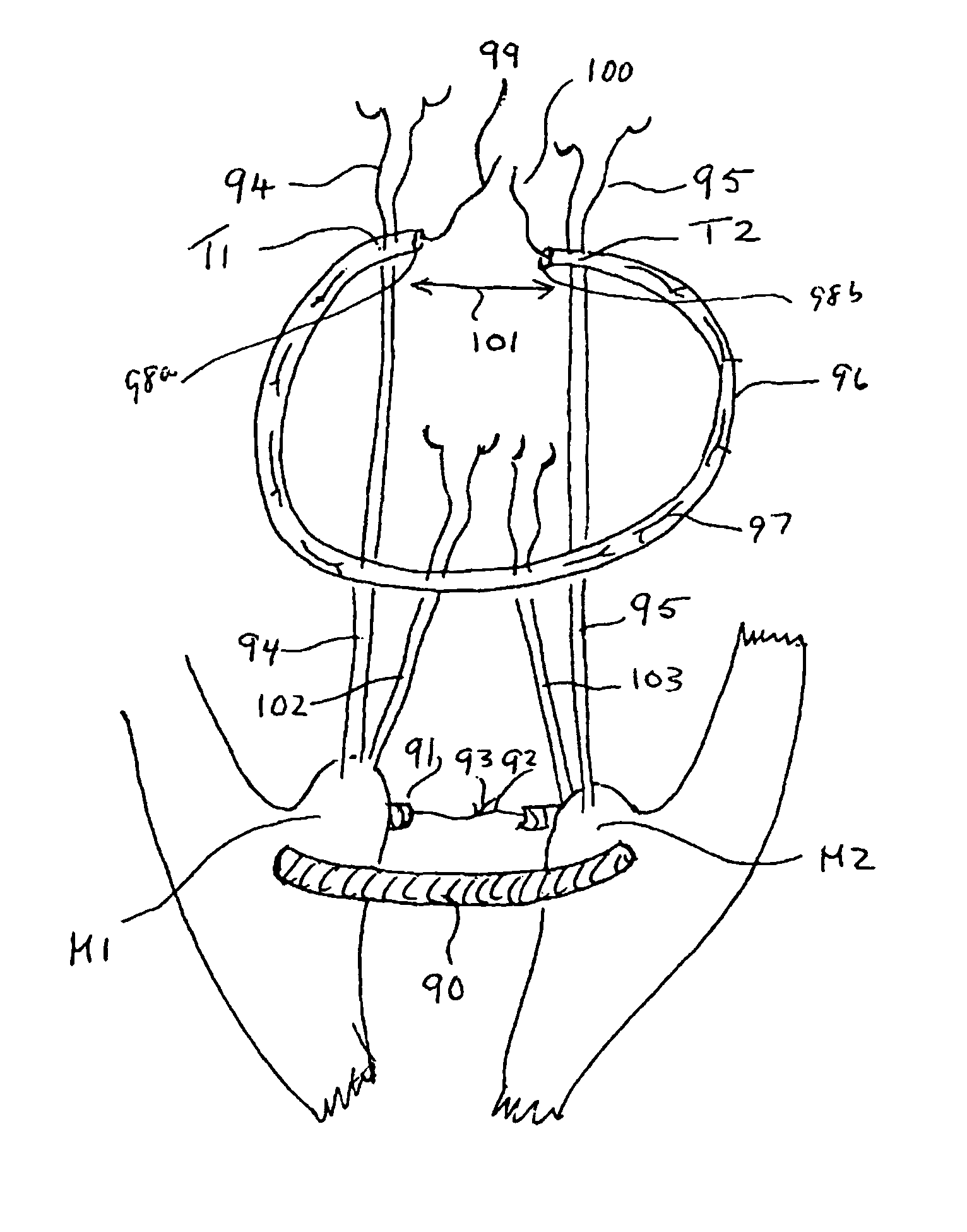
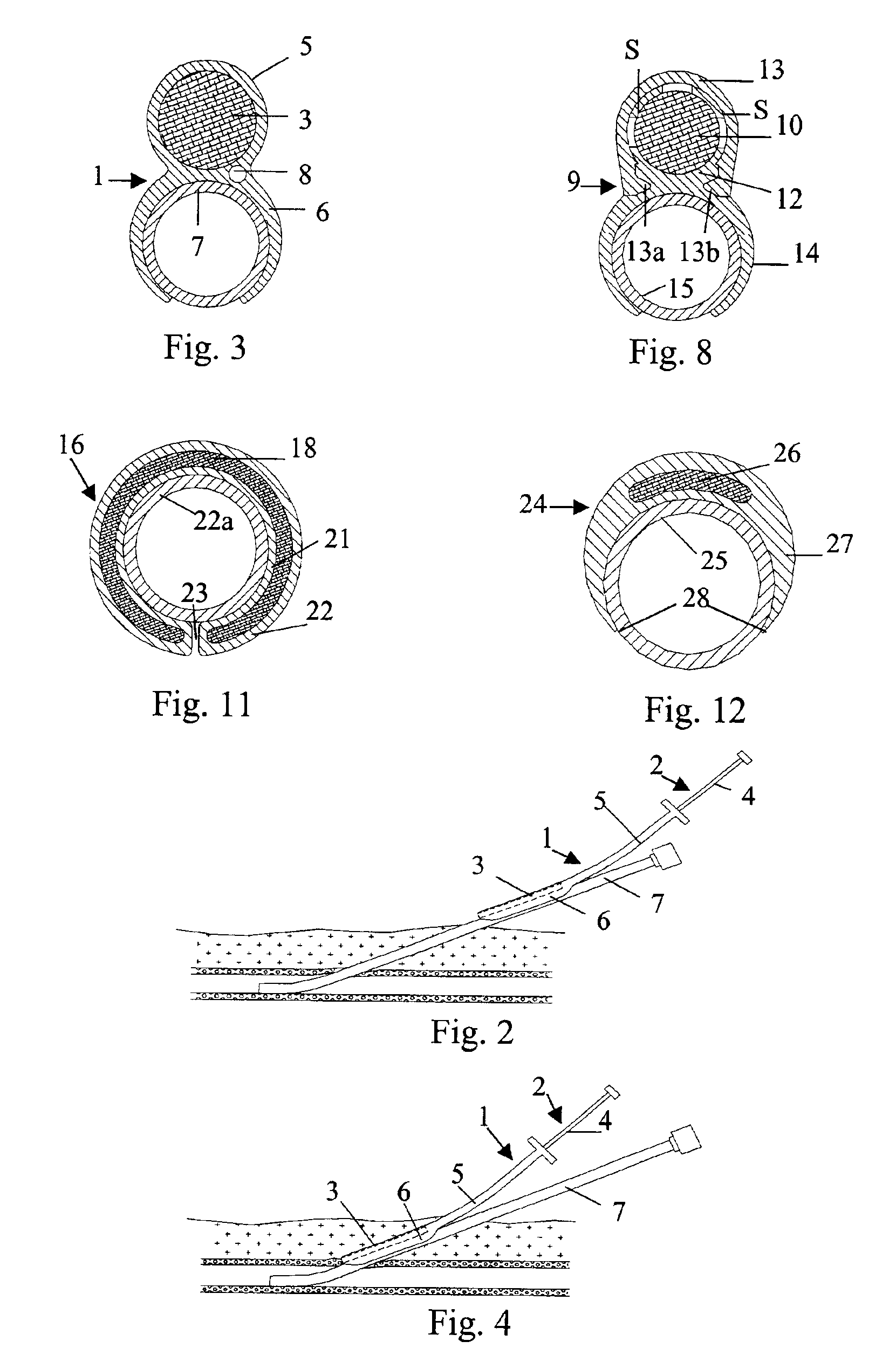
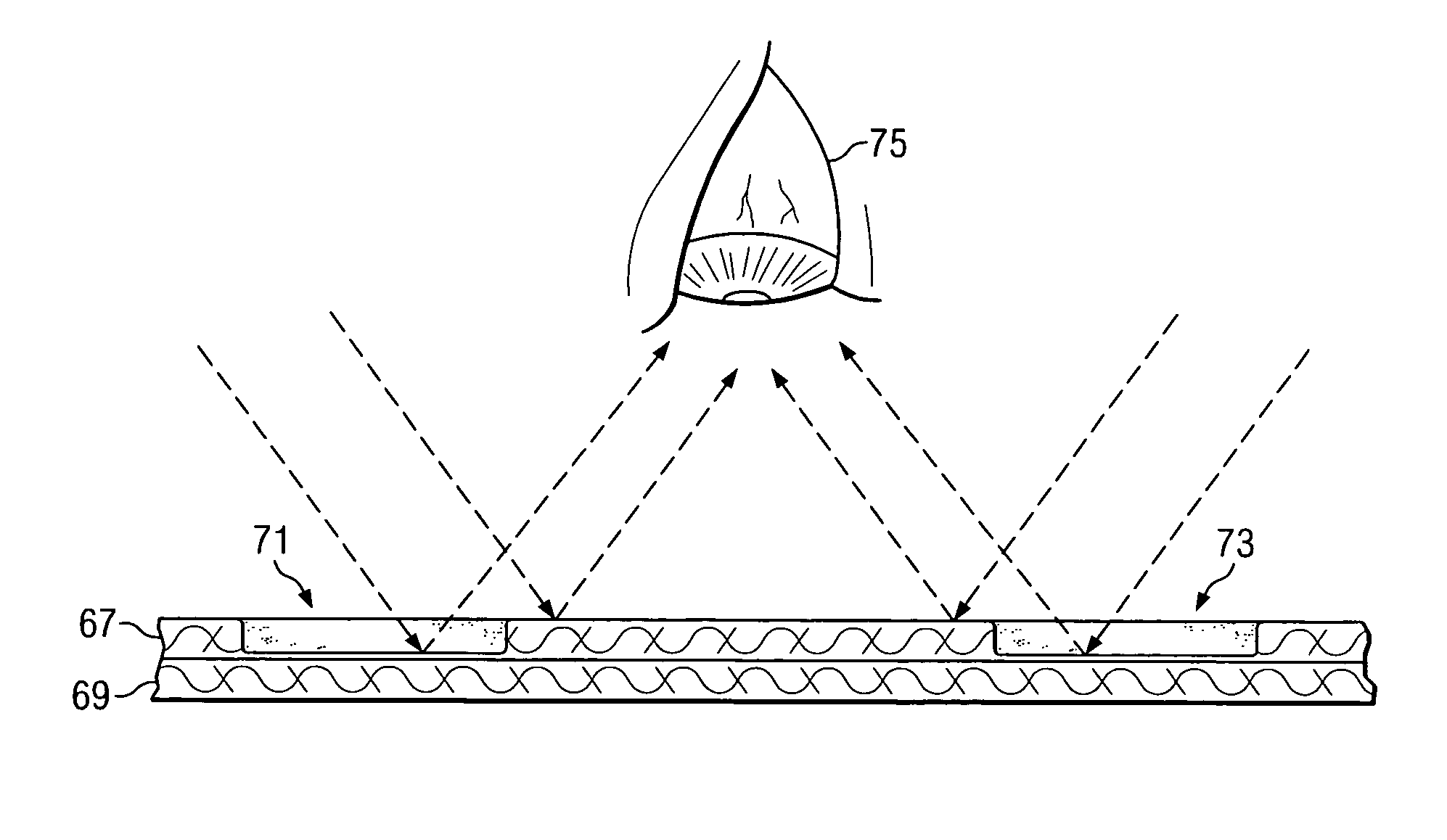
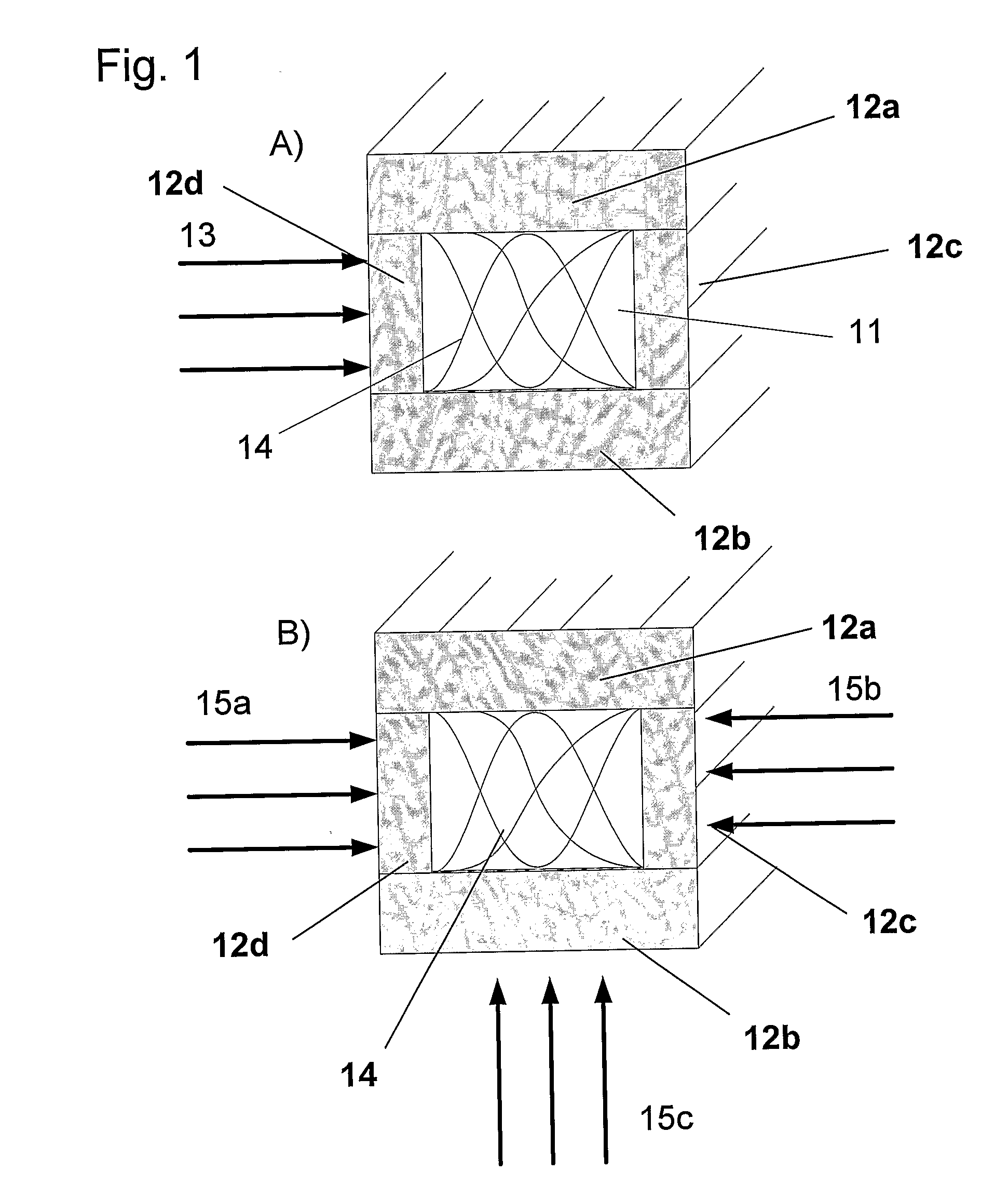
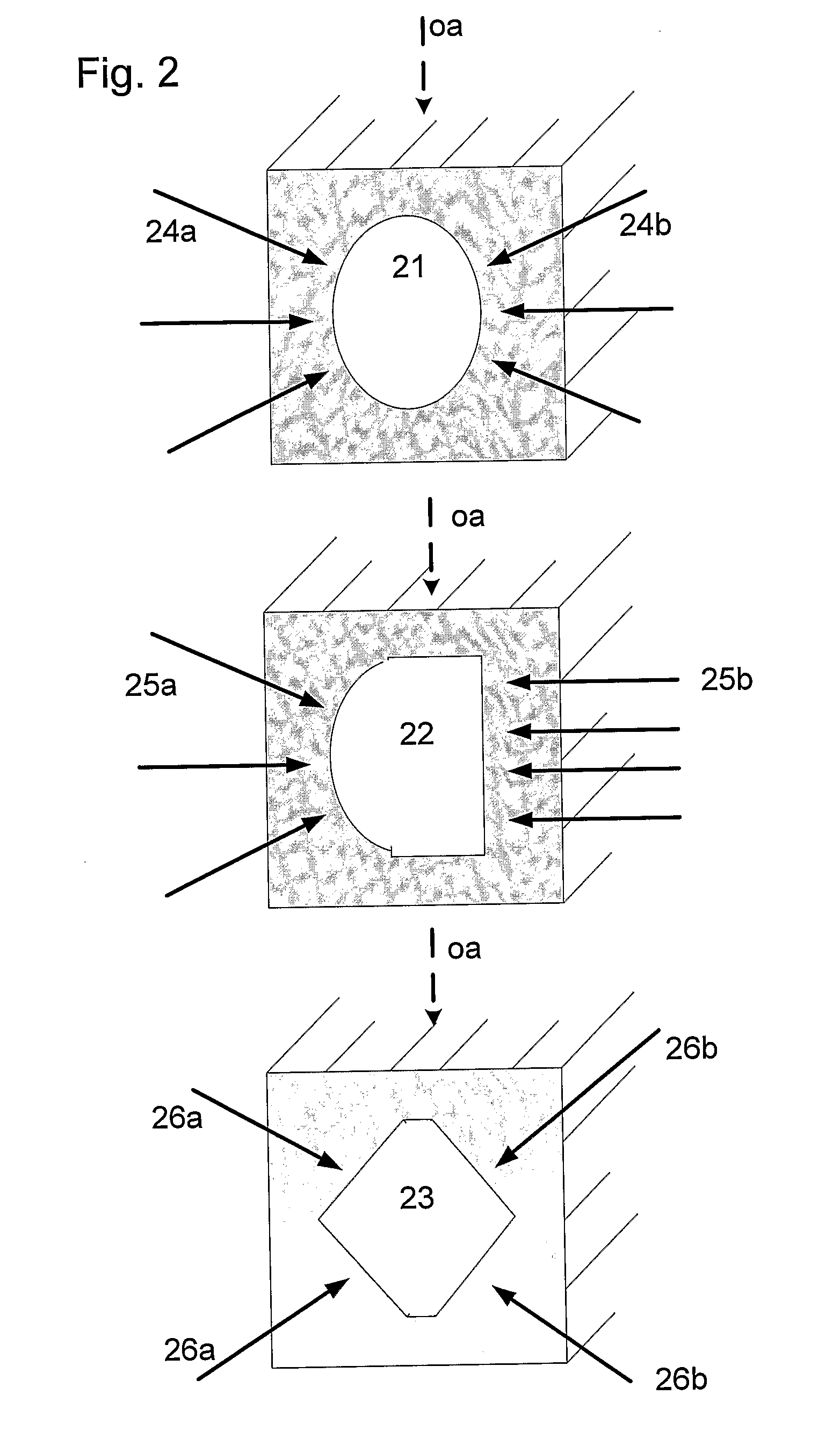
Coaxial catheter instruments for ablation with radiant energy
InactiveUS20050038419A9Rapid and effective photoablationLess timeStentsUltrasound therapyCoaxial catheterTarget tissue
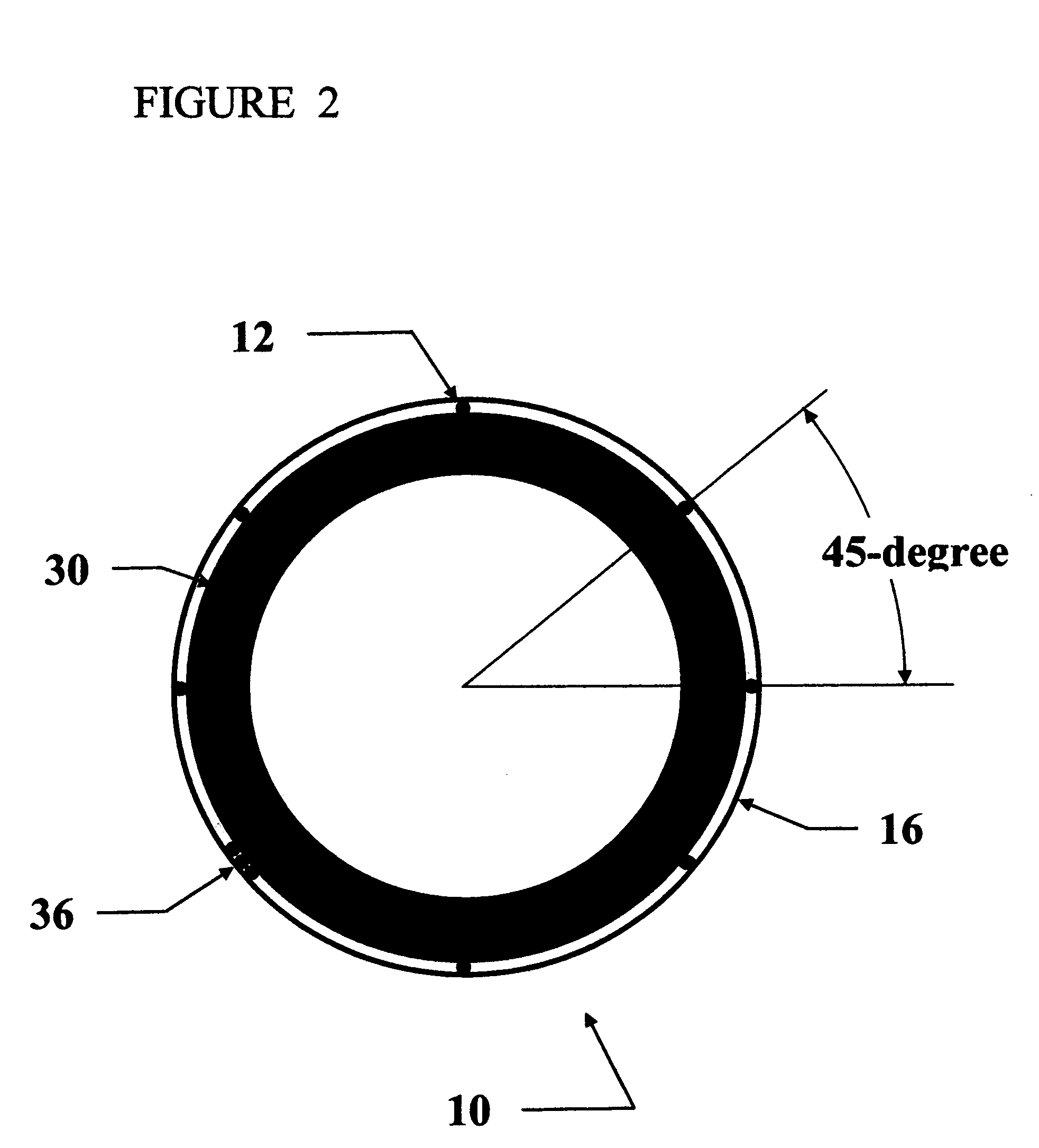
Ablation methods and instruments are disclosed for creating lesions in tissue, especially cardiac tissue for treatment of arrhythmias and the like. Percutaneous ablation instruments in the form of coaxial catheter bodies are disclosed having at least one central lumen therein and having one or more balloon structures at the distal end region of the instrument. The instruments include an energy emitting element which is independently positionable within the lumen of the instrument and adapted to project radiant energy through a transmissive region of a projection balloon to a target tissue site. The instrument can optionally include at least one expandable anchor balloon disposed about, or incorporated into an inner catheter body designed to be slid over a guidewire. This anchor balloon can serve to position the device within a lumen, such as a pulmonary vein. A projection balloon structure is also disclosed that can be slid over the first (anchor balloon) catheter body and inflated within the heart, to define a staging from which to project radiant energy. An ablative fluid can also be employed outside of the instrument (e.g., between the balloon and the target region) to ensure efficient transmission of the radiant energy when the instrument is deployed. In another aspect of the invention, generally applicable to a wide range of cardiac ablation instruments, mechanisms are disclosed for determining whether the instrument has been properly seated within the heart, e.g., whether the device is in contact with a pulmonary vein and / or the atrial surface, in order to form a lesion by heating, cooling or projecting energy. This contact-sensing feature can be implemented by an illumination source situated within the instrument and an optical detector that monitors the level of reflected light. Measurements of the reflected light (or wavelengths of the reflected light) can thus be used to determine whether contact has been achieved and whether such contact is continuous over a desired ablation path.
Owner:CARDIOFOCUS INC
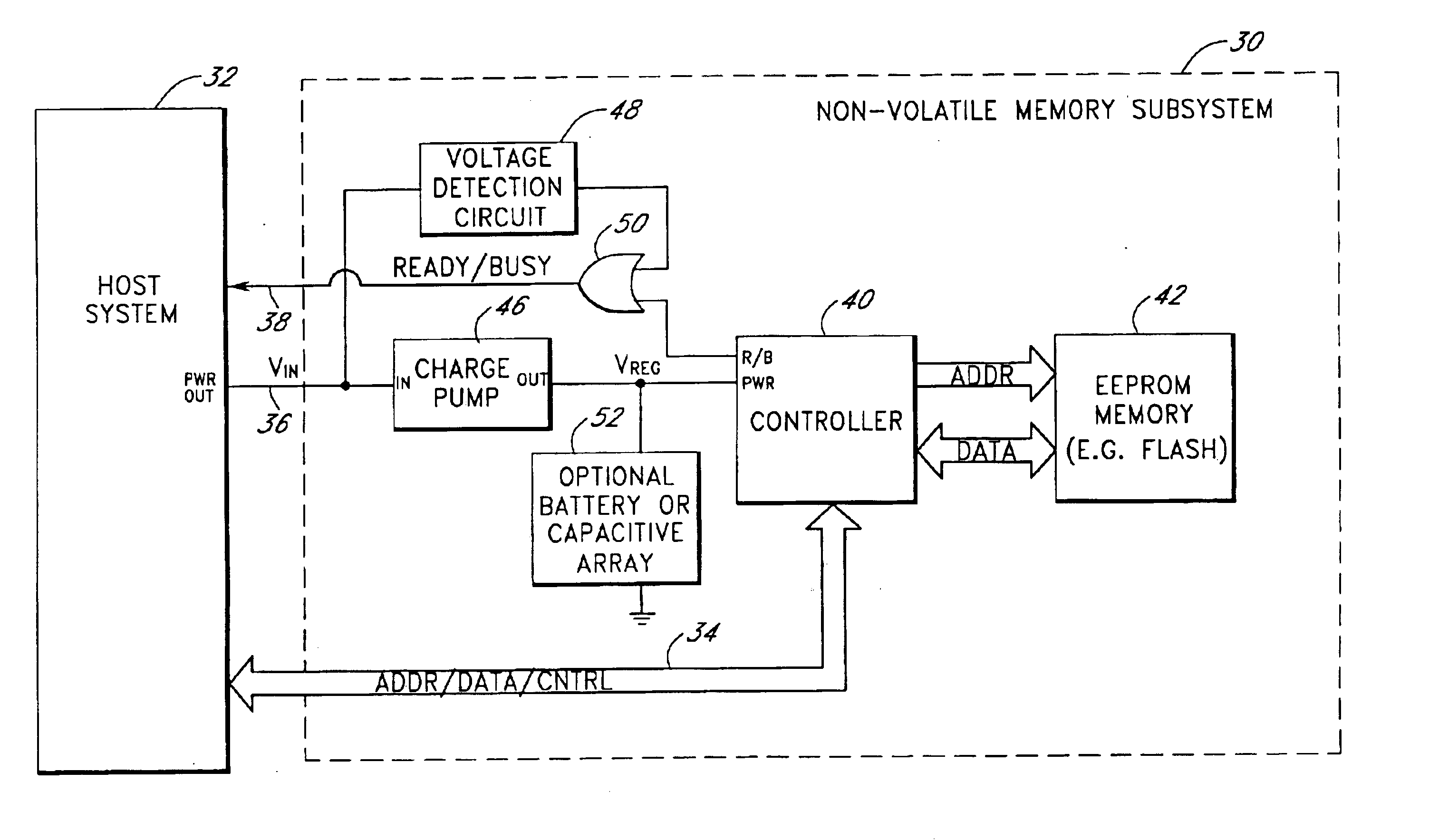
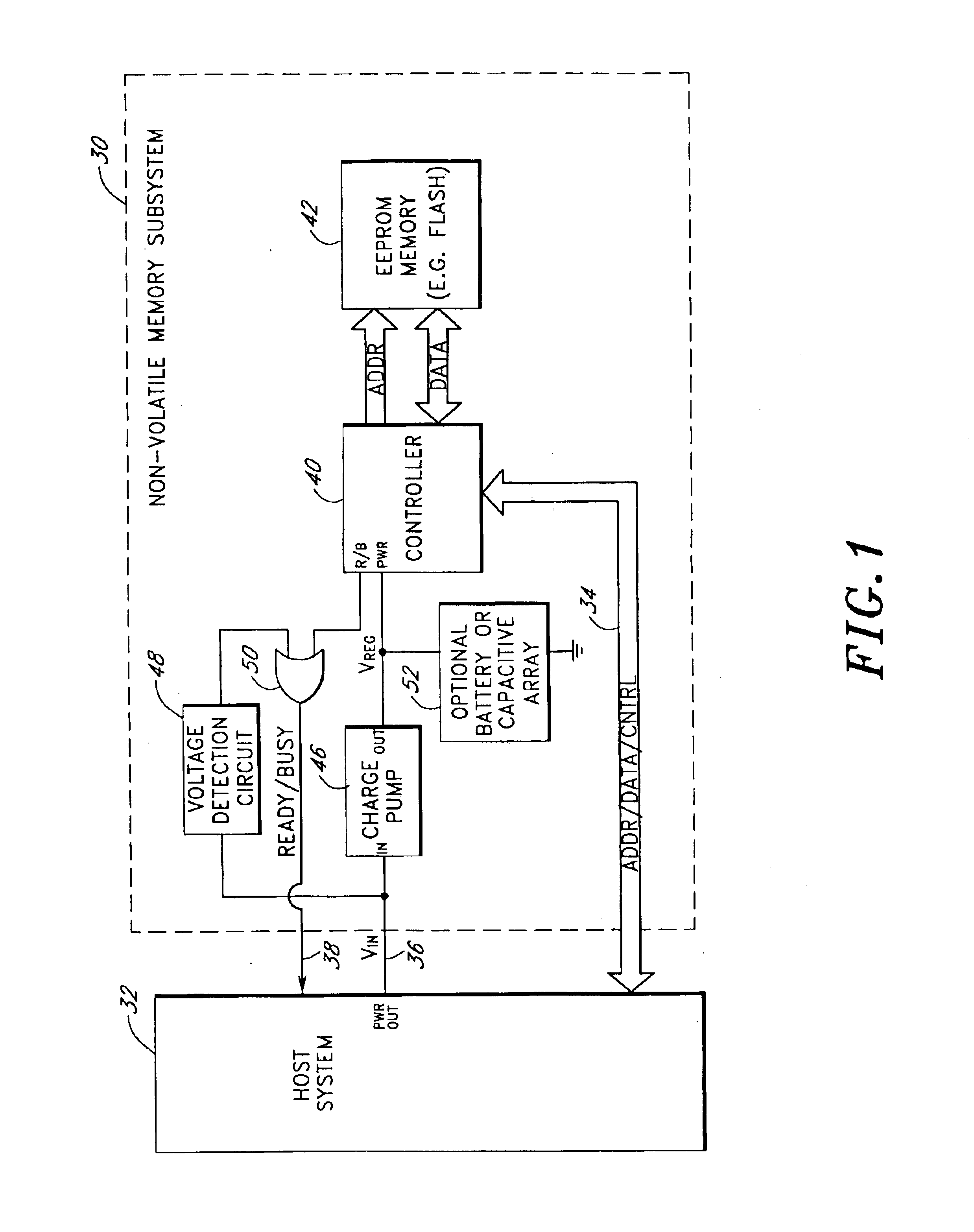
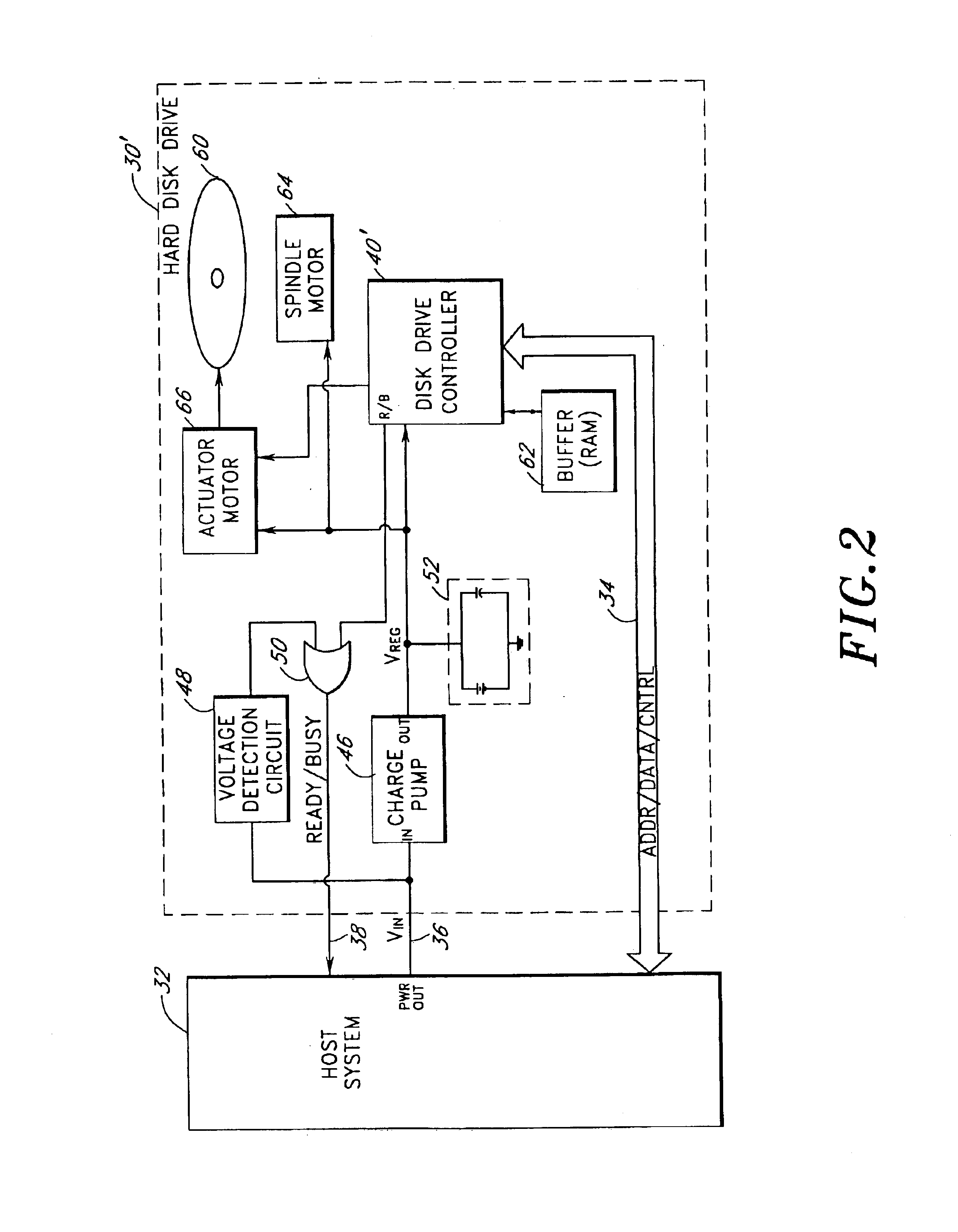
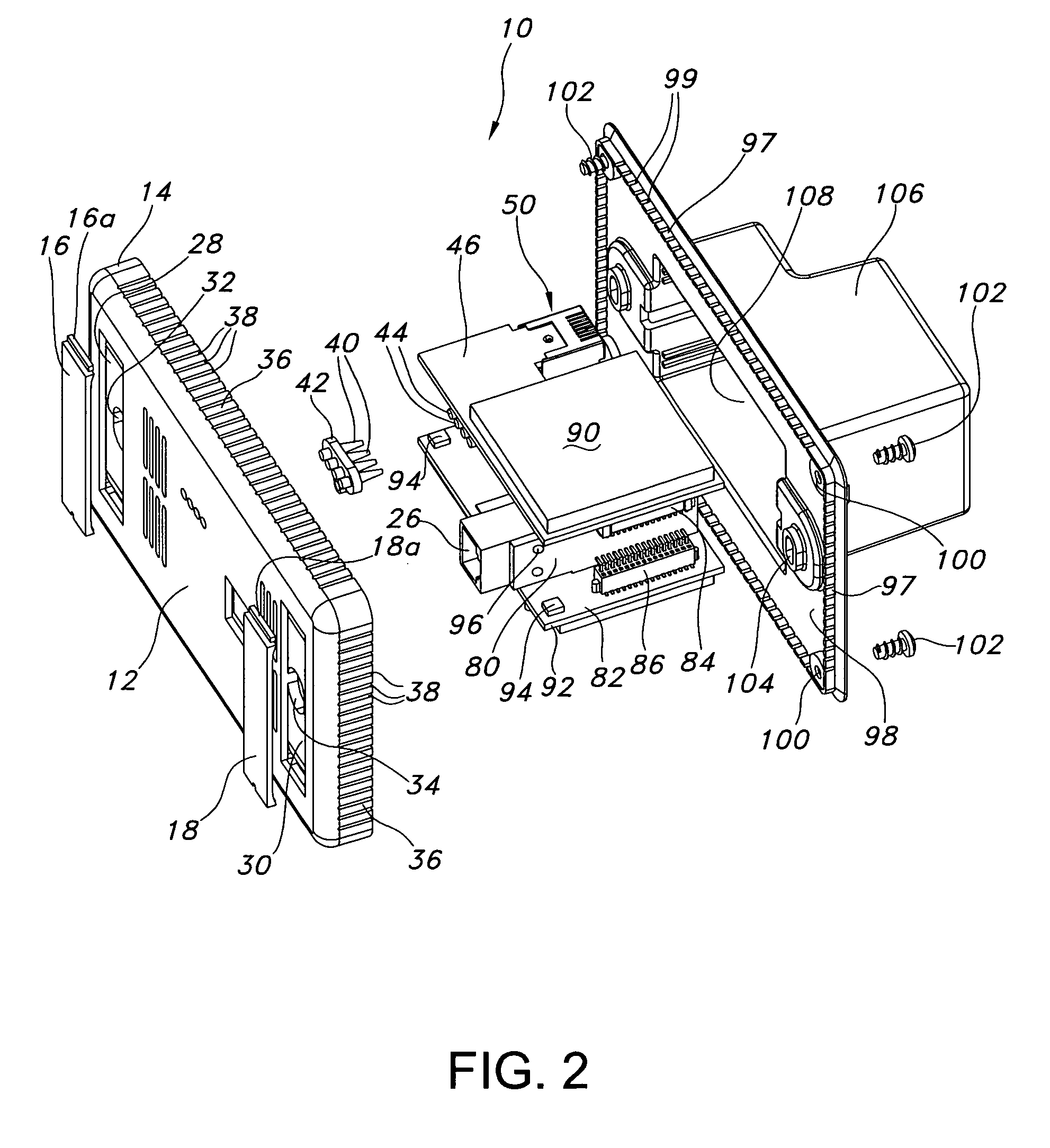
Storage subsystem with embedded circuit for protecting against anomalies in power signal from host
InactiveUS6856556B1Potential damageReduce the possibilityRead-only memoriesDigital storageStandby powerEngineering
A storage subsystem, such as a flash memory card, includes a charge pump that receives a power signal from a host system, and generates a regulated power signal that is provided to the storage subsystem's controller. When the power signal from the host is interrupted, the charge pump additionally acts as a backup power supply such that the storage subsystem can continue to operate temporarily. The storage subsystem also includes a voltage detection circuit that monitors the power signal from the host system to detect anomalies therein. The voltage detection circuit responds to detection of an anomaly by asserting a busy signal to block the host system from performing write operations to the storage subsystem. By asserting the busy signal, the voltage detection circuit substantially ensures that the backup, regulated power provided by the charge pump will be sufficient for the controller to complete all outstanding operations.
Owner:INNOVATIVE MEMORY SYST INC
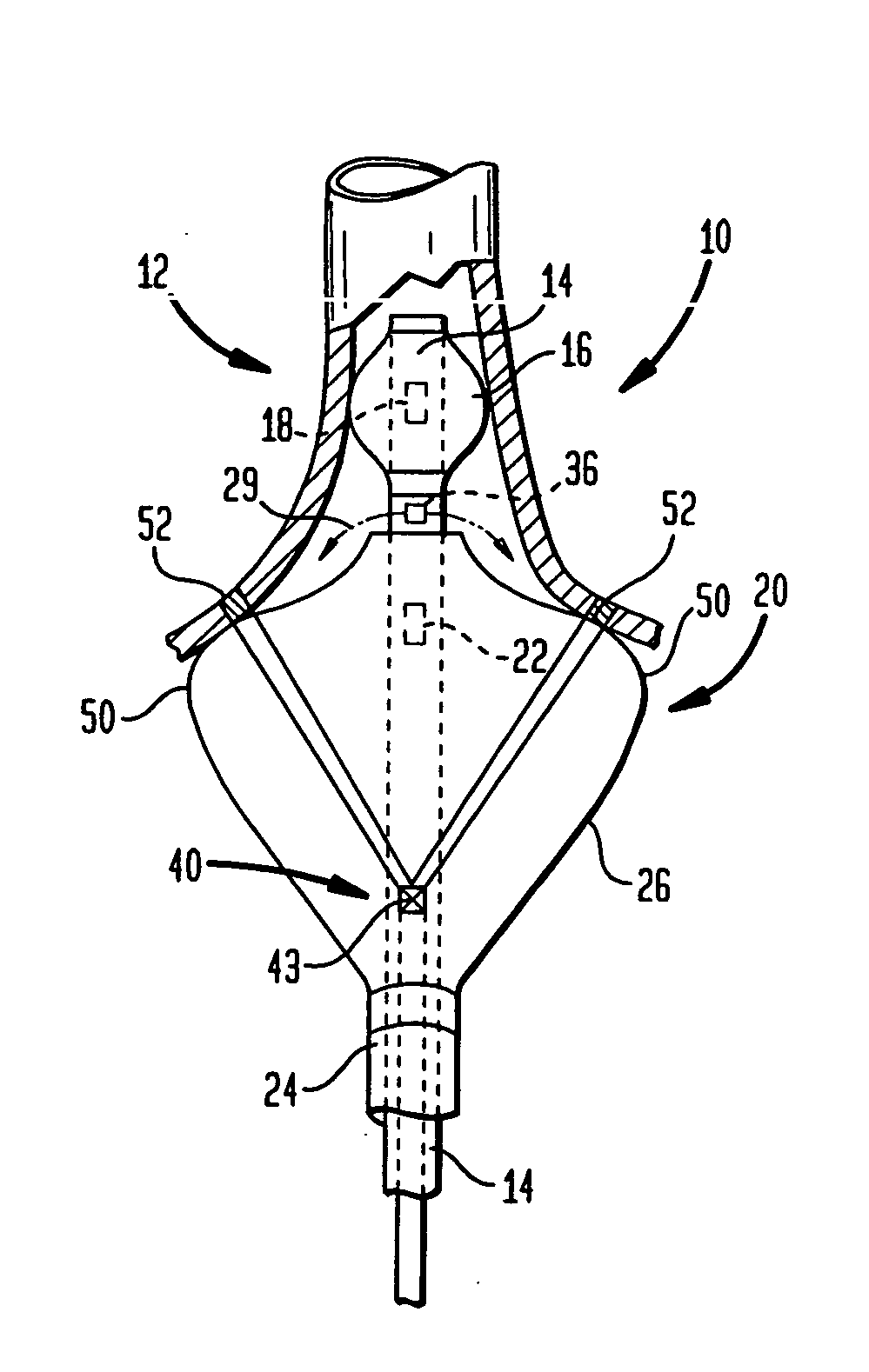
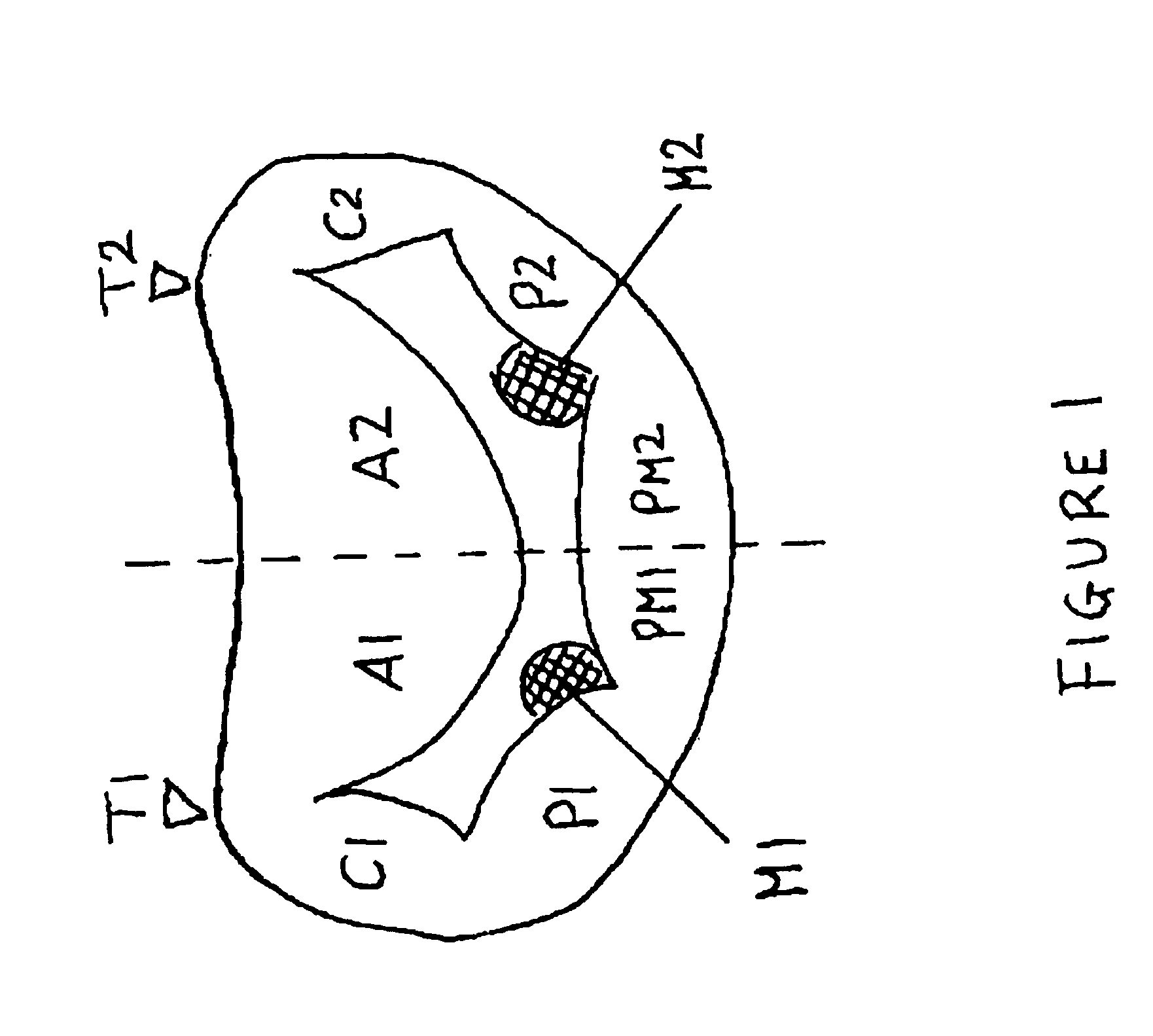
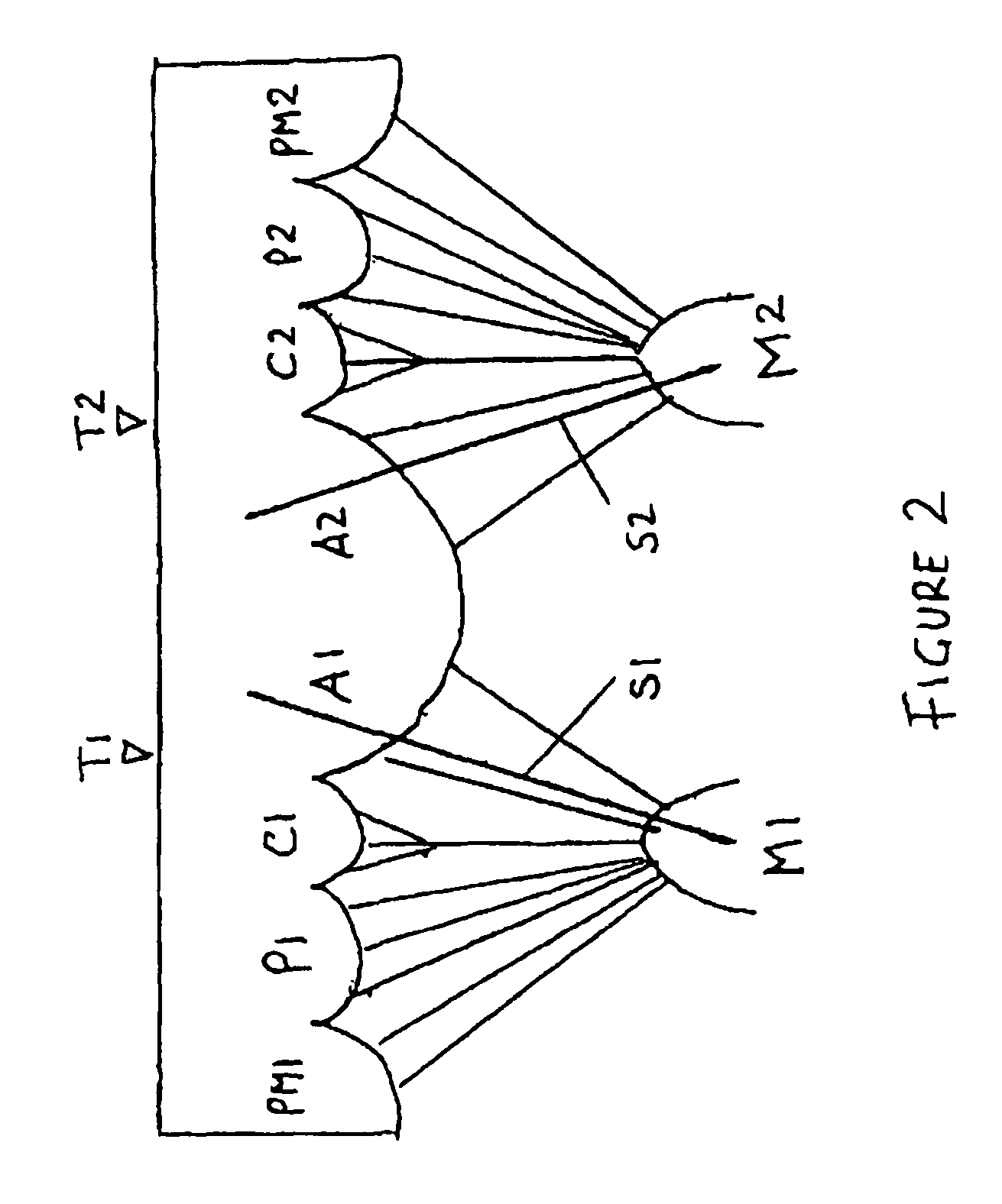
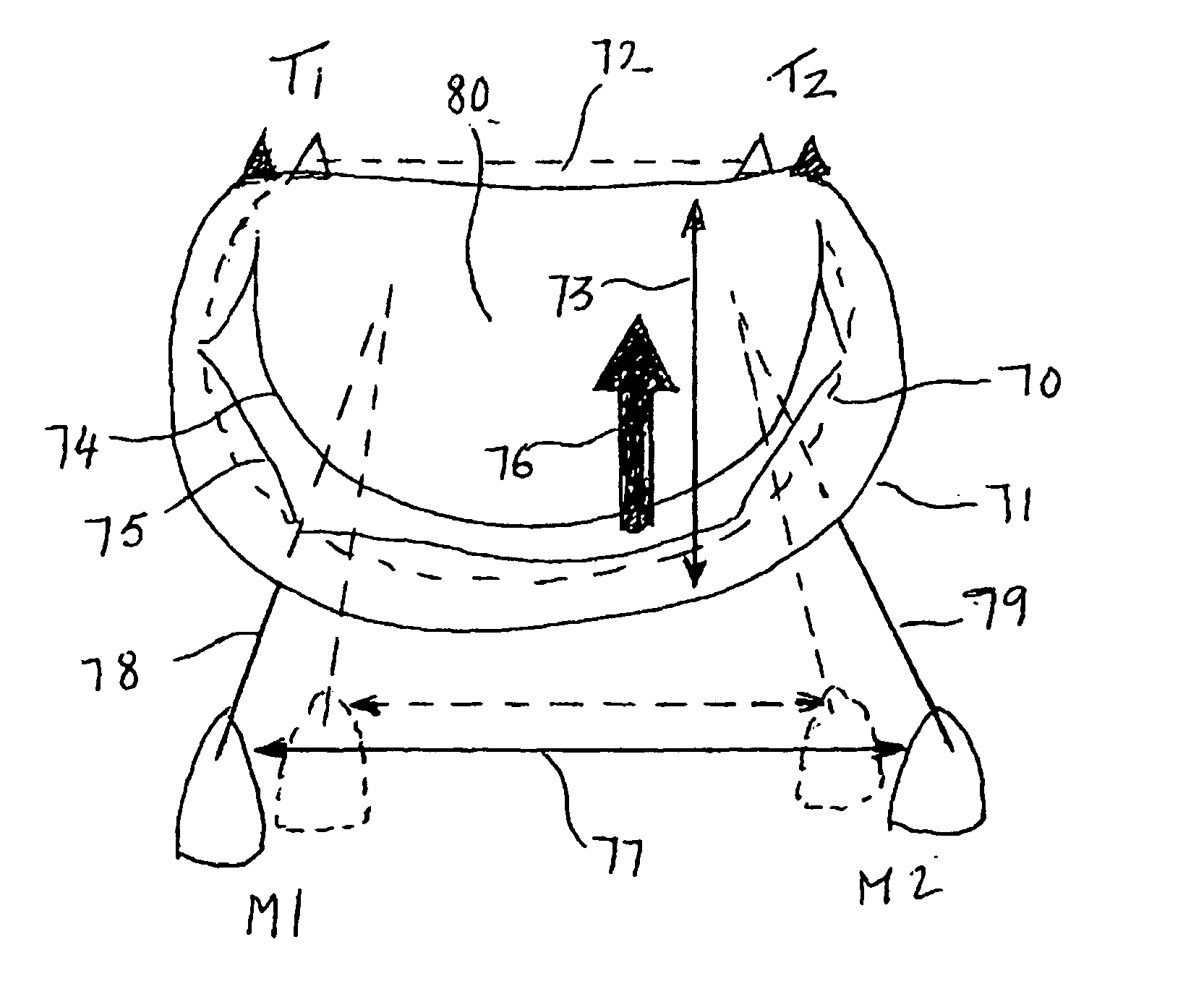
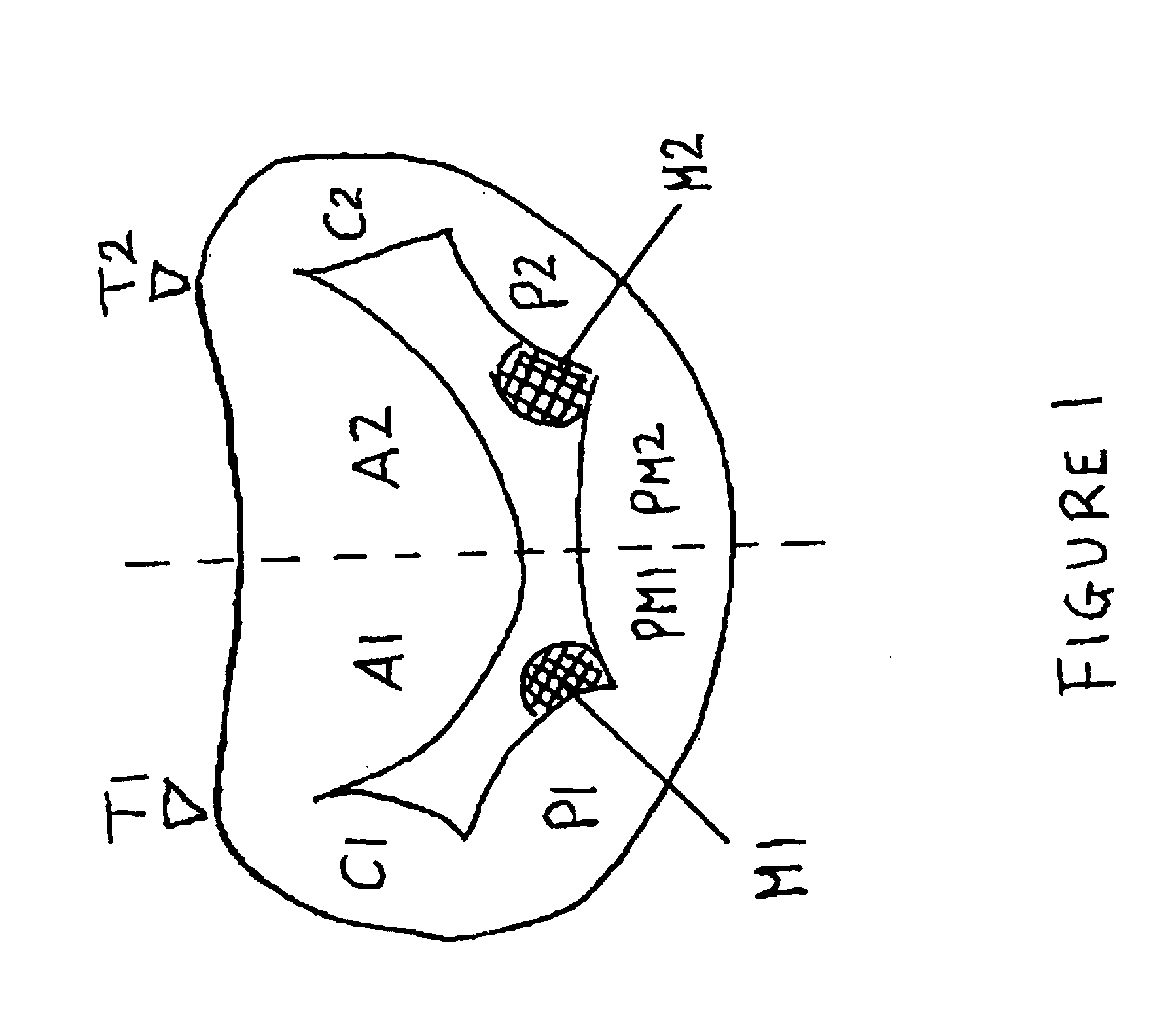
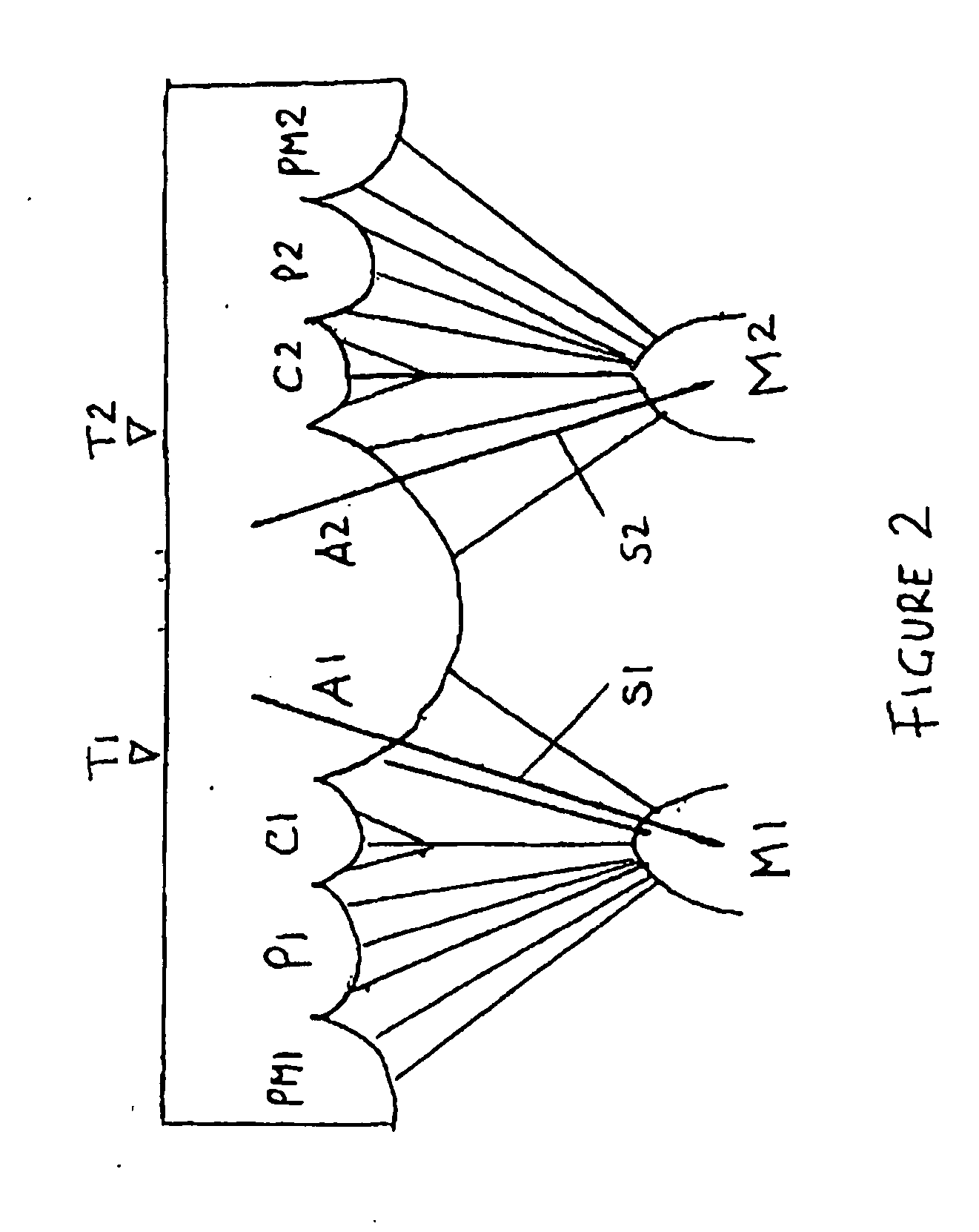
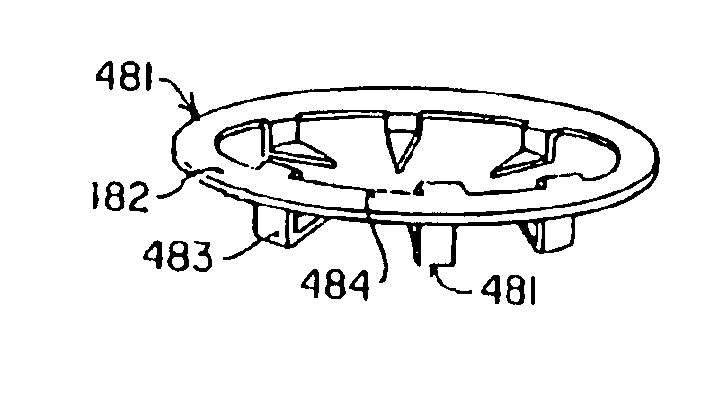
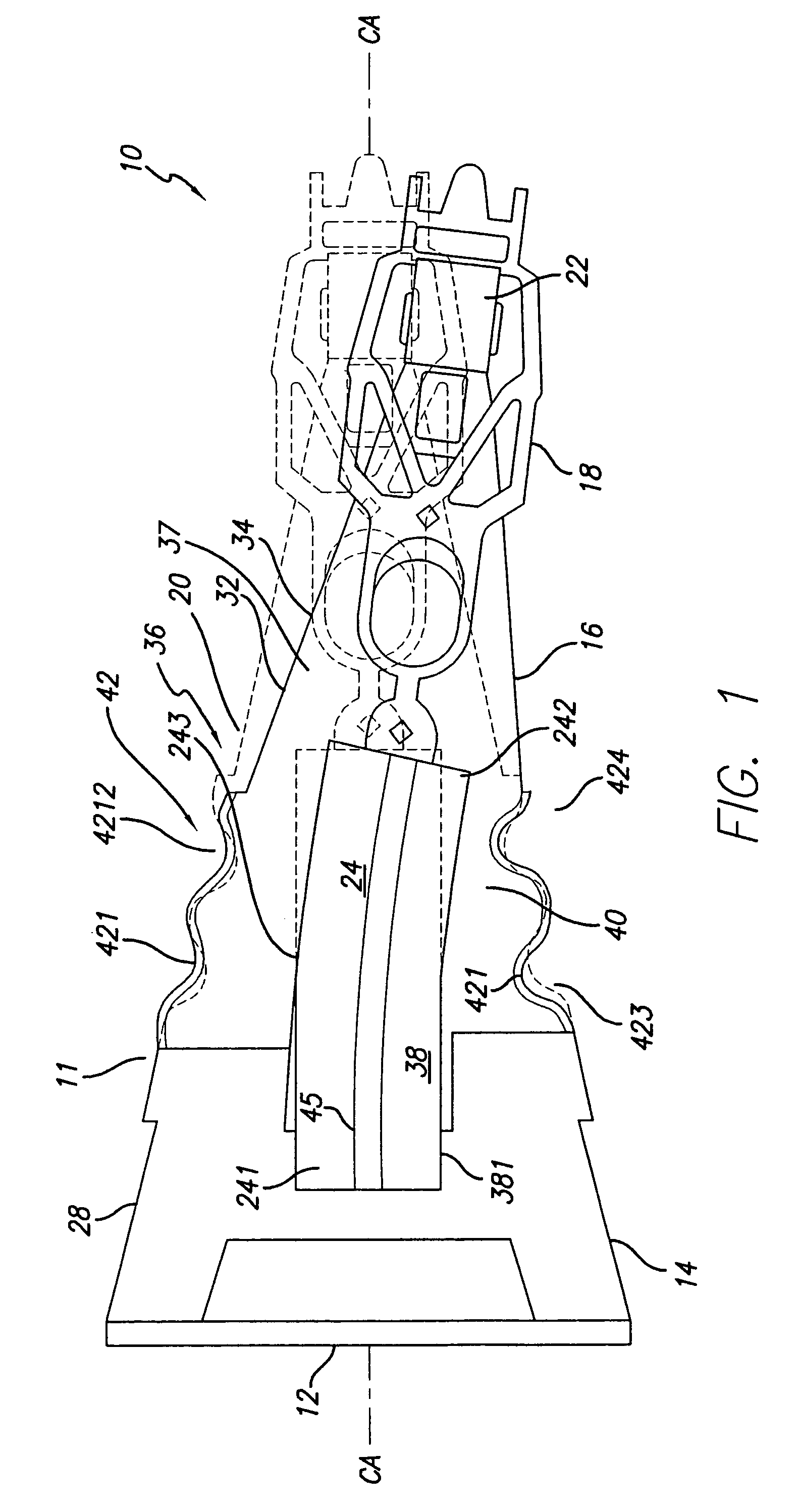
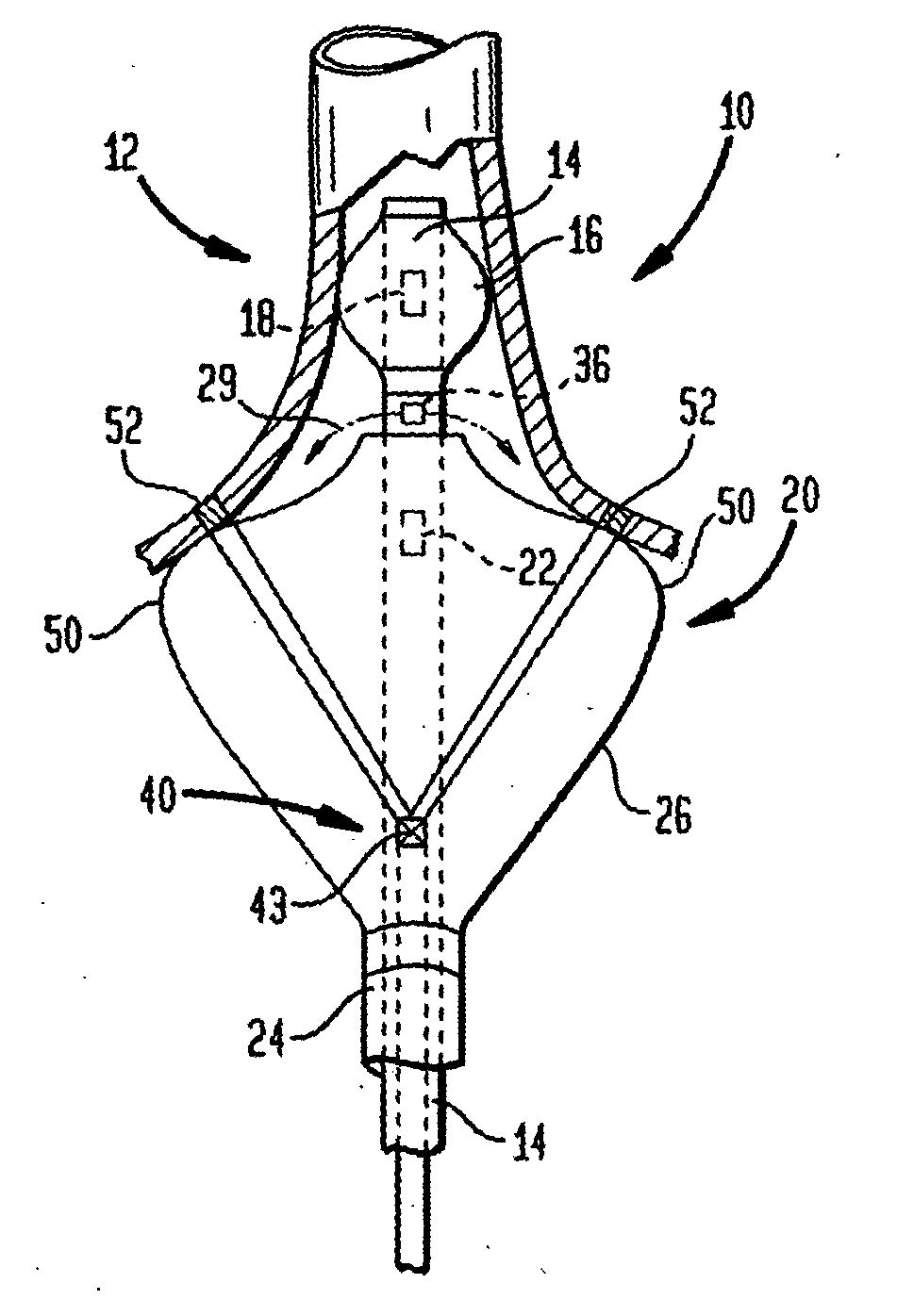
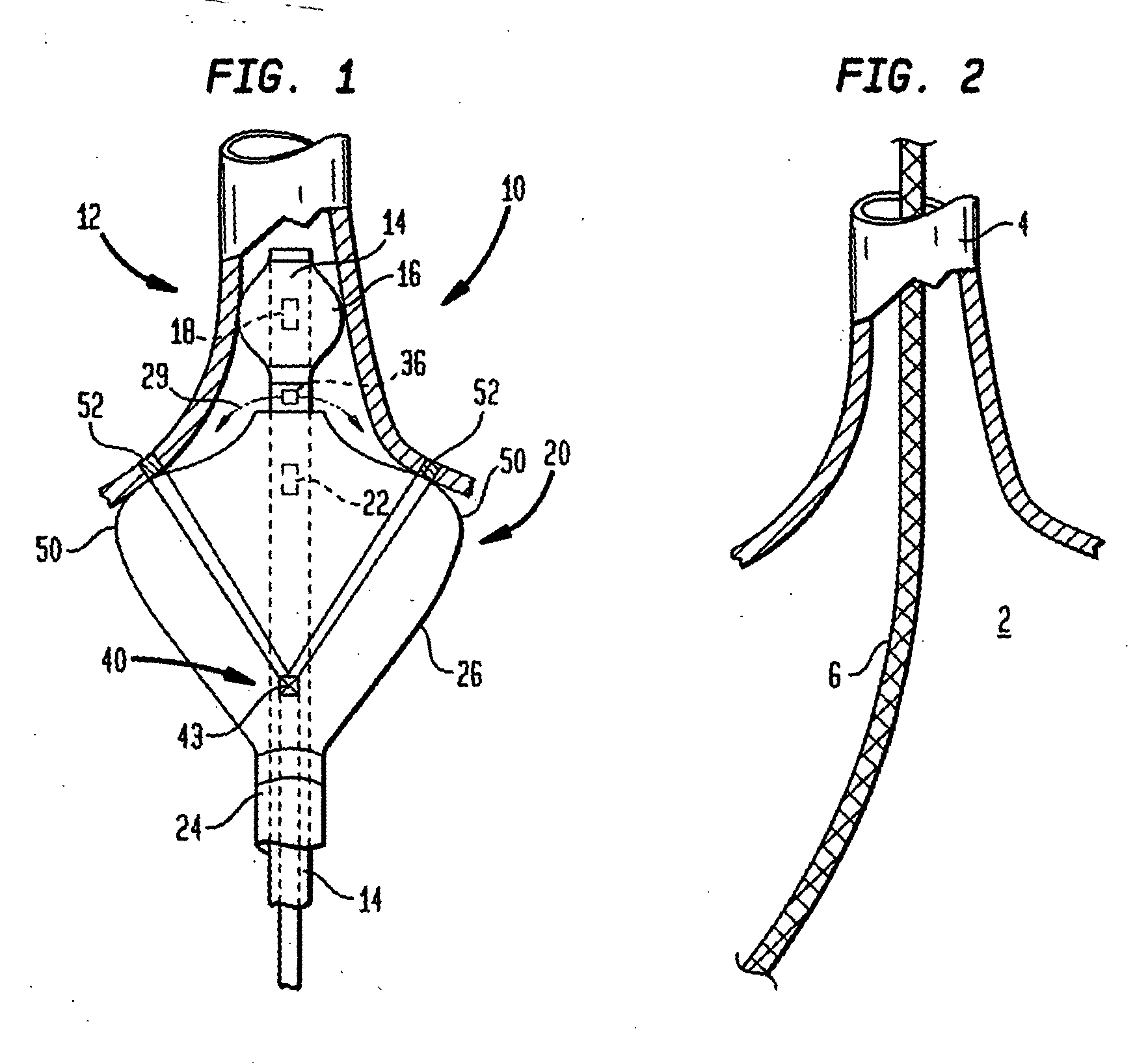
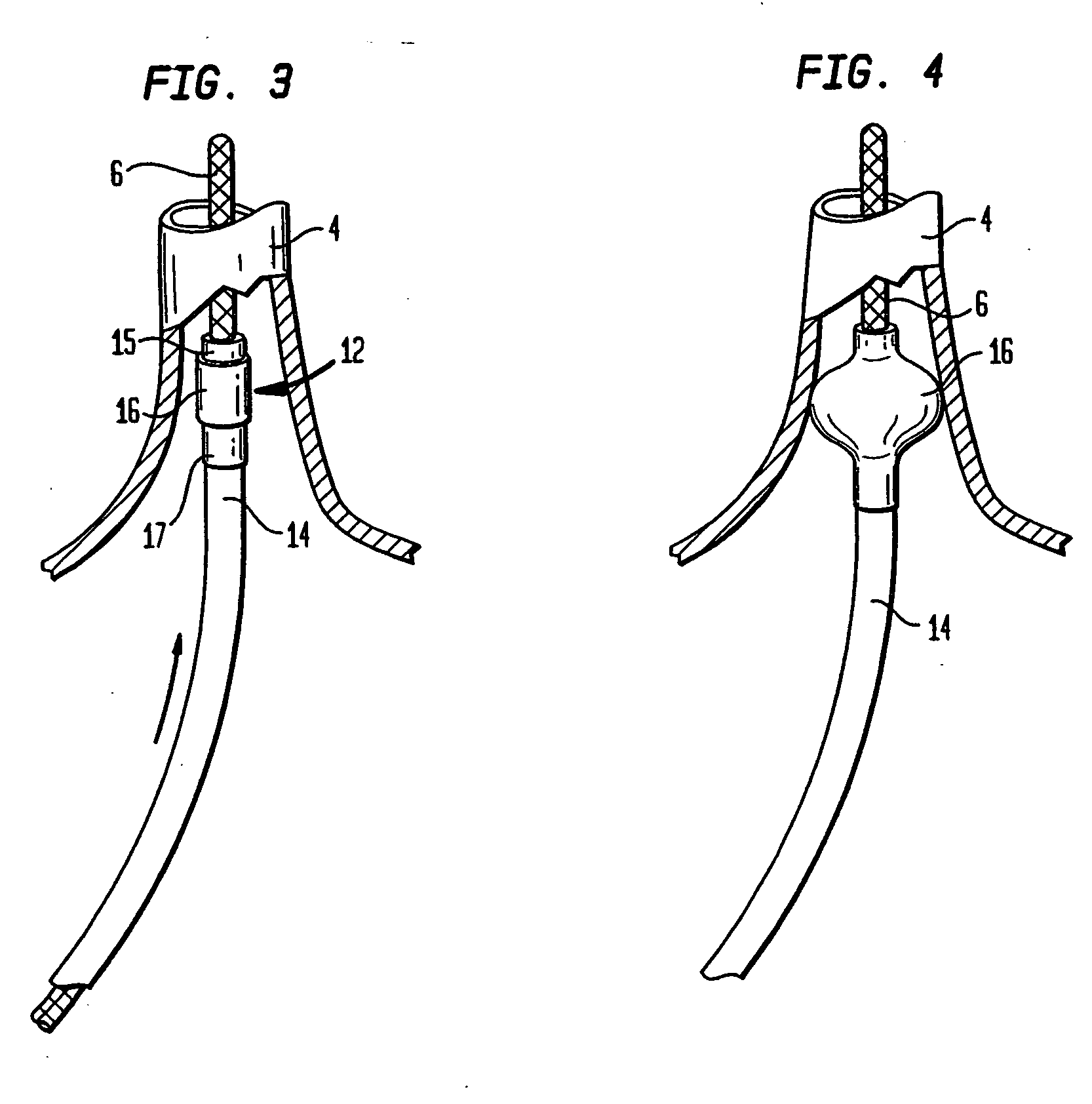
Internal prosthesis for reconstruction of cardiac geometry
InactiveUS8206439B2Efficient use ofAvoid damageAnnuloplasty ringsTubular organ implantsPapillary muscleTricuspid valve.annulus
Unique semi-circular papillary muscle and annulus bands are described that are useful for modifying the alignment of papillary muscles, a mitral valve annulus and / or a tricuspid valve annulus. Methods to effect the alignment are also described and an unique sizing device that can be used for such alignment is described.
Owner:THE INT HEART INST OF MONTANA FOUND
Papilloplasty band and sizing device
Unique semi-circular papillary muscle and annulus bands are described that are useful for modifying the alignment of papillary muscles, a mitral valve annulus and / or a tricuspid valve annulus. Methods to effect the alignment are also described and an unique sizing device that can be used for such alignment is described.
Owner:THE INT HEART INST OF MONTANA FOUND
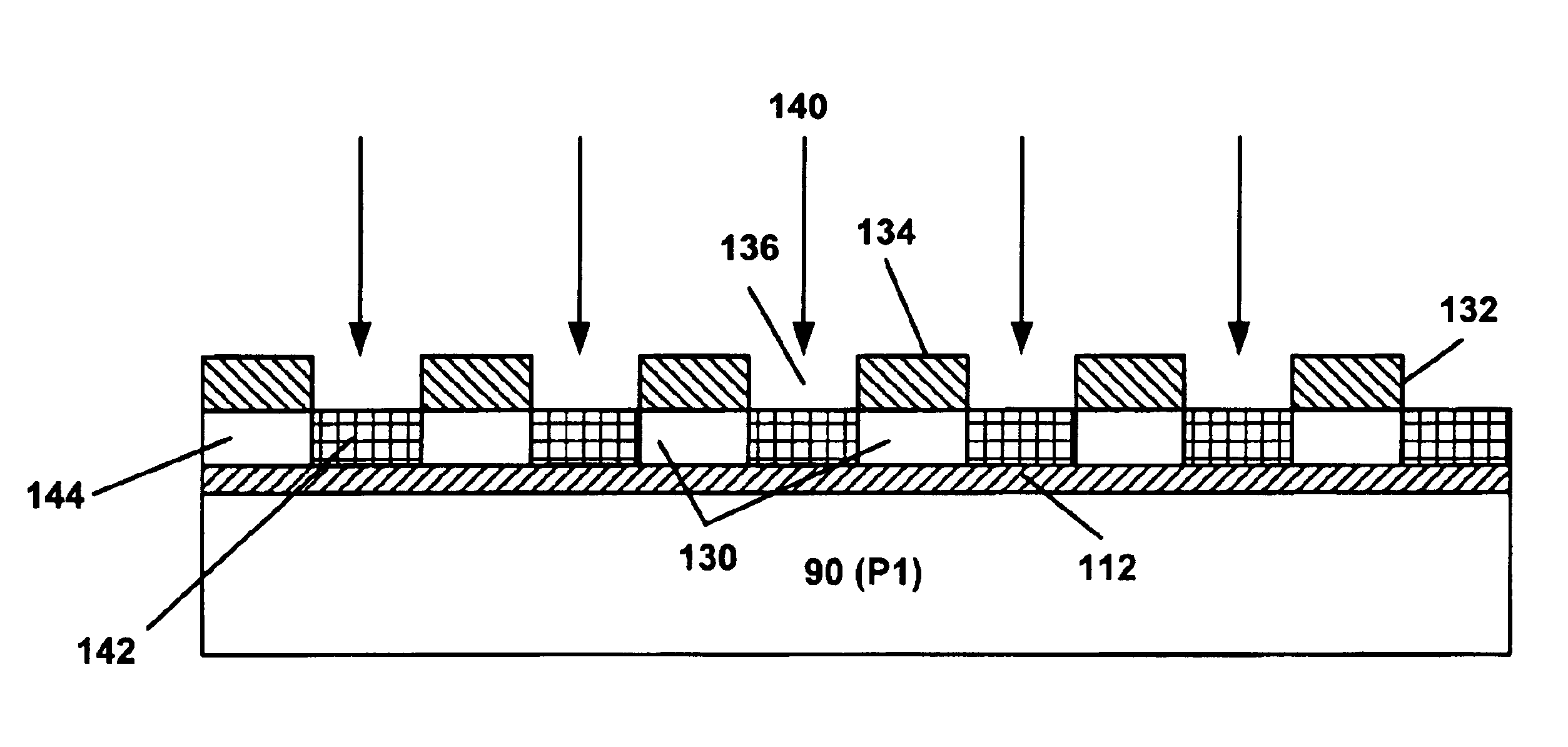
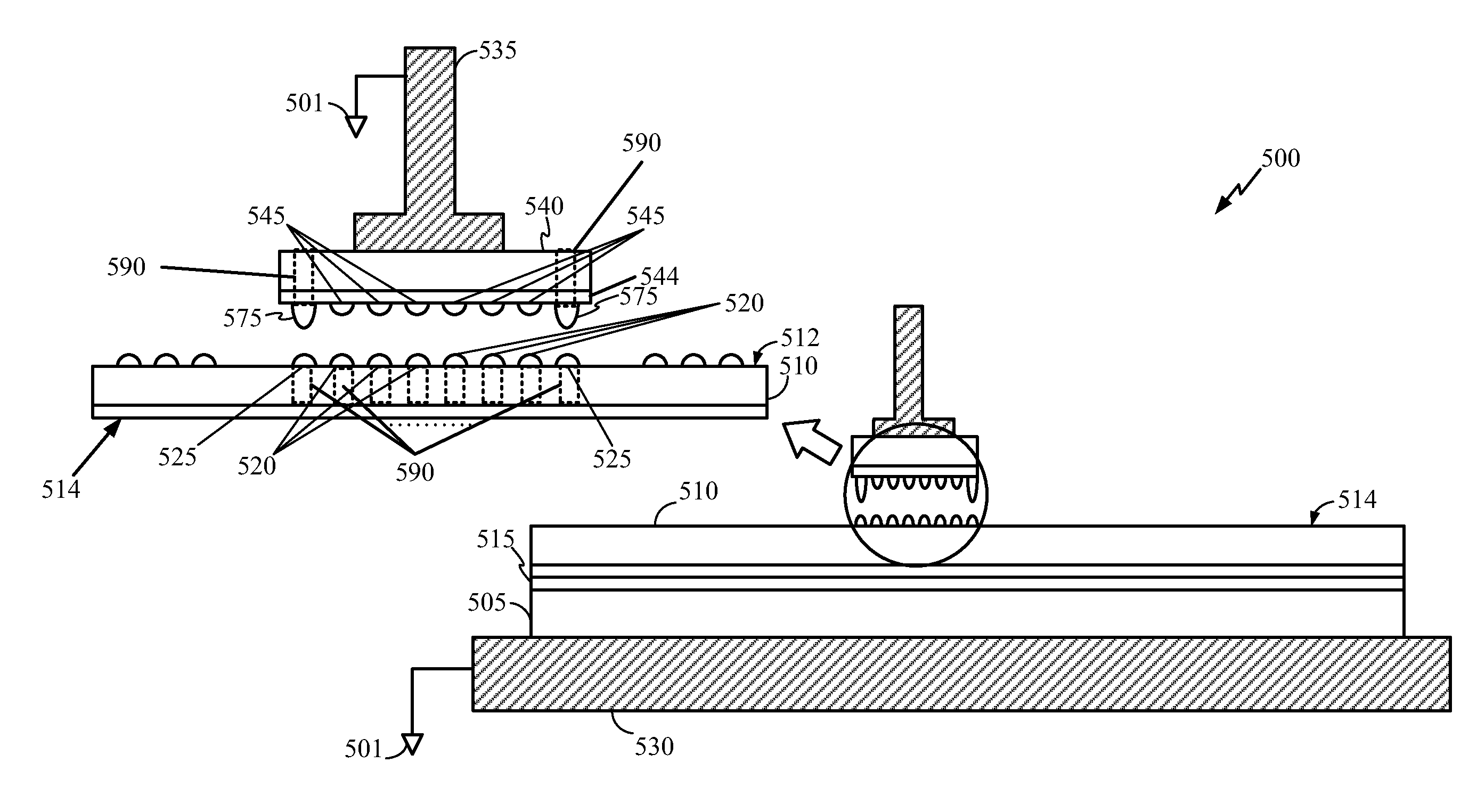
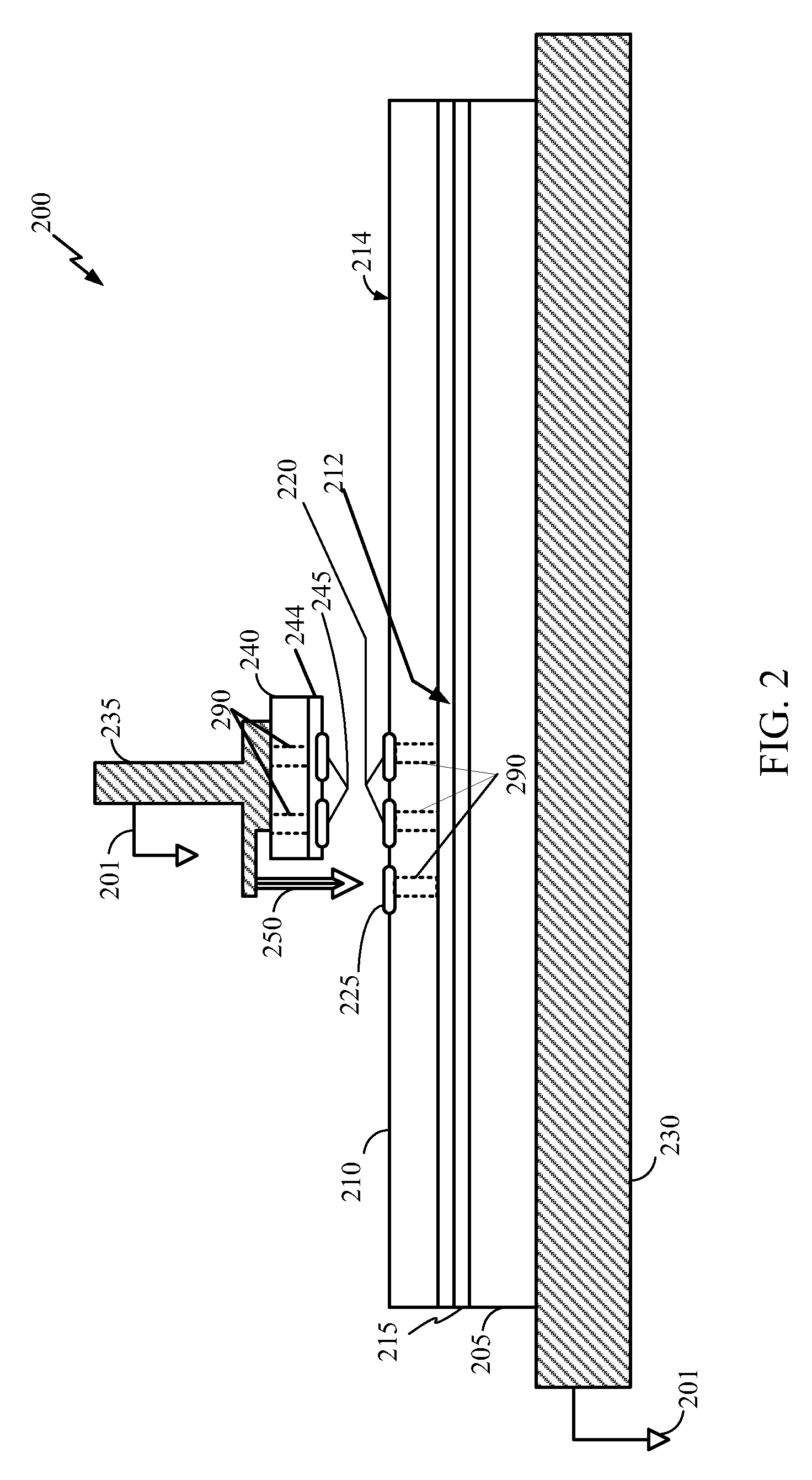
Double winding twin coil for thin-film head writer
InactiveUS6861937B1Small yoke lengthImprove reliabilityConstruction of head windingsManufacture head surfaceElectricityCopper
An enhanced inductive coil design for use in data storage magnetic disk drives with areal density over 35 Gb / in2, features a double wound twin coil that is able to achieve a yoke length of 15 μm or less by reducing the insulation spacing between the two coils. The coil further presents improved reliability by reducing the possibility of occurrence of electrical shorting. The coil is made by forming two interleafing conductors on the same layer with a demesne process. A tri-level process is implemented in the layout of the first conductor to ensure that the coil width and spacing are uniform and even, in order for the second conductor to be wound therebetween. A conformal dielectric layer of approximately 0.1 to 0.2 μm in thickness is deposited between the two conductors and serves as insulation. The two conductors are formed by a copper seed layer plating process that eliminates potential damage to the conductors during production.
Owner:WESTERN DIGITAL TECH INC
Reduced Susceptibility To Electrostatic Discharge During 3D Semiconductor Device Bonding and Assembly
InactiveUS20100258949A1Reduce electrostatic dischargePotential damagePrinted circuit assemblingSemiconductor/solid-state device detailsElectrostatic dischargeGround plane
A method to reduce electrostatic discharge susceptibility when assembling a stacked IC device. The method includes coupling a ground plane of a first semiconductor device and a ground plane of a second semiconductor device to substantially a same electrical potential. Active circuitry on the first semiconductor device and active circuitry on the second semiconductor device are electrically coupled after the ground planes are coupled. Electrically coupling the ground planes of the first and the second semiconductor device creates a preferred electrostatic discharge path to ground, thus minimizing potential damage to sensitive circuit elements.
Owner:QUALCOMM INC
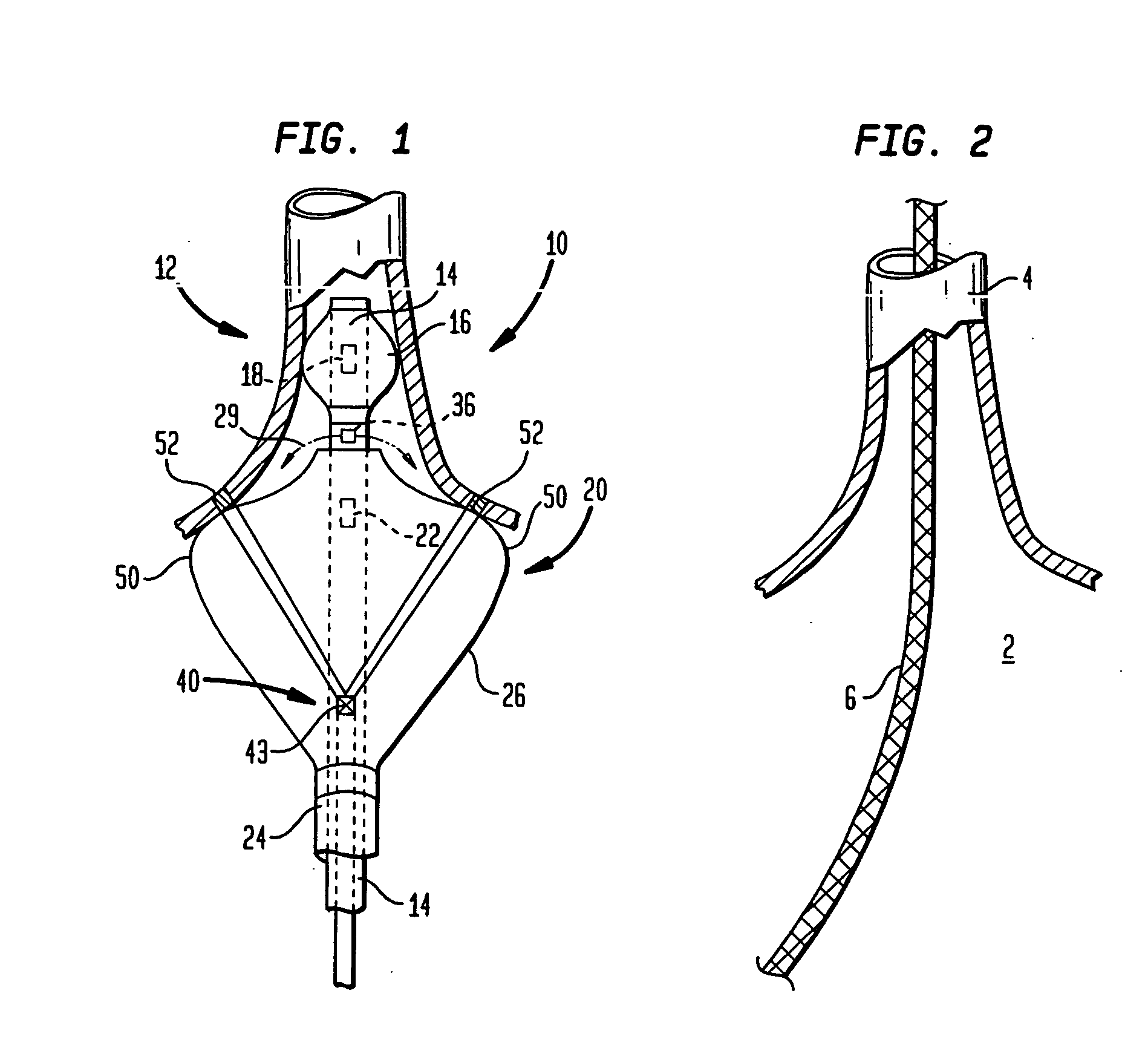
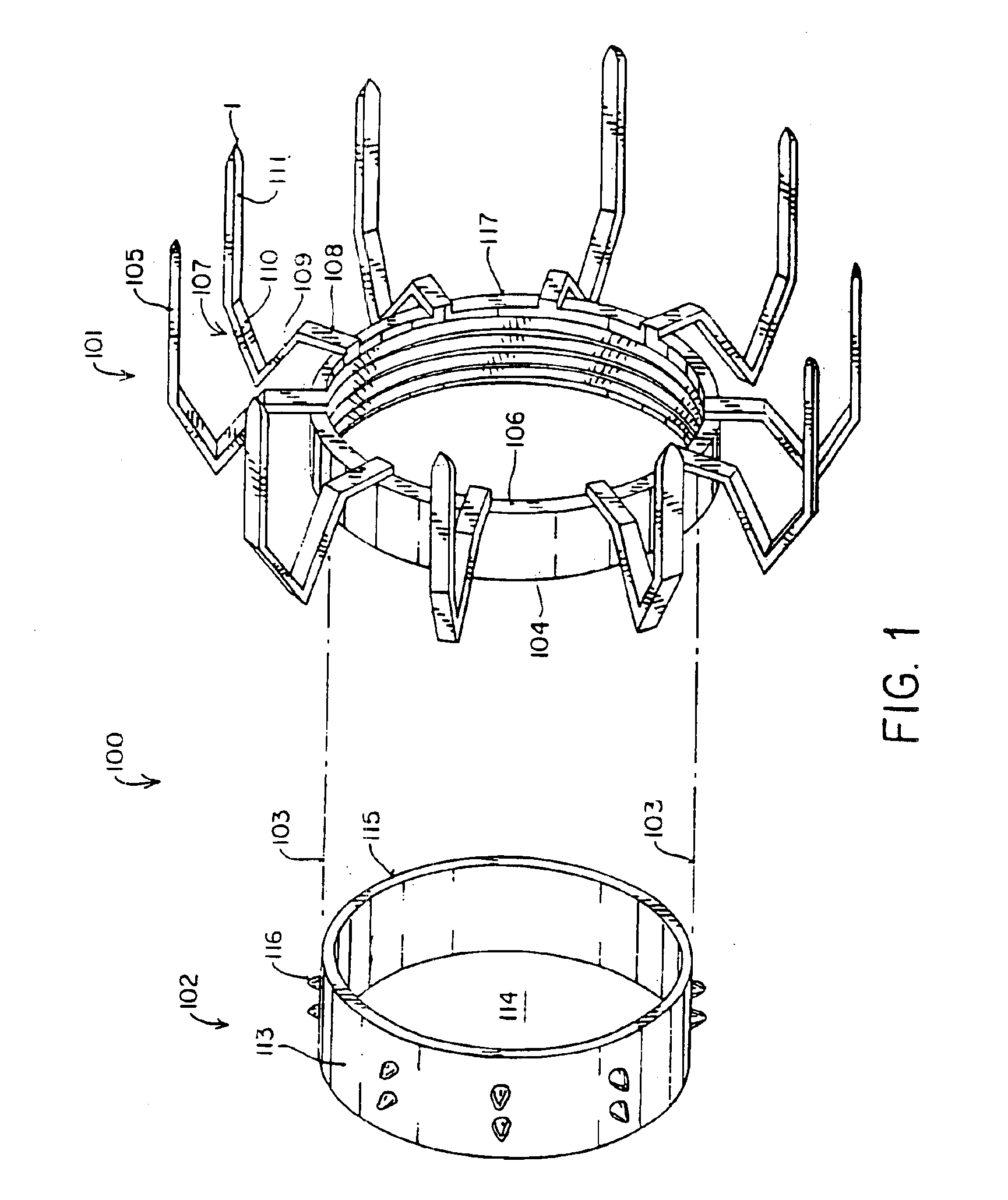
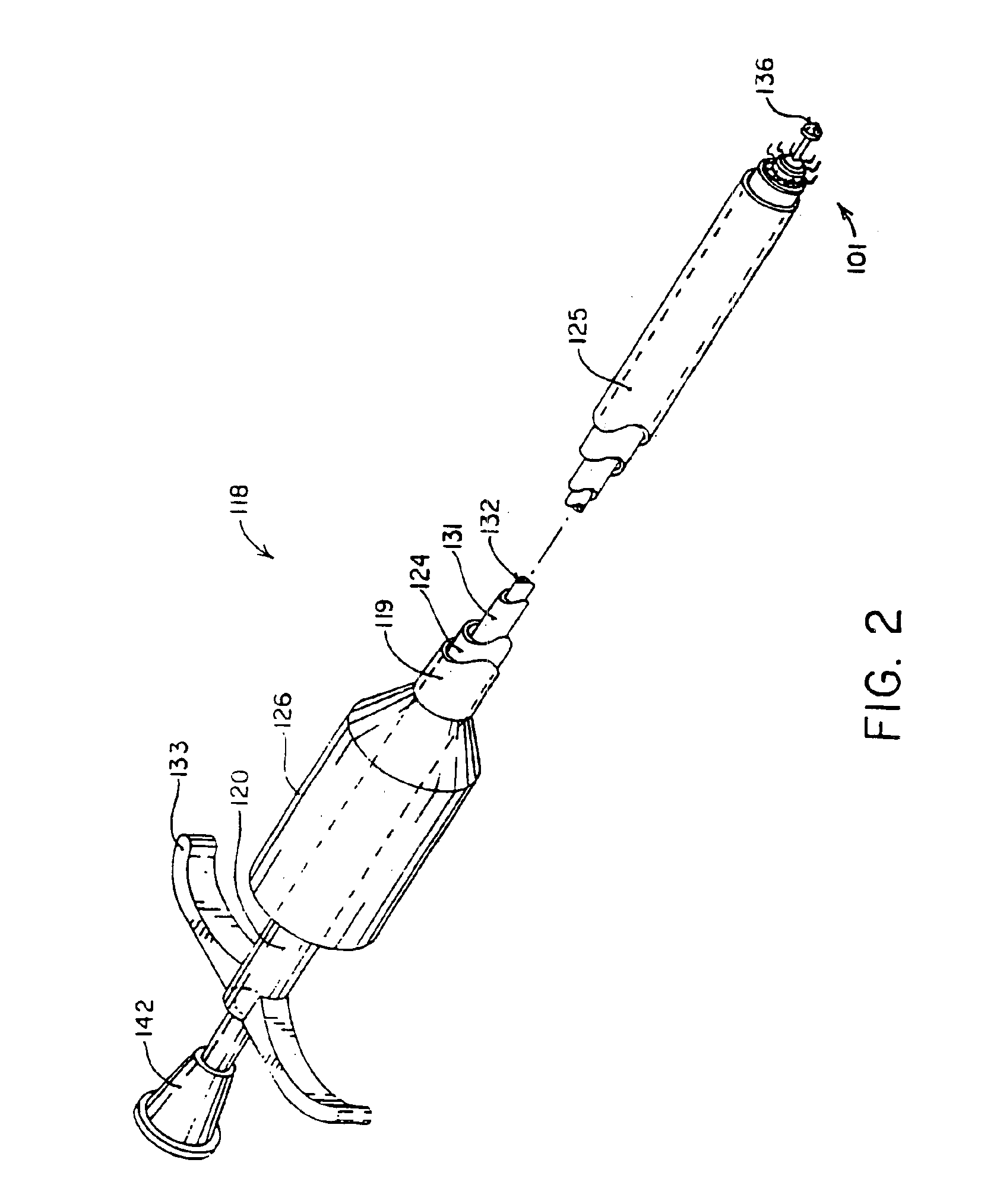
Devices and methods for performing avascular anastomosis
InactiveUS6899718B2Efficient and reliable performanceEfficient executionStaplesNailsVascular anastomosisBlood vessel
Owner:HEARTPORT
Methods and apparatus relating to singulating semiconductor wafers and wafer scale assemblies
ActiveUS20050202651A1Increase distanceAvoid excessive widthSolid-state devicesSemiconductor/solid-state device manufacturingEngineeringSemiconductor
Methods relating to the singulation of dice from semiconductor wafers. Trenches or channels are formed in the bottom surface of a semiconductor wafer, corresponding in location to the wafer streets. The trenches may be formed by etching or through an initial laser cut. The wafer is then singulated along the streets with a laser preferably having a beam narrower than the trenches. Multiple, laterally spaced lasers may be used in combination during a single pass to perform simultaneous singulating cuts. Additional edge protection for integrated circuitry on the active surface of the semiconductor dice may be provided by forming trenches or channels along the streets in the active surface instead of the bottom surface, disposing protective material along the streets and within the trenches prior to singulation and cutting through the wafer, leaving protective material on the sidewalls of the channels.
Owner:MICRON TECH INC
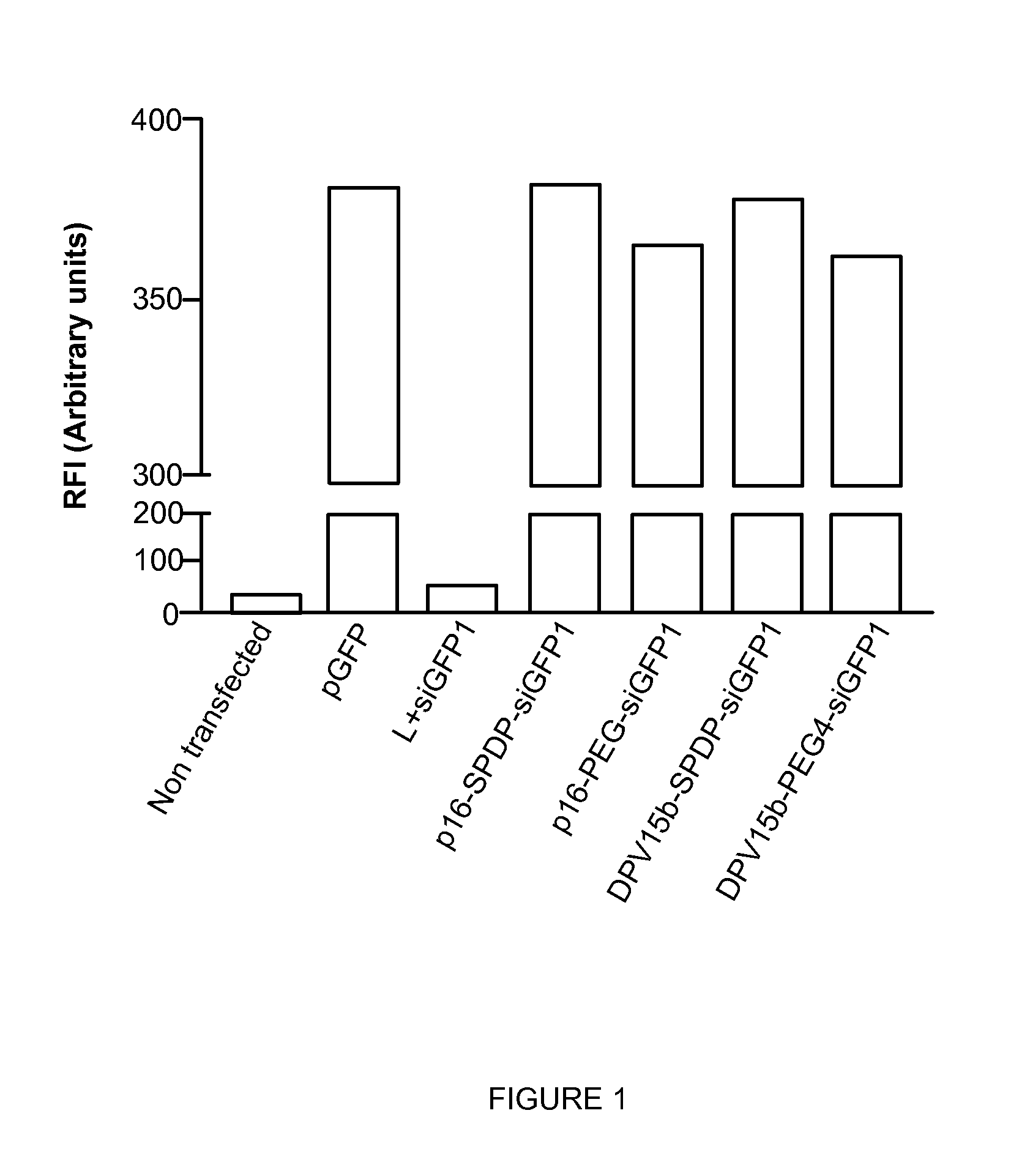
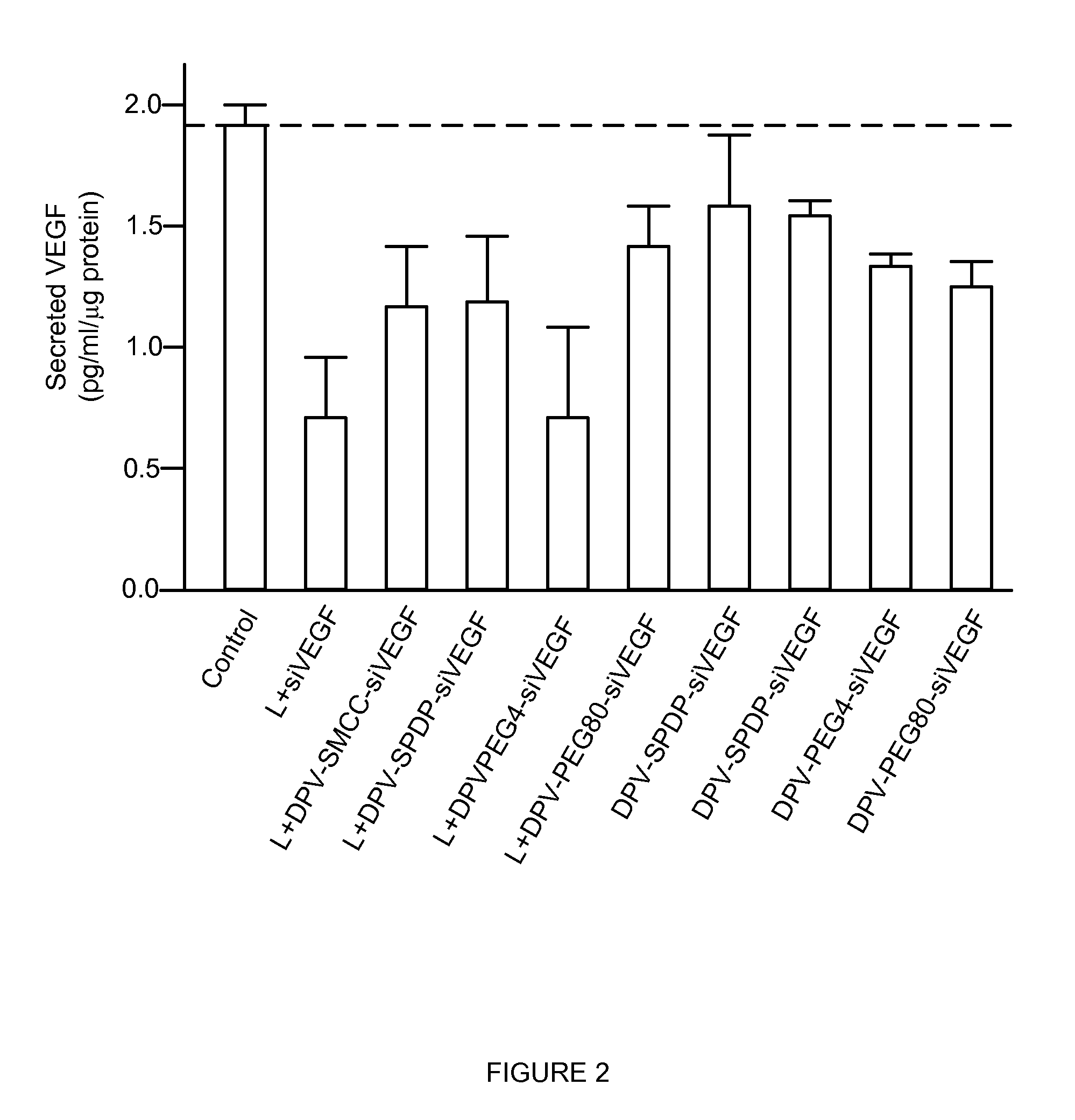
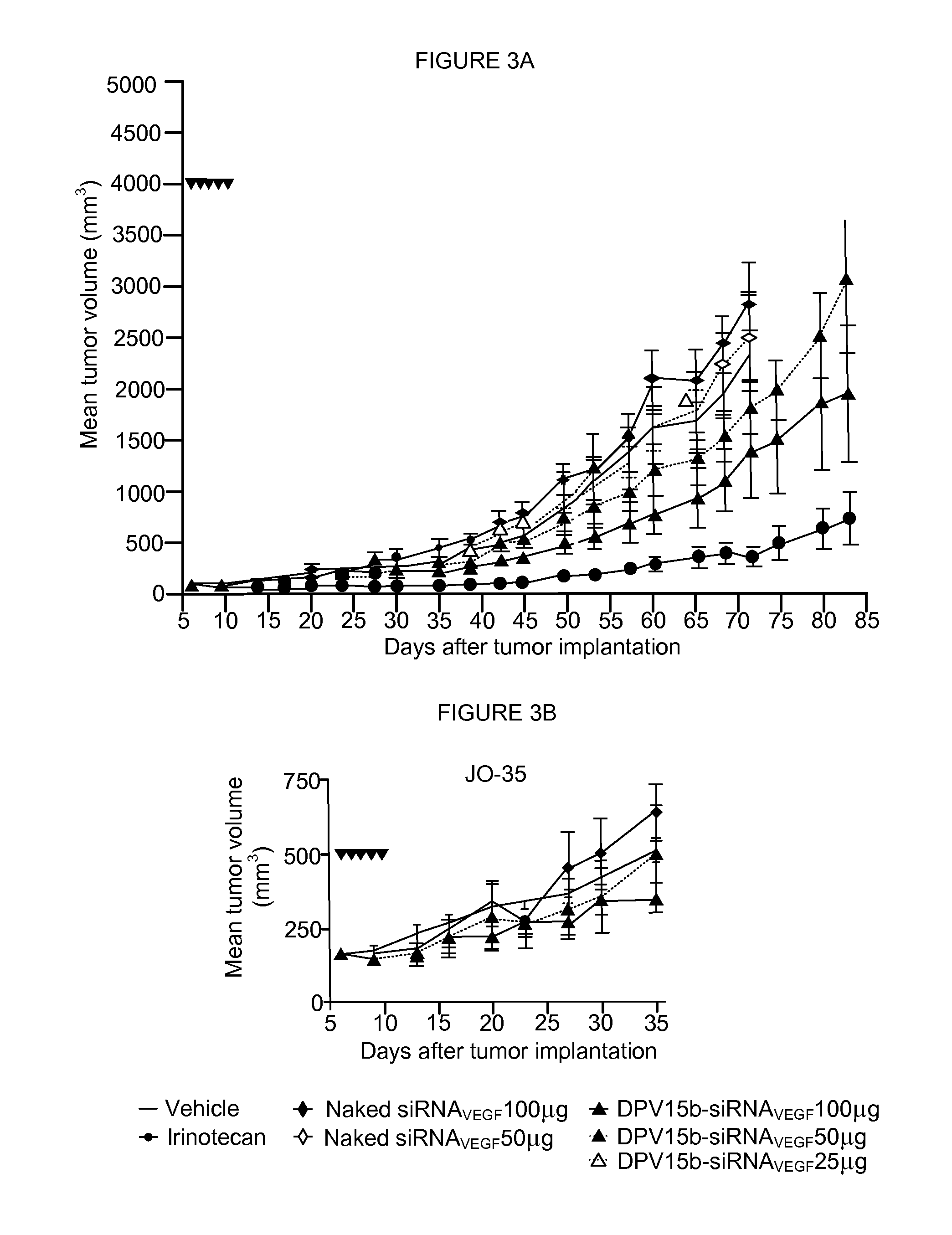
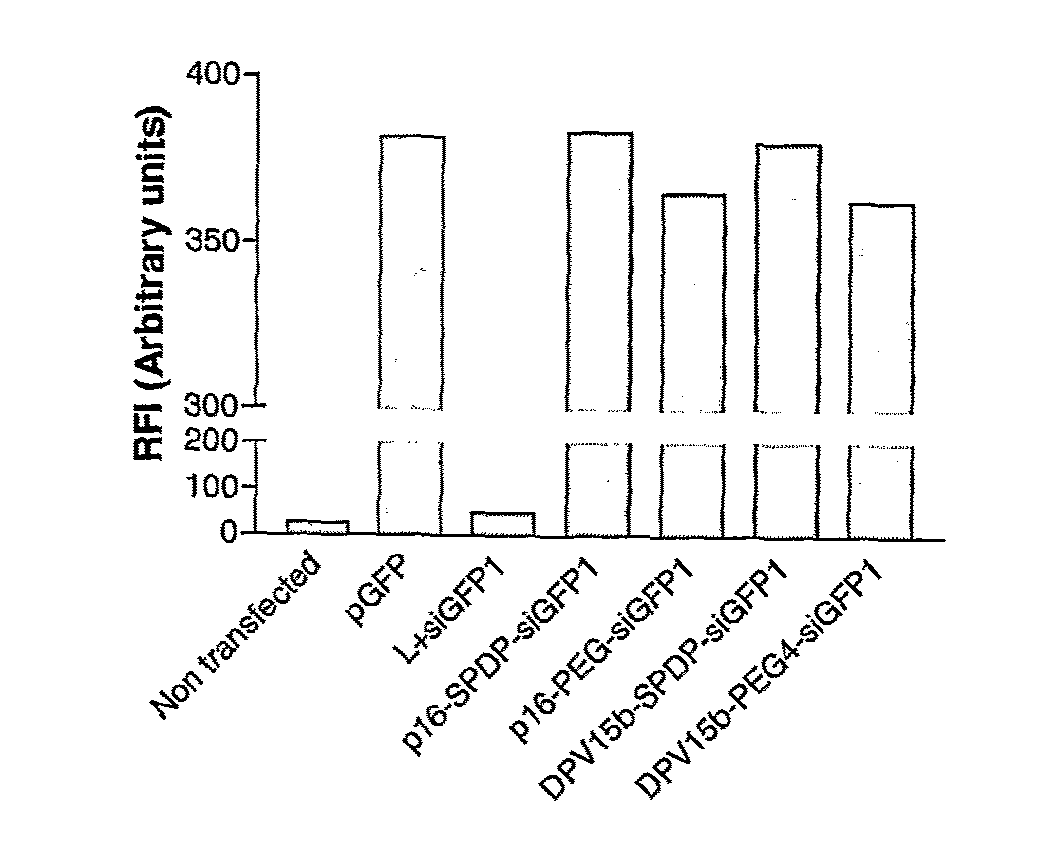
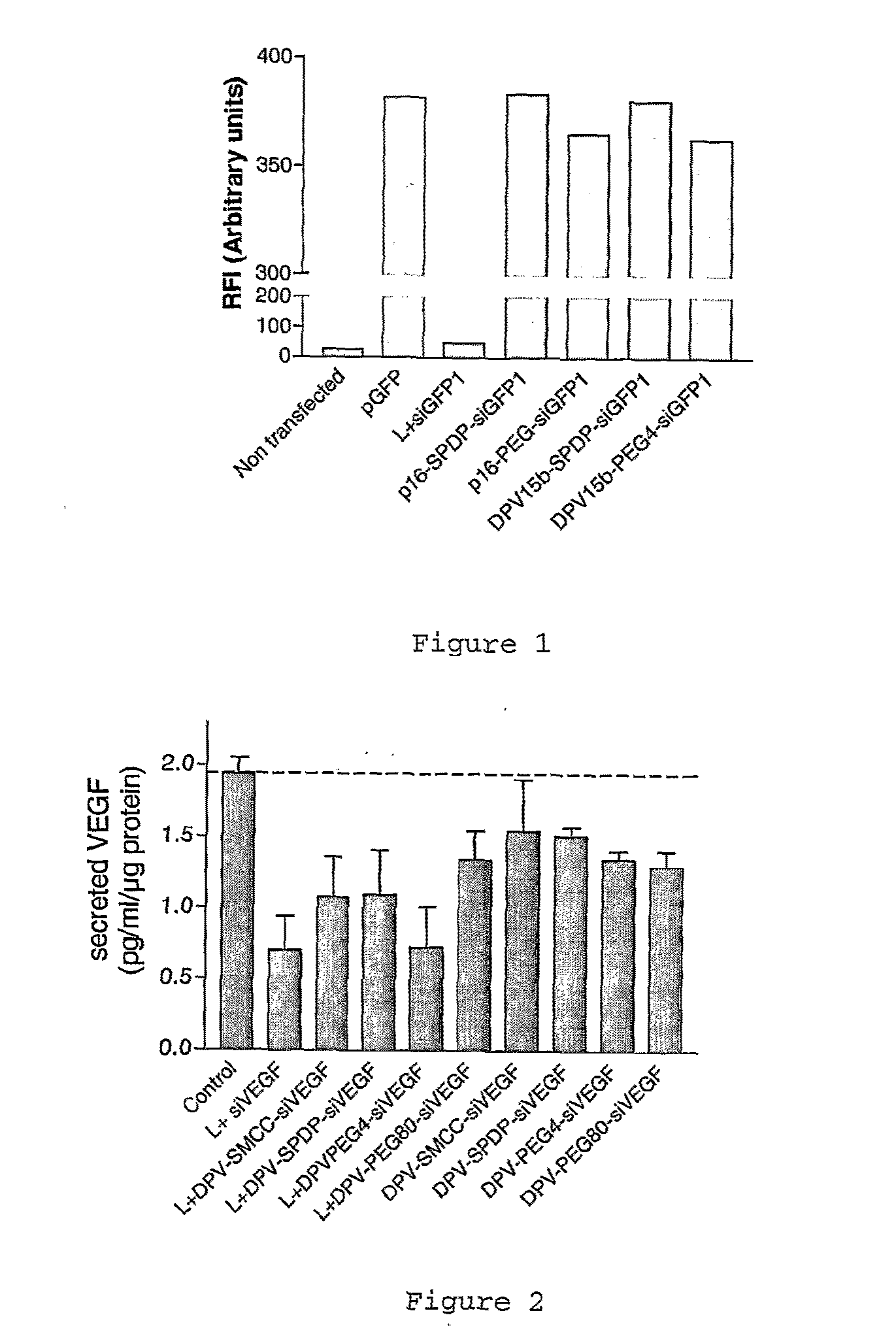
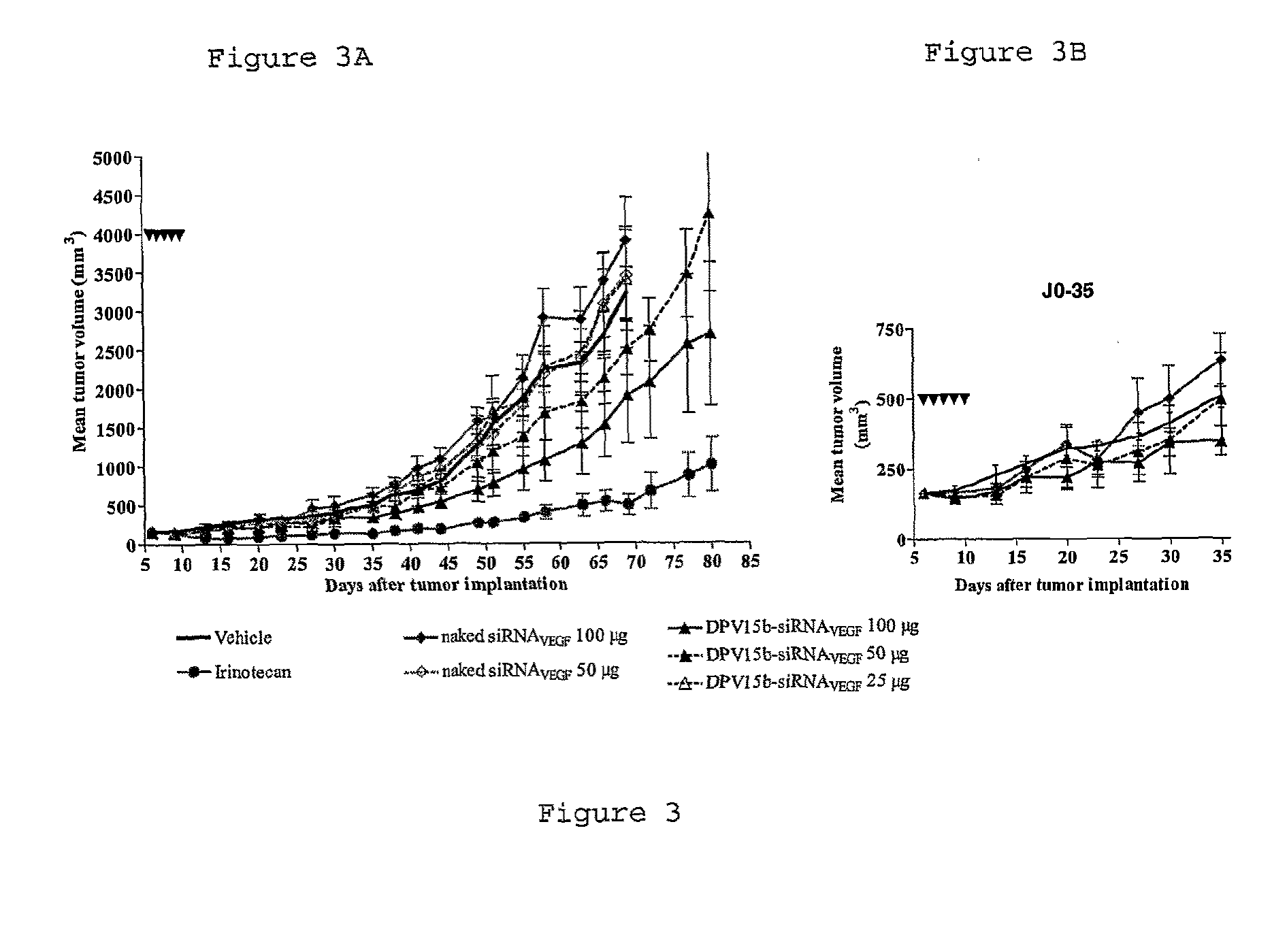
Cell penetrating peptide conjugates for delivering of nucleic acids into a cell
InactiveUS20130137644A1Good curative effectLarge indexNervous disorderAntipyreticHydrophilic polymersPolyethylene glycol
The invention provides cell penetrating peptide-nucleic acid conjugates having the formula P-L-N, wherein P is a cell penetrating peptide, N is a nucleic acid, preferably an oligonucleotide and more preferably a siRNA, and L is a hydrophilic polymer, preferably a polyethylene glycol (PEG)-based linker linking P and N together. Compositions, methods of use and methods for producing such conjugates are also disclosed.
Owner:CELLECTIS SA
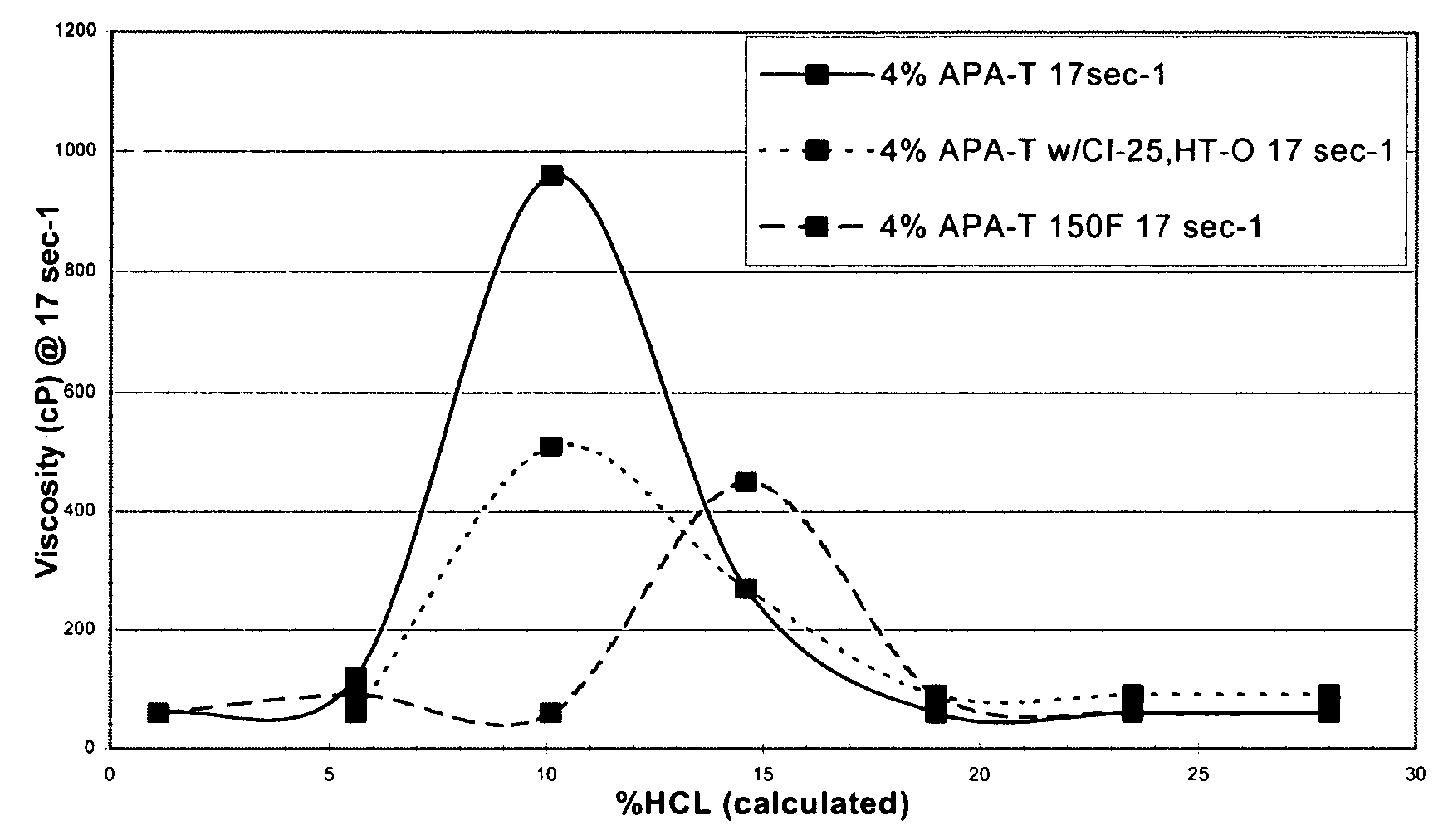
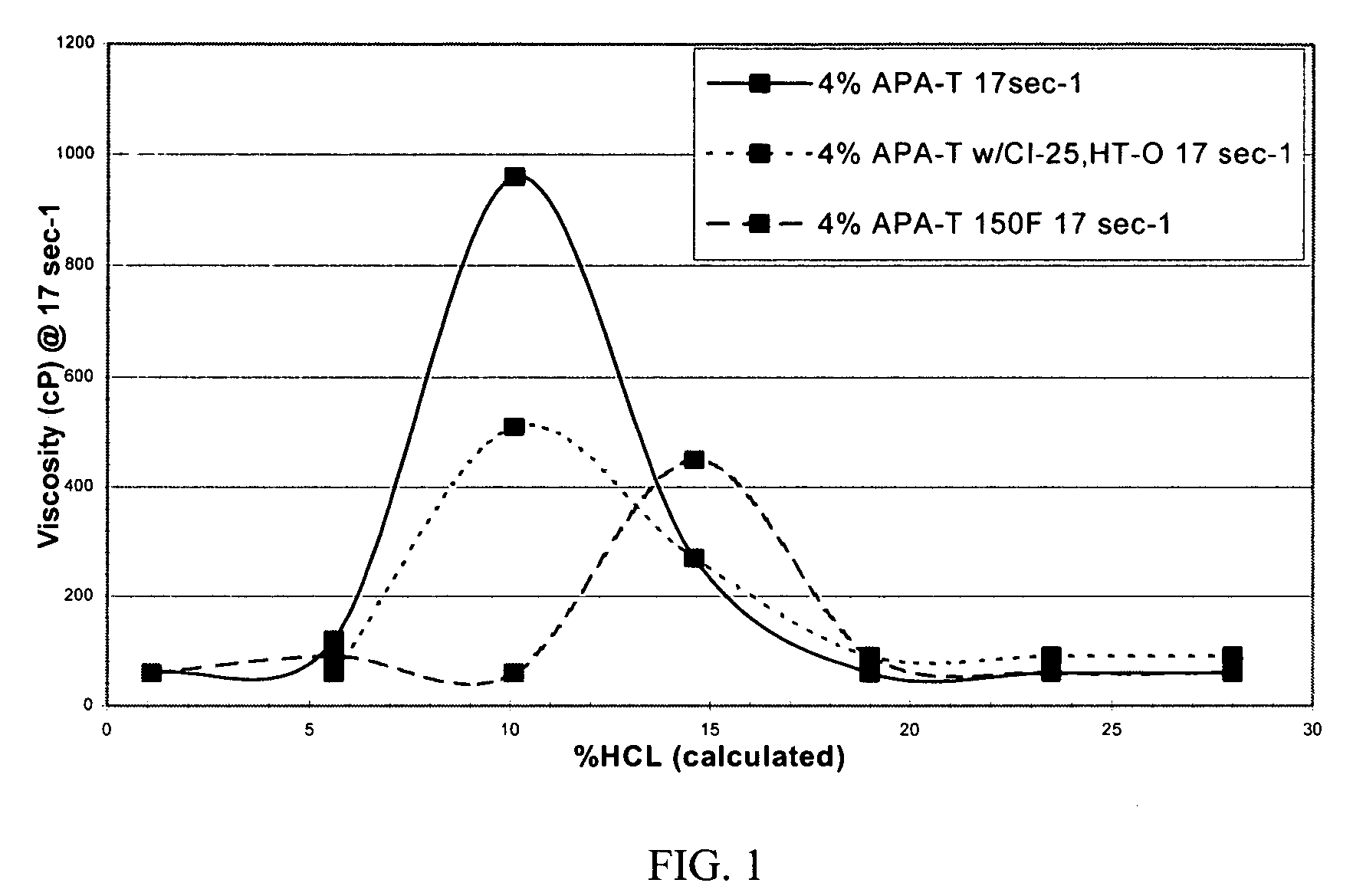
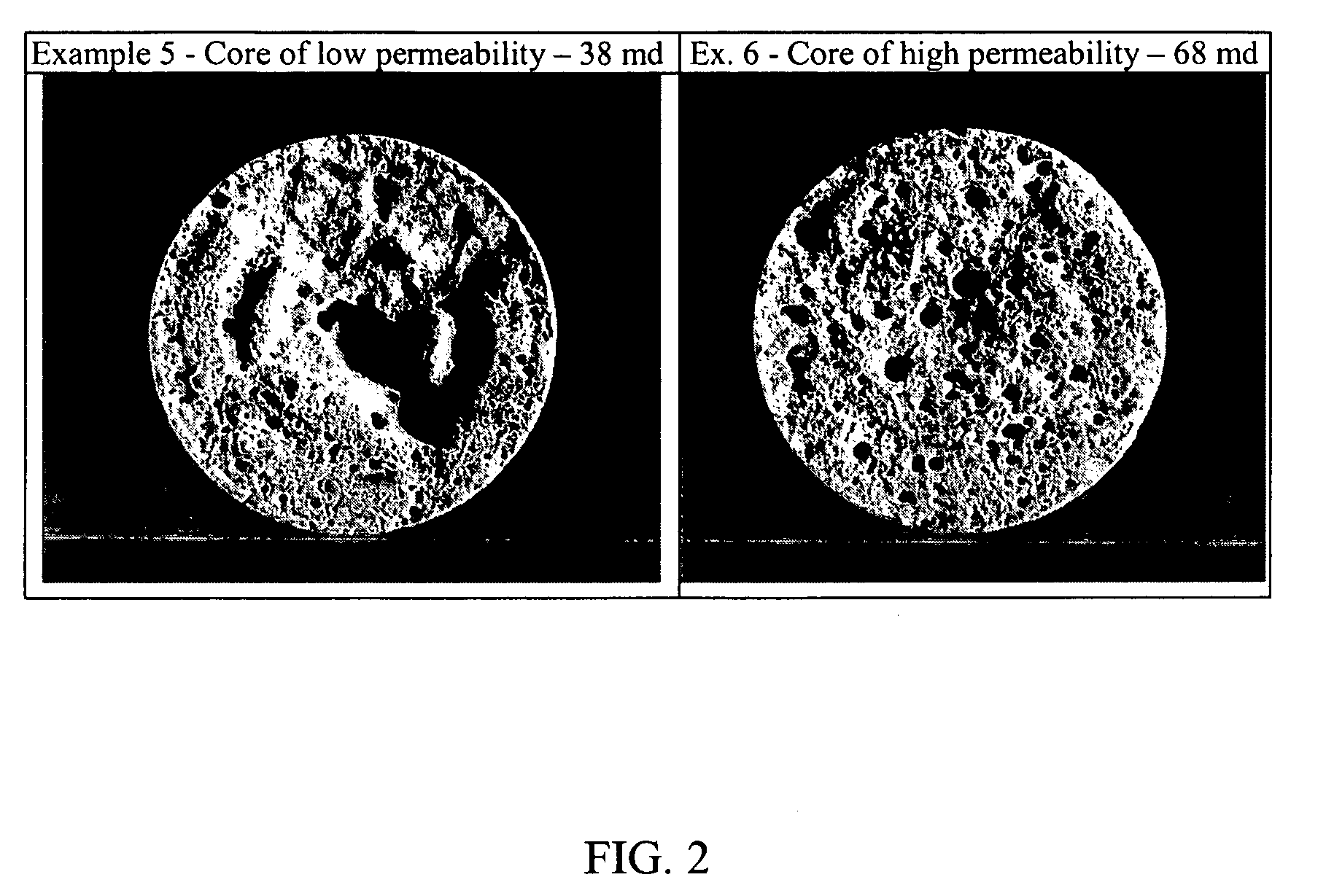
Method of acidizing a subterranean formation with diverting foam or fluid
ActiveUS7303018B2Potential damageHigh viscosityFluid removalDrilling compositionSaline waterFluid viscosity
A method of acidizing a subterranean formation with a diverting agent composed of a gelled or thickened viscoelastic foam or fluid generated from (i.) an amidoamine oxide gelling agent and (ii.) an acid or foam, water and / or brine. The gelled or thickened foam or fluid may be generated in-situ or introduced directly into the formation by mixing of the amidoamine oxide gelling agent and acid or foam, water and / or brine. As the acid spends, the acidizing fluid thickens. When the acid is further spent, the fluid viscosity declines eventually returning to a low viscosity state, allowing for easy cleanup. The process allows for selective acidizing of less permeable zones of the formation and more uniform stimulation of the hydrocarbon bearing formation.
Owner:BAKER HUGHES HLDG LLC
Cell Penetrating Peptide Conjugates for Delivering of Nucleic Acids into a Cell
InactiveUS20090186802A1Improve propertiesGood curative effectNervous disorderAntipyreticPolyethylene glycolOligonucleotide
The invention provides cell penetrating peptide-nucleic acid conjugates having the formula P-L-N, wherein P is a cell penetrating peptide, N is a nucleic acid, preferably an oligonucleotide and more preferably a siRNA, and L is a hydrophilic polymer, preferably a polyethylene glycol (PEG)-based linker linking P and N together. Compositions, methods of use and methods for producing such conjugates are also disclosed.
Owner:CELLECTIS SA
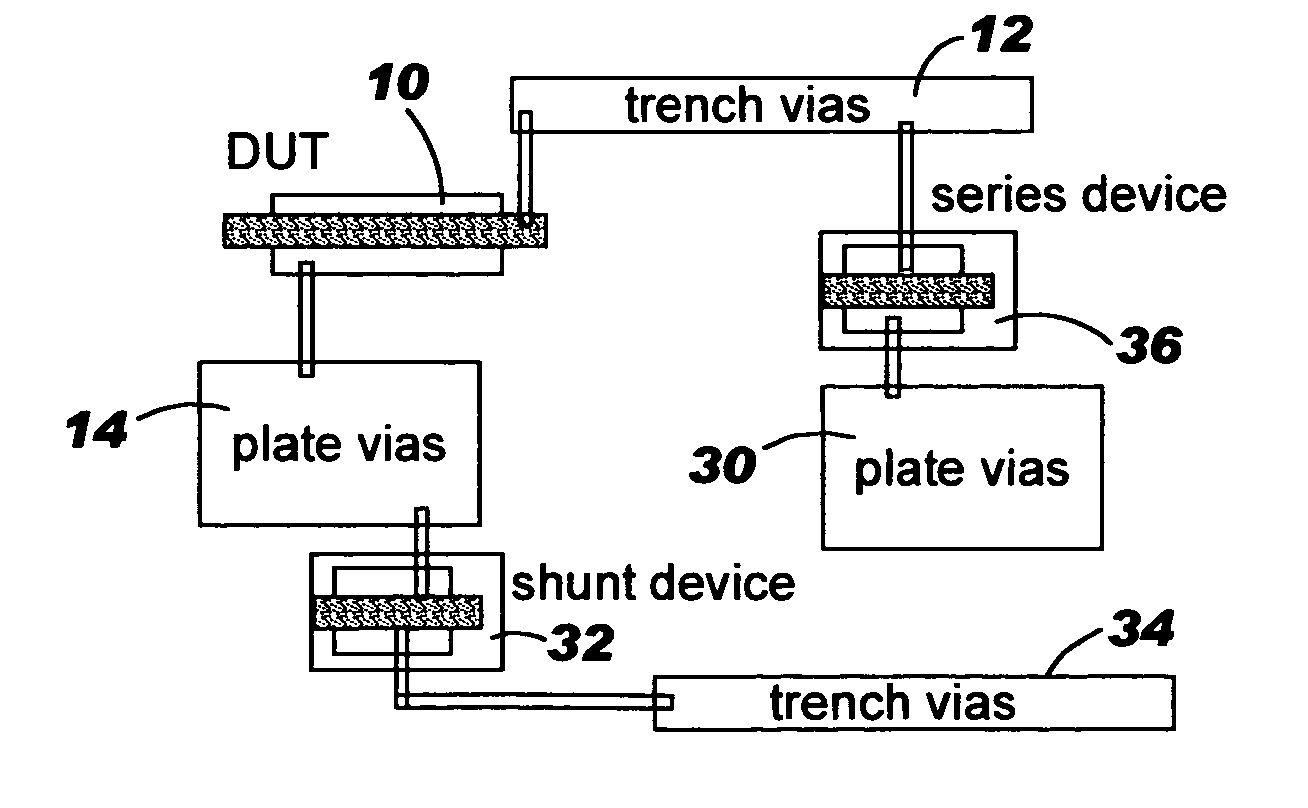
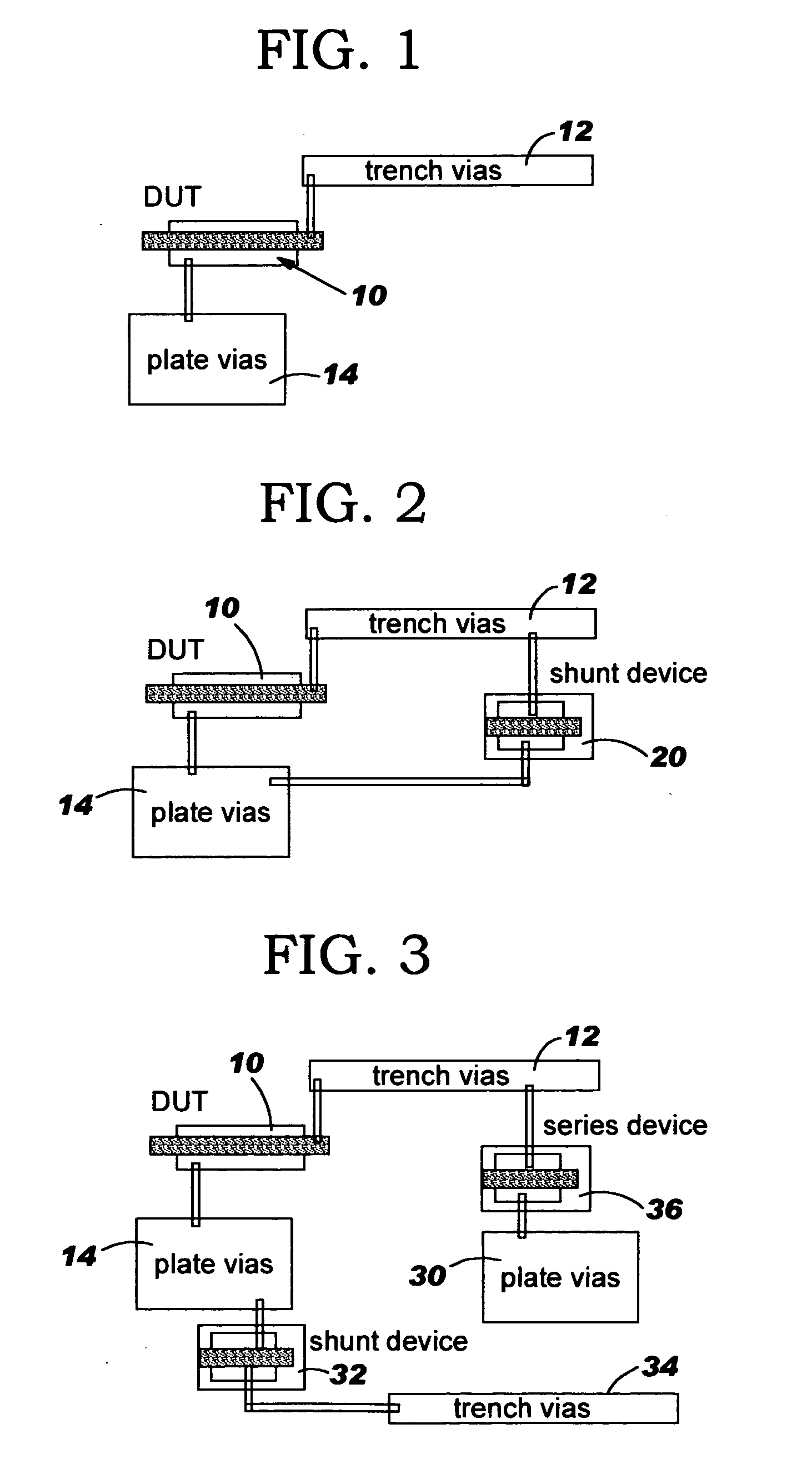
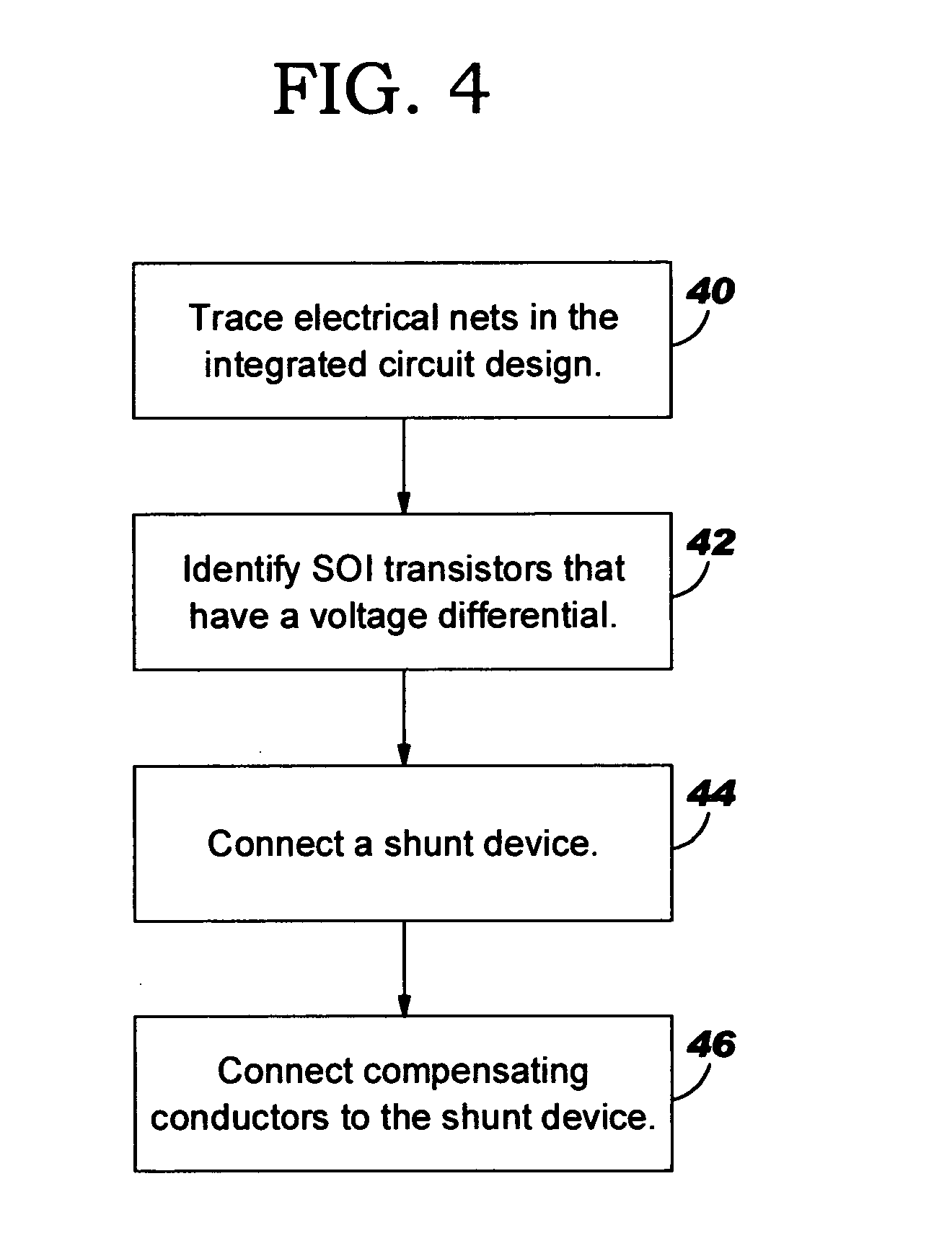
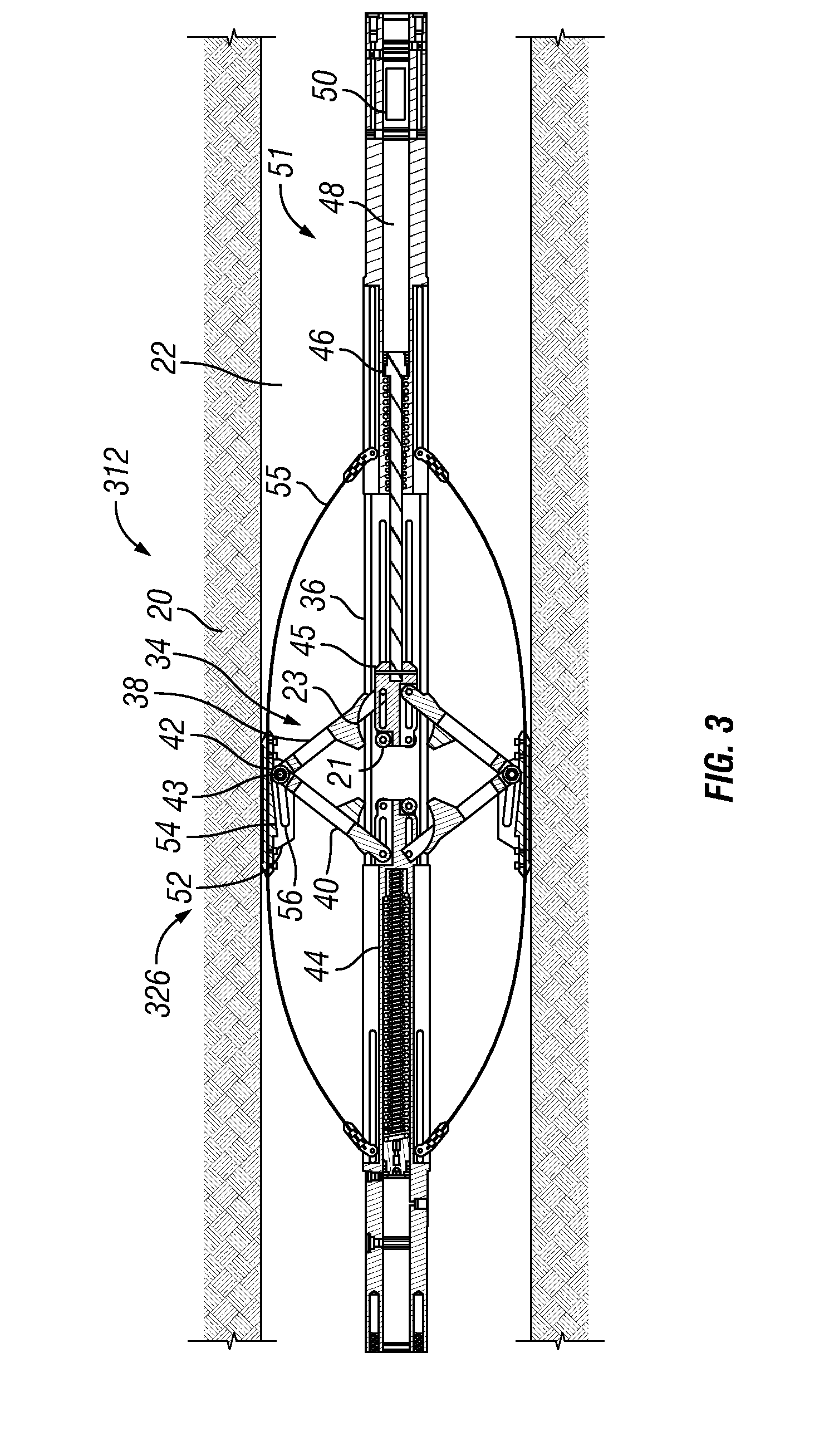
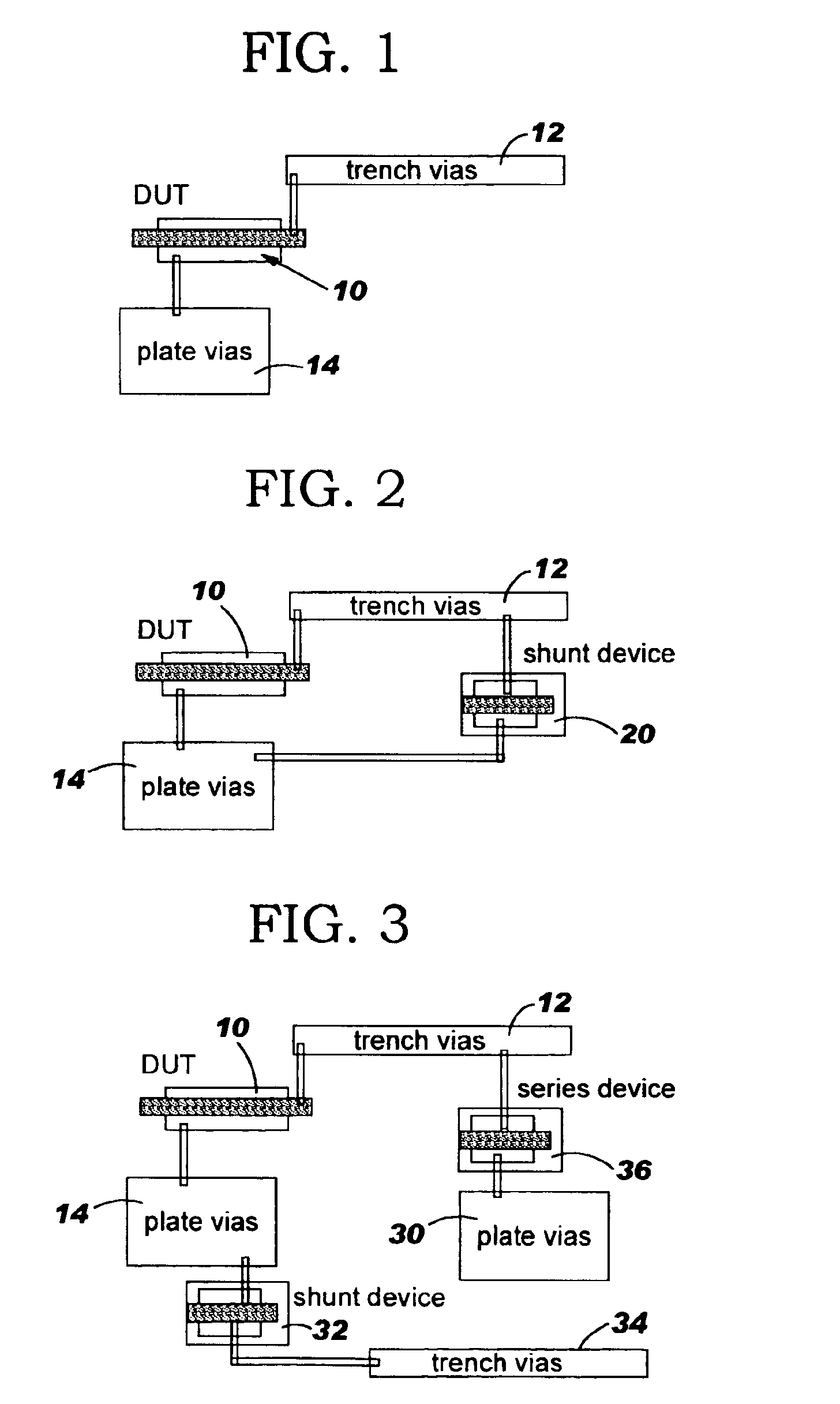
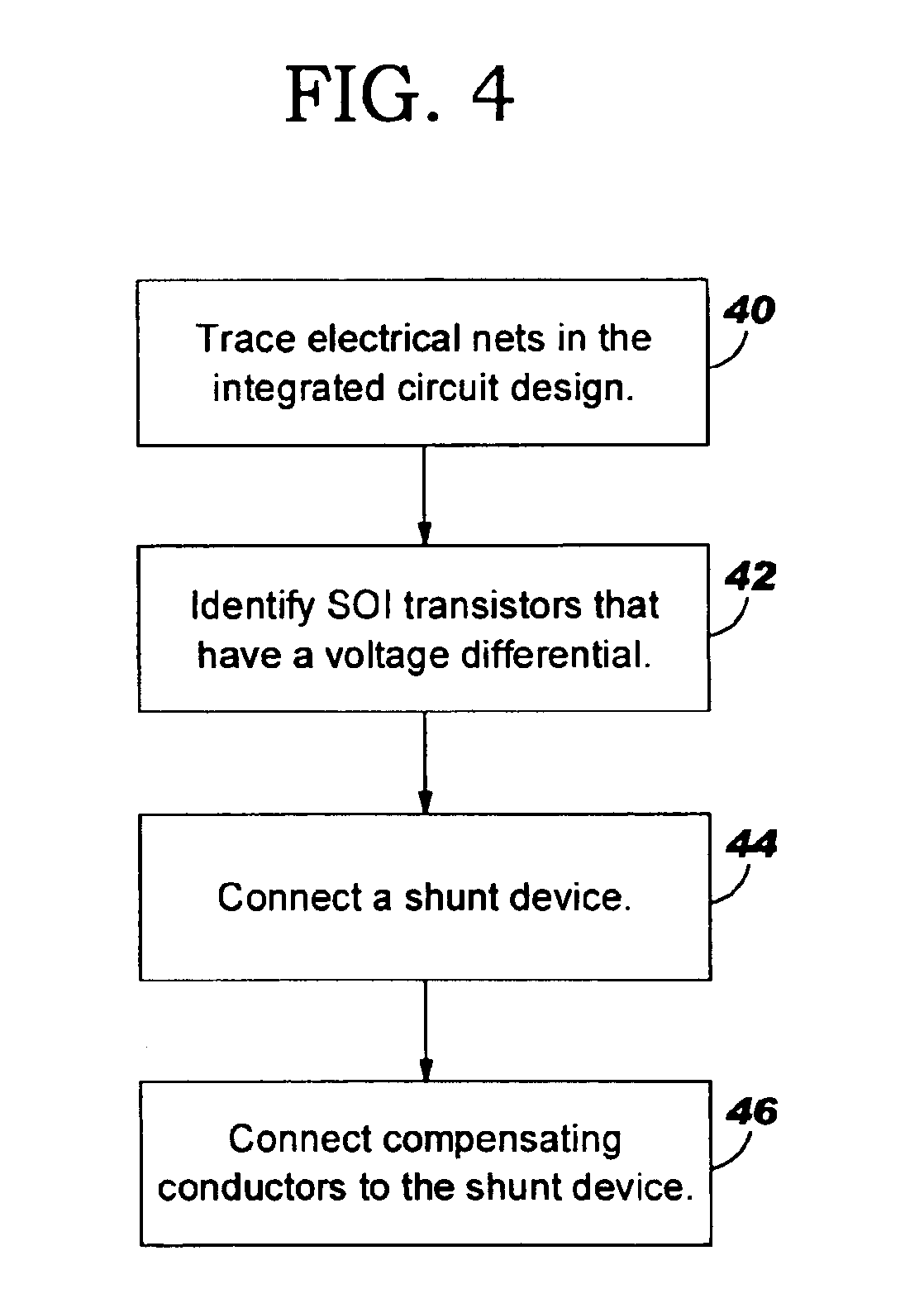
Method of assessing potential for charging damage in soi designs and structures for eliminating potential for damage
InactiveUS20050093072A1Avoid damageReduce the possibility of damageSemiconductor/solid-state device detailsSolid-state devicesShunt DevicePower grid
A method and structure alters an integrated circuit design having silicon over insulator (SOI) transistors. The method / structure prevents damage from charging during processing to the gate of SOI transistors by tracing electrical nets in the integrated circuit design, identifying SOI transistors that have a voltage differential between the source / drain and gate as potentially damaged SOI transistors (based on the tracing of the electrical nets), and connecting a shunt device across the source / drain and the gate of each of the potentially damaged SOI transistors. Alternatively, the method / structure provides for connecting compensating conductors through a series device.
Owner:GLOBALFOUNDRIES INC
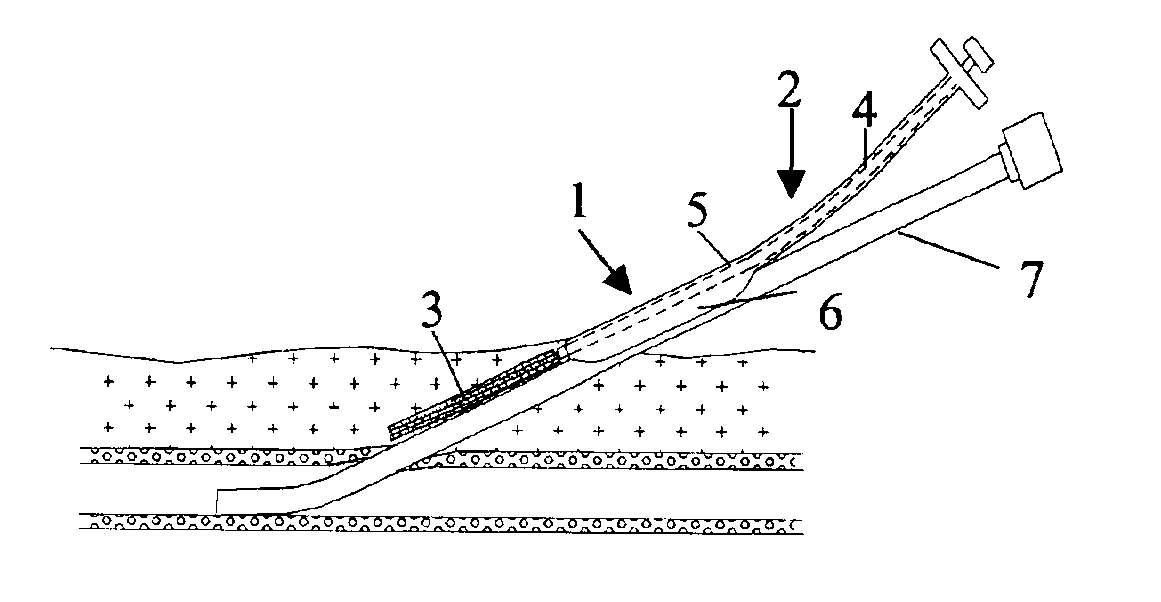
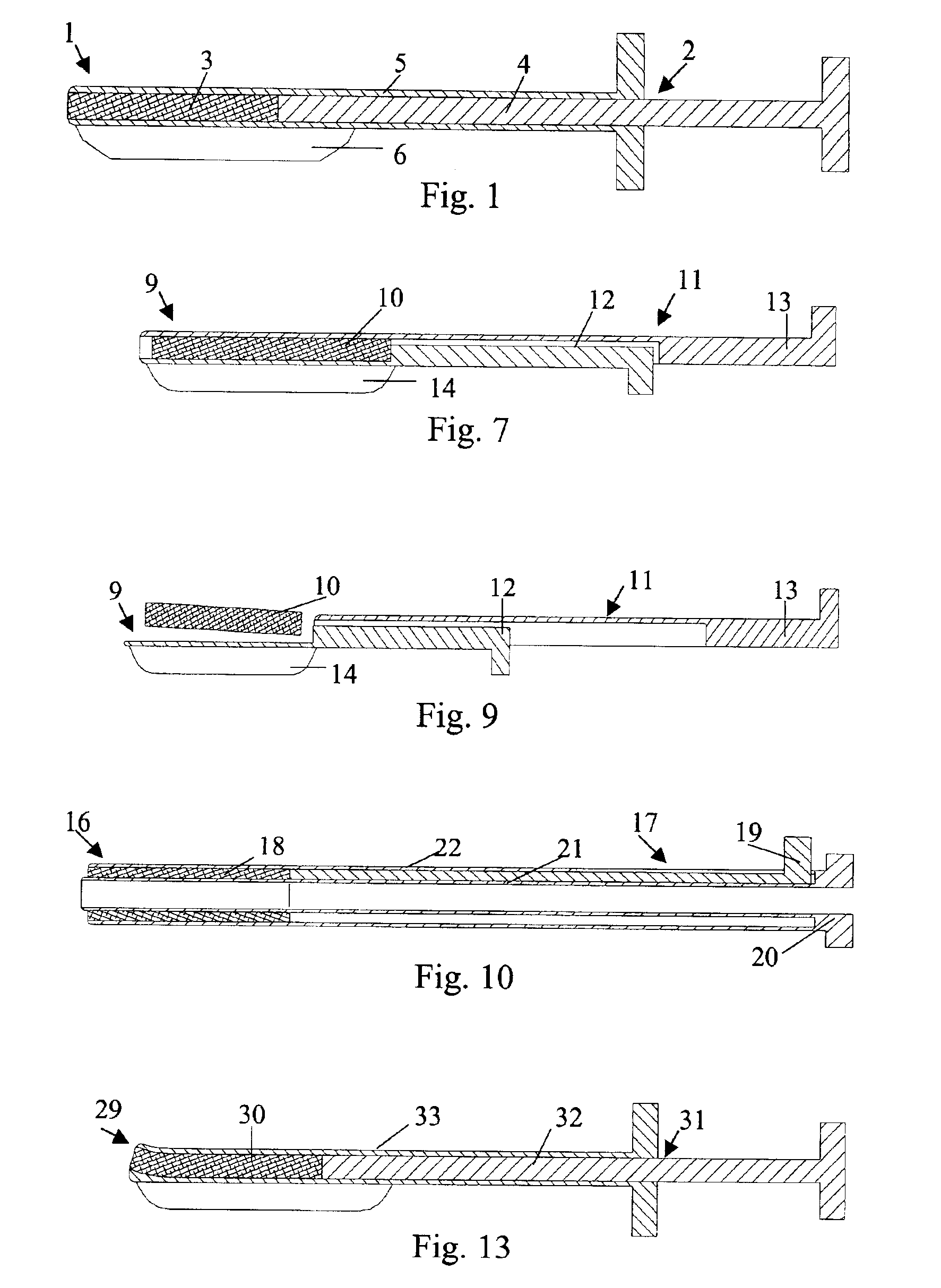
Closure device
InactiveUS6939363B2Eliminate riskPotential damageSuture equipmentsCannulasBlood vesselBiomedical engineering
The invention provides a closure device (1) for sealing an incision channel leading through a vessel wall and into the vessel. The closure device (1) comprises a haemostatic material (3), which is contained in the distal end of an elongated insertion assembly (2). The insertion assembly (2), which comprises a stationary part (4) and a retractable part (5) being slidably movable with regard to each other, is adapted to be attached to an introducer (7) being in position in the incision channel, so that the insertion assembly (2) can be slid along the introducer (7) until the distal end of the insertion assembly (2) is in contact with the vessel wall, where the haemostatic material (3) is delivered in the incision channel by a retracting movement of the retractable part (5).
Owner:ST JUDE MEDICAL COORDINATION CENT
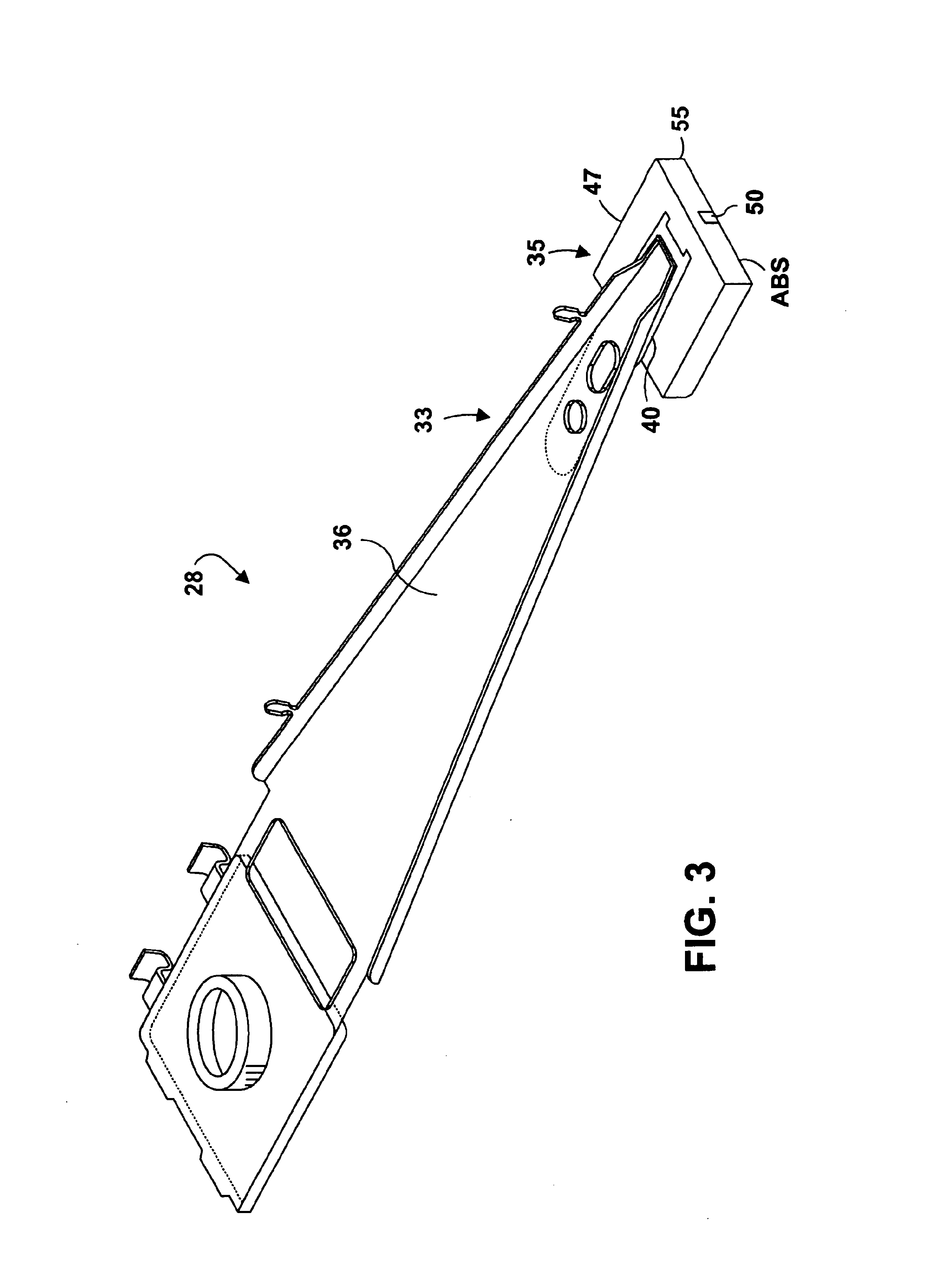
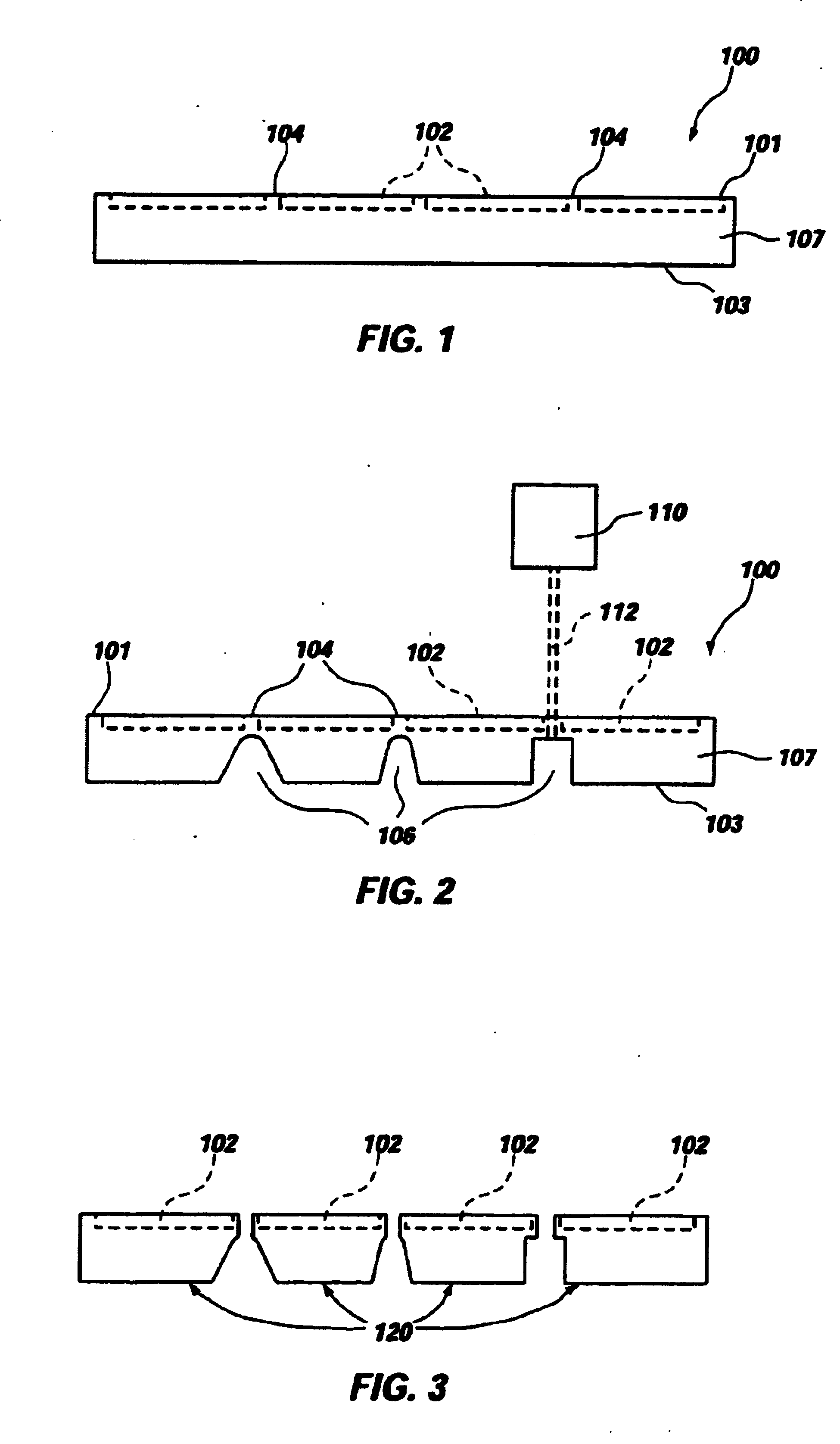
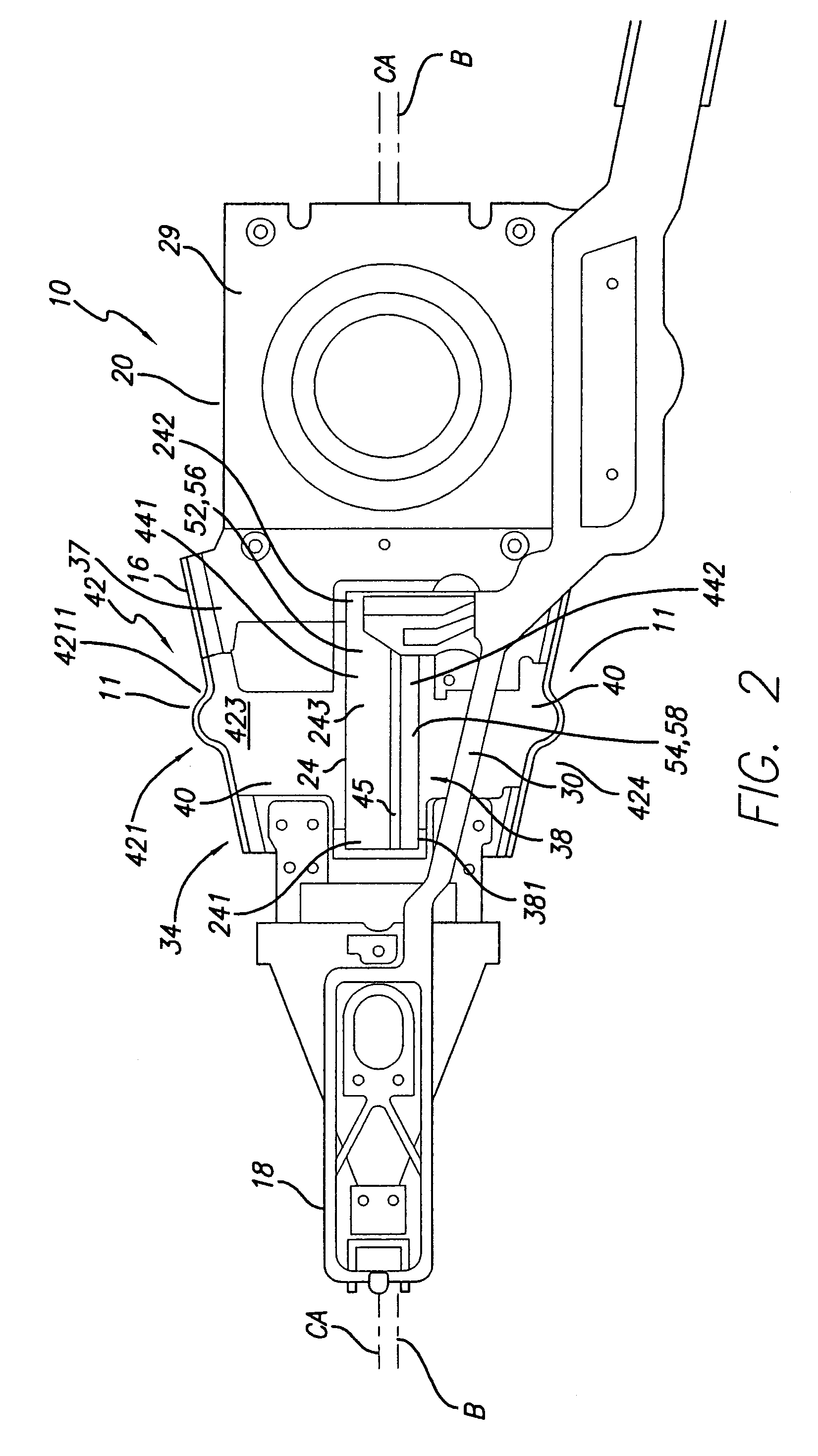
Loading-protected bending microactuator in additive suspensions
ActiveUS7459835B1Improved disk drive suspensionLow costPiezoelectric/electrostriction/magnetostriction machinesArm with actuatorsDistal portionEngineering
A microactuated disk drive suspension for supporting a slider at a disk includes a load beam extending in a plane and having on a common axis a base section adapted for mounting to an actuator, a spring section and a beam section carrying a flexure and the slider thereon. The suspension has relatively movable proximate and distal portions on the common axis that are joined by a bending system cantilevered from the proximate portion and including a cantilevered bending motor opposed to the common axis and having a laterally bendable unsupported region. A cantilevered laterally bendable load assist structure defined by the suspension edges is provided arranged to block undue loading of the bending motor unsupported region.
Owner:MAGNECOMP
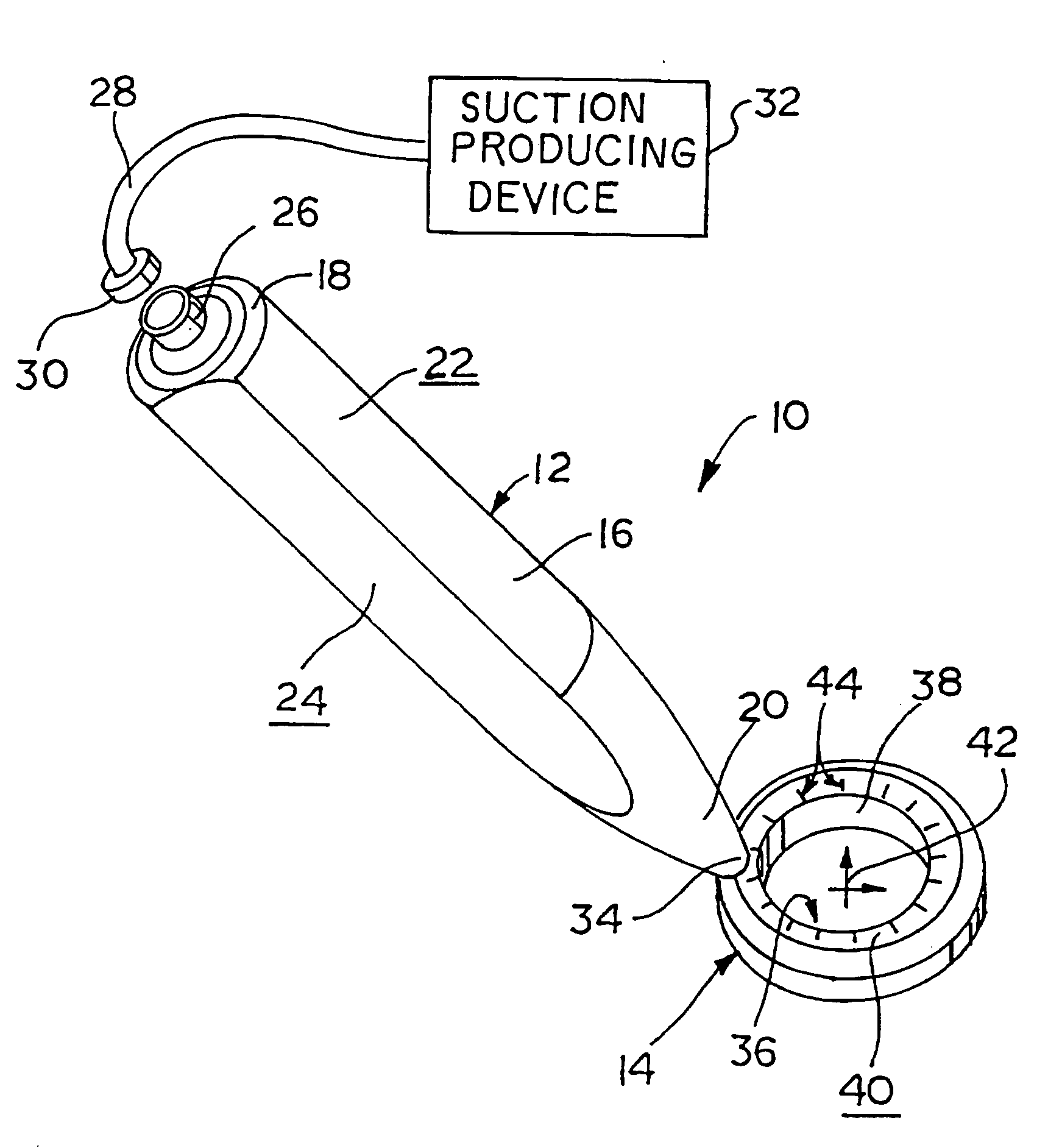
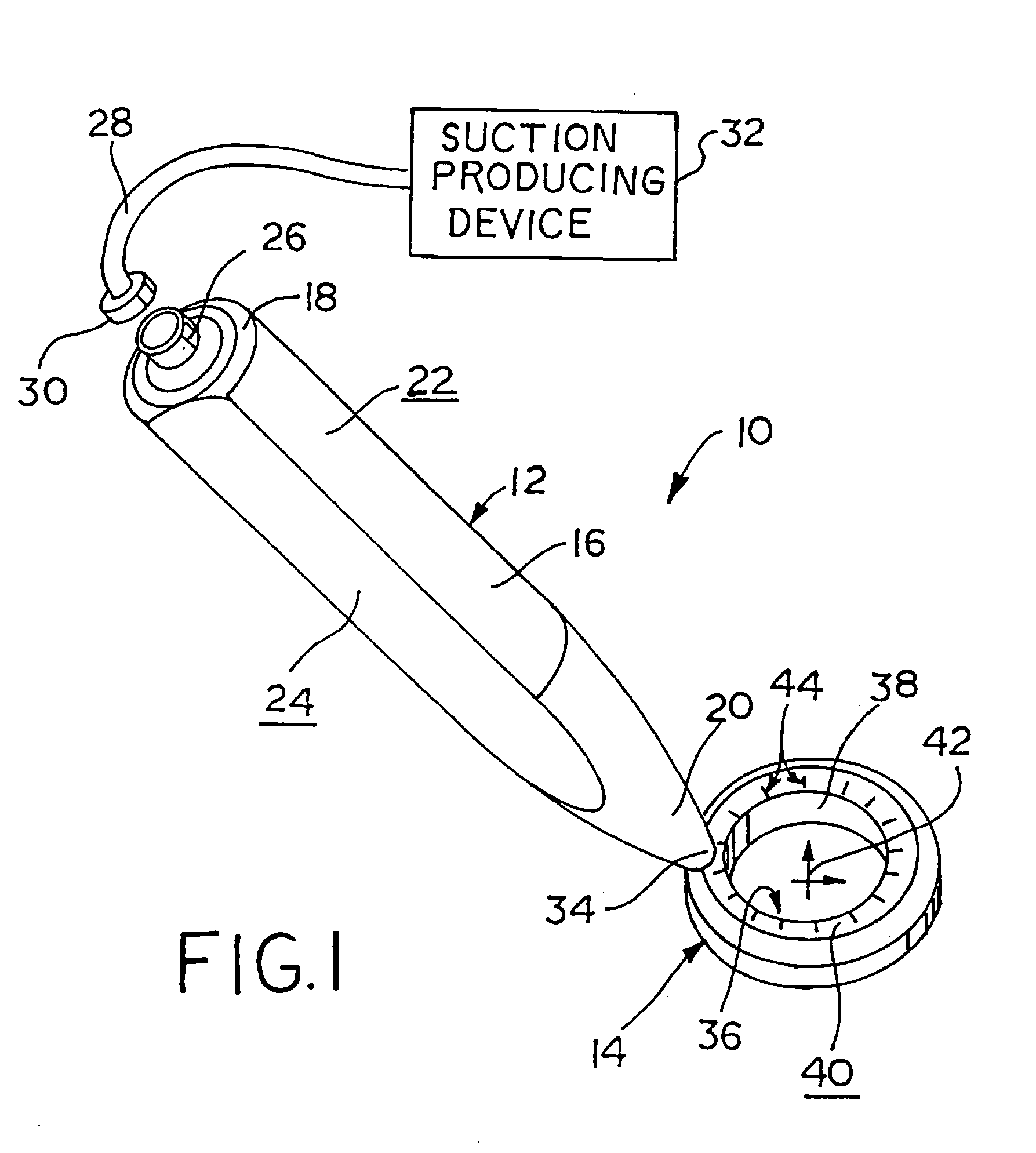
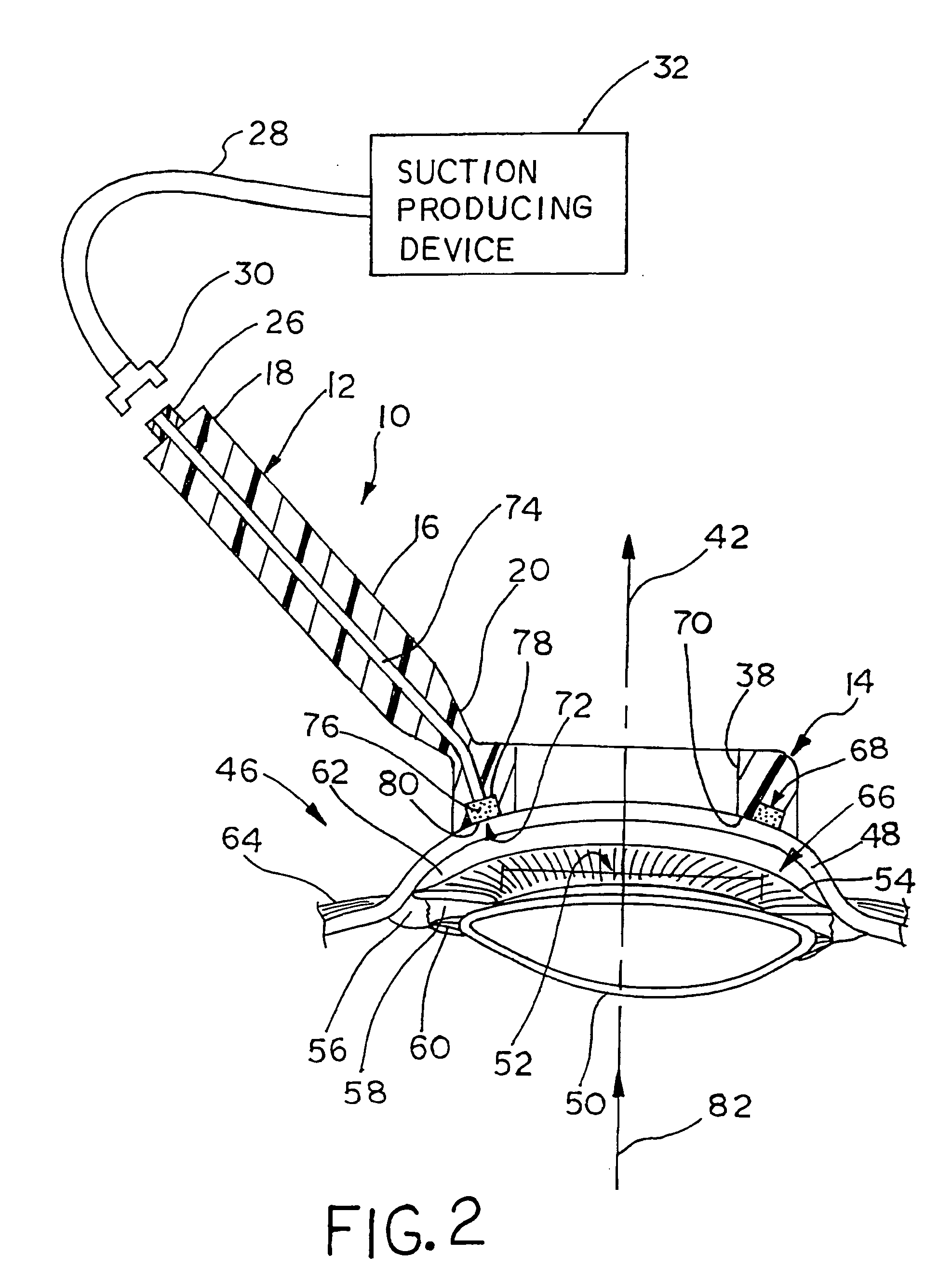
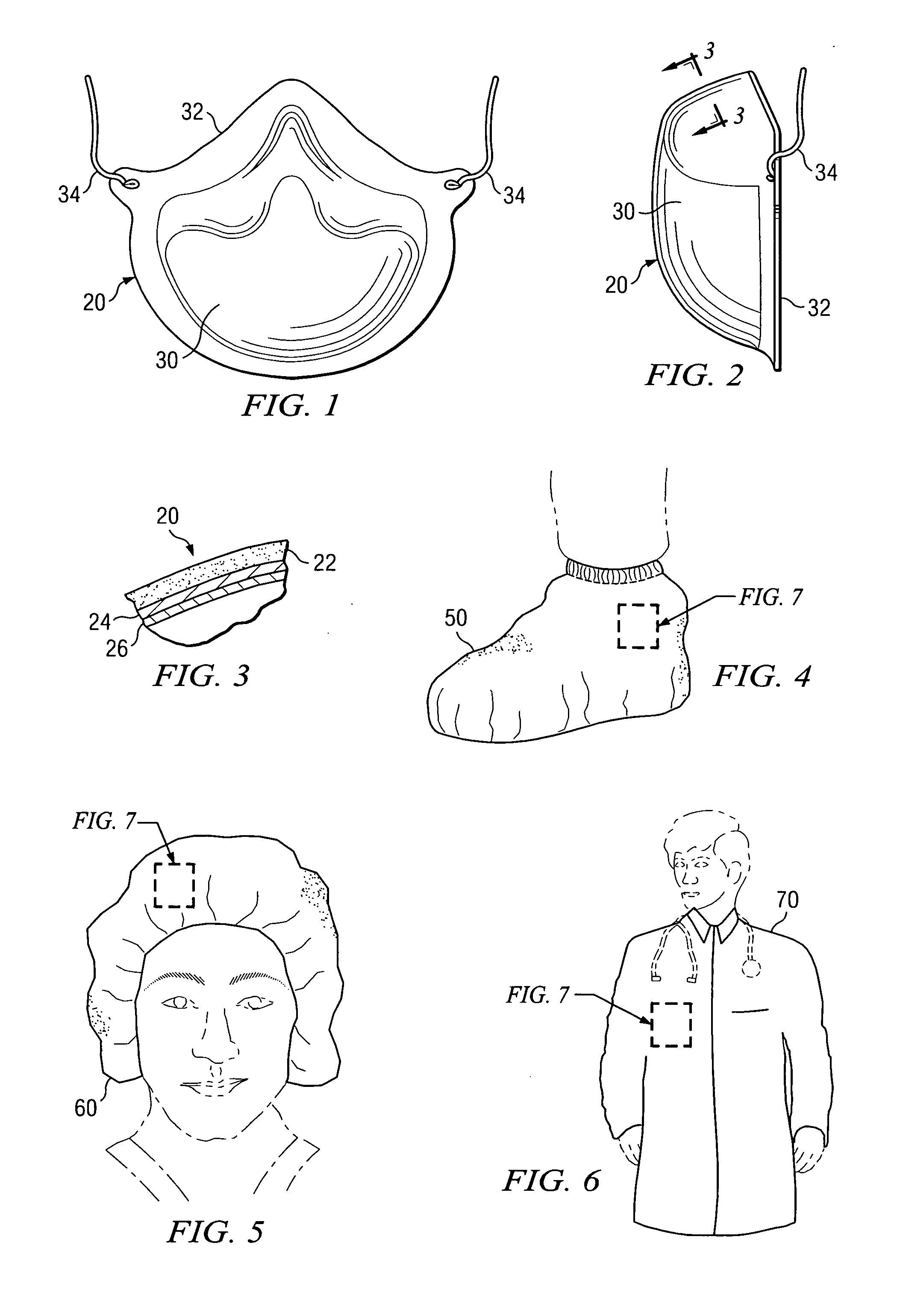
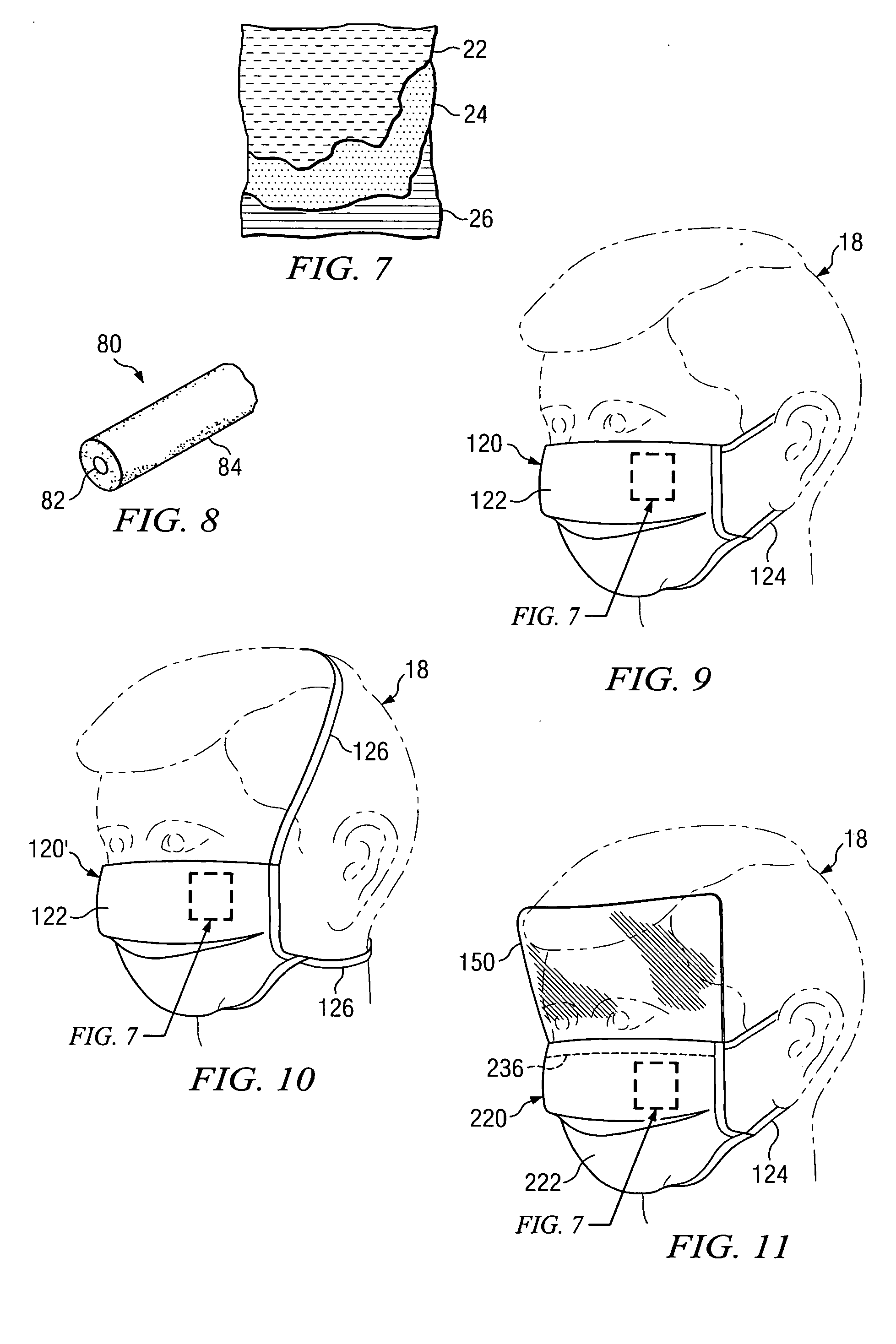
Fixator with membrane
InactiveUS20070083087A1Restrict absorptionCorneal tissue is prevented from becomingEye surgerySurgerySurgical instrumentMembrane configuration
A surgical instrument releasably securable to an eye using suction is provided. The surgical instrument comprises a body, a handle, and a porous member. The body forms an annular suction cavity. The annular suction cavity receives the suction and has an open end in a concave lower surface. The open end is directed toward the eye. The handle is integrally formed with the body. The handle extends upwardly away from the eye and radially outwardly from the body. The handle includes a passage adapted to deliver the suction to the suction cavity. The porous member is disposed within the suction cavity. The porous member is adapted to restrict absorption of the eye into the suction cavity through the open end and to permit the suction to permeate the suction cavity and reach the open end such that the surgical instrument is releasably securable to the eye using the suction.
Owner:SISMED
Methods for ablation with radiant energy
InactiveUS20060253113A1Rapid and efficient creationRapid and effective photoablationStentsUltrasound therapyCoaxial catheterTarget tissue
Ablation methods and instruments are disclosed for creating lesions in tissue, especially cardiac tissue for treatment of arrhythmias and the like. Percutaneous ablation instruments in the form of coaxial catheter bodies are disclosed having at least one central lumen therein and having one or more balloon structures at the distal end region of the instrument. The instruments include an energy emitting element which is independently positionable within the lumen of the instrument and adapted to project radiant energy through a transmissive region of a projection balloon to a target tissue site. The instrument can optionally include at least one expandable anchor balloon disposed about, or incorporated into an inner catheter body designed to be slid over a guidewire. This anchor balloon can serve to position the device within a lumen, such as a pulmonary vein. A projection balloon structure is also disclosed that can be slid over the first (anchor balloon) catheter body and inflated within the heart, to define a staging from which to project radiant energy. An ablative fluid can also be employed outside of the instrument (e.g., between the balloon and the target region) to ensure efficient transmission of the radiant energy when the instrument is deployed. In another aspect of the invention, generally applicable to a wide range of cardiac ablation instruments, mechanisms are disclosed for determining whether the instrument has been properly seated within the heart, e.g., whether the device is in contact with a pulmonary vein and / or the atrial surface, in order to form a lesion by heating, cooling or projecting energy. This contact-sensing feature can be implemented by an illumination source situated within the instrument and an optical detector that monitors the level of reflected light. Measurements of the reflected light (or wavelengths of the reflected light) can thus be used to determine whether contact has been achieved and whether such contact is continuous over a desired ablation path.
Owner:CARDIOFOCUS INC
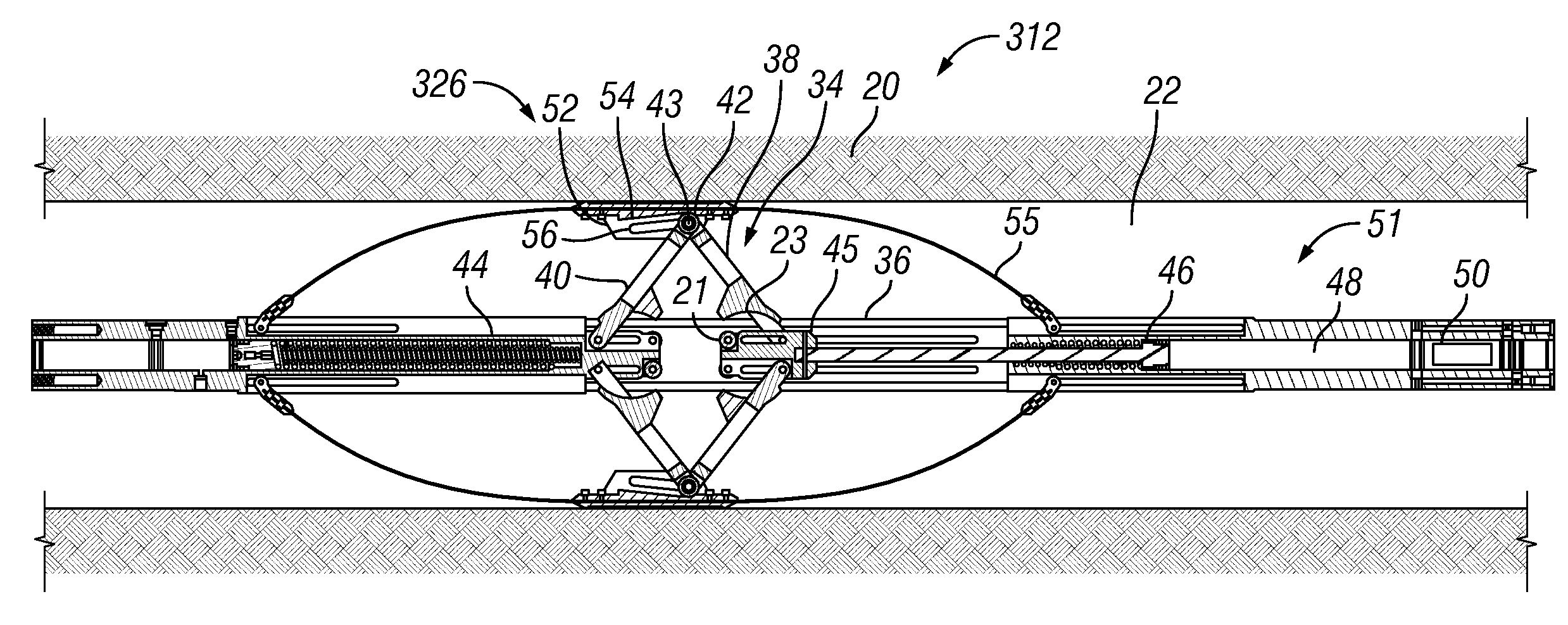
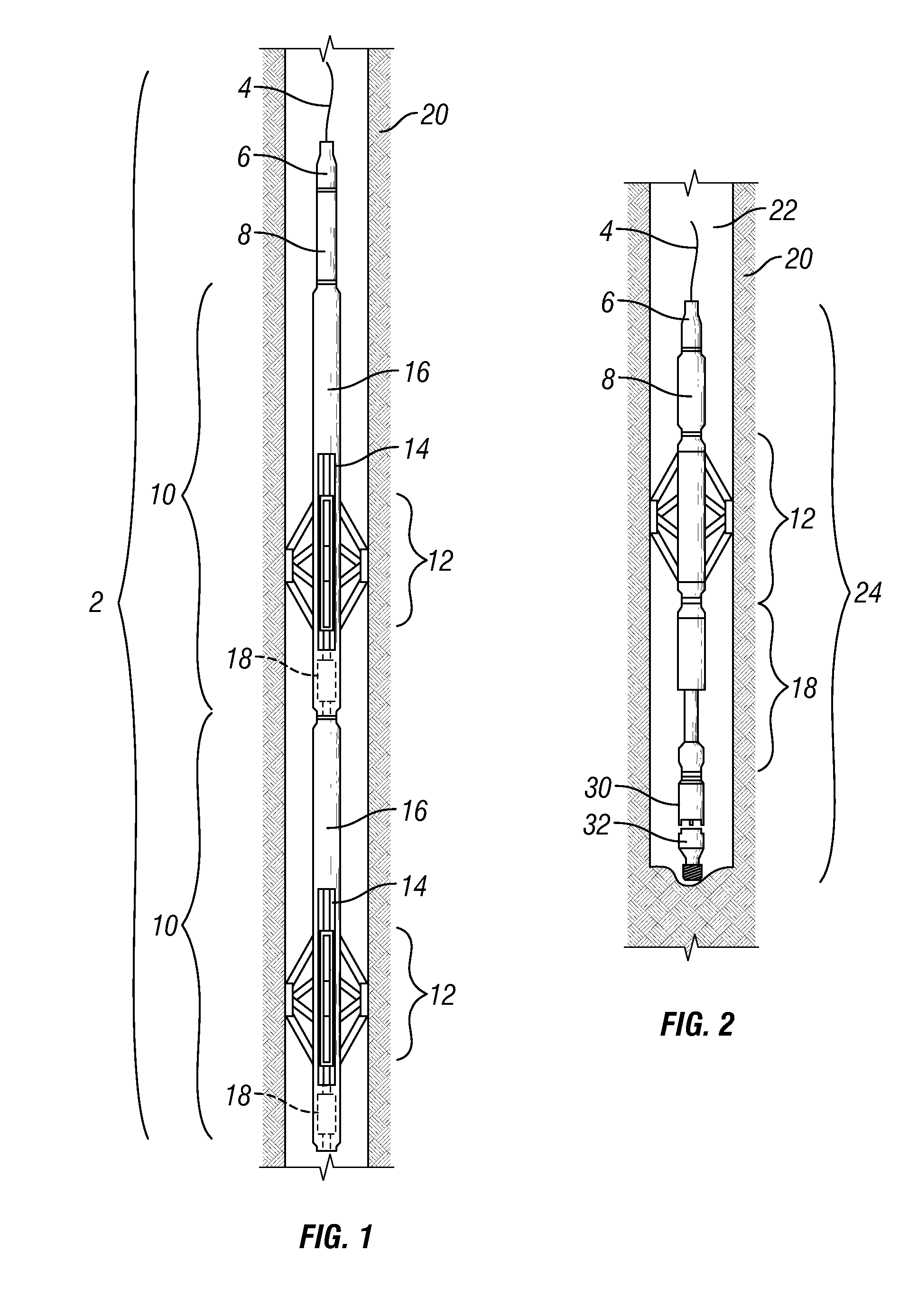
Self-anchoring device with force amplification
ActiveUS20070181298A1Potential damageLower potentialDrilling rodsFluid removalEngineeringAudio power amplifier
A downhole tool is provided that includes a grip assembly for contacting a well formation. The grip assembly includes a gripper body; and a centralizer that is attached to and radially expandable with respect to the gripper body and that has a geometry which is lockable by a locking device. The grip assembly also includes a force amplifier in force transmitting relation with the centralizer, wherein the force amplifier transfers a force in a first direction to a much larger force in a second direction when the centralizer is locked by the locking device.
Owner:SCHLUMBERGER TECH CORP
Method of assessing potential for charging damage in SOI designs and structures for eliminating potential for damage
InactiveUS7067886B2Avoid damagePotential damageSemiconductor/solid-state device detailsSolid-state devicesShunt DevicePower grid
A method and structure alters an integrated circuit design having silicon over insulator (SOI) transistors. The method / structure prevents damage from charging during processing to the gate of SOI transistors by tracing electrical nets in the integrated circuit design, identifying SOI transistors that have a voltage differential between the source / drain and gate as potentially damaged SOI transistors (based on the tracing of the electrical nets), and connecting a shunt device across the source / drain and the gate of each of the potentially damaged SOI transistors. Alternatively, the method / structure provides for connecting compensating conductors through a series device.
Owner:GLOBALFOUNDRIES INC
Multiple layer nonwoven products and methods for creating color schemes and for producing such products
InactiveUS20050170726A1Reduce in quantityEliminating and substantially reducing potential damageLayered productsMedical devicesColor schemeMaterials science
Owner:K B AVIATION INC
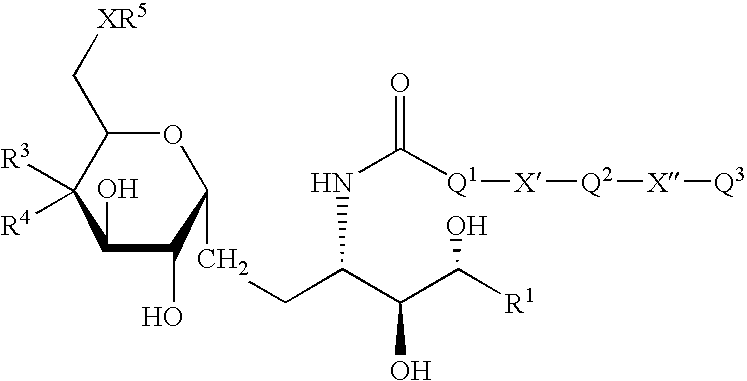
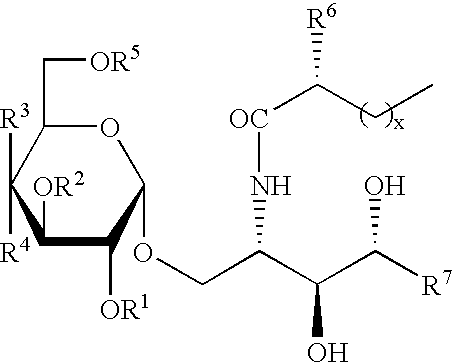
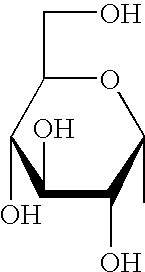
Synthetic C-glycolipid and its use for treating cancer, infectious diseases and autoimmune diseases
The invention is directed to compounds of formula (I) wherein X is O or NH; R' is a hydrocarbon chain; R<3 >and R<4 >are hydrogen, OH or a monosaccharide; R<5 >is hydrogen or a monosaccharide; Q' is optionally present and may be a C1-10 hydrocarbon; X' is optionally present and may be O, S or NR<8>; and Q<3 >may be a hydrocarbon or hydrogen. The invention is also directed to the use of the compounds for treating cancer, infectious diseases and autoimmune diseases. The invention is also directed to syntheses of the compounds of formula (I).
Owner:RES FOUND THE CITY UNIV OF NEW YORK +1
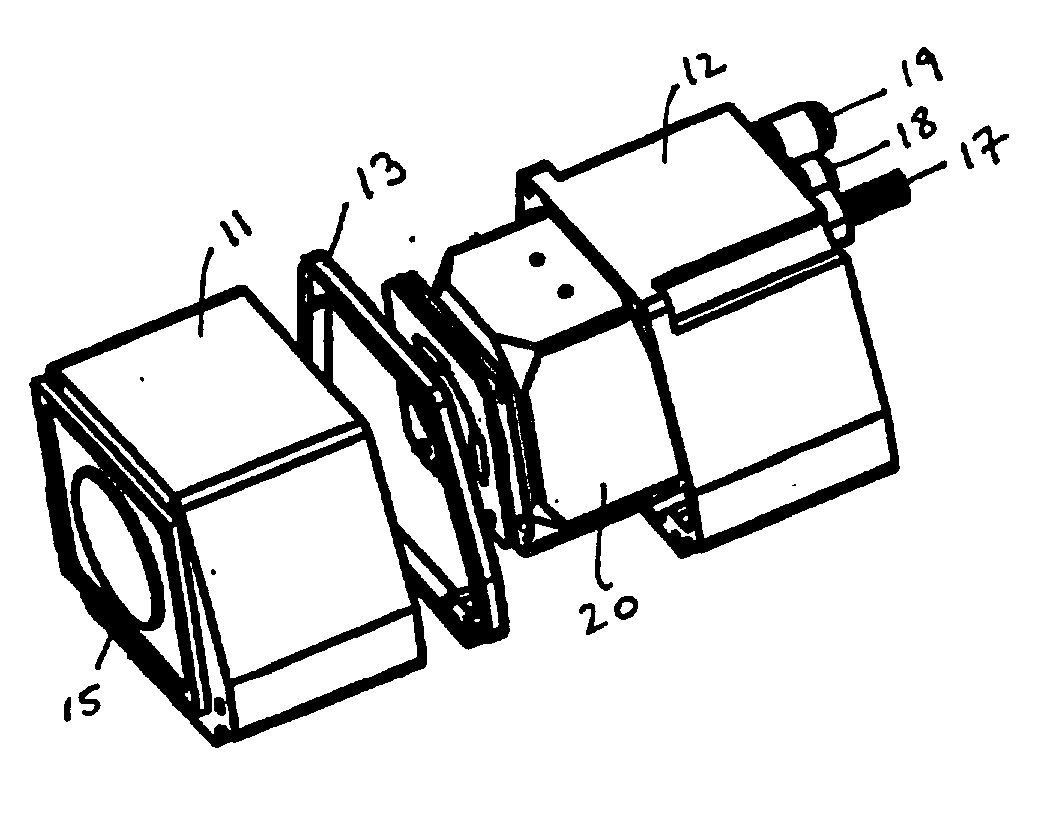
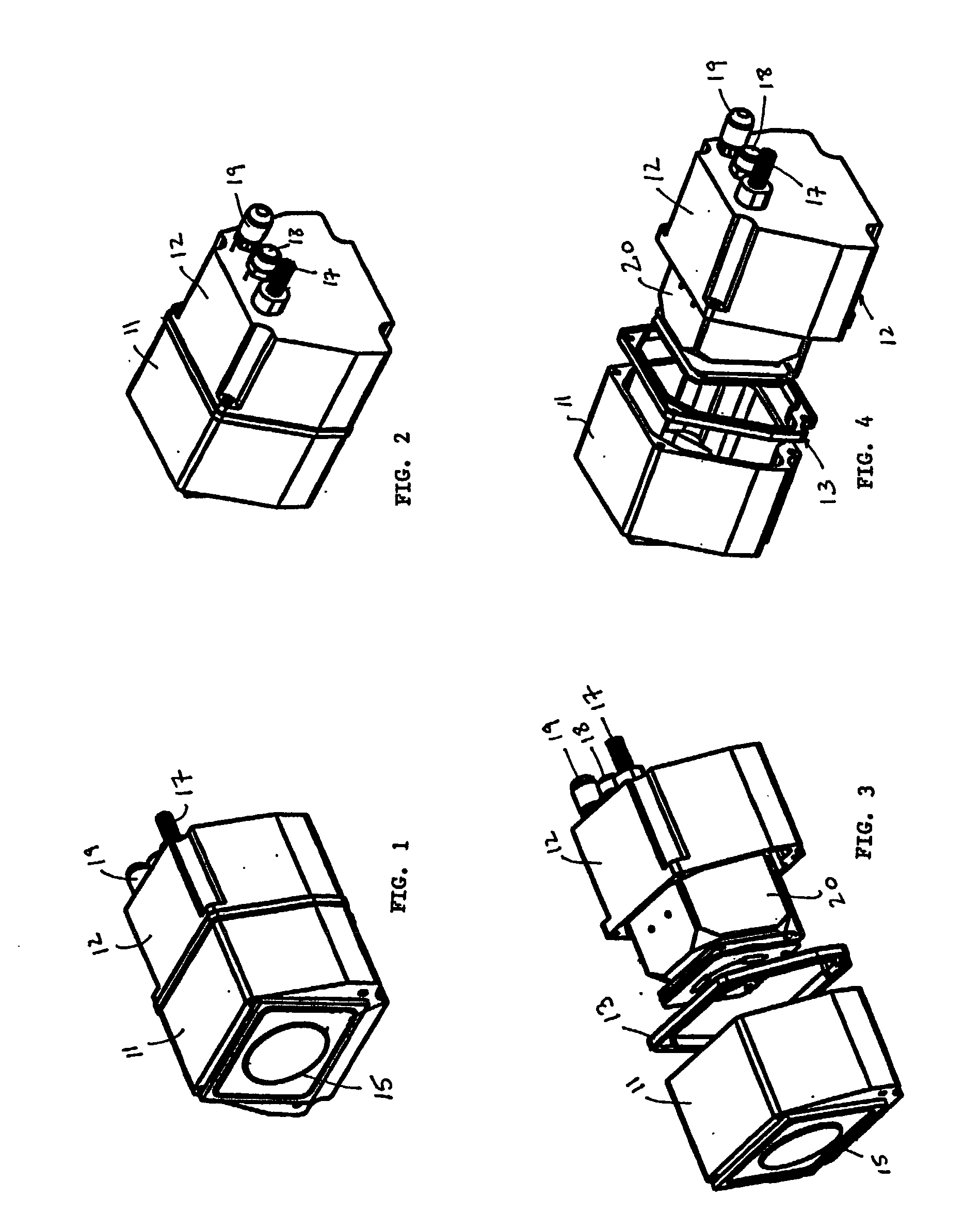
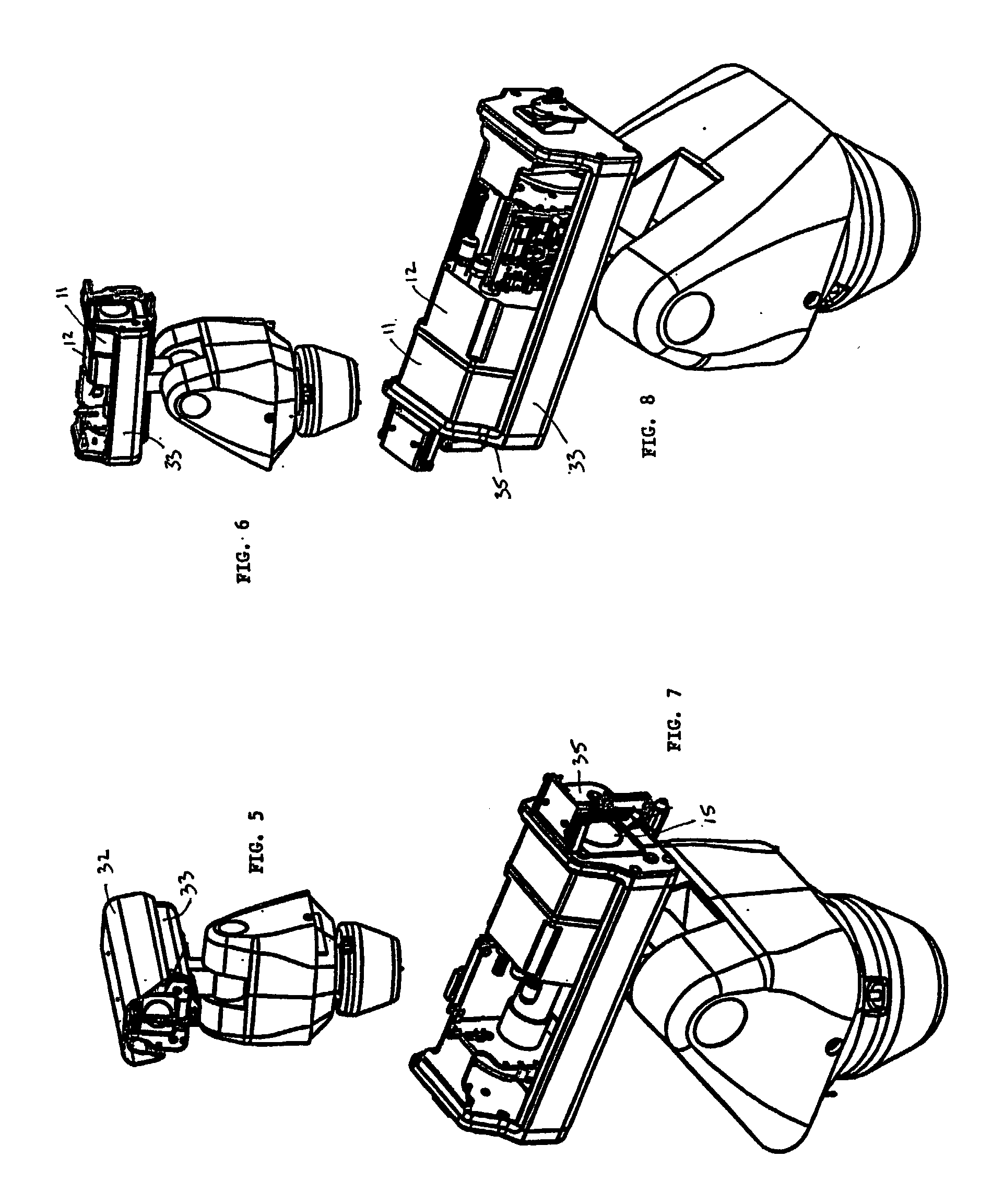
Controllable sealed chamber for surveillance camera
InactiveUS20020140848A1Easy to deployMinimizing chanceTelevision system detailsColor television detailsCamera lensDisplay device
A chamber for a surveillance camera that is designed to be mounted inside a larger camera housing. The chamber is sealed and provides a controlled internal environment for sensitive camera optics and internal electronics. A flush mount window is provided for the front lens of the camera, and a sealed feed-through electronic connector is provided for attachment to external controls. Valves for both adding and removing gasses to / from the chamber are provided. In one embodiment, temperature, pressure and / or humidity sensors may be deployed inside the chamber and connected electronically to a display or computer for monitoring and adjustment. In another embodiment of, a heating element is provided to evaporate moisture from the camera lens and / or from the window, and to help control the temperature inside the chamber.
Owner:PELCO INC
Protective Fiber Optic Union Adapters
ActiveUS20080019642A1Highly efficient optical couplingLow insertion lossCoupling light guidesFiberEngineering
Devices to enhance the reliability of optical networks and to reduce the cost of repair are disclosed in this invention. In particular, compact and inexpensive fiber optic union adapters with built-in protective isolation prevent the transfer of damage from one connectorized fiber optic cable to another. The fiber optic union includes a split sleeve with an interior channel and a fiber stub centrally located within the interior channel. The fiber stub makes direct optical contact with the cable endfaces to enable efficient optical transmission between interconnected cables while providing a low loss, low back reflection adiabatic transition between the waveguide cores of the two cables.
Owner:TELESCENT
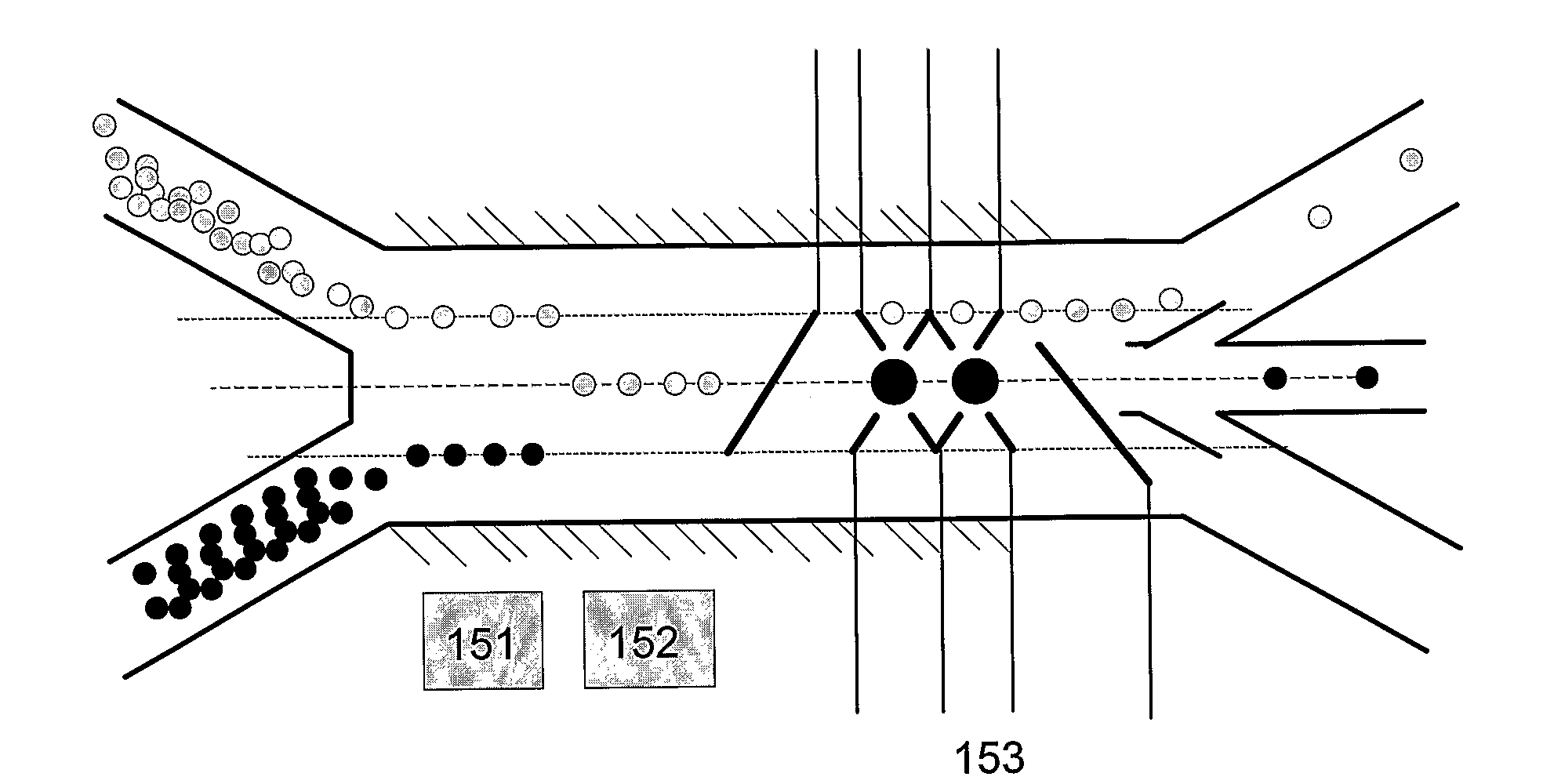
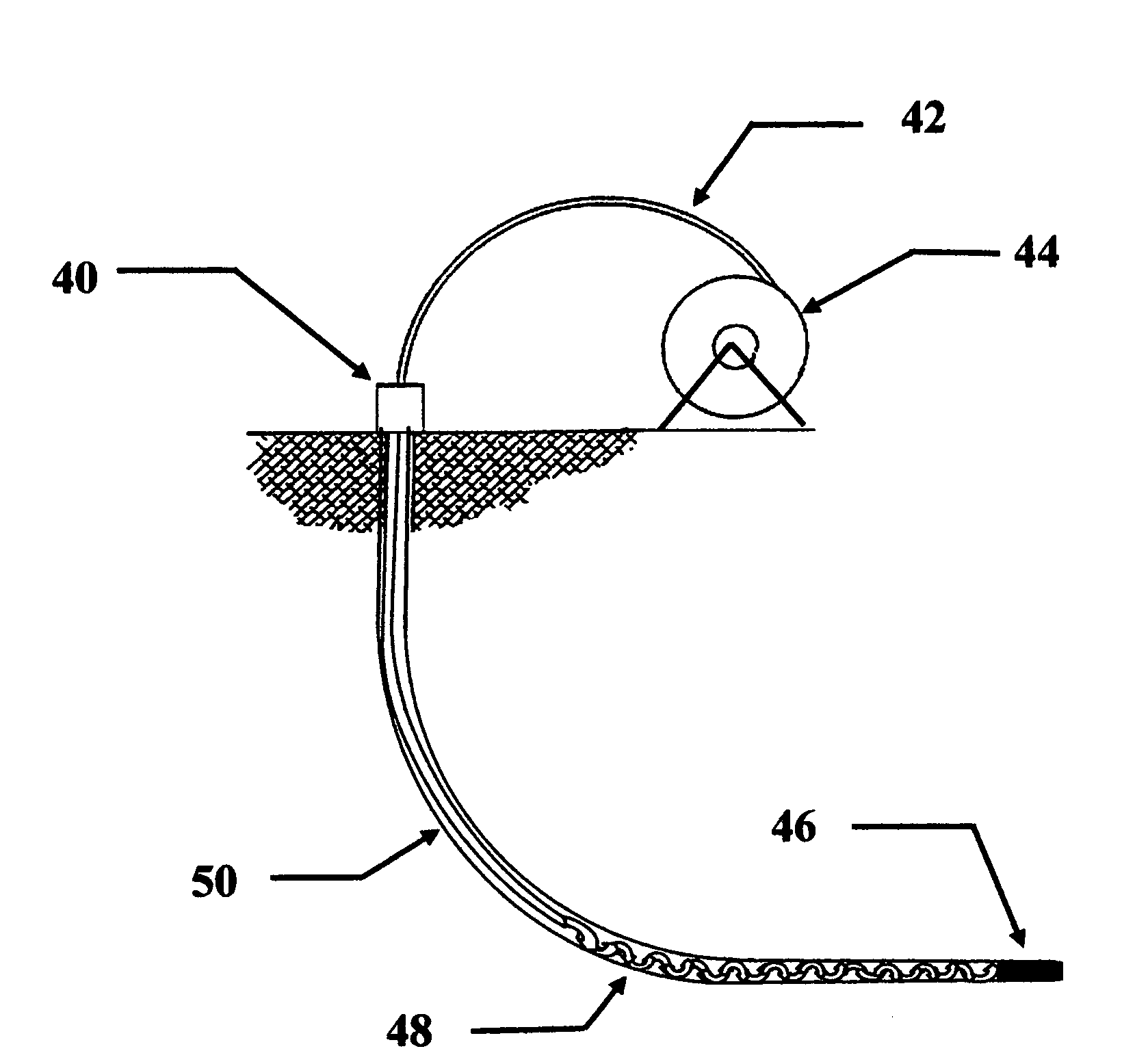
Method and Device for Acoustic Manipulation of Particles, Cells and Viruses
InactiveUS20090226994A1Efficient couplingEasy to controlBioreactor/fermenter combinationsBiological substance pretreatmentsSuspended particlesPresent method
The present invention relates to a method and device for non-intrusively manipulating suspended particles and / or cells and / or viruses, which are supplied to a micro-chamber or to a micro-channel (46) of a substrate, said micro-chamber or micro-channel (46) having at least a bottom wall as well as lateral walls. At least one acoustic wave (41) is applied via at least one acoustic transducer (42, 44) from outside of said substrate to an inner volume of said micro-chamber or micro-channel (46), a frequency of said acoustic wave (41) being selected to generate a standing and / or stationary acoustic wave in said volume. In the present method and device the acoustic wave (41) is applied laterally to said volume. The present device and method allow an efficient coupling of energy into the channels as well as an improved control of standing and / or stationary acoustic wave fields along the channels. Furthermore the device and method allow for transmission optical microscopy to observe the manipulated particles in the channels during manipulation.
Owner:FRAUNHOFER GESELLSCHAFT ZUR FOERDERUNG DER ANGEWANDTEN FORSCHUNG EV
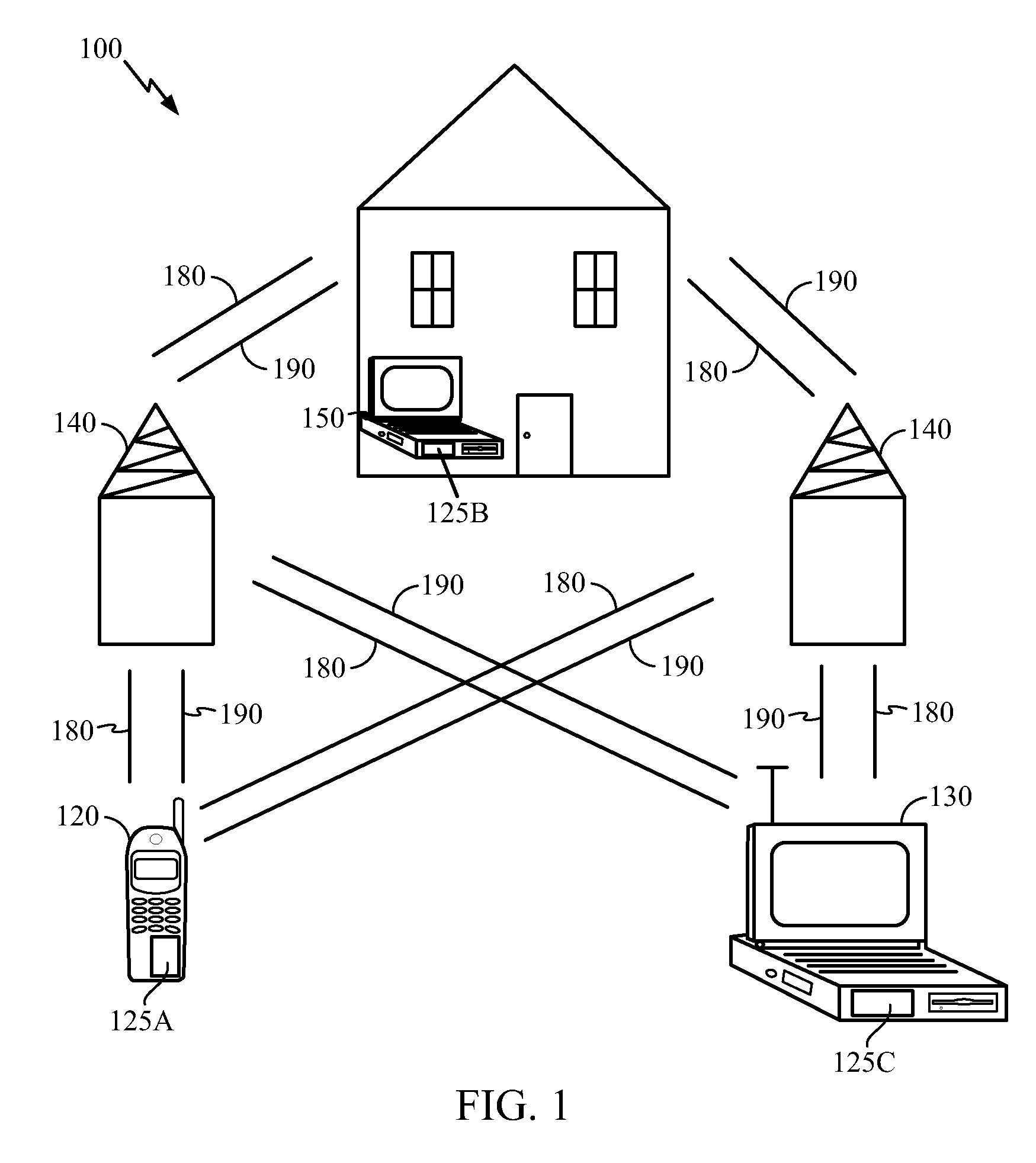
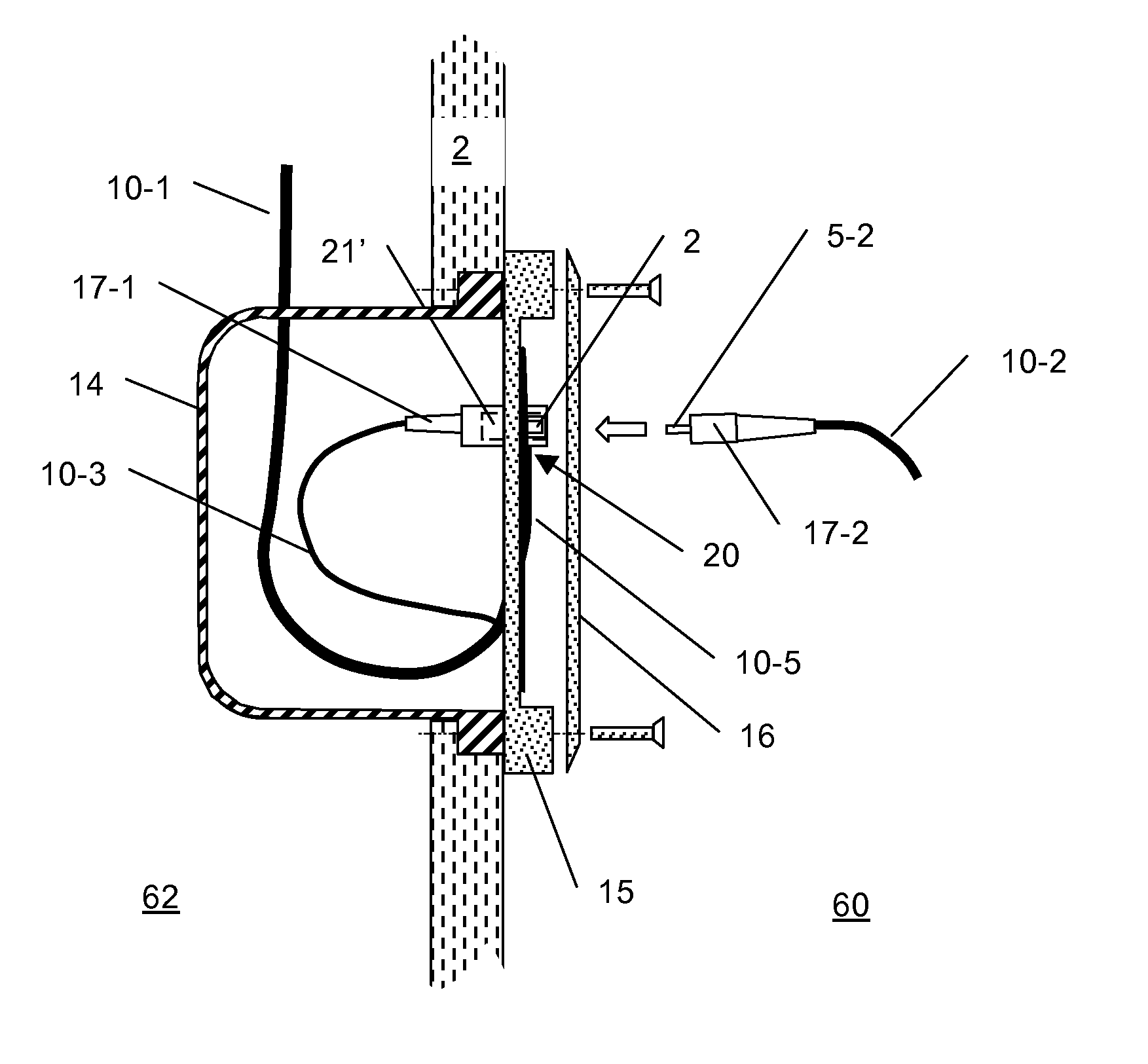
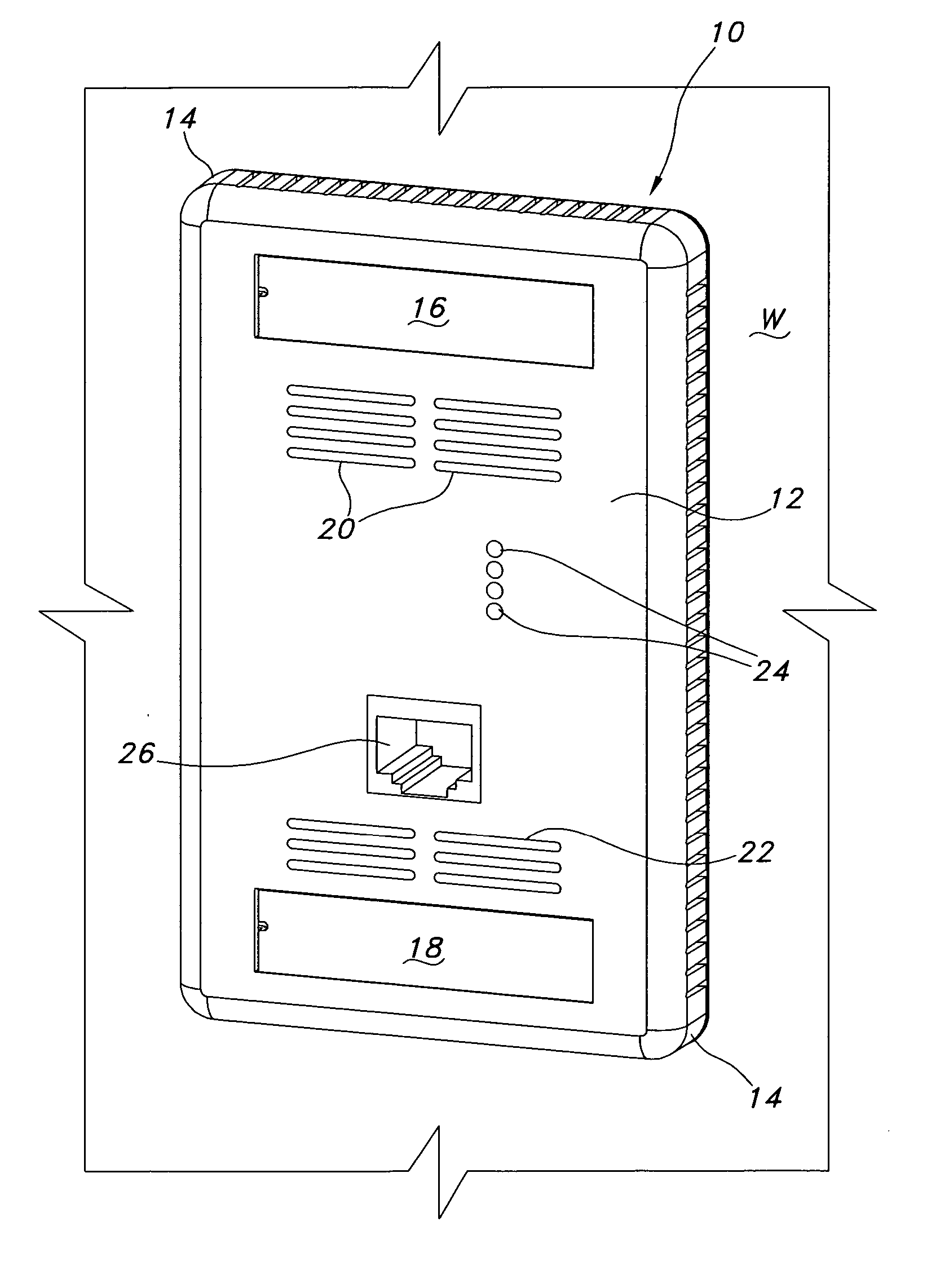
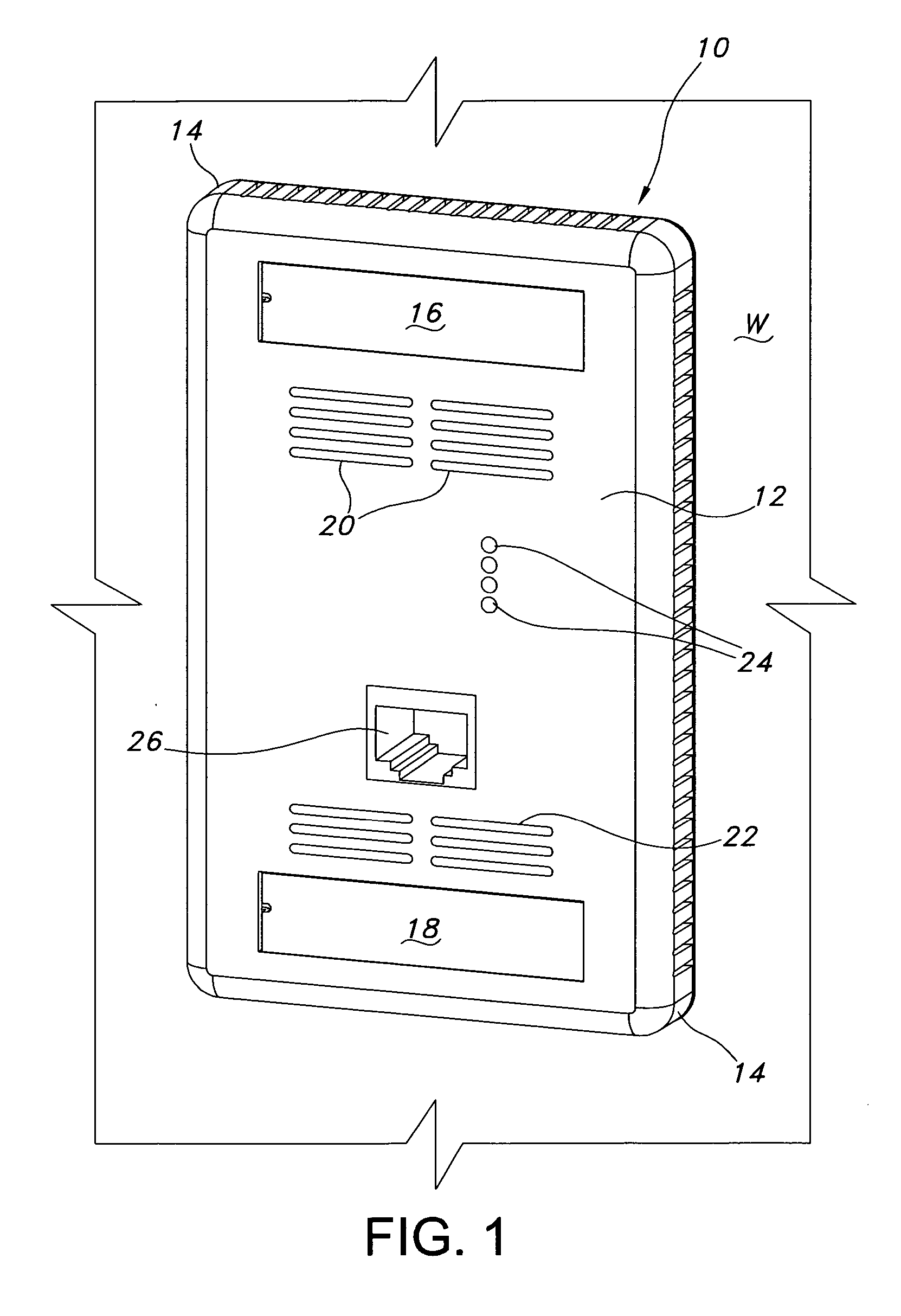
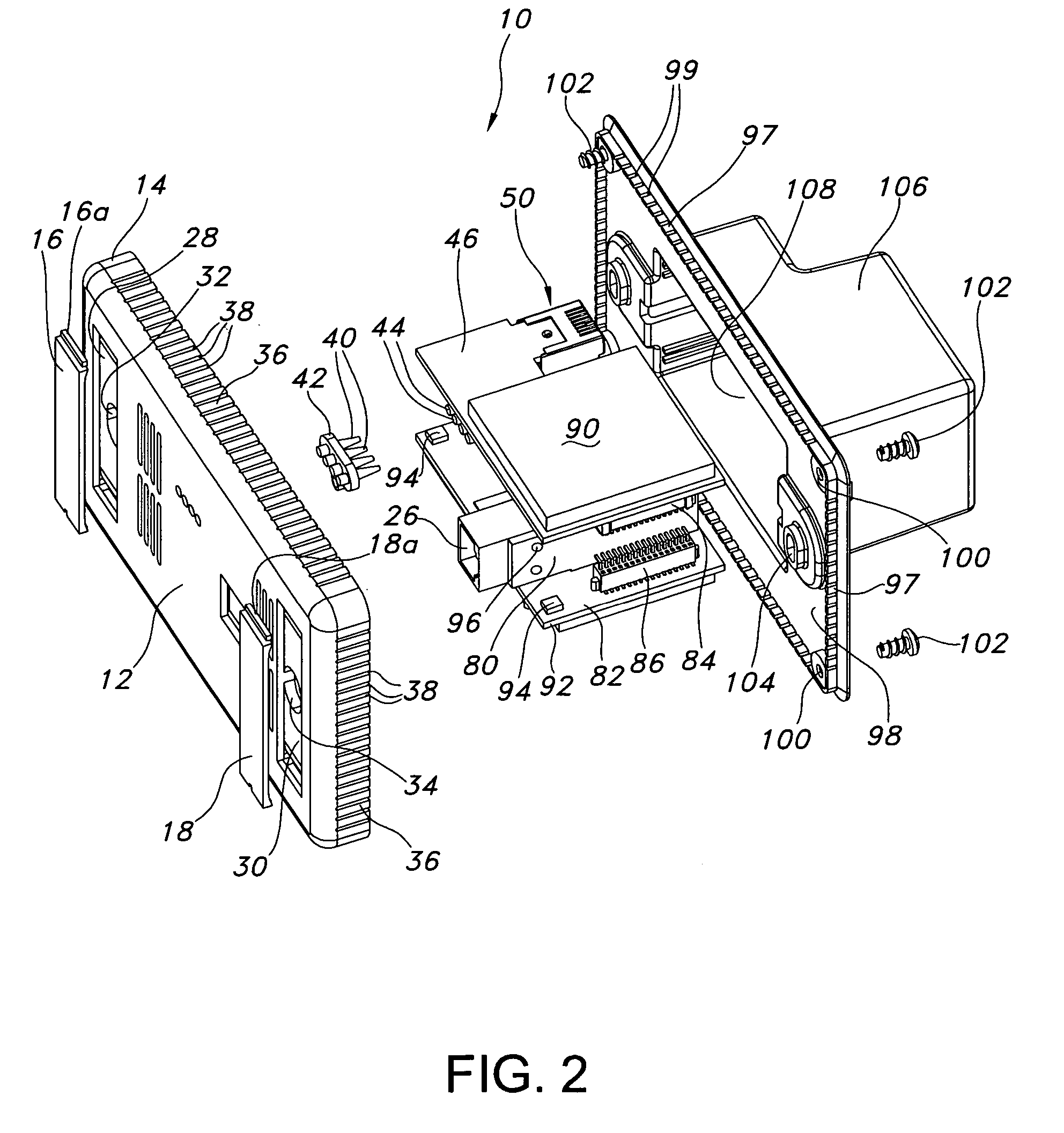
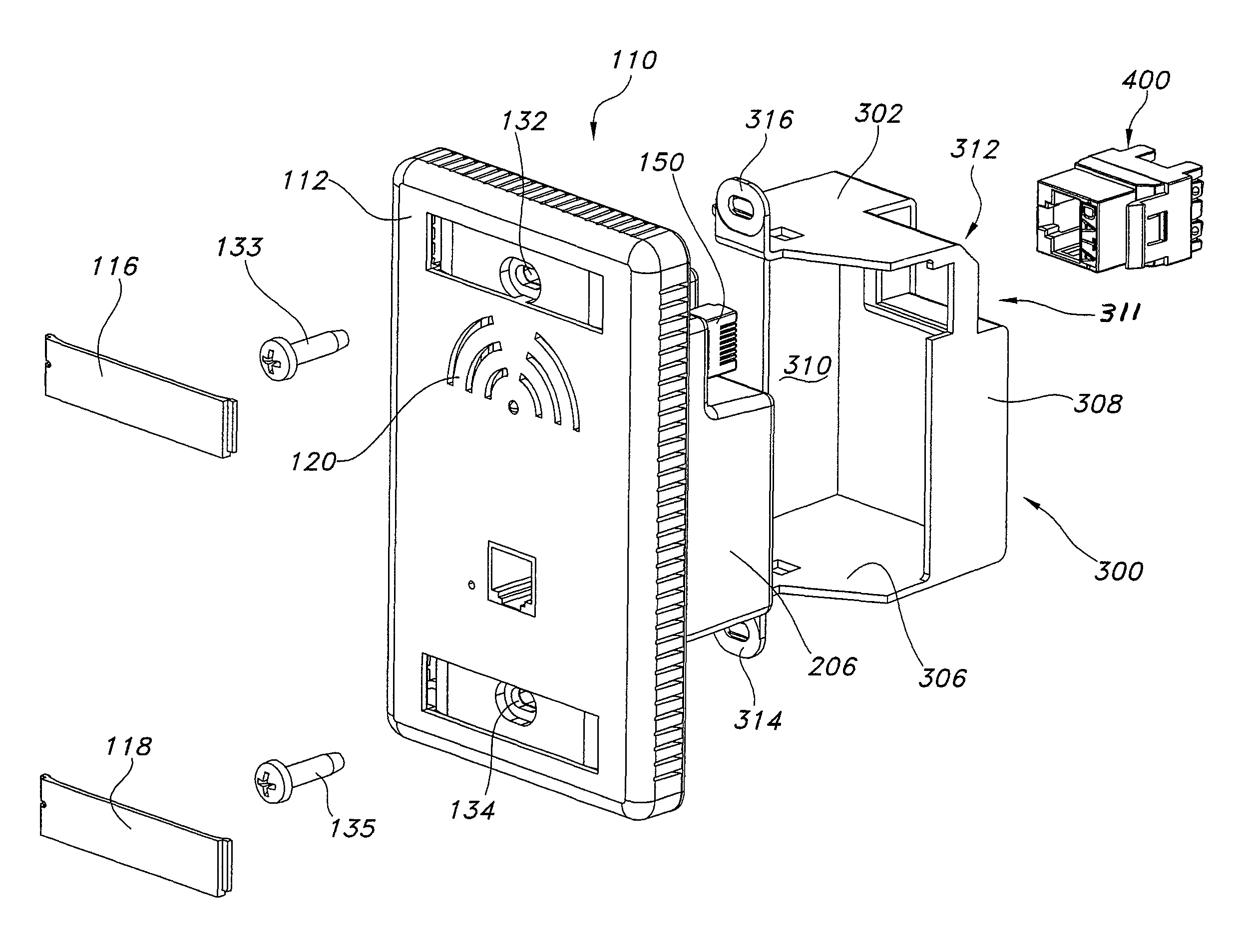
Wireless access point
InactiveUS20070254714A1Good space utilizationFacilitatesInterconnection arrangementsDevices with wireless LAN interfaceFacilitated communicationPower control
An access point device and access point system support wireless and wired communications. The access point includes a front face and a rear housing sized to fit within a conventional wall box, e.g., a single gang box. The electrical components associated with the access point device include a plurality of printed circuit boards that are configured in an H-shaped or U-shaped manner, such that they fit within the rear housing. Interface members are provided to facilitate communications between and among the printed circuit boards. At least one jack is provided in the front face of the access device for wired communication, and a plug is outwardly directed from the rear housing to facilitate network connection. Power for the access point device is supplied over a cable or conduit that engages the outwardly directed plug using Power-over-Ethernet (PoE) technology. The printed circuit boards include circuitry for managing operation of the access device and, in exemplary embodiments, includes power control circuitry to moderate potential heat generation.
Owner:ORTRONICS INC
Dynamic performance monitoring of long slender structures using optical fiber strain sensors
A method is described using optical fiber technology to measure the vibration characteristics of long slender structures subjected to dynamic disturbances imposed by water or wind generated loads. The method is based on making bending strain measurements at selected locations along the length of long slender structures such as marine risers or large ropes using fiber optics technology including Optical Time Domain Reflectometry and Bragg diffraction gratings. Engineering interpretation of information obtained from bending strains determines the vibration characteristics including frequency, amplitude, and wave length. Maximum bending strain measurements assess pending structural damage. One application is measurement of vortex induced vibrations (VIV) response of marine risers. The fiber optics based method is also applicable to the measurement of the bending characteristics of spoolable pipe using plastic optical fibers which can be interpreted to assess the pipe structural integrity and to prevent lock-up during deployment into a small diameter annulus.
Owner:WILLIAMS JERRY GENE
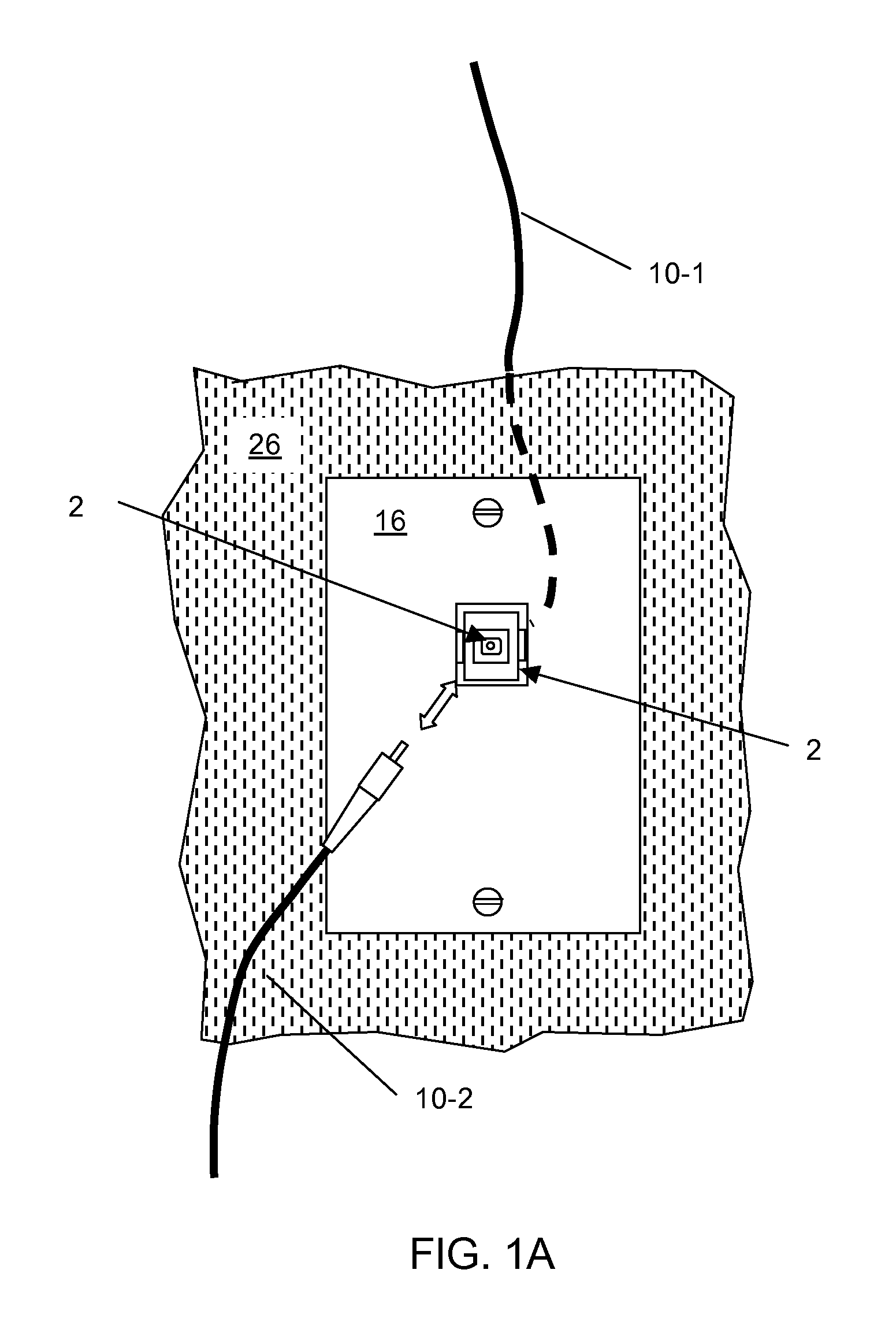
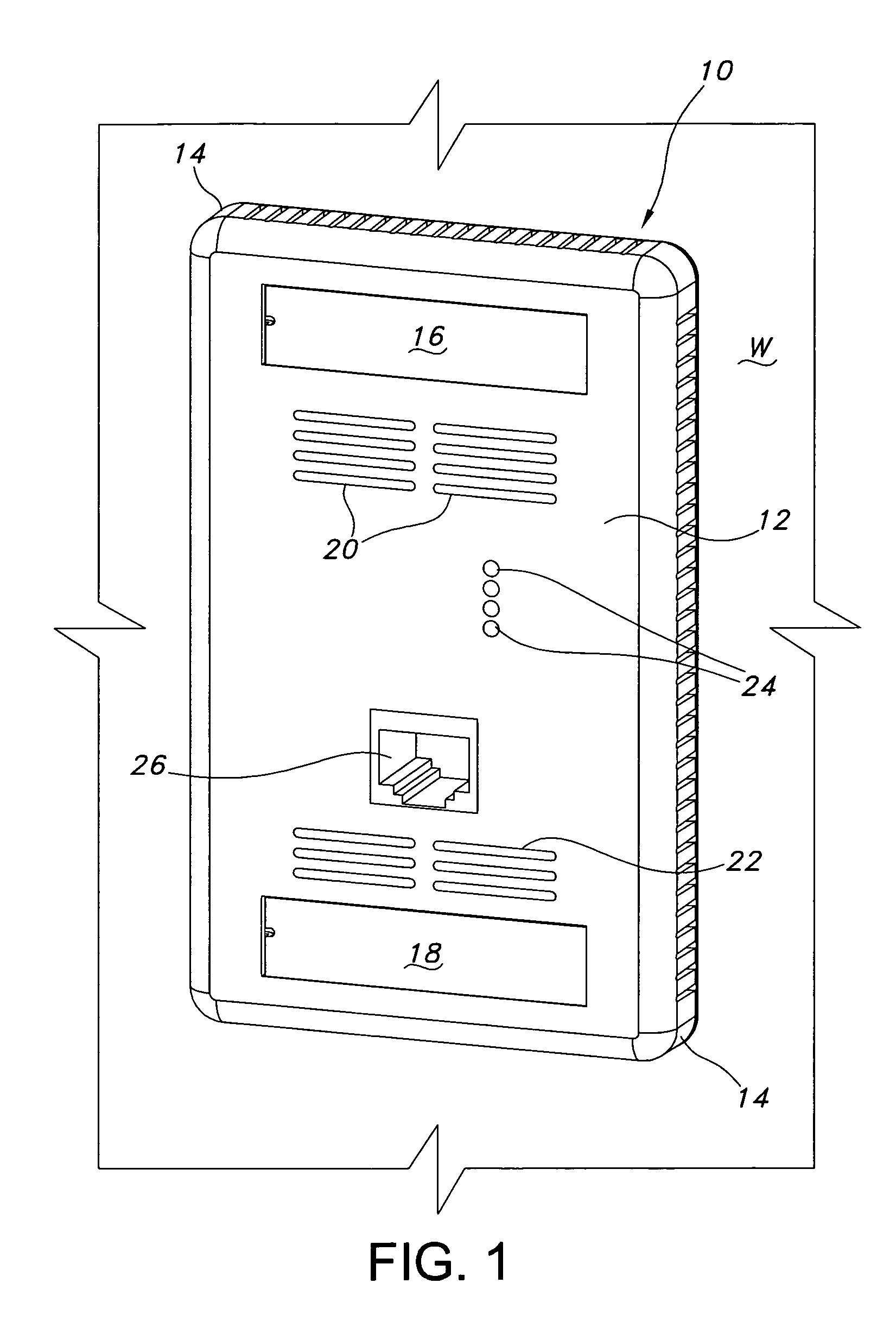
Electrical receptacle with open corner region
InactiveUS7734038B2Facilitate electrical communicationIncrease contactInterconnection arrangementsCouplings bases/casesElectrical connectionElectrical devices
An electrical receptacle with an open corner region facilitates electrical connection between an electrical device positioned in the receptacle and a conduit, cable or like wiring that passes through the open corner region. The open corner region is defined by a side wall, top face and rear wall of the receptacle. The receptacle is particularly adapted for use with electrical devices that include a connector that aligns with the open corner region, e.g., an access point.
Owner:ORTRONICS INC
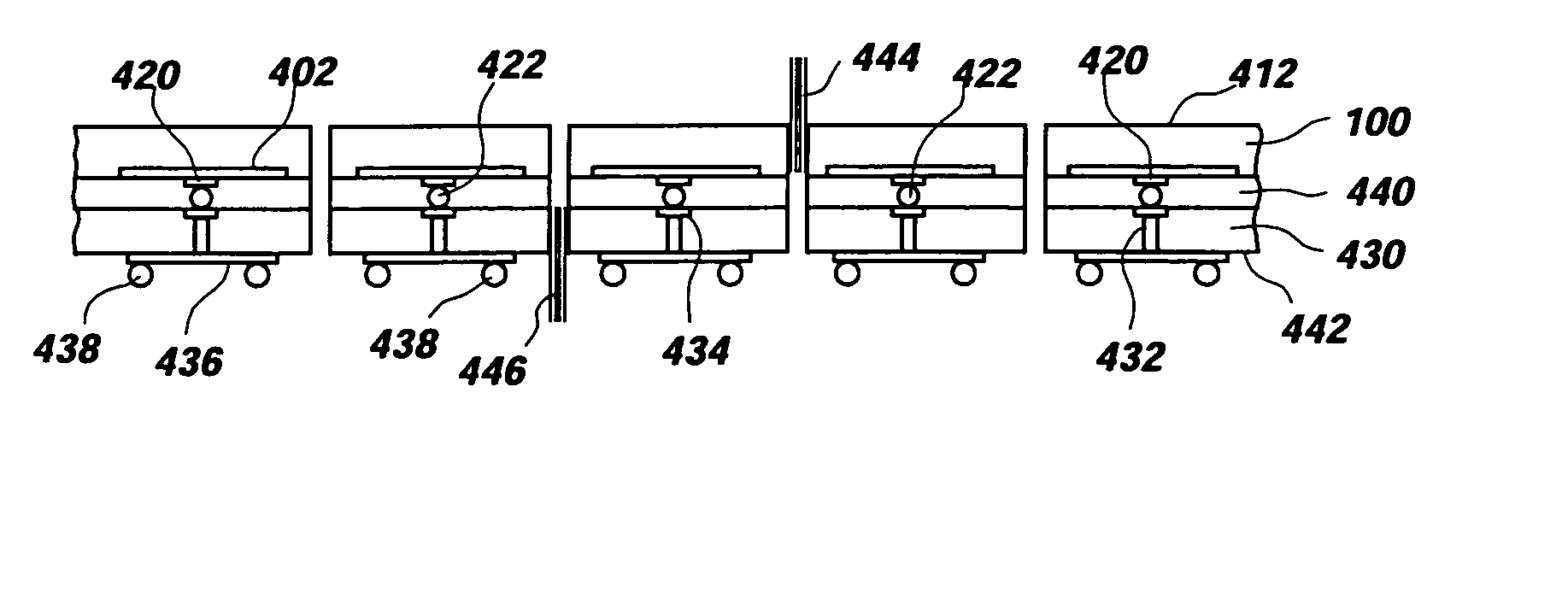
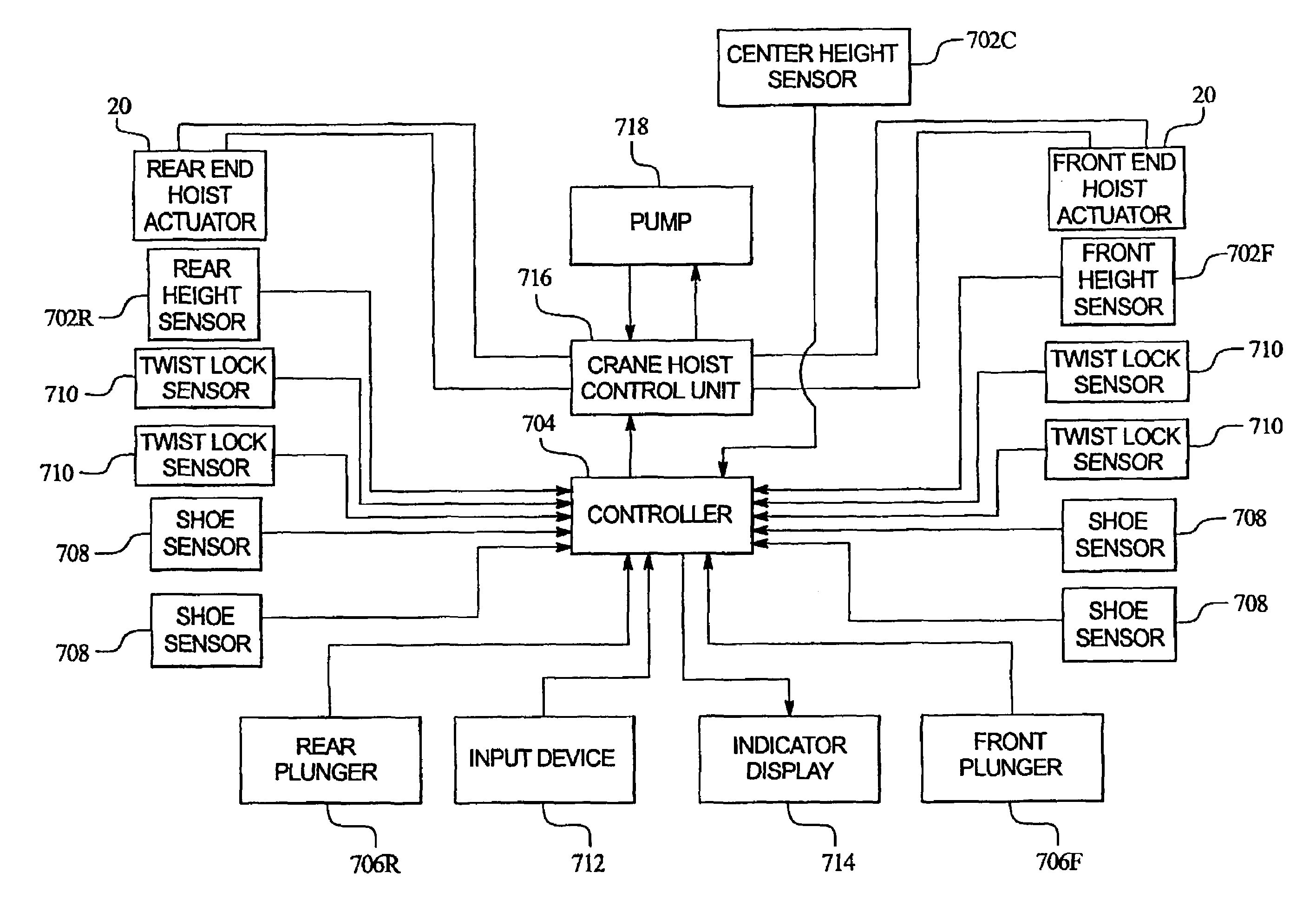
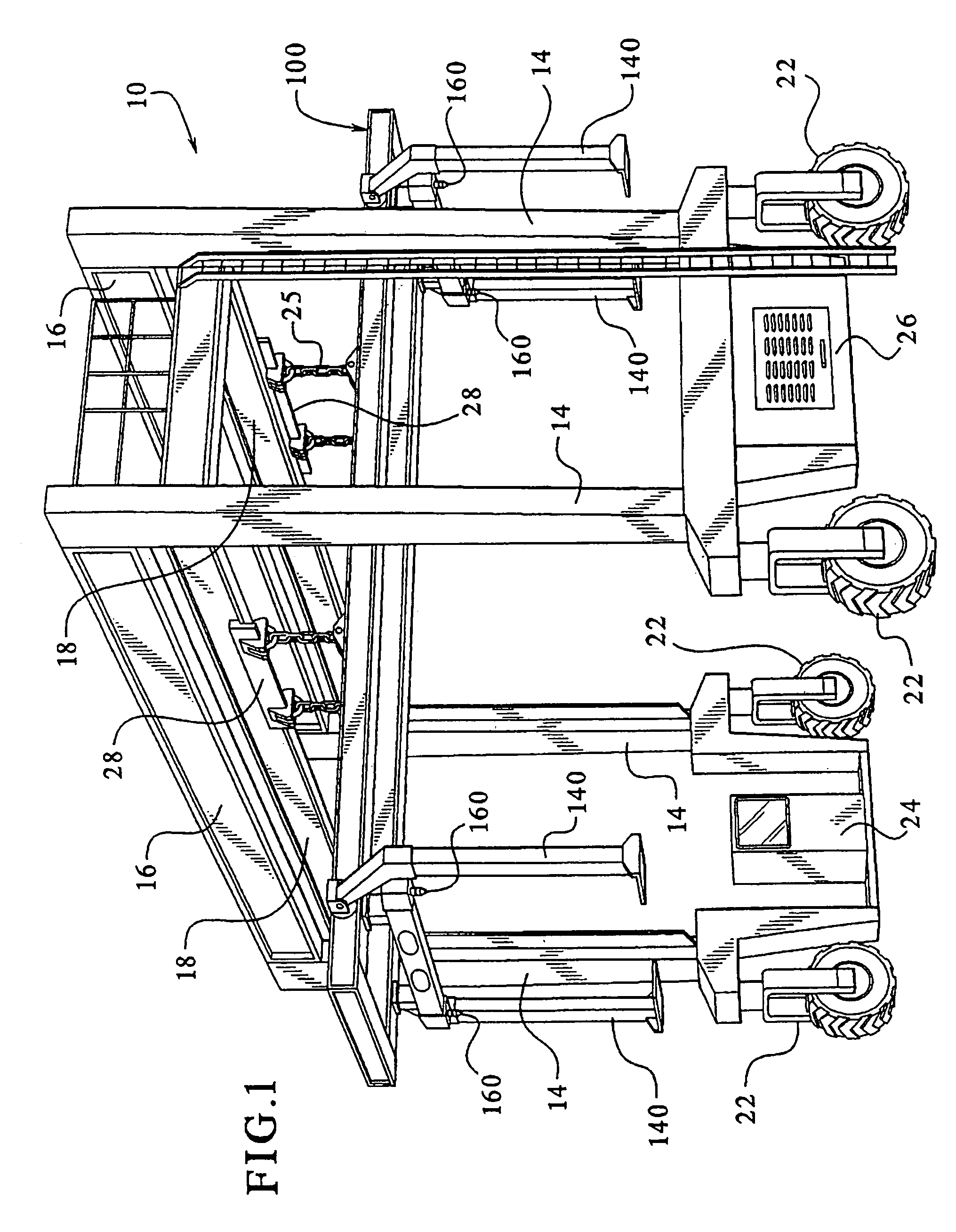
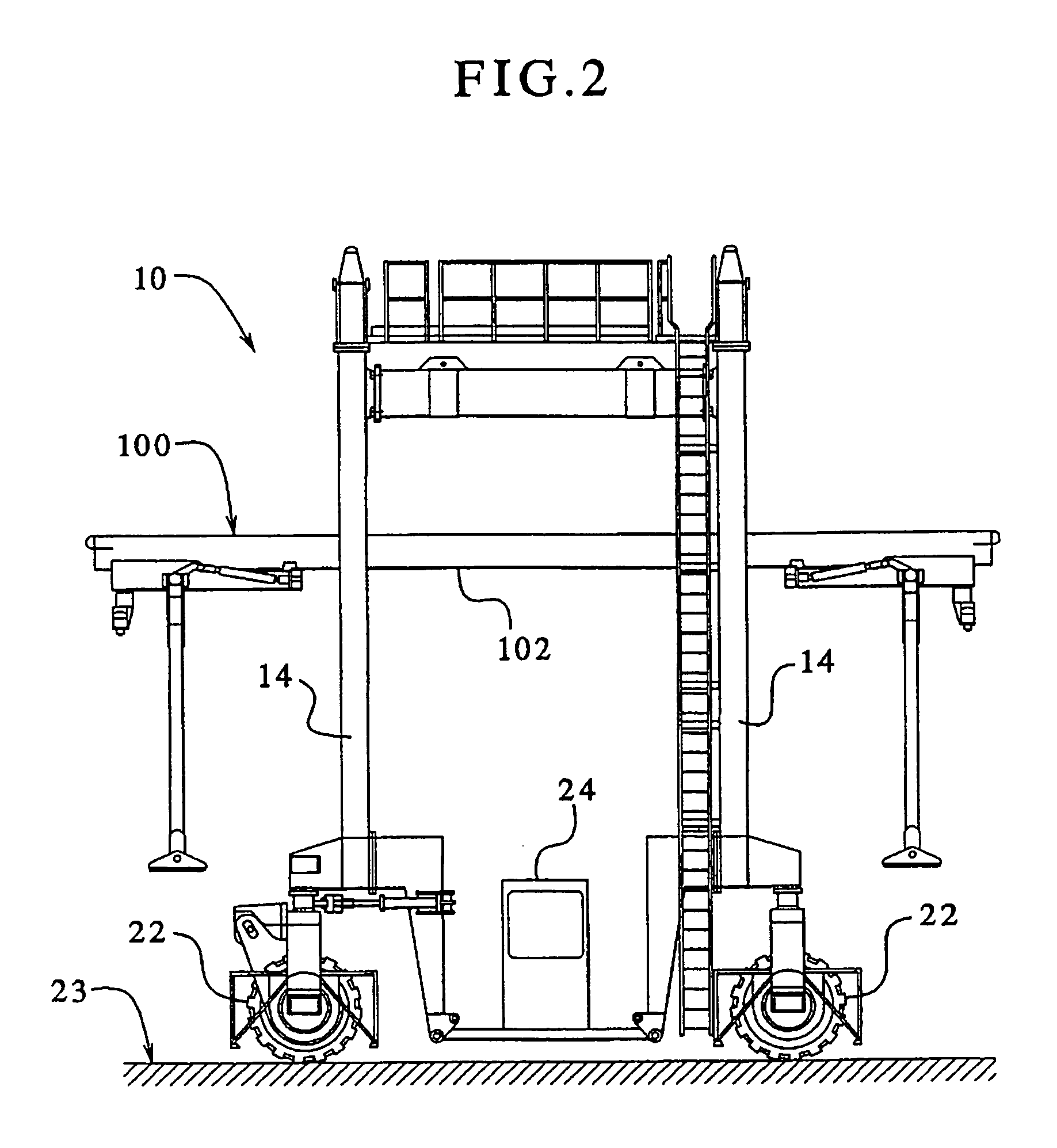
Grappler control system for a gantry crane
InactiveUS6968963B1Potential damageExtended reaction timeTrolley cranesThin material handlingVertical motionGantry crane
A system and process are provided for controlling motion of a grappler of a gantry crane to avoid damaging an object to be lifted. In an embodiment, a speed of grappler movement is automatically reduced when in close proximity to the object. Furthermore, the grappler automatically stops when positioned appropriately to permit a latching mechanism to engage the object for lifting. Normal speed grappler motion is restored when the latching mechanism is fully engaged. In a particular embodiment, the grappler includes a plurality of height sensors at various positions along the grappler to determine the respective height of the grappler above a top of the object. Vertical motion of front and rear ends of the grappler are independently actuated and controlled to permit appropriate control when the grappler and / or the object are not level.
Owner:MI JACK PRODS
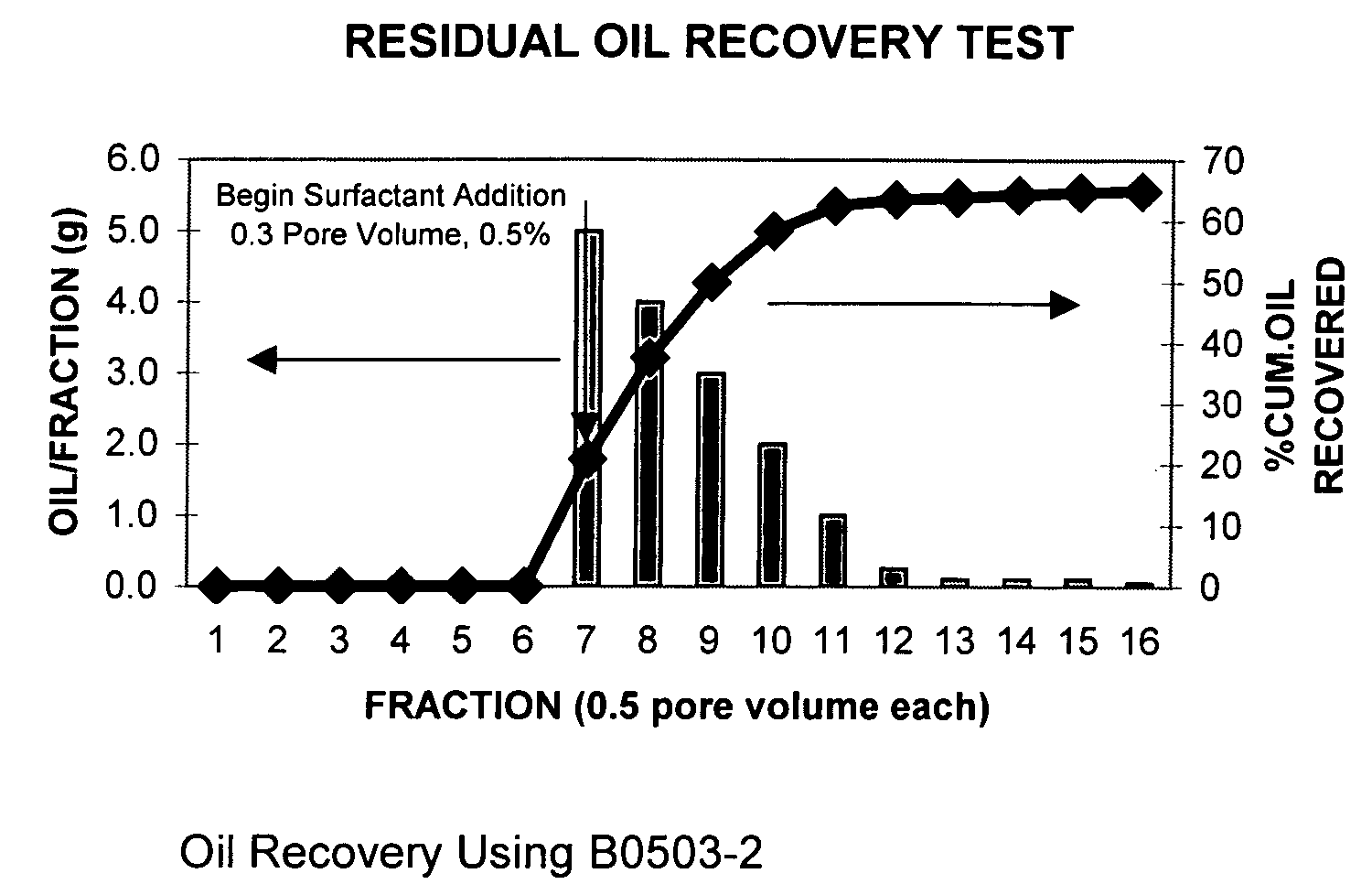
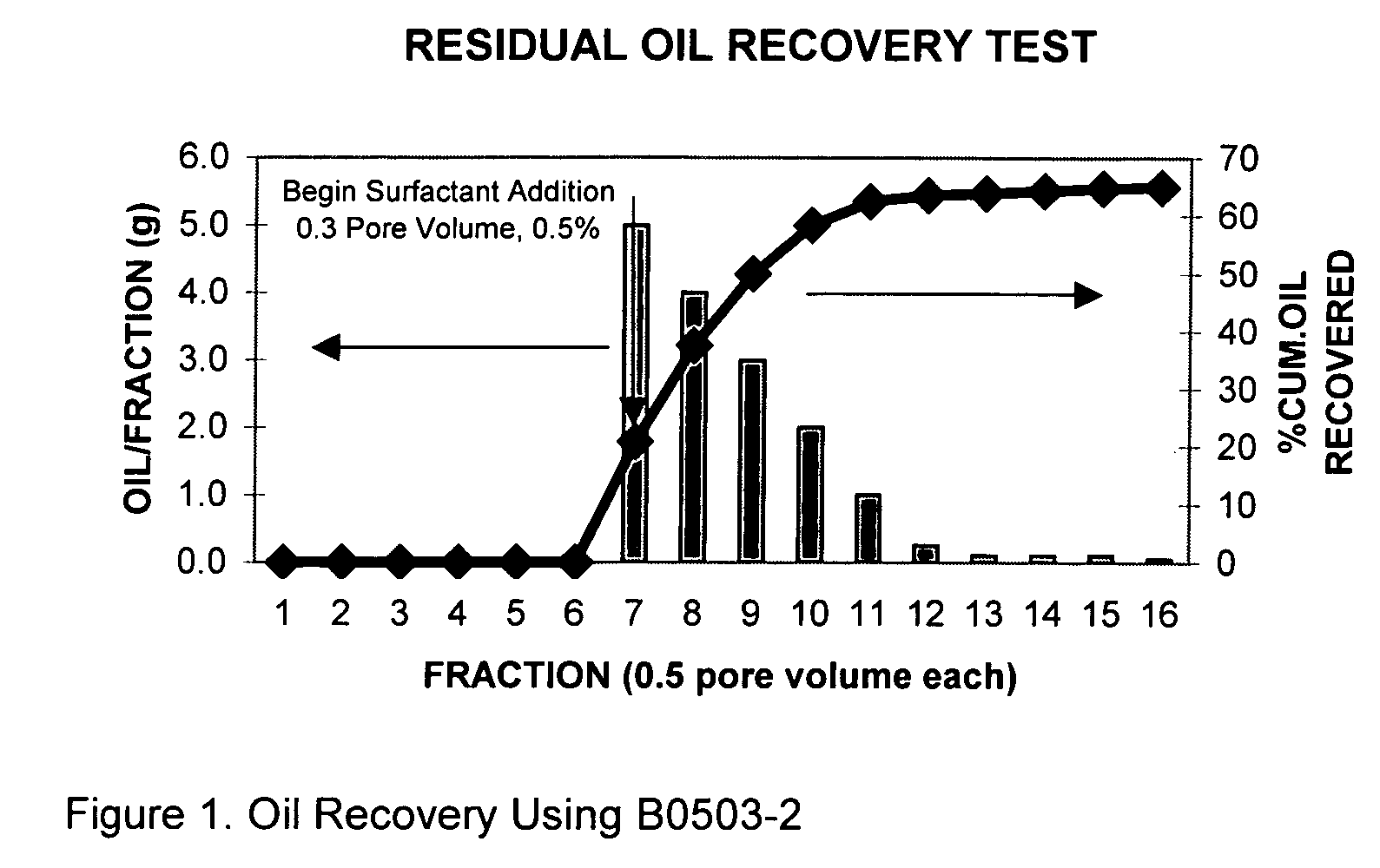
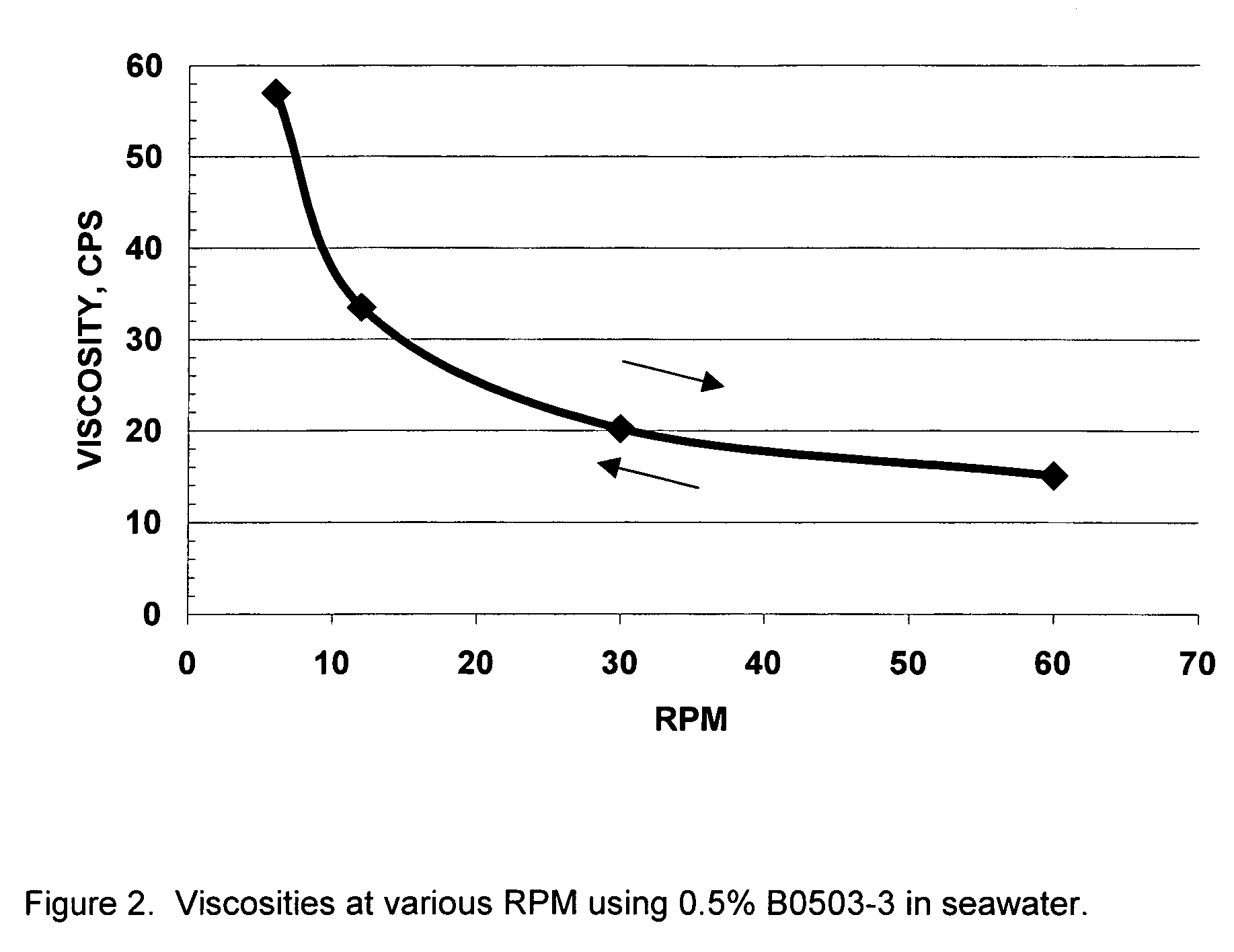
Process for oil recovery employing surfactant gels
Owner:OIL CHEM TECH
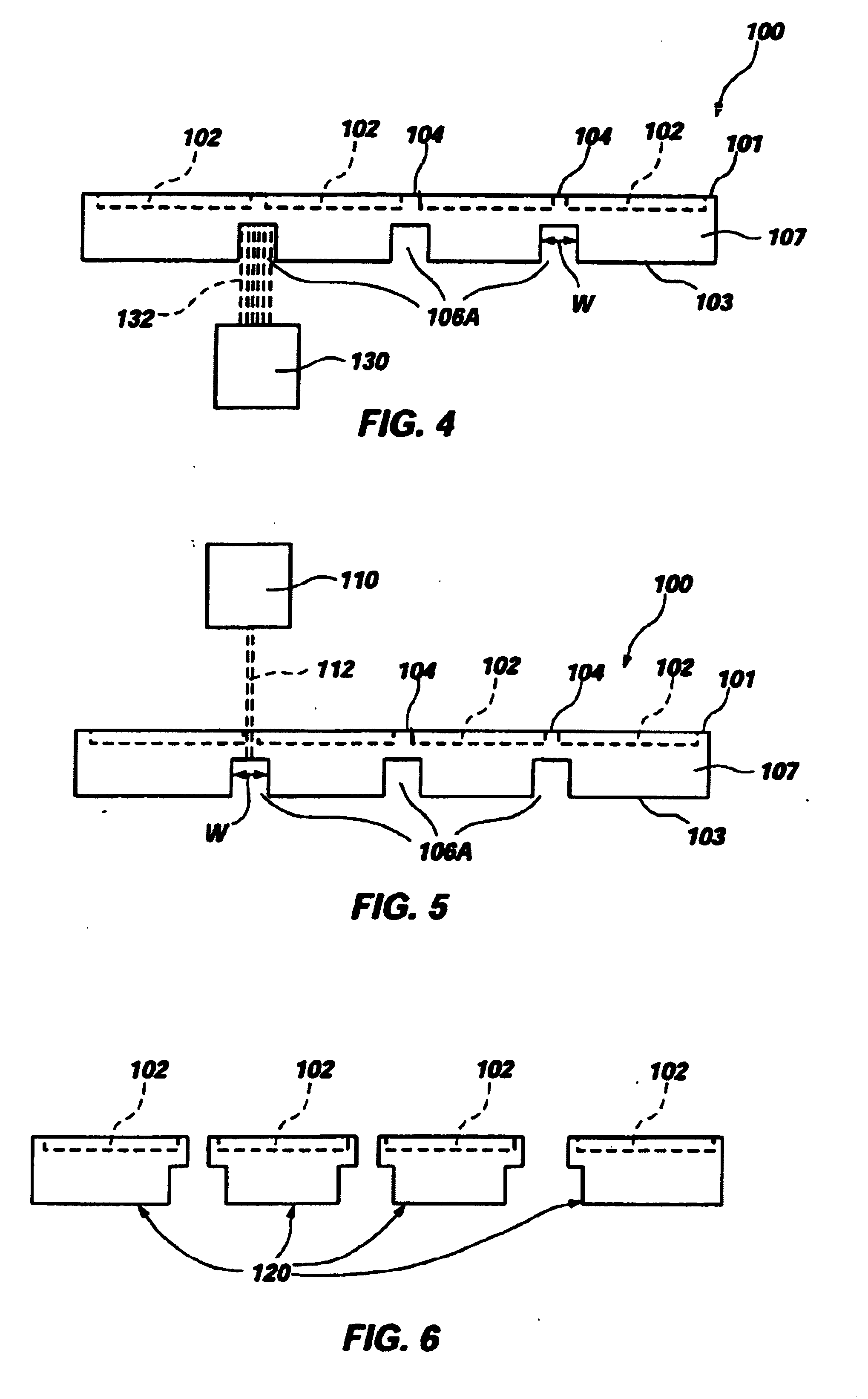
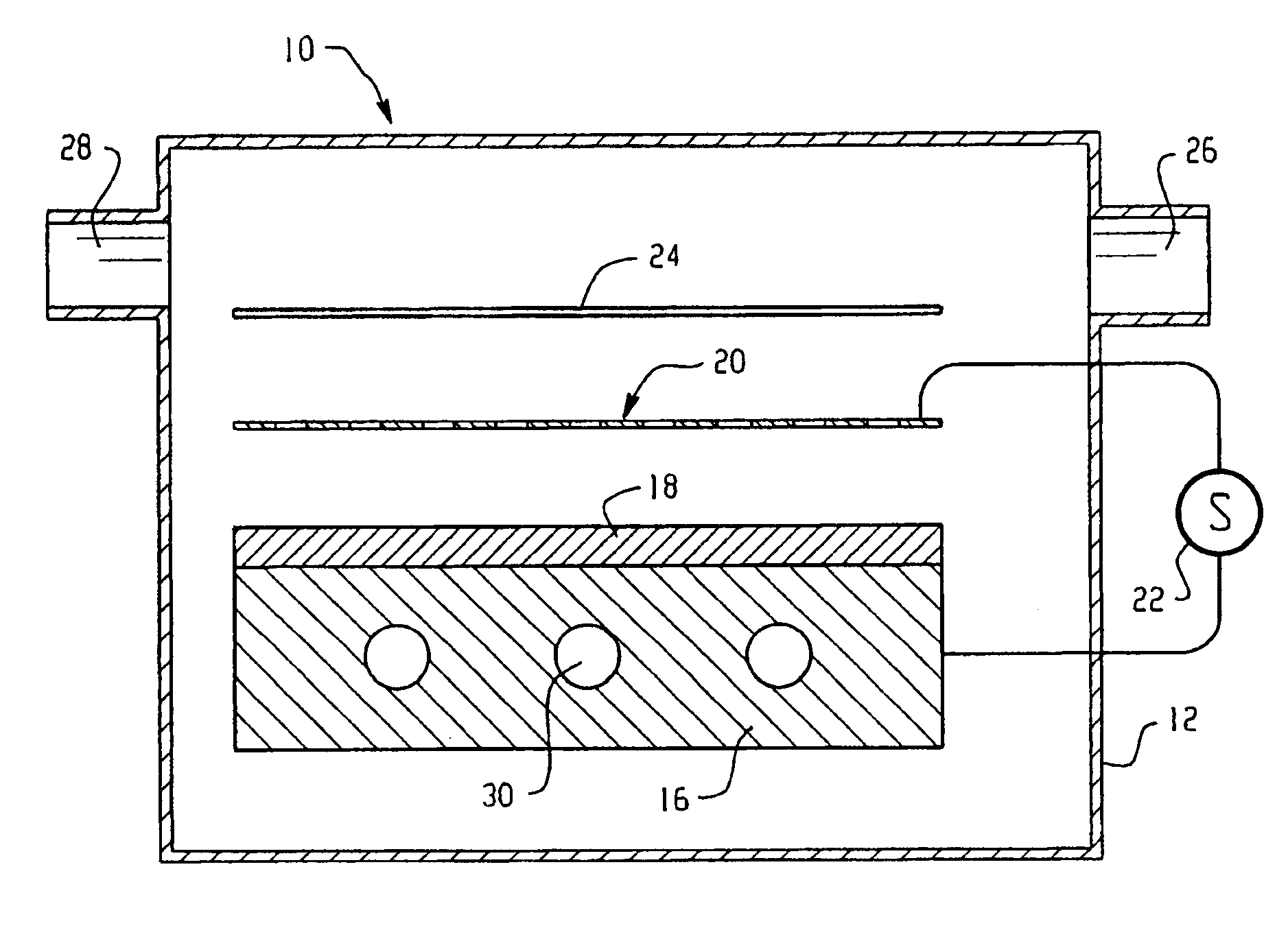
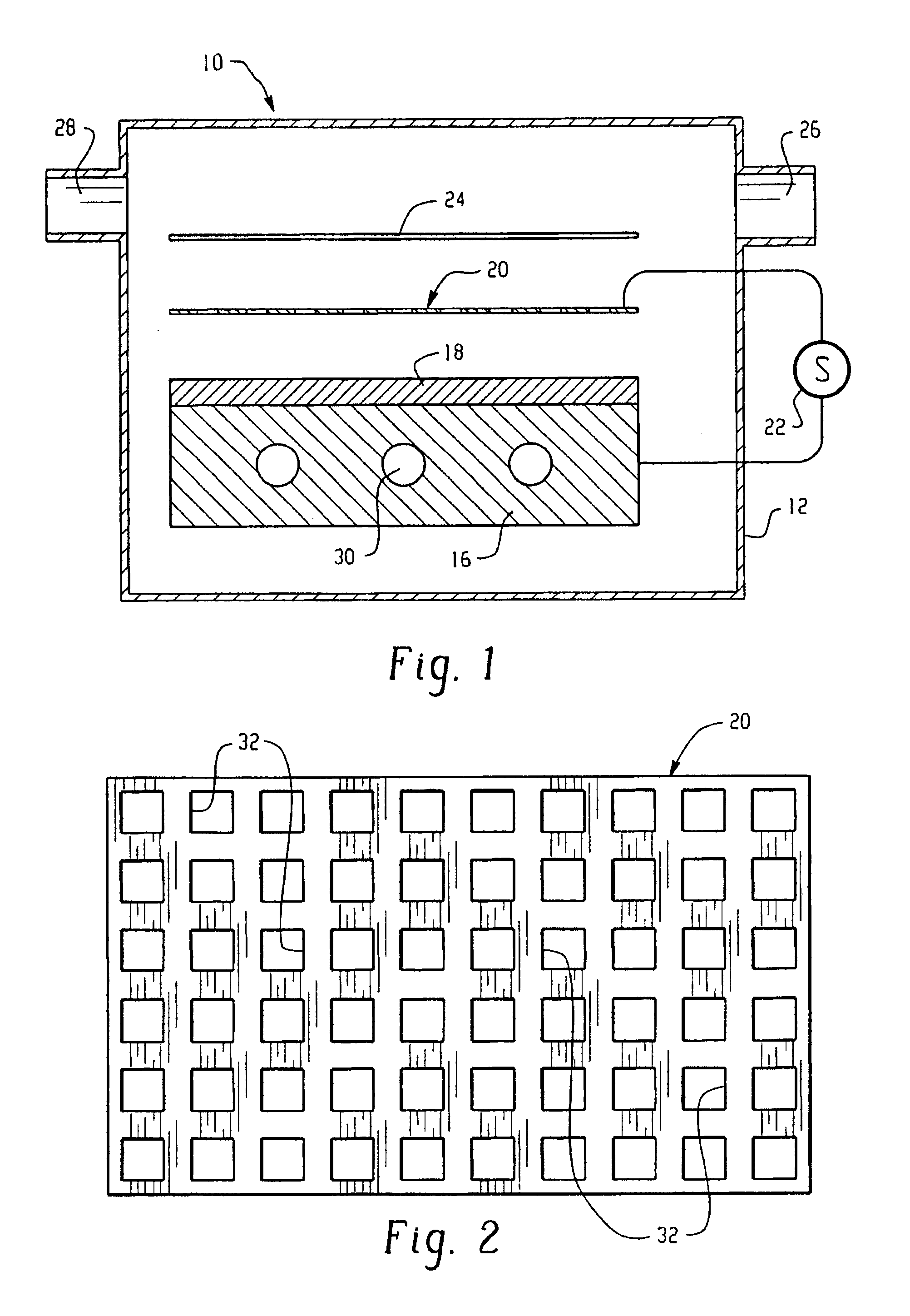
Dielectric barrier discharge apparatus and process for treating a substrate
InactiveUS6664737B1Improve responseEasy dischargeElectric discharge tubesElectric arc lampsPlanar electrodeOptoelectronics
A dielectric barrier discharge apparatus for treating a substrate includes a first planar electrode; a dielectric layer disposed on a surface of the first planar electrode; a porous planar electrode spaced above and in a parallel plane with the dielectric layer, wherein the porous planar electrode has a geometric transmission factor greater than 70 percent; and a power supply in electrical communication with the first electrode and the second electrode. A process for treating a substrate includes exposing the substrate surface to reactants produced by the dielectric barrier discharge apparatus.
Owner:AXCELIS TECHNOLOGIES
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com